Abstract
Purpose
Four joint arthroplasty registries (JARs) levels exist based on the recorded data type. Level I JARs are national registries that record primary data. Hospital or institutional JARs (Level II–IV) document further data (patient-reported outcomes, demographic, radiographic). A worldwide list of Level II–IV JARs must be created to effectively assess and categorize these data.
Methods
Our study is a systematic scoping review that followed the PRISMA guidelines and included 648 studies. Based on their publications, the study aimed to map the existing Level II–IV JARs worldwide. The secondary aim was to record their lifetime, publications’ number and frequency and recognise differences with national JARs.
Results
One hundred five Level II–IV JARs were identified. Forty-eight hospital-based, 45 institutional, and 12 regional JARs. Fifty JARs were found in America, 39 in Europe, nine in Asia, six in Oceania and one in Africa. They have published 485 cohorts, 91 case-series, 49 case–control, nine cross-sectional studies, eight registry protocols and six randomized trials. Most cohort studies were retrospective. Twenty-three per cent of papers studied patient-reported outcomes, 21.45% surgical complications, 13.73% postoperative clinical and 5.25% radiographic outcomes, and 11.88% were survival analyses. Forty-four JARs have published only one paper. Level I JARs primarily publish implant revision risk annual reports, while Level IV JARs collect comprehensive data to conduct retrospective cohort studies.
Conclusions
This is the first study mapping all Level II–IV JARs worldwide. Most JARs are found in Europe and America, reporting on retrospective cohorts, but only a few report on studies systematically.
Keywords: Arthroplasty replacement, Joint registry, Arthroplasty registry, Hospital-based registry, Regional registry, Registry level
Introduction
Joint arthroplasty registries (JARs) are databases that report the outcomes of joint arthroplasties (JAs). Their primary goal is the JAs quality improvement [1], and they are considered the gold standard source for informed medical decision-making. There are four levels of JARs based on the type of data recorded. Level I JARs record basic data, Level II demographic and comorbidity data, Level III patient-reported outcome data and Level IV imaging and radiographic data. Most well-known national JARs collect type I data because further data collection is expensive. Fewer regional, institutional, or hospital-based JARs collect more detailed patients’ data (type II–IV) [1, 2].
National arthroplasty registries (Level I) report primary data on patients and procedures using revision arthroplasty as the endpoint. They collect large data volume nationally, reporting annual survival outcomes and revision risk of specific implants [3, 4]. However, national JARs reports are extensive and interpreted with difficulty by clinicians having little statistical training. The reports’ interpretation may also be misleading due to the absence of more comprehensive registry data (type II–IV) [5, 6].
On the other hand, Level II–IV regional or hospital-based registries collect smaller volumes but more inclusive data correlating efficiently radiologic or patient history data with arthroplasty outcomes. These JARs may complement national JARs, allowing further scrutiny and deeper causative correlation of JAs failure, improving outcomes [5]. Currently, an attempt to record the hip and knee JARs in Europe is being made [6]. However, a worldwide list of hospital-based JARs does not exist, and their contribution to assessing arthroplasty results remains unclear.
Level I JARs have been thoroughly researched, but there is a lack of information on the importance of Level II–IV JARs in the literature. To accurately evaluate and classify the more specific and patient-centric data they provide, we require a comprehensive inventory of both institutional and hospital-based JARs. Knowing the quantity and location of these JARs and the number and variety of publications they produce can enhance our comprehension of their value and necessity.
The present study is a systematically performed scoping review. The primary aim of this study was to map the existing institutional and hospital-based (Level II–IV) JARs worldwide and their lifetime. The secondary aim was to record their lifetime, publications’ number and frequency and recognize differences with national JARs. Countries with national and hospital-based JARs were also recorded.
Materials and methods
Our study is a systematic scoping review that followed the PRISMA 2020 statement [7].
Search strategy
A systematic review of published articles from several databases such as MEDLINE (PubMed), Cochrane Database of Systematic Reviews and Clinical Trials by the U.S. National Library of Medicine was conducted from conception to July 2022. The following keywords and Mesh terms were utilized with “AND” or “OR”: “arthroplasty, replacement, knee,” “arthroplasty, replacement, hip,” “arthroplasty, replacement, ankle,” “arthroplasty, replacement, shoulder,” “registries,” “arthroplasty registry,” “joint registry,” “regional registry,” “hospital registry”,” registry level,” “national registry.” The authors created the keywords, drawing on their own experience, and employed different names to refer to the term "registry". They did not involve any input from a librarian.
Inclusion and exclusion criteria
Specific inclusion criteria were the following: i) randomized (RCTs) and non-randomized control trials, prospective and retrospective cohorts, case series and comparative studies, (ii) studies involving adult patients (> 18 years) that underwent elective total joint arthroplasty (TJA), (iii) studies evaluating joint arthroplasty outcomes based on Level II–IV JARs data (regional, institutional or hospital-based arthroplasty registries), (iv) studies providing extractable data (studies that have organized and fully structured data that can be extracted from the manuscript).
On the other hand, studies were excluded if they i) reported national type I JARs data, (ii) used non-arthroplasty registries data (hospital discharge or other ailments registries), (iii) were narrative reviews, letters to the editor, editorial comments, meta-analysis or systematic reviews related to the topic, (iv) were conducted in animals or cadavers, (v) were written in a non-English language, (vi) had no full-text available.
Data extraction
The searched papers with abstract information were managed in Mendeley to remove duplicated citations. The remaining studies were screened independently by two authors. Firstly, titles and abstracts were screened using the search strategy to fulfil the inclusion criteria. The data extraction process was done by the two authors independently. The final extracted data were cross-checked. A third senior author resolved any disagreement.
Data synthesis
Data synthesis was performed and analyzed by the same two authors that recorded the following information for JARs: i) the location (country, city, hospital name); (ii) the quality of reported studies (study type, methodology, population and other characteristics) (iii) their lifetime calculated from the time of the first and last found publication and (iv) if the countries of hospital-based registries had also a national registry. Differences in the published information between national and hospital-based registries were also evaluated.
Results
Search results
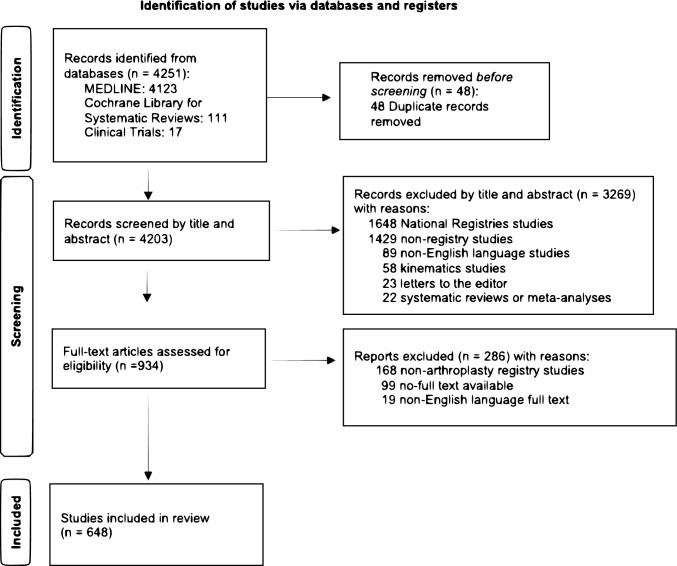
The initial electronic search yielded 4251 studies. After eliminating 48 duplicated studies, 4203 were reviewed on their title and abstract. According to our inclusion and exclusion criteria, 3269 records were excluded based on title and abstract, and 934 papers were deemed suitable and screened in the full article text. Finally, 648 studies were included in this systematic review. The flow diagram of the search strategy is shown in Fig. 1.
Fig. 1.
PRISMA 2020 flow diagram of search strategy
Demographics and patient characteristics, study type, design & primary aim
The included studies were published from 1997 to 2022 [8–12]. The sample size of the studied population ranged from 9 to 84,998 patients [13, 14]. Almost 60 per cent of the patients were women. The follow-up of patients varied from three months to twenty-five years [15, 16].
According to the study type, 485 (74.85%) were cohorts [2, 3, 8–12, 14–316], 91 (14.04%) were case-series [13, 317–406], 49 (7.56%) were case–control studies [407–455], nine (1.39%) cross-sectional studies [456–464], eight (1.23%) protocols for registry-based studies [465–472] and six (0.93%) randomised control trials (RCT) [473–478]. Three hundred twenty-seven cohort studies were retrospective [2, 8, 11, 14, 17, 18, 21–26, 29–34, 36, 38, 41, 42, 44–46, 54–56, 64–71, 83–91, 106–118, 123, 137–146, 155–190, 200–217, 233–266, 273, 281–308, 311–315, 479–590], and 158 were prospective [9, 10, 12, 15, 16, 19, 20, 27, 28, 35, 37, 39, 40, 43, 47–53, 58–63, 73–82, 92–105, 119–136, 147–154, 191–199, 210, 218–232, 267–272, 274–280, 309, 310, 316, 591–629]. In thirty-seven cohort studies, a comparison between two cohorts was made [57, 72, 147, 188–191, 200, 233, 265, 309–316, 479–482, 526–528, 560–567, 630–633].
Almost half of the included papers studied the patient-reported outcome measures (PROMs), the Quality-of-Life Years (QALYs) and the intra- and postoperative complications rate. In detail, the primary outcome in 149 (23%) studies were PROMs and QALYs [18, 19, 23, 34, 40, 55, 59, 61, 68, 81, 92, 99, 100, 108, 111, 117, 124, 127, 129, 135, 137, 139, 150, 153, 161, 168, 170, 173, 182, 187, 191, 193, 196–200, 206, 207, 210, 212, 215, 217, 222, 223, 225, 227, 236, 242, 244, 245, 263, 265, 267, 268, 273, 275–278, 281, 283, 300, 301, 307, 310, 314, 339, 352, 353, 357, 368, 378, 382, 395, 396, 400, 401, 403, 405, 408, 412, 417, 425, 426, 434, 439, 440, 445, 446, 449, 460–463, 481, 483–485, 487, 492, 494, 499, 501, 512, 513, 516, 523, 525, 528, 530, 533, 542, 546, 548, 549, 564, 565, 574–576, 579, 587, 589–591, 593–595, 601, 602, 605–609, 612–614, 619, 621, 622, 625, 628, 629, 634–636], while in 139 (21.45%) studies were surgical complications (i.e., infections, fractures, thrombosis etc.) [9, 13, 15–17, 20, 21, 25, 45, 58, 63, 66, 69, 73, 77–80, 84, 85, 88, 101–105, 107, 109, 110, 113, 119, 121, 125, 130, 133, 146, 147, 152, 157, 159, 160, 162, 163, 166, 172, 174, 175, 180, 183, 194, 195, 202, 204, 209, 213, 234, 237, 239, 240, 250, 252, 254, 257, 264, 266, 269–271, 279, 282, 287, 289, 290, 295, 298, 306, 311, 312, 316, 317, 319, 327, 334, 336, 341, 354, 356, 365, 366, 370, 377, 381, 388, 392, 397, 398, 409, 413, 416, 422, 427, 432, 437, 441, 442, 444, 451, 452, 474, 475, 478, 480, 488, 498, 500, 504, 509, 520, 522, 529, 534, 536, 545, 547, 550, 554–556, 558, 560, 561, 568, 596, 597, 600, 630, 637–639]. Eighty-nine studies (13.73%) evaluated postoperative patients’ clinical outcomes [11, 27, 47, 50, 62, 74, 83, 91, 95–97, 106, 112, 114, 120, 128, 134, 149, 151, 176, 178, 181, 185, 188, 190, 192, 203, 205, 208, 210, 216, 221, 224, 229, 230, 235, 238, 247, 261, 286, 291, 292, 296, 302, 303, 305, 348, 349, 369, 372, 373, 375, 379, 380, 386, 387, 391, 411, 415, 419, 420, 424, 429, 430, 436, 454, 493, 496, 497, 503, 521, 526, 531, 537, 553, 559, 566, 567, 570, 573, 584, 616, 617, 633, 640–643], 34 (5.25%) postoperative radiographic outcomes [35, 56, 116, 148, 167, 169, 171, 246, 248, 274, 284, 304, 309, 324, 335, 343, 363, 364, 376, 447, 450, 453, 459, 464, 477, 489, 490, 514, 517, 535, 539, 572, 618, 644] and 46 (7.10%) studies assessed the efficacy of a specific implant [22, 24, 41–44, 71, 72, 86, 87, 118, 126, 165, 184, 201, 219, 233, 241, 243, 256, 262, 297, 325, 332, 337, 347, 359, 394, 410, 423, 431, 443, 479, 506, 541, 544, 580, 586, 598, 615, 624, 627, 632, 645, 646]. Seventy-seven (11.88%) studies were survival analyses [2, 10, 26, 37, 38, 46, 64, 67, 70, 115, 122, 136, 154, 155, 164, 177, 179, 189, 211, 231, 232, 251, 260, 272, 280, 288, 293, 308, 321, 329, 331, 340, 342, 344–346, 351, 360, 361, 371, 385, 402, 414, 421, 433, 438, 482, 491, 495, 502, 507, 508, 511, 515, 518, 519, 524, 527, 532, 540, 551, 557, 563, 569, 581–583, 585, 588, 592, 599, 603, 611, 631, 647, 648] but 21 (3.24%) studied the long-term arthroplasty outcomes [29, 48, 49, 82, 93, 141, 218, 228, 285, 322, 383, 384, 407, 458, 505, 543, 562, 623, 626, 649]. Besides, 17 (2.62%) studies compared different surgical techniques [28, 53, 144, 145, 186, 253, 338, 358, 362, 374, 390, 428, 538, 552, 578, 650, 651] and seven (1.08%) studies evaluated various levels of surgeons’ experience [30, 33, 36, 214, 255, 294, 299], while in 18 (2.78%) studies, a prediction of pre- or postoperative risk factors was made [14, 39, 52, 54, 98, 131, 132, 143, 355, 367, 389, 404, 435, 448, 456, 457, 604, 620]. Finally, 15 (2.31%) were cost analysis studies [57, 65, 75, 90, 138, 140, 142, 156, 158, 226, 315, 326, 328, 399, 486], 13 papers (2%) studied the patients’ mortality rate [31, 60, 76, 258, 259, 313, 320, 323, 333, 418, 577, 652, 653], 12 (1.85%) studies offered general registry information [8, 51, 89, 123, 220, 249, 318, 330, 350, 393, 571, 610], nine (1.39%) were protocols [465–473] and two (0.31%) genetic studies [32, 476].
Global mapping of Level ΙΙ–IV registries
105 Level II–IV registries were identified. Forty-eight (45.71%) were hospital-based, forty-five (42.86%) were institutional, and twelve (11.43%) were regional JARs. Tables 1, 2, and 3 show the distribution of the included JARs per continent. Specifically, 50 (47.62%) Level II–IV JARs were found in America (USA:44, Canada:5, SouthAmerica:1), 39 (37.14%) in Europe (Switzerland:7, UK:7, France:5, Germany:4, Italy:3, Spain:2, Greece:2, Ireland:2, Sweden:2, Norway:1, Denmark:1, Austria:1, Scotland:1, Turkey:1), nine (8.57%) in Asia (China:4, Taiwan:1, Japan:1, Hong Kong:1, Korea:1, Singapore:1), six (5.71%) in Oceania (Australia:5, New Zealand:1) and one (0.95%) in Africa (Tunisia) (Tables 1, 2 and 3). Some countries have more than one institutional JARs in different cities, while others have only one hospital-based arthroplasty JAR. The global geographic distribution of the included type II–IV JARs is depicted in Fig. 2.
Table 1.
Mapping of hospital-based arthroplasty registries in Oceania, Asia and Africa continent
| Continent | Country | Region | JAR |
|---|---|---|---|
| Oceania | Australia | Adelaide | (Revision Knee) Repatriation General HS Adelaide [590] |
| Melbourne | 1. St. Vincent’s HS Melbourne (SMART) [65, 158, 197, 214, 228, 303, 347, 397, 460, 465, 470, 472, 478, 525, 536, 558, 571, 607] | ||
| 2. Alfred HS [341] | |||
| Nedlands | Hollywood HS H&K [34] | ||
| Victoria | (Barwon) St John of God HS [399] | ||
| New Zealand | Tauranga | Regional Tauranga Public HS [386] | |
| Asia | China | Hebei | Hebei Medical University [204] |
| Fujian | First Affiliated HS of Fujian Medical University [555] | ||
| Peking | 1. Knee Peking Union Medical College HS [370] | ||
| 2. Chinese People’s Liberation Army [539] | |||
| Hong Kong | Hong Kong | Institutional Queen Mary HS [282, 367, 471, 554, 617, 622] | |
| Japan | Takatsuki | (Hip) Takatsuki General HS [359] | |
| Korea | Korea | Korean Hip (KHR) [489] | |
| Republic of China | Taiwan | Chang Gung Memorial HS [83, 422, 475, 557] | |
| Singapore | Singapore | Singapore General HS [108, 124, 168, 192, 227, 229, 245, 253, 273, 277, 284, 434, 436, 440, 443, 466, 467, 513, 538, 546, 579, 591, 595, 602, 608, 612, 616, 621, 623, 640, 641, 649, 657] | |
| Africa | Tunisia | Tunisia | Local TKA Kassab Orthopaedic Institute [388] |
JAR Joint Arthroplasty Registry, H&K Hip and Knee, HS Hospital, S&E Shoulder and Elbow, THR Total Hip Registry, TJA Total Joint Arthroplasty, TKA Total Knee Arthroplasty
[] Numbers in parentheses are the relevant references
Table 2.
Mapping of hospital-based arthroplasty registries in Europe
| Country | Region | JAR |
|---|---|---|
| Austria | Innsbruck | Tirol Landeskrankheitstalten GmbH [396, 423] |
| Denmark | Hvidovre | Copenhagen University HS [278, 587] |
| France | Livet | Livet HS [334] |
| Lyon | 1. Hopital Prive Jean Mermoz Shoulder [398] | |
| 2. Hôpital Edouard Herriot [280, 361] | ||
| Nice | Hopital Pasteur 2 Shoulder, Universite Cote d’Azur [398] | |
| Paris | SoFCOT Group [41, 102, 104, 115, 130, 340, 657] | |
| Germany | Dresden | 1. ORTHOTEP University HS Carl Gustav Carus [109, 619] |
| 2. Dresden Hip Surgery Registry [52, 196] | ||
| Heidelberg | University of Heidelberg [410] | |
| Regensburg | Regensburg University [198, 255, 292, 296, 299] | |
| Greece | Athens | General HS KAT [155, 384, 646] |
| Thessaloniki | Arthroplasty RG Thessaloniki (ART) [2, 12, 406, 455, 647] | |
| Italy | Emilia-Romanga | Register of Orthopaedic Prosthetic Implant (RIPO) [24, 26, 39, 43, 57, 145, 164, 189, 231, 288, 297, 468, 476, 482, 491, 502, 506, 508, 527, 540, 562, 563, 569, 585, 592, 597, 599, 624, 630, 645] |
| Milano | Italian Arthroplasty RG (RIAP) [87, 378, 395, 451, 570] | |
| Toscana | Santo Stefano HS [442] | |
| Ireland | Limerick | University HS Limerick [431] |
| Northern Ireland | Musgrove Park HS [32] | |
| Norway | Trondheim | H&K, St Olavs HS [176, 628] |
| Scotland | Edinburgh | University Edinburgh, Scotland [528] |
| Spain | Catalonia | Catalan Arthroplasty Register (RACat) [203, 313, 556, 350, 469, 658] |
| Madrid | University HS Gregorio Maranon [226] | |
| Sweden | Stockholm | Department of Orthopedics Södersjukhuset [105, 175] |
| Uppsala | Uppsala University HS [262] | |
| Switzerland | Bern | Shoulder, Orthopädie Sonnenhof [444] |
| Geneva | Geneva Arthroplasty RG (HUG) [51, 103, 131, 219, 267, 271, 310, 311, 458, 594, 620, 625, 626] | |
| Lausanne | Lausanne Uni HS—CHUV [584, 638, 394] | |
| Liesta | Kantonsspital Baselland Liesta [239, 342] | |
| St. Gallen | TKA RG, Kantonsspital St. Gallen [351, 428, 439, 514, 528, 575, 614] | |
| Zurich | 1. Balgrist Uni HS Zürich [91, 453] | |
| 2. Schulthess Shoulder Arthroplasty RG (SAR) [248, 382, 387, 391, 496, 545, 561, 610] | ||
| Turkey | Konya | Selcuk University Medical Faculty [368] |
| United Kingdom | Bistrol | Avon Knee RG [29, 36] |
| Derby | Royal Derby Hospital [402] | |
| Leicester | Trent [9, 20–22, 27, 53, 218, 256, 276, 329] | |
| London | Royal National Orthopaedic HS RG [177] | |
| Newcastle | Freeman Joint RG [111, 178, 349, 364, 613, 642] | |
| SouthWest London | SouthWest London Elective Orthopaedic Centre [117, 139, 324, 337, 461–463] | |
| Wringtington | North West Wrightington HS [30, 33] |
JAR Joint Arthroplasty Registry, H&K Hip and Knee, HS Hospital, RG Registry, S&E Shoulder and Elbow, TJA Total Joint Arthroplasty, TKA Total Knee Arthroplasty
[] Numbers in parentheses are the relevant references
Table 3.
Mapping of hospital-based arthroplasty registries in America
| Country | State-region | JAR |
|---|---|---|
| Canada | Calgary | ABJHI [534] |
| Ontario | 1. OJRR [55, 328, 330] 2. Southwestern Ontario [23] | |
| Toronto | 1. St Michael’s HS [611, 433] 2. Toronto Western HS [15, 40, 48–50, 54, 68, 107, 603, 411, 456] | |
| Winnpeg | University of Manitoba [300, 366, 477, 487, 492] | |
| South America | Colombia Bogota | HS Universitario Fundación Santa Fe de Bogotá [220, 291, 376, 615] |
| United States of America | California | 1. CJRR [146, 150, 215, 317, 353, 365] 2. Saint Vincent Medical Center [38] 3. University California, San Francisco [18, 392] 4. Stanford University Medical Center, San Francisco, Redwood City [438] |
| Colorado | 1. Colorando JRR [446] 2. Steadman Philippon Research Institute Registry, Vail [457] | |
| Connecticut | 1. CJRI [17] 2. University Connecticut Health Center, Farmington [275, 314, 316] | |
| Florida | 1. FOI [419] 2. Center for Advanced Orthopedics Larkin, Miami [200, 355, 426] 3. Joint RG Mercy HS, Miami [408] 4. Knee Registry St. Vincent’s Healthcare, Jacksonville [347] | |
| Illinois | 1. American Hip Institute, Westmont [435, 549, 553, 445, 605] 2. Rush Uni (Shoulder), Chicago [209, 302, 535, 565, 588] | |
| Kentucky | Kentucky University, Lexington [144, 212, 216, 304, 352, 358, 441, 531] | |
| Massachusetts | 1. New England Baptist, Tufts [296–306] 2. PAR [307–310] 3. Harris, Massachusetts General HS [311–316, 591–599] 4. FORCE-TJR Massachusetts University [594, 595] | |
| Michigan | 1. MARCQI [14, 186, 202, 205, 221, 254, 369, 373, 381, 404, 437, 520, 637, 651] 2. Retrieved Orthopedic, Beaumont Health [336] | |
| Minnesota | 1. HealthEast [28, 37, 42, 70, 72, 331, 414] 2. Minneapolis Veteran’s Affairs (VA) [185] 3. Minnesota University [136, 160, 345] | |
| Missouri | Barnes-Jewish HS Washington University [56, 133, 141, 162, 184, 213, 230, 285, 400, 421, 448, 644, 657] | |
| New Mexico | (JRR) New Mexico Orthopaedics [16] | |
| New York | 1. CHKR [74] 2. NY-Presbyterian HS Columbia University [75] 3. Sinai HS, Baltimore [86] 4. HS for Special Surgery [11, 19, 59, 61, 63, 98, 113, 116, 119, 121, 128, 148, 156, 167, 170, 173, 181, 187, 193, 206–208, 210, 217, 222, 223, 233, 235, 236, 238, 241–243, 246, 261, 265, 266, 268, 270, 279, 281, 283, 298, 301, 307, 479, 483–485, 488, 493, 494, 499, 501, 512, 517, 521, 530, 533, 541, 542, 483–485, 573, 580, 589, 632, 635, 643, 339, 346, 357, 372, 377, 389, 405, 412, 420, 425, 427, 429, 430, 432, 447, 473, 601, 618, 658–665] 5. Mount Sinai [147, 504] 6. Mayo Clinic, Rochester [8, 13, 25, 31, 45, 58, 60, 62, 64, 67, 69, 73, 76–82, 84, 85, 88, 92–95, 106, 110, 118, 120, 122, 125–127, 129, 132, 134, 135, 137, 138, 140, 142, 143, 152, 154, 157, 159, 163, 166, 169, 174, 179, 180, 190, 194, 195, 201, 232, 234, 240, 244, 247, 249, 251, 252, 257–260, 263, 264, 269, 289, 290, 293, 305, 306, 308, 312, 320–323, 325–327, 500, 507, 509–511, 515, 518, 519, 524, 529, 532, 543, 548, 550, 551, 559, 568, 576, 578, 582, 583, 586, 652, 653, 631, 650, 509–511, 321–323, 325–327, 332, 333, 335, 338, 348, 354, 356, 363, 371, 374, 375, 380, 383, 385, 390, 407, 409, 416, 449, 450, 666–671] | |
| North Carolina | 1. OrthoCarolina H&K, Charlotte [46, 165, 172, 237, 272] 2. OrthoCarolina S&E Center, Charlotte [537] 3. Ankle, Duke University Medical Center, Durham [672] | |
| Ohio | 1. Joint Implant Surgeons Practice RG [171, 250, 295,505, 344, 360, 379, 498, 503, 418, 673] 2. EVEREST [47] 3. Cleveland Clinic Foundation [188, 319, 362, 474] 4. University of Cincinnati Medical Center, Cincinnati [572] | |
| Pennsylvania | 1. TKA Dartmouth-Hitchcock Medical Center, Lebanon [294] 2. Thomas Jefferson University HS, Rothman Institute of Orthopaedics, Philadelphia [35, 44, 66, 325, 581, 627] | |
| Texas | 1. FORI (Shoulder) [153, 182, 183, 424, 526, 566, 567, 604] 2. Texas Southwestern University [211, 459] | |
| Virginia | OrthoVirginia [287, 547] |
ABJHI Alberta Bone and Joint Health Institute, CHKR Center for Hip and Knee Replacement Joint Registry, CJRI Connecticut Joint Replacement Institute, CJRR California Joint Replacement Registry, FOI Florida Orthopaedic Institute, Shoulder, FORI Fondren Orthopedic Research Institute, H&K Hip and Knee, HS Hospital, JAR Joint Arthroplasty Registry, JRR Joint Replacement Registry, MARCQI Michigan Collaborative Quality Initiative, NY New York, RG Registry, OJRR Ontario Joint Replacement Registry, PAR Partners Massachusetts Registry, S&E Shoulder and Elbow, TJA Total Joint Arthroplasty, TKA Total Knee Arthroplasty
[] Numbers in parentheses are the relevant references
Fig. 2.
