Abstract
Female genital mutilation (FGM) is a common cultural practice, which involves the partial or complete removal of the external female genitalia. With increasing immigration from regions where the practice is endemic, there has been a growing prevalence of FGM in the United States and other developed nations. However, most medical professionals lack the baseline knowledge regarding FGM and its associated health complications. Given this increasing trend, dermatologists should anticipate an increasing number of patients with a history of FGM in their practice. While some of the obstetric, gynecologic, and psychologic consequences of FGM have been well-reported, the dermatologic findings are less characterized. Thus, this review article aims to provide dermatologists with a fundamental understanding of the prevalence, cultural significance, and health implications of FGM with a focus on the associated dermatological findings and provides recommendations on how dermatologists can address this sensitive matter.
Key words: female circumcision, female genital cutting, female genital mutilation
Capsule Summary.
-
•
This article provides a summary of the prevalence, health complications, cultural significance, and dermatologic consequences of female genital mutilation.
-
•
The field of dermatology is evolving, and dermatologists must expand their knowledge to better assist their diverse patients. This article will equip dermatologists with the necessary tools to effectively care for patients with female genital mutilation.
Introduction
Female genital mutilation (FGM) encompasses all nonmedical procedures involving removal or injury to the external female genitalia.1 Previously termed female genital circumcision, FGM was formally adopted by the United Nations to reflect the grave inhumane nature of the practice, and anatomical similarity to the partial or full resection of the male penis.2 FGM is prominent within 31 countries, including African regions from the Atlantic coast to the Horn of Africa, the Middle East, including Iraq and Yemen, and in Asia such as Indonesia (Fig 1). Data collected from these countries between 2012 and 2020 have shown that over 200 million women and girls have experienced FGM, and nearly 3 million girls are at-risk of undergoing the practice annually.3,4 Currently, there is an increasing number of girls and women in the United States at-risk of undergoing FGM. This risk is determined by applying country- and age-specific rates of FGM prevalence to the number of American women/girls with ties to those countries.5 FGM can no longer be seen as a phenomenon prevalent in underdeveloped regions but rather as a serious medical concern to be faced in the industrialized world. Herein, we review the prevalence, cultural significance, and health implications of FGM, and provide recommendations on how dermatologists can address this sensitive matter.
Fig 1.
Global prevalence indicating the percentage of women and girls aged 0 to 49 years who have undergone female genital mutilation/circumcision, by country (2012-2020).3
Source: Based on “Female Genital Mutilation/Cutting. A global concern,” UNICEF global database. FGM, Female genital mutilation.
FGM in the United States
With increasing immigration from regions where the practice is endemic, there is a growing prevalence of FGM in the United States. Although FGM was criminalized in the United States in 1996, over 500,000 women and girls in the country were at-risk of undergoing FGM in 2012—a marked increase from the 228,000 in 2000 (Fig 2).5 Within the United States, the practice is performed discreetly by traditional circumcisers, and in some instances, by physicians. Alternatively, families may travel overseas to undergo FGM, a practice known as “vacation cutting.”6
Fig 2.
Women and girls at risk of female genital mutilation (FGM) within the United States in 2012. At-risk: calculated by applying country- and age-specific FGM/circumcision prevalence rates to the number of US women and girls with ties to those countries (“country ties” as meeting at least one of the following criteria: (1) persons who were born in a high-FGM/circumcision prevalence country and (2) persons under age 30 who are residing with a parent who was born in a high FGM/circumcision prevalence country).5
Source: Based on “Female genital mutilation/cutting in the United States: updated estimates of women and girls at risk, 2012.” Public Health Records.
