Abstract
Background
Pancreatic cancer is one of the deadliest cancer types and represents a major unmet medical need. CheckMate 032 investigated safety and efficacy of nivolumab monotherapy and nivolumab plus ipilimumab with/without cobimetinib in advanced/metastatic solid tumors, including pancreatic cancer.
Methods
In the original pancreatic cancer cohort, previously treated patients (≥1 prior regimen) with advanced/metastatic pancreatic adenocarcinoma were assigned to nivolumab 3 mg/kg every 2 weeks (monotherapy arm) or nivolumab 1 mg/kg and ipilimumab 1 mg/kg or 3 mg/kg every 3 weeks for four doses, followed by nivolumab 3 mg/kg every 2 weeks (combination arm). A subsequent modified pancreatic cohort (one or two prior regimens) received nivolumab 3 mg/kg every 2 weeks, ipilimumab 1 mg/kg every 6 weeks, and cobimetinib 60 mg orally once daily for 21 days on and 7 days off (triplet arm). The primary endpoint was investigator-assessed objective response rate (ORR). Secondary endpoints were investigator-assessed progression-free survival (PFS), PFS rate, overall survival (OS), OS rate, safety, and tolerability. Additionally, ORR, PFS, and duration of response were assessed by blinded independent central review (BICR) in the triplet arm.
Results
18 patients received nivolumab monotherapy, 21 received nivolumab plus ipilimumab, and 30 received nivolumab plus ipilimumab plus cobimetinib. In the triplet arm, partial responses were observed in two patients per investigator (ORR 6.7% (95% CI 0.8% to 22.1%)) and in three patients per BICR (ORR 10% (95% CI 2.1% to 26.5%)); no responses were observed in the other arms. Median (95% CI) PFS per investigator was 1.4 (1.3 to 2.0), 1.4 (1.2 to 2.7), and 3.0 (1.5 to 4.1) months for the monotherapy, nivolumab plus ipilimumab, and triplet arms, respectively. Median (95% CI) OS was 5.1 (2.0 to 9.0) months, 4.0 (1.9 to 5.6) months, and 6.2 (3.9 to 11.4) months, respectively. Most treatment-related adverse events were grade 2 or less.
Conclusions
Nivolumab with or without ipilimumab did not elicit objective responses in previously treated patients with advanced pancreatic adenocarcinoma, although three confirmed partial responses and manageable safety were observed with cobimetinib-containing triplet therapy. The small sample size and differences in baseline disease-specific characteristics between arms limit interpretation of these results.
Keywords: Nivolumab, Ipilimumab, Immune Checkpoint Inhibitors, Immunotherapy
WHAT IS ALREADY KNOWN ON THIS TOPIC
Pancreatic cancer has a high mortality rate, with a 5-year relative survival rate of 12.5%, underscoring the need for more treatment options.
Immunotherapy with single or dual checkpoint inhibitors or in combination with other agents has transformed the treatment of many solid tumors, but their clinical application in pancreatic cancer remains investigational.
WHAT THIS STUDY ADDS
Given the distinct and complementary mechanisms of action of nivolumab, ipilimumab, and the MEK inhibitor cobimetinib, this study was conducted to investigate their efficacy and safety in patients with advanced/metastatic pancreatic adenocarcinoma.
In the pancreatic cancer cohorts of CheckMate 032, three confirmed partial responses and a manageable safety profile were observed with nivolumab plus ipilimumab plus cobimetinib triplet therapy, whereas no responses were observed with nivolumab monotherapy or nivolumab plus ipilimumab combination therapy.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The small sample size and differences in baseline disease-specific characteristics between treatment arms limit interpretation of these results. Further studies are needed to identify novel combinations of checkpoint inhibitors with other antineoplastic agents, such as targeted therapies or chemotherapies, which may benefit previously treated patients with advanced pancreatic adenocarcinoma.
Introduction
Pancreatic cancer is one of the deadliest forms of cancer. It is the seventh-leading cause of cancer-related mortality worldwide.1 In the USA, the incidence of pancreatic cancer between 2000 and 2019 increased by about 1% annually in both men and women,2 and over 62,000 new cases and nearly 50,000 deaths from pancreatic carcinoma were estimated in 20223; the 5-year relative survival rate is 12.5% for all pancreatic cancer stages combined.3 Given the poor survival rate, especially in the advanced or metastatic setting, there is a critical need to investigate and develop new therapeutic options for this malignancy.4
Immune checkpoint inhibitors, such as nivolumab (a fully human monoclonal IgG4 programmed death-1 (PD-1) antibody) and ipilimumab (a cytotoxic T-lymphocyte antigen-4 (CTLA-4) antibody), have changed the treatment paradigm for several solid tumors; however, their clinical application in pancreatic cancer remains under investigation. In patients with locally advanced or metastatic pancreatic cancer, limited activity has been observed with ipilimumab monotherapy and its combinations.5 6 In a study of patients with various tumor types who received pembrolizumab monotherapy, objective response rate (ORR) was 18% in 22 patients with advanced microsatellite instability high/mismatch repair deficient (MSI-H/dMMR) pancreatic cancer, and median progression-free survival (PFS) and overall survival (OS) were 2.1 and 4.0 months, respectively.7 In patients with locally advanced or metastatic pancreatic cancer, combination therapy with gemcitabine plus nab-paclitaxel and either pembrolizumab8 or nivolumab9 resulted in an ORR of 20% and 18%, respectively; median PFS of 9.1 and 5.5 months, respectively; and median OS of 15.0 and 9.9 months, respectively.
Nivolumab and ipilimumab have distinct but complementary mechanisms of action that contribute to the restoration of antitumor T-cell function and induction of de novo antitumor T-cell responses, respectively.10–14 Combination therapy with these two agents is active in several tumor types15–18 and is approved for the treatment of unresectable/metastatic melanoma, metastatic non-small cell lung cancer, advanced renal cell carcinoma, MSI-H/dMMR metastatic colorectal cancer, hepatocellular carcinoma, and unresectable malignant pleural mesothelioma.19 Therefore, we sought to investigate if the combination of nivolumab plus ipilimumab has clinically relevant activity in patients with pancreatic cancer. Furthermore, the MEK pathway is a critical mediator in constitutively active KRAS mutated cancers, including most pancreatic ductal adenocarcinomas.20 21 Since MEK inhibitors in combination with PD-1 and CTLA-4 receptor blockade have been shown to exhibit synergistic antitumor activity in mouse models with increased tumor-infiltrating CD8+ T cells in CT26 tumors,22 we hypothesized that this combination may have similar activity in KRAS mutant tumors in the clinical setting.
The CheckMate 032 trial was originally designed to investigate the safety and efficacy of nivolumab monotherapy or nivolumab plus ipilimumab in patients with advanced or metastatic tumors including triple-negative breast cancer, gastric cancer, pancreatic cancer, small cell lung cancer, bladder/urothelial cancer, and ovarian cancer. An additional modified cohort of nivolumab plus ipilimumab and cobimetinib, an MEK inhibitor, was later added to the pancreatic cancer cohort. We report the results for the pancreatic cancer cohorts, including patients whose tumor did not respond to previous systemic therapy.