Global distribution of institutional and hospital-based (Level II–IV) arthroplasty registries. The figure was created in Google Maps (online). Each color point represents an arthroplasty registry (Level II–IV) in this area
Table 4 shows the number of publications and the time of the first and last publication for those JARs with more than one published study. Forty-four JARs have published only one paper, and 74 JARs have a publication lifetime of fewer than five years. The “Mayo Clinic Total Joint Registry” has been reporting studies for twenty-five consecutive years, followed by the “Trent” JAR for twenty-one years and the “Register of Orthopaedic Prosthetic Implant (RIPO) of Emilia-Romagna region” for twenty years. The “Mayo Clinic Total Joint Registry” has published 149 papers from 1997 to 2022 [8, 650], including 120 cohort studies [8, 25, 31, 45, 58, 60, 62, 64, 67, 69, 73, 76–82, 84, 85, 88, 92–97, 99–101, 106, 110, 112, 114, 118, 120, 122, 123, 125–127, 129, 132, 134, 135, 137, 138, 140, 142, 143, 152, 154, 157, 159, 163, 166, 169, 174, 179, 180, 190, 194, 195, 201, 232, 234, 240, 244, 247, 249, 251, 252, 257–260, 263, 264, 269, 289, 290, 293, 305, 306, 308, 312, 480, 486, 495, 497, 500, 507, 509–511, 515, 518, 519, 524, 529, 532, 543, 548, 550, 551, 559, 568, 576, 578, 582, 583, 586, 593, 596, 598, 631, 639, 648, 650, 652, 653], 24 case series [13, 320–323, 325–327, 332, 333, 335, 338, 348, 354, 356, 363, 371, 374, 375, 380, 383, 385, 390] and five case–control studies [407, 409, 416, 449, 450]. Among the most frequent study types were 48 documents that focused on surgical complications [13, 25, 45, 58, 69, 73, 77–80, 84, 85, 88, 101, 110, 125, 152, 157, 159, 163, 166, 174, 180, 194, 195, 234, 240, 252, 257, 264, 269, 289, 290, 306, 312, 327, 354, 356, 409, 416, 480, 500, 509, 529, 550, 568, 596, 639], 27 on implant survival [64, 67, 122, 154, 179, 232, 251, 260, 293, 308, 321, 371, 385, 495, 507, 510, 511, 515, 518, 519, 524, 532, 551, 582, 583, 631, 648], 17 on postoperative clinical outcomes [62, 95–97, 106, 112, 114, 120, 134, 190, 247, 305, 348, 375, 380, 497, 559] and 15 on PROMs and QALYs [81, 92, 99, 100, 127, 129, 135, 137, 244, 263, 449, 548, 576, 593, 636]. Besides, ten studies evaluated the patients’ mortality rate [31, 60, 76, 258, 259, 320, 323, 333, 652, 653], seven different implant types [118, 126, 201, 325, 332, 586, 598] and seven the long-term postoperative outcomes [82, 93, 94, 322, 383, 407, 543]. The “Trent” JAR published ten studies from 1997 to 2018 [9, 276], including nine cohort studies [9, 20–22, 27, 53, 218, 256, 276] and one case series [329]. Postoperative complications, short and long-term clinical outcomes, PROMs and QALYs, the efficacy of specific implants, comparison of different surgical techniques and survival analyses were among the main outcome of the published studies. The “Register of Orthopaedic Prosthetic Implant (RIPO) of Emilia-Romagna region” published 30 papers from 2002 to 2022 [24, 645]. Among them, twenty-eight were cohort studies [24, 26, 39, 43, 57, 145, 164, 189, 231, 288, 297, 482, 491, 502, 506, 508, 527, 540, 562, 563, 569, 585, 592, 597, 599, 624, 630, 645], one was RCT [476] and one registry protocol [468]. Of these 30 studies, 16 were survival [26, 164, 189, 231, 288, 482, 491, 502, 508, 527, 540, 563, 569, 585, 592, 599], six analysed implant types [24, 43, 297, 506, 624, 645], and two studied postoperative complications [597, 630]. Long-term postoperative outcomes [562], cost [57] and risk factors analysis [39], genetic studies [476], a protocol for registry study [468] and comparison of different surgical techniques [145] were among the primary outcomes of other study types.
Table 4.
Hospital-based Arthroplasty Registry with more than one publication
| JAR | Country | Lifetime (first—last year publication) | Number of papers | Number of papers/lifetime |
|---|---|---|---|---|
| THR RG HS for Special Surgery | USA | 11 (2011–22) | 89 | 8.09 |
| Mayo Clinic TJR, Rochester | USA | 25 (1997–22) | 147 | 5.88 |
| Partners Arthroplasty RG Massachusetts (PAR) | USA | 1 (2020–21) | 4 | 4.00 |
| Singapore General HS Joint RG | Singapore | 9 (2013–22) | 33 | 3.67 |
| Joint RG,Center for Advanced Orthopedics Larkin, Miami | USA | 1 (2015–16) | 3 | 3.00 |
| Joint RG Uni Connecticut Health Center, Farmington | USA | 1 (2018–19) | 3 | 3.00 |
| Endoprothesenregister in Regensburg Uni | Germany | 2 (2016–18) | 5 | 2.50 |
| Michigan Arthroplasty RG Collaborative Quality Initiative | USA | 6 (2016–22) | 14 | 2.33 |
| Schulthess local Shoulder Arthroplasty RG (SAR) | Switzerland | 4 (2017–21) | 8 | 2.00 |
| American Hip Institute RG, Westmont, Illinois | USA | 3 (2017–20) | 6 | 2.00 |
| North West Regional Arthroplasty Register Wrightington HS | UK | 1 (2004–05) | 2 | 2.00 |
| New England Baptist HS RG, Tufts Medical Center, Massachusetts | USA | 6 (2016–22) | 11 | 1.83 |
| Joint Implant Surgeons Practice RG, Ohio | USA | 6 (2013–19) | 10 | 1.67 |
| Joint Replacement RG Uni of Manitoba | Canada | 3 (2016–19) | 5 | 1.67 |
| St. Vincent’s HS Melbourne (SMART) | Australia | 11 (2011–22) | 18 | 1.64 |
| Register of Orthopaedic Prosthetic Implant (RIPO) of Emilia-Romagna | Italy | 20 (2002–22) | 30 | 1.50 |
| Total Joint RG Barnes-Jewish HS Washington Uni, Missouri | USA | 8 (2014–22) | 12 | 1.50 |
| Joint RG Lausanne Uni HS—CHUV | Switzerland | 2 (2020–22) | 3 | 1.50 |
| Total Joint Replacement RG Minnesota Uni, Minnesota | USA | 2 (2013–15) | 3 | 1.50 |
| Shoulder Arthroplasty RG Fondren Orthopedic Research Institute (FORI), Texas | USA | 6 (2015–21) | 8 | 1.33 |
| TJA RG Kentucky University, Lexington | USA | 6 (2014–20) | 8 | 1.33 |
| Arthroplasty RG Thessaloniki (ART) | Greece | 4 (2018–22) | 5 | 1.25 |
| RG Queen Mary HS | Hong Kong | 5 (2016–21) | 6 | 1.20 |
| Geneva Arthroplasty RG (HUG) | Switzerland | 12 (2010–22) | 13 | 1.08 |
| Local TKA RG Kantonsspital St. Gallen | Switzerland | 7 (2014–21) | 7 | 1.00 |
| California Joint Replacement RG (CJRR), California | USA | 6 (2014–20) | 6 | 1.00 |
| Rush Uni (Shoulder) Registry Chicago | USA | 5 (2016–21) | 5 | 1.00 |
| HS Universitario Fundación Santa Fe de Bogotá | Colombia | 4 (2017–21) | 4 | 1.00 |
| Replacement RG OrthoVirginia, Virginia | USA | 2 (2018–20) | 2 | 1.00 |
| Institutional Joint RG in Hôpital Edouard Herriot | France | 2 (2016–18) | 2 | 1.00 |
| TJA RG Texas Southwestern Uni, Texas | USA | 2 (2016–18) | 2 | 1.00 |
| Department of Orthopedics Södersjukhuset | Sweden | 2 (2013–15) | 2 | 1.00 |
| Toronto Western HS Joint Replacement RG | Canada | 12 (2008–20) | 11 | 0.92 |
| Catalan Arthroplasty Register (RACat) | Spain | 6 (2014–20) | 5 | 0.84 |
| Harris Joint RG Massachusetts General HS | USA | 19 (2001–20) | 15 | 0.79 |
| Freeman Joint RG | UK | 8 (2013–21) | 6 | 0.75 |
| Ontario Joint Replacement RG (OJRR) | Canada | 4 (2006–10) | 3 | 0.75 |
| HealthEast Joint RG, Minnesota, | USA | 10 (2003–13) | 7 | 0.70 |
| Arthroplasty RG Copenhagen Uni HS | Denmark | 3 (2018–21) | 2 | 0.67 |
| Arthroplasty RG Uni California, San Francisco, | USA | 3 (2017–20) | 2 | 0.67 |
| Italian Arthroplasty RG (RIAP) | Italy | 9 (2012–21) | 5 | 0.55 |
| OrthoCarolina H&K Center, Charlotte, | USA | 9 (2009–18) | 5 | 0.55 |
| SoFCOT Group (Socie ´te ´ Franc ¸aise de Chirurgie Orthope ´dique et Traumatologique) | France | 14 (2008–22) | 7 | 0.50 |
| Chang Gung Memorial HS Joint RG, Taiwan | China | 8 (2012–20) | 4 | 0.50 |
| Retrieved Orthopedic Implant RG Beaumont Health | USA | 8 (2011–19) | 4 | 0.50 |
| Regional Joint RG Tauranga Public HS | New Zealand | 6 (2013–19) | 3 | 0.50 |
| Institutional RG St Michael’s HS, Toronto Uni | Canada | 4 (2016–20) | 2 | 0.50 |
| Total Joint RG Mount Sinai, NY | USA | 4 (2015–19) | 2 | 0.50 |
| Register Kantonsspital Baselland Liesta | Switzerland | 4 (2013–17) | 2 | 0.50 |
| Avon Knee RG | UK | 4 (2003–07) | 2 | 0.50 |
| Trent Leicester | UK | 21 (1997–2018) | 10 | 0.48 |
| Institutional RG SouthWest London Elective Orthopaedic Centre, | UK | 16 (2006–22) | 7 | 0.44 |
| Institutional H&K arthroplasty RG St Olavs HS | Norway | 7 (2015–22) | 3 | 0.43 |
| RG General HS KAT | Greece | 7 (2015–22) | 3 | 0.43 |
| Arthroplasty Register Tirol Landeskrankheitstalten GmbH, Innsbruck | Austria | 5 (2015–20) | 2 | 0.40 |
| Dresden Hip Surgery Registry | Germany | 6 (2010–16) | 2 | 0.33 |
| Thomas Jefferson Uni HS, Arthroplasty RG Rothman Institute of Orthopaedics, Philadelphia | USA | 16 (2006–22) | 5 | 0.31 |
| Implant RG Cleveland Clinic Foundation, Ohio | USA | 14 (2003–17) | 4 | 0.28 |
| ORTHOTEP RG Uni HS Carl Gustav Carus | Germany | 8 (2013–21) | 2 | 0.25 |
| Arthroplasty RG Balgrist Uni HS Zürich | Switzerland | 10 (2012–22) | 2 | 0.20 |
The JARs are listed based on the frequency of their publications to their lifetime
H&K Hip and Knee, HS Hospital, RG Registry, S&E Shoulder and Elbow, THR Total Hip Registry, TJA Total Joint Arthroplasty, TJR Total Joint Registry, TKA Total Knee Arthroplasty, TKR Total Knee Registry, Uni University
Concerning the publications’ frequency (number of publications/years of the JAR’s operation), the "THR Registry in Hospital for Special Surgery" is in the first place, with more than eight publications per year (89 papers from 2011 to 2022). "Mayo Clinic Total Joint Registry" is in second place with almost six publications per year (149 papers in twenty-five years), followed by the "Partners Arthroplasty Registry Massachusetts (PAR)" with four publications per year (4 articles in one year). More details are shown in Table 4.
Countries with Level I and Level IV arthroplasty registries
Nine countries have national (Level I) and institutional (Level II–IV) JARs. In these countries, institutional JARs belong to the national JARs but publish their results independently. There are two national JARs in Oceania (Australian Orthopaedic Association National Joint Replacement Registry, New Zealand national joint registry) and six institutional JARs (Repatriation General Hospital, St. Vincent’s Hospital SMART, The Alfred Hospital, The Hollywood Hospital, Barwon in St John of God Hospital, Tauranga Public Hospital) The last one is distinct from but complementary to the New Zealand National Joint Registry. In Europe, six countries (Denmark, Germany, Norway, Sweden, Switzerland and the United Kingdom) own both Levels I and IV JARs. There is a national registry in Germany (Endoprosthesenregister Deutschland EPRD), and two out of four hospital-based registries (Registries at the University of Heidelberg and Regensburg University) work independently. In the United States of America, there are national JARs and 44 hospital-based or institutional registries. More details are shown in Tables 1, 2 and 3.
Some countries have only institutional JARs. Seven Asian and African countries (China, Hong Kong, Japan, Korea, Republic of China-Taiwan, Singapore and Tunisia) have hospital-based JARs. Still, no national JAR can be found on these continents (Table 1). Besides, seven European countries (Austria, France, Greece, Italy, Scotland, Spain, and Turkey) do not have national but only institutional JARs.
Discussion
Our study mapped all Level II–IV JARs worldwide systematically based on their publications. Few hospital or institutional JARs have been found in Asia and Africa, with limited published studies. In Australia, Europe and the United States of America, all JARs levels can be found. The northern European countries (Scandinavia, United Kingdom) have well-known national JARs and institutional registries. In contrast, southern countries (Greece, Spain, Italy) lack a national but own hospital-based JARs publishing data. Due to financial, legal, and regulatory challenges in the United States of America [654], hospital-based JARs prevail, along with the existence of national registries: American Joint Replacement Registry (AJRR) and Kaiser Permanente. Most Level II–IV JARs are found in Europe and America. Some publish their data independently, while others also report through their relative national registries. All institutional or hospital-based JARs in the United Kingdom are part of the National Joint Registry. On the other hand, the "Endoprothesenregister in Regensburg University" and the "Endoprosthesis Register in Department of Orthopedic Surgery, University of Heidelberg" are institutional JARs that do not transfer data to the German national registry "Endoprothesenregister Deutschland (ERPD) ".
It is imperative to obtain a comprehensive inventory of institutional and hospital-based JARs, including Level II–IV, to thoroughly assess and categorize the patient-focused data they offer. The significance and necessity of these JARs can only be fully understood by identifying their quantity, location, and the variety and number of publications they generate. Therefore, we must prioritize acquiring this information to advance our understanding and improve patient care.
Hospital-based and institutional JARs worldwide reported all types of evidence-based pyramid studies. A few published studies are randomized clinical trials; most are cohorts, case-series and case–control studies. The published data are mainly retrospective, with the prospective studies being a minority. The study types differ among Level I and II–IV JARs. Level I national registries publish prospectively annual reports, including revision risk data for various implants. Level II–IV JARs collect more inclusive data to perform cohort and comparative studies; however, most are retrospective. Level I JARs data mainly control implant survival by monitoring the revision rate, the institutional performance and evaluating the quality offered pre-, intra- and postoperatively by all surgeons [8]. Level II–IV JARs data come mainly from senior high-volume surgeons and specialized centres worldwide and cannot be quickly adopted and generalized. However, Level II–IV JARs data are more inclusive. Demographics and baseline characteristics of patients, the type of implants, surgeons, surgical approaches and other procedural features and clinical and radiographical data are usually more detailed. Quality of patients’ life and medical complications other than implant failure as infections, deep vein thrombosis or pulmonary embolism, are also frequently recorded [63, 518, 655, 656]. The Harris Hip Score (HHS) and Hip disability and Osteoarthritis Outcome Score (HOOS) are used to report patients’ quality of life from most registries [2, 647]. There are also implant survival studies from various institutional JARs simultaneously reporting clinical outcomes, complications, PROMs and radiological implants’ data as secondary study outcomes [64, 321, 511, 524, 647]. Radiological data are beneficial to follow implants and understanding the reasons for failure, but they are only available by Level IV JARs [2, 116, 335, 450]. Several surgical approaches and comparative clinical studies of surgical outcomes between specialist orthopaedic surgeons and trainees have been evaluated [255, 428]. Level II–IV JARs often report studies that analyze risk factors (obesity/rheumatic diseases) of TJA outcomes, but also cost analysis studies of the length of hospital stay following TJA improving the cost-effectiveness of joint replacements [76, 158, 333, 425, 456, 486]. Genetic studies have also been performed [350, 476].
The lifetime and publishing frequency varies considerably between JARs. As previously mentioned, among the longest-running Level IV JARs are the "Mayo Clinic Total Joint Registry" from 1997 to 2022, followed by the "Trent" from 1997 to 2018 and the "Register of Orthopedic Prosthetic Implant (RIPO) of Emilia-Romagna Region" from 2002 to 2022. These JARs have published 147, 10 and 30 papers, respectively. The "Mayo Clinic Total Joint Registry" seems to be the oldest institutional registry and has published the most articles. However, the "Total Hip Registry in the Hospital for Special Surgery" is the JAR with the highest publishing frequency, with more than eight published papers per year, followed by the "Mayo Clinic Total Joint Registry" with almost six publications per year, and the "Partners Arthroplasty Registry Massachusetts (PAR)" with four publications per year. On the other hand, twenty-eight JARs publish less than one paper per year in their lifetime.
Besides, many institutional or hospital-based JARs have published only one article during their lifetime. This may be attributed to several factors. The patients and data enrollment of institutional registries is lower than the national ones, and a longer time is needed to complete and report studies. So, their lifetime may be longer than the actual measures from the first and last publication. However, the existence of some long-lasting low-frequency publishing JARs may be disputed in the future.
Our study has some limitations. The principal limit is that the institutional or hospital-based JARs data may not be fully accessible for several reasons. First, there are Level IV JARs, such as the “ German Orthopaedic Foot and Ankle Association's (D. A. F.)” registry [657], that only publish studies in their native language. Thus they are not included in this report. Secondly, only a few regional and hospital-based JARs manage a website to publish annual reports, such as national JARs, due to a lack of funding. Thirdly, most Level IV JARs do not have yearly reports available. If the reports are available online, they are not open to the public, contrary to national JARs [654]. Lastly, many Level IV JARs publish studies only once or twice in their lifetime [21, 24]. That way, a lot of helpful information may be lost.
Conclusion
To our knowledge, this is the first systematic review mapping all institutional or hospital-based JARs worldwide. Most of these registries are found in Europe and America, reporting all types of evidence-based pyramid studies. The reported studies may have data missing from national registry reports as radiographic data, but they are often retrospective. The frequency of data reporting varies considerably among Level II–IV JARs, but this is generally not systematic. Their contribution is undeniable, mainly due to the detailed and variable data they collect. Further studies are needed to evaluate the quality of the offered knowledge in the clinical setting, especially for Level IV registries that do not publish their data annually or in a non-English language.
Author contributions
Conceptualisation: EK; Literature Search and data Analysis: AZ, EK; Writing—original draft preparation: AZ, EK; Writing—review and editing: EK, ET; Supervision: ET, MP.
Funding
Open access funding provided by HEAL-Link Greece. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This is a scoping review study. No ethical approval was required. The authors submitted the study to PROSPERO (registration number: 356482); however, it was automatically rejected as a scoping review (scoping reviews do not meet the requirements of PROSPERO).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Franklin PD, Lewallen D, Bozic K, et al. Implementation of patient-reported outcome measures in U.S. Total joint replacement registries: rationale, status, and plans. J Bone Joint Surg Am. 2014;96(Suppl 1):104–109. doi: 10.2106/JBJS.N.00328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kenanidis E, Kakoulidis P, Anagnostis P, et al. Constrained liners revisited: favourable mid-term results in patients with high-risk of dislocation: technical considerations for the optimal outcome. Hip Int. 2021 doi: 10.1177/11207000211010712. [DOI] [PubMed] [Google Scholar]
- 3.Labek G, Janda W, Agreiter M, et al. Organisation, data evaluation, interpretation and effect of arthroplasty register data on the outcome in terms of revision rate in total hip arthroplasty. Int Orthop. 2011;35:157–163. doi: 10.1007/s00264-010-1131-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Labek G, Sekyra K, Pawelka W, et al. Outcome and reproducibility of data concerning the Oxford unicompartmental knee arthroplasty: a structured literature review including arthroplasty registry data. Acta Orthop. 2011;82:131–135. doi: 10.3109/17453674.2011.566134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malchau H, Garellick G, Berry D, et al. Arthroplasty implant registries over the past five decades: development, current, and future impact. J Orthop Res. 2018;36:2319–2330. doi: 10.1002/jor.24014. [DOI] [PubMed] [Google Scholar]
- 6.Lübbeke A, Silman AJ, Barea C, et al. Mapping existing hip and knee replacement registries in Europe. Health Policy. 2018;122:548–557. doi: 10.1016/j.healthpol.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. The BMJ. 2021 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berry DJ, Kessler M, Morrey BF. Maintaining a hip registry for 25 years. Mayo Clinic experience. Clin Orthop Relat Res. 1997 doi: 10.1097/00003086-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Fender D, Harper WM, Thompson JR, Gregg PJ. Mortality and fatal pulmonary embolism after primary total hip replacement. Results from a regional hip register. J Bone Joint Surg Br. 1997;79:896–899. doi: 10.1302/0301-620x.79b6.7677. [DOI] [PubMed] [Google Scholar]
- 10.Girard J, Epinette JA, Martinot P, Dartus J. French hip resurfacing registry: a study of 1650 cases. Orthop Traumatol Surg Res. 2022;108:103087. doi: 10.1016/j.otsr.2021.103087. [DOI] [PubMed] [Google Scholar]
- 11.Bendich I, Tarity TD, Alpaugh K, et al. Minimal Clinically Important Difference (MCID) at one year postoperatively in aseptic revision total hip arthroplasty. J Arthroplasty. 2022;37:S954–S957. doi: 10.1016/j.arth.2022.01.044. [DOI] [PubMed] [Google Scholar]
- 12.Kenanidis E, Paparoidamis G, Milonakis N, et al. Comparative outcomes between a new robotically assisted and a manual technique for total knee arthroplasty in patients with osteoarthritis: a prospective matched comparative cohort study. Eur J Orthop Surg Traumatol. 2022 doi: 10.1007/s00590-022-03274-3. [DOI] [PubMed] [Google Scholar]
- 13.Turner NS, 3rd, Pagnano MW, Sim FH. Total knee arthroplasty after ipsilateral peripheral arterial bypass graft: acute arterial occlusion is a risk with or without tourniquet use. J Arthroplasty. 2001;16:317–321. doi: 10.1054/arth.2001.21502. [DOI] [PubMed] [Google Scholar]
- 14.Layson JT, Markel DC, Hughes RE, et al. John N. Insall Award: MARCQI’s Pain-Control Optimization Pathway (POP): impact of registry data and education on opioid utilization. J Arthroplasty. 2022;37:S19–S26. doi: 10.1016/j.arth.2022.02.109. [DOI] [PubMed] [Google Scholar]
- 15.Gandhi R, Razak F, Tso P, et al. Metabolic syndrome and the incidence of symptomatic deep vein thrombosis following total knee arthroplasty. J Rheumatol. 2009;36:2298–2301. doi: 10.3899/jrheum.090282. [DOI] [PubMed] [Google Scholar]
- 16.Carothers JT, White RE, Tripuraneni KR, et al. Lessons learned from managing a prospective, private practice joint replacement registry: a 25-year experience. Clin Orthop Relat Res. 2013;471:537–543. doi: 10.1007/s11999-012-2541-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inneh IA, Lewis CG, Schutzer SF. Focused risk analysis: regression model based on 5,314 total hip and knee arthroplasty patients from a single institution. J Arthroplasty. 2014;29:2031–2035. doi: 10.1016/j.arth.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Berliner JL, Brodke DJ, Chan V, et al. Can preoperative patient-reported outcome measures be used to predict meaningful improvement in function after TKA? Clin Orthop Relat Res. 2017;475:149–157. doi: 10.1007/s11999-016-4770-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poultsides LA, Ghomrawi HMK, Lyman S, et al. Change in preoperative expectations in patients undergoing staged bilateral primary total knee or total hip arthroplasty. J Arthroplasty. 2012;27:1609–1615.e1. doi: 10.1016/j.arth.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Fender D, Harper WM, Gregg PJ. Outcome of Charnley total hip replacement across a single health region in England: the results at five years from a regional hip register. J Bone Joint Surg Br. 1999;81:577–581. doi: 10.1302/0301-620x.81b4.9859. [DOI] [PubMed] [Google Scholar]
- 21.Fender D, Harper WM, Gregg PJ. The trent regional arthroplasty study. Experiences with a hip register. J Bone Joint Surg Br. 2000;82:944–947. doi: 10.1302/0301-620x.82b7.10762. [DOI] [PubMed] [Google Scholar]
- 22.Hassan T, Birtwistle S, Power RA, Harper WM. Revision hip arthroplasty activity in a single UK health region: an audit of 1265 cases. Ann R Coll Surg Engl. 2000;82:283–286. [PMC free article] [PubMed] [Google Scholar]
- 23.Bourne RB, Sibbald WJ, Doig G, et al. The Southwestern Ontario Joint Replacement Pilot Project: electronic point-of-care data collection. Southwestern Ontario Study Group. Can J Surg. 2001;44:199–202. [PMC free article] [PubMed] [Google Scholar]
- 24.Stea S, Bordini B, Sudanese A, Toni A. Registration of hip prostheses at the Rizzoli Institute. 11 years’ experience. Acta Orthop Scand Suppl. 2002;73:40–44. doi: 10.1080/000164702760379549. [DOI] [PubMed] [Google Scholar]
- 25.Mantilla CB, Horlocker TT, Schroeder DR, et al. Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty. Anesthesiology. 2002;96:1140–1146. doi: 10.1097/00000542-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 26.Toni A, Stea S, Bordini B, Traina F. Lost to follow-up in a hip prosthesis register. Experience of R.I.P.O. Acta Orthop Scand Suppl. 2002;73:49–53. doi: 10.1080/000164702760379567. [DOI] [PubMed] [Google Scholar]
- 27.Fender D, van der Meulen JHP, Gregg PJ. Relationship between outcome and annual surgical experience for the charnley total hip replacement. Results from a regional hip register. J Bone Joint Surg Br. 2003;85:187–190. doi: 10.1302/0301-620x.85b2.12759. [DOI] [PubMed] [Google Scholar]
- 28.Gioe TJ, Killeen KK, Hoeffel DP, et al. Analysis of unicompartmental knee arthroplasty in a community-based implant registry. Clin Orthop Relat Res. 2003 doi: 10.1097/01.blo.0000093004.90435.d1. [DOI] [PubMed] [Google Scholar]
- 29.Kennedy LG, Newman JH, Ackroyd CE, Dieppe PA. When should we do knee replacements? Knee. 2003;10:161–166. doi: 10.1016/s0968-0160(02)00138-2. [DOI] [PubMed] [Google Scholar]
- 30.Malik MHA, Gambhir AK, Bale L, et al. Primary total hip replacement: a comparison of a nationally agreed guide to best practice and current surgical technique as determined by the North West Regional Arthroplasty Register. Ann R Coll Surg Engl. 2004;86:113–118. doi: 10.1308/003588404322827509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parvizi J, Ereth MH, Lewallen DG. Thirty-day mortality following hip arthroplasty for acute fracture. J Bone Joint Surg Am. 2004;86:1983–1988. doi: 10.2106/00004623-200409000-00017. [DOI] [PubMed] [Google Scholar]
- 32.Meenagh GK, McGibbon D, Nixon J, et al. Lack of support for the presence of an osteoarthritis susceptibility locus on chromosome 6p. Arthritis Rheum. 2005;52:2040–2043. doi: 10.1002/art.21120. [DOI] [PubMed] [Google Scholar]
- 33.Malik MHA, Chougle A, Pradhan N, et al. Primary total knee replacement: a comparison of a nationally agreed guide to best practice and current surgical technique as determined by the North West Regional Arthroplasty Register. Ann R Coll Surg Engl. 2005;87:117–122. doi: 10.1308/1478708051676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harse JD, Holman CDJ. Charlson’s Index was a poor predictor of quality of life outcomes in a study of patients following joint replacement surgery. J Clin Epidemiol. 2005;58:1142–1149. doi: 10.1016/j.jclinepi.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 35.Parvizi J, Kim K-I, Goldberg G, et al. Recurrent instability after total hip arthroplasty: beware of subtle component malpositioning. Clin Orthop Relat Res. 2006;447:60–65. doi: 10.1097/01.blo.0000218749.37860.7c. [DOI] [PubMed] [Google Scholar]
