Abstract
Objective
To test whether a musculoskeletal multifactorial and individualised hamstring muscle injury (HMI) risk reduction programme could reduce HMI risk in professional football.
Methods
We conducted a prospective cohort study in Finnish premier football league teams, with the 2019 season used as a control and an intervention conducted in the 2021 season. Screening was conducted to provide individualised programmes and monitor progress. Cox regression with hazard ratio (HR) was used with HMI as outcome and season as explanatory variable, including all players for primary analysis and those who performed the two seasons for secondary analysis.
Results
90 players were included in the control and 87 in the intervention seasons; 31 players performed in the 2 seasons. Twenty HMIs were recorded during the control and 16 during the intervention seasons. Cox regression analyses revealed that HMI risk at any given time was not significantly different between control and intervention seasons (for all players: HR 0.77 (95% CI 0.39 to 1.51), p=0.444; for the 31 players: HR 0.32 (95% CI 0.01 to 1.29), p=0.110)). For the 31 players, the HMI burden was significantly reduced in the intervention compared with the control season (RR 0.67 (95% CI 0.53 to 0.85)). Higher compliance with knee strength training, maximal velocity exposure and lower performance reductions in maximal theoretical horizontal force and knee flexor force were associated with lower HMI incidence.
Conclusions
Although the primary analysis did not reveal any significant effect of the intervention to reduce HMI risk in professional football, the programme was feasible, and additional secondary analyses showed a significant association between the intervention and lower HMI burden, incidence and risk.
Keywords: Football, Hamstring, Injury, Prevention
WHAT IS ALREADY KNOWN ON THIS TOPIC
Hamstring muscle injuries (HMIs) remain the most common injury in modern professional football.
Most successful HMI risk reduction interventions in professional football have mainly focused on only one component and on eccentric knee flexor strength.
It is relatively agreed upon that not reduced HMI rates could be partly due to the lack of multifactorial approaches and issues with compliance.
WHAT THIS STUDY ADDS
The innovative musculoskeletal multifactorial and individualised HMI risk programme was feasible in a professional football setting.
The HMI risk at any given time was not significantly different between the control and the intervention seasons.
When considering only players who performed the two seasons, the HMI burden was significantly reduced in the intervention season.
Higher compliance with knee strength training and maximal velocity exposure was associated with lower HMI incidence.
Decreases in maximal theoretical horizontal force and knee flexor force during the season increased the odds of sustaining an HMI.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These promising results support the interest in disseminating the present musculoskeletal multifactorial and individualised programme and promoting its use in football. Although it was conceived to be multifactorial, end-users could also consider using, more specifically, some components of the programme which have been associated with lower HMI incidence and risk (ie, knee strength training, maximal theoretical horizontal force and maximal velocity exposure).
Introduction
Hamstring muscle injuries (HMIs) remain the most common injury in modern professional football.1 Successful HMI risk reduction interventions in professional football have mainly focused on eccentric knee flexor strength.2 Despite this, the occurrence of HMI remains a problem.1 It is relatively agreed on that this could be partly due to the lack of multifactorial approaches and issues with compliance.3–6
Consequently, Lahti et al6 suggested a programme aiming at managing modifiable musculoskeletal intrinsic risk factors from a multifactorial perspective, including isolated and multijoint posterior-chain strength, lumbopelvic control, range of motion (ROM), manual therapy, triceps surae health and sprint performance.6 Indeed, the systematic inclusion of sprint-focused training may be beneficial both from a performance and injury risk reduction perspective,7 which could promote a ‘win-win’ collaboration between medical and training staff to a multidisciplinary approach for reducing HMI occurrence.
Furthermore, football players have been shown to vary in which risk factors they individually possess across the season.8 To our knowledge, only one multifactorial and individualised HMI risk reduction study has been conducted in professional football.9 However, this study only focused on one club,9 whereas a broader inclusion of more clubs would have to inevitably consider different environmental constraints (eg, facility, budget, culture). Thus, more accessible approaches are likely warranted.6
In this context, this study aimed to present the results of the published protocol from Lahti et al,6 and thus to determine if a specific musculoskeletal multifactorial and individualised programme can reduce the occurrence of HMI in professional football teams with already ongoing HMI risk reduction efforts.
Methods
Study design and overall procedure
We conducted a prospective cohort study among professional football teams over two professional football seasons.6 The 2019 season was the control season, and the 2021 season was the intervention season. The intervention season was initially planned for 2020 but was postponed for 1 year due to the COVID-19 pandemic. Sport exposure and injury data were collected using the same procedure during the two seasons. Implementing a multifactorial and individualised HMI risk reduction programme was only for the 2021 season. Both seasons took place between April and October. The study outline is presented in more detail in Lahti et al.6
Patient and public involvement
The public was involved in the development of the intervention and the study. The patient was not involved.
Population
The recruitment was performed in Finnish premier football league teams. For each team, the recruitment was done by contacting each team’s strength and conditioning coach and physiotherapist separately. Inclusion criteria were players involved in training sessions during the 2019 or 2021 seasons and accepting that their medical data can be used for the research. Goalkeepers were excluded from the study due to low injury risk.6 More details can be found in Lahti et al.6
Primary outcome data collection
The primary outcome of the study was the occurrence of an index HMI.6 HMI was defined as ‘traumatic or overuse physical damage that occurred during sport exposure and that caused absence from the next training sessions or matches’,10 was located at the posterior side of the thigh and involved muscular tissue.6 The diagnosis was made via examination and interview of the players by the medical staff and confirmed by ultrasound or MRI.6
Other data collection
Other collected data included baseline information (ie, anthropometrics, team, position,11 HMI history during the two previous seasons), within-season sport exposure (ie, match and training hours), screening test results and questionnaires assigned for the coaching staff; more information can be found in Lahti et al.6
Intervention: musculoskeletal multifactorial and individualised HMI risk reduction programme for professional football
The intervention protocol and the scheduling are briefly introduced in this section, more detail can be found in Lahti et al.6 The intervention protocol was only implemented during the 2021 season. The programme first started with screening tests to determine the individualised programme for each player. For each team, all screening tests were planned at the start of the preseason, end of preseason, mid-season and the end of the season. The screening protocol was divided into four categories: lumbopelvic control, ROM, posterior chain strength and sprint mechanical output (figure 1).6 In each screening, category players were ranked as positive or negative within each team based on the percentiles presented in figure 1. Each training category included the same exercises for all players, but the training volume was adjusted based on the individual screening results. Thus, all players continued to train in each category, but those ranking above the percentile in specific categories were given a training volume target that prioritised maintenance (figure 1). The non-individualised component of the intervention (ie, ‘training for all players’) included high-speed sprinting, postsport ROM, triceps surae health and manual therapy (figure 1). The separation of these categories into a non-individualised group for multiple reasons, including time constraints and differences between teams in the budget (eg, some teams did not have functioning Global Positioning System (GPS) for all players to allow for maximal velocity exposure individualisation).
