Abstract
Background
A multidisciplinary team of health scientists and educators at an academic medical center came together to consider the various factors that impact well-being among self-identified women working in healthcare and conducted a comprehensive literature review to identify the existing body of knowledge.
Objectives
To examine how well-being is defined, what instruments are used to measure it, and correlation between professional and personal gender-specific factors that impact the well-being of women in healthcare occupations.
Methods
A total of 71 studies published in 26 countries between 1979-2022 were extracted from PubMed. Studies enrolled adult women (18-74 y.o.) healthcare professionals including nurses, physicians, clinical social workers, and mental health providers. Well-being related phenomena such as quality of life (QOL), stress, burnout, resiliency, and wellness were investigated. In this review, women are broadly defined to include any individual who primarily identifies as a woman regardless of their sex assigned at birth.
Results
The results of our analysis were consistent across the scope of the literature and indicated that women in healthcare occupations endure a significantly higher level of stress and burnout compared to their male counterparts. The following gender-specific factors were identified as having direct correlation to well-being: job satisfaction, psychological health, and work-life integration.
Conclusions
The findings from this review indicate a need for evidence-based integrative interventions across healthcare enterprises to combat stress and burnout and strengthen the resiliency and well-being of women in healthcare. Using information from this review, our team will launch a comprehensive well-being assessment and a series of interventions to support resiliency and well-being at our academic medical center.
Keywords: clinicians, healthcare providers, women’s health, quality of life, stress, burnout, resiliency, well-being, job satisfaction, psychological health, work-life integration
Introduction
Women have driven 80% of the overall growth in the booming healthcare field since the turn of the century. 1 The number of full-time, year-round workers in healthcare occupations almost doubled since 2000, increasing from 5 million to 9 million according to the US Census Bureau, where women currently account for 3 quarters of this number. 1 The global increase of women working in healthcare has raised concerns regarding their well-being. 1 Due to the varying roles that women play in society, they are more prone to experiencing mental health issues brought on by immense pressure and stress to succeed both at home and at work simultaneously. This issue can affect their physical and mental health to the point of causing psychological distress, occupational burnout, depression, anxiety, rapid turnover, or suicidal thoughts. 2 For example, a 2018 study revealed that 60% of female physicians experienced burnout compared to 40% of male physicians. 3 Similar circumstances appear in the literature as early as graduate studies.4-6 The magnitude of this issue leads to decreased work performance, lower quality care, and a loss of patient trust and adherence to treatment protocols.3,7,8 Further, this issue negatively affects employee productivity, healthcare system costs, and turnover rates—each associated with a sizeable cost burden. 3 As the number of women entering the healthcare profession continues to rise, concerns about the health of women are becoming more prevalent, and it is critical that they receive adequate support.
The George Washington University (GW) School of Medicine and Health Sciences (SMHS) Resiliency & Well-being Center (R&WC) was recently founded to support whole person health, which is grounded in purpose–one’s reason for being or existing. The R&WC serves the GW medical enterprise and strives to strengthen resilience (elastic adaptation) and well-being (health and wellness) of SMHS faculty, staff, and medical trainees. To effectively serve our community, we must prepare for program assessment by measuring the well-being of our community members at baseline. The R&WC utilizes a version of the Center for Disease Control and Prevention (CDC) definition of well-being: an integration of mental health (mind) with physical health (body) resulting in a more complete approach to disease prevention and health promotion that also takes into consideration high life satisfaction, a sense of meaning or purpose, and the ability to manage stress.
With women’s well-being as a priority for the R&WC, we begin our investigation by determining methods and strategies grounded in empirical research and evidence for assessing well-being in women healthcare professionals by way of this comprehensive, scoping review. In our evaluation of existing instruments, we aim to assess if they reflect the above definition of well-being and comprehensively assess both physical and mental components of it including threats to well-being.
The findings of this review will inform the metrics we use to measure well-being at the GW medical enterprise. Therefore, this review aims to identify the primary factors that determine the well-being of women in healthcare professions, determine the most effective, evidence-based metrics of well-being in this population, and inform the design of a well-being instrument to be used annually in the GW medical enterprise.
Methods
This review followed the five-stage process of developing a scoping review as outlined by Arksey and O’Malley: 9
(1) Identifying the Research Question
(2) Identifying Inclusion/Exclusion Criteria (language, target population, study design, outcomes)
(3) Identifying Relevant Studies
(4) Study Selection
(5) Charting the Data
(6) Collecting, Summarizing, and Reporting the Data
The protocol for this review was previously published as a preprint in PsyArXiv. 10
Identifying the Research Question
With the primary objectives of this review in mind, our research team, which includes a nutrition scientist, health sciences researchers, psychotherapist, librarian, and a physician assistant, designed specific research questions:
(1) How do women in healthcare define/understand well-being?
(2) What instruments are used to measure well-being among healthcare workers?
(3) What gender specific factors that emerge from biological differences, societal norms, and cultural expectations related to masculinity, femininity, or other gender identities impact an individual’s sense of well-being?
Identification of Relevant Studies and Search Terms
A systematic search of the literature was conducted with the help of a GW reference librarian, who assisted in developing the search strategy for PubMed. Our choice of PubMed was determined by its public accessibility, focus on biomedical and life sciences literature, and reliability based on peer reviewed sources.
We have not included other databases such as Scopus and Cochrane. First, PubMed should be sufficient to cover much of the literature relating to this topic including previously published scoping or systematic reviews. Further, our team needs to identify relevant metrics quickly to operationalize our study and minimize alteration of the baseline well-being of women in our medical enterprise given that we are soon launching new well-being campaigns as part of the R&WC opening. Our full search strategy is provided in Table 1.
