Abstract
Depression is considered to be an “emotional disease” in ancient books of traditional Chinese medicine. Its clinical features are similar to those of “Lily disease” in the ancient Chinese medicine book Synopsis of the Golden Chamber written by Zhang Zhongjing in the Han Dynasty. Baihe Zhimu (Lilium lancifolium bulb and Anemarrhena asphodeloides rhizome) decoction (LBRAD) is the first prescription of “Lily Disease” in this book. It is also a special remedy for “Lily disease” after sweating. The classic recipe LBRAD consists of two herbs, fresh lily bulbs and dried Rhizoma Anemarrhena slice. It has the effect of supplementing nutrition and clearing heat, nourishing Yin and moistening. After more than two thousand years of clinical practice, it has been currently widely used in clinical treatment of depression. In this paper, the relationship between LBRAD and depression was systematically reviewed from both clinical and experimental studies, as well as the preparation, the clinical application, the pharmacological mechanism and the effective material basis for the treating depression of LBRAD. The core targets and biological processes of the depression treatment were explored through network pharmacological analysis, so as to speculate its potential mechanism. Finally, the association between LBRAD and post-COVID-19 depression was discussed. We concluded with a summary and future prospects. This review may provide a theoretical basis for the expansion of the clinical application of LBRAD and the development of new drugs for the treatment of depression, as well as new ideas for the secondary development of classical prescriptions.
Keywords: Depression, Baihe Zhimu decoction, Clinical application, Pharmacodynamic mechanism, Effective material basis
Graphical abstract
Highlights
-
•
LBRAD is traditionally valued for the treatment of pulmonary disease and emotional disease in traditional Chinese medicine.
-
•
The components of LBRAD may account for its medicinal properties.
-
•
LBRAD has the potential to be used as a safely, effectively and sustainably antidepressant to achieve a homeostatic state of multi-system functions in depression.
-
•
There are further unknown molecular mechanisms and targets playing an important role in potential antidepressant effect waiting for us to explore for LBRAD.
1. Introduction
Depression is a common affective disorder caused by multiple factors and is characterized by significant and persistent low mood, loss of interest and pleasure, retardation of thinking, cognitive impairment, decreased volitional activity, social anxiety, decreased sense of self-worth and physical Disorder symptoms as the main clinical manifestation [1,2]. According to the statistics of the World Health Organization in 2017, the global incidence rate of depression is about 4.4 %, and the lifetime prevalence rate is about 16.7 %, accounting for 10 % of the global total burden of non-fatal diseases, and the trend is rising year by year [3,4]. Depression is a high-risk factor for suicide, causing nearly 800,000 self-inflicted deaths worldwide each year, making it the second leading killer of human health after cancer, and taking a greater toll on disability globally than any other condition [5]. The rising numbers are likely to make matters worse. Therefore, depression seriously affects the quality of life of patients, brings great economic burden to families and society, and is considered one of the major public health problems [6].
Depression is a heterogeneous disorder with a complex etiology whose pathogenesis is not fully understood and may be influenced by a variety of factors such as genetic, psychological, biochemical, and social-environmental factors, leading to the formation of different pathogenesis hypotheses. When depression occurs, the body is mostly in an inflammatory state, and inflammatory factors will cause the disorder of neuro-endocrine-immune system. At the same time, the hyperfunction of the hypothalamo-pituitary-adrenal (HPA) axis occurs, and the imbalance of the endocrine immune network hub under the control is aggravated [7]. Among them, the decreased level of monoamine neurotransmitters (such as serotonin, norepinephrine and dopamine) in the central nervous system and the decreased expression of monoamine neurotransmitter receptors in the hippocampus may lead to the occurrence of a depression. Moreover, insulin resistance and the decreased diversity and abundance of intestinal flora may lead to the decreased function of brain-derived neurotrophic factor (BDNF). The dysfunction of BDNF metabolic regulatory factors and related signaling pathways ultimately resulted in impaired neural plasticity, reduced neuron regeneration and increased apoptosis [8]. In this process, the disturbance of kynurenine pathway (KP) causes abnormal amino acid metabolism, excitatory amino acid (glutamic acid) level is too high, inhibitory amino acid level (gamma-aminobutyric acid) is reduced, and eventually the neurons calcium overload and degenerative death [3,9]. Unfortunately, many mechanism hypotheses do not fully illuminate the puzzling process of depression, so there is no consensus on drugs to treat depression. Currently, the first-line clinical treatment of depression is dominated by antidepressants guided by the monoamine neurotransmitter theory. Although these drugs have achieved some therapeutic effects, the effect was delayed, with only 70 % of patients have a good effect [10]. In addition, drug-induced tolerance increases in single-target treatment modalities, leaving many residual symptoms and dysfunction, and therefore clinical efficacy is not ideal (Fig. 1). With the development of non-invasive technology, Transcranial stimulation by either magnetic (transcranial magnetic stimulation: TMS), electrical methods (transcranial electrical stimulation: tES), or transcranial ultrasound stimulation (TUS) allow for the induction of similar neuroplastic alterations, which are a young neuromodulation technology, but are still experimental, there is insufficient evidence to assess the clinical risks [11]. Consequently, it has become a challenge for clinical and scientific researchers to find and develop more methods to treat depression with high targeting, strong safety and few side effects. Under the guidance of the syndrome differentiation and treatment, TCM compounds, with their characteristics of multiple components, multiple pathways, multiple effects and the overall regulation, emphasize the integration of multiple biological systems in the human body, which is fully compatible with the nature of diseases caused by body complexity and can treat multiple pathological aspects of depression, with unique advantages and good prospects for prevention and treatment.
Fig. 1.
The etiology of depression and the current clinical antidepressants and their pharmacological mechanism.
Traditional Chinese medicine (TCM) is an Oriental traditional medicine based on the concept of holistic view. As the main medical method used in ancient China, it has accumulated rich practical experience in the development history of China for thousands of years. In recent years, with the development of high-quality formula in Chinese medicine. In fact, although the potential pharmacological mechanisms of some TCM prescriptions have not been fully elucidated, their therapeutic advantages of the multi-pathway, the strong potency and the low toxicity have been widely used in the treatment of a depression [[11], [12], [13]]. These traditional herbal formulations are considered a new source of potential new antidepressant drug development. Lilium lancifolium Bulb and Anemarrhena asphodeloides rhizome Decoction (LBRAD), composed of Lilium lancifolium bulb and Anemarrhena asphodeloides rhizome, is a classical herbal formula for treating emotional disease in Golden Chamber. LBRAD has the functions of replenishing deficiency, clearing heat, nourishing Yin and moistening dryness, and regulating mood. At present, it has become a classical Chinese medicine prescription for the treatment of depression, anxiety, sleep disorders and the other mental and neurological diseases. However, the effective material foundation and underlying mechanism of its treatment of depression are not fully understood.
The emergence and development of TCM classical famous prescriptions have condensed the clinical practice experience of doctors of all dynasties. Up to now, classical famous prescriptions have been endowed with new conceptual connotation and mission of The Times. With the establishment of the Law of the People's Republic of China on Traditional Chinese Medicine and the whole process policy system of the research and development registration of classical famous prescription compound preparations, the research and development of classical famous prescriptions is moving towards the direction of innovation requirements. The research and development of compound preparations derived from classical famous prescriptions has become one of the breakthroughs in the inheritance and innovation of traditional Chinese medicine in the new era. LBRAD was listed as one of the ancient prescriptions in order to promote the process of simplified registration and clinical application of traditional Chinese medicine compound preparations. In October 2020, the issuance of the Key Information Research Principles of Ancient Classical Famous Recipes and the Key Information Research Principles of Ancient Classical Famous Recipes (7 Prescriptions) has played the guiding and exemplary role in the key information research of classical famous recipes. Under the guidance of the general rules for the research of key information, the research rules for the basis, the processing, the dosage and the preparation of traditional Chinese medicine were formulated [14]. Therefore, the author consulted the literature in the past 20 years to summarized the preparation, the clinical application, the modern pharmacological mechanism, the effective substance basis and the other aspects of LBRAD standard decoction, so as to provide modern scientific basis for studying the efficacy and mechanism of LBRAD standard decoction in treating depression, the formulation of dispatching drugs, the registration of Chinese traditional medicine compound preparations, and the improvement of clinical applicability.
2. Depression and lily disease
Although there is no record of the name of depression in TCM, there is a long history of knowledge of disorders that resemble the clinical symptoms of depression. The manifestation of depression can be found in the symptom group of “depressive syndrome”, “epilepsy syndrome”, “lily disease”, “dirty and manic”, “insomnia” and other TCM diseases, belonging to the category of “emotional disease”, the relevant discussion can be seen in ancient books. As early as the Spring and Autumn Period, “loss of ambition” was recorded in Zuo Zhuan · Zhao AD, and the Warring States period Guiguzi first proposed “loss of ambition”, implying would be evident in the earliest typical manifestation of will, just depression, slow thinking, would decline [15]. In the Huangdi Neijing of the early Western Han Dynasty, the descriptive records of “depression”, “Qi knot”, “epilepsy” and “running dolphin” were all similar to the symptoms of depression. According to the theory of Qi and five elements, the etiology and pathogenesis of excessive emotions were proposed, the treatment of the five qi depression was expounded, and the earliest emotional therapy was proposed from the method of emotion combining with emotion. The emotional changes of “anger, sadness, apprehension, and fear” were used to alleviate abnormal mental depression symptoms [16]. In addition, the herbs recorded in Shennong Materia Medica such as “Hyacuria”, “Polygonia” and “jujube kernel” can regulate mood and restore the body function, which is suitable for the medication of depression symptoms. Through long-term practical experience, the ancients also used acupuncture points such as Taichong, the Sun and Baihui for the purpose of regulating the body and stabilizing the mind [17].
At the end of the Eastern Han Dynasty, “Shaoyang Syndrome” and “irritability” were recorded in Treatise on Cold Injuries, and “Lily disease”, “manic viscera” and “running dolphin” were described in Synopsis of the Golden Chamber. The characteristics of these diseases and symptoms were very similar to the manifestations of emotional disorders of depression [18]. Among them, “Lily disease” first appeared in the Golden Chamber · Lily Fox Confused Yin and Yang Toxic Disease Pulse Syndrome and Treatment, “Lily disease, one hundred pulse, known to cause the disease”, detailed discussion of the etiology, the pathogenesis and the main manifestations of the disease, the main characteristics of the disease are trance, nervous, silent, uncertain diet, movement disorders, sensory disorders, bitter mouth and red urine, little red tongue body and tongue coating, pulse fine and spirit and the number of different symptoms. The main symptoms of lily disease share many similarities with the mental state of depression, sleep eating, speech act, and perceptual disturbances [19]. In the Qing Dynasty, the Medical Emperor Jin Jian believed that lily disease was caused by delayed treatment of external sensations, mistreatment or excessive thinking, emotional paralysis, and disturbance of all emotions, which was also consistent with the research of modern etiology on depression induced by negative emotional experience [20]. In general, lily disease is residual heat injury Yin, or due to emotional disorders caused by fire Yin deficiency of the heart and lung, gradually internal heat, 100 pulse disharmony, brain loss, all the symptoms are born. There is more overlap with depression in terms of etiology, pathogenesis and symptoms. Yin deficiency (Fig. 2) causes internal heat (cardiopulmonary) and leads to vascular abnormalities, further affecting central nervous function abnormalities, which can be used as the pathophysiological explanation of “Lily disease".
Fig. 2.
Etiology and pathogenesis of lily disease. LBRAD treated lily disease by nourishing Yin and clearing heat, focusing on treating both symptoms and the root causes and dual modulation.
The unique concept of treating “lily disease” in traditional Chinese medicine pays particular attention to the holistic concept and treatment based on syndrome differentiation. It adopts the principle of harmony between form and spirit to achieve the homeostasis of the body, the state of harmony between Yin and Yang and form and spirit. According to the Synopsis of the Golden Chamber, Zhong Jing created 7 prescriptions for internal and external use of detergent to treat “lily disease” and “lily lesion syndrome”. Among them, LBRAD is a special treatment for “lily disease” after sweating [21]. The classical prescription LBRAD is composed of fresh Lilium lancifolium bulbs and dried Anemarrhena asphodeloides rhizome. According to the performance theory of traditional Chinese medicine, Lilium lancifolium bulb is considered to be cold and sweet, and can be attributed to the heart and lung channels. Lilium lancifolium bulbs are known to nourish Yin, nourish the lungs, clear the heart, soothe coughs, reduce irritability, and calm the mind. The function of Lilium lancifolium bulb nourishing Yin is to prevent the inner heat of the heart and lung Yin deficiency of lily disease. Anemarrhena asphodeloides rhizome colds and bitters taste, mostly in the lung, stomach, kidney three viscera obvious effect, with heat purging fire, nourishing Yin moistening dryness effect, can be used for lily disease after sweating error treatment, deficiency heat aggravation, upset thirst syndrome, and Lilium lancifolium bulb line Yin effect. The combination of the two drugs provided the greatest modulation of symptoms such as depressed mood, insomnia, sleep disturbance, irritability and disordered eating behavior [22]. These symptoms are closely related to the clinical features of patients with depression. Therefore, LBRAD has significant antidepressant effect and LBRAD has unique advantages and potential application prospects in the treatment of affective disorder depression [23].
