Abstract
Background:
Delayed cerebrospinal fluid (CSF) leaks are a known complication following intradural spinal tumor surgery. The placement of subfascial drains in these patients undergoing requisite intradural surgery is controversial. Here, we demonstrated that placing a subfascial drain on partial suction for 48 h, with early ambulation, proved to be safe and effective in preventing early/delayed recurrent CSF fistulas.
Methods:
Medical records of 17 patients undergoing surgery for intradural spinal tumors over a 30-month were reviewed. All patients underwent intradural tumor resection followed by primary dural closure, placement of Gelfoam in a non-compressive fashion, application of fibrin sealant, and utilization of a subfascial drain placed on partial suction for 48 h postoperatively. Patients are mobilized the morning following surgery. We tracked the incidence of postoperative recurrent CSF leaks, over drainage, infection, wound dehiscence, pseudo meningocele formation, and the reoperation rate.
Results:
For the 17 patients, our programmed average utilization of subfascial drains was 48 h. Moreover, the average drain output was 165 mL. Over the 1-year follow-up period, no patient developed a recurrent early/ delayed CSF leak, there were no wound complications, nor need for revision surgery.
Conclusion:
Utilizing subfascial drains on partial suction following the resection of intradural spinal tumors with primary dural closure proved to be safe and effective.
Keywords: Intentional durotomy, Intradural spinal tumors, Postoperative cerebrospinal fluid leak, Subfascial drains

INTRODUCTION
Delayed cerebrospinal fluid (CSF) leak following the resection of intradural spinal tumors may lead to early/delayed recurrent fistulas, over drainage, infection, wound dehiscence, pseudo meningocele, intracranial hemorrhage, and reoperations. Recurrent CSF leaks contribute to the intraoperative times, postoperative length of hospital stay, and perioperative costs.[1-8] Here, we utilized primary dural closure followed by placement of Gelfoam, fibrin sealant, and subfascial drains on partial suction for approximately 48 postoperative hours. Notably, we sought to determine whether, with the early patient mobilization on the 1st postoperative day, this technique would prove to be safe and effective in preventing postoperative CSF leaks.
MATERIALS AND METHODS
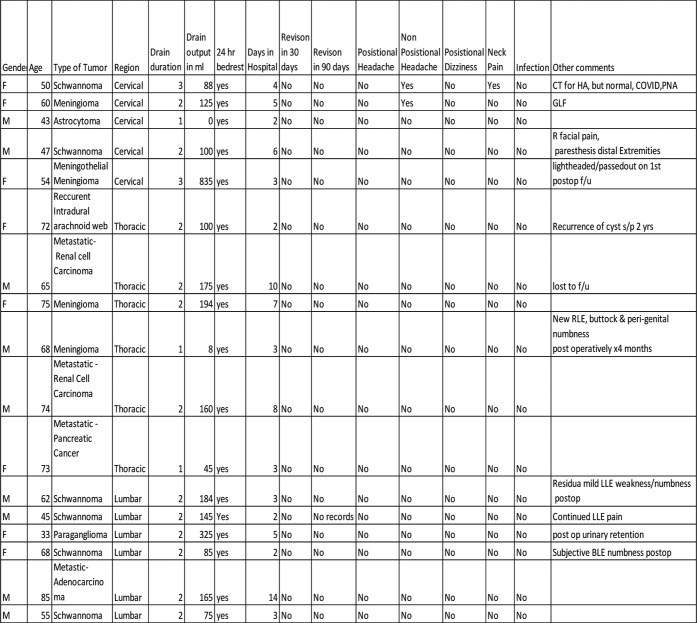
Seventeen patients who met multiple inclusion criteria underwent the resection of intradural tumors; they were followed over an average 30-month postoperative period [Figure 1]. The nine males and eight females averaged 61 years of age [Figure 2]. Following primary dural closures and the application of Gelfoam, a fibrin sealant, all patients had subfascial drains placed on partial suction for 48 postoperative hours. For patients who were all mobilized on postoperative day 1, the following parameters were monitored: daily drain output, duration of bed rest, length of hospital stay, early/ delayed postoperative recurrent CSF leaks, infection, wound dehiscence, pseudomeningocele, and reoperations.
