Abstract
Introduction: Bilateral inguinal hernia is a distinct entity in the inguinal hernia category. Open and minimally invasive techniques for the treatment of bilateral inguinal hernia have been previously described. If resources and surgeon expertise are available, guidelines recommend laparoscopic repair for this entity.
Methods:We analyzed data from 83 patients who underwent laparoscopic inguinal hernia repair (total extraperitoneal repair – TEP) of 158 hernias (146 inguinal hernias and 12 other types). Patients had bilateral symptomatic hernias.
Results:Male predominance, with a mean age of 56.7 years, was noted. Lateral hernias (according to EHS classification) were prevalent (71.08%). In the majority of cases (77.11%), meshes made up of a custom polypropylene monofilament mesh were used, followed by Bard 3D Max mesh and Ultralight mesh. Regarding postoperative complications, seroma was the most frequently encountered one in our series (7.23%), followed by urinary retention and ‘feeling’ of mesh (2.41%). Hydrocele, wound hematoma, cord hematoma and chronic pain were seen in 1.20% of patients. No wound infections were observed. The average operative time was 97.77 minutes (SD=17.08); when associated surgery was present, it prolonged the operative time, and we found statistical significance (p=0.002). Similarly, the presence of recurrent hernia extended the operative time, which was found to be statistically significant (p=0.003). The conversion rate in our data was 2.41%. Drainage, which was performed in 13 patients (15.66%), decreased the incidence of complications, especially seroma (p=0.026). The mean length of hospital stay was 2.93 days (SD=1.81), with most of the patients having been discharged on the second postoperative day (37.35%). Only one recurrence was identified (1.20%).
Conclusion:The laparoscopic approach for bilateral inguinal hernia treatment is feasible and has been proven to be advantageous. Our study emphasizes that the TEP procedure has low rates of complications, conversion and recurrence; hence, we recommend bilateral hernia repair.
Keywords:hernia, inguinal hernia, bilateral, Rives-Stoppa, total extraperitoneal repair – TEP, laparoscopic, minimally invasive.
INTRODUCTION
Bilateral inguinal hernia repair represents a topic which is usually associated with unilateral or recurrent hernia repairs. Few studies focus only on the outcome of bilateral inguinal hernia repairs. There are a couple of surgical options for bilateral inguinal hernia repair: open vs laparo-endoscopic procedures. HerniaSurge Group has recently updated the recommendation on bilateral primary inguinal hernia repair, according to which laparo-endoscopic repair is recommended if surgical expertise and sufficient resources are available (1).
The laparo-endoscopic approach has gained popularity and, even if the learning curve is steep, the advantages of this surgical procedure are not negligeable, especially in younger patients where there could be socio-economic benefits over the open approach (1). Similarly, the EAES guidelines conclude that, particularly in bilateral groin hernia, an endoscopic approach is an excellent choice (level 1B consensus 96%) (2).
Our study aim was to evaluate the results obtained in a single center focusing on bilateral symptomatic inguinal hernias among patients subjected to laparoscopic TEP (total extraperitoneal approach). After analyzing the features and complications related to the surgical procedure, we could emphasize that TEP is a safe and feasible treatment in bilateral inguinal hernia repair.
MATERIAL AND METHODS
Data collection
We examined the data of patients who underwent laparoscopic TEP repair between January 1, 2019 and March 1, 2023 in the surgical department of Saint John Hospital, Bucharest, Romania. The sampling was consecutive and exhaustive after obtaining institutional authorization and ethical committee approval to conduct the study (Approval code: 9089; date of approval: 12.04.2023). The inclusion criterion was represented by bilateral inguinal hernias using TEP as the surgical procedure. All operated patients selected by us had symptomatic bilateral groin hernias. We excluded morbid obesity patients (BMI >35 kg/m2), strangulated hernias or massive scrotal hernias. We selected 83 patients, with a total number of 158 hernias, including 146 inguinal hernias and 12 other types. Those with incomplete clinical records were excluded.
Operative technique
Under general anesthesia, a 10-mm port was placed below the umbilicus and a channel between the rectus muscle and posterior sheath. In most of the cases, the development of the preperitoneal space was made with plain dissection (Figure 1) (balloon dissection was used in five cases). Other two 5 mm ports were placed in the midline and planes were developed. The dissection on each side was similar; we followed a modified Dulucq's technique (3). The hernia sac was assessed and reduced. If a peritoneal tear was created, a resorbable suture was placed. A polypropylene mesh measuring 15*12 cm was inserted and unfolded to accommodate each myopectineal orifice (MPO).
We assume that, if the mesh occupies the entire dissected space, the migration or slippage of the mesh is avoided and there is no need for fixation devices (Figure 2), which is in agreement with recent studies (4). Also, nerve entrapment and secondary neuralgia are avoided.
