Abstract
Background
There exists a high burden of oral diseases. Yet, the utilization of oral health care remains low. Understanding how, when, and why/why not individuals utilize dental healthcare resources is essential for planning health services and developing policies as it reflects the population's oral health needs, helps allocate resources efficiently, and formulate policies that are tailored to address their needs.
Objectives
To assess the utilization of dental health services and its associated factors along with barriers and facilitators among adults residing in Ernakulam district, Kerala, using the Anderson healthcare model for healthcare utilization.
Methods
A mixed-method study was conducted among adults aged 18 years and above in urban and rural wards of Ernakulam district using the cluster sampling method. Univariate and multivariate analysis were used for the quantitative part, and thematic analysis was used for the qualitative aspect. The total sample size was 544.
Results
The dental healthcare utilization was 15.4 ± 2.9 % among the study participants. Age and education were associated with dental healthcare utilization. The level of education, pain, and self-consciousness of oral diseases were independent predictors. Barriers identified were negative attitudes, financial restraints, and difficulty in access, while facilitators were trust in service providers, availability of services, and a positive attitude.
Conclusion
Utilization was poor despite the perceived need for oral health care. This was affected by several personal and system-level facilitators and barriers.
Keywords: Dental, Health care utilization, Anderson model, Adults, Barriers, Facilitators
Graphical abstract

1. Introduction
Dental caries, gingival and periodontal disease, loss of teeth, mucosal lesions and oropharyngeal carcinomas, Human Immunodeficiency Virus (Acquired Immuno-Deficiency Syndrome) - related oral manifestations and dento-oral trauma are leading oral health problems globally, and India is not an exception.1 While there has been notable progress in overall and dental health, the improvements have been unevenly distributed, resulting in a disproportionate burden of oral diseases among the underprivileged and vulnerable segments of the population.2
The prevalence rates of dental caries, early childhood caries, and periodontal disease in India are high, with a prevalence of 54.16 %, 49.6 %, and 51 %, respectively, as reported in various systematic reviews.3, 4, 5 Pregnant women lack an understanding of oral health which is vital during this period, leading to poor oral health care utilization.6 A significant lack of knowledge about conditions like oral precancers has also led to delayed treatment-seeking behavior.7 A systematic review highlights insufficient knowledge among community health workers, requiring more education on preventative and curative measures for oral health.8 Despite the high number of dental graduates in India, only a tiny percentage provide dental care to the rural population.9 Very few Primary Health Centres, considered the first contact point with the health care system, have dental surgeons and only a quarter of health centres in an Indian city offered dental services.10 Social health insurance programs in the country provide limited dental services, but their availability and usage are limited.11
It is argued that healthcare utilization should correlate with the need for care, awareness of that need, desire for care, and accessibility.12 Ensuring adequate access and availability for oral health care services is crucial, as it provides prospects for better health promotion, early disease prevention, timely diagnosis, and effective management of oral diseases and related conditions. In the Indian context, poor oral health awareness, limited availability of oral health care services in rural areas, and predominance of the private sector in health care delivery which is costlier compromise oral health-seeking behavior, which is further complicated by the excessive variation on social parameters such as income and education.13
Perceived need drives service utilization, while the absence of it hinders service delivery.14 Dental health services underutilization is associated with low socio-economic status, dental phobia, inconvenient location of care, and fatalistic beliefs. However, overutilization of dental services also increases the economic burden both on the individual and the healthcare administration.15 The World Dental Federation categorizes barriers to accessing dental services into three main groups: individual factors (lack of perceived need, anxiety or fear, financial considerations, and limited access), the dental profession (inadequate resources, uneven distribution, inadequate training, and insufficient consideration of patient attitudes), and society (lack of public support, limited facilities, inadequate planning, and insufficient research provision).16 Enablers for consistent dental health utilization include positive past experiences, trust in healthcare providers, availability of treatment centres, awareness of dental health importance, and dental health insurance.17
Healthcare utilization is crucial for health policy decision-making and are generally measured by the number of visits or the count of individuals who have visited in the past year.18 Several theoretical models, considering economic, psychosocial, cultural, and behavioral factors, have been developed to understand healthcare utilization.19 One prominent model is Andersen's Behavioural Model, which includes contextual and individual determinants.15 These determinants include predisposing characteristics (e.g., age, sex), enabling resources (e.g., income, perceived access), and need factors (e.g., self-rated health, chronic illness). The Andersen model has been widely studied and applied to dental services utilization, incorporating factors such as age, sex, education, dental attitudes, family income, and perceived difficulty visiting the dentist.20 A study which used this model defined utilization of dental services as number of visits to the dental professional over two years.21
Although applicable to dental settings, the Andersen model has been underutilized by researchers, particularly in India. Enablers and barriers to oral health utilization are context-specific22 and can vary across different geographic regions, particularly in culturally, economically, and socially diverse countries.23 Therefore, it is essential to understand why individuals decide to seek or not seek regular dental care to develop effective health policy interventions and reduce disparities in oral health outcomes.
Kerala is a state in the southern peninsular region of India. The state has been consistently ranked high in terms of health indicators.24 Yet, the burden of diseases, especially non-communicable diseases, remains high.25 Oral diseases are also highly prevalent in Kerala, with dental caries prevalence ranging from 37 to 69 %, periodontal diseases from 65 to 78 %, and the incidence of oral cancer per one lakh population about 16.4–21.6 in males and 6.4–9.1 in females.26 Kerala is also known for being highly literate which we assume would translate into better health awareness and thus better health-seeking behavior. Oral diseases are generally accorded low priority despite being ubiquitous, leading to poor oral health-seeking behavior.27 Assessing the utilization rate and their factors would be vital in addressing unmet dental health needs and crucial for efficient resource allocation, equitable access to care, and evidence-based policy development, ultimately leading to improved healthcare delivery and better oral health outcomes. Thus, this study aimed to quantitatively assess the prevalence of dental health utilization and associated factors based on the Anderson model and qualitatively assess the barriers and facilitators influencing dental health utilization.
2. Methodology
2.1. Study design and setting
A community-based mixed-method study was adopted for this study. This study was designed as a quantitative dominant mixed-method research where qualitative data was concurrently or parallelly collected. A questionnaire-based quantitative survey was carried out to determine the utilization of dental health services and associated factors. Using the descriptive qualitative approach, barriers, and facilitators to dental health service utilization were further explored among a sub-set of participants included in the study using an in-depth interview method. The interview guides were developed based on a literature review and were modified after each interview. In-depth interviews were conducted by an investigator trained in qualitative research. The study was conducted in urban and rural wards of Ernakulam district, located in the Indian state of Kerala. The Ernakulam administrative division comprises a corporation known as Kochi, thirteen municipalities, seven taluks, fourteen block panchayats, and one hundred and twenty-four villages.28 Districts in India have Taluks as administrative divisions, and Panchayat is the governance system that operates at the district, block, and village levels, with Gram Panchayats being the fundamental units of administration. The study was conducted over five months – between April 2022 and August 2022.
