Abstract
Background
In CheckMate 9LA, nivolumab plus ipilimumab with chemotherapy prolonged overall survival (OS) versus chemotherapy regardless of tumor PD-L1 expression or histology. We report updated efficacy and safety in all randomized patients with a minimum 4-year follow-up and an exploratory treatment-switching adjustment analysis in all treated patients who received chemotherapy and subsequent immunotherapy.
Methods
Adults with stage IV/recurrent non-small cell lung cancer (NSCLC), no sensitizing EGFR/ALK alterations, and ECOG performance status ≤1 were randomized 1:1 to nivolumab 360 mg every 3 weeks plus ipilimumab 1 mg/kg every 6 weeks with chemotherapy (two cycles) or chemotherapy (four cycles, with optional maintenance pemetrexed for the nonsquamous population). Assessments included OS, progression-free survival, and objective response rate. Exploratory analyses included efficacy by tumor PD-L1 expression and histology and in patients who discontinued nivolumab plus ipilimumab with chemotherapy due to treatment-related adverse events (TRAEs), and a treatment-switching adjustment analysis using inverse probability of censoring weighting.
Results
With a 47.9-month minimum follow-up for OS, nivolumab plus ipilimumab with chemotherapy continued to prolong OS over chemotherapy in all randomized patients (HR 0.74, 95% CI 0.63 to 0.87; 4-year OS rate: 21% versus 16%), regardless of tumor PD-L1 expression (HR (95% CI): PD-L1<1%, 0.66 (0.50 to 0.86) and ≥1%, 0.74 (0.60 to 0.92)) or histology (squamous, 0.64 (0.48 to 0.84) and non-squamous, 0.80 (0.66 to 0.97)). In patients who discontinued all components of nivolumab plus ipilimumab with chemotherapy due to TRAEs (n=61), the 4-year OS rate was 41%. With treatment-switching adjustment for the 36% of patients receiving subsequent immunotherapy in the chemotherapy arm, the estimated HR of nivolumab plus ipilimumab with chemotherapy versus chemotherapy was 0.66 (95% CI 0.55 to 0.80). No new safety signals were observed.
Conclusions
In this 4-year update, patients treated with nivolumab plus ipilimumab with chemotherapy continued to have long-term, durable efficacy benefit over chemotherapy regardless of tumor PD-L1 expression and/or histology. A greater estimated relative OS benefit was observed after adjustment for subsequent immunotherapy use in the chemotherapy arm. These results further support nivolumab plus ipilimumab with chemotherapy as a first-line treatment for patients with metastatic/recurrent NSCLC, including those with tumor PD-L1<1% or squamous histology, populations with high unmet needs.
Keywords: clinical trials, phase III as topic; drug therapy, combination; immunotherapy; non-small cell lung cancer; programmed cell death 1 receptor
Video Abstract.
Disclaimer: this video summarises a scientific article published by BMJ Publishing Group Limited (BMJ). The content of this video has not been peer-reviewed and does not constitute medical advice. Any opinions expressed are solely those of the contributors. Viewers should be aware that professionals in the field may have different opinions. BMJ does not endorse any opinions expressed or recommendations discussed. Viewers should not use the content of the video as the basis for any medical treatment. BMJ disclaims all liability and responsibility arising from any reliance placed on the content.
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Immunotherapies that target the programmed cell death (ligand) 1 (PD-(L)1) pathway, with or without other treatment modalities, have improved the overall survival of patients with metastatic non-small cell lung cancer (NSCLC) without targetable mutations. The CheckMate 9LA regimen of nivolumab plus ipilimumab with two cycles of chemotherapy was shown to provide long-term clinical benefit over chemotherapy as first-line treatment in patients with metastatic or recurrent NSCLC. However, unmet needs remain in patients with metastatic NSCLC.
WHAT THIS STUDY ADDS
With 4 years of follow-up data, this report indicates that nivolumab plus ipilimumab with two cycles of chemotherapy provides long-term, durable survival benefit over chemotherapy alone in patients with metastatic NSCLC, including those with tumor PD-L1 expression <1% or squamous histology. The survival benefit of nivolumab plus ipilimumab with chemotherapy versus chemotherapy was further proven by the results from exploratory treatment-switching adjustment analyses, which demonstrated greater estimated overall survival benefit after adjusting for the potential bias introduced by subsequent immunotherapy received by patients in the chemotherapy arm.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This study provides additional support for the use of nivolumab plus ipilimumab with chemotherapy as a first-line treatment for patients with metastatic or recurrent NSCLC, regardless of tumor PD-L1 expression level or tumor histology, among which, tumor PD-L1 expression <1% and squamous histology populations represent a high unmet need.
Introduction
Over the past decade, immunotherapy-based regimens have transformed the treatment landscape for non-small cell lung cancer (NSCLC) and are currently first-line therapy options for eligible patients with metastatic NSCLC without targetable mutations.1–3 Nivolumab and ipilimumab are immune checkpoint inhibitors with distinct but complementary mechanisms of action targeting programmed death 1 (PD-1) and cytotoxic T lymphocyte antigen-4 (CTLA-4), respectively. Dual immunotherapy with first-line nivolumab plus ipilimumab, with or without concurrent chemotherapy, has shown long-term, durable overall survival (OS) benefit in patients with several advanced cancers, including metastatic NSCLC.4–8 Although multiple phase 3 randomized trials of immunotherapy alone9 or in combination with chemotherapy10 11 have reported clinical survival outcomes at the 5-year milestone, long-term survival in certain subpopulations, such as those with tumor programmed death ligand 1 (PD-L1) expression <1%12 13 or squamous histology,11 remains suboptimal.
In the randomized, phase 3 CheckMate 9LA trial (NCT03215706), OS was significantly improved in patients with metastatic NSCLC treated with first-line nivolumab plus ipilimumab combined with two cycles of platinum-doublet chemotherapy versus four cycles of chemotherapy alone (median OS 14.1 versus 10.7 months, respectively; HR 0.69, 96.71% CI 0.55 to 0.87), meeting the primary endpoint.14 On the basis of these results, the combination regimen of nivolumab plus ipilimumab combined with two cycles of chemotherapy was approved in the USA, European Union, and several other countries for the first-line treatment of metastatic NSCLC.15 16 Treatment guidelines by the National Comprehensive Cancer Network, the American Society of Clinical Oncology, and the European Society for Medical Oncology currently recommend nivolumab plus ipilimumab with chemotherapy as a first-line therapy option for patients with metastatic NSCLC, regardless of tumor PD-L1 expression level or tumor histology.1–3 At the 3-year follow-up from CheckMate 9LA, nivolumab plus ipilimumab with chemotherapy continued to prolong OS versus chemotherapy alone (HR 0.74, 95% CI 0.62 to 0.87; 3-year OS rate 27% versus 19%), despite the fact that 36% of patients in the chemotherapy arm received subsequent immunotherapy.4
With the approval of several immunotherapy agents in the second-line setting, there has been growing use of subsequent immunotherapy postprogression on first-line chemotherapy, which can confound OS analyses in clinical trials that compare first-line immunotherapies to chemotherapy control arms.17 18 Previous reports have demonstrated that adjusting for potential biases in the calculation of treatment effect introduced by patients switching from chemotherapy to immunotherapy increased the relative survival with immunotherapy-based treatment versus the adjusted chemotherapy arm.19 20
Here, we present updated efficacy and safety data from CheckMate 9LA in patients with at least 4 years of follow-up. Additionally, we report exploratory efficacy outcomes from patients who discontinued nivolumab plus ipilimumab with chemotherapy due to treatment-related adverse events (TRAEs) and results from an exploratory treatment-switching adjustment analysis in patients who switched from chemotherapy to subsequent immunotherapy. See also the graphical abstract.
jitc-2023-008189supp002.pdf (1.2MB, pdf)
Materials and methods
The study design, patient eligibility criteria, and protocol of CheckMate 9LA have previously been described4 14 21 and are briefly summarized here.
