Abstract
Human-caused climate change has increased the average temperature of the Earth by over 1°C since the 19th century with larger increases expected by 2100 due to continued human influence. This change in mean ambient temperature has had nonlinear effects, resulting in more high temperature extremes, i.e., heat waves, that have increased in frequency, duration, and magnitude. Additional occurrences of humid heatwaves have significantly affected human health due to the physiological strain associated with a relative inability for evaporative cooling. Inability to efficaciously cool the body, whether during passive heat exposure or physical activity, not only leads to elevated core temperatures but also places strain on the cardiovascular system, often exacerbating age-related co-morbidities. As part of the PSU HEAT (Pennsylvania State University – Human Environmental Age Thresholds) Project, a progressive environmental strain protocol has been developed to determine critical environmental limits – combinations of ambient temperature and humidity -- associated with uncompensable heat stress and intractable rises in core temperature (Tc). These human heat balance thresholds, well below those originally theorized by climatologists, have been surpassed in recent heatwaves and be exceeded on a more regular basis in the future, providing additional impetus to the urgency of adaptative measures and climate change mitigation.
Keywords: climate change, critical environmental limits, wet-bulb temperature, heatwaves, heat-health
Introduction
Earth’s average temperature has increased ~1.1°C since 1900 and is projected to further rise by 1.4 – 4.4°C by 2100 given continued human-caused climate change (1). While regional heterogeneity exists in the magnitude of temperature increase across the globe, the majority of land areas on Earth have experienced new heat extremes due to human-induced impacts of elevated greenhouse gas emissions and associated radiative forcing (1). The increase in global temperature is not simply relegated to the mean but occurs throughout the entire distribution range of temperatures. This temperature distribution shift not only increases the probability of extreme heat due to a rightward shift of the temperature distribution, but also, nonlinear effects may further exacerbate extreme heat events (2). Extreme heat events, or heatwaves, have increased in frequency, duration, and magnitude over the observational record (3) and will continue to increase in the future (4) (Figure 1). Other research has shown that these heatwaves are occurring earlier which cuts down on heat acclimatization time (5).The relatively new and emerging field of climate attribution has proven useful in linking climate change to singular heatwave events. For example, the heatwave that engulfed the Pacific Northwest of the United States and Canada in 2021 would not have been possible without the influence of climate change (6). Similarly, the April – May 2022 heatwave that devastated Pakistan and India was made 30 times more likely to occur because of human-induced climate change (7).