Statistical analysis
For the statistical analysis, the SPSS version 23.0 was used. The association between variables was determined using the chi-squared test. Statistical significance was defined as a p-value of less than 0.05.
RESULTS
Regarding sex distribution, a predominance of male patients was observed (95%).
Age distribution is shown in Table 1 and Figure 3. There was a predominance of patients aged 40-70 years. Subjects’ minimum age was 21 years and maximum age 88 years. Their mean age was 56.7 years (SD±15.2).
We analyzed patients’ comorbidities and found a predominance of cardiac diseases, with 26.51% of all subjects having hypertension. Diabetes and chronic obstructive pulmonary disease (COPD) were less frequently encountered among our study participants (10.85% and 2.41%, respectively). Prostate hyperplasia, a commonly encountered comorbidity associated with inguinal hernia in patients over 65 years old, was seen in 8.43% of patients. Anticoagulants, frequently used by patients with cardiopulmonary diseases, were found in five cases (6.02%). These observations are illustrated in Table 2 and Figure 4.
Regarding the smoking status, 29 (34.94%) of all participants were smokers.
The ASA score, another variable analyzed by us, is a physical status classification system defined from 1 to 6. For our study, patients were included in ASA 1 to 4, with ASA 1 meaning a healthy patient, ASA 2 well controlled mild to moderate systemic disease, ASA 3 severe disease with functional limitation that is not incapacitating, and ASA 4 incapacitating severe disease with constant threat to life (Table 3).
Most of the cases (80.72%) were included in ASA classes 1-2. Two patients (2.41%), including a 70-year-old male and an 80-years old male with several cardiac diseases, were categorized as being in ASA classes 3-4 – the first one was an anticoagulant user with coronary stent who had a hemorrhagic complication in the third postoperative day, which necessitated reintervention with hemostasis and drainage as well as prolonged hospitalization (11 days); the second patient, also an anticoagulant user but with a history of myocardial infarction, was successfully managed by the TEP procedure, and needed to stay in hospital for only five days. We found that longer hospitalization was associated with anticoagulant use (p=0.007) and ASA scores of 3 and 3-4 (p=0.003), but not also with age over 65 (p=0.081). The findings are summarized in Table 4.
Based on EHS classification (5), we analyzed three categories: medial (direct), lateral (indirect) and combined hernias (medial and lateral). This location is in relation to epigastric vessels. A medial hernia is considered when its position is medial to the vessels and a lateral one is lateral to the vessels. In our results, there was a predominance of lateral hernias (71.08%).
We found more lateral left than right hernias (62 versus 56 cases, respectively) and conversely, more medial hernias for the right than left hernias (21 versus 15 cases, respectively). For the combined categories, results were equal (six cases) (Table 5 and Figure 5). In our study, we found 12 (8.21%) recurrent inguinal hernias after open repairs.
Associated surgery was performed in 15.66% of all study subjects (Table 6). Eight patients (9.63%) had umbilical hernia repair (five cases with mesh and the remaining three ones without mesh) depending on the size of the hernia. Two femoral hernias and two obturator hernias were identified and repaired, and one large iliac adenopathy excision (histopathology revealed inflammatory tissue) was done, which was an advantage over open repair.
The operative time had an average value of 97.77 minutes (SD=17.08), with a minimum of 60 minutes and a maximum of 140 minutes. We studied it in relation to the presence of associated surgery and found statistical significance (p=0.002), with associated surgery leading to prolonged operative duration. Also, the presence of recurrent hernia extended the operative time, which was found statistically significant (p=0.003) (Table 7).
Mesh was used in all patients. Custom polipropylene monofilament mesh was predominant (77.11%), followed by Bard 3D max mesh (14 of all cases) and Ultralight mesh in five cases (Table 8).
Drainage was chosen in 13 cases (15.66%). Interestingly, the use of drainage decreased the incidence of complications (p=0.026).
Mean hospitalization was 2.93 days (SD=1.81), with a minimum of one day and a maximum of 11 days. Further analysis showed that most of the study subjects were discharged the second postoperative day (37.35%), followed by the third postoperative day (22.89%), while 11 patients (13.25%) were discharged on the first postoperative day (Figure 6).
Complications occurred in 21.69% of cases (Table 9 and Figure 7). Regarding intraoperative complications, there were two conversions: one to open surgery (Lichtenstein procedure) and another one to TAPP procedure. As for postoperative complications (Figure 7), seroma was the most frequent finding in our series (7.23%), followed by urinary retention and mesh ‘feeling’ (2.41%). Hydrocele, wound hematoma, cord hematoma, chronic pain was found in 1.20 %. No wound infection was noted. One recurrence was identified (1.20%).