- 36.White SP, Smith EJ. Minimal access surgery for total hip arthroplasty—current beliefs and activity profile in the UK. Ann R Coll Surg Engl. 2007;89:36–40. doi: 10.1308/003588407X160800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gioe TJ, Sinner P, Mehle S, et al. Excellent survival of all-polyethylene tibial components in a community joint registry. Clin Orthop Relat Res. 2007;464:88–92. doi: 10.1097/BLO.0b013e31812f7879. [DOI] [PubMed] [Google Scholar]
- 38.Le Duff MJ, Amstutz HC, Dorey FJ. Metal-on-metal hip resurfacing for obese patients. J Bone Joint Surg Am. 2007;89:2705–2711. doi: 10.2106/JBJS.F.01563. [DOI] [PubMed] [Google Scholar]
- 39.Stea S, Bordini B, Viceconti M, et al. Is laterality associated with a higher rate of hip arthroplasty on the dominant side? Artif Organs. 2008;32:73–77. doi: 10.1111/j.1525-1594.2007.00457.x. [DOI] [PubMed] [Google Scholar]
- 40.Gandhi R, Davey JR, Mahomed NN. Predicting patient dissatisfaction following joint replacement surgery. J Rheumatol. 2008;35:2415–2418. doi: 10.3899/jrheum.080295. [DOI] [PubMed] [Google Scholar]
- 41.Middernacht B, De Wilde L, Molé D, et al. Glenosphere disengagement: a potentially serious default in reverse shoulder surgery. Clin Orthop Relat Res. 2008;466:892–898. doi: 10.1007/s11999-007-0090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dudley TE, Gioe TJ, Sinner P, Mehle S. Registry outcomes of unicompartmental knee arthroplasty revisions. Clin Orthop Relat Res. 2008;466:1666–1670. doi: 10.1007/s11999-008-0279-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stea S, Bordini B, De Clerico M, et al. First hip arthroplasty register in Italy: 55,000 cases and 7 year follow-up. Int Orthop. 2009;33:339–346. doi: 10.1007/s00264-007-0465-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Restrepo C, Ghanem E, Houssock C, et al. Isolated polyethylene exchange versus acetabular revision for polyethylene wear. Clin Orthop Relat Res. 2009;467:194–198. doi: 10.1007/s11999-008-0533-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Galat DD, McGovern SC, Larson DR, et al. Surgical treatment of early wound complications following primary total knee arthroplasty. J Bone Joint Surg Am. 2009;91:48–54. doi: 10.2106/JBJS.G.01371. [DOI] [PubMed] [Google Scholar]
- 46.Springer BD, Fehring TK, Griffin WL, et al. Why revision total hip arthroplasty fails. Clin Orthop Relat Res. 2009;467:166–173. doi: 10.1007/s11999-008-0566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hyer CF, Portera WB, Haglund EM. Lower extremity implant registries: Has the time come in the United States? Foot Ankle Spec. 2010;3:148–152. doi: 10.1177/1938640010369254. [DOI] [PubMed] [Google Scholar]
- 48.Gandhi R, Razak F, Davey JR, Mahomed NN. Metabolic syndrome and the functional outcomes of hip and knee arthroplasty. J Rheumatol. 2010;37:1917–1922. doi: 10.3899/jrheum.091242. [DOI] [PubMed] [Google Scholar]
- 49.Gandhi R, Dhotar H, Razak F, et al. Predicting the longer term outcomes of total knee arthroplasty. Knee. 2010;17:15–18. doi: 10.1016/j.knee.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 50.Gandhi R, Dhotar H, Davey JR, Mahomed NN. Predicting the longer-term outcomes of total hip replacement. J Rheumatol. 2010;37:2573–2577. doi: 10.3899/jrheum.100149. [DOI] [PubMed] [Google Scholar]
- 51.Lübbeke A, Garavaglia G, Barea C, Hoffmeyer P. Why do we need hospital-based registries? The Geneva Hip Arthroplasty Registry. Hug. 2010;22:66. [Google Scholar]
- 52.Schäfer T, Krummenauer F, Mettelsiefen J, et al. Social, educational, and occupational predictors of total hip replacement outcome. Osteoarthr Cartil. 2010;18:1036–1042. doi: 10.1016/j.joca.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 53.Ibrahim T, Bloch B, Esler CN, et al. Temporal trends in primary total hip and knee arthroplasty surgery: results from a UK regional joint register, 1991–2004. Ann R Coll Surg Engl. 2010;92:231–235. doi: 10.1308/003588410X12628812458572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gandhi R, Dhotar H, Tsvetkov D, Mahomed NN. The relation between body mass index and waist-hip ratio in knee osteoarthritis. Can J Surg. 2010;53:151–154. [PMC free article] [PubMed] [Google Scholar]
- 55.Bourne RB, Chesworth B, Davis A, et al. Comparing patient outcomes after THA and TKA: Is there a difference? Clin Orthop Relat Res. 2010;468:542–546. doi: 10.1007/s11999-009-1046-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mall NA, Nunley RM, Smith KE, et al. The fate of grafting acetabular defects during revision total hip arthroplasty. Clin Orthop Relat Res. 2010;468:3286–3294. doi: 10.1007/s11999-010-1427-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Di Tanna GL, Ferro S, Cipriani F, et al. Modeling the cost-effectiveness for cement-less and hybrid prosthesis in total hip replacement in Emilia Romagna, Italy. J Surg Res. 2011;169:227–233. doi: 10.1016/j.jss.2009.10.031. [DOI] [PubMed] [Google Scholar]
- 58.Singh JA, Lewallen DG. Association of peptic ulcer disease and pulmonary disease with risk of periprosthetic fracture after primary total knee arthroplasty. Arthritis Care Res. 2011;63:1471–1476. doi: 10.1002/acr.20548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ghomrawi HMK, Mandl LA, Rutledge J, et al. Is there a role for expectation maximization imputation in addressing missing data in research using WOMAC questionnaire? Comparison to the standard mean approach and a tutorial. BMC Musculoskelet Disord. 2011;12:109. doi: 10.1186/1471-2474-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Singh JA, Sperling JW, Cofield RH. Ninety day mortality and its predictors after primary shoulder arthroplasty: an analysis of 4,019 patients from 1976–2008. BMC Musculoskelet Disord. 2011;12:231. doi: 10.1186/1471-2474-12-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ebrahimpour PB, Do HT, Bornstein LJ, Westrich GH. Relationship between demographic variables and preoperative pain and disability in 5945 total joint arthroplasties at a single institution. J Arthroplasty. 2011;26:133–137.e1. doi: 10.1016/j.arth.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 62.Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: analysis of 2588 shoulders over three decades (1976 to 2008) J Bone Joint Surg Br. 2011;93:1513–1517. doi: 10.1302/0301-620X.93B11.26938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dushey CH, Bornstein LJ, Alexiades MM, Westrich GH. Short-term coagulation complications following total knee arthroplasty: a comparison of patient-reported and surgeon-verified complication rates. J Arthroplasty. 2011;26:1338–1342. doi: 10.1016/j.arth.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 64.Howard JL, Kremers HM, Loechler YA, et al. Comparative survival of uncemented acetabular components following primary total hip arthroplasty. J Bone Joint Surg Am. 2011;93:1597–1604. doi: 10.2106/JBJS.J.00195. [DOI] [PubMed] [Google Scholar]
- 65.Dowsey MM, Liew D, Choong PFM. Economic burden of obesity in primary total knee arthroplasty. Arthritis Care Res. 2011;63:1375–1381. doi: 10.1002/acr.20563. [DOI] [PubMed] [Google Scholar]
- 66.Zmistowski B, Restrepo C, Kahl LK, et al. Incidence and reasons for nonrevision reoperation after total knee arthroplasty. Clin Orthop Relat Res. 2011;469:138–145. doi: 10.1007/s11999-010-1558-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Abdel MP, Morrey ME, Jensen MR, Morrey BF. Increased long-term survival of posterior cruciate-retaining versus posterior cruciate-stabilizing total knee replacements. J Bone Joint Surg Am. 2011;93:2072–2078. doi: 10.2106/JBJS.J.01143. [DOI] [PubMed] [Google Scholar]
- 68.Alzahrani K, Gandhi R, Debeer J, et al. Prevalence of clinically significant improvement following total knee replacement. J Rheumatol. 2011;38:753–759. doi: 10.3899/jrheum.100233. [DOI] [PubMed] [Google Scholar]
- 69.Jacob AK, Mantilla CB, Sviggum HP, et al. Perioperative nerve injury after total knee arthroplasty: regional anesthesia risk during a 20-year cohort study. Anesthesiology. 2011;114:311–317. doi: 10.1097/ALN.0b013e3182039f5d. [DOI] [PubMed] [Google Scholar]
- 70.Gioe TJ, Sharma A, Tatman P, et al. Do “premium” joint implants add value?: analysis of high cost joint implants in a community registry. Clin Orthop Relat Res. 2011;469:48–54. doi: 10.1007/s11999-010-1436-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Callanan MC, Jarrett B, Bragdon CR, et al. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319–329. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Johnson TC, Tatman PJ, Mehle S, Gioe TJ. Revision surgery for patellofemoral problems: should we always resurface? Clin Orthop Relat Res. 2012;470:211–219. doi: 10.1007/s11999-011-2036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Singh JA, Sperling JW, Cofield RH. Cardiopulmonary complications after primary shoulder arthroplasty: a cohort study. Semin Arthritis Rheum. 2012;41:689–697. doi: 10.1016/j.semarthrit.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Choi JK, Geller JA, Yoon RS, et al. Comparison of total hip and knee arthroplasty cohorts and short-term outcomes from a single-center joint registry. J Arthroplasty. 2012;27:837–841. doi: 10.1016/j.arth.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 75.Wang W, Geller JA, Nyce JD, et al. Does ipsilateral knee pain improve after hip arthroplasty? Clin Orthop Relat Res. 2012;470:578–583. doi: 10.1007/s11999-011-2116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Singh JA, Lewallen DG. Ninety-day mortality in patients undergoing elective total hip or total knee arthroplasty. J Arthroplasty. 2012;27:1417–1422.e1. doi: 10.1016/j.arth.2012.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Singh JA, Jensen MR, Lewallen DG. Patient factors predict periprosthetic fractures after revision total hip arthroplasty. J Arthroplasty. 2012;27:1507–1512. doi: 10.1016/j.arth.2011.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Singh JA, Lewallen DG. Peptic ulcer disease and heart disease are associated with periprosthetic fractures after total hip replacement. Acta Orthop. 2012;83:353–359. doi: 10.3109/17453674.2012.717844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sviggum HP, Jacob AK, Mantilla CB, et al. Perioperative nerve injury after total shoulder arthroplasty: assessment of risk after regional anesthesia. Reg Anesth Pain Med. 2012;37:490–494. doi: 10.1097/AAP.0b013e31825c258b. [DOI] [PubMed] [Google Scholar]
- 80.Singh JA, Sperling JW, Schleck C, et al. Periprosthetic infections after shoulder hemiarthroplasty. J Shoulder Elbow Surg. 2012;21:1304–1309. doi: 10.1016/j.jse.2011.08.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Singh JA, Lewallen DG. Predictors of use of pain medications for persistent knee pain after primary Total Knee Arthroplasty: a cohort study using an institutional joint registry. Arthritis Res Ther. 2012;14:R248. doi: 10.1186/ar4091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Singh JA, Sperling JW, Cofield RH. Risk factors for revision surgery after humeral head replacement: 1,431 shoulders over 3 decades. J Shoulder Elbow Surg. 2012;21:1039–1044. doi: 10.1016/j.jse.2011.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yu Y-H, Chen AC-Y, Hu C-C, et al. Acute delirium and poor compliance in total hip arthroplasty patients with substance abuse disorders. J Arthroplasty. 2012;27:1526–1529. doi: 10.1016/j.arth.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 84.Singh JA, Sperling J, Schleck C, et al. Periprosthetic fractures associated with primary total shoulder arthroplasty and primary humeral head replacement: a thirty-three-year study. J Bone Joint Surg Am. 2012;94:1777–1785. doi: 10.2106/JBJS.J.01945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kubista B, Hartzler RU, Wood CM, et al. Reinfection after two-stage revision for periprosthetic infection of total knee arthroplasty. Int Orthop. 2012;36:65–71. doi: 10.1007/s00264-011-1267-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Plate JF, Seyler TM, Stroh DA, et al. Risk of dislocation using large- vs. small-diameter femoral heads in total hip arthroplasty. BMC Res Notes. 2012;5:553. doi: 10.1186/1756-0500-5-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Labek G, Kovac S, Levasic V, et al. The outcome of the cementless tapered SL-Plus stem: an analysis of arthroplasty register data. Int Orthop. 2012;36:1149–1154. doi: 10.1007/s00264-011-1421-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Severson EP, Singh JA, Browne JA, et al. Total knee arthroplasty in morbidly obese patients treated with bariatric surgery: a comparative study. J Arthroplasty. 2012;27:1696–1700. doi: 10.1016/j.arth.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Barr CJ, Barbalace RJ, Wessinger SJ, et al. Validation of a hospital-based joint registry: quantification of errors and maximizing utility. J Arthroplasty. 2012;27:1766–1771. doi: 10.1016/j.arth.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 90.Lawless BM, Greene M, Slover J, et al. Does age or bilateral disease influence the value of hip arthroplasty? Clin Orthop Relat Res. 2012;470:1073–1078. doi: 10.1007/s11999-011-2118-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Farshad M, Grögli M, Catanzaro S, Gerber C. Revision of reversed total shoulder arthroplasty Indications and outcome. BMC Musculoskelet Disord. 2012;13:160. doi: 10.1186/1471-2474-13-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Singh JA, Lewallen DG. Better functional and similar pain outcomes in osteoarthritis compared to rheumatoid arthritis after primary total knee arthroplasty: a cohort study. Arthritis Care Res. 2013;65:1936–1941. doi: 10.1002/acr.22090. [DOI] [PubMed] [Google Scholar]
- 93.Riddle DL, Singh JA, Harmsen WS, et al. Clinically important body weight gain following knee arthroplasty: a five-year comparative cohort study. Arthritis Care Res. 2013;65:669–677. doi: 10.1002/acr.21880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Riddle DL, Singh JA, Harmsen WS, et al. Clinically important body weight gain following total hip arthroplasty: a cohort study with 5-year follow-up. Osteoarthr Cartil. 2013;21:35–43. doi: 10.1016/j.joca.2012.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Singh JA, Lewallen DG. Diabetes: a risk factor for poor functional outcome after total knee arthroplasty. PLoS ONE. 2013;8:e78991. doi: 10.1371/journal.pone.0078991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Singh JA, Lewallen DG. Medical and psychological comorbidity predicts poor pain outcomes after total knee arthroplasty. Rheumatology. 2013;52:916–923. doi: 10.1093/rheumatology/kes402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Singh JA, Lewallen DG. Medical comorbidity is associated with persistent index hip pain after total hip arthroplasty. Pain Med. 2013;14:1222–1229. doi: 10.1111/pme.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vulcano E, Lee Y-Y, Yamany T, et al. Obese patients undergoing total knee arthroplasty have distinct preoperative characteristics: an institutional study of 4718 patients. J Arthroplasty. 2013;28:1125–1129. doi: 10.1016/j.arth.2012.10.028. [DOI] [PubMed] [Google Scholar]
- 99.Singh JA, Lewallen DG. Operative diagnosis for revision total hip arthroplasty is associated with patient-reported outcomes (PROs) BMC Musculoskelet Disord. 2013;14:210. doi: 10.1186/1471-2474-14-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Singh JA, Lewallen DG. Patient-level clinically meaningful improvements in activities of daily living and pain after total hip arthroplasty: data from a large US institutional registry. Rheumatology. 2013;52:1109–1118. doi: 10.1093/rheumatology/kes416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Singh JA, Jensen M, Lewallen D. Predictors of periprosthetic fracture after total knee replacement: an analysis of 21,723 cases. Acta Orthop. 2013;84:170–177. doi: 10.3109/17453674.2013.788436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Girard J, Kern G, Migaud H, et al. Primary total hip arthroplasty revision due to dislocation: prospective French multicenter study. Orthop Traumatol Surg Res. 2013;99:549–553. doi: 10.1016/j.otsr.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 103.Lübbeke A, Garavaglia G, Rothman KJ, et al. Statins may reduce femoral osteolysis in patients with total Hip arthroplasty. J Orthop Res. 2013;31:814–820. doi: 10.1002/jor.22262. [DOI] [PubMed] [Google Scholar]
- 104.Delaunay C, Hamadouche M, Girard J, Duhamel A. What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res. 2013;471:3863–3869. doi: 10.1007/s11999-013-2935-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Olivecrona C, Lapidus LJ, Benson L, Blomfeldt R. Tourniquet time affects postoperative complications after knee arthroplasty. Int Orthop. 2013;37:827–832. doi: 10.1007/s00264-013-1826-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Duncan CM, Moeschler SM, Horlocker TT, et al. A self-paired comparison of perioperative outcomes before and after implementation of a clinical pathway in patients undergoing total knee arthroplasty. Reg Anesth Pain Med. 2013;38:533–538. doi: 10.1097/AAP.0000000000000014. [DOI] [PubMed] [Google Scholar]
- 107.Wasserstein D, Farlinger C, Brull R, et al. Advanced age, obesity and continuous femoral nerve blockade are independent risk factors for inpatient falls after primary total knee arthroplasty. J Arthroplasty. 2013;28:1121–1124. doi: 10.1016/j.arth.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 108.Siow WM, Chin PL, Chia SL, et al. Comparative demographics, ROM, and function after TKA in Chinese, Malays, and Indians. Clin Orthop Relat Res. 2013;471:1451–1457. doi: 10.1007/s11999-012-2776-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Beyer-Westendorf J, Lützner J, Donath L, et al. Efficacy and safety of thromboprophylaxis with low-molecular-weight heparin or rivaroxaban in hip and knee replacement surgery: findings from the ORTHO-TEP registry. Thromb Haemost. 2013;109:154–163. doi: 10.1160/TH12-07-0510. [DOI] [PubMed] [Google Scholar]
- 110.Singh JA, Lewallen DG. Income and patient-reported outcomes (PROs) after primary total knee arthroplasty. BMC Med. 2013;11:62. doi: 10.1186/1741-7015-11-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Baker P, Muthumayandi K, Gerrand C, et al. Influence of body mass index (BMI) on functional improvements at 3 years following total knee replacement: a retrospective cohort study. PLoS ONE. 2013;8:e59079. doi: 10.1371/journal.pone.0059079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Singh JA, Lewallen DG. Ipsilateral lower extremity joint involvement increases the risk of poor pain and function outcomes after hip or knee arthroplasty. BMC Med. 2013;11:144. doi: 10.1186/1741-7015-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Johnson BK, Goodman SM, Alexiades MM, et al. Patterns and associated risk of perioperative use of anti-tumor necrosis factor in patients with rheumatoid arthritis undergoing total knee replacement. J Rheumatol. 2013;40:617–623. doi: 10.3899/jrheum.121171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sierra RJ, Kassel CA, Wetters NG, et al. Revision of unicompartmental arthroplasty to total knee arthroplasty: not always a slam dunk! J Arthroplasty. 2013;28:128–132. doi: 10.1016/j.arth.2013.02.040. [DOI] [PubMed] [Google Scholar]
- 115.Argenson J-N, Boisgard S, Parratte S, et al. Survival analysis of total knee arthroplasty at a minimum 10 years’ follow-up: a multicenter French nationwide study including 846 cases. Orthop Traumatol Surg Res. 2013;99:385–390. doi: 10.1016/j.otsr.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 116.Suero EM, Citak M, Claps C, et al. Variations in ankle registration using two different anatomic landmarks: a radiographic study. Knee Surg Sports Traumatol Arthrosc. 2013;21:2759–2763. doi: 10.1007/s00167-012-2165-5. [DOI] [PubMed] [Google Scholar]
- 117.Dakin H, Gray A, Murray D. Mapping analyses to estimate EQ-5D utilities and responses based on Oxford Knee Score. Qual Life Res. 2013;22:683–694. doi: 10.1007/s11136-012-0189-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kamath AF, Prieto H, Lewallen DG. Alternative bearings in total hip arthroplasty in the young patient. Orthop Clin N Am. 2013;44:451–462. doi: 10.1016/j.ocl.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 119.Colwell CWJ, Froimson MI, Anseth SD, et al. A mobile compression device for thrombosis prevention in hip and knee arthroplasty. J Bone Joint Surg Am. 2014;96:177–183. doi: 10.2106/JBJS.L.01031. [DOI] [PubMed] [Google Scholar]
- 120.Singh JA, Lewallen DG. Cerebrovascular disease is associated with outcomes after total knee arthroplasty: a US total joint registry study. J Arthroplasty. 2014;29:40–43. doi: 10.1016/j.arth.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ast MP, Gorab AH, Banka TR, et al. Clinical outcomes of patients with non-fatal VTE after total knee arthroplasty. J Arthroplasty. 2014;29:37–39. doi: 10.1016/j.arth.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 122.Kremers HM, Sierra RJ, Schleck CD, et al. Comparative survivorship of different tibial designs in primary total knee arthroplasty. J Bone Joint Surg Am. 2014;96:e121. doi: 10.2106/JBJS.M.00820. [DOI] [PubMed] [Google Scholar]
- 123.Hansen VJ, Greene ME, Bragdon MA, et al. Registries collecting level-I through IV Data: institutional and multicenter use: AAOS exhibit selection. J Bone Joint Surg Am. 2014;96:e160. doi: 10.2106/JBJS.M.01458. [DOI] [PubMed] [Google Scholar]
- 124.Seah RB, Yeo SJ, Chin PL, et al. Evaluation of medial-lateral stability and functional outcome following total knee arthroplasty: results of a single hospital joint registry. J Arthroplasty. 2014;29:2276–2279. doi: 10.1016/j.arth.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 125.Singh JA, Lewallen DG. Increasing obesity and comorbidity in patients undergoing primary total hip arthroplasty in the U.S.: a 13-year study of time trends. BMC Musculoskelet Disord. 2014;15:441. doi: 10.1186/1471-2474-15-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Owens CJ, Sperling JW, Cofield RH. Long-stemmed humeral components in primary shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1492–1498. doi: 10.1016/j.jse.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 127.Singh JA, Lewallen DG. Patient-level improvements in pain and activities of daily living after total knee arthroplasty. Rheumatology. 2014;53:313–320. doi: 10.1093/rheumatology/ket325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Goodman SM, Ramsden-Stein DN, Huang W-T, et al. Patients with rheumatoid arthritis are more likely to have pain and poor function after total hip replacements than patients with osteoarthritis. J Rheumatol. 2014;41:1774–1780. doi: 10.3899/jrheum.140011. [DOI] [PubMed] [Google Scholar]
- 129.Singh JA, Lewallen DG. Predictors of pain medication use for arthroplasty pain after revision total knee arthroplasty. Rheumatology. 2014;53:1752–1758. doi: 10.1093/rheumatology/ket443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ehlinger M, Delaunay C, Karoubi M, et al. Revision of primary total hip arthroplasty for peri-prosthetic fracture: a prospective epidemiological study of 249 consecutive cases in France. Orthop Traumatol Surg Res. 2014;100:657–662. doi: 10.1016/j.otsr.2014.03.030. [DOI] [PubMed] [Google Scholar]
- 131.Lübbeke A, Rothman KJ, Garavaglia G, et al. Strong association between smoking and the risk of revision in a cohort study of patients with metal-on-metal total hip arthroplasty. J Orthop Res. 2014;32:762–768. doi: 10.1002/jor.22603. [DOI] [PubMed] [Google Scholar]
- 132.Singh JA, Lewallen DG. Time trends in the characteristics of patients undergoing primary total knee arthroplasty. Arthritis Care Res. 2014;66:897–906. doi: 10.1002/acr.22233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Brophy RH, Gray BL, Nunley RM, et al. Total knee arthroplasty after previous knee surgery: expected interval and the effect on patient age. J Bone Joint Surg Am. 2014;96:801–805. doi: 10.2106/JBJS.M.00105. [DOI] [PubMed] [Google Scholar]
- 134.Noiseux NO, Long WJ, Mabry TM, et al. Uncemented porous tantalum acetabular components: early follow-up and failures in 613 primary total hip arthroplasties. J Arthroplasty. 2014;29:617–620. doi: 10.1016/j.arth.2013.07.037. [DOI] [PubMed] [Google Scholar]
- 135.Singh JA, Lewallen DG. Underlying diagnosis predicts patient-reported outcomes after revision total knee arthroplasty. Rheumatology. 2014;53:361–366. doi: 10.1093/rheumatology/ket357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Salassa T, Hoeffel D, Mehle S, et al. Efficacy of revision surgery for the dislocating total hip arthroplasty: report from a large community registry. Clin Orthop Relat Res. 2014;472:962–967. doi: 10.1007/s11999-013-3344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Singh JA, Lewallen DG. Are outcomes after total knee arthroplasty worsening over time? A time-trends study of activity limitation and pain outcomes. BMC Musculoskelet Disord. 2014;15:440. doi: 10.1186/1471-2474-15-440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ashraf A, Larson AN, Maradit-Kremers H, et al. Hospital costs of total hip arthroplasty for developmental dysplasia of the hip. Clin Orthop Relat Res. 2014;472:2237–2244. doi: 10.1007/s11999-014-3587-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Imam MA, Barke S, Stafford GH, et al. Loss to follow-up after total hip replacement: a source of bias in patient reported outcome measures and registry datasets? Hip Int. 2014;24:465–472. doi: 10.5301/hipint.5000141. [DOI] [PubMed] [Google Scholar]
- 140.Maradit Kremers H, Visscher SL, Kremers WK, et al. Obesity increases length of stay and direct medical costs in total hip arthroplasty. Clin Orthop Relat Res. 2014;472:1232–1239. doi: 10.1007/s11999-013-3316-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Adelani MA, Mall NA, Nyazee H, et al. Revision total hip arthroplasty with retained acetabular component. J Bone Joint Surg Am. 2014;96:1015–1020. doi: 10.2106/JBJS.L.01177. [DOI] [PubMed] [Google Scholar]
- 142.Kremers HM, Visscher SL, Kremers WK, et al. The effect of obesity on direct medical costs in total knee arthroplasty. J Bone Joint Surg Am. 2014;96:718–724. doi: 10.2106/JBJS.M.00819. [DOI] [PubMed] [Google Scholar]
- 143.Ahmadi S, Lawrence TM, Sahota S, et al. The incidence and risk factors for blood transfusion in revision shoulder arthroplasty: our institution’s experience and review of the literature. J Shoulder Elbow Surg. 2014;23:43–48. doi: 10.1016/j.jse.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 144.Christensen CP, Karthikeyan T, Jacobs CA. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty. 2014;29:1839–1841. doi: 10.1016/j.arth.2014.04.036. [DOI] [PubMed] [Google Scholar]
- 145.Bordini B, Stea S, Falcioni S, et al. Unicompartmental knee arthroplasty: 11-year experience from 3929 implants in RIPO register. Knee. 2014;21:1275–1279. doi: 10.1016/j.knee.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 146.Inacio MCS, Kritz-Silverstein D, Raman R, et al. The impact of pre-operative weight loss on incidence of surgical site infection and readmission rates after total joint arthroplasty. J Arthroplasty. 2014;29:458–64.e1. doi: 10.1016/j.arth.2013.07.030. [DOI] [PubMed] [Google Scholar]
- 147.Issa K, Rifai A, Boylan MR, et al. Do various factors affect the frequency of manipulation under anesthesia after primary total knee arthroplasty? Clin Orthop Relat Res. 2015;473:143–147. doi: 10.1007/s11999-014-3772-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Esposito CI, Gladnick BP, Lee Y-Y, et al. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty. 2015;30:109–113. doi: 10.1016/j.arth.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dowsey MM, Smith AJ, Choong PFM. Latent Class Growth Analysis predicts long term pain and function trajectories in total knee arthroplasty: a study of 689 patients. Osteoarthr Carti. 2015;23:2141–2149. doi: 10.1016/j.joca.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 150.Patel J, Lee JH, Li Z, et al. Predictors of low patient-reported outcomes response rates in the california joint replacement registry. J Arthroplasty. 2015;30:2071–2075. doi: 10.1016/j.arth.2015.06.029. [DOI] [PubMed] [Google Scholar]