2.2. Study participants and sampling
The study was conducted among adults aged 18 years and above residing in the selected wards of Ernakulam district. Persons under isolation and quarantine restrictions due to COVID-19 and those unwilling to participate in the study were excluded.
The sample size was estimated based on a previous study where the proportion of people who had a dental health care visit during the past year was 28 %.29 With a 95 % confidence interval and relative precision of 20 % using the formula:
| N = Z (α/2)2 × P (1 − P)/C 2 |
where C is the relative precision, P is the population proportion & Z (α/2) = 1.96. The sample size was estimated to be 257. Since cluster sampling method was used, multiplying with a design effect of 2, the minimum sample size was 514.
A multi-stage cluster sampling method was used for the quantitative component of the study. Out of the thirteen municipalities in one municipality and out of fourteen blocks, one block was selected using a simple random method, and eight wards were chosen randomly by lottery method. Four panchayats were selected randomly from the selected block, and from each panchayath, two wards were chosen by a simple random technique. Thus, a total of 16 clusters were selected. Thirty-four participants from each cluster were selected to participate in the study. Concurrent with the quantitative questionnaires, the qualitative interviews were also conducted with respondents willing for an in-depth interview. Purposive sampling was adopted, and qualitative data collection was done until data saturation, leading to a comprehensive collection of 27 interviews.
2.3. Data collection tools and techniques
The quantitative cross-sectional study used a questionnaire validated by previous authors21 and adapted to the local context. The structured questionnaire based on the Anderson healthcare utilization model had six questions under predisposing factors: age, gender, education, household income, employment status, and place of residence. In-depth interviews were conducted using a semi-structured guide, which was prepared after extensive formative research.16,17,30,31 The interview guide addressed themes such as affecting the utilization of dental health services in domains such as a history of dental care, past experiences, access to service, oral health behaviors, barriers, and knowledge. Other additional probes were added to the interview guide as and when identified. Prior informed consent was obtained, and anonymity of data was promised.
2.4. Data analysis
The values obtained by the cross-sectional study were tabulated on Microsoft excel® sheet, and the analysis was done using IBM Statistical Package for Social Sciences (SPSS)®Version 25.0. Armonk, NY: IBM Corp. Categorical data were expressed as frequency and percentage & continuous data were expressed as mean and standard deviation. ‘Utilization of dental health care services among adults’ was expressed as a proportion with a 95 % confidence interval. Statistical significance of the association of various factors with dental health care utilization was tested using the chi-square test. Logistic regression analysis was used to find the independent predictors of dental health care utilization among adults and was expressed as Odds ratio and 95 % confidence interval. (p-value <0.05 was considered statistically significant). Qualitative data was translated to English, transcribed, and open-coded to categorize key themes and subthemes, and identified patterns with the help of Computer Assisted Qualitative Data Analysis Software, QDA Miner lite® for Windows. Each theme was analyzed to gain a deeper understanding of the factors associated with the utilization of dental health care services. Peer debriefing and member checking over telephonic feedback were conducted to ensure validity for the qualitative arm. Data were triangulated, and conclusions were drawn.
2.5. Ethical considerations
The study was approved by the Institutional Ethical Committee of Amrita Institute of Medical Sciences (ECASM-AIMS-2022-059). Written informed consent was obtained from all the participants prior to the data collection.
3. Results
3.1. Quantitative arm
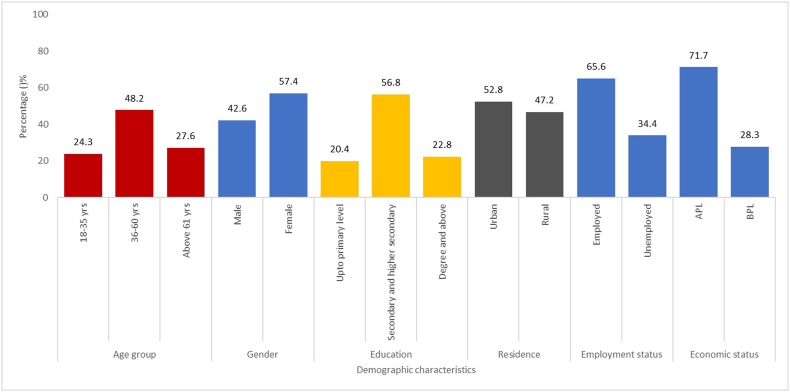
The study included 544 participants who met the inclusion criteria, with their demographic characteristics presented in Fig. 1 and Table 1. Table 2 outlines the factors associated with healthcare utilization based on the Anderson model, and the utilization of dental health services among adults residing in Ernakulam district was found to be 15.4 ± 2.9 %, with 84 individuals having consulted a dentist in the last year.
Fig. 1.
Characteristics of the study population (n = 544).
Table 1.
Characteristics of the study population (n = 544).
| Socio demographic characteristics | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| Age (In completed years) | 18–35 years | 132 | 24.3 |
| 36–60 years | 262 | 48.2 | |
| 61 years and above | 150 | 27.6 | |
| Gender | Males | 232 | 42.6 |
| Females | 312 | 57.4 | |
| Education | Up To Primary Level | 111 | 20.4 |
| Secondary and Higher Secondary | 309 | 56.8 | |
| Degree and above | 124 | 22.8 | |
| Economic status | APL | 390 | 71.7 |
| BPL | 154 | 28.3 | |
| Employment status | Employed | 357 | 65.6 |
| Unemployed | 187 | 34.4 | |
| Place of residence | Urban | 287 | 52.8 |
| Rural | 257 | 47.2 | |
Table 2.