3. Traditional uses
Prescribed as bitter, sweet, and cold, and to the heart, lung, stomach and kidney meridian after action, LBRAD has the effects of replenishing deficiency, clearing heat, nourishing Yin and moistening dryness, and regulating mood, contributing to the treatment of Lily disease, depression, sleep disorders, climacteric syndrome, long-term low fever, breast disease, andrology disease, bronchial asthma, neurasthenia and oral ulcer [24]. The recommended dosage described for oral administration in the Chinese Pharmacopeia (2020 Edition) is 6–12 g/day for two kinds of herbal medicine [25]. LBRAD has traditionally been used in the treatment of emotional disease. Two clinical randomized control studies indicated that LBRAD may effectively relieve symptoms of depression and anxiety, reduce somatization symptom scores, and improve quality of life compared with the western treatment group [26,27]. However, the complexity of depression symptoms and the uncertainty of diagnosis often rely on quantitative indicators to objectively assess the extent of the disease. Common somatization symptoms include sleep disorders, long-term staged low fever, irritability, breast disease, and andrological diseases. Two case reports reported that LBRAD addition and subtraction may significantly improve sleep disorders in syndrome of yin deficiency and fire, with the total effective rate higher than 90 % [28,29]. For patients with depression, anxiety, and irritability, two randomized, controlled, and parallel clinical trials confirmed that the LBRAD combined with other TCM prescriptions improved symptoms more significantly than Western medicine alone, and the effective rate was higher [30,31]. Clinical findings showed that LBRAD combined with Xiao Chaihu decoction was used to treat 20 cases of long-term low fever, and the recovery rate was 100 % after 1 to 5 consecutive weeks, and one case had no recurrence after three years of follow-up, and the effect was better 2 h before the onset of medication [32]. LBRAD acts a lifesaver for breast diseases by relieving anxiety, irritability, irritability and other symptoms [33]. According to the theory of syndrome differentiation and treatment, andrology disease with yin deficiency, fire hyperactivity syndrome, LBRAD has a palliative effect by nourishing Yin and clearing heat, such as prostate disease, impotence and premature ejaculation [34] (Table 1).
Table 1.
LBRAD treatment clinical trials/case reports in somatization symptoms of depression.
| Study | Subjects | LBRAD administration | Results |
|---|---|---|---|
| Zhao., 2017 [26] | 68 patients with depression and anxiety | Group 1: Treated with Delexin, take 1 tablet once a day in the morning and noon for 8 weeks. Group 2: LBRAD(30 g lily bulbs; 10 g Anemarrhena) and Ganmai Dazao decoction were taken once a day in 2 divided doses for 8 weeks. |
The total effective rate of treatment: Group 2(97.06 %) was higher than Group 1(73.53 %); Group 2 vs Group 1(X2 = 7.503, P = 0.006); Overall scores of HAMD after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.05); The incidence of adverse reactions between the two groups during treatment(X2 = 7.503, P = 0.006), The incidence of adverse reactions in Group 2 was lower than that in Group 1. |
| Feng et al., 2020 [27] | 105 patients with depression and anxiety | Group 1: Fluoxetine hydrochloride capsules (produced by Eli Lilly Suzhou Pharmaceutical Co., Ltd., national drug approval number J20170022), taken orally in the morning, 1 capsule/d, for a total of 8 weeks of treatment. Group 2: The same administration method as group 1; LBRAD(30 g lily bulbs; 10 g Anemarrhena) and Ganmai Dazao decoction were taken once a day in 2 divided doses for 8 weeks, and psychotherapy. |
The total effective rate of treatment: Group 2(92.73 %) was higher than Group 1(74.00 %); Group 2 vs Group 1(P < 0.05); Overall scores of QOL-BREF after the intervention: Group 2 was higher than Group 1; Group 2 vs Group 1(P < 0.05); Overall scores of HAMD after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.05); The incidence of adverse reactions between the two groups during treatment(X2 = 8.376, P < 0.05), The incidence of adverse reactions in Group 2 was lower than that in Group 1. |
| Zhu and Zhang., 2000 [28] | 46 patients with depression and sleep disorders | LBRAD(50 g lily bulbs; 15 g Anemarrhena) addition and subtraction, prepared 500 ml, taken 200 ml after dinner, and taken another 300 ml before going to bed every night, for 10 consecutive days of treatment. | 24 cases were cured, 18 cases were effective, and 4 cases were ineffective. The total effective rate was 91.30 %. |
| Fang., 2012 [29] | 52 patients with depression and sleep disorders | LBRAD(30 g lily bulbs; 10 g Anemarrhena) addition and subtraction, was taken once a day in 2 divided doses for 10 consecutive days. | 45 cases were cured, 6 cases were markedly effective, and 1 case was ineffective. The total effective rate was 98.08 %. |
| Liu., 2018 [30] | 130 patients with depression and irritability | Group 1: Oral estazolam tablets (Beijing Shuanghe Pharmaceutical Co., Ltd., national drug approval number: H11020744), 1–2 mg each time, once a day, for 1 month. Group 2: LBRAD(30 g lily bulbs; 10 g Anemarrhena) addition and subtraction, was taken once a day in 2 divided doses for 1 month. |
The total effective rate of treatment: Group 2(90.77 %) was higher than Group 1(56.92 %); Group 2 vs Group 1(X2 = 19.277, P < 0.05); Overall scores of SAS, SDS, and PSQI after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.05). |
| Chen and Ding., 2012 [31] | 80 patients with depression and irritability | Group 1: Oral fluoxetine hydrochloride capsules (produced by Eli Lilly and Company of the United States, national drug approval number J20080016, capsule, 20 mg/capsule), 20 mg per day, taken with a meal in the morning, for 8 weeks. Group 2: LBRAD(30 g lily bulbs; 15 g Anemarrhena) and Longgu Muli decoction were taken once a day in 2 divided doses for 8 weeks. |
The total effective rate of treatment: Group 2(92.5 %) was higher than Group 1(87.5 %); Group 2 vs Group 1(P < 0.05); |
| Gao and Liu., 2006 [33] | 1 patient with depression and breast hyperplasia | LBRAD(30 g lily bulbs; 12 g Anemarrhena) addition and subtraction, was taken once a day in 2 divided doses for 3 consecutive months. | Overall treatment rate 100 % |
| Zhang et al., 2021 [34] | Case 1: 1 patient with depression and chronic prostatitis; Case 2: 1 patient with depression and impotence | Case 1: LBRAD(20 g lily bulbs; 10 g Anemarrhena) addition and subtraction, was taken once a day in 2 divided doses for 5 consecutive weeks. Case 2: LBRAD(20 g lily bulbs; 15 g Anemarrhena) addition and subtraction, was taken once a day in 2 divided doses for 5 consecutive weeks. |
Case 1: The SDS score was significantly lower than before treatment. Overall treatment rate 100 % Case 2: Overall treatment rate 100 % |
Based on satistical analysis and data mining, in the Chinese Pharmacopeia (2020 Edition), there are more than 40 Chinese medicine preparations containing Lilium lancifolium bulb or/and Anemarrhena asphodeloides rhizome as an ingredient, the majority of which are used to treat Pulmonary disease and emotional disease [25,35,36]. Among them, Lilium lancifolium bulb is even used in Baihe Gujin pills as a Monarch drug, which leads the actions of the formulae. Therefore, in the Chinese patent medicines with the effects of nourishing the heart and nourishing the lung, Lilium lancifolium bulb and Anemarrhena asphodeloides rhizome plays the fundamental role and influences the effects. Furthermore, based on the TCM theory, LBRAD is used to treat diabetes and oral ulcer in some areas.
4. Preparation of standard decoction of LBRAD
Previous decoction research mainly focused on the composition of prescriptions and the ratio of traditional Chinese medicines, ignoring the source of medicinal materials and preparation principles, and has not yet formed clear quality control standards, which greatly reduces the efficacy of traditional Chinese medicines. Therefore, some scholars have proposed that the development of classic famous prescriptions must first be clear Based on relevant literature research, determining high-quality medicinal materials or decoction pieces is the basis, and research and development of material benchmarks is the core. Modern standardized processes are used for preparation to ensure quality [37]. The preparation method of decocting liquid plays an important role in quality control to maximize the effect of classical herbal formula [38]. For this reason, through the literature research, we have investigated for the first time to the Lilium lancifolium bulb, the mother of the original origin and dosage of the authentic herbal medicine survey. Then, the original dose of Lilium lancifolium bulb and Anemarrhena asphodeloides rhizome was converted into the current dose in LBRAD and the standard decoction of LBRAD was prepared by the original decocting method.
The dried fleshy scale leaves of Lilium lancifolium Thunb are used as medicine, which is recorded in the Shennong Materia Medica. The bulbs are enlarged and are used as medicinal and food plants. In terms of processing, the main methods are purification and cutting. These two methods were first seen in Golden Chamber. It is cold in nature and sweet in taste, and has the effects of nourishing yin and clearing the lungs, resolving phlegm and relieving cough, and calming the heart and mind [39,40]. Clinically, it is often used to treat tuberculosis, diabetes, hyperthyroidism; schizophrenia, insomnia, depression, anxiety; stubborn itchy skin in the elderly, and herpes zoster [41]. The current standards and norms are used as a reference to connect the ancient records with the current norms and to support the uniform quality control of classical recipes in order to meet the modernization requirements of classical recipes. In previous studies, our team concluded that the Lilium lancifolium bulb in the Golden Chamber is the fresh fleshy bulb of the liliaceae plant, Lilium lancifolium Thunb weighing about 70g per fresh Lilium lancifolium bulb and about 25g per dried Lilium lancifolium bulb. Shennongjia, Hubei Province is the best source of medicinal materials for Lilium lancifolium bulb. Therefore, we selected seven authentic Lilium lancifolium bulbs from Shennongjia, which were washed and soaked overnight. The total weight of modern Lilium lancifolium bulb was about 490g.
Anemarrhena asphodeloides rhizome was first recorded in Shennong Materia Medica. It is the dried rhizome of the asparagaceae plant, Anemarrhena asphodeloides Bunge. According to the processing method, Anemarrhena asphodeloides rhizome is removed from the hair and skin, sliced and dried with a low fire. It has the effect of clearing heat, benefiting water and nourishing. It is clinically used in the treatment of depression, diabetes, cerebrovascular diseases and tumor diseases [42]. The Compendium of Materia Medica of the Ming Dynasty records the processing of Anemarrhena asphodeloides rhizome: “The upper part of the meridian is baked with wine, and the lower part is baked with salt water.” When LBRAD was used to treat lily disease, the disease position was on the upper part, namely the heart and lung, it is generally believed that according to the cutting method of Anemarrhena asphodeloides rhizome, today's Anemarrhena asphodeloides rhizome is the ancient Anemarrhena asphodeloides rhizome processed with wine [43]. Ancient texts record that yellow flowers were produced in Hanoi, now in Pengcheng, Zhili, and mainly in modern Hebei, Henan, Shanxi, and Jiangsu regions, with the best origin being Xiling town, Yi County, Hebei [44].
Changes in measurement over the ages have had a great impact on the dosage conversion of meridian prescriptions. Qin Dynasty implemented unified weights and measures throughout the country, and the Eastern Han Dynasty basically followed and improved the weights and measures of Qin Dynasty. Due to the changes of weights and measures in the past dynasties, the size of the contemporary square conversion standard is different, and there is no standard to follow. Li [45] believed that one liang in the Eastern Han Dynasty was equal to the current 15.625g. Doctors in the Ming and Qing Dynasties proposed to convert one liang into one qian in ancient times. Li Peisheng [46] pointed out that a liang in the Eastern Han Dynasty was equivalent to 3g in modern times. According to some scholars, 1 L in the Han Dynasty was equal to 200 mL in modern times [47]. Therefore, our team proposed that one pair in the Eastern Han Dynasty is approximately equal to 3g in modern times, and 1 L is equal to 200 ml in modern times. Therefore, our team proposed that one pair in the Eastern Han Dynasty is approximately equal to 3g in modern times, and 1 L is equal to 200 ml in modern times.
According to the Summary of the Golden Chamber, 7 lilies were boiled with 2 L (400 ml) of spring water into 1 L (200 ml) of decoction, and then 9g of Anemarrhena asphodeloides rhizome was boiled with 2 L (400 ml) of spring water into 1 L (200 ml) of decoction. Secondly, 200 ml of Lilium lancifolium bulb decoction were mixed with 200 ml of Anemarrhena asphodeloides rhizome decoction, and finally boiled into 300 ml of decoction. Heat the clothes twice. Therefore, we selected Xiling Anemarrhena asphodeloides rhizome dried rhizome wine sliced from Yi County and Shennongjia fresh Lilium lancifolium bulb to determine the dosage of LBRAD. Produced in Xiling Town, Yi County, washed and sliced fur wine, sun-dried weight of about 9g. Seven fresh Lilium lancifolium bulbs from Shennongjia weigh about 490g and 175g when dried.
Based on the above studies, we finally selected Shennongjia Fresh Lilium lancifolium bulb 490g, Yi County Xiling Anemarrhena asphodeloides rhizome 9g, prepared 300 ml decoction, as the standard decoction of LBRAD, as a standard carrier for the study of depression treatment (Fig. 3).
Fig. 3.
