Abstract
Purpose:
In a cross-sectional sample of US Hispanic/Latino adults, we aimed to describe step-based metric distributions, estimate their associations with activity counts and self-report, and calibrate step-based translations of current (2018) US physical activity (PA) guidelines, i.e., ≥150 min/week moderate-to-vigorous PA (MVPA) from accelerometer counts and self-report.
Methods:
The Hispanic Community Health Study/Study of Latinos enrolled 16,415 Hispanic/Latino adults 18–74 years from four US cities (2008–2011). Participants completed the Global PA Questionnaire and one week of Actical accelerometer wear (n=12,528). Weighted medians were used to describe step-based metrics, and Spearman correlations estimated their relationships with count-based and self-reported PA indicators. Receiver operator characteristic (ROC) curve analyses were used to examine the ability of each step-based metric to classify participants meeting PA guidelines.
Results:
Overall, US Hispanic/Latino adults accumulated medians of 6,770 steps/day and 6, 18, 236, and 630 min/day at ≥100, ≥70, 1–69, and 0 steps/min, respectively. Count-based time in MVPA, light PA, and sedentary behavior were most strongly correlated (rs=0.79–0.85) with times ≥70, 1–69, and 0 steps/min, respectively, while self-reported MVPA had similar correlations with steps/day and times ≥40 and ≥70 steps/min (rs=0.28–0.29). Time ≥70 steps/min had the greatest capacity to classify participants meeting PA guidelines with both measures of MVPA.
Conclusions:
This study provides the first normative values (based on percentiles) of step-based metrics for US Hispanic/Latino adults, which can facilitate surveillance, program planning, research, and data interpretation. Our finding that PA guidelines corresponded to 6,000–7,000 steps/day or ~20 min/day at ≥70 steps/min with an Actical accelerometer can be considered alongside dose-response relationships with health outcomes to develop step-based recommendations that are consistent with and better communicate PA guidelines.
Keywords: ACCELEROMETER, CADENCE, PEDOMETER, ACTICAL, WALKING, LATINO
INTRODUCTION
Nearly 70 years of research (1) have demonstrated the beneficial effects of physical activity (PA) on various health outcomes, yet physical inactivity remains responsible for 7.2% and 7.6% of global all-cause and cardiovascular disease deaths, respectively (2). An extensive review of this evidence (3) informed the 2018 United States (US) PA guidelines, which convey the minimum amount of moderate-to-vigorous intensity PA (MVPA) required for acquiring the majority of health benefits. While much of this research was based on self-reported PA (3), technological advances have allowed accelerometers to become feasible for use in large-scale epidemiological studies (4). These wearable devices enable patterns of PA to be assessed with greater accuracy and higher resolution than previous questionnaire-based methods (5).
Traditionally, the electronic signals produced by accelerometers are digitally translated into ‘activity counts’ (6), a derived measure conveying the acceleration values accumulated over a defined time interval (i.e., epoch). Alternatively, with the proliferation of smartphones and wearable devices offering a step-counting feature (7), step-based metrics may provide a simpler and more accessible approach to monitoring PA and communicating PA guidelines to the general public (3, 8). For these reasons, the 2018 PA Guidelines Advisory Committee (3) examined the relationships between daily step volume (i.e., steps/day) and several health outcomes, but were unable to provide a recommended number of steps/day due to insufficient evidence. The Committee (3, 8) further stated a need for exploring the relationship between stepping cadence (steps/min; a proxy for intensity (9, 10)) and health.
Subsequent studies have continued to inform step-based translations of PA guidelines by quantifying dose-response relationships between volumes and patterns of stepping and health outcomes (11, 12). A complementary approach may be to examine how step-based metrics correspond to PA levels concurrently assessed through self-report and activity counts (13, 14) and thus transitively inform step-based recommendations using the full body of literature on PA and health (3). This approach is also necessary to ensure that future step-based recommendations are congruent with the levels of MVPA recommended in current PA guidelines.
In addition to the importance of guidelines for public health, normative values are essential for monitoring trends over time, facilitating research and program planning, and aiding in data interpretation (15). Normative values describing patterns of stepping are available for several populations (16–18), yet no such values exist for US Hispanic/Latino adults, a population with lower self-reported leisure time (19) but higher accelerometer-assessed (20, 21) PA than non-Hispanic Black and non-Hispanic white adults. Therefore, the aims of this cross-sectional study were to 1) describe the volumes and patterns of stepping observed in a community-based cohort of US Hispanic/Latino adults, 2) estimate associations between step-based metrics and those based on activity counts and self-report, and 3) calibrate preliminary step-based translations of US national PA guidelines using MVPA levels from activity counts and self-report.
METHODS
Participants were included from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL; http://www.cscc.unc.edu/hchs). This community-based cohort included 16,415 self-identified Hispanic/Latino men and women from 18–74 years of age who were recruited and enrolled between March 2008 and June 2011 from randomly selected households through a multistage area probability design in four US communities (Bronx, NY; Chicago, IL; Miami, FL; San Diego, CA) (22, 23). The study protocol was approved by Institutional Review Boards from all participating institutions and informed consent was obtained from all participants.
Physical activity assessments
During the HCHS/SOL baseline clinic visit, participants were asked to wear an Actical accelerometer (version B-1, model 198–0200-03; Respironics Co. Inc., Bend, OR). Technical specifications for the Actical (24) and a detailed description of adherence and performance in HCHS/SOL (25) are available elsewhere. Briefly, participants were fitted with a belt at the baseline clinic visit and instructed to continue wearing the Actical above their right iliac crest for seven days while undertaking their usual activities, removing it only for swimming, showering, and sleeping. The Actical was programmed to summarize accelerations sampled at 32 Hz into counts and steps in 1-min epochs. To standardize the monitoring period across sites, accelerometer data were truncated to include the six days following the baseline clinic visit. Nonwear was defined as periods of ≥90 mins with zero counts, allowing for ≤2 min intervals of nonzero counts if no counts were detected during the preceding and subsequent 30 mins (26). Adherence was defined as ≥10 hours of wear on ≥3 of the 6 possible days. All metrics derived from accelerometer data were averaged across a participant’s adherent wear days.
To describe the distributions of step-based metrics in HCHCS/SOL (Aim 1), we derived 1) daily step volume (total steps/day), 2) time above three cadence thresholds (min/day at ≥40 steps/min, ≥70 steps/min, and ≥100 steps/min), 3) time in two cadence bands (min/day at 1–39 steps/min and 1–69 steps/min), 4) peak 30-min cadence (average steps/min of the 30 highest, but not necessarily consecutive, minutes in a day), and 5) time at zero cadence (min/day at 0 steps/min) (10). For additional comparisons with prior studies, we also derived the time in each of 20 step/min cadence bands developed by Tudor Locke et al (27). These step-based metrics are summarized in Supplemental Table 1 (see Supplemental Digital Content 1, Definitions of step-based metrics).