Methods
Study design and treatment
CheckMate 032 (NCT01928394) was a multicenter, open-label, two-stage, phase 1/2 trial to evaluate the safety and efficacy of nivolumab monotherapy or nivolumab plus ipilimumab in adults with advanced or metastatic solid tumors. The pancreatic cancer cohort enrolled patients at 16 sites in four countries (Finland, Spain, the UK, and the USA). Initially, the pancreatic cancer cohort had two arms: nivolumab monotherapy or nivolumab plus ipilimumab. Enrolment in these two arms began in October 2013. Based on minimal activity observed in the nivolumab monotherapy or combination therapy arms, the protocol (online supplemental file 2) was amended to include a third arm: nivolumab plus ipilimumab and cobimetinib (triplet therapy arm). Enrolment into the triplet therapy arm began in January 2017 (at sites in the USA only).
jitc-2023-007883supp002.pdf (2.1MB, pdf)
The original arms followed a modified Simon two-stage design to test whether nivolumab monotherapy or nivolumab plus ipilimumab yielded an ORR that was of clinical interest in pancreatic cancer. Only treatment arms that met an ORR threshold of 10% progressed from stage 1 to stage 2; enrolment to stage 2 in a given treatment arm could continue even if the other treatment arm(s) were still at stage 1. After completion of enrolment of the initial 40 patients, additional patients could be assigned to the nivolumab monotherapy arm or nivolumab plus ipilimumab combination arm up to a total of 100 patients (including those from stage 1).
In the monotherapy arm, nivolumab 3 mg/kg monotherapy was administered intravenously every 2 weeks. For combination therapy dose level 1, nivolumab 1 mg/kg intravenously and ipilimumab 1 mg/kg intravenously were administered every 3 weeks for four doses followed by nivolumab 3 mg/kg intravenously every 2 weeks. For combination therapy dose level 2, nivolumab 1 mg/kg intravenously plus ipilimumab 3 mg/kg intravenously were administered every 3 weeks for four doses, followed by nivolumab 3 mg/kg every 2 weeks. Patients in the nivolumab monotherapy arm who had confirmed progression were allowed to cross over to one of the nivolumab plus ipilimumab combination arms.
For the triplet arm, a one-stage design was used to treat 30 patients with nivolumab 3 mg/kg every 2 weeks, ipilimumab 1 mg/kg every 6 weeks and cobimetinib 60 mg orally once daily for 21 days on and 7 days off. No more than six patients were enrolled in the first week of the study, with subsequent enrolment of six or more patients per week during the first month. A scheduled safety review by the medical monitor occurred after 12 patients were treated and had been followed for at least 1 month. Patients received treatment until disease progression (investigator assessed, per Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1), unacceptable toxicity, withdrawal of consent, or the end of study, whichever occurred first. Treatment with nivolumab or nivolumab plus ipilimumab beyond initial disease progression was permitted based on investigator’s judgment.
Patients and eligibility requirements
The study population in the pancreatic cancer cohort included adults (≥18 years) with histologically confirmed advanced or metastatic pancreatic adenocarcinoma and no clinically relevant ascites at baseline (defined as not requiring paracentesis), measurable disease by CT or MRI per RECIST V.1.123 (radiographic tumor assessment within 28 days before the first dose), and Eastern Cooperative Oncology Group performance status (ECOG PS) of 0 or 1. Tumor MSI, KRAS, and RAF status were not assessed at baseline. Patients in the nivolumab monotherapy and nivolumab plus ipilimumab combination arms were required to have either best response of stable disease (SD) or progressive disease (PD), or refractory disease during or after at least one chemotherapy regimen in the metastatic/advanced setting, or have actively refused chemotherapy considered as standard treatment for the treatment of metastatic or locally advanced disease. For the triplet arm, patients were required to have had treatment with at least one, but not more than two, previous lines of chemotherapy in the metastatic/advanced setting, documented objective radiographic disease progression at study entry and Royal Marsden score 0 or 1, or have actively refused chemotherapy considered as standard treatment for the treatment of metastatic or locally advanced disease. Key exclusion criteria included active brain or leptomeningeal metastases; known or suspected autoimmune disease; hepatitis B, hepatitis C, or HIV infections; conditions requiring corticosteroids or other immunosuppressive medications within 14 days of first dose; and previous therapy with experimental antitumor vaccines or any T-cell costimulation or checkpoint pathways. Because cobimetinib was included in the triplet arm, patients with low left ventricular ejection fraction (<50% or below the institutional lower limit of normal) and ECG with corrected QT≥450 ms were excluded.
Endpoints and assessments
The primary endpoint was investigator-assessed ORR, defined as the number of patients with a best overall response of complete response (CR) or partial response (PR) divided by the number of treated patients. The ORR was further characterized by the duration of response (DOR) and the magnitude of reduction in tumor volume. Tumor assessments were done at screening and then every 6 weeks from the first dose for the first 24 weeks, then every 12 weeks while on treatment or on treatment hold for any reason until disease progression or treatment discontinuation, whichever occurred later. Secondary endpoints were investigator-assessed PFS, PFS rate, OS, and OS rate. Additionally, ORR, PFS, and DOR were assessed by blinded independent central review (BICR) in the triplet arm. Other secondary endpoints were safety and tolerability, analyzed by the incidence of all on-study adverse events (AEs; collected continuously during the treatment period and for a minimum of 100 days following the last dose of study treatment). AEs were coded according to the Medical Dictionary for Regulatory Activities (MedDRA) version 21.0 and tabulated using worst grade according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0. Immune-mediated AEs included pneumonitis, diarrhea/colitis, hepatitis, nephritis/renal dysfunction, rash, endocrine (adrenal insufficiency, hypothyroidism/thyroiditis, hyperthyroidism, diabetes mellitus, and hypophysitis), and other specific events considered to be potential immune-mediated events by investigator that occurred within 100 days of the last dose, regardless of causality, and were treated with immune-modulating medication. Evaluation of biomarkers, such as tumor cell PD-L1 expression, was an exploratory endpoint. Tumor cell PD-L1 expression was evaluated by IHC and defined as the percent of viable tumor cells with membrane staining (partial or complete) in a minimum of 100 viable tumor cells per validated Dako PD-L1 IHC 28–8 pharmDx kit (Dako, an Agilent Technologies, Inc. company, Santa Clara, California, USA).
Statistical analyses
This study included a dose-escalating safety evaluation phase for the nivolumab plus ipilimumab combination arm followed by a staged enrolment for the nivolumab monotherapy arm and the nivolumab plus ipilimumab combination arm. The staged enrolment part used a modified Simon two-stage design with the treatment of 40 patients to evaluate whether nivolumab or the combination of nivolumab plus ipilimumab yielded an ORR that was of clinical interest. In this study, an ORR of ≥10% was considered of clinical value, and an ORR of ≥25% was considered of strong clinical interest. The modified Simon design evaluated the null hypothesis that the true response rate was ≤10% vs the alternative hypothesis that the true response rate was >10%. The two-stage testing targeted a type I error rate of 5% and had 80% power (based on the original N=40) to reject the null hypothesis if the true response rate was 25%.
For the nivolumab monotherapy arm, the modified Simon design required 18 treated patients for the first stage and would be terminated at stage 1 if there was ≤1 responder among the 18 treated patients in the cohort. If ≥2 responders were identified in up to 18 treated patients in a cohort, additional patients were assigned up to a total of 40 treated patients in that cohort per the initial protocol. After a protocol amendment, additional patients could be assigned up to a total of 100 patients. The treatment was to be considered of clinical interest if, at the end of the second stage, there were ≥8 responders among the first 40 treated patients in any one cohort. A cross-over option to one of the nivolumab plus ipilimumab arms was available for patients in the nivolumab monotherapy arm who progressed on monotherapy. For the triplet arm, a one-stage design was used, with 30 patients treated. This sample size provided 70% power to reject the null hypothesis of a 10% response rate if the true response rate was 25% with a two-sided type I error rate of 5%.