Currently, only 8 states: California, New York, Minnesota, Texas, Maryland, New Jersey, Virginia, and Washington, account for the majority of girls/women at-risk. California is estimated to have the highest number of girls/women at-risk (57,000), trailed by New York and Minnesota, with estimates of 48,000 and 44,000, respectively.5 The inordinate estimate in Minnesota can be attributed to the large Somali immigrant population in the state, estimated to be over 31,000 in 2013. Notably, 40% of reported cases are concentrated in 5 prominent cities: Los Angeles, Minneapolis-St. Paul, Seattle, New York, and Washington.5 The majority of these girls/women originate from 3 main countries—Egypt, Ethiopia, and Somalia. The FGM rates in Egypt is 74% within the Coptic population and 91% among Muslim Egyptians, while the estimates for Ethiopia and Somalia are 74% and 98%, respectively.4
Given the rise of FGM within the immigrant population, efforts to discontinue the practice have been implemented. FGM is currently outlawed in 35 states; however, state laws vary with respect to the age at which prohibition takes effect, those subject to prosecution, the penalties, and whether religious or cultural beliefs can be used as a legal defense.6 Additionally, in 2013, the US Congress criminalized the transportation of a minor outside the country for the purposes of FGM.6 Despite these efforts, the practice persists, and the numbers continue to rise.
Cultural significance
Describing the cultural significance of FGM is incredibly difficult, given the many nuances existing among cultures. Perpetrators of FGM commonly cite social acceptance, religious doctrine, purity/hygiene, preserving chastity, and ensuring marriageability as rationale for continuing the practice. In some cultures that practice FGM, the clitoris is a connotation of masculinity and therefore must be excised. For this reason, the female external genitalia in its natural form is considered unsightly and unclean. Thus, the act of mutilation aims to create a “more feminine,” aesthetic appearance. Interestingly, among women who have had reconstructive surgery, many have expressed feeling unattractive and preferred their preprocedure image.7 This may explain why women are socially and culturally conditioned to perceive FGM as an integral element of their femininity and womanhood—leading them to perpetuate the practice through generations.8
Comparable to menstruation in many cultures, practicing communities recognize FGM as a cultural rite of passage into womanhood. For many, FGM is viewed as a valuable achievement on the path to becoming an ideal woman and an avenue for inclusion into the network of respectable women within their community.9 For example, in certain cultures, young girls may even request to undergo FGM to secure social and cultural acceptance. Those who have not undergone FGM may be scrutinized and considered “impure” by their counterparts and society, leading to additional pressure on young girls to conform in order to feel a sense of belonging.10
Culturally, FGM provides prestige and guarantees to deliver on a chaste life and cleanliness. Although FGM carries no medical or hygienic benefits, practicing communities view uncut women as unhealthy, and unclean.10 In preserving chastity, FGM can play a significant role in a woman’s eligibility for marriage. For example, in cultures within Egypt, Somalia, and Sudan, extramarital sex is strictly prohibited and FGM serves to maintain chastity, and thus marriageability.8 In such areas with little economic opportunities, ensuring a daughter undergoes FGM is seen as an act of love to guarantee her financial security, marital success, and cultural acceptance.8
In certain regions, the tradition continues due to religious beliefs. However, studies have traced the origin of FGM to ancient Egypt in the fifth century BC, predating both Islam and Christianity.11 While in some countries, the majority of those engaged in FGM identify as Muslim (ie, Somalia, Guinea, Mali), the rates are comparable between faiths in high prevalence nations. For example, in Eritrea, where the population of both Muslims and Christians is roughly even, the rates for FGM among both groups exceed 80%.4 In some instances, FGM is more common among Christians, such as in Niger, where over 50% of Nigerien women and girls have undergone FGM, compared to less than 5% within the Muslim population.4 Given the practice is observed in a diverse set of countries, FGM cannot be attributed to a specific culture or religion.11
The cultural significance of FGM is highly intricate and multilayered, drawing from elements such as culture, tradition, and religion. The origin of the practice is deeply intertwined with one’s sense of self-identity, leading to its perpetuation.
