ABSTRACT
Carcinoma cuniculatum is a rare variant of well-differentiated squamous cell carcinoma. To date, there are less than 30 cases of esophageal carcinoma cuniculatum reported. It is frequently a diagnostic challenge: A definitive diagnosis typically cannot be made before esophagectomy. We present a uniquely aggressive case of esophageal carcinoma cuniculatum complicated by a bronchoesophageal fistula and successfully palliated with dual esophageal and endobronchial stenting.
KEYWORDS: carcinoma cuniculatum, esophagus, bronchoesophageal fistula, esophageal stent, endobronchial stent
INTRODUCTION
Carcinoma cuniculatum, an unusual form of well-differentiated squamous cell carcinoma, typically has an indolent clinical course. It was first described by Aird et al in 1954 in the plantar skin1 with subsequent reports of oral mucosa and larynx involvement.2,3 The largest series of esophageal carcinoma cuniculatum had 9 cases in total.4 Bronchoesophageal fistula (BEF) is a rare complication of this malignancy; the only 3 previous reported BEF cases were fatal within 6 weeks of diagnosis.4 We describe a uniquely aggressive case of esophageal carcinoma cuniculatum, leading to a complex BEF with the patient successfully palliated for more than 5 months by esophageal and endobronchial stenting.
CASE REPORT
A 67-year-old woman with well-controlled HIV on antiretroviral therapy presented with significant unexplained weight loss of 12.3 kg over 6 months. The patient initially denied symptoms of dysphagia and was started on somatropin for suspected HIV-associated cachexia. When the patient continued to have weight loss, despite treatment and developed dysphagia for solids, a workup for malignancy was initiated. A positron emission tomography scan demonstrated an FDG-avid esophageal mass with presumed metastatic mediastinal lymph nodes based on radiographic appearance. Upper endoscopy performed at an outside facility showed a midesophageal circumferential ulcerated mass, but endoscopic biopsies were unrevealing. The patient was referred to our institution for repeat biopsies and endoscopic ultrasound (EUS); a new bronchoesophageal fistula was discovered on our index endoscopy. Further workup with bronchoscopy revealed fistula involvement of the left main stem bronchus. The patient subsequently underwent multiple endoscopic mucosal, EUS-guided, and bronchoscopic biopsies of the mass and of the mediastinal lymphadenopathy. All biopsies were nondiagnostic, showing occasional squamous hyperplasia and atypia. The case underwent extensive multidisciplinary review with gastroenterology, pulmonary, cardiothoracic, and HIV services; the patient's operative risk was deemed prohibitively high. All treatment options were discussed with the patient in detail, and the patient opted for palliative stenting to optimize the nutritional and functional state to improve patient's surgical candidacy. A 18 × 149-mm fully covered esophageal stent was placed with occlusion of the fistula (Agile; Boston Scientific Inc). Follow-up bronchoscopy noted near occlusion of the left main stem bronchus. The decision was made to place a self-expanding 12 × 30-mm metal stent in the left main stem bronchus (Bonastent; Thorasent, Inc) to improve the patient's ventilation capacity (Figure 1). The dual stenting allowed for successful palliation of the fistula, and the patient resumed oral intake with soft mechanical diet and was discharged from the hospital. Over the subsequent 5 months, the patient continued to tolerate soft mechanical diet and gained weight with some improvement in functional status. The several repeat biopsies during this time interval were also nondiagnostic. The patient died 5 months after the initial stenting when she experienced an acute episode of hemoptysis. This was believed to be related to progression of the fistula with erosion into a pulmonary vessel. Ultimately, the diagnosis was established through autopsy with histopathologic findings consistent with esophageal carcinoma cuniculatum (Figure 2).
Figure 1.
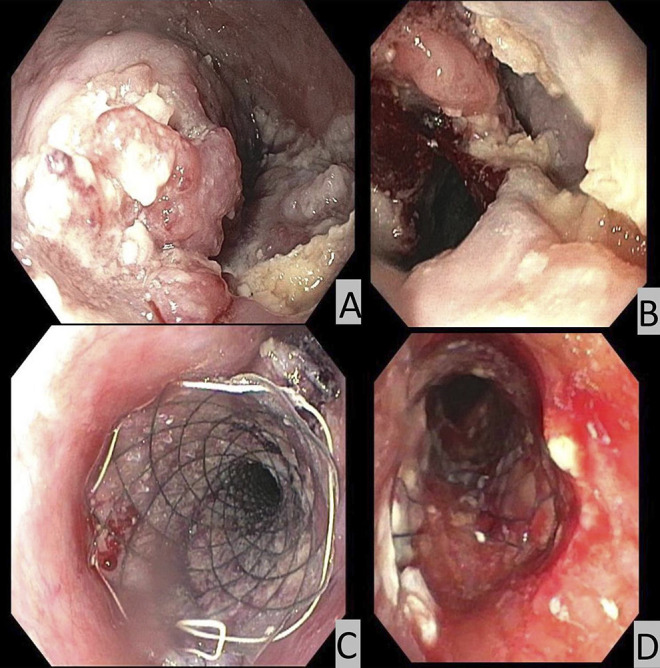
Endoscopic images of the esophageal mass (A) and bronchoesophageal fistula (B). Endoscopic image after placement of esophageal stent (C) and bronchoesophic view after bronchial stent placement (D).
Figure 2.
