Volume overload and ascites, or the accumulation of fluid in the abdomen, is a debilitating manifestation of chronic liver disease and portal hypertension that is associated with reduced survival and quality of life.1,2 In patients with compensated cirrhosis, ascites occur in 5%–10% per year, and its onset is a key indicator of hepatic decompensation and progression of liver disease. 3 The presence of volume overload and, specifically, ascites increases the risk of additional complications, including malnutrition, infection, electrolyte imbalance, and hepatorenal syndrome.
CRITERIA FOR MEDICAL TREATMENT OF VOLUME OVERLOAD
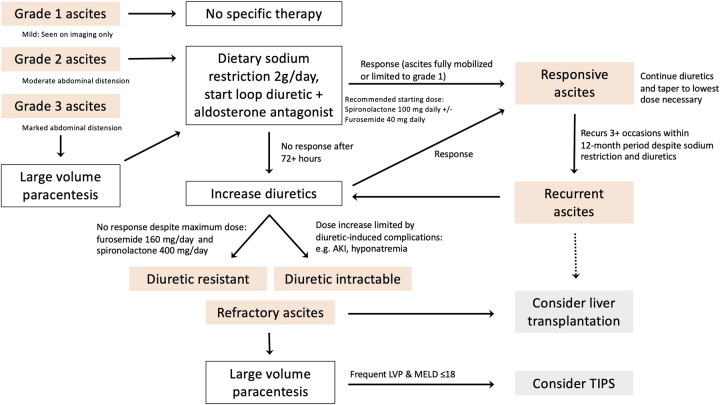
Volume overload in patients with cirrhosis most commonly presents as ascites but can also manifest as hepatic hydrothorax (right or left-sided) or peripheral or generalized edema, for which the management is similar. The first-line therapy for symptomatic volume overload is dietary sodium restriction, with a goal of 2 grams of sodium or less per day to achieve negative sodium balance and fluid loss (Figure 1). Only patients with severe hyponatremia (Na < 125 mEq/L) should be placed on a fluid restriction. In addition to sodium restriction, most patients also require diuretic therapy. The combination of aldosterone antagonists and loop diuretics is the mainstay of treatment, with an initial recommended dose of spironolactone at 100 mg daily and furosemide at 40 mg daily. For the first episode of ascites, spironolactone may be initiated as monotherapy, with the addition of loop diuretic for incomplete response or recurrent ascites. Spironolactone may be uptitrated in a stepwise manner to 400 mg daily and furosemide to 160 mg daily to reach maximal doses, as tolerated. Bumetanide and torsemide can be considered alternative loop diuretics if furosemide is not adequately effective. Patients with chronic kidney disease may require lower levels of aldosterone antagonists and higher levels of loop diuretics. Most patients respond to diuretic therapy — however, 20%–40% experience adverse effects from diuretic therapy, such as gynecomastia (spironolactone), muscle cramps, HE, electrolyte imbalance, and acute kidney injury. Close monitoring of electrolytes and renal function is essential, particularly during the first weeks of treatment.
FIGURE 1.
Suggested algorithm for management of ascites in cirrhosis. Abbreviation: AKI, acute kidney injury; TIPS, transjugular intrahepatic portosystemic shunt.
Refractory ascites, or ascites that is unable to be mobilized or recurs early after large-volume paracentesis despite diuresis and sodium restriction, occurs in 5%–10% of patients with cirrhosis and ascites and portends poor survival of 50% at 6 months. 4 Diuretic resistance is defined as persistent ascites despite maximal doses of diuretics, whereas ascites is considered diuretic-intractable when side effects prevent the use of maximal doses of diuretics. Large volume paracenteses (LVP), that is, the removal of >5 liters of ascites, can help to manage ascites in such cases.
APPROACH TO PARACENTESIS
A diagnostic paracentesis should be performed for all patients with new-onset ascites to confirm the etiology. Ascites due to cirrhosis and portal hypertension is typically characterized by an elevated serum albumin ascites gradient of >1.1 g/dL and an ascitic fluid protein <2.5 g/dL. Upon suspicion of infection, fluid cell count and culture should be sent to rule out spontaneous bacterial peritonitis (SBP), a serious complication of ascites that requires prompt identification and inpatient treatment to prevent undue mortality. Patients with ascites and cirrhosis being admitted to the hospital should undergo diagnostic paracentesis even in the absence of symptoms or signs of infection, as SBP can be associated with minimal or no symptoms of typical infection and may present with only acute kidney injury, encephalopathy, or other signs of hepatic decompensation. 5 SBP is diagnosed by a fluid polymorphonuclear leukocyte count of > 250/mm3, with or without positive fluid cultures. Ascitic fluid culture and sensitivities can help guide antibiotic choice for the patient at hand, as well as for future patients, that is, SBP prophylaxis and culture-negative SBP.
Therapeutic paracentesis is the first-line treatment for tense ascites, and serial LVP is often needed in cases of refractory ascites. Albumin infusion is recommended at the time of LVP, at a dose of 6–8 g per liter removed, to preserve the effective circulating volume and mitigate the risk of postparacentesis circulatory dysfunction, including renal dysfunction and potentially hepatorenal syndrome. Twenty-five percent albumin is preferred to 5% albumin to reduce volume and infusion time. The risk of postparacentesis circulatory dysfunction may increase when >8 liters of fluid are removed during LVP. Albumin infusion should also be considered for smaller volume paracentesis (<5 L) in patients with hypotension, hyponatremia, and/or the presence of acute kidney injury. Correction of elevated INR or platelet count by transfusion is not routinely recommend before paracentesis, given the overall low risk of bleeding and not insignificant risk of transfusion-related adverse effects.