- 151.Wiater BP, Koueiter DM, Maerz T, et al. Preoperative deltoid size and fatty infiltration of the deltoid and rotator cuff correlate to outcomes after reverse total shoulder arthroplasty. Clin Orthop Relat Res. 2015;473:663–673. doi: 10.1007/s11999-014-4047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Singh JA, Inacio MCS, Namba RS, Paxton EW. Rheumatoid arthritis is associated with higher ninety-day hospital readmission rates compared to osteoarthritis after hip or knee arthroplasty: a cohort study. Arthritis Care Res. 2015;67:718–724. doi: 10.1002/acr.22497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Morris BJ, Haigler RE, Laughlin MS, et al. Workers’ compensation claims and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:453–459. doi: 10.1016/j.jse.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 154.Wilke B, Wagner E, Trousdale R. Long-term survival of a semi-constrained implant following revision for infection. J Arthroplasty. 2015;30:808–812. doi: 10.1016/j.arth.2014.10.037. [DOI] [PubMed] [Google Scholar]
- 155.Lampropoulou-Adamidou K, Macheras GA, Hartofilakidis G. Bilateral character of total hip replacement does not change the overall survival. Hip Int. 2015;25:138–141. doi: 10.5301/hipint.5000202. [DOI] [PubMed] [Google Scholar]
- 156.Soukup DS, O’Malley MJ, Ellis SJ. Costs versus benefits of routine histopathological examination in total ankle replacement. Foot Ankle Int. 2015;36:801–805. doi: 10.1177/1071100715576371. [DOI] [PubMed] [Google Scholar]
- 157.Maradit Kremers H, Lewallen LW, Mabry TM, et al. Diabetes mellitus, hyperglycemia, hemoglobin A1C and the risk of prosthetic joint infections in total hip and knee arthroplasty. J Arthroplasty. 2015;30:439–443. doi: 10.1016/j.arth.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 158.Peel TN, Cheng AC, Liew D, et al. Direct hospital cost determinants following hip and knee arthroplasty. Arthritis Care Res. 2015;67:782–790. doi: 10.1002/acr.22523. [DOI] [PubMed] [Google Scholar]
- 159.Maradit Kremers H, Lewallen LW, Lahr BD, et al. Do claims-based comorbidities adequately capture case mix for surgical site infections? Clin Orthop Relat Res. 2015;473:1777–1786. doi: 10.1007/s11999-014-4083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Naranje S, Lendway L, Mehle S, Gioe TJ. Does operative time affect infection rate in primary total knee arthroplasty? Clin Orthop Relat Res. 2015;473:64–69. doi: 10.1007/s11999-014-3628-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Foster SA, Hambright DS, Antoci V, et al. Effects of obesity on health related quality of life following total hip arthroplasty. J Arthroplasty. 2015;30:1551–1554. doi: 10.1016/j.arth.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 162.Helwani MA, Avidan MS, Ben Abdallah A, et al. Effects of regional versus general anesthesia on outcomes after total hip arthroplasty: a retrospective propensity-matched cohort study. J Bone Joint Surg Am. 2015;97:186–193. doi: 10.2106/JBJS.N.00612. [DOI] [PubMed] [Google Scholar]
- 163.Wagner ER, Demark RV, 3rd, Wilson GA, et al. Intraoperative periprosthetic fractures associated with metacarpophalangeal joint arthroplasty. J Hand Surg Am. 2015;40:945–950. doi: 10.1016/j.jhsa.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 164.Fitch DA, Ancarani C, Bordini B. Long-term survivorship and complication rate comparison of a cementless modular stem and cementless fixed neck stems for primary total hip replacement. Int Orthop. 2015;39:1827–1832. doi: 10.1007/s00264-015-2894-4. [DOI] [PubMed] [Google Scholar]
- 165.Fehring TK, Fehring K, Odum SM. Metal artifact reduction sequence MRI abnormalities occur in metal-on-polyethylene hips. Clin Orthop Relat Res. 2015;473:574–580. doi: 10.1007/s11999-014-3873-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Houdek MT, Wagner ER, Watts CD, et al. Morbid obesity: a significant risk factor for failure of two-stage revision total hip arthroplasty for infection. J Bone Joint Surg Am. 2015;97:326–332. doi: 10.2106/JBJS.N.00515. [DOI] [PubMed] [Google Scholar]
- 167.Gulotta LV, Chambers KL, Warren RF, et al. No differences in early results of a hybrid glenoid compared with a pegged implant. Clin Orthop Relat Res. 2015;473:3918–3924. doi: 10.1007/s11999-015-4558-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Thambiah MD, Nathan S, Seow BZX, et al. Patient satisfaction after total knee arthroplasty: an Asian perspective. Singapore Med J. 2015;56:259–263. doi: 10.11622/smedj.2015074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Yuan BJ, Lewallen DG, Hanssen AD. Porous metal acetabular components have a low rate of mechanical failure in THA after operatively treated acetabular fracture. Clin Orthop Relat Res. 2015;473:536–542. doi: 10.1007/s11999-014-3852-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Maratt JD, Lee Y, Lyman S, Westrich GH. Predictors of satisfaction following total knee arthroplasty. J Arthroplasty. 2015;30:1142–1145. doi: 10.1016/j.arth.2015.01.039. [DOI] [PubMed] [Google Scholar]
- 171.Hurst JM, Berend KR, Adams JB, Lombardi AVJ. Radiographic comparison of mobile-bearing partial knee single-peg versus twin-peg design. J Arthroplasty. 2015;30:475–478. doi: 10.1016/j.arth.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 172.Stryker LS, Odum SM, Fehring TK, Springer BD. Revisions of monoblock metal-on-metal THAs have high early complication rates. Clin Orthop Relat Res. 2015;473:469–474. doi: 10.1007/s11999-014-3791-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ast MP, Abdel MP, Lee Y-Y, et al. Weight changes after total hip or knee arthroplasty: prevalence, predictors, and effects on outcomes. J Bone Joint Surg Am. 2015;97:911–919. doi: 10.2106/JBJS.N.00232. [DOI] [PubMed] [Google Scholar]
- 174.Wagner ER, Houdek MT, Elhassan BT, et al. What are risk factors for intraoperative humerus fractures during revision reverse shoulder arthroplasty and do they influence outcomes? Clin Orthop Relat Res. 2015;473:3228–3234. doi: 10.1007/s11999-015-4448-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Blomfeldt R, Kasina P, Ottosson C, et al. Prosthetic joint infection following hip fracture and degenerative hip disorder: a cohort study of three thousand, eight hundred and seven consecutive hip arthroplasties with a minimum follow-up of five years. Int Orthop. 2015;39:2091–2096. doi: 10.1007/s00264-015-2989-y. [DOI] [PubMed] [Google Scholar]
- 176.Winther SB, Foss OA, Wik TS, et al. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing fast-track. Acta Orthop. 2015;86:78–85. doi: 10.3109/17453674.2014.957089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Asaad A, Hart A, Khoo MMY, et al. Frequent femoral neck osteolysis with Birmingham mid-head resection resurfacing arthroplasty in young patients. Clin Orthop Relat Res. 2015;473:3770–3778. doi: 10.1007/s11999-015-4348-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Mackie A, Muthumayandi K, Shirley M, et al. Association between body mass index change and outcome in the first year after total knee arthroplasty. J Arthroplasty. 2015;30:206–209. doi: 10.1016/j.arth.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 179.Watts CD, Abdel MP, Lewallen DG, et al. Increased risk of periprosthetic femur fractures associated with a unique cementless stem design. Clin Orthop Relat Res. 2015;473:2045–2053. doi: 10.1007/s11999-014-4077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Watts CD, Wagner ER, Houdek MT, et al. Morbid obesity: increased risk of failure after aseptic revision TKA. Clin Orthop Relat Res. 2015;473:2621–2627. doi: 10.1007/s11999-015-4283-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.McLawhorn AS, Bjerke-Kroll BT, Blevins JL, et al. Patient-reported allergies are associated with poorer patient satisfaction and outcomes after lower extremity arthroplasty: a retrospective cohort study. J Arthroplasty. 2015;30:1132–1136. doi: 10.1016/j.arth.2015.01.043. [DOI] [PubMed] [Google Scholar]
- 182.Morris BJ, Laughlin MS, Elkousy HA, et al. Preoperative opioid use and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:11–16. doi: 10.1016/j.jse.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 183.Morris BJ, O’Connor DP, Torres D, et al. Risk factors for periprosthetic infection after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:161–166. doi: 10.1016/j.jse.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 184.Keeney JA, Martell JM, Pashos G, et al. Highly cross-linked polyethylene improves wear and mid-term failure rates for young total hip arthroplasty patients. Hip Int. 2015;25:435–441. doi: 10.5301/hipint.5000242. [DOI] [PubMed] [Google Scholar]
- 185.Hightower CD, Hightower LS, Tatman PJ, et al. How often is the office visit needed? Predicting total knee arthroplasty revision risk using pain/function scores. BMC Health Serv Res. 2016;16:429. doi: 10.1186/s12913-016-1669-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Maratt JD, Gagnier JJ, Butler PD, et al. No difference in dislocation seen in anterior vs posterior approach total hip arthroplasty. J Arthroplasty. 2016;31:127–130. doi: 10.1016/j.arth.2016.02.071. [DOI] [PubMed] [Google Scholar]
- 187.Goodman SM, Mandl LA, Parks ML, et al. Disparities in TKA outcomes: census tract data show interactions between race and poverty. Clin Orthop Relat Res. 2016;474:1986–1995. doi: 10.1007/s11999-016-4919-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Lum ZC, Lombardi AV, Hurst JM, et al. Early outcomes of twin-peg mobile-bearing unicompartmental knee arthroplasty compared with primary total knee arthroplasty. Bone Joint J. 2016;98-B:28–33. doi: 10.1302/0301-620X.98B10.BJJ-2016-0414.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Bordini B, Ancarani C, Fitch DA. Long-term survivorship of a medial-pivot total knee system compared with other cemented designs in an arthroplasty registry. J Orthop Surg Res. 2016;11:44. doi: 10.1186/s13018-016-0388-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Watts CD, Martin JR, Houdek MT, et al. Prior bariatric surgery may decrease the rate of re-operation and revision following total hip arthroplasty. Bone Joint J. 2016;98-B:1180–1184. doi: 10.1302/0301-620X.98B9.37943. [DOI] [PubMed] [Google Scholar]
- 191.Hansen LE, Stone GL, Matson CA, et al. Total joint arthroplasty in patients taking methadone or buprenorphine/naloxone preoperatively for prior heroin addiction: a prospective matched cohort study. J Arthroplasty. 2016;31:1698–1701. doi: 10.1016/j.arth.2016.01.032. [DOI] [PubMed] [Google Scholar]
- 192.Bin Abd Razak HR, Tan C-S, Chen YJD, et al. Age and preoperative knee society score are significant predictors of outcomes among asians following total knee arthroplasty. J Bone Joint Surg Am. 2016;98:735–741. doi: 10.2106/JBJS.15.00280. [DOI] [PubMed] [Google Scholar]
- 193.Werner BC, Wong AC, Mahony GT, et al. Causes of poor postoperative improvement after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25:e217–e222. doi: 10.1016/j.jse.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 194.Wagner ER, Kamath AF, Fruth KM, et al. Effect of body mass index on complications and reoperations after total hip arthroplasty. J Bone Joint Surg Am. 2016;98:169–179. doi: 10.2106/JBJS.O.00430. [DOI] [PubMed] [Google Scholar]
- 195.Wagner ER, Kamath AF, Fruth K, et al. Effect of body mass index on reoperation and complications after total knee arthroplasty. J Bone Joint Surg Am. 2016;98:2052–2060. doi: 10.2106/JBJS.16.00093. [DOI] [PubMed] [Google Scholar]
- 196.Haase E, Kopkow C, Beyer F, et al. Patient-reported outcomes and outcome predictors after primary total hip arthroplasty: results from the Dresden Hip Surgery Registry. Hip Int. 2016;26:73–81. doi: 10.5301/hipint.5000300. [DOI] [PubMed] [Google Scholar]
- 197.Schilling C, Dowsey MM, Clarke PM, Choong PF. Using patient-reported outcomes for economic evaluation: getting the timing right. Value Health. 2016;19:945–950. doi: 10.1016/j.jval.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 198.Benditz A, Drescher J, Greimel F, et al. Implementing a benchmarking and feedback concept decreases postoperative pain after total knee arthroplasty: a prospective study including 256 patients. Sci Rep. 2016;6:38218. doi: 10.1038/srep38218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Hussey DK, Madanat R, Donahue GS, et al. Worse health-related quality of life and hip function in female patients with elevated chromium levels. Acta Orthop. 2016;87:485–491. doi: 10.1080/17453674.2016.1213596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.D’Apuzzo MR, Villa JM, Alcerro JC, et al. Total joint arthroplasty: a granular analysis of outcomes in the economically disadvantaged patient. J Arthroplasty. 2016;31:41–44. doi: 10.1016/j.arth.2016.02.066. [DOI] [PubMed] [Google Scholar]
- 201.Houdek MT, Wagner ER, Wyles CC, et al. All-polyethylene tibial components: an analysis of long-term outcomes and infection. J Arthroplasty. 2016;31:1476–1482. doi: 10.1016/j.arth.2015.12.048. [DOI] [PubMed] [Google Scholar]
- 202.Markel DC, Allen MW, Zappa NM. Can an arthroplasty registry help decrease transfusions in primary total joint replacement? A quality initiative. Clin Orthop Relat Res. 2016;474:126–131. doi: 10.1007/s11999-015-4470-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Guerrero-Ludueña RE, Comas M, Espallargues M, et al. Predicting the Burden of Revision Knee Arthroplasty: simulation of a 20-year Horizon. Value Health. 2016;19:680–687. doi: 10.1016/j.jval.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 204.Long G, Hao C, Li G, et al. Predictive value of B-type natriuretic peptide (BNP) for adverse cardiac events in patients undergoing primary total knee arthroplasty (TKA) J Orthop Sci. 2016;21:826–830. doi: 10.1016/j.jos.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 205.Hallstrom B, Singal B, Cowen ME, et al. The Michigan experience with safety and effectiveness of tranexamic acid use in hip and knee arthroplasty. J Bone Joint Surg Am. 2016;98:1646–1655. doi: 10.2106/JBJS.15.01010. [DOI] [PubMed] [Google Scholar]
- 206.Lyman S, Lee Y-Y, Franklin PD, et al. Validation of the HOOS, JR: a short-form hip replacement survey. Clin Orthop Relat Res. 2016;474:1472–1482. doi: 10.1007/s11999-016-4718-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Lyman S, Lee Y-Y, Franklin PD, et al. Validation of the KOOS, JR: a short-form knee arthroplasty outcomes survey. Clin Orthop Relat Res. 2016;474:1461–1471. doi: 10.1007/s11999-016-4719-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Werner BC, Chang B, Nguyen JT, et al. What change in american shoulder and elbow surgeons score represents a clinically important change after shoulder arthroplasty? Clin Orthop Relat Res. 2016;474:2672–2681. doi: 10.1007/s11999-016-4968-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Tetreault MW, Della Valle CJ, Bohl DD, et al. What factors influence the success of medial gastrocnemius flaps in the treatment of infected TKAs? Clin Orthop Relat Res. 2016;474:752–763. doi: 10.1007/s11999-015-4624-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Goodman SM, Johnson B, Zhang M, et al. Patients with rheumatoid arthritis have similar excellent outcomes after total knee replacement compared with patients with osteoarthritis. J Rheumatol. 2016;43:46–53. doi: 10.3899/jrheum.150525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Emerson RH, Alnachoukati O, Barrington J, Ennin K. The results of Oxford unicompartmental knee arthroplasty in the United States: a mean ten-year survival analysis. Bone Joint J. 2016;98-B:34–40. doi: 10.1302/0301-620X.98B10.BJJ-2016-0480.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Jacobs CA, Morris BJ, Sciascia AD, Edwards TB. Comparison of satisfied and dissatisfied patients 2 to 5 years after anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25:1128–1132. doi: 10.1016/j.jse.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 213.Haynes JA, Stambough JB, Sassoon AA, et al. Contemporary surgical indications and referral trends in revision total hip arthroplasty: a 10-year review. J Arthroplasty. 2016;31:622–625. doi: 10.1016/j.arth.2015.09.026. [DOI] [PubMed] [Google Scholar]
- 214.Wilson MD, Dowsey MM, Spelman T, Choong PFM. Impact of surgical experience on outcomes in total joint arthroplasties. ANZ J Surg. 2016;86:967–972. doi: 10.1111/ans.13513. [DOI] [PubMed] [Google Scholar]
- 215.Berliner JL, Brodke DJ, Chan V, et al. John Charnley Award: preoperative patient-reported outcome measures predict clinically meaningful improvement in function after THA. Clin Orthop Relat Res. 2016;474:321–329. doi: 10.1007/s11999-015-4350-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Morris BJ, Sciascia AD, Jacobs CA, Edwards TB. Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25:619–623. doi: 10.1016/j.jse.2015.09.017. [DOI] [PubMed] [Google Scholar]
- 217.Liu JN, Garcia GH, Mahony G, et al. Sports after shoulder arthroplasty: a comparative analysis of hemiarthroplasty and reverse total shoulder replacement. J Shoulder Elbow Surg. 2016;25:920–926. doi: 10.1016/j.jse.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 218.Shannak O, Palan J, Esler C. A regional registry study of 216 patients investigating if patient satisfaction after total knee arthroplasty changes over a time period of five to 20years. Knee. 2017;24:824–828. doi: 10.1016/j.knee.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 219.Gonzalez AI, Bartolone P, Lubbeke A, et al. Comparison of dual-mobility cup and unipolar cup for prevention of dislocation after revision total hip arthroplasty. Acta Orthop. 2017;88:18–23. doi: 10.1080/17453674.2016.1255482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Bautista MP, Bonilla GA, Mieth KW, et al. Data quality in institutional arthroplasty registries: description of a model of validation and report of preliminary results. J Arthroplasty. 2017;32:2065–2069. doi: 10.1016/j.arth.2017.02.030. [DOI] [PubMed] [Google Scholar]
- 221.Charles RJ, Singal BM, Urquhart AG, et al. Data sharing between providers and quality initiatives eliminate unnecessary nursing home admissions. J Arthroplasty. 2017;32:1418–1425. doi: 10.1016/j.arth.2016.11.041. [DOI] [PubMed] [Google Scholar]
- 222.Werner BC, Wong AC, Chang B, et al. Depression and patient-reported outcomes following total shoulder arthroplasty. J Bone Joint Surg Am. 2017;99:688–695. doi: 10.2106/JBJS.16.00541. [DOI] [PubMed] [Google Scholar]
- 223.Ghomrawi HMK, Mancuso CA, Dunning A, et al. Do surgeon expectations predict clinically important improvements in WOMAC scores after THA and TKA? Clin Orthop Relat Res. 2017;475:2150–2158. doi: 10.1007/s11999-017-5331-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Singleton N, Poutawera V. Does preoperative mental health affect length of hospital stay and functional outcomes following arthroplasty surgery? A registry-based cohort study. J Orthop Surg. 2017;25:2309499017718902. doi: 10.1177/2309499017718902. [DOI] [PubMed] [Google Scholar]
- 225.Franklin PD, Miozzari H, Christofilopoulos P, et al. Important patient characteristics differ prior to total knee arthroplasty and total hip arthroplasty between Switzerland and the United States. BMC Musculoskelet Disord. 2017;18:14. doi: 10.1186/s12891-016-1372-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Sanz-Ruiz P, Matas-Diez JA, Sanchez-Somolinos M, et al. Is the commercial antibiotic-loaded bone cement useful in prophylaxis and cost saving after knee and hip joint arthroplasty? The transatlantic paradox. J Arthroplasty. 2017;32:1095–1099. doi: 10.1016/j.arth.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 227.Ang J-GE, Bin Abd Razak HR, Howe T-S, et al. Obesity does not affect outcomes in hybrid versus cemented total knee arthroplasty in Asians. J Arthroplasty. 2017;32:3643–3646. doi: 10.1016/j.arth.2017.06.043. [DOI] [PubMed] [Google Scholar]
- 228.Schilling CG, Dowsey MM, Petrie DJ, et al. Predicting the long-term gains in health-related quality of life after total knee arthroplasty. J Arthroplasty. 2017;32:395–401.e2. doi: 10.1016/j.arth.2016.07.036. [DOI] [PubMed] [Google Scholar]
- 229.bin Abd Razak HR, Acharyya S, Tan S-M et al (2017) Predictors of midterm outcomes after medial unicompartmental knee arthroplasty in Asians. Clin Orthop Surg 9:432–438. 10.4055/cios.2017.9.4.432 [DOI] [PMC free article] [PubMed]
- 230.Rothermich MA, Nam D, Brophy RH, et al. The impact of prior surgery after total knee arthroplasty. J Knee Surg. 2017;30:57–62. doi: 10.1055/s-0036-1579666. [DOI] [PubMed] [Google Scholar]
- 231.Castagnini F, Sudanese A, Bordini B, et al. Total knee replacement in young patients: survival and causes of revision in a registry population. J Arthroplasty. 2017;32:3368–3372. doi: 10.1016/j.arth.2017.05.052. [DOI] [PubMed] [Google Scholar]
- 232.Wagner ER, Houdek MT, Schleck C, et al. Increasing body mass index is associated with worse outcomes after shoulder arthroplasty. J Bone Joint Surg Am. 2017;99:929–937. doi: 10.2106/JBJS.15.00255. [DOI] [PubMed] [Google Scholar]
- 233.Barlow BT, Oi KK, Lee Y-Y, et al. Incidence, indications, outcomes, and survivorship of stems in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25:3611–3619. doi: 10.1007/s00167-016-4227-6. [DOI] [PubMed] [Google Scholar]
- 234.Kosola J, Kaipia A, Laitinen MK, Nieminen J. Complications after surgical treatment of femoral neck fractures in men with alcohol dependence syndrome: retrospective register analysis of 154 cases. Arch Orthop Trauma Surg. 2017;137:967–973. doi: 10.1007/s00402-017-2713-z. [DOI] [PubMed] [Google Scholar]
- 235.Ghomrawi HMK, Lee Y-Y, Herrero C, et al. A crosswalk between UCLA and lower extremity activity scales. Clin Orthop Relat Res. 2017;475:542–548. doi: 10.1007/s11999-016-5130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.McLawhorn AS, Steinhaus ME, Southren DL, et al. Body mass index class is independently associated with health-related quality of life after primary total hip arthroplasty: an institutional registry-based study. J Arthroplasty. 2017;32:143–149. doi: 10.1016/j.arth.2016.06.043. [DOI] [PubMed] [Google Scholar]
- 237.Fehring TK, Fehring KA, Anderson LA, et al. Catastrophic varus collapse of the tibia in obese total knee arthroplasty. J Arthroplasty. 2017;32:1625–1629. doi: 10.1016/j.arth.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 238.Moussa ME, Lee Y-Y, Patel AR, Westrich GH. Clinical outcomes following the use of constrained condylar knees in primary total knee arthroplasty. J Arthroplasty. 2017;32:1869–1873. doi: 10.1016/j.arth.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 239.Sendi P, Lötscher PO, Kessler B, et al. Debridement and implant retention in the management of hip periprosthetic joint infection: outcomes following guided and rapid treatment at a single centre. Bone Joint J. 2017;99-B:330–336. doi: 10.1302/0301-620X.99B3.BJJ-2016-0609.R1. [DOI] [PubMed] [Google Scholar]
- 240.Maradit Kremers H, Schleck CD, Lewallen EA, et al. Diabetes mellitus and hyperglycemia and the risk of aseptic loosening in total joint arthroplasty. J Arthroplasty. 2017;32:S251–S253. doi: 10.1016/j.arth.2017.02.056. [DOI] [PubMed] [Google Scholar]
- 241.Rowan FE, Salvatore AJ, Lange JK, Westrich GH. Dual-mobility vs fixed-bearing total hip arthroplasty in patients under 55 years of age: a single-institution, matched-cohort analysis. J Arthroplasty. 2017;32:3076–3081. doi: 10.1016/j.arth.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 242.Swarup I, Henn CM, Nguyen JT, et al. Effect of pre-operative expectations on the outcomes following total shoulder arthroplasty. Bone Joint J. 2017;99-B:1190–1196. doi: 10.1302/0301-620X.99B9.BJJ-2016-1263.R1. [DOI] [PubMed] [Google Scholar]
- 243.Christ AB, Baral E, Koch C, et al. Patellofemoral arthroplasty conversion to total knee arthroplasty: retrieval analysis and clinical correlation. Knee. 2017;24:1233–1239. doi: 10.1016/j.knee.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 244.Yao JJ, Maradit Kremers H, Schleck CD, et al. Patient-reported outcomes can be used to streamline post-total hip arthroplasty follow-up to high-risk patients. J Arthroplasty. 2017;32:3319–3321. doi: 10.1016/j.arth.2017.05.033. [DOI] [PubMed] [Google Scholar]
- 245.Goh GS-H, Liow MHL, Bin Abd Razak HR, et al. Patient-reported outcomes, quality of life, and satisfaction rates in young patients aged 50 years or younger after total knee arthroplasty. J Arthroplasty. 2017;32:419–425. doi: 10.1016/j.arth.2016.07.043. [DOI] [PubMed] [Google Scholar]
- 246.Li Z, Esposito CI, Koch CN, et al. Polyethylene damage increases with varus implant alignment in posterior-stabilized and constrained condylar knee arthroplasty. Clin Orthop Relat Res. 2017;475:2981–2991. doi: 10.1007/s11999-017-5477-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Viste A, Perry KI, Taunton MJ, et al. Proximal femoral replacement in contemporary revision total hip arthroplasty for severe femoral bone loss: a review of outcomes. Bone Joint J. 2017;99-B:325–329. doi: 10.1302/0301-620X.99B3.BJJ-2016-0822.R1. [DOI] [PubMed] [Google Scholar]
- 248.Glanzmann CM, Kolling C, Schwyzer H-K, et al. Radiological and functional 24-month outcomes of resurfacing versus stemmed anatomic total shoulder arthroplasty. Int Orthop. 2017;41:375–384. doi: 10.1007/s00264-016-3310-4. [DOI] [PubMed] [Google Scholar]
- 249.Maradit Kremers H, Salduz A, Schleck CD, et al. Referral bias in primary total knee arthroplasty: retrospective analysis of 22,614 surgeries in a Tertiary Referral Center. J Arthroplasty. 2017;32:390–394. doi: 10.1016/j.arth.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 250.Crawford DA, Berend KR, Morris MJ, et al. Results of a modular revision system in total knee arthroplasty. J Arthroplasty. 2017;32:2792–2798. doi: 10.1016/j.arth.2017.03.076. [DOI] [PubMed] [Google Scholar]
- 251.Hernandez NM, Chalmers BP, Wagner ER, et al. Revision to reverse total shoulder arthroplasty restores stability for patients with unstable shoulder prostheses. Clin Orthop Relat Res. 2017;475:2716–2722. doi: 10.1007/s11999-017-5429-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Ledford CK, Statz JM, Chalmers BP, et al. Revision total hip and knee arthroplasties after solid organ transplant. J Arthroplasty. 2017;32:1560–1564. doi: 10.1016/j.arth.2016.11.047. [DOI] [PubMed] [Google Scholar]
- 253.Lim JBT, Chong HC, Pang HN, et al. Revision total knee arthroplasty for failed high tibial osteotomy and unicompartmental knee arthroplasty have similar patient-reported outcome measures in a two-year follow-up study. Bone Joint J. 2017;99-B:1329–1334. doi: 10.1302/0301-620X.99B10.BJJ-2017-0034.R1. [DOI] [PubMed] [Google Scholar]
- 254.Courtney PM, Huddleston JI, Iorio R, Markel DC. Socioeconomic risk adjustment models for reimbursement are necessary in primary total joint arthroplasty. J Arthroplasty. 2017;32:1–5. doi: 10.1016/j.arth.2016.06.050. [DOI] [PubMed] [Google Scholar]
- 255.Weber M, Benditz A, Woerner M, et al. Trainee surgeons affect operative time but not outcome in minimally invasive total hip arthroplasty. Sci Rep. 2017;7:6152. doi: 10.1038/s41598-017-06530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Kumar A, Bloch BV, Esler C. Trends in total hip arthroplasty in young patients—results from a regional register. Hip Int. 2017;27:443–448. doi: 10.5301/hipint.5000485. [DOI] [PubMed] [Google Scholar]
