Abstract
Background
Peroneus longus tendon (PLT) is a known graft utilised in the ligamentous reconstructions of knee. The current review was performed to analyze the available evidence regarding PLT in the arthroscopic anterior cruciate ligament (ACL) reconstruction.
Methods
A comprehensive search of literature was performed on March 1, 2023 using 5 databases (for manuscripts published between 2010 and 2023). All studies reporting ACL reconstruction with PL graft in adults ≥18 years were considered; and final studies were shortlisted based on specific exclusion criteria.
Results
The search identified 684 articles, among which 26 manuscripts were finally selected. PLT has been used in primary ACL reconstruction (ACLR), revision ACLR, ACLR in multiligamentous injuries and those at risk for anterior knee pain. The full-thickness PLT graft is variable in its dimensions with the mean size ranging between 7 and 8.8 mm (half-PLT grafts ≤8.1 mm). The ultimate strength of doubled PLT graft is significantly higher than native ACL and comparable to the quadrupled hamstring.
There was statistically insignificant difference in the laxity and functional outcome of knee following ACLR with PLT, as compared with other autografts (p > 0.05). PLT harvest is associated with satisfactory clinical foot and ankle outcomes, as well as excellent regenerative ability. Overall, studies have demonstrated lower complications with PLT (p < 0.05).
Conclusion
The dimensions of harvested PLT graft are more consistent than HT. It has similar functional outcome and survival, as compared to other autografts. It also has lower risk for donor-site morbidity and lower complications than HT. PLT is a promising, alternative autograft choice in patients undergoing ACLR.
Keywords: Peroneus longus, Tendon graft, Anterior cruciate ligament, Ligament injury, Autograft
1. Introduction
Tendon grafts are widely utilised globally for diverse areas of reconstructive surgeries in orthopaedics.1 Over the past decades, various autologous tendon grafts have been employed in anterior cruciate ligament reconstruction (ACLR) surgeries.2,3 Among them, the most commonly utilised options include patellar, quadriceps, semitendinosus, iliotibial band and gracilis tendons.3,4 Over the past years, it has been postulated that the neo-tendon develops in the area of graft harvest.5 Even since the initial report of regenerative potential of a harvested tendon in 1992, several clinical and experimental studies have further substantiated this observation, although there is still insufficient evidence that neo-tendon functions similar to a normal tendon.6,7,7,8,8,9,9, 9, 10, 11, 12, 13
The mean length and width of normal ACL measure 38 mm (range: 25–41 mm) and 10 mm (range: 7–12 mm), respectively.14,15 Over the past decades, bone-patellar tendon-bone (B-PT-B) graft has been acknowledged as the gold standard graft option (with tensile load and stiffness of 2,977 N and 620 N/mm) for replacing a deficient ACL.4 However, the use of patellar tendon graft has been correlated with diverse complications including anterior or patellofemoral joint pain, patellar chondromalacia, patellar fractures, ruptures of patellar tendon, patellar tendon shortening or persistent weakness of quadriceps mechanism.16, 17, 18, 19, 20 Although donor-site morbidity has remained less of a concern with hamstring (HT) grafts, these grafts have been associated with issues including higher objective laxity on KT-1000 testing,21significant weakening of the hamstring mechanism (which is crucial to protecting the reconstructed ACL from unopposed, anterior pull of the quadriceps musculature)22, 23, 24; and the unpredictability in the size of harvested hamstring graft (yielding graft of diameter < 7–8 mm).25,26 Based on previous studies, it has been observed that patients weighing less than 50 kg, vertical height shorter than 140 cm, body mass index (BMI) of under 18 and thigh girth <37 cm, are significantly predisposed to the risk of yielding quadrupled hamstring autograft of diameter < 7 mm.27, 28, 29, 30, 31, 32, 33, 34 The quadriceps tendon autograft (central 1/3) has also been purported as an available option. While the supporters of quadriceps graft report higher collagen content (approximately 50 %) in comparison to similar-sized patellar ligament graft; weakness of the quadriceps musculature and patellofemoral pain have remained the crucial drawbacks.35
To circumvent these difficulties, allograft use for ACLR has been gradually gaining in popularity.36 The benefits of using an allograft include reduced operative time, mitigated post-operative pain and reduced donor-site morbidity.37 Additionally, allograft reconstruction can be a highly suitable procedure in elderly patients, revision ACLR and multi-ligamentous knee injuries.37 However, the performance of allografts depends upon various factors like its immunogenicity, preservation modality, host remodelling, positions of tunnel and graft, graft preparation, graft tension; and post-operative rehabilitation.38 While allograft-related disease transmission is substantially lowered with donor screening and ȣ-irradiation,39 exposure to radiation greater than 2.5 Mrad negatively affects the graft strength and integrity.15,39 Allografts also require substantial resources for sterilization and storage.
In view of these disadvantages attributed to the traditional autograft and allograft alternatives, the option of peroneus longus tendon (PLT) graft, discrete from the knee joint was explored. Since 1997, PLT graft has been employed for diverse ligament reconstructions within the knee joint.40 It has been considered as a promising autograft, with diverse purported benefits like simple harvesting technique, larger graft diameter, and minimal complication rates (including preservation of ankle joint functions).23,41, 42, 43 This review was therefore, planned in order to thoroughly evaluate the current evidence regarding PLT in the reconstruction of ACL during arthroscopic knee surgeries.
2. Methods
2.1. Strategy for literature search
-
•
A thorough search of literature was conducted on 1st March 2023 with the PEO (Population, Exposure, Outcome; Table 1) framework using 5 databases (Embase, Web of Science, Google scholar, Pubmed, Cochrane library) evaluating the literature published during the period 2010 to 2023. The article search was performed using the key words combined with the Boolean operators: (((ACL reconstruction) OR (anterior cruciate ligament reconstruction) AND ((PL tendon graft) OR (peroneus longus tendon autograft))). The search strategy is depicted in Fig. 1.
Table 1.
PEO framework.
| Population | Anterior cruciate ligament reconstruction (ACLR) and Peroneus longus autograft |
| Exposure | |
| Outcome | Dimensions or biomechanical properties of graft, Clinical knee function scores, Clinical knee function scores, Patient satisfaction scores, Complication rates, |
Fig. 1.
Strategy for manuscript selection.
2.2. Eligibility criteria
-
•
All studies reporting ACL reconstruction with PL graft in adults ≥18 years (including revision surgeries, multi-ligamentous reconstructions or additional procedures like osteotomies) were identified. Among them, review articles (systematic or narrative), non-clinical or patho-physiological studies, letters to editor, non-English manuscripts, studies involving inflammatory arthritis or rheumatological disorders and case reports were excluded (Table 2).
Table 2.
Criteria for inclusion and exclusion of studies.
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Study Design | Clinical studies, RCTs, observational studies, | Reviews, meta-analysis, case reports, grey literature |
| Patient Population | >18 years with ACL instability | Inflammatory diseases, other rheumatic conditions |
| Language | English language | Non-English language |
2.3. Article selection and extraction of data
-
•
The search results from the aforementioned databases were extracted onto End-note, de-duplicated and manually selected. The manuscript titles were initially assessed by 2 authors (VKV, VKJ). Following this, individual abstracts or complete manuscripts were screened based on the aforementioned criteria (Table 2). The disagreements during manuscript selection were resolved following arbitration by senior-most author. Following this, the review of complete, individual manuscripts was performed by the two authors (VKV and VKJ).
