Abstract
Purpose
The PRESTIGIO Registry was established in 2017 to collect clinical, virological and immunological monitoring data from people living with HIV (PLWH) with documented four-class drug resistance (4DR). Key research purposes include the evaluation of residual susceptibility to specific antiretrovirals and the validation of treatment and monitoring strategies in this population.
Participants
The PRESTIGIO Registry collects annual plasma and peripheral blood mononuclear cell samples and demographic, clinical, virological, treatment and laboratory data from PLWH followed at 39 Italian clinical centres and characterised by intermediate-to-high genotypic resistance to ≥1 nucleoside reverse transcriptase inhibitors, ≥1 non-nucleoside reverse transcriptase inhibitors, ≥1 protease inhibitors, plus either intermediate-to-high genotypic resistance to ≥1 integrase strand transfer inhibitors (INSTIs) or history of virological failure to an INSTI-containing regimen. To date, 229 people have been recorded in the cohort. Most of the data are collected from the date of the first evidence of 4DR (baseline), with some prebaseline information obtained retrospectively. Samples are collected from the date of enrollment in the registry.
Findings to date
The open-ended cohort has been used to assess (1) prognosis in terms of survival or development of AIDS-related or non-AIDS-related clinical events; (2) long-term efficacy and safety of different antiretroviral regimens and (3) virological and immunological factors predictive of clinical outcome and treatment efficacy, especially through analysis of plasma and cell samples.
Future plans
The registry can provide new knowledge on how to implement an integrated approach to study PLWH with documented resistance to the four main antiretroviral classes, a population with a limited number of individuals characterised by a high degree of frailty and complexity in therapeutic management. Given the scheduled annual updates of PLWH data, the researchers who collaborate in the registry can send study proposals at any time to the steering committee of the registry, which evaluates every 3 months whether the research studies can be conducted on data and biosamples from the registry and whether they are aimed at a better understanding of a specific health condition, the emergence of comorbidities or the effect of potential treatments or experimental drugs that may have an impact on disease progression and quality of life. Finally, the research studies should aim to be inclusive, innovative and in touch with the communities and society as a whole.
Trial registration number
Keywords: HIV & AIDS, Public health, REGISTRIES, Sexually Transmitted Disease, VIROLOGY
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The registry specifically includes people living with HIV and documented four-class drug resistance.
The cohort is readily available for research projects; the data sources (clinical centres) have already been linked, and data have been collected in order to enable easier and simpler querying across source systems.
Annual collection of cryopreserved plasma and peripheral blood mononuclear cell samples for research purposes.
Limited representativeness of subtype non-B viral strains and non-Italian natives with HIV.
Incomplete information before evidence of four-class drug resistance.
Introduction
Continuous progress in antiretroviral therapy (ART) has resulted in a high rate of virological suppression and a consequent improvement in life expectancy for individuals with HIV.1–5 Nevertheless, heavily treatment-experienced (HTE) people living with HIV (PLWH) have a history of previous virological failures on different antiretroviral regimens and limited treatment options because of multidrug resistance and/or drug intolerance.6 7 ART options can also be limited by drug–drug interactions or drug toxicity due to the need for both prophylaxis or treatment for opportunistic infections and concomitant therapies for multiple comorbidities that are common in HTE PLWH,8 9 especially with ageing.10 This fragile group often needs complex, unusual and asymmetrical regimens (a mixture of one time per day and two times per day schedules or oral, subcutaneous and intravenous administrations) with a high pill burden, possibly leading to suboptimal adherence, which in turn increases the risk of virological failure with emergent resistance and worsens the prognosis.11 12
Even though there is no consensus in defining HTE individuals, these PLWH generally have two or fewer antiretroviral classes available for use, with limited fully active antiretroviral drugs within each class,13 and represent a group at increased risk of low adherence and clinical progression. Therefore, establishing cohorts aimed at characterising this population better appears essential.
Among these difficult-to-treat individuals, those who harbour a virus with four-class drug resistance (4DR) (characterised by resistance to nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (PIs) and integrase strand transfer inhibitors (INSTIs)) represent a particular group with a very high burden of disease and very limited therapeutic options.14 In terms of epidemiology, the prevalence of HIV 4DR on a global scale is unknown; a prospective study in North Carolina estimated this prevalence at approximately 1% of PLWH, with a slight increase since 2007.15 Recent Italian studies quantified subjects with HIV 4DR at about 2% of treatment-experienced PLWH in 2011–2018.16 According to the most recent WHO report on HIV drug resistance (2014–2020), virological suppression (defined as HIV RNA <1000 copies/mL) was ≥90% among adults on ART for ≥48 months in only 6/14 middle-income and low-income countries with available data; in virologically non-suppressed PLWH on a NNRTI-based regimen for ≥48 months, high-level resistance to efavirenz or nevirapine was estimated to range from 50% to 95%, resistance to tenofovir from 5% to 56%.17 However, among individuals failing a dolutegravir-based regimen, NRTI resistance was reported in 2%–91% (data available from four countries only) and INSTI resistance in 0 cases (data available from Zambia only).17 Cases of three-class drug resistance (NRTIs, NNRTIs and PIs) have been described in Sub-Saharan Africa, with a high prevalence (>20%) in the setting of virological failure to a second-line PI-containing regimen.18–20 Furthermore, resistance to INSTIs has been documented in a high percentage of individuals failing INSTI-containing regimens,21 suggesting that 4DR might be increasing in low-income countries.
The PRESTIGIO Registry is an Italian open multicentre cohort comprising routinely collected data and samples in 4DR-PLWH. The cohort is a valuable tool for studying individual characteristics, including clinical, virological and molecular patterns associated with disease progression. Although 4DR might be considered a rare condition in PLWH from high-income countries, further studies are needed to assess the temporal evolution of this phenomenon, improve the management of individuals with 4DR through a multidisciplinary approach and evaluate the efficacy of the newest ART options. Furthermore, results from the PRESTIGIO Registry could be particularly beneficial for middle-income and low-income countries, especially with the widespread use of INSTI-based regimens, both in the first-line setting and in more advanced lines of therapy. Therefore, this paper describes the new opportunities in healthcare research emerging from the PRESTIGIO Registry.
Cohort description
Study design
The PRESTIGIO Registry is an ongoing Italian observational, prospective, open-ended, multicentre cohort collecting biological samples and data on clinical, laboratory, treatment and virological characteristics of 4DR-PLWH.
