Abstract
Background
Fungal opportunistic infections in burn wound patients are among the leading cause of morbidity and mortality. Attention remains focused on preventing bacterial infection at the expense of increasing fungal infection in burn wound patients.
Objective
To determine the occurrence of common fungi in admitted burn wound patients and their environment: and their antifungal susceptibility patterns at the University Teaching Hospitals, Lusaka, Zambia.
Methods
This laboratory-based cross-sectional study enrolled a total 101 participants whose pus swab specimens were collected from their burn wounds as well as 50 environmental swabs collected from strategic points. Wet mount, gram stain, culture on Sabouraud dextrose agar, Corn meal agar and Germ tube were used to identify possible fungal isolates. Agar based disc susceptibility test was carried out using fluconazole. Data was analysed using Excel and STAT version 14.
Results
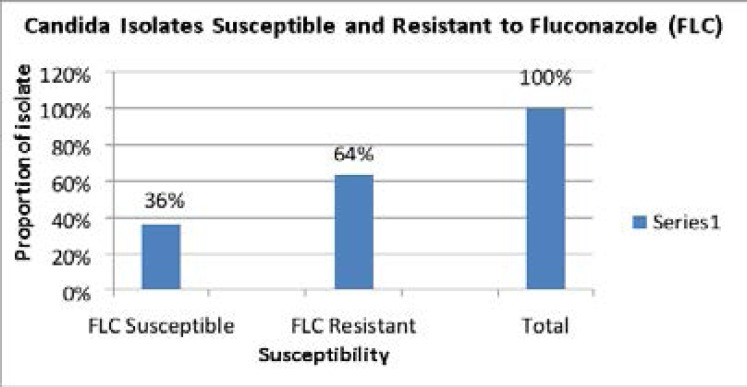
Median age was 3 years and median burn % of TBSA was 18 in participants' who had burn wound fungal infection and consisted of 3 males and 6 females. Organisms isolated included Candida albicans from 8(7.9%) participants and 2(4%) from 50 environmental swabs. 1(1%) Candida spp was isolated from pus swabs. Out of the total 11 Candida isolates, 4 (36.4%) were susceptible to fluconazole and 7 (63.6%) were resistant.
Conclusion
The isolation of Candida albicans and Candida spp from burn wound patients and the hospital ward environment suggests presence of fungi in burn wound patients and hospital ward environments. Candida isolated showed varying susceptibility patterns to fluconazole.
Keywords: Burns, Candida albicans, CLSI, fungal infection, Susceptibility patterns
Introduction
Burn patients are continually at risk of contracting fungal infections as they may be exposed based on the degree of burned total body surface area (TBSA). Burn wounds may result from damage to the skin caused by non-mechanical sources such as heat, electricity, chemicals, and nuclear radiations 1. Burn Wound Infection (BWI) remains a major public health problem and a cause of devastating trauma that can induce immediate immunosuppression which may attract predisposition to infectious complications. There has been noticeable improvement in outcomes of burn wound patients, attributed to fluid resuscitation, nutritional support and general advanced use of barrier nursing and antimicrobial agents 2. This however, is still in contrast to opportunistic fungal infections in burn wounds patients that have been reported to be on an upswing 2,3,4,32.
The skin provides an important immune barrier and if damaged, it may result in suppression of local and systemic host cellular and humoral immune responses that can destroy circulatory immune factors and result in severe opportunistic infectious complications 5,6,7. Burn wound patients with increased percentage of total body surface area burned (%TBSA) and nursed in intensive care unit for a long-time are at higher risk of fungal infections 6,8,9. Although it is known that some fungi might colonize human beings as part of normal flora, fungi still opportunistically infect burn wounds, resulting into Fungal Wound Infection (FWI) 10]which this study was concerned with. Reports from burn centres around the world show variations in the incidence of fungal infections 8,11,12,13. Candida albicans which frequently colonizes burn wounds is associated with the surrounding environment or as commensals and often causes infections within the second week of thermal injury, after patients may have received multiple antimicrobials 12,14,15. In resource poor settings, fungal infections related to burn wounds often go undiagnosed due to several factors that include limited clinical awareness and inadequate mycological laboratory facilities to distinguish them from bacterial opportunistic infections. The study aimed at investigating the occurrence of common fungi associated with admitted burn wound patients and their environment and determined antifungal susceptibility pattern of such fungi at the University Teaching Hospitals, Lusaka, Zambia.