Table 1.
PubMed Search Terms.
| (burnout [tiab] OR work life [tiab] OR work-life [tiab] OR job satisfaction [tiab] OR personal satisfaction [tiab] OR well being [tiab] OR well-being [tiab] OR mental health [tiab]) |
| AND |
| (female [tiab] OR women [tiab] OR woman [tiab]) |
| AND |
| (physician* [tiab] OR doctor* [tiab] OR healthcare worker* [tiab] OR nurse* [tiab] OR clinician* [tiab] OR therapist* [tiab] OR pharmacist* [tiab] OR pathologist* [tiab] OR phlebotomist* [tiab] OR medical laboratory scientist* [tiab] OR dietician* [tiab] OR social worker* [tiab] OR counselor* [tiab] OR healthcare technologist* [tiab] OR healthcare technician* [tiab] OR medical assistant* [tiab]) |
Study Selection: Inclusion/Exclusion Criteria
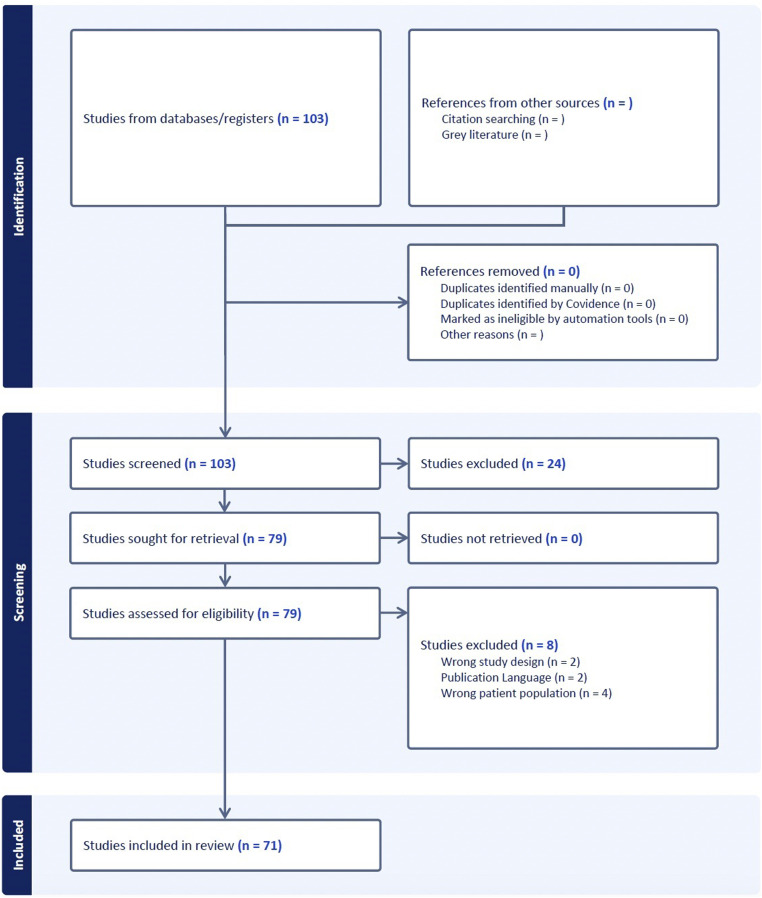
From our search we identified 103 studies from 26 countries (e.g., US, Canada, China, and Japan) published between 1979 (the earliest article that returned from our literature search) and 2022. Those studies were imported into Covidence systematic review software (Veritas Health Innovation; Melbourne, Australia) for screening of their titles and abstracts to determine relevance to our research question. At this stage, 3 members of the research team voted on the inclusion of each article. To move forward into full-text analysis, articles had to have at least 2 votes for inclusion. At this stage, a total of 24 studies were excluded for various reasons including being publishes in any language other than English, Russian, Ukrainian, or Polish, or for considering a topic unrelated to the well-being of women in healthcare. We then assessed the full-text of the remaining 79 manuscripts and further excluded 8 studies that did not consider women healthcare professionals (n=4), were not peer-reviewed academic articles (n=2), and did not contain full-text in our languages of review (n=2). A total of 71 studies were included in this comprehensive review (Figure 1).
Figure 1.
Literature review search and screening process.
Charting the Data: Data Extraction from Full-Text Review
In our review of the literature, we searched for well-being as a broad phenomenon and discovered data on related concepts such as job satisfaction, burnout, stress, resiliency, psychological health, quality of life, and work-life integration. We systematized results based on how the above factors impacted the well-being of women healthcare workers. The outcome measure instruments that were used to assess well-being ranged widely depending on the angle from which each source viewed this phenomenon.
Reviewing the Quality of Literature
Some studies that we investigated were conducted using evidence-based instruments to measure well-being, including Maslach Burnout Inventory (MBI),10-27 Copenhagen Burnout Inventory (CBI),28-31 Short-Form Health Survey (SF 36 V-2),7,31,32 Minnesota Satisfaction Questionnaire (MSQ),10,33,34 Effort-Reward Imbalance Questionnaire (ERI).16,25 Of note, the World Health Organization (WHO) 5 Well-being Index (WHO-5) was only used once 35 but was the most concise well-being instrument among those used in the literature. Further, being designed by the WHO lends credibility to the metric. However, there were several other sources that used various non-validated self-developed outcome measurement tools, including qualitative instruments.36-55 Most studies used cross-sectional study design as well as descriptive correlational methods.