Figure 1:
Summary of collected data. HA: Headache, PNA: Pneumonia, GLF: Ground level fall, RLE: Right lower extremity, F/U: Follow up, s/p: Status post, LLE: Left lower extremity
Figure 2:
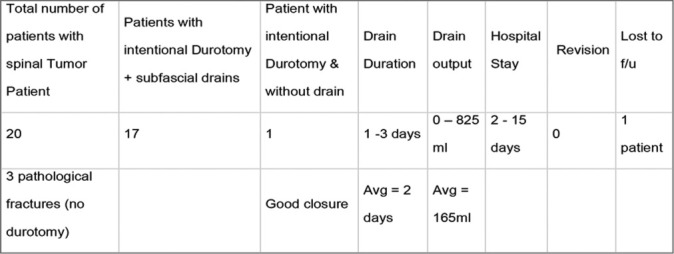
Results summary.
Surgical technique and protocol
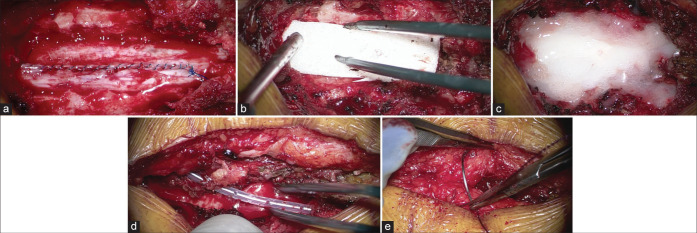
After tumor resection, primary dural closure was performed under the operating microscope using a running simple 5-0 Prolene suture. Next, Gelfoam and fibrin sealant were applied over the dura in a non-compressive fashion, followed by the application of an intraoperative subfascial drain placed on “partial suction” for 48 postoperative hours; routine closure followed using Polydioxanone Stratafix 2-0, and VICRYL 3-0. Patients were mobilized the morning after surgery [Figures 3a-e].
Figure 3:
(a) Primary dural closure with 5-0 Prolene suture. (b) Placement of Gelfoam over dural closure. (c) Fibrin Sealant was applied over Gelfoam to reinforce dural closure. (d) Subfascial drain placement. (e) Fascia closure with Polydioxanone Stratafix.
It should be noted that placement of Gelfoam, particularly under a lamina, is not advisable and can be contra-indicated. In our technique, Gelfoam is placed in a non-compressive fashion and not under the lamina. We believe that this is more cost-effective and may have better absorptive/sealant properties than standard dural substitutes.
RESULTS
Subfascial drains were put in place for between 1 and 3 days, 82% of them for only two days; drain output averaged 165 mL. The average length of stay was five days (range: 2 days–15 days). The majority of patients stay for rehab placement, not CSF leak-related complications. One patient was lost to follow-up, and the average length of follow-up was 11.7 months (range 8–12 months). Sixteen patients had ≥12 months of follow-up [Figure 2].
Adverse events/complications
Postoperatively, one patient had nonpositional headaches, one had nonpositional head and neck pain, and one had neck pain. Note the patient with a headache and neck pain was later diagnosed with COVID pneumonia. No surgical revisions were required for delayed CSF leaks occurring between 30 and 90 days following surgery.
DISCUSSION
Primary dural closure
Few studies investigate the outcomes following resection of intradural spinal tumors, particularly regarding CSF early/ delayed recurrent leaks and other adverse events. Primary dural closure, various dural closing techniques with/without synthetic patches, grafts, and layered watertight closure with supplemental sealants help reduce the risk of postoperative CSF leaks.