Study design and patients
CheckMate 9LA is a randomized, open-label, international phase 3 trial.14 Enrolled patients were aged ≥18 years with squamous or non-squamous stage IV/recurrent NSCLC, Eastern Cooperative Oncology Group performance status 0 or 1, and no known sensitizing EGFR/ALK alterations. Patients were stratified by tumor histology (squamous versus non-squamous), sex (male versus female), and tumor PD-L1 expression (<1% versus ≥1%); patients without quantifiable tumor PD-L1 expression were stratified with the <1% population but were only included in analyses of the all-randomized population, as previously described.14 21
Patients were randomized 1:1 to receive nivolumab (360 mg every 3 weeks) plus ipilimumab (1 mg/kg every 6 weeks) combined with platinum-doublet chemotherapy (every 3 weeks for two cycles) or chemotherapy alone (every 3 weeks for four cycles) (online supplemental figure S1). Treatment continued until disease progression (unless prespecified criteria were met for treatment beyond progression in the experimental arm), unacceptable toxicity, or until patients had received 2 years of immunotherapy in the experimental arm. Optional pemetrexed maintenance therapy (500 mg/m2 every 3 weeks), permitted for the non-squamous population of the control arm only, has been described previously.4 14 21 Per protocol, no crossover between treatment arms was allowed; however, patients could receive subsequent immunotherapy at the physician’s discretion if study treatment was discontinued in either group.
jitc-2023-008189supp001.pdf (1.5MB, pdf)
Endpoints and assessments
The primary, secondary, and other protocol-specified and exploratory endpoints have been reported previously (online supplemental figure S1).4 14 21 With a 4-year minimum follow-up, exploratory analyses of updated OS, progression-free survival (PFS), objective response rate (ORR), and duration of response (DOR) were conducted in all randomized patients, in patients by tumor PD-L1 expression (<1%, ≥1%, 1%–49%, or ≥50%), tumor histology (squamous or non-squamous), and by both tumor PD-L1 expression and histology. Other exploratory analyses included efficacy assessments in patients who discontinued all components of nivolumab plus ipilimumab with chemotherapy due to TRAEs (OS from randomization; PFS and DOR from time of treatment discontinuation)21 and treatment-switching adjustment analyses, which were conducted to account for potential bias in the estimation of OS due to subsequent immunotherapy treatment in the chemotherapy-alone arm. The subsequent use of immunotherapy in patients after chemotherapy can introduce bias in the calculation of treatment effect, potentially leading to an underestimation of the survival benefit of the experimental treatment regimen. Thus, these analyses were performed to better clarify the efficacy difference between nivolumab plus ipilimumab with chemotherapy and chemotherapy alone.
Safety outcomes were reported as adverse events observed between the first dose and 30 days after the last dose of study therapy and graded per National Cancer Institute Common Terminology Criteria for Adverse Events (version 4.0), with the exception of immune-mediated adverse events (IMAEs), which were recorded between the first dose and within 100 days after the last dose of study therapy. Additional details of the study endpoints were previously reported.4 14 21
Statistical analysis
Efficacy and safety outcomes were evaluated in all randomized patients and in all patients who received ≥1 dose of study drug (all treated patients), respectively. Kaplan-Meier methodology was used to estimate OS and PFS curves. HRs and associated 95% CIs were estimated using stratified (all randomized patients) or unstratified (patient subgroups) Cox proportional hazards models with treatment arm as a single covariate. The Clopper-Pearson method was used to estimate response rates and exact two-sided 95% CIs.
Treatment-switching adjustment analyses were conducted in all-treated patients using four statistical methods as recommended by NICE Decision Support Unit Technical Support Document 16,22 similar to previously described analyses20: inverse probability of censoring weighting (IPCW),23 rank-preserving structural failure time (RPSFT),24 iterative parameter estimation (IPE),25 and simplified two-stage estimation (TSE).18 The primary treatment-switching analysis was conducted using IPCW because of its ability to handle informative censoring and not require a common treatment effect assumption.26 27
Sensitivity analyses to test the robustness of the IPCW methodology were conducted using RPSFT, IPE, and TSE methods. Details on these analyses can be found in the online supplemental methods.
Baseline and time-varying covariates for the IPCW, RPSFT, IPE, and TSE analyses were selected using clinical knowledge and hypotheses (online supplemental table S1). SAS (V.9.4) and R (V.4.2.3) software were used for all treatment-switching adjustment analyses.
Results
Patient disposition and treatment summary
As previously reported,4 14 21 719 patients were randomly assigned to receive nivolumab plus ipilimumab with chemotherapy (n=361) or chemotherapy alone (n=358); 358 (99%) patients and 349 (97%) patients received at least one dose of the study treatment, respectively (online supplemental figure S2). Baseline characteristics for the overall population have been previously reported and were generally well balanced between treatment arms.4 14 21 Of all randomized patients, 227 (32%) had squamous and 492 (68%) had non-squamous NSCLC. At the current database lock (February 13, 2023), the median follow-up was 54.5 months (range, 49.1–64.4), and the minimum follow-up for OS was 47.9.
Patients in the nivolumab plus ipilimumab with chemotherapy and chemotherapy-alone arms received study treatment for a median of 6.1 months (range, 0–24.4) and 2.5 months (range, 0–58.2), respectively (online supplemental table S2). Most patients in the nivolumab plus ipilimumab with chemotherapy arm (93%) received two cycles of chemotherapy, and 14% (n=50) completed the protocol-defined 2-year treatment period. Patients in the nivolumab plus ipilimumab with chemotherapy arm received a median of 9 (range, 1–36) nivolumab doses and 4 (range, 1–18) ipilimumab doses. In the chemotherapy-alone arm, 261 patients (75%) received at least four cycles of chemotherapy, and 159 patients (67%) with non-squamous NSCLC received pemetrexed maintenance (online supplemental table S2); 4 patients (1%) continued to receive pemetrexed maintenance therapy at the 4-year follow-up. Among all randomized patients, 135 (37%) in the nivolumab plus ipilimumab with chemotherapy arm and 174 (49%) in the chemotherapy-alone arm received subsequent systemic therapy (table 1). Subsequent immunotherapy was administered to 26 (7%) patients and 130 (36%) patients, respectively, while 71 (20%) and 22 (6%) received subsequent platinum-doublet chemotherapy (table 1).
Table 1.