LBRAD standard decoction preparation. First, seven Lilium lancifolium bulbs (500 g) were washed in water and soaked for one night (490 g). Second, the soaking water was eliminated and then the Lilium lancifolium bulbs were decocted in 400 ml of spring water to obtain a 200 ml decoction, followed by boiling for 30 min. Finally, 9 g Anemarrhena asphodeloides rhizome decoction was added to the Lilium lancifolium bulbs decoction to obtain a 300 ml mixture, which was further decocted in mild fire for 45 min.
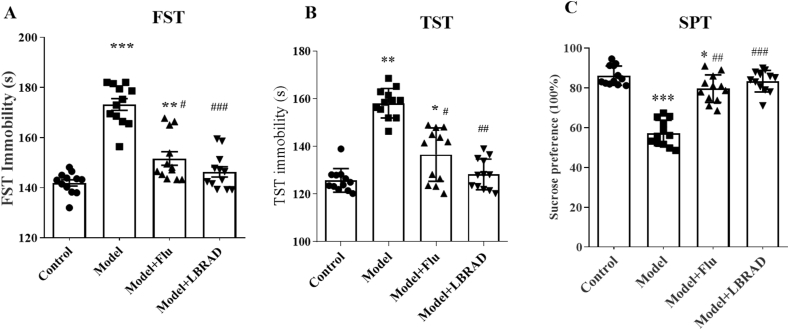
Secondly, we used sucrose water preference test (SPT), tail suspension test (TST), and forced the swimming test (FST) in Sprague-Dawley (SD) rats to investigate the antidepressant like effects of LBRAD Standard decoction. The antidepressant behavior assessment is listed in the supplement. The results showed that continuous 150 g/kg LBRAD intervention for 35 days significantly increased sucrose water intake and shortened fixation time in rats compared to the depressed group (P < 0.05, Fig. 4). We also found that LBRAD's antidepressant effect was superior to fluoxetine, which is commonly used to treat depression.
Fig. 4.
LBRAD (standard decoction) intervention improved the CUMS-induced depression-like behavior. A-C) LBRAD (standard decoction) and fluoxetine treatment were significantly decreased immobility time of forced the swimming test, tail suspension test and increased in sugar intake. *Represents a comparison with the control group, **P < 0.01, ***P < 0.001; #Represents a comparison with Model, #P < 0.05, ##P < 0.01, ###P < 0.001. Model + Saline: Model + Saline group, Model + Flu: Model + fluoxetine group, Model + LBRAD: CUMS + Lily Bulb and Rhizoma Anemarrhena Decoction (standard decoction), n = 12 per/group.
5. Clinical application of LBRAD in the treatment of depression
In recent years, studies have demonstrated that LBRAD and its plus and subtraction formula, when combined with other prescriptions or chemicals, can significantly reduce depressive symptoms with fewer side effects compared to conventional drugs, which warrants further expansion of its clinical applicability [48]. Clinical trials compared the efficacy of LBRAD in combination with votioxetine and votioxetine alone in the treatment of depression. The results of the randomized, controlled, double-blind, parallel trials showed that the Hamilton Depression Scale (HAMD) score of LBRAD group was significantly lower than that of votioxetine alone, and the total response rate was significantly higher than that of the control group [49]. Another retrospective cohort study reported the efficacy of LBRAD plus and minus plus Ganmai Dazao Decoction in the treatment of depression. The anti-depression effect of LBRAD plus and minus plus Ganmai Dazao Decoction was better than fluoxetine hydrochloride, the total effective rate was 86.11 %, and the incidence of side effects was less than that of western medicine group [50]. According to the theory of TCM syndrome differentiation and treatment, 100 cases of menopausal depression patients with liver-kidney Yin deficiency were randomly divided into LBRAD intervention group and oral Xiaoyao Pill group. After 4 weeks of treatment, the scores of Athens Insomnia Scale (AIS) in LBRAD intervention group were significantly improved. The recovery rate of the follicle-stimulating hormone (FSH) and luteinizing hormone (LH) was significantly faster than the Xiaoyao Pill group, and the total effective rate was 88.00 %, which was higher than that of control group (60.00 %) [51]. Other researchers have conducted serological analysis on 90 patients with the perimenopausal depression. Controlled trials suggested that modified LBRAD could regulate serum sex hormone levels, increase the expression of serotonin (5-HT) and brain-derived neurotrophic factor (BDNF), and decrease the expression of adrenocorticotropic hormone (ACTH) and corticosterone (CORT). It can effectively alleviate depressive symptoms in perimenopausal patients [52]. In addition, LBRAD has been widely used in combination with other therapies to treat depression. Randomized controlled data showed that LBRAD combined with electroencephalograph (EEG) bionic electrical stimulation for 6 weeks of continuous treatment under basic symptomatic treatment significantly improved neurological function and symptoms of TCM syndrome, improved hematology, and reduced depression levels without increasing adverse effects [53]. Meanwhile, another researcher reviewed and analyzed the clinical effect of LBRAD combined with Shuyuan acupuncture in the treatment of post-stroke depression in elderly patients, and found that the experimental group could effectively improve the depression-like behavior of patients and restore the neurological deficit function, and the serum levels of 5-HT, BDNF and the score of the activities of daily living scale (ADL) were significantly higher than the control group. The total effective rate of the experimental group was 97.62 %, and the clinical effect was fast and beneficial to the prognosis [54]. In conclusion, these clinical studies confirm that LBRAD has a good antidepressant effect, is less tolerated, and has fewer side effects than conventional drugs. It is a promising drug for the treatment of depression [55] (Table 2).
Table 2.
LBRAD treatment clinical trials in depression.
| Study | Subjects | LBRAD administration | Results |
|---|---|---|---|
| Liu., 2021 [49] | 105 patients with depression | Group 1: Oral vortioxetine (manufacturer: H.Lundbeck A/S; registration number H20170383) 10 mg/time, once a day, for 2 months. Group 2: The same administration method as group 1; LBRAD(7 lily bulbs; 30 g Anemarrhena) was taken once a day in 2 divided doses for 2 months. |
The total effective rate of treatment: Group 2(92.00 %) was higher than Group 1(76.36 %); Group 2 vs Group 1(X2 = 4.719, P = 0.030); Overall scores of HAMD after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(t = 5.465, P = 0.044); The incidence of adverse reactions between the two groups during treatment(X2 = 1.428, P = 0.133). |
| Jin., 2018 [50] | 72 patients with depression | Group 1: Fluoxetine (Suzhou Yushi Pharmaceutical Co., Ltd., national drug approval number: H20093454, 20 mg/tablet) is taken orally in the morning, 1 pill each time, once a day. Continuous treatment for 8 weeks. Group 2: The same administration method as group 1; LBRAD(30 g lily bulbs; 10 g Anemarrhena) and Ganmai Dazao decoction were taken once a day in 2 divided doses for 8 weeks. |
The total effective rate of treatment: Group 2(86.11 %) was higher than Group 1(69.44 %); Group 2 vs Group 1(X2 = 7.604, P = 0.006); The incidence of adverse reactions between the two groups during treatment(X2 = 8.867, P = 0.003). |
| Ding., 2015 [51] | 100 patients with yin deficiency in liver and kidney perimenopausal depression | Group 1: Xiaoyao Pill (produced by Shanghai Baolong Anqing Pharmaceutical Co., Ltd., national drug approval number Z34020541) 6 g orally, 2 times a day. Continuous treatment for 4 weeks. Group 2: LBRAD(50 g lily bulbs; 15 g Anemarrhena) was taken once a day in 2 divided doses for 4 weeks. |
The total effective rate of treatment: Group 2(88.0 %) was higher than Group 1(60.0 %); Group 2 vs Group 1(P < 0.05); After treatment, the FSH and LH levels in group 2 were significantly improved compared with those in group 1(P<0.05); the AIS score in group 2 was significantly improved compared with before treatment and after treatment in group 1(X2 = 11.652, P = 0.018). |
| Zheng et al., 2020 [52] | 90 patients with perimenopausal depression | Group 1: Flupentixol-melitracen tablets (produced by H. Lundbeck A/S, Denmark, approval number: H20080175) are taken orally, 1 tablet each time, 2 times a day, in the morning and at noon. Continuous treatment for 8 weeks. Group 2: The same administration method as group 1; LBRAD(30 g lily bulbs; 15 g Anemarrhena) was taken once a day in 2 divided doses for 8 weeks. |
The total effective rate of treatment: Group 2 was higher than Group 1; Group 2 vs Group 1(Z = 5.682, P = 0.016); Overall scores of HAMD and Kupperman after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.01); Levels of serum 5-HT and BDNF after the intervention: Group 2 was higher than Group 1; Group 2 vs Group 1(P < 0.01); Levels of serum ACTH and CORT after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.01). |
| Ji et al., 2022 [53] | 92 patients with post-stroke depression | Group 1: Treated with the EEG Bionic Electrical Stimulator only (frequency 50 Hz, current 14.5 mA). 30 min each time, once a day. Continuous treatment for 6 weeks. Group 2: The same administration method as group 1; LBRAD(30 g lily bulbs; 15 g Anemarrhena) was taken 250 mL each time, 2 times a day for 8 weeks. |
The total effective rate of treatment: Group 2(95.65 %) was higher than Group 1(76.09 %); Group 2 vs Group 1(P < 0.05); Overall scores of HAMD and NIHSS after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.05); Overall scores of the TCM syndrome after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.01); Levels of high shear whole blood viscosity and low shear whole blood viscosity after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.01); The incidence of adverse reactions between the two groups during treatment(X2 = 3.101, P > 0.05). |
| Zhang and Xing., 2022 [54] | 82 patients aged 64–85 years old with post-stroke depression | Group 1: Flupentixol and Melitracen Tablets (Chongqing Shenghuaxi Pharmaceutical Co., Ltd., National Drug Approval Number H20153122, specifications: flupentixol 0.5 mg and melitracen 10 mg/tablet), 1 tablet/time, 2 times/d, taken in the morning and evening; Acupuncture treatment (Shenshu, Taichong, Taixi, Ganshu, etc.), 20 min, then acupuncture once, for a total of 40 min, once a day, 6 times a week. Continuous treatment for 5 weeks. Group 2: The same acupuncture method as group 1; LBRAD(30 g lily bulbs; 15 g Anemarrhena) was taken 200 mL each time, 2 times a day for 5 weeks. |
The total effective rate of treatment: Group 2(97.62 %) was higher than Group 1(75.00 %); Group 2 vs Group 1(Z = 9.024, P = 0.003); Overall scores of HAMD, Self-Rating Depression Scale(SDS), and NIHSS after the intervention: Group 2 was lower than Group 1; Group 2 vs Group 1(P < 0.05); Overall scores of ADL after the intervention: Group 2 was higher than Group 1; Group 2 vs Group 1(P < 0.05); Levels of serum 5-HT and BDNF after the intervention: Group 2 was higher than Group 1; Group 2 vs Group 1(P < 0.05). |
6. Pharmacological mechanism of LBRAD in treating depression
To further understand the mechanism of LBRAD in treating depression, the antidepressant effect of LBAD has been evaluated in recent decades by macroscopically improving depression-like abnormal behavior in experimental animal models. Besides, studies on anti-inhibitory mechanisms in terms of modulating HPA axis hyperactivity, inhibiting neuronal apoptosis, enhancing monoamine neuron function, and regulating intestinal flora homeostasis are still limited. Liu [[56], [57], [58]] noted that continuous gavage of LBRAD significantly improved depressive behavioral characteristics in chronic unpredictable mild stress (CUMS) combined isolated rats compared to saline controls. Meanwhile, LBRAD could significantly increase the contents of serum DA, 5-HT and NE, and decrease the contents of serum ACTH and GLU. Moreover, the contents of 5-HT and NE in the cerebral cortex of rats were increased. Li [59] found that LBRAD total saponins could promote 5-HT synthesis and transport in the brain tissue of CUMS rats, inhibit reuptake, increase central 5-HT content, improved synaptic transmitter signaling ability, and enhance antidepressant effect. Another scholar explored that continuous administration of LBRAD for 4 weeks could significantly reduce adrenal index of CUMS-induced depressed rats, thus enhancing the function of neuronal regeneration and repair in hippocampus and effectively improving the depressive state of rats [60]. In addition, other researchers have also emphasized that LBRAD plays an obvious antidepressant role by reversing HAP axis overactivity in the abnormal mechanism of brain-intestinal interaction and up-regulating the content of monoamine neurotransmitters in brain tissue [61]. In addition to animal model studies, many molecular and cellular signaling pathways have been analyzed. Among them, LBRAD can improve depressive symptoms in rats and restore nerve regeneration and memory, and its mechanism may be related to the activation of the cAMP/PKA/CREB/BDNF signal transduction pathway [62]. Studies have shown that LBRAD could affect key molecules such as CaM/CaMKⅡ/CREB/BDNF in the rat hippocampus signaling pathway and improve the damage and loss of neurons [63]. Another report [64] analyzed that LBRAD may exert an antidepressant effect by up-regulating the MAPK/PKC/MEK/ERK1/2/CREB/BDNF cascade, inhibiting neuronal apoptosis and enhancing hippocampal neuronal regeneration and the repair function. It is suggested that LBRAD has a good anti-depressant effect, and its mechanism may be related to increasing the level of monoamine neurotransmitters, inhibiting the overactivity of glutaminergic nervous system, reversing the hyperfunction of HPA axis, up-regulating the transduction pathways of cAMP, CaM and MAPK, increasing the level of BDNF and related proteins in brain, thus reducing neuronal apoptosis and improving nerve damage. Regeneration is concerned.