- 257.Wagner ER, Srnec JJ, Mehrotra K, Rizzo M. What are the risk factors and complications associated with intraoperative and postoperative fractures in total wrist arthroplasty? Clin Orthop Relat Res. 2017;475:2694–2700. doi: 10.1007/s11999-017-5442-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Chalmers BP, Ledford CK, Statz JM, et al. What risks are associated with primary THA in recipients of hematopoietic stem cell transplantation? Clin Orthop Relat Res. 2017;475:475–480. doi: 10.1007/s11999-016-5029-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Alentorn-Geli E, Clark NJ, Assenmacher AT, et al. What are the complications, survival, and outcomes after revision to reverse shoulder arthroplasty in patients older than 80 years? Clin Orthop Relat Res. 2017;475:2744–2751. doi: 10.1007/s11999-017-5406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Ledford CK, Chalmers BP, Statz JM, et al. Primary total knee arthroplasty after solid organ transplant: survivorship and complications. J Arthroplasty. 2017;32:101–105. doi: 10.1016/j.arth.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 261.Hurwit DJ, Liu JN, Garcia GH, et al. A comparative analysis of work-related outcomes after humeral hemiarthroplasty and reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:954–959. doi: 10.1016/j.jse.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 262.Brüggemann A, Fredlund E, Mallmin H, Hailer NP. Are porous tantalum cups superior to conventional reinforcement rings? Acta Orthop. 2017;88:35–40. doi: 10.1080/17453674.2016.1248315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Maradit Kremers H, Kremers WK, Berry DJ, Lewallen DG. Patient-reported outcomes can be used to identify patients at risk for total knee arthroplasty revision and potentially individualize postsurgery follow-up. J Arthroplasty. 2017;32:3304–3307. doi: 10.1016/j.arth.2017.05.043. [DOI] [PubMed] [Google Scholar]
- 264.Njathi CW, Johnson RL, Laughlin RS, et al. Complications after continuous posterior lumbar plexus blockade for total hip arthroplasty: a retrospective cohort study. Reg Anesth Pain Med. 2017;42:446–450. doi: 10.1097/AAP.0000000000000589. [DOI] [PubMed] [Google Scholar]
- 265.Lyman S, Lee Y-Y, McLawhorn AS, et al. What are the minimal and substantial improvements in the HOOS and KOOS and JR versions after total joint replacement? Clin Orthop Relat Res. 2018;476:2432–2441. doi: 10.1097/CORR.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Lange JK, Spiro SK, Westrich GH. Utilizing dual mobility components for first-time revision total hip arthroplasty for instability. J Arthroplasty. 2018;33:505–509. doi: 10.1016/j.arth.2017.09.029. [DOI] [PubMed] [Google Scholar]
- 267.Garriga C, Sanchez-Santos MT, Judge A, et al. Development of a model predicting non-satisfaction 1 year after primary total knee replacement in the UK and transportation to Switzerland. Sci Rep. 2018;8:3380. doi: 10.1038/s41598-018-21713-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Goodman SM, Mehta B, Zhang M, et al. Disparities in total hip arthroplasty outcomes: census tract data show interactions between race and community deprivation. J Am Acad Orthop Surg. 2018;26:e457–e464. doi: 10.5435/JAAOS-D-17-00393. [DOI] [PubMed] [Google Scholar]
- 269.Christensen TC, Wagner ER, Harmsen WS, et al. Effect of physical parameters on outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2018;100:1829–1837. doi: 10.2106/JBJS.18.00248. [DOI] [PubMed] [Google Scholar]
- 270.Pitta M, Esposito CI, Li Z, et al. Failure after modern total knee arthroplasty: a prospective study of 18,065 knees. J Arthroplasty. 2018;33:407–414. doi: 10.1016/j.arth.2017.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Gonzalez AI, Luime JJ, Uçkay I, et al. Is there an association between smoking status and prosthetic joint infection after primary total joint arthroplasty? J Arthroplasty. 2018;33:2218–2224. doi: 10.1016/j.arth.2018.02.069. [DOI] [PubMed] [Google Scholar]
- 272.Gladnick BP, Fehring KA, Odum SM, et al. Midterm survivorship after revision total hip arthroplasty with a custom triflange acetabular component. J Arthroplasty. 2018;33:500–504. doi: 10.1016/j.arth.2017.09.026. [DOI] [PubMed] [Google Scholar]
- 273.Goh GS-H, Liow MHL, Pang H-N, et al. Patients with poor baseline mental health undergoing unicompartmental knee arthroplasty have poorer outcomes. J Arthroplasty. 2018;33:2428–2434. doi: 10.1016/j.arth.2018.02.074. [DOI] [PubMed] [Google Scholar]
- 274.Matuszak SJ, Galea VP, Connelly JW, et al. Periprosthetic acetabular radiolucency progression in mid-term follow-up of the articular surface replacement hip system. Arch Orthop Trauma Surg. 2018;138:1021–1028. doi: 10.1007/s00402-018-2962-5. [DOI] [PubMed] [Google Scholar]
- 275.Halawi MJ, Cote MP, Singh H, et al. The effect of depression on patient-reported outcomes after total joint arthroplasty is modulated by baseline mental health: a registry study. J Bone Joint Surg Am. 2018;100:1735–1741. doi: 10.2106/JBJS.17.01677. [DOI] [PubMed] [Google Scholar]
- 276.Thomas C, Patel V, Mallick E, et al. The outcome of secondary resurfacing of the patella following total knee arthroplasty: results from the Trent and Wales Arthroplasty Register. Knee. 2018;25:146–152. doi: 10.1016/j.knee.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 277.Goh GS-H, Bin Abd Razak HR, Tay DK-J, et al. Unicompartmental knee arthroplasty achieves greater flexion with no difference in functional outcome, quality of life, and satisfaction vs total knee arthroplasty in patients younger than 55 years. A propensity score-matched cohort analysis. J Arthroplasty. 2018;33:355–361. doi: 10.1016/j.arth.2017.09.022. [DOI] [PubMed] [Google Scholar]
- 278.Ingelsrud LH, Roos EM, Terluin B, et al. Minimal important change values for the Oxford Knee Score and the Forgotten Joint Score at 1 year after total knee replacement. Acta Orthop. 2018;89:541–547. doi: 10.1080/17453674.2018.1480739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Mahony GT, Werner BC, Chang B, et al. Risk factors for failing to achieve improvement after anatomic total shoulder arthroplasty for glenohumeral osteoarthritis. J Shoulder Elbow Surg. 2018;27:968–975. doi: 10.1016/j.jse.2017.12.018. [DOI] [PubMed] [Google Scholar]
- 280.Franck F, Ouanezar H, Jacquel A, et al. The predictive factors of secondary patellar resurfacing in computer-assisted total knee arthroplasty. A prospective cohort study. Int Orthop. 2018;42:1051–1060. doi: 10.1007/s00264-017-3630-z. [DOI] [PubMed] [Google Scholar]
- 281.Ponzio DY, Chiu Y-F, Salvatore A, et al. An analysis of the influence of physical activity level on total knee arthroplasty expectations, satisfaction, and outcomes: increased revision in active patients at five to ten years. J Bone Joint Surg Am. 2018;100:1539–1548. doi: 10.2106/JBJS.17.00920. [DOI] [PubMed] [Google Scholar]
- 282.Siu KT, Ng FY, Chan PK, et al. Bacteriology and risk factors associated with periprosthetic joint infection after primary total knee arthroplasty: retrospective study of 2543 cases. Hong Kong Med J. 2018;24:152–157. doi: 10.12809/hkmj176885. [DOI] [PubMed] [Google Scholar]
- 283.Padgett DE, Christ AB, Joseph AD, et al. Discharge to inpatient rehab does not result in improved functional outcomes following primary total knee arthroplasty. J Arthroplasty. 2018;33:1663–1667. doi: 10.1016/j.arth.2017.12.033. [DOI] [PubMed] [Google Scholar]
- 284.Tan SM, Bin Abd Razak HR, Singh Rikhraj I. Early functional, radiological outcomes and satisfaction rates of total ankle arthroplasty in an Asian population. Foot Ankle Spec. 2018;11:425–432. doi: 10.1177/1938640017750252. [DOI] [PubMed] [Google Scholar]
- 285.Ford MC, Hellman MD, Kazarian GS, et al. Five to ten-year results of the birmingham hip resurfacing implant in the U.S.: a single institution’s experience. J Bone Joint Surg Am. 2018;100:1879–1887. doi: 10.2106/JBJS.17.01525. [DOI] [PubMed] [Google Scholar]
- 286.Menendez ME, Lawler SM, Ring D, Jawa A. High pain intensity after total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:2113–2119. doi: 10.1016/j.jse.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 287.Garfinkel JH, Gladnick BP, Roland N, Romness DW. Increased incidence of bleeding and wound complications with Factor-Xa Inhibitors after total joint arthroplasty. J Arthroplasty. 2018;33:533–536. doi: 10.1016/j.arth.2017.08.039. [DOI] [PubMed] [Google Scholar]
- 288.Boyer B, Bordini B, Caputo D, et al. Is Cross-linked polyethylene an improvement over conventional ultra-high molecular weight polyethylene in total knee arthroplasty? J Arthroplasty. 2018;33:908–914. doi: 10.1016/j.arth.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 289.Hartzler MA, Abdel MP, Sculco PK, et al. Otto Aufranc Award: dual-mobility constructs in revision THA reduced dislocation, rerevision, and reoperation compared with large femoral heads. Clin Orthop Relat Res. 2018;476:293–301. doi: 10.1007/s11999.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Statz JM, Wagner ER, Sperling JW, Cofield RH. Outcomes of shoulder arthroplasty in diabetic patients as assessed by peri-operative A1C. Int Orthop. 2018;42:1923–1934. doi: 10.1007/s00264-018-3874-2. [DOI] [PubMed] [Google Scholar]
- 291.Bautista M, Muskus M, Llinás A, et al. Peri-articular injection of an analgesic mixture in primary total hip arthroplasty: an effective strategy for pain control during the first post-operative day. Int Orthop. 2018;42:1803–1810. doi: 10.1007/s00264-018-3788-z. [DOI] [PubMed] [Google Scholar]
- 292.Weber M, Craiovan B, Woerner ML, et al. Predictors of outcome after primary total joint replacement. J Arthroplasty. 2018;33:431–435. doi: 10.1016/j.arth.2017.08.044. [DOI] [PubMed] [Google Scholar]
- 293.Chalmers BP, Tibbo ME, Trousdale RT, et al. Primary total hip arthroplasty for charcot arthropathy is associated with high complications but improved clinical outcomes. J Arthroplasty. 2018;33:2912–2918. doi: 10.1016/j.arth.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 294.Bao MH, Keeney BJ, Moschetti WE, et al. Resident participation is not associated with worse outcomes after TKA. Clin Orthop Relat Res. 2018;476:1375–1390. doi: 10.1007/s11999.0000000000000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Lombardi AVJ, Kolich MT, Berend KR, et al. Revision of unicompartmental knee arthroplasty to total knee arthroplasty: Is it as good as a primary result? J Arthroplasty. 2018;33:S105–S108. doi: 10.1016/j.arth.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 296.Weber M, Renkawitz T, Voellner F, et al. Revision surgery in total joint replacement is cost-intensive. Biomed Res Int. 2018;2018:8987104. doi: 10.1155/2018/8987104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Giardina F, Castagnini F, Stea S, et al. Short stems versus conventional stems in cementless total hip arthroplasty: a long-term registry study. J Arthroplasty. 2018;33:1794–1799. doi: 10.1016/j.arth.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 298.Boddapati V, Fu MC, Tetreault MW, et al. Short-term complications after revision hip arthroplasty for prosthetic joint infection are increased relative to noninfectious revisions. J Arthroplasty. 2018;33:2997–3002. doi: 10.1016/j.arth.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 299.Weber M, Worlicek M, Voellner F et al (2018) Surgical training does not affect operative time and outcome in total knee arthroplasty. PLoS ONE 13:e0197850. 10.1371/journal.pone.0197850 [DOI] [PMC free article] [PubMed]
- 300.Zhang L, Lix LM, Ayilara O, et al. The effect of multimorbidity on changes in health-related quality of life following hip and knee arthroplasty. Bone Joint J. 2018;100-B:1168–1174. doi: 10.1302/0301-620X.100B9.BJJ-2017-1372.R1. [DOI] [PubMed] [Google Scholar]
- 301.Konopka JF, Buly RL, Kelly BT, et al. The effect of prior hip arthroscopy on patient-reported outcomes after total hip arthroplasty: an institutional registry-based, matched cohort study. J Arthroplasty. 2018;33:1806–1812. doi: 10.1016/j.arth.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 302.Sershon RA, Tecle N, Della Valle CJ, et al. The impact of an acute, traumatic wound dehiscence on clinical outcomes following primary knee arthroplasty. J Arthroplasty. 2018;33:2613–2615. doi: 10.1016/j.arth.2018.02.090. [DOI] [PubMed] [Google Scholar]
- 303.Murphy BP d’S, Dowsey MM, Spelman T, Choong PFM (2018) The impact of older age on patient outcomes following primary total knee arthroplasty. Bone Joint J 100-B:1463–1470. 10.1302/0301-620X.100B11.BJJ-2017-0753.R6 [DOI] [PubMed]
- 304.Webb BT, Ulrich SD, MacKinlay KGW, et al. Use of shorter intramedullary guide for ipsilateral total knee arthroplasty following prior total hip arthroplasty. J Knee Surg. 2018;31:348–351. doi: 10.1055/s-0037-1603796. [DOI] [PubMed] [Google Scholar]
- 305.Hernandez NM, Parry JA, Mabry TM, Taunton MJ. Patients at risk: preoperative opioid use affects opioid prescribing, refills, and outcomes after total knee arthroplasty. J Arthroplasty. 2018;33:S142–S146. doi: 10.1016/j.arth.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 306.Yao JJ, Maradit Kremers H, Kremers WK, et al. Perioperative inpatient use of selective serotonin reuptake inhibitors is associated with a reduced risk of THA and TKA revision. Clin Orthop Relat Res. 2018;476:1191–1197. doi: 10.1007/s11999.0000000000000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Goodman SM, Mandl LA, Mehta B, et al. Does education level mitigate the effect of poverty on total knee arthroplasty outcomes? Arthritis Care Res. 2018;70:884–891. doi: 10.1002/acr.23442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Parry JA, Hernandez NM, Berry DJ, et al. Risk factors for subsidence of modular fluted tapered stems used during revision total hip arthroplasty for periprosthetic hip fractures. J Arthroplasty. 2018;33:2967–2970. doi: 10.1016/j.arth.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 309.Galea VP, Botros MA, Madanat R, et al. Promising early outcomes of a novel anatomic knee system. Knee Surg Sports Traumatol Arthrosc. 2019;27:1067–1074. doi: 10.1007/s00167-018-5248-0. [DOI] [PubMed] [Google Scholar]
- 310.Perneger T V, Hannouche D, Miozzari HH, Lübbeke A (2019) Symptoms of osteoarthritis influence mental and physical health differently before and after joint replacement surgery: A prospective study. PLoS ONE 14:e0217912. 10.1371/journal.pone.0217912 [DOI] [PMC free article] [PubMed]
- 311.Ferguson RJ, Silman AJ, Combescure C, et al. ASA class is associated with early revision and reoperation after total hip arthroplasty: an analysis of the Geneva and Swedish Hip Arthroplasty Registries. Acta Orthop. 2019;90:324–330. doi: 10.1080/17453674.2019.1605785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Hernandez NM, Fruth KM, Larson DR, et al. Conversion of hemiarthroplasty to THA carries an increased risk of reoperation compared with primary and revision THA. Clin Orthop Relat Res. 2019;477:1392–1399. doi: 10.1097/CORR.0000000000000702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Arias-de la Torre J, Valderas JM, Evans JP, et al. Differences in risk of revision and mortality between total and unicompartmental knee arthroplasty. The influence of hospital volume. J Arthroplasty. 2019;34:865–871. doi: 10.1016/j.arth.2019.01.046. [DOI] [PubMed] [Google Scholar]
- 314.Halawi MJ, Cote MP, Savoy L, et al. The effect of payer type on patient-reported outcomes in total joint arthroplasty is modulated by baseline patient characteristics. J Arthroplasty. 2019;34:1072–1075. doi: 10.1016/j.arth.2019.01.069. [DOI] [PubMed] [Google Scholar]
- 315.Harris WH, Muratoglu OK. The role of crosslinked polyethylene in reducing aggregated costs of total hip arthroplasty in the United States. J Arthroplasty. 2019;34:1089–1092. doi: 10.1016/j.arth.2019.02.038. [DOI] [PubMed] [Google Scholar]
- 316.Halawi MJ, Caminiti N, Cote MP, et al. The most significant risk factors for urinary retention in fast-track total joint arthroplasty are iatrogenic. J Arthroplasty. 2019;34:136–139. doi: 10.1016/j.arth.2018.08.042. [DOI] [PubMed] [Google Scholar]
- 317.Amanatullah DF, Lawson KA, Li Z, et al. Risk adjustment in the California Joint Replacement Registry: Is patient complexity accurately assessed in academic versus nonacademic hospitals? J Arthroplasty. 2020;35:3437–3444. doi: 10.1016/j.arth.2020.06.075. [DOI] [PubMed] [Google Scholar]
- 318.Hauser DL, Wessinger SJ, Condon RT, et al. An electronic database for outcome studies that includes digital radiographs. J Arthroplasty. 2001;16:71–75. doi: 10.1054/arth.2001.28366. [DOI] [PubMed] [Google Scholar]
- 319.Akisue T, Yamaguchi M, Bauer TW, et al. “Backside” polyethylene deformation in total knee arthroplasty. J Arthroplasty. 2003;18:784–791. doi: 10.1016/s0883-5403(03)00255-9. [DOI] [PubMed] [Google Scholar]
- 320.Pagnano MW, McLamb LA, Trousdale RT. Primary and revision total hip arthroplasty for patients 90 years of age and older. Mayo Clin Proc. 2003;78:285–288. doi: 10.4065/78.3.285. [DOI] [PubMed] [Google Scholar]
- 321.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85:259–265. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 322.Parvizi J, Sullivan T, Duffy G, Cabanela ME. Fifteen-year clinical survivorship of Harris-Galante total hip arthroplasty. J Arthroplasty. 2004;19:672–677. doi: 10.1016/j.arth.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 323.Schneiderbauer MM, von Knoch M, Schleck CD, et al. Patient survival after hip arthroplasty for metastatic disease of the hip. J Bone Joint Surg Am. 2004;86:1684–1689. doi: 10.2106/00004623-200408000-00011. [DOI] [PubMed] [Google Scholar]
- 324.Field RE, Singh PJ, Latif AMH, et al. Five-year prospective clinical and radiological results of a new cannulated cemented polished Tri-Taper femoral stem. J Bone Joint Surg Br. 2006;88:315–320. doi: 10.1302/0301-620X.88B3.17314. [DOI] [PubMed] [Google Scholar]
- 325.Parvizi J, Wade FA, Rapuri V, et al. Revision hip arthroplasty for late instability secondary to polyethylene wear. Clin Orthop Relat Res. 2006;447:66–69. doi: 10.1097/01.blo.0000218751.14989.a6. [DOI] [PubMed] [Google Scholar]
- 326.Sanchez-Sotelo J, Haidukewych GJ, Boberg CJ. Hospital cost of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2006;88:290–294. doi: 10.2106/JBJS.D.02799. [DOI] [PubMed] [Google Scholar]
- 327.Haidukewych GJ, Jacofsky DJ, Hanssen AD, Lewallen DG. Intraoperative fractures of the acetabulum during primary total hip arthroplasty. J Bone Joint Surg Am. 2006;88:1952–1956. doi: 10.2106/JBJS.E.00890. [DOI] [PubMed] [Google Scholar]
- 328.Burns AWR, Bourne RB, Chesworth BM, et al. Cost effectiveness of revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:29–33. doi: 10.1097/01.blo.0000214420.14088.76. [DOI] [PubMed] [Google Scholar]
- 329.Allami MK, Fender D, Khaw FM, et al. Outcome of Charnley total hip replacement across a single health region in England. The results at ten years from a regional arthroplasty register. J Bone Joint Surg Br. 2006;88:1293–1298. doi: 10.1302/0301-620X.88B10.17933. [DOI] [PubMed] [Google Scholar]
- 330.Cipriano LE, Chesworth BM, Anderson CK, Zaric GS. Predicting joint replacement waiting times. Health Care Manag Sci. 2007;10:195–215. doi: 10.1007/s10729-007-9013-z. [DOI] [PubMed] [Google Scholar]
- 331.Gioe TJ, Novak C, Sinner P, et al. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res. 2007;464:83–87. doi: 10.1097/BLO.0b013e31812f79a9. [DOI] [PubMed] [Google Scholar]
- 332.Cheung EV, Sperling JW, Cofield RH. Polyethylene insert exchange for wear after total shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16:574–578. doi: 10.1016/j.jse.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 333.Sierra RJ, Timperley JA, Gie GA. Contemporary cementing technique and mortality during and after Exeter total hip arthroplasty. J Arthroplasty. 2009;24:325–332. doi: 10.1016/j.arth.2008.01.301. [DOI] [PubMed] [Google Scholar]
- 334.Pinaroli A, Piedade SR, Servien E, Neyret P. Intraoperative fractures and ligament tears during total knee arthroplasty. A 1795 posterostabilized TKA continuous series. Orthop Traumatol Surg Res. 2009;95:183–189. doi: 10.1016/j.otsr.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 335.Larson AN, McIntosh AL, Trousdale RT, Lewallen DG. Avascular necrosis most common indication for hip arthroplasty in patients with slipped capital femoral epiphysis. J Pediatr Orthop. 2010;30:767–773. doi: 10.1097/BPO.0b013e3181fbe912. [DOI] [PubMed] [Google Scholar]
- 336.Kempton LB, Ankerson E, Wiater JM. A complication-based learning curve from 200 reverse shoulder arthroplasties. Clin Orthop Relat Res. 2011;469:2496–2504. doi: 10.1007/s11999-011-1811-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Noble PC, Durrani SK, Usrey MM, et al. Constrained cups appear incapable of meeting the demands of revision THA. Clin Orthop Relat Res. 2012;470:1907–1916. doi: 10.1007/s11999-011-2212-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Khan FA, Rose PS, Yanagisawa M, et al. Surgical technique: Porous tantalum reconstruction for destructive nonprimary periacetabular tumors. Clin Orthop Relat Res. 2012;470:594–601. doi: 10.1007/s11999-011-2117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Greenbaum JN, Bornstein LJ, Lyman S, et al. The validity of self-report as a technique for measuring short-term complications after total hip arthroplasty in a joint replacement registry. J Arthroplasty. 2012;27:1310–1315. doi: 10.1016/j.arth.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 340.Epinette J-A, Brunschweiler B, Mertl P, et al. Unicompartmental knee arthroplasty modes of failure: wear is not the main reason for failure: a multicentre study of 418 failed knees. Orthop Traumatol Surg Res. 2012;98:S124–S130. doi: 10.1016/j.otsr.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 341.Summers JC, Bedi HS. Reoperation and patient satisfaction after the Mobility total ankle arthroplasty. ANZ J Surg. 2013;83:371–375. doi: 10.1111/ans.12002. [DOI] [PubMed] [Google Scholar]
- 342.Clauss M, Gersbach S, Butscher A, Ilchmann T. Risk factors for aseptic loosening of Müller-type straight stems: a registry-based analysis of 828 consecutive cases with a minimum follow-up of 16 years. Acta Orthop. 2013;84:353–359. doi: 10.3109/17453674.2013.810517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Goldvasser D, Marchie A, Bragdon LK, et al. Incidence of osteolysis in total knee arthroplasty: comparison between radiographic and retrieval analysis. J Arthroplasty. 2013;28:201–206. doi: 10.1016/j.arth.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 344.Bergeson AG, Berend KR, Lombardi AVJ, et al. Medial mobile bearing unicompartmental knee arthroplasty: early survivorship and analysis of failures in 1000 consecutive cases. J Arthroplasty. 2013;28:172–175. doi: 10.1016/j.arth.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 345.Wechter J, Comfort TK, Tatman P, et al. Improved survival of uncemented versus cemented femoral stems in patients aged < 70 years in a community total joint registry. Clin Orthop Relat Res. 2013;471:3588–3595. doi: 10.1007/s11999-013-3182-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Figgie MP, Wright TM, Drinkwater D. What design and material factors impact the wear and corrosion performance in total elbow arthroplasties? Clin Orthop Relat Res. 2014;472:3770–3776. doi: 10.1007/s11999-014-3781-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Heekin RD, Fokin AA. Incidence of bicompartmental osteoarthritis in patients undergoing total and unicompartmental knee arthroplasty: is the time ripe for a less radical treatment? J Knee Surg. 2014;27:77–81. doi: 10.1055/s-0033-1349401. [DOI] [PubMed] [Google Scholar]
- 348.Streubel PN, Simone JP, Sperling JW, Cofield R. Thirty and ninety-day reoperation rates after shoulder arthroplasty. J Bone Joint Surg Am. 2014;96:e17. doi: 10.2106/JBJS.M.00127. [DOI] [PubMed] [Google Scholar]
- 349.Ramaskandhan JR, Kakwani R, Kometa S, et al. Two-year outcomes of MOBILITY Total Ankle Replacement. J Bone Joint Surg Am. 2014;96:e53. doi: 10.2106/JBJS.L.00536. [DOI] [PubMed] [Google Scholar]
- 350.Allepuz A, Martínez O, Tebé C, et al. Joint registries as continuous surveillance systems: the experience of the Catalan Arthroplasty Register (RACat) J Arthroplasty. 2014;29:484–490. doi: 10.1016/j.arth.2013.07.048. [DOI] [PubMed] [Google Scholar]
- 351.Bachmann M, Bolliger L, Ilchmann T, Clauss M. Long-term survival and radiological results of the Duracon™ total knee arthroplasty. Int Orthop. 2014;38:747–752. doi: 10.1007/s00264-013-2154-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Jacobs CA, Christensen CP, Karthikeyan T. Chronic non-orthopedic conditions more common in patients with less severe degenerative changes that have elected to undergo total knee arthroplasty. J Arthroplasty. 2015;30:1146–1149. doi: 10.1016/j.arth.2015.01.051. [DOI] [PubMed] [Google Scholar]
- 353.SooHoo NF, Li Z, Chenok KE, Bozic KJ. Responsiveness of patient reported outcome measures in total joint arthroplasty patients. J Arthroplasty. 2015;30:176–191. doi: 10.1016/j.arth.2014.09.026. [DOI] [PubMed] [Google Scholar]
- 354.von Roth P, Abdel MP, Harmsen WS, Berry DJ. Cemented bipolar hemiarthroplasty provides definitive treatment for femoral neck fractures at 20 years and beyond. Clin Orthop Relat Res. 2015;473:3595–3599. doi: 10.1007/s11999-015-4462-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Lavernia CJ, Villa JM. Does race affect outcomes in total joint arthroplasty? Clin Orthop Relat Res. 2015;473:3535–3541. doi: 10.1007/s11999-015-4481-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Wagner ER, Van Demark R III, Kor DJ et al (2015) Intraoperative periprosthetic fractures in proximal interphalangeal joint arthroplasty. J Hand Surg Am 40:2149–2154. 10.1016/j.jhsa.2015.06.101 [DOI] [PubMed]
- 357.Garcia GH, Taylor SA, DePalma BJ, et al. Patient activity levels after reverse total shoulder arthroplasty: what are patients doing? Am J Sports Med. 2015;43:2816–2821. doi: 10.1177/0363546515597673. [DOI] [PubMed] [Google Scholar]
- 358.Jacobs CA, Christensen CP, Karthikeyan T. Subchondral bone marrow edema had greater effect on postoperative pain after medial unicompartmental knee arthroplasty than total knee arthroplasty. J Arthroplasty. 2016;31:491–494. doi: 10.1016/j.arth.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 359.Fujishiro T, Hiranaka T, Hashimoto S, et al. The effect of acetabular and femoral component version on dislocation in primary total hip arthroplasty. Int Orthop. 2016;40:697–702. doi: 10.1007/s00264-015-2924-2. [DOI] [PubMed] [Google Scholar]
- 360.Lombardi AVJ, Berend KR, Adams JB, Satterwhite KL. Adverse reactions to metal on metal are not exclusive to large heads in total hip arthroplasty. Clin Orthop Relat Res. 2016;474:432–440. doi: 10.1007/s11999-015-4539-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Ouanezar H, Franck F, Jacquel A, et al. Does computer-assisted surgery influence survivorship of cementless total knee arthroplasty in patients with primary osteoarthritis? A 10-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2016;24:3448–3456. doi: 10.1007/s00167-016-4112-3. [DOI] [PubMed] [Google Scholar]
- 362.Brooks PJ. Hip resurfacing: a large, US single-surgeon series. Bone Joint J. 2016;98-B:10–13. doi: 10.1302/0301-620X.98B1.36360. [DOI] [PubMed] [Google Scholar]
- 363.Fehring KA, Howe BM, Martin JR, et al. Preoperative evaluation for pelvic discontinuity using a new reformatted computed tomography scan protocol. J Arthroplasty. 2016;31:2247–2251. doi: 10.1016/j.arth.2016.02.028. [DOI] [PubMed] [Google Scholar]
- 364.Chambers S, Ramaskandhan J, Siddique M. Radiographic severity of arthritis affects functional outcome in total ankle replacement (TAR) Foot Ankle Int. 2016;37:351–354. doi: 10.1177/1071100716638021. [DOI] [PubMed] [Google Scholar]
- 365.SooHoo NF, Li Z, Chan V, et al. The importance of risk adjustment in reporting total joint arthroplasty outcomes. J Arthroplasty. 2016;31:590–595. doi: 10.1016/j.arth.2015.09.041. [DOI] [PubMed] [Google Scholar]