Antibiotic prophylaxis was not administered routinely. Analgesia was kept on required basis only. Scrotal support and early mobilization were recommended. On discharge, patients were advised to undergo regular daily activities, except for lifting heavy weights or involving in strenuous activity for at least two weeks after surgery.
Postoperative follow-ups were conducted on day 10, day 15 (if any stiches, the removal was done on that day), at one month and three months.
DISCUSSION
Laparo-endoscopic procedures (TEP, TAPP) for hernia repair have proven benefits for the patient, including comfort of small incisions, fast recovery and few related complications (6, 7), but also for the surgeon, to whom they provide an enhanced anatomy and detail visualization. Whether there is a winner between TEP and TAPP, it remains unclear (6). First of all, the TAPP technique is easier to learn than TEP. In emergent hernias, there is an advantage for the TAPP procedure as its intraperitoneal access enables laparoscopic inspection and safe management of hernia contents. Also, it avoids unnecessary dissection to visualize contralateral hernia defect. However, complications related to bowel injury and possible adhesions to the peritoneal suture are described (7).
Instead, TEP has an ‘inner beauty’ that only a hernia surgeon will understand. From the ‘angel hair’ appearance (the preperitoneal entrance) to ‘lighthouse’ (i.e., Cooper’s ligament), and ‘transversalis sling’ (lateral aspect of the cord), TEP enhances the surgeon’s skills and teaches the anatomy of the preperitoneal space (3). Also, the risk of abdominal organs injury is lowered since the TEP technique is an extraperitoneal approach (8).
Bilateral repair is facilitated by pneumo-dissection (carbon-dioxide pressure) and minimal use of electrocautery. We subscribe to the no fixation technique and using large mesh to cover the entire MPO (3). Another idea supported by us to is that mesh coverage without proper overlap to the hernia orifice can cause mesh protrusion and hernia recurrence (4, 9). Robotic approach has been recently studied, with data showing that robotic bilateral inguinal hernia repair had similar results to the laparoscopic approach (regarding operative time and postoperative complications) (10).
Our study included 83 patients with a total of 158 hernias, of which there were two obturator, two femoral and eight umbilical hernias. Symptomatic bilateral hernias constituted the inclusion criterion. As a first observation that can be made here, the laparoscopic technique allows for the identification and repair of associated hernias of the femoral and obturator spaces.
A male predominance (95% of all subjects) was seen among study participants with a mean age of 56.7 years (SD+-15.2). Regarding the type of hernia according to EHS, our results showed a predominance of lateral hernias (71.08%), which was in accordance with the literature (11).
Of all our study subjects, 10.85% and 2.41% had diabetes and COPD, respectively. Prostate hyperplasia has been often associated with inguinal hernia in patients over 50 years old (12, 13); in our study, this association had significance (p=0.003) and it was found in 8.43% of the total number of patients.
Anticoagulants, a commonly prescribed medication in patients with cardio-pulmonary diseases, were used by five subjects (6.02%). Regarding the smoking status, 29 (34.94%) of all study participants were smokers.
The average operative time was 97.77 minutes (SD=17.08), with a minimum of 60 minutes and a maximum of 140 minutes. Some studies reported a shorter operative time, but their exclusion criteria were different from ours (14). In our study there were 12 (14.46%) recurrent inguinal hernias which had been previously treated by anterior approach, and 15.66% of patients had associated surgery, which lead to prolonged operative time. One can observe the advantage of laparo-endoscopic approach in recurrent hernias and the guidelines encourage this method (1, 2). In this respect, we underline the advantage of TEP procedure over open repair in treating other associated hernias, which is also reported by Chowbey et al (15). Our study found two femoral and two obturator hernias that had been concomitantly treated via TEP approach.
Complications constitute another important topic to bring upon in the TEP procedure. In our study, we found two conversions: one to open surgery and another one to the TAPP technique. Intense adhesions and difficult controlling of bleeding were the two main reasons for our decision to quit TEP. Our findings reveled a conversion rate of 2.41%. In a prospective cohort study on 3457 patients who underwent TEP, Gass et al reported a conversion rate of 1% (p=0.011), but their subjects had unilateral, not bilateral, inguinal hernias (16). Another study revealed a conversion rate of 7%, but its findings should be interpreted with caution as 20 years ago the technique was still new and some surgeons were at the beginning of their learning curve (17). Similar results were reported by X Feliu-Pala et al (14). Nevertheless, it is important to mention there were no bladder, bowel or epigastric vessel injury detected in our series.