Materials and methods
Study site
The study was conducted on swab samples from 101 participants with an extra 50 environmental swabs from a dedicated burn unit of the Adult Hospital of the University Teaching Hospitals, Lusaka, Zambia. This hospital serves as the main referral hospital in Zambia.
Specimen collection
Patients who presented with burn wounds were recruited into the study based on the inclusion and exclusion criteria. Consent was obtained from participants or their guardians prior to obtaining specimens. The specimens were carefully obtained from the burn wounds by rolling the tip of the swab on its side for one full rotation on the surface and edges of burn wound without touching intact skin to avoid possible contamination. The first specimen was collected on day eight after admission, with a follow up specimen being collected on day fourteen. In addition, environmental swabs were collected from surfaces of bath tubs, mattresses, linen and the floor.
Culture of pus and environmental swabs
Swabs collected were cultured in duplicate on Sabouraud dextrose agar plates (Mast diagnostic Ltd, Merseyside, United Kingdom). One culture plate was incubated aerobically at 37°C for 1 week and checked for any growth daily. The other culture plate was incubated at 25°C (room temperature) for 2 weeks and checked daily.
Identification of isolates
All culture growth suggestive of fungi was subjected to gram stain.
Germ tube test for yeast
Wet mounts in light microscopy were used to look for any sprouting yeast cells and any cells exhibiting tube-like outgrowths.
Corn meal agar
Corn Meal Agar Medium was used to check for chlamydospore production by Candida albicans. These would appear as thick-walled mycelia bearing a ball like cluster of budding cells. Yeast colonies grown on Saboraud dextrose agar (Mast diagnostic Ltd, Merseyside, United Kingdom) were sub cultured using sterile straight wire and streaked (horizontal furrow) onto corn meal agar (Oxoid Ltd, Basingstoke, Hampshire, United Kingdom). A flamed-sterilised cover slip was placed over the line of inoculum. The streaks were examined microscopically for any growth using a low power objective after 48 hours of incubation at 220C.
In order to differentiate C. albicans from C. dubliniensis, pure candida species isolates were inoculated on sabouraud dextrose agar and incubated at 42°C for 48 hours. On plates where growth was obtained at 42°C, the isolate was identified as C. albicans and not C. dubliniensis because C. albicans is able to grow at higher temperatures such as 42°C 34,35
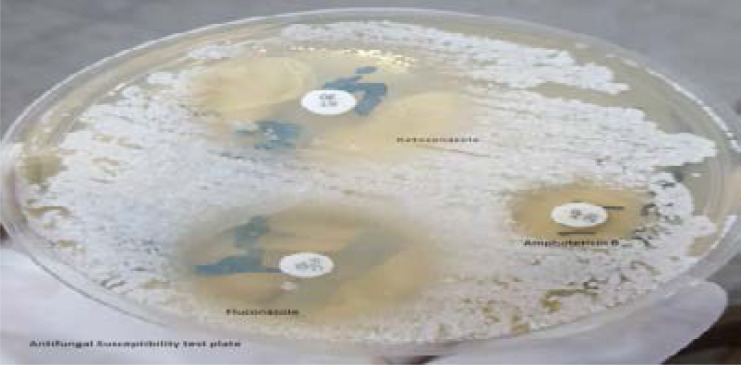
Antifungal susceptibility testing
The antifungal susceptibility testing in this study was performed on Candida albicans isolates using the agar-based Disc diffusion method by plating the inoculum on Muller Hinton (Oxoid Ltd, Basingstoke, Hants, United Kingdom) supplemented with 2% glucose (Skylabs, Springfield, South Africa) and 0.5 microgram/millilitre methylene blue (Himedia, Mumbai, India) in 130 mm diameter plates according to clinical laboratory standard institute guidelines.
The plates were inoculated by dipping a sterile swab into an isolate suspension adjusted to 0.5 McFarland standard units (10^6 cells/ml). The standardised inoculum was then streaked across the surface of the agar plates and allowed to dry at ambient temperature for 15 minutes. Antifungal discs were then placed on the inoculated plates. The susceptibility test results were determined after 24 and 48hours of incubation at 350C. The following antifungal agents were used: 10µg fluconazole, 20µg Amphotericin B and 30µg Ketoconazole (Himedia, Mumbai, India). These antifungal agents are commonly used for the treatment of fungal infections in Zambia. Susceptibility of isolates to Amphotericin B and Ketoconazole could not be interpreted due to luck of CLSI guidelines. However, all specimens were preserved in vials containing 50% glycerol solution and frozen at −80°C for future reference. Zone diameter breakpoints for disc diffusion method for fluconazole: Sensitive ≥17, Intermediate 14 – 16, Resistance ≤13.