2.4. Research objectives (RO)
-
•The main objectives of this review are:
- RO1: Indications in ACL reconstruction (ACLR)
- RO2: Dimensions and characteristics of the PL tendon grafts
- RO3: Biomechanical properties of the graft; RO4: Complications of PL graft; RO5: Outcome – Clinical, functional and radiological following ACLR with PL graft
3. Results
Literature Search: The search of the literature identified a total of 684 manuscripts. On compilation and de-duplication using Endnote, 256 articles were included. Following the scrutiny of titles, 97 studies were identified. After screening individual abstracts/full-texts, 26 studies were eventually selected for the review (Fig. 1).
Description of reviewed studies: Out of the 26 reviewed studies, 4 emanated from the United States of America (USA), 8 from India, 4 from China; 5 from Indonesia and 1 each emanated from Iran, Thailand, Taiwan, Turkey and Vietnam. While 4 studies were experimental, 9 were retrospective, 2 were randomized clinical trials and the remaining were prospective studies. The respective publishing journals have been tabulated vide-infra (Table 3).
Table 3.
Descriptive details of individual studies.
| SNo | Authors | Publication Year | Country | Journal | Study type |
|---|---|---|---|---|---|
| 1 | Pearsall | 2003 | USA | Arthroscopy: The Journal of Arthroscopic and Related Surgery | Biomechanical study |
| 2 | Kerimoglu | 2009 | Turkey | Knee Surg Sports Traumatol Arthrosc | Retrospective |
| 3 | Chan | 2010 | USA | Arthroscopy: The Journal of Arthroscopic and Related Surgery | Biomechanical study |
| 4 | Zhao | 2012 | China | The American Journal of Sports Medicine | Biomechanical study & retrospective case series |
| 5 | Nazem | 2014 | Iran | Advanced Biomedical Research | Prospective |
| 6 | Liu | 2015 | Taiwan | Journal of Orthopedic Science | Prospective |
| 7 | Angthong | 2015 | Thailand | Journal of Medical Association of Thailand | Biomechanical study & retrospective case series |
| 8 | Rudy | 2017 | Indonesia | International Journal of Surgery Open | Biomechanical study |
| 9 | Wong | 2018 | USA | Clinical Biomechanics | Biomechanical study' |
| 10 | Bi | 2018 | China | The Journal of Knee Surgery | Prospective randomized clinical study |
| 11 | Khajotia | 2018 | India | International Journal of Research in Orthopaedics | Prospective |
| 12 | Shi | 2018 | USA | The Journal of Knee Surgery | Prospective |
| 13 | Song | 2018 | China | Medicine | Retrospective |
| 14 | Rhatomy | 2019 | Indonesia | Annals of Medicine and Surgery | Retrospective |
| 15 | Trung | 2019 | Vietnam | Open Access Maced J Med Sci. | Prospective |
| 16 | Kumar | 2019 | India | International Journal of Research in Medical Sciences | Prospective |
| 17 | Rhatomy | 2019 | Indonesia | Knee Surgery, Sports Traumatology, Arthroscopy | Prospective |
| 18 | Rhatomy | 2019 | Indonesia | The Orthopedic Journal of Sports Medicine | Retrospective |
| 19 | Sharma | 2019 | India | Indian Journal of Orthopaedics Surgery | Retrospective |
| 20 | Sakti | 2020 | India | Journal of Orthopaedics | Prospective |
| 21 | Rhatomy | 2020 | Indonesia | Journal of Clinical Orthopaedics and Trauma | Retrospective |
| 22 | Shao | 2020 | China | The Bone & Joint Journal | Retrospective |
| 23 | Kumar | 2020 | India | European Journal of Molecular & Clinical Medicine | Prospective |
| 24 | Joshi | 2021 | India | Nigerian Journal of Surgery | Prospective |
| 25 | Vijay | 2022 | India | Journal of Orthopaedics, Trauma and Rehabilitation | Prospective randomized clinical study |
| 26 | Goyal | 2023 | India | European Journal of Orthopedic Surgery and Traumatology | Prospective |
3.1. Indications
PLT graft has been used for diverse ligamentous reconstructions of the knee (in scenarios of primary or revison ACL, PCL, collateral or multi-ligamentous reconstruction surgeries), as shown in Table 4. A majority of the studies have utilised PLT graft in patients undergoing primary ACLR. In patients at risk for bothersome post-operative anterior knee pain (where patellar or quadriceps tendon grafts may be difficult options) or for inadequate harvest of hamstring tendon (HT) graft, PLT may provide an excellent alternative.4,6,12,14,15,26,28,43 In revision ACL reconstructions or multi-ligament reconstructions of the knee, the PLT graft may serve as an excellent source of autograft.43 In ACL injuries associated with medial patella-femoral ligament (MPFL) or medial collateral ligament (MCL) damage, PLT may serve as a good alternative to hamstring graft, because the harvest of the latter graft may further enhance medial knee instability in such scenarios.2,21,44 Shi et al.2 concluded that PLT is a suitable graft material for reconstructing ACL injuries with concomitant grade-3 MCL injuries. Angthong et al.16 observed that patients with high-level sporting activities requiring extreme ankle functions (such as soccer), dancers, and those with previous history of ankle injury or instability, were at relatively high risk for poorer outcome following the harvest of PLT grafts.
Table 4.
Uses of personal tendon in different situations.
|
3.2. Graft harvest and surgical technique
Across the literature, PLT has been harvested in the form of full-width or partial grafts11 (anterior or posterior half of the tendon; Table 5). The partial grafts have also been employed as the sole graft material or as an adjuvant graft to reinforce the other autograft materials (especially, in weak or inadequate hamstring tendons).12 The graft has been utilised as doubled, tripled or quadrupled constructs to reconstruct the ACLs. All the studies have highlighted that these PLT grafts are usually easy to harvest and involve relatively shorter operative time; in view of the superficial location.44, 45, 46 In general, for single-bundle ACL reconstruction, two-strand full-width PLT graft is preferred.
Table 5.
-Significant observations from the individual studies.