The recruitment period started in December 2017 and is still ongoing. From this date, individuals with 4DR are informed about the registry, after which they can either sign a written informed consent or opt-out. Follow-up accrues from the first evidence of 4DR (baseline) until death, loss to follow-up or the patient’s withdrawal of consent.
Plasma and peripheral blood mononuclear cell (PBMC) samples are collected annually for each person, starting from the date of enrollment, cryopreserved and stored in a biobank (BioRep, www.biorep.it).
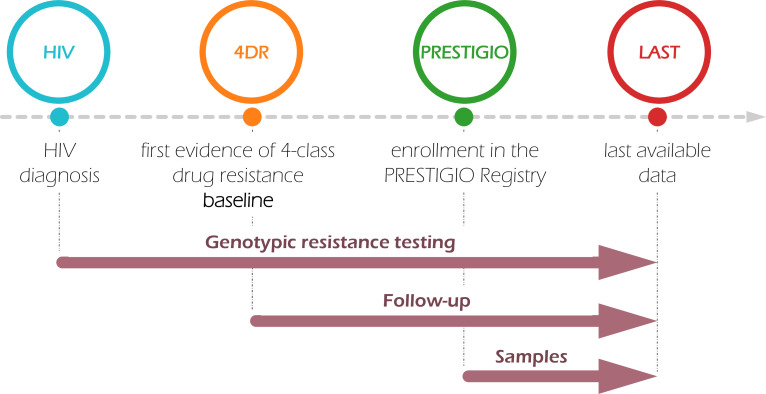
Clinical, laboratory, treatment and virological data are annually collected (by the end of January) since the enrollment; data between the first evidence of 4DR and the date of enrollment and some prebaseline data are backlogged retrospectively (figure 1). An online electronic case report form (eCRF) is available, and dedicated health staff (within each centre) manually inputs the requested information.
Figure 1.
PRESTIGIO timeline. Genotypic resistance tests have been collected since the first available HIV diagnosis. Follow-up for clinical, laboratory, treatment and virological data accrues from the first evidence of four-class drug resistance (baseline). Plasma and cell sample collection on an annual basis starts at the date of enrollment in the registry.
Registry setting
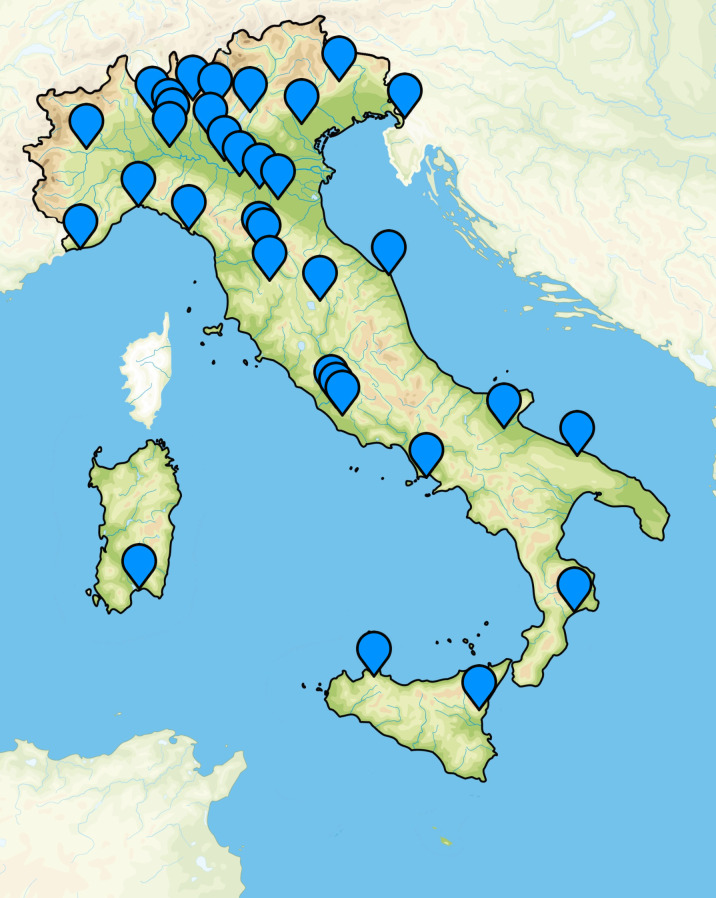
The PRESTIGIO Registry was established in December 2017; currently, there are 39 participating infectious diseases clinics located throughout Italy (23 in Northern, eight in Central, four in Southern Italy and four in Sicily and Sardinia (figure 2)).
Figure 2.
The 39 infectious diseases clinics participating in the PRESTIGIO Registry located throughout Italy.
The PRESTIGIO Registry is coordinated by the principal investigator and a steering committee designed to direct and supervise the research activities. The steering committee is composed of experts in different areas of infectious diseases.
The principal investigator is responsible for coordinating all the activities of the registry within the coordinating and the participating centres. The steering committee of the registry is responsible for (1) overseeing the monitoring and data quality control procedures; (2) promoting inclusion into the registry; (3) further developing the registry study protocol (eg, by considering additional components) and (4) making decisions on the collected biosamples in future follow-up visits.
Study population
The PRESTIGIO Registry includes PLWH who are (1) 18 years of age or older and (2) harbouring a strain with 4DR. The 4DR is defined as intermediate or high-level resistance to at least one NRTI, at least one NNRTI, at least one PI and at least one INSTI, according to the Stanford algorithm (V.9.4.1, hivdb.stanford.edu) and considering cumulative data from all the RNA-based genotypic resistance tests performed for each person. In cases of the unavailability of any integrase genotype, a documented virological failure (two consecutive HIV-1 RNA detections ≥50 copies/mL or one detection ≥1000 copies/mL) to an INSTI-containing regimen is accepted as an inclusion criterion.