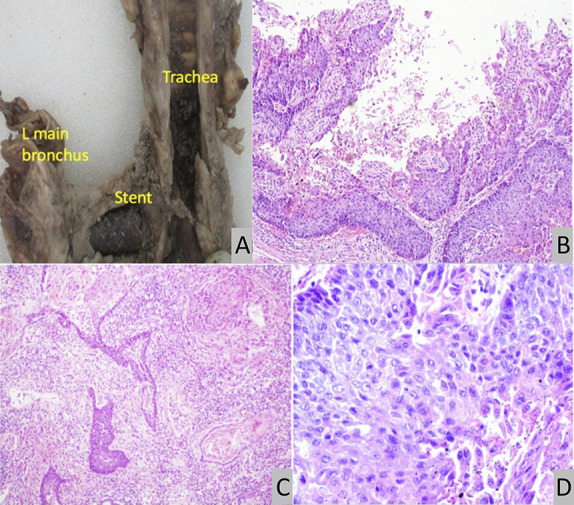
Left main stem endobronchial metal stent covering bronchoesophageal fistula (A). H&E sections of the distal esophagus and gastroesphageal junction show clusters of neoplastic squamous cells displaying endophytic growth pattern, moderate nuclear plemorphism, increased mitotic activity, and squamous pearl formation (B,C,D). H&E, hematoxylin & eosin.
DISCUSSION
Esophageal carcinoma cuniculatum, a well-differentiated variant of squamous cell carcinoma, presents unique diagnostic and treatment challenges. Weight loss and progressive dysphagia, like in our case, are frequent initial complaints with an obstructive esophageal mass invading the esophageal wall typically found on endoscopy. In our case, along with most others before it, multiple mucosal endoscopic, bronchoscopic, as well as EUS-guided biopsies of the mass were all nondiagnostic.4–7 The reasons for this diagnostic dilemma are multiple. Common histologic features of esophageal carcinoma cuniculatum: acanthosis, hyperkeratosis, dyskeratosis, deep keratinization, intraepithelial neutrophils, focal cytologic atypia, and keratin-fill cysts/burrows are nonspecific.4,5,7 As carcinoma cuniculatum is a well-differentiated subtype of squamous cell cancer, cytologic atypia seen in this malignancy resembles squamous reactive or reparative changes.7 Thus, superficial endoscopic biopsies are frequently misinterpreted as esophagitis or papilloma; in most cases, the diagnosis can only be made based on surgically resected or autopsy specimens. Finally, because of its rarity, the criteria for histologic diagnosis are not fully established.
The BEF, a rapidly fatal diagnosis,4,5 posed an additional management challenge in our case: The patient's high operative risk because of poor functional and nutritional status from chronic, progressive dysphagia limited the treatment options. Combined esophageal and endobronchial stenting allowed for successful palliation of both the BEF and the patient's dysphagia. The collaborative approach between multiple services was critical in the management of this complex case. The rarity of the malignancy coupled with the difficulty in obtaining pathologic diagnosis emphasizes the importance of its consideration in patients exhibiting a similar clinical course with negative or inconclusive biopsy results.
DISCLOSURES
Author contributions: MT Bell and S. Reicher: aided in conception and creation of manuscript, drafting of the manuscript, final approval, and agreement of accountability for all aspects of the work. KK Woo, M. Wu, C. Yap, and DW Hsia: aided conception of manuscript, drafting of the manuscript, final approval, and agreement of accountability for all aspects of the work. S. Reicher is the article guarantor.
Financial disclosure: S. Reicher: consultant for Boston Scientific Inc. None of the other authors have relevant financial disclosures.
Previous presentation: Case presented as a poster at the ACG Annual Scientific Meeting; October 23, 2023, Vancouver, BC, Canada.
Informed consent was obtained for this case report.
Contributor Information
Kenneth K. Woo, Email: kwoo@dhs.lacounty.gov.
Meifang Wu, Email: mewu@dhs.lacounty.gov.
Caroline Yap, Email: CYap@dhs.lacounty.gov.
David W. Hsia, Email: dhsia@dhs.lacounty.gov.
Sofiya Reicher, Email: sreicher@sbcglobal.net.
REFERENCES
- 1.Aird I, Johnson HD, Lennox B, Stansfeld AG. Epithelioma cuniculatum: A variety of squamous carcinoma peculiar to the foot. Br J Surg. 1954;42(173):245–50. [DOI] [PubMed] [Google Scholar]
- 2.Datar UV, Kale A, Mane D. Oral carcinoma cuniculatum: A new entity in the clinicopathological spectrum of oral squamous cell carcinoma. J Clin Diagn Res. 2017;11(1):ZD37–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puxeddu R, Cocco D, Parodo G, Mallarini G, Medda M, Brennan PA. Carcinoma cuniculatum of the larynx: A rare clinicopathological entity. J Laryngol Otol. 2008;122(10):1118–23. [DOI] [PubMed] [Google Scholar]
- 4.Landau M, Goldblum JR, DeRoche T, et al. Esophageal carcinoma cuniculatum: Report of 9 cases. Am J Surg Pathol. 2012;36(1):8–17. [DOI] [PubMed] [Google Scholar]
- 5.De Petris G, Lewin M, Shoji T. Carcinoma cuniculatum of the esophagus. Ann Diagn Pathol. 2005;9(3):134–8. [DOI] [PubMed] [Google Scholar]
- 6.Goh GH, Venkateswaran K, Leow PC, Loh KS, Thamboo TP, Petersson F. Carcinoma cuniculatum of the esophagus and tongue: Report of two cases, including TP53 mutational analysis. Head Neck Pathol. 2014;8(3):261–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu X, Yang D, Zhang X, Oduntan O. Esophageal carcinoma cuniculatum diagnosed on mucosal biopsies using a semiquantitative histologic schema: Report of two esophagectomy-confirmed cases. Gastroenterol Res. 2020;13(1):44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]