The primary analysis of investigator-assessed ORR was summarized by a binomial response rate and corresponding two-sided 95% exact CI using the Clopper-Pearson method for arms using the one-stage design. For the triplet arm, ORR per BICR was summarized similarly. Investigator-assessed DOR (and BICR-assessed DOR for the triplet arm) was summarized for patients who achieved confirmed PR or CR using Kaplan-Meier (KM) methodology. Median DOR and two-sided 95% CI, using the Brookmeyer and Crowley method, was also calculated within each treatment arm. Similar KM methodology was used to descriptively summarize investigator-assessed PFS, BICR-assessed PFS (for the triplet arm), and OS. Median PFS and OS, with two-sided 95% CIs, were calculated for within each treatment arm. In addition, PFS and OS rates (and 95% CIs) at fixed time points were estimated from the PFS and OS KM curves, respectively. All efficacy analyses were performed in all treated patients.
Safety was summarized for treated patients across all three treatment arms according to MedDRA v21.0. The safety profile was assessed through summaries of deaths, serious AEs, AEs leading to discontinuation, overall AEs, and laboratory abnormalities. Treatment-related AEs leading to drug discontinuations between the first dose and 30 days after the last dose of study therapy were summarized.
Analyses of tumor cell PD-L1 expression were intended to assess potential associations between tumor cell PD-L1 expression and efficacy measures. For each baseline tumor cell PD-L1 subgroup, ORR was summarized by a binomial response rate and corresponding two-sided 95% CIs using the Clopper-Pearson method, and median (and two-sided 95% CIs) PFS and OS were estimated using KM methodology. All statistical analyses were done with SAS software (V.9.02; SAS Institute).
Results
Patients
Between October 21, 2013 and June 22, 2018, 93 patients were enrolled and 69 were treated. Of these, 18 patients received nivolumab monotherapy (treated between November 14, 2013 and January 27, 2014) and 21 received nivolumab plus ipilimumab (treated between November 7, 2013 and June 5, 2014) at 16 sites in 4 countries (both arms), and 30 received triplet therapy (treated between January 23, 2017 and June 29, 2017 at 6 US sites). Of patients who received nivolumab plus ipilimumab, 3 received dose level 1 and 18 received dose level 2. At data cut-off, median (range) follow-up (time from first dose to last known date alive or death) was 5.1 (0.6–20.8) months in the nivolumab monotherapy arm, 4.0 (0.9–19.5) months in the nivolumab plus ipilimumab arm, and 6.0 (0.6–17.0) months in the nivolumab plus ipilimumab plus cobimetinib arm. At the time of the clinical data cut-off for the current analysis (June 22, 2018; database lock August 3, 2018), patients in all three treatment arms had discontinued treatment. The most common reason for discontinuation was disease progression, reported in 16 of 18 patients (89%) in the monotherapy arm, 14 of 21 (67%) in the doublet arm, and 22 of 30 (73%) in the triplet arm (online supplemental figure 1). Two patients who had crossed over from the nivolumab monotherapy arm to the nivolumab plus ipilimumab arm discontinued because of disease progression.
jitc-2023-007883supp001.pdf (559.5KB, pdf)
The extent of prior therapies differed somewhat across treatment arms, in part because the triplet therapy protocol required treatment with at least one but no more than two prior systemic therapies in the advanced/metastatic setting. The proportion of patients with ≥3 prior systemic regimens in the metastatic setting was 11% in the monotherapy arm, 57% in the nivolumab plus ipilimumab arm, and 7% in the triplet arm (table 1). The proportion of patients receiving either neoadjuvant or adjuvant therapy was highest in the nivolumab monotherapy arm (50%), followed by the triplet arm (37%), and duplet arm (29%) (table 1, online supplemental table 1). The proportion of patients receiving both neoadjuvant and adjuvant therapy was highest in the triplet arm (17%), followed by the monotherapy arm (6%). Mean cumulative dose of nivolumab was similar in the monotherapy and triplet arms (18.7 and 18.4 mg/kg, respectively; patients in both arms received nivolumab 3 mg/kg) but lower in the nivolumab plus ipilimumab arm (2.7 mg/kg; patients in this arm received nivolumab 1 mg/kg) (online supplemental table 2). As expected, mean cumulative dose of ipilimumab in the nivolumab plus ipilimumab arm (which received ipilimumab 3 mg/kg) was higher (6.7 mg/kg) than in the triplet arm (2.2 mg/kg), which received ipilimumab 1 mg/kg.
Table 1.
Baseline demographic and clinical characteristics in all randomized patients
| Nivolumab (n=18) |
Nivolumab plus ipilimumab (n=21) |
Nivolumab plus ipilimumab plus cobimetinib (n=30) | |
| Age, median (range), years | 66.5 (35‒76) | 63.0 (47‒79) | 65.0 (31‒78) |
| <65 | 5 (28) | 11 (52) | 13 (43) |
| ≥65 | 13 (72) | 10 (48) | 17 (57) |
| Sex, n (%) | |||
| Male | 13 (72) | 11 (52) | 18 (60) |
| Female | 5 (28) | 10 (48) | 12 (40) |
| Race, n (%) | |||
| White | 16 (89) | 19 (90) | 23 (77) |
| Black or African American | 1 (6) | 1 (5) | 4 (13) |
| Asian | 1 (6) | 1 (5) | 1 (3) |
| Other | 0 | 0 | 2 (7) |
| Region, n (%) | |||
| USA | 16 (89) | 16 (76) | 30 (100) |
| Rest of the world | 2 (11) | 5 (24) | 0 |
| Prior lines of therapy, n (%) | |||
| 0 | 0 | 0 | 1 (3) |
| 1 | 9 (50) | 2 (10) | 10 (33) |
| 2 | 3 (17) | 8 (38) | 17 (57) |
| ≥3 | 6 (33) | 11 (52) | 2 (7) |
| Prior systemic regimens in the neoadjuvant setting,* n (%) | |||
| 0 | 15 (83) | 20 (95) | 25 (83) |
| 1 | 1 (6) | 1 (5) | 5 (17) |
| 2 | 2 (11) | 0 | 0 |
| Prior systemic regimens in the adjuvant setting,* n (%) | |||
| 0 | 11 (61) | 16 (76) | 19 (63) |
| 1 | 7 (39) | 5 (24) | 11 (37) |
| Prior systemic regimens in the metastatic setting, n (%) | |||
| 0 | 3 (17) | 0 | 6 (20) |
| 1 | 6 (33) | 3 (14) | 9 (30) |
| 2 | 7 (39) | 6 (29) | 13 (43) |
| ≥3 | 2 (11) | 12 (57) | 2 (7) |
| Prior surgery related to cancer, n (%) | |||
| Yes | 11 (61) | 8 (38) | 10 (33) |
| No | 7 (39) | 13 (62) | 20 (67) |
| ECOG PS, n (%) | |||
| 0 | 12 (67) | 10 (48) | 4 (13) |
| 1 | 6 (33) | 11 (53) | 25 (83) |
| 2 | 0 | 0 | 1 (3) |
| Site of metastases,† n (%) | |||
| Liver | 10 (56) | 16 (76) | 18 (60) |
| Lung | 6 (33) | 9 (43) | 11 (37) |
| Lymph node | 7 (39) | 8 (38) | 12 (40) |
| Median (range) index tumor burden, mm | 68.5 (10–135) | 80.0 (19–237) | 79.0 (15–221) |
| Time from initial diagnosis to study treatment, median (range), years | 1.2 (0.6–4.1) | 1.2 (0.4–2.6) | 1.2 (0.5–5.3) |
| LDH | |||
| ≤ULN | 16 (89) | 17 (81) | 25 (83) |
| >ULN | 2 (11) | 4 (19) | 4 (3) |
| Not reported | 0 | 0 | 1 (3) |
| Neutrophil/lymphocyte ratio, n (%) | |||
| ≤5 | 9 (50) | 15 (71) | 19 (63) |
| >5 | 9 (50) | 6 (29) | 11 (37) |
| ≤8 | 13 (72) | 19 (90) | 25 (83) |
| >8 | 5 (28) | 2 (10) | 5 (17) |
| Albumin | |||
| <LLN | 0 | 3 (14) | 5 (17) |
| ≥LLN | 1 (6) | 9 (43) | 25 (83) |
| Not reported | 17 (94) | 9 (43) | 0 |
*One patient in the nivolumab arm and five patients in the nivolumab plus ipilimumab plus cobinetinib arm received systemic therapies in both neoadjuvant and adjuvant settings.