Distribution of Anderson model health utilization factors (n = 544).
| Domains | Factors | Responses | Frequency (n) | Percentage (%) |
|---|---|---|---|---|
| Enabling resources | Difficulty in getting routine care | Yes | 50 | 9.2 |
| No | 494 | 90.8 | ||
| Need for care | Having problem that requires treatment | Yes | 232 | 42.6 |
| No | 312 | 57.4 | ||
| Health behaviours | Last visit to the dentist | Up to 1 year ago | 84 | 15.4 |
| Between 1 and 2 years | 33 | 6.1 | ||
| Between 2 and 5 years | 98 | 18.0 | ||
| More than 5 years ago | 164 | 30.1 | ||
| Never been to a dentist | 165 | 30.3 | ||
| Why to go to the dentist for | To have a regular check up | 9 | 1.7 | |
| To have an occasional check up | 21 | 3.9 | ||
| Only when having trouble with teeth | 349 | 64.2 | ||
| Never been to a dentist before | 165 | 30.3 | ||
| Oral health outcomes (In the last 12 months) | Painful aching in mouth | Yes | 156 | 28.7 |
| No | 388 | 71.3 | ||
| Discomfort in eating | Yes | 159 | 29.2 | |
| No | 385 | 70.8 | ||
| Self-consciousness of oral diseases | Never | 154 | 28.3 | |
| Hardly ever | 233 | 42.8 | ||
| Occasionally | 96 | 17.6 | ||
| Fairly often | 36 | 6.6 | ||
| Very often | 25 | 4.6 | ||
| Oral health status Self-assessment | Excellent | 87 | 16.0 | |
| Very good | 169 | 31.1 | ||
| Good | 204 | 37.5 | ||
| Poor | 77 | 14.2 | ||
| Very poor | 7 | 1.3 |
The study found a significant association between the utilization of dental healthcare among adults and their socio-demographic factors. Specifically, individuals aged 36–60 years comprised half of the dental healthcare users, while those with secondary and higher secondary education constituted the majority. These results were statistically significant, with a p-value of less than 0.001 (Table 3).
Table 3.
Univariate analysis for association of utilization with socio-demographic factors.
| Socio demographic characteristics | Categories | Dental health utilization |
Chi square value (p-value) | ||
|---|---|---|---|---|---|
| ≤1yr n (%) | >1yr n (%) | Never n (%) | |||
| Gender | Male | 33(39.3) | 120(40.7) | 79(47.9) | 2.702 (0.259) |
| Female | 51(60.7) | 175(59.3) | 86(52.1) | ||
| Economic status | APL | 62(73.8) | 210(71.2) | 118(71.5) | 0.225 (0.893) |
| BPL | 22(26.2) | 85(28.8) | 47(28.5) | ||
| Place of residence | Urban | 42(50.0) | 153(51.9) | 92(55.8) | 0.943 (0.623) |
| Rural | 42(50.0) | 142(48.1) | 73(44.2) | ||
| Age group | 18–35 | 18(21.4) | 45(15.3) | 69(41.8) | 41.91 (<0.001) |
| 36–60 | 42(50.0) | 155(52.5) | 65(39.4) | ||
| 61 and above | 24(28.6) | 95(32.2) | 31(18.8) | ||
| Employment status | Employed | 56(66.7) | 196(66.4) | 105(63.6) | 0.417 (0.812) |
| Unemployed | 28(33.3) | 99(33.6) | 60(36.4) | ||
| Education level | Up To Primary Level | 16(19.0) | 69(23.4) | 26(15.8) | 18.301 (0.001) |
| Secondary and Higher Secondary | 39(46.4) | 178(60.3) | 92(55.8) | ||
| Degree and above | 29(34.5) | 48(16.3) | 47(28.5) | ||
Table 4 presents the association between Anderson's factors and dental healthcare utilization. The study found a statistically significant proportion of individuals (64.3 %) who utilized dental healthcare had a perceived need for treatment, while 35 % had an unmet need for dental healthcare utilization. However, no association was found between enabling resources and dental health utilization. About 20 % of individuals utilizing dental healthcare occasionally experienced self-consciousness about their oral condition, while 11.9 % felt self-consciousness fairly often and 8.3 % felt it very often; furthermore, 44 % of those who had dental health utilization under one year self-assessed their oral health status as good, 26.2 % as very good and 8.3 % as excellent. A statistically significant proportion of individuals who did not receive dental healthcare within the past year experienced oral discomfort and self-consciousness due to oral problems. Specifically, 21.1 % experienced painful aching in the mouth, 25.4 % experienced discomfort while eating, and 26.7 % felt self-conscious about oral problems.
Table 4.
Univariate analysis for association of utilization with Anderson model factors.
| Variables | Dental health utilization |
Chi square value (p-value) | ||||
|---|---|---|---|---|---|---|
| ≤1yr n (%) | >1yr n (%) | Never n (%) | ||||
| Need for care | Having problem that requires treatment | Yes | 54(64.3) | 135(45.8) | 43(26.1) | 35.81 (<0.001) |
| No | 30(35.7) | 160(54.2) | 122(73.9) | |||
| Health behaviours | Why to go to the dentist | To have a regular check up | 9(10.7) | 0(0.0) | 0(0.0) | (<0.001) |
| To have an occasional check up | 11(13.1) | 10(3.4) | 0(0.0) | |||
| Only when having trouble with teeth | 64(76.2) | 285(96.6) | 0(0.0) | |||
| Never been to a dentist before | 0(0.0) | 0(0.0) | 165(100) | |||
| Painful aching in mouth | Yes | 59(70.2) | 74(25.1) | 23(13.9) | 90.32 (<0.001) | |
| No | 25(29.8) | 221(74.9) | 142(86.1) | |||
| uncomfortable to eat | Yes | 42(50.0) | 91(30.8) | 26(15.8) | 32.37 (<0.001) | |
| No | 42(50.0) | 204(69.2) | 139(84.2) | |||
| Self-consciousness of oral diseases | Never | 18(21.4) | 53(18.0) | 83(50.3) | 67.260 (<0.001) | |
| Hardly ever | 32(38.1) | 143(48.5) | 58(35.2) | |||
| Occasionally | 17(20.2) | 64(21.7) | 15(9.1) | |||
| Fairly often | 10(11.9) | 22(7.5) | 4(2.4) | |||
| Very often | 7(8.3) | 13(4.4) | 5(3.0) | |||
| Oral health status Self-assessment | Excellent | 7(8.3) | 15(5.1) | 65(39.4) | (<0.001) * | |
| Very good | 22(26.2) | 97(32.9) | 50(30.3) | |||
| Good | 37(44.0) | 128(43.4) | 39(23.6) | |||
| Poor | 18(21.4) | 52(17.6) | 7(4.2) | |||
| Very poor | 0(0.0) | 3(1.0) | 4(2.4) | |||
After categorizing dental health utilization into two groups (utilized and non-utilized) for multivariate analysis, it was found that education level, history of painful aching in the mouth, and self-consciousness about dental diseases were associated with dental health utilization (p-value <0.05), with individuals having secondary and higher secondary education having the highest odds of utilization compared to those with primary education (odds ratio of 7.21, 95 % CI 2.93–17.744, p-value <0.001). Self-consciousness about dental diseases and experiencing a painful aching in the mouth during the past year were also strong predictors of dental health utilization (Table 5).
Table 5.