Figure 1.
Intervention screening and training structure of the musculoskeletal multifactorial individualised programme for hamstring muscle injury risk reduction in professional football. The individualised approach included four training categories. The screening result within each category determined each player’s training structure. For example, if a player within a specific team was under the 33% percentile in the lumbopelvic control test, his target training volume for lumbopelvic control was four times per week instead of two (see the last column for training outcome). This was also assuming there was only one game. In two game weeks, volume was dropped by 50%. Training for all players was not individualised, and thus, the same training volume was targeted for all players. More info can be found in Lahti et al.6 ASLR, active straight leg raise; ROM, range of motion.
General programming advice on where to place specific training stimuli during one and two match weeks was provided to all teams. Based on our discussions with the teams, it was expected that there would be inevitable differences in weekly programming strategies in different clubs. All teams physical coaching staff confirmed that they would try their best to find space for training targets, while no guarantees could be made. After screening, full responsibility was given to each team’s physiotherapist and strength and conditioning coach to implement the programme best. Video material of exercises and a weekend workshop were provided for all the physical coaching staff involved in the study. The coaching staff registered compliance data in each training category for each player weekly.
Sample size calculation
Based on an HMI prevalence of 22%, with the goal of 66% HMI reduction, taking into account a power of 80% (a=5%), the recruitment targeted 93 players per group.6
Statistical analysis
Descriptive analysis was first performed for players’ characteristics, screening test results, sport exposure and HMI, using frequency with percentages for categorical variables and mean with SDs (±SD) for continuous variables and usual epidemiological variables.6 Compliance with the intervention programme was calculated for each player in all the intervention categories (training and manual therapy) in the following manner: (completed intervention sessions/targeted intervention sessions)×100. Afterwards, total intervention compliance was calculated by averaging all the intervention categories. We compared the players’ characteristics for the 2019 and 2021 seasons using t-tests for continuous variables and χ2 for categorical variables.
For the primary analysis to determine if a specific multifactorial and individualised programme can reduce the occurrence of HMI in a professional football setting, we performed a Cox proportional hazards regression (or Cox regression) using ‘seasons’ (ie, control 2019 season vs intervention 2021 season) as the explanatory variables and the time to the first occurrence of a ‘new HMI’ as outcome. The regression was adjusted for age, team, body mass, height and history of HMI during the two previous seasons. The unit of analysis was the individual players. The time to the first event was analysed using hours of football practice (ie, cumulative training and competition time). The HR was reported with 95% CI, and the assumption that the HR was constant over time was tested.
As a secondary analysis, we used a case-crossover design. We included only players who participated in the two seasons in the analysis, allowing each participant to be under their control and reducing the between-person confounding. We performed the same procedure of Cox regression on these players.
Furthermore, we analysed the differences in HMI prevalence, incidence and burden between the two seasons for all included players and those who performed the two seasons using relative risk (RR) (95% CI) and the relationship between performance drops in screening variables (%D) during the season and HMI occurrence postperformance drops using OR calculations (OR).
We analysed statistics by using R V.4.2.0 (V.4.2.0, Copyright 2016 The Foundation for Statistical Computing (Comprehensive R Archive Network, http://www.R-project.org; accessed on 13 December 2023). Significance was accepted at p<0.05.
Deviations from the protocol
The intervention season was initially planned for the 2020 season but was postponed by 1 year to the 2021 season due to the outburst of the COVID-19 pandemic. The pandemic also led to three measurement rounds being conducted instead of four. Due to software issues, the walk test was removed, and the lumbopelvic control category only included the kickback test. For the statistical analysis, we compared the players’ characteristics for the 2019 and 2021 seasons using t-tests for continuous variables and χ2 for categorical variables to help interpret potential differences between seasons. We conducted a secondary analysis using a case-crossover design. We also conducted additional statistical analysis: (1) RR analyses for the HMI prevalence, incidence and burden, (2) correlations between compliance and HMI incidence and (3) explorations between reductions in screening test performances and HMI risk.
Results
Population
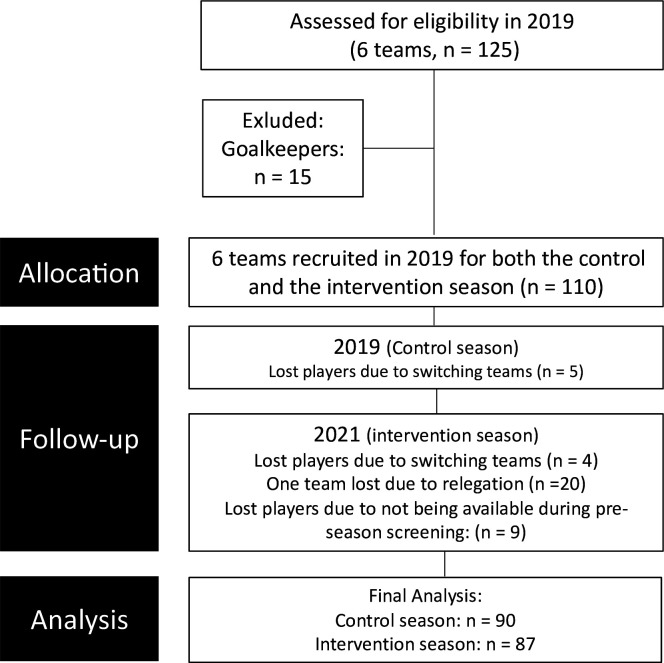
From a total of 130 eligible professional male football players from 6 teams within the professional male football premier league in Finland ‘Veikkausliiga’, the final sample included 5 teams with a total of 90 players for the control season (2019) and 87 for the intervention season (2021); 31 players participated at the two seasons. The flow chart of the population selection is presented in figure 2, and the characteristics of the included players are in table 1.
