Abstract
Background
Psoriasis is a frequent form of chronic inflammation in dermatology that is unmistakably linked to the metabolic syndrome (MetS) and its elements. This study was to explore the current status and new developments in the global research, and the holistic landscape of this field more intuitively through bibliometric analysis of scientific output and activity.
Methods
Publications regarding psoriasis and MetS were searched and chosen from the database of the Web of Science Core Collection. Excel 2019, VOSviewer, and CiteSpace software were utilized to conduct bibliometric analysis.
Results
There were 1096 publications included. The scientific outputs in this field had increased from 2004 to 2022, and the expansion could continue in the following years. The United States contributed the most publications (241, 21.99%) and had the most citation frequency (13,489 times). The University of California System was the most productive affiliation. Girolomoni G., Armstrong A.W., Gisondi P. and Gelfand J.M. were key and influential researchers. Journal of the European Academy of Dermatology and Venereology published the greatest number of articles (65 articles). By analyzing keyword frequency and clustering, we have identified the following areas of research interest and frontiers: prevalence, risk, association, gene expression, waist circumference, adipose tissue inflammation, vascular inflammation, cardiovascular disease, psoriatic arthritis, and fibrosis.
Conclusion
This bibliometric analysis elucidates research domain of psoriasis and MetS, portraying present hotspots and future emerging trends. This field has generated significant interest and displays potential for further growth. The United States has made distinguished contributions, and currently dominates this field.
Keywords: psoriasis, metabolic syndrome, gene expression, vascular, inflammation
Introduction
Psoriasis is an immunologically mediated refractory inflammatory skin condition with multisystemic consequences.1–3 Recent studies strongly indicate a positive relationship between psoriasis and metabolic syndrome (MetS).1,4 MetS is a condition characterized by enhanced inflammatory cytokine activity and a pro-inflammatory state. It is an umbrella term for a group of conditions that includes insulin resistance, obesity, type 2 diabetes, hypertension, and dyslipidemia.1,4 Increasing observational studies have repeatedly confirmed strong associations between psoriasis and MetS and its components. The incidence of MetS among individuals afflicted with psoriasis is between 20% and 50%, with psoriasis patients having at least twice the risk of developing metabolic syndrome compared to non-psoriatic individuals.1 Emerging evidence indicates that psoriasis and MetS have a common genetic background, multiple metabolic risk factors, and pathogenic pathways. In the Chinese Han population, psoriasis vulgaris and MetS might share overlapping susceptible genes.5 The correlation between psoriasis and MetS is of significant clinical importance. Certain conventional systemic treatments should be administered with caution in psoriatic individuals with MetS due to their potential adverse effects on coexisting metabolic conditions, especially with prolonged use. As a consequence, it is essential for dermatologists to provide recommendations.
Recently, the association between psoriasis and MetS has gained substantial attention, with numerous related achievements being published. However, few efforts have been made to comprehensively and systematically assess the global scientific outputs and current status in this area. Therefore, we integrated two visualization tools into a fitting visualization method to examine the worldwide state, focal areas of research, and pioneering tendencies in this domain.
Bibliometrics has the capabilities to quantitatively and objectively analyze scientific outputs on a particular topic and visualize the field’s development and emerging trends over time.6–8 It usually takes advantage of visualization tools such as VOSviewer, HistCite, and CiteSpace for creating knowledge network maps through mathematical and statistical methods.6,9,10 Thus, researchers can evaluate scientific outputs qualitatively and quantitatively, thereby tracing research developments, and exploring emerging hotspots. Researchers from various research fields have adopted it as an auxiliary research method.8,10–13 However, a bibliometric analysis of research on psoriasis and MetS has not yet been performed.
This study aims to comprehensively and systematically evaluate the research on psoriasis and MetS. Our aim was to estimate the pattern of publication for global research in this field. Moreover, we sought to evaluate the international collaboration of authors, affiliations and countries. Additionally, we analyzed the research hotspots and emerging trends in this field.
Materials and Methods
Data Source and Search Strategy
We conducted a literature search for the Science Citation Index-Expanded (SCIE) of Web of Science Core Collection (WoSCC) database. The search was performed by two independent authors who used the search strategy: Topic=(psoria*) AND Topic=(Metabolic Syndrome). To prevent any deviations caused by database updates, data was retrieved on February 8, 2023, within a single day.