†Patients could have lesions at more than one site.
ECOG PS, Eastern Cooperative Oncology Group performance status; LDH, lactate dehydrogenase; LLN, lower limit of normal; ULN, upper limit of normal.
Efficacy
In the nivolumab monotherapy and nivolumab plus ipilimumab combination therapy arms, ORR was less than the 10% cut-off for clinical interest (0% in each arm), so stage 2 was not reached. In the triplet arm, investigator-assessed objective responses were observed in 2 of 30 patients (ORR 6.7%; 95% CI 0.8 to 22.1), with best overall response of PR. By BICR assessment, objective responses were observed in three of 30 patients (ORR 10.0%; 95% CI 2.1 to 26.5), with best overall response of PR (table 2). A further 15 of 30 patients (50%) in the triplet arm had SD (per investigator and per BICR), giving a disease control rate per BICR of 60% (table 2). The best overall response was SD in 5 of 18 patients (28%) in the nivolumab monotherapy arm and 7 of 21 patients (33%) in the nivolumab plus ipilimumab arm. Objective responses in the triplet arm were observed regardless of tumor cell PD-L1 expression status (<5% or ≥5%, <1% or ≥1%; online supplemental table 3).
Table 2.
Summary of responses per RECIST V.1.1 and overall survival for all treated patients
| Nivolumab (n=18) |
Nivolumab plus ipilimumab (n=21) |
Nivolumab plus ipilimumab plus cobimetinib (n=30) |
||
| Investigator assessment | Investigator assessment | Investigator assessment | BICR assessment | |
| Objective response rate,* n/N (%) | 0/18 (0) | 0/21 (0) | 2/30 (6.7) | 3/30 (10.0) |
| 95% CI | 0.0 to 18.5 | 0.0 to 16.1 | 0.8 to 22.1 | 2.1 to 26.5 |
| Best overall response, n (%) | ||||
| Complete response | 0 | 0 | 0 | 0 |
| Partial response | 0 | 0 | 2 (7) | 3 (10) |
| Stable disease | 5 (28) | 7 (33) | 15 (50) | 15 (50) |
| Progressive disease | 9 (50) | 12 (57) | 9 (30) | 10 (33) |
| Unable to determine | 4 (22) | 2 (10) | 4 (13) | 2 (7) |
| Death before disease assessment | 3 (17) | 1 (5) | 2 (7) | 0 |
| Early discontinuation due to toxicity | 0 | 0 | 1 (3) | 0 |
| Other | 1 (6) | 1 (5) | 1 (3) | 0 |
| Median time to response‡ (range), months | 0 | 0 | 3.5 (2.5–4.4) | 1.4 (1.3–2.7) |
| Median duration of response‡ (95% CI), months | 0 | 0 | NE (3.3–NE) | NE (5.1–NE) |
| PFS | ||||
| Events, n (%) | 18 (100) | 19 (90) | 25 (83) | 23 (77) |
| Median (months) (95% CI) | 1.4 (1.3 to 2.0) | 1.4 (1.2 to 2.7) | 3.0 (1.5 to 4.1) | 3.1 (1.5 to 4.7) |
| PFS rate, % (95% CI) | ||||
| 3 months | 22 (7 to 43) | 19 (5 to 40) | 44 (26 to 62) | 52 (33 to 68) |
| 6 months | 6 (<1 to 22) | 6 (<1 to 25) | 17 (6 to 34) | 23 (9 to 41) |
| OS | ||||
| Events, n (%) | 18 (100) | 21 (100) | 22 (73) | – |
| Median (months) (95% CI) | 5.1 (2.0 to 9.0) | 4.0 (1.9 to 5.6) | 6.2 (3.9 to 11.4) | – |
| OS rate, % (95% CI) | ||||
| 3 months | 61 (35 to 79) | 62 (38 to 79) | 83 (65 to 93) | – |
| 6 months | 50 (26 to 70) | 24 (9 to 43) | 53 (33 to 69) | – |
| 12 months | 17 (4 to 37) | 10 (2 to 26) | 28 (13 to 45) | – |
*Evaluated in all treated patients.
†Percentages may not add up to 100% due to rounding.
‡Evaluated in patients who had an objective response.
BICR, blinded independent central review; NE, not estimable; OS, overall survival; PFS, progression-free survival; RECIST, Response Evaluation Criteria in Solid Tumors.
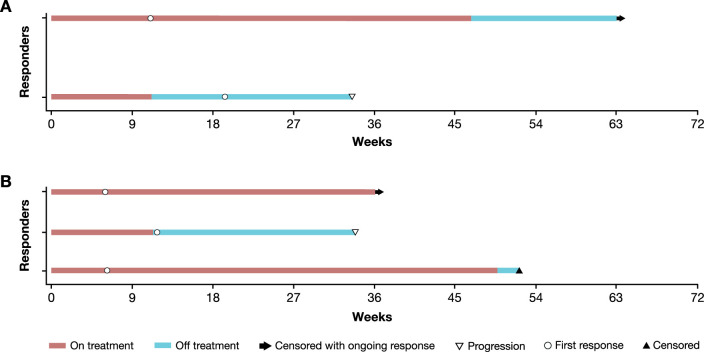
In the two patients in the triplet arm who had investigator-assessed PR, the median (range) time to objective response was 3.5 (2.5–4.4) months and median (95% CI) DOR (in months) was not estimable (3.3–not estimable; figure 1). In the three patients with BICR-assessed PR, median (range) time to objective response was 1.4 (1.3–2.7) months, and the median (95% CI) DOR (in months) was not estimable (5.1–not estimable). One responder had an ECOG PS of 1 and tumor cell PD-L1 expression ≥1% at baseline; time to response was 2.5 months and DOR was 12.0 months. The other responder had an ECOG PS of 1 and tumor cell PD-L1 expression <1% at baseline; time to response was 4.4 months and DOR was 3.3 months. At baseline, these responders had a time from initial diagnosis to study treatment of <2 years (median (range) <1 (0.6–1.3) years). The additional responder identified by BICR had an ECOG PS of 1 and tumor cell PD-L1 expression <1% at baseline; time to response was 1.4 months and DOR was 10.6 months.