Subsequent systemic therapy for all randomized patients
| Nivolumab plus ipilimumab with chemotherapy (n=361) | Chemotherapy (n=358) | |
| Received subsequent systemic therapy, n (%) | 135 (37) | 174 (49) |
| Any immunotherapy | 26 (7) | 130* (36) |
| Anti-PD-1 | 15 (4) | 107 (30) |
| Nivolumab | 11 (3) | 72 (20) |
| Pembrolizumab | 4 (1) | 36 (10) |
| Anti-PD-L1 | 8 (2) | 24 (7) |
| Anti-CTLA-4 | 2 (1) | 2 (1) |
| Other immunotherapy | 5 (1) | 6 (2) |
| Targeted therapy | 26 (7) | 30 (8) |
| Chemotherapy | 126 (35) | 99 (28) |
| Platinum-doublet chemotherapy | 71 (20) | 22 (6) |
Percentages based on all randomized patients. Patients may have received more than one type of subsequent therapy. Subsequent therapy was defined as therapy that started on or after the first dosing date (randomization date if the patient was never treated).
*Includes one patient who was randomized to the chemotherapy arm but did not receive treatment.
Efficacy
Overall survival
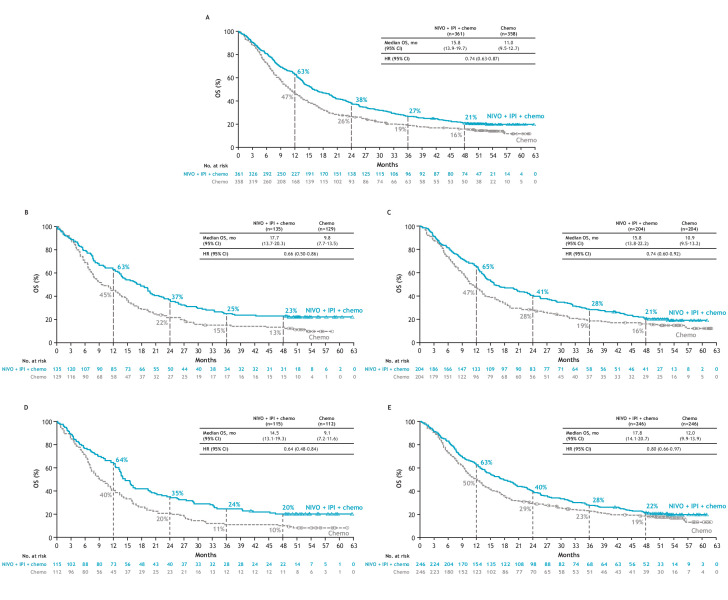
At a minimum follow-up of 47.9 months for OS, nivolumab plus ipilimumab with chemotherapy continued to provide sustained OS benefit versus chemotherapy alone. In the all-randomized population, median OS was 15.8 months (95% CI 13.9 to 19.7) in the nivolumab plus ipilimumab with chemotherapy arm versus 11.0 months (95% CI 9.5 to 12.7) in the chemotherapy-alone arm (HR 0.74, 95% CI 0.63 to 0.87); 4-year OS rates were 21% versus 16%, respectively (figure 1A).
Figure 1.
OS in (A) all randomized patients, (B) patients with tumor PD-L1 expression <1%, (C) patients with tumor PD-L1 expression ≥1%, (D) patients with squamous histology, and (E) patients with non-squamous histology. Minimum follow-up for OS was 47.9 months. 95% CIs for 4-year OS rates with nivolumab (NIVO) plus ipilimumab (IPI) with chemotherapy (Chemo) and chemotherapy alone, respectively, were: (A) 17–25 and 12–20; (B) 16–30 and 8–20; (C) 16–27 and 11–22; (D) 13–28 and 5–16; and (E) 17–27 and 14–24. OS, overall survival; PD-L1, programmed death ligand 1.
Consistent with previous reports, nivolumab plus ipilimumab with chemotherapy improved OS versus chemotherapy alone across most subgroups (online supplemental figure S3), including by tumor PD-L1 expression (<1%, ≥1% (figure 1B,C), 1%–49%, and ≥50% (online supplemental figure S4A,B)) and histology (figure 1D,E). In patients with tumor PD-L1 expression <1% or ≥1%, 4-year OS rates in the nivolumab plus ipilimumab with chemotherapy arm versus the chemotherapy-alone arm were 23% versus 13% and 21% versus 16%, respectively (figure 1B,C); in patients with squamous or non-squamous NSCLC, 4-year OS rates were 20% versus 10% and 22% versus 19%, respectively (figure 1D,E).
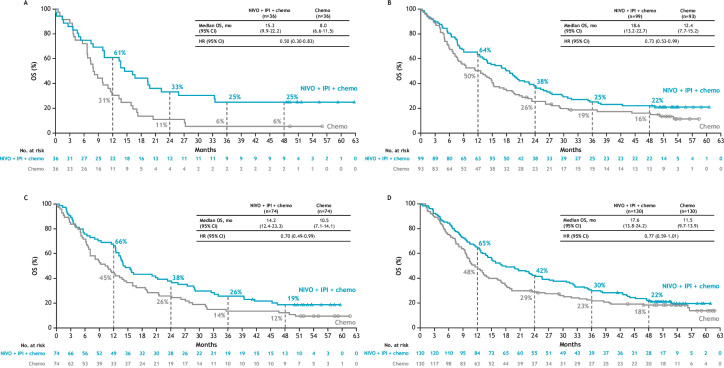
Similar to all randomized CheckMate 9LA patients and subgroups by tumor PD-L1 expression or histology, an OS benefit of nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone was also observed in smaller subgroups by both tumor PD-L1 expression and tumor histology combined. In the tumor PD-L1 expression <1% and squamous NSCLC subgroups (n=36 per arm), median OS was 15.3 months (95% CI 9.9 to 22.2) versus 8.0 months (95% CI 6.6 to 11.5) (HR 0.50, 95% CI 0.30 to 0.83), whereas in the tumor PD-L1 expression <1% and non-squamous NSCLC subgroups (n=99 and n=93, respectively), median OS was 18.6 months (95% CI 13.2 to 22.7) versus 12.4 months (95% CI 7.7 to 15.2) (HR 0.73, 95% CI 0.53 to 0.99) (figure 2A,B); respective 4-year OS rates were 25% versus 6% and 22% versus 16%. In the tumor PD-L1 expression ≥1% and squamous subgroups (n=74 per arm), the HR and 4-year OS rates of nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone were 0.70 (95% CI 0.49 to 0.99) and 19% versus 12%, whereas in the tumor PD-L1 expression ≥1% and non-squamous NSCLC subgroups (n=130 per arm), the HR and 4-year OS rates were 0.77 (95% CI 0.59 to 1.01) and 22% versus 18%, respectively (figure 2C,D).
Figure 2.