Figure 2.
Flow chart of the population selection.
Table 1.
Comparison of the players’ characteristics, football exposure and HMI history of the players between the two seasons
| Variables | Control season (2019) | Intervention season (2021) | P value |
| No of players | 90 | 87 | |
| Anthropometry (mean (SD)) | |||
| Age | 25.9 (5.0) | 25.3 (5.2) | 0.409 |
| Height | 1.80 (0.07) | 1.81 (0.07) | 0.550 |
| Body mass | 77.1 (6.8) | 76.4 (7.3) | 0.509 |
| History of HMI (n (%)) | 0.405 | ||
| Yes | 19 (21.1) | 23 (26.4) | |
| No | 71 (78.9) | 64 (73.6) | |
| Team (n (%)) | 0.995 | ||
| Team 1 | 20 (22.2) | 18 (20.7) | |
| Team 2 | 17 (18.9) | 18 (20.7) | |
| Team 3 | 16 (17.8) | 14 (16.1) | |
| Team 4 | 17 (18.9) | 17 (19.5) | |
| Team 5 | 20 (22.2) | 20 (23.0) | |
| Position (n (%)) | 0.605 | ||
| Defender | 35 (38.9) | 34 (39.1) | |
| Midfielder | 29 (32.2) | 33 (37.9) | |
| Forward | 26 (28.9) | 20 (23.0) | |
| Exposure (hours) (mean (SD)) | |||
| Total | 353.2 (39.4) | 364.4 (49.9) | 0.011 |
| Match | 26.4 (14.8) | 28.1 (14.9) | 0.432 |
| Training | 326.8 (33.4) | 336.3 (44.6) | 0.009 |
| Exposure (hours) (sum) | |||
| Total | 31 789 | 31 706 | |
| Match | 2374 | 2447 | |
| Training | 29 415 | 29 258 |
HMI, hamstring muscle injury.
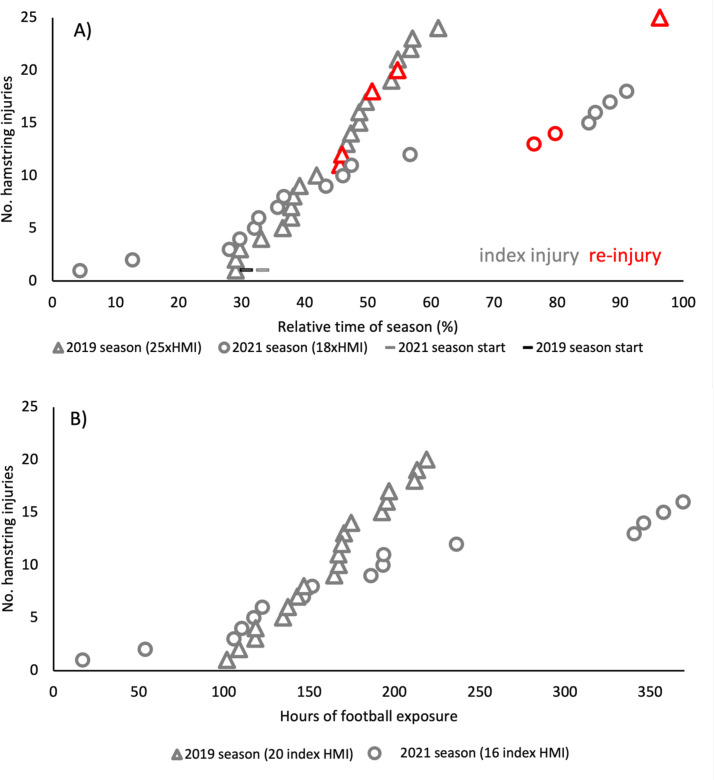
Hamstring muscle injuries
Twenty-five (27.8% of all injuries) and 18 (25.0%) HMI were collected during the 2019 and 2021 seasons, respectively. These corresponded to 20 and 16 players with at least one HMI, respectively, leading to 480 and 459 days lost from sports (figure 3 and table 2). There were no significant differences in HMI risk between the 2019 and 2021 seasons for HMI prevalence (RR 0.80 (95% CI 0.42 to 1.55)), incidence (RR 0.72 (95% CI 0.39 to 1.32)) and burden (RR 0.96 (95% CI 0.84 to 1.09)).
Figure 3.
Timeline of hamstring injuries during the 2019 and 2021 seasons (including preseason and in-season). (A) All HMI from both seasons relative to season length, including reinjuries. (B) Index HMI from both seasons concerning football exposure used in the Cox regression analysis. The 2019 injuries are visualised as triangles and the 2021 season as circles. The grey shapes are index injuries, and the red represents reinjuries. HMI, hamstring muscle injury.
Table 2.
Injuries between 2019 (control) and 2021 (intervention)
| Variables | Control (2019) season | Intervention (2021) season |
| No of all injuries | 90 | 72 |
| No of HMI (including reinjuries) | ||
| Total | 25 | 18 |
| Match | 15 | 12 |
| Training | 10 | 6 |
| Severe (>28 days) | 6 | 6 |
| Injury circumstance (n, (% of all index HMI)) | ||
| Sprinting | 14 (70.0) | 10 (62.5) |
| Change of direction | 3 (15.0) | 2 (12.5) |
| Overstretch action | 2 (10.0) | 3 (25.0) |
| Unknown | 1 (5.0) | 0 (0.0) |
| No of players with at least one HMI (n, (% of all injuries)) | ||
| Total | 20 (22.2) | 16 (22.2) |
| Match | 12 (13.3) | 10 (13.8) |
| Training | 10 (11.1) | 6 (8.33) |
| Severe | 6 (6.7) | 6 (8.33) |
| No of days lost for HMI | 480 | 459 |
| Incidence of HMI (no per 1000 hours (95% CI)) | ||
| Total | 0.79 (0.31) | 0.57 (0.26) |
| Match | 6.32 (3.19) | 4.90 (2.77) |
| Training | 0.34 (0.21) | 0.21 (0.16) |
| HMI burden (no of days lost per 1000 hours of football (95% CI)) | 15.1 (1.34) | 14.5 (1.31) |
| HMI burden (mean of individual no of time lost (in days) per 1000 hours of football, mean (SD)) | 16.3 (37.7) | 16.0 (44.9) |
HMI, hamstring muscle injury.