| S.No | Study | Sample population | Type and characteristics of PLT graft | Significant findings |
|---|---|---|---|---|
| 1 | Chan | Biomechanical study (4 cadaveric specimens of PLT) | PLT graft tested on MTS machine in a single-looped manner | Ultimate tensile strength:3050 N |
| Stiffness: 346 N/mm | ||||
| 2 | Zhao | Ninety two patients undergoing knee ligamentous reconstruction | Anterior ½ of PLT (AHPLT) | Mean failure load: 322.35 ± 663.18 N(97.69 ± 19.48 % of semitendinosus, 147.94 ± 41.3 % of gracilis) |
| Distance between tendon stripperand bifurcation of deep peroneal nerve:4.6–10.4 cm | ||||
| PreoperativeAOFAS: 97.4 ± 2.0 | ||||
| Postoperative AOFAS:97.2 ± 1.6 (p = 0.85) | ||||
| Preoperative FADI: 96.8 ± 2.2 | ||||
| Postoperative FADI:96.9 ± 2.5 (p = 0.91) | ||||
| No peroneal nerve injury, PLT tendinopathy | ||||
| 3 | Nazem | 15 patients with insufficient (size < 8 mm) hamstring tendons for ACL reconstruction | Hamstring tendon reinforced with PLT |
|
| 4 | Liu | 8patients with non-satisfactory HT graft (diameter < 7 mm) in ACLR | Half-PLT graft augmentation of HT (HT+1/2PLT) |
Mean diameter (HT+1/2PLT):9.6 mm (Range: 9.5–10 mm) Outcome:
|
| 5 | Angthong | 24 patients undergoing ACL reconstruction | PL autograft and endobutton fixation | Mean follow-up: 12.8 months |
| Ankle anterior drawer: Normal – 83.3 %; average pre-operative AOFAS: 100.0 ± 0.0; Mean post-operative (6 months) AOFAS: 96.0 ± 9.6 (p = 0.06); Mean pre-operative VAS-FA score:99.7 ± 1.1; Mean post-operative (13 months) VAS-FA scores:95.4 ± 12 | ||||
| At 7th month isokinetic testing: Significantly lower peak eversion and inversion torquesafter PLT harvest (p < 0.05) | ||||
| Authors DIDNOT recommend PLT as first option in ACLR due to ankle morbidity(in 1 year) | ||||
| 6 | Rudy | Biomechanical study (6 cadaveric specimens of PLT) | Compared cadaveric PLT and hamstring grafts | Tensile strength of PLT: Similar to hamstring |
| Both PLT and hamstring: Similar biomechanical properties | ||||
| P longus: Recommended as alternative donor in multiligamentous reconstruction (Not as 1st option in ACLR) | ||||
| 7 | Rhatomy | Patients undergoing single bundle ACLR (52 patients with 24 PLT grafts) | Compared PLT and hamstring grafts |
PLT vs Hamstring:8.8 ± 0.7 mm vs 8.2 ± 0.8 mm (p = 0.012); Statistically similar pre- and post-operative (at 1 year) knee scores (IKDC, modified Cincinnati Lysholm) between hamstring and PLT groups PLT group: Mean AOFAS: 97.3 ± 4.2; Mean FADI: 98 ± 3.4 Hamstring group: Significant decrease in thigh circumference (p = 0.002) Benefits of PLT graft:Large graft diameter; Minimal thigh wasting; Excellent ankle functional scores (AOFAS, FADI) |
| 8 | Wong | Biomechanical | 38 PLT prepared using 2-strand graft technique; cyclic loading | No significant difference in intrinsic material property or tendon fatigue |
| Tendon stiffness: Decreased with age | ||||
| 9 | Bi | Patients undergoing all inside anatomical single bundle ACLR | Compared reconstruction with AHPLT (62 cases) and semitendinosus grafts | Comparison between semitendinosus and AHPLT: No significant difference w.r.t IKDC score, KT 1000, Pivot shift test, VAS |
| No ankle-related complications | ||||
| Mean AOFAS score: No significant differences between semitendinosus (99.5 ± 1.21) and AHPLT (99.1 ± 1.40) | ||||
| Clinical and radiological outcome similar between the two groups | ||||
| 10 | Khajotia | 25 patients undergoing ACL repair | Triple layered PLT autograft | IKDC score:Normal −84 %, Abnormal/severely abnormal −16 % |
| Mean IKDC Score: 83.53 | ||||
| Lachman test: Normal - 72 %, 1+ laxity - 20 %, 2+ and 3+ - 4 % | ||||
| Pivot shift: Negative - 60 %, Pivot glide - 36 %, Gross pivot shift – 4 % | ||||
| Donor site morbidity: No patient had ankle dysfunction; Pressure pain – 2 patients | ||||
| 11 | Shi | Biomechanical testing 38 ACL + MCL(GradeIII) injuries |
ACL reconstruction using doubled autologous PLT or quadrupled autologous HT | Doubled PLT: Ultimate tensile strength – Comparable with quadrupled HT and significantly better than native ACL |
| PLT vs HT groups: Similar clinical/functional outcome | ||||
| PLT: No deterioration in ankle biomechanical testing after graft harvest; Suitable autograft in ACL + MCL(GradeIII) injuries | ||||
| 12 | Song | 156 single-bundle ACLR | Mean PLT graft diameter: 8.3 mm | |
| Graft diameter: Associated with duration since injury and height/weight | ||||
| <8 mm: 21 (13.5 %) patients | ||||
| 8 and 9 mm: 85 (54.5 %) patients | ||||
| ≥9 mm:50 (32.0 %) patients | ||||
| 13 | Rhatomy | 39 patients(28 males) with isolated rupture of ACL (16–45 years of age) | PLT girth:8.56 ± 0.82 | |
| PL diameter correlates significantly (p < 0.05) with height/weight/BMI (p < 0.05) | ||||
| 14 | Trung | 30 patients with combined ACL + MCL injuries | Arthroscopic ACLR with AHPLT | Mean diameter of AHPLT autograft: 7 mm |
| Pre-operative vs 6-months post-operative: Significantly improved Lysholm score (59 vs 94.27); no difference in AOFAS | ||||
| PLT: Safe autograft choice in ACLR | ||||
| 15 | Kumar | 25 patients(28 males) with isolated rupture of ACL | Preserved power of foot eversion after graft harvest | |
| IKDC score: Normal in 92 % (23 cases) | ||||
| PLT Harvest: Minimally affect gait or stability of ankle | ||||
| PLT: Satisfactory graft choice for ACLR – easier graft harvesting, satisfactory size, good cosmesis | ||||
| 16 | Rhatomy | 52 patients undergoing isolated ACLR | ACL reconstruction using HT (n = 28), versus PLT (n = 24) grafts | PL diameter: 8.8 ± 0.7 mm; Hamstring diameter: 8.2 ± 0.8 mm (significant difference: p = 0.012) |
| Similar functional outcome between PL and HT grafts (IKDC, modified Cincinnati, Lysholm) | ||||
| Mean AOFAS Score: 97.3 ± 4.2 (PLT) | ||||
| Mean FADI:98 ± 3.4 (PLT) | ||||
| Hamstring group: Significant decrease in thigh circumference (p = 0.002) | ||||
| PLT autograft: | ||||
| Comparable functional knee scores to hamstring graft at 1 year | ||||
| Benefits of PL: Less thigh wasting, excellent ankle function, excellent graft size | ||||