Figure 1.
Time to and duration of response for responders by investigator assessment (A) and BICR assessment (B). Bar indicates last known date alive. BICR, blinded independent central review.
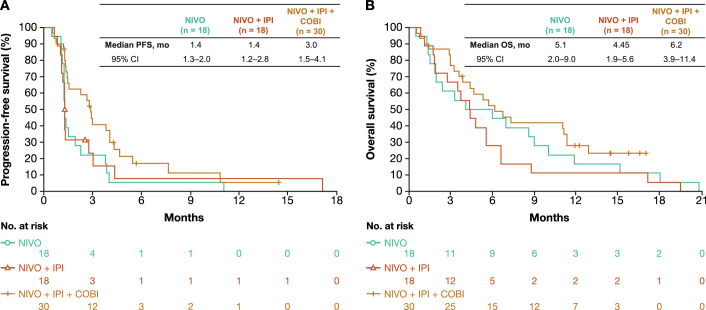
Among evaluable patients, 3 of 14 (21%), 4 of 16 (25%), and 14 of 25 (56%) patients in the monotherapy, combination therapy, and the triplet arms, respectively, had any reduction in tumor burden from baseline per investigator assessment (online supplemental figure 2 and online supplemental figure 3). Median (95% CI) PFS per investigator was 1.4 (1.3 to 2.0), 1.35 (1.2 to 2.7), and 3.0 (1.5 to 4.1) months for the nivolumab monotherapy, nivolumab plus ipilimumab, and triplet arms (3.1 (1.5 to 4.7) months per BICR in the triplet arm), respectively (figure 2A). Median (95% CI) OS was 5.1 (2.0 to 9.0) months in the nivolumab monotherapy arm, 4.0 (1.9 to 5.6) months in the nivolumab plus ipilimumab arm, and 6.2 (3.9 to 11.4) months in the triplet arm (figure 2B). Investigator-assessed PFS rates at 3 and 6 months, respectively, were 22% and 6% for the monotherapy arm, 19% and 6% for the nivolumab plus ipilimumab arm, and 44% and 17% in the triplet arm (52% and 23% per BICR; table 2). The corresponding OS rates at 3, 6, and 12 months were 61%, 50%, and 17% for the monotherapy arm, 62%, 24%, and 10% for the nivolumab plus ipilimumab arm, and 83%, 53%, and 28% for the triplet arm (table 2).
Figure 2.
Kaplan-Meier curves showing progression-free survival (PFS) by investigator (A) and overall survival (OS) (B).
Safety
Median (95% CI) duration of therapy was 1.7 (0.9 to 2.9) months in the nivolumab monotherapy arm, 0.7 (0.7 to 1.4) months in the nivolumab plus ipilimumab arm, and 2.4 (1.4 to 3.2) months in the triplet arm. Most patients (≥70%) in each arm received 90% to <110% of the planned dose intensity of nivolumab and ipilimumab (online supplemental table 2). The most frequently reported treatment-related AE of any grade across all treatment arms was diarrhea, reported in 28%, 48%, and 53% of patients in the nivolumab monotherapy arm, nivolumab plus ipilimumab arm, and triplet arm, respectively; the majority of treatment-related AEs were grade two or less in each arm (table 3).
Table 3.
Summary of treatment-related adverse events (TRAEs)
| Event, n (%) | Nivolumab (n=18)* |
Nivolumab plus ipilimumab (n=21)* |
Nivolumab plus ipilimumab plus cobimetinib (n=30)* | |||
| Any grade | Grade 3/4 | Any grade | Grade 3/4 | Any grade | Grade 3/4 | |
| Any TRAE | 12 (67) | 2 (11) | 18 (86) | 8 (38) | 28 (93) | 11 (37) |
| Serious TRAE | 3 (17) | 1 (6) | 6 (29) | 6 (29) | 5 (17) | 3 (10) |
| TRAEs leading to discontinuation | 1 (6) | 1 (6) | 4 (19) | 4 (19) | 5 (17) | 2 (7) |
| TRAEs of any grade in ≥20% of patients in any treatment arm | ||||||
| Diarrhea | 5 (28) | 0 | 10 (48) | 1 (5) | 16 (53) | 1 (3) |
| Pyrexia | 4 (22) | 0 | 5 (24) | 1 (5) | 5 (17) | 1 (3) |
| Fatigue | 3 (17) | 0 | 6 (29) | 2 (10) | 12 (40) | 3 (10) |
| Pruritus | 1 (6) | 0 | 5 (24) | 0 | 9 (30) | 1 (3) |
| Nausea | 1 (6) | 0 | 5 (24) | 0 | 4 (13) | 0 |
| Dermatitis acneiform | 1 (6) | 0 | 0 | 0 | 6 (20) | 0 |
| Rash | 0 | 0 | 3 (14) | 0 | 11 (37) | 0 |
*Patients who received at least one dose of any study medication. Adverse events were assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events, V.4.0, and Medical Dictionary for Regulatory Activities V.21.0.
Fatigue was the most commonly reported grade 3/4 treatment-related AE, occurring in 0%, 10%, and 10% of patients in the nivolumab monotherapy, nivolumab plus ipilimumab, and triplet arms, respectively. Grade 3/4 treatment-related AEs leading to discontinuation occurred in 1 patient (6%, colitis) in the nivolumab monotherapy arm, 4 patients (19%) in the nivolumab plus ipilimumab arm (2 cases of colitis and 1 case each of diarrhea, increased aspartate aminotransferase, and increased liver function test), and 2 patients (7%) in the triplet arm (1 case each of anemia and steatohepatitis). Serious treatment-related AEs of any grade were reported in 3 patients (17%) in the nivolumab monotherapy arm, 6 patients (29%), in the nivolumab plus ipilimumab arm, and 5 patients (17%) in the triplet arm. The most frequently reported serious grade 3/4 treatment-related AEs in each arm were 1 case each (6%) of colitis and increased alanine aminotransferase in the nivolumab monotherapy arm; 2 cases of colitis (10%) and 1 case each (6%) of diarrhea, pyrexia, increased aspartate aminotransferase, increased liver function test, autoimmune thyroiditis, and hyperbilirubinemia in the nivolumab plus ipilimumab arm; and 1 case each (6%) of diarrhea, adrenal insufficiency, and steatohepatitis in the triplet arm. There were no treatment-related deaths in any arm. The most frequently reported immune-mediated AEs were maculopapular rash (2/18; 11%) in the nivolumab monotherapy arm, diarrhea (4/21; 19%) in the nivolumab plus ipilimumab arm, and rash (5/30; 17%) in the triplet arm (table 4).
Table 4.
