Abstract
Background
Successful post-knee replacement rehabilitation requires adequate access to health information, social support, and periodic monitoring by a health professional. Mobile health (mHealth) and computer-based technologies are used for rehabilitation and remote monitoring. The extent of technology use and its function in post-knee replacement rehabilitation care in low and middle-income settings are unknown.
Objective
To inform future mHealth intervention development, we conducted a scoping review to map the features and functionality of existing technologies and determine users’ perspectives on telerehabilitation and technology for self-management.
Methods
We followed the Joanna Briggs Institute methodology for scoping reviews. We searched the Embase, Medline, PsycINFO via OVID, and Cochrane Central Register of Controlled Trials databases for manuscripts published from 2001 onward. We included original research articles reporting the use of mobile or computer-based technologies by patients, health care providers, researchers, or family members. Studies were divided into the following 3 categories based on the purpose: validation studies, clinical evaluation, and end user feedback. We extracted general information on study design, technology features, proposed function, and perspectives of health care providers and patients. The protocol for this review is accessible in the Open Science Framework.
Results
Of the 5960 articles, 158 that reported from high-income settings contributed to the qualitative summary (64 studies on mHealth or telerehabilitation programs, 28 validation studies, 38 studies describing users’ perceptions). The highest numbers of studies were from Europe or the United Kingdom and North America regarding the use of a mobile app with or without wearables and reported mainly in the last decade. No studies were from low and middle-income settings. The primary functions of technology for remote rehabilitation were education to aid recovery and enable regular, appropriate exercises; monitoring progress of pain (n=19), activity (n=20), and exercise adherence (n=30); 1 or 2-way communication with health care professionals to facilitate the continuum of care (n=51); and goal setting (n=23). Assessment of range of motion (n=16) and gait analysis (n=10) were the commonly validated technologies developed to incorporate into a future rehabilitation program. Few studies (n=14) reported end user involvement during the development stage. We summarized the reasons for satisfaction and dissatisfaction among users across various technologies.
Conclusions
Several existing mobile and computer-based technologies facilitate post-knee replacement rehabilitation care for patients and health care providers. However, they are limited to high-income settings and may not be extrapolated to low-income settings. A systematic needs assessment of patients undergoing knee replacement and health care providers involved in rehabilitation, involving end users at all stages of development and evaluation, with clear reporting of the development and clinical evaluation can make post-knee replacement rehabilitation care in resource-poor settings accessible and cost-effective.
Keywords: knee arthroplasty, telerehabilitation, mHealth, rehabilitation, monitoring, self-management, knee, arthroplasty, social support, mHealth intervention, development, scoping review, knee replacement
Introduction
Knee arthroplasty is the gold standard treatment for end-stage osteoarthritis when conservative treatments fail to relieve symptoms [1]. Wound care and postarthroplasty physiotherapy are essential components of this treatment. Poor adherence to physiotherapy could delay the recovery and lead to suboptimal functional outcomes [2]. Beyond in-hospital clinical care and initiation of physical therapy before discharge, continued and reliable access to information, support from health care providers, awareness of the recovery pathway, easy access to rehabilitation centers, and periodic monitoring are influential factors for optimal recovery [3-6]. In addition to an uneventful surgery, postarthroplasty outcomes are associated with several patient-related factors such as their preoperative physical and mental state, comorbidities, social support, and socioeconomic status, emphasizing the need for personalized approaches [7]. Hence, monitoring of the rehabilitation phase is essential, whether at clinics, in rehabilitation units, or at home [8-10].
Technology-assisted remote monitoring methods are increasingly being advocated in high-income countries. There is low to moderate-quality evidence on the superiority of telerehabilitation compared with unsupported home-based rehabilitation and noninferiority compared with clinic-based monitoring with respect to range of motion (ROM), pain, function, quality of life, and cost-effectiveness at 3 months between clinic-based and home-based rehabilitation strategies using technology [11-17]. Hence, current evidence supports the adaptation of technology-based rehabilitation as feasible, as safe, and as good as clinic-based monitoring with an additional benefit of saving out-of-pocket expenditure. Technology-based approaches are diverse, varying from telehealth [17] to virtual reality techniques [13] aimed at improving adherence to physical therapy and facilitating remote monitoring [12] of patient progress during the post-acute rehabilitation phase [18].
Therefore, the aim of this scoping review was to summarize the extent, range, and nature of technology used for provision of rehabilitation or to monitor progress following knee arthroplasty. This scoping review aimed to address the following objectives:
To map the characteristic features and functionality of the technologies, guiding or theoretical framework for designing the technology, and evaluation methodologies of mobile technology–based apps for rehabilitation monitoring and self-management following knee arthroplasty
To understand the patient and physical therapist perspectives regarding the use of mobile technology–based apps for rehabilitation monitoring and self-management following knee arthroplasty
To our knowledge, there are no existing scoping reviews that address our aims [19]. The information from this review will help us and other researchers make an informed decision on future mobile health (mHealth) interventions for monitoring post-knee arthroplasty rehabilitation care by physiotherapists and orthopedic surgeons and to promote self-management by individuals. This review will also help highlight existing gaps in the context of low and middle-income countries (LMICs).
Methods
We conducted this scoping review following the Joanna Briggs Institute (JBI) methodology for JBI Scoping Reviews [20] and consulted the PRISMA-ScR (Preferred Reporting Items for Systematic Review and Meta-Analyses Extension for Scoping Reviews) checklist for reporting [21]. The protocol was registered at the Open Science Framework [22].
Data Sources and Searches
To identify relevant studies, an electronic database literature search was conducted in the Embase, Medline, PsycINFO via OVID, and Cochrane Central Register of Controlled Trials (CENTRAL) databases using the following key terms: “Knee arthroplasty OR Knee replacement,” “mobile,” “web,” “remote sensor,” “computer,” “telerehabilitation,” and “m-health” (Tables S1 and S2 in Multimedia Appendix 1). The search was executed in October 2021 and updated in August 2023. The search was restricted to 2001 onward. There were no language restrictions during the search. We searched the reference list of included articles to identify potentially eligible studies.
Study Selection
Predefined inclusion criteria were articles reporting the use of mobile or computer apps or any other technologies such as sensor-based devices for delivering or monitoring rehabilitation either scheduled or following knee joint replacement. We also included proof- of-concept papers that described the development process of a mobile or technology-based solution for rehabilitation. The purpose of technology could be for a health care provider to monitor rehabilitation adherence, to aid patient-health care provider communication, to promote self-management, to act as reminders, or to act as a source of education or any other function that is aimed at rehabilitation care following knee replacement. The app or technology could be used by patients, health care providers, researchers, or a family member. Included studies could have been conducted in the community or home for any clinical setting in any geographic region. The studies were required to be original research articles, and we included experimental and observational studies using quantitative or qualitative research methods. Reviews (narrative or systematic reviews), non-English articles, and articles without abstracts or full texts were excluded.
Data Extraction
Screening of manuscript titles and abstracts was conducted by 2 independent reviewers using the web app Rayyan [23]. Prior to screening, reviewers discussed inclusion and exclusion criteria to ensure consistency between individuals. Two reviewers assessed the eligibility of the full text, and disagreements were resolved by discussion. Systematic reviews were not included in the review but were used to obtain potentially relevant references. Multiple publications originating from a single technology were grouped and presented as 1 study.
For data charting purposes, the studies were divided into the following 3 categories: (1) studies that had no rehabilitation program but included an app or a technology to assess ROM or gait and were validation studies, (2) studies reporting the use of a mobile or computer app or a telehealth delivery platform for a rehabilitation program with or without sensor-based devices and wearable sensors, (3) studies that reported end users’ perceptions of the technology used for rehabilitation monitoring. Data on the general information for the studies, features of the technology, the proposed function, and perspectives of health care providers and patients were extracted and entered in Microsoft Excel. If only the protocol of a planned study was available, there was no information on clinical evaluation, or the study included <6 individuals, we did not extract data beyond the general information.
Results
Search Results
The database search, including the ad hoc search, yielded 5960 articles. Of these articles, 300 articles were considered potentially relevant. Of these, 158 articles were included for data extraction, 131 articles were excluded, and 11 articles were not available (Table S3 in Multimedia Appendix 1). Of the 158 articles, 91 articles (64 studies) reported the clinical evaluation of a technology-based rehabilitation program, 29 articles (28 studies) reported the validation or a proof of concept of technology intended to be used for rehabilitation, and 13 articles were protocols of evaluation studies. In addition, 25 articles reported end users’ perceptions on technology (Figure 1) as stand-alone articles or part of clinical evaluation studies (n=13), totaling 38 studies. The 13 studies that reported the perceptions of technology that were also included in rehabilitation program studies were removed from the final list of included full-text articles to avoid double counting.
Figure 1.
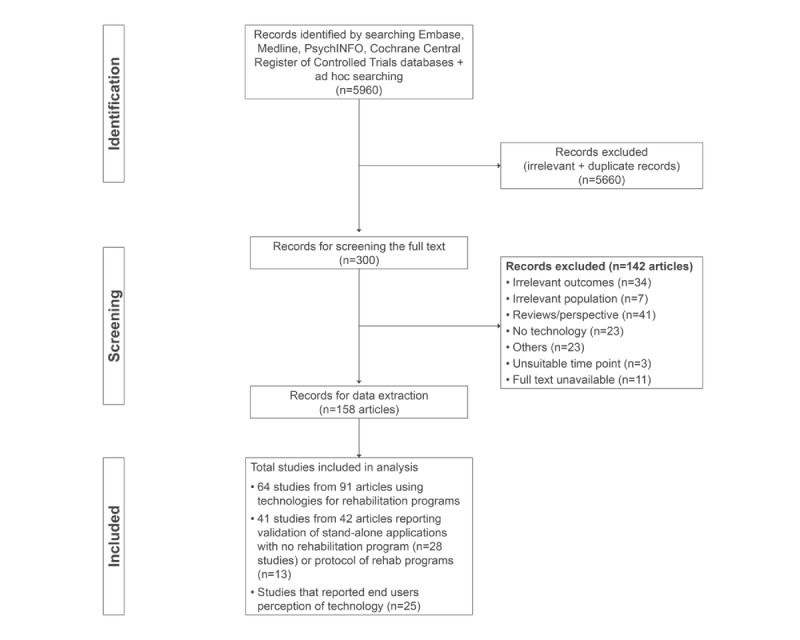
Process of identifying and including studies according to PRISMA-ScR (Preferred Reporting Items for Systematic Review and Meta-Analyses Extension for Scoping Reviews).
Technology for Rehabilitation
Characteristics of the 105 Studies
Studies were reported from Europe and the United Kingdom (n=45) [11, 24-60, 62-66, 169, 170], North America (n=34) [6, 67-99], Australia and New Zealand (n=10) [100-109], and Asia (n=16) [110-125]. None of the studies were from LMICs. Reports of mobile-based technologies represented the highest number (54/105, 51.4%) [6, 25-27, 31, 32, 36, 37, 41-50, 52, 55, 56, 58-60, 62, 64, 67-69, 74, 75, 78, 80, 82, 83, 90-92, 95, 101, 103, 106-108, 112, 113, 117, 121-126, 169], followed by computer applications (31/105, 29.5%) [24, 29, 30, 33-35, 39, 53, 54, 57, 65, 66, 70, 73, 76, 79, 84-86, 89, 93, 97, 98, 100, 102, 104, 111, 114, 116, 120, 127], and tele/video/web conferencing (20/105, 19%) for rehabilitation monitoring [28, 38, 51, 63, 71, 72, 77, 81, 87, 88, 94, 96, 99, 105, 109, 110, 115, 118, 119, 170]. The highest use of mobile apps associated with or without a wearable was in Europe and the United Kingdom, followed by North America. Tele/video/web conferencing was used across regions, with the highest number in North America (Figure 2).
Figure 2.
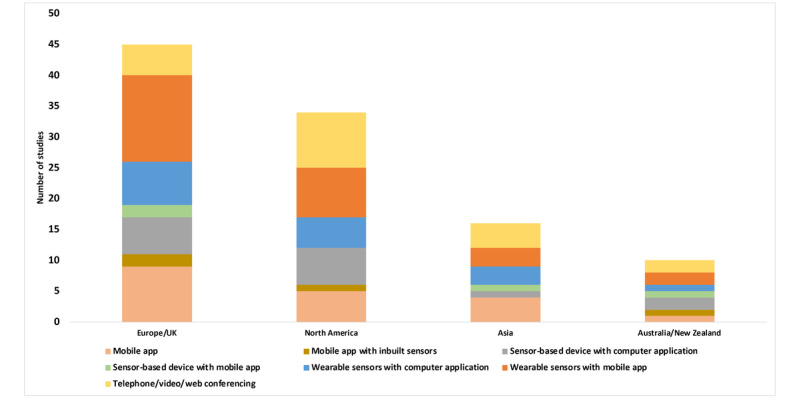
Number of studies published by region based on different technologies (n=105).
Validation Studies
There were 28 validation studies. Studies that validated stand-alone technologies included those to assess ROM (n=16) [24, 29, 43, 45, 48, 49, 52, 68, 73, 84, 100, 101, 111, 112, 116, 125] or gait or posture (n=10) [29, 30, 33, 53, 57, 74, 89, 97, 102, 124], and 2 studies involved technologies to monitor exercises [98, 114]. The technologies involved were either wearables (n=20) [24, 29, 30, 33, 45, 48, 49, 57, 68, 73, 84, 89, 97, 98, 100, 111, 112, 114, 116, 125], sensor-based devices (nonwearables; n=4) [53, 66, 102, 124], or inbuilt sensors available within a smartphone (n=4) [43, 52, 74, 101] (Table S4 in Multimedia Appendix 1).
In terms of study design, 9 were cross-sectional studies [33, 48, 52, 57, 84, 89, 97, 101, 116], 7 were cohort or longitudinal studies [45, 53, 68, 74, 100, 111, 125], 5 were pre-post studies [29, 30, 43, 73, 102], 1 was an uncontrolled trial [112], 1 was a randomized controlled trial (RCT) [66], and 5 were articles that described the proof of concept or development plan for the technologies [24, 49, 98, 114, 124]. The participant sample size ranged from 1 to 60. Most studies reported reliability between a standard or universal goniometer and smartphone app goniometry and the clinical evaluation of sensors to measure gait parameters (Table S4 in Multimedia Appendix 1). In 7 studies, gait was measured using sensors provided by a health care provider in a hospital setting [29, 33, 57, 74, 89, 97, 102], and 3 studies did not describe the measurement setting [30, 53, 124].