We analyzed complications in relation to comorbidities. We noted no association between the rate of complications and ASA score (p=0.237), anticoagulant use (p=0.147), presence of diabetes mellitus (p=0.130), COPD (p=0.423), HBP (p=0.127), obesity (p=0.449), presence of smoking status (p=0.873). Also, we did not find an association between complication rate and the status of complicated hernia (p=0.743). Age >65 years was not found to be associated with increased complication rates (p=0.594).
Postoperative complications were divided into general (not related to surgery) and surgical (related to surgery) complications. The first category included only urinary retention (2.41%); hence, we should specify that at least half of patients had preoperative urinary catheterization. One reason for this action is related to optimization of the preperitoneal space and enhanced dissection of the Retzius space, although some studies suggest the contrary (18, 19). In the second category we included seroma (7.23% of all patients), but all cases were not clinically significant and had no impact on the postoperative outcome. This incidence is similar to other studies (20, 21), with data from those studies suggesting that the size of defect influences seroma formation. Also, whether the mesh type influences seroma formation is a matter of debate. One meta-analysis did not show any difference in the impact of lightweight versus heavyweight meshes on seroma rate after TEP repair (22).
In our study, we noted there was no association between seroma rate and inguinoscrotal hernias (p=0.650), but the mesh choice did influence the seroma rate: thus, the use of Ultralight mesh decreased this rate, with a statistical significance (p=0.001) being noted, while no significance was seen for Bard 3D max (p=0.684) and PPMF mesh (p=0.124).
Another aspect in seroma rate is related to the use of drainage. Some studies prove that drain insertion after TEP repair may reduce the incidence of seroma formation, but guidelines are against routine drain insertion after primary uncomplicated repair (1). We used drains in 13 patients (15.66%), but most of those were anticoagulant users and had complicated hernias.
Interestingly, the use of drainage decreased the incidence of overall complications (p=0.026). We reported one hemorrhage (1.2%) that occurred on the third postoperative day and required reintervention, one cord hematoma (1.2%) that was treated conservatively, and one preperitoneal hematoma (1.2%) which has also necessitated reintervention.
The mean hospital stay was 2.93 days (SD=1.81), with a minimum of one day and a maximum of 11 days. The analysis on this parameter revealed that only 13.25% of patients were treated as day cases, which must be interpreted in the light of the hospital public regulations (23). Moreover, data from clinical records showed that most of the patients could have been discharged on the first postoperative day; hence, patient subjectivity is incriminated. However, less than a third of patients were discharged after more than three days postoperatively.
On follow-up, two patients (2.41%) had a mesh-related complication, ‘mesh-feeling’, which did not influence the patient’s quality of life or daily activities. Little is known about such experiences of patients and further studies are needed (24). We identified one patient with hydrocele (1.2%), another one with chronic groin pain (1.2%) and a third one with recurrence (1.2%), which was in agreement with the literature (25, 26).
A discussion can be made on chronic groin pain after TEP repair: the origin of this pain is thought to be less related to direct nerve injury and more inflammatory-mediated and related to mechanical or fibrotic responses of scar tissue formation (27).
However, spontaneous pain reduction after TEP repair has been described before and can be explained by the self-limiting condition of the inflammatory reaction, lasting up to six months after surgery (28). Magnetic resonance imaging (MRI) can help in demonstrating the mesh position and, to some extent, the presence of fibrosis (29).
CONCLUSION
In bilateral inguinal hernia repair, laparoscopic TEP approach is an excellent option which offers considerable advantages for the patient. With proper mesh size and placement, recurrence is reduced, and also postoperative pain due to no fixation technique. One advantage over the open approach is that the TEP procedure can identify and treat concomitant hernias such as femoral or obturator hernias. The results of our study encourage this surgical approach to treat bilateral inguinal hernias whenever surgical expertise and resources are available.
Study limitations
The present study has two main limitations: the first one is related to the small number of patients and the retrospective nature of the study, and the second one to potential biases resulting from surgeons’ preferences and patients’ selection.
Informed consent: Due to the retrospective nature of the present study, patients’ signed informed consent was waived.
Data availability: Data that support the findings of this study are available upon request.
Conflicts of interest: none declared.
Financial support: none declared.
Acknowledgments: This article was published with the support granted by the project entitled "Net4SCIENCE: Applied doctoral and postdoctoral research network in the fields of smart specialization Health and Bioeconomy", project code POCU/993/6/13/154722.
FIGURE 1.

