Abstract
In 2023, the National Science Foundation (NSF) and the National Institute of Health (NIH) brought together engineers, scientists, and clinicians by sponsoring a conference on computational modelling in neurorehabiilitation. To facilitate multidisciplinary collaborations and improve patient care, in this perspective piece we identify where and how computational modelling can support neurorehabilitation. To address the where, we developed a patient-in-the-loop framework that uses multiple and/or continual measurements to update diagnostic and treatment model parameters, treatment type, and treatment prescription, with the goal of maximizing clinically-relevant functional outcomes. This patient-in-the-loop framework has several key features: (i) it includes diagnostic and treatment models, (ii) it is clinically-grounded with the International Classification of Functioning, Disability and Health (ICF) and patient involvement, (iii) it uses multiple or continual data measurements over time, and (iv) it is applicable to a range of neurological and neurodevelopmental conditions. To address the how, we identify state-of-the-art and highlight promising avenues of future research across the realms of sensorimotor adaptation, neuroplasticity, musculoskeletal, and sensory & pain computational modelling. We also discuss both the importance of and how to perform model validation, as well as challenges to overcome when implementing computational models within a clinical setting. The patient-in-the-loop approach offers a unifying framework to guide multidisciplinary collaboration between computational and clinical stakeholders in the field of neurorehabilitation.
Keywords: Computational modeling, Patient-in-the-loop, Sensorimotor adaptation, Digital Twin, Neuroplasticity, Musculoskeletal, Sensory, Pain, Neurological condition, Neurodevelopment
Introduction
Neurorehabilitation exemplifies how multiple disciplines—physical therapy, biomedical engineering, medicine, neuroscience, kinesiology, and others—come together with the common purpose of improving the lives of those with a neurological condition [1–5]. Yet major challenges for multidisciplinary research are differences in theory, approach, and terminology between disciplines [6, 7], all of which may hinder both collaboration and the development of improved neurorehabilitation. In this perspective piece, we propose a general, operational framework to promote synergistic collaboration among computational modellers, clinicians, and patients to improve functionality and quality of life.
Our proposed framework is built upon the International Classification of Functioning, Disability and Health (ICF) [8], a recent framework for precision rehabilitation [9], patient involvement in health care decision making [10], and works where computational models have been used to improve health care [11–14]. The ICF is the world health organization (WHO) framework to measure both disability and health of a patient, and is commonly utilized for rehabilitation management in clinical practice [8, 15–21]. Of particular interest here is the use of the ICF to identify a patient’s body structure and function, which can all be targeted during therapy to promote recovery or habilitation to a condition state [8]. Recently, a precision rehabilitation framework has been proposed that incorporates the IFC and high-fidelity data to, critically, continuously monitor a patient’s condition over time [9]. This precision rehabilitation framework also considers clinically important factors such as clinical phenotype, treatment type, and prescription. Further, patient involvement in clinical care has been shown to improve patient satisfaction and health, productivity of the service provider, and treatment outcome [22–28]. It is important to consider the aforementioned clinically grounded work when identifying where along a clinical pipeline that computational modelling can provide support to neurorehabilitation.
Computational modelling has proven particularly effective for drug delivery [11–14]. One well-known success story is the use of feedback control theory to deliver insulin in diabetics [11]. Continual monitoring of glucose levels and a computational model of both glucose and insulin dynamics are used to optimize insulin delivery through a pump. Critical to this approach is that the patient is directly within the control loop, where continual monitoring of glucose to determine optimal insulin delivery has been shown more effective than conventional treatment and leads to less diabetic complications [12]. This ‘patient-in-the-loop’ approach has also been proposed for anesthesia and HIV medicine [13, 14]. To improve mobility and functionality, there have been recent advances using a patient-in-the-loop approach in the areas of deep brain stimulation (DBS) for Parkinson’s disease [29, 30] and prosthetics for amputees [31, 32]. Our framework differs from these works and others [29–33], since our framework also jointly considers the ICF, diagnostic models, and patient involvement. Here we will consider how various sensorimotor adaptation, neuroplasticity, musculoskeletal, and sensory & pain models can be used within a patient-in-the-loop framework to facilitate neurorehabilitation.
We propose a comprehensive patient-in-the-loop framework that incorporates computational modelling, the ICF, continually monitoring a patient’s condition [9], and patient involvement to support neurorehabilitation. In particular, we will focus on where and how sensorimotor adaptation, neuroplasticity, musculoskeletal, and sensory computational models could be used to diagnose and optimize treatment for patients to improve their functionality and quality of life. Objectives of this perspective piece are (i) to create a patient-in-the-loop framework that identifies where along a clinical pipeline that computational modelling can support neurorehabilitation for a broad range of neurological and neurodevelopmental conditions, (ii) to identify current state-of-the-art and future directions in computational modelling that can support neurorehabilitation, and (iii) highlight the importance of model validation.
In the following sections, we will first address the patient-in-the-loop framework (ICF: patient body structure & function, data, diagnostic models & clinical decision-making by practitioner, intervention type, treatment models and prescription, recovery and habilitation, and patient involvement). We will then address types of models (data-driven and fundamental models), models for neurorehabilitation (sensorimotor adaptation & learning models, neuroplasticity models, musculoskeletal models, sensory and pain models), and model validation. Finally, we will discuss future challenges and provide a summary of this perspective piece.
Patient-in-the-loop framework
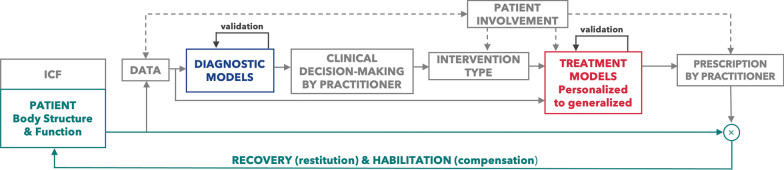
Our goal was to develop a patient-in-the-loop framework to identify where and how computational modelling can be implemented within clinical care to further support neurorehabilitation (Fig. 1). This framework considers the ICF, the use of multiple or continuous data measurements over time as in a recent precision rehabilitation framework [9], patient involvement, and computational models to support diagnostics and treatment prescription while continually assessing and optimizing the recovery and habilitation of a patient’s body structure and function. Our framework is intentionally general, in a similar vein to the ICF, so that it can be applied to a range of neurological and neurodevelopmental conditions (Figs. 2, 3, 4). Within this paper, we refer to computational models very generally as equation(s) that can be used to simulate some system or describe some phenomena, such as a dynamical system, control policy, adaptive process, a mapping between inputs and outputs, etc. We define diagnostic models and treatment models as any computational model that can be used to aid in the diagnosis or treatment prescription of a patient, respectively. Note that in some cases that the same computational model, such as one that describes the musculoskeletal system, may be used either as a diagnostic model or treatment model depending on the particular context that it is used. Directly below we expand on each component of this patient-in-the-loop framework.
Fig. 1.
Patient-in-the-Loop Framework. This general framework promotes the use of the ICF, multiple or continuous data measurements over time, patient involvement, and computational models to aid clinicians in diagnosing and prescribing treatment. Specifically, within this ‘patient-in-the-loop’ framework, continual monitoring of a patient’s body structure and function allows for updates to diagnostic and treatment models that inform new and revised prescription by a practitioner to maximize recovery and habilitation. Both fundamental (e.g., motor adaptation, neuroplasticity, musculoskeletal, and sensory) and data-driven (e.g., machine learning) diagnostic and treatment models, which must be properly validated, can be utilized to better inform and facilitate more effective neurorehabilitation for a range of neurological and neurodevelopmental conditions
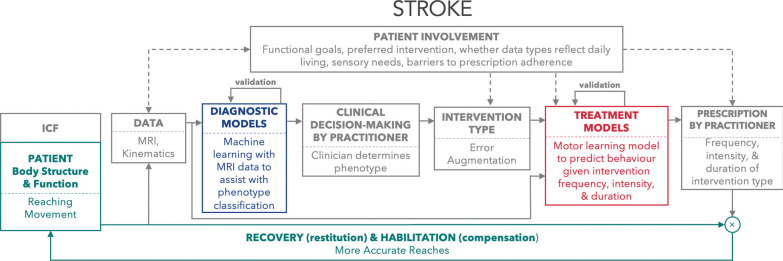
Fig. 2.
Computational models can be used within a patient-in-the-loop framework to improve post-stroke reaching. This example uses machine learning to assist with phenotype classification, error augmentation as the intervention type, and a sensorimotor learning model to better inform treatment prescription with the goal of improving reach accuracy during the recovery & habilitation process. Error augmentation magnifies visual and or haptic error signals, the difference between sensory feedback and an expected sensory target, which has been shown to improve both reaching behaviour and clinical measures of functionality for individuals post-stroke [114]. Patient involvement at several points within this loop is used to support model personalization, adherence, and tailoring of intervention plans to functional goals
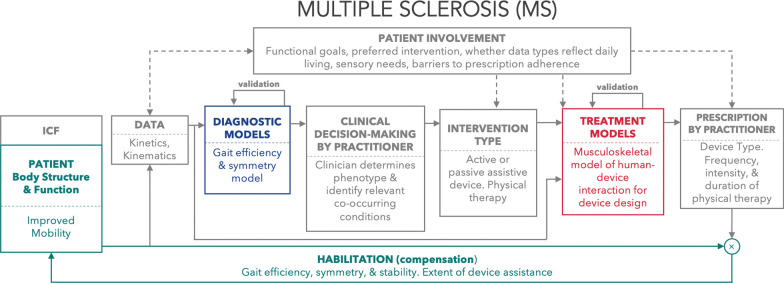
Fig. 3.
Here we use a worked example of multiple sclerosis within the patient-in-the-loop framework to improve mobility. Here musculoskeletal models of gait efficiency and symmetry are used to aid diagnosis, a device is used for intervention, and a musculoskeletal model of human-device interaction is used to predict several gait metrics when using the device. Patient involvement occurs at several points within the loop
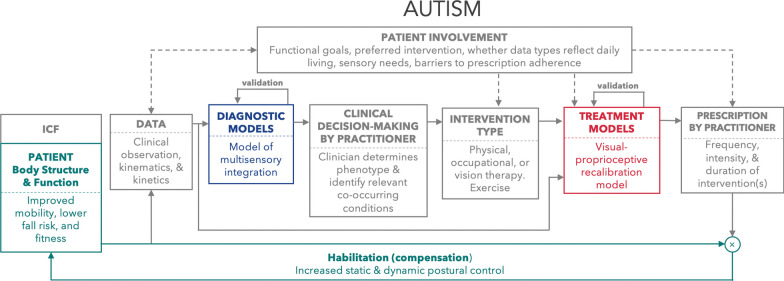
Fig. 4.
Computational models of multisensory integration and the oculomotor system can be applied to habilitation in autism. Patient involvement at each point in the loop can inform selection of data inputs, diagnostic and treatment model development and implementation, and selection of intervention type based on potential barriers to adherence, sensory needs, and personal functional goals. Treatment prescription can be informed via model predictions of visual-proprioceptive recalibration that account for developmental changes across the lifespan, with the goal of improving static and postural control to aid mobility, lower fall risk, and improve fitness
ICF: patient body structure and function
We begin the patient-in-the-loop framework with the ICF [8, 34]. The ICF is a well-known framework to guide therapy across a variety of domains [8, 15–21, 34], including neurorehabilitation for neural injury (e.g., Stroke [35]), movement conditions (e.g., Parkinson’s disease [36]), or neurodivergence (e.g., autism [37]). Here we focus on a patient’s body structure and function within the ICF, which are important to consider for computational modelling. While we apply the ICF in our patient-in-the-loop framework, we do not provide an exhaustive description of the ICF and would refer the reader to [34].
Data
Our patient-in-the-loop framework promotes the use of monitoring patient data that relates to their body structure or function. These data can be collected continuously or at multiple time-points to support neurorehabilitation [9]. Such data can include kinematic and kinetic measurements of eye and body movement, electromyography (EMG) and electroencephalography (EEG) to respectively measure muscle and brain activity, medical imaging with ultrasound, X-ray, and magnetic resonance imaging (MRI), and clinical measures of functionality (e.g., Fugl-Meyer [38] and MDS-UPDRS [39]). Moreover, it is becoming increasingly possible to collect much of this data not only in laboratory settings, but also in the clinic and at home due to exponential improvements in wearable and portable sensors [40–44] and markerless video-based technologies [45, 46] in the past decade. Further, the low-cost and widespread use of wearable technologies may also enable collecting baseline data of an individual’s health and behaviour prior to the onset of a neurological condition. We envision that these advancements will enable researchers and clinicians to monitor patient condition in both controlled and naturalistic environments, as well as comparing data following the onset of a neurological condition to both normative measures across the lifespan and an individual’s own baseline.
Diagnostic models and clinical decision-making by practitioner
Once patient data has been collected, computational models can assist a clinical practitioner with an initial or revised diagnosis of the patient condition. For example, a computational model may indicate the likelihood that a patient has a particular neurological condition based on kinematics [47] or neuroimaging [48]. It has been suggested that early disease onset detection can improve patient outcomes, such as in Parkinson’s disease [48]. Further, such models may also provide information as to whether it might be beneficial to try a different neurorehabilitation strategy. Below in "Models for neurorehabilitation", we discuss the use and potential of several computational models (sensorimotor adaptation, neuroplasticity, musculoskeletal, and sensory & pain) to aid in diagnosing a condition. An important consideration is ensuring that these models are properly validated, which we address in more detail below (see "Model validation"). Importantly, within the framework a trained medical practitioner (e.g., physical therapist, medical doctor, etc.) makes a diagnosis that is informed by a computational model.
Intervention type
Once a medical practitioner has made a diagnosis informed by a diagnostic model, they are responsible for selecting the type of intervention used to treat the patient. Traditional therapy guided by a physical therapist or occupational therapist, often with drug management (e.g., L-Dopa for Parkinson’s disease [49]), remain the standard of care for neurological conditions. In addition to traditional approaches, technological advancements have and will continue to offer new alternatives that may further improve patient outcomes. Some common examples of different intervention types include robot-guided therapy [50–53], treadmill training [54–56], exoskeleton [57–59], orthotics [60–64], and brain-machine interfaces [65–68]. Whether receiving traditional therapy or interacting with a device, it is important to consider how a patient will adapt and respond to their particular prescribed treatment.
Treatment models and prescription
Computational models can play an important role in the process of prescribing and monitoring outcomes of treatment for neurological conditions. For the purposes of this perspective piece, we will focus on sensorimotor adaptation, neuroplasticity, musculoskeletal, and sensory computational models. As an example, sensorimotor adaptation models describe how human motor behaviour changes over time in response to an environmental stimuli (e.g., external loads), and can be used to specify treatment duration that maximizes the retention of relearned, functional motor skills [69]. Further below, we expand on several different model types (i.e., machine learning, sensorimotor adaptation, neuroplasticity, musculoskeletal, and sensory & pain) and how they can be used to aid in treatment prescription. This manuscript primarily focuses on fundamental models that, in contrast to data-driven machine learning models, often generalize better since they attempt to understand and capture underlying mechanisms (see "Fundamental models"). It might be possible to use model simulations to generate synthetic data to make comparisons between the patient and outcomes at multiple point across the framework (e.g., diagnostic model outputs). Further, another potential approach would be comparing different treatment models at the stage of selecting the type of intervention [9]. That is, using models to simulate different intervention types may help guide the selection of intervention type.
A critical component of the proposed patient-in-the-loop framework, is the use of computational modelling for helping the medical practitioner in prescribing appropriate treatment. The FITT (frequency, intensity, time, and type) principle can be applied in this context [70]. Frequency is how often the treatment is performed, such as once per day. Intensity is the difficulty of a particular activity, such as maintaining some target level of heart-rate, walking speed, or load. Time is how long the treatment is performed, such as 30 min. Treatment type we have previously described above, which can include traditional therapy to interacting with some passive or powered device. Moreover, behavioural support for neurodivergent individuals can also fall under the FITT principle [71]. Computational modelling has the potential to provide insights into which type of treatment should be utilized, while optimizing the optimal frequency, intensity, and time to to maximize the recovery and habilitation of the patient’s body structure and function.
Recovery (restitution) and habilitation (compensation)
Our patient-in-the-loop framework aims to prescribe treatment that promotes recovery or habilitation to patient body structure or body function (represented by the multiplication symbol in Fig. 1). As in Levin and colleagues, here we use the term recovery as improvements that result from restitution of biological structure and function [72]. The word habilitation represents a compensation to neurodivergence (e.g., autism) or a neurological condition (e.g., stroke). Habilitation is the use of different biological structures or function one would typically use, or the use of a passive or powered device, to carry out some desired activity. Habilitation as a term also encapsulates neurodivergent individuals, such as those with autism, where the goal is to improve outcomes since it is not possible to recover from a condition that someone is born with [73, 74]. However, it is important to consider that individuals will likely respond differently to the same treatment or may appear to have a different capacity to improve [75]. Moreover, computational models that prescribe treatment are unlikely to yield a perfect prediction of how a patient will respond to treatment prescription.
To address individual differences and imperfect model predictions, the proposed framework promotes the use of continual or multiple data measurements of body structure and function. Crucially, continual or multiple data measurements over time allows for updates to treatment models parameters—thereby placing the ‘patient-in-the-loop’—so that treatment models can better predict and inform prescription that aims to maximize the recovery and habilitation of the patient’s body structure and function.