| 17 | Rhatomy | 31 patients undergoing ACL reconstruction(22 male); age: 27.58 ± 8.69 years | PLT autograft | Similar ankle eversion [Harvest side: 65.87 ± 7.63 N vs contralateral side: 66.96 ± 8.38 N] and 1st ray plantar flexion [Harvest side: 150.64 ± 11.67 N vs contralateral side: 152.10 ± 12.16 N] strengths |
| Ankle function: Excellent results | ||||
| Mean FADI: 99.71 ± 0.57, AOFAS: 98.71 ± 3.03 | ||||
| 18 | Sharma | 10 cases of ACL reconstruction | PLT autograft | PLT: Excellent graft for ACLR |
| Advantages: Simple harvest technique, large size, less complications (decreased thigh wasting), satisfactory ankle function (AOFAS/FADI), Comparable knee function to hamstring autografts at 1 year (Modified Cincinnati, Lysholm) | ||||
| 19 | Sakti | 20 patients undergoing primary ACL reconstruction | PLT autograft | Height, weight, true leg and shank lengths: Significantly correlated with graft diameter |
| Height, true leg length: Significantly correlated with PLT graft length | ||||
| 20 | Rhatomy | 75 patients undergoing single-bundle ACLR | PLT | PLT graft diameter: 8.38 ± 0.68 mm |
| Excellent knee (IKDC, Tegner-Lysholm and modified Cincinnati) and ankle function (mean AOFAS - 98.93 ± 3.1; mean FADI – 99.79 ± 0.59) at 2 years post-operatively | ||||
| Low complication rate: Maintained thigh girth (knee); excellent serial ankle hop | ||||
| 21 | Shao | 21 patients (mean age: 34 ± 11.2 years [mean follow-up 31.8 ± 7.7 months | Whole length, full-thickness PLT | Clinical ankle parameters: |
| AOFAS: 98.7 ± 2.5 (pre-operative) vs 98.5 ± 2.4 (post-operative); p = 0.48 | ||||
| Karlsson-Peterson (hindfoot score): 98.3 ± 2.4 (pre-operative) vs 97.9 ± 2.5 (post-operative); p = 0.162 | ||||
| Statistically similar a. Bilateral square hop (p = 0.109); b. Bilateral plantar flexion peak force (p = 0.371) | ||||
| Substantially reduced eversion peak force (p < 0.001) | ||||
| MRI: Universal PL regeneration | ||||
| Total bilateral PLT index: 82.9 ± 17.4 % [in healthy controls, 99.4 ± 4.3 %] | ||||
| Excellent foot/ankle functional outcome and PLT regenerative potential | ||||
| 22 | Kumar | 100 (80 males; age: 27.25 ± 9.11 years) patients undergoing single bundle primary ACL reconstruction | Mean diameter of PLT graft: 8.55 ± 0.73 mm | |
| Mean IKDC score: 55.77 ± 15.11 (Pre-operative); 96.12 ± 3.52 (post-operative) | ||||
| Mean Modified Cincinnati score: 66.12 ± 17.32 (pre-operative); 94.36 ± 7.21 (post-operative) | ||||
| Mean Tegner-Lysholm score: 68.45 ± 15.65 (pre-operative); 90.44 ± 8.56 (post-operative) | ||||
| 23 | Joshi | 48 non-athletic adults undergoing primary ACL reconstruction | Graft harvest time: 7.4 (ranging between 5 and 9) minutes Doubled graft thickness: 7.9 mm (ranging between 7 and 9 mm) Mean length: 29.4 ± 2.34 cm |
At 2-year followup: |
| Patient satisfaction with outcome of knee surgery: 96 % | ||||
| Patient satisfaction with status of ankle joint: 95 % | ||||
| Mean postoperative IKDC and AOFAS scores: 78.16 ± 6.23 and 98.4 ± 4.1, respectively | ||||
| Neurovascular deficit: None | ||||
| Benefits of PLT: Easier to harvest, better ultimate tensile strength, better graft size (girth and length), shorter time to harvest, minimal harvest-related morbidity; good functional outcome/stability of knee | ||||
| 24 | Vijay | 23 patients of ACL injury | Mean length of PLT graft - 8.5–9.0 cm Mean diameter - 8.5 mm PLT (vs HT) autograft – better graft size (diameter, length) |
Functional outcome of the knee (Lysholm and Modified Cincinnati scores) - Significant improvement in PLT group (p = 0.002) compared to hamstring PLT group: Ankle function (AOFAS): Reduced at 6 months; Improved at 1-year Knee flexion strength: Significantly improved |
| 25 | Goyal | Revision ACLR (10 patients) and multi-ligamentous knee injury (27 patients) | Mean length and diameter of doubled PLT: 26.2 ± 2.6 (22–31) cm; and 7.9 ± 0.68 (7.5–8.5) mm | Substantially improved 2-year knee functional scores [VAS, Lysholm and IKDC scores] |
| No significant harvest-treated morbidity or complications |
3.2.1. Surgical technique16
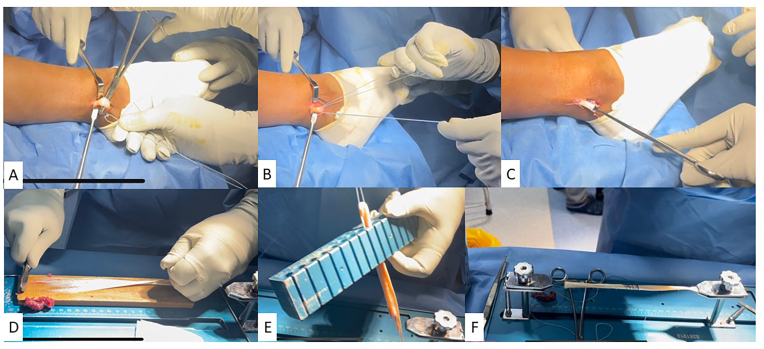
A 2 cm-long vertical incision is made along posterior lateral malleolar border. The superior peroneal retinaculum (SPR) is identified and dissected, until the posterolateral border of the tendon is clearly visualised. The peroneal tendons (longus - PL and brevis - PB) are gradually dissected out. Presence of greater proportion of muscle fibres at the level of ankle aids in distinguishing PB from PL. The P longus stump is then sutured on to P brevis using vicryl no. 1 sutures. A loop is then created on the tendon proximal to the sutured stump. The portion of tendon, which is just distal to the loop and proximal to the sutured stump, is then cut sharply. The proximal end is then released with a tendon stripper, to a length of around 4–5 cm proximally from fibular head in order to obviate any peroneal nerve injury. Tendon is dissected off the muscle; and the dimensions are measured. Graft is folded upon itself; and 2 parallel strands (“double-looped” graft) are obtained. The “double-looped” P longus grafts, thus obtained, are approximately 8–10 mm and 10–15 cm in diameter and length, respectively (Fig. 2).
Fig. 2.
Steps of graft harvest:A – Peroneus longus tendon identified; B – Loop passed around the tendon; C – Graft harvested; D & E − Graft preparation and sizing; F – Graft tensioning.
3.2.2. Half-PLT graft harvest11,13
Alternatively, half-PLT grafts have been utilised as a means to reinforce under-sized hamstring grafts. After dissecting the SPR and exposing the PLT, the graft is pulled with the help of a peon clamp and longitudinally bisected with a knife. The distal cut is performed with a pair of scissors and posterior PLT is freed. The tendon's free end is grasped with Allis clamp; and whipstitch stitches are applied. Tendon is divided along its length further proximally. A tendon stripper is employed to harvest the graft from muscular portion of P longus. The 1/2 PLT is then procured as a salvage graft; while the remaining part is left alone.