- 366.Singh J, Politis A, Loucks L, et al. Trends in revision hip and knee arthroplasty observations after implementation of a regional joint replacement registry. Can J Surg. 2016;59:304–310. doi: 10.1503/cjs.002916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Chan VW, Chan PK, Chiu KY, et al. Why do Hong Kong patients need total hip arthroplasty? An analysis of 512 hips from 1998 to 2010. Hong Kong Med J. 2016;22:11–15. doi: 10.12809/hkmj144483. [DOI] [PubMed] [Google Scholar]
- 368.Albayrak I, Apiliogullari S, Dal CN, et al. Efficacy of pulsed radiofrequency therapy to dorsal root ganglion adding to tens and exercise for persistent pain after total knee arthroplasty. J Knee Surg. 2017;30:134–142. doi: 10.1055/s-0036-1583268. [DOI] [PubMed] [Google Scholar]
- 369.Zarling BJ, Sikora-Klak J, Bergum C, Markel DC. How do preoperative medications influence outcomes after total joint arthroplasty? J Arthroplasty. 2017;32:S259–S262. doi: 10.1016/j.arth.2017.04.031. [DOI] [PubMed] [Google Scholar]
- 370.Feng B, Lin J, Jin J, et al. Thirty-day postoperative complications following primary total knee arthroplasty: a retrospective study of incidence and Risk Factors at a Single Center in China. Chin Med J. 2017;130:2551–2556. doi: 10.4103/0366-6999.213071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Abdel MP, Ledford CK, Kobic A, et al. Contemporary failure aetiologies of the primary, posterior-stabilised total knee arthroplasty. Bone Joint J. 2017;99-B:647–652. doi: 10.1302/0301-620X.99B5.BJJ-2016-0617.R3. [DOI] [PubMed] [Google Scholar]
- 372.Ricciardi BF, Henderson PW, McLawhorn AS, et al. Gluteus maximus advancement flap procedure for reconstruction of posterior soft tissue deficiency in revision total hip arthroplasty. Orthopedics. 2017;40:e495–e500. doi: 10.3928/01477447-20170308-06. [DOI] [PubMed] [Google Scholar]
- 373.Markel DC, Allen MW, Hughes RE, et al. Quality initiative programs can decrease total joint arthroplasty transfusion rates—a multicenter study using the MARCQI Total Joint Registry Database. J Arthroplasty. 2017;32:3292–3297. doi: 10.1016/j.arth.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 374.Statz JM, Schoch BS, Sanchez-Sotelo J, et al. Shoulder arthroplasty for locked anterior shoulder dislocation: a role for the reversed design. Int Orthop. 2017;41:1227–1234. doi: 10.1007/s00264-017-3450-1. [DOI] [PubMed] [Google Scholar]
- 375.Statz JM, Chalmers BP, Ledford CK, et al. Outcomes of shoulder arthroplasty in haematopoietic stem cell transplant patients. Int Orthop. 2017;41:2555–2564. doi: 10.1007/s00264-017-3553-8. [DOI] [PubMed] [Google Scholar]
- 376.Rojas J, Bautista M, Bonilla G, et al. A retrospective study on the relationship between altered native acetabular angle and vertical implant malpositioning. Int Orthop. 2018;42:769–775. doi: 10.1007/s00264-017-3584-1. [DOI] [PubMed] [Google Scholar]
- 377.Postler A, Lützner C, Beyer F, et al. Analysis of total knee arthroplasty revision causes. BMC Musculoskelet Disord. 2018;19:55. doi: 10.1186/s12891-018-1977-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Torre M, Luzi I, Mirabella F, et al. Cross-cultural adaptation and validation of the Italian version of the Hip disability and Osteoarthritis Outcome Score (HOOS) Health Qual Life Outcomes. 2018;16:115. doi: 10.1186/s12955-018-0935-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Hurst JM, Ranieri R, Berend KR, et al. Outcomes after arthroscopic evaluation of patients with painful medial unicompartmental knee arthroplasty. J Arthroplasty. 2018;33:3268–3272. doi: 10.1016/j.arth.2018.05.031. [DOI] [PubMed] [Google Scholar]
- 380.Werthel J-D, Schoch B, Frankle M, et al. Shoulder arthroplasty for sequelae of obstetrical brachial plexus injury. J Hand Surg Am. 2018;43:871.e1–871.e7. doi: 10.1016/j.jhsa.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 381.Hughes RE, Zheng H, Igrisan RM, et al. The Michigan Arthroplasty Registry Collaborative Quality Initiative Experience: improving the quality of care in Michigan. J Bone Joint Surg Am. 2018;100:e143. doi: 10.2106/JBJS.18.00239. [DOI] [PubMed] [Google Scholar]
- 382.Kolling C, Borovac M, Audigé L, et al. Return to sports after reverse shoulder arthroplasty-the Swiss perspective. Int Orthop. 2018;42:1129–1135. doi: 10.1007/s00264-017-3715-8. [DOI] [PubMed] [Google Scholar]
- 383.Boe C, Wagner E, Rizzo M. Long-term outcomes of silicone metacarpophalangeal arthroplasty: a longitudinal analysis of 325 cases. J Hand Surg Eur. 2018;43:1076–1082. doi: 10.1177/1753193418778461. [DOI] [PubMed] [Google Scholar]
- 384.Lampropoulou-Adamidou K, Hartofilakidis G. Comparison of the long-term outcome of cemented Charnley low-friction arthroplasty with hybrid arthroplasty in patients with congenital hip disease. Bone Joint J. 2019;101-B:1050–1057. doi: 10.1302/0301-620X.101B9.BJJ-2018-1208.R1. [DOI] [PubMed] [Google Scholar]
- 385.Hernandez NM, Sierra RJ, Trousdale RT. Constrained liner revision is less effective with each subsequent constrained liner revision at preventing instability. J Arthroplasty. 2019;34:S282–S286. doi: 10.1016/j.arth.2019.01.061. [DOI] [PubMed] [Google Scholar]
- 386.Singleton N, Nicholas B, Gormack N, Stokes A. Differences in outcome after cruciate retaining and posterior stabilized total knee arthroplasty. J Orthop Surg. 2019;27:2309499019848154. doi: 10.1177/2309499019848154. [DOI] [PubMed] [Google Scholar]
- 387.Audigé L, Graf L, Flury M, et al. Functional improvement is sustained following anatomical and reverse shoulder arthroplasty for fracture sequelae: a registry-based analysis. Arch Orthop Trauma Surg. 2019;139:1561–1569. doi: 10.1007/s00402-019-03224-5. [DOI] [PubMed] [Google Scholar]
- 388.Raddaoui K, Khedhri W, Zoghlami K, et al. Perioperative morbidity in total knee arthroplasty. Pan Afr Med J. 2019;33:233. doi: 10.11604/pamj.2019.33.233.19095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Bass AR, Mehta B, Szymonifka J, et al. Racial disparities in total knee replacement failure as related to poverty. Arthritis Care Res. 2019;71:1488–1494. doi: 10.1002/acr.24028. [DOI] [PubMed] [Google Scholar]
- 390.Kang JR, Logli AL, Tagliero AJ, Sperling JW. The router bit extraction technique for removing a well-fixed humeral stem in revision shoulder arthroplasty. Bone Joint J. 2019;101-B:1280–1284. doi: 10.1302/0301-620X.101B10.BJJ-2018-1592.R1. [DOI] [PubMed] [Google Scholar]
- 391.Toft F, Moro F. Does ORIF of rare scapular spine fractures sustained after reverse shoulder arthroplasty benefit elderly patients? A case-series appraisal. Orthop Traumatol Surg Res. 2019;105:1521–1528. doi: 10.1016/j.otsr.2019.07.023. [DOI] [PubMed] [Google Scholar]
- 392.Shah RF, Bini S, Vail T. Data for registry and quality review can be retrospectively collected using natural language processing from unstructured charts of arthroplasty patients. Bone Joint J. 2020;102-B:99–104. doi: 10.1302/0301-620X.102B7.BJJ-2019-1574.R1. [DOI] [PubMed] [Google Scholar]
- 393.Florissi I, Galea VP, Sauder N, et al. Development and early findings of a semiautomated arthroplasty registry in a multi-institutional healthcare network. Bone Joint J. 2020;102-B:90–98. doi: 10.1302/0301-620X.102B7.BJJ-2019-1622.R1. [DOI] [PubMed] [Google Scholar]
- 394.Wegrzyn J, Malatray M, Pibarot V, et al. Is isolated mobile component exchange an option in the management of intraprosthetic dislocation of a dual mobility cup? Clin Orthop Relat Res. 2020;478:279–287. doi: 10.1097/CORR.0000000000001055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Ulivi M, Meroni V, Orlandini L, et al. Opportunities to improve feasibility, effectiveness and costs associated with a total joint replacements high-volume hospital registry. Comput Biol Med. 2020;121:103775. doi: 10.1016/j.compbiomed.2020.103775. [DOI] [PubMed] [Google Scholar]
- 396.Liebensteiner M, Köglberger P, Ruzicka A, et al. Unicondylar vs. total knee arthroplasty in medial osteoarthritis: a retrospective analysis of registry data and functional outcome. Arch Orthop Trauma Surg. 2020;140:545–549. doi: 10.1007/s00402-020-03377-8. [DOI] [PubMed] [Google Scholar]
- 397.Song JH, Kwon WH, Oh S-B, Moon KH. Use of a constrained acetabular liner to prevent and treat recurrent dislocation after total hip replacement arthroplasty. Orthop Surg. 2020;12:2004–2012. doi: 10.1111/os.12811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Gauci M-O, Cavalier M, Gonzalez J-F, et al. Revision of failed shoulder arthroplasty: epidemiology, etiology, and surgical options. J Shoulder Elbow Surg. 2020;29:541–549. doi: 10.1016/j.jse.2019.07.034. [DOI] [PubMed] [Google Scholar]
- 399.Gill SD, Hill-Buxton L-M, Gwini SM, et al. Simultaneous (two-surgeon) versus staged bilateral knee arthroplasty: an observational study of intraoperative and post-operative outcomes. ANZ J Surg. 2020;90:826–832. doi: 10.1111/ans.15766. [DOI] [PubMed] [Google Scholar]
- 400.Barrack TN, Abu-Amer W, Schwabe MT, et al. The burden and utility of routine follow-up at one year after primary arthroplasty. Bone Joint J. 2020;102-B:85–89. doi: 10.1302/0301-620X.102B7.BJJ-2019-1632.R1. [DOI] [PubMed] [Google Scholar]
- 401.LaHaise KM, Vargo DV, Barrazueta GA, et al. Range of motion at discharge predicts need for manipulation following total knee arthroplasty. J Knee Surg. 2021;34:187–191. doi: 10.1055/s-0039-1694024. [DOI] [PubMed] [Google Scholar]
- 402.Borton ZM, Prasad G, Konstantopoulos G, et al. Mid- to long-term survivorship of the cemented, semiconstrained discovery total elbow arthroplasty. J Shoulder Elbow Surg. 2021;30:1662–1669. doi: 10.1016/j.jse.2020.12.007. [DOI] [PubMed] [Google Scholar]
- 403.Zhang S, Lau BPH, Ng YH, et al. Machine learning algorithms do not outperform preoperative thresholds in predicting clinically meaningful improvements after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;30:2624–2630. doi: 10.1007/s00167-021-06642-4. [DOI] [PubMed] [Google Scholar]
- 404.Markel JF, Driscoll JA, Zheng TH, et al. Causes of early hip revision vary by age and gender: analysis of data from a statewide quality registry. J Arthroplasty. 2022;37:S616–S621. doi: 10.1016/j.arth.2022.03.014. [DOI] [PubMed] [Google Scholar]
- 405.Mathew JI, Nicholson AD, Finocchiaro A, et al. Outcomes of shoulder arthroplasty by year of index procedure: Are we getting better? J Shoulder Elbow Surg. 2022;31:245–251. doi: 10.1016/j.jse.2021.08.024. [DOI] [PubMed] [Google Scholar]
- 406.Tsiridis E, Kenanidis E, Potoupnis M, Sayegh FE. Direct superior approach with standard instrumentation for total hip arthroplasty: safety and efficacy in a prospective 200-case series. Hip Int. 2020;30:552–558. doi: 10.1177/1120700019843120. [DOI] [PubMed] [Google Scholar]
- 407.Sierra RJ, Cabanela ME. Conversion of failed hip hemiarthroplasties after femoral neck fractures. Clin Orthop Relat Res. 2002;66:129–139. doi: 10.1097/00003086-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 408.Lavernia C, D’apuzzo M, Hernandez VH, Lee DJ. Patient-perceived outcomes in thigh pain after primary arthroplasty of the hip. Clin Orthop Relat Res. 2005;441:268–273. doi: 10.1097/00003086-200512000-00041. [DOI] [PubMed] [Google Scholar]
- 409.Schneiderbauer MM, Sierra RJ, Schleck C, et al. Dislocation rate after hip hemiarthroplasty in patients with tumor-related conditions. J Bone Joint Surg Am. 2005;87:1810–1815. doi: 10.2106/JBJS.D.02830. [DOI] [PubMed] [Google Scholar]
- 410.Geiger F, Mau H, Krüger M, Thomsen M. Comparison of a new mobile-bearing total knee prosthesis with a fixed-bearing prosthesis: a matched pair analysis. Arch Orthop Trauma Surg. 2008;128:285–291. doi: 10.1007/s00402-007-0552-z. [DOI] [PubMed] [Google Scholar]
- 411.Gandhi R, Razak F, Tso P, et al. Greater perceived helplessness in osteoarthritis predicts outcome of joint replacement surgery. J Rheumatol. 2009;36:1507–1511. doi: 10.3899/jrheum.080466. [DOI] [PubMed] [Google Scholar]
- 412.Ghomrawi HMK, Dolan MM, Rutledge J, Alexiades MM. Recovery expectations of hip resurfacing compared to total hip arthroplasty: a matched pairs study. Arthritis Care Res. 2011;63:1753–1757. doi: 10.1002/acr.20626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Elson LC, Barr CJ, Chandran SE, et al. Are morbidly obese patients undergoing total hip arthroplasty at an increased risk for component malpositioning? J Arthroplasty. 2013;28:41–44. doi: 10.1016/j.arth.2013.05.035. [DOI] [PubMed] [Google Scholar]
- 414.Huang D-CT, Tatman P, Mehle S, Gioe TJ. Cumulative revision rate is higher in metal-on-metal THA than metal-on-polyethylene THA: analysis of survival in a community registry. Clin Orthop Relat Res. 2013;471:1920–1925. doi: 10.1007/s11999-013-2821-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Wiater BP, Boone CR, Koueiter DM, Wiater JM. Early outcomes of staged bilateral reverse total shoulder arthroplasty: a case-control study. Bone Joint J. 2013;95-B:1232–1238. doi: 10.1302/0301-620X.95B9.31445. [DOI] [PubMed] [Google Scholar]
- 416.Stryker LS, Abdel MP, Morrey ME, et al. Elevated postoperative blood glucose and preoperative hemoglobin A1C are associated with increased wound complications following total joint arthroplasty. J Bone Joint Surg Am. 2013;95(808–14):S1–2. doi: 10.2106/JBJS.L.00494. [DOI] [PubMed] [Google Scholar]
- 417.Boyle MJ, Singleton N, Frampton CMA, Muir D. Functional response to total hip arthroplasty in patients with hip dysplasia. ANZ J Surg. 2013;83:554–558. doi: 10.1111/j.1445-2197.2012.06198.x. [DOI] [PubMed] [Google Scholar]
- 418.Berend KR, Lombardi AVJ, Morris MJ, et al. Two-stage treatment of hip periprosthetic joint infection is associated with a high rate of infection control but high mortality. Clin Orthop Relat Res. 2013;471:510–518. doi: 10.1007/s11999-012-2595-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Pappou I, Virani NA, Clark R, et al. Outcomes and costs of reverse shoulder arthroplasty in the morbidly obese: a case control study. J Bone Joint Surg Am. 2014;96:1169–1176. doi: 10.2106/JBJS.M.00735. [DOI] [PubMed] [Google Scholar]
- 420.Goodman SM, Zhu R, Figgie MP, et al. Short-term total hip replacement outcomes in ankylosing spondylitis. J Clin Rheumatol. 2014;20:363–368. doi: 10.1097/RHU.0000000000000138. [DOI] [PubMed] [Google Scholar]
- 421.Adelani MA, Crook K, Barrack RL, et al. What is the prognosis of revision total hip arthroplasty in patients 55 years and younger? Clin Orthop Relat Res. 2014;472:1518–1525. doi: 10.1007/s11999-013-3377-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Chang C-H, Chang Y, Chen DW, et al. Topical tranexamic acid reduces blood loss and transfusion rates associated with primary total hip arthroplasty. Clin Orthop Relat Res. 2014;472:1552–1557. doi: 10.1007/s11999-013-3446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Krismer M, Nogler M, Huber D, Oberaigner W. Cemented ABG-II prosthesis: 5-year results. Hip Int. 2015;25:56–60. doi: 10.5301/hipint.5000185. [DOI] [PubMed] [Google Scholar]
- 424.Morris BJ, Haigler RE, O’Connor DP, et al. Outcomes of staged bilateral reverse shoulder arthroplasties for rotator cuff tear arthropathy. J Shoulder Elbow Surg. 2015;24:474–481. doi: 10.1016/j.jse.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 425.Shah UH, Mandl LA, Mertelsmann-Voss C, et al. Systemic lupus erythematosus is not a risk factor for poor outcomes after total hip and total knee arthroplasty. Lupus. 2015;24:900–908. doi: 10.1177/0961203314566635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Lavernia CJ, Villa JM, Iacobelli DA. What is the role of mental health in primary total knee arthroplasty? Clin Orthop Relat Res. 2015;473:159–163. doi: 10.1007/s11999-014-3769-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.LoVerde ZJ, Mandl LA, Johnson BK, et al. Rheumatoid arthritis does not increase risk of short-term adverse events after total knee arthroplasty: a retrospective case-control study. J Rheumatol. 2015;42:1123–1130. doi: 10.3899/jrheum.141251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Langen S, Gaber S, Zdravkovic V, et al. Lateral subvastus approach with tibial tubercle osteotomy for primary total knee arthroplasty: clinical outcome and complications compared to medial parapatellar approach. Eur J Orthop Surg Traumatol. 2016;26:215–222. doi: 10.1007/s00590-015-1718-y. [DOI] [PubMed] [Google Scholar]
- 429.Mandl LA, Zhu R, Huang W-T, et al. Short-term total hip arthroplasty outcomes in patients with psoriatic arthritis or psoriatic skin disease compared to patients with osteoarthritis. Arthritis Rheumatol. 2016;68:410–417. doi: 10.1002/art.39431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Fein AW, Figgie CA, Dodds TR, et al. Systemic lupus erythematosus does not increase risk of adverse events in the first 6 months after total knee arthroplasty. J Clin Rheumatol. 2016;22:355–359. doi: 10.1097/RHU.0000000000000435. [DOI] [PubMed] [Google Scholar]
- 431.Rowan FE, Gorenchtein M, Aslam S, et al. A comparison of acetabular impaction grafting and trabecular metal for revision arthroplasty. Hip Int. 2016;26:350–354. doi: 10.5301/hipint.5000362. [DOI] [PubMed] [Google Scholar]
- 432.Roberts JE, Mandl LA, Su EP, et al. Patients with systemic lupus erythematosus have increased risk of short-term adverse events after total hip arthroplasty. J Rheumatol. 2016;43:1498–1502. doi: 10.3899/jrheum.151373. [DOI] [PubMed] [Google Scholar]
- 433.Morison Z, Moojen DJF, Nauth A, et al. Total hip arthroplasty after acetabular fracture is associated with lower survivorship and more complications. Clin Orthop Relat Res. 2016;474:392–398. doi: 10.1007/s11999-015-4509-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Lim JBT, Bin Abd Razak HR, Zainul-Abidin S, et al. What are the preoperative outcome measures that predispose to periprosthetic fractures after primary total knee arthroplasty? J Arthroplasty. 2017;32:2531–2534. doi: 10.1016/j.arth.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 435.Redmond JM, Gupta A, Dunne K, et al. What factors predict conversion to THA after arthroscopy? Clin Orthop Relat Res. 2017;475:2538–2545. doi: 10.1007/s11999-017-5437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Tay KS, Cher EWL, Zhang K, et al. Comorbidities have a greater impact than age alone in the outcomes of octogenarian total knee arthroplasty. J Arthroplasty. 2017;32:3373–3378. doi: 10.1016/j.arth.2017.05.041. [DOI] [PubMed] [Google Scholar]
- 437.Charpentier PM, Srivastava AK, Zheng H, et al. Readmission rates for one versus two-midnight length of stay for primary total knee arthroplasty: analysis of the Michigan Arthroplasty Registry Collaborative Quality Initiative (MARCQI) Database. J Bone Joint Surg Am. 2018;100:1757–1764. doi: 10.2106/JBJS.18.00166. [DOI] [PubMed] [Google Scholar]
- 438.Song SY, Goodman SB, Suh G, et al. Surgery before subspecialty referral for periprosthetic knee infection reduces the likelihood of infection control. Clin Orthop Relat Res. 2018;476:1995–2002. doi: 10.1097/CORR.0000000000000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Behrend H, Zdravkovic V, Bösch M, Hochreiter B. No difference in joint awareness after TKA: a matched-pair analysis of a classic implant and its evolutional design. Knee Surg Sports Traumatol Arthrosc. 2019;27:2124–2129. doi: 10.1007/s00167-019-05407-4. [DOI] [PubMed] [Google Scholar]
- 440.Lim JBT, Pang HN, Tay KJD, et al. Clinical outcomes and patient satisfaction following revision of failed unicompartmental knee arthroplasty to total knee arthroplasty are as good as a primary total knee arthroplasty. Knee. 2019;26:847–852. doi: 10.1016/j.knee.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 441.Jochimsen KN, Jacobs CA, Duncan ST. Femoroacetabular impingement is more common in military veterans with end-stage hip osteoarthritis than civilian patients: a retrospective case control study. Mil Med Res. 2019;6:27. doi: 10.1186/s40779-019-0218-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Benelli G, Maritato M, Cerulli Mariani P, Sasso F. Revision of ASR hip arthroplasty: analysis of two hundred and ninety six recalled patients at seven years. Int Orthop. 2019;43:97–101. doi: 10.1007/s00264-018-4128-z. [DOI] [PubMed] [Google Scholar]
- 443.Lim JBT, Pang HN, Tay KJD, et al. Increased constraint of rotating hinge knee prosthesis is associated with poorer clinical outcomes as compared to constrained condylar knee prosthesis in total knee arthroplasty. Eur J Orthop Surg Traumatol. 2020;30:529–535. doi: 10.1007/s00590-019-02598-x. [DOI] [PubMed] [Google Scholar]
- 444.Nyffeler RW, Altioklar B, Bissig P. Causes of acromion and scapular spine fractures following reverse shoulder arthroplasty: a retrospective analysis and literature review. Int Orthop. 2020;44:2673–2681. doi: 10.1007/s00264-020-04813-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Lall AC, Secretov E, Battaglia MR, et al. Effect of alcohol consumption on patient-reported outcomes in hip arthroscopy: a matched controlled study with minimum 2-year follow-up. Hip Int. 2020;30:457–468. doi: 10.1177/1120700019853554. [DOI] [PubMed] [Google Scholar]
- 446.White BJ, Patterson J, Scoles AM, et al. Hip arthroscopy in patients aged 40 years and older: greater success with labral reconstruction compared with labral repair. Arthroscopy. 2020;36:2137–2144. doi: 10.1016/j.arthro.2020.04.031. [DOI] [PubMed] [Google Scholar]
- 447.Jacob I, Benson J, Shanaghan K, Gonzalez Della Valle A. Acetabular positioning is more consistent with the use of a novel miniature computer-assisted device. Int Orthop. 2020;44:429–435. doi: 10.1007/s00264-020-04484-2. [DOI] [PubMed] [Google Scholar]
- 448.Schafer KA, Clohisy JC, Nepple JJ. Rapidly progressive arthritis in femoroacetabular impingement: patient characteristics and risk factors for total hip arthroplasty by the age of forty. Iowa Orthop J. 2020;40:129–134. [PMC free article] [PubMed] [Google Scholar]
- 449.Dugdale EM, Siljander MP, Trousdale RT. Factors associated with early return to driving following total joint arthroplasty. J Arthroplasty. 2021;36:3392–3400. doi: 10.1016/j.arth.2021.05.028. [DOI] [PubMed] [Google Scholar]
- 450.Rainer WG, Abdel MP, Freedman BA, et al. Pelvic tilt and the pubic symphysis to sacrococcygeal junction distance: risk factors for hip dislocation observed on anteroposterior pelvis radiographs. J Arthroplasty. 2021;36:S367–S373. doi: 10.1016/j.arth.2021.02.079. [DOI] [PubMed] [Google Scholar]
- 451.Loppini M, Pisano A, Gandolfi CE, et al. Complications, readmission and reoperation rates in one-stage bilateral versus unilateral total hip arthroplasty: a high-volume single center case-control study. Sci Rep. 2021;11:6299. doi: 10.1038/s41598-021-85839-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Damsgaard CW, Gad BV, Bono OJ, et al. Intraoperative proximal tibia periprosthetic fractures in primary total knee arthroplasty. J Knee Surg. 2021;34:1269–1274. doi: 10.1055/s-0040-1708037. [DOI] [PubMed] [Google Scholar]
- 453.Kriechling P, Hodel S, Paszicsnyek A, et al. Incidence, radiographic predictors, and clinical outcome of acromial stress reaction and acromial fractures in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2022;31:1143–1153. doi: 10.1016/j.jse.2021.11.012. [DOI] [PubMed] [Google Scholar]
- 454.Forlizzi JM, Puzzitiello RN, Hart P-A, et al. Predictors of poor and excellent outcomes after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2022;31:294–301. doi: 10.1016/j.jse.2021.07.009. [DOI] [PubMed] [Google Scholar]
- 455.Kenanidis E, Paparoidamis G, Pegios VF, et al. Earlier functional recovery and discharge from hospital for THA patients operated on via direct superior compared to standard posterior approach: a retrospective frequency-matched case-control study. Hip Int. 2022 doi: 10.1177/11207000221086506. [DOI] [PubMed] [Google Scholar]
- 456.Gandhi R, Wasserstein D, Razak F, et al. BMI independently predicts younger age at hip and knee replacement. Obesity. 2010;18:2362–2366. doi: 10.1038/oby.2010.72. [DOI] [PubMed] [Google Scholar]
- 457.Philippon MJ, Briggs KK, Carlisle JC, Patterson DC. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res. 2013;471:2492–2496. doi: 10.1007/s11999-012-2779-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Lübbeke A, Zimmermann-Sloutskis D, Stern R, et al. Physical activity before and after primary total hip arthroplasty: a registry-based study. Arthritis Care Res. 2014;66:277–284. doi: 10.1002/acr.22101. [DOI] [PubMed] [Google Scholar]
- 459.Heffler MA, Barlow R, Xi Y, et al. Multi-parametric muscle and fat correlation of computed tomography parameters to outcomes in a total hip arthroplasty population. BMC Musculoskelet Disord. 2018;19:4. doi: 10.1186/s12891-017-1926-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Klem N-R, Smith A, O’Sullivan P, et al. What influences patient satisfaction after TKA? A qualitative investigation. Clin Orthop Relat Res. 2020;478:1850–1866. doi: 10.1097/CORR.0000000000001284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Baryeh K, Maillot C, Gummaraju A, Rivière C. Disappointing relationship between functional performance and patient satisfaction of UKA patients: a cross sectional study. Orthop Traumatol Surg Res. 2021;107:102865. doi: 10.1016/j.otsr.2021.102865. [DOI] [PubMed] [Google Scholar]
- 462.Gummaraju A, Maillot C, Baryeh K, et al. Oxford Knee Score and EQ-5d poorly predict patient’s satisfaction following mechanically aligned total knee replacement: a cross-sectional study. Orthop Traumatol Surg Res. 2021;107:102867. doi: 10.1016/j.otsr.2021.102867. [DOI] [PubMed] [Google Scholar]
- 463.Maillot C, Harman C, Al-Zibari M, et al. Moderate relationship between function and satisfaction of total hip arthroplasty patients: a cross sectional study. Hip Int. 2022;32:25–31. doi: 10.1177/1120700020921110. [DOI] [PubMed] [Google Scholar]
- 464.Moverman MA, Puzzitiello RN, Menendez ME, et al. Rotator cuff fatty infiltration and muscle atrophy: relation to glenoid deformity in primary glenohumeral osteoarthritis. J Shoulder Elbow Surg. 2022;31:286–293. doi: 10.1016/j.jse.2021.07.007. [DOI] [PubMed] [Google Scholar]
- 465.Dowsey MM, Scott A, Nelson EA, et al. Using discrete choice experiments as a decision aid in total knee arthroplasty: study protocol for a randomised controlled trial. Trials. 2016;17:416. doi: 10.1186/s13063-016-1536-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 466.Page RS, Williams S, Selvaratnam A, et al. Protocol for a single-centre, parallel-arm, double-blind randomised trial evaluating the effects of tourniquet use in total knee arthroplasty on intra-operative and post-operative outcomes. BMC Musculoskelet Disord. 2018;19:435. doi: 10.1186/s12891-018-2352-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Abdullah HR, Tan SR, Lee SJ et al (2018) Protocol for a single-centre prospective observational study of postoperative delirium following total joint arthroplasties among South East Asians. BMJ Open 8:e019426. 10.1136/bmjopen-2017-019426 [DOI] [PMC free article] [PubMed]