For examining the correspondence between step-based metrics and those derived from activity counts and self-report (Aim 2), four additional measures were computed using the Actical count data: 1) daily count volume (total counts/day), 2) sedentary time (≤99 counts/min), 3) time in light intensity PA (100–1,534 counts/min), and 4) time in MVPA (sum of daily moderate [1,535–3,961 counts/min] and vigorous [≥3,962 counts/min] PA) (28–30).
Self-reported PA in a typical week was assessed using an interviewer-administered modified Global Physical Activity Questionnaire (GPAQ) (31, 32), which is available at the study website. As detailed elsewhere (33), this questionnaire asked participants about frequency (days/week) and duration (mins/day) of activities performed in a typical week for ≥10 mins within 3 activity domains: work (6 questions), transportation (3 questions), and recreation (6 questions). Time spent sitting or reclining in a typical day was assessed with one question. Activity within the work, transportation, and recreation domains was used to derive weekly moderate PA (small increases in breathing and heart rate), while vigorous PA (large increases in breathing and heart rate) was based only on activities within the work and recreation domains. Responses to these questions were used to derive 1) time in MVPA, calculated by summing min/day of moderate and vigorous intensity activities, 2) metabolic equivalent (MET-) min/day, based on assigning moderate and vigorous PA intensities of 4 and 8 METs, respectively, and 3) sedentary time, representing usual daily minutes spent sitting or reclining. PA levels based on counts and self-report in HCHS/SOL have been described previously (33).
To calibrate preliminary step-based translations of the 2018 US national PA guidelines (Aim 3), participants were classified into meeting or not meeting guidelines based on accelerometer-assessed as well as self-reported levels of MVPA. As reported previously (25, 33), meeting PA guidelines was operationalized as attaining ≥150 min/week of moderate PA, ≥75 minutes/week of vigorous PA, or a combination of the two (i.e., a sum of moderate and vigorous PA ≥150 min/week, with min/week of vigorous PA multiped by two). Because participants contributed 3 to 6 days of adherent accelerometer data, weekly MVPA from counts was estimated using average daily MVPA multiplied by seven (25).
Other descriptive measures
HCHS/SOL participants were interviewed in Spanish or English at the baseline clinic visit to assess sex (female or male), age, marital status (single, separated/widowed, or married/partnered), employment status (retired, unemployed, part time [≤35 hrs/week], or full time [>35 hrs/week]), educational attainment (no, at most, or greater than a high school diploma/GED), current occupation (non-skilled, service, skilled, professional/administrative/office, or other), self-identified Hispanic/Latino background (Central American, Cuban, Dominican, Mexican, Puerto Rican, South American, >1 heritage, or other), time residing in US 50 states/DC (US-born, ≥10 years, or <10 years), and language preference (Spanish or English). Height and weight were measured using standardized protocols (23) and body mass index (BMI) was categorized as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), or obese (≥30.0 kg/m2).
Analytic sample
The HCHS/SOL sample design and cohort selection have been described previously (22). Briefly, 16,415 self-identified Hispanic/Latino persons aged 18 to 74 years were recruited and enrolled from randomly selected households in each of the four US communities using a stratified two-stage area probability design. Of the 14,913 HCHS/SOL participants who returned the Actical with at least some wear time and without a device malfunction previously identified from the count data, 12,750 (85%) met wear time adherence criteria, as described elsewhere (25). Data for participants with outlying stepping patterns (e.g., one or more days with >40,000 steps, <10% of epochs with 0 steps/min, or a >6-hr bout of consecutive non-zero step/min) were visually inspected and 68 were excluded due to device malfunctions. Specifically, these data included non-zero step values (typically of 20–40 steps/min) for implausibly long periods of time. After excluding an additional 42 participants with missing steps data, 43 with missing GPAQ data, 64 with an average accelerometer wear time ≥23 hrs/day, and 5 participants over 74 years of age at the clinic visit, the final analytic sample consisted of 12,528 participants.
Because oversampling occurred at both stages of sample selection to increase the likelihood of selecting eligible households, participants were assigned sampling weights calibrated to the 2010 US Census according to age, sex, and Hispanic/Latino background. The HCHS/SOL target population was defined as all non-institutionalized Hispanic/Latino adults 18–74 years of age residing in the defined geographical areas (census block groups) across the four participating sites. Inverse probability weights for missing accelerometry data (34) were also computed based on predicted Actical adherence and multiplied by the sampling weights, as described elsewhere (25). These weights were applied when calculating sample characteristics, descriptive statistics (e.g., means, medians, and proportions) related to Aim 1, and negative predictive values (NPV) and positive predictive values (PPV) in Aim 3. These statistics therefore represent the characteristics of the underlying population rather than the cohort members studied.
Statistical analysis
To account for the potential influence of wear time on time at zero cadence and sedentary time (r = 0.79 and 0.83, respectively) and differences in mean sedentary time across sites, time at zero cadence and sedentary time were standardized to the approximate mean daily wear time in the sample (16 hrs/day) using the residual method (35). Other step-based metrics had weaker correlations with wear time (all r ≤0.29) and therefore were not adjusted for wear time in primary analyses. All analyses were performed using R version 3.6.1 9 (R Foundation for Statistical Computing, Vienna, Austria).
To address Aim 1, the median of each step-based metric was estimated for the total sample as well as by sociodemographic groups (sex, age, marital status, employment status, current occupation, and educational attainment), BMI, site, and sociocultural groups (self-identified Hispanic/Latino background, time residing in the US, and language preference). Medians for each grouping variable except age group were adjusted for age using quantile regression. Specifically, we modeled each step-based metric as a function of age group and each grouping variable, and medians were estimated for the corresponding subgroups by 1) inputting the age distribution reported in the 2010 US Census and 2) fitting the model with replication weights (36). This analysis was conducted using the `quantreg` and `survey` R packages.
Median time above each cadence from 1 to 140 steps/min in 1 step/min intervals was also calculated and plotted. Wald 95% confidence intervals (CIs) for each median were constructed using inverse estimated cumulative distribution functions that accounted for the survey design and sampling weights (37). To aid in describing trends by subgroups, we evaluated 1) whether percent differences between pairs of medians (difference divided by average of two medians) were >20%, and 2) whether 95% CIs overlapped, as to also consider the precision of median estimates. These should not be interpreted as formal null hypothesis tests.
To address Aim 2, associations between each step-based metric and each PA indicator based on counts (average daily count volume, MVPA, light PA, and sedentary time) and on self-report (weekly MET-min, MVPA, and sedentary time) were quantified with Spearman correlations (rs).