Patient involvement
The primary goal of the patient-in-the-loop framework is to utilize computational models to maximize recovery and habilitation of a patient’s body structure and function. This should ideally include continuous patient involvement throughout the processes of providing data, selecting intervention type, goals and constraints of models, and prescription. Patient involvement has been shown to improve treatment outcome, patient satisfaction, and health [22–28]. In line with the National Institutes of Health (NIH) recommendations [10], we encourage patient involvement with their care in decision-making at each step in their care trajectory, from first concern to intervention. As one would expect, the patient or their caregiver is responsible for consenting to and providing data to help make a diagnosis (dashed arrow from patient involvement to data; Fig. 1). The collected data and the interpretation of those data should also be shared with the patient (dashed arrow from data to patient involvement), so that they can be involved with subsequent clinical care decision-making. Once a patient is well-informed, they should be involved with both selecting the intervention type and the prescription. For example, the patient may have a preference for a particular treatment based on comfort levels, cost or time constraints, or several other personal factors. Further, it is possible to incorporate some of these personal constraints into computational modelling. For example, a patient’s constraints on the amount of time and frequency with which they can engage in physical therapy can be factored into sensorimotor adaptation models. Likewise, the patient may have their own personal goals on their desired outcomes and functionality, which may influence the intensity or type of the prescribed treatment. Patients can also inform the process of model development and feature selection, for example by reporting on their own experiences and internal states. This information adds value to development of diagnostic models by grounding them in patients’ lived experiences. Finally, the patient can continue to provide feedback on the treatment type and prescription in followup appointments, and be involved in decisions as to whether the care should continue as planned or if there should be changes to the treatment.
Types of models
Data-driven models
Data-driven computational modelling approaches are often used to identify patterns or relationships from data in an effort to drive neurorehabilitation efforts. In this paper and the sections below, we focus primarily on mechanistic models that aim to understand or capture the physiological processes underlying these relationships (see "Fundamental models"). However, purely data-driven models also hold significant potential to aid treatment prescription to estimate recovery and habilitation [76]. In contrast to mechanistic models, data-driven modelling approaches look for features in the recorded data (clinical, biomechanical, physiological, etc.) that are associated with and/or predictive of some meaningful outcome measure (e.g., functional impairment level, community participation, etc.) without modelling the underlying processes that produce those relationships. While there are some additional examples in the "Models for neurorehabilitation", here we provide a very brief overview of data-driven modelling efforts for neurorehabilitation.
Data-driven models for neurorehabilitation can generally be classified in two categories: (1) regression and classification approaches, and (2) deep learning approaches. The first step to regression and classification approaches is typically a data reduction process, in which high-dimensional data is transformed into a lower-dimensional representation via manual feature selection or algorithms such as principal component analysis [77–83]. This step helps to make the variability in complex continuous and/or multi-modal data amenable to interpretation and further analysis. The identified variables can then be used as input to regression, Bayesian, and classification models. For example, a recent study using regression approaches identified that younger ”brain age”, as measured from whole-brain structural neural imaging, was associated with better functional outcomes after a stroke [84]. Such a result points towards the importance of including brain age as a covariate in models predicting the response to neurorehabilitation. Classification models (e.g., support-vector machines, cluster analysis, etc.) that group data points based on their similarity have enabled the subdivision of stroke patients based on their underlying impairments [85–89], identifying potential targets for neurorehabilitation. However, relying on a lower-dimensional representation may limit the ability to capture subtle but important individual-specific patterns within the data underlying impaired function and/or improvements with rehabilitation. Deep learning approaches, on the other hand, that use the entire dataset instead of relying on a reduced representation, may better capture the diverse array of variables associated with biological processes that vary individually and change over time [90]. Such approaches have shown promise in making diagnoses, predicting treatment outcomes, providing real-time feedback, and guiding clinical decision-making [90–95]. Moreover, causal deep reinforcement learning to find an optimal dynamic treatment regime [9, 96] could be used to optimally select the best treatment type and prescription according to an optimal reinforcement learning control policy, which can be refined over time using continual data measurements.
Not only may data-driven models be useful for predicting individual-level treatment responses and provide insights intervention targets, they may also influence mechanistic, fundamental modelling efforts by serving as input to mechanistic, fundamental models. Moreover, relationships between data and outcome measures revealed via data-driven models may serve as motivation for developing novel mechanistic models to elucidate the physiological mechanisms underlying these relationships.
Fundamental models
The role of fundamental modelling research in a patient-centered treatment paradigm
models are being developed not just as tools for clinicians, but as tools for building fundamental understanding of human motor control, adaptation, development, and impairment. While not always directly translational to a model-based treatment pipeline, this work is nonetheless essential for improving clinical outcomes. By improving our understanding of underlying mechanisms that cause neurological or behavioural changes, we improve the foundation for new treatments to be developed, whether or not the treatment directly involves a computational model. Conversely, without rigorous testing of our understanding of mechanisms that treatments exploit, we risk developing inaccurate models and ineffective, or worse, harmful treatment plans.
Mechanistic and phenomenological models
Mechanistic models explicitly describe the fundamental mechanisms that drive the relationship between observable inputs and outputs from first principles. Conversely, phenomenological models attempt to describe this relationship with a direct mapping from input to output (i.e., describing the “behaviour” of a system rather than lower-level contributions of its component parts).
Mechanistic models are capable of representing specific theoretical frameworks for a given mechanism. If a mechanism is theorized from first principles and is able to accurately and robustly describe the empirically observed relationship between input and output, it can be used to predict the response of the mechanism to novel interventions and new inputs. However, it is not practical or currently possible to derive every relationship between two phenomena down to the interaction between individual atoms, therefore mechanistic models are built with phenomenological components. Additionally, for describing processes within humans, while mechanistic models offer concrete theories that can be tested, it is often not possible to design experiments that can isolate the effect of a particular mechanism in humans. Therefore there is no guarantee that a mechanistic model can be confidently falsified even if it is incorrect. Despite these limitations, mechanistic models are important for neurorehabilitation because our understanding remains limited in many critical areas.
Phenomenological models are in many ways more practical when the question is not, “how does this system work?” but instead “what will the outcome be?”. Yet phenomenological models may not be as robust to novel circumstances as mechanistic models. That is, novel inputs may interact with internal mechanisms that did not significantly contribute to previously observed outputs. Nevertheless, phenomenological models are essential for model-based research with applications in neurorehabilitation. A well-characterized phenomenological model for a specific mechanism is often more useful in a practical sense than a mechanistic model of the same mechanism, because it allows for direct computation of the output in question. Rigorously validated phenomenological models are more likely to be directly translatable as practical tools for clinicians.
Using models to create new knowledge
In many situations, a model can be thought of as a formal representation of theory [97]. Such a model can be used to help design an experiment and test whether a priori model predictions are observed in the data [98, 99], or to investigate novel circumstances that have not been or cannot be experimentally tested [100]. Models can also be used to challenge prevailing interpretations of experimental work by demonstrating mechanistic validity of alternative interpretations [101]. If a model captures the mechanism of a particular neurological condition then it should be able to predict how an individual responds to treatment. If a model can reliably predict behaviour then it can also be used to optimize a treatment plan to promote recovery and habilitation. Next, we highlight how models of sensorimotor adaptation & learning, neuroplasticity, musculoskeletal, and sensory & pain can be used to support diagnostics and treatment.
Models for neurorehabilitation
Sensorimotor adaptation and learning models
In the interest of identifying unifying principles across the field of neurorehabilitation, we propose that adaptation is a universally-relevant treatment goal across a wide range of post-injury, neurodegenerative, and neurodevelopmental conditions. The ability of the sensorimotor system to adapt depends on the involved neural circuits and is critical to neurorehabilitation, where one must (re)learn functional motor skills to access a desired level of mobility and quality of life [2, 102]. In this section, we primarily focus on models of sensorimotor adaptation that characterize the biological process responsible for changes in motor behaviour over time. These models have been successfully applied to study common and functional motor skills, including reaching and gait. Adaptation models have been critical to understanding the learning principles of the sensorimotor system [103–106]. Understanding learning principles can be leveraged to determine the expected behavioural outcomes due to a neurological condition and aid in diagnosis, as well as predicting the behavioural response to treatment.
Sensorimotor adaptation and learning models to improve diagnosis
Studies that examine sensorimotor adaptation in individuals with a neurological condition may be useful for identifying disease biomarkers (e.g., kinematics, neural signals) and developing models that aid a medical practitioner to make a diagnosis. Reaching and gait paradigms have been used to study neurological conditions, including cerebellar ataxia, Parkinson’s disease, and Stroke. For example, during force-field reaching tasks [107], visuomotor rotation reaching tasks [108], and split-belt gait tasks [109] it has been shown that individuals with cerebellar ataxia have less ability to adapt their movement behaviour. Using the kinematic or kinetic data from similar adaptation paradigms could be used by a statistical or machine learning model, potentially in combination with other data (e.g., MRI, eye-tracking), to further inform a diagnosis. Some studies have fit a model separately to neurologically-atypical and neurologically-typical groups [104, 110], and in some instances accounting for medication status [111]. There are limited studies that have used adaptation models to explain a neurological condition [104], which is a very promising direction for future research.
Sensorimotor adaptation and learning models to improve treatment
An attractive feature of adaptation models is that they are dynamic and capture changes in sensorimotor behaviour over time [103–106], which could be leveraged by a medical practitioner to prescribe treatment. Predicting treatment outcomes represents an exciting opportunity for research. An important aspect of the patient-in-the-loop framework is the use of the FITT (frequency, intensity, time, and type) principle to prescribe treatment. Given some type of treatment, adaptation models could theoretically be used to find the optimal frequency, intensity, and time of some therapy to maximize patient outcomes. In terms of movement, these patient outcomes could range from generating straighter reaches [112–114] to producing more symmetric and energetically efficient gait [115–117]. Constraints, such as available time or physical effort, could also be factored into these optimization. Iterative collection of data over time in a patient-in-the-loop framework is necessary to continuously update and personalize model parameters to improve treatment predictions. Better treatment predictions may lead to more informed and effective treatment prescriptions that bolster recovery and habilitation.
State-of-the-art in sensorimotor adaptation and learning modelling
Sensorimotor adaptation can occur through several different mechanisms and their associated neural circuitry, including error-based, reinforcement, and use-dependent learning. Error-based adaptation has implicit and explicit components that reflect cerebellar processes [109, 118–122] and cognitive strategy [123–127], respectively. Error augmentation applies principles of error-based adaptation and has been shown as an effective approach to promote neurorehabilitation for those with stroke [112–114, 128, 129]. Error augmentation magnifies visual and or haptic error signals, the difference between sensory feedback and an expected sensory target, which has been shown to improve both reaching behaviour and clinical measures of functionality for individuals post-stroke [114]. In Fig. 2, we provide a worked example of the patient-in-the-loop framework that uses error augmentation as an intervention type and a model of sensorimotor adaptation to aid in prescribing treatment, with the goal of improving reaching accuracy for an individual post-stroke. Reinforcement-based processes promotes adaptation and neuroplasticity [98, 99, 106, 130–134], Reinforcement processes are linked to the dopaminergic system and basal ganglia, which become impaired with Parkinson’s disease [110, 135, 136]. Interestingly, reinforcement feedback can be used to promote sensorimotor adaptation for individuals with cerebellar ataxia, suggesting that intact reinforcement-based neural circuits can be exploited when there is damage to error-based neural circuits [104]. Use-dependent adaptation refers to the idea that the repetition of movements alone causes a change to the motor system [137, 138], perhaps through Hebbian-like processes (see "Neuroplasticity models" section below). Past research has focussed on isolating these different forms of adaptation [98, 139]. Understanding how these different adaptation processes interact [140], including when specific neural circuits are impacted by a neurological condition, will likely be a fruitful direction moving forward.
Future directions in sensorimotor adaptation and learning modelling to support neurorehabilitation
There are several promising future avenues where computational approaches may facilitate neurorehabilitation. Many of the aforementioned adaptation models have provided strong insights into learning principles and their respective neural circuitry [103, 104, 106, 133]. The majority of these models focus on short-term adaptation and retention, which is thought to reflect the refinement of an already existing motor controller [141]. However, neurorehabilitation occurs over long timescales where it is important to retain (re)learned behaviour over days, months, and even years. Motor learning and retention over these long timescales may align more with de novo learning, where there is thought to be a formation of a new motor controller [141–144]. An example of de novo learning is a child learning (and never forgetting) how to ride a bike (see [145]). More experiments and models are needed to better understand the principles that underlie de novo learning and its potential role in neurorehabilitation [145].
Another exciting opportunity for future research is to better understand how humans co-adapt with a device that aids mobility [146–149]. Wearable robotics that adapt to the human can lead to more energetically efficient gait [150, 151]. Yet further improvements to human-device interaction may be achievable by modelling the co-adaptation between a human and a device [152–154]. An important consideration for devices that (co)adapt is not to provide too much compensation and consequently limit the potential of true recovery by the patient. Rather in some instances it may be better for devices to utilize error augmentation techniques that amplify visual errors or haptic resistance, which has improved recovery for individuals post-stroke [114]. Several open questions remain on how two co-adapting agents interact, whether it be a human-device or therapist-patient, and how this knowledge can be used to support neurorehabilitation (Table 1).
Table 1.
Sensorimotor adaptation and learning: state-of-the-art and future directions
| State-of-the-art | a. Separate models for different adaptation processes: error, reinforcement, |
| and use-dependency. | |
| b. Neural conditions and neural circuits associated with separate learning processes. | |
| c. Experiments and models that focus on short-term (i.e., single day) adaptation | |
| and retention. | |
| Future directions | a. Studies and models that focus on the interaction of multiple learning processes, |
| and exploiting these interacting and or redundant processes for neurorehabilitation. | |
| b. Research paradigms that focus on how motor controllers are constructed from | |
| scratch (de novo) to better understand long-term learning and retention to | |
| provide more effective and long-lasting patient outcomes. | |
| c. Develop models / devices that co-adapt and incorporate how humans learn, | |
| while optimizing assistance and resistance to maximize patient recovery. |
Neuroplasticity models
One of the underlying mechanisms of sensorimotor adaptation and learning is neuroplasticity. Broadly, the term applies to processes by which the nervous system changes, especially in response to experience [155]. Neuroplasticity is related to but not synonymous with the term ‘critical period’. A critical period specifically refers to times of heightened neuroplasticity during development or shortly following a neural injury. An example of a critical period following a neural injury is evident following a stroke. Even within the first few days following stroke there is heightened neuroplasticity, highlighting the importance of early neurorehabilitation [156].
Neuroplasticity models to improve diagnosis
Observations of neuroplasticity at the microscale, mesoscale, or behavioural level could be used to track disease state and update diagnoses. In an animal model of stroke, squirrel monkeys were given subtotal infarcts in hand representation of primary motor cortex [157]. Following subtotal infarcts, there were cortical map changes that were quantified by applying a microelectrode at successive sites in motor cortical area and measuring evoked movements in the upper extremity. These cortical map changes included relative expansion of motor areas subserving proximal forelimb into areas subserving distal forelimb. Although studies of this nature are commonly accepted as proof of neuroplasticity, there are limitations. Rigorous experiments and models must account for pre- and post-operative training and accurately represent human factors, such as relative lesion size and mapping conditions (e.g., during anesthesia vs. during movement).
Neuroplasticity models to improve treatment
Understanding the neuroplastic mechanisms is particularly important to identify precise intervention targets and monitor treatment response [158]. Noninvasive brain stimulation and human-device interaction are promising areas of investigation that tap into neuroplasticity with the goal of improving function after stroke [159].
The literature on efficacy of transcranial magnetic stimulation (TMS) has historically been mixed [160]. Smaller trials have shown efficacy [161, 162], while some large clinical trials have not shown efficacy [163]. It is possible that stimulation models would benefit from parameter optimization [164] to achieve a balance between generalizability and personalization. Excitatory TMS most likely potentiates residual circuitry to make concomitant training more effective [165] and represents a worthwhile avenue of future investigation.
Brain-machine interfaces and brain-computer interfaces have offered a promising approach for studying brain-behaviour relationships across scales in the context of neuroplasticity [166, 167]. The use of brain-machine interfaces and their corresponding algorithms to restore sensorimotor function has gained popularity in recent years for therapeutic purposes. Many promising results have been reported in neurorehabilitation, such as decoding communication for paralyzed people with tetraplegia and anarthria [168] as well as spinal cord injury [169]. These experimental outcomes primarily focus on restoring behavioural and motor functions at a behavioural level. Brain-machine interfaces also offer new avenues to understand neuroplasticity mechanisms that change brain connections at the neuron levels, making them particularly promising for rehabilitative purposes since the neurons involved in these interfaces are causally linked to behaviour. Prior studies have shown positive results, indicating that long-term brain-computer interface training could lead to stable neurocortical mapping [170] and enhance long-term cortical network connectivity [171].
State-of-the-art in neuroplasticity modelling
Neuroplasticity can be observed at multiple spatial scales: synaptic (i.e., microscale), mesoscale, and behavioural [172–174]. Perhaps, the most well-known type of plasticity is Hebbian plasticity, referring to the synaptic principle that “neurons that fire together, wire together” [175]. Hebbian plasticity has been extensively modelled and shown to be regulated by coordinated firing of pre- and post- synaptic neurons at millisecond time intervals, a phenomenon known as spike-time dependence and long-term potentiation [176]. Related concepts are homeostatic plasticity and long-term depression [177]. At the mesoscale, intracortical mapping studies and functional magnetic resonance show reliable changes in cortical areas in response to experience [157, 178–180] as observed with expert musicians [181–185]. Behaviourally, changes in measured behavioural variables are taken to represent changes in nervous system structure and function at the micro- and meso-scale [186]. Additionally, it is important to consider principles of neuroplasticity when developing or utilizing brain-machine interface algorithms that link different spatial scales.