Figure 1.
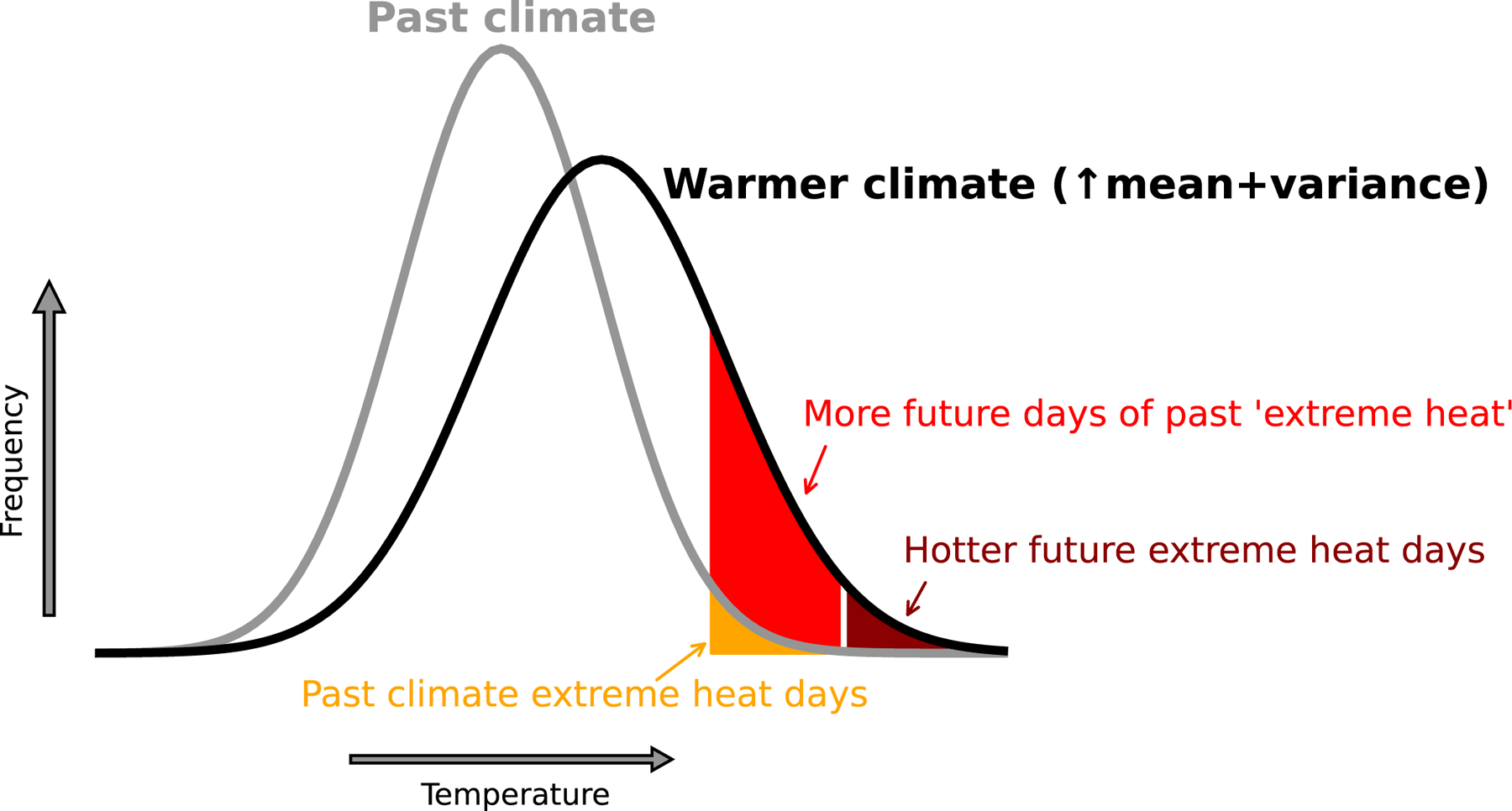
Schematic representation of changing temperature distributions with climate change and its effect on extreme heat events.
Climate impacts on health
Climate change is the largest threat to planetary health (8). One direct and specific impact it will have on humans is the rise in warm season temperatures and heat extremes and their subsequent influence on health. Heat is the number one weather-related killer in the United States (9) and contributes to a significant number of deaths across the world. Several epidemiological studies have shown that heatwaves exacerbate direct heat-related morbidity and mortality (10) and are also associated with increased cardiovascular, respiratory, and renal illnesses (11). This risk is heightened in vulnerable populations such as young children, the elderly, pregnant women, and outdoor laborers whose physiological dysfunction, generalized lack of behavioral adaptation, forced exposure duration, or combinations thereof, present roadblocks to remaining heat-healthy (12). These detrimental heat-health effects most often result from heat production plus heat gain in excess of heat loss, resulting in increased body heat storage and elevated Tc. Past heatwaves, such as the 1995 Chicago, USA, 2003 European, 2010 Russian, 2015 India, and 2021 Pacific US and Canadian Northwest, have illustrated that prolonged exposure to heat, even in the absence of overt physical activity, can be deadly given the ambient environment’s impact on physiological strain on the body (13).
Humans can maintain thermal homeostasis in many environments of extreme heat via their tropically evolved thermoregulatory capabilities (14) (Figure 2). As heat builds in the body core, either through passive exposure to a hot environment or an increased metabolic rate (i.e., manual labor, exercise, etc.), there is an increase in blood flow directed to the skin. Secondary to an increased cardiac output coupled with redistribution of blood flow from renal and splanchnic vascular beds, blood is transferred toward the surface, and heat can be dissipated to the ambient environment via conduction and convection (dry heat loss). This process increases cardiorespiratory strain as cardiac output must increase in the absence of maintained or increased preload. The second, more efficient mechanism of cooling the body is through the activation of eccrine sweat glands to produce sweat and excrete it onto the surface of the skin. If that sweat is evaporated, the latent heat of vaporization cools the skin, provided that there is an adequate water vapor pressure gradient between the wetted skin surface and the ambient environment. However, fluid loss through sweating results in dehydration which can limit evaporative cooling and lead to increase cardiac strain and renal dysfunction if fluids are not adequately replenished (15).
Figure 2.