Among the 31 players participating in the two seasons, 9 HMI were collected in 2019 and 9 in 2021, corresponding to 7 and 5 injured players, respectively, leading to 173 and 114 days lost from sports, respectively. There were no significant differences in HMI risk between the 2019 and 2021 seasons for HMI prevalence (RR 0.73 (95%CI 0.23 to 2.29)) and incidence (RR 0.68 (95% CI 0.24 to 1.90)). Still, there was a significant reduction of HMI burden from the 2019 control season (15.6 number of days lost per 1000 hours of football (95% CI 13.3 to 17.9) to the 2021 intervention season (10.5 (95% CI 8.6 to 12.4)) (RR 0.67 (95% CI 0.53 to 0.85)).
Primary and secondary analyses
The primary analysis using adjusted Cox proportional hazards regression revealed that the HMI risk at any given time was not significantly different between the control and the intervention seasons (adjusted HR 0.77, 95% CI 0.39 to 1.51; p=0.444).
The secondary analysis, including the 31 players participating in the two seasons, also revealed that the HMI risk at any given time was not significantly different between the control and the intervention seasons (adjusted HR 0.32, 95% CI 0.01 to 1.29; p=0.110).
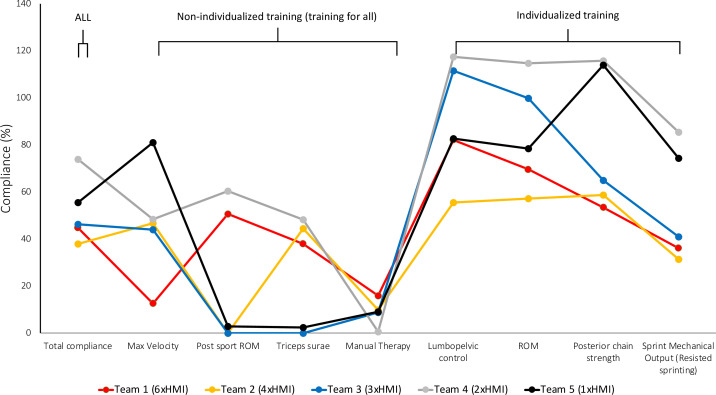
Compliance with the intervention
Relative compliance (% of completed sessions) in all categories of the intervention averaged over the entire season is presented in table 3 and figure 4. Correlations between compliance and HMI incidence (1000 hours of football exposure) showed significant and negative correlations in strength training (knee) and maximal velocity exposure (table 3).
Table 3.
Compliance with the intervention categories in each team during the 2021 season (intervention)
| Teams | Total compliance (%) | Individualisation compliance (%) | Training for all compliance (%) | Max velocity (%) | Post sport ROM (%) | Triceps surae health (%) | Manual therapy (%) | Lumbopelvic control (%) | ROM (%) |
Strength knee (%) | Strength hip (%) | Compliance strength (%) | Sprint mechanical output (%) |
| Team 1 (6×HMI; 1.19 HMI/1000 hours) | 45.9 (4.93) | 23.1 (13.4) | 41.8 (6.59) | 12.6 (3.01) | 50.6 (5.89) | 38.0 (3.92) | 15.9 (21.5) | 82.1 (20.9) | 69.6 (30.9) | 54.4 (27.7) | 52.4 (23.7) | 53.4 (22.4) | 36.1 (9.27) |
| Team 2 (4×HMI; 0.60 HMI/1000 hours) | 38.1 20.0) | 21.0 (12.0) | 20.9 (10.9) | 46.7 (25.2) | 0.00 (0.00) | 44.4 (23.2) | 9.85 (5.78) | 55.5 (32.2) | 57.2 (30.5) | 60.4 (36.1) | 56.9 (33.9) | 58.7 (32.6) | 31.4 (17.9) |
| Team 3 (3×HMI; 0.61 HMI/1000 hours) | 42.4 (3.77) | 76.2 (35.9) | 8.80 (1.00) | 44.0 (4.81) | 0.00 (0.00) | 0.00 (0.00) | 8.85 (7.77) | 112 (42.9) | 99.8 (33.7) | 65.0 (23.1) | 65.0 (24.0) | 65.0 (18.9) | 41.0 (2.31) |
| Team 4 (2×HMI; 0.30 HMI/1000 hours) | 73.9 (34.7) | 94.8 (58.4) | 49.3 (22.9) | 48.4 (22.6) | 60.3 (28.0) | 48.2 (22.9) | 0.60 (1.91) | 117 (61.5) | 115 (60.3) | 85.6 (47.8) | 146 (75.7) | 116 (60.4) | 85.0 (40.3) |
| Team 5 (1×HMI; 0.15 HMI/1000 hours) | 49.3 (20.6) | 68.2 (38.1) | 18.2 (8.40) | 81.1 (34.1) | 2.85 (5.80) | 2.38 (4.83) | 9.16 (5.32) | 82.7 (38.2) | 78.4 (40.1) | 110 (60.8) | 117 (60.2) | 114 (58.6) | 74.3 (31.3) |
| Correlation between compliance (%) and HMI incidence (1000 hours exposure) | −0.43 | −0.78 | 0.05 | −0.93* | 0.27 | 0.435 | 0.71 | −0.36 | −0.50 | −0.89* | −0.79 | −0.86 | −0.79 |
*p<0.05.
HMI, hamstring muscle injury; ROM, range of motion.
Figure 4.
Relative compliance was reported as the total for each intervention category of the five teams separately during the intervention season. The total compliance % is reported first to the left. The intervention categories are divided into non-individualised (max velocity, postsport ROM, triceps surae and manual therapy) and individualised clusters (lumbopelvic control, ROM, posterior chain strength and sprint mechanical output). The number of index injuries reported per team is on the bottom legend. HMI, hamstring muscle injury; ROM, range of motion.