Future directions in neuroplasticity to support neurorehabilitation
Here we identify several potential fruitful areas where neuroplasticity can facilitate neurorehabilitation. First, an attractive idea is for neuroplasticity models to aid in treatment planning. Ideally, one would develop a computational model of neuroplasticity that takes as input the intervention type and frequency of a prescribed treatment to predict functional outcomes. Before this can happen, mathematical equations of neuroplasticity need to be further developed. It will be important to define the specific scales at which these equations are operating, including synaptic, mesoscale, or phenotypic. Synaptic models of plasticity, such as spike-time dependent plasticity, have not been shown to generalize across more than one synapse or to the mesoscale or phenotype/behavioural outcome scales. As such, there is a need for computational models that characterize neuroplastic mechanisms across multiple spatial scales. Second, in addition to spatial scales, new models of neuroplasticity should also account for time scales and how they vary phenotypically within and between populations. The interaction among motor processes also likely changes over time and varies by phenotype. In upper extremity hemiparesis and recovery after stroke, there are multiple motor processes engaged, including reinforcement-based or error-based learning mechanisms [187]. While these processes are dissociable [98], their interaction across the time-course of recovery and habilitation has yet to be characterized. Third, brain-computer interfaces could aid in chronic stroke recovery by inducing neuroplasticity that changes brain connectivity [188]. However, a comprehensive understanding of how to engineer neuroplasticity through the design of brain-machine interfaces is still lacking. Exploring the potential to shape neuroplasticity through the design or adaptation of brain-machine interfaces represents a promising direction for future research [189]. Fourth, few studies have sought to understand the effects of movement itself on structural and functional neuroplasticity. Given that movement is a mainstay of treatment in neurorehabilitation (e.g., in the context of physical or occupational therapy), this is a promising avenue for investigation with high translational potential. Moving forward it will be important to link spatial and temporal neuroplastic changes to behaviour, and then target these neuroplastic-behavioural relationships with treatment to improve functional outcomes for those with neurological conditions (Table 2).
Table 2.
Neuroplasticity: state-of-the-art and future directions
| State-of-the-art | a. Hebbian learning models: spike-time dependence, long-term potentiation, |
| homeostatic plasticity, and long-term depression | |
| b. Models at distinct spatial scales: microscale, mesoscale, phenotypic / behaviour. | |
| c. Brain-machine interface algorithms that relate neuronal activity to behaviour. | |
| Future directions | a. Experiments and models that link the multiple spatial and temporal scales of |
| neuroplasticity that can be used to developed informed and optimized treatment. | |
| b. Improving brain machine interface (BMI) design and developing brain machine | |
| interface algorithms that enhance neuroplasticity. | |
| c. More fundamental studies that examine understand the influence of movement | |
| on structural and functional neuroplasticity. |
Musculoskeletal models
Musculoskeletal models are computational representations of the biological musculoskeletal system, designed to simulate and analyze biological movements. By leveraging patients’ physical data (e.g., height, weight, age, strength, MRI, etc.) and movement data (e.g., kinematics and force/moments), customized models can be built to analyze recorded movements and estimate muscle activations and states (”tracking approach”) [190]. Additionally, musculoskeletal models, or neuromechanical models that also encompass neural control models in addition to musculoskeletal components, can be used to produce new motions in response to changes in the musculoskeletal system and environment, known as the ”predictive approach” [191, 192]. By using musculoskeletal models to track and predict movements, critical insights can be gained, providing timely diagnosis, personalized treatment for movement condition, and advanced understanding of biomechanics.
Musculoskeletal models to improve diagnosis
Musculoskeletal models are crucial for dissecting the root causes of neuromusculoskeletal conditions, quantifying their features, and communicating the nuances of these conditions to clinicians and patients. One promising application is to help identify underlying causes of impairments [116, 193, 194]. Once a model incorporating all potential neuromechanical factors of a patient is developed (e.g., muscle atrophy and sensorimotor noise), an ablation study can be performed (e.g., simulate with the potential factors one-by-one) to identify the most critical factors that most likely contributed to the impairment. Treatment plans can then be tailored more precisely, potentially leading to more effective interventions. Another potential use of musculoskeletal and neuromechanical models is to provide clinicians with a comprehensive quantification and visualization of a patient’s neuromechanics of movement, offering a detailed depiction of aspects such as joint movement [195], muscle length and force [196], muscle activations [197] and synergies [198, 199], and energy consumption [200]. Using these enhanced analyses on a patient’s movement could improve both clinicians’ and patients’ understanding of the impairments, clarifying the rationale behind prescribed treatments. These models can also be used to quantify the severity of movement abnormalities, complementing clinical metrics that are often subjective (e.g., Fugl-Meyer score [38]).
Musculoskeletal models to improve treatment
Musculoskeletal and neuromechanical models can also be used in the design, outcome prediction, and monitoring of various treatment modalities for movement conditions. For example, potential effects of physical therapy and exercise interventions can be simulated with these models [201, 202], leading to more precise implementation of targeted interventions that promote neuroplasticity and adaptation. Musculoskeletal simulations can also help surgeons to predict the potential impact of different surgical strategies on musculoskeletal outcomes [203, 204]. Furthermore, assistive device design (e.g., exoskeletons, prostheses, braces) can benefit from musculoskeletal models by analyzing and predicting interactions between the devices and the human body [205–207]. Musculoskeletal models can estimate patient body states in real-time, providing a basis for the control of assistive devices [208–210]. Musculoskeletal models can also facilitate the monitoring of rehabilitation progress, enabling clinicians to objectively assess the effectiveness of interventions and track patient improvement over time.
State-of-the-art in musculoskeletal modelling
Over the last two decades, musculoskeletal and neuromechanical modelling has advanced significantly. Initially focused on tracking approaches to estimate joint dynamics and muscle activations [190, 211], the field is now embracing predictive methodologies to study motion variations under different musculoskeletal and environmental conditions [191, 192]. These models have enriched understanding of human movement and musculoskeletal conditions, shedding light on injury mechanisms like ACL ruptures [212] and ankle sprains [213], and aiding clinical decisions in osteoarthritis cases by assessing joint load [214, 215]. They have been used in evaluating surgical outcomes, such as hamstring lengthening surgery for children with crouch gait [216], and have helped characterize the impacts of musculoskeletal changes on movement patterns in aging [193], muscle atrophy [194, 217], and hemiparetic gait [116]. Moreover, these models are being applied in developing exoskeletons and prostheses [206, 218–220], and integrated into real-time controllers for assistive devices [209, 218, 221, 222].
Future directions in musculoskeletal modelling to support neurorehabilitation
While primarily used to study and evaluate musculoskeletal conditions today, musculoskeletal models are poised for substantial progress that could dramatically enhance their precision and clinical relevance in neurorehabilitation. As shown in the worked example of the patient-in-the-loop framework in Figure 3, musculoskeletal models could be employed to customize physical therapy programs and the design or prescription of assistive devices. This customization would be specifically tailored to an individual patient’s mobility level, clinical phenotype, and rehabilitation goals, thus underlining the pivotal role of these models in future neurorehabilitation strategies.
Model customization is necessary to capture patient-specific musculoskeletal features for diagnosis and treatment, possibly through the use of MRI, ultrasound, dynamometry, and motion data. Despite the importance of developing neuromechanical control and learning models that can predict human behaviour, it remains an immense challenge largely due to our limited understanding of the nervous system. Here we highlight potentially valuable directions. First, it will be important to refine objective functions to generate more reliable and accurate predictions. Current research predominantly utilizes optimality principles based on metabolic energy and muscle activation to produce predictions. However, it will be valuable to explore other physiologically-plausible objectives, such as stability [223, 224], fatigue [225], and comfort [226]. Second, more advanced physiologically-plausible control models [227–230] are necessary, extending beyond the current focus on locomotion to include a broader range of movements. The integration of advanced machine learning techniques, such as deep reinforcement learning, could be critical in training controllers to produce this more diverse range of movements [192]. Third, the inclusion of further neurological details, such as sensory dynamics, activation dynamics, and the properties of neural activation, could make our neuromechanical models more congruent with actual neural activity recordings [231], thereby enhancing their realism and applicability. Fourth, incorporating sensorimotor adaptation and learning models into neuromechanical simulations holds potential for advancing neurorehabilitation modelling. Such incorporations could show how musculoskeletal alterations, assistive devices, or interventions may induce movement adaptations. Fifth, adapting these control models to accommodate neural pathologies represents both a significant challenge and an indispensable step towards enhancing their relevance in neurorehabilitation (Table 3). Collectively, these advancements could be complemented by rigorous experimental validation involving human experiments [232]. Importantly, collaboration with clinicians is necessary to ensure that any advanced models tools are developed and utilized to meet the requirements of clinical practice and patient care.
Table 3.
Musculoskeletal: state-of-the-art and future directions
| State-of-the-art | a. Predictive models of motion under different musculoskeletal and environmental |
| conditions, ranging from changes due to age and walking over uneven terrains. | |
| b. Modelling musculoskeletal conditions and injury, such as osteoarthritis. | |
| c. Evaluating surgical outcomes, such as hamstring lengthening for crouch gait. | |
| d. Modelling human-assistive device interactions with integrated real-time control. | |
| Future directions | a. Consider plausible objectives in cost functions that relate to patient goals, |
| including stability, fatigue, and comfort. | |
| b. Inclusion of neurological details that become impacted with neurological | |
| conditions, such as sensory feedback and other neural dynamics. | |
| c. Incorporating learning and neuroplasticity principles, which are important | |
| when recovering from a neural condition or interacting with an assistive device. | |
| d. Advancing models to accommodate various neural condition and injury. |
Sensory and pain models
Mathematical and computational techniques can be used to simulate processes underlying sensory perception and pain sensation. These models aim to capture the complex interactions between various physiological, neural, and cognitive factors across a wide range of conditions including neuropathic pain, migraine, autism, and Parkinsonism. Sensory models can inform the development of better diagnostic tools and treatment approaches, including advanced neuroprosthetic devices. Computational modelling offers a less-invasive means of generating new knowledge on human sensation and pain compared to in vivo experimental paradigms. Yet, such models have been based on neurotypical function and development, neglecting to characterize atypical acquisition, processing, integration, and use of sensory information. This has limited their application in clinical research and in diagnosis and management of conditions with known sensory processing differences.
Sensory models to improve diagnosis
Current diagnostic practice for atypical sensory function in neurodevelopmental and neurodegenerative conditions relies heavily on clinician observation (e.g., Romberg’s Test [233]), patient self-report (e.g., Adolescent/Adult Sensory Profile [234]) or standardized assessments with binary or ternary scoring systems (e.g., Mini-BEST [235]). We have yet to comprehensively model the complexities of atypical sensory processing and their manifestation within or between clinical populations, and across development. For example, a clinician may observe similar postural instability and sensitivity to auditory stimuli in a patient diagnosed with superior canal dehiscence syndrome and a patient diagnosed with autism, but the two have very different neurobiology and require different management of their sensory experiences.
Visuomotor integration is a promising target for computational modelling to characterize the link between behaviour and neural mechanisms. Sensory weighting for postural control and movement is heavily reliant on visual input in early and middle childhood, and more adaptable in adolescence [236–238]. [239]. Neurotypical adults maintain the ability to reweigh sensory information based on its integrity or availability but return to visual over-dependence with aging, which increases their risk of falls [240]. However, neurodevelopmental conditions like developmental coordination condition and autism may not exhibit typical sensory reweighing in some contexts [241–244]. Condition-specific models could offer precise diagnostic tools for distinguishing typical from atypical development and differentiating between neurodevelopmental conditions.
Recent advances in human-device interaction also support precise diagnosis of atypical sensory function. For example, to assess proprioceptive integrity following stroke or in response to perturbation [52, 245–248]. To optimize diagnostic and treatment applications of computational modelling, we must address questions of model sensitivity and specificity. Both condition-specific and general models must characterize the functional and temporal interplay between sensory systems [249], given the known importance of multisensory processing.
Sensory models to improve treatment
Visuo-proprioceptive recalibration represents a promising intervention type to improve sensory function, as evidenced in the reaching literature [250–253]. Computational modelling has been used recently to explain this sensorimotor adaptation process [254]. Visuo-proprioceptive feedback training shows promise for fall prevention in healthy aging [255] and improvement of bradykinesia in Parkinsonism [256]. Recent work suggests that proprioceptive, but perhaps not visual, recalibration is retained after remapping [257]. Computational modelling can be used to determine whether sensory recalibration potential differs between or within populations, enabling clinicians to predict who may benefit most from this approach.
Computational models personalized to patient-specific factors can predict the success of adaptation to neuroprosthetics, as seen in cochlear implant development [258]. As users adapt to implants, sensory remapping improves speech perception [5]. This process takes time and can lead to frustration or disuse. Acoustic models that drive cochlear implants are constrained by the number and tuning of channels, temporal resolution, and topographical discrepancy between the frequency information provided by the electrode and the natural tuning of the cochlea. Interactive genetic algorithms and evolutionary algorithms can support optimization of acoustic models at a more efficient rate of convergence than natural adaptation [259, 260]. Models simulating listener errors can also be used to inform development of such algorithms [258]. Demonstrating the utility of integrating models into a patient-in-the-loop framework, self-selected acoustic models for cochlear implants tuned to individual parameters via method-of-adjustment outperform high-dimensional models [261]. This approach highlights the need for a balance between efficient, generalizable models, and those personalized to account for individual features to optimize the efficiency and quality of rehabilitation.
State-of-the-art in sensory modelling
In the recent past, researchers focused on mimicking the natural coding of touch and integrating them into bionic devices in form of so-called biomimetic paradigms [262, 263]. To replicate the reality, receptor and afferent responses are simulated to estimate how mechanical input will be transformed into afferent spike trains and transmitted to higher-order somatosensory areas [264, 265]. These models offer a better understanding of touch afferent activation, as well as overcoming a major limitation of direct electrophysiological measurements which require stationary conditions, enabling analysis of activity in situations like walking or jogging. Similar models are also used to mimic the response of proprioceptors [266, 267], providing a novel guideline for controlling sensory restoration. Improvement of these models depends on the availability of large human and animal datasets containing electrophysiological recordings of afferent responses across a variety of different types of stimulation.
Mathematical representations of pain can guide development of hypotheses about underlying intervention targets. Most established computational models of pain focus primarily on binary prediction of pain perception using machine learning algorithms [268, 269]. These approaches typically fail to account for the specific features driving pain perception [270]. Computational models can also be used to understand and predict the pain perception-action cycle [271]. These models describe the dynamic interaction between the sensory experience of pain and the behavioural response [272, 273]. Most established models of pain are data-driven and based on neural networks [274–278]. By contrast, to our knowledge, there are relatively few hypothesis-driven, mechanistic models of pain.
Future directions in sensory modelling to support neurorehabilitation
The field of neurorehabilitation is faced with several remaining challenges in pursuit of robust, comprehensive sensory models. Models of motor control based on neurotypical development may not capture critical variability in sensory information acquisition. For example, atypical oculomotor control is a feature of many conditions (e.g., autism, schizophrenia, Parkinsonism) that poses challenges for the development of robust eye movement models. Atypical postural control is also a feature of many conditions that poses challenges for the development of generalizable models of body movement. Comprehensive multisensory models are essential for advancing technologies used in research and clinical contexts to quantify sensory processing in more naturalistic, less-invasive contexts.
Sensory experiences are highly subjective and influenced by psychological factors such as expectation [279], catastrophizing [280], optimization to the environment and task [281], and co-occurring conditions [282]. Pain experiences are also subject to the influence of contextual, social, psychological, and cultural factors [283]. These factors are often neglected or poorly operationalized in physiological studies. Mixed-methods approaches can be used to characterize the human sensory-perceptual experience, as qualitative responses can help to contextualize physiological and behavioural data [284]. Models that account for the full complexity of sensation and pain perception are needed to support development of comprehensive pain management strategies that address all relevant dimensions in concert (Table 4).
Table 4.
Sensory and pain: state-of-the-art and future directions
| State-of-the-art | a. Separate models for typical development and for specific neurodevelopmental |
| and neurodegenerative conditions. | |
| b. Experimental paradigms and models that constrain dimensionality. | |
| Future directions | a. Multisensory models that consider feedforward and feedback mechanisms. |
| b. Sensitive and specific diagnostic models that account for general population | |
| variability and phenotypic heterogeneity within conditions. | |
| c. High-dimensional diagnostic and treatment models that account for interplay | |
| between physiological, cognitive, emotional, and behavioral factors to support | |
| optimization and personalization. |
The proposed patient-in-the-loop framework is a means of ensuring that lived experiences and psychological/perceptual influences on sensory and pain processes are not lost in assessment and management. Fig. 4 offers a worked example of applying this framework to specific visuomotor neurohabilitation goals in autism, though certainly it has many other habilitation and rehabilitation applications. As in other domains of modelling, it is crucial to achieve a balance between data-driven and hypothesis-driven approaches to ensure that resulting knowledge is theoretically-productive and interpretable. Focus should be directed to development of models that offer new information about the relative importance of specific features used to predict or explain clinically-relevant outcomes [285], while factoring patient goals and constraints.
Model validation
Modelling across all domains depends on rigorous validation to render models reliable as diagnostic, treatment, or research tools. Unification of validation processes across the field of neurorehabilitation is crucial to maximize the validity and translational potential of computational modelling. Best practice guidelines proposed for musculoskeletal model validation [286] could be adapted and extended to also accommodate models of adaptation, neuroplasticity, and sensation/perception.