Summary of immune-mediated adverse events (AEs) for which immune-modulating medication was used*
| Event, n (%) | Nivolumab (n=18) |
Nivolumab plus ipilimumab (n=21) | Nivolumab plus ipilimumab plus cobimetinib (n=30) | |||
| Any grade | Grade 3/4 | Any grade | Grade 3/4 | Any grade | Grade 3/4 | |
| Rash | 0 | 0 | 2 (10) | 0 | 5 (17) | 0 |
| Diarrhea | 1 (6) | 0 | 4 (19) | 1 (5) | 1 (3) | 0 |
| Maculopapular rash | 2 (11) | 1 (6) | 0 | 0 | 3 (10) | 1 (3) |
| AST increased | 0 | 0 | 2 (10) | 2 (10) | 1 (3) | 0 |
| Colitis | 1 (6) | 1 (6) | 1 (5) | 1 (5) | 0 | 0 |
| ALT increased | 0 | 0 | 1 (5) | 1 (5) | 1 (3) | 0 |
| Pneumonitis | 0 | 0 | 0 | 0 | 2 (7) | 0 |
| Blood bilirubin increased | 0 | 0 | 1 (5) | 1 (5) | 0 | 0 |
| Hyperbilirubinemia | 0 | 0 | 1 (5) | 1 (5) | 0 | 0 |
| Autoimmune thyroiditis | 0 | 0 | 1 (5) | 1 (5) | 0 | 0 |
| Vesicular rash | 0 | 0 | 0 | 0 | 1 (3) | 1 (3) |
| Adrenal insufficiency | 0 | 0 | 0 | 0 | 1 (3) | 1 (3) |
| Hyperthyroidism | 0 | 0 | 1 (5) | 0 | 0 | 0 |
*Endocrine AEs (adrenal insufficiency, hypothyroidism/thyroiditis, hyperthyroidism, diabetes mellitus, and hypophysitis) were considered immune-mediated AEs regardless of immune-modulating medication use, as endocrine drug reactions are often managed without immune-modulating medication.
ALT, alanine aminotransferase; AST, aspartate aminotransferase.
Discussion
In the triplet arm of the CheckMate 032 pancreatic cancer cohort, the ORR was 7% by investigator assessment and 10% by BICR in patients with advanced or metastatic cancer whose disease had progressed on up to two prior therapies and had a Royal Marsden prognostic score of 0 or 1. No responses were observed in the nivolumab monotherapy and nivolumab plus ipilimumab treatment arms. The 12-month OS rate was numerically higher with triplet therapy (28%) than with nivolumab monotherapy (17%) or nivolumab plus ipilimumab (10%). While a median OS of 6.2 months was reported in the triplet arm, the magnitude of increase compared with the nivolumab monotherapy and nivolumab plus ipilimumab arms (5.1 and 4.0 months, respectively) was small. The observations in the triplet arm of CheckMate 032 are consistent with the results of several phase 3 studies of different second-line chemotherapeutic regimens in patients with metastatic pancreatic cancer.24
Considering the characteristics of the individual responders in the triplet arm (investigator assessed), both had a baseline ECOG PS of 1, Royal Marsden prognostic score of ≤1, and time from initial diagnosis to study treatment of <2 years but differed in baseline tumor cell PD-L1 expression status (<1% and ≥1%). The additional BICR-assessed responder had a baseline ECOG PS of 1 and tumor cell PD-L1 expression <1%. There was no notable pattern in time to response or DOR among the three responders. None of the BICR-assessed responders had lung metastases; two patients had liver metastases and one patient had kidney, peritoneum, and intestinal metastases. Future analyses of genetic characteristics and other biomarkers may help to identify individuals who may respond to triplet therapy.
Due to differences in eligibility criteria between the triplet arm (nivolumab plus ipilimumab plus cobimetinib) and the nivolumab monotherapy and nivolumab plus ipilimumab treatment arms, baseline characteristics of patients in the triplet arm were potentially more favorable (eg, the requirement for ≤2 previous lines of chemotherapy and Royal Marsden prognostic score of 0 or 1). Conversely, the proportion of patients who had received ≥3 prior lines of therapy was highest in the nivolumab plus ipilimumab arm compared with the monotherapy and triplet arms, which might have contributed to the lower antitumor activity in this arm. In addition, differences in nivolumab and ipilimumab dosages in each arm resulted in cumulative doses of nivolumab being higher in the monotherapy and triplet therapy arms than in the nivolumab plus ipilimumab arm, while the cumulative dose of ipilimumab was higher in the nivolumab plus ipilimumab arm than in the triplet arm.
The overall safety profile of nivolumab as a single agent, in combination with ipilimumab, or in combination with ipilimumab and cobimetinib was generally consistent with the known toxicity profiles of each agent,5 16 25–28 and no new safety signals were identified across treatment arms. Given that the toxicity profile of the nivolumab plus ipilimumab combination is well characterized and that cobimetinib does not have an overlapping toxicity profile with either nivolumab or ipilimumab, the combination of these three agents would not be expected to increase the frequency and/or severity of treatment-associated toxicities. The possible exception to this was an increased risk for skin immune-related AEs (rash/maculopapular rash), which were more frequently reported in the triplet arm than in the other two arms.
A phase 2 study of the immune-checkpoint inhibitors durvalumab (anti-PD-1 antibody) and tremelimumab (anti-CTLA-4 antibody) was performed in 65 patients with metastatic pancreatic ductal adenocarcinoma who had previously received one first-line fluorouracil-based or gemcitabine-based chemotherapy regimen and could have received one other prior line of therapy in adjuvant, neoadjuvant, or definitive chemoradiation settings.29 ORR was 3% for patients treated with durvalumab plus tremelimumab and 0% for durvalumab monotherapy; median PFS was 1.5 months in both arms, median OS was 3.1 and 3.6 months, and the 12-month OS rate was 9% and 6%, respectively. The study did not meet the ORR cut-off to proceed to the second part of the trial. Survival data from our study for the nivolumab and nivolumab plus ipilimumab arms are consistent with these findings except for the 12-month OS rates, which were higher in our study (17% with nivolumab, 10% with nivolumab plus ipilimumab, and 28% with nivolumab plus ipilimumab plus cobimetinib), although more than half of patients in these arms had received at least two prior systemic regimens in the metastatic setting.
Other studies have been conducted to evaluate the drugs investigated in the current trial, either as single agents or in combinations. In a phase 2 study, single-agent ipilimumab 3 mg/kg was ineffective (ORR 0% in 27 patients; 2 patients with locally advanced disease showed a minor response) for the treatment of patients with metastatic or locally advanced pancreatic adenocarcinoma, 70% of whom had received at least two prior treatments.5 In a phase 1b study of ipilimumab plus gemcitabine in patients with advanced pancreatic cancer, ORR was 14%, median DOR was 11 months, median PFS was 2.8 months, and median OS was 6.9 months.6 In a phase 1 study in Japanese patients with advanced/metastatic pancreatic adenocarcinoma, mogamulizumab (anti-CC chemokine receptor 4 antibody) plus nivolumab had limited efficacy in the second line or later. Confirmed objective responses were reported in 1 of 15 patients (ORR 7%), median PFS was 1.8 months, and median OS was 6.5 months.30 In a phase 1b study of cobimetinib plus GDC-0994 (small molecule extracellular signal responsive kinase 1/2 inhibitor) in patients with locally advanced or metastatic solid tumors, 1 of 7 patients (14%) with pancreatic adenocarcinoma had an unconfirmed partial response; however, the combination was associated with intolerable toxicity.26 Taken together, these studies and our current study suggest that single-agent and dual immune-checkpoint inhibitor therapies have limited activity in advanced pancreatic adenocarcinoma, and that more clinical and biomarker research is needed to identify patients who might benefit from dual immune-checkpoint inhibitor regimens or combinations of immune-checkpoint inhibitors with targeted therapies or chemotherapies.