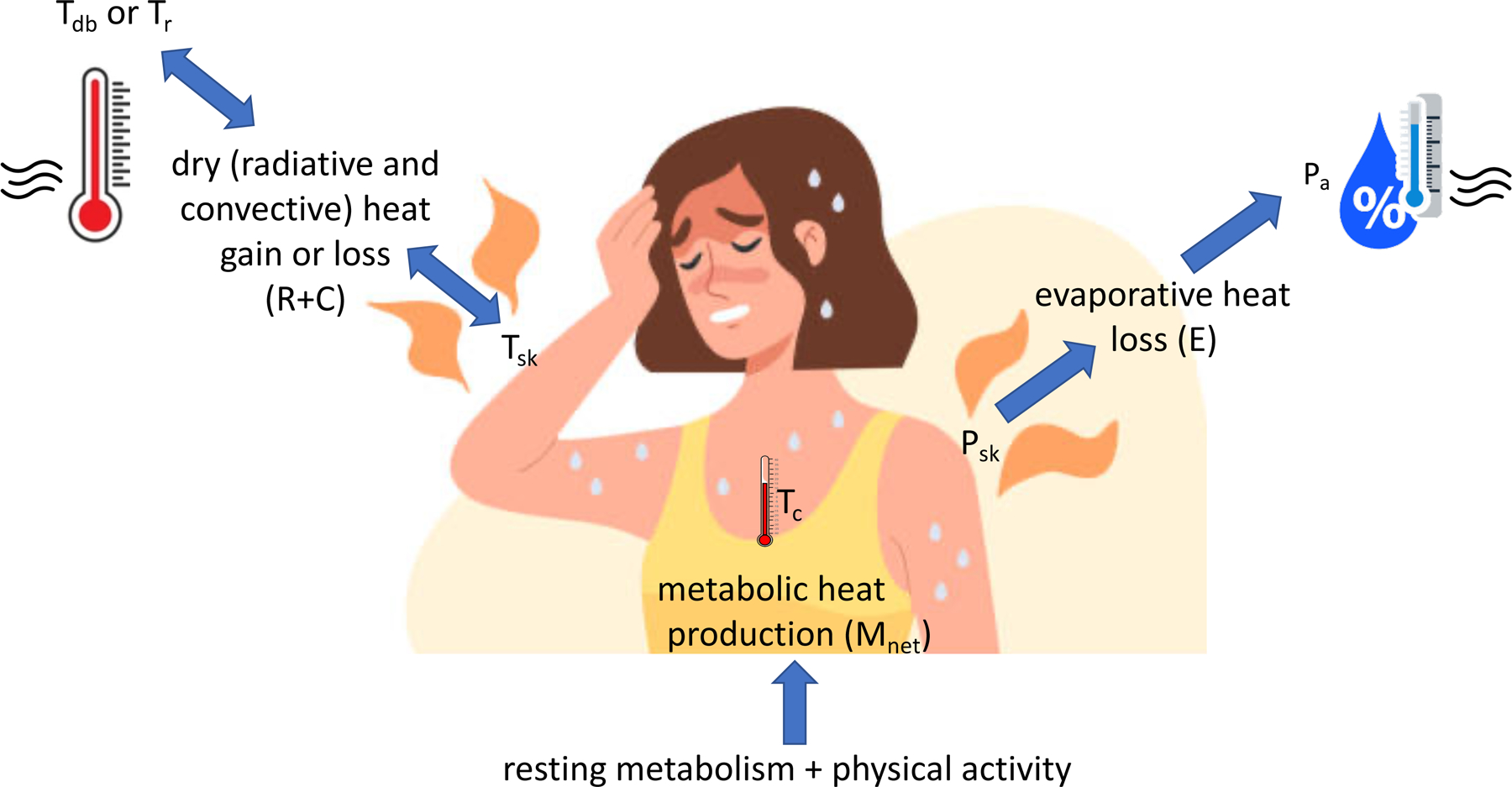
Simplified schematic of heat exchange between humans and their environment. Net metabolic heat production (Mnet) is the combination of resting heat production plus that associated with physical activity, minus any external work being performed. Dry heat exchange (R+C) is determined by the gradient between mean skin temperature (Tsk) and ambient dry-bulb temperature (Tdb) unless there is a significant source of radiant heat that elevated mean radiant temperature (Tr). Dry heat exchange is bidirectional. Evaporative heat exchange (E), on the other hand, is unidirectional (loss only) and is determined by the gradient between the water vapor pressure of the skin (Psk) and the ambient water vapor pressure (Pa). The sum of Mnet ± (R+C) − E determines heat storage, which in turn, determines core temperature (Tc).
Critical environmental limits
A wet-bulb temperature (Twb) of 35°C has been proposed as the theoretical physiological limit for human adaptability. This threshold was based on the fact that there would be no evaporative cooling possible from fully wetted skin which has a temperature of 35°C at Twb = 35°C (16). Only recently have wet-bulb temperatures exceeded this theoretical 35°C adaptability limit, but even then a Twb of 35°C been limited to just a few hours in extremely humid regions of South Asia and the Middle East (17). However, climate models have shown that this part of the world will experience prolonged periods of uncompensable humid heat stress in the future under “business-as-usual” climate forcing (18).