Screening results
For the 2021 interventional season, 87 players completed the first round of screening, 77 completed the second, and 48 completed all 3 rounds (table 4). For the second round, injury was the only reason for missing the testing (n=10). The third round had to be completed for the teams after the season ended due to the ongoing pandemic. However, due to injuries (n=12) or already transitioning to other teams (n=33), only 48 players were available.
Table 4.
Descriptive statistics of the screening tests during the three measurements
| Category | Test | All screening 1 (n=87) | All screening 2 (n=77) | All screening 3 (n=48) | Effect size (first second) | Effect size (first vs third) | Baseline differences between teams |
| Range of motion | Jurdan (o) | 71.0 (9.00) | 72.0 (9.33) | 72.3 (8.88) | 0.20 (−0.02 to 0.44) | 0.76 (0.43 to 1.08) | |
| Jurdan asymmetry (%) | 6.98 (6.77) | 5.82 (4.23) | 6.53 (4.70) | −0.18 (−0.41 to 0.04) | 0.14 (−0.42 to 0.14) | ||
| Active straight leg raise (o) | 90.7 (11.7) | 93.1 (10.3) | 92.7 (8.44) | 0.32 (−0.09 to 0.55) | 0.61 (0.30 to 0.91) | ||
| Active straight leg raise asymmetry (%) | 5.41 (4.35) | 4.79 (3.88) | 5.53 (5.81) | −0.12 (−0.34 to 0.10) | 0.01 (−0.04 to 0.53) | ||
| Lumbo-pelvic control | Kickback (o) | 155 (12.5) |
155 (11.4) |
153 (24.7) |
−0.12 (−0.35 to 0.10) | −0.10 (−0.38 to 0.18) | Team 1 and 5 <team 2* |
| Sprint mechanical output | Maximal theoretical horizontal force (N/kg) | 7.82 (0.44) | 7.93 (0.46) | 7.77 (0.52) | 0.29 (−0.06 to 0.52) | −0.24 (−0.53 to 0.04) | Team 2<team 5* |
| Posterior chain strength | Hip force (N/kg) | 5.12 (0.82) | 5.32 (0.94) | 5.35 (0.82) | 0.23 (−0.01 to 0.45) | 0.43 (−0.13 to 0.72) | Team 5<team 1* |
| Hip force asymmetry (%) | 6.52 (5.39) | 8.01 (5.73) | 6.30 (4.79) | 0.22 (−0.01 to 0.44) | −0.10 (−0.38 to 0.18) | ||
| Knee force (N/kg) | 4.17 (0.64) | 4.33 (0.66) | 4.22 (0.70) | 0.29 (−0.06 to 0.52) | 0.06 (−.022 to 0.35) | Team 5<team 1* | |
| Knee force asymmetry (%) | 7.68 (6.68) | 9.10 (7.31) | 8.29 (6.13) | 0.12 (−0.11 to 0.34) | 0.07 (−0.20 to 0.36) |
*p<0.05.
Table 5 shows the percentage of changes in variables during the season and their potential association with the HMI risk. Players who showed performance reductions in the maximal theoretical horizontal force and knee flexor force between screening rounds one and two had 2.78 and 1.83 times higher odds of getting injured after the second round of screening until the end of the season, respectively (p<0.05).
Table 5.
Changes in performance between the first and second screening rounds
| Test | Δ% non-injured (round 1 vs 2) n=70 | Δ% injured (round 1 vs 2) n=7 | OR between HMI and drops in performance (95% CI) |
| Jurdan | 2.60 (8.73) | −2.04 (7.92) | −0.69 (−2.27 to 0.88) |
| Jurdan asymmetry | −1.54 (7.18) | 1.38 (5.08) | 1.73 (−0.43 to 3.90) |
| Active straight leg raise | 3.41 (8.77) | 0.48 (5.18) | −0.69 (−2.27 to 0.88) |
| Active straight leg raise asymmetry | −0.66 (5.25) | −0.13 (4.46) | 0.86 (−0.85 to 2.57) |
| Kickback | −0.44 (5.10) | −0.38 (1.44) | 0.06 (−1.51 to 1.63) |
| Theoretical maximal horizontal force | 2.22 (5.09) | −4.44 (2.89) | −2.78 (−4.96 to 0.59)* |
| Hip force | 4.29 (16.0) | 0.37 (6.12) | 0.27 (−1.45 to 1.98) |
| Hip force asymmetry | 1.34 (6.98) | 3.88 (9.55) | 1.14 (−1.03 to 3.32) |
| Knee force | 5.01 (12.3) | −6.11 (10.2) | −1.83 (−3.55 to to 0.11)* |
| Knee force asymmetry | 0.91 (8.76) | 2.03 (10.2) | −0.46 (−2.03 to 1.11) |
*p<0.5.
HMI, hamstring muscle injury.
Questionnaire results
The 2019 control and 2021 intervention seasons questionnaire results are in online supplemental figure 1–11. The 2019 season questionnaire (online supplemental figures 1–8) showed that out of all training categories, forms of sprint training (sprint drills, runs, resisted sprinting) were the least used among the five teams. The 2021 questionnaire (online supplemental figures 9–11) demonstrated that teams with lower HMI occurrence seemed to perceive that the largest benefit came from increased sprint training.
bmjsem-2023-001866supp001.pdf (2.8MB, pdf)
Discussion
The main findings of this study were that (1) the HMI risk at any given time was not significantly different between the control and the intervention seasons (for all populations: adjusted HR 0.77 (95% CI 0.39 to 1.51), p=0.444; for the case-crossover design analysis: adjusted HR 0.32 (95% CI 0.01 to 1.29), p=0.110), (2) there was a significant reduction of HMI burden from the control season to the 2021 intervention season (RR 0.67 (95% CI 0.53 to 0.85)) for the case-crossover design analysis, (3) higher compliance with the knee strength training and maximal velocity exposure was associated with lower HMI incidence and (4) higher performance reductions in maximal theoretical horizontal force and knee flexor force were associated with higher HMI risk. Although the primary analysis did not reveal any significant effect of the intervention to reduce HMI risk in professional football, the innovative musculoskeletal multifactorial and individualised injury risk programme was feasible, and additional secondary analyses showed a significant association between the intervention and lower HMI burden, incidence and risk.