Maslach Burnout Inventory (MBI)
Is a measurement of an individual experience of an occupational burnout in 3 dimensions: emotional exhaustion, depersonalization and personal accomplishment. 56 MBI is used for assessing professional burnout in human services, education, medical personnel, students, and the general population. It assesses and validates the three-dimensional structure of burnout and helps to understand the nature of burnout for developing effective interventions. While burnout may be a symptom of poor well-being and even correlate with well-being, it is not a direct measure of well-being itself.
Copenhagen Burnout Inventory (CBI)
Is an instrument for burnout measurement that consists of 3 scales measuring personal burnout, work-related burnout, and client-related burnout. CBI scales are found to differentiate well between occupational groups in the human service sector and correlate with measures of fatigue and psychological well-being. The scales also predict future absence, sleep problems, use of painkillers, and intention to quit. 57 Again, this is not a direct measure of well-being.
Short-Form Health Survey (SF 36 V-2)
Is a 36 item scale designed to survey health status and quality of life based on self-reporting. The SF-36 includes 1 multi-item scale that assesses 8 health concepts: (1) limitations in physical activities because of health problems; (2) limitations in social activities because of physical or emotional problems; (3) limitations in usual role activities because of physical health problems; (4) bodily pain; (5) general mental health (psychological distress and well-being); (6) limitations in usual role activities because of emotional problems; (7) vitality (energy and fatigue); and (8) general health perceptions. 58 It has excellent psychometrics and produces 2 summary scores: the mental health component and the physical health component. This is a direct measure of well-being.
Minnesota Satisfaction Questionnaire (MSQ)
Is a 5-point Likert-type scale with 20 items that measures how vocational needs and values are satisfied on the job. It is a well-known and validated instrument that has been stable over time. 59 It comes in 2 long forms and 1 short form. It is useful when an organization wants to measure the overall level of satisfaction with the job rather than how important specific aspects of the job are to the employee. 60 While job satisfaction is an important contributor to well-being, this is just one of many and thus not a direct measure of well-being as a whole.
Effort-Reward Imbalance Questionnaire (ERI)
Is a measurement of workplace satisfaction related to specific functional demands (the effort element of the instrument) and the professional recognition and rewards (the rewards element of the instrument) and how these are interrelated and impact professional well-being. 61 The tool is useful is measuring imbalance between challenge and reward and can capture information related to individual coping strategies, the management of stress, feelings of job security and adequacy, and how professional life can impact personal identity. The ERI is a more holistic measure of job satisfaction and its contribution to well-being, making it an important element in well-being. However, it is not a direct measure of well-being in its entirety.
World Health Organization 5 Well-being Index (WHO-5)
Is a measurement of overall well-being limited to a very specific timeframe–the assessment only measures well-being across a period of 2 weeks and is highly context dependent. 62 The WHO-5 was initially developed in 1982 as a 28-item instrument to measure well-being and, over time, has been refined and redesigned to ask only 5 questions: 4 related to positive impacts on well-being and 1 related to negative impacts on well-being. Importantly, multiple studies have confirmed clinical and psychometric validity for this tool, which is a direct measure of well-being.
Collecting, Summarizing, and Reporting the Data
Ultimately, the 71 articles included in the full-text review were imported into Dedoose for thematic analysis as described in detail below.
Thematic Review
Our research team followed an inductive coding process wherein we did not enter the review with a preexisting code book. Rather, we took time to familiarize ourselves with the manuscripts through an initial full-text review of the 71 articles, developed a data extraction form to capture relevant characteristics of each manuscript (e.g., country of study, professions examined, outcomes measures utilized, salient findings), and then conducted an initial coding process where we carefully reviewed the data extracted from each manuscript to identify the phenomenon of study, the instruments used to measure outcomes, and the findings, recommendations, and limitations to each manuscript. From here, we began to quantify code appearance and cooccurrence to identify emergent themes from across the literature. This allowed us to group literature together by theme and make comparisons of reported outcomes across countries of publication and professions under study.
In reviewing the literature, 4 distinct correlates with a negative impact to the well-being of women in healthcare professions were identified: (1) gender inequity in the workplace, (2) poor work-life integration, (3) a lack of workplace autonomy, and (4) family caregiving responsibilities. On the other hand, 3 correlates related to positive well-being were: (1) a supportive and flexible work environment, (2) access to professional mentoring, and (3) supportive personal relationships. These themes are discussed in greater detail subsequently (Table 2).
Table 2.
Salient Themes Emerging From Analysis.
| Negative Correlates to Well-being | Thematic Findings | Relevant References |
| Gender Inequity in the Workplace | 2, 6, 10, 23, 24, 30, 47, 52, 54, 66, 72, 75 | |
| Poor Work-life Integration, including family caregiving responsibilities | 2, 3, 5, 8, 11, 15, 20, 23, 24, 26, 30, 38, 39, 44, 51, 54, 65, 66 | |
| Lack of Workplace Autonomy | 3, 7, 10, 16, 20, 23, 25, 27, 33, 37, 39, 52, 66, 67, 68 | |
| Positive correlates to well-being | Thematic findings | Relevant references |
| Supportive and flexible working environment | 3, 10, 21, 38, 46, 48, 49, 52, 53, 57, 66, 67, 69, 70, 71 | |
| Access to professional development, including mentoring | 6, 10, 23, 48, 54, 55, 66 | |
| Supportive personal relationships | 15, 21, 23, 24, 28, 30, 48, 53, 65, 72, 73, 74 | |
| Intentional mindfulness practice | 8, 12, 14, 15, 21, 34, 36, 43, 69, 74,76 |
Results
Measurements of Well-Being in the Literature
Based on the findings of this review, instruments were used to measure the absence of well-being (e.g., burnout) rather than the presence of well-being itself. Many of the studies in this review only conducted disease-centered evaluations reflecting an area in research that has room to grow (See Reviewing the Quality of Literature Section). Just 10% (n=12) of the assessment tools used in this review seek to quantify individual characteristics such as hope, optimism, resiliency, self-acceptance, self-esteem, or the impact of the lived experience like positive work-life integration, personal and professional growth, meaningful social support, religiousness/spirituality, or having a sense of purpose. Given this, to further bring clarity to the definition of well-being, our study will require a substantially greater utilization and dependence on assessment tools that are anchored in a complete approach to holistic well-being and not solely isolating pathology such as the Cassidy Social Support Scale, Chinese Psychological Capital Questionnaire, or Connor-Davidson Resilience Scale, ERI, MBI, or Perceived Stress Scale-10 (PSS-10).