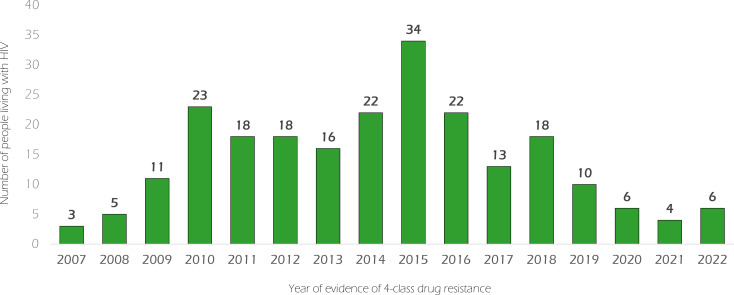
To date (14 March 2023), 229 PLWH have been included, of whom 189 (82.5%) are currently in active care, 30 (13.1%) have died and 10 (4.4%) have been lost to follow-up (tables 1 and 2; figure 3). At the last available visit, after a median follow-up of 7.7 years, the median age was 58.3 years; 27.5% were women at birth, and 91.7% were Italian, with HIV-1 infection for a median of 29.8 years. About a quarter (24.5%) stated intravenous drug use as a mode of transmission; a quarter (24.5%) were men who have sex with men or bisexual men, and a quarter (23.6%) stated heterosexual mode of transmission. Noteworthy, 9.2% were mother-to-child transmissions. All were on ART (median ART duration: 25.8 years), with more than three drug regimens in 41.5% of cases; INSTIs were contained in 85.2% of the current regimens, PIs in 73.4%, NRTIs in 72.9% and NNRTIs only in 31%. Interestingly, at the last visit, maraviroc was used in 21% of the regimens, fostemsavir in 7.4%, lenacapavir in 3.9%, ibalizumab in 3.1% and enfuvirtide in 2.6%. Despite 4DR, 51.5% of individuals reached and maintained stable virological suppression (HIV-1 RNA <50 copies/mL for ≥6 months, without any subsequent failures); at the last available visit, HIV-1 RNA was <50 copies/mL in 70.7% of cases, with a median CD4+ T-cell count of 533 cells/µL.
Table 1.
Demographic, socioeconomic and lifestyle description of the PRESTIGIO Registry at last available visit (freezing date: 14 March 2023)
| Characteristics | Overall (n=229) |
| Age (years) | 58.3 (53.6–61.6) |
| Sex assigned at birth | |
| Female | 63 (27.5%) |
| Male | 166 (72.5%) |
| Birth region | |
| Italy | 210 (91.7%) |
| Europe except Italy | 8 (3.5%) |
| Africa | 8 (3.4%) |
| South America | 2 (0.9%) |
| Asia | 1 (0.4%) |
| Ethnicity | |
| Caucasian | 218 (95.2%) |
| Black | 9 (3.9%) |
| Hispanic | 2 (0.9%) |
| Smoking habit | |
| Yes | 92 (40.2%) |
| No | 58 (25.3%) |
| Previous | 38 (16.6%) |
| Unknown | 41 (17.9%) |
| Reason for not being in active care | |
| Dead | 30 (13.1%) |
| Emigrated/lost to follow-up | 10 (4.4%) |
Data are reported as frequency (percentage) or median (IQR), as appropriate.
Table 2.
Virological, immunological and treatment description of the PRESTIGIO Registry at the last available visit (freezing date: 14 March 2023)
| Characteristics | Overall (n=229) |
| Mode of HIV transmission | |
| Heterosexual | 54 (23.6%) |
| Men who have sex with men/bisexual | 56 (24.5%) |
| Intravenous drug use | 56 (24.5%) |
| Mother to child | 21 (9.2%) |
| Unknown/other | 42 (18.3%) |
| Years since HIV diagnosis | 29.8 (25.3–33.7) |
| Years since evidence of four-class drug resistance (follow-up duration) | 7.7 (4.8–10.2) |
| HIV-1 RNA (copies/mL) | |
| <50 | 162 (70.7%) |
| 50–199 | 28 (12.2%) |
| 200–999 | 14 (6.1%) |
| ≥1000 | 25 (10.9%) |
| HIV-1 RNA <50 copies/mL for ≥6 months without subsequent virological failure | 118 (51.5%) |
| CD4+ T-cell count (cells/μL) | 533 (330.5–794) |
| CD4+ T-cell count (cells/μL) | |
| <200 | 33 (14.4%) |
| 200–349 | 31 (13.5%) |
| 350–499 | 43 (18.8%) |
| ≥500 | 122 (53.3%) |
| CD8+ T-cell count (cells/μL) | 892.5 (664.5–1260) |
| CD4+/CD8+ ratio | 0.63 (0.33–0.90) |
| CD4+ nadir (cells/μL) | 82 (17–183) |
| HIV-1 subtype | |
| B | 163 (71.2%) |
| C | 1 (0.4%) |
| F | 4 (1.7%) |
| G | 1 (0.4%) |
| Circulating recombinant forms | 7 (3.1%) |
| Missing | 53 (23.1%) |
| Tropism | |
| CCR5-tropic | 90 (39.3%) |
| CXCR4-tropic or dual mixed | 94 (41.0%) |
| Missing | 45 (19.7%) |
| CCR-5 tropism detected in all tests performed | 37 (16.2%) |
| On ART | 229 (100%) |
| ART duration (years) | 25.8 (21.9–28.8) |
| Calendar year of ART start | |
| <1998 | 148 (64.6%) |
| ≥1998 | 81 (35.4%) |
| Number of antiretrovirals in the current regimen | |
| ≤3 | 134 (58.5%) |
| 4–5 | 89 (38.9%) |
| 6–7 | 6 (2.6%) |
| NRTI-containing regimens | 167 (72.9%) |
| NNRTI-containing regimens | 71 (31%) |
| PI-containing regimens | 168 (73.4%) |
| INSTI-containing regimens | 195 (85.2%) |
| Maraviroc-containing regimens | 48 (21%) |
| Enfuvirtide-containing regimens | 6 (2.6%) |
| Fostemsavir-containing regimens | 17 (7.4%) |
| Ibalizumab-containing regimens | 7 (3.1%) |
| Lenacapavir-containing regimens | 9 (3.9%) |
Data are reported as frequency (percentage) or median (IQR), as appropriate.
ART, antiretroviral therapy; INSTI, integrase strand transfer inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitors; NRTI, nucleoside reverse transcriptase inhibitor; PI, protease inhibitor.
Figure 3.
Year of evidence of four-class drug resistance.