The role of TCM prescription is the comprehensive result of the regulation of the effective component network in the prescription on the biomolecular network in the disease state of the body [65]. This makes it difficult for traditional pharmacological experiments and analytical methods to reveal its active ingredients and action targets [66]. Network pharmacology is a multidisciplinary science based on the theory of systems biology. Based on the pharmacokinetics of traditional Chinese medicine in vivo, network pharmacology describes biological systems from the perspective of network. By integrating a large number of experiments and virtual models in vitro, potential active components, targets and pathways are screened to construct a multi-level network connection, which is consistent with the integrity principle of traditional Chinese medicine. Potential to elucidate the complexity between TCM, targets and diseases [[67], [68], [69]]. Based on the pharmacology database and the analysis platform of traditional Chinese medicine system, Zhao [70] screened the bioactive components and target genes of LBRAD. It contained 165 related components, 84 components from Lilium lancifolium bulb and 81 components from Anemarrhena asphodeloides rhizome. LBRAD had 23 active compounds and 364 target proteins. KEGG analysis showed that the overlapping genes were mainly concentrated in hypoxia inducible factor-1 (HIF-1), dopaminergic synapses, estrogen and 5-HT synapses signaling pathways, and were mainly involved in cAMP metabolism, monoamine synthesis and transport, and oxidative stress response related biological processes. Molecular docking confirmed a high affinity between LBRAD and key targets of ESR1, MAOA, NR3C1, VEGFA and mTOR associated with depression. Wang [71] analyzed the active ingredients, targets and molecular mechanisms of LBRAD's anti-depressant effects by combining animal experiments with network pharmacology, and constructed a component database containing 163 components and a target database covering 1286 proteins. Twenty-six active components and ten absorbed components of LBRAD were identified by ultra-performance liquid chromatography/quadrupole time-of-flight mass spectrometry (UPLC-QTOF-MS), and 27 potential targets were screened. Two potential signaling pathways, PI3K/Akt and MAPK, were predicted by KEGG pathway enrichment analysis. Western blot indicated that LBRAD could significantly inhibit PI3K/Akt/GSK-3β signaling pathway, while up-regulate MAPK pathway. In addition, other scholars [72] found that LBRAD screened 11 active components, which acted on 106 depression-related target, involved in the regulation of neurotrophic factors, insulin, MAPK, PI3K/Akt, prolactin and other metabolic pathways, and involved in protein phosphorylation, signal transduction, RNA regulation and other major biological processes. These targets and biological pathways are consistent with the pathogenesis of depression.
Du [73] used UPLC-QTOF-MS to study the model metabolomics of LBRAD total saponins in chronic mild CUMS-induced rat depression model and cerebral ischemia reperfusion mouse depression model. The related pathways of different metabolites suggest that LBRAD may play an antidepressant role by regulating amino acid metabolism, energy metabolism, fatty acid metabolism, tricarboxylic acid cycle and oxidative stress response. In addition, Liu [74] found that LBRAD interfered with the restoration of normal levels of 23 different metabolites in serum, mainly by affecting fatty acid amide metabolism, phenylalanine metabolism, glycine metabolism and lipid metabolism to improve depression in rats through a positive control test in SD rats. Fluoxetine could only correct the abnormal levels of 17 metabolites in glycine metabolism and lipid metabolism. These findings suggest that the antidepressant mechanism of LBRAD Standard decoction mainly involves the nervous, endocrine and immune inflammatory systems. By changing a series of biological processes, the homeostasis of depression's multi-system functions can be realized [75]. To provide a scientific basis for the global understanding of the anti-depression mechanism of LBRAD based on multi-component - multi-target - multi-effect omics (Fig. 5).
Fig. 5.
The main mechanism of LBRAD in the treatment of depression. The nervous, immuno-inflammatory, and endocrine systems were mainly involved in the antidepressant mechanisms of the LBRAD standard decoction. Notably, LBRAD standard decoction was involved in many biological processes which up-regulated and down-regulated a series of signaling pathways to achieve a homeostatic state of multi-system functions in depression.
7. Effective material basis of LBRAD in treating depression
The large number of chemical components contained in this prescription is the material basis for its clinical effect. Therefore, it is crucial to clarify the pharmacodynamic material basis of prescription to explore the compatibility and mechanism of action of prescription [76]. However, due to its complex composition and lack of clear evaluation criteria, LBRAD is less understood and accepted than the better studied natural active compounds. Numerous clinical studies and basic research have shown that the total saponins of Lilium lancifolium bulb (Fig. 6A) are the material basis of the antidepressant effect of Lilium lancifolium bulb [77,78]. Based on this, our previous study [[79], [80], [81]] found that verbascoside (Fig. 6B) and dioscin (Fig. 6C) in Lilium lancifolium bulb decoction had better antidepressant activity by high-performance liquid chromatography (HPLC) combined with liquid chromatography–mass spectrometry (LC-MS) analysis technologies. Huang [82] established a rat model of chronic psychological stress depression. The animal experiment showed that the total saponins of Lilium lancifolium bulb could improve the symptoms of the loss of pleasure after drinking sugar water in depressed mice and relieve the sense of behavioral despair in swimming mice. It also enhanced 5-HT-induced head-shaking behavior in mice, suggesting that total saponins in Lilium lancifolium bulb were the main active components of antidepressant effects. At the same time, pharmacological experiments showed that the total saponins of Lilium lancifolium bulb could regulate the homeostasis of brain-intestinal peptides, and it was speculated that the effect of Lilium lancifolium bulb on the improvement of depressive symptoms and gastrointestinal discomfort symptoms might be the result of the synergism between brain-intestinal axis and 5-HT-ergic nervous system. Guo [83] conducted antidepressant efficacy screening of the effective parts of Lilium lancifolium bulb and set up a randomized controlled experiment, finding that the saponins of Lilium lancifolium bulb are the basis of effective substances for antidepressants. Through serological analysis and molecular experiments, it was proposed that the antidepressant mechanism of Lilium lancifolium bulb saponins may be to increase the content of monoamine neurotransmitters in the brain tissue, inhibit HPA axis hyperactivity, and reduce neuronal apoptosis. Fu [84] used orthogonal experiments to optimize the enrichment process of total saponins in Lilium lancifolium bulb, establish quality standards, and explore its anti-depression effect. The optimal extraction conditions were 80 % ethanol, heating reflux for 3 h, and extraction 3 times. Compared with the western medicine group, the total saponins extract of lilium can significantly improve the depression-like behavior of mice, and has better anti-depression activity. Other scholars [85] studied that the total saponins of Lilium lancifolium bulb can normalize the serum ACTH, CORT, CGRP (calcitonin gene-related peptide) and VIP (vasoactive intestinal peptide) active peptide, and play a comprehensive role in the treatment of depression and irritable intestine, and the high dose of Lilium lancifolium bulb saponins has a stronger effect on anti-depression and gastrointestinal discomfort than the low dose. It is suggested that its effect may be related to regulating the disorder of cerebral intestinal axis and HPA axis. In addition, some studies have also shown that stigmasterol (Fig. 6D) and beta-sitosterol (Fig. 6E) in Lilium lancifolium bulb can change the content of monoamine neurotransmitters in the brain tissue and has demonstrated robust neuroprotective effects and shows anxiolytic/antidepressant effects as well [39,40,[86], [87], [88]].
Fig. 6.
Structural formula of eight important compounds in two Chinese herbs of LBRAD. A: Lilium lancifolium bulb saponins; B: Verbascoside; C: Dioscin; D: Stigmasterol; E: Beta-sitosterol; F: Timosaponin BII; G: Timosaponin BIII; H: Mangiferin.
The main components of Anemarrhena asphodeloides rhizome are saponins, flavonoids, polysaccharides, and diphenylpyrones, of which the main active components are saponins and flavonoids. The saponins are mainly composed of Timosaponin BII (Fig. 6F), Timosaponin BIII (Fig. 6G), and Timosaponin AIII. Flavonoids mainly include mangiferin (MG) (Fig. 6H), isomangiferin and neomangiferin (NG) [[89], [90], [91]]. Some studies have reported that the total saponins of Anemarrhena asphodeloides rhizome saponins can improve the survival rate of rat adrenal medulla pheochromocytoma (PC12) cells and reduce the death of neurons [42]. Meanwhile, nosei saponin BⅡ can increase the content of DA and 5-HT in brain by inhibiting monoamine oxidase and play an antidepressant role [92]. Bai Haodong [93] analyzed that the content of polysaccharides, saponins, and flavonoids in Anemarrhena asphodeloides rhizome increased after salt, wine, and stir frying, indicating that its anti-inflammatory and antidepressant pharmacological effects may correspondingly increase. Additionally, pharmacological experiments have shown that flavonoid glycosides such as MG and NG [[94], [95], [96]], steroidal saponins [97,98], as well as phenolic glycosides such as regaloside A (RA) and regaloside I (RI) [99,100] have significant anti-inflammatory effects. Therefore, it is speculated that the above compounds are representative components of the effective substance foundation for LBRAD in treating depression.
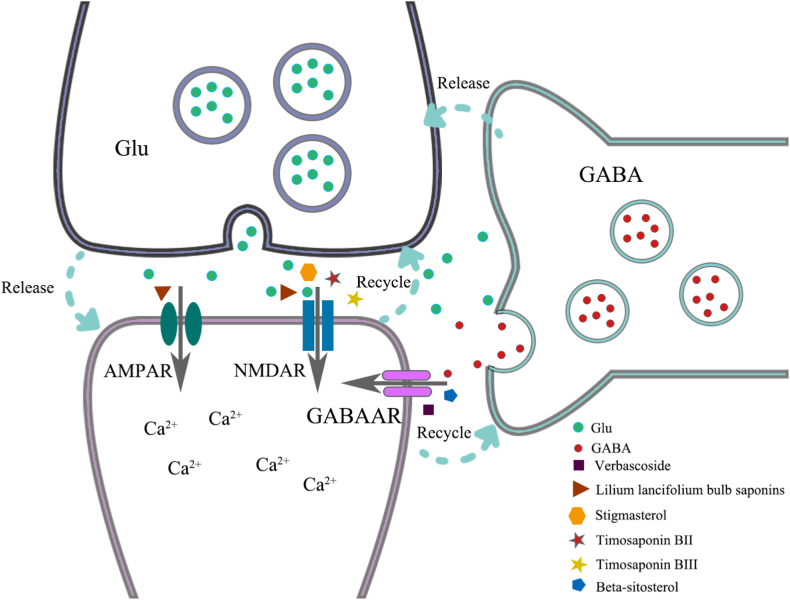
The above-mentioned active compounds act on the main targets and achieve antidepressant effects through related chemical reactions, the detailed mechanism is still unclear. Current research mainly focuses on synaptic transmission. Sourav Ghosh found through animal experiments that stigmasterol coadministration with fluoxetine significantly reversed the depressive-like behavior of mice and altered the hippocampus 5-HT and Glu levels, confirming the antidepressant-like effect of stigmasterol, further molecular docking suggested that stigmasterol has affinity for NMDA receptors, and the mechanism may be mediated by the glutamatergic system [101]. There are research results demonstrated that mangiferin possessed antidepressant and anti-anxiety properties due to its ability to attenuate IL-1β level and oxidative stress (including increasing reduced glutathione concentration and related enzyme activities) evoked by intraperitoneal administration of lipopolysaccharide [94]. Gu screened out Lilium lancifolium bulb saponins through untargeted and targeted metabolomics, found that it can not only effectively increase BDNF deposition but also modulates the glutamine and glutamate metabolism, restoring reduced glutamate levels in the brains of depressed rats; revealed the glutamatergic system was involved in the antidepressant activity of Lilium lancifolium bulb saponins (LS) [102,103]. Du used the CUMS rat depression model and found that Anemarrhena saponins (AS) could significantly restore monoamine neurotransmitter levels in the hippocampus of depressed rats, the metabonomic profile revealed the anti-depressant effect might be related to the regulation of several metabolic pathways, including amino acid, fatty acid, and phospholipid metabolism in rats, suggesting a synergetic effect of AS and LS in the treatment of depression [103]. Zhang used chronic mild stress (CMS) and chronic social defeat stress (CSDS) to jointly model, and found that a structurally modified derivative of one of the primary metabolites of Timosaponin BIII, YY-23 in the brain areas, elicited significant improvements in stress-related behaviors, indicating Timosaponin BIII is a novel non-competitive antagonist of NMDA receptors with promising rapid antidepressant-like effects in mouse depression models [104]. Zhao reviewed the antidepressant mechanism of verbascoside through a systematic review, combining bioinformatics and network pharmacology, showed that the antidepressant effects of verbascoside involves modulating the levels of monoamine neurotransmitters, inhibiting HPA axis hyperfunction, restoring the coding output function of GABAergic neurons, and promoting neuroprotection may be involved in the process of its action against depression [80]. Through pharmacological experiments, Yin found that sitosterol and its derivatives can significantly shorten the immobility time in the TST and FST on male adult mice, and have strong antidepressant activity. Pharmacokinetics showed that this antidepressant-like effect is mediated by the 5-HT, DA and GABA-ergic systems [105]. In summary, due to the complexity of the ingredients of TCM decoction and the uncertainty of pharmacokinetics, the antidepressant effect of LBRAD is currently mainly focused on the study of synaptic transmission of active ingredients, lacking a systematic network mediation system (Fig. 7).
Fig. 7.