FGM procedure and types
FGM is typically carried out by an elderly female traditional circumciser, often with inadequate or no medical training. Anesthesia and antiseptics are not generally used, and instruments include knives, scissors, scalpels, or razor blades. Most girls undergo FGM before age 5 (ranging from 4 to 14 years), either alone or among a cohort of girls.8
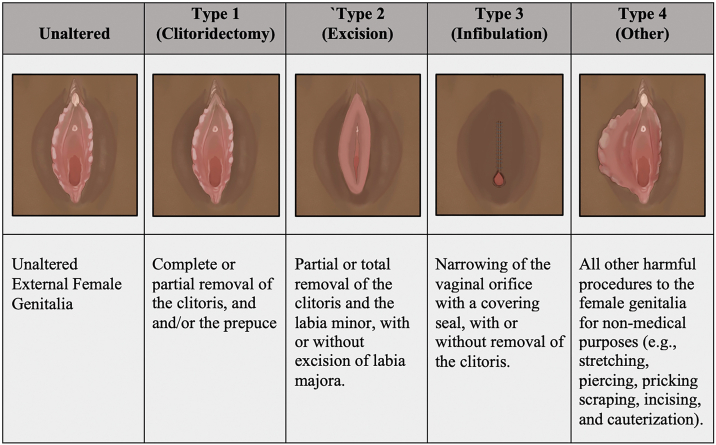
The World Health Organization classifies FGM into 4 types (Fig 3).8 The most common form, type I clitoridectomy, involves complete or partial removal of the clitoris and/or prepuce (clitoral hood). Type II, known as excision, includes all forms of type 1 with additional partial or complete removal of the labia minora and can include excision of the labia majora. The most severe form, type III infibulation, involves narrowing the vaginal orifice with a covering seal. This requires sewing the edges of the labia majora together. When healed, the fused labia create a seal that covers the urethra and a portion of the vagina. A small opening remains to allow for urinary and menstrual flow. Other methods classified as type IV include any harmful procedure (ie, piercing, stretching, incising, cauterization) to the female genitalia for nonmedical purposes. Generally, most women with FGM (80%-85%) have undergone type I and II, while 15% to 20% of women were subject to type III. However, in certain countries such as Djibouti, Somalia, and Sudan, infibulation rates are estimated at 80% to 90%.8
Fig 3.
Classifications of female genital mutilation.8
Source: “Female Genital Mutilation Types,” Illustrations by Ilhan Esse.
FGM health complications
From the onset of FGM and throughout life, those impacted suffer a sequela of complications (Supplementary Table I, available via Mendeley at https://doi.org/10.17632/wdcbgrvdj9.1). Immediately following the surgery, individuals can experience various short-term complications including significant pain related to nerve end damage, bleeding from cutting the clitoral artery or other blood vessels, infections from contaminated instruments, damage to the urethra causing urinary disturbances, and impaired wound healing.12 In particular, hemorrhage or infection can become life-threatening and cause morbidity.