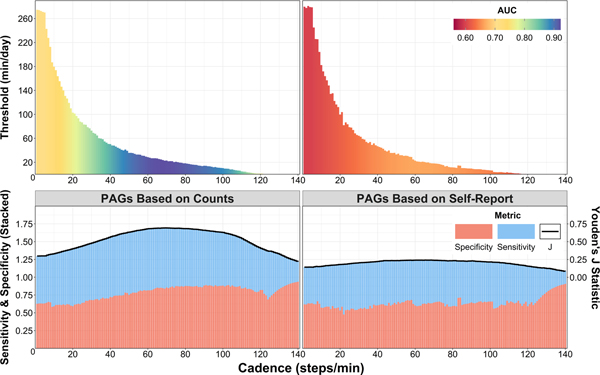
For Aim 3, receiver operator characteristic (ROC) curve analyses were used to examine the ability of each step-based metric to classify whether or not participants met PA guidelines (according to counts and self-report). Optimal thresholds for each step-based metric were then identified as the threshold maximizing Youden’s J statistic (where J = sensitivity + specificity – 1) (38). A 95% CI for each optimal threshold was computed through a bootstrap with 20,000 replicates (39). Classification accuracy was evaluated in terms of area under the ROC curve (AUC), sensitivity, specificity, overall accuracy, and positive and negative predictive values. Because the 150 min/week MVPA threshold provided by PA guidelines is largely based on self-report (20), we prioritized AUC when comparing step-based classifiers of count-derived MVPA, as AUC characterizes the entire ROC curve as opposed to a single threshold (38). These analyses were also conducted stratified by age in three categories (18–39, 40–59, and 60–74 years).
A similar approach was used to evaluate optimal thresholds for time above each cadence from 1 to 140 steps/min. Specifically, we 1) constructed an ROC curve for classifying adherence to PA guidelines from time ≥1 step/min, 2) identified the optimal threshold (min/day) maximizing Youden’s J statistic, 3) computed the corresponding classification accuracy, and 4) repeated this procedure for each cadence integer up to 140 steps/min. We then compared the performance of the 140 resulting optimal thresholds and identified the cadence and optimal threshold resulting in the highest AUC and the highest J statistic. This analysis was intended to augment comparisons of pre-specified step-based metrics (e.g., time ≥40, ≥70, and ≥100 steps/min) by exploring the full range of possible metrics derived from time above a given cadence.
RESULTS
The mean age was 41.1 years (range 18 to 74 years) with a mean BMI of 29.4 (standard error [SE], 0.1) kg/m2. Approximately half of Hispanic/Latino adults were women (52%), a similar proportion were married/partnered (49%), about a third were employed full-time (>35 hrs/week; 34%), most had been in the US 50 states/DC for ≥10 years (50%) or were US-born (23%), and most had a language preference of Spanish (75%). The largest Hispanic/Latino background groups were Mexican (37%), Cuban (20%), and Puerto Rican (16%). The mean (SE) wear time and number of adherent days were 15.9 (0.07) hrs/day and 5.1 (0.02) days, respectively. Sample characteristics stratified by sex are presented in Supplemental Table 2 (n = 12,528) (see Supplemental Digital Content 2, Sample sociodemographic and sociocultural characteristics overall and by sex and Hispanic/Latino background).
Aim 1: Distributions of Step-Based Metrics
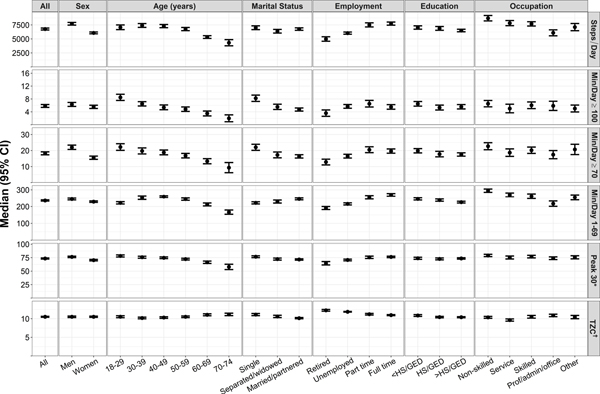
The weighted median (95% CI) for each step-based metric overall and by sociodemographic characteristics and BMI are presented in Figure 1, while medians according to site and sociocultural characteristics are presented in Figure 2. Exact values are provided in Supplemental Table 3 (see Supplemental Digital Content 3, Step-based metric weighted medians and 95% CIs for the total sample and by subgroups) and estimates for the 10th, 25th, 75th, and 90th percentiles as well as time in cadence bands Supplemental Table 4 and Supplemental Figures 1 and 2 (see Supplemental Digital Content 4, Step-based metric weighted 10th, 25th, 50th, 75th, and 90th percentile values with 95% CIs for the total sample and by subgroups; and Supplemental Digital Content 5, Wear time-adjusted step-based metric descriptives overall and by sociodemographic groups, and by BMI, site, and sociocultural characteristics). Overall, Hispanic/Latino adults accumulated a median of 6,770 steps/day, had a median peak 30-min cadence of 74 steps/min, and spent medians of 5.8 mins/day at ≥100 steps/min, 18.3 min/day at ≥70 steps/min, 49.5 mins/day at ≥40 steps/min, 3.9 hrs/day at 1–69 steps/min, and 10.5 hours/day at 0 steps/min.
Figure 1.
Median step-based metrics for HCHS/SOL overall and by sociodemographic groups for HCHS/SOL (N=12,528). Values were standardized to U.S. 2010 Census Population by weighting for survey design, nonresponse, and missing accelerometer data and adjusting for age. *Peak 30-min cadence, units are steps/min. †Daily time at zero cadence (0 steps/min) adjusted for wear time, units are hours/day. CI, confidence interval; Min/day ≥40, daily mins ≥40 steps/min; Min/day ≥70, daily mins ≥70 steps/min; Min/day ≥100, daily mins ≥100 steps/min.
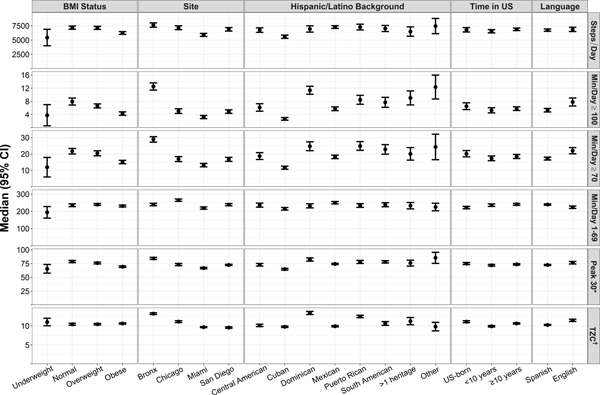
Figure 2.