Inclusion and Exclusion Criteria
Only original articles and reviews related to psoriasis and MetS written in English language were included. Since the first article about psoriasis and MetS in SCIE database was detected in 2014. Thus, the timespan was set from 2004 to 2022. We excluded studies written in non-English, and all other source types including meeting abstracts, letters, early accesses, editorial materials, proceedings papers, corrections and retracted publications.
Data Acquisition and Visualized Analysis
The full records of all results were exported in TXT format. Subsequently, various variables such as the annual output amount, average citations per item, Impact Factor (IF), and Journal Citation Reports (JCR) categories were calculated. Technical abbreviations shall be explained upon first use. Network visualization maps of co-authorship, citation and co-citation, and keyword co-occurrence were built using VOSviewer6 (Version 1.6.17). CiteSpace14 (Version 6.1.R6) was utilized to construct a visual co-occurrence network. This includes the detection of a citation-burst analysis of keywords and references.
Results
Trends in the Output of Publications and Citations
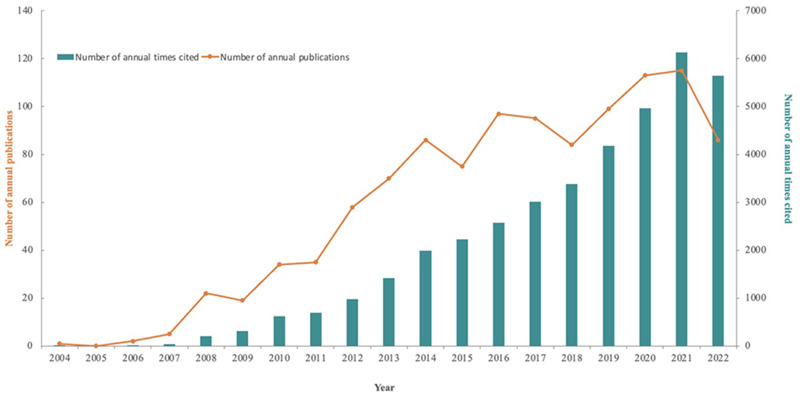
A total of 1096 publications about psoriasis and MetS were retrieved from the SCIE of WoSCC database, comprising 797 articles and 299 reviews. The annual literature output was below 100, except in 2020 and 2021. Notably, from 2004 to 2007, publication output was exceptionally low, signaling a research hiatus during that period. From 2008 to 2022, there was an overall increase in the yearly publication volume, reflecting increasing research interest. While the number of publications on psoriasis and MetS fluctuated, an overall upward trend was observed. In contrast, the annual total citations of articles have been rapidly rising since 2004. The total number of citations was 38,555, with an average of 35.18 citations per item (Figure 1).
Figure 1.
Trends in the annual number of outputs and the annual total citations of articles.
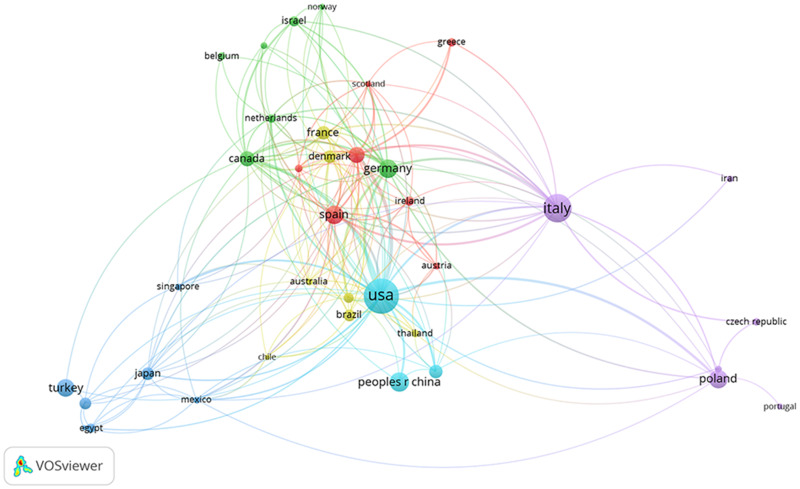
Contributions of Countries/Regions
Seventy-three countries/regions have contributed to the study of psoriasis and MetS. Table 1 shows the top 10 most productive countries and regions in their outputs on the subject, with the United States leading at 21.99% (241/1096) of the overall publication numbers, followed by Italy at 14.69% (161/1096) and China at 6.66% (73/1096). The United States also had the most citations (13,489) and the highest H-index (63). Figure 2 illustrates the close collaboration between these countries/regions, highlighting the United States’ extensive collaborations with countries such as Germany, England, and Canada.