The impact of FGM on gynecological health is significant, considering 45% to 75% of women experience dysmenorrhea, irregular, and/or prolonged menstrual flow.13, 14, 15 Furthermore, numerous studies have shown that women with FGM often experience a lack of sexual desire, anorgasmia, apareunia or dyspareunia, and vaginismus.16 Interestingly, research has suggested FGM may facilitate the transmission of HIV through various pathways.17 When multiple girls undergo the procedure together, the use of contaminated instruments can heighten infection rates. Additionally, tearing from sexual penetration—particularly in type 3 infibulation, where penetration can be especially painful, and nearly impossible—can cause tissue damage, postcoital bleeding, and impair wound healing. This can result in increased vaginal epithelium permeability, thereby promoting the spread of HIV and other sexually transmitted diseases.17
Undoubtedly, some of the most severe complications of FGM are seen during pregnancy and childbirth. Women with FGM have higher rates of emergency caesarean sections, postpartum hemorrhage, obstetric tears, instrumental deliveries, and extended maternal hospital stays.12 A recent systematic review found that women who underwent FGM were twice as likely as those without FGM to experience dyspareunia, perineal tears, prolonged labor, and episiotomy.18
The classic complications of FGM are not only physical but can lead to long-term effects on a victim's psychological and emotional well-being. These include higher rates of anxiety, depression, posttraumatic stress, substance use, and mood disorders.19 Many cultures that practice FGM may also stigmatize mental health, leaving victims hesitant to seek medical assistance, further contributing to the growing rates of undiagnosed and untreated mental health disorders seen amongst FGM victims.19
Reconstructive treatments
FGM results in long-term or even permanent damage to the genital area. Fortunately, there are options available for women in search of a reconstructive solution. However, these treatments and the surgeons qualified to perform them are limited and often only found at tertiary centers. Generally, all forms of FGM involve removing the clitoris; however, a portion of clitoral tissue may remain under the scar tissue. Clitoral reconstruction is a surgical technique that reveals the clitoris, and attempts to restore the function, appearance, and sensation to the structures damaged in FGM.20 This procedure has been considered safe and effective in reducing clitoral pain and restoring vulvar appearance. The combined postoperative complications rate generally range from 5% to 15%, frequently including hematoma, infection, and wound dehiscence.21 Studies have noted that while most participants self-reported significant symptomatic improvement, as many as 22% of women reported worsening sexuality-related outcomes following reconstruction.20,21 Potential limitations of these studies include small sample size, loss to follow-up, and a short follow-up period.21 Thus, additional research concerning the potential risks, and efficacy of the procedure is necessary to better understand the potential long-term outcomes.
In women with type 3 infibulation, deinfibulation may be performed to facilitate childbirth and reduce the risk of obstetric complications. Deinfibulation involves the reopening of the vaginal introitus, which is sealed in type 3 FGM. The procedure attempts to separate the fused labial tissue that partly obstructs the vaginal introitus and/or urethra, to restore normal vaginal appearance and expose the urethra.22 Deinfibulation is typically well tolerated with minimal to no postoperative complications. Some studies have indicated that deinfinbulation can lower the risk of postpartum hemorrhage and cesarean deliveries. Conversely, other research has reported the risk of episiotomy, cesarean delivery, vaginal lacerations, peripartum, and postpartum hemorrhage is comparable in women, regardless of prior type 3 FGM status.22,23 The potential benefits of defibulation are unclear and contradictory, therefore further research is warranted.
Addressing FGM in the dermatology clinical setting
Patients with FGM may seek dermatologic care for several types of cutaneous complications including keloids, abscess formation, clitoral neuromas, vulvar lymphangiectasias, and epidermoid cysts.24 Women with FGM, the majority being of African descent, are particularly susceptible to forming severe keloids, likely due to inflammation from various FGM related complications including poor wound healing, recurrent infections, and increased urinary retention.25 Following surgery, poor surgical technique and unsterile instruments can result in local abscess formation and severe vulvar inflammation. Latent abscess formation can also develop within inflamed or infected cysts, leading to recurrent dyspareunia.26 Additionally, clitoral neuromas may occur due to clitoral nerve entrapment in carelessly placed stitches or from scar tissue causing increased nerve strain. This can cause severe pain and often requires surgical removal (Fig 4).26,27
Fig 4.
Female genital mutilation (type II-III), complicated by a painful clitoral neuroma (arrow).26
Source: 2017, “Management of painful clitoral neuroma after female genital mutilation/cutting,” Jasmine Abdulcadir, Jean-Christophe Tille, Patrick Petignat, https://doi.org/10.1186/s12978-017-0288-3 CC BY 4.0 and CC0 1.0.