As what concerns virological aspects, at the last visit, 163/176 (92.6%) PLWH harbour a subtype B virus and 90/184 (48.9%) a CCR5-tropic strain (table 2). In particular, among these 90 individuals, tropisms different from CCR5 had never been detected in 41.1%. According to cumulative data from genotypic resistance testing (RNA-based, Sanger sequencing method), the most common resistance-associated mutations for each class were M184V for NRTIs (205/229 (89.5%)), K103N for NNRTIs (121/229 (52.8%)), L90M for PIs (99/229 (43.2%)) and G140S for INSTIs (78/175 (44.6%), of which 74/78 (94.9%) in combination with Q148H) (online supplemental figure 1). Fifty-four PLWH did not have an available integrase genotype at the time of virological failure to an INSTI-containing regimen because the method was not available at the centres where these individuals were in care; among them, 75.9% were included in the registry after a virological failure to a raltegravir-containing regimen, 10.5% to a dolutegravir-containing regimen and 0.6% to an elvitegravir/cobicistat-containing regimen.
bmjopen-2023-080606supp001.pdf (164.5KB, pdf)
Study objectives
The primary objectives of the PRESTIGIO Registry include (1) the clinical characterisation of the population with HIV 4DR at baseline; (2) the quantification of incidence and prevalence of AIDS-defining and non-AIDS-defining clinical events; (3) the evaluation of the long-term efficacy of different ART regimens; (4) the evaluation of ART adherence and related outcomes; (5) the description of 4DR-PLWH in terms of immunological, virological and inflammatory parameters; (6) the description of genotypic and phenotypic resistance evolution, especially after new virological failures and (7) the use of new tools to describe the resistance patterns in 4DR-PLWH.
Cohort variables and eCRF
Variables at baseline include (1) sociodemographic data (date of birth, sex at birth, country of birth, ethnicity and employment); (2) lifestyle information (height, weight, smoking habit, alcohol use and recreational drug use); (3) HIV-related clinical characteristics (mode of HIV transmission, date of last negative HIV test, date of first positive HIV test, date of ART start, date of highly active ART start (defined as a combination of drugs from at least two classes), date of 4DR, all the available RNA-based and DNA-based genotypic resistance tests [considering both Sanger sequencing and next-generation sequencing (NGS) methods and including data on capsid, envelope, viral tropism and/or subtype characterisation), CD4+ lymphocyte nadir with date, HIV-1 RNA before ART start, HIV-1 RNA, CD4+ and CD8+ T-cell count); (4) hepatitis B virus and hepatitis C virus co-infections; (5) complete blood count and blood chemistry examinations (complete blood cell count, plasma levels of glucose, triglycerides, total/high-density lipoprotein-cholesterol/low-density lipoprotein-cholesterol, creatinine, transaminases, direct and indirect bilirubin); (6) ongoing antiretrovirals and concomitant drugs (with starting date, dosages, schedules and routes of administration); (7) AIDS-defining conditions and non-AIDS-related clinical events (including malignancies of any type, diabetes, arterial hypertension requiring treatment, major adverse cardiovascular events, chronic liver or kidney diseases, osteoporosis and related fractures, neurocognitive disorders, chronic obstructive pulmonary disease, etc) and (8) sexually transmitted infections (STIs).
Data collected during follow-up include (1) an update of hepatitis co-infections; (2) further RNA-based and DNA-based genotypic resistance tests, HIV-1 RNA, CD4+ and CD8+ T-cell count determinations; (3) new complete blood chemistry; (4) modifications in ART or concomitant therapies (including also date and cause of discontinuation for each drug); (5) vaccinations; (6) incident AIDS-related and non-AIDS-related clinical events with or without hospitalisation and (7) incident STIs (online supplemental table 1).
Standard procedures to insert data into an eCRF (trials-ice2.advicepharma.com/PRESTIGIO/) have been defined, and the staff dedicated to recording information have been trained with specific data management training courses.
Participant data are entered after creating a unique pseudonym for each participant; the pseudonym is a progressive eight-digit code (centre code (three digits), dash and individual’s code (four digits)). All the collected data are managed anonymously.
The eCRF access is regulated by a permission-based security methodology that limits access to study data based on the user ID. Permissions are carefully maintained to allow only the required level of access to study data. User IDs are required to change passwords on a regular basis. All eCRF data and other critical study data are fully audit trail enabled so that all changes to the data can be monitored and/or recovered and secured via a decentralised daily backup. Every precaution has been taken to ensure that computer confidentiality is maintained.
All data entered into the eCRF are controlled and verified at multiple levels: the eCRF has several automated control mechanisms (eg, the time difference between a visit and the date of tests associated with that visit cannot be >6 months); a statistical and monitoring team verifies the appropriateness and completeness of the provided information, and the data manager of the registry may request clarifications to the staff responsible for recording information of each centre through queries on the eCRF platform or personal contact; in case of doubt about the validity or completeness of the recorded virological information, a virology team is also involved and queries are made through the eCRF platform.
To date, data monitoring has been performed online, but the PRESTIGIO Registry has planned to undertake annual on-site monitoring to check source documents and data entry since 2024.
Patient and public involvement
Until November 2022, a representative from the community of PLWH was co-opted to the steering committee, together with representatives from the main (those with at least 10 4DR-PLWH) participating centres of the PRESTIGIO Registry, and was involved in the approval of all the proposed studies. The inclusion of a new member of the community in the steering committee has been foreseen for the next few months.
Findings from the past 6 years to present
Studies on clinical and immunological characteristics of 4DR-PLWH
Considering the high risk of death and comorbidities in individuals with three-class drug-resistant HIV,12 22 Galli et al performed a retrospective cohort study on 148 4DR-PLWH from the PRESTIGIO Registry, followed by a median follow-up of 47 months, to assess the incidence of clinical events and death in this fragile population.14 This investigation showed a high burden of disease in the population with 4DR, with a markedly increased incidence of AIDS-related (2.65/100 person-years-of-follow-up) and non-AIDS-related clinical events (4.71/100 person-years-of-follow-up) and death for any cause (1.76/100 person-years-of-follow-up); further studies to better characterise the burden of disease in the PRESTIGIO cohort are ongoing. For example, we recently used retrospective data from the registry to evaluate the occurrence of STIs in 178 4DR-PLWH and found a non-negligible incidence of bacterial infections (1.3/100 person-years-of-follow-up in men, 0 in women), together with the occurrence of viral infections (first diagnosis of genital herpes simplex virus in 3.8% of men and 2.2% of women; first diagnosis of human papillomavirus in 8.3% of men and 6.5% of women).23 Although all bacterial STIs were diagnosed when HIV-1 RNA was <200 copies/mL, these findings highlight the need for strict HIV viremia monitoring, accurate ART adherence and STI prevention counselling in the population with HIV 4DR.