Table 1.
The Top 10 Productive Countries/Regions for Publishing Research on Psoriasis and MetS
| Rank | Countries/Regions | Article Counts | Percentage (n/1096) | H-Index | Total Citations | Average Article Citations |
|---|---|---|---|---|---|---|
| 1 | United States | 241 | 21.99% | 63 | 13,489 | 55.97 |
| 2 | Italy | 161 | 14.69% | 40 | 5837 | 36.25 |
| 3 | China | 73 | 6.66% | 17 | 934 | 12.79 |
| 4 | Spain | 70 | 6.39% | 24 | 2065 | 29.50 |
| 5 | Germany | 68 | 6.20% | 29 | 4846 | 71.26 |
| 6 | Poland | 67 | 6.11% | 18 | 1001 | 14.94 |
| 7 | Turkey | 63 | 5.75% | 18 | 835 | 13.25 |
| 8 | England | 51 | 4.65% | 28 | 3427 | 67.20 |
| 9 | Canada | 45 | 4.11% | 24 | 2450 | 54.44 |
| 10 | Taiwan | 38 | 3.47% | 18 | 1399 | 36.82 |
Figure 2.
International collaboration map of research on psoriasis and MetS generated by VOSviewer.
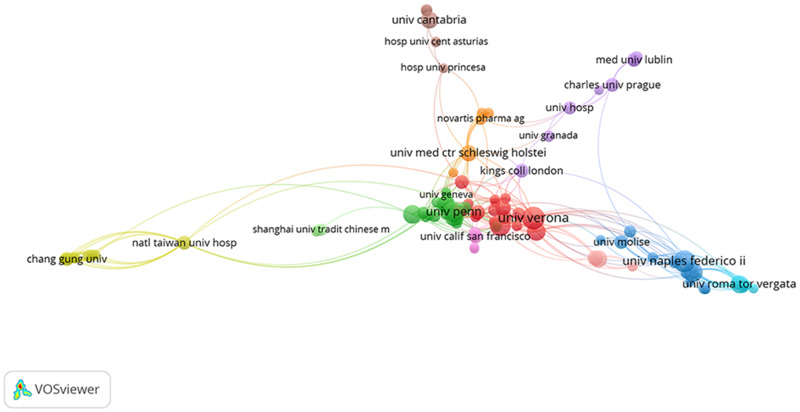
Contributions of Affiliations
From the 1096 publications, 1698 affiliations were identified. The United States represented a significant share of the research network. The University of California System led in publication volume, closely followed by the University of Naples Federico II and Harvard University. The University of Pennsylvania and the University of California System achieved the highest average citations per article and H-index, respectively. For further details, refer to Table 2. VOSviewer was used to generate a network visualization map for affiliations’ collaboration. We visualized affiliations with a minimum of 5 publications. Figure 3 reveals the collaboration map among 109 affiliations, represented by 109 nodes. The affiliations were organized into ten clusters of various colors, and there was considerable coordination between the affiliations, particularly those inside the same cluster.
Table 2.
The Top 10 Productive Affiliations Ranked by the Numbers of Publications
| Rank | Affiliations | Countries | Article Counts | H-Index | Total Citations | Average Citations per Article |
|---|---|---|---|---|---|---|
| 1 | University of California System | United States | 46 | 26 | 3045 | 66.20 |
| 2 | University of Naples Federico II | Italy | 38 | 21 | 1178 | 31.00 |
| 3 | Harvard University | United States | 32 | 20 | 1920 | 60.00 |
| 4 | University of Verona | Italy | 30 | 21 | 2458 | 81.93 |
| 5 | University of Copenhagen | Denmark | 29 | 16 | 1044 | 36.00 |
| 6 | University of Pennsylvania | United States | 26 | 20 | 3428 | 131.85 |
| 7 | Medical University of Bialystok | Poland | 25 | 10 | 327 | 13.08 |
| 8 | Harvard Medical School | United States | 22 | 15 | 1410 | 64.09 |
| 9 | University of Toronto | Canada | 22 | 15 | 1326 | 60.27 |
| 10 | University of California Davis | United States | 20 | 17 | 1688 | 84.40 |
Figure 3.
The affiliations’ collaboration network visualization map generated by VOSviewer.