Active ingredients interact with NMDA receptors, GABAA receptors, and AMPA receptor-related receptors to exert antidepressant effects.
Previous studies have focused on the antidepressant activity of lilium lilium extract or its components. The active ingredients contained in LBRAD's effective substance base for treating depression have not been studied. The pharmacokinetics of TCM compounds is not only the addition of drug effects, but also plays a synergistic role in the functional integration of multiple systems of human body based on the action of various active components according to the law of prescription compatibility, and plays a preventive or therapeutic effect. Besides, the effect of drug efficacy is realized by component metabolism after absorption into blood, and the rate and degree of drug biotransformation in depression also changes compared with normal people. Consequently, advanced analytical techniques such as high performance liquid chromatography-fingerprint and liquid chromatography-tandem mass spectrometry are applied to study the content of LBRAD active component and its pharmacokinetics. It is helpful to discover the leading compounds of TCM in the treatment of depression, and provides the scientific basis for evaluating the clinical efficacy of LBRAD in the treatment of depression and improving the treatment plan.
8. Potential mechanism prediction of LBRAD in treating depression
Traditional Chinese medicine network pharmacology is a powerful approach that integrates systems biology, bioinformatics and diversity pharmacology to transform drug development from a point or linear model to a holistic and systemic model. Coincidentally with the principles of holistic view, differentiation of symptoms and treatment, and formulation and compatibility of traditional Chinese medicine, it transforms traditional Chinese medicine from empirical medicine to evidence-based medicine, revealing effective ways for the synergistic and potential mechanisms of traditional Chinese medicine [[106], [107], [108], [109]]. In order to better understand how the multi-component treatment system of LBRAD has multiple effects on depression. We used comprehensive network pharmacology analysis to evaluate the active biomarker and core targets of LBRAD in the treatment of depression. This method aims at predicting the relationship between LBRAD, active biomarker, targets and depression.
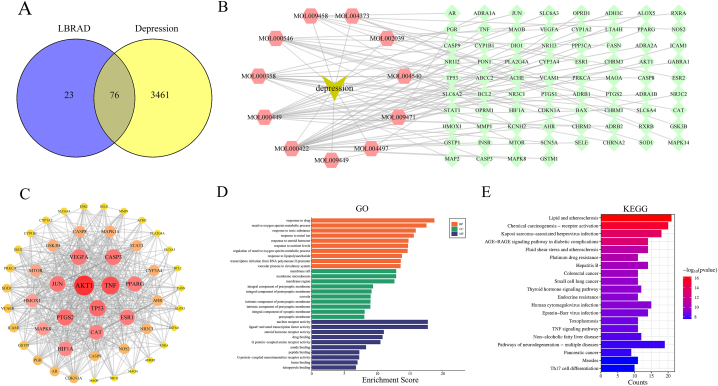
Firstly, we will start with the website TCMSP (http://tcmspw.com/tcmsp.php) We searched for the traditional Chinese medicine ingredients and targets of Lilium lancifolium bulb and Anemarrhena asphodeloides rhizome, and ultimately confirmed 99 LBRAD targets. Secondly, from OMIM (https://www.omim.org/) 3537 depression related genes were obtained from the Genecards (https://www.genecards. org/) database. Subsequently, 76 intersecting genes were obtained through Venn plots (Fig. 8A). In this study, the corresponding relationships between “drug component targets” were organized and imported into Cytoscape 3.9.2 to construct a pharmacological map of the LBRAD network for the treatment of depression (Fig. 8B). The drug component target network diagram shows that the antidepressant effect of LBRAD is the result of the combined action of multiple targets and chemical components. By String (https://string-db.org/) Platform, import intersection genes, and construct a protein interaction (PPI) network diagram (Fig. 8C). The PPI network results indicate that the potential target genes for LBRAD regulation of depression are mainly AKT1, TNF, TP53, PTGS2, JUN, VEGFA, CASP3, ESR1, PPARG, and CAT. At the same time, there is a close interaction among these goals. Interfering with many biological processes related to nourishing yin and moistening dryness, clearing heat and resolving depression, thereby exerting the aforementioned network pharmacological effects. Using the bioinformatics open source software Bioconductor (http://www.bioconductor. org/) with a screening condition of P < 0.05, genomic (GO and KEGG) pathway analysis was conducted on 76 potential cross targets for the LBRAD treatment of depression in R software, to speculate on the potential pathways for the LBRAD treatment of depression. GO enrichment analysis shows that the main biological processes involved include drug reaction, active oxygen metabolism, steroid hormone reaction, lipopolysaccharide reaction, cell junction, synaptic or plasma membrane composition and the receptor activity (Fig. 8D). KEGG enrichment analysis results showed that lipid and atherosclerosis, chemical carcinogenesis receptor activation, Kaposi sarcoma associated herpesvirus infection, AGE-RAGE signal pathway, thyroid hormone, endocrine resistance and TNF signal pathway in diabetes complications may be the main signal pathways of LBRAD in the treatment of depression (Fig. 8E). LBRAD can be used to treat depression through multiple links and targets, and related signaling pathways is also able to execute specific biological processes through interactions between targets.
Fig. 8.
LBRAD attenuates depression via the multiple compounds, multiple targets and the several signaling pathways. A: The intersection genes of LBRAD and depression. B: “LBRAD drug-component-target network”. 76 disease targets have established networks with LBRAD and depression. Green node represents intersection gene, yellow node represents depression, and red node represents active compounds. C: PPI network of core targets. The darker the color, the more the core target. The core genes of LBRAD regulating depression are mainly AKT1, TNF, TP53, PTGS2, JUN, VEGFA, CASP3, ESR1, PPARG and CAT. D: GO enrichment analysis of key targets. The first 10 significant P values of BP; The first 10 significant P values of CC; The first 10 significant P values of MF; E: KEGG enrichment analysis. The first 20 significant P values of KEGG pathways. BP = biological process, CC = cellular component; MF = molecular function. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
9. LBRAD and COVID-19 post rehabilitation depression
In late 2019, novel coronavirus pneumonia (COVID-19) began spreading globally and became a major global public health event [110]. Up to now, the number of “rehabilitation” patients has been increasing, and more and more evidence shows that among the “rehabilitation” patients after COVID-19, there are a considerable number of people with long-term complications and sequelae of multiple organs and systems [111,112], including various physical and neuropsychiatric symptoms, whose duration is uncertain, severity is different, and seriously affects people's physical and mental health [113,114]. Although the symptoms of patients recovering from COVID-19 are complex and changeable, digging into the TCM classic book Golden Chamber; reveals that the symptoms of lily disease are quite similar to those of patients recovering from COVID-19. It can be seen that through syndrome differentiation and treatment, the syndrome and treatment principles of lily disease can be applied to the recovery and conditioning of COVID-19 [115]. LBRAD regulates lung qi, nourishes yin and clears heat, which is consistent with the syndrome of COVID-19. Based on this theory, we screened 90 active pharmaceutical ingredients through network pharmacology and obtained 5823 genes related to COVID-19. We screened out 208 intersection genes. KEGG analysis found that the top 20 pathways were enriched in PI3K-Akt signaling pathway, Th17 cell differentiation, and C-type lectin receptor signaling pathway, which shows that LBRAD may play a role in treating COVID-19 through anti-viral, anti-inflammatory, immune-regulation (Fig. S1). Qi [116] used high-throughput molecular docking and dynamic simulation ADMET (absorption, distribution, metabolism, excretion, and toxicity) technology to screen 116 traditional Chinese medicines and found that Anemarrhena Rhizoma extract may act on the main protease of SARS-CoV-2(Mpro), inhibits viral replication and transcription and exerts antiviral effects, with an inhibition rate of 78.9 %. Ran [115] collected a case report of severe COVID-19, the virus turned negative after three consecutive weeks of LBRAD combined with other TCM prescriptions and antibiotics, and the effect was significantly higher than the previous treatment period with western medicine alone. It can be inferred that LBRAD may inhibit viral replication by acting on viral proteases, regulate host cell self-defense system, reduce the secretion of pro-inflammatory factors by inflammatory cells and immune cells, and interfere overexpression of cytokines (including interleukins, TNFα, and interferon), reduce systemic inflammatory response and tissue damage, and play an antiviral and immune-enhancing role [117].
In this general environment, people are generally anxious and flustered. Mazza [118] reported that the proportion of rehabilitation patients suffering from depression and anxiety was 31 % and 42 % respectively. A large-scale cohort study showed that compared with other rehabilitation sequelae, the diagnosis rate of patients with mental diseases increased [119]. Depressed patients recovering from COVID-19 can have a serious impact on their quality of life due to a combination of illnesses involving multiple causes including immune dysfunction and elevated levels of inflammatory cytokines, as well as psychological factors such as sudden infection, advanced age, social isolation, and fear of disease recurrence, which can contribute to psychological disorders [120]. Based on the theory of etiology and pathogenesis in traditional Chinese medicine, although the pathogenic energy of COVID-19 has disappeared during the recovery period, the remaining pathogenic factors stagnate and heat up, causing burning of body fluids. Prolonged illness leads to depletion of qi and damage to yin, exacerbation of deficiency heat, and emotional fluctuations [121]. Ma [122] pointed out that the abnormal function of the five zang organs and seven emotions caused by the “plague” and the syndrome of yin deficiency and internal heat are the main causes of mental disorders in the rehabilitation of COVID-19. Thus, after COVID-19 rehabilitation, depression and “lily disease” sweating lead to the loss of yin fluid, worsening of deficiency heat, and mental unease. The pathogenesis and clinical symptoms are consistent. LBRAD, as a specialized treatment formula for post sweating symptoms of lily disease, conforms to the etiology and clinical characteristics of COVID-19 post rehabilitation depression. LBRAD combined with modern medical drugs or other therapies have achieved significant clinical efficacy in treating depression. By investigating 5 cases of insomnia caused by COVID-19 infection, Yu [123] reported that LBRAD combined with other TCM prescriptions has a good prognosis in alleviating infection symptoms and sleep disorders without obvious side effects. In addition, LBRAD pays attention to both the symptoms and the symptoms, leveraging the unique advantages of traditional Chinese medicine in treating pre illness and preventing relapse after recovery, improving post rehabilitation immunity, reducing and reducing repeated infections, and preventing pre illness [124]. It is expected to be a powerful treatment method for post rehabilitation depression in COVID-19.
10. Conclusions and perspectives
Due to the unclear understanding of the etiology and pathogenesis of depression, all the current treatment methods have defects such as high recurrence, high internal friction and many side effects. Finding standardized and targeted treatment for depression has always been a great challenge in modern clinical practice. Therefore, it is extremely important to develop drugs that can target the pathogenesis of depression, prevent or reverse the further development of depression in the early stage, and effectively relieve the symptoms of patients. Classical famous prescriptions are outstanding representatives of traditional Chinese medicine prescriptions, a summary of clinical experience in the past dynasties, and the most essential part of the great treasure house of traditional Chinese medicine, carrying the profound accumulation of the splendid civilization of traditional Chinese medicine for thousands of years. According to a recent study, LBRAD, a 2000-year-old classical of traditional Chinese medicine, is effective in treating depression with fewer side effects. It could be used as a new source of energy for the development of lead drugs for the treatment of depression, so as to obtain both safe and effective drugs for the treatment of depression.
A comprehensive review of the research status of LBRAD shows that modern clinical and experimental studies have not paid enough attention to the decoction method and dosage of traditional Chinese medicine, and there is also a lack of perfect evaluation criteria for its efficacy. Secondly, pharmacological studies are relatively few, and the direction is mostly limited to the study of the effective parts, active ingredients and the quality control of Lilium lancifolium bulb or Anemarrhena asphodeloides rhizome single medicine. There is a lack of systematic understanding of the active ingredients in the compound and the characteristics, rules and metabolic processes of the interactions among the components, and it is difficult to interpret the scientific connotation of their compatibility. In addition, pharmacological mechanism studies mainly focus on the direction of anti-depression, anti-anxiety, sedation and hypnosis, and mostly stay at the level of monoamine neurotransmitters in the central nervous system, and there is no complete explanation of pharmacological mechanism for clinical indications. Besides, although the formulation of LBRAD is simple, its chemical composition and efficacy may change with different processing techniques. For example, the difference of the fresh and dried Lilium lancifolium bulb and the different stir-frying methods of Anemarrhena asphodeloides rhizome LBRAD may cause differences in pharmacological effects. Moreover, the extraction of LBRAD effective ingredients has not been comprehensively compared with soaking time, extraction time, solvent concentration and other factors, so it is difficult to screen the optimal process. Finally, the effective ingredients in TCM prescriptions should be fully absorbed into plasma or target organs to exert the therapeutic effect. Currently, few experimental studies have conducted comparative studies on the pharmacokinetics of LBRAD in normal and depressed subjects. There is little recognition of the biological transformation of drugs in vivo under the two states. It is a major constraint to evaluate the clinical efficacy of LBRAD in the treatment of depression, improve the treatment plan and the secondary development of LBRAD.