Only one other intervention study has explored the value of evolving an HMI risk reduction protocol into a multifactorial and individualised approach.9 Contrary to the results of Suarez-Arrones et al,9 our intervention did not significantly reduce the risk of HMI. Differences in study setting and design can explain these different statistical outcomes. Suarez-Arrones et al9 focused on one team instead of multiple teams, reporting a seasonal HMI incidence average of 7.7 from the control seasons (our population had an average of 5.0 in the control season). The COVID-19 pandemic could have influenced HMI risk in the 2021 season. Indeed, previous studies reported that COVID-19 may increase HMI risk for players returning from quarantine,12–14 although contradictory evidence also exists.12 Although our primary analysis did not show HMI risk reduction with the intervention, it is noted that additional secondary analyses reported significant results supporting the efficacy of the intervention to reduce HMI burden, incidence and risk. In addition, at the human and team levels, avoiding four index injuries and seven HMI in total could be considered highly relevant from multiple perspectives (eg, player level, club financial level).15
The differences in injury burden between seasons should also be discussed as they also portray HMI severity and reinjury differences between seasons. For example, HMI incidence may be reduced, but it is not of high value if the total time lost is similar. There were five reinjuries in the control season (three out of five teams) vs two in the intervention season (one team). Three out of five teams reduced their injury burden from the control to the intervention season by 59% (19.6 vs 8.9 lost days per 1000 player hours). Two teams increased their injury burden, one with 413% (5.3 vs 27.3 lost days per 1000 player hours) and 19% (15.0 vs 17.9 lost days per 1000 player hours). The team that had a 413% increase was also the only team that increased HMI incidence between seasons (four vs eight injuries, including two reinjuries in 2021). For this team, the injuries were more severe in the intervention season (10 vs 31 average days lost per player). Interestingly, the team that had a 19% increase in injury burden decreased their HMI from five to two. This discrepancy is explained by the severity of one of their injuries that was 5 SD above the average HMI severity (26.9±17.2 days); a single grade 2 hamstring distal tear that caused 80 lost days. In such a small sample, this single injury substantially affected the mean injury burden within the season. Furthermore, in the case-crossover design analysis, our results showed a significant reduction of HMI burden from the control season to the 2021 intervention season (RR 0.67 (95% CI 0.53 to 0.85)), supporting the interest of this innovative musculoskeletal multifactorial and individualised injury risk programme to reduce HMI impact in professional football.
Compliance with the intervention might have played a role, as presented in table 3 and figure 4. Hypotheses regarding the compliance issues are of interest as they could, in part, explain the failure of the intervention in significantly reducing HMI occurrence and also help to improve compliance for future studies and/or implementation in the field. One reason could be a lack of buy-in from the assistant coach and head coach, with maximal velocity exposure mentioned as the most difficult training category to include systematically. This corresponds to the extrinsic risk factors reported in a recent HMI risk survey study among high-level European clubs.3 Furthermore, the physical coaching staff could have difficulties implementing the programme on double match weeks, irrespective of the reduction in target volume. Another reason could have been the lack of continuous, high-quality education on the approach. Thus, future studies should provide improved programming strategies and more robust approaches to inspire innovation within the entire staff and emphasise continued high-quality education before and during the season.
Compliance was the average of all intervention training categories and the manual therapy category, which assumes all categories are of equal value in reducing HMI risk. Although a holistic approach is considered optimal,9 16 17 there is realistically some stimuli hierarchy. Additional analysis demonstrated which intervention categories may have been of the highest value in reducing the occurrence of HMI. Simple correlational analysis revealed that higher compliance in knee flexor strength training (r=−0.89; p<0.05) and maximal velocity exposure (r=−0.93; p<0.05) were significantly and negatively correlated with HMI incidence (table 3). This means that there was an association between higher training compliance and a lower HMI risk level in these training categories. The individualised training categories also allowed for more in-depth analysis as we could assess the value of performance changes during the season. Our findings show that the players with performance drops in knee flexor strength or maximal theoretical horizontal force during sprint acceleration between the first and second screening rounds showed increased odds of sustaining an HMI later in the season (ORs=1.83 and 2.78, respectively, p<0.05). This was consistent with the expert experience, including strength testing and training for HMI risk reduction in professional football.3 According to our control season questionnaire, using evidence-based HMI risk reduction strength training methods was common practice among teams. Three out of five teams used the Nordic Hamstring Exercise (NHE) weekly (online supplemental figure 1), and the average HMI per team (including reinjuries) was 5.0±0.7 in the control season. This was close to the reported HMI team average of 17 elite UEFA clubs successfully implementing the NHE weekly during the 2020–2021 season (5±2).5 However, our intervention protocol included hamstring knee-joint focused (eg, the NHE) and hip-joint-focused exercises (eg, Romanian deadlift variants) to support the broader evidence-based intramuscular development of the hamstrings and synergists.18 19 The questionnaire did not specifically assess if the knee-joint or hip-joint exercise categories were perceived to increase in volume and/or detail. However, teams with lower rates of HMI perceived a higher magnitude than the programming detail for posterior strength training improved during the intervention season (online supplemental figure 10). Indeed, studies have shown that strength- and sprint-training programmes can positively influence hamstring architecture and lumbopelvic control,18 20 21 which are associated with HMI risk.22 23 Sprint volume was also shown to have a U-shaped injury risk curve in a professional sprint-based team sport. This indicates the importance of optimising training via individualisation and its systematic inclusion.24 This is arguably true for all training categories that may cause fatigue; thus, optimising testing and training strategies are likely of essential importance.25 Thus, it may be possible that the teams who evolved their ongoing HMI risk reduction strategies within posterior chain strength and sprint training were the most successful in reducing the risk of HMI. Furthermore, the successful teams seemed to be better at maintaining high compliance during the entire season in these training categories, possibly leading to a reduced risk of performance drops. Although these additional findings should be explored further in larger cohorts, they support frequent training and testing to control individual decrements in physical performance during the season. One positive result of this study was that the screening protocol was feasible multiple times over the season in different settings. The importance of frequent screening has been discussed in previous studies,26 27 focusing on controlling for performance decrements via fatigue or lack of adequate training exposure.