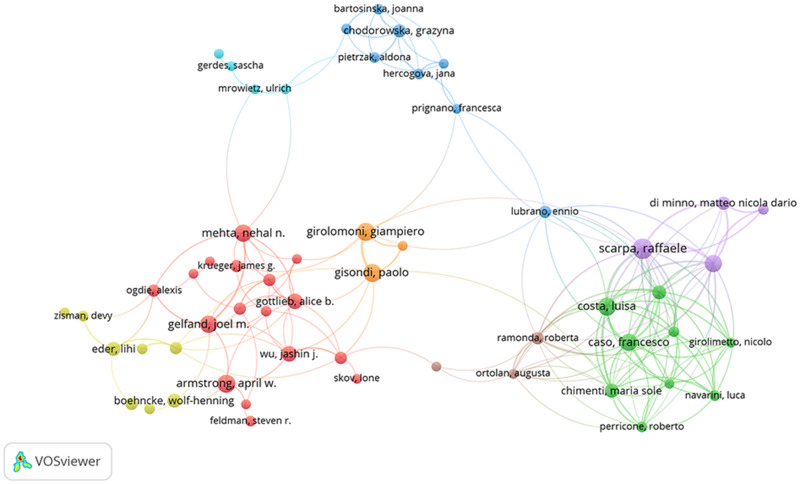
Authors and Co-Authorship
The psoriasis and MetS papers included work from 5039 authors in total. There were 171 articles (15.60%) produced by the top 10 most active writers. Among them, five were from the United States, four were from Italy, and the remaining author was from Portugal. Girolomoni G. from University of Verona contributed the most articles (22 articles), followed by Armstrong A.W. from University of Southern California with 21 articles, and Gisondi P. from University of Verona with 19 articles. Regarding the total citations, Gelfand J.M. (2958 times) from University of Pennsylvania ranked first, followed by Girolomoni G. (2101 times) from University of Verona and Gisondi P. (1776 times) from University of Verona. See Table 3 for details. As displayed in Figure 4, Scarpa R., Caso F., and Gelfand J.M. were located at a central position of the cooperating clusters in the cooperative network map of authors. The prolific authors engaged in active collaboration.
Table 3.
The Top 10 Most Productive Authors in Publications on Psoriasis and MetS
| Rank | Author | Count | H-Index | Total Citations | Countries | Institutions |
|---|---|---|---|---|---|---|
| 1 | Girolomoni G. | 22 | 17 | 2101 | Italy | Sections of Dermatology and Venereology, Department of Medicine, University of Verona |
| 2 | Armstrong A.W. | 21 | 16 | 1676 | United States | University of Southern California, Los Angeles |
| 3 | Gisondi P. | 19 | 18 | 1776 | Italy | Sections of Dermatology and Venereology, Department of Medicine, University of Verona |
| 4 | Gelfand J.M. | 18 | 14 | 2958 | United States | Dermatology and the Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania |
| 5 | J.J. Wu | 17 | 9 | 834 | United States | Department of Dermatology, University of Miami Miller School of Medicine, Miami, FL, USA |
| 6 | Costa L. | 16 | 11 | 377 | Portugal | Rheumatology Unit, Department of Clinical Medicine and Surgery, University Federico II |
| 7 | Caso F. | 15 | 10 | 363 | Italy | Rheumatology Unit, Department of Clinical Medicine and Surgery, University Federico II |
| 8 | Peluso R. | 15 | 12 | 471 | Italy | Rheumatology Unit, Department of Clinical Medicine and Surgery, University Federico II |
| 9 | Mehta N.N. | 14 | 14 | 1581 | United States | Section of Inflammation and Cardiometabolic Diseases, National Heart, Lung and Blood Institute, Bethesda, Maryland (Mehta) |
| 10 | Gottlieb A.B. | 14 | 11 | 1002 | United States | Department of Dermatology at New York Medical College, Valhalla |
Figure 4.
The authors’ collaboration network visualization map generated by VOSviewer.
Journals and Co-Cited Journals
Two hundred and ninety-five scholarly journals published papers concerning psoriasis and MetS. Table 4 presents the leading 10 active journals by publication quantity in ranked order. Four of these journals were from the United States and two came from England, and the others were from Poland, Sweden, Japan, and Germany. These journals published 303 articles, taking up 27.65% of all the publications. There were 9 journals with at least 20 publications, of which Journal of the European Academy of Dermatology and Venereology (IF 2022=9.228) published the largest number of articles (65, 6.28%), followed by British Journal of Dermatology (IF 2022=11.113) and Journal of the American Academy of Dermatology (IF 2022=15.487). The British Journal of Dermatology attained the highest value of H-index (33), and Journal of the American Academy of Dermatology had the highest IF (IF 2022=15.487) and largest number of total citations (3956 times).