Step-based metric descriptives by BMI, site, and sociocultural characteristics for HCHS/SOL (N=12,528). Values were standardized to U.S. 2010 Census Population by weighting for survey design, nonresponse, and missing accelerometer data and adjusting for age. *Peak 30-min cadence, units are steps/min. †Daily time at zero cadence (0 steps/min) adjusted for wear time, units are hours/day. CI, confidence interval; Min/day ≥40, daily mins ≥40 steps/min; Min/day ≥70, daily mins ≥70 steps/min; Min/day ≥100, daily mins ≥100 steps/min.
Based on the differences in median values, women accumulated ~1,600 (24%) fewer steps/day and ~6.5 (35%) fewer min/day at ≥70 step/min than men. Higher age and BMI were associated with monotonic decreases in time ≥100 steps/min and time ≥70 steps/min (Figure 1) while adults ≥60 years of age had 1,400–3,100 (24–53%) fewer steps/day than younger age groups. Additionally, single adults accumulated 24–54% more time at ≥100 and ≥70 steps/min than both separated/widowed and married/partnered adults. Employment status, from unemployed to part-time to full-time, was associated with greater step volumes and times at 1–69 steps/min and – when stratified by current occupation – non-skilled workers had the highest step volume (~8,700 steps/day) while those with a professional/administrative/office occupation had the lowest step volumes and times at 1–69 steps/min.
Median times ≥100 and ≥70 steps/min were higher for the Bronx site and lower for the Miami site compared to the other study sites. Additionally, among Hispanic/Latino background subgroups, Cuban adults had the lowest median step volume (~5,500 steps/day), times ≥100 and ≥70 step/min, and peak 30-min cadence while Dominican and Puerto Rican adults had higher time at zero cadence than other backgrounds. However, Dominican adults also had 2.9–8.7 min/day (29–124%) more time at ≥100 steps/min than South American, Central American, or Mexican populations. Finally, adults who preferred English spent 4.8 min/day (25%) longer at ≥70 steps/min and 2.5 min/day (38%) longer at ≥100 steps/min compared to those who preferred Spanish. Trends did not change after adjusting for wear time (see Supplemental Figures 1, 2 and 3, Supplemental Digital Content 5, Wear time-adjusted step-mased metric descriptives overall and by sociodemographic groups; by BMI, site, and sociocultural characteristics; and wear time-adjusted median daily time at or above each cadence from 1 to 140 steps/min).
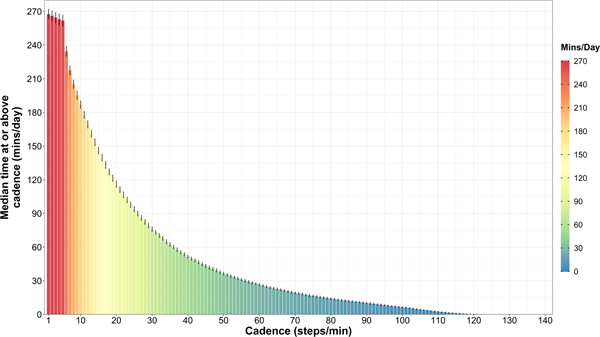
Medians and 95% CIs for times above each minimum cadence from 1 to 140 steps/min (in 1 step/min intervals) are shown in Figure 3. Daily time at ≥1 through ≥5 steps/min were similar (268 to 265 min/day) – indicating that few minutes registered with a cadence of 1–5 steps/min – but dropped to 234 min/day at ≥6 steps/min and continued to decrease curvilinearly with increasing minimum cadence (e.g., 76 and 27 min/day at ≥30 and ≥60 steps/min, respectively).
Figure 3.
Median (95% CI) daily time at or above each cadence from 1 to 140 steps/min among HCHS/SOL (N=12,528). All values were standardized to U.S. 2010 Census Population and weighted for survey design, nonresponse, and missing accelerometer data. CI, confidence interval.
Aim 2: Correlations Between Step-Based Metrics, Activity Counts, and Self-Report
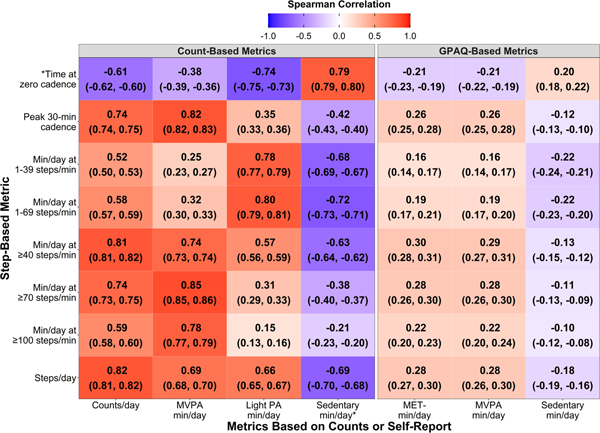
Daily count volume (counts/day) was most strongly correlated with step volume (rs = 0.82) and time ≥40 steps/min (0.81; Figure 4). Daily minutes of MVPA from counts were most strongly correlated with time ≥70 steps/min (0.85) followed by peak 30-min cadence (0.82), while the correlation between daily MVPA and time ≥100 steps/min was slightly weaker (0.78). Count-derived time in light PA and sedentary behavior were most strongly correlated with time at 1–69 steps/min (0.80) and time at zero cadence (0.79), respectively.
Figure 4.
Spearman correlations (95% CIs) between step-based metrics and metrics based on counts or self-report (GPAQ) in the total sample (N=12,528). Values presented as Spearman correlation (95% CI). *Adjusted for wear time. CI, confidence interval; GPAQ, Global Physical Activity Questionnaire; PA, Physical activity; MVPA, moderate-to-vigorous intensity physical activity; MET, Metabolic equivalents.
Associations between steps-based metrics and metrics based on self-report were notably weaker than those with metrics from counts (all rs ≤0.30; Figure 4). Self-reported MET-min/day and MVPA min/day were both most strongly correlated with time ≥40 steps/min (0.30 and 0.29, respectively) followed by step volume and time ≥70 steps/min (all rs = 0.28). Sedentary min/day from self-report had a positive correlation with time at zero cadence (0.20), but this correlation was slightly weaker those with time at 1–39 and 1–69 steps/min (both rs = −0.22).
Aim 3: Step-Based Translations of Physical Activity Guidelines
In the ROC analyses using step-based metrics to classify participants meeting US national PA guidelines, operationalizing the guidelines using counts resulted in higher optimal thresholds, AUC values, and classification accuracies compared to when based on self-reported MVPA (Table 1). For example, accumulating 6,947 and 6,326 steps/day were associated with meeting PA guidelines defined using MVPA from counts (AUC = 0.84) and self-report (AUC = 0.64), respectively.