Vulvar lymphangiectasia is a rare cutaneous malformation resulting from obstruction of the superficial lymphatic channels causing abnormal dilation. Most often, the causes include infectious agents (filariasis, sexually transmitted diseases, and tuberculosis), scleroderma, Crohn’s disease, obstruction secondary to neoplasia, and surgery or radiotherapy.28 Clinically, lesions can present as clusters of translucent vesicles with clear or serosanguinous fluid. In some cases, these lesions can appear as firm, hyperkeratotic papules, and commonly misdiagnosed as genital warts.29 Patients may be asymptomatic or report intense pain, pruritus, recurrent infections, and frequent drainage. Itching can be acute and persistent resulting in overlying lichenified skin. Current treatment methods include surgical excision, cryosurgery, electrocautery, carbon dioxide laser surgery, and sclerotherapy. Despite treatment, lesions frequently return and require multiple interventions.28
The most frequently reported dermatologic complication is the creation of epidermal inclusion cysts, typically seen among women with infibulation (Fig 5).30 Cysts tend to develop at the surgical site as small, painless swellings but can expand progressively over the course of multiple years—and even decades—to form a large clitoral or vulvar mass.24 In most cases, the treatment is surgical removal, or carbon dioxide laser surgery.31 Even with excision, patients can still endure years of pelvic pain, dyspareunia, and micturition disruptions. Particularly large cysts may also complicate vaginal birth, necessitating prenatal removal, subsequently increasing the likelihood of additional obstetric complications.30
Fig 5.
Female genital mutilation (type I) complicated by a large epidermoid cyst at the site of mutilation.30
Source: 2016, “Vulvar epidermal inclusion cyst as a long-term complication of female genital mutilation,” Victoria-Martínez AM, Cubells-Sánchez L, Martínez-Leborans L, Sánchez-Carazo JL, de Miquel VA, https://doi.org/10.4103/0019-5154.174090, CC BY-NC-SA 3.0.
When FGM is encountered in clinical practice, dermatologists should personally acknowledge any preconceived biases regarding FGM and actively pursue further education on the topic before providing treatment. Women who have undergone FGM often delay treatment due to feelings of shame, especially in areas where FGM is stigmatized.8 Additionally, it is important to consider that women with FGM are more likely to refer to this practice as “circumcision.”32 Therefore, providers should maintain a respectful, empathetic, and nonjudgmental tone when addressing FGM to provide cultural humility that empowers patients to speak freely.8 Finally, due to its sensitive nature, FGM is an issue many providers may remain reluctant to address. By establishing rapport with patients, a comfortable environment can be fostered whereby practitioners can counsel patients on the health implications of FGM and thus play an essential role in eradicating this harmful practice.
Conclusion
The management of FGM transcends the boundaries of just a single health care branch to include fields as diverse as obstetrics-gynecology, internal medicine, psychiatry, urology, plastic surgery, and dermatology—all of whom benefit from baseline knowledge regarding FGM and its proper management. Studies investigating the knowledge, opinions, and practices of health care providers have exposed a considerable need for continued education at all medical levels and specialties.33,34 Therefore, prior to providing care, providers must ensure they are well-informed on the cultural significance of FGM, the health-related outcomes, and the personal experiences of those afflicted.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
Patient consent: Not applicable.
IRB approval status: Not applicable.