Table 4.
The Top 10 Journals of Research on Psoriasis and MetS Ranked by Publication Outputs
| Rank | Journal | Count | IF 2022 | JCR 2022 | H-Index | Total Citations |
|---|---|---|---|---|---|---|
| 1 | Journal of the European Academy Dermatology and Venereology (England) | 65 | 9.228 | Q1 | 29 | 2494 |
| 2 | British Journal of Dermatology (England) | 48 | 11.113 | Q1 | 33 | 3461 |
| 3 | Journal of the American Academy of Dermatology (United States) | 41 | 15.487 | Q1 | 28 | 3956 |
| 4 | Postepy Dermatologii i Alergologii (Poland) | 25 | 1.664 | Q4 | 9 | 239 |
| 5 | Journal of Dermatological Treatment (Sweden) | 23 | 3.230 | Q2 | 11 | 446 |
| 6 | Journal of Dermatology (Japan) | 22 | 3.468 | Q2 | 15 | 618 |
| 7 | Archives of Dermatological Research (Germany) | 21 | 3.033 | Q2 | 14 | 951 |
| 8 | International Journal of Dermatology (United States) | 20 | 3.204 | Q2 | 13 | 396 |
| 9 | International Journal of Molecular Sciences (United States) | 20 | 6.208 | Q1 | 10 | 526 |
| 10 | Dermatologic Therapy (United States) | 18 | 3.858 | Q2 | 8 | 368 |
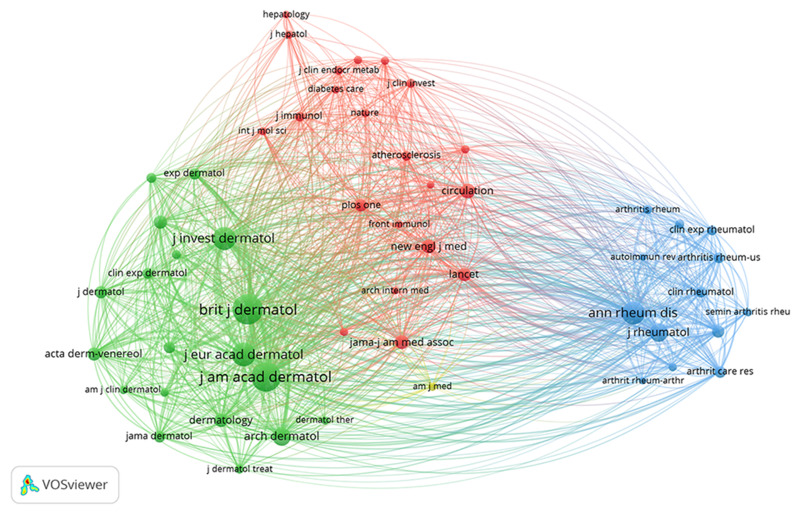
Co-citation exists when two journals are cited by one or more works simultaneously. Journal influence is measured by the number of co-occurrences, which indicates whether the journal is significantly influential in a particular field of research.8 Of the 4464 co-cited scholarly journals, seven had co-citations exceeding 1000, of which four were published in England, two in the United States and one in Canada. The British Journal of Dermatology obtained the highest amount of co-citations (n=3591, IF 2022=11.113), followed by the Journal of the American Academy of Dermatology (n =3377, IF 2022=15.487) and the Journal of the European Academy of Dermatology and Venereology (n=2149, IF 2022=9.228). Only journals with co-citations greater or equal to 200 (54/4464, 1.21%) were included in the co-citation network (Figure 5). British Journal of Dermatology and Journal of the American Academy of Dermatology exhibited larger bubbles caused by greater co-citations. Additionally, British Journal of Dermatology showed active co-citation relationships with Journal of the American Academy of Dermatology and Journal of the European Academy of Dermatology and Venereology.
Figure 5.
The journal co-citation network visualization map generated by VOSviewer.