While the 35°C limit has become popular in the scientific literature and media over the past decade, it lacks physiological accuracy due to its assumptions and lack of incorporation of physiological principles such as evaporative efficiency. Moreover, it has not been empirically validated until recently. As part of the Pennsylvania State University - Human Environmental Age Thresholds (PSU HEAT) project, critical environmental limits -- combinations of dry-bulb temperature (Tdb) and ambient water vapor pressure (Pa) above which heat stress becomes uncompensable and a Tc equilibrium can no longer be maintained -- were determined from a large cohort of young, healthy men and women using a programmable environmental chamber with controlled temperature and humidity (19, 20).
In warm, humid environments characterized by Tdb ranging from 34°C to 40°C and relative humidity (RH) values above 50%, a mean critical Twb of ~31°C was found for metabolic heat production that mimicked the minimal activities of daily life (e.g., fidgeting, brushing teeth, self-care, etc.). This value was much lower than the theoretical 35°C limit of Sherwood and Huber (Figure 3). When metabolic rates were increased to those associated with light ambulatory activities (e.g., gardening, washing dishes, gentle walks), the mean critical Twb decreased further, to 27 – 28°C in the same ambient environments (not shown). Hotter and drier environments were found to have even lower critical wet-bulb temperature limits, though the ambient conditions needed to reach these critical limits (Figure 4) are much less common in our current climate. Based on previous research, one would expect these critical limits to continue to decrease as metabolic activity continues to increase (21).
Figure 3.
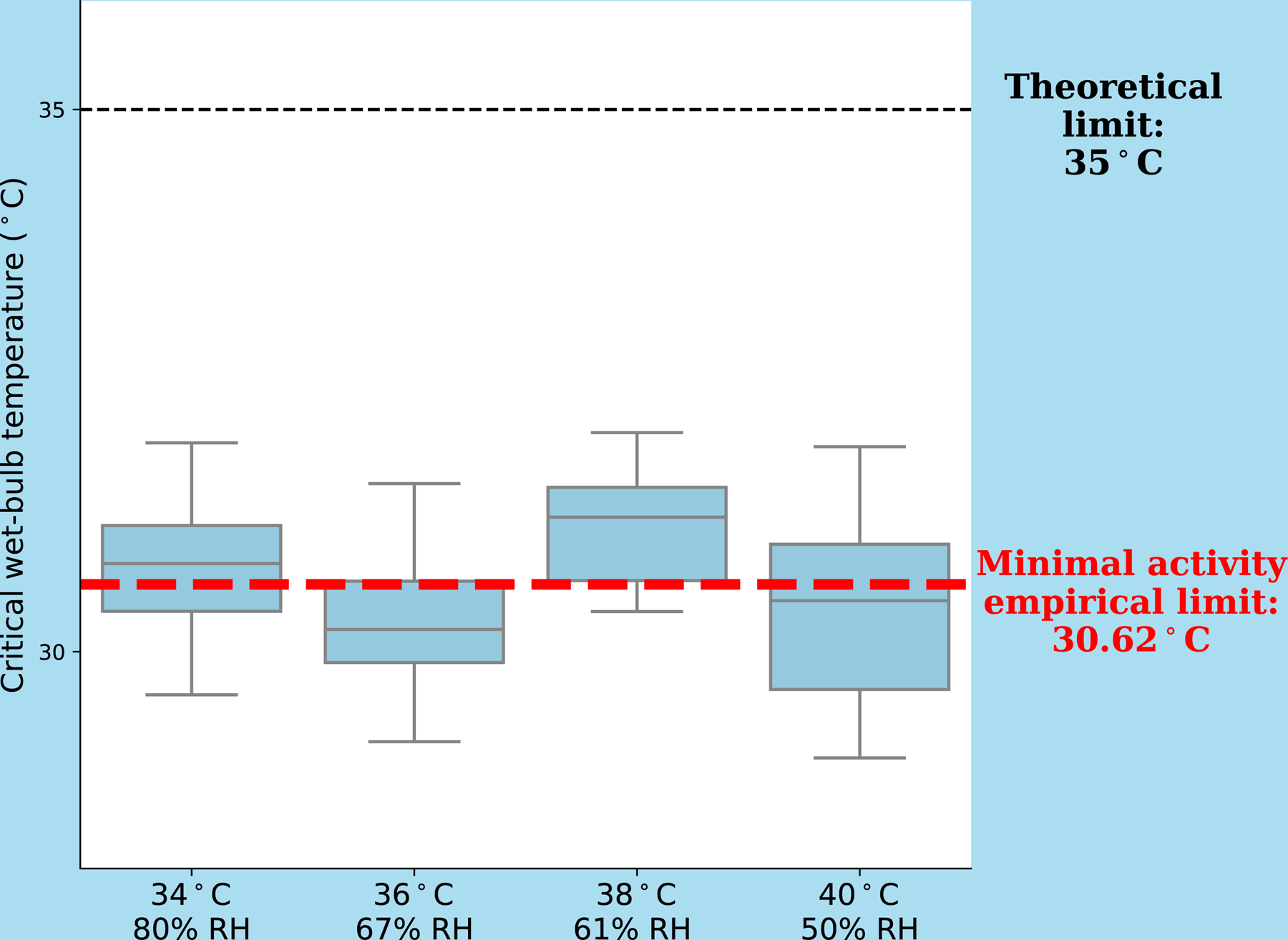
Empirically derived critical wet-bulb temperatures above which heat balance cannot be maintained (uncompensable heat stress) during minimal activity experiments performed by a sample of 48 young (18–34 yrs) men and women in warm, humid environments. The subject sample included a wide range of body weights, surface areas, and fitness levels (20). The critical wet-bulb temperature was relatively consistent across this range of hot, humid environments but well below the theorized Twb threshold of 35°C.