Data processing and analysis
Data generated from the study was analysed using Excel and STATA version 14. All continuous variables were tested for normality using the Shapiro – Wilk test. Median and interquartile range were used as descriptive statistics for data which was not normally distributed. Mann-Whitney test was used to analyse asymmetrical data and multiple logistic regressions was used to determine factors such as age, burn percent of TBSA and HIV status associated with burn wound fungal infection.
Results
In this study, burn wounds swabs were collected from a total of 101 participants who met the inclusion criteria and consented to the study. Of the total 101 burn wounds, 8 were infected with Candida albicans and 1 was infected with Candida spp. An additional 50 environmental swabs were also collected from various surfaces in the wards. Of these, 2 had Candida albicans, isolated from a floor swab in the bathroom and the other from the floor in the burn's unit in ward G 12.
Table 1 below shows that median age was 3 years and interquartile range was 1.3 – 21 in participants with fungal wound infection. The median burn percentage of TBSA in participants where fungi was isolated was 18 % with interquartile range 15 – 26 while median burn percentage of TBSA in participants with no fungal isolates was 12.5 % with interquartile ranges of 8 – 20.5. Of the total 9 participants with burn wound fungal infection, 1(11%) was HIV positive while 8 (89%) participants were HIV negative, 6 (67%) participants were female while 3 (33%) were male.
Table 1.
Fungal isolates per participant
| Predictors | Fungi Isolated | Fungi not Isolated | P - Value |
| Age (years) M (IQR) | 3 (1.3 - 21) | 3 (1 – 5) | 0.4485MW |
| Burn % of TBSA | 18 (15 – 26) | 12.5 (8 – 20.5) | 0.1294MW |
| HIV Status: Number (%) | |||
| HIV Positive | 1 (11%) | 1 (1%) | 0.171F |
| HIV Negative | 8 (89%) | 91 (99%) | |
| Gender: Number (%) | |||
| Female | 6 (67%) | 46 (50%) | 0.489F |
| Male | 3 (33%) | 46 (50%) |
Key: Fisher's exact test=F, Manny-Whitney=MW, Median=M, Interquartile, Range=IQR
A total of 11 fungal organisms were isolated, 9 from burn wounds and 2 were isolated from the environment, 5 were found in G02 and another 5 was from G12. Only 1 was isolated in G21 as shown in table 2.
Table 2.
Distribution of Fungal isolates
| Surgical Ward | Number of fungal organisms | Name of fungal organism | ||
| Pus swabs | Environment | C. albicans | Candida spp | |
| G02 | 5 | 0 | 4 | 1 |
| G11 | 0 | 0 | 0 | 0 |
| G12 | 3 | 2 | 5 | 0 |
| G21 | 1 | 0 | 1 | 0 |
| G22 | 0 | 0 | 0 | 0 |
| Total | 9 | 2 | 10 | 1 |
Most participants whose burn wounds were positive for Candida infection had burn percentage of total body surface area (TBSA) ranging from 16 – 20 (n=3 and 26+ (n=3) followed by 11 -15 (n=2) and 2 – 5 (n=1), confirming data that reported incidence of burn wound fungal infection to be more in individuals with greater TBSA, as shown in table 3.
Table 3.
Burn % of TBSA of participants with Candida isolates
| Burn % of TBSA | Frequency |
| 1 – 5 | 1 |
| 6 - 10 | 0 |
| 11 - 15 | 2 |
| 16 - 20 | 3 |
| 21 - 25 | 0 |
| 26+ | 3 |
| Total | 9 |
Figure 1: Showing susceptibility results to Fluconazole (FLC)
Figure 1.
Susceptibility patterns of 11 Candida isolates, 4(36%) were susceptible to Fluconazole (FLC) and 7(64%) were resistant
The investigator-led backward stepwise regression approach was used to arrive at best predictor model. Table 4 below shows that Burn percentage of TBSA and HIV status were the best predictors of fungal infection of burn wound, with burn percentage of TBSA having a p-value = 0.097 and HIV status a p-value = 0.092 statistically significant at alpha 0.1 with confidence interval of 90%.