Validation targets
Determining the validity of a model entails evaluating: 1. Is the model feasible (e.g., does the fundamental model appropriately represent the hypothesis it aims to capture)?, and 2. Is the model accurate (i.e., does the model correctly reproduce the input–output relationship observed in the real world)? Feasibility must be satisfied before any meaningful interpretation of model behaviour can be made. Otherwise, model outputs do not reflect the hypothesized relationship, regardless of how well they may fit experimental data. Model accuracy must be evaluated against experimental observations. Models can be adjusted or reconceptualized to reduce model error (the difference between model-generated outputs and experimentally observed outputs), or discarded if experiments indicate no relationship between the hypothesis represented by the model and the observed behaviour.
The use of robust statistics and obtaining confidence intervals of parameter values are useful for model fitting. An absolute loss function, specifically the absolute difference between model-generated outputs and experimentally observed outputs, is known to be more robust than squared error since it is less sensitive to outliers [98, 287–289]. Once a loss function is selected, it is useful to find the confidence intervals of each model parameter. Bootstrapping is a resampling technique that can provide a nonparametric confidence interval for each model parameter [290]. Another benefit of bootstrapping is that statistical inference can be performed between different models since the confidence intervals are known [99, 106]. For example, one can calculate the probability that a neurotypical group will have significantly different model parameters than those with a neurological condition.
Goodness of fit versus overfitting
It is also important to consider, however, that perfectly matching a set of observed behaviours is not the only purpose of a model. Instead, a useful model captures the critical dynamics between phenomena that drive most of the change in output given some change in input. Identifying the model parameters that dominate input–output dynamics is possible through sensitivity and uncertainty analyses [291], which generally involve perturbing model inputs in sequence and measuring the output response.
To find the simplest model that best explains the data and prevent overfitting an over-parameterized model to noise [292], tools such as AIC (Akaike Information Criterion) and BIC (Bayesian Information Criterion) consider the quality of the fit while penalizing the number of free parameters. Further, BIC and AIC can also provide insight into which of several theories, each represented by a model, is more likely to be true [99, 292, 293]. Cross validation is another useful approach to prevent overfitting and to test model accuracy. Cross validation uses multiple different subsets of the original data to fit the data, and then tests the resulting model accuracy on the remaining subsets of the data [294, 295]. This approach is particularly popular for machine learning and is useful for testing how accurate a model is when applied to new data sets. Utilizing models that are not overfit and generalize to new data sets will be particularly important when attempting to diagnose or prescribe treatment.
Future factors to consider for model validation
Adherence to rigorous model validation is a critical step for ensuring that the development of a model-assisted neurorehabilitation paradigm will be appropriately robust. Ensuring that experiments are sufficiently powered is an important factor not only for reproducibility, but also for testing theories and model validation [296–300]. Model validation efforts should be supported by standardized criteria that are valid across the spectrum of proposed model scope, from population-level models to fully individualized “digital twins”. Clinical acceptance of computational models in a clinical rehabilitation framework will likely be greatly aided by such an effort to reliably demonstrate that these models are trustworthy. It is the responsibility of computational modellers to ensure that models do not impede the ability of clinicians or patients to make informed decisions, but rather strengthen it.
Challenges
In addition to the model-specific challenges already discussed, there also exist challenges related to the data which serve as the input to all models described above. The access to high-dimensional, multi-modal data collected from ecologically-valid situations represents a potential paradigm shift in neurorehabilitation. However, there are several open challenges that must first be addressed to use this data effectively within computational modelling for neurorehabilitation. First, it is critical to identify what data is needed for each model. This involves identifying primary outcome measure(s) of interest (e.g., walking speed, community participation, etc.) and the physiological, biomechanical, and or clinical variables that are most relevant to that outcome measure. This step can require large samples of diverse patients to overcome the heterogeneity within a population (e.g., stroke, Parkinson’s disease, etc.), often necessitating multi-site collaboration. Thus, the second challenge is to overcome the potential inconsistency in data quality or availability across locations, people, days, etc. For example, MRI imaging quality can vary depending on scanner type, strength, pulse sequences, etc. A model that overcomes this variability will have the most potential for impact on neurorehabilitation [301]. In a similar vein, wearable sensor data to monitor movement can be sensitive to sensor placement and orientation [302–304]. Thus, models that rely on wearable sensor data must account for such variability to achieve optimal performance. Third, it is critical to carefully assess the performance of group-level statistics versus individualized data for model predictions. Or in other words, how much model personalization is necessary. In some cases, group-level statistics may be sufficient. For example, many studies have successfully grouped stroke patients based on their similarity in clinical, biomechanical, and/or physiological impairments [85, 86, 88, 89]. Do patients within each of these groups respond similarly to rehabilitation? If so, then models based on group-level statistics may be sufficient. In other cases, however, personalization may be critical. For example, personalized neural control models are able to better predict the immediate response to surgery in children with cerebral palsy [305] and stroke gait under novel conditions [306] than group-level and generic models. Determining the optimal level of personalization for any model will require careful assessment and evaluation of the extent to which additional and meaningful predictive capabilities are gained with increasing personalization. Lastly, developing models that rely on multiple time-point and/or continuous monitoring of multi-modal data in real-world settings require careful processing and advanced modelling techniques to analyze the large data sets that are generated. Deep learning methods that use the entire dataset instead of a reduced representation show promise in capturing subtle but important individual-specific patterns, which can guide clinical decision making via purely data-driven modelling approaches or serve as input into mechanistic, fundamental models. However, there is still substantial work to be done to guarantee the accuracy of these models in capturing the heterogeneity present across individuals and their utility in predicting response to neurorehabilitation.
We believe that implementing computational modelling within the clinical setting is a fruitful goal to strive towards. Yet there are several potential challenges, some of which we briefly mention here. There will likely have to be agreement on some of the tasks used to collect patient data [307], so that there is consistent and a sufficient amount of data to properly validate models. As mentioned above, it is imperative to ensure models are properly validated and viable before implementing to inform diagnostics and treatment. From a modelling perspective, many of the computation models have been designed and validated for very specific scenarios (e.g., walking in a straight line at a steady velocity, or reaching towards a target while moving the arm only in the horizontal plane). It will be important to develop models that generalize and capture more naturalistic movements that are relevant to the functionality of a patient. As mentioned in the introduction, a major challenge is getting researchers from multiple disciplines (engineerings, clinicians, etc.) to productively work together towards a common goal, despite often very different approaches and skillsets [6, 7]. To facilitate these collaborations, educational and technical workshops aimed at both clinicians and computational modellers would be beneficial to better understand one another’s theory, approach, and terminology. Increased federal funding towards (i) providing educational and technical workshops for modellers and clinicians, (ii) conferences that focus on computational modelling in neurorehabiliation that is attended by both clinicians and modellers, and (iii) grants that support collaboration between clinicians and computational modellers with the goal of improving neurorehabilitation would help to overcome many of these challenges.
Summary and moving forward
We have proposed where and how computational modelling can be used to aid clinical diagnosis and treatment within our proposed patient-in-the-loop framework. In this perspective piece, we identified current state-of-the-art and highlighted potentially fruitful avenues of computational modelling across sensorimotor adaptation (e.g., co-adaptation with a device), neuroplasticity (e.g., linking spatial scales of neurons), musculoskeletal (e.g., stability), sensory (e.g., pain perception), and machine learning (e.g., optimal dynamic treatment regime [9, 96]) that can be used to support neurorehabilitation. It is imperative to validate these models before using them to help inform diagnosis and treatment. We believe that it will be equally important to take both mechanistic or patient-centered approaches that respectively consider underlying processes and functional outcomes, to eventually provide causal links along the continuum between neurons and behaviour.
Our patient-in-the-loop framework provides a guide to facilitate multidisciplinary research to improve patient recovery and habilitation. Our framework is intentionally general, in a similar vein to the ICF that it incorporates, so that it can be applied to a broad range of neurological diseases (e.g., Stroke, multiple sclerosis, etc.) and neurodevelopment conditions (e.g., autism). It incorporates the idea of multiple and or continuous data measurements of a patient’s condition over time, as described in a recent precision rehabilitation framework [9]. Further, this framework includes patient involvement throughout the process, from data collection to prescribed treatment, which has shown to improve patient satisfaction, treatment outcome, and health [22–28]. Importantly, this patient-in-the-loop framework identifies where and how computational modelling can support neurorehabilitation within a clinical pipeline. We encourage clinicians and modellers to utilize or adapt this patient-in-the-loop framework to develop informed and effective neurorehabilitation.
Acknowledgements
The authors would like to thank John Buggeln and Darcy Reisman for early discussion on the patient-in-the-loop framework, as well as R. James Cotton for discussion related to the precision rehabilitation framework. We would also like to thank the organizers, Francisco Velero-Cuevas, James Finley, Amy Orsborn, Kat Steele, and Natalie Fung, of the 2023 NSF DARE conference: Transformative Opportunities for Modeling in Neurorehabilitation, for putting together the team of authors and the opportunity to write this perspective piece.
Author contributions
All authors contributed to conceptualization and manuscript writing.
Funding
National Science Foundation (NSF CAREER 2146888) Grant awarded to JGAC. National Science Foundation (NSF DARE 2245260) Grant awarded to JLA. Department of Veterans Affairs (1IK2RX004237) award to DJL.
National Institutes of Health (NIH R00AG065524) Grant to SS. National Institutes of Health (K01-MH107774) Grant to HLM. Project IDEJE by Science Fund of the Republic of Serbia (7753949) awarded to NKS.
NSF DARE (2240277). NSF CBET DARE (2240277).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Joshua G. A. Cashaback, Email: cashabackjga@gmail.com
Haylie L. Miller, Email: millerhl@umich.edu
References
- 1.Albert SJ, Kesselring J. Neurorehabilitation of stroke. J Neurol. 2012;259(5):817–832. doi: 10.1007/s00415-011-6247-y. [DOI] [PubMed] [Google Scholar]
- 2.Reinkensmeyer DJ, Dietz V, et al. Neurorehabilitation technology. Berlin: Springer; 2016. [Google Scholar]
- 3.Krebs HI, Hogan N, Aisen ML, Volpe BT. Robot-aided neurorehabilitation. IEEE Trans Rehabilit Eng. 1998;6(1):75–87. doi: 10.1109/86.662623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weiss PL, Kizony R, Feintuch U, Katz N, et al. Virtual reality in neurorehabilitation. Textb Neural Repair Rehabilit. 2006;51(8):182–97. [Google Scholar]
- 5.Holden MK, Dyar T. Virtual environment training: a new tool for neurorehabilitation. J Neurol Phys Ther. 2002;26(2):62–71. [Google Scholar]
- 6.Oppenheimer R, Regep C, Rukat T, Skates A, et al. Ten simple rules for surviving an interdisciplinary PhD. PLoS Comput Biol. 2017;13(5):e1005512. doi: 10.1371/journal.pcbi.1005512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Islam S, Wells CA. Ten simple rules for navigating the computational aspect of an interdisciplinary PhD. PLoS Comput Biol. 2021;17(2):e1008554. doi: 10.1371/journal.pcbi.1008554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Üstün TB, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The international classification of functioning, disability and health: a new tool for understanding disability and health. Disabil Rehabilit. 2003;25(11–12):565–571. doi: 10.1080/0963828031000137063. [DOI] [PubMed] [Google Scholar]
- 9.Cotton RJ, Seamon B, McLead M, David R, Sahu A, Ramey S, Segal R. Portable, in-clinic, video-based analysis of gait impairments. In: NSF DARE Conference: Transformative Opportunities for Modeling in Neurorehabilitation. 2023.
- 10.Translational science spectrum. https://ncats.nih.gov/translation/spectrum. Accessed 20 Apr 2023.
- 11.Haidar A. The artificial pancreas: how closed-loop control is revolutionizing diabetes. IEEE Control Syst Mag. 2016;36(5):28–47. [Google Scholar]
- 12.Ramli R, Reddy M, Oliver N. Artificial pancreas: current progress and future outlook in the treatment of type 1 diabetes. Drugs. 2019;79:1089–1101. doi: 10.1007/s40265-019-01149-2. [DOI] [PubMed] [Google Scholar]
- 13.Ghita M, Neckebroek M, Muresan C, Copot D. Closed-loop control of anesthesia: Survey on actual trends, challenges and perspectives. IEEE Access. 2020;8:206264–206279. [Google Scholar]
- 14.Zurakowski R. Nonlinear observer output-feedback MPC treatment scheduling for HIV. Biomed Eng Online. 2011;10(1):1–16. doi: 10.1186/1475-925X-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stucki G. International classification of functioning, disability, and health (ICF): a promising framework and classification for rehabilitation medicine. Am J Phys Med Rehabilit. 2005;84(10):733–740. doi: 10.1097/01.phm.0000179521.70639.83. [DOI] [PubMed] [Google Scholar]
- 16.Stucki G, Cieza A, Ewert T, Kostanjsek N, Chatterji S, Ustun TB. Application of the international classification of functioning, disability and health (ICF) in clinical practice. Disabil Rehabilit. 2002;24(5):281–282. doi: 10.1080/09638280110105222. [DOI] [PubMed] [Google Scholar]
- 17.Schneidert M, Hurst R, Miller J, Üstün B. The role of environment in the international classification of functioning, disability and health (ICF) Disabil Rehabilit. 2003;25(11–12):588–595. doi: 10.1080/0963828031000137090. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . International classification of functioning, disability, and health: children & youth version: ICF-CY. Geneva: World Health Organization; 2007. [Google Scholar]
- 19.Rauch A, Cieza A, Stucki G. How to apply the international classification of functioning, disability and health (ICF) for rehabilitation management in clinical practice. Eur J Phys Rehabilit Med. 2008;44(3):329–342. [PubMed] [Google Scholar]
- 20.Simeonsson RJ, Leonardi M, Lollar D, Bjorck-Akesson E, Hollenweger J, Martinuzzi A. Applying the international classification of functioning, disability and health (ICF) to measure childhood disability. Disabil Rehabilit. 2003;25(11–12):602–610. doi: 10.1080/0963828031000137117. [DOI] [PubMed] [Google Scholar]
- 21.Imrie R. Demystifying disability: a review of the international classification of functioning, disability and health. Sociol Health Illn. 2004;26(3):287–305. doi: 10.1111/j.1467-9566.2004.00391.x. [DOI] [PubMed] [Google Scholar]
- 22.Marzban S, Najafi M, Agolli A, Ashrafi E. Impact of patient engagement on healthcare quality: a scoping review. J Patient Exp. 2022;9:23743735221125439. doi: 10.1177/23743735221125439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care: effects on patient outcomes. Ann Int Med. 1985;102(4):520–528. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- 24.Vahdat S, Hamzehgardeshi L, Hessam S, Hamzehgardeshi Z. Patient involvement in health care decision making: a review. Iran Red Crescent Med J. 2014;16(1):e12454. doi: 10.5812/ircmj.12454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Entwistle VA, Watt IS. Patient involvement in treatment decision-making: the case for a broader conceptual framework. Patient Educ Couns. 2006;63(3):268–278. doi: 10.1016/j.pec.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 26.Thompson AG. The meaning of patient involvement and participation in health care consultations: a taxonomy. Soc Sci Med. 2007;64(6):1297–1310. doi: 10.1016/j.socscimed.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 27.Martin LR, Di Matteo MR, Lepper HS. Facilitation of patient involvement in care: development and validation of a scale. Behav Med. 2001;27(3):111–120. doi: 10.1080/08964280109595777. [DOI] [PubMed] [Google Scholar]
- 28.Davis RE, Jacklin R, Sevdalis N, Vincent CA. Patient involvement in patient safety: what factors influence patient participation and engagement? Health Expect. 2007;10(3):259–267. doi: 10.1111/j.1369-7625.2007.00450.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parastarfeizabadi M, Kouzani AZ. Advances in closed-loop deep brain stimulation devices. J Neuroeng Rehabilit. 2017;14(1):1–20. doi: 10.1186/s12984-017-0295-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Velisar A, Syrkin-Nikolau J, Blumenfeld Z, Trager M, Afzal M, Prabhakar V, Bronte-Stewart H. Dual threshold neural closed loop deep brain stimulation in Parkinson disease patients. Brain Stimul. 2019;12(4):868–876. doi: 10.1016/j.brs.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 31.Christ O, Wojtusch J, Beckerle P, Wolff K, Vogt J, von Stryk O, Rinderknecht S. Prosthesis-user-in-the-loop: user-centered design parameters and visual simulation. In: 2012 Annual international conference of the IEEE Engineering in Medicine and Biology Society. IEEE, 2012:1929–32. [DOI] [PubMed]
- 32.Welker CG, Voloshina AS, Chiu VL, Collins SH. Shortcomings of human-in-the-loop optimization of an ankle-foot prosthesis emulator: a case series. R Soc Open Sci. 2021;8(5):202020. doi: 10.1098/rsos.202020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fregly BJ. A conceptual blueprint for making neuromusculoskeletal models clinically useful. Appl Sci. 2021;11(5):2037. [Google Scholar]
- 34.World Health Organization. Towards a common language for functioning, disability, and health: ICF. In: The international classification of functioning, disability and health. 2002.