It is of utmost importance to thoroughly repair the SPR, so as to obviate any risk of peroneal tendon subluxation post-operatively.5,11,29,44 Some authors have recommended an initial zig-zag incision of the retinaculum, so as to facilitate easier repair at the end of the procedure.5
3.3. Dimensions and characteristics of the PL tendon grafts
In general, a majority of the studies have shown that PLT grafts are more consistent and reliable with regard to their dimensions, as compared to HT autografts.28, 29, 30, 31 Previous studies have demonstrated that utilising grafts of sizes larger than 8.5 cm can potentially mitigate the risk of failure.46 For every 0.5 mm graft diameter increase of up to the size of 10 mm, there is an increase in the stability rendered by the graft. Beyond the size of 10 mm, the benefit remains unclear.46
Fermin et al.46 showed that similar to HT graft, the full-thickness PLT graft is variable in its dimensions with the mean size ranging between 7 and 8.8 mm (based on technique of graft preparation). The half-PLT autografts are routinely not wider than 8.1 mm. In the recently published study by Goyal et al.,43 average diameter of a doubled PLT autotgraft was 7.9 ± 0.68 mm (range: 7.5 to 8.5). Average length of PLT graft was 26.2 ± 2.6 cm (range: 22–31). In another recent study, Vijay et al.23 concluded the mean length of PLT graft to range between 8.5 and 9 cm.
It has been shown that various anthropometric measurements can be helpful in predicting the size of PLT grafts.46 Sakti et al.36 concluded that height, weight, body mass index (BMI), leg length and shank length correlated significantly with PLT graft diameter. On the other hand, height and TLL closely correlated with PLT graft length. It has therefore been recommended that these aforementioned parameters may need to be considered pre-operatively for predicting PLT dimensions. Overall, the general consensus is that quadriceps tendon-patellar bone autografts have better reliability (than both HT and PLT) with regard to the autograft size, in view of the fact that it is a partial harvest from a large tendon, as compared to the other grafts.46
3.4. Biomechanical properties of the graft
Various biomechanical studies have evaluated the physical properties of PLT graft.2,4,14 Based on the biomechanical testing by Shi et al.,2 the ultimate strength of doubled PLT graft is significantly higher than native ACL and comparable to the quadrupled HT graft. Wong et al.14 observed that the stiffness of the tendon progressively reduces with age; and PLT grafts become slender with the advancement of age. Based on biomechanical trial by Chan et al.4 involving autografts examined in single-looped fashion in an MTS machine (MTS systems, Eden Prairie, MN), the ultimate load to failure of fascia lata (FL), tibialis anterior (TA), tibialis posterior (TP), peroneus longus (PL) and BPTB grafts were 3266 N, 3012 N, 3666 N, 3050 N and 1403 N, respectively. Based on previous studies, the strength of native ACL is reported as 2160 N47. Stiffness for the aforementioned grafts were 414 N/mm, 342 N/mm, 392 N/mm, 346 N/mm, and 224 N/mm, respectively. In this study, although the ultimate tensile strengths and stiffness between FL and BPTB grafts were substantially different, the values for the remaining graft options were statistically similar.
3.5. Outcome – clinical, functional and radiological following ACL reconstruction with PL graft
Knee outcome: Based on the published studies, there was insignificant difference in knee ligament laxity (Lachman, drawer, Pivot shift tests) scores following ACLR with PLT, as compared with the reconstruction using other autograft choices.42,44, 45, 46 There was good improvement in the post-operative laxity scores after ACLR with PLT graft (in comparison with the pre-operative status). In the review article by Dharmayuda,42 it was concluded that the post-operative Pivot shift was absent in 80.7 % in patients undergoing PLT-based ACLR.
Studies have used Tegner movement scale, Lysholm, International Knee Documentation Committee (IKDC), visual analog (VAS), and Modified Cincinnati scores to evaluate the functional knee outcome during follow-up.25,39,41, 42, 43, 44, 45, 46 Most of the studies demonstrated statistically similar outcome with regard to all these aforementioned functional knee scores among all the autograft options.27,31 Dharmayuda et al.42 showed that Lysholm and IKDC scores were satisfactory in 83.96 % and 75.82 % of patients undergoing ACLR with PLT graft. They also showed that the patients undergoing PLT had substantially higher Lysholm (p = 0.05) and IKDC scores (p = 0.00001). Sharma27 and Rhatomy28, 29, 30, 31 showed substantially mitigated thigh hypotrophy following ACLR with PLT, in comparison with HT graft. Vijay et al.23 showed substantially improved knee flexion strength (p = 0.02) following PLT graft, as compared to HT.
Kerimoglu et al.10 demonstrated normal IKDC score and Lysholm scores in 58.6 % and 41.4 % of patients undergoing ACLR with PLT graft. In another series by Zhai,47 there was no tunnel enlargement until 2 years post-operatively, following ACLR with PLT along with bone morphogenic protein (BMP) and allograft. Thus, the graft harvest is considered to be associated with relatively lower knee morbidity.
Ankle outcome: A major concern initially put forth regarding PLT harvest was the donor-site morbidity at the ankle joint. The functional outcome scores used to assess the ankle included AOFAS, Karlsson-Peterson hindfoot and FADI scores.42,44, 45, 46 In general, all the studies demonstrated that the harvest of PLT did not significantly impact the ankle function, based on the aforementioned functional scores. Nazem12 demonstrated a statistically significant difference in flexion/extension range of motion (ROM), as well as moments of the ankles in the transverse plane and forces in all three planes following harvest of PLT graft. Angthong et al.16 showed significantly lower peak torques of eversion and inversion at speeds of 60°/s and 120°/s, in comparison with the contralateral side. All the other studies demonstrated no significant impact of PLT graft harvest on the clinical and functional scores of the ankle.11,42,45,46
Shao et al.5 assessed clinical and morphological recovery following PLT harvest. They demonstrated no significant difference in American Orthopedic Foot and Ankle Society (AOFAS) hindfoot (p = 0.480) and Karlsson Peterson (p = 0.162) scores between pre-operative and post-operative time points. They also did not observe any significant difference in square hop and peak plantar flexion force (p = 0.109, 0.371, respectively) bilaterally. Harvested foot had substantially reduced peak eversion force, in comparison with other side. They also evaluated the regeneration of PLT on magnetic resonance imaging (MRI) scan. Based on their observation, they concluded that there was probable evidence of universal regeneration of peroneal tendon on MRI {as evidenced by total bilateral peroneal tendon index of 82.9 ± 17.4 %}.
Thus, based on our review, PLT harvest has been associated with acceptable foot and ankle-related outcome, as well as acceptable regenerative ability on MRI. Nevertheless, certain studies have remained circumspect regarding the validity of AOFAS or FADI clinical rating system in view of its poor construct validity. In addition, the scoring system does not review the high-level activities of the patients or include power of strength examination.48 Therefore, despite such encouraging evidence; a recent review has emphasized upon the need for additional long-term assessment of the donor site-related ankle morbidity using more validated (and objective) scoring systems such as PROMIS score.46
3.6. Complications of PL graft
Overall, studies have suggested that PLT may been associated with low knee and ankle complication rates, as compared to the other graft choices.
There still exists controversial evidence regarding the effect of graft harvest on the ankle function. The function of PLT is plantar flexion of 1st ray, as well as plantar flexion and eversion of foot. These movements are paramount during the stance phase of gait, which can be crucial in athletes.10,49 Kerimoglu et al.10 demonstrated a deficient plantar flexion of first ray and functional deteriorations in the push-off of stance phase following the harvest of PLT graft. However, in the studies by Joshi48 and Rhatomy,30 there was not reduction in mean AOFAS score at following after the harvest of PLT. Based on their observation, Joshi et al.49 concluded that PLT harvest did not affect the shape of the arch or alter the stability of foot or ankle.