Table 4.
Adjusted best predictor model for burn wounds and HIV status
| Predictor | Odds ratio | P - Value | 90% Conf. Interval |
| Burn % of TBSA | 1.067901 | 0.097 | 1.000542 – 1.139794 |
| HIV Status | 11.85972 | 0.092 | 1.058589 – 132.8683 |
Discussion
Fungi remain an important emerging cause of complications in burn wound infection (BWI), in both monomicrobial and polymicrobial infection 10,12,16.
This study involved 101 participants recruited, 53 (52.5%) being females [n=44 children, n= 9 adults] and 48 (47.5%) were males [n=45 children, n=3 adults]. The participant's age distribution ranged from 9 months to 63 years. The modal age group was 0 – 5 years old, indicating more children in the study. The modal range of burn percentage of TBSA were 16 -20 and 26+ in this study. One participant had burn percentage range of 1 – 5 representing a percentage of 11.1%.
Most fungal isolates came from specimens collected on day 14 after admission. Of the 9(8.9%) total burn wound isolates only 1 (1%) isolate was from the collection on day 8. These findings agree with earlier studies of burn wound infections such as an Indian study that documented 9 (75%) from 12 patients producing positive fungal growth during the second and third-week post burn 4. As in our study Candida albicans were found to be the most common pathogen in 8(88.9%) and Candida spp. being positive in 1(11.1%). In a similar study in Egypt at Cairo University burn centre by Ibrahim et al., fungal organisms were also isolated late in the second week post burn 17. Even with existing variations in findings of burn centres, the incidence of fungal opportunistic infection in burn individuals is still high at 6.3% to 15% 8.
In the current study, Candida albicans 8(7.9%) and 1(1%) Candida spp, were found to be the prominent fungi isolated. Fungi are widely distributed and are often implicated in open wound infections, as another study in America 8 documented. In that study of 6918 patients, 435 (6.3%) had positive fungal cultures isolated which included Candida species (371 patients; 85%), Candida spp (93 patients, 21%), Aspergillus (60 patients, 14%), and other mould (39 patients, 9.0%). A study determining the profiles of bacteria and fungi of burn wound infections in a tertiary care centre in India 18 found that of a total 218 isolates, 10 (4.59%) were fungal organisms and all were yeast. Among these, Candida albicans 5 (2.3%) was the most common isolate followed by a few combined Candida species.
General surveillance studies have equally reported presence of fungi in hospital environments 19. Reported fungi as being responsible for causing 9.5 % of hospital acquired infections, with Candida species alone causing 9% of the infections. Another hospital ward environmental study 13 reported 6(12%) of 50 patients admitted with thermal burns in the surgical unit had Candida albicans and 4(8%) non-albicans candida spp. Another Indian study from the National Mycology Referral Laboratory at a Postgraduate Institute of Medical Sciences, found that 25 severely burnt patients and their environment revealed fungal contamination by Candida spp, Penicillium, Aspergillus and Fusarium 20,21.
In our study, similar revelations of Candida albicans isolation from the environmental swabs collected from various surfaces in the burns unit especially in moist areas confirm the risk these organisms pose to not only burn wound patients but to all other patients admitted in hospitals. Children with burn wounds seem to be most at risk of fungal infections as shown by our results of the age group of 0-5 (n=6, 66.7%) with burn percentage of TBSA in the range of 16 – 20 (n=3, 33.3%) and 26+ (n=3, 33.3%). Having reported that burn wounds suppress immunity, it becomes more worrying for children with burn wounds whose immunity is not even fully developed, making this group of patients to be at heightened risk of fungal infection.
HIV infection (2%) among participants is another added risk to fungal infections in burn wound patients. HIV infections greatly lower immunity and thus makes burn wound patients more likely to be infected, not only with fungi but with other common environmental microorganisms too. Our study isolated fungi from 1(1%) of the participants who was HIV infected. Our statistical results confirm the risk association of HIV infection and burn percent of TBSA with risk of fungal infection (Burn % of TBSA: p-value=0.097, 90% CI 1.000542- 1.139794, HIV status: p-value=0.092, 90% CI 1.058589-132.8683) 1,5,4,22,33.