Plain dissection of the preperitoneal space with the telescope – detail; yellow arrow points to the Cooper’s ligament – ‘lighthouse’ in TEP approach (1)
FIGURE 2.

Placement of the two meshes overlapping in the middle (yellow arrows point to Cooper’s ligaments, green arrow points urinary bladder)
FIGURE 3.

Age distribution in patients with bilateral hernia repair
TABLE 1.
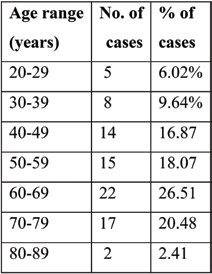
Age distribution in patients with bilateral hernia repair
TABLE 2.

Comorbidities in patients with bilateral hernia repair
FIGURE 4.

Comorbidities in patients with bilateral hernia repair
TABLE 3.
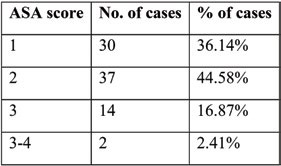
ASA score in patients with bilateral hernia repair
TABLE 4.
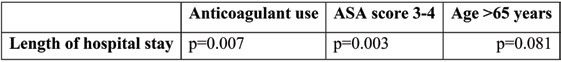
Association between length of hospital stay and different variables (significant association is considered when p<0.05)
TABLE 5.

Type of inguinal hernias based on location
FIGURE 5.

Type of bilateral hernias (orange for right inguinal hernia and blue for left inguinal hernia)
TABLE 6.

Associated surgery in patients with bilateral hernia repair
TABLE 7.

Association between operative time and different variables, with significant association being considered when p <0.05
TABLE 8.

Mesh type in patients with bilateral hernia repair
FIGURE 6.

Discharge day among patients with bilateral hernia repair
TABLE 9.

Overall complications in patients with bilateral hernia repair
FIGURE 7.