Multivariate analysis for association of different variables with dental health care utilization.
| Variables | Responses | Dental healthcare utilization |
Adjusted odds ratio (95 % CI) | p value | |
|---|---|---|---|---|---|
| Utilized n (%) | Non utilized n (%) | ||||
| Self-conscious of dental disease | No | 50(59.5) | 337(73.3) | 2.359 (1.289–4.32) | 0.005 |
| Yes | 34(40.5) | 123(26.7) | |||
| Education level | Up to primary level | 16(19.0) | 95(20.7) | ||
| Secondary and higher secondary | 39(46.4) | 270(58.7) | 7.210 (2.93–17.744) | <0.001 | |
| Degree and masters | 29(34.5) | 95(20.7) | 4.706 (2.403–9.215) | <0.001 | |
| Painful aching in last 12 months | Yes | 59(70.2) | 97(21.1) | 13.109 (7.177–23.943) | <0.001 |
| No | 25(29.8) | 363(78.9) | |||
Individuals who had dental problems during the survey (need for care) were more likely to experience dental pain in the past year (oral health outcome), with an odds ratio of 22.176. Those who had difficulty accessing dental care had higher odds of feeling uncomfortable while eating, with an odds ratio of 5.012. Those with an existing need for care had higher odds of feeling uncomfortable while eating, with an odds ratio of 7.587(p-value <0.001).
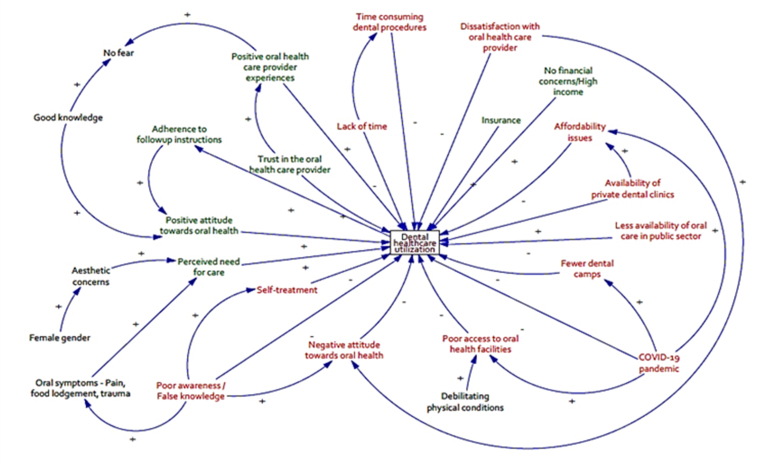
3.2. Qualitative arm
Data was collected from 27 participants regarding their perspectives on barriers and facilitators of dental health service utilization using in-depth interviews based on the customized interview guide. The selection of participants was based on the judgment of the investigator. The age of the participants ranged from 18 to 78 years, with a mean of 49.8 ± 15.9 years. The majority of the participants were females (60 %). Results were interpreted from which, themes and subthemes were identified. Financial and structural factors, dental service provider-related factors, and individual factors were the main themes under both categories of barriers (Appendix Table 1.) and facilitators (Appendix Table 2.) to dental healthcare utilization. Financial concerns, COVID-19-related barriers, and poor access were subthemes identified under financial and structural factors. Dissatisfaction with the provider and long waiting times were provider-related barriers, whereas fear/anxiety, self-treatment, negative attitude, and poor adherence were individual barriers. Availability, high income, and insurance were financial and structural facilitators. Trust in dental care providers, proper knowledge and absence of fear, need for care, gender, and aesthetics were individual facilitators. A past positive experience with the dental service provider was as a provider-related facilitator.
3.3. Meta-inferences
The majority of the findings from the quantitative data agreed with qualitative data. The lower percentage of dental healthcare utilization in the quantitative arm can be explained by the qualitative observation of the reduced mobility and financial instability of participants brought about by the COVID-19 pandemic. Dental healthcare utilization was observed to be lower in 61 and older years; this can be explained by the qualitative finding of the physical conditions acting as barriers to accessing dental care.
The higher education level was significantly associated with dental health utilization, supported by facilitators such as positive attitude and accurate knowledge about dental health. The participants below the poverty line used dental healthcare less than their economically higher counterparts, as observed from the quantitative data. This finding is supported by qualitative data that economic restraints were a significant barrier to dental healthcare utilization. Females were reported to have higher utilization of dental services in the survey; the underlying reason can be attributed to aesthetic concerns, as supported by in-depth interviews.
The qualitative findings indicate adequate availability of dental healthcare facilities, which aligns with the quantitative data, showing that most did not face difficulties accessing dental care. However, correlating with other emergent themes revealed a preference for private facilities due to a lack of awareness about public options. The participants' health behavior suggested that care was sought only while having some dental problems rather than routine checkups. The qualitative interviews yielded this negative attitude as a barrier to dental care. Participants who maintained a positive attitude towards dental health and good adherence to dental treatment were more confident about their oral health. This is supported by the quantitative data of a higher percentage of dental healthcare utilization by those who self-rated their oral health as good to excellent.
Although difficulty in getting routine dental care was associated with most of the oral health outcomes as inferenced from the quantitative data, qualitative data suggested differently. Upon experiencing the outcomes such as pain, chewing difficulty, and aesthetic concerns, most of the participants did not consider the challenges in getting dental care as a barrier as they wanted to rectify the presenting complaint as soon as possible. A causal interaction diagram of the various factors affecting dental healthcare utilization and its dynamics was generated by group discussion using Vensim® software(Fig. 2.).
Fig. 2.
Causal interaction model (+ indicates increase of factor, - indicates reduction of factor, red font indicates barrier, green font indicates facilitators).
4. Discussion
Several socio-demographic and interdependent factors, including difficulties in access, perceived treatment needs, and health behaviors, impacted the utilization of dental health services. These factors had an inter-relationship with oral health outcomes, as proposed by Anderson's healthcare utilization model, which our study had confirmed through univariate and multivariate analysis methods. Qualitative results further revealed barriers and facilitators influencing dental healthcare utilization. Higher education level, positive attitude, and accurate knowledge about dental health were significant facilitators for dental health utilization. The availability of dental healthcare facilities was sufficient, and participants who kept a positive attitude and good adherence to treatment were more confident about their oral health. In contrast, self-consciousness about dental diseases and experiencing painful aching in the mouth were strong predictors of dental health utilization.