Table 1.
Step-based metric optimal thresholds and corresponding classification accuracies for categorizing meeting PA guidelines operationalized from activity counts or self-report (N=12,528)
| Threshold (95% CI) | AUC (95% CI) | Sensitivity | Specificity | PPVa | NPVa | Accuracy | J | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Meeting PAG based on counts | ||||||||
| Steps/day | 6947 (6822, 7329) | 0.84 (0.84, 0.85) | 0.82 | 0.70 | 0.67 | 0.84 | 0.75 | 0.52 |
| Min/day ≥40 steps/min | 50.4 (45.9, 50.6) | 0.86 (0.85, 0.87) | 0.85 | 0.72 | 0.70 | 0.87 | 0.77 | 0.57 |
| Min/day ≥70 steps/min | 22.9 (21.3, 23.4) | 0.92 (0.92, 0.93) | 0.84 | 0.86 | 0.82 | 0.88 | 0.85 | 0.70 |
| Min/day ≥100 steps/min | 10.3 (10.1, 10.4) | 0.88 (0.88, 0.89) | 0.75 | 0.88 | 0.85 | 0.83 | 0.83 | 0.63 |
| Peak 30-min cadenceb | 79.3 (78.2, 81.2) | 0.91 (0.91, 0.92) | 0.81 | 0.84 | 0.81 | 0.86 | 0.83 | 0.65 |
| Meeting PAG based on self-report | ||||||||
| Steps/day | 6326 (5801, 7259) | 0.64 (0.63, 0.65) | 0.63 | 0.58 | 0.75 | 0.43 | 0.61 | 0.21 |
| Min/day ≥40 steps/min | 46.8 (39.8, 51.6) | 0.65 (0.64, 0.66) | 0.62 | 0.60 | 0.76 | 0.43 | 0.61 | 0.22 |
| Min/day ≥70 steps/min | 18.2 (14.2, 21.3) | 0.66 (0.65, 0.67) | 0.59 | 0.64 | 0.77 | 0.43 | 0.61 | 0.23 |
| Min/day ≥100 steps/min | 6.5 (4.2, 7.9) | 0.64 (0.63, 0.65) | 0.56 | 0.66 | 0.77 | 0.42 | 0.59 | 0.22 |
| Peak 30-min cadenceb | 69.6 (66.7, 77.4) | 0.66 (0.65, 0.67) | 0.66 | 0.57 | 0.76 | 0.45 | 0.63 | 0.23 |
PAG, physical activity guidelines; CI, confidence interval; PPV, positive predictive value; NPV, positive predictive value; J, Youden’s J statistic
Accuracy = proportion of sample correctly classified; J = sensitivity + specificity – 1; 95% CIs calculated using bootstraps with 20,000 replicates
Values standardized to U.S. 2010 Census Population and weighted for survey design, nonresponse, and missing accelerometer data
Units are steps/min
When meeting PA guidelines was based on counts, time ≥70 steps/min had the highest AUC (0.92) and overall accuracy (0.85), closely followed by peak 30-min cadence (0.91 and 0.83, respectively). Similarly, when meeting PA guidelines was based on self-report, time ≥70 steps/min and peak 30-min cadence both had the highest AUC value (0.66) while overall accuracy was marginally greater for peak 30-min cadence (0.63 versus 0.62 for time ≥70 steps/min). However, the other step-based metrics classified those meeting PA guidelines according to self-report with only slightly lower AUC (0.64–65) and accuracy (0.59–0.61) values (Table 1). When these ROC analyses were stratified by age (see Supplemental Tables 5 and 6, Supplemental Digital Content 6, Optimal thresholds and corresponding classification accuracies by three age groups, and Optimal thresholds and corresponding classification accuracies by six age groups), optimal thresholds were similar across the three age groups when meeting PA guidelines was based on counts. When guidelines were based on self-reported MVPA, older age was more strongly associated with a lower optimal threshold for step volume (range of 6,225 to 8046 steps/day) and times ≥40, 70, and 100 steps/min (ranges of 36.5–67.1, 10.7–24.9, and 3.6–11.2 min/day, respectively).
Among cadences from 1 to 140 steps/min, the highest AUC for classifying count-derived and self-reported meeting of PA guidelines times ≥68 steps/min (0.92) and ≥62 steps/min (0.66), respectively (Figure 5). The highest J statistic values resulted from using a cadence (optimal threshold; sensitivity, specificity) of ≥69 steps/min (22.8 min/day; 0.85, 0.84) and ≥68 steps/min (18.7 min/day; 0.61, 0.63) to classify guidelines from counts and self-report, respectively.
Figure 5.
Optimal thresholds and corresponding classification accuracies for classifying meeting PA guidelines with time (min/day) above each minimum cadence from 1 to 140 steps (N=12,528).
DISCUSSION
In this study of US Hispanic/Latino adults, we observed medians of approximately 6,800 steps/day, 20 min/day at ≥70 steps/min, 4 hrs/day at 1–69 steps/min, and 11 hrs/day at 0 steps/min. However, volumes and patterns of stepping varied substantially between sociodemographic and sociocultural groups (Figures 1 and 2). Additionally, as one approach to informing step-based translations of US national PA guidelines, we examined the correspondence between step-based metrics and PA levels derived from activity counts and self-report. Attaining ≥150 min/week of MVPA was associated with accruing at least 6,000–7,000 steps/day. However, time at ≥70 steps/min had 1) the strongest correlation with count-defined MVPA and one of the strongest correlations with self-reported MVPA, 2) the greatest capacity for classifying participants meeting PA guidelines, and 3) optimal thresholds that were consistent with the recommended minimum levels of MVPA (i.e., ~20 min/day). These findings support that free-living, accelerometer-assessed time ≥70 steps/min provides approximate translations of MVPA from Actical counts and self-report.
Distributions of Step-Based Metrics
Volumes and patterns of stepping varied substantially between sociodemographic and sociocultural groups. Step-based activity levels were generally lower among adults who were female, older, had obesity, or were Cuban. However, other trends by subgroup were only similar between step volume and time at 1–69 steps/min or between times at ≥70 and ≥100 steps/min. For example, step volume and time at 1–69 step/min had greater differences by employment status and occupation, indicating occupational PA may be associated with a greater volume of ambulatory activity levels, accrued through more time at slower cadences. Times at ≥70 and ≥100 steps/min had negative, monotonic associations with age and BMI (Figure 1) and were higher in adults who were single, Dominican, Puerto Rican, or had indicators of greater acculturation (US-born or preferred English). A prior study in this cohort (33) similarly reported higher accelerometer-assessed MVPA in Hispanic/Latino men compared to women, younger compared to older adults, and individuals of Dominican or Puerto Rican background particularly in comparison to those who were Cuban, who had the lowest levels of MVPA. Comparing the step-based activity levels reported herein to those of the general US adult population in the National Health and Nutrition Examination Survey (NHANES) is obscured by two factors: the relevant estimates available from NHANES (27, 40) are reported as means instead of medians and are from an accelerometer (ActiGraph 7164) with a more sensitive step detection algorithm (40, 41). However, Tudor-Locke et al. (40) censored steps taken at a low intensity in NHANES 2005–2006 to produce step counts more congruent with other devices. They reported that US adults accumulated a mean (standard deviation) of 6,540 (106) steps/day, which is 7% lower than the median and 21% lower than the mean step volume of the Hispanic/Latino population included herein (6,992 and 7,935 steps/day, respectively).