OS in patients with (A) tumor PD-L1 expression <1% and squamous histology, (B) tumor PD-L1 expression <1% and non-squamous histology, (C) tumor PD-L1 expression ≥1% and squamous histology, and (D) tumor PD-L1 expression ≥1% and non-squamous histology. Subgroups defined on the basis of baseline tumor PD-L1 expression level in the clinical database and histology per interactive response technology. The 95% CIs for 4-year rates for nivolumab (NIVO) plus ipilimumab (IPI) with chemotherapy (chemo) and chemo alone, respectively, were: (A) 12–40 and 1–16; (B) 15–31 and 10–25; (C) 11–28 and 6–21; (D) 15–30 and 12–26. OS, overall survival; PD-L1, programmed death ligand 1.
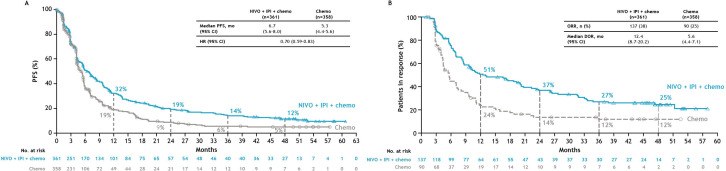
PFS and tumor response
Nivolumab plus ipilimumab with chemotherapy continued to improve PFS compared with chemotherapy alone in all randomized patients (HR 0.70; 95% CI 0.59 to 0.83) with 4-year PFS rates of 12% versus 5% (figure 3A) and across all tumor PD-L1 expression or histology subgroups (online supplemental table S3), as well as subgroups of both tumor PD-L1 expression and histology combined (online supplemental table S4).
Figure 3.
(A) PFS and (B) DOR in the all-randomized population. PFS and DOR were per blinded independent central review. Minimum follow-up for PFS was 47.1 months. The 95% CIs for 4-year rates for nivolumab (NIVO) plus ipilimumab (IPI) with chemotherapy (Chemo) and chemotherapy alone, respectively, were: (A) 8–15 and 3–8; (B) 17–33 and 6–20. DOR, duration of response; ORR, objective response rate; OS, overall survival. PFS, progression-free survival.
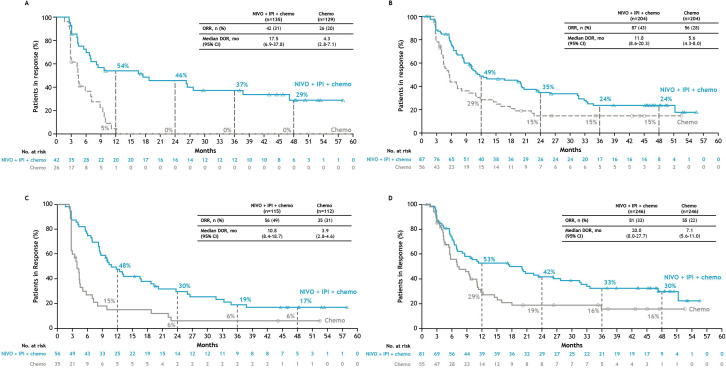
The ORR among all randomized patients was 38% in the nivolumab plus ipilimumab with chemotherapy arm versus 25% in the chemotherapy-alone arm; the complete response rate was 4% versus 1%, respectively (online supplemental table S5). Median DOR in the nivolumab plus ipilimumab with chemotherapy arm was 12.4 months (95% CI 8.7 to 20.2) versus 5.6 months (95% CI 4.4 to 7.1) in the chemotherapy-alone arm, and responses were ongoing at 4 years in 25% versus 12% of patients, respectively (figure 3B). Similar prolonged DOR rates were observed with nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone in subgroups by tumor PD-L1 expression (figure 4A,B) and by histology (figure 4C,D). Median DOR for the tumor PD-L1 expression <1% subgroup was 17.5 months (95% CI 6.9 to 37.8) versus 4.3 months (95% CI 2.8 to 7.1) and 11.8 months (95% CI 8.6 to 20.3) versus 5.6 months (95% CI 4.3 to 8.0) in the tumor PD-L1 expression ≥1% subgroup, respectively (figure 4A,B), with ongoing responses at 4 years in 29% versus 0% (PD-L1 <1 %) and 24% versus 15% (PD-L1 ≥1%), respectively (figure 4A,B). Median DOR in patients with squamous histology was 10.8 months (95% CI 8.4 to 18.7) versus 3.9 months (95% CI 2.8 to 4.6) and 20.0 months (95% CI 8.0 to 27.7) versus 7.1 months (95% CI 5.6 to 11.0) in the non-squamous subgroup (figure 4C,D), respectively, with ongoing responses at 4 years in 17% versus 6% (squamous histology) and 30% versus 16% (non-squamous histology), respectively (figure 4C,D). It is notable that a numerically greater magnitude of DOR benefit was seen in patients with tumor PD-L1 expression <1% (figure 4A) compared with tumor PD-L1 ≥1% (figure 4B) or with squamous histology (figure 4C) compared with non-squamous histology (figure 4D) at the 4-year follow-up. DOR results in patients with other tumor PD-L1 expression (1%–49% and ≥50%) subgroups are shown in online supplemental table S6.
Figure 4.
DOR for patients with (A) tumor PD-L1 expression <1%, (B) tumor PD-L1 expression ≥1%, (C) squamous histology, and (D) non-squamous histology. The 95% CIs for 4-year rates for nivolumab (NIVO) plus ipilimumab (IPI) with chemotherapy (chemo) and chemotherapy alone are: (A) 15–45 and not applicable (NA); (B) 15–34 and 7–26; (C) 8–29 and 1–17; and (D) 19–41 and 7–28. DOR, duration of response; ORR, objective response rate; PD-L1, programmed death ligand 1.
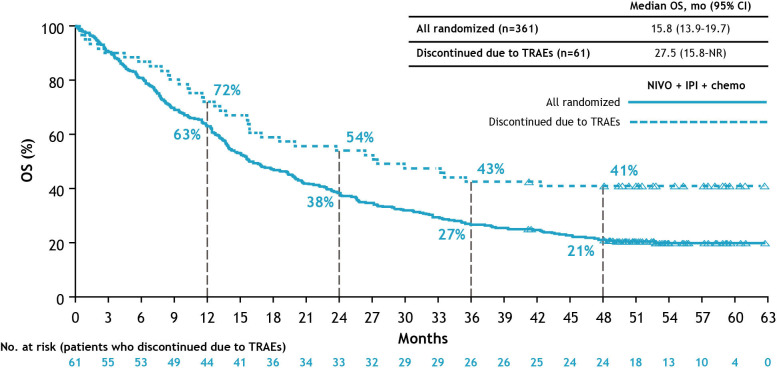
Efficacy in patients who discontinued nivolumab plus ipilimumab with chemotherapy due to TRAEs
As described previously, an exploratory analysis was performed in patients who discontinued all components of nivolumab plus ipilimumab with chemotherapy because of TRAEs; baseline characteristics of this subgroup were generally similar to those of the all-randomized population.21 TRAEs led to discontinuation of all study drugs in 61 (17%) patients treated with nivolumab plus ipilimumab with chemotherapy; these patients received treatment for a median of 4.4 months (95% CI 2.9 to 6.9). The most common toxicities (≥3% of patients) reported in patients who discontinued all study drugs were gastrointestinal disorders (n=14; 4%) and hepatobiliary disorders (n=11; 3%). Consistent with results from the 2- year update,21 at the 4-year analysis, median OS was 27.5 months (95% CI 15.8 to not reached (NR)), and the 4-year OS rate was 41% (95% CI 29 to 53) (figure 5). Median PFS was 5.1 months (95% CI 2.6 to 14.5), with a 4-year PFS rate of 17%; median DOR was 14.5 months (95% CI 2.9 to 35.3), with 23% of patients having an ongoing response at 4 years (online supplemental table S7).