Top Cited Publications and References Bursts
Table 5 presents the 10 most cited original articles on psoriasis and MetS.15–24 Notably, Journal of the American Academy of Dermatology, Archives of Dermatological Research and British Journal of Dermatology have an important impact on researchers and academics in this field. The study authored by Neimann et al,15 published in Journal of the American Academy of Dermatology, has the highest number of citations with 739 to date. Table 6 lists the top 10 co-cited references,15–18,22,25–29 each with more than 100 citations and at least 115 co-citations.
Table 5.
The Top 10 Highly Cited Articles About Psoriasis and MetS
| Title | Journal | IF 2022 | Year | Citations |
|---|---|---|---|---|
| Prevalence of cardiovascular risk factors in patients with psoriasis15 | Journal of the American Academy of Dermatology | 15.487 | 2006 | 739 |
| Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis16 | Archives of Dermatological Research | 3.033 | 2006 | 477 |
| Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study17 | British Journal of Dermatology | 11.113 | 2007 | 468 |
| Prevalence of Metabolic Syndrome in Patients with Psoriasis: A Population-Based Study in the United Kingdom18 | Journal of Investigative Dermatology | 7.590 | 2012 | 303 |
| Epidemiology and comorbidities of psoriasis patients in a national database in Taiwan19 | Journal of Dermatological Science | 5.408 | 2011 | 220 |
| Co-morbidity and Age-related Prevalence of Psoriasis: Analysis of Health Insurance Data in Germany20 | Acta Dermato-Venereologica | 3.875 | 2010 | 215 |
| Weight loss improves the response of obese patients with moderate-to-severe chronic plaque psoriasis to low-dose cyclosporine therapy: a randomized, controlled, investigator-blinded clinical trial21 | American Journal of Clinical Nutrition | 8.472 | 2008 | 208 |
| Prevalence of the Metabolic Syndrome in Psoriasis Results From the National Health and Nutrition Examination Survey, 2003–200622 | Archives of Dermatology (Now renamed JAMA Dermatology) | 11.816 | 2011 | 207 |
| Obesity and the risk of psoriatic arthritis: a population-based study23 | Annals of the Rheumatic Diseases | 27.973 | 2012 | 189 |
| Psoriasis and the risk of diabetes and hypertension – A prospective Study of US female nurses24 | Archives of Dermatology | 11.816 | 2009 | 185 |
Table 6.
The Top 10 Co-Cited References on Psoriasis and MetS
| Rank | Co-Cited Reference | Citations |
|---|---|---|
| 1 | Gelfand Joel M, et al (2006). Journal of the American Medical Association, V296, P1735.25 | 287 |
| 2 | Gisondi P, et al (2007). British Journal of Dermatology, V157, P68.17 | 245 |
| 3 | Sommer Dorothea M, et al (2006). Archives of Dermatological Research, V298, P321.16 | 225 |
| 4 | Neimann Andrea L, et al (2006). Journal of the American Academy of Dermatology, V55, P829.15 | 224 |
| 5 | Langan Sinéad M, et al (2012). Journal of Investigative Dermatology, V132, P556.18 | 174 |
| 6 | Love Thorvardur Jon, et al (2011). Archives of Dermatology, V147, P419.22 | 135 |
| 7 | Armstrong April W, et al (2013). Journal of the American Academy of Dermatology, V68, P654.26 | 125 |
| 8 | Naldi Luigi.et al, (2005). Journal of Investigative Dermatology, V125, P61.27 | 118 |
| 9 | Boehacke Wolf-Henning, et al (2011). Experimental Dermatology, V20, P303.28 | 115 |
| 10 | Davidovici Batya B, et al (2010). Journal of Investigative Dermatology, V130, P1785.29 | 115 |
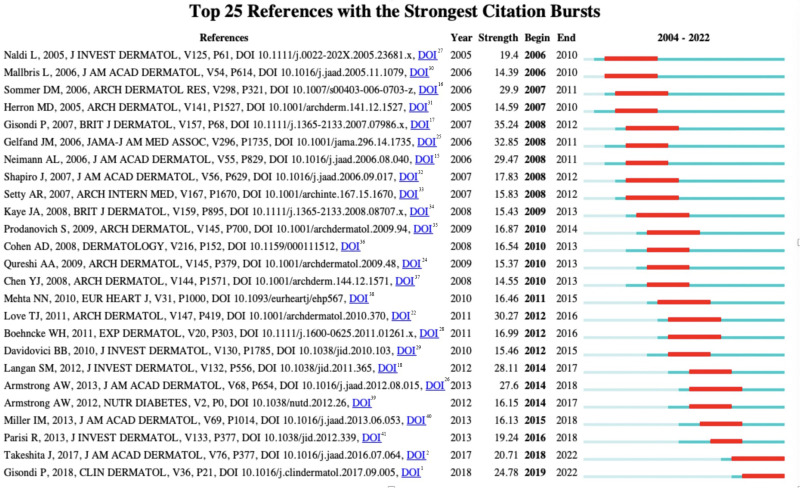
References with high-frequency citations of related research within a specific period are known as “citations bursts”. In this study, we utilized the CiteSpace software to analyze the 25 references with the most frequent citation bursts. The time interval is represented by the blue line segment in Figure 6,1,2,15–18,22,24–41 and the red line segment indicates the time frame during which the references were actively co-cited. Sixty-four percent of the top 25 references experienced citation surges from 2009 to 2019, suggesting significant interest in the study of psoriasis and MetS, which may continue to grow. Notably, the most recent citation bursts were detected in 2018 and 2019 indicating continued interest in the topic.