The study aimed to determine dental healthcare utilization among adults in Ernakulam district, which was found to be 15.4 %, with similar studies in India reporting utilization rates of 28 % and 21.4 %, and studies in Thailand and Turkey showing rates of 36.1 % and 40.4 %, respectively.29,32,33,34 The lower utilization rates in our study could be corroborated by the qualitative finding in meta-inference that the COVID-19 pandemic had affected the dental health utilization pattern over the past two years, where overall reduction in access and availability of dental services occurred. This was similar to a study in Taiwan where after the COVID-19 outbreak, 17 % fewer patients had dental emergency utilization at a hospital emergency center relative to the previous period.35
We found that the proportion of females utilizing dental health care was higher than males, although the comparisons were not statistically significant. A similar pattern was observed in another study in India, which also shows higher utilization among females.32 On the contrary, few other studies revealed that males had higher dental visits.31,36 Urban and rural areas had similar dental healthcare utilization pattern, but the differences were not statistically significant. This was contrary to the findings by Pradeep et al., in which utilization was higher in people living in urban areas.32 Urban residents were more likely to use dental healthcare than rural residents.37 Utilization was lower among the 61-year-old age group when compared with the 36–60 years group, and this association was statistically significant. This agreed with the findings from a study that found the utilization was lower for those aged more than 55 years.36 People with employment and those belonging to Above Poverty Line (APL) were more likely to utilize dental healthcare, which may be linked to better socio-economic status, negating financial constraints as a barrier. A study done in Brazil also established that better socio-economic status was an enabling factor for dental healthcare use.38 Respondents with education up to a primary level were less utilizing dental healthcare, but surprisingly, they were least among those who never consulted a dentist. This may be due to the more prevalent dental problems forcing to have a consultation only in emergencies. The less educated population showed a lesser likelihood of dental visits.31,39
Most of our study population responded that they did not perceive any difficulty obtaining routine dental care. Yet actual utilization was less than which could be attributed to the health-seeking behavior pattern of visiting a dentist only on having dental problems. On further exploration in the qualitative interviews, it was opined that many did not find it necessary to go for a regular checkup. The overall perceived need for care was 42.6 %, whereas the utilization rate was 15.4 %, implying an existing gap between demand and utilization. The qualitative analysis further explained that financial concerns and personal accessibility barriers were some of the reasons for the proper utilization of dental healthcare. These findings were similar to a study in India where 40 % of the study participants had perceived treatment needs and lack of money as one barrier to dental care.32
Dental pain was the main reason for dental health utilization compared to other outcomes, such as chewing difficulty and perceived self-consciousness about dental problems. This finding was also validated through qualitative interviews. Many participants also felt that lack of pain indicated good oral health. Comparable results were observed in other studies conducted in India.16,32
Oral health status was measured as a self-assessment in our study. Perceived dental and gingival health were possible predictors for oral health status.40 The in-depth interviews indicated that the respondents’ self-assessments were based on the number of remaining teeth in the mouth, the ability to chew, and missing front teeth.
Financial and structural barriers to dental health utilization included compromised financial status, high cost of dental treatment, and COVID-related restrictions. Poverty was linked to a lesser utilization of dental health services.41 External constraints like dental insurance and social support were some of the other barriers identified by Amin and Perez.42 Dissatisfaction with a prior dental service provider and time concerns were barriers to dental healthcare service utilization as per our qualitative analysis, which is also agreed upon by other authors.43
In our study, a few facilitators emerged that were found to be conducive to dental healthcare utilization. These included an optimistic outlook towards dental health and strict adherence to instructions provided by dentists. Notably, these findings are consistent with the research conducted by Grembowski et al., which found that having a regular dental source or provider was also a facilitator for the utilization of dental healthcare services.44 Person-level factors like perceived need for care and concern for aesthetics were other facilitators identified.
4.1. Strengths, limitations, and recommendations
The study's strength lies in its community-based approach, allowing for an understanding of the local context and equitable distribution patterns of variables across urban and rural areas. Including diverse age groups and using cluster sampling with random methods ensured a high level of representativeness. At the same time, the mixed research design provided a deeper insight into participants' attitudes toward dental healthcare through qualitative explanations. This study has policy implications. The National Oral Health Programme is being implemented across the country and observations obtained from this study could help in planning and implementation of the program in the local context. Barriers to oral health seeking behaviour seem to be linked to socio-economic factors which warrants attention from the healthcare administration.
The model recommends considering oral health status as a health outcome, but due to the COVID-19 pandemic, it was not possible to conduct an objective assessment of oral health status in this study. The willingness of participants to undergo oral examinations was also compromised, possibly due to public stigma, as indicated by a preliminary survey. Therefore, self-reported oral conditions were utilized instead. However, we acknowledge that self-reporting may have introduced recall bias, particularly when inquiring about the timing of the last dental visit. At the same time, since the study included every adult from each household, it is possible that health behaviors and attitudes within the sample were similar, which could have partially overcome the bias.
Dental healthcare utilization was found to be significantly less than treatment needs, and closing this gap is necessary. Oral health awareness needs to be given importance by the policymakers to undertake efforts to uplift the public attitudes about regular dental attendance. The behavioral pattern of seeking dental care only for pain is to be rectified by an integrated approach where dental and medical practitioners can provide the correct information and advice, molding a preventive dental approach.
In the case of dental treatments, relying solely on primary prevention motivation may not be sufficient. Our study participants facing dental problems reported economic difficulties in accessing dental services and perceived high treatment costs. Increasing the availability of public dental care centres is crucial to address this issue. The integration of primary dental care into primary health care should be prioritized. Another approach that can be effective for dental treatments is public-private partnerships, which can reduce out-of-pocket expenses without negatively impacting the existing private dental care sector. Currently, the private sector plays a significant role in bridging the gap between dental care needs and utilization. The popularization of dental health insurance should be done carefully and only considered an adjunct, as even medical insurance utilization is limited to many unprivileged populations.
5. Conclusion
There exists a gap between the perceived need and actual utilization of dental health care. The economic limitations and negative attitudes towards routine checkups are significant barriers to accessing dental healthcare, particularly in old age, where physical conditions further exacerbate this issue. Despite more than half of the population having a favorable perception of oral health, there remains a need to improve the utilization of dental health services. This can be achieved by addressing issues related to the accessibility of public dental facilities, affordability of oral care, and the promotion of dental health education at the community level. To overcome these challenges, it is crucial to prioritize integrating primary dental care into primary health care and establish public-private partnerships to alleviate out-of-pocket expenses. Our study provides valuable insights into the current situation and lays the groundwork for future research.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Data availability statement
Raw data will be given to individuals for academic purposes upon reasonable request.
Disclosure
During the preparation of this work the author(s) used ChatGPT in order to improve the language and shortening few paragraphs in the introduction and discussion section. After using this tool/service, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
Financial support and sponsorship
Nil.