Clinical Evaluation Studies
There were 64 clinical evaluation studies. The technology consisted of a mobile or computer app with a wearable device (n=18) [6, 26, 31, 32, 39, 44, 46, 50, 54, 64, 67, 69, 90, 92, 95, 106, 108, 169], a mobile or computer app with a sensor-based device (n=13) [25, 34, 35, 40, 42, 65, 70, 76, 79, 85, 86, 93, 120], only a mobile app (n=14) [36, 37, 55, 56, 62, 75, 78, 80, 83, 107, 113, 117, 123, 128], or only telephone or videoconferencing (n=19) for remote monitoring [28, 38, 51, 63, 71, 72, 77, 81, 88, 94, 96, 99, 105, 109, 110, 115, 118, 119, 170]. Of the studies that used a mobile app, 9 studies were developed only for iOS [55, 67, 69, 71, 77, 92, 106, 107, 109], 1 was an Android app [42], 7 were for both Android and iOS devices [28, 36, 56, 88, 108, 115, 117], and 21 studies did not specify the platform (Multimedia Appendix 2). A web-based clinician portal for synchronous or asynchronous remote monitoring of patients was reported by 36 studies (Table 1). The number of published studies and the intervention arm sample size (ranging from 7 to 2292), especially for those that included wearable sensors and mobile apps, steadily increased over the last 2 decades (Figure 3).
Table 1.
Summary of application functionality (N=64).
| First author, year | Web portal | Devices | Peer | App name | |||
|
|
Monitoring | Wearables | Sensor-based devices |
|
|
||
| Alexander, 2023 [67] | ✓ | Apple Watch | —a | — | mymobility | ||
| An, 2021 [110] | — | — | — | — | — | ||
| Argent, 2019 [169] | — | IMUb | Avatar | — | — | ||
| Bäcker, 2021 [25] | — | GenuSport | — | — | GenuSport | ||
| Bade, 2020 [166] | — | In-shoe sensors | — | — | — | ||
| Bell, 2020 [90] | ✓ | InterACTION IMU | — | — | — | ||
| Bini, 2017 [71] | ✓ | — | — | — | Capture proof | ||
| Blasco, 2022 [28] | — | — | — | — | WeChat app | ||
| Campbell, 2019 [72] | ✓ | — | — | — | StreaMD | ||
| Chughtai, 2018 [76] | ✓ | — | VERAc | — | VERA | ||
| Chughtai, 2019 [75] | — | — | — | ✓ | PReHab | ||
| Colomina, 2021 [31] | ✓ | Fitbit Flex 2 | — | — | — | ||
| Correia, 2019 [32] | ✓ | IMU | — | — | — | ||
| De Berardinis, 2022 [26] | ✓ | Magnetic sensors with Velcro bands | — | — | kari | ||
| Doiron-Cadrin, 2020 [77] | — | — | — | — | Reacts Lite | ||
| Duong, 2023 [106] | ✓ | Fitbit, ActivPal, Goniometer Pro | — | — | — | ||
| Eichler, 2019 [34] | ✓ | Kinect sensor | — | — | MainReha app | ||
| Eisermann, 2004 [39] | ✓ | Accelerometers, wrist band, chest sensors | Web cams | — | — | ||
| Farr-Wharton, 2020 [108] | ✓ | Garmin Vivosmart heart rate activity tracker | — | — | — | ||
| Fung, 2012 [79] | — | — | Wii sensor balance | — | — | ||
| Gianola, 2020 [35] | — | — | Avatar | — | — | ||
| Gohir, 2021 [36] | ✓ | — | — | — | i-Beat app | ||
| Gray, 2022 [37] | ✓ | — | — | — | Digital Joint School using GoWell health program | ||
| Gunduz, 2021 [38] | — | — | — | — | — | ||
| Hadamus, 2022 [40] | — | — | Kinetic camera | — | — | ||
| Hardwick-Morris, 2022 [107] | ✓ | — | — | — | Physitrack | ||
| Hong, 2022 [80] | — | — | — | — | Digital Musculoskeletal Surgical Care Program app | ||
| Huang, 2017 [113] | — | — | — | — | Yishu | ||
| Janhunen, 2023 [42] | — | — | Kinect sensor with TV and tablet | — | — | ||
| Juhl, 2016 [44] | ✓ | IMU | — | — | ICURA app | ||
| Klement, 2019 [81] | ✓ | — | — | — | — | ||
| Knapp, 2021 [83] | ✓ | — | — | — | — | ||
| Kramer, 2003 [99] | — | — | — | — | — | ||
| Kuether, 2019 [85] | ✓ | — | VERA | — | — | ||
| Lam, 2016 [86] | ✓ | IMU | — | — | ReHab system | ||
| Lebleu, 2023 [46] | ✓ | Activity tracker Garmin vívofit 4 | — | — | moveUP Therapy | ||
| LeBrun, 2022 [78] | ✓ | — | — | — | MyChart app | ||
| Li, 2023 [115] | — | — | — | ✓ | — | ||
| Lu, 2021 [117] | — | — | — | ✓ | — | ||
| McDonall, 2022 [147] | ✓ | — | — | — | — | ||
| Mehta, 2020 [6] | ✓ | Activity tracker | — | ✓ | — | ||
| Milliren, 2022 [88] | — | — | — | — | Ubicare Smart X | ||
| Nuevo, 2023 [50] | ✓ | Accelerometer, gyroscope, magnetometer (DyCare) | — | — | ReHub | ||
| Osterloh, 2023 [51] | ✓ | — | — | ✓ | YOLii | ||
| Park, 2017 [118] | — | — | — | — | — | ||
| Park, 2023 [119] | — | — | — | — | — | ||
| Piqueras, 2013 [54] | ✓ | (WAGYRO) | Avatar | — | — | ||
| Pournajaf, 2022 [65] | — | — | — | — | — | ||
| Pronk, 2020 [55] | — | — | — | — | Pain coach app | ||
| Prvu Bettger, 2019 [70] | ✓ | — | VERA | — | — | ||
| Ramkumar, 2019 [92] | ✓ | Motion sensors | — | — | Focus ventures RPM | ||
| Russell, 2011 [105] | — | — | — | — | — | ||
| Scheper, 2019 [56] | ✓ | — | — | — | Woundcare app | ||
| Su, 2015 [120] | — | Kinect sensor | — | — | — | ||
| Summers, 2023 [93] | ✓ | — | Electro-mechanical device | — | — | ||
| Szöts, 2016 [170] | — | — | — | — | — | ||
| Timmers, 2019 [62] | — | — | — | — | The Patient Journey app | ||
| Torpil, 2022 [63] | — | — | — | — | — | ||
| Tousignant, 2011 [94] | ✓ | — | — | — | — | ||
| Tripuraneni, 2021 [95] | ✓ | Smart watch | — | — | — | ||
| van Dijk-Huisman, 2020 [64] | ✓ | MOX activity monitor | — | — | — | ||
| Visperas, 2021 [96] | ✓ | — | — | — | — | ||
| Wang, 2023 [121] | — | — | — | ✓ | WeChat app | ||
| Zhang, 2021 [123] | — | — | — | ✓ | WeChat app | ||
aNot applicable.
bIMU: inertial motion unit.
cVERA: Virtual Exercise Rehabilitation Assistant.
Figure 3.
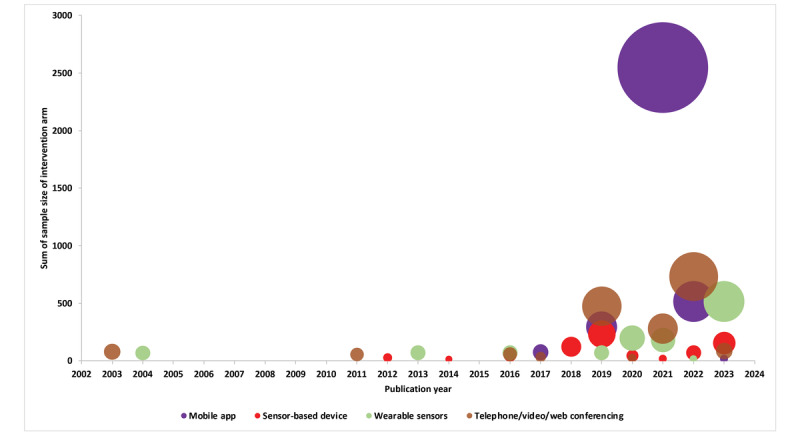
Technologies developed over the years by sample size (n=64), with the size of the bubble indicating the sample size of the intervention arm of all the studies published that particular year per technology category. Mobile app = mobile app + mobile app with inbuilt sensors; sensor-based device = sensor-based device with a mobile app + sensor-based device with a computer application; wearable sensors = wearable sensors with a mobile app + wearable sensors with a computer application + wearable sensors.
Although most studies described the features and functionality of the technology to deliver the intervention, they lacked details about the technological aspects that could benefit future researchers. For example, 2 studies [31, 86] explicitly reported information on the software, programming language and tools used, or calibration procedures either along with the main study or cited the article that described the development phase. Information on conceptualization of the technology-based intervention was described in only 3 studies [37, 38, 120]. End users’ involvement was typically late during the development phase (ie, prototype stage) and involved refining the functionalities and features of technology [32, 51, 64, 65, 75-77, 80, 86, 88, 115, 118, 169] prior to deployment. Patient feedback on their needs at an early development phase was reported only by Blasco et al [28].
Clinical effectiveness was tested using an RCT design in 57.8% (37/64) of the studies [6, 25, 28, 34-36, 39, 42, 44, 50, 51, 54, 55, 62, 63, 65, 67, 70-72, 77, 79, 90, 94-96, 99, 105, 106, 108-110, 117-119, 128, 170], and the rest of the studies were either retrospective comparative cohort studies (n=3) [26, 37, 78], uncontrolled cohort studies (n=9) [46, 56, 69, 76, 81, 83, 85, 92, 169], cross-sectional studies (n=1) [86], or non-RCTs (n=14) [31, 32, 38, 40, 64, 75, 80, 88, 93, 107, 113, 115, 120, 123].
We found 13 study protocols, of which 12 were RCTs published between 2013 and 2023 [11, 41, 47, 58-60, 82, 87, 91, 103, 104, 122], for which we could not find a published report and hence were not included in this summary. User experience was measured in trials using quantitative (n=9) [32, 34, 38, 50, 55, 94, 96, 105, 123], qualitative (n=2) [61, 128], and mixed methods (n=3) [39, 90, 109] approaches.
Application Functionality for Rehabilitation Programs
The key functionalities of the telerehabilitation technologies extracted from 64 studies are summarized under 4 themes, namely education and enablement, monitoring progress, communication, and goal setting (Table 2).
Table 2.
Themes of the key functionalities of the telerehabilitation technologies.