- 468.Grassi A, Golinelli D, Tedesco D, et al. Patient-reported outcome measures (PROMs) after elective hip, knee and shoulder arthroplasty: protocol for a prospective cohort study. BMC Musculoskelet Disord. 2019;20:374. doi: 10.1186/s12891-019-2745-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Arias-de la Torre J, Domingo L, Martínez O, et al. Evaluation of the effectiveness of hip and knee implant models used in Catalonia: a protocol for a prospective registry-based study. J Orthop Surg Res. 2019;14:61. doi: 10.1186/s13018-019-1087-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Gould D, Dowsey M, Spelman T, et al. Patient-related risk factors for unplanned 30-day readmission following total knee arthroplasty: a protocol for a systematic review and meta-analysis. Syst Rev. 2019;8:215. doi: 10.1186/s13643-019-1140-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Lo CWT, Brodie MA, Tsang WWN, et al. Acceptability and feasibility of a community-based strength, balance, and Tai Chi rehabilitation program in improving physical function and balance of patients after total knee arthroplasty: study protocol for a pilot randomized controlled trial. Trials. 2021;22:129. doi: 10.1186/s13063-021-05055-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Zhou Y, Weeden C, Patten L, et al. Evaluating willingness for surgery using the SMART Choice (Knee) patient prognostic tool for total knee arthroplasty: study protocol for a pragmatic randomised controlled trial. BMC Musculoskelet Disord. 2022;23:179. doi: 10.1186/s12891-022-05123-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.Gausden EB, Garner MR, Warner SJ, et al. Tranexamic acid in hip fracture patients: a protocol for a randomised, placebo controlled trial on the efficacy of tranexamic acid in reducing blood loss in hip fracture patients. BMJ Open. 2016;6:e010676. doi: 10.1136/bmjopen-2015-010676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Turan A, Babazade R, Elsharkawy H, et al. Novel needle guide reduces time to perform ultrasound-guided femoral nerve catheter placement: a randomised controlled trial. Eur J Anaesthesiol. 2017;34:135–140. doi: 10.1097/EJA.0000000000000584. [DOI] [PubMed] [Google Scholar]
- 475.Lin S-J, Chang F-C, Huang T-W, et al. Temporal change of interleukin-6, C-reactive protein, and skin temperature after total knee arthroplasty using triclosan-coated sutures. Biomed Res Int. 2018;2018:9136208. doi: 10.1155/2018/9136208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Alleva R, Tognù A, Tomasetti M, et al. Effect of different anaesthetic techniques on gene expression profiles in patients who underwent hip arthroplasty. PLoS ONE. 2019;14:e0219113. doi: 10.1371/journal.pone.0219113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Turgeon TR, Cameron B, Burnell CD, et al. A double-blind randomized controlled trial of total knee replacement using patient-specific cutting block instrumentation versus standard instrumentation. Can J Surg. 2019;62:460–467. doi: 10.1503/cjs.018318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Dowsey MM, Brown WA, Cochrane A, et al. Effect of bariatric surgery on risk of complications after total knee arthroplasty: a randomized clinical trial. JAMA Netw Open. 2022;5:e226722. doi: 10.1001/jamanetworkopen.2022.6722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 479.James EW, Blevins JL, Gausden EB, et al. Increased utilization of constraint in total knee arthroplasty following anterior cruciate ligament and multiligament knee reconstruction. Bone Joint J. 2019;101-B:77–83. doi: 10.1302/0301-620X.101B7.BJJ-2018-1492.R1. [DOI] [PubMed] [Google Scholar]
- 480.Hart A, Wyles CC, Abdel MP, et al. Thirty-day major and minor complications following total hip arthroplasty—a comparison of the direct anterior, lateral, and posterior approaches. J Arthroplasty. 2019;34:2681–2685. doi: 10.1016/j.arth.2019.06.046. [DOI] [PubMed] [Google Scholar]
- 481.Rojanasopondist P, Galea VP, Connelly JW, et al. What preoperative factors are associated with not achieving a minimum clinically important difference after THA? Findings from an international multicenter study. Clin Orthop Relat Res. 2019;477:1301–1312. doi: 10.1097/CORR.0000000000000667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 482.Mazzotti A, Perna F, Golinelli D, et al. Preoperative valgus deformity has twice the risk of failure as compared to varus deformity after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27:3041–3047. doi: 10.1007/s00167-018-5331-6. [DOI] [PubMed] [Google Scholar]
- 483.Pitta M, Khoshbin A, Lalani A, et al. Age-related functional decline following total knee arthroplasty: risk adjustment is mandatory. J Arthroplasty. 2019;34:228–234. doi: 10.1016/j.arth.2018.09.046. [DOI] [PubMed] [Google Scholar]
- 484.Fontana MA, Lyman S, Sarker GK, et al. Can machine learning algorithms predict which patients will achieve minimally clinically important differences from total joint arthroplasty? Clin Orthop Relat Res. 2019;477:1267–1279. doi: 10.1097/CORR.0000000000000787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 485.Kahlenberg CA, Lyman S, Joseph AD, et al. Comparison of patient-reported outcomes based on implant brand in total knee arthroplasty: a prospective cohort study. Bone Joint J. 2019;101-B:48–54. doi: 10.1302/0301-620X.101B7.BJJ-2018-1382.R1. [DOI] [PubMed] [Google Scholar]
- 486.Abdel MP, Miller LE, Hanssen AD, Pagnano MW. Cost analysis of dual-mobility versus large femoral head constructs in revision total hip arthroplasty. J Arthroplasty. 2019;34:260–264. doi: 10.1016/j.arth.2018.09.085. [DOI] [PubMed] [Google Scholar]
- 487.Yadegari I, Bohm E, Ayilara OF, et al. Differential item functioning of the SF-12 in a population-based regional joint replacement registry. Health Qual Life Outcomes. 2019;17:114. doi: 10.1186/s12955-019-1166-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 488.Stambough JB, Curtin BM, Odum SM, et al. Does change in ESR and CRP guide the timing of two-stage arthroplasty reimplantation? Clin Orthop Relat Res. 2019;477:364–371. doi: 10.1097/01.blo.0000533618.31937.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Kim S-C, Lim Y-W, Jo W-L, et al. Fourth-generation ceramic-on-ceramic THA results in improvements in midterm outcomes compared to third-generation THA but does not resolve noise problems: a cohort study of a single-hip system. BMC Musculoskelet Disord. 2019;20:263. doi: 10.1186/s12891-019-2641-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 490.Lombardo DJ, Siljander MP, Gehrke CK, et al. Fretting and corrosion damage of retrieved dual-mobility total hip arthroplasty systems. J Arthroplasty. 2019;34:1273–1278. doi: 10.1016/j.arth.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 491.Castagnini F, Bordini B, Stea S, et al. Highly porous titanium cup in cementless total hip arthroplasty: registry results at eight years. Int Orthop. 2019;43:1815–1821. doi: 10.1007/s00264-018-4102-9. [DOI] [PubMed] [Google Scholar]
- 492.Ayilara OF, Zhang L, Sajobi TT, et al. Impact of missing data on bias and precision when estimating change in patient-reported outcomes from a clinical registry. Health Qual Life Outcomes. 2019;17:106. doi: 10.1186/s12955-019-1181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493.Gungor S, Fields K, Aiyer R, et al. Incidence and risk factors for development of persistent postsurgical pain following total knee arthroplasty: a retrospective cohort study. Medicine. 2019;98:e16450. doi: 10.1097/MD.0000000000016450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 494.Mehta B, Szymonifka J, Dey S, et al. Living in immigrant communities does not impact total knee arthroplasty outcomes: experience from a high-volume center in the United States. BMC Musculoskelet Disord. 2019;20:67. doi: 10.1186/s12891-019-2446-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 495.Hart A, Janz V, Trousdale RT, et al. Long-term survivorship of total hip arthroplasty with highly cross-linked polyethylene for osteonecrosis. J Bone Joint Surg Am. 2019;101:1563–1568. doi: 10.2106/JBJS.18.01218. [DOI] [PubMed] [Google Scholar]
- 496.Marks M, Hensler S, Wehrli M, et al. Minimal important change and patient acceptable symptom state for patients after proximal interphalangeal joint arthroplasty. J Hand Surg Eur. 2019;44:175–180. doi: 10.1177/1753193418799568. [DOI] [PubMed] [Google Scholar]
- 497.Statz JM, Duethman NC, Trousdale RT, Taunton MJ. Outcome of direct anterior total hip arthroplasty complicated by superficial wound dehiscence requiring irrigation and debridement. J Arthroplasty. 2019;34:1492–1497. doi: 10.1016/j.arth.2019.03.020. [DOI] [PubMed] [Google Scholar]
- 498.Crawford DA, Adams JB, Morris MJ, et al. Partial 2-stage exchange for infected total hip arthroplasty: an updated report. J Arthroplasty. 2019;34:3048–3053. doi: 10.1016/j.arth.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 499.Khoshbin A, Stavrakis A, Sharma A, et al. Patient-reported outcome measures of total knee arthroplasties for post-traumatic arthritis versus osteoarthritis: a short-term (5- to 10-year) retrospective matched cohort study. J Arthroplasty. 2019;34:872–876.e1. doi: 10.1016/j.arth.2019.01.022. [DOI] [PubMed] [Google Scholar]
- 500.Hart A, Hernandez NM, Abdel MP, et al. Povidone-iodine wound lavage to prevent infection after revision total hip and knee arthroplasty: an analysis of 2,884 cases. J Bone Joint Surg Am. 2019;101:1151–1159. doi: 10.2106/JBJS.18.01152. [DOI] [PubMed] [Google Scholar]
- 501.Fu MC, Chang B, Wong AC, et al. PROMIS physical function underperforms psychometrically relative to American Shoulder and Elbow Surgeons score in patients undergoing anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:1809–1815. doi: 10.1016/j.jse.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 502.Affatato S, Cosentino M, Castagnini F, Bordini B. Registry study on failure incidence in 1,127 revised hip implants with stem trunnion re-use after 10 years of follow-up: limited influence of an adapter sleeve. Acta Orthop. 2019;90:417–420. doi: 10.1080/17453674.2019.1618649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 503.Crawford DA, Adams JB, Morris MJ, et al. Revision of failed metal-on-metal total hip arthroplasty: midterm outcomes of 203 consecutive cases. J Arthroplasty. 2019;34:1755–1760. doi: 10.1016/j.arth.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 504.Jennings JM, White S, Martin JR, et al. Revisions of modular metal-on-metal THA have a high risk of early complications. Clin Orthop Relat Res. 2019;477:344–350. doi: 10.1097/CORR.0000000000000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 505.Crawford DA, Adams JB, Hurst JM, et al. Ten-year minimum outcomes and survivorship with a high flexion knee system. J Arthroplasty. 2019;34:1975–1979. doi: 10.1016/j.arth.2019.04.039. [DOI] [PubMed] [Google Scholar]
- 506.Busanelli L, Castagnini F, Bordini B, et al. The biological acetabular reconstruction with bone allografts in hip revision arthroplasty. Musculoskelet Surg. 2019;103:173–179. doi: 10.1007/s12306-018-0573-5. [DOI] [PubMed] [Google Scholar]
- 507.Goldman AH, Sierra RJ, Trousdale RT, et al. The Lawrence D. Dorr Surgical Techniques & Technologies Award: Why are contemporary revision total hip arthroplasties failing? An analysis of 2500 cases. J Arthroplasty. 2019;34:S11–S16. doi: 10.1016/j.arth.2019.01.031. [DOI] [PubMed] [Google Scholar]
- 508.Boyer B, Bordini B, Caputo D, et al. Unilateral versus bilateral total knee arthroplasty: a registry study on survival and risk factors. Orthop Traumatol Surg Res. 2019;105:627–631. doi: 10.1016/j.otsr.2019.01.023. [DOI] [PubMed] [Google Scholar]
- 509.Hernandez NM, Hart A, Taunton MJ, et al. Use of Povidone-Iodine Irrigation Prior to wound closure in primary total hip and knee arthroplasty: an analysis of 11,738 cases. J Bone Joint Surg Am. 2019;101:1144–1150. doi: 10.2106/JBJS.18.01285. [DOI] [PubMed] [Google Scholar]
- 510.Ledford CK, Perry KI, Hanssen AD, Abdel MP. What are the contemporary etiologies for revision surgery and revision after primary, noncemented total hip arthroplasty? J Am Acad Orthop Surg. 2019;27:933–938. doi: 10.5435/JAAOS-D-17-00842. [DOI] [PubMed] [Google Scholar]
- 511.Brown TS, McLaughlin RJ, Berry DJ, et al. What is the survivorship of revision surgery performed for the chronically dislocated THA? Clin Orthop Relat Res. 2019;477:374–379. doi: 10.1097/CORR.0000000000000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 512.Lalani A, Lee Y-Y, Pitta M, et al. Age-related decline in patient-reported outcomes 2 and 5 years following total hip arthroplasty. J Arthroplasty. 2019;34:1999–2005. doi: 10.1016/j.arth.2019.02.023. [DOI] [PubMed] [Google Scholar]
- 513.Lee WC, Bin Abd Razak HR, Allen JC, et al. Achieving Minimum Clinically Important Difference in Oxford Knee Score and Short Form-36 physical component summary is less likely with single-radius compared with multiradius total knee arthroplasty in Asians. J Knee Surg. 2019;32:227–232. doi: 10.1055/s-0038-1641139. [DOI] [PubMed] [Google Scholar]
- 514.Lampart M, Behrend H, Moser LB, Hirschmann MT. Due to great variability fixed HKS angle for alignment of the distal cut leads to a significant error in coronal TKA orientation. Knee Surg Sports Traumatol Arthrosc. 2019;27:1434–1441. doi: 10.1007/s00167-018-5041-0. [DOI] [PubMed] [Google Scholar]
- 515.Abdel MP, Petis SM, Taunton MJ, et al. Long-term results of patellar bone-grafting for severe patellar bone loss during revision total knee arthroplasty. J Bone Joint Surg Am. 2019;101:1636–1644. doi: 10.2106/JBJS.19.00519. [DOI] [PubMed] [Google Scholar]
- 516.Menendez ME, Shaker J, Lawler SM, et al. Negative patient-experience comments after total shoulder arthroplasty. J Bone Joint Surg Am. 2019;101:330–337. doi: 10.2106/JBJS.18.00695. [DOI] [PubMed] [Google Scholar]
- 517.Burger JA, Kleeblad LJ, Laas N, Pearle AD. The influence of preoperative radiographic patellofemoral degenerative changes and malalignment on patellofemoral-specific outcome scores following fixed-bearing medial unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2019;101:1662–1669. doi: 10.2106/JBJS.18.01385. [DOI] [PubMed] [Google Scholar]
- 518.Hernandez NM, Petis SM, Hanssen AD, et al. Infection after unicompartmental knee arthroplasty: a high risk of subsequent complications. Clin Orthop Relat Res. 2019;477:70–77. doi: 10.1097/CORR.0000000000000372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Chalmers BP, Limberg AK, Athey AG, et al. Total knee arthroplasty after distal femoral osteotomy long-term survivorship and clinical outcomes. Bone Joint J. 2019;101-B:660–666. doi: 10.1302/0301-620X.101B6.BJJ-2018-1334.R2. [DOI] [PubMed] [Google Scholar]
- 520.Hood BR, Cowen ME, Zheng HT, et al. Association of aspirin with prevention of venous thromboembolism in patients after total knee arthroplasty compared with other anticoagulants: a noninferiority analysis. JAMA Surg. 2019;154:65–72. doi: 10.1001/jamasurg.2018.3858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 521.Blevins JL, Chiu Y-F, Lyman S, et al. Comparison of expectations and outcomes in rheumatoid arthritis versus osteoarthritis patients undergoing total knee arthroplasty. J Arthroplasty. 2019;34:1946–1952.e2. doi: 10.1016/j.arth.2019.04.034. [DOI] [PubMed] [Google Scholar]
- 522.Kim E, Talmo CT, Anderson MC, et al. Incidence and risk factors for posterior cruciate ligament avulsion during cruciate retaining total knee arthroplasty. J Knee Surg. 2019;32:1138–1142. doi: 10.1055/s-0038-1676068. [DOI] [PubMed] [Google Scholar]
- 523.Carducci MP, Zimmer ZR, Jawa A. Predictors of unsatisfactory patient outcomes in primary reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:2113–2120. doi: 10.1016/j.jse.2019.04.009. [DOI] [PubMed] [Google Scholar]
- 524.Chalmers BP, Limberg AK, Tibbo ME, et al. Total knee arthroplasty after high tibial osteotomy results in excellent long-term survivorship and clinical outcomes. J Bone Joint Surg Am. 2019;101:970–978. doi: 10.2106/JBJS.18.01060. [DOI] [PubMed] [Google Scholar]
- 525.Bunzli S, O’Brien P, Klem N, et al. Misconceived expectations: Patient reflections on the total knee replacement journey. Musculoskelet Care. 2020;18:415–424. doi: 10.1002/msc.1475. [DOI] [PubMed] [Google Scholar]
- 526.Sheth MM, Morris BJ, Laughlin MS, et al. Outcomes of anatomic shoulder arthroplasty performed on B2 vs. A1 type glenoids. J Shoulder Elbow Surg. 2020;29:2571–2577. doi: 10.1016/j.jse.2020.03.050. [DOI] [PubMed] [Google Scholar]
- 527.Castagnini F, Bordini B, Biondi F, et al. Mixed ceramic combinations in primary total hip arthroplasty achieved reassuring mid-to-longterm outcomes. J Mater Sci Mater Med. 2020;31:56. doi: 10.1007/s10856-020-06393-7. [DOI] [PubMed] [Google Scholar]
- 528.Giesinger JM, Giesinger K, Federico B, et al. Differences in case mix and outcomes between Swiss and Scottish total knee arthroplasty patients. Knee Surg Sports Traumatol Arthrosc. 2020;28:1797–1804. doi: 10.1007/s00167-019-05597-x. [DOI] [PubMed] [Google Scholar]
- 529.Goldman AH, Osmon DR, Hanssen AD, et al. Aseptic reoperations within 1 year of primary total knee arthroplasty markedly increase the risk of later periprosthetic joint infection. J Arthroplasty. 2020;35:3668–3672. doi: 10.1016/j.arth.2020.06.054. [DOI] [PubMed] [Google Scholar]
- 530.Goodman SM, Mehta BY, Kahlenberg CA, et al. Assessment of a satisfaction measure for use after primary total joint arthroplasty. J Arthroplasty. 2020;35:1792–1799.e4. doi: 10.1016/j.arth.2020.02.039. [DOI] [PubMed] [Google Scholar]
- 531.Sachdeva S, Baker JF, Bauwens JE, et al. Can revision TKA patients achieve similar clinical functional improvement compared to primaries? J Knee Surg. 2020;33:1219–1224. doi: 10.1055/s-0039-1693415. [DOI] [PubMed] [Google Scholar]
- 532.Owen AR, Markos JR, Mabry TM, et al. Contemporary primary total knee arthroplasty is durable in patients diagnosed with ankylosing spondylitis. J Arthroplasty. 2020;35:3161–3165. doi: 10.1016/j.arth.2020.06.033. [DOI] [PubMed] [Google Scholar]
- 533.Polascik BA, Hidaka C, Thompson MC, et al. Crosswalks between knee and hip arthroplasty short forms: HOOS/KOOS JR and Oxford. J Bone Joint Surg Am. 2020;102:983–990. doi: 10.2106/JBJS.19.00916. [DOI] [PubMed] [Google Scholar]
- 534.Abdulla I, Mahdavi S, Khong H, et al. Does body mass index affect the rate of adverse outcomes in total hip and knee arthroplasty? A retrospective review of a total joint replacement database. Can J Surg. 2020;63:E142–E149. doi: 10.1503/cjs.006719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 535.Bigart KC, Nahhas CR, Ruzich GP, et al. Does femoral morphology predict the risk of periprosthetic fracture after cementless total hip arthroplasty? J Arthroplasty. 2020;35:S359–S363. doi: 10.1016/j.arth.2020.02.048. [DOI] [PubMed] [Google Scholar]
- 536.Tew M, Dalziel K, Dowsey M, et al. Exploring the impact of quality of life on survival: a case study in total knee replacement surgery. Med Decis Mak. 2020;40:302–313. doi: 10.1177/0272989X20913266. [DOI] [PubMed] [Google Scholar]
- 537.Johnson NR, Trofa DP, Saltzman BM, et al. Healing rate and clinical outcomes of lesser tuberosity osteotomy for anatomic shoulder arthroplasty. J Am Acad Orthop Surg Glob Res Rev. 2020 doi: 10.5435/JAAOSGlobal-D-19-00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 538.Pua Y-H, Kang H, Thumboo J, et al. Machine learning methods are comparable to logistic regression techniques in predicting severe walking limitation following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020;28:3207–3216. doi: 10.1007/s00167-019-05822-7. [DOI] [PubMed] [Google Scholar]
- 539.Li J, Ji Q, Ni M, et al. Management of intraoperative acetabular fracture in primary total hip arthroplasty. BMC Musculoskelet Disord. 2020;21:383. doi: 10.1186/s12891-020-03356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 540.Maniscalco P, Quattrini F, Ciatti C, et al. Neck modularity in total hip arthroplasty: a retrospective study of nine hundred twenty-eight titanium neck implants with a maximum follow-up of eighteen years. Int Orthop. 2020;44:2261–2266. doi: 10.1007/s00264-020-04686-8. [DOI] [PubMed] [Google Scholar]
- 541.Blevins JL, Rao V, Chiu Y-F, et al. Predicting implant size in total knee arthroplasty using demographic variables. Bone Joint J. 2020;102-B:85–90. doi: 10.1302/0301-620X.102B6.BJJ-2019-1620.R1. [DOI] [PubMed] [Google Scholar]
- 542.Ghomrawi HMK, Lee LY-Y, Nwachukwu BU, et al. Preoperative expectations associated with postoperative dissatisfaction after total knee arthroplasty: a cohort study. J Am Acad Orthop Surg. 2020;28:e145–e150. doi: 10.5435/JAAOS-D-18-00785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 543.Pallante GD, Statz JM, Milbrandt TA, Trousdale RT. Primary total hip arthroplasty in patients 20 years old and younger. J Bone Joint Surg Am. 2020;102:519–525. doi: 10.2106/JBJS.19.00699. [DOI] [PubMed] [Google Scholar]
- 544.Buller LT, Rao V, Chiu Y-F, et al. Primary total knee arthroplasty performed using high-viscosity cement is associated with higher odds of revision for aseptic loosening. J Arthroplasty. 2020;35:S182–S189. doi: 10.1016/j.arth.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 545.Glanzmann MC, Audigé L, Schwyzer H-K, Kolling C. Re-intervention and revision rates following primary reverse total shoulder arthroplasty—review of a local shoulder arthroplasty registry. Int Orthop. 2020;44:2365–2370. doi: 10.1007/s00264-020-04721-8. [DOI] [PubMed] [Google Scholar]
- 546.Bin Abd Razak HR, Lee JHM, Tan SM, et al. Satisfaction rates are low following revision total knee arthroplasty in Asians Despite improvements in patient-reported outcome measures. J Knee Surg. 2020;33:1041–1046. doi: 10.1055/s-0039-1692629. [DOI] [PubMed] [Google Scholar]
- 547.Pachter CS, Garfinkel JH, Cochrane NH, et al. Smoking is a risk factor for wound complications after direct anterior hip arthroplasty with mesh tape closure. Adv Skin Wound Care. 2020;33:43–46. doi: 10.1097/01.ASW.0000613544.11947.8b. [DOI] [PubMed] [Google Scholar]
- 548.Desai VS, Pareek A, DeDeugd CM, et al. Smoking, unemployment, female sex, obesity, and medication use yield worse outcomes in patellofemoral arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020;28:2962–2969. doi: 10.1007/s00167-019-05704-y. [DOI] [PubMed] [Google Scholar]
- 549.Domb BG, Chen SL, Shapira J, et al. The evolution of hip arthroscopy: what has changed since 2008-a single surgeon’s experience. Arthroscopy. 2020;36:761–772. doi: 10.1016/j.arthro.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 550.Goldman AH, Osmon DR, Hanssen AD, et al. The Lawrence D. Dorr Surgical Techniques & Technologies Award: aseptic reoperations within one year of primary total hip arthroplasty markedly increase the risk of later periprosthetic joint infection. J Arthroplasty. 2020;35:S10–S14. doi: 10.1016/j.arth.2020.02.054. [DOI] [PubMed] [Google Scholar]
- 551.Carlson SW, Sierra RJ, Trousdale RT. Total hip arthroplasty in patients with osteogenesis imperfecta. J Arthroplasty. 2020;35:2131–2135. doi: 10.1016/j.arth.2020.03.023. [DOI] [PubMed] [Google Scholar]
- 552.Greenberg A, Kandel L, Liebergall M, et al. Total knee arthroplasty for Valgus Deformity via a lateral approach: clinical results, comparison to medial approach, and review of recent literature. J Arthroplasty. 2020;35:2076–2083. doi: 10.1016/j.arth.2020.03.037. [DOI] [PubMed] [Google Scholar]
- 553.Rosinsky PJ, Annin S, Maldonado DR, et al. Arthroscopic Ligamentum Teres reconstruction: minimum 2-year patient-reported outcomes with subanalysis of patients with Ehlers–Danlos syndrome. Arthroscopy. 2020;36:2170–2182. doi: 10.1016/j.arthro.2020.04.028. [DOI] [PubMed] [Google Scholar]
- 554.Chan PK, Hwang YY, Cheung A, et al. Blood transfusions in total knee arthroplasty: a retrospective analysis of a multimodal patient blood management programme. Hong Kong Med J. 2020;26:201–207. doi: 10.12809/hkmj198289. [DOI] [PubMed] [Google Scholar]
- 555.Zhang C-F, He L, Fang X-Y, et al. Debridement, antibiotics, and implant retention for acute periprosthetic joint infection. Orthop Surg. 2020;12:463–470. doi: 10.1111/os.12641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 556.Arias-de la Torre J, Smith K, Dregan A, et al. Impact of comorbidity on the short- and medium-term risk of revision in total hip and knee arthroplasty. BMC Musculoskelet Disord. 2020;21:447. doi: 10.1186/s12891-020-03455-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 557.Lee S-H, Shih H-N, Chang C-H, et al. Influence of extension stem length and diameter on clinical and radiographic outcomes of revision total knee arthroplasty. BMC Musculoskelet Disord. 2020;21:15. doi: 10.1186/s12891-019-3030-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 558.Hoskins W, Dowsey MM, Spelman T, Choong PFM. Early surgical complications of total hip arthroplasty related to surgical approach. ANZ J Surg. 2020;90:2050–2055. doi: 10.1111/ans.16149. [DOI] [PubMed] [Google Scholar]
- 559.Hatta T, Statz JM, Itoi E, et al. Shoulder arthroplasty in patients with immunosuppression following solid organ transplantation. J Shoulder Elbow Surg. 2020;29:44–49. doi: 10.1016/j.jse.2019.05.042. [DOI] [PubMed] [Google Scholar]
- 560.Moverman MA, Menendez ME, Mahendraraj KA, et al. Patient risk factors for acromial stress fractures after reverse shoulder arthroplasty: a multicenter study. J Shoulder Elbow Surg. 2021;30:1619–1625. doi: 10.1016/j.jse.2020.09.012. [DOI] [PubMed] [Google Scholar]
- 561.Helder O, Marks M, Schweizer A, et al. Complications after surface replacing and silicone PIP arthroplasty: an analysis of 703 implants. Arch Orthop Trauma Surg. 2021;141:173–181. doi: 10.1007/s00402-020-03663-5. [DOI] [PubMed] [Google Scholar]
- 562.Montalti M, Bordini B, Natali S, et al. Revisions for periprosthetic hip infections do not fail more than revisions for aseptic loosening, but mortality is higher. J Arthroplasty. 2021;36:1074–1079. doi: 10.1016/j.arth.2020.09.038. [DOI] [PubMed] [Google Scholar]
- 563.Di Martino A, Castagnini F, Stefanini N, et al. Survival rates and reasons for revision of different stem designs in total hip arthroplasty for developmental dysplasia: a regional registry study. J Orthop Traumatol. 2021;22:29. doi: 10.1186/s10195-021-00590-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 564.Ponzio DY, Rothermel SD, Chiu Y-F, et al. Does physical activity level influence total hip arthroplasty expectations, satisfaction, and outcomes? J Arthroplasty. 2021;36:2850–2857. doi: 10.1016/j.arth.2021.03.052. [DOI] [PubMed] [Google Scholar]
- 565.Drager J, Polce EM, Fu M, et al. Patients undergoing anatomic total shoulder arthroplasty achieve clinically significant outcomes faster than those undergoing reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30:2523–2532. doi: 10.1016/j.jse.2021.02.015. [DOI] [PubMed] [Google Scholar]
- 566.Poondla RK, Sheth MM, Heldt BL, et al. Anatomic and reverse shoulder arthroplasty in patients 70 years of age and older: a comparison cohort at early to midterm follow-up. J Shoulder Elbow Surg. 2021;30:1336–1343. doi: 10.1016/j.jse.2020.08.030. [DOI] [PubMed] [Google Scholar]
- 567.Sheth MM, Morris BJ, Laughlin MS, et al. Early to midterm outcomes of anatomic shoulder arthroplasty performed on dysplastic glenoids. J Shoulder Elbow Surg. 2021;30:S77–S83. doi: 10.1016/j.jse.2020.08.017. [DOI] [PubMed] [Google Scholar]
- 568.Owen AR, Tibbo ME, van Wijnen AJ, et al. Acquired idiopathic stiffness after contemporary total knee arthroplasty: incidence, risk factors, and results over 25 years. J Arthroplasty. 2021;36:2980–2985. doi: 10.1016/j.arth.2021.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 569.Di Martino A, Coppola MAR, Bordini B, et al. Clinical and radiological outcomes of total hip arthroplasty in patients affected by Paget’s disease: a combined registry and single-institution retrospective observational study. J Orthop Traumatol. 2021;22:13. doi: 10.1186/s10195-021-00574-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 570.Russo A, Cavagnaro L, Chiarlone F, et al. Clinical outcomes and survivorship of two-stage total hip or knee arthroplasty in septic arthritis: a retrospective analysis with a minimum five-year follow-up. Int Orthop. 2021;45:1683–1691. doi: 10.1007/s00264-021-05013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 571.Gould D, Thuraisingam S, Shadbolt C et al (2021) Cohort profile: the St Vincent’s Melbourne Arthroplasty Outcomes (SMART) Registry, a pragmatic prospective database defining outcomes in total hip and knee replacement patients. BMJ Open 11:e040408. 10.1136/bmjopen-2020-040408 [DOI] [PMC free article] [PubMed]
- 572.Shah NS, Foote AM, Steele CA, et al. Does preoperative disease severity influence outcomes in reverse shoulder arthroplasty for cuff tear arthropathy? J Shoulder Elbow Surg. 2021;30:2745–2752. doi: 10.1016/j.jse.2021.04.035. [DOI] [PubMed] [Google Scholar]