In their study involving 24 patients undergoing PLT harvest with a mean 12.8-month follow-up, Angthong et al.16 demonstrated 1+ laxity on anterior drawer and varus tilt tests in 16.7 % and 4.2 % of patients, respectively. They also reported complaints including ankle stiffness, bulging of proximal stumps, sural nerve neuropraxia and inversion strain of ankle joint in 8.3 %, 20.8 %, 8.3 % and 4.2 % of patients, respectively during the initial 6 months. Based on their findings, they concluded that PLT graft had higher rate of ankle morbidities during the initial 12 months after surgery; and therefore, did not recommend it as the first option of donor graft.
Zhao11 reported no significant increase in prevalence of peroneal nerve palsy and PLT rupture or tendinopathy following PLT harvest. They also demonstrated that the gap between head of the tendon stripper and point of deep peroneal nerve bifurcation ranged between 4.6 and 10.4 cm. Numbness related to sural nerve damage is a known complication (in view of its close proximity), although it is relatively tolerated.49
Although PLT has been purported as a substitute for BPTB graft in patients at risk for anterior knee pain and kneeling difficulties; there is substantial paucity in the current literature on this subject.46 Sharma et al.27 showed that PLT graft had significantly lower knee-related complications like thigh hypotrophy and quadriceps-hamstring mismatch, as compared with HT graft.
4. Discussion
PLT autograft was initially harvested by Kerimoglu et al.10 (2008), followed by further description by Zhao et al.11(in 2012) and Rhatomy et al.28, 29, 30, 31(in 2019). It has been demonstrated that PLT represents a reasonable choice for ACLR due to its inherent strength, appropriate length and easy harvestability.23,48, 49, 50 PLT has important functions such as ankle plantar flexion, foot eversion, maintenance of pedal arch; as well as stabilization of leg over foot; and concerns have been raised about the donor-site morbidity associated with its harvest.43,45 In the current scenario, there is substantial ambiguity with regard to the exact role of PLT, as compared to the alternate graft choices in context of ACLR. The current review was thus planned to comprehensively compare the graft dimensions or characteristics, donor-site morbidity, complications, functional outcome, and survival of PLT graft with other graft choices in patients undergoing ACLR.
PLT is growingly recognized as a graft alternative among orthopedicians managing ACL injuries.46 It is considered as a suitable choice for ACLR in kneeling population, multi-ligamentous injuries [especially medial patellofemoral (MPFL) or medial collateral (MCL)injury], revision surgeries, non-athletic individualsand situations of non-availability of other graft options.50, 51, 52 Biomechanical studies have recommended 8 mm 2-strand PLT as a suitable graft option with comparable (or even superior) failure load and stiffness to 10 mm PT graft, native ACL and 4-strand HT graft.6,53
The proponents of the graft have purported relatively greater tensile strength, better graft thickness and length, shorter graft harvest time, good knee functional outcome; as well as lower donor-site morbidity as its potential benefits.46 Nevertheless, a majority of the current data is based on non-clinical studies, clinical studies with relatively shorter follow-up and less-reliable outcome evaluations (based on non-validated outcome tools).10,46
4.1. Other review articles and meta-analyses
In a recent review article by Malige et al.,44 diverse graft options like BPTB, HT, quadriceps, TA, TP, achilles tendon, PL, tensor fascia lata (TFL), and iliotibial band (ITB) which have been utilised in the reconstruction of ACL, were compared. They concluded that most of these autograft options were biomechanically superior to native ACL. Nevertheless, they recommended the need for further focused research to assess whether any of the autografts was biomechanically better than the others; and to determine if the biomechanical differences observed in in-vitro studies actually resulted in a substantial difference in the eventual clinical outcome.
The recent review articles by He45 and Dharmayuda42 concluded that PLT demonstrates similar functional outcome and graft survival as HT. He et al.45 warned against some loss of ankle function (AOFAS score) following PLT harvest. They concluded that PLT is a reasonable autograft (harvested outside knee) for ACLR, and can potentially eliminate the quadriceps-hamstring mismatch arising from grafts harvests around the knee.
To the contrary, in the review article by Fermin,46 it was concluded that although clinical- and stability-related outcome following ACLR using PLT autograft were comparable to HT graft in the short-term; the evidence to support its utility in kneeling population and those with concomitant ACL/MCL injuries (the population for whom the use of this graft has been primarily implemented) is still insufficient. On a similar note, despite extensive evidence regarding the consistent dimensions of the harvested graft, they emphasized upon the need for further assessment of the donor-graft ankle morbidity with validated tools and objective score, prior to implementing this graft as the primary choice of autograft.
5. Limitations
Our current review has various limitations inherent to all non-systematic reviews. There was no definitive strategy utilised to assess the methodological quality of the included studies. The sample size of a majority of reviewed studies was small. Three different types of PLT grafts (full-thickness, anterior half and posterior half) have been employed; and the graft has been employed for diverse indications (primary isolated ACLR, ACLR in the setting of multi-ligamentous injuries and revision ACLR). Nevertheless, our comprehensive review lucidly summarises our understanding on this subject hitherto.
6. Conclusion
PLT is a suitable autograft for ACLR. The dimensions (diameter and length) of the harvested PLT graft are relatively more consistent than HT. It has similar functional outcome and survival rates, as compared to the other autograft choices. It also has lower risk for donor-site morbidity and lower complication rates than HT grafts. However, a majority of the available data is based on non-clinical studies, clinical studies with relatively shorter follow-up and less-reliable outcome evaluations; and the importance of larger clinical trials with longer follow-up utilising validated outcome measures for clearly determining its role in ACLR cannot be understated.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Consent to participate and publish
Not applicable.
Ethical statement
Not applicable (Narrative review).
CRediT authorship contribution statement
Vibhu Krishnan Viswanathan: Methodology, Formal analysis, and, Investigation, Writing – original draft, preparation. Karthikeyan. P. Iyengar: Conceptualization, Methodology, Writing – review & editing. Vijay Kumar Jain: Conceptualization, Methodology, Writing – review & editing, Resources, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
Contributor Information
Vibhu Krishnan Viswanathan, Email: drvibu007@gmail.com.
Karthikeyan. P. Iyengar, Email: kartikp31@hotmail.com.
Vijay Kumar Jain, Email: drvijayortho@gmail.com.