Limitations of this phase 1/2 study included the small sample size, the open-label, non-randomized design, the absence of a standard-of-care comparator, and the study not being powered for formal comparisons across arms. These limitations were partly mitigated by the use of both investigator and BICR assessments of response in the triplet arm. There were also differences in prior therapies across the arms, which limit interpretation of the results. In addition, identification of potential biomarkers of response was limited by the small sample size. Ongoing studies might help to identify biomarker-defined subgroups of patients who may benefit from nivolumab-based therapy.31
In conclusion, nivolumab monotherapy and nivolumab plus ipilimumab combination therapy did not result in objective responses in patients with previously treated advanced pancreatic adenocarcinoma. While three confirmed partial responses were observed with cobimetinib-containing triplet therapy and the overall safety profile was manageable in all arms, the small sample size and differences in baseline disease-specific characteristics between treatment arms limit interpretation of these results. Further studies are needed to identify novel combinations of checkpoint inhibitors with other antineoplastic agents, such as targeted therapies or chemotherapies, which may benefit previously treated patients with advanced pancreatic adenocarcinoma.
Acknowledgments
This study was supported by Bristol Myers Squibb and Ono Pharmaceutical. We thank the patients and their families who made this study possible, the investigators, the clinical study teams at Bristol Myers Squibb (Princeton, New Jersey, USA), and Ono Pharmaceutical (Osaka, Japan) and Dako (an Agilent Technologies company) for collaborative development of the PD-L1 IHC 28-8 pharmDx assay. Professional medical writing and editorial assistance were provided by Yvonne Yarker, PhD; Christiane Dresch, PhD; and Ben Labbe, PhD, of Parexel, funded by Bristol Myers Squibb.
Footnotes
Contributors: Concept and design: MT (triplet arm only). Data acquisition: MC, AA, FJK, MAM, MHT, KJP, PS, EO’R and DTL. Data analysis: SMS, SO’B and MT. Data interpretation: MC, AA, FJK, MAM, MHT, KJP, PS, EO’R, SMS, SO’B, MT and DTL. Guarantor: MC.
Funding: This study was funded by Bristol Myers Squibb.
Competing interests: MC reports research support from Bristol Myers Squibb; consulting fees from AstraZeneca, Bristol Myers Squibb, ImmunoCore, InCyte, Merck, and Moderna; and is an employee at UConn Health. AA reports support for the present manuscript from Bristol Myers Squibb; honoraria from Bristol Myers Squibb, Merck, and Regeneron; travel/meetings funding from Bristol Myers Squibb, Merck, and Regeneron; and participation in advisory board for Bristol Myers Squibb, Eisai, and Sanofi. FJK reports no conflicts of interest. MM reports support for the present manuscript from Bristol Myers Squibb; and consulting fees and honoraria from Ipsen. MHT reports grants or contracts from Bristol Myers Squibb, Exelixis, Merck, and Pfizer; consulting fees from Array Biopharma, Bayer, Cascade Prodrug, Immune-Onc, Incyte, Merck, Novartis, Pfizer, Regeneron, and Sanofi/Genzyme; honoraria from Blueprint Medicines, Bristol Myers Squibb, Eisai, and Merck; participation in advisory board for Oncosec; and is an employee at Providence Cancer Institute. KP reports support for the present manuscript from Bristol Myers Squibb; consulting fees and honoraria from Bristol Myers Squibb, Lilly, Merck Sharp & Dohme, Pfizer, Novartis, and Ipsen; participation in advisory board for Bristol Myers Squibb, Merck Sharp & Dohme, and Ipsen; owning stocks/stock options from Faron Pharmaceuticals; and other financial/non-financial interests for Bristol Myers Squibb, Lilly, Novartis, Exelixis, Pfizer, Merck Sharp & Dohme, Incyte, Eisai, and Bayer. PS reports participation in advisory board and stock or stock options for Achelois, Adaptive Biotechnologies, Affini-T, Apricity, BioAtla, BioNTech, Candel Therapeutics, Catalio, Codiak, Dragonfly, Earli, Enable Medicine, Glympse, Hummingbird, ImaginAb, Infinity Pharma, JSL Health, Lava Therapeutics, Lytix, Marker, Oncolytics, PBM Capital, Phenomic AI, Polaris Pharma, Sporos, Time Bioventures, Trained Therapeutix, Two Bear Capital, Venn Biosciences. EO’R reports consulting fees from Seagen, Boehringer Ingelheim, BioNTech, Ipsen, Merck, IDEAYA, Novartis, AstraZeneca, BioSapien, Cend Therapeutics, Astellas, Thetis, Autem, Tempus, Agios, Genentech-Roche, and Eisai; and other financial/non-financial interests for Genentech/Roche, Celgene/ Bristol Myers Squibb, BioNTech, AstraZeneca, Arcus, Elicio, Pertzye, Elicio Therapeutics, and Parker Institute. SMS reports owning stocks/stock options and being an employee of Bristol Myers Squibb. SO’B reports being an employee of Bristol Myers Squibb. MT reports owning stocks/stock options and being an employee of Bristol Myers Squibb. DTL reports grants or contracts from Bristol Myers Squibb, Merck, Aduro Biotech, Medivir, Nouscom, Curegenix, and AbbVie; consulting fees from Bristol Myers Squibb, Merck, Nouscom, G1 Therapeutics, Janssen, Merus, and Regeneron; and honoraria from Merck.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The Bristol Myers Squibb data sharing policy can be found online. Bristol Myers Squibb will honor legitimate requests for our clinical trial data from qualified researchers. Data will be shared with external researchers whose proposed use of the data has been approved. Complete deidentified patient data sets will be eligible for sharing 2 years after completion of the CheckMate 032 study. Before data are released, the researcher(s) must sign a data sharing agreement, after which the deidentified and anonymized datasets can be accessed within a secured portal. For the Bristol Myers Squibb data sharing policy, see https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and multiple committees and IRBs were involved. The trial protocol and all amendments were approved by local institutional review boards or independent ethics committees at each site and conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines, as defined by the International Conference on Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (details available on clinicaltrials.gov), and the protocol was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines, as defined by the International Council on Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. All patients provided written informed consent before enrollment.
References
- 1.International Agency for Research on Cancer, World Health Organization . GLOBOCAN 2020: all cancers. Available: https://gco.iarc.fr/today/data/factsheets/cancers/39-All-cancers-fact-sheet.pdf [Accessed 22 Jul 2022].
- 2.Abidoye O, Cho YM, Ahoussougbemey Mele A, et al. Trends in pancreatic cancer incidence and mortality in the United States from 2000 to 2019: a SEER-based study. JCO 2023;41:755. 10.1200/JCO.2023.41.4_suppl.755 [DOI] [Google Scholar]
- 3.National Cancer Institute, Surveillance, Epidemiology, and End Results Program . Cancer STAT facts: pancreatic cancer. Available: https://seer.cancer.gov/statfacts/html/pancreas.html [Accessed 12 Jun 2023].