TRANSJUGULAR INTRAHEPATIC PORTOSYSTEMIC SHUNT AND ALTERNATIVE THERAPIES
For selected patients, TIPS can be an effective option for refractory ascites.6,7 The TIPS reduces portal pressure and refills the effective arterial blood volume, with ascites able to be cleared in ~80% of patients. 8 However, the associated potential complications of liver failure, HE, and heart failure can be limiting. Transthoracic echocardiogram, which may reveal pathology, such as cirrhotic cardiomyopathy, pulmonary hypertension, or congestive heart failure, should be performed as part of the evaluation for TIPS. Conventionally, patients with MELD of ≥18 have been considered suboptimal candidates for this procedure, as well as those with advanced age, cardiovascular disease, and sarcopenia, due to a higher risk of such complications. 9 The use of smaller diameter TIPS (8–10 mm) has been associated with a lower risk of post-TIPS encephalopathy. 10
Alternative therapies, such as permanent indwelling peritoneal catheters, have not been well established due to low-quality studies and an average infection rate of 12.7%. 11 Devices may have an emerging role in the management of ascites— for example, Alfapump, an implantable battery-powered pump that transports ascites from the peritoneum to the bladder and has been shown to reduce the need for paracentesis and improve quality of life and nutrition, although it is not currently available in North America outside of clinical trials. 12
SUMMARY
Ascites is a defining event in the progression of chronic liver disease, with significant medical and psychological consequences. The management of ascites can be approached in a stepwise manner, from sodium restriction and diuretic therapy, to paracentesis and TIPS. Patients with cirrhosis and persistent ascites, despite these available medical therapies, should be considered for liver transplant evaluation.
Footnotes
Abbreviations: LVP, large volume paracenteses; SBP, spontaneous bacterial peritonitis.
Contributor Information
Allison J. Kwong, Email: ajk@stanford.edu.
Joshua Norman, Email: normanjs@stanford.edu.
Scott W. Biggins, Email: bigginssw@upmc.edu.
FUNDING INFORMATION
Allison J. Kwong is supported in part by the AASLD Foundation and the National Institutes of Health (K23AA029197).
CONFLICTS OF INTEREST
The authors have no conflicts to report.
REFERENCES
- 1.Biggins SW, Angeli P, Garcia-Tsao G, Ginès P, Ling SC, Nadim MK, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74:1014–1048. [DOI] [PubMed] [Google Scholar]
- 2.Solà E, Watson H, Graupera I, Turón F, Barreto R, Rodríguez E, et al. Factors related to quality of life in patients with cirrhosis and ascites: Relevance of serum sodium concentration and leg edema. J Hepatol. 2012;57:1199–1206. [DOI] [PubMed] [Google Scholar]
- 3.D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies. J Hepatol. 2006;44:217–231. [DOI] [PubMed] [Google Scholar]
- 4.Moreau R, Delègue P, Pessione F, Hillaire S, Durand F, Lebrec D, et al. Clinical characteristics and outcome of patients with cirrhosis and refractory ascites. Liver Int. 2004;24:457–464. [DOI] [PubMed] [Google Scholar]
- 5.Kim JJ, Tsukamoto MM, Mathur AK, Ghomri YM, Hou LA, Sheibani S, et al. Delayed paracentesis is associated with increased in-hospital mortality in patients with spontaneous bacterial peritonitis. Am J Gastroenterol. 2014;109:1436–1442. [DOI] [PubMed] [Google Scholar]
- 6.Boyer TD, Haskal ZJ, American Association for the Study of Liver Diseases . The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension: Update 2009. Hepatology. 2010;51:306. [DOI] [PubMed] [Google Scholar]
- 7.Boike JR, Thornburg BG, Asrani SK, Fallon MB, Fortune BE, Izzy MJ, et al. North American Practice-based recommendations for transjugular intrahepatic portosystemic shunts in portal hypertension. Clinical Gastroenterology and Hepatology. 2022;20:1636–1662.e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan HK, James PD, Sniderman KW, Wong F. Long-term clinical outcome of patients with cirrhosis and refractory ascites treated with transjugular intrahepatic portosystemic shunt insertion. J Gastroenterol Hepatol. 2015;30:389–395. [DOI] [PubMed] [Google Scholar]
- 9.Shin DS, Vo H, Johnson G, Pichler R, Biggins SW. Transjugular Intrahepatic portosystemic shunts in high-risk patients. Digest Dis Intervent. 2020;04:148–156. [Google Scholar]
- 10.Bosch J. Small diameter shunts should lead to safe expansion of the use of TIPS. J Hepatol. 2021;74:230–234. [DOI] [PubMed] [Google Scholar]
- 11.Macken L, Hashim A, Mason L, Verma S. Permanent indwelling peritoneal catheters for palliation of refractory ascites in end-stage liver disease: A systematic review. Liver Int. 2019;39:1594–1607. [DOI] [PubMed] [Google Scholar]
- 12.Bureau C, Adebayo D, Chalret de Rieu M, Elkrief L, Valla D, Peck-Radosavljevic M, et al. Alfapump® system vs. large volume paracentesis for refractory ascites: A multicenter randomized controlled study. J Hepatol. 2017;67:940–949. [DOI] [PubMed] [Google Scholar]