Author contribution
SS: conception and design, acquisition of data, interpretation of data, drafting the article, final approval of the version to be published.
RV: conception and design, data analysis and interpretation of data, revising article critically, final approval of the version to be published.
VK: design, analysis and interpretation of data, revising article critically, final approval of the version to be published.
GR: data analysis and interpretation of data, revising article critically, final approval of the version to be published.
Ethics statement
Study protocol was approved by the Institutional Ethical Committee of Amrita Institute of Medical Sciences (Ethical approval number: ECASM-AIMS-2022-059). Written informed consent was obtained from all the participants before the conduct of the study.
Declaration of competing interest
There are no conflicts of interest.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jobcr.2024.01.010.
Appendix.
Appendix Table 1.
Barriers in dental healthcare utilization
| Main themes | Subthemes | Inference | Quotes |
|---|---|---|---|
| Financial and structural factors | Financial concerns | Lack of money was the main barrier to dental healthcare utilization. Some found the cost of transport was unaffordable. Many had the impression that the dental treatments were costly. Poor availability of public dental health treatment facilities such as dental treatment availability in primary health centres were reported. Many of the participants are unaware of the dental services offered by public dental facilities. |
“But we have very less money with us so are not able to afford quality dental treatment”. (47-year-old female) “Government dental hospitals were very far and received advice that there waiting times is much more than these private clinics”. (50-year-old male) |
| COVID-19 related barriers | Many of the respondents reported that the spread of disease affected their financial status, many restricted themselves to their homes and thus depended on some home remedies. The closure of many dental facilities during the lockdown also created a mix-up. Many felt that dental camps were not available as a result of the Covid pandemic. | “Corona was also very much high at that time so it was very difficult to go to different and distant places during the lockdown, so took some pain medicines for dental pain”. (43-year-old female) | |
| Poor access | Access was poor for many respondents due to their own physical conditions which restricted their movement. Many older persons had to depend on others to visit a dentist, which they preferred to avoid. The distance of dental centres from the residence was an important barrier for them. Non-availability of regional dental check-up camps was also reported as a barrier. | “My son will come with a two-wheeler or auto rikshaw to take me to see the doctor during the appointment. I don't want to disturb him much so I won't call him to take me here and there every time.“. (67-year-old female) | |
| Individual factors/personal factors | Fear/anxiety | One respondent had expressed fear of pain that was limiting her from visiting a dentist despite the request from her parents. Drug allergy was a concern among one of the participants. Persons with medical conditions, feared complications such as bleeding which was a personal barrier among them in seeking proper dental care. | “Now I don't want to do any dental treatment. It is risky as said by a dental doctor I once consulted, as bleeding won't be stopping.” (70-year-old male) “because of this allergy problem, I usually don't go for any kind of dental treatments.” (39-year-old female) |
| Negative attitude and poor adherence | Some of the participants had a negative attitude toward regular dental check-ups restricting them from dental health utilization. Lack of pain was a reason for not visiting a dentist as they felt the absence of pain is an indicator of good health. Some of them didn't find it important to adhere to the instructions and visit for follow ups after their visit to the dentist. |
“But there is no need for me to go to the dentist as I don't have any tooth-related complaints”. (58-year-old male) “I will go to the doctor when only in pain, otherwise I will take medicines.” (43-year-old female) |
|
| Self-treatment | Some respondents had a habit of self-managing of dental problems with medicines such as pain killers. One person said that he had done alteration of dental appliance such as dentures by himself without proper medical advice. | “At first small edges were there which I adjusted myself, using a file to grind the sharp edges and polished with the sandpaper.” (70-year-old male) | |
| Dental service provider factors | Dissatisfaction with provider | A few persons recollected about unpleasant experiences during their past dental visits, as a result of which they haven't consulted the same dentist again. There were persons who felt that the treatments they received were unnecessary whereas complications arose from dental procedures were considered as the fault of the provider by a few participants. The difficulty in obtaining a specialist consent was a barrier for not consulting a dentist. | “There was a root left in my mouth during tooth removal which was done sometimes back in that hospital. It was causing pain and I have to undergo surgery to remove the root. After that, I never visited that doctor” (40-year-old female) |
| Time-consuming/long waiting time | Long waiting time at the dental facility is a barrier as it affects patients work schedule. | “a lot of people will be coming there; it will be crowded every time. It will take a full day for getting a treatment done because of the number of people waiting”. (43-year-old female) |
Appendix Table 2.
Facilitators for dental healthcare utilization
| Main themes | Subthemes | Inference | Quotes |
|---|---|---|---|
| Financial and structural factors | Availability | The availability of private or government dental health centres in an area was an enabler for most of the participants. The availability of dentist in the late evening was an enabling factor for some respondents as they felt it was very convenient. The dental treatment system available for the ex-defence personnel was an enabling factor in dental health utilization as per one respondent. One of the participants had utilized the vehicle facility by the dental college for transportation for denture placement. |
“But in the private clinic it is very convenient because doctor will be present every day. It is very easy for me to go to the clinic as it is very near, it is in a walkable distance from here” (43-year-old female) “Where I go there the doctor is working in a hospital and he will consult in the evening, it is open till night 10. So, it's very convenient for me.” (72-year-old male) |
| High income and insurance | Persons with a good source of income such as salary and pension didn't find utilizing dental health care a financial burden. Although dental health insurance is not commonly available one participant had benefitted from general health insurance which covered dental treatment following an accident. |