References
- 1.Claes S., Verdonk P., Forsyth R., Bellemans J. The “ligamentization” process in anterior cruciate ligament reconstruction: what happens to the human graft? A systematic review of the literature. Am J Sports Med. 2011;39(11):2476–2483. doi: 10.1177/0363546511402662. [DOI] [PubMed] [Google Scholar]
- 2.Shi F.D., Hess D.E., Zuo J.Z., et al. Peroneus longus tendon autograft is a safe and effective alternative for anterior cruciate ligament reconstruction. J Knee Surg. 2019;32(8):804–811. doi: 10.1055/s-0038-1669951. [DOI] [PubMed] [Google Scholar]
- 3.Paschos N.K., Howell S.M. Anterior cruciate ligament reconstruction: principles of treatment. EFORT Open Rev. 2016;1(11):398–408. doi: 10.1302/2058-5241.1.160032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan D.B., Temple H.T., Latta L.L., Mahure S., Dennis J., Kaplan L.D. A biomechanical comparison of fan-folded, single-looped fascia lata with other graft tissues as a suitable substitute for anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(12):1641–1647. doi: 10.1016/j.arthro.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Shao X., Shi L.L., Bluman E.M., et al. Satisfactory functional and MRI outcomes at the foot and ankle following harvesting of full thickness peroneus longus tendon graft. Bone Joint Lett J. 2020;102-B(2):205–211. doi: 10.1302/0301-620X.102B2.BJJ-2019-0949.R1. [DOI] [PubMed] [Google Scholar]
- 6.Pearsall A.W., Hollis J.M., Russell G.V., Scheer Z. A biomechanical comparison of three lower extremity tendons for ligamentous reconstruction about the knee. Arthroscopy. 2003;19(10):1091–1096. doi: 10.1016/j.arthro.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Frank R.M., Hamamoto J.T., Bernardoni E., et al. ACL reconstruction basics: quadruple (4-strand) hamstring autograft harvest. Arthrosc Tech. 2017;6(4):e1309–e1313. doi: 10.1016/j.eats.2017.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta R., Bahadur R., Malhotra A., Masih G.D., Gupta P. Anterior cruciate ligament reconstruction using hamstring tendon autograft with preserved insertions. Arthrosc Tech. 2016;5(2):e269–e274. doi: 10.1016/j.eats.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGee R., Daggett M., Jacks A., Hoang V., Theobald H.A. Patellar tendon graft anterior cruciate ligament reconstruction technique with suture tape augmentation. Arthrosc Tech. 2019;8(4):e355–e361. doi: 10.1016/j.eats.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kerimoğlu S., Koşucu P., Livaoğlu M., Yükünç I., Turhan A.U. Magnetic resonance imagination of the peroneus longus tendon after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17(1):35–39. doi: 10.1007/s00167-008-0626-7. [DOI] [PubMed] [Google Scholar]
- 11.Zhao J., Huangfu X. The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med. 2012;40(3):662–671. doi: 10.1177/0363546511428782. [DOI] [PubMed] [Google Scholar]
- 12.Nazem K., Barzegar M., Hosseini A., Karimi M. Can we use peroneus longus in addition to hamstring tendons for anterior cruciate ligament reconstruction? Adv Biomed Res. 2014;3:115. doi: 10.4103/2277-9175.132696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu C.T., Lu Y.C., Huang C.H. Half-peroneus-longus-tendon graft augmentation for unqualified hamstring tendon graft of anterior cruciate ligament reconstruction. J Orthop Sci. 2015;20(5):854–860. doi: 10.1007/s00776-015-0744-2. [DOI] [PubMed] [Google Scholar]
- 14.Wong A.K., Calvo M.R., Schaffler B.C., et al. Biomechanical and geometric characterization of peroneus longus allografts with respect to age. Clin Biomech. 2019;67:90–95. doi: 10.1016/j.clinbiomech.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 15.Bi M., Zhao C., Zhang S., Yao B., Hong Z., Bi Q. All-inside single-bundle reconstruction of the anterior cruciate ligament with the anterior half of the peroneus longus tendon compared to the semitendinosus tendon: a two-year follow-up study. J Knee Surg. 2018;31(10):1022–1030. doi: 10.1055/s-0038-1627466. [DOI] [PubMed] [Google Scholar]
- 16.Angthong C., Chernchujit B., Apivatgaroon A., Chaijenkit K., Nualon P., Suchao-in K. The anterior cruciate ligament reconstruction with the peroneus longus tendon: a biomechanical and clinical evaluation of the donor ankle morbidity. J Med Assoc Thai. 2015;98(6):555–560. [PubMed] [Google Scholar]
- 17.Aglietti P., Buzzi R., Zaccherotti G., De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22(2):211–217. doi: 10.1177/036354659402200210. discussion 217-218. [DOI] [PubMed] [Google Scholar]
- 18.Marques F. da S., Barbosa P.H.B., Alves P.R., et al. Anterior knee pain after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2020;8(10) doi: 10.1177/2325967120961082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Christen B., Jakob R.P. Fractures associated with patellar ligament grafts in cruciate ligament surgery. J Bone Joint Surg Br. 1992;74(4):617–619. doi: 10.1302/0301-620X.74B4.1624526. [DOI] [PubMed] [Google Scholar]
- 20.Khajotia B.L., Chauhan S., Sethia R., Chopra B.L. Functional outcome of arthroscopic reconstruction of anterior cruciate ligament tear using peroneus longus tendon autograft. International Journal of Research in Orthopaedics. 2018;4(6):898–903. doi: 10.18203/issn.2455-4510.IntJResOrthop20184382. [DOI] [Google Scholar]
- 21.Song X., Li Q., Wu Z., Xu Q., Chen D., Jiang Q. Predicting the graft diameter of the peroneus longus tendon for anterior cruciate ligament reconstruction. Medicine (Baltim) 2018;97(44) doi: 10.1097/MD.0000000000012672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adachi N., Ochi M., Uchio Y., Sakai Y., Kuriwaka M., Fujihara A. Harvesting hamstring tendons for ACL reconstruction influences postoperative hamstring muscle performance. Arch Orthop Trauma Surg. 2003;123(9):460–465. doi: 10.1007/s00402-003-0572-2. [DOI] [PubMed] [Google Scholar]
- 23.Vijay C., Santosh M.S., Avinash C., Adarsh T. Is Peroneus longus autograft a better alternative to the Hamstring autograft for anterior cruciate ligament reconstruction? – a randomised control study. Journal of Orthopaedics, Trauma and Rehabilitation. 2022;29(1) doi: 10.1177/22104917221088335. [DOI] [Google Scholar]
- 24.Rose T., Hepp P., Venus J., Stockmar C., Josten C., Lill H. Prospective randomized clinical comparison of femoral transfixation versus bioscrew fixation in hamstring tendon ACL reconstruction--a preliminary report. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):730–738. doi: 10.1007/s00167-006-0034-9. [DOI] [PubMed] [Google Scholar]
- 25.Trung D.T., Manh S.L., Thanh L.N., Dinh T.C., Dinh T.C. Preliminary result of arthroscopic anterior cruciate ligament reconstruction using anterior half of peroneus longus tendon autograft. Open Access Maced J Med Sci. 2019;7(24):4351–4356. doi: 10.3889/oamjms.2019.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kv K., Ns K., Vr B. A study on peroneus longus autograft for anterior cruciate ligament reconstruction. International Journal of Research in Medical Sciences. 2020;8(1):183–188. doi: 10.18203/2320-6012.ijrms20195904. [DOI] [Google Scholar]
- 27.Sharma D., Agarwal A., Shah K., Shah R., Shah H. Peroneus longus: most promising autograft for arthroscopic ACL reconstruction. Indian J Orthop Surg. 2019;5(3):172–175. doi: 10.18231/j.ijos.2019.033. [DOI] [Google Scholar]