- 4.Park W, Chawla A, O’Reilly EM. Pancreatic cancer: a review. JAMA 2021;326:851–62. 10.1001/jama.2021.13027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Royal RE, Levy C, Turner K, et al. Phase 2 trial of single agent Ipilimumab (anti-CTLA-4) for locally advanced or metastatic pancreatic adenocarcinoma. J Immunother 2010;33:828–33. 10.1097/CJI.0b013e3181eec14c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamath SD, Kalyan A, Kircher S, et al. Ipilimumab and gemcitabine for advanced pancreatic cancer: a phase IB study. Oncologist 2020;25:e808–15. 10.1634/theoncologist.2019-0473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marabelle A, Le DT, Ascierto PA, et al. Efficacy of pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair-deficient cancer: results from the phase II KEYNOTE-158 study. J Clin Oncol 2020;38:1–10. 10.1200/JCO.19.02105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiss GJ, Blaydorn L, Beck J, et al. Phase IB/II study of gemcitabine, NAB-paclitaxel, and pembrolizumab in metastatic pancreatic adenocarcinoma. Invest New Drugs 2018;36:96–102. 10.1007/s10637-017-0525-1 [DOI] [PubMed] [Google Scholar]
- 9.Wainberg ZA, Hochster HS, Kim EJ, et al. Open-label, phase I study of nivolumab combined with NAB-paclitaxel plus gemcitabine in advanced pancreatic cancer. Clin Cancer Res 2020;26:4814–22. 10.1158/1078-0432.CCR-20-0099 [DOI] [PubMed] [Google Scholar]
- 10.Das R, Verma R, Sznol M, et al. Combination therapy with anti-CTLA-4 and anti-PD-1 leads to distinct immunologic changes in vivo. J Immunol 2015;194:950–9. 10.4049/jimmunol.1401686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brahmer JR, Drake CG, Wollner I, et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. JCO 2010;28:3167–75. 10.1200/JCO.2009.26.7609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang C, Thudium KB, Han M, et al. In vitro characterization of the anti-PD-1 antibody nivolumab, BMS-936558, and in vivo toxicology in non-human primates. Cancer Immunol Res 2014;2:846–56. 10.1158/2326-6066.CIR-14-0040 [DOI] [PubMed] [Google Scholar]
- 13.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 2012;12:252–64. 10.1038/nrc3239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wei SC, Duffy CR, Allison JP. Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov 2018;8:1069–86. 10.1158/2159-8290.CD-18-0367 [DOI] [PubMed] [Google Scholar]
- 15.Lei M, Siemers NO, Pandya D, et al. Analyses of PD-L1 and inflammatory gene expression association with efficacy of nivolumab +/- ipilimumab in gastric cancer/gastroesophageal junction cancer. Clin Cancer Res 2021;27:3926–35. 10.1158/1078-0432.CCR-20-2790 [DOI] [PubMed] [Google Scholar]
- 16.Janjigian YY, Bendell J, Calvo E, et al. CheckMate-032 study: efficacy and safety of nivolumab and nivolumab plus ipilimumab in patients with metastatic esophagogastric cancer. J Clin Oncol 2018;36:2836–44. 10.1200/JCO.2017.76.6212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 2015;373:23–34. 10.1056/NEJMoa1504030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tawbi HA, Forsyth PA, Hodi FS, et al. Long-term outcomes of patients with active melanoma brain metastases treated with combination nivolumab plus ipilimumab (CheckMate 204): final results of an open-label, multicentre, phase 2 study. Lancet Oncol 2021;22:1692–704. 10.1016/S1470-2045(21)00545-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.OPDIVO (nivolumab). Prescribing information. Princeton, New Jersey: Bristol Myers Squibb; 2022. [Google Scholar]
- 20.Jiang J, Xu Y, Chang L, et al. Genomic landscape in neoplasm-like stroma reveals distinct prognostic subtypes of pancreatic ductal adenocarcinoma. Front Oncol 2021;11:771247. 10.3389/fonc.2021.771247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waters AM, Der CJ. KRAS: the critical driver and therapeutic target for pancreatic cancer. Cold Spring Harb Perspect Med 2018;8:a031435. 10.1101/cshperspect.a031435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu L, Mayes PA, Eastman S, et al. The BRAF and MEK inhibitors dabrafenib and trametinib: effects on immune function and in combination with immunomodulatory antibodies targeting PD-1, PD-L1, and CTLA-4. Clin Cancer Res 2015;21:1639–51. 10.1158/1078-0432.CCR-14-2339 [DOI] [PubMed] [Google Scholar]
- 23.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 24.Petrelli F, Parisi A, Tomasello G, et al. Comparison of different second line treatments for metastatic pancreatic cancer: a systematic review and network meta-analysis. BMC Gastroenterol 2023;23:212. 10.1186/s12876-023-02853-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kang Y-K, Boku N, Satoh T, et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017;390:2461–71. 10.1016/S0140-6736(17)31827-5 [DOI] [PubMed] [Google Scholar]
- 26.Weekes C, Lockhart A, LoRusso P, et al. A phase IB study to evaluate the MEK inhibitor cobimetinib in combination with the Erk1/2 inhibitor GDC-0994 in patients with advanced solid tumors. Oncologist 2020;25:833–e1438. 10.1634/theoncologist.2020-0292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosen LS, LoRusso P, Ma WW, et al. A first-in-human phase I study to evaluate the mek1/2 inhibitor, cobimetinib, administered daily in patients with advanced solid tumors. Invest New Drugs 2016;34:604–13. 10.1007/s10637-016-0374-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gogas H, Dréno B, Larkin J, et al. Cobimetinib plus atezolizumab in BRAFV600 wild-type melanoma: primary results from the randomized phase III Imspire170 study. Ann Oncol 2021;32:384–94. 10.1016/j.annonc.2020.12.004 [DOI] [PubMed] [Google Scholar]
- 29.O’Reilly EM, Oh D-Y, Dhani N, et al. Durvalumab with or without tremelimumab for patients with metastatic pancreatic ductal adenocarcinoma: a phase 2 randomized clinical trial. JAMA Oncol 2019;5:1431–8. 10.1001/jamaoncol.2019.1588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Doi T, Muro K, Ishii H, et al. A phase I study of the anti-CC chemokine receptor 4 antibody, mogamulizumab, in combination with nivolumab in patients with advanced or metastatic solid tumors. Clin Cancer Res 2019;25:6614–22. 10.1158/1078-0432.CCR-19-1090 [DOI] [PubMed] [Google Scholar]
- 31.Padrón LJ, Maurer DM, O’Hara MH, et al. Sotigalimab and/or nivolumab with chemotherapy in first-line metastatic pancreatic cancer: clinical and immunologic analyses from the randomized phase 2 PRINCE trial. Nat Med 2022;28:1167–77. 10.1038/s41591-022-01829-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2023-007883supp002.pdf (2.1MB, pdf)
jitc-2023-007883supp001.pdf (559.5KB, pdf)
Data Availability Statement
Data are available on reasonable request. The Bristol Myers Squibb data sharing policy can be found online. Bristol Myers Squibb will honor legitimate requests for our clinical trial data from qualified researchers. Data will be shared with external researchers whose proposed use of the data has been approved. Complete deidentified patient data sets will be eligible for sharing 2 years after completion of the CheckMate 032 study. Before data are released, the researcher(s) must sign a data sharing agreement, after which the deidentified and anonymized datasets can be accessed within a secured portal. For the Bristol Myers Squibb data sharing policy, see https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.