| First author, year | Exercise | Monitoring progress | Functions | Communication | |||||||||||||||
|
|
Repository | Diary | Tracker or reminder | Biofeedback | VRa | Feedback to patient | Pain | ROMb | Knee function | Physical activity | Sedentary time | Sleep | Triggers | Goal setting | Direction | Mode | |||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
| Alexander, 2023 [67] | ✓ | —c | ✓ | — | — | SPd | — | — | ✓ | ✓ | — | — | — | — | 2-way | Text, F2Fe | |||
| An, 2021 [110] | ✓ | — | — | — | — | SP | — | — | — | — | — | — | — | — | 2-way | Video | |||
| Argent, 2019 [169] | ✓ | — | ✓ | ✓ | ✓ | SAf | ✓ | ✓ | — | — | — | — | — | Exercise | 2-way | F2F | |||
| Bäcker, 2021 [25] | ✓ | — | ✓ | ✓ | — | SA | — | — | — | — | — | — | — | Exercise | — | — | |||
| Bade, 2020 [166] | ✓ | — | ✓ | ✓ | — | SA | — | — | — | — | — | — | — | — | 2-way | F2F | |||
| Bell, 2020 [90] | ✓ | — | ✓ | ✓ | — | SA, APg | — | ✓ | — | — | — | — | — | — | 2-way | Video | |||
| Bini, 2017 [71] | ✓ | — | — | — | — | AP | — | — | — | — | — | — | — | — | 2-way | Text, video, F2F | |||
| Blasco, 2022 [28] | — | — | — | — | — | — | — | — | — | — | — | — | SCh | — | 1-way, 2-way | Text, audio, F2F | |||
| Campbell, 2019 [72] | ✓ | — | ✓ | — | — | AP | — | — | — | — | — | — | — | — | 1-way (SMS text messaging bot) | Video, text | |||
| Chughtai, 2018 [76] | ✓ | — | ✓ | ✓ | ✓ | SA, SP | ✓ | ✓ | ✓ | ✓ | — | — | — | — | 2-way | Video | |||
| Chughtai, 2019 [75] | ✓ | ✓ | — | — | — | — | ✓ | — | — | — | — | — | — | — | — | — | |||
| Colomina, 2021 [31] | — | — | ✓ | — | — | SA, AP | ✓ | — | — | ✓ | ✓ | ✓ | SC | Exercise | 2-way | Text | |||
| Correia, 2019 [32] | ✓ | — | ✓ | ✓ | — | SA, AP | — | ✓ | — | — | — | — | — | — | 2-way | Audio, F2F | |||
| De Berardinis, 2022 [26] | ✓ | — | ✓ | ✓ | — | SA | — | — | — | — | — | — | SC | Exercise | 2-way | F2F | |||
| Doiron-Cadrin, 2019 [77] | ✓ | — | ✓ | — | — | SP | — | — | — | — | — | — | — | — | 2-way | Video | |||
| Duong, 2023 [106] | ✓ | — | ✓ | — | — | AAi, AP | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | SC | Activity | 1-way, 2-way | Text, video | |||
| Eichler, 2019 [34] | ✓ | — | ✓ | ✓ | ✓ | SA, AP | — | ✓ | — | — | — | — | — | Exercise | 1-way, 2-way | Audio, video, text, F2F | |||
| Eisermann, 2004 [39] | ✓ | — | — | ✓ | — | SA, AP | ✓ | — | — | ✓ | — | — | — | — | 2-way | Text | |||
| Farr-Wharton, 2020 [108] | ✓ | — | ✓ | — | — | AA, AP | ✓ | ✓ | — | ✓ | — | ✓ | DSj | Function | 1-way | Text, audio | |||
| Fung, 2012 [79] | ✓ | — | ✓ | ✓ | ✓ | SA | — | — | — | — | — | — | — | Lower extremity function | 2-way | F2F | |||
| Gianola, 2020 [35] | ✓ | — | ✓ | ✓ | ✓ | SA | — | — | — | — | — | — | — | Exercise | — | — | |||
| Gohir, 2021 [36] | ✓ | — | ✓ | — | — | AA, AP | — | — | — | — | — | — | — | Exercise | 1-way, 2-way | Text, audio (tele) | |||
| Gray, 2022 [37] | ✓ | — | — | — | — | SP | — | — | — | — | — | — | — | — | 1-way, 2-way | Text | |||
| Gunduz, 2021 [38] | ✓ | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — | |||
| Hadamus, 2022 [40] | ✓ | — | — | ✓ | ✓ | SA, SP | — | — | — | — | — | — | — | Exercise | 2-way | F2F | |||
| Hardwick-Morris, 2022 [107] | ✓ | ✓ | — | — | — | SP | ✓ | — | — | — | — | — | SC | — | 2-way | Video, text | |||
| Hong, 2022 [80] | ✓ | — | — | — | — | SP | — | — | — | — | — | — | — | Recovery goals | 2-way | Video | |||
| Huang, 2017 [113] | ✓ | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — | |||
| Janhunen, 2023 [42] | ✓ | ✓ | — | ✓ | ✓ | SA | — | — | — | — | — | — | — | Exercise | — | — | |||
| Juhl, 2016 [44] | ✓ | — | — | ✓ | — | SP | — | — | — | — | — | — | SC | — | 2-way | Unclear | |||
| Klement, 2019 [81] | ✓ | — | ✓ | — | — | — | — | — | — | — | — | — | — | — | 1-way, 2-way | Text, videos, F2F | |||
| Knapp, 2021 [83] | ✓ | — | ✓ | — | — | — | — | — | — | — | — | — | NUk | — | — | — | |||
| Kramer, 2003 [99] | — | — | ✓ | — | — | — | — | — | — | — | — | — | SC | — | 2-way | Audio | |||
| Kuether, 2019 [85] | ✓ | — | ✓ | ✓ | ✓ | SA, SP | — | — | ✓ | ✓ | — | — | — | — | 2-way | F2F, video | |||
| Lam, 2016 [86] | ✓ | — | ✓ | ✓ | ✓ | SA, SP | — | ✓ | — | — | — | — | — | ROM, strength | — | — | |||
| Lebleu, 2023 [46] | ✓ | ✓ | — | ✓ | — | SA, AP | ✓ | ✓ | ✓ | ✓ | — | — | DS | — | 2-way | Text | |||
| LeBrun, 2022 [78] | ✓ | — | — | — | — | SP | — | — | — | — | — | — | SC | — | 2-way | Audio, video | |||
| Li, 2023 [115] | ✓ | — | ✓ | — | — | SP | — | — | — | — | — | — | — | — | 2-way | Video, text | |||
| Lu, 2021 [117] | ✓ | — | — | — | — | SP | — | — | — | — | — | — | SC | — | 2-way | Video | |||
| McDonall, 2022 [147] | ✓ | — | — | — | — | — | — | — | — | — | — | — | — | Pain management, knee function, avoiding complications | — | — | |||
| Mehta, 2020 [6] | — | — | ✓ | — | — | AA | ✓ | — | — | ✓ | — | — | DS, NU | Activity | 1-way, 2-way | Text, F2F | |||
| Milliren, 2022 [88] | — | — | — | — | — | — | — | — | — | — | — | — | — | Discharge goal | 1-way | Text (automatic) | |||
| Nuevo, 2023 [50] | ✓ | — | ✓ | ✓ | — | SA | ✓ | ✓ | — | — | — | — | DS, NU | — | 2-way | Video, text | |||
| Osterloh, 2023 [51] | ✓ | — | — | — | — | SP | — | — | — | — | — | — | SC | — | 2-way | Video | |||
| Park, 2017 [118] | — | — | ✓ | — | — | — | — | — | — | — | — | — | SC | — | 1-way, 2-way | Text, audio (tele), | |||
| Park, 2023 [119] | — | — | — | — | — | SP | — | — | — | — | — | — | SC | — | 2-way | Audio calls | |||
| Piqueras, 2013 [54] | ✓ | — | ✓ | ✓ | ✓ | SA, AP | — | ✓ | — | — | — | — | — | — | 2-way | Audio (tele) | |||
| Pournajaf, 2022 [65] | ✓ | — | — | ✓ | ✓ | SA | — | — | — | — | — | — | VR-based balance board | Exercise | ✓ | Exercise | |||
| Pronk, 2020 [55] | ✓ | — | — | — | — | Unclear | ✓ | — | — | — | — | — | — | — | — | — | |||
| Prvu Bettger, 2019 [70] | ✓ | — | — | ✓ | ✓ | SA, SP, AP | — | — | ✓ | ✓ | ✓ | — | — | Exercise | 2-way | Video, F2F | |||
| Ramkumar, 2019 [92] | ✓ | — | ✓ | ✓ | ✓ | SA | ✓ | ✓ | — | ✓ | — | — | DS | Exercise | 1-way | Text | |||
| Russell, 2011 [105] | ✓ | ✓ | — | — | — | SP | — | ✓ | — | ✓ | — | — | SC | Unclear | 2-way | Video | |||
| Scheper, 2019 [56] | — | — | — | — | — | — | ✓ | — | — | — | — | — | DS | — | 1-way | Text | |||
| Su, 2015 [120] | ✓ | — | — | ✓ | ✓ | SA | — | — | — | — | — | — | — | Exercise | — | — | |||
| Summers, 2023 [93] | ✓ | — | ✓ | ✓ | — | SA, SP | ✓ | ✓ | ✓ | ✓ | — | — | DS | — | 2-way | Video | |||
| Szöts, 2016 [170] | — | — | — | — | — | — | — | — | — | — | — | — | — | — | 2-way | Audio (tele) | |||
| Timmers, 2019 [62] | ✓ | — | — | — | — | — | ✓ | — | — | — | — | — | — | — | 1-way | Audio, video, text | |||
| Torpil, 2022 [63] | — | — | — | — | — | — | — | — | — | — | — | — | SC | Occupation related | 2-way | Video | |||
| Tousignant, 2011 [94] | — | — | — | — | — | SP | — | — | — | — | — | — | SC | — | 2-way | Video | |||
| Tripuraneni, 2021 [95] | ✓ | — | ✓ | — | — | AA | — | — | — | ✓ | ✓ | — | — | — | 1-way | Text | |||
| van Dijk-Huisman, 2020 [64] | ✓ | — | ✓ | ✓ | — | SA, AP | — | — | — | ✓ | — | — | SC | — | 2-way | Video | |||
| Visperas, 2021 [96] | ✓ | — | — | — | — | AP | ✓ | — | ✓ | — | — | — | DS, SC | — | 1-way, 2-way | Text, audio (telephone) | |||
| Wang, 2023 [121] | ✓ | ✓ | ✓ | — | — | AP | — | — | — | — | — | — | — | Task | 2-way | Text | |||
| Zhang, 2021 [123] | ✓ | — | — | — | — | — | — | — | — | — | — | — | — | — | 2-way | Audio, text, video | |||
aVR: virtual reality.
bROM: range of motion.
cNot applicable.
dSP: synchronous from physiotherapist.
eF2F: face to face.
fSA: synchronous from app.
gAP: asynchronous from physiotherapist.
hSC: scheduled call.
iAA: asynchronous from app.
jDS: danger signs.
kNU: non-use.
Education and Enablement
An exercise repository in the form of videos, text, or infographics was one of the main features in the studies (n=53), of which only 20 studies described the list of exercises (Table S5 in Multimedia Appendix 1). Education for patients was part of the rehabilitation program in 17 studies. Table S6 in Multimedia Appendix 1 lists the topic areas covered in the education materials. Regarding exercise, 6 studies reported using an e-diary for maintaining an exercise log, 11 studies reported using reminders to perform exercises, and 13 studies reported using a tracker for exercise adherence (Multimedia Appendix 2). Feedback on the appropriateness of exercise performance was synchronous (biofeedback or virtual reality) from the app (n=19), directly from the health care provider via a video call with the patients (patient performing exercise live, measurement of ROM during video call, transmission of virtual avatar data to health care provider; n=14), or provided via both (n=6; Table 2). Feedback to the patient, which was either in the form of push notifications or a progress summary, was asynchronous from the app using automated programs in 2 studies. Asynchronous feedback from a health care provider in the form of instructions, messages, or an exercise regimen was reported in 13 studies. Feedback via both the app and a health care provider was provided in 3 studies (Table 2). Only 7 studies [6, 51, 75, 115, 117, 123, 128] had an option for peer support for patients.
Measuring Progress
Measurement of patient-reported outcomes such as pain (n=19) was an inbuilt feature in the app. Changes in knee function and activity were monitored directly via wearables or captured using patient-reported outcome measures. These included ROM in 15 studies, knee function in 8 studies, physical activity in 20 studies, sedentary behavior in 5 studies, and sleep in 4 studies. Automatic alerts were provided to the health care provider for any danger signs such as knee pain, wound health, opioid consumption, function, ROM, number of steps, exercise adherence, and any negative response to questions after entering the postoperative follow-up in 9 studies; for non-use of the technology by patients in 4 studies; and for scheduled consultations in 18 studies (Table 2).
Communication
Mobile app–enabled 1-way communication included push messages, notifications, reminders, patients’ replies to inbuilt questions in the app, information sent to the patient by the health care team, and an SMS text messaging bot (n=10). Two-way communication, either via an app or in face-to-face visits, was reported in 41 studies. In addition, 11 studies reported a combination of both 1 and 2-way communication, and 1 study did not provide sufficient information about communication. Electronic communication was delivered in the form of text, audio or video messages, and direct communication (Table 2).
Goal Setting
Goal setting for exercises, activity, pain management, knee function, ROM, muscle strength, rehabilitation, and discharge as part of the rehabilitation program was reported in 23 studies. The goals were set by either the health care provider or the patient (Table 2).
End Users’ Perceptions
Of the 38 studies that reported user perspectives, 2 focused on the perspectives of health care providers, 27 focused on the perspectives of patients and caregivers, and 9 focused on the perspectives of both groups (health care providers and patients and caregivers). The approach for data collection was quantitative (n=23), qualitative (n=9), or mixed methods (n=6). The sample size ranged from 2 to 200 health care providers and from 5 to 2292 patients (Tables S7 and S8 in Multimedia Appendix 1).
Commonly used quantitative questionnaires to assess satisfaction were the System Usability Scale [129] and the net promoter score [130]. To ratify the experience with telerehabilitation, the Telemedicine Perception Questionnaire was used [131]. Acceptability and usability were assessed using the acceptance of information technology questionnaire [132] and the Telemedicine Usability Questionnaire [133]. Some studies used bespoke questionnaires to report user experience and satisfaction [32, 39, 61, 90, 94, 105, 109, 134-146].
Overall, health care providers perceived telerehabilitation and the use of technology such as biosensors as a way of improving efficiency in providing care [146], patient adherence to exercises [39, 136, 146], patient-physician communication [136], and case management [137, 146]. The main factors associated with user satisfaction with e-consultations were reliable technology, good voice or image synchronization, the refresh rate of images, sound quality, and operability of the peripherals [94, 96, 138, 139]. The key factors they perceived would influence use and uptake of technology were decreased workload (rather than increased) [140], reliability of measurements aided by technology [146], ability to measure functional outcomes objectively [141], clearer criteria when choosing appropriate patients to be enrolled in the program [140], self-efficacy in the use of technology [94, 138, 146], and ease of reporting and tracking of patient data [90]. Patients and health care providers felt e-learning modules, push notifications, and appropriate feedback from sensors and virtual reality improved self-management [138, 142-144] (Figure 4).
Figure 4.
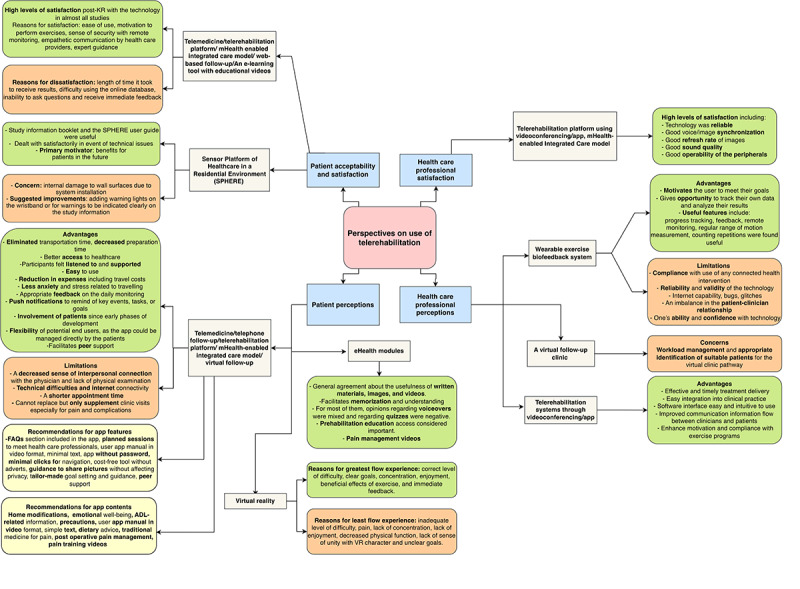
Perceptions of patients and health care providers about the technology used. ADL: activities of daily living; FAQs: frequently asked questions; KR: knee replacement; mHealth: mobile health; VR: virtual reality.