Successful clinical therapy of burn wound fungal infection has often been a challenge due to lack of mycology laboratories to do susceptibility testing and because of that some burn centres choose to use topical applications of antifungal agents to treat local colonization and fungal infections. Such treatments work but may also conceal deeper seated infections 23,24. Systemic use of antifungal agents therefore remains the main therapy of choice and administered dependant on the condition of the burn patient and possible laboratory confirmation of fungemia 1,8.
This study also considered subjecting the isolated fungal organisms to antifungal susceptibility testing to check susceptibility patterns of the commonly used antifungals in our environment. Susceptibility testing promotes accurate administration of antifungal agents and helps in monitoring emergence of antifungal resistance 25,26. Of the 11 Candida isolates tested against fluconazole, 4 (33.4%) were susceptible and 7 (63.6%) were resistant, a clear indication that there is resistance to fluconazole among the common fungi infecting burn wound patients. Two of the candida albicans isolates susceptible to fluconazole came from the environment swabs and the other two isolates were from burn wounds. This result echoes earlier findings in a study in Zambia by Sarenje et al., which observed multi-drug resistance in 5 Candida isolates, with Candida albicans, being the most resistant species to fluconazole and amphotericin B 27. C. albicans isolates were also found to be resistant to fluconazole in an Iranian study with patients responding poorly to treatment with these drugs 28,29,30,31.
Limitations
The study might have suffered limitations arising from loss of burn wound patients who were admitted for less than a week and those who left against medical advice. Failure to collect and examine burn wound tissue for histology deprived the study useful data. Lack of guidelines on interpretation of zone of inhibition for antifungal disc diffusion methods for ketoconazole and amphotericin B also made it difficult to interpret the susceptibility patterns of the two antifungal medicines. Molecular methods were not used due to limited financial resources.
Conclusion
This study contributes to documented fungal infections being likely to occur in burn wound patients. Candida albicans and Candida spp are present in the hospital ward environments and pose risk of opportunistic infection to burn wound patients at UTHs. The isolation of other Candida species with varying susceptibility patterns to fluconazole pose higher resistance to other antifungal substances and may be associated with poor prognosis. Therefore, screening burn wound patients for fungi should be routine; and preventive measures should include frequent fungal surveillance and appropriate antifungal therapy.
Figure 2.
Antifungal Susceptibility test for C.albicans isolated from burn wound of a 1year 3months old girl on Mueller Hinton Agar + 2% Glucose + 0.5mcg/ml Methylene Blue Dye Medium (GMB
Acknowledgment
We would like to thank Dr Gina Mulundu for her principal supervisory role, Mr Darlintone M. Mwenya and Mr Paul Simusika for their co-supervisory roles, their guidance and support. All other authors contributed to reading the manuscript and approved valuable advice. We wish to thank UTHs management for allowing me to do the study in bacteriology laboratory.
Ethical approval and permission
The study was approved by the University of Zambia Biomedical Research Ethics Committee (UNZA-BREC) Reference number 004-11-18 and permission for its conduct was granted by the National Health Research Authority (NHRA).
Consent for publication
Not applicable.
Availability of data and materials
Data generated and /or analysed in this study is available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests
Funding
None of the authors received financial support.
Author's contributions
GM conceived the study, KS and GM designed the study. KS collected and analysed specimens. GM, DMM and PS supervised the study. KS and GM drafted and finalized the manuscript. All others provided critical comments. All authors read and approved the final manuscript.
Author's information
Not applicable.
References
- 1.Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn wound infections. Clin Microbiol Rev. 2006;19:403–434. doi: 10.1128/CMR.19.2.403-434.2006. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jithendra K, Pathapati RM, Nadakuduru P, Buchineni M, Pasupuleti S, Sateesh S. Identification of fungal pathogens in burns patients with reference to Candida. Journal of Evidence based Medicine and Healthcare. 2015;2:1–8. [Google Scholar]
- 3.Pruitt BA, Jr, McManus AT, Kim SH, Goodwin CW. Burn wound infections: current status. World J Surg. 22:135–145. doi: 10.1007/s002689900361. 199. [DOI] [PubMed] [Google Scholar]
- 4.Sarabahi S, Tiwari VK, Arora S, et al. Changing pattern of fungal infection in burn patients. Burns. 2012;38:520–528. doi: 10.1016/j.burns.2011.09.013. PubMed. [DOI] [PubMed] [Google Scholar]
- 5.Barreto MX, Leonardi DF, Silva MA. Infecção em queimaduras: estudo da flora predominante na UTI queimados do Hospital de Pronto-socorro de Porto Alegre. Rev Bras Ter Intens. 1998;10:177–180. [Google Scholar]
- 6.Macedo JLS, Rosa SC, Castro C. Sepsis in burned patients. Rev Bras Med Trop. 2003;36:647–652. doi: 10.1590/s0037-86822003000600001. PubMed. [DOI] [PubMed] [Google Scholar]
- 7.Chamania S, Hemvani N, Joshi S. Burn wound infection: Current problem and unmet needs. Indian J Burns. 2012. pp. 18–22.