Associations Between Step-Based Metrics, Activity Counts, and Self-Report
Since the 2018 PA guidelines Advisory Committee (3, 8) highlighted the need for evidence to inform step-based PA recommendations, several studies have examined dose-response relationships between stepping and health outcomes (11, 12). Examining the correspondence between steps, activity counts, and self-report can complement this research by enabling approximate conversions between these measures to facilitate harmonizing methods and evidence across the field (13, 14).
Daily count volume (counts/day) was most strongly correlated with step volume (rs = 0.82), This correlation is slightly stronger than that previously reported (0.79) between step and count volumes from the ActiGraph 7164 accelerometer in NHANES data (42). Count-derived time in MVPA, light PA, and sedentary behavior had their strongest correlations with time ≥70 steps/min (0.85), time at 1–69 steps/min (0.80), and time at zero cadence (0.79), respectively. These associations were stronger and had more variability across step-based metrics than those with self-reported physical behaviors. For example, PA volume (MET-min/day) and MVPA from self-report were most strongly correlated with time at ≥40 steps/min (0.30 and 0.29, respectively), but had similar correlations with step volume and time ≥70 steps/min (all rs = 0.28). Additionally, the strongest correlation for self-reported sedentary time was with time at 1–69 steps/min (−0.22), yet its correlation with time at zero cadence (0.20) was only marginally weaker. This negative association between time at 1–69 steps/min and self-reported sedentary time may be analogous to inverse relationship observed between light PA and sedentary behavior (43, 44). Together these results suggests that time ≥70 steps/min, time at 1–69 steps/min, and time at zero cadence may be reasonable proxies for free-living, accelerometer-assessed times in MVPA, light PA, and sedentary behavior, respectively.
Step-Based Translations of Physical Activity Guidelines
Our ROC analyses provide more direct step-based translations of US national PA guidelines (3). We found that, overall, attaining ≥150 min/week of MVPA from counts and self-report was associated with accruing at least 6,900 and 6,300 steps/day, respectively. In a 2011 review summarizing six cross-sectional studies, Tudor-Locke et al. (13) concluded that 7,000–8,000 steps/day was associated with attaining recommended levels of MVPA. However, the studies informing this result 1) assessed MVPA through accelerometry or direct observation (none used self-report), 2) reported thresholds based on the classification accuracy of a set steps/day value (e.g., the 25th percentile) or the average step volume of all participants meeting PA guidelines, and 3) did not examine any step-based metrics beyond step volume. Although some similar studies have been conducted in youth (45, 46), to our knowledge, this is the first attempt we are aware of to calibrate step-based translations of PA guidelines using an analytic approach that maximizes a measure of performance (i.e., Youden’s J statistic) in adults and to do so for a variety of step-based metrics, encompassing all cadence thresholds within the range of walking behavior.
The potential value of considering other step-based metrics was shown in our ROC analyses. Time at ≥70 steps/min and peak 30-min cadence demonstrated the greatest ability to classify adults meeting PA guidelines, with AUC values and J statistics that were 0.07–0.17 and 0.01–0.03 higher than those for step volume when PA guidelines were based on counts and steps, respectively. Additionally, while laboratory-based studies of directly-observed steps have reported that continuous walking at ~100 steps/min is associated with moderate intensity (10, 47) and free-living walking behavior has been characterized using incremental 20 step/min “cadence bands” constructed from expert opinion (10, 27), we are not aware of any empirically-supported cadence thresholds for classifying intensity from free-living accelerometer data. Therefore, we chose to extend our evaluations of pre-specified step-based metrics by conducting ROC analyses evaluating each cadence threshold from 1 to 140 steps/min (Figure 5). The results of these analyses further support the strong correspondence between time ≥70 steps/min and MVPA in free-living Actical accelerometer data collected from US Hispanic/Latino adults.
The minimum amount of MVPA recommended in current national and global PA guidelines (150 min/week) averages to ~20 min/day. Interestingly, this daily duration of activity is similar to the optimal thresholds of time ≥70 steps/min that corresponded to meeting PA guidelines when using MVPA from counts (22.9 min/day) or self-report (18.2 min/day). These optimal threshold values, their classification accuracies, and the correlations observed in Aim 2 all support that time ≥70 steps/min provides reasonable translations of time MVPA in these data, with ~20 min/day corresponding to PA guidelines. Whether this result is generalizable to other populations and to other accelerometers with different step detection algorithms requires further research. Additionally, we explored optimal thresholds by age group (see Supplemental Figures 1 and 2, Supplemental Digital Content 5) and observed some variation in ROC analyses using self-reported MVPA. However, we have not national PA guidelines meant for simple public health messaging recommend ≥150 min/week of absolutely-defined moderate intensity PA, or an equivalent volume of vigorous PA, for all adults regardless of age.
Strengths and Limitations
This study is the first to describe patterns of stepping in a large sample of US Hispanic/Latino adults from diverse backgrounds. We also excluded the first wear day for participants who wore the device the same day as their clinic visit, which may help reduce bias due to reactivity (48). In an attempt to be comprehensive, our analyses incorporated a variety of step-based metrics, including a systematic evaluation of time above the full range of walking cadences. Consistencies in the results provided by two analytic approaches (correlations and ROC analyses) with two established methods of PA assessment (activity counts and self-report) further strengthen our results.