Patient satisfaction levels were reported when teleconsultation was provided via a computer, smartphone, or tablet [34, 39, 55, 56, 80, 92, 105, 121, 123, 134, 135, 145, 147-149]; telephone [61], videoconferencing [38, 77, 94, 105, 139, 141, 150-152], a web-based system [32, 50, 90, 96, 140, 153], and an mHealth-enabled integrated care model [46, 88, 138]. Patients were satisfied with telemonitoring due to improved access to services, continued support after discharge from hospital, ability for self-management, reduced need for clinic visits, reduction in cost and travel time, ability of health care providers to provide personalized care [32, 61, 94, 121, 136, 138, 140, 141, 145, 153-155], ease of use [34, 50, 55, 56, 92, 105, 135, 138, 147, 148], motivation to perform exercises [134, 135], sense of security with remote monitoring [134, 155], and empathetic communication by a health care provider [121, 135, 136, 145, 152, 155]. The reasons for dissatisfaction were lack of an in-person examination, shorter appointment times, delay in receiving reports (eg, x-ray), and an inability to transfer pictures from one technology to another [140, 145, 149, 153]. Patients provided suggestions for the app functionalities to improve the ease of use such as minimal clicks, an instructional video for app navigation, and restriction of commercial advertisements [149]. Home modifications [149], emotional well-being, information related to activities of daily living in simple text, dietary advice, frequently asked questions, and use of traditional medicine for postoperative pain management were a few of the suggestions for app content [121].
Patients were generally satisfied with the telerehabilitation program and were ready to recommend it to others [39, 80, 85, 96, 121, 135, 151]. The use of technology for rehabilitation was influenced by computer literacy [141, 150]. However, interruption of virtual physiotherapy sessions due to poor internet issues [139] was not commonly reported (Figure 4).
Discussion
Principal Findings
This scoping review summarized the extent, user perceptions, range, and nature of technologies used to support rehabilitation following knee arthroplasty. All studies reported in this review were from upper and middle-to-upper–income countries, with a steep increase in studies in the last decade. The technologies focused on enabling patients to remember prescribed exercises as well as be able to perform them appropriately by providing synchronous and asynchronous feedback via biosensors or virtual reality. Motivation and support during recovery via technology-enabled 1-way or 2-way communication gave patients access to health care providers. Self-management and monitoring of progress were dependent on active input using e-diaries by patients or passive input through wearables. In the context where these technologies were evaluated, end users were satisfied and found remote monitoring to be acceptable for routine use.
The last decade has seen an exponential increase in the number of arthroplasties worldwide [156]; however, a corresponding increase in technological solutions to facilitate remote monitoring is nonexistent in resource-limited settings such as LMICs where the need for monitoring and a continuum of care may be higher due to lower literacy levels and lack of access to rehabilitation clinics. Research on this topic that can inform clinical practice is nonexistent in the LMIC context. Despite a high penetration of the smartphone market [157] in LMICs, a higher initial investment to develop the technology, especially in the health care sector [158], or a lack of publication of such efforts could be reasons. In LMICs, there is an increasing trend of lower limb joint replacement procedures [156]. High out-of-pocket expenditures incurred due to home visits by physiotherapists or clinic visits by patients [159] dictate the need for a cost-effective and feasible technology-based strategy to fit the context while using lessons learned from available research.
There is unequivocal evidence that there is a need for physical and psychological support from professionals during the recovery period for pain management, adherence to exercises, and modifications to therapy planning based on one’s progress [3, 160, 161]. The apps were either focused on a single function (such as communication or knowledge transfer) or were multifunctional. They were generally received well by end users; however, the usability and acceptability of these applications or remote monitoring modalities cannot be extrapolated to low health literacy and tech literacy settings. The challenges we expect with using remote monitoring in the LMIC context could be inequitable smartphone access or tech literacy, internet speed, affordability of wearables, the burden to the health system if these needs are provided free of cost, and the need for educational content in multiple languages in countries with a non-native English-speaking, multilingual population such as in India [162].
Implications for Future Research
mHealth interventions have the potential to expand the reach and effectiveness of health support by facilitating behavior change. However, to ensure these “digital behavior health interventions” effectively engage users and are effective, both microengagement (the mHealth interface) and macroengagement (evidence-based behavior change techniques) are essential [163, 164]. However, we found only a handful of studies that reported user involvement during the development stage [28, 32, 51, 58, 64, 65, 75-77, 80, 86, 88, 115, 118, 169]. Studies rarely provided an adequate explanation of the theoretical behavioral framework behind the technology-based interventions [165].
Since the context and technologies are so varied, any new applications that are developed, especially in the LMIC context, should undertake formative research with end users to understand their needs, understand their preferences, and study the local digital regulatory requirements before investing time and effort. Feasibility and pilot testing by a multidisciplinary team should be crucial steps before a full-scale evaluation [69, 166], and embedding end users’ involvement and documenting their experiences at every stage are vital to refining future interventions [164]. Further, the rehabilitation protocols should map the application features with the desired function [167, 168], and this should be confirmed by means of a process evaluation embedded within the clinical evaluation to inform the mechanism of the impact in a real-life setting [147].
Limitations
This review needs to be interpreted in light of the following limitations. This scoping review focused only on technology interventions for post-knee replacement rehabilitation and hence cannot be extrapolated to other orthopedic procedures. We did not include articles for which the full text was not available. Further, incomplete reporting on the features and functions of the technology is possible and may have affected our qualitative summary and conclusion.
We did not perform a consultation phase as per the guidelines [20], and the research question was formulated upon discussion between the researchers of the scoping review team, physiotherapists, and clinicians. We limited our search from 2001 onward; however, since knee arthroplasty and mHealth came into practice in the last 2 decades, this restriction in the search may not have an implication for our review findings.
Conclusion
Several technologies have been identified to promote adherence, increase self-efficacy, enhance self-management, and support remote monitoring. However, all the available technologies have been developed and used in developed countries. The need for remote monitoring is compelling in resource-limited countries where knee arthroplasty is on the rise. However, irrespective of the context, it is important to involve a multidisciplinary team and include users’ perspectives during the development stage.
What Was Already Known About the Topic
Computer and mobile technologies to support rehabilitation following knee arthroplasty are in wide use. Telerehabilitation and remote monitoring are as effective and safe as clinic-based rehabilitation programs. They reduce out-of-pocket expenditure or health cost expenditure by reducing the time to discharge following surgery and the number of clinic visits after discharge.
What This Study Adds
This study provides a map of the types of technology and the functionality of mobile and computer-based multifunction applications. We summarized end users’ perceptions and reasons for satisfaction or dissatisfaction with available technology. The findings reflect the lack of research and readily available technologies for LMICs.
Acknowledgments
The authors would like to thank distinguished Professor Gordon Guyatt, in the Department of Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, Ontario, Canada, for providing expert comments. We also thank Dr. Shyamashree Biswas, Research Intern at the George institute, for assisting with the quality check of the extracted data.
This scoping review is a part of a fellowship funded by DBT/Wellcome Trust India Alliance (grant number: IA/CPHI/20/1/505224).
Abbreviations
- CENTRAL
Cochrane Central Register of Controlled Trials
- JBI
Joanna Briggs Institute
- LMIC
low and middle-income countries
- mHealth
mobile health
- PRISMA-ScR
Preferred Reporting Items for Systematic Review and Meta-Analyses Extension for Scoping Reviews
- RCT
randomized controlled trial
- ROM
range of motion
Supplementary information on search strategy, included and excluded studies.
Raw data extraction file for rehabilitation program studies.
PRISMA-ScR checklist.
Footnotes
Authors' Contributions: ND conceptualized the protocol and conducted the search. ND, SP, PS, and ShP screened and extracted the data. The first draft was written by SP. RM and AK interpreted the study findings and gave significant feedback to the early drafts. RMad provided expert comments and suggestions and edited the later version of manuscript. ND takes responsibility for the data. All authors read and agreed to the final version of the manuscript.
Conflicts of Interest: None declared.
References
- 1.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008 Feb;16(2):137–62. doi: 10.1016/j.joca.2007.12.013. https://linkinghub.elsevier.com/retrieve/pii/S1063-4584(07)00397-4 .S1063-4584(07)00397-4 [DOI] [PubMed] [Google Scholar]
- 2.Artz N, Elvers KT, Lowe CM, Sackley C, Jepson P, Beswick AD. Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis. BMC Musculoskelet Disord. 2015 Feb 07;16(1):15. doi: 10.1186/s12891-015-0469-6. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-015-0469-6 .10.1186/s12891-015-0469-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldsmith LJ, Suryaprakash N, Randall E, Shum J, MacDonald V, Sawatzky R, Hejazi S, Davis JC, McAllister P, Bryan S. The importance of informational, clinical and personal support in patient experience with total knee replacement: a qualitative investigation. BMC Musculoskelet Disord. 2017 Mar 24;18(1):127. doi: 10.1186/s12891-017-1474-8. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-017-1474-8 .10.1186/s12891-017-1474-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Groeneveld BS, Dekkers T, Mathijssen NMC, Vehmeijer SBW, Melles M, Goossens RHM. Communication preferences in total joint arthroplasty: exploring the patient experience through generative research. Orthop Nurs. 2020;39(5):292–302. doi: 10.1097/NOR.0000000000000694.00006416-202009000-00005 [DOI] [PubMed] [Google Scholar]
- 5.Westby MD, Backman CL. Patient and health professional views on rehabilitation practices and outcomes following total hip and knee arthroplasty for osteoarthritis:a focus group study. BMC Health Serv Res. 2010 May 11;10(1):119. doi: 10.1186/1472-6963-10-119. https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-10-119 .1472-6963-10-119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehta SJ, Hume E, Troxel AB, Reitz C, Norton L, Lacko H, McDonald C, Freeman J, Marcus N, Volpp KG, Asch DA. Effect of remote monitoring on discharge to home, return to activity, and rehospitalization after hip and knee arthroplasty: a randomized clinical trial. JAMA Netw Open. 2020 Dec 01;3(12):e2028328. doi: 10.1001/jamanetworkopen.2020.28328. https://europepmc.org/abstract/MED/33346847 .2774354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwartz FH, Lange J. Factors that affect outcome following total joint arthroplasty: a review of the recent literature. Curr Rev Musculoskelet Med. 2017 Sep 29;10(3):346–355. doi: 10.1007/s12178-017-9421-8. https://europepmc.org/abstract/MED/28664450 .10.1007/s12178-017-9421-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.L Snell D, Hipango J, Sinnott KA, Dunn JA, Rothwell A, Hsieh CJ, DeJong G, Hooper G. Rehabilitation after total joint replacement: a scoping study. Disabil Rehabil. 2018 Jul 23;40(14):1718–1731. doi: 10.1080/09638288.2017.1300947. [DOI] [PubMed] [Google Scholar]
- 9.Alrawashdeh W, Eschweiler J, Migliorini F, El Mansy Y, Tingart M, Rath B. Effectiveness of total knee arthroplasty rehabilitation programmes: A systematic review and meta-analysis. J Rehabil Med. 2021 Jun 02;53(6):jrm00200. doi: 10.2340/16501977-2827. doi: 10.2340/16501977-2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buhagiar MA, Naylor JM, Harris IA, Xuan W, Adie S, Lewin A. Assessment of outcomes of inpatient or clinic-based vs home-based rehabilitation after total knee arthroplasty: a systematic review and meta-analysis. JAMA Netw Open. 2019 Apr 05;2(4):e192810. doi: 10.1001/jamanetworkopen.2019.2810.2731681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jansson MM, Rantala A, Miettunen J, Puhto A, Pikkarainen M. The effects and safety of telerehabilitation in patients with lower-limb joint replacement: A systematic review and narrative synthesis. J Telemed Telecare. 2020 Apr 21;28(2):96–114. doi: 10.1177/1357633x20917868. [DOI] [PubMed] [Google Scholar]