Work-Life Integration
Among the articles reviewed, the negative relationship between poor work-life integration and a general sense of well-being appeared in approximately a quarter of all studies. 8,11,15,20,24,26,38,44,51,65,66 Studies cite how women are encouraged to prioritize the needs of their children and families over their own personal and professional development, often to their own detriment.2,8,30,39 In the context of our research question, our review found an emphasis on the dissatisfaction women feel when they are required to leave their careers to provide care to their family, even when they are the higher income earner in their families.2,3,5,23,54
Professional Autonomy
Almost 25% of the articles in this review suggest deficient working conditions and limited professional autonomy contribute to women experiencing burnout at greater rates than their male colleagues.16,20,25,27,37,39,52,67,68 Studies indicate that women feel powerless,10,39,52 more constricted by time pressures, 3 have higher workloads,7,33 and expend more emotional energy on psychosocially complex patients than their male colleagues. 3 These articles acknowledged deep professional conflict women have, as they tend to be the compassionate, empathic listeners in an environment that values speed.3,23,66
Supportive Work Environments
In 22% of included articles, the propensity of general satisfaction and a reduction of burnout in the workplace was linked to a supportive environment and flexible schedules, which accommodate childcare and other contributors to well-being.21,46,53,69 In the context of this review, a supportive work environment included those that provided professional recognition,10,66 offered flexibility in terms of scheduling,3,38,70 provided vacation leave, 53 and extended additional training for those interested.3,10,45,48,49,52,57,67,71 The literature also reveals the positive impact of an atmosphere of camaraderie in the workplace. 15
Personal Relationships
Across the literature, 21% of the studies in this review emphasized the importance that personal relationships inside and outside of the workplace have on well-being.21,23,30,48,65,72 The community of friendships,15,28,73 romantic,53,74 and familial relationships24,53,65 provides an essential element of emotional support that positively influences the experiences of women employed in healthcare. These studies show the central phenomenon of well-being ultimately involving the individual’s lived-experience and the impact of environmental influence like social support to relieve stressors.
Implicit Gender Bias
In this comprehensive review, 16% of the articles cited instances of implicit gender bias in the workplace as a significant cause of mental distress among women in healthcare.6,23,24,30,52,54,66,75 This inequity appeared in various forms, from unequal pay for equal work,2,47,52,72,75 to a refusal to acknowledge women clinicians by their titles (i.e., referring to women physicians by their first names but using the Doctor honorific for their male colleagues), 2 and fewer opportunities for professional advancement for women despite similar qualifications to men.6,10,30,54,72,75 Importantly, these inequities were cited widely across the literature regardless of year of publication or country of study, suggesting that this phenomenon remains a persistent if not universal issue.
Intentional Mindfulness
Just 15% of the studies we collected focused on the positive relationship between well-being and intentional mindfulness (n=4),21,36,43,69 nutrition and exercise (n=4),8,12,14,15 and restorative sleep (n=3).34,74,76 These studies add to the growing body of knowledge that lifestyle interventions can reduce compassion fatigue, stress, and burnout with yoga, prayer, meditation, a balanced diet (non-specific), and quality sleep. The correlation between active coping mechanisms and stress management in the literature engenders discussions for future well-being research and the specific challenges of women in healthcare. At our center, this will be a key component of our interventions.77-83
Professional Development Opportunities
Opportunities to pursue professional development and mentoring made a positive difference in 11% of the articles included in this review. Mentoring relationships and professional development allow for a greater sense of belonging,48,54,55,66 a deeper connection to their supervisor, 48 fulfillment in professional opportunities,48,66 and more job satisfaction.6,10,23,54,55 This awareness highlights the fundamental importance of self-actualization in the workplace.
Discussion
This is the first comprehensive review, to our knowledge, to examine multiple study designs related to the well-being of women working in the healthcare profession across various countries and social contexts. Most studies describe well-being as the absence of a disease state and/or absence of adverse effects due to low reward or dissatisfaction in the workplace. However, utilizing just the former definition is not truly indicative of well-being, as well-being goes beyond lack of disease and includes the promotion of security, comfort, and happiness. Therefore, a clear, widely accepted definition will be necessary to implement a standardized approach to well-being research. It is our recommendation that the definition from the CDC be utilized, “a positive outcome that is meaningful for people and for many sectors of society, because it tells us that people perceive that their lives are going well,” be adopted by the research community as part of harmonization efforts. 63 We have adapted the CDC’s language to craft the following definition for the GW R&WC:
Well-being integrates mental health (mind) with physical health (body) resulting in a more complete approach to disease prevention and health promotion that also takes into consideration high life satisfaction, a sense of meaning or purpose, and the ability to manage stress. Tracking these conditions is important for public policy. Yet, many indicators that measure living conditions fail to measure what people think and feel about their lives, fundamental states such as the quality of their relationships, their positive emotions and resilience, the realization of their potential, or their overall satisfaction with life—their “well-being.” 64
Multiple overlapping themes in connection with the absence of well-being in women healthcare professionals emerged throughout this literature review. Despite the significance of the analysis examined, the limited longitudinal data, self-reported questionnaires, and homogeneity of smaller participant groups in some studies could arguably weaken their overall strength and generalizability. This literature review analyzes the key gender-specific factors impacting an individual’s sense of well-being.