Figure 4.
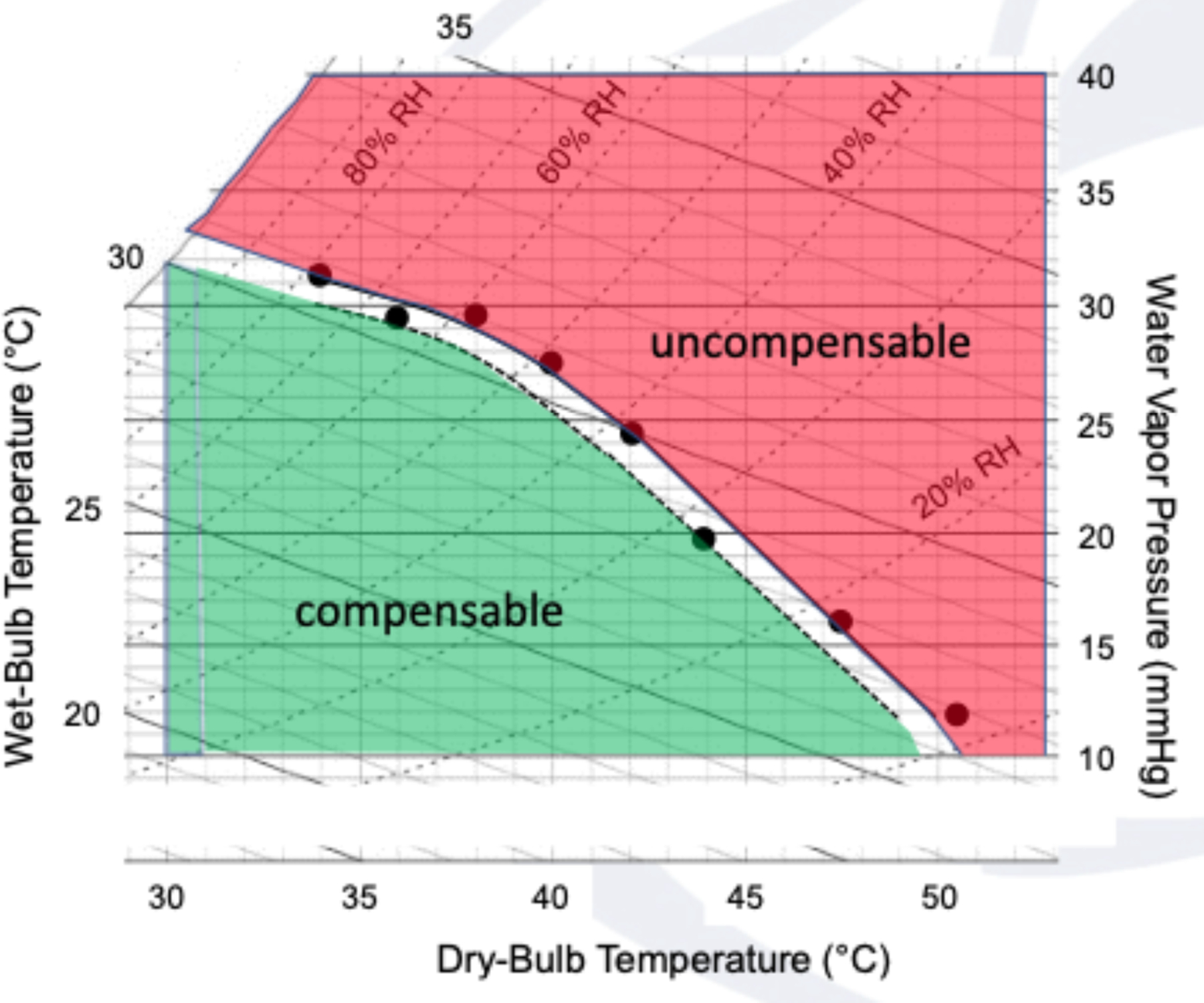
A simple psychrometric chart showing environments of compensable (green) and uncompensable (red) heat stress for young, healthy adults in minimal activity scenarios. Dots represent mean values of study participants. Dry-bulb temperature is on the x-axis and ambient water vapor pressure on the y-axis. Wet-bulb temperature is read on the solid diagonal lines from upper left to lower right and relative humidity (RH) on the dashed curved lines from lower left to upper right. The unshaded area is the lower 95% confidence interval associated with the uncompensable limit line (solid line and data points).