- 12.Bernhardsson S, Larsson A, Bergenheim A, Ho-Henriksson C, Ekhammar A, Lange E, Larsson MEH, Nordeman L, Samsson KS, Bornhöft L. Digital physiotherapy assessment vs conventional face-to-face physiotherapy assessment of patients with musculoskeletal disorders: A systematic review. PLoS One. 2023 Mar 21;18(3):e0283013. doi: 10.1371/journal.pone.0283013. https://dx.plos.org/10.1371/journal.pone.0283013 .PONE-D-22-34676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peng L, Zeng Y, Wu Y, Si H, Shen B. Virtual reality-based rehabilitation in patients following total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. Chin Med J (Engl) 2021 Dec 13;135(2):153–163. doi: 10.1097/CM9.0000000000001847. https://europepmc.org/abstract/MED/34908004 .00029330-202201200-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Constantinescu D, Pavlis W, Rizzo M, Vanden Berge D, Barnhill S, Hernandez VH. The role of commercially available smartphone apps and wearable devices in monitoring patients after total knee arthroplasty: a systematic review. EFORT Open Rev. 2022 Jul 05;7(7):481–490. doi: 10.1530/EOR-21-0115. https://europepmc.org/abstract/MED/35900191 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Özden F, Sarı Z. The effect of mobile application-based rehabilitation in patients with total knee arthroplasty: A systematic review and meta-analysis. Arch Gerontol Geriatr. 2023 Oct;113:105058. doi: 10.1016/j.archger.2023.105058.S0167-4943(23)00136-X [DOI] [PubMed] [Google Scholar]
- 16.Gianzina E, Kalinterakis G, Delis S, Vlastos I, Platon Sachinis N, Yiannakopoulos CK. Evaluation of gait recovery after total knee arthroplasty using wearable inertial sensors: A systematic review. Knee. 2023 Mar;41:190–203. doi: 10.1016/j.knee.2023.01.006.S0968-0160(23)00006-6 [DOI] [PubMed] [Google Scholar]
- 17.McKeon JF, Alvarez PM, Vajapey AS, Sarac N, Spitzer AI, Vajapey SP. Expanding role of technology in rehabilitation after lower-extremity joint replacement: a systematic review. JBJS Rev. 2021 Sep 13;9(9):A. doi: 10.2106/JBJS.RVW.21.00016.01874474-202109000-00010 [DOI] [PubMed] [Google Scholar]
- 18.Wang X, Hunter DJ, Vesentini G, Pozzobon D, Ferreira ML. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019 Nov 03;20(1):506. doi: 10.1186/s12891-019-2900-x. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-019-2900-x .10.1186/s12891-019-2900-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seron P, Oliveros MJ, Gutierrez-Arias R, Fuentes-Aspe R, Torres-Castro RC, Merino-Osorio C, Nahuelhual P, Inostroza J, Jalil Y, Solano R, Marzuca-Nassr GN, Aguilera-Eguía R, Lavados-Romo P, Soto-Rodríguez FJ, Sabelle C, Villarroel-Silva G, Gomolán P, Huaiquilaf S, Sanchez P. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther. 2021 Jun 01;101(6):A. doi: 10.1093/ptj/pzab053. https://europepmc.org/abstract/MED/33561280 .6131423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, Godfrey CM, Khalil H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020 Oct;18(10):2119–2126. doi: 10.11124/JBIES-20-00167.02174543-202010000-00004 [DOI] [PubMed] [Google Scholar]
- 21.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp. Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018 Oct 02;169(7):467–473. doi: 10.7326/m18-0850. [DOI] [PubMed] [Google Scholar]
- 22.Pritwani S, Devasenapathy N. Mobile technology-based applications for rehabilitation monitoring and self-management after knee arthroplasty: A scoping review. Open Science Framework. 2022. Jun 21, [2023-12-11]. https://osf.io/srxkc . [DOI] [PMC free article] [PubMed]
- 23.Rayyan. [2023-12-11]. https://www.rayyan.ai/
- 24.Ayoade M, Morton L, Baillie L. Investigating the feasibility of a wireless motion capture system to aid in the rehabilitation of total knee replacement patients. 5th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth) and Workshops; May 23-26, 2011; Dublin, Ireland. 2011. [DOI] [Google Scholar]
- 25.Bäcker HC, Wu CH, Schulz MRG, Weber-Spickschen TS, Perka C, Hardt S. App-based rehabilitation program after total knee arthroplasty: a randomized controlled trial. Arch Orthop Trauma Surg. 2021 Sep 06;141(9):1575–1582. doi: 10.1007/s00402-021-03789-0. https://europepmc.org/abstract/MED/33547927 .10.1007/s00402-021-03789-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Berardinis L, Senarighi M, Ciccullo C, Forte F, Spezia M, Gigante AP. Fast-track surgery and telerehabilitation protocol in unicompartmental knee arthroplasty leads to superior outcomes when compared with the standard protocol: a propensity-matched pilot study. Knee Surg Relat Res. 2022 Dec 12;34(1):44. doi: 10.1186/s43019-022-00173-z. https://kneesurgrelatres.biomedcentral.com/articles/10.1186/s43019-022-00173-z .10.1186/s43019-022-00173-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bitsaki M, Koutras G, Heep H, Koutras C. Cost-effective mobile-based healthcare system for managing total joint arthroplasty follow-up. Healthc Inform Res. 2017 Jan;23(1):67–73. doi: 10.4258/hir.2017.23.1.67. https://europepmc.org/abstract/MED/28261533 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blasco J, Roig-Casasús S, Igual-Camacho C, Díaz-Díaz B, Pérez-Maletzki J. Conversational chatbot to promote adherence to rehabilitation after total knee replacement: implementation and feasibility. Archives of Physical Medicine and Rehabilitation. 2022 Dec;103(12):e125. doi: 10.1016/j.apmr.2022.08.764. [DOI] [Google Scholar]
- 29.Bonora S, Pirani R, Amadori E, Fantini C, Chiari L, Merlo A, Prati P, Mazzoli D. Use of a haptic biofeedback in the rehabilitation of patients with total knee arthroplasty (TKA): A pilot study. Gait & Posture. 2017 Sep;57:16–17. doi: 10.1016/j.gaitpost.2017.07.069. [DOI] [Google Scholar]
- 30.Calliess T, Bocklage R, Karkosch R, Marschollek M, Windhagen H, Schulze M. Clinical evaluation of a mobile sensor-based gait analysis method for outcome measurement after knee arthroplasty. Sensors (Basel) 2014 Aug 28;14(9):15953–64. doi: 10.3390/s140915953. https://www.mdpi.com/resolver?pii=s140915953 .s140915953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Colomina J, Drudis R, Torra M, Pallisó F, Massip M, Vargiu E, Nadal N, Fuentes A, Ortega Bravo M, Miralles F, Barbé F, Torres G, de Batlle J, CONNECARE-Lleida Group Implementing mHealth-enabled integrated care for complex chronic patients with osteoarthritis undergoing primary hip or knee arthroplasty: prospective, two-arm, parallel trial. J Med Internet Res. 2021 Sep 02;23(9):e28320. doi: 10.2196/28320. https://www.jmir.org/2021/9/e28320/ v23i9e28320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Correia FD, Nogueira A, Magalhães I, Guimarães J, Moreira M, Barradas I, Molinos M, Teixeira L, Tulha J, Seabra R, Lains J, Bento V. Medium-term outcomes of digital versus conventional home-based rehabilitation after total knee arthroplasty: prospective, parallel-group feasibility study. JMIR Rehabil Assist Technol. 2019 Feb 28;6(1):e13111. doi: 10.2196/13111. https://rehab.jmir.org/2019/1/e13111/ v6i1e13111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Vroey H, Staes F, Weygers I, Vereecke E, Vanrenterghem J, Deklerck J, Van Damme G, Hallez H, Claeys K. The implementation of inertial sensors for the assessment of temporal parameters of gait in the knee arthroplasty population. Clin Biomech (Bristol, Avon) 2018 May;54:22–27. doi: 10.1016/j.clinbiomech.2018.03.002.S0268-0033(18)30199-2 [DOI] [PubMed] [Google Scholar]
- 34.Eichler S, Salzwedel A, Rabe S, Mueller S, Mayer F, Wochatz M, Hadzic M, John M, Wegscheider K, Völler H. The effectiveness of telerehabilitation as a supplement to rehabilitation in patients after total knee or hip replacement: randomized controlled trial. JMIR Rehabil Assist Technol. 2019 Nov 07;6(2):e14236. doi: 10.2196/14236. https://rehab.jmir.org/2019/2/e14236/ v6i2e14236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gianola S, Stucovitz E, Castellini G, Mascali M, Vanni F, Tramacere I, Banfi G, Tornese D. Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: A randomized controlled trial. Medicine (Baltimore) 2020 Feb;99(7):e19136. doi: 10.1097/MD.0000000000019136. https://europepmc.org/abstract/MED/32049833 .00005792-202002140-00059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gohir SA, Eek F, Kelly A, Abhishek A, Valdes AM. Effectiveness of internet-based exercises aimed at treating knee osteoarthritis: the iBEAT-OA randomized clinical trial. JAMA Netw Open. 2021 Feb 01;4(2):e210012. doi: 10.1001/jamanetworkopen.2021.0012. https://europepmc.org/abstract/MED/33620447 .2776721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gray J, McCarthy S, Carr E, Danjoux G, Hackett R, McCarthy A, McMeekin P, Clark N, Baker P. The impact of a digital joint school educational programme on post-operative outcomes following lower limb arthroplasty: a retrospective comparative cohort study. BMC Health Serv Res. 2022 Apr 29;22(1):580. doi: 10.1186/s12913-022-07989-1. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-022-07989-1 .10.1186/s12913-022-07989-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gündüz CS, Çalişkan N. The effect of preoperative video based pain training on postoperative pain and analgesic use in patients Undergoing Total Knee Arthroplasty: a non-randomized control group intervention study. Clin Nurs Res. 2021 Jul 31;30(6):741–752. doi: 10.1177/1054773820983361. [DOI] [PubMed] [Google Scholar]
- 39.Eisermann U, Haase I, Kladny B. Computer-aided multimedia training in orthopedic rehabilitation. Am J Phys Med Rehabil. 2004 Sep;83(9):670–80. doi: 10.1097/01.phm.0000137307.44173.5d.00002060-200409000-00002 [DOI] [PubMed] [Google Scholar]
- 40.Hadamus A, Błażkiewicz M, Wydra KT, Kowalska AJ, Łukowicz M, Białoszewski D, Marczyński W. Effectiveness of early rehabilitation with exergaming in virtual reality on gait in patients after total knee replacement. J Clin Med. 2022 Aug 23;11(17):4950. doi: 10.3390/jcm11174950. https://www.mdpi.com/resolver?pii=jcm11174950 .jcm11174950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harmelink KEM, Zeegers AVCM, Tönis TM, Hullegie W, Nijhuis-van der Sanden MWG, Staal JB. The effectiveness of the use of a digital activity coaching system in addition to a two-week home-based exercise program in patients after total knee arthroplasty: study protocol for a randomized controlled trial. BMC Musculoskelet Disord. 2017 Jul 05;18(1):290. doi: 10.1186/s12891-017-1647-5. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-017-1647-5 .10.1186/s12891-017-1647-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Janhunen M, Katajapuu N, Paloneva J, Pamilo K, Oksanen A, Keemu H, Karvonen M, Luimula M, Korpelainen R, Jämsä T, Kautiainen H, Mäkelä K, Heinonen A, Aartolahti E. Effects of a home-based, exergaming intervention on physical function and pain after total knee replacement in older adults: a randomised controlled trial. BMJ Open Sport Exerc Med. 2023 Mar 03;9(1):e001416. doi: 10.1136/bmjsem-2022-001416. https://europepmc.org/abstract/MED/36896366 .bmjsem-2022-001416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jenny J. Measurement of the knee flexion angle with a smartphone-application is precise and accurate. J Arthroplasty. 2013 May;28(5):784–7. doi: 10.1016/j.arth.2012.11.013.S0883-5403(13)00100-9 [DOI] [PubMed] [Google Scholar]
- 44.Juhl C, Roth S, Schierbeck R, Nielsen L, Nordlien A, Hansen N, Bistrup I, Svenningsen B, Jepsen U, Hofland D. Effectiveness of technology assisted exercise compared to usual care in total knee arthroplasty. Osteoarthritis and Cartilage. 2016 Apr;24:S473. doi: 10.1016/j.joca.2016.01.864. [DOI] [Google Scholar]
- 45.Kontadakis G, Chasiouras D, Proimaki D, Halkiadakis M, Fyntikaki M, Mania K. Gamified platform for rehabilitation after total knee replacement surgery employing low cost and portable inertial measurement sensor node. Multimed Tools Appl. 2018 Sep 12;79(5-6):3161–3188. doi: 10.1007/s11042-018-6572-6. [DOI] [Google Scholar]
- 46.Lebleu J, Pauwels A, Anract P, Parratte S, Van Overschelde P, Van Onsem S. Digital rehabilitation after knee arthroplasty: a multi-center prospective longitudinal cohort study. J Pers Med. 2023 May 13;13(5):824. doi: 10.3390/jpm13050824. https://www.mdpi.com/resolver?pii=jpm13050824 .jpm13050824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mark-Christensen T, Thorborg K, Kallemose T, Bandholm T. Physical rehabilitation versus no physical rehabilitation after total hip and knee arthroplasties: Protocol for a pragmatic, randomized, controlled, superiority trial (The DRAW1 trial) F1000Res. 2021 Feb 25;10:146. doi: 10.12688/f1000research.50814.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marques CJ, Bauer C, Grimaldo D, Tabeling S, Weber T, Ehlert A, Mendes AH, Lorenz J, Lampe F. Sensor positioning influences the accuracy of knee ROM data of an e-rehabilitation system: a preliminary study with healthy subjects. Sensors (Basel) 2020 Apr 15;20(8):2237. doi: 10.3390/s20082237. https://www.mdpi.com/resolver?pii=s20082237 .s20082237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Msayib Y, Gaydecki P, Callaghan M, Dale N, Ismail S. An intelligent remote monitoring system for total knee arthroplasty patients. J Med Syst. 2017 Jun 18;41(6):90. doi: 10.1007/s10916-017-0735-2. https://core.ac.uk/reader/161892494?utm_source=linkout .10.1007/s10916-017-0735-2 [DOI] [PubMed] [Google Scholar]
- 50.Nuevo M, Rodríguez-Rodríguez D, Jauregui R, Fabrellas N, Zabalegui A, Conti M, Prat-Fabregat S. Telerehabilitation following fast-track total knee arthroplasty is effective and safe: a randomized controlled trial with the ReHub platform. Disabil Rehabil. 2023 Jul 05;:1–11. doi: 10.1080/09638288.2023.2228689. [DOI] [PubMed] [Google Scholar]