Figure 5.
OS in patients who discontinued nivolumab plus ipilimumab with chemotherapy due to TRAEs. Minimum follow-up for OS was 47.9 months. An exploratory analysis was conducted in patients with TRAEs (reported between first dose and 30 days after the last dose of study treatment) leading to the discontinuation of all components of study treatment. The 95% CIs for the 4-year OS rates for patients who discontinued due to TRAEs and for the all-randomized population, respectively, were 29–53 and 17–25. IPI, ipilimumab; NIVO, nivolumab; NR, not reached; OS, overall survival; TRAEs, treatment-related adverse events.
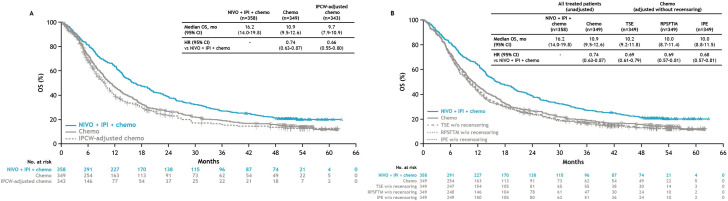
Treatment-switching adjustment analysis
Patients in the chemotherapy-alone arm who switch to subsequent immunotherapy can introduce bias in the calculation of treatment effect, making treatment outcomes in the chemotherapy-alone arm appear more favorable than they would be in the absence of subsequent immunotherapy treatment. Thus, a treatment-switching adjustment analysis was conducted. The baseline demographics and disease characteristics of patients who switched treatment from chemotherapy alone to immunotherapy are shown in online supplemental table S8 and were generally similar to those of the all-treated population (data not shown).
All-treated and IPCW-adjusted analysis
After adjustment for treatment switching using the IPCW model, the estimated median OS for all treated patients in the chemotherapy-alone arm was revised from 10.9 months (95% CI 9.5 to 12.6) to 9.7 months (95% CI 7.9 to 10.9) (figure 6A). The adjusted HR for nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone was 0.66 (95% CI 0.55 to 0.80), compared with an unadjusted HR of 0.74 (95% CI 0.63 to 0.87) from the all-treated population.
Figure 6.
OS in patients in the all-treated population after adjustments using (A) IPCW (primary analysis) and (B) TSE, RPSFT, and IPE (sensitivity analyses) methodologies. Chemo, chemotherapy; IPCW, inverse probability of censoring weighting; IPE, iterative parameter estimation; IPI, ipilimumab; NIVO, nivolumab; OS, overall survival; RPSFT, rank-preserving structural failure time; TSE, two-stage estimation; w/o, without.
Sensitivity analyses
Results from sensitivity analyses using other treatment-switching adjustment methods were generally consistent with the IPCW analysis. Median OS for all treated patients in the chemotherapy-alone arm after adjustment without recensoring using the TSE, RPSFT, and IPE models was 10.2 months (95% CI 9.2 to 11.8), 10.0 months (95% CI 8.7 to 11.4), and 10.0 months (95% CI 8.8 to 11.5), respectively (figure 6B). The respective adjusted HR values were 0.69 (95% CI 0.61 to 0.79), 0.69 (95% CI 0.57 to 0.81), and 0.68 (95% CI 0.57 to 0.81). Adjustment analyses were also performed using the RPSFT and IPE models with recensoring, and similar results were obtained (data not shown).
Safety
With a minimum follow-up of 49.1 months, safety in all treated patients was consistent with prior reports,4 14 21 and no new safety signals were identified (online supplemental table S9). Per protocol, patients discontinued nivolumab plus ipilimumab with chemotherapy after a maximum of 2 years of treatment; thus, no new safety signals were identified in this 4-year analysis. The summary of TRAEs in all treated patients is provided in online supplemental table S9, and the incidence of IMAEs in the nivolumab plus ipilimumab with chemotherapy arm is summarized in online supplemental table S10.
Discussion
In CheckMate 9LA, with a minimum of 4 years of follow-up, patients with metastatic NSCLC continued to derive long-term, durable OS benefit from first-line nivolumab plus ipilimumab with two cycles of chemotherapy versus four cycles of chemotherapy alone (HR 0.74), regardless of tumor PD-L1 expression level or histology. PFS and DOR continued to favor nivolumab plus ipilimumab with chemotherapy compared with chemotherapy alone; durable responses were seen in all randomized patients and across all subgroups, including patients with limited efficacious treatment options (tumor PD-L1 expression <1% or squamous histology). The clinical benefit of nivolumab plus ipilimumab with chemotherapy was further supported by exploratory analyses of efficacy in patients who discontinued treatment due to TRAEs and in patients who switched from chemotherapy to subsequent immunotherapy treatment, which revealed a greater estimated relative OS benefit for nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone (OS HR 0.66) than in the unadjusted population of all-treated patients (OS HR 0.74). No new safety signals were identified at the 4-year follow-up.
In this clinical update from CheckMate 9LA, although patients have been off of immunotherapy treatment for at least 2 years per protocol, the long-term survival benefit of nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone was clearly evident with the continued separation of the Kaplan-Meier OS curves; 21% of patients in the nivolumab plus ipilimumab with chemotherapy arm were still alive at 4 years versus 16% of patients in the chemotherapy-alone arm. Sustained PFS benefit and durable responses were also demonstrated at 4 years; the difference in the proportion of responders with an ongoing response between treatment arms appeared to be nearly twofold in all randomized patients and threefold or more in certain subgroups, such as tumor PD-L1 expression <1% and squamous histology.
Recently, several phase 3 clinical trials of first-line immunotherapy in patients with metastatic NSCLC have reported milestone 5-year clinical outcomes, including trials with immunotherapy alone,9 28 in combination with chemotherapy,10 11 or dual-immunotherapy combination regimens.8 Although patients with NSCLC with high tumor PD-L1 expression (≥50%) consistently have improved long-term survival benefit from all immunotherapy regimens,8–11 clinical outcomes with immunotherapy plus chemotherapy in certain patient populations, such as those with tumor PD-L1 expression <1% and/or squamous histology, remain suboptimal.10–12 29–31 No incremental benefit was evident with pembrolizumab plus chemotherapy versus chemotherapy alone at 5 years in patients with tumor PD-L1 expression <1% and squamous histology (OS rates, 11% versus 13%).11 Furthermore, the survival curves appeared to be converging between the treatment arms for patients with tumor PD-L1 expression <1% and non-squamous histology with extended follow-up.10 In contrast, data from the CheckMate 9LA 4-year update showed sustained long-term OS benefit with nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone in patients with either tumor PD-L1 expression <1% or ≥1%; in addition, the magnitude of survival benefit was apparently greater in patients with tumor PD-L1 expression <1% (HR 0.66) or squamous histology (HR 0.64) than in those with tumor PD-L1 expression ≥1% (HR 0.74) or non-squamous histology (HR 0.80). In addition to the survival benefit, the durability of response with nivolumab plus ipilimumab with chemotherapy was more notable in CheckMate 9LA in both tumor PD-L1 expression and histology subgroups than in the pembrolizumab plus chemotherapy profile in these subgroups,10 11 although caution is needed when performing cross-trial comparisons. Similar to the results from the 4-year analysis of CheckMate 9LA, long-term durable clinical benefit has been reported with nivolumab plus ipilimumab in CheckMate 227,32 underscoring the potential contribution of ipilimumab to a sustained response through enhanced memory T cell induction.33–35 Furthermore, a recent systematic review of first-line therapies for advanced NSCLC also demonstrated the long-term benefit of nivolumab plus ipilimumab compared with immunotherapy-based combinations.13 36 As long-term data with first-line immunotherapy-based regimens continue to mature, the 4-year update from CheckMate 9LA supports first-line nivolumab plus ipilimumab-based regimens as efficacious treatment options for patients with metastatic NSCLC, including those with tumor PD-L1 expression <1% or squamous histology who have high unmet needs.