- 35.Tempest S, McIntyre A. Using the ICF to clarify team roles and demonstrate clinical reasoning in stroke rehabilitation. Disabil Rehabilit. 2006;28(10):663–667. doi: 10.1080/09638280500276992. [DOI] [PubMed] [Google Scholar]
- 36.van Uem JM, Marinus J, Canning C, van Lummel R, Dodel R, Liepelt-Scarfone I, Berg D, Morris ME, Maetzler W. Health-related quality of life in patients with Parkinson’s disease–a systematic review based on the ICF model. Neurosci Biobehav Rev. 2016;61:26–34. doi: 10.1016/j.neubiorev.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 37.Mahdi S, Albertowski K, Almodayfer O, Arsenopoulou V, Carucci S, Dias JC, Khalil M, Knüppel A, Langmann A, Lauritsen MB, et al. An international clinical study of ability and disability in autism spectrum disorder using the WHO-ICF framework. J Autism Dev Disord. 2018;48:2148–2163. doi: 10.1007/s10803-018-3482-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gladstone DJ, Danells CJ, Black SE. The Fugl-Meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabilit Neural Repair. 2002;16(3):232–240. doi: 10.1177/154596802401105171. [DOI] [PubMed] [Google Scholar]
- 39.Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23(15):2129–2170. doi: 10.1002/mds.22340. [DOI] [PubMed] [Google Scholar]
- 40.Tao W, Liu T, Zheng R, Feng H. Gait analysis using wearable sensors. Sensors. 2012;12(2):2255–2283. doi: 10.3390/s120202255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hester T, Hughes R, Sherrill DM, Knorr B, Akay M, Stein J, Bonato P. Using wearable sensors to measure motor abilities following stroke. In: International Workshop on Wearable and Implantable Body Sensor Networks (BSN’06). IEEE, 2006. p. 4.
- 42.Chang JO, Levy SS, Seay SW, Goble DJ. An alternative to the balance error scoring system: using a low-cost balance board to improve the validity/reliability of sports-related concussion balance testing. Clin J Sport Med. 2014;24(3):256–262. doi: 10.1097/JSM.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 43.Poitras I, Bielmann M, Campeau-Lecours A, Mercier C, Bouyer LJ, Roy J-S. Validity of wearable sensors at the shoulder joint: combining wireless electromyography sensors and inertial measurement units to perform physical workplace assessments. Sensors. 2019;19(8):1885. doi: 10.3390/s19081885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nordin AD, Hairston WD, Ferris DP. Dual-electrode motion artifact cancellation for mobile electroencephalography. J Neural Eng. 2018;15(5):056024. doi: 10.1088/1741-2552/aad7d7. [DOI] [PubMed] [Google Scholar]
- 45.Mathis A, Mamidanna P, Cury KM, Abe T, Murthy VN, Mathis MW, Bethge M. DeepLabCut: markerless pose estimation of user-defined body parts with deep learning. Nat Neurosci. 2018;21(9):1281–1289. doi: 10.1038/s41593-018-0209-y. [DOI] [PubMed] [Google Scholar]
- 46.Kanko RM, Laende EK, Davis EM, Selbie WS, Deluzio KJ. Concurrent assessment of gait kinematics using marker-based and markerless motion capture. J Biomech. 2021;127:110665. doi: 10.1016/j.jbiomech.2021.110665. [DOI] [PubMed] [Google Scholar]
- 47.Drotár P, Mekyska J, Rektorová I, Masarová L, Smékal Z, Faundez-Zanuy M. Evaluation of handwriting kinematics and pressure for differential diagnosis of Parkinson’s disease. Artificial Intell Med. 2016;67:39–46. doi: 10.1016/j.artmed.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 48.Pagan FL. Improving outcomes through early diagnosis of Parkinson’s disease. Am J Manag Care. 2012;18(7):S176. [PubMed] [Google Scholar]
- 49.Mercuri NB, Bernardi G. The ‘magic’of L-dopa: why is it the gold standard Parkinson’s disease therapy? Trends Pharmacol Sci. 2005;26(7):341–344. doi: 10.1016/j.tips.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 50.Kahn LE, Lum PS, Rymer WZ, Reinkensmeyer DJ. Robot-assisted movement training for the stroke-impaired arm: does it matter what the robot does? J Rehabilit Res Dev. 2014;43(5):619–630. doi: 10.1682/jrrd.2005.03.0056. [DOI] [PubMed] [Google Scholar]
- 51.Kwakkel G, Kollen BJ, Krebs HI. Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Neurorehabilit Neural Repair. 2008;22(2):111–121. doi: 10.1177/1545968307305457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Semrau JA, Herter TM, Scott SH, Dukelow SP. Examining differences in patterns of sensory and motor recovery after stroke with robotics. Stroke. 2015;46(12):3459–3469. doi: 10.1161/STROKEAHA.115.010750. [DOI] [PubMed] [Google Scholar]
- 53.Picelli A, Melotti C, Origano F, Waldner A, Gimigliano R, Smania N. Does robotic gait training improve balance in Parkinson’s disease? A randomized controlled trial. Parkinsonism Relat Disord. 2012;18(8):990–993. doi: 10.1016/j.parkreldis.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 54.da Cunha Jr IT, Lim PA, Qureshy H, Henson H, Monga T, Protas EJ. Gait outcomes after acute stroke rehabilitation with supported treadmill ambulation training: a randomized controlled pilot study. Arch Phys Med Rehabilit. 2002;83(9):1258–1265. doi: 10.1053/apmr.2002.34267. [DOI] [PubMed] [Google Scholar]
- 55.Laufer Y, Dickstein R, Chefez Y, Marcovitz E. The effect of treadmill training on the ambulation of stroke survivors in the early stages of rehabilitation: a randomized study. J Rehabil Res Dev. 2001;38(1):69–78. [PubMed] [Google Scholar]
- 56.Carda S, Invernizzi M, Baricich A, Comi C, Croquelois A, Cisari C. Robotic gait training is not superior to conventional treadmill training in Parkinson disease: a single-blind randomized controlled trial. Neurorehabilit Neural Repair. 2012;26(9):1027–1034. doi: 10.1177/1545968312446753. [DOI] [PubMed] [Google Scholar]
- 57.Banala SK, Kim SH, Agrawal SK, Scholz JP. Robot assisted gait training with active leg exoskeleton (ALEX) IEEE Trans Neural Syst Rehabilit Eng. 2008;17(1):2–8. doi: 10.1109/TNSRE.2008.2008280. [DOI] [PubMed] [Google Scholar]
- 58.Ho N, Tong K, Hu X, Fung K, Wei X, Rong W, Susanto E. An EMG-driven exoskeleton hand robotic training device on chronic stroke subjects: task training system for stroke rehabilitation. In: 2011 IEEE international conference on rehabilitation robotics. IEEE, 2011:1–5. [DOI] [PubMed]
- 59.McGibbon CA, Sexton A, Jayaraman A, Deems-Dluhy S, Gryfe P, Novak A, Dutta T, Fabara E, Adans-Dester C, Bonato P. Evaluation of the Keeogo exoskeleton for assisting ambulatory activities in people with multiple sclerosis: an open-label, randomized, cross-over trial. J Neuroeng Rehabilit. 2018;15:1–14. doi: 10.1186/s12984-018-0468-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boes MK, Bollaert RE, Kesler RM, Learmonth YC, Islam M, Petrucci MN, Motl RW, Hsiao-Wecksler ET. Six-minute walk test performance in persons with multiple sclerosis while using passive or powered ankle-foot orthoses. Arch Phys Med Rehabilit. 2018;99(3):484–490. doi: 10.1016/j.apmr.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 61.Sutliff MH, Naft JM, Stough DK, Lee JC, Arrigain SS, Bethoux FA. Efficacy and safety of a hip flexion assist orthosis in ambulatory multiple sclerosis patients. Arch Phys Med Rehabilit. 2008;89(8):1611–1617. doi: 10.1016/j.apmr.2007.11.065. [DOI] [PubMed] [Google Scholar]
- 62.Ates S, Haarman CJ, Stienen AH. SCRIPT passive orthosis: design of interactive hand and wrist exoskeleton for rehabilitation at home after stroke. Auton Robots. 2017;41:711–723. [Google Scholar]
- 63.Alam M, Choudhury IA, Mamat AB. Mechanism and design analysis of articulated ankle foot orthoses for drop-foot. Sci World J. 2014 doi: 10.1155/2014/867869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stein J, Narendran K, McBean J, Krebs K, Hughes R. Electromyography-controlled exoskeletal upper-limb-powered orthosis for exercise training after stroke. Am J Phys Med Rehabilit. 2007;86(4):255–261. doi: 10.1097/PHM.0b013e3180383cc5. [DOI] [PubMed] [Google Scholar]
- 65.Nicolelis MA. Brain-machine interfaces to restore motor function and probe neural circuits. Nat Rev Neurosci. 2003;4(5):417–422. doi: 10.1038/nrn1105. [DOI] [PubMed] [Google Scholar]
- 66.Venkatakrishnan A, Francisco GE, Contreras-Vidal JL. Applications of brain-machine interface systems in stroke recovery and rehabilitation. Curr Phys Med Rehabilit Rep. 2014;2:93–105. doi: 10.1007/s40141-014-0051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ramos-Murguialday A, Broetz D, Rea M, Läer L, Yilmaz Ö, Brasil FL, Liberati G, Curado MR, Garcia-Cossio E, Vyziotis A, et al. Brain-machine interface in chronic stroke rehabilitation: a controlled study. Ann Neurol. 2013;74(1):100–108. doi: 10.1002/ana.23879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Soekadar SR, Birbaumer N, Slutzky MW, Cohen LG. Brain-machine interfaces in neurorehabilitation of stroke. Neurobiol Dis. 2015;83:172–179. doi: 10.1016/j.nbd.2014.11.025. [DOI] [PubMed] [Google Scholar]
- 69.Reinkensmeyer DJ, Burdet E, Casadio M, Krakauer JW, Kwakkel G, Lang CE, Swinnen SP, Ward NS, Schweighofer N. Computational neurorehabilitation: modeling plasticity and learning to predict recovery. J Neuroeng Rehabilit. 2016;13(1):1–25. doi: 10.1186/s12984-016-0148-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Billinger SA, Boyne P, Coughenour E, Dunning K, Mattlage A. Does aerobic exercise and the FITT principle fit into stroke recovery? Curr Neurol Neurosci Rep. 2015;15:1–8. doi: 10.1007/s11910-014-0519-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dunlap G, Fox L. A demonstration of behavioral support for young children with autism. J Posit Behav Interv. 1999;1(2):77–87. [Google Scholar]
- 72.Levin MF, Kleim JA, Wolf SL. What do motor “recovery" and "compensation" mean in patients following stroke? Neurorehabilit Neural Repair. 2009;23(4):313–319. doi: 10.1177/1545968308328727. [DOI] [PubMed] [Google Scholar]
- 73.Giddan JJ, Obee VL. Adults with autism: habilitation challenges and practices. J Rehabilit. 1996;62(1):72. [Google Scholar]
- 74.Bellani M, Fornasari L, Chittaro L, Brambilla P. Virtual reality in autism: state of the art. Epidemiol Psychiatr Sci. 2011;20(3):235–238. doi: 10.1017/s2045796011000448. [DOI] [PubMed] [Google Scholar]
- 75.Hawe RL, Scott SH, Dukelow SP. Taking proportional out of stroke recovery. Stroke. 2019;50(1):204–211. doi: 10.1161/STROKEAHA.118.023006. [DOI] [PubMed] [Google Scholar]
- 76.Scott SH, Lowrey CR, Brown IE, Dukelow SP. Assessment of neurological impairment and recovery using statistical models of neurologically healthy behavior. Neurorehabilit Neural Repair. 2022 doi: 10.1177/154596832211154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Olney SJ, Griffin MP, McBride ID. Multivariate examination of data from gait analysis of persons with stroke. Phys Ther. 1998;78(8):814–828. doi: 10.1093/ptj/78.8.814. [DOI] [PubMed] [Google Scholar]
- 78.Nieuwboer A, Weerdt W, Dom R, Lesaffre E. A frequency and correlation analysis of motor deficits in Parkinson patients. Disabil Rehabilit. 1998;20(4):142–150. doi: 10.3109/09638289809166074. [DOI] [PubMed] [Google Scholar]
- 79.Sanger TD. Human arm movements described by a low-dimensional superposition of principal components. J Neurosci. 2000;20(3):1066–1072. doi: 10.1523/JNEUROSCI.20-03-01066.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kordelaar J, van Wegen EEH, Nijland RH, Daffertshofer A, Kwakkel G. Understanding adaptive motor control of the paretic upper limb early poststroke: the EXPLICIT-stroke program. Neurorehabilit Neural Repair. 2013;27(9):854–863. doi: 10.1177/1545968313496327. [DOI] [PubMed] [Google Scholar]
- 81.Valero-Cuevas FJ, Klamroth-Marganska V, Winstein CJ, Riener R. Robot-assisted and conventional therapies produce distinct rehabilitative trends in stroke survivors. J Neuroeng Rehabilit. 2016;13:1–10. doi: 10.1186/s12984-016-0199-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gong L, Liu Y, Yi L, Fang J, Yang Y, Wei K. Abnormal gait patterns in autism spectrum disorder and their correlations with social impairments. Autism Res. 2020;13(7):1215–1226. doi: 10.1002/aur.2302. [DOI] [PubMed] [Google Scholar]
- 83.Vandekerckhove I, Verreydt I, Van Grinderbeek M, De Beukelaer N, Van den Hauwe M, Van Campenhout A, De Waele L, Goemans N, De Groote F, Desloovere K. Gait stage classification for children with Duchenne muscular dystrophy based on longitudinal follow-up of progressive gait pathology. Gait Posture. 2022;97:S239–S241. [Google Scholar]
- 84.Liew S-L, Schweighofer N, Cole JH, Zavaliangos-Petropulu A, Lo BP, Han LK, Hahn T, Schmaal L, Donnelly MR, Jeong JN, et al. Association of brain age, lesion volume, and functional outcome in patients with stroke. Neurology. 2023;100(20):e2103–e2113. doi: 10.1212/WNL.0000000000207219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mainali S, Darsie ME, Smetana KS. Machine learning in action: stroke diagnosis and outcome prediction. Front Neurol. 2021;12:734345. doi: 10.3389/fneur.2021.734345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sanchez N, Schweighofer N, Mulroy S, Roemmich RT, Kesar TM, Torres-Oviedo G, Fisher BE, Finley J, Winstein CJ. Multi-site identification and generalization of clusters of walking impairment in individuals with chronic stroke. bioRxiv, 2023:2023–05. [DOI] [PMC free article] [PubMed]
- 87.Lau H-Y, Tong K-Y, Zhu H. Support vector machine for classification of walking conditions of persons after stroke with dropped foot. Hum Mov Sci. 2009;28(4):504–514. doi: 10.1016/j.humov.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 88.Mulroy S, Gronley J, Weiss W, Newsam C, Perry J. Use of cluster analysis for gait pattern classification of patients in the early and late recovery phases following stroke. Gait Posture. 2003;18(1):114–125. doi: 10.1016/s0966-6362(02)00165-0. [DOI] [PubMed] [Google Scholar]
- 89.Clark DJ, Ting LH, Zajac FE, Neptune RR, Kautz SA. Merging of healthy motor modules predicts reduced locomotor performance and muscle coordination complexity post-stroke. J Neurophysiol. 2010;103(2):844–857. doi: 10.1152/jn.00825.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Weng C, Shah NH, Hripcsak G. Deep phenotyping: embracing complexity and temporality—towards scalability, portability, and interoperability. J Biomed Inform. 2020;105:103433. doi: 10.1016/j.jbi.2020.103433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Khodatars M, Shoeibi A, Sadeghi D, Ghaasemi N, Jafari M, Moridian P, Khadem A, Alizadehsani R, Zare A, Kong Y, et al. Deep learning for neuroimaging-based diagnosis and rehabilitation of autism spectrum disorder: a review. Comput Biol Med. 2021;139:104949. doi: 10.1016/j.compbiomed.2021.104949. [DOI] [PubMed] [Google Scholar]
- 92.Liao Y, Vakanski A, Xian M. A deep learning framework for assessing physical rehabilitation exercises. IEEE Trans Neural Syst Rehabilit Eng. 2020;28(2):468–477. doi: 10.1109/TNSRE.2020.2966249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lin P-J, Zhai X, Li W, Li T, Cheng D, Li C, Pan Y, Ji L. A transferable deep learning prognosis model for predicting stroke patients’ recovery in different rehabilitation trainings. IEEE J Biomed Health Inform. 2022;26(12):6003–6011. doi: 10.1109/JBHI.2022.3205436. [DOI] [PubMed] [Google Scholar]
- 94.Campagnini S, Arienti C, Patrini M, Liuzzi P, Mannini A, Carrozza MC. Machine learning methods for functional recovery prediction and prognosis in post-stroke rehabilitation: a systematic review. J NeuroEng Rehabilit. 2022;19(1):1–22. doi: 10.1186/s12984-022-01032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chauhan S, Vig L, De Grazia M De Filippo, Corbetta M, Ahmad S, Zorzi M. A comparison of shallow and deep learning methods for predicting cognitive performance of stroke patients from MRI lesion images. Front Neuroinform. 2019;13:53. doi: 10.3389/fninf.2019.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Murphy SA. Optimal dynamic treatment regimes. J R Stat Soc Ser B: Stat Methodol. 2003;65(2):331–355. [Google Scholar]
- 97.Wilson RC, Collins AG. Ten simple rules for the computational modeling of behavioral data. Elife. 2019;8:e49547. doi: 10.7554/eLife.49547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cashaback JG, McGregor HR, Mohatarem A, Gribble PL. Dissociating error-based and reinforcement-based loss functions during sensorimotor learning. PLoS Comput Biol. 2017;13(7):e1005623. doi: 10.1371/journal.pcbi.1005623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Roth AM, Calalo JA, Lokesh R, Sullivan SR, Grill S, Jeka JJ, van der Kooij K, Carter MJ, Cashaback JG. Reinforcement-based processes actively regulate motor exploration along redundant solution manifolds. bioRxiv, 2023:2023–02. [DOI] [PMC free article] [PubMed]
- 100.Price M, Huber ME, Hoogkamer W. Minimum effort simulations of split-belt treadmill walking exploit asymmetry to reduce metabolic energy expenditure. J Neurophysiol. 2023;129(4):900–913. doi: 10.1152/jn.00343.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Abdikadirova B, Lee J, Hogan N, Huber ME. Muscle-reflex model of human locomotion entrains to mechanical perturbations. In: 2021 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS). IEEE 2021:7544–9.