Therefore, future reviews considering well-being utilizing a whole-body framework are merited. We suggest examining neurological, psychological, and musculoskeletal outcomes of a supportive work environment, opportunities for professional mentoring, positive personal relationships, and attention to whole body health (e.g., mindfulness, nutrition, exercise, sleep) in relation to valid and reliable measures for disease prevention, health promotion, life satisfaction, a sense of meaning or purpose, and the ability to manage stress.
Conclusion
This review provides a comprehensive overview of studies conducted across 26 countries within the last 4 decades, which explored the well-being of women healthcare professionals and examined the correlation between complex work-related stressors and well-being. The included literature has revealed several important factors contributing to a higher prevalence of job dissatisfaction, emotional turmoil, and a lack of work-life integration, which has devastating effects on healthcare professionals and the quality of patient care. Based on the findings of this review, our future study will examine the impact of positive wellness culture and well-being in a larger construct in relation to women in healthcare professions.
This literature review can inform further investigation of different levels of gender-sensitive interventions, not only on individual but also on organizational level, and their effectiveness. They could take into account the broader context and structural determinants of gender inequality and look into increasing awareness and training on gender sensitivity, gender bias, and structured challenges faced by women in healthcare occupations. Our research would target interventions that could potentially create a more positive and well-being-focused work place culture for women healthcare workers. We present the hypothesis that positive wellness culture and holistic well-being practices will mutually reinforce each other and improve outcome measurements in our vulnerable population. For future study, we propose a definition of well-being that integrates mental health (mind) with physical health (body) resulting in a more complete approach to disease prevention and health promotion that also takes into consideration high life satisfaction, a sense of meaning or purpose, and the ability to manage stress. Furthermore, we want to implement prophylactic methods such as mindfulness practices, educational workshops, institutional policy, and professional- and peer-support to investigate the impact of more holistic well-being practices specific to women.
Acknowledgments
Our team would like to acknowledge the valuable contribution of the following individuals: Thomas Harrod, Associate Director of Reference, Instruction and Access of George Washington University’s Himmelfarb Health Science Library provided guidance in developing a search strategy that would provide rich data in a short window of time. We are also grateful to Ashley Drapeau, Physician Assistant at the George Washington University’s Resiliency & Well-Being Center, for her support in screening studies along with the authors.
Footnotes
Author Contributions: Conceptualization, VK and LAF; methodology, LAF and PGC; analysis, VK and PGC; writing—original draft, VK, HW, PGC, and LAF.; writing—review & editing, VK, PGC, and LAF; supervision, LAF; project administration, VK and PGC; funding acquisition, LAF. All authors have read and agreed to the published version of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the the Rosemary Bowes, PhD, Women’s Mental Health Fund at the George Washington University School of Medicine and Health Sciences, which played no role in the design or conduct of this study.
ORCID iD
Leigh A. Frame https://orcid.org/0000-0002-1475-2778
Data Availability Statement
The template data collection form and extracted data may be available by request after the appropriate application process.
References
- 1.Cheeseman-Day J, Christnacht C. Women hold 76% of all health care jobs, gaining in higher-paying occupations. US Census Bureau. 2019. https://www.census.gov/library/stories/2019/08/your-health-care-in-womens-hands.html [Google Scholar]
- 2.Bogler T, Lazare K, Rambihar V. Female family physicians and the first 5 years: In pursuit of gender equity, work-life integration, and wellness. Can Fam Physician. 2019;65(8):585-588. [PMC free article] [PubMed] [Google Scholar]
- 3.Linzer M, Harwood E. Gendered expectations: Do they contribute to high burnout among female physicians? J Gen Intern Med. 2018;33(6):963-965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takahashi K, Nin T, Akano M, Hasuike Y, Iijima H, Suzuki K. Views of Japanese medical students on the work-life balance of female physicians. Int J Med Educ. 2017;8:165-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt M, Umans T. Experiences of well-being among female doctoral students in Sweden. Int J Qual Stud Health Well-being 2014;9:23059. doi: 10.3402/qhw.v9.23059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muldoon OT, Kremer JM. Career aspirations, job satisfaction and gender identity in female student nurses. J Adv Nurs. 1995;21(3):544-550. [DOI] [PubMed] [Google Scholar]
- 7.Wu SY, Li HY, Wang XR, Yang SJ, Qiu H. A comparison of the effect of work stress on burnout and quality of life between female nurses and female doctors. Arch Environ Occup Health. 2011;66(4):193-200. [DOI] [PubMed] [Google Scholar]