At present, the exploration and innovation of TCM classical famous prescriptions have become the trend of medical development in the 21st century, and countries all over the world attach great importance to it. The Chinese government has also designated relevant laws and regulations as a strong guarantee for the development of classical classics. Secondly, with the development of modern science and technology, such as bioinformatics, network pharmacology, high throughput sequencing, high performance liquid chromatography, liquid chromatograms and mass spectrometry, the standardized quality control of classical prescriptions has been optimized, and the standard and targeted therapy paradigm of traditional Chinese medicine prescriptions has been successfully established. In addition, with the development of treatment technologies and the constant updating of novel drug delivery strategies, including nanodrug delivery technology, intervention research strategies may be developed for neurological diseases from the perspective of natural medicines for depression treatment [125]. In the context of big data and artificial intelligence, classical prescriptions combined with modern artificial intelligence (AI), network pharmacological research and evidence-based medicine to achieve multidisciplinary integration, innovative addition and subtraction treatment of traditional Chinese medicine will play an increasingly important role in the mechanism research of LBRAD's treatment of depression and the improvement of treatment plans. It is a key to open the door of standardization and modernization of TCM to carry out standardization research from multiple angles based on the theory system of classical prescription [126].
Institutional review board statement
The animal experiments covered in this review was conducted under the Guidelines of National Institutes of Health, USA for the Care and Use of Laboratory Animals and approved by the Animal Care and Use Committee of Shandong University of Traditional Chinese Medicine (SDUTCM201805311223).
We affirm that the above guidelines have always been followed in our research.
Data availability statement
Data will be made available on request.
CRediT authorship contribution statement
Wenchao Pan: Formal analysis. Huishan Shi: Resources. Zhiping Zang: Data curation. Qingwen Meng: Investigation. Yiran Cheng: Software. Lili Liang: Writing – original draft. Yuanhui Zhai: Investigation. Guoliang Yin: Project administration. Lingzhi Sun: Project administration. Ke Ma: Investigation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This study was granted by Shandong Provincial Natural Science Foundation (ZR2023QH052, ZR2020QH32, and ZR2021MH180), National Nature Science Foundation of China (81903948 and 82204795), Furthermore, it was also supported by special fund for high-level talent cultivation project of traditional Chinese medicine in Shandong Province (2023-143), Shanghai Science and Technology Development Foundation (2023–761027) and Shandong Province Universities' Development Plan for Youth Innovation Teams (2019-9-202 and 2022KJ34). All funding sources only supported the conduct of the experiments. We strictly disclosed that all funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e25171.
Contributor Information
Wenchao Pan, Email: pan1997eye@163.com.
Huishan Shi, Email: 1906197003@qq.com.
Zhiping Zang, Email: zhipingzang@sina.com.
Qingwen Meng, Email: honeymeng1987@163.com.
Yiran Cheng, Email: 943506971@qq.com.
Lili Liang, Email: lianglililucky@163.com.
Yuanhui Zhai, Email: 381153150@qq.com.
Guoliang Yin, Email: whathemamba@163.com.
Lingzhi Sun, Email: slzsunny@126.com.
Ke Ma, Email: make19880710@163.com.
Glossary
- LBRAD
Lilium lancifolium bulb and Anemarrhena asphodeloides rhizome Decoction
- COVID-19
Novel coronavirus pneumonia
- CNKI
China National Knowledge Infrastructure
- ADMET
Absorption-distribution-metabolism-elimination-toxicity
- HPA
Hypothalamo-pituitary-adrenal
- 5-HT
Serotonin
- NE
Norepinephrine
- DA
Dopamine
- BDNF
Brain-derived neurotrophic factor
- KP
Kynurenine pathway
- TCM
Traditional Chinese medicine
- SPT
Sucrose water preference test
- FST
Forced swimming test
- TST
Tail suspension test
- HAMD
Hamilton Depression Scale
- AIS
Athens Insomnia Scale
- FSH
Follicle-stimulating hormone
- LH
Luteinizing hormone
- ACTH
Adrenocorticotropic hormone
- CORT
Corticosterone
- EEG
Electroencephalograph
- ADL
Activities of daily living scale
- CUMS
Chronic unpredictable mild stress
- GIU
Glutamic acid
- HIF-1
Hypoxia inducible factor-1
- UPLC-QTOF-MS
Ultra-performance liquid chromatography/quadrupole time-of-flight mass spectrometry
- SD
Sprague-Dawley
- CGRP
Calcitonin gene-related peptide
- VIP
Vasoactive intestinal peptide
- PC12
Rat adrenal medulla pheochromocytoma
- NG
Neomangiferin
- MG
Mangiferin
- RA
Regaloside A
- RI
Regaloside I
- TCMSP
Traditional Chinese Medicine Systems Pharmacology
- OMIM
Online Mendelian Inheritance in Man
- PPI
Protein protein interaction
- KEGG
Kyoto encyclopedia of genes and genomes
- GO
Gene Ontology
- BP
Biological process
- CC
Cellular component
- MF
Molecular function
- AI
Artificial Intelligence
- ESR1
Estrogen receptor 1
- MAOA
Monoamine oxidase A
- NR3C1
Nuclear receptor subfamily 3 group C member 1 Gene
- VEGFA
Vascular Endothelial Growth Factor A
- mTOR
Mammalian target of rapamycin
- AKT1
AKT Serine/Threonine Kinase 1
- TNF
Tumor Necrosis Factor
- TP53
Tumor Protein P53
- PTGS2
Prostaglandin-Endoperoxide Synthase 2
- JUN
Jun Proto-Oncogene, AP-1 Transcription Factor Subunit
- VEGFA
Vascular Endothelial Growth Factor A
- CASP3
Caspase 3
- ESR1
Estrogen Receptor 1
- PPARG
PPARG Coactivator 1 Alpha
- CAT
Catalase
- PI3K/Akt
Phosphatidylinositol-3-kinase/Protein kinase B
- PI3K/Akt/GSK-3β
Phosphatidylinositol-3-kinase/Protein kinase B/Glycogen synthase kinase-3β
- cAMP/PKA/CREB/BDNF
Cyclic adenosine monophosphate/Protein kinase A/Cyclic adenosine monophosphate response element binding protein/Brain-derived neurotrophic factor
- CaM/CaMKⅡ/CREB/BDNF
Calmodulin/Calmodulin-dependent protein kinase II/Cyclic adenosine monophosphate response element binding protein/Brain-derived neurotrophic factor
- MAPK/PKC/MEK/ERK1/2/CREB/BDNF
Mitogen-activated protein kinase/Protein kinase C/Mitogen-activated protein kinase kinase/Extracellular signal-regulated kinase 1/2/Cyclic adenosine monophosphate response element binding protein/Brain-derived neurotrophic factor
Appendix A. Supplementary data
The following is the Supplementary data to this article.
figs1.
References
- 1.Yin Y.Y., Liu J.L., Wang J.P., Zhu Y.B., Li Y.Z., Lu W.H. Research progress in pathogenesis of depression. Med. Recapitulate. 2022;28:2368–2372. [Google Scholar]
- 2.Wang L.W., Huang D.H., Qin X.M., Du G.H., Zhou Y.Z. Advances in the pathogenesis of depression based on PBMCs multiomics technique. Pharm. Clinic. Chin. Med. 2022;38:206–212. [Google Scholar]
- 3.Xu Q.K., Hao G.S. Research progress on the relationship between depressive disorder and kynurenine pathway and its metabolites. J. Neuro. Mental. Health. 2022;22:139–143. [Google Scholar]
- 4.Tian M., Zheng D., Liu C.L. Research progress on the involvement of intestinal microbes in the pathogenesis of depression. J. Clinical. Military. Med. 2022;50:658–660. [Google Scholar]
- 5.Chi X.S., Wang S.J., Baloch Z., Zhang H.X., Li X.Y., Zhang Z., Zhang H.L., Dong Z.F., Lu Y., Yu H.Y., Ma K. Research progress on classical traditional Chinese medicine formula Lily Bulb and Rehmannia Decoction in the treatment of depression. Biomed. Pharmacother. 2019;112 doi: 10.1016/j.biopha.2019.108616. [DOI] [PubMed] [Google Scholar]
- 6.Liu X.Y., Ran L.Y., wang W. Research progress of depression and insulin resistance. J. Psychol. 2022;35:198–200. [Google Scholar]
- 7.Bian H.T., Wang G.H., Xiao L., Wang H.L. Research progress of cytokines and inflammatory pathogenesis of depression. J. Neuro. Mental. Health. 2020;20:153–156. [Google Scholar]
- 8.Liu C., Wang Y.H., Zhao H.Q., Zou M.S., Ling J. Research advances in microbiota-gut-brain Axis and depression. Med. Recapitulate. 2022;28:224–228. [Google Scholar]
- 9.Liu X., Hong H. Progress in studies of Glutamate ⁃ glutamine cycle in the pathogenesis of depression. Pharm. Today. 2022;32:206–210. [Google Scholar]
- 10.Wang L., Zhang X.J., Jin L.M., Yang H.J. Progress in Antidepressants, Chem. World. 2022;63:83–93. [Google Scholar]
- 11.Wang C.F., Tian W.G., Chen J.P., Ren T., Gai X.H., Liu Y., Tian C.W. Research progress on antidepressive effect and mechanism of traditional Chinese medicine. Chin. Tradit. Herb. Drugs. 2022;53:2890–2901. [Google Scholar]
- 12.Xu X.J., Li T.Y., Fan W.D., Ma Y.X., Zhang Y., Qi Z.T., Sun Q., Xie L. Research survey of Traditional Chinese Medicine cmpound therapy for depression. Med. Recapitulate. 2021;27:3687–3693. [Google Scholar]
- 13.Yu B.Q., Shao X.X., Fu X.F., Zhou M.J., Chen C. Study on composition characteristics and mechanism of anti-depression traditional Chinese medicine compound based on literature mining and correlation analysis. Chin. Tradit. Herb. Drugs. 2021;52:3344–3352. [Google Scholar]
- 14.Li B., Zhang L., Zhan Z.L., Zhang W., Peng H.S., Xu H.Y., Zhang H.M. Discussion on common problems of historical evolution of famous classical formulas and its textural research of key information, chin. J. Exper. Tradit. Med. Formulae. 2023;29:1–8. [Google Scholar]
- 15.Wang H.L. Trace to the source of depression in traditional Chinese medicinal literature. J. Liaoning. Univ. Chin. Med. 2012;14:177–178. [Google Scholar]
- 16.Liu Q.X., Ma X.L. Analys is of depression-related emotional diseases. Chin. Arch. Tradit. Chin. Med. 2010;28:866–868. [Google Scholar]
- 17.Liang Z.H. College of Traditional Chinese Medicine Guangxi University of Tradit Chin Med; Guangxi: 2016. The Ancient and Contemporary Researches of Application Compatibility of Eight Influential Points; pp. 37–39. [Google Scholar]
- 18.Han T.Z., Sun L.Y., Wu Y.F. Analysis of related diseases of depression in ancient books. Information. Tradit. Chin. Med. 2011;28:5–6. [Google Scholar]
- 19.Yu J.Y., Tian J.Z. Related knowledge of TCM literature on depression. J. Shandong Univ. Tradit. Chin. Med. 2012;36:187–189. [Google Scholar]
- 20.Tian X.S. Discussion on the corresponding relationship between depression and TCM related diseases. J. New. Chin. Med. 2007:97–98. [Google Scholar]
- 21.Xiao Y., Zhao Z.F. The understanding and treatment of depression in traditional Chinese medicine, Beijing. J. Tradit. Chin. Med. 2008:740–742. [Google Scholar]
- 22.Zhang J., Yang Z.N. Modern research progress of traditional Chinese medicine treatment for lily disease. Shandong J. Tradit. Chin. Med. 2022;41:1244–1249. [Google Scholar]
- 23.Zhang Q., Zhang L.J., Liu Y., Tian X., Li X.Y., Han B.B., Zhang Y.N., Wu Z.C., Yu H.Y., Zhao H.J., Wang S.J., Ma K., Wang Y. Research progress on the pharmacological effect and clinical application of Tongqiao Huoxue Decoction in the treatment of ischaemic stroke. Biomed. Pharmacother. 2021;138 doi: 10.1016/j.biopha.2021.111460. [DOI] [PubMed] [Google Scholar]
- 24.Hu G.H. Overview of clinical application of Baihe zhimu decoction. Guangming J of Chin med. 2020;35:1604–1606. [Google Scholar]
- 25.Committee N.P. China Medical Science and Technology Publishing house; Beijing: 2020. The 2020 Edition of the Pharmacopoeia of the People's Republic of China (Chinese Pharmacopoeia 2020 Edition) [Google Scholar]
- 26.Zhao X.L. Clinical study on the treatment of depression by Ganmai Dazao decoction and Baihe zhimu decoction. Asian-Pacific. Tradit. Med. 2017;13:157–158. [Google Scholar]