In light of the known association of inflammatory biomarkers with morbidity and mortality in the general population with HIV,24–31 we performed a cross-sectional study to evaluate inflammation, immune activation, microbial translocation and T-cell exhaustion in 4DR-PLWH.32 Comparing age-matched, sex-matched and smoking habit-matched 30 viremic individuals with 4DR from the PRESTIGIO Registry, 30 non-viremic 4DR-PLWH from the PRESTIGIO Registry and 20 non-viremic subjects without 4DR (from the MODAt study),33 we found that a higher inflammatory burden was associated with HIV multidrug resistance, viremia and a previous cancer diagnosis. Furthermore, T cells were more activated and ‘exhausted’ in viremic than non-viremic individuals with 4DR. These findings stress the need for further investigations to better characterise immune dysregulation in the fragile population with HIV 4DR and to evaluate new therapeutic approaches with an impact on inflammation and potential morbidity and mortality.
Virological studies on 4DR strains
Biological samples collected in PRESTIGIO were used to evaluate the residual susceptibility of four-class drug-resistant viral strains to some already-approved or investigational antiretroviral drugs. Particularly, Santoro et al analysed 22 samples from 17 4DR-PLWH who previously failed twice-daily raltegravir-based or twice-daily dolutegravir-based regimens, obtaining genotypic and phenotypic data that confirmed that bictegravir and dolutegravir retain activity against most isolates derived from this fragile HTE population.34 Similarly, Saladini et al evaluated the phenotypic susceptibility to NNRTIs from 22 viremic 4DR-PLWH from the PRESTIGIO Registry: doravirine appeared to be a valid option for some 4DR-PLWH, and its activity seemed to be inferred with fair accuracy by the Stanford HIVdb algorithm.35 As what concerns molecules with new mechanisms of action, Saladini et al investigated the genotypic and phenotypic susceptibility to temsavir in a panel of samples collected from 24 individuals with 4DR (79% previously exposed to maraviroc or enfuvirtide): temsavir resistance-associated mutations were detected only in three cases, and there was no impact of viral tropism and/or exposure to other entry inhibitors on fostemsavir susceptibility.36 Analogously, Rusconi et al analysed samples from 24 4DR-PLWH, showing that only 33% harboured a phenotypically CCR5-tropic virus, but in these cases, leronlimab maintained full activity despite the presence of extensive drug resistance and heavy treatment experience.37 In addition, leronlimab susceptibility did not appear to be significantly altered by previous or current exposure to maraviroc. Similar studies can be performed for other recently approved or investigational antiretroviral drugs.
Finally, the role of NGS in genotypic drug resistance testing has been explored. Armenia et al used NGS to evaluate HIV-DNA and HIV-RNA mutational loads of drug resistance and apolipoprotein B messenger RNA editing enzyme catalytic polypeptide (APOBEC)-related mutations in 20 virologically failing individuals enrolled in the PRESTIGIO Registry.38 The study concluded that using NGS in HIV-DNA and HIV-RNA together with measurement of APOBEC editing might help identify HTE individuals with multidrug resistance who are more prone to experience virological failure. Furthermore, in a recently published case of an HTE woman from the PRESTIGIO Registry, RNA-based NGS, performed at virological failure, was used to exclude the presence of minority resistance-associated mutations and, together with available prior genotypic resistance tests, clinical history and adherence issues, to select an effective antiretroviral regimen with a low pill burden.39 In light of this evidence, the PRESTIGIO study group is performing further studies on the use of NGS in clinical practice.
Studies on treatment strategies for 4DR-PLWH
Given the need for optimising ART in HTE individuals, Castagna et al performed a retrospective study evaluating the virological efficacy of dolutegravir 50 mg two times per day in 190 virologically failing PLWH with previous exposure to first-generation INSTIs.40 The estimated probability of virological failure was limited (17%, 33% and 52% at 12, 36 and 60 months since baseline, respectively), highlighting the favourable long-term efficacy of dolutegravir 50 mg two times per day, associated with an optimised background regimen in HTE failing subjects with an INSTI-resistant virus.
Retrospective data from the PRESTIGIO Registry also showed that a small group of 10 4DR-PLWH who underwent ART simplification with a high genetic barrier two-drug regimen (containing darunavir/ritonavir two times per day and/or dolutegravir 50 mg two times per day), for any reason, was able to maintain a long-term suppression in 90% of cases.41 These findings suggest that a high genetic barrier two-drug regimen might represent an effective option for carefully selected PLWH with 4DR who need simplification. Moreover, in a case report on an 80-year-old HTE man from the PRESTIGIO Registry, ART was successfully simplified by reducing drug and pill burden after the achievement of virological suppression, thanks to a careful evaluation of cumulative genotypic resistance testing and drug–drug interactions.42 Larger studies on the possibility of simplifying complex regimens in this fragile population are ongoing in the PRESTIGIO cohort.
Collaborations
Any HIV care provider from a centre participating in the PRESTIGIO Registry may propose a project to the steering committee. After approval of the proposal, anonymised data and/or samples from the registry will be made available to the study proponent, together with the support of a statistical and monitoring team.
The PRESTIGIO Registry is also available to collaborate with national and international cohorts or centres with high expertise in specific fields (eg, virology, immunology, reservoir quantification, molecular biology, etc). In particular, given the limited prevalence of HIV 4DR in high-income countries, collaboration with other cohorts of individuals with multidrug-resistant viral strains may help to characterise this population better and to draw more easily generalisable conclusions. In addition, for many clinical, immunological and virological studies, a control group of PLWH without 4DR but with a long HIV infection and ART duration could be useful to estimate the effect of multidrug resistance. Finally, in addition to clinical and treatment characterisation, highly specialised studies may be useful not only to better understand the mechanisms underlying this population’s frailty but also to offer innovative and targeted treatment approaches.
Future plans
The PRESTIGIO Registry provides a unique asset to study long-term treatment, comorbidities, and drug resistance patterns in people with multidrug-resistant HIV in Italy.
On one side, 29% of 4DR-PLWH still have an unsuppressed viral load, requiring new antiretroviral treatment options. On the other hand, non-viremic individuals with complex ART regimens require safe and robust simplification strategies to minimise toxicity and maximise adherence. Furthermore, attempts are made to conduct virological studies on drug resistance mechanisms and the possibility of using new tools to predict treatment success. Finally, with our ageing fragile cohort, studies on comorbidities and their underlying molecular mechanisms become more important, especially to better characterise the disease burden in this population and assess the role of long-term ART exposure and past or current uncontrolled viral replication. In this sense, the study of the quality of life of these fragile individuals could also be useful for their correct management. The studies of the registry are generally aimed at a better understanding of a specific health condition, the emergence of comorbidities or the effect of potential treatments or experimental drugs that may have an impact on disease progression. The research studies should also aim to be inclusive, innovative and in touch with communities and society as a whole.