- 8.Uhlig-Reche H, Larson AR, Silver JK. Investigation of work-life integration on burnout symptoms in women physician runners: A cross-sectional survey study. BMJ Open Sport Exerc Med 2021;7(1):e001028. doi: 10.1136/bmjsem-2020-001028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arksey H, O’Malley L. Scoping studies: Toward a methodological framework. Int. J. Social Research Methodology. 2005;8(1):19-32. [Google Scholar]
- 10.Karakcheyeva V, Willis-Johnson H, Corr P, Frame L. The well-being of women in healthcare professions: A comprehensive review. PsyArXiv. 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aziz AA, Kahlout BH, Bashir K. Female physicians suffer a higher burnout rate: A 10-year experience of the Qatar EM Residency Training Programme. J Coll Physicians Surg Pak. 2018;28(8):651-652. [DOI] [PubMed] [Google Scholar]
- 12.Chico-Barba G, Jiménez-Limas K, Sánchez-Jiménez B, Sámano R, Rodríguez-Ventura AL, Castillo-Pérez R, Tolentino M. Burnout and metabolic syndrome in female nurses: An observational study. Int J Environ Res Public Health 2019;16(11):1993. doi: 10.3390/ijerph16111993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cui J, Ren YH, Zhao FJ, Chen Y, Huang YF, Yang L, You XM. Cross-sectional study of the effects of job burnout on immune function in 105 female oncology nurses at a tertiary oncology hospital. Med Sci Monit 2021;27:e929711. doi: 10.12659/MSM.929711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo Y, Lam L, Luo Y, Plummer V, Cross W, Li H, Yin Y, Zhang J. Female nurses' burnout symptoms: No association with the Hypothalamic-pituitary-thyroid (HPT) axis. Psychoneuroendocrinology. 2017;77:47-50. [DOI] [PubMed] [Google Scholar]
- 15.Kandolin I. Burnout of female and male nurses in shiftwork. Ergonomics. 1993;26(1-3):141-147. [DOI] [PubMed] [Google Scholar]
- 16.Kocalevent RD, Pinnschmidt H, Nehls S, Boczor S, Siegert S, Scherer M, Bussche HVD. Burnout and gratification crises in female and male physicians during posgraduate medical education in Germany - A longitudinal study. Psychother Psychosom Med Psychol. 2020;70(8):319-329. [DOI] [PubMed] [Google Scholar]
- 17.Maruyama A, Suzuki E, Takayama Y. Factors affecting burnout in female nurses who have preschool-age children. Jpn J Nurs Sci. 2016;13(1):123-134. [DOI] [PubMed] [Google Scholar]
- 18.Myakotnykh VS, Borovkova TA. Syndrome of emotional burnout among women-physicians elderly. Adv Gerontol. 2017;30(2):208-214. [PubMed] [Google Scholar]
- 19.Payne N. Occupational stressors and coping as determinants of burnout in female hospice nurses. J Adv Nurs. 2001;22(3):396-405. [DOI] [PubMed] [Google Scholar]
- 20.Soltanifar A, Pishbin E, Attaran Mashhadi N, Najaf Najafi M, Siahtir M. Burnout among female emergency medicine physicians: A nationwide study. Emerg Med Australas. 2018;30(4):517-522. [DOI] [PubMed] [Google Scholar]
- 21.Takayama Y, Suzuki E, Kobiyama A, Maruyama A, Sera Y. Factors related to the burnout of Japanese female nurses with children under 3 years old. Jpn J Nurs Sci. 2017;14(3):240-254. [DOI] [PubMed] [Google Scholar]
- 22.Tanguturi VK, Hidrue MK, Rigotti NA, Lehrhoff S, Donelan K, Del Carmen M, Wasfy JH. Does the addition of a child affect burnout differentially in male and female physicians? J Intern Med. 2020;288(4):481-483. [DOI] [PubMed] [Google Scholar]
- 23.Wang L, Wang H, Shao S, Jia G, Xiang J. Job burnout on subjective well-being among Chinese female doctors: The moderating role of perceived social support. Front Psychol. 2020;11:435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y, Chang Y, Fu J, Wang L. Work-family conflict and burnout among Chinese female nurses: The mediating effect of psychological capital. BMC Public Health. 2012;12:915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu H, Liu L, Sun W, Zhao X, Wang J, Wang L. Factors related to burnout among Chinese female hospital nurses: cross-sectional survey in Liaoning Province of China. J Nurs Manag. 2014;22(5):621-629. [DOI] [PubMed] [Google Scholar]
- 26.Zhu X, Shen L, Du P, Guan J. The mediating role of psychological capital between Dayadi stress and job burnout in female nurses with two children. Transl Pediatr. 2021;10(10):2449-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zou G, Shen X, Tian X, Liu C, Li G, Kong L, Li P. Correlates of psychological distress, burnout, and resilience among Chinese female nurses. Ind Health. 2016;54(5):389-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Divinakumar KJ, Bhat PS, Prakash J, Srivastava K. Personality traits and its correlation to burnout in female nurses. Ind Psychiatry J. 2019;28(1):24-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haffizulla FS, Newman C, Kaushal S, Williams CA, Haffizulla A, Hardigan P, Templeton K. Assessment of burnout: A pilot study of international women physicians. Perm J. 2020;24:1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Minamizono S, Nomura K, Inoue Y, Hiraike H, Tsuchiya A, Okinaga H, Illing J. Gender division of labor, burnout, and intention to leave work among young female nurses in Japan: A cross-sectional study. Int J Environ Res Public Health. 2019;16(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang M, Loerbroks A, Li J. Job burnout predicts decline of health-related quality of life among employees with cardiovascular disease: A one-year follow-up study in female nurses. Gen Hosp Psychiatry. 2018;50:51-53. [DOI] [PubMed] [Google Scholar]