- 27.Feng L., Qi Z.X., Yao Z., Wei D.B., Yu L., Ye Z.X., Gao J. Clinical effect of Ganmai Dazao decoction and Baihe zhimu decoction combined with psychotherapy in the treatment of depression. Chin. Arch. Tradit. Chin. Med. 2021;39:169–172. [Google Scholar]
- 28.Yuan Z.S., Zhang B.G. Central Plains Medical J; 2000. Baihe Zhimu Anshen Decoction in the Treatment of 46 Cases of Insomnia in the Elderly Due to Yin Deficiency and Fire Exuberance; pp. 55–56. [Google Scholar]
- 29.Fang X.S. A report of treating 52 cases of insomnia with the Baihe Dihuang Zhimu decoction plus the Ganmai Dazao decoction. Clin J Chin Med. 2012;4:90. [Google Scholar]
- 30.Liu Y. Clinical analysis of Lily Zhimu Dihuang decoction and Suanzaoren decoction in the treatment of hyperthyroidism and insomnia. J of Prac Trad Chin Med. 2018;34:525–526. [Google Scholar]
- 31.Chen Z., Ding L.W. Clinical observation on treating 40 cases of depression with the Chaihu plus Longgu Muli decoction and lily anemarrhena decoction. Clin J Chin Med. 2012;4:38–39. [Google Scholar]
- 32.Wang Y.Z., Shi G.Z. 20 cases of long-term low fever treated with modified Xiaochaihu decoction and Baihe Zhimu decoction. Henan Tradit Chin Med. 1997:333. [Google Scholar]
- 33.Gao X.F., Liu S. Liu Sheng's experience in using Baihe Zhimu Decoction to treat breast disease. Liaoning J of Trad Chin Med. 2006:1068–1069. [Google Scholar]
- 34.Zhang T.Y., Yang K., Lu G.L., Dong P.P., Zeng Q.Q. "Synopsis of the Golden Chamber" clinical clinical application of lily prescriptions in andrology. Shandong J. Tradit. Chin. Med. 2021;40:762–764. [Google Scholar]
- 35.Ma L.J., Jiang Z.W., Ran C.L., Chen S.C. Collection status of Chinese patent medicines for children in the Chinese pharmacopoeia (2020 edition, volume I) China Pharm. 2021;30:6–8. [Google Scholar]
- 36.Yin X.B., Qu C.H., Dong X.X., Shen M.R., Ni J. Preparation regularity of Chinese patent medicine in Chinese Pharmacopoeia (2020 edition. China J. Chin. Mater. Med. 2022;I(47):4529–4535. doi: 10.19540/j.cnki.cjcmm.20220419.601. [DOI] [PubMed] [Google Scholar]
- 37.Chi X.S., Zhao H.J., Wang Y., Ma K. Modernization development of classical traditional Chinese medicine formulation based on literature verification and material benchmark evaluation. Chin J of Trad Chin Med and Pharm. 2021;36:643–647. [Google Scholar]
- 38.Chen L.M., Liu S.Y., Zhang L., Fu Y.L. Comparison of the difference on total dose between classical prescription and modern prescription of traditional Chinese medicine. Chin. J. Tradit. Chin. Med. Pharm. 2015;30:735–738. [Google Scholar]
- 39.Zhang H.F. Nanjing University of Chinese Medicine, Nanjing Univer of Chin Med; Jiangsu: 2007. Study on Chemical Constituents and Pharmacodynamic Mechanism of Lily. [Google Scholar]
- 40.Li H.J. Northwest Agriculture and Forestry University, Nor Agr and For Univer; Shanxi: 2007. Research on Nutritional Components, Active Substances and Cultivation Characteristics of Lily Officinale. [Google Scholar]
- 41.Ai Q.Y., Kang S.Y., Zhao Y.F. Research and application of Chinese medicine lily. J of Yan 'an Univer(Med Sci) 2016;14:63–65. [Google Scholar]
- 42.Feng F. A review on pharmacological effects of Rhizoma Anemarrhenae. Clinical. Resear. Tradit. Chin. Med. 2017;9:133–137. [Google Scholar]
- 43.Dai T., Li G.Y., Xu M.H. The historical evolution and modern research on the processing method of Cicadas. Chin. Tradit. Pat. Med. 2020;42:3255–3258. [Google Scholar]
- 44.Zhao X.Q., Huang X.J., Xu L., Gao P., Wen Y.S., Zhou S.Y. Herbalogical research and field study of Anemarrhena asphodeloides beg, Aisa-Pacific. Tradit. Med. 2019;15:77–79. [Google Scholar]
- 45.Li Y.M., Jiang L.D. A humble opinion on the conversion of prescription weight. J. Tradit. Chin. Med. 2010;51:7–9. [Google Scholar]
- 46.Shi J.X., Shi X.G. Preliminary study on conversion and usage of prescription quantity in ancient and modern times. Jiangxi. J. Tradit. Chin. Med. 2016;47:18–20. [Google Scholar]
- 47.Hao W.S. Han Dynasty system of weights and measures and the conversion of prescription medicine, Modern. Dis. Edu. Chin. Tradit. Med. 2005;3:48–51. [Google Scholar]
- 48.Kang L.J., Yang X.J., Ding N.N., Li Y.D., Zhou E.H., Zhang N., Xu E.P. Research progress on Baihe zhimu decoction. Chin. Arch. Tradit. Chin. Med. 2023;42:132–137. [Google Scholar]
- 49.Liu Z.M. Influence of Baihe zhimu decoction combined with vortioxetine on patients with depression. Chin. Foreign. Med. Resear. 2021;19:131–133. [Google Scholar]
- 50.Jin Y.M. Clinical observation of Baihe Zhimu decoction combined with Ganmai Dazao decoction and fluoxetine hydrochloride in the treatment of depression. Chin. Folk. Therapy. 2018;26:73–74. [Google Scholar]
- 51.Ding N. Treatment of 50 cases of climacteric syndrome of yin deficiency of liver and kidney with Baihe zhimu decoction. Henan. Tradit. Chin. Med. 2015;35:24–25. [Google Scholar]
- 52.Zheng L., Sun Y., Liang X.L., Tian Y., Lu S., Song D. Curative effect analysis of Baihe zhimu decoction on perimenopausal depression. J. Sichuan. Tradit. Chin. Med. 2020;38:162–165. [Google Scholar]
- 53.Ji Q.Z., Zhang W., Li H.Y. Effect of Baihe zhimu decoction combined with EEG bionic electrical stimulator in the treatment of post-stroke depression. J. Changchun. Univ. Chin. Med. 2022;38:998–1001. [Google Scholar]
- 54.Zhang H.W., Xing H.Y. Clinical effect of Baihe Zhimu decoction combined with acupuncture at Yuyuan point on senile post-stroke depression. Chin. J. Geronto. 2020;40:5001–5004. [Google Scholar]
- 55.Zhou Q., Zhao X.Y., Pang B., Peng Z.P. Professor tong xiaolin's experience in applying lily dihuang decoction and lily zhimu decoction analyse. J. Emerg. Tradit. Chin. Med. 2013;22:581–582. [Google Scholar]
- 56.Jia D., Chen Y.C., Chen D., Rong X.L., Gao Y., Li W.M. Antidepressant efficacy studies on Lily Zhimu decoction. Nor. Pharm. 2014;11:4–6. [Google Scholar]
- 57.Liu Q., Yuan L., Li D.S., Wu J.H., Zhang Z.H., Lu Y.J., Wang S.Y. Baihe zhimu decoction on depression Rats'Behavior and monoamine neurotransmitters. Chin. Arch. Tradit. Chin. Med. 2016;34:1729–1732. [Google Scholar]
- 58.Yang L., Gao Y., Jia D., Li W.M. Effect of Baihe zhimu decoction on depressive rats fed by high-fat diet. Tradit. Chin. Drug Res. Clin. Pharmacol. 2016;27:376–380. [Google Scholar]
- 59.Li Z.W., Jia D., Dang Y.X., Gao Y., Li W.M. Mechanism of saponins of Baihe zhimu tang in treating major depression by regulating 5-HT function. Chin. J. Exp. Tradit. Med. Formulae. 2018;24:131–138. [Google Scholar]
- 60.Yuan L., Liu Q., Fan Z., Li D.S., Wu J.H., Zhang Z.H., Lu Y.J., Han Y.M. Effect of Baihe Zhimu decoction on key molecules in calmodulin signaling pathway in hippocampus of depressed rats and its antidepressant mechanism. J. Jilin. Univ (Med Edit) 2016;42:704–710+845. [Google Scholar]
- 61.Chen D. Guangzhou University of Tradit Chin Med; Guangzhou: 2015. Based on the Brain-Gut Interaction Theory Preliminary Study the Treatment Mechanism of Lily Saponin and Timosaponin on Rats with Depression Accompanied IBS College of Traditional Chinese Medicine; pp. 15–36. [Google Scholar]
- 62.Li D.S., Yuan L., Liu Q., Wu J.H., Zhang Z.H., Lu Y.J. Effect of Baihe zhimu decoction on cAMP signal transduction pathway of depression rats. J. Wuhan Univ. (Nat. Sci. Ed.) 2015;36:867–871. [Google Scholar]
- 63.Yuan L., Li D.S., Wu J.H., Han Y.M. Effect of Baihe zhimu decoction to depression on behavior and expression of BDNF/TrKB in Hippocampus. Chin. arch. Tradit. Chin. Med. 2016;34:2941–2944. [Google Scholar]
- 64.Cao Q.S., Li D.S., Yuan L., Wu J.H., Han Y.M. Influence of Baihe zhimu decoction in leveles of key factors of ERK1/2 singaling pathway in hippocapus tissues of depression rats. Chin. Arch. Tradit. Chin. Med. 2017;35:3154–3157. [Google Scholar]
- 65.Zhang R.Z., Zhu X., Bai H., Ning K. Network pharmacology databases for traditional Chinese medicine: review and assessment. Front. Pharmacol. 2019;10:123. doi: 10.3389/fphar.2019.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Corson T.W., Crews C.M. Molecular understanding and modern application of traditional medicines: triumphs and trials. Cell. 2007;130:769–774. doi: 10.1016/j.cell.2007.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang G.B., Li Q.Y., Chen Q.L., Su S.B. Network pharmacology: a new approach for Chinese herbal medicine research. Evid. Based. Comp. Alter. Med. 2013;2013 doi: 10.1155/2013/621423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang X., Wang Z.Y., Zheng J.H., Li S. TCM network pharmacology: a new trend towards combining computational, experimental and clinical approaches. Chin. J. Nat. Med. 2021;19:1–11. doi: 10.1016/S1875-5364(21)60001-8. [DOI] [PubMed] [Google Scholar]
- 69.Li S., Zhang B. Traditional Chinese medicine network pharmacology: theory, methodology and application. Chin. J. Nat. Med. 2013;11:110–120. doi: 10.1016/S1875-5364(13)60037-0. [DOI] [PubMed] [Google Scholar]
- 70.Zhao Q., Pan W., Shi H. Network pharmacology and molecular docking analysis on the mechanism of Baihe Zhimu decoction in the treatment of postpartum depression. Medicine (Baltim.) 2022;101 doi: 10.1097/MD.0000000000029323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang H.Q., Liu H.T., Wang L., Min L., Chen B., Li H. Uncovering the active components, prospective targets, and molecular mechanism of Baihe Zhimu decoction for treating depression using network pharmacology-based analysis. J. Ethnopharmacol. 2021;281 doi: 10.1016/j.jep.2021.114586. [DOI] [PubMed] [Google Scholar]
- 72.Wang B.L., Liu Z.Q., Chen C.L. Network pharmacology study of anti-depression mechanism of Baihe zhimu tang. J. Pharm. Chin. 2018;53:988–995. [Google Scholar]
- 73.Du H.L. PLA Navy Medical University, Sec Military Med University; Shanghai: 2016. Metabolomic Study on the Anti-depressant Effects of Zhimu and Baihe; pp. 21–37. [Google Scholar]
- 74.Liu Z.R., Yang B., Liu F., Guo Y.L., Xia P.Y. A metabolomic study of Baihe Zhimu decoction in a rat model of depression. J. Thir. Militar. Med. Univ. 2019;41:1917–1925. [Google Scholar]
- 75.Zhang H.X., Xue X.Y., Pan J., Song X.B., Chang X., Mao Q.C., Lu Y.T., Zhao H.J., Wang Y., Chi X.S., Wang S.J., Ma K. Integrated analysis of the chemical-material basis and molecular mechanisms for the classic herbal formula of Lily Bulb and Rehmannia Decoction in alleviating depression. Chin. Med. 2021;16:107. doi: 10.1186/s13020-021-00519-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Qin K.M., Fang Q.B., Cai H., Li W.D., Cai B.C. HPLC fingerprints of Baihe Zhimu Decoction and its correlation to single herb. Chin. J. Chromatogr. 2009;27:781–786. [PubMed] [Google Scholar]
- 77.Wang Y. Extraction technology and anti-depression activity of saponins from lilium brownii. Med. Plants. 2014;5:46–48. [Google Scholar]
- 78.Peng X.J., Yang X.J., Chen Y.B., Lu L., Xu H.Y., Xu H.Y., Ding T., Liu F. Action mechanism of Baihe Dihuang decoction on depression based on integrative pharmacology of traditional Chinese medicine. J. Chin. Tradit. Med. 2018;43:1338–1344. [Google Scholar]
- 79.Zhang H.X., Chi X.S., Pan W.C., Wang S.J., Zhang Z., Zhao H.J., Wang Y., Wu Z.C., Zhou M.M., Ma S., Zhao Q.T., Ma K. Antidepressant mechanism of classical herbal formula lily bulb and Rehmannia decoction: insights from gene expression profile of medial prefrontal cortex of mice with stress-induced depression-like behavior. Gene Brain Behav. 2020;19 doi: 10.1111/gbb.12649. [DOI] [PubMed] [Google Scholar]
- 80.Zhao Y., Wang S.J., Pan J., Ma K. Verbascoside: a neuroprotective phenylethanoid glycosides with anti-depressive properties. Phytom. 2023;120 doi: 10.1016/j.phymed.2023.155027. [DOI] [PubMed] [Google Scholar]