“I am a retired government employee and I have a pension now, so money is not a problem for me. My wife also has pension. So dental treatment is not a problem” (67-year-old male) “That doctor helped me with the required documents and in the insurance conditions they have mentioned that they will cover dental bridge placement following accident. 80 % of the expense was reimbursed by the insurance company” (34-year-old male) |
|
| Individual factors/personal factors | Trust in dental care provider | The trust in the doctor was expressed, as many had high opinions about the dentist whom they were consulting. The provision of discounts and facility to pay the treatment cost in instalments were some enablers as per some respondents. Affordable treatment costs were the reason for trust for some. The familiarity with the provider was an enabler as one person believed that the doctor knows about her allergies and he will be careful while prescribing medicines. | “This clinic was near to my place and we used to know this doctor for long time”. (38-year-old female) “because of my allergy I am fearful to go any new places as new doctors won't be knowing about my allergies. Already these doctors know I am allergic to drugs and which medicines to give”. (34-year-old female) |
| Proper knowledge and absence of fear | The attitude was better among persons who had a proper knowledge from qualified dental health professionals. Absence of fear was a facilitating factor for proper follow up treatments such as multiple tooth extractions |
“We had to bear the pain to remove teeth otherwise we can't put the set teeth so there is no point in fearing”. (43-year-old female) “Once in a year I will go to do teeth cleaning as my dentist advised me to do so.” (34-year-old female) |
|
| Need for care, gender and aesthetics | Pain from caries or trauma was usually assessed as a need for care and was a major enabler to dental health utilization. Some had to utilize dental health care following accidents whereas some had aesthetic reasons as a facilitator for utilization. One respondent wanted to do orthodontic treatment as she was a girl, gender becoming an enabling factor in this case. |
“I was really sad when my front teeth broke When the front teeth break away it's difficult face others. Isn't it?” (43-year-old female) “Once I went to nearby clinic for tooth cleaning because my gums had pain and blood was coming after brushing.” (37-year-old female) |
|
| Dental service provider factors | Past positive experiences from the dental service provider | Past experiences from previous dental service providers were enabler to consult the dentist repeatedly. Past experiences created a trust in the dentist and indirectly influenced in developing a positive attitude. The positive experiences were from both the dentist and staff. |
“My sister did orthodontic treatment there. It was very good treatment given by them and that's why I went there.” (18-year-old male) “The temporary tooth was replaced by a doctor who did it for free understanding my life situation .it was a very big help from that doctor” (52-year-old female) |
Appendix ASupplementary data
The following is/are the supplementary data to this article:
References
- 1.Petersen P.E., Bourgeois D., Ogawa H., Estupinan-Day S., Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83(9):661–669. [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen P.E. The World oral health report 2003: continuous improvement of oral health in the 21st century--the approach of the WHO global oral health Programme. Community Dent Oral Epidemiol. 2003;31(Suppl 1):3–23. doi: 10.1046/j..2003.com122.x. [DOI] [PubMed] [Google Scholar]
- 3.Pandey P., Nandkeoliar T., Tikku A.P., Singh D., Singh M.K. Prevalence of dental caries in the Indian population: a systematic review and meta-analysis. J Int Soc Prev Community Dent. 2021;11(3):256–265. doi: 10.4103/jispcd.JISPCD_42_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Devan I., Ramanarayanan V., Janakiram C. Prevalence of early childhood caries in India: a systematic review and meta-analysis. Indian J Publ Health. 2022;66(Supplement):S3–S11. doi: 10.4103/ijph.ijph_1078_22. [DOI] [PubMed] [Google Scholar]
- 5.Janakiram C., Mehta A., Venkitachalam R. Prevalence of periodontal disease among adults in India: a systematic review and meta-analysis. J Oral Biol Craniofacial Res. 2020;10(4):800–806. doi: 10.1016/j.jobcr.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gambhir R.S., Nirola A., Gupta T., Sekhon T.S., Anand S. Oral health knowledge and awareness among pregnant women in India: a systematic review. J Indian Soc Periodontol. 2015;19(6):612–617. doi: 10.4103/0972-124X.162196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhargava S. Need of oral pre cancer awareness initiatives in India. Open Dent J. 2016;10:417–419. doi: 10.2174/1874210601610010417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gambhir R.S., Anand S., Gupta T., Singh A., Kahlon H., Kaur A. Knowledge and awareness regarding oral health among anganwadi workers in India: a systematic review. J Indian Assoc Public Health Dent. 2016;14(2):231–236. doi: 10.4103/2319-5932.181900. [DOI] [Google Scholar]
- 9.Yaddanapalli S.C., Parveen Sultana S., Lodagala A., Babu P.C., Ravoori S., Pachava S. Oral healthcare-seeking behavior and perception of oral health and general healthcare among WHO indexed age groups in East-Coast India. J Fam Med Prim Care. 2020;9(7):3600–3606. doi: 10.4103/jfmpc.jfmpc_350_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iyer K., Krishnamurthy A., Pathak M., Krishnan L., Kshetrimayum N., Moothedath M. Oral health taking a back seat at primary health centers of Bangalore urban district, India - a situation analysis. J Fam Med Prim Care. 2019;8(1):251–255. doi: 10.4103/jfmpc.jfmpc_270_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kadaluru U.G., Naryanappa R.J. Social insurance for oral healthcare: analysis of two insurance schemes in India. J Oral Health Community Dent. 2022;15(3):122–128. doi: 10.5005/jp-journals-10062-0112. [DOI] [Google Scholar]
- 12.Health-Care Utilization as a Proxy in Disability Determination. National Academies Press (US); 2018. National academies of Sciences E, division H and M, services B on HC, disabilities C on HCU and A with. Factors that affect health-care utilization.https://www.ncbi.nlm.nih.gov/books/NBK500097/ [PubMed] [Google Scholar]
- 13.Singh A., Purohit B.M. Addressing oral health disparities, inequity in access and workforce issues in a developing country. Int Dent J. 2013;63(5):225–229. doi: 10.1111/idj.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malik Normaliza Ab, Rosalien Robbykha, Khalissya Nadine, Badruddin Iwany Amalliah, Maharani Diah Ayu. Perceived need and utilization of dental health car ed need and utilization of dental health care services in vices in Indonesia: a secondary analysis using the national socioeconomic data. Makara J Health Res. 2020;24(2):121–127. [Google Scholar]
- 15.Jönsson B., Holde G.E., Baker S.R. The role of psychosocial factors and treatment need in dental service use and oral health among adults in Norway. Community Dent Oral Epidemiol. 2020;48(3):215–224. doi: 10.1111/cdoe.12518. [DOI] [PubMed] [Google Scholar]
- 16.Fotedar S., Sharma K.R., Bhardwaj V., Sogi G.M. Barriers to the utilization of dental services in Shimla, India. Eur J Gen Dent. 2013;2(2):139–143. doi: 10.4103/2278-9626.112314. [DOI] [Google Scholar]