However, we have to acknowledge some limitations. We did not conduct a randomised controlled trial. The previous season was used as a control, assuming the seasons were exchangeable. The 2019 season was unaffected by the COVID-19 pandemic and can be considered normal. The 2021 season followed the same framework as the 2019 season and, as such, can be considered normal. However, we can not ignore that the COVID-19 pandemic could have also influenced the 2021 season. The gap year that took place due to the pandemic caused numerous difficulties, with likely the largest being the sample size. One involved team dropped out of the Finnish premier league this year. Our sample size calculations were calculated based on HMI prevalence, while our primary analysis was a Cox regression analysis. It targeted 93 players per season, whereas we ended up with 90 and 87 after 1 team dropped out; our study may thus have been slightly underpowered. In addition, the HMI prevalence and the effect of the intervention used for the a priori sample size calculation could have been overestimated, increasing the risk of underpowering. Competing events were not considered in this study and Cox regression analyses. This study was conducted in Finland, which could impact the generalisation of the results given cultural specificities and especially football season design (eg, from April to October without the winter season). We did not have the details of HMI, for example, the exact muscle involved or the severity grade. For the exposure, we only considered the volume/duration of the activity (ie, football training and match duration in hours). Adding the intensity (eg, Borg scale) or using GPS data could have provided more accurate information for exposure. Since coaching staff were free to organise the individualised programme for each player inside the training, it could have been of interest to have the details of this organisation/periodisation and the compliance and analyse its potential effect on HMI risk. Not all the screening tests could have been performed, and not all players could have participated in all test sessions. Our proposed test and training methods should also be constantly improved. For example, technological updates may allow for a more thorough analysis of force output and movement competency. Systematic use of GPS systems will likely improve individual load monitoring in the context of our protocol and will allow for individualisation of maximal velocity exposure. We performed additional secondary analyses that were thought relevant, but that was not presented in the study protocol, which can lead to selection bias, thus caution should be taken in their interpretation.6 For transparency to the readers, these are mentioned in the deviations from the protocol paragraph.
Practical implications
Although our primary analysis did not reveal a significant reduction in HMI risk in professional football settings that were already ongoing HMI risk reduction efforts, the proposed innovative musculoskeletal multifactorial and individualised programme was feasible and associated with reduction of HMI burden, incidence and risk for some aspects. It was also not associated with higher HMI risk. Although further studies should confirm these results and, if possible, with a higher level of evidence using a randomised controlled design, these promising results support the interest in disseminating the present musculoskeletal multifactorial and individualised programme and promoting its use in football. Although it was conceived to be multifactorial, end-users could also consider using, more specifically, some components of the programme, which have been associated with HMI risk reduction (ie, knee strength training, maximal theoretical horizontal force and maximal velocity exposure).
Conclusions
In the primary analysis, the proposed innovative musculoskeletal multifactorial and individualised programme was not associated with a significant HMI risk reduction at any given time. However, additional secondary analyses showed a significant association between the intervention and lower HMI burden, incidence and risk. These promising results support the interest in disseminating this programme and approach and promoting its use in football.
Acknowledgments
We thank all the teams and players participating in this project. We also would like to thank the following sprint coaches for their input to our training programme format: Håkan Andersson, Jonas Dodoo and Stuart McMillan.
Footnotes
Twitter: @PascalEdouard42, @lahti_johan, @jb_morin
PE and JL contributed equally.
Contributors: The authors JL, JM, J-BM and PE conceived the idea behind the study. JL, LF, JA, J-JU, TL, NV, TT, MB, VP, MT, TH and -were responsible for data acquisition and management. PE and JL performed statistical analyses. PE and JL drafted the manuscript, and all coauthors contributed substantially to interpreting the results, provided important revisions and approved the manuscript. All authors understand that they are accountable for all aspects of the work and ensure the accuracy or integrity of this manuscript. PE is the guarantor of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: PE is an Associate Editor for the British Journal of Sports Medicine and the BMJ Open Sports and Exercise Medicine.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Requests for data sharing from appropriate researchers and entities will be considered case-by-case. Interested parties should contact PE (pascal.edouard@univ-st-etienne.fr).
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and this study has received two separate ethical approvals. The first was received for the prospective data collection in the 2019 season by the Saint-Etienne University Hospital Ethics Committee (Institutional Review Board: IORG0007394; IRBN322016/CHUSTE) and the other for the intervention season by the Central Finland Health Care District (U6/2019). Participants gave informed consent to participate in the study before taking part.