- 102.Krakauer JW. Motor learning: its relevance to stroke recovery and neurorehabilitation. Curr Opin Neurol. 2006;19(1):84–90. doi: 10.1097/01.wco.0000200544.29915.cc. [DOI] [PubMed] [Google Scholar]
- 103.Smith MA, Ghazizadeh A, Shadmehr R. Interacting adaptive processes with different timescales underlie short-term motor learning. PLoS Biol. 2006;4(6):e179. doi: 10.1371/journal.pbio.0040179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Therrien AS, Wolpert DM, Bastian AJ. Effective reinforcement learning following cerebellar damage requires a balance between exploration and motor noise. Brain. 2016;139(1):101–114. doi: 10.1093/brain/awv329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lee J-Y, Schweighofer N. Dual adaptation supports a parallel architecture of motor memory. J Neurosci. 2009;29(33):10396–10404. doi: 10.1523/JNEUROSCI.1294-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Cashaback JG, Lao CK, Palidis DJ, Coltman SK, McGregor HR, Gribble PL. The gradient of the reinforcement landscape influences sensorimotor learning. PLoS Comput Biol. 2019;15(3):e1006839. doi: 10.1371/journal.pcbi.1006839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Criscimagna-Hemminger SE, Bastian AJ, Shadmehr R. Size of error affects cerebellar contributions to motor learning. J Neurophysiol. 2010;103(4):2275–2284. doi: 10.1152/jn.00822.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tseng Y-W, Diedrichsen J, Krakauer JW, Shadmehr R, Bastian AJ. Sensory prediction errors drive cerebellum-dependent adaptation of reaching. J Neurophysiol. 2007;98(1):54–62. doi: 10.1152/jn.00266.2007. [DOI] [PubMed] [Google Scholar]
- 109.Morton SM, Bastian AJ. Cerebellar contributions to locomotor adaptations during splitbelt treadmill walking. J Neurosci. 2006;26(36):9107–9116. doi: 10.1523/JNEUROSCI.2622-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pekny SE, Izawa J, Shadmehr R. Reward-dependent modulation of movement variability. J Neurosci. 2015;35(9):4015–4024. doi: 10.1523/JNEUROSCI.3244-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Frank MJ, Seeberger LC, O’reilly RC. By carrot or by stick: cognitive reinforcement learning in parkinsonism. Science. 2004;306(5703):1940–1943. doi: 10.1126/science.1102941. [DOI] [PubMed] [Google Scholar]
- 112.Wei Y, Bajaj P, Scheidt R, Patton J. Visual error augmentation for enhancing motor learning and rehabilitative relearning. In: 9th International Conference on Rehabilitation Robotics, 2005. ICORR 2005. IEEE, 2005:505–10.
- 113.Patton JL, Wei YJ, Bajaj P, Scheidt RA. Visuomotor learning enhanced by augmenting instantaneous trajectory error feedback during reaching. PLoS ONE. 2013;8(1):e46466. doi: 10.1371/journal.pone.0046466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Abdollahi F, Case Lazarro ED, Listenberger M, Kenyon RV, Kovic M, Bogey RA, Hedeker D, Jovanovic BD, Patton JL. Error augmentation enhancing arm recovery in individuals with chronic stroke: a randomized crossover design. Neurorehabilit Neural Repair. 2014;28(2):120–128. doi: 10.1177/1545968313498649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Finley JM, Bastian AJ, Gottschall JS. Learning to be economical: the energy cost of walking tracks motor adaptation. J Physiol. 2013;591(4):1081–1095. doi: 10.1113/jphysiol.2012.245506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Johnson RT, Bianco NA, Finley JM. Patterns of asymmetry and energy cost generated from predictive simulations of hemiparetic gait. PLoS Comput Biol. 2022;18(9):e1010466. doi: 10.1371/journal.pcbi.1010466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Finley JM, Bastian AJ. Associations between foot placement asymmetries and metabolic cost of transport in hemiparetic gait. Neurorehabilit Neural Repair. 2017;31(2):168–177. doi: 10.1177/1545968316675428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Shadmehr R, Mussa-Ivaldi FA. Adaptive representation of dynamics during learning of a motor task. J Neurosci. 1994;14(5):3208–3224. doi: 10.1523/JNEUROSCI.14-05-03208.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Smith MA, Shadmehr R. Intact ability to learn internal models of arm dynamics in Huntington’s disease but not cerebellar degeneration. J Neurophysiol. 2005;93(5):2809–2821. doi: 10.1152/jn.00943.2004. [DOI] [PubMed] [Google Scholar]
- 120.Schlerf JE, Xu J, Klemfuss NM, Griffiths TL, Ivry RB. Individuals with cerebellar degeneration show similar adaptation deficits with large and small visuomotor errors. J Neurophysiol. 2013;109(4):1164–1173. doi: 10.1152/jn.00654.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Herzfeld DJ, Kojima Y, Soetedjo R, Shadmehr R. Encoding of action by the Purkinje cells of the cerebellum. Nature. 2015;526(7573):439–442. doi: 10.1038/nature15693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Brooks JX, Carriot J, Cullen KE. Learning to expect the unexpected: rapid updating in primate cerebellum during voluntary self-motion. Nat Neurosci. 2015;18(9):1310–1317. doi: 10.1038/nn.4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Taylor JA, Klemfuss NM, Ivry RB. An explicit strategy prevails when the cerebellum fails to compute movement errors. Cerebellum. 2010;9:580–586. doi: 10.1007/s12311-010-0201-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.McDougle SD, Bond KM, Taylor JA. Explicit and implicit processes constitute the fast and slow processes of sensorimotor learning. J Neurosci. 2015;35(26):9568–9579. doi: 10.1523/JNEUROSCI.5061-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bond KM, Taylor JA. Flexible explicit but rigid implicit learning in a visuomotor adaptation task. J Neurophysiol. 2015;113(10):3836–3849. doi: 10.1152/jn.00009.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sokolov AA, Miall RC, Ivry RB. The cerebellum: adaptive prediction for movement and cognition. Trends Cogn Sci. 2017;21(5):313–332. doi: 10.1016/j.tics.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Miyamoto YR, Wang S, Smith MA. Implicit adaptation compensates for erratic explicit strategy in human motor learning. Nat Neurosci. 2020;23(3):443–455. doi: 10.1038/s41593-020-0600-3. [DOI] [PubMed] [Google Scholar]
- 128.Wei Y, Patton J, Bajaj P, Scheidt R. A real-time haptic/graphic demonstration of how error augmentation can enhance learning. In: Proceedings of the 2005 IEEE international conference on robotics and automation. IEEE, 2005:4406–11.
- 129.Sharp I, Huang F, Patton J. Visual error augmentation enhances learning in three dimensions. J Neuroeng Rehabilit. 2011;8:1–6. doi: 10.1186/1743-0003-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Izawa J, Shadmehr R. Learning from sensory and reward prediction errors during motor adaptation. PLoS Comput Biol. 2011;7(3):e1002012. doi: 10.1371/journal.pcbi.1002012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nikooyan AA, Ahmed AA. Reward feedback accelerates motor learning. J Neurophysiol. 2015;113(2):633–646. doi: 10.1152/jn.00032.2014. [DOI] [PubMed] [Google Scholar]
- 132.Holland P, Codol O, Galea JM. Contribution of explicit processes to reinforcement-based motor learning. J Neurophysiol. 2018;119(6):2241–2255. doi: 10.1152/jn.00901.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.McDougle SD, Boggess MJ, Crossley MJ, Parvin D, Ivry RB, Taylor JA. Credit assignment in movement-dependent reinforcement learning. Proc Natl Acad Sci. 2016;113(24):6797–6802. doi: 10.1073/pnas.1523669113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Palidis DJ, Cashaback JG, Gribble PL. Neural signatures of reward and sensory error feedback processing in motor learning. J Neurophysiol. 2019;121(4):1561–1574. doi: 10.1152/jn.00792.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Schultz W, Dayan P, Montague PR. A neural substrate of prediction and reward. Science. 1997;275(5306):1593–1599. doi: 10.1126/science.275.5306.1593. [DOI] [PubMed] [Google Scholar]
- 136.Schultz W. Dopamine reward prediction-error signalling: a two-component response. Nat Rev Neurosci. 2016;17(3):183–195. doi: 10.1038/nrn.2015.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wolpert DM, Diedrichsen J, Flanagan JR. Principles of sensorimotor learning. Nat Rev Neurosci. 2011;12(12):739–751. doi: 10.1038/nrn3112. [DOI] [PubMed] [Google Scholar]
- 138.Diedrichsen J, White O, Newman D, Lally N. Use-dependent and error-based learning of motor behaviors. J Neurosci. 2010;30(15):5159–5166. doi: 10.1523/JNEUROSCI.5406-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Vaswani PA, Shmuelof L, Haith AM, Delnicki RJ, Huang VS, Mazzoni P, Shadmehr R, Krakauer JW. Persistent residual errors in motor adaptation tasks: reversion to baseline and exploratory escape. J Neurosci. 2015;35(17):6969–6977. doi: 10.1523/JNEUROSCI.2656-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Therrien AS, Wong AL. Mechanisms of human motor learning do not function independently. Front Hum Neurosci. 2022;15:785992. doi: 10.3389/fnhum.2021.785992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Yang CS, Cowan NJ, Haith AM. De novo learning versus adaptation of continuous control in a manual tracking task. elife. 2021;10:e62578. doi: 10.7554/eLife.62578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yang C, Cowan N, Haith A. Control becomes habitual early on when learning a novel motor skill. J Neurophysiol. 2022;128(5):1278–1291. doi: 10.1152/jn.00273.2022. [DOI] [PubMed] [Google Scholar]
- 143.Haith AM, Yang CS, Pakpoor J, Kita K. De novo motor learning of a bimanual control task over multiple days of practice. J Neurophysiol. 2022;128(4):982–993. doi: 10.1152/jn.00474.2021. [DOI] [PubMed] [Google Scholar]
- 144.Greenwell D, Vanderkolff S, Feigh J. Understanding de novo learning for brain-machine interfaces. J Neurophysiol. 2023;129(4):749–750. doi: 10.1152/jn.00496.2022. [DOI] [PubMed] [Google Scholar]
- 145.Krakauer JW, Hadjiosif AM, Xu J, Wong AL, Haith AM. Motor learning. Compr Physiol. 2019;9(2):613–663. doi: 10.1002/cphy.c170043. [DOI] [PubMed] [Google Scholar]
- 146.Orsborn AL, Pesaran B. Parsing learning in networks using brain-machine interfaces. Curr Opin Neurobiol. 2017;46:76–83. doi: 10.1016/j.conb.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gallego JA, Makin TR, McDougle SD. Going beyond primary motor cortex to improve brain-computer interfaces. Trends Neurosci. 2022 doi: 10.1016/j.tins.2021.12.006. [DOI] [PubMed] [Google Scholar]
- 148.Dadarlat MC, Canfield RA, Orsborn AL. Neural plasticity in sensorimotor brain-machine interfaces. Ann Rev Biomed Eng. 2022;25:51–76. doi: 10.1146/annurev-bioeng-110220-110833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.McRuer DT, Graham D, Krendel ES. Manual control of single-loop systems: Part I. J Franklin Inst. 1967;283(1):1–29. [Google Scholar]
- 150.Collins SH, Wiggin MB, Sawicki GS. Reducing the energy cost of human walking using an unpowered exoskeleton. Nature. 2015;522(7555):212–215. doi: 10.1038/nature14288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ding Y, Kim M, Kuindersma S, Walsh CJ. Human-in-the-loop optimization of hip assistance with a soft exosuit during walking. Sci Robot. 2018;3(15):eaar5438. doi: 10.1126/scirobotics.aar5438. [DOI] [PubMed] [Google Scholar]
- 152.De Santis D. A framework for optimizing co-adaptation in body-machine interfaces. Front Neurorobot. 2021;15:662181. doi: 10.3389/fnbot.2021.662181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Madduri MM, Burden SA, Orsborn AL. A game-theoretic model for co-adaptive brain-machine interfaces. In: 2021 10th International IEEE/EMBS Conference on Neural Engineering (NER). IEEE, 2021:327–30.
- 154.Madduri M, Burden S, Orsborn A. Biosignal-based co-adaptive user-machine interfaces for motor control. Curr Opin Biomed Eng. 2023 doi: 10.1016/j.cobme.2023.100462. [DOI] [Google Scholar]
- 155.Will B, Dalrymple-Alford J, Wolff M, Cassel J-C. The concept of brain plasticity—Paillard’s systemic analysis and emphasis on structure and function (followed by the translation of a seminal paper by Paillard on plasticity) Behav Brain Res. 2008;192(1):2–7. doi: 10.1016/j.bbr.2007.11.030. [DOI] [PubMed] [Google Scholar]
- 156.Dromerick AW, Geed S, Barth J, Brady K, Giannetti ML, Mitchell A, Edwardson MA, Tan MT, Zhou Y, Newport EL, et al. Critical Period After Stroke Study (CPASS): A phase II clinical trial testing an optimal time for motor recovery after stroke in humans. Proc Natl Acad Sci. 2021;118(39):e2026676118. doi: 10.1073/pnas.2026676118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Nudo RJ, Milliken GW. Reorganization of movement representations in primary motor cortex following focal ischemic infarcts in adult squirrel monkeys. J Neurophysiol. 1996;75(5):2144–2149. doi: 10.1152/jn.1996.75.5.2144. [DOI] [PubMed] [Google Scholar]
- 158.Ganguly K, Khanna P, Morecraft RJ, Lin DJ. Modulation of neural co-firing to enhance network transmission and improve motor function after stroke. Neuron. 2022;110(15):2363–2385. doi: 10.1016/j.neuron.2022.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Raffin E, Hummel FC. Restoring motor functions after stroke: multiple approaches and opportunities. Neuroscientist. 2018;24(4):400–416. doi: 10.1177/1073858417737486. [DOI] [PubMed] [Google Scholar]
- 160.Raffin E, Siebner HR. Transcranial brain stimulation to promote functional recovery after stroke. Curr Opin Neurol. 2014;27(1):54. doi: 10.1097/WCO.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Adeyemo BO, Simis M, Macea DD, Fregni F. Systematic review of parameters of stimulation, clinical trial design characteristics, and motor outcomes in non-invasive brain stimulation in stroke. Front Psychiatr. 2012;3:88. doi: 10.3389/fpsyt.2012.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.He Y, Li K, Chen Q, Yin J, Bai D. Repetitive transcranial magnetic stimulation on motor recovery for patients with stroke: a PRISMA compliant systematic review and meta-analysis. Am J Phys Med Rehabilit. 2020;99(2):99–108. doi: 10.1097/PHM.0000000000001277. [DOI] [PubMed] [Google Scholar]
- 163.Harvey RL, Edwards D, Dunning K, Fregni F, Stein J, Laine J, Rogers LM, Vox F, Durand-Sanchez A, Bockbrader M, et al. Randomized sham-controlled trial of navigated repetitive transcranial magnetic stimulation for motor recovery in stroke: the NICHE trial. Stroke. 2018;49(9):2138–2146. doi: 10.1161/STROKEAHA.117.020607. [DOI] [PubMed] [Google Scholar]
- 164.Xiang H, Sun J, Tang X, Zeng K, Wu X. The effect and optimal parameters of repetitive transcranial magnetic stimulation on motor recovery in stroke patients: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabilit. 2019;33(5):847–864. doi: 10.1177/0269215519829897. [DOI] [PubMed] [Google Scholar]
- 165.Putrino D, Krakauer JW. Neurotechnology’s Prospects for Bringing About Meaningful Reductions in Neurological Impairment. Neurorehabilit Neural Repair. 2023;37(6):356–366. doi: 10.1177/15459683221137341. [DOI] [PubMed] [Google Scholar]
- 166.Hochberg LR, Donoghue JP. Sensors for brain-computer interfaces. IEEE Eng Med Biol Mag. 2006;25(5):32–38. doi: 10.1109/memb.2006.1705745. [DOI] [PubMed] [Google Scholar]
- 167.Hochberg LR, Bacher D, Jarosiewicz B, Masse NY, Simeral JD, Vogel J, Haddadin S, Liu J, Cash SS, Van Der Smagt P, et al. Reach and grasp by people with tetraplegia using a neurally controlled robotic arm. Nature. 2012;485(7398):372–375. doi: 10.1038/nature11076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Moses DA, Metzger SL, Liu JR, Anumanchipalli GK, Makin JG, Sun PF, Chartier J, Dougherty ME, Liu PM, Abrams GM, et al. Neuroprosthesis for decoding speech in a paralyzed person with anarthria. New Engl J Med. 2021;385(3):217–227. doi: 10.1056/NEJMoa2027540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Willett FR, Avansino DT, Hochberg LR, Henderson JM, Shenoy KV. High-performance brain-to-text communication via handwriting. Nature. 2021;593(7858):249–254. doi: 10.1038/s41586-021-03506-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ganguly K, Carmena JM. Emergence of a stable cortical map for neuroprosthetic control. PLoS Biol. 2009;7(7):e1000153. doi: 10.1371/journal.pbio.1000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Balasubramanian K, Vaidya M, Southerland J, Badreldin I, Eleryan A, Takahashi K, Qian K, Slutzky MW, Fagg AH, Oweiss K, et al. Changes in cortical network connectivity with long-term brain-machine interface exposure after chronic amputation. Nat Commun. 2017;8(1):1796. doi: 10.1038/s41467-017-01909-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Wiesel TN, Hubel DH. Single-cell responses in striate cortex of kittens deprived of vision in one eye. J Neurophysiol. 1963;26(6):1003–1017. doi: 10.1152/jn.1963.26.6.1003. [DOI] [PubMed] [Google Scholar]
- 173.Hubel DH, Wiesel TN. Receptive fields of cells in striate cortex of very young, visually inexperienced kittens. J Neurophysiol. 1963;26(6):994–1002. doi: 10.1152/jn.1963.26.6.994. [DOI] [PubMed] [Google Scholar]
- 174.Wiesel TN, Hubel DH. Effects of visual deprivation on morphology and physiology of cells in the cat’s lateral geniculate body. J Neurophysiol. 1963;26(6):978–993. doi: 10.1152/jn.1963.26.6.978. [DOI] [PubMed] [Google Scholar]
- 175.Brown RE, Milner PM. The legacy of Donald O. Hebb: more than the Hebb synapse. Nat Rev Neurosci. 2003;4(12):1013–1019. doi: 10.1038/nrn1257. [DOI] [PubMed] [Google Scholar]
- 176.Dan Y, Poo M-M. Spike timing-dependent plasticity: from synapse to perception. Physiol Rev. 2006;86(3):1033–1048. doi: 10.1152/physrev.00030.2005. [DOI] [PubMed] [Google Scholar]