Strengths and limitations
The main strength of the PRESTIGIO Registry is its unicity: to our knowledge, it is the first cohort that specifically includes 4DR-PLWH. Furthermore, the registry is already available for research projects: clinical centres enrolling individuals with 4DR have been linked, patient pathways have been identified, and data have been centralised to enable convenient querying. The accuracy, completeness and consistency of data from the date of the first evidence of 4DR are high, especially for genotypic resistance tests, virological and immunological information, antiretroviral treatment and clinical events. Also, the availability of cryopreserved PBMC and plasma samples collected annually allows for the conduct of virological and immunological studies to better characterise this population. The multicentre design overcomes the limitations of single-centre studies on this small population, even though the number of individuals included in the cohort remains limited due to the rarity of HIV 4DR in high-income countries. Some variables are sparsely available in the PRESTIGIO Registry, which currently limits their use for research purposes, but efforts to retrieve this information or obtain it through laboratory analysis (eg, tropism and subtype) are underway. Furthermore, the vast majority of the cohort was born in Italy and harbours a subtype B viral strain, presumably due to the long duration of HIV infection; most diagnoses could be dated to a period when Italy was considered a B-restricted area. However, it is possible that non-Italian-born individuals and subtype non-B viruses with 4DR could be enrolled in the PRESTIGIO Registry in the coming years, following the trend of new diagnoses.43 Another limitation is the lack of data before the first evidence of 4DR (except for genotypes), although extra information from a limited number of individuals can be easily added by the enrolling centres for specific studies.
bmjopen-2023-080606supp002.pdf (65.4KB, pdf)
Supplementary Material
Footnotes
Contributors: AnCa, LG, VS and TC planned and designed the cohort profile description. LG and RL performed the statistical analysis. TC, LG and VS drafted the manuscript. RL, RG, FL, MF, AMC, EF, ADB, AdCe, LC, FM, GM, GC, SR, MZ, MMS and AnCa revised the manuscript and approved the final version. TC, LG, VS and AnCa, as guarantors, accepted full responsibility for the work, had access to the data and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: RG reports payments to her institution from Gilead Sciences; personal fees for speaker panels and educational material from ViiV Healthcare, Merck Sharp and Dohme and Gilead Sciences and advisory boards from Theratechnologies, Janssen-Cilag and Gilead Sciences. FL reports personal fees for speaker panels from ViiV Healthcare, Janssen-Cilag and Merck Sharp and Dohme; travel grants from Gilead Sciences, ViiV Healthcare and Janssen-Cilag and advisory boards from ViiV Healthcare and Janssen-Cilag. EF reports personal fees for consultancy from Merck Sharp and Dohme, ViiV Healthcare, Gilead Sciences and Swedish Orphan Biovitrum; speaker panels and educational material from ViiV Healthcare and Gilead Sciences and advisory boards from ViiV Healthcare, Gilead Sciences and Merck Sharp and Dohme. ADB reports personal fees for speaker panels and educational material from ViiV Healthcare and Gilead Sciences and travel grants from ViiV Healthcare. AdCe reports personal fees for speaker panels from ViiV Healthcare. FM reports personal fees for consultancy and advisory boards from Merck Sharp and Dohme, ViiV Healthcare and Gilead Sciences. GM reports personal fees for speaker panels and educational material from Gilead Sciences; travel grants from Janssen-Cilag, Gilead Sciences and ViiV Healthcare and advisory boards from Gilead Sciences, ViiV Healthcare and Angelini Pharma. GC reports personal fees for speaker panels and educational material from Gilead Sciences, ViiV Healthcare and AbbVie and travel grants from Gilead Sciences. SR reports payments to his institution from Gilead Sciences, Janssen-Cilag and ViiV Healthcare; personal fees for travel grants from Gilead Sciences, Janssen-Cilag and ViiV Healthcare and advisory boards from Gilead Sciences, Janssen-Cilag, ViiV Healthcare and Merck Sharp and Dohme. MZ reports personal fees for consultancy and speaker panels and educational material from Gilead Sciences, ViiV Healthcare and Merck Sharp and Dohme. MMS reports personal fees for speaker panels and educational material from ViiV Healthcare, Merck Sharp and Dohme and Janssen-Cilag and advisory boards from ViiV Healthcare and Theratechnlogies. VS reports grants from Gilead Sciences and personal fees for speaker panels from Gilead Sciences, ViiV Healthcare and Merck Sharp & Dohme. AnCa reports personal fees for advisory boards, speaker panels and educational materials from Gilead Sciences, ViiV Healthcare, Janssen-Cilag, Merck Sharp & Dohme and Theratechnlogies. PRESTIGIO Registry received funding from Gilead Sciences, ViiV Healthcare, Merck Sharp & Dohme, and Theratechnologies.
All other authors: no potential conflicts.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data can be made available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants. The PRESTIGIO Registry was approved by the Ethic Committee of the coordinating centre (IRCCS San Raffaele Scientific Institute, Milan, Italy, protocol number 41/int/December 2017) and by the Ethic Committees of all the participating centres (University Hospital 'Ospedali Riuniti', Ancona, Italy; Centro di riferimento oncologico, Aviano, Italy; Santa Maria Annunziata Hospital, Bagno a Ripoli, Italy; Hospital-University Polyclinic of Bari, Bari, Italy; Azienda Ospedaliera Papa Giovanni XXIII, Bergamo, Italy; S. Orsola Hospital, Bologna, Italy; Azienda Ospedaliera Spedali Civili di Brescia, Brescia, Italy; ASST della Valle Olona, Busto Arsizio Hospital, Busto Arsizio, Italy; University Hospital of Cagliari, Cagliari, Italy; SS Trinità Hospital, ASSL Cagliari, Italy; Garibaldi Hospital, Catania, Italy; AOU Mater Domini, Catanzaro, Italy; ASST di Cremona, Cremona, Italy; Careggi University Hospital, Florence, Italy; Plesso Colonnello D’Avanzo, Foggia, Italy; Galliera Hospital, Genoa, Italy; IRCCS Policlinico San Martino Hospital, Genoa, Italy; Sant’Andrea Hospital La Spezia, La Spezia, Italy; ASST Fatebenefratelli Sacco, Luigi Sacco Hospital, Milan, Italy; San Paolo Hospital, ASST Santi Paolo e Carlo, Milan, Italy; ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy; IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy; Azienda Ospedaliero-Universitaria di Modena, Modena, Italy; AORN dei Coli, PO Cotugno, Naples, Italy; Padua University Hospital, Padua, Italy; AOU Policlinico 'P. Giaccone', Palermo, Italy; AO-Universitaria, Parma, Italy; Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; University Hospital 'S. Maria della Misericordia', Perugia, Italy; Arcispedale S. Maria Nuova-IRCSS, Reggio Emilia, Italy; National Institute for Infectious Diseases 'L. Spallanzani' IRCCS, Rome, Italy; Tor Vergata University Hospital PTV, Rome, Italy; Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy; Sanremo Hospital, Sanremo, Italy; University Hospital of Siena, Siena, Italy; Amedeo di Savoia Hospital, Turin, Italy; Trieste University Hospital ASUGI, Trieste, Italy; AULSS9 Azienda Scaligera di Verona, Verona, Italy). Participants gave informed consent to participate in the study before taking part.