No new safety signals were observed with nivolumab plus ipilimumab with chemotherapy in our updated analysis. Discontinuation of nivolumab plus ipilimumab with chemotherapy due to TRAEs did not negatively impact the long-term clinical or efficacy benefit, with a 4-year OS rate of 41%. These results are consistent with previous reports in patients who discontinued dual nivolumab plus ipilimumab due to TRAEs, including data from CheckMate 227 and from patients with advanced sarcomatoid renal cell carcinoma in CheckMate 214.8 37 Similar findings have been reported recently from a real-world data analysis in melanoma38 and NSCLC,39 40 which showed that patients may experience a durable response even after discontinuing immunotherapy for any reason or due to adverse events.
With the availability of second-line immunotherapy options for patients with NSCLC, treatment switching to subsequent immunotherapy in the chemotherapy arm can potentially impact the calculation of the OS benefit observed in the study by making the survival benefit from chemotherapy appear larger than it would be if second-line immunotherapy were unavailable. At the time of this analysis, 36% of patients in the chemotherapy arm of CheckMate 9LA had switched to subsequent immunotherapy. A treatment-switching adjustment analysis substituting these patients with “like” patients who did not receive subsequent immunotherapy lowered the calculated median OS in the chemotherapy arm from 10.9 to 9.7 months, improving the estimated relative OS benefit from nivolumab plus ipilimumab with chemotherapy (adjusted HR 0.66). Recent reports of treatment-switching adjustment analyses conducted for clinical trials of immunotherapy regimens versus chemotherapy, such as KEYNOTE-024 and CheckMate 227, have found similar improvements in relative survival outcomes compared with chemotherapy.19 20 Of note, although only 7% of the patients in the nivolumab plus ipilimumab with chemotherapy arm received subsequent immunotherapy, any potential impact of this on the OS benefit is undetermined. This adjustment for treatment switching supports the evidence for the efficacy of nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone and can also inform other analyses, such as indirect treatment comparisons, meta-analyses, and assessments of cost-effectiveness.
In conclusion, this 4-year update from CheckMate 9LA showed that patients with metastatic or recurrent NSCLC continued to derive long-term, durable efficacy benefit from first-line nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone regardless of tumor PD-L1 expression or histology. These findings, taken together with exploratory analyses in patients who discontinued nivolumab plus ipilimumab with chemotherapy due to TRAEs and treatment-switching adjustment analysis, further support the use of nivolumab plus ipilimumab with chemotherapy as an efficacious first-line treatment option for metastatic NSCLC, particularly for patients with tumor PD-L1 expression <1% or squamous histology, populations with high unmet needs.
Acknowledgments
This work was supported by Bristol Myers Squibb. We thank the patients and families who made this trial possible, the investigators and clinical study teams who participated in the trial, and Dako, an Agilent Technologies company, for collaborative development of the PD‑L1 IHC 28-8 pharmDx assay. Medical writing and editorial support for the development of this manuscript, under the direction of the authors, was provided by Christine Billecke, PhD, Sabrina Hom, PhD, and Celia Nelson of Ashfield MedComms, an Inizio Company, funded by Bristol Myers Squibb.
Footnotes
Contributors: All authors listed have actively participated in the production of this manuscript through trial conception/design, data acquisition, analysis, and/or interpretation. All authors contributed to the drafting of the manuscript and approved the final version. DPC is responsible for the overall content as guarantor.
Funding: This work was supported by Bristol Myers Squibb.
Competing interests: DPC has received consulting fees from Arcus Biosciences, Bristol Myers Squibb, BMS KK, Boehringer Ingelheim, Curio Science, Daiichi Sankyo, Genentech/Roche, GI Therapeutics (Intellisphere), GSK, Janssen, Merck, Mirati, Novartis, Novocure, OncoCyte, OncoHost, Roche China, and Seattle Genetics; and has participated on the advisory board of Amgen, Arcus Biosciences, AstraZeneca, Merck, Flame Biosciences, Gritstone Oncology, Cantargia (PPD), Daiichi Sankyo, EMD Serono GSK, Lilly, Regeneron, Sanofi, and Seattle Genetics and the data safety monitoring board of EORTC, AbbVie, and Lilly. T-EC has received honoraria from Astellas Pharma, Janssen, MSD, Merck Serono, Amgen, Roche, Pfizer, Sanofi Genzyme, Servier, Ipsen, AstraZeneca, Lilly, Novartis, Boehringer Ingelheim, and Bristol Myers Squibb; and has participated on a data safety monitoring board or advisory board of Astellas Pharma, Janssen, MSD, Merck Serono, Amgen, Roche, Pfizer, Sanofi Genzyme, Servier, Ipsen, AstraZeneca, Lilly, Novartis, Boehringer Ingelheim, and Bristol Myers Squibb. MS has received funding from Bristol Myers Squibb, MSD, Merck Serono, Pfizer, GSK, Roche, Bayer, Astellas, Amgen, Gilead, Tesaro, Clovis, Eli Lilly, Novartis, Regeneron, AbbVie, AstraZeneca, PharmaMar, Mylan, Samsung Pharmaceuticals, Bioven, BeiGene, and Daiichi Sankyo. OJ-V has received grants from AstraZeneca Spain, honoraria from Bristol Myers Squibb, Roche/Genentech, MSD Oncology, AstraZeneca/MedImmune, and Takeda; has served as a consultant for Bristol Myers Squibb, Lilly, Takeda, AstraZeneca Spain, and Janssen Oncology, and has received travel support from Takeda, AstraZeneca/MedImmune. NR has received honoraria from AstraZeneca, Bristol Myers Squibb, Boehringer Ingelheim, Daiichi Sankyo, GSK, Hoffmann-La Roche, Janssen, Lilly, MSD, Merck, Pfizer, Symphogen, and Takeda; travel support from AstraZeneca, Bristol Myers Squibb, Boehringer Ingelheim, Janssen, Hoffmann-La Roche, and Takeda; and has participated on a data safety monitoring board or advisory board for Merck and Symphogen. BZ has received honoraria from Amgen, AstraZeneca, Bristol Myers Squibb, GSK, Janssen-Cilag, MSD and Roche. AA has received consulting fees from Boehringer Ingelheim and Roche, provided expert testimony for Bristol Myers Squibb, Novartis, and Sandoz, and received travel support from AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Pfizer, Roche, and Sanofi. LP-A has received grants or contracts from MSD, AstraZeneca, Pfizer, and Bristol Myers Squibb; consulting fees from Lilly, MSD, Roche, PharmaMar, Merck KGaA (Darmstadt, Germany), AstraZeneca, Novartis, Servier, Amgen, Pfizer, Sanofi, Bayer, Bristol Myers Squibb, Mirati, GSK, Janssen, Takeda, and Daichii Sankyo; honoraria from AstraZeneca, Janssen, Merck, and Mirati; and has participated on a data safety monitoring board or advisory board for Altum Sequencing and Genomica. SL has received consulting fees from AstraZeneca, Boehringer Ingelheim, Hutchinson MediPharma, Simcere, ZaiLab, GenomiCare, Roche, and Hanosh, and honoraria from AstraZeneca, Roche, and Hanosh. TJ has received consulting fees from Roche, Merck, MSD, Puma, AstraZeneca, Bristol Myers Squibb, Amgen, Gilead, and Specialised Therapeutics; and honoraria from AstraZeneca. XZ holds stock in Bristol Myers Squibb. IS has received consulting fees from Bristol Myers Squibb. JRP holds stock in Bristol Myers Squibb. AL holds stock in Bristol Myers Squibb. MR has received consulting fees from Amgen, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, BeiGene, Lilly, Mirati, MSD, Merck, Novartis, Pfizer, Sanofi, Regeneron, Roche, Takeda, and Samsung Bioepis; honoraria from Amgen, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, BeiGene, Lilly, Mirati, MSD, Merck, Novartis, Pfizer, Sanofi, Regeneron, Roche, Takeda, and Samsung Bioepis; travel support from Amgen, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, BeiGene, Lilly, Mirati, MSD, Merck, Novartis, Pfizer, Sanofi, Regeneron, Roche, Takeda, and Samsung Bioepis; and has participated on a data safety monitoring board or advisory board for Amgen, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, BeiGene, Lilly, Mirati, MSD, Merck, Novartis, Pfizer, Sanofi, Regeneron, Roche, Takeda, and Samsung Bioepis. All other authors declare no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/clinical-trials-and-research/disclosure-commitment.html.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was conducted according to the Declaration of Helsinki and International Standards of Good Clinical Practice. The independent ethics committee or institutional review board of each participating study center approved the protocol and all amendments. All patients provided written informed consent.
References
- 1.Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) for Non-Small Cell Lung Cancer V5.2023. National Comprehensive Cancer Network, Inc . All rights reserved. Accessed November 16, 2023. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. 2023.
- 2.Singh N, Jaiyesimi IA, Ismaila N, et al. Therapy for stage IV non-small-cell lung cancer without driver alterations: ASCO living guideline, version 2023.1. J Clin Oncol 2023;41:e51–62. 10.1200/JCO.23.00282 [DOI] [PubMed] [Google Scholar]
- 3.Hendriks LE, Kerr KM, Menis J, et al. Non-oncogene-addicted metastatic non-small-cell lung cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol 2023;34:358–76. 10.1016/j.annonc.2022.12.013 [DOI] [PubMed] [Google Scholar]
- 4.Paz-Ares LG, Ciuleanu T-E, Cobo M, et al. First-line nivolumab plus ipilimumab with chemotherapy versus chemotherapy alone for metastatic NSCLC in CheckMate 9LA: 3-year clinical update and outcomes in patients with brain metastases or select somatic mutations. J Thorac Oncology 2023;18:204–22. 10.1016/j.jtho.2022.10.014 [DOI] [Google Scholar]
- 5.Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Long-term outcomes with nivolumab plus ipilimumab or nivolumab alone versus ipilimumab in patients with advanced melanoma. J Clin Oncol 2022;40:127–37. 10.1200/JCO.21.02229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Motzer RJ, McDermott DF, Escudier B, et al. Conditional survival and long-term efficacy with nivolumab plus ipilimumab versus sunitinib in patients with advanced renal cell carcinoma. Cancer 2022;128:2085–97. 10.1002/cncr.34180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zalcman G, Oulkhouir Y, Cornelissen R, et al. First-line nivolumab (NIVO) plus ipilimumab (IPI) versus chemotherapy (chemo) in patients (pts) with unresectable malignant pleural mesothelioma (uMPM): 4-year update from CheckMate 743. Ann Oncol 2022;33:S1438–9. 10.1016/j.annonc.2022.08.077 [DOI] [PubMed] [Google Scholar]
- 8.Brahmer JR, Lee J-S, Ciuleanu T-E, et al. Five-year survival outcomes with nivolumab plus ipilimumab versus chemotherapy as first-line treatment for metastatic non-small-cell lung cancer in CheckMate 227. J Clin Oncol 2023;41:1200–12. 10.1200/JCO.22.01503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reck M, Rodríguez-Abreu D, Robinson AG, et al. Five-year outcomes with pembrolizumab versus chemotherapy for metastatic non-small-cell lung cancer with PD-L1 tumor proportion score ≥ 50. J Clin Oncol 2021;39:2339–49. 10.1200/JCO.21.00174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garassino MC, Gadgeel S, Speranza G, et al. Pembrolizumab plus pemetrexed and platinum in nonsquamous non-small-cell lung cancer: 5-year outcomes from the phase 3 KEYNOTE-189 study. J Clin Oncol 2023;41:1992–8. 10.1200/JCO.22.01989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Novello S, Kowalski DM, Luft A, et al. Pembrolizumab plus chemotherapy in squamous non-small-cell lung cancer: 5-year update of the phase III KEYNOTE-407 study. J Clin Oncol 2023;41:1999–2006. 10.1200/JCO.22.01990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gadgeel S, Rodríguez-Abreu D, Halmos B, et al. 5-year survival of pembrolizumab plus chemotherapy for metastatic NSCLC with PD-L1 tumor proportion score <1%. J Thoracic Oncol 2023;18:S77–8. 10.1016/j.jtho.2023.09.078 [DOI] [PubMed] [Google Scholar]
- 13.O’Byrne K, Popoff E, Badin F, et al. Efficacy of nivolumab + ipilimumab versus other first-line treatments for metastatic NSCLC with PD-L1 <1%: a network meta-analysis. presentation at the IASLC world conference on lung cancer; September 9–12, 2023; Singapore. Available: https://cattendee.abstractsonline.com/meeting/10925/Session/183 [Accessed 22 Sep 2023].
- 14.Paz-Ares L, Ciuleanu T-E, Cobo M, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncol 2021;22:198–211. 10.1016/S1470-2045(20)30641-0 [DOI] [PubMed] [Google Scholar]
- 15.OPDIVO® (nivolumab) [package insert]. Princeton, NJ: Bristol Myers Squibb. 2023.