- 177.Turrigiano GG. The dialectic of Hebb and homeostasis. Philos Trans R Soc B: Biol Sc. 2017;372(1715):20160258. doi: 10.1098/rstb.2016.0258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Nudo RJ, Wise BM, SiFuentes F, Milliken GW. Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science. 1996;272(5269):1791–1794. doi: 10.1126/science.272.5269.1791. [DOI] [PubMed] [Google Scholar]
- 179.Grefkes C, Fink GR. Connectivity-based approaches in stroke and recovery of function. Lancet Neurol. 2014;13(2):206–216. doi: 10.1016/S1474-4422(13)70264-3. [DOI] [PubMed] [Google Scholar]
- 180.Cramer SC, Nelles G, Benson RR, Kaplan JD, Parker RA, Kwong KK, Kennedy DN, Finklestein SP, Rosen BR. A functional MRI study of subjects recovered from hemiparetic stroke. Stroke. 1997;28(12):2518–2527. doi: 10.1161/01.str.28.12.2518. [DOI] [PubMed] [Google Scholar]
- 181.Münte TF, Altenmüller E, Jäncke L. The musician’s brain as a model of neuroplasticity. Nat Rev Neurosci. 2002;3(6):473–478. doi: 10.1038/nrn843. [DOI] [PubMed] [Google Scholar]
- 182.Hoenig K, Müller C, Herrnberger B, Sim E-J, Spitzer M, Ehret G, Kiefer M. Neuroplasticity of semantic representations for musical instruments in professional musicians. NeuroImage. 2011;56(3):1714–1725. doi: 10.1016/j.neuroimage.2011.02.065. [DOI] [PubMed] [Google Scholar]
- 183.Bianchi F, Hjortkjær J, Santurette S, Zatorre RJ, Siebner HR, Dau T. Subcortical and cortical correlates of pitch discrimination: evidence for two levels of neuroplasticity in musicians. Neuroimage. 2017;163:398–412. doi: 10.1016/j.neuroimage.2017.07.057. [DOI] [PubMed] [Google Scholar]
- 184.Jäncke L. The plastic human brain. Restor Neurol Neurosci. 2009;27(5):521–538. doi: 10.3233/RNN-2009-0519. [DOI] [PubMed] [Google Scholar]
- 185.Elbert T, Rockstroh B. Reorganization of human cerebral cortex: the range of changes following use and injury. Neuroscientist. 2004;10(2):129–141. doi: 10.1177/1073858403262111. [DOI] [PubMed] [Google Scholar]
- 186.Bernhardt J, Hayward KS, Kwakkel G, Ward NS, Wolf SL, Borschmann K, Krakauer JW, Boyd LA, Carmichael ST, Corbett D, et al. Agreed definitions and a shared vision for new standards in stroke recovery research: the stroke recovery and rehabilitation roundtable taskforce. Int J Stroke. 2017;12(5):444–450. doi: 10.1177/1747493017711816. [DOI] [PubMed] [Google Scholar]
- 187.Leech KA, Roemmich RT, Gordon J, Reisman DS, Cherry-Allen KM. Updates in motor learning: implications for physical therapist practice and education. Phys Ther. 2022;102(1):pzab250. doi: 10.1093/ptj/pzab250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Yuan K, Chen C, Wang X, Chu WC-W, Tong RK-Y. BCI training effects on chronic stroke correlate with functional reorganization in motor-related regions: A concurrent EEG and fMRI study. Brain Sci. 2021;11(1):56. doi: 10.3390/brainsci11010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Orsborn AL, Moorman HG, Overduin SA, Shanechi MM, Dimitrov DF, Carmena JM. Closed-loop decoder adaptation shapes neural plasticity for skillful neuroprosthetic control. Neuron. 2014;82(6):1380–1393. doi: 10.1016/j.neuron.2014.04.048. [DOI] [PubMed] [Google Scholar]
- 190.Seth A, Hicks JL, Uchida TK, Habib A, Dembia CL, Dunne JJ, Ong CF, DeMers MS, Rajagopal A, Millard M, Hamner SR, Arnold EM, Yong JR, Lakshmikanth SK, Sherman MA, Ku JP, Delp SL. OpenSim: simulating musculoskeletal dynamics and neuromuscular control to study human and animal movement. PLoS Comput Biol. 2018;14(7):e1006223. doi: 10.1371/journal.pcbi.1006223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.De Groote F, Falisse A. Perspective on musculoskeletal modelling and predictive simulations of human movement to assess the neuromechanics of gait. Proc Biol Sci. 2021;288(1946):20202432. doi: 10.1098/rspb.2020.2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Song S, Kidziński Ł, Peng XB, Ong C, Hicks J, Levine S, Atkeson CG, Delp SL. Deep reinforcement learning for modeling human locomotion control in neuromechanical simulation. J Neuroeng Rehabil. 2021;18(1):126. doi: 10.1186/s12984-021-00919-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Song S, Geyer H. Predictive neuromechanical simulations indicate why walking performance declines with ageing. J Physiol. 2018;596(7):1199–1210. doi: 10.1113/JP275166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ong CF, Geijtenbeek T, Hicks JL, Delp SL. Predicting gait adaptations due to ankle plantarflexor muscle weakness and contracture using physics-based musculoskeletal simulations. PLoS Comput Biol. 2019;15(10):e1006993. doi: 10.1371/journal.pcbi.1006993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lu TW, O’Connor JJ. Bone position estimation from skin marker co-ordinates using global optimisation with joint constraints. J Biomech. 1999;32(2):129–134. doi: 10.1016/s0021-9290(98)00158-4. [DOI] [PubMed] [Google Scholar]
- 196.Thelen DG, Anderson FC. Using computed muscle control to generate forward dynamic simulations of human walking from experimental data. J Biomech. 2006;39(6):1107–1115. doi: 10.1016/j.jbiomech.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 197.Tanis D, Calalo JA, Cashaback JG, Kurtzer IL. Accuracy and effort costs together lead to temporal asynchrony of multiple motor commands. J Neurophysiol. 2023;129(1):1–6. doi: 10.1152/jn.00435.2022. [DOI] [PubMed] [Google Scholar]
- 198.Ting LH, McKay JL. Neuromechanics of muscle synergies for posture and movement. Curr Opin Neurobiol. 2007;17(6):622–628. doi: 10.1016/j.conb.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Allen JL, Neptune RR. Three-dimensional modular control of human walking. J Biomech. 2012;45(12):2157–2163. doi: 10.1016/j.jbiomech.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Koelewijn AD, Heinrich D, van den Bogert AJ. Metabolic cost calculations of gait using musculoskeletal energy models, a comparison study. PLoS ONE. 2019;14(9):e0222037. doi: 10.1371/journal.pone.0222037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Neptune RR, Kautz SA. Knee joint loading in forward versus backward pedaling: implications for rehabilitation strategies. Clin Biomech. 2000;15(7):528–535. doi: 10.1016/s0268-0033(00)00005-x. [DOI] [PubMed] [Google Scholar]
- 202.Uhlrich SD, Falisse A, Kidziński Ł, Muccini J, Ko M, Chaudhari AS, Hicks JL, Delp SL. OpenCap: 3D human movement dynamics from smartphone videos. PLoS Comput Biol. 2022 doi: 10.1371/journal.pcbi.1011462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Delp SL, Loan JP, Hoy MG, Zajac FE, Topp EL, Rosen JM. An interactive graphics-based model of the lower extremity to study orthopaedic surgical procedures. IEEE Trans Biomed Eng. 1990;37(8):757–767. doi: 10.1109/10.102791. [DOI] [PubMed] [Google Scholar]
- 204.Mansouri M, Clark AE, Seth A, Reinbolt JA. Rectus femoris transfer surgery affects balance recovery in children with cerebral palsy: a computer simulation study. Gait Posture. 2016;43:24–30. doi: 10.1016/j.gaitpost.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 205.Ferrati F, Bortoletto R, Pagello E. Virtual modelling of a real exoskeleton constrained to a human musculoskeletal model. In: Lepora NF, Mura A, Krapp HG, Verschure PFMJ, Prescott TJ, editors. Biomimetic and biohybrid systems. Berlin Heidelberg: Springer; 2013. pp. 96–107. [Google Scholar]
- 206.Price MA, Beckerle P, Sup FC. Design optimization in lower limb prostheses: a review. IEEE Trans Neural Syst Rehabil Eng. 2019;27(8):1574–1588. doi: 10.1109/TNSRE.2019.2927094. [DOI] [PubMed] [Google Scholar]
- 207.Wang H, Caggiano V, Durandau G, Sartori M, Kumar V. MyoSim: fast and physiologically realistic MuJoCo models for musculoskeletal and exoskeletal studies. In: 2022 International Conference on Robotics and Automation (ICRA). ieeexplore.ieee.org, 2022:8104–11.
- 208.Crouch DL, Huang H. Lumped-parameter electromyogram-driven musculoskeletal hand model: a potential platform for real-time prosthesis control. J Biomech. 2016;49(16):3901–3907. doi: 10.1016/j.jbiomech.2016.10.035. [DOI] [PubMed] [Google Scholar]
- 209.Durandau G, Farina D, Asín-Prieto G, Dimbwadyo-Terrer I, Lerma-Lara S, Pons JL, Moreno JC, Sartori M. Voluntary control of wearable robotic exoskeletons by patients with paresis via neuromechanical modeling. J Neuroeng Rehabil. 2019;16(1):91. doi: 10.1186/s12984-019-0559-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Durandau G, Rampeltshammer WF, van der Kooij H, Sartori M. Neuromechanical model-based adaptive control of bilateral ankle exoskeletons: biological joint torque and electromyogram reduction across walking conditions. IEEE Trans Rob. 2022;38(3):1380–94. [Google Scholar]
- 211.Anderson FC, Pandy MG. Dynamic optimization of human walking. J Biomech Eng. 2001;123(5):381–390. doi: 10.1115/1.1392310. [DOI] [PubMed] [Google Scholar]
- 212.Chaudhari AM, Andriacchi TP. The mechanical consequences of dynamic frontal plane limb alignment for non-contact ACL injury. J Biomech. 2006;39(2):330–338. doi: 10.1016/j.jbiomech.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 213.DeMers MS, Hicks JL, Delp SL. Preparatory co-activation of the ankle muscles may prevent ankle inversion injuries. J Biomech. 2017;52:17–23. doi: 10.1016/j.jbiomech.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Fregly BJ, Besier TF, Lloyd DG, Delp SL, Banks SA, Pandy MG, D’Lima DD. Grand challenge competition to predict in vivo knee loads. J Orthop Res. 2012;30(4):503–513. doi: 10.1002/jor.22023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Holder J, Trinler U, Meurer A, Stief F. A systematic review of the associations between inverse dynamics and musculoskeletal modeling to investigate joint loading in a clinical environment. Front Bioeng Biotechnol. 2020;8:603907. doi: 10.3389/fbioe.2020.603907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Arnold AS, Liu MQ, Schwartz MH, Õunpuu S, Dias LS, Delp SL. Do the hamstrings operate at increased muscle-tendon lengths and velocities after surgical lengthening? J Biomech. 2006;39(8):1498–1506. doi: 10.1016/j.jbiomech.2005.03.026. [DOI] [PubMed] [Google Scholar]
- 217.Falisse A, Serrancolí G, Dembia CL, Gillis J, Jonkers I, De Groote F. Rapid predictive simulations with complex musculoskeletal models suggest that diverse healthy and pathological human gaits can emerge from similar control strategies. J R Soc Interface. 2019;16(157):20190402. doi: 10.1098/rsif.2019.0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Thatte N, Geyer H. Toward Balance Recovery With Leg Prostheses Using Neuromuscular Model Control. IEEE Trans Biomed Eng. 2016;63(5):904–913. doi: 10.1109/TBME.2015.2472533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Handford ML, Srinivasan M. Energy-optimal human walking with feedback-controlled robotic prostheses: a computational study. IEEE Trans Neural Syst Rehabil Eng. 2018;26(9):1773–1782. doi: 10.1109/TNSRE.2018.2858204. [DOI] [PubMed] [Google Scholar]
- 220.Grabke EP, Masani K, Andrysek J. Lower limb assistive device design optimization using musculoskeletal modeling: a review. J Med Device. 2019;13(4):040801. [Google Scholar]
- 221.Wu AR, Dzeladini F, Brug TJH, Tamburella F, Tagliamonte NL, van Asseldonk EHF, van der Kooij H, Ijspeert AJ. An Adaptive neuromuscular controller for assistive lower-limb exoskeletons: a preliminary study on subjects with spinal cord injury. Neurorobot Front. 2017;11:30. doi: 10.3389/fnbot.2017.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Shu T, Shallal C, Chun E, Shah A, Bu A, Levine D, Yeon SH, Carney M, Song H, Hsieh T-H, Herr HM. Modulation of prosthetic ankle plantarflexion through direct myoelectric control of a subject-optimized neuromuscular model. IEEE Robot Autom Lett. 2022;7(3):7620–7627. [Google Scholar]
- 223.Cashaback JG, Cluff T. Increase in joint stability at the expense of energy efficiency correlates with force variability during a fatiguing task. J Biomech. 2015;48(4):621–626. doi: 10.1016/j.jbiomech.2014.12.053. [DOI] [PubMed] [Google Scholar]
- 224.Perreault E, Kirsch R, Crago P. Multijoint dynamics and postural stability of the human arm. Exp Brain Res. 2004;157(4):507–517. doi: 10.1007/s00221-004-1864-7. [DOI] [PubMed] [Google Scholar]
- 225.Potvin JR, Fuglevand AJ. A motor unit-based model of muscle fatigue. PLoS Comput Biol. 2017;13(6):e1005581. doi: 10.1371/journal.pcbi.1005581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Davidson JB, Cashaback JG, Fischer SL. Exploring optimal objective function weightings to predict lifting postures under unfatigued and fatigued states. Hum Fact. 2022 doi: 10.1177/0018720822109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Geyer H, Herr H. A muscle-reflex model that encodes principles of legged mechanics produces human walking dynamics and muscle activities. IEEE Trans Neural Syst Rehabil Eng. 2010;18(3):263–273. doi: 10.1109/TNSRE.2010.2047592. [DOI] [PubMed] [Google Scholar]
- 228.Dzeladini F, van den Kieboom J, Ijspeert A. The contribution of a central pattern generator in a reflex-based neuromuscular model. Front Hum Neurosci. 2014;8:371. doi: 10.3389/fnhum.2014.00371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Song S, Geyer H. A neural circuitry that emphasizes spinal feedback generates diverse behaviours of human locomotion. J Physiol. 2015;593(16):3493–3511. doi: 10.1113/JP270228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Aoi S, Ohashi T, Bamba R, Fujiki S, Tamura D, Funato T, Senda K, Ivanenko Y, Tsuchiya K. Neuromusculoskeletal model that walks and runs across a speed range with a few motor control parameter changes based on the muscle synergy hypothesis. Sci Rep. 2019;9(1):369. doi: 10.1038/s41598-018-37460-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.McCrea DA, Rybak IA. Organization of mammalian locomotor rhythm and pattern generation. Brain Res Rev. 2008;57(1):134–146. doi: 10.1016/j.brainresrev.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Song S, Geyer H. Evaluation of a neuromechanical walking control model using disturbance experiments. Front Comput Neurosci. 2017;11:15. doi: 10.3389/fncom.2017.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Black FO, Wall C, III, Rockette HE, Jr, Kitch R. Normal subject postural sway during the Romberg test. Am J Otolaryngol. 1982;3(5):309–318. doi: 10.1016/s0196-0709(82)80002-1. [DOI] [PubMed] [Google Scholar]
- 234.Engel-Yeger B. Validating the adolescent/adult sensory profile and examining its ability to screen sensory processing difficulties among Israeli people. Br J Occup Ther. 2012;75(7):321–329. [Google Scholar]
- 235.Leddy AL, Crowner BE, Earhart GM. Utility of the Mini-BESTest, BESTest, and BESTest sections for balance assessments in individuals with Parkinson disease. J Neurol Phys Ther JNPT. 2011;35(2):90. doi: 10.1097/NPT.0b013e31821a620c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Ernst MO, Banks MS. Humans integrate visual and haptic information in a statistically optimal fashion. Nature. 2002;415(6870):429–433. doi: 10.1038/415429a. [DOI] [PubMed] [Google Scholar]
- 237.Crevecoeur F, Munoz DP, Scott SH. Dynamic multisensory integration: somatosensory speed trumps visual accuracy during feedback control. J Neurosci. 2016;36(33):8598–8611. doi: 10.1523/JNEUROSCI.0184-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Lokesh R, Sullivan SR, St. Germain L, Roth AM, Calalo JA, Buggeln J, Ngo T, Marchhart VR, Carter MJ, Cashaback JG. Visual accuracy dominates over haptic speed for state estimation of a partner during collaborative sensorimotor interactions. J Neurophysiol. 2023 doi: 10.1152/jn.00053.2023. [DOI] [PubMed] [Google Scholar]
- 239.Bair W-N, Kiemel T, Jeka JJ, Clark JE. Development of multisensory reweighting for posture control in children. Exp Brain Res. 2007;183(4):435–446. doi: 10.1007/s00221-007-1057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Jeka JJ, Allison LK, Kiemel T. The dynamics of visual reweighting in healthy and fall-prone older adults. J Mot Behav. 2010;42(4):197–208. doi: 10.1080/00222895.2010.481693. [DOI] [PubMed] [Google Scholar]
- 241.Fears NE, Sherrod GM, Templin TN, Bugnariu NL, Patterson RM, Miller HL. Community-based postural control assessment in autistic individuals indicates a similar but delayed trajectory compared to neurotypical individuals. Autism Res. 2023;16(3):543–557. doi: 10.1002/aur.2889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Bair W-N, Kiemel T, Jeka JJ, Clark JE. Development of multisensory reweighting is impaired for quiet stance control in children with developmental coordination disorder (DCD) PLoS ONE. 2012;7(7):e40932. doi: 10.1371/journal.pone.0040932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Lim YH, Partridge K, Girdler S, Morris SL. Standing postural control in individuals with autism spectrum disorder: systematic review and meta-analysis. J Autism Dev Disord. 2017;47(7):2238–2253. doi: 10.1007/s10803-017-3144-y. [DOI] [PubMed] [Google Scholar]
- 244.Noriega G. A neural model to study sensory abnormalities and multisensory effects in autism. IEEE Trans Neural Syst Rehabil Eng. 2015;23(2):199–209. doi: 10.1109/TNSRE.2014.2363775. [DOI] [PubMed] [Google Scholar]
- 245.Semrau JA, Herter TM, Scott SH, Dukelow SP. Robotic identification of kinesthetic deficits after stroke. Stroke. 2013;44(12):3414–3421. doi: 10.1161/STROKEAHA.113.002058. [DOI] [PubMed] [Google Scholar]
- 246.Semrau JA, Herter TM, Scott SH, Dukelow SP. Vision of the upper limb fails to compensate for kinesthetic impairments in subacute stroke. Cortex. 2018;109:245–59. doi: 10.1016/j.cortex.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 247.Zhang H, Santamaria V, Agrawal S. Applying force perturbations using a wearable robotic neck brace. In: 2020 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), 2020:4197–202.