References
- 1. Smith CJ, Ryom L, Weber R, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a Multicohort collaboration. Lancet 2014;384:241–8. 10.1016/S0140-6736(14)60604-8 [DOI] [PubMed] [Google Scholar]
- 2. Legarth RA, Ahlström MG, Kronborg G, et al. Long-term mortality in HIV-infected individuals 50 years or older: A nationwide, population-based cohort study. J Acquir Immune Defic Syndr 2016;71:213–8. 10.1097/QAI.0000000000000825 [DOI] [PubMed] [Google Scholar]
- 3. Trickey A, May MT, Vehreschild J-J, et al. Antiretroviral therapy cohort collaboration. survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. The Lancet HIV 2017;4:e349–56. 10.1016/S2352-3018(17)30066-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marcus JL, Leyden WA, Alexeeff SE, et al. Comparison of overall and Comorbidity-free life expectancy between insured adults with and without HIV infection, 2000-2016. JAMA Netw Open 2020;3:e207954. 10.1001/jamanetworkopen.2020.7954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wandeler G, Johnson LF, Egger M. Trends in life expectancy of HIV-positive adults on antiretroviral therapy across the globe. Current Opinion in HIV and AIDS 2016;11:492–500. 10.1097/COH.0000000000000298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Armenia D, Di Carlo D, Flandre P, et al. HIV MDR is still a relevant issue despite its dramatic drop over the years. J Antimicrob Chemother 2020;75:1301–10. 10.1093/jac/dkz554 [DOI] [PubMed] [Google Scholar]
- 7. Cutrell J, Jodlowski T, Bedimo R. The management of treatment-experienced HIV patients (including virologic failure and switches). Ther Adv Infect Dis 2020;7:2049936120901395. 10.1177/2049936120901395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Priest J, Hulbert E, Gilliam BL, et al. Characterization of heavily treatment-experienced people with HIV and impact on health care resource utilization in US commercial and Medicare advantage health plans. Open Forum Infect Dis 2021;8:ofab562. 10.1093/ofid/ofab562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pelchen-Matthews A, Borges ÁH, Reekie J, et al. Prevalence and outcomes for heavily treatment-experienced individuals living with human immunodeficiency virus in a European cohort. J Acquir Immune Defic Syndr 2021;87:806–17. 10.1097/QAI.0000000000002635 [DOI] [PubMed] [Google Scholar]
- 10. Pelchen-Matthews A, Ryom L, Borges ÁH, et al. Aging and the evolution of Comorbidities among HIV-positive individuals in a European cohort. AIDS 2018;32:2405–16. 10.1097/QAD.0000000000001967 [DOI] [PubMed] [Google Scholar]
- 11. Enriquez M, McKinsey DS. Strategies to improve HIV treatment adherence in developed countries: clinical management at the individual level. HIV AIDS (Auckl) 2011;3:45–51. 10.2147/HIV.S8993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zaccarelli M, Tozzi V, Lorenzini P, et al. Multiple drug class-wide resistance associated with poorer survival after treatment failure in a cohort of HIV-infected patients. AIDS 2005;19:1081–9. 10.1097/01.aids.0000174455.01369.ad [DOI] [PubMed] [Google Scholar]
- 13. Spivack S, Pagkalinawan S, Samuel R, et al. HIV: how to manage heavily treatment-experienced patients. Drugs Context 2022;11:2021-9-1. 10.7573/dic.2021-9-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Galli L, Parisi MR, Poli A, et al. Burden of disease in PWH harboring a multidrug-resistant virus: data from the PRESTIGIO Registry. Open Forum Infect Dis 2020;7:ofaa456. 10.1093/ofid/ofaa456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Davy-Mendez T, Eron JJ, Brunet L, et al. New antiretroviral agent use affects prevalence of HIV drug resistance in clinical care populations. AIDS 2018;32:2593–603. 10.1097/QAD.0000000000001990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lombardi F, Giacomelli A, Armenia D, et al. Prevalence and factors associated with HIV-1 multi-drug resistance over the past two decades in the Italian ARCA database. Int J Antimicrob Agents 2021;57:106252. 10.1016/j.ijantimicag.2020.106252 [DOI] [PubMed] [Google Scholar]
- 17. World Health Organization . HIV drug resistance report 2021. 2021. Available: https://www.who.int/publications/i/item/9789240038608 [Accessed 31 Jul 2023].