- 81.Pan W.C., Pan J., Xue X.Y., Lu Y.T., Wang Y., Ma M.H., Chi X.S., Zhou X.Y., Ma K. Study on the chemical composition of modern prescription of Baihe Dihuang Decoction. Lishizhen Med and Materia Medica Res. 2021;32:1884–1888. [Google Scholar]
- 82.Huang J.J. College of Traditional Chinese Medicine Guangzhou University of Tradit Chin Med; Guangzhou: 2011. Studies on Quality Standard and Antidepressant Effect of the Effective Parts in Bulbus Lilii; pp. 37–53. [Google Scholar]
- 83.Guo Q.P. College of Traditional Chinese Medicine Guangzhou University of Tradit Chin Med; Guangzhou: 2009. Studies on Quality Standard and Antidepression Effect of Lilium Brownii; pp. 41–55. [Google Scholar]
- 84.Fu C.Y., Liu Y.H., Li M.J., Wang X.H., Yin W.Q. Extraction and purification techniques and antidepression activity of total saponins from bulbs of lilium brownii. Nat. Product. Resear. Deve. 2012;24:682–686. [Google Scholar]
- 85.Gao S.Y. College of Traditional Chinese Medicine Guangzhou University of Tradit Chin Med; Guangzhou: 2013. Quality Standard Research of the Total Saponins of Lily and Discussing on Anti-depression Accompanied with IBS; pp. 66–81. [Google Scholar]
- 86.Zhao D.H., Zheng L.W., Qi L., Wang S.R., Guan L.P., Xia Y.N., Cai J.H. Structural features and potent antidepressant effects of total sterols and β-sitosterol extracted from sargassum horneri. Mar. Drugs. 2016;14 doi: 10.3390/md14070123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yadav M., Parle M., Jindal D.K., Dhingra S. Protective effects of stigmasterol against ketamine-induced psychotic symptoms: possible behavioral, biochemical and histopathological changes in mice. Pharmacol. Rep. 2018;70:591–599. doi: 10.1016/j.pharep.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 88.Wang P.Y., Li J., Attia F.A.K., Kang W.Y., Wei J.F., Liu Z.H., Li C.Q. A critical review on chemical constituents and pharmacological effects of Lilium. Food Sci. Hum. Wellness. 2019;8:330–336. [Google Scholar]
- 89.Zhong M., Tian X.T., Chen S.J., Chen M.C., Guo Z.Q., Zhang M.N., Zheng G.P., Li Z.X., Shi Z.P., Wang G.H., Gao H.G., Liu F., Huang C.G. Identifying the active components of Baihe-Zhimu decoction that ameliorate depressive disease by an effective integrated strategy: a systemic pharmacokinetics study combined with classical depression model tests. Chin. Med. 2019;14:37. doi: 10.1186/s13020-019-0254-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jiang Y.X., Jiang D.C., Chen L., Su Y., Weng L.L. Study on correlation between content and color of three flvonoids in zhimu(anemarrhena asphodeloides), chin. Arch. Tradit. Chin. Med. 2020;38:198–202. [Google Scholar]
- 91.Gong X.Y., Chang L.J., Li M.Y., Wei H.H., Chen X. Study on the correlation between the contents of active components and characters of anemarrhenae rhizoma and its grade standard. J. Chin. Med. Mater. 2021;44:567–573. [Google Scholar]
- 92.Lu M.Z., Zhang Z.Q., Yi J., Chen W.S., Hou Z.H., Li T.J. Study on the effect and mechanisms of timosaponin B-Ⅱ antidepressant. J. Pharm. Pract. 2010;28:283–287. [Google Scholar]
- 93.Bai H.D., Zhang Z.D., Su H.L., Li Y.X., Kuang H.X., Wang Q.H. Research progress on the influence of processing on chemical constituents and pharmacological effects of Anemarrhena asphodeloides. China Pharm. 2021;32:2159–2163. [Google Scholar]
- 94.Jangra A., Lukhi M.M., Sulakhiya K., Baruah C.C., Lahkar M. Protective effect of mangiferin against lipopolysaccharide-induced depressive and anxiety-like behaviour in mice. Eur. J. Pharmacol. 2014;740:337–345. doi: 10.1016/j.ejphar.2014.07.031. [DOI] [PubMed] [Google Scholar]
- 95.Lim S.M., Kang G.D., Jeong J.J., Choi H.S., Kim D.H. Neomangiferin modulates the Th17/Treg balance and ameliorates colitis in mice. Phytomedicine. 2016;23:131–140. doi: 10.1016/j.phymed.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 96.Marquez L., Garcia-Bueno B., Madrigal J.L., Leza J.C. Mangiferin decreases inflammation and oxidative damage in rat brain after stress. Eur. J. Nutr. 2012;51:729–739. doi: 10.1007/s00394-011-0252-x. [DOI] [PubMed] [Google Scholar]
- 97.Lu W.Q., Qiu Y., Li T.J., Tao X., Sun L.N., Chen W.S. Timosaponin B-II inhibits pro-inflammatory cytokine induction by lipopolysaccharide in BV2 cells. Arch Pharm. Res. (Seoul) 2009;32:1301–1308. doi: 10.1007/s12272-009-1916-4. [DOI] [PubMed] [Google Scholar]
- 98.Lei X., Dong W.T., Bi X.Y., Su X.L., Xia Y.G., Wang Q.H., Kuang H.X. Therapeutic material basis of chemical subdivisions of anemarrhenae rhizoma on anti-inflammatory and immunomudulatory effects. J. Chin. Med. Mater. 2015;38:1904–1907. [PubMed] [Google Scholar]
- 99.Kwon O.K., Lee M.Y., Yuk J.E., Oh S.R., Chin Y.W., Lee H.K., Ahn K.S. Anti-inflammatory effects of methanol extracts of the root of Lilium lancifolium on LPS-stimulated Raw264.7 cells. J. Ethnopharmacol. 2010;130:28–34. doi: 10.1016/j.jep.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 100.Lee E., Yun N., Jang Y.P., Kim J. Lilium lancifolium Thunb. extract attenuates pulmonary inflammation and air space enlargement in a cigarette smoke-exposed mouse model. J. Ethnopharmacol. 2013;149:148–156. doi: 10.1016/j.jep.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 101.Ghosh S., Kumar A., Sachan N., Chandra P. Evaluation of the antidepressant-like effect of total sterols fraction and stigmasterol isolated from leaves of aegle marmelos and possible mechanism(s) of action involved. Curr. Drug Discov. Technol. 2022;19 doi: 10.2174/1570163818666210729165310. [DOI] [PubMed] [Google Scholar]
- 102.Gu S., Mou T.T., Chen J., Wang J., Zhang Y., Cui M.R., Hao W.Q., Sun Y., Zhang C.Q., Zhao T.T., Wei B.B. Develop a stepwise integrated method to screen biomarkers of Baihe-Dihuang Tang on the treatment of depression in rats applying with composition screened, untargeted, and targeted metabolomics analysis. J. Separ. Sci. 2022;45:1656–1671. doi: 10.1002/jssc.202100841. [DOI] [PubMed] [Google Scholar]
- 103.Du H.L., Wang K.Q., Su L., Zhao H.X., Gao S.Y., Lin Q.S., Ma X.F., Zhu B.K., Dong X., Lou Z.Y. Metabonomic identification of the effects of the Zhimu-Baihe saponins on a chronic unpredictable mild stress-induced rat model of depression. J. Pharm. Biomed. Anal. 2016;128:469–479. doi: 10.1016/j.jpba.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 104.Zhang Q., Guo F., Fu Z.W., Zhang B., Huang C.G., Li Y. Timosaponin derivative YY-23 acts as a non-competitive NMDA receptor antagonist and exerts a rapid antidepressant-like effect in mice. Acta Pharmacol. Sin. 2015;37:166–176. doi: 10.1038/aps.2015.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yin Y.X., Liu X.F., Liu J.P., Cai E.B., Zhao Y., Li H.J., Zhang L.X., Li P.Y., Gao Y.G. The effect of beta-sitosterol and its derivatives on depression by the modification of 5-HT, DA and GABA-ergic systems in mice. RSC Adv. 2018;8:671–680. doi: 10.1039/c7ra11364a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhao Q.Q., Li X., Zeng M.L., Huang X.L., Yu H.Y. A network pharmacology based study of regulation effects of the main active components in honghua injection on cerebrovascular disease network. J. Pharm. China. 2015;50:1402–1407. [Google Scholar]
- 107.Zhang Y., Wu Z.N., Shu Y., Wang F., Cao W.J., Li W.H. A novel bioactive vaterite-containing tricalcium silicate bone cement by self hydration synthesis and its biological properties. Mater. Sci. Eng., C. 2017;79:23–29. doi: 10.1016/j.msec.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 108.Yuan W.F., Tu M.Y., Chen C., Wang S.M., Liang S.W. Network pharmacology study of compound danshen dropping pill based on molecular docking and recognition of biological network function module. J. Pharm. Chin. 2017;52:743–749. [Google Scholar]
- 109.Meng X.L., Liu X.N., Zhang X., Chen C.L. Study on the mechanisms of chemical components for Lotus (Nelumbo nucifera gaertn.) seed embryo in preventing and treating alzheimer's disease based on network pharmacology. J. Liaoning Univ. (Nat. Sci. Ed.) 2021;48:289–299. [Google Scholar]
- 110.Sun J.S. The COVID-19 outbreak and Global governance reform. World. Eco. Politics. 2020;71 95+157-158. [Google Scholar]
- 111.Carfi A., Bernabei R., Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Soriano J.B., Murthy S., Marshall J.C., Relan P., Diaz J.V., Condition W.H.O.C.C.D.W.G.o.P.-C.- A clinical case definition of post-COVID-19 condition by a Delphi consensus, Lancet. Inf. Disp. 2022;22:e102–e107. doi: 10.1016/S1473-3099(21)00703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mahase E. Covid-19: what do we know about "long covid"? BMJ. 2020;370:m2815. doi: 10.1136/bmj.m2815. [DOI] [PubMed] [Google Scholar]
- 114.Sykes D.L., Holdsworth L., Jawad N., Gunasekera P., Morice A.H., Crooks M.G. Post-COVID-19 symptom burden: what is long-COVID and how should we manage it? Lung. 2021;199:113–119. doi: 10.1007/s00408-021-00423-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ran C.Y., Wu X.B., Yang X.Q., Yang F., Li Y.H., Xu S.C. Analysison the rehabilitation of COVID-19 from the perspective of lily disease. Chin. J. Ethnomed. Ethnopharmacy. 2021;30:90–94. [Google Scholar]
- 116.Qi X.Y., Li B.L., Omarini A.B., Gand M., Zhang X.L., Wang J. Discovery of TCMs and derivatives against the main protease of SARS-CoV-2 via high throughput screening, ADMET analysis, and inhibition assay in vitro. J. Mol. Struct. 2022;1268 doi: 10.1016/j.molstruc.2022.133709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Shen X.H., Yin F.G. The mechanisms and clinical application of Traditional Chinese Medicine Lianhua-Qingwen capsule. Biomed. Pharmacother. 2021;142 doi: 10.1016/j.biopha.2021.111998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mazza M.G., De Lorenzo R., Conte C., Poletti S., Vai B., Bollettini I., Melloni E.M.T., Furlan R., Ciceri F., Rovere-Querini P., group C.-B.O.C.S., Benedetti F. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA, Lancet. Psychiatry. 2021;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Li N., Wang Z., Bao Y.L., Tang H.R., Huang J., Ding X.H., Zhang J.C. COVID⁃19 sequelae: clinical features and research progress. J. Hainan. Med. Univ. 2022;28:1041–1049. [Google Scholar]
- 121.Huang Y.H., Tan H.X., Zou F.J., Zhao C.L. Treatment of the sequelae of corona virus disease 2019 during the convalescence based on traditional Chinese medicine theory and classic prescriptions. Chin. Manipul. Rehab. Med. 2022;13:5–9. [Google Scholar]
- 122.Ma K., Wang X., Feng S.Y., Xia X.S., Zhang H.X., Rahaman A., Dong Z.F., Lu Y.T., Li X.Y., Zhou X.Y., Zhao H.J., Wang Y., Wang S.J., Baloch Z. From the perspective of Traditional Chinese Medicine: treatment of mental disorders in COVID-19 survivors, Biomed. Pharma. 2020;132 doi: 10.1016/j.biopha.2020.110810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yu X. Five medical cases of insomnia caused by novel coronavirus infection were treated with lily disease prescriptions in Synopsis of Golden Chamber. China's Naturopathy. 2023;31:122–125. [Google Scholar]
- 124.Li L.L., Song Y.Y., Hu X.Y., Jiao X., Tang J.Y., Lu Y. Preliminary study on the clinical scheme of traditional Chinese medicine promoting the rehabilitation of patients with novel coronavirus infection. Pharm. Clinics. Chin. Materia. Med. 2021;37:2–6. [Google Scholar]
- 125.Yuan S., Ma T., Zhang Y.N., Wang N., Baloch Z., Ma K. Novel drug delivery strategies for antidepressant active ingredients from natural medicinal plants: the state of the art. J. Nanobiotechnol. 2023;21 doi: 10.1186/s12951-023-02159-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lin S.Y., Zhu W.P., Cao L.Y. Discussion on new ideas of TCM standardization from the theoretical characteristics of classical prescriptions. J. Tradit. Chin. Med. 2017;58:2080–2083. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.