- 32.Al-Natour A, Alshareideh KH, Obeisat SM, Alzoubi F, ALBashtawy M. Marital violence affecting female nurses and its physical and mental health consequences. Int Nurs Rev. 2020;67(2):258-264. [DOI] [PubMed] [Google Scholar]
- 33.Bagheri Hosseinabadi M, Etemadinezhad S, Khanjani N, Ahmadi O, Gholinia H, Galeshi M, Samaei SE. Evaluating the relationship between job stress and job satisfaction among female hospital nurses in Babol: An application of structural equation modeling. Health Promot Perspect. 2018;8(2):102-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chang WP, Chang YP. Relationship between job satisfaction and sleep quality of female shift-working nurses: using shift type as moderator variable. Ind Health. 2019;57(6):732-740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khamis F, Al Mahyijari N, Al Lawati F, Badahdah AM. The mental health of female physicians and nurses in Oman during the COVID-19 pandemic. Oman Med J. 2020;35(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alyousef SM, Alhamidi SA. Exploring the value of mindfulness for Saudi Arabian women mental health nurses. Natl Med J India. 2021;34(1):19-23. [DOI] [PubMed] [Google Scholar]
- 37.Birrell N. A comparative analysis into nurse job satisfaction at kameda medical centre and mercy hospital for women. Jpn Hosp. 1998;17:13-26. [PubMed] [Google Scholar]
- 38.Clemen NM, Blacker BC, Floen MJ, Schweinle WE, Huber JN. Work-life balance in women physicians in South Dakota: results of a state-wide assessment survey. S D Med. 2018;71(12):550-558. [PubMed] [Google Scholar]
- 39.Dillon EC, Stults CD, Deng S, Martinez M, Szwerinski N, Koenig PT, Gregg L, Cobb JK, Mahler E, Frosch DL, Le Sieur S, Hanley M, Pertsch S. Women, younger clinicians', and caregivers' experiences of burnout and well-being during COVID-19 in a US healthcare system. J Gen Intern Med. 2022;37(1):145-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.El-Gilany A, Al-Wehady A. Job satisfaction of female Saudi nurses. East Mediterr Health J. 2001;7(1-2):31-37. [PubMed] [Google Scholar]
- 41.Győrffy Z, Dweik D, Girasek E. Reproductive health and burn-out among female physicians: nationwide, representative study from Hungary. BMC Womens Health. 2014;14:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Győrffy Z, Dweik D, Girasek E. Workload, mental health and burnout indicators among female physicians. Hum Resour Health. 2016;14:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jin JH, Lee EJ. Factors affecting quality of work life in a sample of cancer survivor female nurses. Medicina (Kaunas) 2020;56(12):721. doi: 10.3390/medicina56120721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khuwaja AK, Qureshi R, Andrades M, Fatmi Z, Khuwaja NK. Comparison of job satisfaction and stress among male and female doctors in teaching hospitals of Karachi. J Ayub Med Coll Abbottabad 2004;16(1):23-27. [PubMed] [Google Scholar]
- 45.Koivu A, Saarinen PI, Hyrkas K. Who benefits from clinical supervision and how? The association between clinical supervision and the work-related well-being of female hospital nurses. J Clin Nurs. 2012;21(17-18):2567-2578. [DOI] [PubMed] [Google Scholar]
- 46.Kudo Y, Kido S, Shahzad MT, Shida K, Satoh T, Aizawa Y. Enhancing work motivation for Japanese female nurses in small to medium-sized private hospitals by analyzing job satisfaction. Tohoku J Exp Med. 2010;220(3):237-245. [DOI] [PubMed] [Google Scholar]
- 47.Verduzco-Gutierrez M, Larson AR, Capizzi AN, Bean AC, Zafonte RD, Odonkor CA, Bosques G, Silver JK. How physician compensation and education debt affects financial stress and burnout: A survey study of women in physical medicine and rehabilitation. PM R. 2021;13(8):836-844. [DOI] [PubMed] [Google Scholar]
- 48.Von Vultée PJ, Axelsson R, Arnetz B. Individual and organizational well-being of female physicians--an assessment of three different management programs. MedGenMed. 2004;6(1):4. [PMC free article] [PubMed] [Google Scholar]
- 49.Yamazaki Y, Uka T, Marui E. Professional fulfillment and parenting work-life balance in female physicians in Basic Sciences and medical research: a nationwide cross-sectional survey of all 80 medical schools in Japan. Hum Resour Health. 2017;15(1):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zawacki RA, Shahan R, Carey M. Who has higher job satisfaction: male or female nurses? Nurs Manage. 1995;26(1):54-55. [PubMed] [Google Scholar]
- 51.Fernandes JD, Ferreira SL, Albergaria AK, da Conceição FM. Mental health and women's work: images and representations of nurses. Rev Lat Am Enfermagem. 2002;10(2):199-206. [PubMed] [Google Scholar]
- 52.Gold N. Using participatory research to help promote the physical and mental health of female social workers in child welfare. Child Welfare. 1998;77(6):701-724. [PubMed] [Google Scholar]
- 53.Phillips J, Hustedde C, Bjorkman S, Prasad R, Sola O, Wendling A, Bjorkman K, Paladine H. Rural women family physicians: strategies for successful work-life balance. Ann Fam Med. 2016;14(3):244-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schueller-Weidekamm C, Kautzky-Willer A. Challenges of work-life balance for women physicians/mothers working in leadership positions. Gend Med. 2012;9(4):244-250. [DOI] [PubMed] [Google Scholar]
- 55.Woolnough HM, Davidson MJ, Fielden SL. The experiences of mentors on a career development and mentoring programme for female mental health nurses in the UK National Health Service. Health Serv Manage Res. 2006;19(3):186-196. [DOI] [PubMed] [Google Scholar]