- 51.Osterloh J, Knaack F, Bader R, Behrens M, Peschers J, Nawrath L, Bergschmidt P, Darowski M. The effect of a digital-assisted group rehabilitation on clinical and functional outcomes after total hip and knee arthroplasty-a prospective randomized controlled pilot study. BMC Musculoskelet Disord. 2023 Mar 14;24(1):190. doi: 10.1186/s12891-023-06270-8. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-023-06270-8 .10.1186/s12891-023-06270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pereira L, Rwakabayiza S, Lécureux E, Jolles B. Reliability of the knee smartphone-application goniometer in the acute orthopedic setting. J Knee Surg. 2017 Mar 24;30(3):223–230. doi: 10.1055/s-0036-1584184. [DOI] [PubMed] [Google Scholar]
- 53.Pfeufer D, Monteiro P, Gililland J, Anderson MB, Böcker W, Stagg M, Kammerlander C, Neuerburg C, Pelt C. Immediate postoperative improvement in gait parameters following primary total knee arthroplasty can be measured with an insole sensor device. J Knee Surg. 2022 May 25;35(6):692–697. doi: 10.1055/s-0040-1716852. [DOI] [PubMed] [Google Scholar]
- 54.Piqueras M, Marco E, Coll M, Escalada F, Ballester A, Cinca C, Belmonte R, Muniesa J. Effectiveness of an interactive virtual telerehabilitation system in patients after total knee arthoplasty: a randomized controlled trial. J Rehabil Med. 2013 Apr;45(4):392–6. doi: 10.2340/16501977-1119. doi: 10.2340/16501977-1119. [DOI] [PubMed] [Google Scholar]
- 55.Pronk Y, Peters MCWM, Sheombar A, Brinkman J. Effectiveness of a mobile eHealth app in guiding patients in pain control and opiate use after total knee replacement: randomized controlled trial. JMIR Mhealth Uhealth. 2020 Mar 13;8(3):e16415. doi: 10.2196/16415. https://mhealth.jmir.org/2020/3/e16415/ v8i3e16415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scheper H, Derogee R, Mahdad R, van der Wal R, Nelissen R, Visser L, de Boer M. A mobile app for postoperative wound care after arthroplasty: Ease of use and perceived usefulness. Int J Med Inform. 2019 Sep;129:75–80. doi: 10.1016/j.ijmedinf.2019.05.010.S1386-5056(18)30816-5 [DOI] [PubMed] [Google Scholar]
- 57.Boekesteijn RJ, Smolders JMH, Busch VJJF, Geurts ACH, Smulders K. Independent and sensitive gait parameters for objective evaluation in knee and hip osteoarthritis using wearable sensors. BMC Musculoskelet Disord. 2021 Mar 03;22(1):242. doi: 10.1186/s12891-021-04074-2. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-021-04074-2 .10.1186/s12891-021-04074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stauber A, Schüßler N, Palmdorf S, Schürholz N, Bruns D, Osterbrink J, Nestler N. RECOVER-E - a mobile app for patients undergoing total knee or hip replacement: study protocol. BMC Musculoskelet Disord. 2020 Feb 04;21(1):71. doi: 10.1186/s12891-020-3090-2. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-020-3090-2 .10.1186/s12891-020-3090-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Straat AC, Maarleveld JM, Smit DJM, Visch L, Hulsegge G, Huirne JAF, van Dongen JM, van Geenen RC, Kerkhoffs GMMJ, Anema JR, Coenen P, Kuijer PPFM. (Cost-)effectiveness of a personalized multidisciplinary eHealth intervention for knee arthroplasty patients to enhance return to activities of daily life, work and sports - rationale and protocol of the multicentre ACTIVE randomized controlled trial. BMC Musculoskelet Disord. 2023 Mar 04;24(1):162. doi: 10.1186/s12891-023-06236-w.10.1186/s12891-023-06236-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Strahl A, Graichen H, Haas H, Hube R, Perka C, Rolvien T, Hubert J. Evaluation of the patient-accompanying app "alley ortho companion" for patients with osteoarthritis of the knee and hip: study protocol for a randomized controlled multi-center trial. Trials. 2022 Aug 29;23(1):716. doi: 10.1186/s13063-022-06662-6. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-022-06662-6 .10.1186/s13063-022-06662-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Szöts K, Konradsen H, Solgaard S, Bogø S, Østergaard B. Nurse-led telephone follow-up after total knee arthroplasty--content and the patients' views. J Clin Nurs. 2015 Oct 14;24(19-20):2890–9. doi: 10.1111/jocn.12905. [DOI] [PubMed] [Google Scholar]
- 62.Timmers T, Janssen L, van der Weegen W, Das D, Marijnissen W, Hannink G, van der Zwaard BC, Plat A, Thomassen B, Swen J, Kool RB, Lambers Heerspink FO. The effect of an app for day-to-day postoperative care education on patients with total knee replacement: randomized controlled trial. JMIR Mhealth Uhealth. 2019 Oct 21;7(10):e15323. doi: 10.2196/15323. https://mhealth.jmir.org/2019/10/e15323/ v7i10e15323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Torpil B, Kaya The effectiveness of client-centered intervention with telerehabilitation method after total knee arthroplasty. OTJR (Thorofare N J) 2022 Jan 22;42(1):40–49. doi: 10.1177/15394492211038293. [DOI] [PubMed] [Google Scholar]
- 64.van Dijk-Huisman HC, Weemaes AT, Boymans TA, Lenssen AF, de Bie RA. Smartphone app with an accelerometer enhances patients' physical activity following elective orthopedic surgery: a pilot study. Sensors (Basel) 2020 Aug 02;20(15):4317. doi: 10.3390/s20154317. https://www.mdpi.com/resolver?pii=s20154317 .s20154317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pournajaf S, Goffredo M, Pellicciari L, Piscitelli D, Criscuolo S, Le Pera D, Damiani C, Franceschini M. Effect of balance training using virtual reality-based serious games in individuals with total knee replacement: A randomized controlled trial. Ann Phys Rehabil Med. 2022 Nov;65(6):101609. doi: 10.1016/j.rehab.2021.101609. https://linkinghub.elsevier.com/retrieve/pii/S1877-0657(21)00126-3 .S1877-0657(21)00126-3 [DOI] [PubMed] [Google Scholar]
- 66.Ficklscherer A, Stapf J, Meissner KM, Niethammer T, Lahner M, Wagenhäuser M, Müller PE, Pietschmann MF. Testing the feasibility and safety of the Nintendo Wii gaming console in orthopedic rehabilitation: a pilot randomized controlled study. Arch Med Sci. 2016 Dec 01;12(6):1273–1278. doi: 10.5114/aoms.2016.59722. doi: 10.5114/aoms.2016.59722.27500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Alexander JS, Redfern RE, Duwelius PJ, Berend KR, Lombardi AV, Crawford DA. Use of a smartphone-based care platform after primary partial and total knee arthroplasty: 1-year follow-up of a prospective randomized controlled trial. J Arthroplasty. 2023 Jul;38(7 Suppl 2):S208–S214. doi: 10.1016/j.arth.2023.02.082.S0883-5403(23)00213-9 [DOI] [PubMed] [Google Scholar]
- 68.Antunes R, Jacob P, Meyer A, Conditt MA, Roche MW, Verstraete MA. Accuracy of measuring knee flexion after TKA through wearable IMU sensors. J Funct Morphol Kinesiol. 2021 Jul 05;6(3):60. doi: 10.3390/jfmk6030060. https://www.mdpi.com/resolver?pii=jfmk6030060 .jfmk6030060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bade M, Cheuy V, Zeni J, Christiansen C, Stevens-Lapsley J. Effects Of real-time biofeedback using instrumented insoles on recovery after total knee arthroplasty: a pilot study. Osteoarthritis and Cartilage. 2023 Mar;31:S124. doi: 10.1016/j.joca.2023.01.078. [DOI] [Google Scholar]
- 70.Prvu Bettger J, Green CL, Holmes DN, Chokshi A, Mather RC, Hoch BT, de Leon AJ, Aluisio F, Seyler TM, Del Gaizo DJ, Chiavetta J, Webb L, Miller V, Smith JM, Peterson ED. Effects of virtual exercise rehabilitation in-home therapy compared with traditional care after total knee arthroplasty. The Journal of Bone and Joint Surgery. 2019 Nov 18;102(2):101–109. doi: 10.2106/jbjs.19.00695. [DOI] [PubMed] [Google Scholar]
- 71.Bini S, Mahajan J. Clinical outcomes of remote asynchronous telerehabilitation are equivalent to traditional therapy following total knee arthroplasty: A randomized control study. J Telemed Telecare. 2016 Jul 09;23(2):239–247. doi: 10.1177/1357633x16634518. [DOI] [PubMed] [Google Scholar]
- 72.Campbell KJ, Louie PK, Bohl DD, Edmiston T, Mikhail C, Li J, Khorsand DA, Levine BR, Gerlinger TL. A novel, automated text-messaging system is effective in patients undergoing total joint arthroplasty. The Journal of Bone and Joint Surgery. 2019 Jan 16;101(2):145–151. doi: 10.2106/jbjs.17.01505. [DOI] [PubMed] [Google Scholar]
- 73.Chapman RM, Moschetti WE, Van Citters DW. Is clinically measured knee range of motion after total knee arthroplasty ‘good enough?’: A feasibility study using wearable inertial measurement units to compare knee range of motion captured during physical therapy versus at home. Medicine in Novel Technology and Devices. 2021 Sep;11:100085. doi: 10.1016/j.medntd.2021.100085. [DOI] [Google Scholar]
- 74.Christensen JC, Stanley EC, Oro EG, Carlson HB, Naveh YY, Shalita R, Teitz LS. The validity and reliability of the OneStep smartphone application under various gait conditions in healthy adults with feasibility in clinical practice. J Orthop Surg Res. 2022 Sep 14;17(1):417. doi: 10.1186/s13018-022-03300-4. https://josr-online.biomedcentral.com/articles/10.1186/s13018-022-03300-4 .10.1186/s13018-022-03300-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chughtai M, Shah NV, Sultan AA, Solow M, Tiberi JV, Mehran N, North T, Moskal JT, Newman JM, Samuel LT, Bhave A, Mont MA. The role of prehabilitation with a telerehabilitation system prior to total knee arthroplasty. Ann Transl Med. 2019 Feb;7(4):68–68. doi: 10.21037/atm.2018.11.27. https://europepmc.org/abstract/MED/30963063 .atm-07-04-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chughtai M, Kelly J, Newman J, Sultan A, Khlopas A, Sodhi N, Bhave A, Kolczun M, Mont M. The role of virtual rehabilitation in total and unicompartmental knee arthroplasty. J Knee Surg. 2018 Jan 16;32(1):105–110. doi: 10.1055/s-0038-1637018. [DOI] [PubMed] [Google Scholar]
- 77.Doiron-Cadrin P, Kairy D, Vendittoli P, Lowry V, Poitras S, Desmeules F. Feasibility and preliminary effects of a tele-prehabilitation program and an in-person prehablitation program compared to usual care for total hip or knee arthroplasty candidates: a pilot randomized controlled trial. Disabil Rehabil. 2020 Apr 13;42(7):989–998. doi: 10.1080/09638288.2018.1515992. [DOI] [PubMed] [Google Scholar]
- 78.LeBrun DG, Martino B, Biehl E, Fisher CM, Gonzalez Della Valle A, Ast MP. Telerehabilitation has similar clinical and patient-reported outcomes compared to traditional rehabilitation following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022 Dec 26;30(12):4098–4103. doi: 10.1007/s00167-022-06931-6.10.1007/s00167-022-06931-6 [DOI] [PubMed] [Google Scholar]
- 79.Fung V, Ho A, Shaffer J, Chung E, Gomez M. Use of Nintendo Wii Fit in the rehabilitation of outpatients following total knee replacement: a preliminary randomised controlled trial. Physiotherapy. 2012 Sep;98(3):183–8. doi: 10.1016/j.physio.2012.04.001.S0031-9406(12)00048-X [DOI] [PubMed] [Google Scholar]
- 80.Hong M, Loeb J, Yang M, Bailey JF. Postoperative outcomes of a digital rehabilitation program after total knee arthroplasty: retrospective, observational feasibility study. JMIR Form Res. 2022 Sep 19;6(9):e40703. doi: 10.2196/40703. https://formative.jmir.org/2022/9/e40703/ v6i9e40703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Klement MR, Rondon AJ, McEntee RM, Greenky MR, Austin MS. Web-based, self-directed physical therapy after total knee arthroplasty is safe and effective for most, but not all, patients. J Arthroplasty. 2019 Jul;34(7S):S178–S182. doi: 10.1016/j.arth.2018.11.040.S0883-5403(18)31168-9 [DOI] [PubMed] [Google Scholar]
- 82.Kline PW, Melanson EL, Sullivan WJ, Blatchford PJ, Miller MJ, Stevens-Lapsley JE, Christiansen CL. Improving physical activity through adjunct telerehabilitation following total knee arthroplasty: randomized controlled trial protocol. Phys Ther. 2019 Jan 01;99(1):37–45. doi: 10.1093/ptj/pzy119. https://europepmc.org/abstract/MED/30329126 .5134176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Knapp PW, Keller RA, Mabee KA, Pillai R, Frisch NB. Quantifying patient engagement in total joint arthroplasty using digital application-based technology. J Arthroplasty. 2021 Sep;36(9):3108–3117. doi: 10.1016/j.arth.2021.04.022. https://linkinghub.elsevier.com/retrieve/pii/S0883-5403(21)00384-3 .S0883-5403(21)00384-3 [DOI] [PubMed] [Google Scholar]
- 84.Krebs DE, Huddleston JI, Goldvasser D, Scarborough DM, Harris WH, Malchau H. Biomotion community-wearable human activity monitor: total knee replacement and healthy control subjects. International Workshop on Wearable and Implantable Body Sensor Networks (BSN'06); April 3-5; Cambridge, MA. 2006. [DOI] [Google Scholar]
- 85.Kuether J, Moore A, Kahan J, Martucci J, Messina T, Perreault R, Sembler R, Tarutis J, Zazulak B, Rubin LE, O'Connor MI. Telerehabilitation for total hip and knee arthroplasty patients: a pilot series with high patient satisfaction. HSS J. 2019 Oct 21;15(3):221–225. doi: 10.1007/s11420-019-09715-w. https://journals.sagepub.com/doi/abs/10.1007/s11420-019-09715-w?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .9715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lam AWK, Varona-Marin D, Li Y, Fergenbaum M, Kulić D. Automated rehabilitation system: movement measurement and feedback for patients and physiotherapists in the rehabilitation clinic. Human–Computer Interaction. 2016 Nov 18;31(3):294–334. doi: 10.1080/07370024.2015.1093419. [DOI] [Google Scholar]
- 87.Losina E, Collins JE, Daigle ME, Donnell-Fink LA, Prokopetz JJ, Strnad D, Lerner V, Rome BN, Ghazinouri R, Skoniecki DJ, Katz JN, Wright J. The AViKA (Adding Value in Knee Arthroplasty) postoperative care navigation trial: rationale and design features. BMC Musculoskelet Disord. 2013 Oct 12;14(1):290. doi: 10.1186/1471-2474-14-290. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-14-290 .1471-2474-14-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Milliren CE, Lindsay B, Biernat L, Smith TA, Weaver B. Can digital engagement improve outcomes for total joint replacements? Digit Health. 2022 Apr 24;8:20552076221095322. doi: 10.1177/20552076221095322. https://journals.sagepub.com/doi/abs/10.1177/20552076221095322?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_20552076221095322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Na A, Buchanan TS. Validating wearable sensors using self-reported instability among patients with knee osteoarthritis. PM R. 2021 Feb 12;13(2):119–127. doi: 10.1002/pmrj.12393. [DOI] [PubMed] [Google Scholar]