Figure 6.
The top 25 references with the strongest citation bursts generated by CiteSpace software.1,2,15–18,22,24–40.
Analysis of Research Hotspots
Keywords are the essence and concentration of publications, reflecting the focus of a certain research field. According to high-frequency keywords, keyword co-occurrence analysis and keyword clusters analysis, scholars could explore the current status, development, and major trends of various research hotspots in the field. Similarly, keywords with the strongest citation burst can also predict the potential frontiers in the study of psoriasis and MetS.
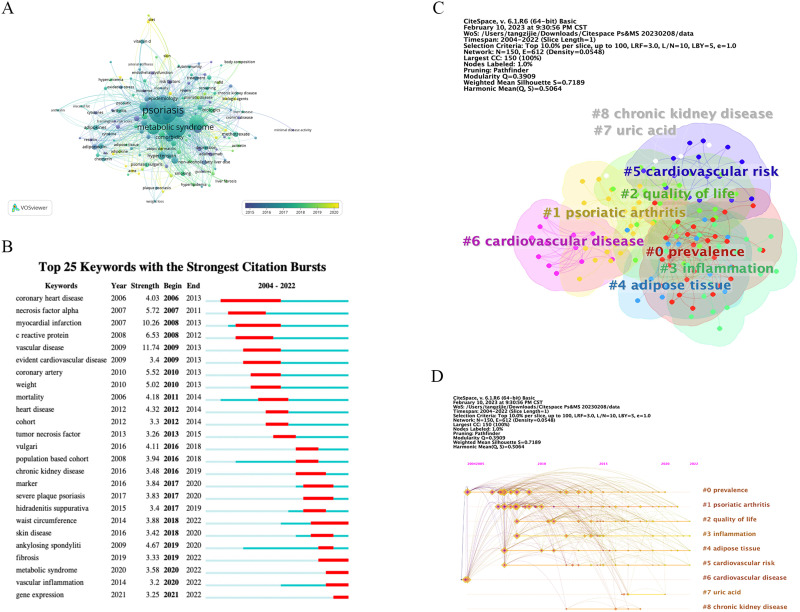
Table 7 displays the top 10 high-frequency keywords by CiteSpace software, including “metabolic syndrome”, “prevalence”, “disease”, “rheumatoid arthritis”, “risk”, “association”, “cardiovascular disease (CVD)”, “risk factor”, “psoriatic arthritis (PsA)”, and “myocardial infarction”. The author keyword co-occurrence analysis is illustrated in Figure 7A. Each circle, color-coded, represents the mean year in which the keyword appeared. Each circle with various size represents the frequency of the keyword occurrence. The separation between any two circles denotes the connection between them, and the thickness of the connecting line denotes the strength of the connection.
Table 7.
The Top 10 High-Frequency Keywords on Research of Psoriasis and MetS from 2004 to 2022
| Rank | Keyword | Frequency | Centrality |
|---|---|---|---|
| 1 | Metabolic syndrome | 697 | 0.17 |
| 2 | Prevalence | 309 | 0.04 |
| 3 | Disease | 218 | 0.08 |
| 4 | Rheumatoid arthritis | 211 | 0.17 |
| 5 | Risk | 203 | 0.06 |
| 6 | Association | 192 | 0.06 |
| 7 | Cardiovascular disease | 191 | 0.18 |
| 8 | Risk factor | 165 | 0.06 |
| 9 | Psoriatic arthritis | 148 | 0.11 |
| 10 | Myocardial infarction | 146 | 0.08 |
Figure 7.