Complications in patients with bilateral hernia repair
Contributor Information
Claudiu-Octavian UNGUREANU, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; General Surgery Department, “Sf. Ioan” Clinical Emergency Hospital, 13 Vitan-Bârzeşti Road, 042122 Bucharest, Romania.
Octav GINGHINA, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; General Surgery Department, “Sf. Ioan” Clinical Emergency Hospital, 13 Vitan-Bârzeşti Road, 042122 Bucharest, Romania.
Floris STANCULEA, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; General Surgery Department, “Sf. Ioan” Clinical Emergency Hospital, 13 Vitan-Bârzeşti Road, 042122 Bucharest, Romania.
Razvan IOSIFESCU, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; General Surgery Department, “Sf. Ioan” Clinical Emergency Hospital, 13 Vitan-Bârzeşti Road, 042122 Bucharest, Romania.
Dan CRISTIAN, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; General Surgery Department, “Coltea” Clinical Hospital, 1 Bratianu Boulevard, 030171 Bucharest, Romania.
Valentin Titus GRIGOREAN, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; General Surgery Department, “Bagdasar-Arseni” Clinical Emergency Hospital, 12 Berceni Road, 041915 Bucharest, Romania.
Razvan-Ionut POPESCU, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; Urology Department, “Th. Burghele” Clinical Hospital, 20 Panduri Street, 050659 Bucharest, Romania.
Ramona DOBRE, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; Endocrinology Department “C. I. Parhon” Institute of Endocrinology, 34-38 Aviatorilor Blvd. 011863 Bucharest, Romania.
Niculae IORDACHE, “Carol Davila” University of Medicine and Pharmacy, 37 Dionisie Lupu Street, 020021 Bucharest, Romania; General Surgery Department, “Sf. Ioan” Clinical Emergency Hospital, 13 Vitan-Bârzeşti Road, 042122 Bucharest, Romania.
References
- 1.HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22:1–165. doi: 10.1007/s10029-017-1668-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poelman MM, van den Heuvel B, Deelder JD, et al. EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc. 2013;27:3505–3519. doi: 10.1007/s00464-013-3001-9. [DOI] [PubMed] [Google Scholar]
- 3.Agrawal M, Bhagwat S, Rao P. Dulucq's technique for laparoscopic totally extraperitoneal hernioplasty. J Minim Access Surg. 2020;16:94–96. doi: 10.4103/jmas.JMAS_66_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hiratsuka T, Shigemitsu Y, Etoh T, et al. Appropriate mesh size in the totally extraperitoneal repair of groin hernias based on the intraoperative measurement of the myopectineal orifice. Surg Endosc. 2021;35:2126–2133. doi: 10.1007/s00464-020-07616-2. [DOI] [PubMed] [Google Scholar]
- 5.Miserez M, Alexandre JH, Campanelli G, et al. The European hernia society groin hernia classification: simple and easy to remember. Hernia. 2007;11:113–116. doi: 10.1007/s10029-007-0198-3. [DOI] [PubMed] [Google Scholar]
- 6.Köckerling F, Schug-Pass C, Adolf D, Keller T, Kuthe A. Bilateral and unilateral total extraperitoneal inguinal hernia repair (TEP) has equivalent early outcomes: analysis of 9395 cases. World J Surg. 2015;39:1887–1894. doi: 10.1007/s00268-015-3055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacob DA, Hackl JA, Bittner R, et al. Perioperative outcome of unilateral versus bilateral inguinal hernia repairs in TAPP technique: analysis of 15,176 cases from the Herniamed Registry. Surg Endosc. 2015;29:3733–3740. doi: 10.1007/s00464-015-4146-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Łomnicki J, Leszko A, Kuliś D, Szura M. Current treatment of the inguinal hernia – the role of the totally extraperitoneal (TEP) hernia repair. Folia Med Cracov. 2018;58:103–114. doi: 10.24425/fmc.2018.125076. [DOI] [PubMed] [Google Scholar]
- 9.Knook MT, van Rosmalen AC, Yoder BE, et al. Optimal mesh size for endoscopic inguinal hernia repair: a study in a porcine model. Surg Endosc. 2001;15:1471–1477. doi: 10.1007/s00464-001-0048-9. [DOI] [PubMed] [Google Scholar]
- 10.Solaini L, Cavaliere D, Avanzolini A, et al. Robotic versus laparoscopic inguinal hernia repair: an updated systematic review and meta-analysis. J Robot Surg. 2022;16:775–781. doi: 10.1007/s11701-021-01312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niebuhr H, Köckerling F. Surgical risk factors for recurrence in inguinal hernia repair – a review of the literature. Innov Surg Sci. 2017;2:53–59. doi: 10.1515/iss-2017-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reis RB, Rodrigues Neto AA, Reis LO, et al. Correlation between the presence of inguinal hernia and the intensity of lower urinary tract symptoms. Acta Cirurgica Brasileira. 2011;26 Suppl 2:125–128. doi: 10.1590/s0102-86502011000800023. [DOI] [PubMed] [Google Scholar]