- 16.Union register of medicinal products for human use. European Commission, Available: https://ec.europa.eu/health/documents/community-register/html/h1014.htm [Accessed 28 Jun 2023].
- 17.Jönsson L, Sandin R, Ekman M, et al. Analyzing overall survival in randomized controlled trials with crossover and implications for economic evaluation. Value Health 2014;17:707–13. 10.1016/j.jval.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 18.Latimer NR, Abrams KR, Lambert PC, et al. Adjusting for treatment switching in randomised controlled trials—A simulation study and a simplified two-stage method. Stat Methods Med Res 2017;26:724–51. 10.1177/0962280214557578 [DOI] [PubMed] [Google Scholar]
- 19.Reck M, Rodríguez-Abreu D, Robinson AG, et al. Updated analysis of KEYNOTE-024: pembrolizumab versus platinum-based chemotherapy for advanced non-small-cell lung cancer with PD-L1 tumor proportion score of 50% or greater. J Clin Oncol 2019;37:537–46. 10.1200/JCO.18.00149 [DOI] [PubMed] [Google Scholar]
- 20.Reck M, De T, Paz-Ares L, et al. 1026P—Treatment switching adjustment of overall survival in the CheckMate 227 clinical trial of nivolumab plus ipilimumab versus chemotherapy in first-line treatment of patients with advanced non-small cell lung cancer. Ann Oncol 2022;33:S448–554. 10.1016/annonc/annonc1064 [DOI] [Google Scholar]
- 21.Reck M, Ciuleanu T-E, Cobo M, et al. First-line nivolumab plus ipilimumab with two cycles of chemotherapy versus chemotherapy alone (four cycles) in advanced non-small-cell lung cancer: CheckMate 9LA 2-year update. ESMO Open 2021;6:100273. 10.1016/j.esmoop.2021.100273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Latimer NR, Abrams KR. NICE DSU Technical Support Document 16: Adjusting Survival Time Estimates in the Presence of Treatment Switching. London: National Institute for Health and Care Excellence (NICE), July 2014. [PubMed] [Google Scholar]
- 23.Robins JM, Finkelstein DM. Correcting for noncompliance and dependent censoring in an AIDS clinical trial with inverse probability of censoring weighted (IPCW) log-rank tests. Biometrics 2000;56:779–88. 10.1111/j.0006-341x.2000.00779.x [DOI] [PubMed] [Google Scholar]
- 24.Robins JM, Tsiatis AA. Correcting for non-compliance in randomized trials using rank preserving structural failure time models. Comm Stat Theory Methods 1991;20:2609–31. 10.1080/03610929108830654 [DOI] [Google Scholar]
- 25.Branson M, Whitehead J. Estimating a treatment effect in survival studies in which patients switch treatment. Stat Med 2002;21:2449–63. Available: 10.1002/sim.1219 [DOI] [PubMed] [Google Scholar]
- 26.Robins JM. Marginal structural models versus structural nested models as tools for causal inference. In: Halloran M, Berry D, eds. Statistical Models in Epidemiology: The Environment and Clinical Trials. New York: Springer;1999:95–134, 10.1007/978-1-4612-1284-3 [DOI] [Google Scholar]
- 27.Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the joint causal effect of nonrandomized treatments. J Am Statist Associat 2001;96:440–8. 10.1198/016214501753168154 [DOI] [Google Scholar]
- 28.de Castro G, Kudaba I, Wu Y-L, et al. Five-year outcomes with pembrolizumab versus chemotherapy as first-line therapy in patients with non-small-cell lung cancer and programmed death ligand-1 tumor proportion score ≥ 1% in the KEYNOTE-042 study. J Clin Oncol 2023;41:1986–91. 10.1200/JCO.21.02885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Socinski MA, Obasaju C, Gandara D, et al. Current and emergent therapy options for advanced squamous cell lung cancer. J Thorac Oncol 2018;13:165–83. 10.1016/j.jtho.2017.11.111 [DOI] [PubMed] [Google Scholar]
- 30.Paik PK, Pillai RN, Lathan CS, et al. New treatment options in advanced squamous cell lung cancer. Am Soc Clin Oncol Educ Book 2019;39:e198–206. 10.1200/EDBK_237829 [DOI] [PubMed] [Google Scholar]
- 31.Xu Y, Wan B, Chen X, et al. The association of PD-L1 expression with the efficacy of anti-PD-1/PD-L1 immunotherapy and survival of non-small cell lung cancer patients: a meta-analysis of randomized controlled trials. Transl Lung Cancer Res 2019;8:413–28. 10.21037/tlcr.2019.08.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramalingam S, Ciuleanu TE, Caro RB, et al. Oral presentation at the IASLC world conference on lung cancer; September 9–12, 2023; Singapore. Abstract OA14.03.
- 33.Das R, Verma R, Sznol M, et al. Combination therapy with anti-CTLA-4 and anti-PD-1 leads to distinct immunologic changes in vivo. J Immunol 2015;194:950–9. 10.4049/jimmunol.1401686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wei SC, Duffy CR, Allison JP. Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov 2018;8:1069–86. 10.1158/2159-8290.CD-18-0367 [DOI] [PubMed] [Google Scholar]
- 35.Sharma P, Allison JP. Dissecting the mechanisms of immune checkpoint therapy. Nat Rev Immunol 2020;20:75–6. 10.1038/s41577-020-0275-8 [DOI] [PubMed] [Google Scholar]
- 36.O’Byrne K, Popoff E, Badin F, et al. Long-term comparative efficacy and safety of nivolumab plus ipilimumab relative to other first-line therapies for advanced non-small-cell lung cancer: a systematic literature review and network meta-analysis. Lung Cancer 2023;177:11–20. 10.1016/j.lungcan.2023.01.006 [DOI] [PubMed] [Google Scholar]
- 37.Rini BI, Signoretti S, Choueiri TK, et al. Long-term outcomes with nivolumab plus ipilimumab versus sunitinib in first-line treatment of patients with advanced sarcomatoid renal cell carcinoma. J Immunother Cancer 2022;10:e005445. 10.1136/jitc-2022-005445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fink M, Vittrup AS, Bastholt L, et al. Comparison of efficacy in patients with metastatic melanoma treated with ipilimumab and nivolumab who did or did not discontinue treatment due to immune-related adverse events: a real-world data study. Cancers (Basel) 2021;13:5550. 10.3390/cancers13215550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Faoro L, Brusegan A, Russi A, et al. Analysis of the relation between adverse events and overall survival in patients treated with Pembrolizumab as a first-line treatment for metastatic NSCLC. BMC Pharmacol Toxicol 2023;24:32. 10.1186/s40360-023-00663-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim H, Kim D-W, Kim M, et al. Long-term outcomes in patients with advanced and/or metastatic non-small cell lung cancer who completed 2 years of immune Checkpoint inhibitors or achieved a durable response after discontinuation without disease progression: multicenter, real-world data (KCSG Lu20-11). Cancer 2022;128:778–87. 10.1002/cncr.33984 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2023-008189supp002.pdf (1.2MB, pdf)
jitc-2023-008189supp001.pdf (1.5MB, pdf)
Data Availability Statement
Data are available on reasonable request. The Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/clinical-trials-and-research/disclosure-commitment.html.