References
- 1.Ekstrand J, Bengtsson H, Waldén M, et al. Hamstring injury rates have increased during recent seasons and now constitute 24% of all injuries in men’s professional football: the UEFA Elite Club Injury Study from 2001/02 to 2021/22. Br J Sports Med 2023;57:292–8. 10.1136/bjsports-2021-105407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fanchini M, Steendahl IB, Impellizzeri FM, et al. Exercise-based strategies to prevent muscle injury in elite footballers: a systematic review and best evidence synthesis. Sports Med 2020;50:1653–66. 10.1007/s40279-020-01282-z [DOI] [PubMed] [Google Scholar]
- 3.Ekstrand J, Ueblacker P, Van Zoest W, et al. Risk factors for hamstring muscle injury in male elite football: medical expert experience and conclusions from 15 European Champions League clubs. BMJ Open Sport Exerc Med 2023;9:e001461. 10.1136/bmjsem-2022-001461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van der Horst N, Hoef S van de, Otterloo P van, et al. Effective but not adhered to: how can we improve adherence to evidence-based hamstring injury prevention in amateur football? Clin J Sport Med 2021;31:42–8. 10.1097/JSM.0000000000000710 [DOI] [PubMed] [Google Scholar]
- 5.Ekstrand J, Bengtsson H, Walden M, et al. Still poorly adopted in male professional football: but teams that used the Nordic Hamstring Exercise in team training had fewer hamstring injuries - a retrospective survey of 17 teams of the UEFA Elite Club Injury Study during the 2020-2021 season. BMJ Open Sport Exerc Med 2022;8:e001368. 10.1136/bmjsem-2022-001368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lahti J, Mendiguchia J, Ahtiainen J, et al. Multifactorial individualised programme for hamstring muscle injury risk reduction in professional football: protocol for a prospective cohort study. BMJ Open Sport Exerc Med 2020;6:e000758. 10.1136/bmjsem-2020-000758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edouard P, Mendiguchia J, Guex K, et al. Sprinting: a key piece of the hamstring injury risk management puzzle. Br J Sports Med 2023;57:4–6. 10.1136/bjsports-2022-105532 [DOI] [PubMed] [Google Scholar]
- 8.Ribeiro-Alvares JB, Dornelles MP, Fritsch CG, et al. Prevalence of hamstring strain injury risk factors in professional and under-20 male football (soccer) players. J Sport Rehabil 2020;29:339–45. 10.1123/jsr.2018-0084 [DOI] [PubMed] [Google Scholar]
- 9.Suarez-Arrones L, Nakamura FY, Maldonado RA, et al. Applying a holistic hamstring injury prevention approach in elite football: 12 seasons, single club study. Scand J Med Sci Sports 2021;31:861–74. 10.1111/sms.13913 [DOI] [PubMed] [Google Scholar]
- 10.Waldén M, Hägglund M, Ekstrand J. Injuries in Swedish elite football--A prospective study on injury definitions, risk for injury and injury pattern during 2001. Scand J Med Sci Sports 2005;15:118–25. 10.1111/j.1600-0838.2004.00393.x [DOI] [PubMed] [Google Scholar]
- 11.Thoseby B, Govus AD, Clarke AC, et al. Positional and temporal differences in peak match running demands of elite football. Biol Sport 2023;40:311–9. 10.5114/biolsport.2023.116006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seshadri DR, Thom ML, Harlow ER, et al. Case report: return to sport following the COVID-19 lockdown and its impact on injury rates in the German Soccer League. Front Sports Act Living 2021;3:604226.:604226. 10.3389/fspor.2021.604226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Demir C, Subasi B, Harput G. Effects of the COVID-19 confinement period on hip strength, flexibility and muscle injury rate in professional soccer players. Phys Sportsmed 2023;51:56–63. 10.1080/00913847.2021.1985384 [DOI] [PubMed] [Google Scholar]
- 14.Wezenbeek E, Denolf S, Willems TM, et al. Association between SARS-COV-2 infection and muscle strain injury occurrence in elite male football players: a prospective study of 29 weeks including three teams from the Belgian professional football league. Br J Sports Med 2022;0:1–7. 10.1136/bjsports-2021-104595 [DOI] [PubMed] [Google Scholar]
- 15.Ekstrand J. Keeping your top players on the pitch: the key to football medicine at a professional level. Br J Sports Med 2013;47:723–4. 10.1136/bjsports-2013-092771 [DOI] [Google Scholar]
- 16.Mendiguchia J, Alentorn-Geli E, Brughelli M. Hamstring strain injuries: are we heading in the right direction? Br J Sports Med 2012;46:81–5. 10.1136/bjsm.2010.081695 [DOI] [PubMed] [Google Scholar]
- 17.Buckthorpe M, Wright S, Bruce-Low S, et al. Recommendations for hamstring injury prevention in elite football: translating research into practice. Br J Sports Med 2019;53:449–56. 10.1136/bjsports-2018-099616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bourne MN, Duhig SJ, Timmins RG, et al. Impact of the Nordic hamstring and hip extension exercises on hamstring architecture and morphology: implications for injury prevention. Br J Sports Med 2017;51:469–77. 10.1136/bjsports-2016-096130 [DOI] [PubMed] [Google Scholar]
- 19.Van Hooren B, Vanwanseele B, van Rossom S, et al. Muscle forces and fascicle behavior during three hamstring exercises. Scand J Med Sci Sports 2022;32:997–1012. 10.1111/sms.14158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mendiguchia J, Castaño-Zambudio A, Jiménez-Reyes P, et al. Can we modify maximal speed running posture? Implications for performance and hamstring injury management. Int J Sports Physiol Perform 2022;17:374–83. 10.1123/ijspp.2021-0107 [DOI] [PubMed] [Google Scholar]
- 21.Mendiguchia J, Conceição F, Edouard P, et al. Sprint versus isolated eccentric training: comparative effects on hamstring architecture and performance in soccer players. PLoS One 2020;15:e0228283. 10.1371/journal.pone.0228283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Timmins RG, Bourne MN, Shield AJ, et al. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): a prospective cohort study. Br J Sports Med 2016;50:1524–35. 10.1136/bjsports-2015-095362 [DOI] [PubMed] [Google Scholar]
- 23.Schuermans J, Van Tiggelen D, Palmans T, et al. Deviating running kinematics and hamstring injury susceptibility in male soccer players: cause or consequence? Gait Posture 2017;57:270–7. 10.1016/j.gaitpost.2017.06.268 [DOI] [PubMed] [Google Scholar]
- 24.Malone S, Owen A, Mendes B, et al. High-speed running and sprinting as an injury risk factor in soccer: can well-developed physical qualities reduce the risk? J Sci Med Sport 2018;21:257–62. 10.1016/j.jsams.2017.05.016 [DOI] [PubMed] [Google Scholar]
- 25.Lovell R, Knox M, Weston M, et al. Hamstring injury prevention in soccer: Before or after training? Scand J Med Sci Sports 2018;28:658–66. 10.1111/sms.12925 [DOI] [PubMed] [Google Scholar]
- 26.Dauty M, Menu P, Fouasson-Chailloux A. Cutoffs of isokinetic strength ratio and hamstring strain prediction in professional soccer players. Scand J Med Sci Sports 2018;28:276–81. 10.1111/sms.12890 [DOI] [PubMed] [Google Scholar]
- 27.van Dyk N, Farooq A, Bahr R, et al. Hamstring and ankle flexibility deficits are weak risk factors for hamstring injury in professional soccer players: a prospective cohort study of 438 players including 78 injuries. Am J Sports Med 2018;46:2203–10. 10.1177/0363546518773057 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2023-001866supp001.pdf (2.8MB, pdf)
Data Availability Statement
Data are available on reasonable request. Requests for data sharing from appropriate researchers and entities will be considered case-by-case. Interested parties should contact PE (pascal.edouard@univ-st-etienne.fr).