- 18. Barabona G, Mahiti M, Masoud S, et al. Pre-treatment and acquired HIV drug resistance in Dar es Salaam, Tanzania in the era of tenofovir and routine viral load monitoring. J Antimicrob Chemother 2019;74:3016–20. 10.1093/jac/dkz272 [DOI] [PubMed] [Google Scholar]
- 19. von Braun A, Sekaggya-Wiltshire C, Bachmann N, et al. HIV-1 drug resistance among Ugandan adults attending an urban out-patient clinic. J Acquir Immune Defic Syndr 2018;78:566–73. 10.1097/QAI.0000000000001717 [DOI] [PubMed] [Google Scholar]
- 20. Inzaule SC, Hamers RL, Mukui I, et al. Emergence of Untreatable, multidrug-resistant HIV-1 in patients failing second-line therapy in Kenya. AIDS 2017;31:1495–8. 10.1097/QAD.0000000000001500 [DOI] [PubMed] [Google Scholar]
- 21. Ngoufack Jagni Semengue E, Santoro MM, Ndze VN, et al. HIV-1 Integrase resistance associated mutations and the use of Dolutegravir in sub-Saharan Africa: A systematic review and meta-analysis. PLOS Glob Public Health 2022;2:e0000826. 10.1371/journal.pgph.0000826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Costagliola D, Lodwick R, Ledergerber B, et al. Trends in virological and clinical outcomes in individuals with HIV-1 infection and virological failure of drugs from three antiretroviral drug classes: a cohort study. Lancet Infect Dis 2012;12:119–27. 10.1016/S1473-3099(11)70248-1 [DOI] [PubMed] [Google Scholar]
- 23. Clemente T, Lolatto R, Papaioannu Borjesson R, et al. Sexually transmitted infections in people with multidrug-resistant HIV. AIDS 2023;37:2425–30. 10.1097/QAD.0000000000003690 [DOI] [PubMed] [Google Scholar]
- 24. Hunt PW, Lee SA, Siedner MJ. Immunologic biomarkers, morbidity, and mortality in treated HIV infection. J Infect Dis 2016;214 Suppl 2:S44–50. 10.1093/infdis/jiw275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Erlandson KM, Allshouse AA, Jankowski CM, et al. Association of functional impairment with inflammation and immune activation in HIV type 1-infected adults receiving effective antiretroviral therapy. J Infect Dis 2013;208:249–59. 10.1093/infdis/jit147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mooney S, Tracy R, Osler T, et al. Elevated biomarkers of inflammation and coagulation in patients with HIV are associated with higher Framingham and VACS risk index scores. PLoS One 2015;10:e0144312. 10.1371/journal.pone.0144312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Montoya JL, Campbell LM, Paolillo EW, et al. Inflammation relates to poorer complex motor performance among adults living with HIV on suppressive antiretroviral therapy. J Acquir Immune Defic Syndr 2019;80:15–23. 10.1097/QAI.0000000000001881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kuller LH, Tracy R, Belloso W, et al. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med 2008;5:e203. 10.1371/journal.pmed.0050203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hunt PW, Sinclair E, Rodriguez B, et al. Gut epithelial barrier dysfunction and innate immune activation predict mortality in treated HIV infection. J Infect Dis 2014;210:1228–38. 10.1093/infdis/jiu238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. So-Armah KA, Tate JP, Chang C-CH, et al. Do biomarkers of inflammation, monocyte activation, and altered coagulation explain excess mortality between HIV infected and uninfected people J Acquir Immune Defic Syndr 2016;72:206–13. 10.1097/QAI.0000000000000954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Freiberg MS, Bebu I, Tracy R, et al. D-Dimer levels before HIV seroconversion remain elevated even after viral suppression and are associated with an increased risk of non-AIDS events. PLoS One 2016;11:e0152588. 10.1371/journal.pone.0152588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Clemente T, Caccia R, Galli L, et al. Inflammation burden score in multidrug-resistant HIV-1 infection. J Infect 2023;86:453–61. 10.1016/j.jinf.2023.03.011 [DOI] [PubMed] [Google Scholar]
- 33. Castagna A, Spagnuolo V, Galli L, et al. Simplification to Atazanavir/Ritonavir monotherapy for HIV-1 treated individuals on virological suppression: 48-week efficacy and safety results. AIDS 2014;28:2269–79. 10.1097/QAD.0000000000000407 [DOI] [PubMed] [Google Scholar]
- 34. Santoro MM, Fornabaio C, Malena M, et al. Susceptibility to HIV-1 Integrase strand transfer inhibitors (Instis) in highly treatment-experienced patients who failed an INSTI-based regimen. Int J Antimicrob Agents 2020;56:106027. 10.1016/j.ijantimicag.2020.106027 [DOI] [PubMed] [Google Scholar]
- 35. Saladini F, Giammarino F, Maggiolo F, et al. Residual Phenotypic susceptibility to Doravirine in multidrug-resistant HIV-1 from subjects enrolled in the PRESTIGIO Registry. Int J Antimicrob Agents 2023;61:106737. 10.1016/j.ijantimicag.2023.106737 [DOI] [PubMed] [Google Scholar]
- 36. Saladini F, Giannini A, Giammarino F, et al. In vitro susceptibility to Fostemsavir is not affected by long-term exposure to antiviral therapy in MDR HIV-1-infected patients. J Antimicrob Chemother 2020;75:2547–53. 10.1093/jac/dkaa178 [DOI] [PubMed] [Google Scholar]
- 37. Rusconi S, Saladini F, Bellocchi MC, et al. Leronlimab (PRO 140) in vitro activity against 4-class drug resistant HIV-1 from heavily treatment experienced subjects. Pharmacol Res 2022;176:106064. 10.1016/j.phrs.2022.106064 [DOI] [PubMed] [Google Scholar]
- 38. Armenia D, Santoro MM, Bellocchi MC, et al. Viral resistance burden and APOBEC editing correlate with virological response in heavily treatment-experienced people living with multi-drug resistant HIV. Int J Antimicrob Agents 2022;59:106492. 10.1016/j.ijantimicag.2021.106492 [DOI] [PubMed] [Google Scholar]
- 39. Labate L, Bruzzone B, Spagnuolo V, et al. PRESTIGIO RING: “A 59-year-old HIV-1 positive, highly treatment-experienced woman failing Darunavir/ Ritonavir plus Raltegravir New Microbiol 2023;46:226–30. [PubMed] [Google Scholar]
- 40. Castagna A, Ferrara M, Galli L, et al. Long-term efficacy of Dolutegravir in treatment-experienced subjects failing therapy with HIV-1 Integrase strand inhibitor-resistant virus. J Antimicrob Chemother 2018;73:177–82. 10.1093/jac/dkx371 [DOI] [PubMed] [Google Scholar]
- 41. Canetti D, Galli L, Gianotti N, et al. Simplification to high genetic barrier 2-drug regimens in people living with HIV harboring 4-class resistance enrolled in the PRESTIGIO Registry. J Acquir Immune Defic Syndr 2020;84:e24–8. 10.1097/QAI.0000000000002378 [DOI] [PubMed] [Google Scholar]
- 42. Mazzitelli M, Zazzi M, Marchetti G, et al. PRESTIGIO RING: “An 80-year-old man living with HIV resistant to all four antiretroviral classes and desiring treatment simplification.” New Microbiol 2023;46:407–11. [PubMed] [Google Scholar]
- 43. Rossetti B, Di Giambenedetto S, Torti C, et al. Evolution of transmitted HIV-1 drug resistance and viral subtypes circulation in Italy from 2006 to 2016. HIV Med 2018;19:619–28. 10.1111/hiv.12640 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-080606supp001.pdf (164.5KB, pdf)
bmjopen-2023-080606supp002.pdf (65.4KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data can be made available upon reasonable request.