Current status and future implications
It is important to note that the exceedance of these critical environmental limits does not directly relate to increased probability or certainty of heat-related morbidity or mortality. Within the PSU HEAT experiments, at the time of core temperature inflection representative of uncompensable stress, Tc was still well below those associated with heat-related illness (i.e., heat stroke). In such warm-humid environments that exceed the critical environmental limits, it is projected that it would still take multiple hours of prolonged exposure without intervention for core temperatures to exceed temperatures typically associated with heat illnesses (22). However, in vulnerable populations based on exposure and heat load (i.e., outdoor workers, homeless persons, athletes) or in the presence of co-morbidities or other physiological or behavioral impairments, critical environmental limits are likely shifted downward to lower combinations of temperature and humidity, as has been shown in a group of active older women (23), and the rate of core temperature increase after inflection may accelerate, causing health to deteriorate more quickly (24).
In the spring of 2022, an early-season heatwave enveloped the majority of India and Pakistan, delivering record-breaking temperatures coupled with high humidity over a prolonged period. On May 14th, the city of Jacobabad, Pakistan experienced a daily maximum Twb of 33.6°C, well above the thresholds shown in Figure 2 and approaching the 35°C upper limit previously theorized in the literature (16). Many other observing sites in the region registered maximum hourly Twb above 30°C (Figure 5) and did so multiple times over the duration of the heat event. This is becoming an ever-increasing occurrence (17, 25) and should be a signal to all that climate change is not simply a future health problem that we can continue to incrementally prepare for, but rather a current one that requires immediate attention, both in terms of adaptation and mitigation, for the well-being of people everywhere (12).
Figure 5.
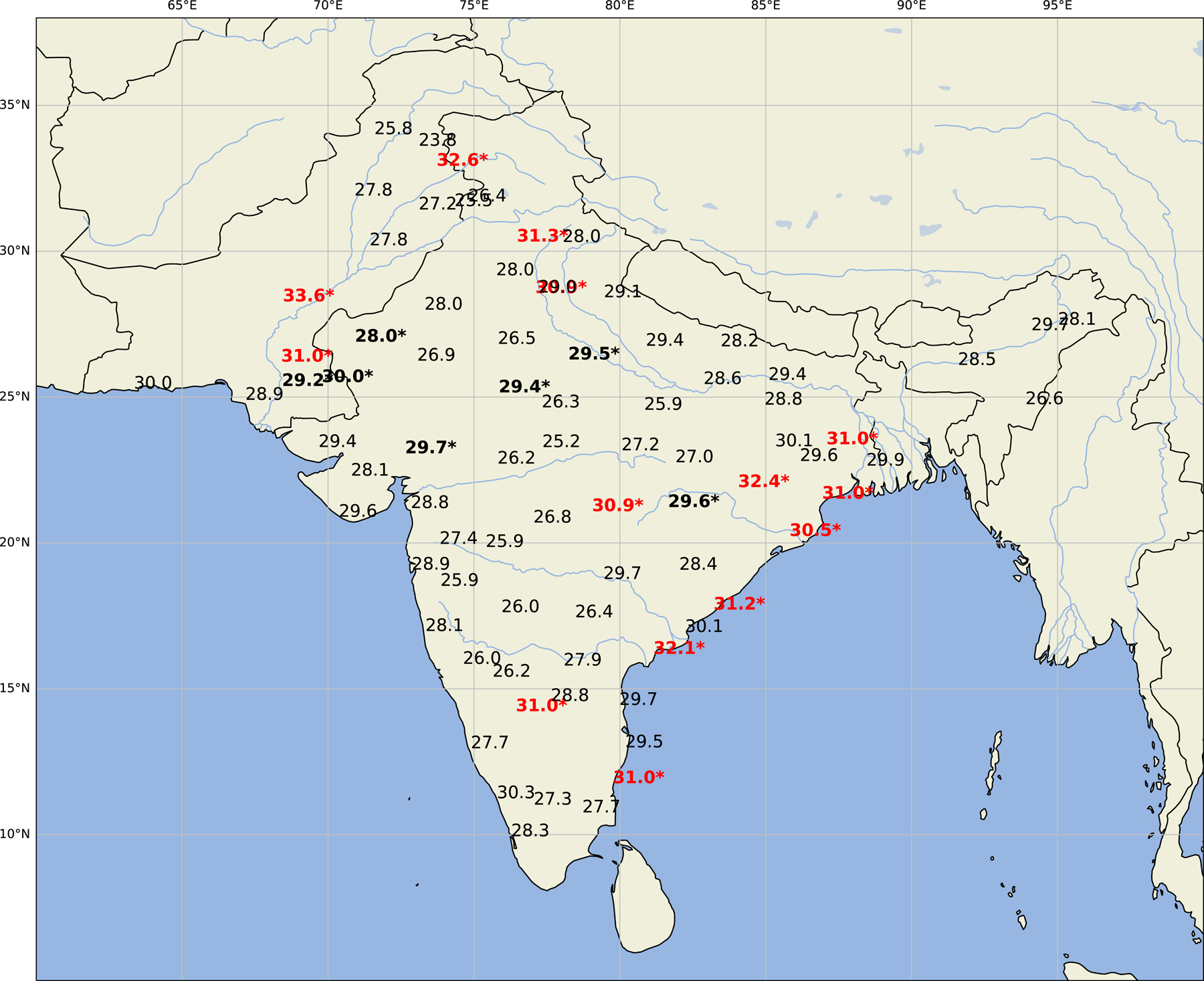
Maximum recorded surface wet-bulb temperatures for the period March 1 – June 1, 2022 in India and Pakistan. Bolded values signify wet-bulb temperatures over the compensability thresholds found in the PSU HEAT Project. Red values are those over 30.5°C, the moist heat stress critical value, while black values with asterisks represent values associated with threshold exceedance in the drier parts of the Tdb – RH distribution. Data from the Hadley Centre’s Integrated Surface Dataset (HadISD).
Conclusion