- 90.Bell KM, Onyeukwu C, Smith CN, Oh A, Devito Dabbs A, Piva SR, Popchak AJ, Lynch AD, Irrgang JJ, McClincy MP. A portable system for remote rehabilitation following a total knee replacement: a pilot randomized controlled clinical study. Sensors (Basel) 2020 Oct 27;20(21):6118. doi: 10.3390/s20216118. https://www.mdpi.com/resolver?pii=s20216118 .s20216118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pellegrini CA, Lee J, DeVivo KE, Harpine CE, Del Gaizo DJ, Wilcox S. Reducing sedentary time using an innovative mHealth intervention among patients with total knee replacement: Rationale and study protocol. Contemp Clin Trials Commun. 2021 Jun;22:100810. doi: 10.1016/j.conctc.2021.100810. https://linkinghub.elsevier.com/retrieve/pii/S2451-8654(21)00111-3 .S2451-8654(21)00111-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ramkumar PN, Haeberle HS, Ramanathan D, Cantrell WA, Navarro SM, Mont MA, Bloomfield M, Patterson BM. Remote patient monitoring using mobile health for total knee arthroplasty: validation of a wearable and machine learning-based surveillance platform. J Arthroplasty. 2019 Oct;34(10):2253–2259. doi: 10.1016/j.arth.2019.05.021.S0883-5403(19)30495-4 [DOI] [PubMed] [Google Scholar]
- 93.Summers SH, Nunley RM, Slotkin EM. A home-based, remote-clinician-controlled, physical therapy device leads to superior outcomes when compared to standard physical therapy for rehabilitation after total knee arthroplasty. J Arthroplasty. 2023 Mar;38(3):497–501. doi: 10.1016/j.arth.2022.10.009.S0883-5403(22)00929-9 [DOI] [PubMed] [Google Scholar]
- 94.Tousignant M, Boissy P, Moffet H, Corriveau H, Cabana F, Marquis F, Simard J. Patients' satisfaction of healthcare services and perception with in-home telerehabilitation and physiotherapists' satisfaction toward technology for post-knee arthroplasty: an embedded study in a randomized trial. Telemed J E Health. 2011 Jun;17(5):376–82. doi: 10.1089/tmj.2010.0198. [DOI] [PubMed] [Google Scholar]
- 95.Tripuraneni KR, Foran JR, Munson NR, Racca NE, Carothers JT. A smartwatch paired with a mobile application provides postoperative self-directed rehabilitation without compromising total knee arthroplasty outcomes: a randomized controlled trial. J Arthroplasty. 2021 Dec;36(12):3888–3893. doi: 10.1016/j.arth.2021.08.007.S0883-5403(21)00647-1 [DOI] [PubMed] [Google Scholar]
- 96.Visperas AT, Greene KA, Krebs VE, Klika AK, Piuzzi NS, Higuera-Rueda CA. A web-based interactive patient-provider software platform does not increase patient satisfaction or decrease hospital resource utilization in total knee and hip arthroplasty patients in a single large hospital system. J Arthroplasty. 2021 Jul;36(7):2290–2296.e1. doi: 10.1016/j.arth.2021.01.037.S0883-5403(21)00077-2 [DOI] [PubMed] [Google Scholar]
- 97.Youn I, Youn J, Zeni J, Knarr B. Biomechanical gait variable estimation using wearable sensors after unilateral total knee arthroplasty. Sensors (Basel) 2018 May 15;18(5):1577. doi: 10.3390/s18051577. https://www.mdpi.com/resolver?pii=s18051577 .s18051577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhao W, Yang S, Luo X. Towards rehabilitation at home after total knee replacement. Tsinghua Science and Technology. 2021;26(6):791–799. doi: 10.26599/TST.2020.9010034. [DOI] [Google Scholar]
- 99.Kramer JF, Speechley M, Bourne R, Rorabeck C, Vaz M. Comparison of clinic- and home-based rehabilitation programs after total knee arthroplasty. Clin Orthop Relat Res. 2003 May;(410):225–34. doi: 10.1097/01.blo.0000063600.67412.11. [DOI] [PubMed] [Google Scholar]
- 100.Bolam SM, Batinica B, Yeung TC, Weaver S, Cantamessa A, Vanderboor TC, Yeung S, Munro JT, Fernandez JW, Besier TF, Monk AP. Remote patient monitoring with wearable sensors following knee arthroplasty. Sensors (Basel) 2021 Jul 29;21(15):5143. doi: 10.3390/s21155143. https://www.mdpi.com/resolver?pii=s21155143 .s21155143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Castle H, Kozak K, Sidhu A, Khan RJK, Haebich S, Bowden V, Fick DP, Goonatillake H. Smartphone technology: a reliable and valid measure of knee movement in knee replacement. Int J Rehabil Res. 2018 Jun;41(2):152–158. doi: 10.1097/MRR.0000000000000276. [DOI] [PubMed] [Google Scholar]
- 102.Levinger P, Zeina D, Teshome AK, Skinner E, Begg R, Abbott JH. A real time biofeedback using Kinect and Wii to improve gait for post-total knee replacement rehabilitation: a case study report. Disabil Rehabil Assist Technol. 2016 Sep 04;11(3):251–62. doi: 10.3109/17483107.2015.1080767. [DOI] [PubMed] [Google Scholar]
- 103.Liptak MG, Theodoulou A, Kaambwa B, Saunders S, Hinrichs SW, Woodman RJ, Krishnan J. The safety, efficacy and cost-effectiveness of the Maxm Skate, a lower limb rehabilitation device for use following total knee arthroplasty: study protocol for a randomised controlled trial. Trials. 2019 Jan 10;20(1):36. doi: 10.1186/s13063-018-3102-9. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-018-3102-9 .10.1186/s13063-018-3102-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Negus J, Cawthorne D, Chen J, Scholes C, Parker D, March L. Patient outcomes using Wii-enhanced rehabilitation after total knee replacement - the TKR-POWER study. Contemp Clin Trials. 2015 Jan;40:47–53. doi: 10.1016/j.cct.2014.11.007.S1551-7144(14)00162-1 [DOI] [PubMed] [Google Scholar]
- 105.Russell TG, Buttrum P, Wootton R, Jull GA. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty. The Journal of Bone and Joint Surgery-American Volume. 2011;93(2):113–120. doi: 10.2106/jbjs.i.01375. [DOI] [PubMed] [Google Scholar]
- 106.Duong V, Dennis S, Harris A, Robbins S, Venkatesha V, Ferreira M, Hunter D. The effects of a disruptive digital technology intervention following total knee replacement: results from the pathway randomised controlled trial. Osteoarthritis and Cartilage. 2023 Mar;31:S30–S31. doi: 10.1016/j.joca.2023.01.521. [DOI] [Google Scholar]
- 107.Hardwick-Morris M, Carlton S, Twiggs J, Miles B, Liu D. Pre- and postoperative physiotherapy using a digital application decreases length of stay without reducing patient outcomes following total knee arthroplasty. Arthroplasty. 2022 Aug 02;4(1):30. doi: 10.1186/s42836-022-00133-8. https://europepmc.org/abstract/MED/35915464 .10.1186/s42836-022-00133-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Farr-Wharton G, Li J, Hussain MS, Freyne J. Mobile Supported Health Services: Experiences in Orthopaedic Care. IEEE 33rd International Symposium on Computer-Based Medical Systems (CBMS); July 28-30, 2020; Rochester, MN. [DOI] [Google Scholar]
- 109.McDonall J, de Steiger R, Reynolds J, Redley B, Livingston PM, Hutchinson AF, Botti M. Patient activation intervention to facilitate participation in recovery after total knee replacement (MIME): a cluster randomised cross-over trial. BMJ Qual Saf. 2019 Oct 11;28(10):782–792. doi: 10.1136/bmjqs-2018-008975. https://europepmc.org/abstract/MED/30975730 .bmjqs-2018-008975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.An J, Ryu H, Lyu S, Yi H, Lee B. Effects of preoperative telerehabilitation on muscle strength, range of motion, and functional outcomes in candidates for total knee arthroplasty: a single-blind randomized controlled trial. Int J Environ Res Public Health. 2021 Jun 04;18(11):6071. doi: 10.3390/ijerph18116071. https://www.mdpi.com/resolver?pii=ijerph18116071 .ijerph18116071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chiang C, Chen K, Liu K, Hsu S, Chan C. Data collection and analysis using wearable sensors for monitoring knee range of motion after total knee arthroplasty. Sensors (Basel) 2017 Feb 22;17(2):418. doi: 10.3390/s17020418. https://www.mdpi.com/resolver?pii=s17020418 .s17020418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Huang Y, Liu Y, Hsu W, Lai L, Lee MS. Progress on range of motion after total knee replacement by sensor-based system. Sensors (Basel) 2020 Mar 18;20(6):1703. doi: 10.3390/s20061703. https://www.mdpi.com/resolver?pii=s20061703 .s20061703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Huang P, He J, Zhang YM. [The mobile application of patient management in education and follow-up for patients following total knee arthroplasty] Zhonghua Yi Xue Za Zhi. 2017 May 30;97(20):1592–1595. doi: 10.3760/cma.j.issn.0376-2491.2017.20.019. [DOI] [PubMed] [Google Scholar]
- 114.Hung LP, Chao YH, Tseng YL, Chung YL. Constructing a home-based knee replacement exercise monitoring system with G sensor. International Conference on Frontier Computing; July 3-6, 2018; Kuala Lumpur, Malaysia. [DOI] [Google Scholar]
- 115.Li Y, Gu Z, Ning R, Yin H. Study on the effect of internet plus continuous nursing on functional recovery and medication compliance of patients with knee joint replacement. J Orthop Surg Res. 2023 Jun 11;18(1):424. doi: 10.1186/s13018-023-03907-1. https://josr-online.biomedcentral.com/articles/10.1186/s13018-023-03907-1 .10.1186/s13018-023-03907-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lou N, Diao Y, Chen Q, Ning Y, Li G, Liang S, Li G, Zhao G. A portable wearable inertial system for rehabilitation monitoring and evaluation of patients with total knee replacement. Front Neurorobot. 2022 Mar 23;16:836184. doi: 10.3389/fnbot.2022.836184. https://europepmc.org/abstract/MED/35401138 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lu G, Wu T, Tan Q, Wu Z, Shi L, Zhong Y. The effect of a micro-visual intervention on the accelerated recovery of patients with kinesiophobia after total knee replacement during neo-coronary pneumonia. Medicine (Baltimore) 2021 Feb 12;100(6):e24141. doi: 10.1097/MD.0000000000024141. https://europepmc.org/abstract/MED/33578519 .00005792-202102120-00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Park KH, Song MR. The effects of postdischarge telephone counseling and short message service on the knee function, activities of daily living, and life satisfaction of patients undergoing total knee replacement. Orthop Nurs. 2017;36(3):229–236. doi: 10.1097/NOR.0000000000000332. https://europepmc.org/abstract/MED/28363197 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Park SA, Jeong Y. The effect of a multidimensional home rehabilitation program for post-total knee arthroplasty elderly patients. Orthop Nurs. 2023;42(1):22–32. doi: 10.1097/NOR.0000000000000913.00006416-202301000-00007 [DOI] [PubMed] [Google Scholar]
- 120.Su C, Cheng C. Developing and evaluating creativity gamification rehabilitation system: the application of PCA-ANFIS based emotions model. Eurasia J Math Sci T. 2016;12(5):1. doi: 10.12973/eurasia.2016.1527a. [DOI] [Google Scholar]
- 121.Wang Q, Hunter S, Lee RL, Chan SW. The effectiveness of a mobile application-based programme for rehabilitation after total hip or knee arthroplasty: A randomised controlled trial. Int J Nurs Stud. 2023 Apr;140:104455. doi: 10.1016/j.ijnurstu.2023.104455. https://linkinghub.elsevier.com/retrieve/pii/S0020-7489(23)00020-2 .S0020-7489(23)00020-2 [DOI] [PubMed] [Google Scholar]
- 122.Yang C, Shang L, Yao S, Ma J, Xu C. Cost, time savings and effectiveness of wearable devices for remote monitoring of patient rehabilitation after total knee arthroplasty: study protocol for a randomized controlled trial. J Orthop Surg Res. 2023 Jun 27;18(1):461. doi: 10.1186/s13018-023-03898-z. https://josr-online.biomedcentral.com/articles/10.1186/s13018-023-03898-z .10.1186/s13018-023-03898-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang X, Chen X, Kourkoumelis N, Gao R, Li G, Zhu C. A social media-promoted educational community of joint replacement patients using the WeChat app: survey study. JMIR Mhealth Uhealth. 2021 Mar 18;9(3):e18763. doi: 10.2196/18763. https://mhealth.jmir.org/2021/3/e18763/ v9i3e18763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zheng Q, Chen H. A monitoring system for walking rehabilitation after THR or TKR surgeries. Annu Int Conf IEEE Eng Med Biol Soc. Jul;2017:2373–2376. doi: 10.1109/EMBC.2017.8037333. [DOI] [PubMed] [Google Scholar]
- 125.Zhang H, Zhou Y. Concept verification of a remote automatic scoring system for evaluating knee function after total knee arthroplasty. J Knee Surg. 2021 Mar 27;34(4):464–470. doi: 10.1055/s-0040-1710568. [DOI] [PubMed] [Google Scholar]
- 126.Jansson M, Vuorinen A, Harjumaa M, Similä H, Koivisto J, Puhto A, Vesty G, Pikkarainen M. The digital patient journey solution for patients undergoing elective hip and knee arthroplasty: Protocol for a pragmatic randomized controlled trial. J Adv Nurs. 2020 Jun 15;76(6):1436–1448. doi: 10.1111/jan.14343. [DOI] [PubMed] [Google Scholar]
- 127.Hadamus A, Białoszewski D, Urbaniak E, Kowalska A, Wydra K, Boratyński R, Kobza A, Marczyński W. The impact of training in virtual reality on balance in patients after total knee replacement is relatively slight. Gait & Posture. 2020 Sep;81:134–135. doi: 10.1016/j.gaitpost.2020.07.101. [DOI] [Google Scholar]
- 128.Wang Q, Hunter S, Lee RL, Wang X, Chan SW. Patients' needs regarding rehabilitation services delivered via mobile applications after arthroplasty: A qualitative study. J Clin Nurs. 2022 Nov 02;31(21-22):3178–3189. doi: 10.1111/jocn.16152. [DOI] [PubMed] [Google Scholar]
- 129.Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. Philadelphia, PA: J. B. Lippincott Company; 1996. [Google Scholar]
- 130.Net Promoter System. [2023-12-12]. https://www.netpromotersystem.com/about/measuring-your-net-promoter-score/