- 8.Ballard J, Edelman L, Saffle J, Sheridan R, Kagan R, Bracco D, et al. Positive fungal cultures in burn patients: a multicenter review. J Burn Care Res. 2008;29:213. doi: 10.1097/BCR.0b013e31815f6ecb. [DOI] [PubMed] [Google Scholar]
- 9.Applegreen P, Bjornhagen V, Jonscon CE, Ransjo U. A prospective study of infection in burn patients. Burns. 2002;28:39–46. doi: 10.1016/s0305-4179(01)00070-5. PubMed. [DOI] [PubMed] [Google Scholar]
- 10.Horvath EE, Murray CK, Vaughan GM, Chung KK, Hospenthal DR, Wade CE, et al. Fungal wound infection (not colonization) is independently associated with mortality in burn patients. Ann Surg. 2007;245:978. doi: 10.1097/01.sla.0000256914.16754.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rafik A, Diouri M, Bachechar N, Chlihi A. Epidemiology of nosocomial fungal infections in the National Center for Burns in Casablanca, Morocco. Annals of burns and fire disasters. 2016;29(2):90–93. [PMC free article] [PubMed] [Google Scholar]
- 12.Mousa HA. Fungal infection of burn wounds in patients with open and occlusive treatment methods. East Mediterr Health J. 1999;5:333–336. PubMed. [PubMed] [Google Scholar]
- 13.Sharma Sanjeev, et al. Fungal infection in thermal burns: A Prospective study in a Tertiary care centre. Journal of clinical and diagnostic research. 2016;10(9):5–7. doi: 10.7860/JCDR/2016/20336.8445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luo G, Peng Y, Yuan Z, et al. Yeast from burn patients at a major burn Centre of China. Burns. 2011;37:299–303. doi: 10.1016/j.burns.2010.03.004. PubMed. [DOI] [PubMed] [Google Scholar]
- 15.Schofield CM, Murray CK, Horvath EE, et al. Correlation of culture with histopathology in fungal burn wound colonization and infection. Burns. 2007;33:341–346. doi: 10.1016/j.burns.2006.08.040. PubMed. [DOI] [PubMed] [Google Scholar]
- 16.Murray CK, Loo FL, Hospenthal DR, Cancio LC, et al. Incidence of systemic fungal infection and related mortality following severe burns. Burns. 2008;34:1108–1112. doi: 10.1016/j.burns.2008.04.007. PubMed. [DOI] [PubMed] [Google Scholar]
- 17.Ibrahim NH, Amer TA. Frequency of bacterial and fungal infections of burn wounds at Cairo university burn centre. Egyptian Journal of Medical Microbiology. 2008;17:573–582. [Google Scholar]
- 18.Mundhada SG, Waghmare PH, Rathod PG, Ingole KV. Bacterial and fungal profile of burn wound infections in Tertiary Care Center. Indian J Burns. 2015;23:55–71. PubMed. [Google Scholar]
- 19.Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004;39:309–317. doi: 10.1086/421946. PubMed. [DOI] [PubMed] [Google Scholar]
- 20.Chakrabarti A, Chatterjee SS, Rao KL, Zameer MM, Shivaprakash MR, Singhi S, et al. Recent experience with fungemia: Change in species distribution and azole resistance. Scand J Infect Dis. 2009;41:275–284. doi: 10.1080/00365540902777105. PubMed. [DOI] [PubMed] [Google Scholar]
- 21.Gupta N, Hague A, Lattif AA, Narayan RP, Mukhopadhyay G, Prasad R. Epidemiology and molecular typing of Candida isolates from burn patients. Mycopathologia. 2005;158:397–405. doi: 10.1007/s11046-004-1820-x. [DOI] [PubMed] [Google Scholar]
- 22.Moore EC, Padiglione AA, Wasiak J, et al. Candida in burns: risk factors and outcomes. J Burn Care Res. 2010;31:257–263. doi: 10.1097/BCR.0b013e3181d0f536. PubMed. [DOI] [PubMed] [Google Scholar]