As the climate continues to warm, environmental conditions will push the limits of human thermoregulatory capacity. Recent laboratory tests revealed a downward shift of the heat stress compensability regime in young, healthy, yet unacclimatized adults from the previously theorized threshold of a wet-bulb temperature of 35°C. These updated empirical thresholds were exceeded in a recent heatwave in South Asia, highlighting that climate change is a clear and present danger to human health. Continued work should be done to determine how these thresholds are altered with respect to individual characteristics such as age and health condition. In addition, given the importance of heat exposure in the acclimatization process, these experiments should be repeated with populations living in warmer climate regimes, both in humid and dry conditions, to determine how longitudinal subjection to heat might improve physiological resilience to these extreme events.
Acknowledgements
The authors would like to thank the anonymous reviewers for their helpful critiques of the manuscript. The results of the present study do not constitute endorsement by the ACSM.
Source of funding
This research was supported by the National Institutes of Health Grant R01 AG067471 (WLK) and the National Institute on Aging Grant T32 AG049676 to The Pennsylvania State University (DJV and RMC).
References
- 1.IPCC. Summary for Policymakers. In: Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change Cambridge University Press, 2021. [Google Scholar]
- 2.Horton RM, Mankin JS, Lesk C, Coffel E, Raymond C. A Review of Recent Advances in Research on Extreme Heat Events. Curr Clim Change Rep 2016;2(4):242–59. doi: 10.1007/s40641-016-0042-x. [DOI] [Google Scholar]
- 3.Perkins SE, Alexander LV, Nairn JR. Increasing frequency, intensity and duration of observed global heatwaves and warm spells. Geophys Res Lett 2012;39(20). doi: 10.1029/2012GL053361. [DOI] [Google Scholar]
- 4.Perkins-Kirkpatrick SE, Gibson PB. Changes in regional heatwave characteristics as a function of increasing global temperature. Scientific Reports 2017;7(1):12256. doi: 10.1038/s41598-017-12520-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shafiei Shiva J, Chandler DG, Kunkel KE. Localized Changes in Heat Wave Properties Across the United States. Earth’s Future 2019;7(3):300–19. doi: 10.1029/2018EF001085. [DOI] [Google Scholar]
- 6.Philip SY, Kew SF, van Oldenborgh GJ, Anslow FS, Seneviratne SI, Vautard R, et al. Rapid attribution analysis of the extraordinary heatwave on the Pacific Coast of the US and Canada June 2021. Earth Syst Dynam Discuss 2021;2021:1–34. doi: 10.5194/esd-2021-90. [DOI] [Google Scholar]
- 7.Zachariah M, T A, AchutaRao K, Saeed F, Jha R, Dhasmana MK, et al. Climate change made devastating early heat in India and Pakistan 30 times more likely. World Weather Attribution 2022. [updated May 23, 2022]. Available from: https://www.worldweatherattribution.org/climate-change-made-devastating-early-heat-in-india-and-pakistan-30-times-more-likely/.