- 131.Demiris G, Speedie S, Finkelstein S. A questionnaire for the assessment of patients' impressions of the risks and benefits of home telecare. J Telemed Telecare. 2000 Jun 24;6(5):278–84. doi: 10.1258/1357633001935914. [DOI] [PubMed] [Google Scholar]
- 132.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989 Sep;13(3):319–340. doi: 10.2307/249008. https://www.jstor.org/stable/249008 . [DOI] [Google Scholar]
- 133.Parmanto B, Lewis AN, Graham KM, Bertolet MH. Development of the Telehealth Usability Questionnaire (TUQ) Int J Telerehabil. 2016 Jul 01;8(1):3–10. doi: 10.5195/ijt.2016.6196. https://europepmc.org/abstract/MED/27563386 .ijt-pg03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Cooper DM, Bhuskute N, Walsh G. Exploring the impact and acceptance of wearable sensor technology for pre- and postoperative rehabilitation in knee replacement patients: a U.K.-based pilot study. JB JS Open Access. 2022;7(2):1. doi: 10.2106/JBJS.OA.21.00154. https://europepmc.org/abstract/MED/35506018 .JBJSOA-D-21-00154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Booth MW, Riegler V, King JS, Barrack RL, Hannon CP. Patients' perceptions of remote monitoring and app-based rehabilitation programs: a comparison of total hip and knee arthroplasty. J Arthroplasty. 2023 Jul;38(7S):S39–S43. doi: 10.1016/j.arth.2023.04.032.S0883-5403(23)00388-1 [DOI] [PubMed] [Google Scholar]
- 136.van Kasteren Y, Freyne J, Hussain MS. Total knee replacement and the effect of technology on cocreation for improved outcomes and delivery: qualitative multi-stakeholder study. J Med Internet Res. 2018 Mar 20;20(3):e95. doi: 10.2196/jmir.7541. https://www.jmir.org/2018/3/e95/ v20i3e95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Jansson MM, Harjumaa M, Puhto A, Pikkarainen M. Healthcare professionals' proposed eHealth needs in elective primary fast-track hip and knee arthroplasty journey: A qualitative interview study. J Clin Nurs. 2019 Dec 18;28(23-24):4434–4446. doi: 10.1111/jocn.15028. [DOI] [PubMed] [Google Scholar]
- 138.de Batlle J, Massip M, Vargiu E, Nadal N, Fuentes A, Ortega Bravo M, Colomina J, Drudis R, Torra M, Pallisó F, Miralles F, Barbé F, Torres G, CONNECARE-Lleida Group Implementing mobile health-enabled integrated care for complex chronic patients: patients and professionals' acceptability study. JMIR Mhealth Uhealth. 2020 Nov 20;8(11):e22136. doi: 10.2196/22136. https://mhealth.jmir.org/2020/11/e22136/ v8i11e22136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Boissy P, Tousignant M, Moffet H, Nadeau S, Brière S, Mérette C, Corriveau H, Marquis F, Cabana F, Ranger P, Belzile. Dimentberg R. Conditions of use, reliability, and quality of audio/video-mediated communications during in-home rehabilitation teletreatment for postknee arthroplasty. Telemed J E Health. 2016 Aug;22(8):637–49. doi: 10.1089/tmj.2015.0157. [DOI] [PubMed] [Google Scholar]
- 140.Parkes RJ, Palmer J, Wingham J, Williams DH. Is virtual clinic follow-up of hip and knee joint replacement acceptable to patients and clinicians? A sequential mixed methods evaluation. BMJ Open Qual. 2019 Mar 01;8(1):e000502. doi: 10.1136/bmjoq-2018-000502. https://bmjopenquality.bmj.com/lookup/pmidlookup?view=long&pmid=31259271 .bmjoq-2018-000502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Russell TG, Buttrum P, Wootton R, Jull GA. Low-bandwidth telerehabilitation for patients who have undergone total knee replacement: preliminary results. J Telemed Telecare. 2003 Dec 02;9 Suppl 2:S44–7. doi: 10.1258/135763303322596246. [DOI] [PubMed] [Google Scholar]
- 142.Lee M, Suh D, Son J, Kim J, Eun S, Yoon B. Patient perspectives on virtual reality-based rehabilitation after knee surgery: Importance of level of difficulty. J Rehabil Res Dev. 2016;53(2):239–252. doi: 10.1682/jrrd.2014.07.0164. [DOI] [PubMed] [Google Scholar]
- 143.Reid H, Mohammadi S, Watson W, Robillard JM, Crocker M, Westby MD, Miller WC. Patient and caregiver perspectives on an eHealth tool: a qualitative investigation of preferred formats, features and characteristics of a presurgical eHealth education module. Rehabil Process Outcome. 2021 Apr 21;10:11795727211010501. doi: 10.1177/11795727211010501. https://journals.sagepub.com/doi/abs/10.1177/11795727211010501?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_11795727211010501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Culliton SE, Bryant DM, MacDonald SJ, Hibbert KM, Chesworth BM. Effect of an e-Learning tool on expectations and satisfaction following total knee arthroplasty: a randomized controlled trial. J Arthroplasty. 2018 Jul;33(7):2153–2158. doi: 10.1016/j.arth.2018.02.040.S0883-5403(18)30171-2 [DOI] [PubMed] [Google Scholar]
- 145.LeBrun DG, Malfer C, Wilson M, Carroll KM, Wang Ms V, Mayman DJ, Cross MB, Alexiades MM, Jerabek SA, Cushner FD, Vigdorchik JM, Haas SB, Ast MP. Telemedicine in an outpatient arthroplasty setting during the COVID-19 pandemic: early lessons from New York City. HSS J. 2021 Feb 21;17(1):25–30. doi: 10.1177/1556331620972659. https://journals.sagepub.com/doi/abs/10.1177/1556331620972659?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_1556331620972659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Argent R, Slevin P, Bevilacqua A, Neligan M, Daly A, Caulfield B. Clinician perceptions of a prototype wearable exercise biofeedback system for orthopaedic rehabilitation: a qualitative exploration. BMJ Open. 2018 Oct 25;8(10):e026326. doi: 10.1136/bmjopen-2018-026326.bmjopen-2018-026326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.McDonall J, Redley B, Livingston P, Hutchinson A, de Steiger R, Botti M. A nurse-led multimedia intervention to increase patient participation in recovery after knee arthroplasty: hybrid type II implementation study. JMIR Hum Factors. 2022 May 19;9(2):e36959. doi: 10.2196/36959. https://humanfactors.jmir.org/2022/2/e36959/ v9i2e36959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Giunta NM, Paladugu PS, Bernstein DN, Makhni MC, Chen AF. Telemedicine hip and knee arthroplasty experience during COVID-19. J Arthroplasty. 2022 Aug;37(8S):S814–S818.e2. doi: 10.1016/j.arth.2022.02.106. https://europepmc.org/abstract/MED/35257819 .S0883-5403(22)00257-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Joshi R, Joseph A, Mihandoust S, Madathil KC, Cotten SR. A mobile application-based home assessment tool for patients undergoing joint replacement surgery: a qualitative feasibility study. Appl Ergon. 2022 Sep;103:103796. doi: 10.1016/j.apergo.2022.103796.S0003-6870(22)00119-3 [DOI] [PubMed] [Google Scholar]
- 150.Glinkowski W, Cabaj D, Kostrubała A, Krawczak K, Górecki A. Pre-surgery and post-surgery telerehabilitation for hip and knee replacement - Treatment options review and patient's attitudes towards telerehabilitation. eChallenges e-2010 Conference; October 27-29, 2010; Warsaw, Poland. 2011. [Google Scholar]
- 151.Moffet H, Tousignant M, Nadeau S, Mérette C, Boissy P, Corriveau H, Marquis F, Cabana F, Belzile. Ranger P, Dimentberg R. Patient satisfaction with in-home telerehabilitation after total knee arthroplasty: results from a randomized controlled trial. Telemed J E Health. 2017 Feb;23(2):80–87. doi: 10.1089/tmj.2016.0060. [DOI] [PubMed] [Google Scholar]
- 152.Williams E, Putnam J, Emkes L, Greenwood J. Patient perspectives and numerical evaluation of a COVID secure hybrid rehabilitation programme following knee replacement surgery. Physiotherapy. 2022 Feb;114:e224–e225. doi: 10.1016/j.physio.2021.12.214. [DOI] [Google Scholar]
- 153.Marsh J, Bryant D, MacDonald SJ, Naudie D, Remtulla A, McCalden R, Howard J, Bourne R, McAuley J. Are patients satisfied with a web-based followup after total joint arthroplasty? Clin Orthop Relat Res. 2014 Jun;472(6):1972–81. doi: 10.1007/s11999-014-3514-0. https://europepmc.org/abstract/MED/24562873 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Grant S, Blom AW, Whitehouse MR, Craddock I, Judge A, Tonkin EL, Gooberman-Hill R. Using home sensing technology to assess outcome and recovery after hip and knee replacement in the UK: the HEmiSPHERE study protocol. BMJ Open. 2018 Jul 28;8(7):e021862. doi: 10.1136/bmjopen-2018-021862. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=30056388 .bmjopen-2018-021862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Kairy D, Tousignant M, Leclerc N, Côté AM, Levasseur M, Researchers T. The patient's perspective of in-home telerehabilitation physiotherapy services following total knee arthroplasty. Int J Environ Res Public Health. 2013 Aug 30;10(9):3998–4011. doi: 10.3390/ijerph10093998. https://www.mdpi.com/resolver?pii=ijerph10093998 .ijerph10093998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hip and knee replacement. OECD iLibrary. [2023-12-12]. http://tinyurl.com/yv339863 .
- 157.Silver L. Smartphone Ownership Is Growing Rapidly Around the World, But Not Always Equally. Pew Research Center. 2019. Feb 05, [2023-12-12]. http://tinyurl.com/39dkhvvd .
- 158.McCool J, Dobson R, Whittaker R, Paton C. Mobile health (mHealth) in low- and middle-income countries. Annu Rev Public Health. 2022 Apr 05;43(1):525–539. doi: 10.1146/annurev-publhealth-052620-093850. https://www.annualreviews.org/doi/abs/10.1146/annurev-publhealth-052620-093850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PubMed] [Google Scholar]
- 159.Malik IV, Devasenapathy N, Kumar A, Dogra H, Ray S, Gautam D, Malhotra R. Estimation of expenditure and challenges related to rehabilitation after knee arthroplasty: a hospital-based cross-sectional study. Indian J Orthop. 2021 Oct 02;55(5):1317–1325. doi: 10.1007/s43465-021-00405-6. https://europepmc.org/abstract/MED/34824731 .405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zhou Z, Hou Y, Lin J, Wang K, Liu Q. Patients' views toward knee osteoarthritis exercise therapy and factors influencing adherence - a survey in China. Phys Sportsmed. 2018 May 16;46(2):221–227. doi: 10.1080/00913847.2018.1425595. [DOI] [PubMed] [Google Scholar]
- 161.Taylor CE, Murray CM, Stanton TR. Patient perspectives of pain and function after knee replacement: a systematic review and meta-synthesis of qualitative studies. PR9. 2022 May 09;7(3):e1006. doi: 10.1097/pr9.0000000000001006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Reddy H, Joshi S, Joshi A, Wagh V. A critical review of global digital divide and the role of technology in healthcare. Cureus. 2022 Sep;14(9):e29739. doi: 10.7759/cureus.29739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Perski O, Blandford A, West R, Michie S. Conceptualising engagement with digital behaviour change interventions: a systematic review using principles from critical interpretive synthesis. Transl Behav Med. 2017 Jun 13;7(2):254–267. doi: 10.1007/s13142-016-0453-1. https://europepmc.org/abstract/MED/27966189 .10.1007/s13142-016-0453-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Voorheis P, Zhao A, Kuluski K, Pham Q, Scott T, Sztur P, Khanna N, Ibrahim M, Petch J. Integrating behavioral science and design thinking to develop mobile health interventions: systematic scoping review. JMIR Mhealth Uhealth. 2022 Mar 16;10(3):e35799. doi: 10.2196/35799. https://mhealth.jmir.org/2022/3/e35799/ v10i3e35799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hussain MS, Li J, Brindal E, van Kasteren Y, Varnfield M, Reeson A, Berkovsky S, Freyne J. Supporting the delivery of total knee replacements care for both patients and their clinicians with a mobile app and web-based tool: randomized controlled trial protocol. JMIR Res Protoc. 2017 Mar 01;6(3):e32. doi: 10.2196/resprot.6498. https://www.researchprotocols.org/2017/3/e32/ v6i3e32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bade MJ, Christensen JC, Zeni JA, Christiansen CL, Dayton MR, Forster JE, Cheuy VA, Stevens-Lapsley JE. Movement pattern biofeedback training after total knee arthroplasty: Randomized clinical trial protocol. Contemp Clin Trials. 2020 Apr;91:105973. doi: 10.1016/j.cct.2020.105973. https://europepmc.org/abstract/MED/32171937 .S1551-7144(20)30051-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wang X, Hunter DJ, Robbins S, Capistrano S, Duong V, Melo L, Harris A, Ferreira M. Participatory health through behavioural engagement and disruptive digital technology for postoperative rehabilitation: protocol of the PATHway trial. BMJ Open. 2021 Jan 17;11(1):e041328. doi: 10.1136/bmjopen-2020-041328. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=33455931 .bmjopen-2020-041328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.McDonall J, de Steiger R, Reynolds J, Redley B, Livingston P, Botti M. Patient participation in postoperative care activities in patients undergoing total knee replacement surgery: Multimedia Intervention for Managing patient Experience (MIME). Study protocol for a cluster randomised crossover trial. BMC Musculoskelet Disord. 2016 Jul 18;17(1):294. doi: 10.1186/s12891-016-1133-5. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-016-1133-5 .10.1186/s12891-016-1133-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Argent R, Slevin P, Bevilacqua A, Neligan M, Daly A, Caulfield B. Wearable sensor-based exercise biofeedback for orthopaedic rehabilitation: a mixed methods user evaluation of a prototype system. Sensors (Basel) 2019 Jan 21;19(2):432. doi: 10.3390/s19020432. https://www.mdpi.com/resolver?pii=s19020432 .s19020432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Szöts K, Konradsen H, Solgaard S, Østergaard B. Telephone follow-up by nurse after total knee arthroplasty: results of a randomized clinical trial. Orthop Nurs. 2016;35(6):411–420. doi: 10.1097/NOR.0000000000000298.00006416-201611000-00010 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information on search strategy, included and excluded studies.
Raw data extraction file for rehabilitation program studies.
PRISMA-ScR checklist.