- 17.Bahramian H., Mohebbi S.Z., Khami M.R., Quinonez R.B. Qualitative exploration of barriers and facilitators of dental service utilization of pregnant women: a triangulation approach. BMC Pregnancy Childbirth. 2018;18(1):153. doi: 10.1186/s12884-018-1773-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poudyal S., Rao A., Shenoy R., Priya H. Utilization of dental services in a field practice area in mangalore, Karnataka. Indian J Community Med Off Publ Indian Assoc Prev Soc Med. 2010;35(3):424–425. doi: 10.4103/0970-0218.69278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernández-Olano C., Hidalgo J.D.L.T., Cerdá-Díaz R., et al. Factors associated with health care utilization by the elderly in a public health care system. Health Policy Amst Neth. 2006;75(2):131–139. doi: 10.1016/j.healthpol.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Reisine S. A path analysis of the utilization of dental services. Community Dent Oral Epidemiol. 1987;15(3):119–124. doi: 10.1111/j.1600-0528.1987.tb00497.x. [DOI] [PubMed] [Google Scholar]
- 21.Marshman Z., Porritt J., Dyer T., Wyborn C., Godson J., Baker S. What influences the use of dental services by adults in the UK? Community Dent Oral Epidemiol. 2012;40(4):306–314. doi: 10.1111/j.1600-0528.2012.00675.x. [DOI] [PubMed] [Google Scholar]
- 22.Phillips K.A., Morrison K.R., Andersen R., Aday L.A. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33(3 Pt 1):571–596. [PMC free article] [PubMed] [Google Scholar]
- 23.Alzubaidi H., Namara K.M., Browning C., Marriott J. Barriers and enablers to healthcare access and use among Arabic-speaking and Caucasian English-speaking patients with type 2 diabetes mellitus: a qualitative comparative study. BMJ Open. 2015;5(11) doi: 10.1136/bmjopen-2015-008687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.NITI Aayog . National Institution for Transforming India, Government of India; 2022. Health Performance : NITI Aayog.http://social.niti.gov.in/hlt-ranking [Google Scholar]
- 25.Sarma P.S., Sadanandan R., Thulaseedharan J.V., et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ Open. 2019;9(11) doi: 10.1136/bmjopen-2018-027880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramanarayanan V., Janakiram C., Joseph J., Krishnakumar K. Oral health care system analysis: a case study from India. J Fam Med Prim Care. 2020;9(4):1950–1957. doi: 10.4103/jfmpc.jfmpc_1191_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Janakiram C., Sanjeevan V., Br R., Joseph J., Stauf N., Benzian H. Political priority of oral health in India: analysis of the reasons for neglect. J Publ Health Dent. 2018;78(2):144–153. doi: 10.1111/jphd.12254. [DOI] [PubMed] [Google Scholar]
- 28.Government of Kerala . 2022. Ernakulam District Website | Kerala State,India | India.https://ernakulam.nic.in/ [Google Scholar]
- 29.Kadaluru U.G., Kempraj V.M., Muddaiah P. Utilization of oral health care services among adults attending community outreach programs. Indian J Dent Res Off Publ Indian Soc Dent Res. 2012;23(6):841–842. doi: 10.4103/0970-9290.111290. [DOI] [PubMed] [Google Scholar]
- 30.Mariño R., Giacaman R.A. Patterns of use of oral health care services and barriers to dental care among ambulatory older Chilean. BMC Oral Health. 2017;17(1):38. doi: 10.1186/s12903-016-0329-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kakatkar G., Bhat N., Nagarajappa R., et al. Barriers to the utilization of dental services in Udaipur, India. J Dent Tehran Iran. 2011;8(2):81–89. [PMC free article] [PubMed] [Google Scholar]
- 32.Pradeep Y., Chakravarty K.K., Simhadri K., Ghenam A., Naidu G.M., Vundavalli S. Gaps in need, demand, and effective demand for dental care utilization among residents of Krishna district, Andhra Pradesh, India. J Int Soc Prev Community Dent. 2016;6(Suppl 2):S116–S121. doi: 10.4103/2231-0762.189737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jaidee J., Ratanasiri A., Chatrchaiwiwatana S., Soonthon S. Prevalence and factors associated with the utilization of dental care services among factory workers in Nava Nakorn industrial estate, Pathumthani Province, Thailand. J Med Assoc Thail Chotmaihet Thangphaet. 2015;98(Suppl 6):S73–S80. [PubMed] [Google Scholar]
- 34.Mumcu G., Sur H., Yildirim C., Soylemez D., Atli H., Hayran O. Utilisation of dental services in Turkey: a cross-sectional survey. Int Dent J. 2004;54(2):90–96. doi: 10.1111/j.1875-595x.2004.tb00261.x. [DOI] [PubMed] [Google Scholar]
- 35.Wu J.H., Lee M.K., Lee C.Y., et al. The impact of the COVID-19 epidemic on the utilization of dental services and attitudes of dental residents at the emergency department of a medical center in Taiwan. J Dent Sci. 2021;16(3):868–876. doi: 10.1016/j.jds.2020.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vashisth S., Gupta N., Bansal M., Rao N.C. Utilization of services rendered in dental outreach programs in rural areas of Haryana. Contemp Clin Dent. 2012;3(6):164–166. doi: 10.4103/0976-237X.101076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Devaraj C., Eswar P. Reasons for use and non-use of dental services among people visiting a dental college hospital in India: a descriptive cross-sectional study. Eur J Dermatol. 2012;6(4):422–427. [PMC free article] [PubMed] [Google Scholar]
- 38.Machry R.V., Tuchtenhagen S., Agostini B.A., et al. Socioeconomic and psychosocial predictors of dental healthcare use among Brazilian preschool children. BMC Oral Health. 2013;13:60. doi: 10.1186/1472-6831-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Afonso-Souza G., Nadanovsky P., Chor D., Faerstein E., Werneck G.L., Lopes C.S. Association between routine visits for dental checkup and self-perceived oral health in an adult population in Rio de Janeiro: the Pró-Saúde Study. Community Dent Oral Epidemiol. 2007;35(5):393–400. doi: 10.1111/j.1600-0528.2006.00343.x. [DOI] [PubMed] [Google Scholar]
- 40.Sharififard N., Sargeran K., Gholami M. Perception of oral health and medical conditions as possible predictors of oral health status in visually impaired adolescents: a cross-sectional study. BMC Oral Health. 2021;21(1):89. doi: 10.1186/s12903-021-01447-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lambert R.F., Orrell C., Haberer J.E. “It was pain. That's it. It was pain.” Lack of oral health care among otherwise healthy young adults living with HIV in South Africa: a qualitative study. PLoS One. 2017;12(12) doi: 10.1371/journal.pone.0188353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amin M., Perez A. Is the wait-for-patient-to-come approach suitable for African newcomers to Alberta, Canada? Community Dent Oral Epidemiol. 2012;40(6):523–531. doi: 10.1111/j.1600-0528.2012.00698.x. [DOI] [PubMed] [Google Scholar]
- 43.Marcus K., Balasubramanian M., Short S., Sohn W. Barriers and facilitators to dental care among culturally and linguistically diverse carers: a mixed-methods systematic review. Community Dent Oral Epidemiol. 2022;51(2):327–344. doi: 10.1111/cdoe.12745. [DOI] [PubMed] [Google Scholar]
- 44.Grembowski D., Spiekerman C., Milgrom P. Racial and ethnic differences in a regular source of dental care and the oral health, behaviors, beliefs and services of low-income mothers. Community Dent Health. 2009;26(2):69–76. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Raw data will be given to individuals for academic purposes upon reasonable request.