- 13.Wu YH, Juan YS, Shen JT, et al. Lower urinary tract symptoms-Benign prostatic hyperplasia may increase the risk of subsequent inguinal hernia in a Taiwanese population: A nationwide population-Based cohort study. PLoS One. 2020;15:e0234329. doi: 10.1371/journal.pone.0234329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feliu X, Claver ´ıa R, Besora P, et al. Bilateral inguinal hernia repair: laparoscopic or open approach? Hernia. 2011;15:15–18. doi: 10.1007/s10029-010-0736-2. [DOI] [PubMed] [Google Scholar]
- 15.Chowbey PK, Bandyopadhyay SK, Khullar R, et al. Endoscopic totally extraperitoneal repair for occult bilateral obturator hernias and multiple groin hernias. J Laparoendosc Adv Surg Tech A. 2004;14:313–316. doi: 10.1089/lap.2004.14.313. [DOI] [PubMed] [Google Scholar]
- 16.Gass M, Banz VM, Rosella L, et al. TAPP or TEP? Population-based analysis of prospective data on 4,552 patients undergoing endoscopic inguinal hernia repair. World J Surg. 2012;36:2782–2786. doi: 10.1007/s00268-012-1760-4. [DOI] [PubMed] [Google Scholar]
- 17.Van Hee R, Goverde P, Hendrickx L, et al. Laparoscopic transperitoneal versus extraperitoneal inguinal hernia repair: a prospective clinical trial. Acta Chir Belg. 1998;98:132–135. [PubMed] [Google Scholar]
- 18.Fafaj A, Lo Menzo E, Alaedeen D, et al. Effect of Intraoperative Urinary Catheter Use on Postoperative Urinary Retention After Laparoscopic Inguinal Hernia Repair: A Randomized Clinical Trial. JAMA Surg. 2022;157:667–674. doi: 10.1001/jamasurg.2022.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garg P, Menon GR, Rajagopal M, Ismail M. Laparoscopic total extraperitoneal repair of recurrent inguinal hernias. Surg Endosc. 2010;24:450–454. doi: 10.1007/s00464-009-0602-4. [DOI] [PubMed] [Google Scholar]
- 20.Lau H, Lee F. Seroma following endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc. 2003;17:1773–1777. doi: 10.1007/s00464-002-8771-4. [DOI] [PubMed] [Google Scholar]
- 21.Berney CR. The Endoloop technique for the primary closure of direct inguinal hernia defect during the endoscopic totally extraperitoneal approach. Hernia. 2012;16:301–305. doi: 10.1007/s10029-011-0892-z. [DOI] [PubMed] [Google Scholar]
- 22.Currie A, Andrew H, Tonsi A, et al. Lightweight versus heavyweight mesh in laparoscopic inguinal hernia repair: a meta-analysis. Surg Endosc. 2012;26:2126–2133. doi: 10.1007/s00464-012-2179-6. [DOI] [PubMed] [Google Scholar]
- 23.Duran A, Chanturidze T, Gheorghe A, Moreno A. Assessment of Public Hospital Governance in Romania: Lessons From 10 Case Studies. Int J Health Policy Manag. 2019;8:199–210. doi: 10.15171/ijhpm.2018.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hooper MA, Renshaw SM, Poulose BK. Patient perspectives on mesh-related complications after hernia repair. Surgery. 2022;171:994–999. doi: 10.1016/j.surg.2021.09.022. [DOI] [PubMed] [Google Scholar]
- 25.Feliu-Palà X, Martín-Gómez M, Morales-Conde S, Fernández-Sallent E. The impact of the surgeon's experience on the results of laparoscopic hernia repair. Surg Endosc. 2001;15:1467–1470. doi: 10.1007/s00464-001-9017-6. [DOI] [PubMed] [Google Scholar]
- 26.Dulucq JL, Wintringer P, Mahajna A. Laparoscopic totally extraperitoneal inguinal hernia repair: lessons learned from 3100 hernia repairs over 15 years. Surg Endosc. 2009;23:482–486. doi: 10.1007/s00464-008-0118-3. [DOI] [PubMed] [Google Scholar]
- 27.Linderoth G, Kehlet H, Aasvang EK, Werner MU. Neu-rophysiological characterization of persistent pain after laparo- scopic inguinal hernia repair. Hernia. 2011;15:521–529. doi: 10.1007/s10029-011-0815-z. [DOI] [PubMed] [Google Scholar]
- 28.Alfieri S, Amid PK, Campanelli G, et al. International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia. 2011;15:239–249. doi: 10.1007/s10029-011-0798-9. [DOI] [PubMed] [Google Scholar]
- 29.Burgmans JPJ, Voorbrood CEH, Van Dalen T, et al. Chronic pain after TEP inguinal hernia repair, does MRI reveal a cause? Hernia. 2016;20:55–62. doi: 10.1007/s10029-015-1448-4. [DOI] [PubMed] [Google Scholar]