- 573.Schwarz JS, Lygrisse KA, Roof MA, et al. Early, mid-term, and late-term aseptic femoral revisions after THA: comparing causes, complications, and resource utilization. J Arthroplasty. 2021;36:3551–3555. doi: 10.1016/j.arth.2021.05.041. [DOI] [PubMed] [Google Scholar]
- 574.Katakam A, Bragdon CR, Chen AF, et al. Elevated body mass index is a risk factor for failure to achieve the knee disability and osteoarthritis outcome score-physical function short form minimal clinically important difference following total knee arthroplasty. J Arthroplasty. 2021;36:1626–1632. doi: 10.1016/j.arth.2020.12.019. [DOI] [PubMed] [Google Scholar]
- 575.Giesinger K, Giesinger JM, Hamilton DF, et al. Higher body mass index is associated with larger postoperative improvement in patient-reported outcomes following total knee arthroplasty. BMC Musculoskelet Disord. 2021;22:635. doi: 10.1186/s12891-021-04512-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 576.Harmer JR, Wyles CC, Mara KC, et al. Impact of perioperative pain control on knee range of motion and development of arthrofibrosis following primary total knee arthroplasty. J Arthroplasty. 2021;36:532–536. doi: 10.1016/j.arth.2020.08.037. [DOI] [PubMed] [Google Scholar]
- 577.Katakam A, Melnic CM, Bragdon CR, et al. Low body mass index is a predictor for mortality and increased length of stay following total joint arthroplasty. J Arthroplasty. 2021;36:72–77. doi: 10.1016/j.arth.2020.07.055. [DOI] [PubMed] [Google Scholar]
- 578.Illgen RL, Lewallen DG, Yep PJ, et al. Migration patterns for revision total hip arthroplasty in the United States as reported in the American Joint Replacement Registry. J Arthroplasty. 2021;36:1401–1406. doi: 10.1016/j.arth.2020.10.030. [DOI] [PubMed] [Google Scholar]
- 579.Goh GS, Khow YZ, Tay DK, et al. Preoperative mental health influences patient-reported outcome measures and satisfaction after revision total knee arthroplasty. J Arthroplasty. 2021;36:2878–2886. doi: 10.1016/j.arth.2021.03.026. [DOI] [PubMed] [Google Scholar]
- 580.Kahlenberg CA, Baral EC, Lieberman LW, et al. Retrieval analysis of polyethylene components in rotating hinge knee arthroplasty implants. J Arthroplasty. 2021;36:2998–3003. doi: 10.1016/j.arth.2021.04.003. [DOI] [PubMed] [Google Scholar]
- 581.Grau LC, Ong AC, Restrepo S, et al. Survivorship, clinical and radiographic outcomes of a novel cementless metal-backed patella design. J Arthroplasty. 2021;36:S221–S226. doi: 10.1016/j.arth.2021.02.032. [DOI] [PubMed] [Google Scholar]
- 582.Gausden EB, Cross WW, III, Mabry TM, et al. Total hip arthroplasty for femoral neck fracture: What are the contemporary reasons for failure? J Arthroplasty. 2021;36:S272–S276. doi: 10.1016/j.arth.2021.02.008. [DOI] [PubMed] [Google Scholar]
- 583.Siljander MP, Trousdale RT, Perry KI, et al. Total hip arthroplasty in patients with osteopetrosis. J Arthroplasty. 2021;36:1367–1372. doi: 10.1016/j.arth.2020.10.018. [DOI] [PubMed] [Google Scholar]
- 584.Palazzuolo M, Antoniadis A, Mahlouly J, Wegrzyn J. Total knee arthroplasty improves the quality-adjusted life years in patients who exceeded their estimated life expectancy. Int Orthop. 2021;45:635–641. doi: 10.1007/s00264-020-04917-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 585.Di Martino A, Bordini B, Barile F, et al. Unicompartmental knee arthroplasty has higher revisions than total knee arthroplasty at long term follow-up: a registry study on 6453 prostheses. Knee Surg Sports Traumatol Arthrosc. 2021;29:3323–3329. doi: 10.1007/s00167-020-06184-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 586.Sagheb E, Ramazanian T, Tafti AP, et al. Use of natural language processing algorithms to identify common data elements in operative notes for knee arthroplasty. J Arthroplasty. 2021;36:922–926. doi: 10.1016/j.arth.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 587.Ingelsrud LH, Terluin B, Gromov K, et al. Which Oxford Knee Score level represents a satisfactory symptom state after undergoing a total knee replacement? Acta Orthop. 2021;92:85–90. doi: 10.1080/17453674.2020.1832304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 588.Tracey RW, Akram F, Della Valle CJ, et al. Clinical outcomes in isolated tibial revision with cruciate retaining total knee arthroplasty. J Arthroplasty. 2021;36:2536–2540. doi: 10.1016/j.arth.2021.02.013. [DOI] [PubMed] [Google Scholar]
- 589.Ling DI, Finocchiaro A, Schneider B, et al. CORR Insights®: what factors are associated with patient-reported outcome measure questionnaire completion for an electronic shoulder arthroplasty registry? Clin Orthop Relat Res. 2021;479:148–150. doi: 10.1097/CORR.0000000000001424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 590.Visvanathan A, Wilson C, Jackman E, et al. Design, construction, and early results of a formal local revision knee arthroplasty registry. J Knee Surg. 2021;34:1284–1295. doi: 10.1055/s-0040-1708040. [DOI] [PubMed] [Google Scholar]
- 591.Teo BJX, Koh JSB, Jiang L, et al. Association of the 36-Item Short Form Health Survey Physical Component Summary Score with patient satisfaction and improvement 2 years after total knee arthroplasty. JAMA Netw Open. 2019;2:e190062. doi: 10.1001/jamanetworkopen.2019.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 592.Castagnini F, Bordini B, Tassinari E, et al. Delta-on-delta ceramic bearing surfaces in revision hip arthroplasty. J Arthroplasty. 2019;34:2065–2071. doi: 10.1016/j.arth.2019.04.068. [DOI] [PubMed] [Google Scholar]
- 593.Johnson RL, Abdel MP, Frank RD, et al. Impact of frailty on outcomes after primary and revision total hip arthroplasty. J Arthroplasty. 2019;34:56–64.e5. doi: 10.1016/j.arth.2018.09.078. [DOI] [PubMed] [Google Scholar]
- 594.Nguyen U-SDT, Perneger T, Franklin PD, et al. Improvement in mental health following total hip arthroplasty: the role of pain and function. BMC Musculoskelet Disord. 2019;20:307. doi: 10.1186/s12891-019-2669-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 595.Chua JL, Goh GS-H, Liow MHL, et al. Modern TKA implants are equivalent to traditional TKA implants in functional and patellofemoral joint-related outcomes. Knee Surg Sports Traumatol Arthrosc. 2019;27:1116–1123. doi: 10.1007/s00167-018-5161-6. [DOI] [PubMed] [Google Scholar]
- 596.Wyles CC, Vargas-Hernandez JS, Carlson SW, et al. Single-dose perioperative antibiotics do not increase the risk of surgical site infection in unicompartmental knee arthroplasty. J Arthroplasty. 2019;34:S327–S330. doi: 10.1016/j.arth.2019.02.041. [DOI] [PubMed] [Google Scholar]
- 597.Bordini B, Stea S, Castagnini F, et al. The influence of bearing surfaces on periprosthetic hip infections: analysis of thirty nine thousand, two hundred and six cementless total hip arthroplasties. Int Orthop. 2019;43:103–109. doi: 10.1007/s00264-018-4097-2. [DOI] [PubMed] [Google Scholar]
- 598.Wyles CC, Tibbo ME, Fu S, et al. Use of natural language processing algorithms to identify common data elements in operative notes for total hip arthroplasty. J Bone Joint Surg Am. 2019;101:1931–1938. doi: 10.2106/JBJS.19.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 599.Boyer B, Bordini B, Caputo D, et al. What are the influencing factors on hip and knee arthroplasty survival? Prospective cohort study on 63619 arthroplasties. Orthop Traumatol Surg Res. 2019;105:1251–1256. doi: 10.1016/j.otsr.2019.07.020. [DOI] [PubMed] [Google Scholar]
- 600.Giordano BD, Kuhns BD, Perets I, et al. Acetabular morphologic characteristics predict early conversion to arthroplasty after isolated hip arthroscopy for femoroacetabular impingement. Am J Sports Med. 2020;48:188–196. doi: 10.1177/0363546519888894. [DOI] [PubMed] [Google Scholar]
- 601.Steinhaus ME, Buller LT, Romero JA, et al. Body mass index classification is independently associated with health-related quality of life after primary total knee arthroplasty: an institutional registry-based study. J Knee Surg. 2020;33:399–409. doi: 10.1055/s-0039-1677811. [DOI] [PubMed] [Google Scholar]
- 602.Goh GS, Liow MHL, Chen JY, et al. Can octogenarians undergoing total knee arthroplasty experience similar functional outcomes, quality of life, and satisfaction rates as their younger counterparts? A propensity score matched analysis of 1188 patients. J Arthroplasty. 2020;35:1833–1839. doi: 10.1016/j.arth.2020.02.033. [DOI] [PubMed] [Google Scholar]
- 603.Chaudhry H, MacDonald SJ, Howard JL, et al. Clinical outcomes and midterm survivorship of an uncemented primary total hip arthroplasty system. J Arthroplasty. 2020;35:1662–1666. doi: 10.1016/j.arth.2020.01.063. [DOI] [PubMed] [Google Scholar]
- 604.Sheth MM, Morris BJ, Laughlin MS, et al. Lower socioeconomic status is associated with worse preoperative function, pain, and increased opioid use in patients with primary glenohumeral osteoarthritis. J Am Acad Orthop Surg. 2020;28:287–292. doi: 10.5435/JAAOS-D-19-00490. [DOI] [PubMed] [Google Scholar]
- 605.Rosinsky PJ, Chen SL, Yelton MJ, et al. Outpatient vs. inpatient hip arthroplasty: a matched case-control study on a 90-day complication rate and 2-year patient-reported outcomes. J Orthop Surg Res. 2020;15:367. doi: 10.1186/s13018-020-01871-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 606.Galea VP, Ingelsrud LH, Florissi I, et al. Patient-acceptable symptom state for the Oxford Hip Score and Forgotten Joint Score at 3 months, 1 year, and 2 years following total hip arthroplasty: a registry-based study of 597 cases. Acta Orthop. 2020;91:372–377. doi: 10.1080/17453674.2020.1750877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 607.Tew M, Dalziel K, Clarke P, et al. Patient-reported outcome measures (PROMs): can they be used to guide patient-centered care and optimize outcomes in total knee replacement? Qual Life Res. 2020;29:3273–3283. doi: 10.1007/s11136-020-02577-4. [DOI] [PubMed] [Google Scholar]
- 608.Liow MHL, Goh GS, Pang H-N, et al. Should patients aged 75 years or older undergo medial unicompartmental knee arthroplasty? A propensity score-matched study. Arch Orthop Trauma Surg. 2020;140:949–956. doi: 10.1007/s00402-020-03440-4. [DOI] [PubMed] [Google Scholar]
- 609.Galea VP, Florissi I, Rojanasopondist P, et al. The patient acceptable symptom state for the harris hip score following total hip arthroplasty: validated thresholds at 3-month, 1-, 3-, 5-, and 7-year follow-up. J Arthroplasty. 2020;35:145–152.e2. doi: 10.1016/j.arth.2019.08.037. [DOI] [PubMed] [Google Scholar]
- 610.Marzel A, Schwyzer H-K, Kolling C, et al. The Schulthess local Shoulder Arthroplasty Registry (SAR): cohort profile. BMJ Open. 2020;10:e040591. doi: 10.1136/bmjopen-2020-040591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 611.Thompson Z, Khoshbin A, Ward S, et al. The early-to medium-term results of a hemispherical, porous coated acetabular shell with multiple different bearing combinations are excellent with the exception of metal-on-metal. Int Orthop. 2020;44:2537–2543. doi: 10.1007/s00264-020-04817-1. [DOI] [PubMed] [Google Scholar]
- 612.Yeo MGH, Goh GS, Chen JY, et al. Are Oxford Hip Score and Western Ontario and McMaster Universities Osteoarthritis Index useful predictors of clinical meaningful improvement and satisfaction after total hip arthroplasty? J Arthroplasty. 2020;35:2458–2464. doi: 10.1016/j.arth.2020.04.034. [DOI] [PubMed] [Google Scholar]
- 613.Ramaskandhan J, Rashid A, Kometa S, Siddique MS. Comparison of 5-year patient-reported outcomes (PROMs) of total ankle replacement (TAR) to total knee replacement (TKR) and total hip replacement (THR) Foot Ankle Int. 2020;41:767–774. doi: 10.1177/1071100720918880. [DOI] [PubMed] [Google Scholar]
- 614.Holtz N, Hamilton DF, Giesinger JM, et al. Minimal important differences for the WOMAC osteoarthritis index and the Forgotten Joint Score-12 in total knee arthroplasty patients. BMC Musculoskelet Disord. 2020;21:401. doi: 10.1186/s12891-020-03415-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 615.Bonilla GA, Montoya BE, Restrepo VE, et al. Institutional arthroplasty registry: what is the minimum acceptable dataset to be included in your hospital? Recommendations from a single-country national consensus using the Delphi method. Int Orthop. 2021;45:5–12. doi: 10.1007/s00264-020-04866-6. [DOI] [PubMed] [Google Scholar]
- 616.Khow YZ, Goh GS, Chen JY, et al. Change in body mass index after simultaneous bilateral total knee arthroplasty: risk factors and its influence on functional outcomes. J Arthroplasty. 2021;36:1974–1979. doi: 10.1016/j.arth.2021.01.059. [DOI] [PubMed] [Google Scholar]
- 617.Ho KK-W, Lau LC-M, Chau W-W, et al. End-stage knee osteoarthritis with and without sarcopenia and the effect of knee arthroplasty—a prospective cohort study. BMC Geriatr. 2021;21:2. doi: 10.1186/s12877-020-01929-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 618.Vigdorchik JM, Sculco PK, Inglis AE, et al. Evaluating alternate registration planes for imageless, computer-assisted navigation during total hip arthroplasty. J Arthroplasty. 2021;36:3527–3533. doi: 10.1016/j.arth.2021.05.037. [DOI] [PubMed] [Google Scholar]
- 619.Lützner J, Beyer F, Günther K-P, Huber J. Higher treatment effect after total knee arthroplasty is associated with higher patient satisfaction. Knee Surg Sports Traumatol Arthrosc. 2021;29:3426–3432. doi: 10.1007/s00167-020-06272-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 620.Miozzari HH, Barea C, Hannouche D, Lübbeke A. History of previous surgery is associated with higher risk of revision after primary total knee arthroplasty: a cohort study from the Geneva Arthroplasty Registry. Acta Orthop. 2021;92:709–715. doi: 10.1080/17453674.2021.1970322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 621.Woo BJ, Chen JY, Lai YM, et al. Improvements in functional outcome and quality of life are not sustainable for patients ≥ 68 years old 10 years after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021;29:3330–3336. doi: 10.1007/s00167-020-06200-4. [DOI] [PubMed] [Google Scholar]
- 622.Ho KW, Pong G, Poon WC, et al. Progression of health-related quality of life of patients waiting for total knee arthroplasty. J Eval Clin Pract. 2021;27:69–74. doi: 10.1111/jep.13388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 623.Khow YZ, Liow MHL, Lee M, et al. Coronal alignment of fixed-bearing unicompartmental knee arthroplasty femoral component may affect long-term clinical outcomes. J Arthroplasty. 2021;36:478–487. doi: 10.1016/j.arth.2020.07.070. [DOI] [PubMed] [Google Scholar]
- 624.Castagnini F, Bordini B, Cosentino M, et al. The influence of bearing surfaces on revisions due to dislocations in total hip arthroplasty. J Mater Sci Mater Med. 2021;32:123. doi: 10.1007/s10856-021-06598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 625.Gonzalez AI, Nguyen U-SDT, Franklin P, et al. 1-year trajectories of patients undergoing primary total hip arthroplasty: Patient reported outcomes and resource needs according to education level. BMC Musculoskelet Disord. 2022;23:84. doi: 10.1186/s12891-022-05004-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 626.Bonnefoy-Mazure A, Poncet A, Gonzalez A, et al. Limping and patient satisfaction after primary total hip arthroplasty: a registry-based cohort study. Acta Orthop. 2022;93:602–608. doi: 10.2340/17453674.2022.3489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 627.Baker CM, Restrepo C, Hozack WJ. Minimum five-year outcomes of modular dual mobility in primary total hip arthroplasty. J Arthroplasty. 2022;37:S566–S570. doi: 10.1016/j.arth.2022.02.118. [DOI] [PubMed] [Google Scholar]
- 628.Wik TS, Klaksvik J, Husby OS, et al. Patient-reported outcome after primary and aseptic revision hip arthroplasty: 1-year follow-up of 3,559 primary and 406 revision THAs in an institutional registry. Acta Orthop. 2022;93:132–137. doi: 10.2340/17453674.2021.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 629.Gifstad T, Nordskar JJ, Egeberg T, et al. Cementless unicompartmental knee arthroplasty results in higher pain levels compared to the cemented technique: a prospective register study. Knee Surg Sports Traumatol Arthrosc. 2022;30:2738–2743. doi: 10.1007/s00167-021-06617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 630.Castiello E, Affatato S. Progression of osteoarthritis and reoperation in unicompartmental knee arthroplasty: a comparison of national joint registries. Int J Artif Organs. 2020;43:203–207. doi: 10.1177/0391398819879697. [DOI] [PubMed] [Google Scholar]
- 631.Hannon CP, Kruckeberg BM, Lewallen DG, et al. Treatment of flexion instability after primary total knee arthroplasty: operative and nonoperative management of 218 cases. J Arthroplasty. 2022;37:S333–S341. doi: 10.1016/j.arth.2022.02.069. [DOI] [PubMed] [Google Scholar]
- 632.Yakkanti RR, Ocksrider JL, Patel AA, et al. Unexpected wear of a uniquely designed moderately cross-linked polyethylene in total hip arthroplasty. J Arthroplasty. 2022;37:1130–1135. doi: 10.1016/j.arth.2022.01.093. [DOI] [PubMed] [Google Scholar]
- 633.Moverman MA, Puzzitiello RN, Pagani NR, et al. Functional somatic syndromes are associated with suboptimal outcomes and high cost after shoulder arthroplasty. J Shoulder Elbow Surg. 2022;31:48–55. doi: 10.1016/j.jse.2021.05.015. [DOI] [PubMed] [Google Scholar]
- 634.Katakam A, Florissi IS, Colon Iban YE, et al. Class III obesity increases risk of failure to achieve the 1-year hip disability and Osteoarthritis Outcome Score-Physical Function Short Form minimal clinically important difference following total hip arthroplasty. J Arthroplasty. 2021;36:187–192. doi: 10.1016/j.arth.2020.07.035. [DOI] [PubMed] [Google Scholar]
- 635.Soh S-E, Harris IA, Cashman K, et al. Minimal clinically important changes in HOOS-12 and KOOS-12 scores following joint replacement. J Bone Joint Surg Am. 2022;104:980–987. doi: 10.2106/JBJS.21.00741. [DOI] [PubMed] [Google Scholar]
- 636.Singh JA, Lewallen DG. Depression in primary TKA and higher medical comorbidities in revision TKA are associated with suboptimal subjective improvement in knee function. BMC Musculoskelet Disord. 2014;15:127. doi: 10.1186/1471-2474-15-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 637.Muscatelli SR, Zheng H, Hughes RE, et al. Non-inferiority of aspirin for venous thromboembolism prophylaxis after hip arthroplasty in a statewide registry. J Arthroplasty. 2021;36:2068–2075.e2. doi: 10.1016/j.arth.2021.01.025. [DOI] [PubMed] [Google Scholar]
- 638.Canetti R, Malatray M, Pibarot V, Wegrzyn J. Dual mobility cups associated with proximal femoral replacement in nontumoral indications: results and complications. Orthop Traumatol Surg Res. 2022;108:103029. doi: 10.1016/j.otsr.2021.103029. [DOI] [PubMed] [Google Scholar]
- 639.Johnson RL, Frank RD, Abdel MP, et al. Frailty transitions one year after total joint arthroplasty: a cohort study. J Arthroplasty. 2022;37:10–18.e2. doi: 10.1016/j.arth.2021.08.022. [DOI] [PubMed] [Google Scholar]
- 640.Koh DTS, Woo YL, Yew AKS, Yeo S-J. Kinematic aligned femoral rotation leads to greater patella tilt but similar clinical outcomes when compared to traditional femoral component rotation in total knee arthroplasty. A propensity score matched study. Knee Surg Sports Traumatol Arthrosc. 2021;29:1059–1066. doi: 10.1007/s00167-020-06081-7. [DOI] [PubMed] [Google Scholar]
- 641.Goh GS, Bin Abd Razak HR, Tay DK-J, et al. Early post-operative oxford knee score and knee society score predict patient satisfaction 2 years after total knee arthroplasty. Arch Orthop Trauma Surg. 2021;141:129–137. doi: 10.1007/s00402-020-03612-2. [DOI] [PubMed] [Google Scholar]
- 642.Allport J, Ramaskandhan J, Alkhreisat M, Siddique MS. Patient-reported outcome measures and radiological outcomes in mobile-bearing total ankle arthroplasty with varus or valgus deformity. Foot Ankle Int. 2021;42:176–182. doi: 10.1177/1071100720949852. [DOI] [PubMed] [Google Scholar]
- 643.Balazs GC, Dooley M, Wang D, et al. Clinical outcomes of open hip abductor tendon repair with minimum two-year follow-up. Hip Int. 2022;32:516–522. doi: 10.1177/1120700020965487. [DOI] [PubMed] [Google Scholar]
- 644.Cherian NJ, Ohnoutka C, Peissig EJ, et al. Cemented patellar implant malposition: a non-issue for the painful total knee arthroplasty. J Arthroplasty. 2022;37:S859–S863. doi: 10.1016/j.arth.2022.02.020. [DOI] [PubMed] [Google Scholar]
- 645.Lucchini S, Baleani M, Giardina F, et al. A case-driven hypothesis for multi-stage crack growth mechanism in fourth-generation ceramic head fracture. J Orthop Surg Res. 2022;17:293. doi: 10.1186/s13018-022-03190-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 646.Macheras GA, Lepetsos P, Galanakos SP, et al. Early failure of an uncemented femoral stem, as compared to two other stems with similar design, following primary total hip arthroplasty performed with direct anterior approach. Hip Int. 2022;32:166–173. doi: 10.1177/1120700020940671. [DOI] [PubMed] [Google Scholar]
- 647.Kenanidis E, Kakoulidis P, Leonidou A, et al. Survival of monoblock RM vitamys compared with modular PINNACLE cups: mid-term outcomes of 200 hips performed by a single surgeon. Hip Int. 2021;31:465–471. doi: 10.1177/1120700019885619. [DOI] [PubMed] [Google Scholar]
- 648.Claxton MR, Wagner ER, Rizzo M. Long-term outcomes of MCP surface replacement arthroplasty in patients with rheumatoid arthritis. Hand. 2022;17:271–277. doi: 10.1177/1558944720926631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 649.Goh GS, Zeng GJ, Khow YZ, et al. No difference in long-term outcomes between men and women undergoing medial fixed-bearing cemented unicompartmental knee arthroplasty: a retrospective cohort study with minimum 10-year follow up. Knee. 2021;30:26–34. doi: 10.1016/j.knee.2021.03.006. [DOI] [PubMed] [Google Scholar]
- 650.Harmer JR, Wyles CC, Larson DR, et al. Changing surgical approach from primary to revision total hip arthroplasty is not associated with increased risk of dislocation or re-revisions. J Arthroplasty. 2022;37:S622–S627. doi: 10.1016/j.arth.2022.03.007. [DOI] [PubMed] [Google Scholar]
- 651.Shaw JH, Rahman TM, Wesemann LD, et al. Comparison of postoperative instability and acetabular cup positioning in robotic-assisted versus traditional total hip arthroplasty. J Arthroplasty. 2022;37:S881–S889. doi: 10.1016/j.arth.2022.02.002. [DOI] [PubMed] [Google Scholar]
- 652.Dagneaux L, Amundson AW, Larson DR, et al. Contemporary mortality rate and outcomes in nonagenarians after primary total knee arthroplasty. J Arthroplasty. 2021;36:3456–3462. doi: 10.1016/j.arth.2021.05.015. [DOI] [PubMed] [Google Scholar]
- 653.Dagneaux L, Amundson AW, Larson DR, et al. Contemporary mortality rate and outcomes in nonagenarians undergoing primary total hip arthroplasty. J Arthroplasty. 2021;36:1373–1379. doi: 10.1016/j.arth.2020.10.040. [DOI] [PubMed] [Google Scholar]
- 654.Hughes RE, Batra A, Hallstrom BR. Arthroplasty registries around the world: valuable sources of hip implant revision risk data. Curr Rev Musculoskelet Med. 2017;10:240–252. doi: 10.1007/s12178-017-9408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 655.Stickles B, Phillips L, Brox WT, et al. Defining the relationship between obesity and total joint arthroplasty. Obes Res. 2001;9:219–223. doi: 10.1038/oby.2001.24. [DOI] [PubMed] [Google Scholar]
- 656.Guo S-J, Shao H-Y, Huang Y, et al. Retrospective cohort study comparing complications, readmission, transfusion, and length of stay of patients undergoing simultaneous and staged bilateral total hip arthroplasty. Orthop Surg. 2020;12:233–240. doi: 10.1111/os.12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 657.Kostuj T, Preis M, Walther M, et al. German Total Ankle Replacement Register of the German Foot and Ankle Society (D. A. F.)—presentation of design and reliability of the data as well as first results. Z Orthop Unfall. 2014;152:446–454. doi: 10.1055/s-0034-1382933. [DOI] [PubMed] [Google Scholar]
- 658.Arias-de la Torre J, Puigdomenech E, Valderas JM, et al. Availability of specific tools to assess patient reported outcomes in hip arthroplasty in Spain. Identifying the best candidates to incorporate in an arthroplasty register. A systematic review and standardized assessment. PLoS One. 2019;14(4):e0214746. doi: 10.1371/journal.pone.0214746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 659.Ranawat CS, Meftah M, Windsor EN, Ranawat AS. Cementless fixation in total knee arthroplasty: down the boulevard of broken dreams - affirms. J Bone Joint Surg Br. 2012;94(11 Suppl A):82–84. doi: 10.1302/0301-620X.94B11.30826. [DOI] [PubMed] [Google Scholar]
- 660.van der List JP, McDonald LS, Pearle AD. Systematic review of medial versus lateral survivorship in unicompartmental knee arthroplasty. Knee. 2015;22(6):454–460. doi: 10.1016/j.knee.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 661.Park CN, White PB, Meftah M, Ranawat AS, Ranawat CS. Diagnostic algorithm for residual pain after total knee arthroplasty. Orthopedics. 2016;39(2):e246–e252. doi: 10.3928/01477447-20160119-06. [DOI] [PubMed] [Google Scholar]
- 662.van der List JP, Zuiderbaan HA, Pearle AD. Why do medial unicompartmental knee arthroplasties fail today? J Arthroplasty. 2016;31(5):1016–1021. doi: 10.1016/j.arth.2015.11.030. [DOI] [PubMed] [Google Scholar]
- 663.van der List JP, Chawla H, Joskowicz L, Pearle AD. Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3482–3495. doi: 10.1007/s00167-016-4305-9. [DOI] [PubMed] [Google Scholar]
- 664.van der List JP, Chawla H, Villa JC, Pearle AD. Why do patellofemoral arthroplasties fail today? A systematic review. Knee. 2017;24(1):2–8. doi: 10.1016/j.knee.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 665.van der List JP, Chawla H, Zuiderbaan HA, Pearle AD. Survivorship and functional outcomes of patellofemoral arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2622–2631. doi: 10.1007/s00167-015-3878-z. [DOI] [PubMed] [Google Scholar]
- 666.Gu A, Michalak AJ, Cohen JS, Almeida ND, McLawhorn AS, Sculco PK. Efficacy of manipulation under anesthesia for stiffness following total knee arthroplasty: a systematic review. J Arthroplasty. 2018;33(5):1598–1605. doi: 10.1016/j.arth.2017.11.054. [DOI] [PubMed] [Google Scholar]
- 667.Stryker LS, Abdel MP, Hanssen AD. Predictive value of inflammatory markers for irrigation and debridement of acute TKA infection. Orthopedics. 2013;36(6):765–770. doi: 10.3928/01477447-20130523-22. [DOI] [PubMed] [Google Scholar]
- 668.Oviedo Baena AM, Moeschler SM, Smith HM, Duncan CM, Schroeder DR, Kopp SL. Perioperative comorbidities and complications among patients undergoing primary total knee arthroplasty: a retrospective analysis and prospective survey. J Clin Anesth. 2015;27(7):558–565. doi: 10.1016/j.jclinane.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 669.Amanatullah DF, Stryker L, Schoenecker P, et al. Similar clinical outcomes for THAs with and without prior periacetabular osteotomy. Clin Orthop Relat Res. 2015;473(2):685–691. doi: 10.1007/s11999-014-4026-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 670.Werthel JD, Lonjon G, Jo S, Cofield R, Sperling JW, Elhassan BT. Long-term outcomes of cemented versus cementless humeral components in arthroplasty of the shoulder: a propensity score-matched analysis. Bone Joint J. 2017;99-B(5):666–673. doi: 10.1302/0301-620X.99B5.BJJ-2016-0910.R1. [DOI] [PubMed] [Google Scholar]
- 671.Brown TS, Van Citters DW, Berry DJ, Abdel MP. The use of highly crosslinked polyethylene in total knee arthroplasty. Bone Joint J. 2017;99-B(8):996–1002. doi: 10.1302/0301-620X.99B8.BJJ-2017-0028.R1. [DOI] [PubMed] [Google Scholar]
- 672.Shi GG, Huh J, Gross CE, et al. Total ankle arthroplasty following prior infection about the ankle. Foot Ankle Int. 2015;36(12):1425–1429. doi: 10.1177/1071100715597430. [DOI] [PubMed] [Google Scholar]
- 673.Mirza AJ, Lombardi AV, Jr, Morris MJ, Berend KR. A mini-anterior approach to the hip for total joint replacement: optimising results: improving hip joint replacement outcomes. Bone Joint J. 2014;96-B(11 Supple A):32–35. doi: 10.1302/0301-620X.96B11.34348. [DOI] [PubMed] [Google Scholar]