- 248.Petros FE, Klenk ME, Agrawal SK. Changes in gait parameters due to visual and head oscillations in football players and non-athletes. IEEE Robot Autom Lett. 2022;7(3):7171–7176. [Google Scholar]
- 249.Crosse MJ, Foxe JJ, Tarrit K, Freedman EG, Molholm S. Resolution of impaired multisensory processing in autism and the cost of switching sensory modality. Commun Biol. 2022;5(1):601. doi: 10.1038/s42003-022-03519-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Cressman EK, Henriques DYP. Motor adaptation and proprioceptive recalibration. Prog Brain Res. 2011;191:91–99. doi: 10.1016/B978-0-444-53752-2.00011-4. [DOI] [PubMed] [Google Scholar]
- 251.Henriques DYP, Cressman EK. Visuomotor adaptation and proprioceptive recalibration. J Mot Behav. 2012;44(6):435–444. doi: 10.1080/00222895.2012.659232. [DOI] [PubMed] [Google Scholar]
- 252.Salomonczyk D, Cressman EK, Henriques DYP. Proprioceptive recalibration following prolonged training and increasing distortions in visuomotor adaptation. Neuropsychologia. 2011;49(11):3053–3062. doi: 10.1016/j.neuropsychologia.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 253.Ostry DJ, Darainy M, Mattar AA, Wong J, Gribble PL. Somatosensory plasticity and motor learning. J Neurosci. 2010;30(15):5384–5393. doi: 10.1523/JNEUROSCI.4571-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Tsay JS, Kim H, Haith AM, Ivry RB. Understanding implicit sensorimotor adaptation as a process of proprioceptive re-alignment. elife. 2022;11:e76639. doi: 10.7554/eLife.76639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.De Carli P, Patrizi M, Pepe L, Cavaniglia G, Riva D, D’Ottavi LR. Postural control and risk of falling in bipodalic and monopodalic stabilometric tests of healthy subjects before, after visuo-proprioceptive vestibulo-postural rehabilitation and at 3 months thereafter: role of the proprioceptive system. Acta Otorhinolaryngol Ital. 2010;30(4):182–189. [PMC free article] [PubMed] [Google Scholar]
- 256.Peterka M, Odorfer T, Schwab M, Volkmann J, Zeller D. LSVT-BIG therapy in Parkinson’s disease: physiological evidence for proprioceptive recalibration. BMC Neurol. 2020;20(1):276. doi: 10.1186/s12883-020-01858-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Wali M, Lee-Miller T, Babu R, Block HJ. Retention of visuo-proprioceptive recalibration in estimating hand position. Sci Rep. 2023;13(1):6097. doi: 10.1038/s41598-023-33290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Başkent D, Edwards B. Simulating listener errors in using genetic algorithms for perceptual optimization. J Acoust Soc Am. 2007;121(6):EL238–EL243. doi: 10.1121/1.2731017. [DOI] [PubMed] [Google Scholar]
- 259.Lineaweaver SK, Wakefield GH. Psychometric augmentation of an interactive genetic algorithm for optimizing cochlear implant programs. In: Proceedings of the 13th annual conference on genetic and evolutionary computation, 2011:1755–62.
- 260.Saadoun A, Schein A, Péan V, Legrand P, Aho Glélé LS, Bozorg Grayeli A. Frequency fitting optimization using evolutionary algorithm in cochlear implant users with bimodal binaural hearing. Brain Sci. 2022;12(2):253. doi: 10.3390/brainsci12020253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Svirsky MA, Capach NH, Neukam JD, Azadpour M, Sagi E, Hight AE, Glassman EK, Lavender A, Seward KP, Miller MK, et al. Valid acoustic models of cochlear implants: one size does not fit all. Otol Neurotol. 2021;42(10):S2–S10. doi: 10.1097/MAO.0000000000003373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Pasluosta C, Kiele P, Stieglitz T. Paradigms for restoration of somatosensory feedback via stimulation of the peripheral nervous system. Clin Neurophysiol. 2018;129(4):851–862. doi: 10.1016/j.clinph.2017.12.027. [DOI] [PubMed] [Google Scholar]
- 263.Saal HP, Bensmaia SJ. Biomimetic approaches to bionic touch through a peripheral nerve interface. Neuropsychologia. 2015;79:344–353. doi: 10.1016/j.neuropsychologia.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 264.Saal HP, Delhaye BP, Rayhaun BC, Bensmaia SJ. Simulating tactile signals from the whole hand with millisecond precision. Proc Natl Acad Sci. 2017;114(28):E5693–E5702. doi: 10.1073/pnas.1704856114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Katic N, Siqueira RK, Cleland L, Strzalkowski N, Bent L, Raspopovic S, Saal H. Modeling foot sole cutaneous afferents: FootSim. Iscience. 2023;26(1):105874. doi: 10.1016/j.isci.2022.105874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Williams I, Constandinou TG. Computationally efficient modeling of proprioceptive signals in the upper limb for prostheses: a simulation study. Front Neurosci. 2014;8:181. doi: 10.3389/fnins.2014.00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Cimolato A, Ciotti F, Kljajić J, Valle G, Raspopovic S. Symbiotic electroneural and musculoskeletal framework to encode proprioception via neurostimulation: ProprioStim. Iscience. 2023;26(3):106248. doi: 10.1016/j.isci.2023.106248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Minamitani H, Hagita N. A neural network model of pain mechanisms: computer simulation of the central neural activities essential for the pain and touch sensations. IEEE Trans Syst Man Cybern. 1981;11(7):481–493. [Google Scholar]
- 269.Keijsers N, Stolwijk N, Louwerens J, Duysens J. Classification of forefoot pain based on plantar pressure measurements. Clin Biomech. 2013;28(3):350–356. doi: 10.1016/j.clinbiomech.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 270.Lang VA, Lundh T, Ortiz-Catalan M. Mathematical and computational models for pain: a systematic review. Pain Med. 2021;22(12):2806–2817. doi: 10.1093/pm/pnab177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Chen ZS, Wang J. Pain, from perception to action: a computational perspective. Iscience. 2023;26:1. doi: 10.1016/j.isci.2022.105707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Anchisi D, Zanon M. A Bayesian perspective on sensory and cognitive integration in pain perception and placebo analgesia. PLoS ONE. 2015;10(2):e0117270. doi: 10.1371/journal.pone.0117270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Tabor A, Burr C. Bayesian learning models of pain: a call to action. Curr Opin Behav Sci. 2019;26:54–61. [Google Scholar]
- 274.Hu B, Kim C, Ning X, Xu X. Using a deep learning network to recognise low back pain in static standing. Ergonomics. 2018;61(10):1374–1381. doi: 10.1080/00140139.2018.1481230. [DOI] [PubMed] [Google Scholar]
- 275.Gioftsos G, Grieve D. The use of artificial neural networks to identify patients with chronic low-back pain conditions from patterns of sit-to-stand manoeuvres. Clin Biomech. 1996;11(5):275–280. doi: 10.1016/0268-0033(96)00013-7. [DOI] [PubMed] [Google Scholar]
- 276.Haeri M, Asemani D, Gharibzadeh S. Modeling of pain using artificial neural networks. J Theor Biol. 2003;220(3):277–284. doi: 10.1006/jtbi.2003.3130. [DOI] [PubMed] [Google Scholar]
- 277.Lopez-Martinez D, Picard R. Continuous pain intensity estimation from autonomic signals with recurrent neural networks. In: 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). IEEE, 2018:5624–7. [DOI] [PubMed]
- 278.Santana AN, Cifre I, De Santana CN, Montoya P. Using deep learning and resting-state fMRI to classify chronic pain conditions. Front Neurosci. 2019;13:1313. doi: 10.3389/fnins.2019.01313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Lawson RP, Mathys C, Rees G. Adults with autism overestimate the volatility of the sensory environment. Nat Neurosci. 2017;20(9):1293–1299. doi: 10.1038/nn.4615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Pei J, Chen H, Ma T, Zhang Y, Wang X, Li C, Ye B, Wang X, Zhao J, Dou X. Pain catastrophizing and associated factors in preoperative total knee arthroplasty in Lanzhou, China: a cross-sectional study. BMC Musculoskelet Disord. 2022;23(1):1–8. doi: 10.1186/s12891-022-05435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Saddler MR, Gonzalez R, McDermott JH. Deep neural network models reveal interplay of peripheral coding and stimulus statistics in pitch perception. Nat Commun. 2021;12(1):7278. doi: 10.1038/s41467-021-27366-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Zale EL, Maisto SA, De Vita MJ, Hooten WM, Ditre JW. Increasing cessation motivation and treatment engagement among smokers in pain: a pilot randomized controlled trial. Exp Clin Psychopharmacol. 2021;29(6):593. doi: 10.1037/pha0000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Koban L, Jepma M, López-Solà M, Wager TD. Different brain networks mediate the effects of social and conditioned expectations on pain. Nat Commun. 2019;10(1):1–13. doi: 10.1038/s41467-019-11934-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Bordeleau M, Fernandez de Cossio L, Chakravarty MM, Tremblay M-È. From maternal diet to neurodevelopmental disorders: a story of neuroinflammation. Front Cell Neurosci. 2021;14:612705. doi: 10.3389/fncel.2020.612705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Han F, Cheng J, Liao S, Deng Y. Building Trust for postoperative pain estimation: towards explainable machine-learning prediction based on multimodal indicators. In: 2022 IEEE International Conference on Multimedia and Expo (ICME). IEEE, 2022:01–06.
- 286.Hicks JL, Uchida TK, Seth A, Rajagopal A, Delp SL. Is my model good enough? Best practices for verification and validation of musculoskeletal models and simulations of movement. J Biomech Eng. 2015;137(2):020905. doi: 10.1115/1.4029304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Gribonval R. Should penalized least squares regression be interpreted as maximum a posteriori estimation? IEEE Trans Signal Process. 2011;59(5):2405–2410. [Google Scholar]
- 288.Cashaback JG, McGregor HR, Pun HC, Buckingham G, Gribble PL. Does the sensorimotor system minimize prediction error or select the most likely prediction during object lifting? J Neurophysiol. 2017;117(1):260–274. doi: 10.1152/jn.00609.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Basset G, Koenker R. Theory of least absolute error regressions. J Am Stat Assoc. 1978;73:618–622. [Google Scholar]
- 290.Good PI. Permutation, parametric and bootstrap tests of hypotheses: a practical guide to resampling methods for testing hypotheses. 2005.
- 291.Cashaback JG, Pierrynowski MR, Potvin JR. Calculating individual and total muscular translational stiffness: a knee example. J Biomech Eng. 2013;135(6):061006. doi: 10.1115/1.4024162. [DOI] [PubMed] [Google Scholar]
- 292.Aho K, Derryberry D, Peterson T. Model selection for ecologists: the worldviews of AIC and BIC. Ecology. 2014;95(3):631–636. doi: 10.1890/13-1452.1. [DOI] [PubMed] [Google Scholar]
- 293.Kim HE, Parvin DE, Ivry RB. The influence of task outcome on implicit motor learning. Elife. 2019;8:e39882. doi: 10.7554/eLife.39882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Campagnini S, Liuzzi P, Mannini A, Basagni B, Macchi C, Carrozza MC, Cecchi F. Cross-validation of predictive models for functional recovery after post-stroke rehabilitation. J NeuroEng Rehabilit. 2022;19(1):1–11. doi: 10.1186/s12984-022-01075-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Bagher-Ebadian H, Jafari-Khouzani K, Mitsias PD, Lu M, Soltanian-Zadeh H, Chopp M, Ewing JR. Predicting final extent of ischemic infarction using artificial neural network analysis of multi-parametric MRI in patients with stroke. PLoS ONE. 2011;6(8):e22626. doi: 10.1371/journal.pone.0022626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Lakens D. Sample size justification. Collabra: Psychol. 2022;8(1):33267. [Google Scholar]
- 297.Lakens D, Caldwell AR. Simulation-based power analysis for factorial analysis of variance designs. Adv Methods Pract Psychol Sci. 2021;4(1):2515245920951503. [Google Scholar]
- 298.McKay B, Corson A, Vinh M-A, Jeyarajan G, Tandon C, Brooks H, Hubley J, Carter MJ. Low prevalence of a priori power analyses in motor behavior research. J Motor Learn Dev. 2022;1(aop):1–14. [Google Scholar]
- 299.McKay B, Bacelar MF, Carter MJ. On the reproducibility of power analyses in motor behavior research. J Motor Learn Dev. 2023;11(1):29–44. [Google Scholar]
- 300.McKay B, Yantha Z, Hussien J, Carter M, Ste-Marie D. Meta-analytic findings of the self-controlled motor learning literature: underpowered, biased, and lacking evidential value. Meta-Psychology. 2022 doi: 10.15626/MP.2021.2803. [DOI] [Google Scholar]
- 301.Liew S-L, Zavaliangos-Petropulu A, Jahanshad N, Lang CE, Hayward KS, Lohse KR, Juliano JM, Assogna F, Baugh LA, Bhattacharya AK, et al. The ENIGMA Stroke Recovery Working Group: Big data neuroimaging to study brain-behavior relationships after stroke. Hum Brain Mapp. 2022;43(1):129–148. doi: 10.1002/hbm.25015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Tan T, Chiasson DP, Hu H, Shull PB. Influence of IMU position and orientation placement errors on ground reaction force estimation. J Biomech. 2019;97:109416. doi: 10.1016/j.jbiomech.2019.109416. [DOI] [PubMed] [Google Scholar]
- 303.Caramia C, Torricelli D, Schmid M, Muñoz-Gonzalez A, Gonzalez-Vargas J, Grandas F, Pons JL. IMU-based classification of Parkinson’s disease from gait: a sensitivity analysis on sensor location and feature selection. IEEE J Biomed Health Inform. 2018;22(6):1765–1774. doi: 10.1109/JBHI.2018.2865218. [DOI] [PubMed] [Google Scholar]
- 304.Mihy JA, Wagatsuma M, Cain SM, Hafer JF. Minimizing the effect of IMU misplacement with a functional orientation method. medRxiv, 2022:2022–11.
- 305.Pitto L, van Rossom S, Desloovere K, Molenaers G, Huenaerts C, De Groote F, Jonkers I. Pre-treatment EMG can be used to model post-treatment muscle coordination during walking in children with cerebral palsy. PLoS ONE. 2020;15(2):e0228851. doi: 10.1371/journal.pone.0228851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Meyer AJ, Eskinazi I, Jackson JN, Rao AV, Patten C, Fregly BJ. Muscle synergies facilitate computational prediction of subject-specific walking motions. Front Bioeng Biotechnol. 2016;4:77. doi: 10.3389/fbioe.2016.00077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Ranganathan R, Tomlinson AD, Lokesh R, Lin T-H, Patel P. A tale of too many tasks: task fragmentation in motor learning and a call for model task paradigms. Exp Brain Res. 2021;239:1–19. doi: 10.1007/s00221-020-05908-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.