- 8.Rossa-Roccor V, Giang A, Kershaw P. Framing climate change as a human health issue: enough to tip the scale in climate policy? Lancet Planet Health 2021;5(8):e553–e9. doi: 10.1016/S2542-5196(21)00113-3. [DOI] [PubMed] [Google Scholar]
- 9.Weinberger KR, Harris D, Spangler KR, Zanobetti A, Wellenius GA. Estimating the number of excess deaths attributable to heat in 297 United States counties. Environmental Epidemiology 2020;4(3):e096. doi: 10.1097/ee9.0000000000000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green H, Bailey J, Schwarz L, Vanos J, Ebi K, Benmarhnia T. Impact of heat on mortality and morbidity in low and middle income countries: A review of the epidemiological evidence and considerations for future research. Environ Res 2019;171:80–91. doi: 10.1016/j.envres.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 11.Sun S, Weinberger KR, Nori-Sarma A, Spangler KR, Sun Y, Dominici F, et al. Ambient heat and risks of emergency department visits among adults in the United States: time stratified case crossover study. BMJ 2021;375:e065653. doi: 10.1136/bmj-2021-065653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ebi KL, Capon A, Berry P, Broderick C, de Dear R, Havenith G, et al. Hot weather and heat extremes: health risks. The Lancet 2021;398(10301):698–708. doi: 10.1016/S0140-6736(21)01208-3. [DOI] [PubMed] [Google Scholar]
- 13.Buzan JR, Huber M. Moist Heat Stress on a Hotter Earth. Ann Rev Earth Pl Sc 2020;48(1):623–55. doi: 10.1146/annurev-earth-053018-060100. [DOI] [Google Scholar]
- 14.Kenney WL, DeGroot DW, Alexander Holowatz L. Extremes of human heat tolerance: life at the precipice of thermoregulatory failure. J Therm Biol 2004;29(7):479–85. doi: 10.1016/j.jtherbio.2004.08.017. [DOI] [Google Scholar]
- 15.Chapman CL, Johnson BD, Vargas NT, Hostler D, Parker MD, Schlader ZJ. Both hyperthermia and dehydration during physical work in the heat contribute to the risk of acute kidney injury. J Appl Physiol 2020;128(4):715–28. doi: 10.1152/japplphysiol.00787.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherwood SC, Huber M. An adaptability limit to climate change due to heat stress. Proc Nat Acad Sci 2010;107(21):9552–5. doi: 10.1073/pnas.0913352107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raymond C, Matthews T, Horton RM. The emergence of heat and humidity too severe for human tolerance. Sci Adv 2020;6(19):eaaw1838. doi: 10.1126/sciadv.aaw1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pal JS, Eltahir EAB. Future temperature in southwest Asia projected to exceed a threshold for human adaptability. Nat Clim Change 2016;6(2):197–200. doi: 10.1038/nclimate2833. [DOI] [Google Scholar]
- 19.Vecellio DJ, Wolf ST, Cottle RM, Kenney WL. Evaluating the 35°C wet-bulb temperature adaptability threshold for young, healthy subjects (PSU HEAT Project). J Appl Physiol 2022;132(2):340–5. doi: 10.1152/japplphysiol.00738.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolf ST, Cottle RM, Vecellio DJ, Kenney WL. Critical environmental limits for young, healthy adults (PSU HEAT Project). J Appl Physiol 2022;132(2):327–33. doi: 10.1152/japplphysiol.00737.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolf ST, Folkerts MA, Cottle RM, Daanen HAM, Kenney WL. Metabolism- and sex-dependent critical WBGT limits at rest and during exercise in the heat. Am J Physiol - Reg I 2021;321(3):R295–R302. doi: 10.1152/ajpregu.00101.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cottle RM, Lichter ZS, Vecellio DJ, Wolf ST, Kenney WL. Core temperature responses to compensable vs. uncompensable heat stress in young adults (PSU HEAT Project). J Appl Physiol 2022;133(4):1011–8. doi: 10.1152/japplphysiol.00388.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kenney WL. Psychrometric limits and critical evaporative coefficients for exercising older women. J Appl Physiol 2020;129(2):263–71. doi: 10.1152/japplphysiol.00345.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kovats RS, Hajat S. Heat Stress and Public Health: A Critical Review. Ann Rev Pub Health 2008;29(1):41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. [DOI] [PubMed] [Google Scholar]
- 25.Speizer S, Raymond C, Ivanovich C, Horton RM. Concentrated and Intensifying Humid Heat Extremes in the IPCC AR6 Regions. Geophys Res Lett 2022;49(5):e2021GL097261. doi: 10.1029/2021GL097261. [DOI] [Google Scholar]