References
- 1.World Health Organization . Regional Office for Europe. WHO Guidelines on the Management of Health Complications From Female Genital Mutilation. World Health Organization; 2016. [PubMed] [Google Scholar]
- 2.World Health Organization . World Health Organization; 2008. Eliminating Female Genital Mutilation: An Interagency Statement-OHCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCR, UNICEF, UNIFEM, WHO. [Google Scholar]
- 3.Female Genital Mutilation/Cutting A global concern: UNICEF DATA. 2016. https://data.unicef.org/resources/female-genital-mutilationcutting-global-concern/
- 4.United Nations Children's Fund. Gupta G.R. Female genital mutilation/cutting: a statistical overview and exploration of the dynamics of change. Reprod Health Matters. 2013;21:184–190. [Google Scholar]
- 5.Goldberg H., Stupp P., Okoroh E., Besera G., Goodman D., Danel I. Female genital mutilation/cutting in the United States: updated estimates of women and girls at risk, 2012. Public Health Rep. 2016;131(2):340–347. doi: 10.1177/003335491613100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atkinson H.G., Ottenheimer D., Mishori R. Public health research priorities to address female genital mutilation or cutting in the United States. Am J Public Health. 2019;109(11):1523–1527. doi: 10.2105/AJPH.2019.305259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brady S.S., Connor J.J., Chaisson N., Sharif Mohamed F., Robinson B.B.E. Female genital cutting and deinfibulation: applying the theory of planned behavior to research and practice. Arch Sex Behav. 2021;50(5):1913–1927. doi: 10.1007/s10508-019-1427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . World Health Organization; 1998. Female Genital Mutilation: An Overview. [Google Scholar]
- 9.Esho T., Enzlin P., Van Wolputte S. Borderlands and Frontiers in Africa. LIT Verlag; 2013. Borders of the present: maasai tradition, modernity, and female identity; pp. 213–233. [Google Scholar]
- 10.Berg R.C., Denison E. A tradition in transition: factors perpetuating and hindering the continuance of female genital mutilation/cutting (FGM/C) summarized in a systematic review. Health Care Women Int. 2013;34(10):837–859. doi: 10.1080/07399332.2012.721417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Llamas J. University of Virginia Medical School Working Paper; 2017. Female Circumcision: The History, The Current Prevalence and The Approach to a Patient. [Google Scholar]
- 12.Libretti A., Bianco G., Corsini C., Remorgida V. Female genital mutilation/cutting: going beyond urogynecologic complications and obstetric outcomes. Arch Gynecol Obstet. 2023;308:1067–1074. doi: 10.1007/s00404-023-06929-6. [DOI] [PubMed] [Google Scholar]
- 13.Johnson-Agbakwu C.E., Fox K.A., Banke-Thomas A., Michlig G.J. Influence of female genital mutilation/cutting on health morbidity, health service utilization and satisfaction with care among Somali women and teenage girls in the United States. J Racial Ethn Health Disparities. 2023;10:788–796. doi: 10.1007/s40615-022-01266-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahmoud M.I.H. Effect of female genital mutilation on female sexual function, Alexandria, Egypt. Alexandria J. Med. 2016;52(1):55–59. [Google Scholar]
- 15.Kaplan A., Forbes M., Bonhoure I., et al. Female genital mutilation/cutting in the Gambia: long-term health consequences and complications during delivery and for the newborn. Int J Womens Health. 2013;5:323–331. doi: 10.2147/IJWH.S42064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berg R.C., Denison E. Does female genital mutilation/cutting (FGM/C) affect women's sexual functioning? A systematic review of the sexual consequences of FGM/C. Sex Res Soc Policy. 2012;9:41–56. [Google Scholar]
- 17.Brady M. Female genital mutilation: complications and risk of HIV transmission. AIDS Patient Care STDS. 1999;13(12):709–716. doi: 10.1089/apc.1999.13.709. [DOI] [PubMed] [Google Scholar]