However, we did not employ a direct measure of PA levels. Self-report is subject to recall and response bias (5), and hip-worn accelerometers may underestimate PA from bicycling, swimming, and activities involving upper-body movement (1, 6). Additionally, the Actical count cutpoint available for sedentary behavior in adults is already based on free-living time at 0 steps/min. We also acknowledge that applying PA guidelines to accelerometer data can be problematic because they are mainly based on studies of self-reported PA (1). Nonetheless, there is no criterion measure of free-living physical behavior and – despite their limitations – the GPAQ is commonly used for assessing PA (31), current guidelines are largely based on studies of self-reported PA (1), and step-based metrics implicitly focus on ambulatory PA, which is the most commonly reported form of PA (49). Additionally, accelerometer cutpoints are largely calibrated to measured intensity levels (29, 30) and are commonly used in epidemiological research (3, 6). Therefore, we argue that translating activity counts to step-based metrics has value through enabling future step-based recommendations to be informed by and congruent with other epidemiological and methodological PA research (13, 14). Because no accelerometer-specific PA guidelines exist, we focused our count-related ROC analyses on AUC – rather than a characteristic of a single threshold (38) – and also based our conclusions on the correlations and ROC analyses with self-report. Step counts in this study were also collected in 1-min epochs and therefore reflect the average cadence over that minute, as opposed to an exact indicator of instantaneous behavior. Finally, participants were recruited from only four US cities and we used Actical accelerometers with 1-min epoch length. Our results may not be generalizable to other populations, accelerometers with a different step-counting algorithm, or epoch length (50).
CONCLUSIONS
Step counting has been embraced as a simple and increasingly accessible means of tracking and communicating PA levels (3, 7, 8, 10). We have provided normative values (based on percentiles) of step-based metrics in Hispanic/Latino adults recruited from four US cities, with overall medians of approximately 7,000 steps/day, 20 min/day at ≥70 steps/min, 4 hrs/day at 1–69 steps/min, and 11 hrs/day at 0 steps/min. We also demonstrated how volumes and patterns of stepping vary across sociodemographic and sociocultural groups. These values have utility for monitoring trends over time, facilitating research and program planning, and aiding in data interpretation (15). Additionally, with the growing interest in creating step-based PA recommendations (3, 8), we examined the correspondence between steps, activity counts, and self-reported PA. Our results indicate that ≥70 steps/min, time at 1–69 steps/min, and time at zero cadence may be reasonable proxies for MVPA, light PA, and sedentary behavior, respectively. Additionally, based on translations of ≥150 min/week of count-derived and self-reported MVPA, US national PA guidelines corresponded to accumulating 6,000–7,000 steps/day or ~20 min/day at ≥70 steps/min. Future studies are needed to expand these findings to other populations and devices. This evidence should be considered alongside dose-response relationships between stepping patterns and health outcomes (11, 12) to develop step-based public health recommendations that are consistent with prior literature and established PA guidelines, while better communicating the levels of PA required to attain the majority of health benefits.
Supplementary Material
Table S1: Definitions of step-based metrics
Table S2: Sample sociodemographic and sociocultural characteristics overall and by sex and Hispanic/Latino background
Table S3: Step-based metric weighted medians and 95% CIs for the total sample and by subgroups
Table S4: Step-based metric weighted 10th, 25th, 50th, 75th, and 90th percentile values with 95% CIs for the total sample and by subgroups
Figure S1 - SDC 5.1. Wear time-adjusted step-based metric descriptives overall and by sociodemographic groups (N=12,528)
Figure S2 - SDC 5.2. Wear time-adjusted step-based metric descriptives by BMI, site, and sociocultural characteristics (N=12,528)
Figure S3 - SDC 5.3. Wear time-adjusted median (95% CI) daily time at or above each cadence from 1 to 140 steps/min
Table S5 - SDC 6.1. Optimal thresholds and corresponding classification accuracies by three age groups
Table S6 - SDC 6.2. Optimal thresholds and corresponding classification accuracies by six age groups
Acknowledgments
The authors thank the staff and participants of HCHS/SOL for their important contributions. A complete list of staff and investigators has been provided by Sorlie P., et al. in Ann Epidemiol. 2010 Aug;20: 642-649 and is also available on the study website http://www.cscc.unc.edu/hchs/. The work of C.C.M. and C.C.C. was funded by the National Health Institute (NIH), National Heart, Lung, and Blood Institute (NHLBI) National Research Service Award (T32-HL007055). The work of D.S.A, Y.M.R. and K.R.E was funded by NIH R01HL136266. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the NIH NHLBI to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), University of Illinois at Chicago (HHSN2682013000031), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following NIH Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements.
Funding Source:
The work of C.C.M. and C.C.C. was funded by the National Health Institute (NIH), National Heart, Lung, and Blood Institute (NHLBI) National Research Service Award (T32-HL007055). The work of D.S.A, Y.M.R. and K.R.E was funded by NIH R01HL136266. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the NIH NHLBI to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), University of Illinois at Chicago (HHSN2682013000031), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following NIH Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of the present study do not constitute endorsement by the American College of Sports Medicine. The content is solely the responsibility of the authors and does represent the official views of the NIH.
Footnotes
Conflicts of interest
The authors declare they have no conflicts of interest. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of the present study do not constitute endorsement by the American College of Sports Medicine. The content is solely the responsibility of the authors and does represent the official views of the NIH.
REFERENCES
- 1.Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med. 2014;48(13):1019–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katzmarzyk PT, Friedenreich C, Shiroma EJ, Lee IM. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br J Sports Med. 2022;56(2):101–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 4.Lee IM, Shiroma EJ. Using accelerometers to measure physical activity in large-scale epidemiological studies: issues and challenges. Br J Sports Med. 2014;48(3):197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med. 2003;37(3):197–206; discussion 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc. 2005;37(11 Suppl):S582–8. [DOI] [PubMed] [Google Scholar]