Subfascial drain placement
We believe that placement of subfascial dural closure, even after primary dural closure, helps divert CSF, blood, and serum from the subfascial space. Diverting the right amount of fluid away from the surgical bed by an Subfascial Drain drain on partial rather than full suction facilitates fascial healing;[1,3-4] We utilized SD for an average of 2 postoperative days, and drain duration averaged only two days. This brief period of drainage allowed for early mobilization and a shorter hospital stay; our average hospital length of stay was five days.[2] Despite the use of SD, we found no postoperative infections, and just one patient reported a nonpositional headache immediately postoperatively and was later found to have COVID pneumonia. Notably, no patients developed postoperative CSF leaks, and no revision procedures were warranted within the 30–90 postoperative window.
CONCLUSION
The use of subfascial drains after intradural spinal tumor surgery proved to be safe and effective.
Footnotes
How to cite this article: Mayeku J, Quiceno E, Cannata C, Barbagli G, Hussein A, Dholaria N, et al. Subfascial drains are safe and effective in preventing postoperative cerebrospinal fluid leaks after intradural spine tumor surgery. Surg Neurol Int. 2024;15:8. doi: 10.25259/SNI_934_2023
Contributor Information
Julie Mayeku, Email: julie.mayeku@bannerhealth.com.
Esteban Quiceno, Email: equicenor@gmail.com.
Christina Cannata, Email: christina.cannata@bannerhealth.com.
Giovanni Barbagli, Email: giovanni.barbagli@bannerhealth.com.
Amna Hussein, Email: amnasaid.hussein@bannerhealth.com.
Nikhil Dholaria, Email: nikhildholaria10@arizona.ed.
Michael Prim, Email: michael.prim@bannerhealth.com.
Ali A. Baaj, Email: ali.baaj@bannerhealth.com.
Ethical approval
Institutional Review Board approval is taken, Number: UA IRBI: STUDY0001817.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Fang Z, Jia YT, Tian R, Liu Y. Subfascial drainage for management of cerebrospinal fluid leakage after posterior spine surgery-a prospective study based on Poiseuille’s law. Chin J Traumatol. 2016;19:35–8. doi: 10.1016/j.cjtee.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lenschow M, Perrech M, Telentschak S, von Spreckelsen N, Pieczewski J, Goldbrunner R, et al. Cerebrospinal fluid leaks following intradural spinal surgery-risk factors and clinical management. Front Surg. 2022;9:959533. doi: 10.3389/fsurg.2022.959533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niu T, Lu DS, Yew A, Lau D, Hoffman H, McArthur D, et al. Postoperative cerebrospinal fluid leak rates with subfascial epidural drain placement after intentional durotomy in spine surgery. Glob Spine J. 2016;6:780–5. doi: 10.1055/s-0036-1582392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ropper AE, Huang KT, Ho AL, Wong JM, Nalbach SV, Chi JH. Intraoperative cerebrospinal fluid leak in extradural spinal tumor surgery. Neurospine. 2018;15:338–47. doi: 10.14245/ns.1836042.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shapiro SA, Scully T. Closed continuous drainage of cerebrospinal fluid via a lumbar subarachnoid catheter for treatment or prevention of cranial/spinal cerebrospinal fluid fistula. Neurosurgery. 1992;30:241–5. doi: 10.1227/00006123-199202000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Tan LA, Takagi I, Straus D, O’Toole JE. Management of intended durotomy in minimally invasive intradural spine surgery: Clinical article. J Neurosurg Spine. 2014;21:279–85. doi: 10.3171/2014.3.SPINE13719. [DOI] [PubMed] [Google Scholar]
- 7.Walid MS, Abbara M, Tolaymat A, Davis JR, Waits KD, Robinson JS, 3rd, et al. The role of drains in lumbar spine fusion. World Neurosurg. 2012;77:564–8. doi: 10.1016/j.wneu.2011.05.058. [DOI] [PubMed] [Google Scholar]
- 8.Woodroffe RW, Nourski KV, Helland LC, Walsh B, Noeller J, Kerezoudis P, et al. Management of iatrogenic spinal cerebrospinal fluid leaks: A cohort of 124 patients. Clin Neurol Neurosurg. 2018;170:61–6. doi: 10.1016/j.clineuro.2018.04.017. [DOI] [PubMed] [Google Scholar]