- 18.Lurie J.M., Weidman A., Huynh S., Delgado D., Easthausen I., Kaur G. Painful gynecologic and obstetric complications of female genital mutilation/cutting: a systematic review and meta-analysis. PLoS Med. 2020;17(3) doi: 10.1371/journal.pmed.1003088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berg R.C., Denison E.M.L., Fretheim A. Norwegian Knowledge Centre for the Health Services; 2010. Psychological, Social and Sexual Consequences of Female Genital Mutilation/Cutting (FGM/C): A Systematic Review of Quantitative Studies. [PubMed] [Google Scholar]
- 20.Abdulcadir J., Rodriguez M.I., Say L. A systematic review of the evidence on clitoral reconstruction after female genital mutilation/cutting. Int J Gynecol Obstet. 2015;129(2):93–97. doi: 10.1016/j.ijgo.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berg R.C., Taraldsen S., Said M.A., Sørbye I.K., Vangen S. The effectiveness of surgical interventions for women with FGM/C: a systematic review. BJOG. 2018;125(3):278–287. doi: 10.1111/1471-0528.14839. [DOI] [PubMed] [Google Scholar]
- 22.Okusanya B.O., Oduwole O., Nwachuku N., Meremikwu M.M. Deinfibulation for preventing or treating complications in women living with type III female genital mutilation: a systematic review and meta-analysis. Int J Gynecol Obstet. 2017;136:13–20. doi: 10.1002/ijgo.12056. [DOI] [PubMed] [Google Scholar]
- 23.Esu E., Udo A., Okusanya B.O., Agamse D., Meremikwu M.M. Antepartum or intrapartum deinfibulation for childbirth in women with type III female genital mutilation: a systematic review and meta-analysis. Int J Gynecol Obstet. 2017;136:21–29. doi: 10.1002/ijgo.12055. [DOI] [PubMed] [Google Scholar]
- 24.Dave A.J., Sethi A., Morrone A. Female genital mutilation: what every American dermatologist needs to know. Dermatol Clin. 2011;29(1):103–109. doi: 10.1016/j.det.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 25.Ezebialu I., Okafo O., Oringanje C., et al. Surgical and nonsurgical interventions for vulvar and clitoral pain in girls and women living with female genital mutilation: a systematic review. Int J Gynecol Obstet. 2017;136:34–37. doi: 10.1002/ijgo.12048. [DOI] [PubMed] [Google Scholar]
- 26.Abdulcadir J., Tille J.C., Petignat P. Management of painful clitoral neuroma after female genital mutilation/cutting. Reprod Health. 2017;14:1–7. doi: 10.1186/s12978-017-0288-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morrone A., Hercogova J., Lotti T. Stop female genital mutilation: appeal to the international dermatologic community. Int J Dermatol. 2002;41(5):253–263. doi: 10.1046/j.1365-4362.2002.01481.x. [DOI] [PubMed] [Google Scholar]
- 28.Franco G., Toma L., Nosotti L., Muscardin L.M., Morrone A. Vulvar lymphangiectases on female genital mutilation mimicking genital warts. J Eur Acad Dermatol Venereol. 2006;20(8):1017–1018. doi: 10.1111/j.1468-3083.2006.01611.x. [DOI] [PubMed] [Google Scholar]
- 29.Khunger N. Combination technique of radiofrequency ablation with sclerotherapy in acquired lymphangiectasis of the vulva. J Cutan Aesthetic Surg. 2009;2(1):33. doi: 10.4103/0974-2077.53098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Victoria-Martínez A.M., Cubells-Sánchez L., Martínez-Leborans L., Sánchez-Carazo J.L., de Miquel V.A. Vulvar epidermal inclusion cyst as a long-term complication of female genital mutilation. Indian J Dermatol. 2016;61(1):119. doi: 10.4103/0019-5154.174090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Penna C., Fallani M.G., Fambrini M., Zipoli E., Marchionni M. Type III female genital mutilation: clinical implications and treatment by carbon dioxide laser surgery. Am J Obstet Gynecol. 2002;187(6):1550–1554. doi: 10.1067/mob.2002.127597. [DOI] [PubMed] [Google Scholar]
- 32.Hearst A.A., Molnar A.M. Female genital cutting: an evidence-based approach to clinical management for the primary care physician. Mayo Clin Proc. 2013;88(6):618–629. doi: 10.1016/j.mayocp.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Reig-Alcaraz M., Siles-González J., Solano-Ruiz C. A mixed-method synthesis of knowledge, experiences and attitudes of health professionals to female genital mutilation. J Adv Nurs. 2016;72(2):245–260. doi: 10.1111/jan.12823. [DOI] [PubMed] [Google Scholar]
- 34.Abdulcadir J., Dugerdil A., Boulvain M., et al. Missed opportunities for diagnosis of female genital mutilation. Int J Gynaecol Obstet. 2014;125(3):256–260. doi: 10.1016/j.ijgo.2013.11.016. [DOI] [PubMed] [Google Scholar]