- 7.Bassett DR Jr., Toth LP, LaMunion SR, Crouter SE. Step counting: a review of measurement considerations and health-related applications. Sports Med. 2017;47(7):1303–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraus WE, Janz KF, Powell KE, et al. Daily step counts for measuring physical activity exposure and its relation to health. Med Sci Sports Exerc. 2019;51(6):1206–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore CC, Aguiar EJ, Ducharme SW, Tudor Locke C. Development of a cadence-based metabolic equation for walking. Med Sci Sports Exerc. 2021;53(1):165–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tudor-Locke C, Han H, Aguiar EJ, et al. How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sports Med. 2018;52(12):776–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall KS, Hyde ET, Bassett DR, et al. Systematic review of the prospective association of daily step counts with risk of mortality, cardiovascular disease, and dysglycemia. Int J Behav Nutr Phys Act. 2020;17(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paluch AE, Bajpai S, Bassett DR, et al. Daily steps and all-cause mortality: a meta-analysis of 15 international cohorts. Lancet Public Health. 2022;7(3):e219–e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tudor-Locke C, Craig CL, Brown WJ, et al. How many steps/day are enough? For adults. Int J Behav Nutr Phys Act. 2011;8:79.21798015 [Google Scholar]
- 14.Tudor-Locke C, Bassett DR Jr. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34(1):1–8. [DOI] [PubMed] [Google Scholar]
- 15.Myers AM. Program Evaluation for Exercise Leaders. Champaign, IL: Human Kinetics; 1999, 168 p. [Google Scholar]
- 16.Takamiya T, Inoue S. Trends in step-determined physical activity among Japanese adults from 1995 to 2016. Med Sci Sports Exerc. 2019;51(9):1852–9. [DOI] [PubMed] [Google Scholar]
- 17.Tudor-Locke C, Schuna JM Jr., Barreira TV, et al. Normative steps/day values for older adults: NHANES 2005–2006. J Gerontol A Biol Sci Med Sci. 2013;68(11):1426–32. [DOI] [PubMed] [Google Scholar]
- 18.Rosenberg M, Mills C, McCormack G et al. Physical Activity Levels of Western Australian Adults 2009. Perth: Health Promotion Evaluation Unit, The University of Western Australia,2010. [Google Scholar]
- 19.Carlson SA, Fulton JE, Schoenborn CA, Loustalot F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. Am J Prev Med. 2010;39(4):305–13. [DOI] [PubMed] [Google Scholar]
- 20.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. [DOI] [PubMed] [Google Scholar]
- 21.Ham SA, Ainsworth BE. Disparities in data on Healthy People 2010 physical activity objectives collected by accelerometry and self-report. Am J Public Health. 2010;100 Suppl 1(Suppl 1):S263–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):642–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):629–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.John D, Freedson P. ActiGraph and Actical physical activity monitors: a peek under the hood. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S86–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evenson KR, Sotres-Alvarez D, Deng YU, et al. Accelerometer adherence and performance in a cohort study of US Hispanic adults. Med Sci Sports Exerc. 2015;47(4):725–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tudor-Locke C, Camhi SM, Leonardi C, et al. Patterns of adult stepping cadence in the 2005–2006 NHANES. Prev Med. 2011;53(3):178–81. [DOI] [PubMed] [Google Scholar]
- 28.Wong SL, Colley R, Connor Gorber S, Tremblay M. Actical accelerometer sedentary activity thresholds for adults. J Phys Act Health. 2011;8(4):587–91. [DOI] [PubMed] [Google Scholar]
- 29.Colley R, Connor Gorber S, Tremblay MS. Quality control and data reduction procedures for accelerometry-derived measures of physical activity. Health Rep. 2010;21(1):63–9. [PubMed] [Google Scholar]
- 30.Colley RC, Tremblay MS. Moderate and vigorous physical activity intensity cut-points for the Actical accelerometer. J Sports Sci. 2011;29(8):783–9. [DOI] [PubMed] [Google Scholar]
- 31.Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6(6):790–804. [DOI] [PubMed] [Google Scholar]
- 32.Hoos T, Espinoza N, Marshall S, Arredondo EM. Validity of the Global Physical Activity Questionnaire (GPAQ) in adult Latinas. J Phys Act Health. 2012;9(5):698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arredondo EM, Sotres-Alvarez D, Stoutenberg M, et al. Physical activity levels in U.S. Latino/Hispanic adults: results from the Hispanic Community Health Study/Study of Latinos. Am J Prev Med. 2016;50(4):500–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22(3):278–95. [DOI] [PubMed] [Google Scholar]
- 35.Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124(1):17–27. [DOI] [PubMed] [Google Scholar]
- 36.Yeo D, Mantel H, Liu T. Bootstrap variance estimation for the National Population Health Survey. American Statistical Association, Proceedings of the Survey Research Methods. 1999. [Google Scholar]
- 37.Woodruff RS. Confidence intervals for medians and other position measures. J Am Stat Assoc. 1952;47(260):635–46. [Google Scholar]
- 38.Fawcett T. Introduction to ROC analysis. Pattern Recognit Lett. 2006;27(8):861–74. [Google Scholar]
- 39.Robin X, Turck N, Hainard A, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps per day in US adults. Med Sci Sports Exerc. 2009;41(7):1384–91. [DOI] [PubMed] [Google Scholar]
- 41.Le Masurier GC, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Med Sci Sports Exerc. 2003;35(5):867–71. [DOI] [PubMed] [Google Scholar]
- 42.Tudor-Locke C, Johnson WD, Katzmarzyk PT. Relationship between accelerometer-determined steps/day and other accelerometer outputs in US adults. J Phys Act Health. 2011;8(3):410–9. [DOI] [PubMed] [Google Scholar]
- 43.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31(2):369–71. [DOI] [PubMed] [Google Scholar]
- 44.Tudor-Locke C, Leonardi C, Johnson WD, Katzmarzyk PT. Time spent in physical activity and sedentary behaviors on the working day: the American time use survey. J Occup Environ Med. 2011;53(12):1382–7. [DOI] [PubMed] [Google Scholar]
- 45.Mayorga-Vega D, Casado-Robles C, López-Fernández I, Viciana J. A comparison of the utility of different step-indices to translate the physical activity recommendation in adolescents. J Sports Sci. 2021;39(4):469–79. [DOI] [PubMed] [Google Scholar]
- 46.Mayorga-Vega D, Casado-Robles C, Viciana J, López-Fernández I. Daily step-based recommendations related to moderate-to-vigorous physical activity and sedentary behavior in adolescents. J Sports Sci Med. 2019;18(4):586–95. [PMC free article] [PubMed] [Google Scholar]
- 47.Tudor-Locke C, Aguiar EJ, Han H, et al. Walking cadence (steps/min) and intensity in 21–40 year olds: CADENCE-adults. Int J Behav Nutr Phys Act. 2019;16(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baumann S, Groß S, Voigt L, et al. Pitfalls in accelerometer-based measurement of physical activity: The presence of reactivity in an adult population. Scand J Med Sci Sports. 2018;28(3):1056–63. [DOI] [PubMed] [Google Scholar]
- 49.Saint-Maurice PF, Berrigan D, Whitfield GP, et al. Amount, type, and timing of domain-specific moderate to vigorous physical activity among US adults. J Phys Act Health. 2021;18(S1):S114–S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Definitions of step-based metrics
Table S2: Sample sociodemographic and sociocultural characteristics overall and by sex and Hispanic/Latino background
Table S3: Step-based metric weighted medians and 95% CIs for the total sample and by subgroups
Table S4: Step-based metric weighted 10th, 25th, 50th, 75th, and 90th percentile values with 95% CIs for the total sample and by subgroups
Figure S1 - SDC 5.1. Wear time-adjusted step-based metric descriptives overall and by sociodemographic groups (N=12,528)
Figure S2 - SDC 5.2. Wear time-adjusted step-based metric descriptives by BMI, site, and sociocultural characteristics (N=12,528)
Figure S3 - SDC 5.3. Wear time-adjusted median (95% CI) daily time at or above each cadence from 1 to 140 steps/min
Table S5 - SDC 6.1. Optimal thresholds and corresponding classification accuracies by three age groups
Table S6 - SDC 6.2. Optimal thresholds and corresponding classification accuracies by six age groups