- 23.Branski LK, Al-Mousawi A, Rivero H, et al. Emerging infections in burns. Surg Infect. 2009;10:389–397. doi: 10.1089/sur.2009.024. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Acar A, Uygur F, Diktaş H. Comparison of silver-coated dressing (Acticoat®), chlorhexidine acetate 0.5% (Bactigrass®) and nystatin for topical antifungal effect in candida albicans-contaminated, full-skin-thickness rat burn wounds. Burns. 2011;37:882–885. doi: 10.1016/j.burns.2011.01.024. PubMed. [DOI] [PubMed] [Google Scholar]
- 25.Spellberg B J, Filter S G, Edwards J E. Current treatment strategies for disseminated candidiasis. Journal of Antimicrobial agents and Chemotherapy. 2006;42:244–251. doi: 10.1086/499057. [DOI] [PubMed] [Google Scholar]
- 26.Arendrup M C. Epidemiology of invasive candidiasis. Journal of Critical Care. 2010;16:445–452. doi: 10.1097/MCC.0b013e32833e84d2. [DOI] [PubMed] [Google Scholar]
- 27.Serenje KL. Doctoral dissertation. The University of Zambia; Characterisation of candida species isolated from clinical specimens at University Teaching Hospital, Lusaka, Zambia. [Google Scholar]
- 28.Ane-Anyangwe I, Meriki HD, Silum SP, Nsongomanyi FR, Zofou D. Antifungal susceptibility profiles and risk factors of vaginal candidiasis amongst female university students in southwest region, Cameroon. Afr J Cln Exper Microbiol. 2015;16(1):67–72. [Google Scholar]
- 29.Asticcioli S, Sacco L, Daturi R, Matti C, Nucleo E, Zara F, et al. Trends in frequency and in vitro antifungal susceptibility patterns of Candida isolates from women attending the STD outpatient's clinic of a tertiary care hospital in northern Italy during the years 2002-2007. New Microbiol. 2009;32(2):199–204. [PubMed] [Google Scholar]
- 30.Njunda AL, Nsagha DS, Assob JCN, Kamga HL, Teyim P. In vitro antifungal susceptibility patterns of Candida albicans from HIV and AIDS patients attending the Nylon Hospital in Douala Cameroon. J Public Health Africa. 2012;3(1):2. doi: 10.4081/jphia.2012.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mohamadi J, Reza Havasian M, Panahi J, Pakzad I. Antifungal drug resistance pattern of Candida spp. isolated from vaginitis in Ilam-Iran during 2013-201. Bioinformation. 2015;11(4):203–206. doi: 10.6026/97320630011203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palackic A, Popp D, Tapking C, Houschyar KS, Branski LK. Fungal infections in Burn Patients. Surgical infections. 2021 Feb;22(1):83. doi: 10.1089/sur.2020.299. Doi: 10.1089/sur.202.299. [DOI] [PubMed] [Google Scholar]
- 33.Pruskowski KA, Mitchell TA, Killely JL, Wellington T, Britton GW, Cancio LC. Diagnosis and management of invasive Fungal wound infection in burn patients. Eur. Burn. J. 2021;2(4):168–183. doi: 10.3390/ebj2040013. [DOI] [Google Scholar]
- 34.Sullivan DJ, Westerneng TJ, Haynes KA, Bennett DE, Coleman DC. Candida dubliniensis Sp.nov: Phenotypic and molecular characterization of a novel species associated with oral candidiasis in HIV infected individuals. Microbiology. 1995;141:1507–1529. doi: 10.1099/13500872-141-7-1507. [DOI] [PubMed] [Google Scholar]
- 35.Coleman DC, Sullivan D J, Bennet D E, Moran G P, Barry H J, Shanley D B. Candidiasis: the emergency of a novel species Candida dubliniensis. AIDS. 1997;11:557–567. doi: 10.1097/00002030-199705000-00002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data generated and /or analysed in this study is available from the corresponding author on reasonable request.