- 56.Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99-113. [Google Scholar]
- 57.Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work and Stress. 2005;19(3):192-207. [Google Scholar]
- 58.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473-483. [PubMed] [Google Scholar]
- 59.Martins H, Proença T. Minnesota satisfaction questionnaire: psychometric properties and validation in a population of Portuguese hospital workers. Investigação e Intervenção em Recursos Humanos. 2014. [Google Scholar]
- 60.Nagy M.S. Using a single-item approach to measure facet job satisfaction. J. Occup. Organ. Psychol. 2002;75:77-86. [Google Scholar]
- 61.Siegrist J, Starke D, Chandola T, Godin I, Marmot M, Niedhammer I, Peter R. The measurement of effort-reward imbalance at work. Social science and medicine. 2004;58(8):1483-1499. [DOI] [PubMed] [Google Scholar]
- 62.Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 well-being Index: A systematic review of the literature. Psychotherapy and Psychosomatics. 2015;84:167-176. [DOI] [PubMed] [Google Scholar]
- 63.Center for Disease Control and Prevention . Health related Quality of Life. Well-being Concepts. 2018. [Google Scholar]
- 64.Resiliency GW, Well-being Center. Definitions. 2021. https://rwc.smhs.gwu.edu [Google Scholar]
- 65.Li C, Song R, Fan X, Zhou Z, Xu L. Moderating effect of work-related social support on the relationship between role conflicts and job satisfaction among female nurses pursuing a further degree in China. Int J Nurs Pract 2022;28(5):e13014. doi: 10.1111/ijn.13014 [DOI] [PubMed] [Google Scholar]
- 66.Chesak SS, Cutshall S, Anderson A, Pulos B, Moeschler S, Bhagra A. Burnout among women physicians: A call to action. Curr Cardiol Rep. 2020;22(7):45. doi: 10.1007/s11886-020-01300-6 [DOI] [PubMed] [Google Scholar]
- 67.Heijstra TM, Rafnsdóttir GL, Jónsdóttir LS. Autonomy and well-being among Nordic male and female hospital physicians. Work. 2011;40(4):437-443. [DOI] [PubMed] [Google Scholar]
- 68.Zhou J, Yang Y, Qiu X, Yang X, Pan H, Ban B, Qiao Z, Wang L, Wang W. Serial multiple mediation of organizational commitment and job burnout in the relationship between psychological capital and anxiety in Chinese female nurses: A cross-sectional questionnaire survey. Int J Nurs Stud. 2018;83:75-82. [DOI] [PubMed] [Google Scholar]
- 69.Rich VL, Rich AR. Personality hardiness and burnout in female staff nurses. Image J Nurs Sch. 1987;19(2):63-66. [DOI] [PubMed] [Google Scholar]
- 70.Hayasaka Y, Nakamura K, Yamamoto M, Sasaki S. Work environment and mental health status assessed by the general health questionnaire in female Japanese doctors. Ind Health. 2007;45(6):781-786. [DOI] [PubMed] [Google Scholar]
- 71.Kane D, Kartha A. Job sharing: impact on the general well-being of female nurses. Can J Nurs Adm. 1992;5(1):6-10. [PubMed] [Google Scholar]
- 72.McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K. The work lives of women physicians results from the physician work life study. The SGIM Career Satisfaction Study Group. J Gen Intern Med. 2000;15(6):372-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Campaniello JA. When professional nurses return to school: A study of role conflict and well-being in multiple-role women. J Prof Nurs. 1988;4(2):136-140. [DOI] [PubMed] [Google Scholar]
- 74.Brown JB. Female family doctors: their work and well-being. Fam Med. 1992;24(8):591-595. [PubMed] [Google Scholar]
- 75.Shoaf PR, Gagnon JP. A comparison of female and male pharmacists' employment benefits, salary, and job satisfaction. Contemp Pharm Pract. 1980;3(1):47-51. [PubMed] [Google Scholar]
- 76.Lin PC, Chen CH, Pan SM, Pan CH, Chen CJ, Chen YM, Hung HC, Wu MT. Atypical work schedules are associated with poor sleep quality and mental health in Taiwan female nurses. Int Arch Occup Environ Health. 2012;85(8):877-884. [DOI] [PubMed] [Google Scholar]
- 77.Freudenberger HJ. Staff burn-out. J Soc Issues. 1974;30:159-165. doi: 10.1111/j.1540-4560.1974.tb00706.x [DOI] [Google Scholar]
- 78.Long KNG, Worthington EL, Jr, VanderWeele TJ, Chen Y. Forgiveness of others and subsequent health and well-being in mid-life: A longitudinal study on female nurses. BMC Psychol. 2020;8(1):104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sveinsdóttir H. Self-assessed quality of sleep, occupational health, working environment, illness experience and job satisfaction of female nurses working different combination of shifts. Scand J Caring Sci. 2006;20(2):229-237. [DOI] [PubMed] [Google Scholar]
- 80.Schmittdiel J, Grumbach K, Selby JV, Quesenberry CP. Effects of physician and patient gender concordance on patient satisfaction and preventative care practices. J Gen Intern Med. 2020;15:761-769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mache S, Klapp BF, Groneberg DA. The well-being and mental health of male and female hospital doctors in Germany. World Hosp Health Serv. 2014;50(4):17-22. [PubMed] [Google Scholar]
- 82.Lazar A. Spirituality and job satisfaction among female Jewish Israeli hospital nurses. J Adv Nurs. 2010;66(2):334-344. [DOI] [PubMed] [Google Scholar]
- 83.Long KNG, Chen Y, Potts M, Hanson J, VanderWeele TJ. Spiritually motivated self-forgiveness and divine forgiveness, and subsequent health and well-being among middle-aged female nurses: An outcome-wide longitudinal approach. Front Psychol. 2020;11:1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The template data collection form and extracted data may be available by request after the appropriate application process.