- 28.Rhatomy S., Wicaksono F.H., Soekarno N.R., Setyawan R., Primasara S., Budhiparama N.C. Eversion and first ray plantarflexion muscle strength in anterior cruciate ligament reconstruction using a peroneus longus tendon graft. Orthop J Sports Med. 2019;7(9) doi: 10.1177/2325967119872462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rhatomy S., Tanzil H., Setyawan R., et al. Influence of anthropometric features on peroneus longus graft diameter in Anterior Cruciate Ligament reconstruction: a cohort study. Ann Med Surg (Lond) 2019;48:77–80. doi: 10.1016/j.amsu.2019.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rhatomy S., Asikin A.I.Z., Wardani A.E., Rukmoyo T., Lumban-Gaol I., Budhiparama N.C. Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3552–3559. doi: 10.1007/s00167-019-05455-w. [DOI] [PubMed] [Google Scholar]
- 31.Rhatomy S., Hartoko L., Setyawan R., et al. Single bundle ACL reconstruction with peroneus longus tendon graft: 2-years follow-up. J Clin Orthop Trauma. 2020;11(Suppl 3):S332–S336. doi: 10.1016/j.jcot.2019.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Papastergiou S.G., Konstantinidis G.A., Natsis K., Papathanasiou E., Koukoulias N., Papadopoulos A.G. Adequacy of semitendinosus tendon alone for anterior cruciate ligament reconstruction graft and prediction of hamstring graft size by evaluating simple anthropometric parameters. Anat Res Int. 2012;2012 doi: 10.1155/2012/424158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conte E.J., Hyatt A.E., Gatt C.J., Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30(7):882–890. doi: 10.1016/j.arthro.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 34.Treme G., Diduch D.R., Billante M.J., Miller M.D., Hart J.M. Hamstring graft size prediction: a prospective clinical evaluation. Am J Sports Med. 2008;36(11):2204–2209. doi: 10.1177/0363546508319901. [DOI] [PubMed] [Google Scholar]
- 35.Fulkerson J.P., Langeland R. An alternative cruciate reconstruction graft: the central quadriceps tendon. Arthroscopy. 1995;11(2):252–254. doi: 10.1016/0749-8063(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 36.Sakti M., Biakto K.T., Usman M.A., Tedjajuwana M.J., Pasallo P., Subagio E.S. Predicting the peroneus longus tendon autograft size in ACL reconstruction by using anthropometric parameters: a study in South Sulawesi population. J Orthop. 2020;22:1–4. doi: 10.1016/j.jor.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jost P.W., Dy C.J., Robertson C.M., Kelly A.M. Allograft use in anterior cruciate ligament reconstruction. HSS J. 2011;7(3):251–256. doi: 10.1007/s11420-011-9212-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shelton W.R., Treacy S.H., Dukes A.D., Bomboy A.L. Use of allografts in knee reconstruction: I. Basic science aspects and current status. J Am Acad Orthop Surg. 1998;6(3):165–168. doi: 10.5435/00124635-199805000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Vangsness C.T., Garcia I.A., Mills C.R., Kainer M.A., Roberts M.R., Moore T.M. Allograft transplantation in the knee: tissue regulation, procurement, processing, and sterilization. Am J Sports Med. 2003;31(3):474–481. doi: 10.1177/03635465030310032701. [DOI] [PubMed] [Google Scholar]
- 40.Keyhani S., Qoreishi M., Mousavi M., Ronaghi H., Soleymanha M. Peroneus longus tendon autograft versus hamstring tendon autograft in anterior cruciate ligament reconstruction: a comparative study with a mean follow-up of two years. Arch Bone Jt Surg. 2022;10(8):695–701. doi: 10.22038/ABJS.2022.59568.2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Faisal M.A., Chowdhury A.Z., Kundu I.K., et al. Evaluation of the clinical outcome of arthroscopic posterior cruciate ligament reconstruction with peroneus longus tendon. International Journal of Nursing and Health Care Research. 2022 https://www.gavinpublishers.com/article/view/evaluation-of-the-clinical-outcome-of-arthroscopic-posterior-cruciate-ligament-reconstruction-with-peroneus-longus-tendon Published online July 11. [Google Scholar]
- 42.Dharmayuda C.G.O., Deriano B. Comparison of clinical outcome between peroneus longus tendon auto graft versus hamstring tendon auto graft for anterior cruciate ligament reconstruction, which one is better?: a systematic review and meta-analysis. Int J Health Sci Res. 2022;12(5):158–169. doi: 10.52403/ijhsr.20220519. [DOI] [Google Scholar]
- 43.Goyal T., Paul S., Choudhury A.K., Sethy S.S. Full-thickness peroneus longus tendon autograft for anterior cruciate reconstruction in multi-ligament injury and revision cases: outcomes and donor site morbidity. Eur J Orthop Surg Traumatol. 2023;33(1):21–27. doi: 10.1007/s00590-021-03145-3. [DOI] [PubMed] [Google Scholar]
- 44.Malige A., Baghdadi S., Hast M.W., Schmidt E.C., Shea K.G., Ganley T.J. Biomechanical properties of common graft choices for anterior cruciate ligament reconstruction: a systematic review. Clin Biomech. 2022;95 doi: 10.1016/j.clinbiomech.2022.105636. [DOI] [PubMed] [Google Scholar]
- 45.He J., Tang Q., Ernst S., et al. Peroneus longus tendon autograft has functional outcomes comparable to hamstring tendon autograft for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2021;29(9):2869–2879. doi: 10.1007/s00167-020-06279-9. [DOI] [PubMed] [Google Scholar]
- 46.Marín Fermín T., Hovsepian J.M., Symeonidis P.D., Terzidis I., Papakostas E.T. Insufficient evidence to support peroneus longus tendon over other autografts for primary anterior cruciate ligament reconstruction: a systematic review. J ISAKOS. 2021;6(3):161–169. doi: 10.1136/jisakos-2020-000501. [DOI] [PubMed] [Google Scholar]
- 47.Zhai W.L., Li D., Lian K.J. [Tunnel enlargement after anterior cruciate ligament reconstruction with peroneus longus muscle combined with BMP and allogeneic bone] Zhong Guo Gu Shang. 2010;23(6):414–416. [PubMed] [Google Scholar]
- 48.SooHoo N.F., Shuler M., Fleming L.L. American orthopaedic foot and ankle society. Evaluation of the validity of the AOFAS clinical rating systems by correlation to the SF-36. Foot Ankle Int. 2003;24(1):50–55. doi: 10.1177/107110070302400108. [DOI] [PubMed] [Google Scholar]
- 49.Joshi S., Shetty U.C., Salim M.D., Meena N., Kumar R.S., Rao V.K.V. Peroneus longus tendon autograft for anterior cruciate ligament reconstruction: a safe and effective alternative in nonathletic patients. Niger J Surg. 2021;27(1):42–47. doi: 10.4103/njs.NJS_22_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gautam D.A., Kumar D.R., Singh D.B. Single bundle ACL reconstruction with peroneus longus tendon autograft: a short-term study. European Journal of Molecular & Clinical Medicine. 2021;7(11):5460–5466. [Google Scholar]
- 51.Wu C., Xie G., Jin W., Ren Z., Xue J., Yang K. [Arthroscopic GraftLink technique reconstruction combined with suture anchor fixation for anterior cruciate ligament and medial collateral ligament injuries] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33(6):685–688. doi: 10.7507/1002-1892.201812062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xu C., Zhao J., Xie G. Medial patella-femoral ligament reconstruction using the anterior half of the peroneus longus tendon as a combined procedure for recurrent patellar instability. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2016;4:21–26. doi: 10.1016/j.asmart.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Noyes F.R., Butler D.L., Grood E.S., Zernicke R.F., Hefzy M.S. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am. 1984;66(3):344–352. [PubMed] [Google Scholar]