Analysis of keywords. (A) The overlay visualization map of keywords related to psoriasis and MetS generated by VOSviewer software; (B) The top 25 keywords with the strongest citation bursts of publications generated by CiteSpace software; (C) Keyword clusters analysis generated by CiteSpace software; (D) The timeline view of keyword clusters generated by CiteSpace software.
The use of CiteSpace software to identify strong keyword bursts has significant implications for exploring emerging trends and hotspots over time. Notably, keywords with strong citation bursts during specific periods were identified, including “waist circumference” (2018–2022), “fibrosis” (2019–2022), “vascular inflammation” (2020–2022), “metabolic syndrome” (2020–2022), and “gene expression” (2020–2022). The citation bursts continue to the present time (see Figure 7B). This indicates that these research topics have been attracting enormous attention recently and have the possibility to become new research focuses in the coming years. Figure 7C presents keyword clusters analysis of research on psoriasis and MetS from 2004 to 2022. We obtained 8 clusters, mainly including cluster #0 prevalence, #1 psoriatic arthritis, #2 quality of life, #3 inflammation, #4 adipose tissue, #5 cardiovascular risk, and #6 cardiovascular disease. Moreover, we performed the timeline view of keyword clusters. As shown in Figure 7D, 4 clustering groups are the most concerned research hotspots, including cluster #2 quality of life, #3 inflammation, #4 adipose tissue, #5 cardiovascular risk.
By combining the keyword frequency and keyword clustering analyses, we were able to identify the following research frontiers and hotspots (see Table 7 and Figure 7): prevalence, risk, association, gene expression, waist circumference, adipose tissue, inflammation, vascular inflammation, cardiovascular disease, psoriatic arthritis, and fibrosis.
Discussion
General Information
In this era of information explosion, managing knowledge efficiently is a constant challenge for scientific researchers. This study aims to provide an innovative approach to the management of knowledge and the visualization of knowledge structures. Our article presents the latest bibliometric visualization of worldwide research on psoriasis and MetS. This is the first-ever study to take advantage of bibliometric indicators and visualization tools to analyze the current status, development, and major trends in research on psoriasis and MetS in an intuitive and informative way.
The annual number of publications in a research field can be a significant indicator to reveal the productivity and evolution of the topic over the years and can also indicate the research focus of this field. As shown in Figure 1, the development of research on psoriasis and MetS from 2004 to 2022 showed an overall rapid increase trend with small fluctuations. Specifically, the extremely small amount of publications from 2004 to 2008 demonstrates that this research remained in its infancy, whereas the annual number of publications exhibited a rapid growth in 2008 and related progress was dramatic. Since that time, the yearly number of scientific outputs has sustained a significant level. The sum of citations a paper garners showcases its extent of influence and dissemination, hence possibly indicating its standard. Based on the citation analysis (Figure 1), the annual total citations of articles have been rapidly increasing since 2004. On the basis of current trends, we believe that this field will flourish in the future.
Among countries/regions, the United States and Italy were the most prolific countries, with an overwhelmingly greater amount of papers than any other country/region. Moreover, the United States had the highest number of citations and achieved the highest H-index, indicating its absolute advantage in this field. Remarkably, the United States and countries such as Germany, England and Canada engaged in relatively active scientific collaborations. Besides, half of the top 10 productive affiliations belonged to the USA. This result suggests that establishing top-tier scientific research affiliations is a crucial cornerstone for enhancing the standing of the country’s academic institutions.
The top 10 most productive authors predominantly hailed from the United States and Italy. Girolomoni G. from the University of Verona produced the most scientific outputs, with Armstrong A.W. from the University of Southern California and Gisondi P. from the University of Verona following closely behind. Regarding the total citations, Gelfand J.M. from the University of Pennsylvania ranked first, followed by Girolomoni G. and Gisondi P. Thus, we can conclude that Girolomoni G., Armstrong A.W., Gisondi P., and Gelfand J.M. are key researchers and have exerted considerable leadership influence on this area. As a result, these authors and their teams are more likely to make remarkable achievements and contribute further crucial publications related to psoriasis and MetS. Therefore, leading researchers from renowned institutions may be suitable candidates for scientific collaboration due to the possible funding priority.
Additionally, of the top 10 journals presented in Table 4, Journal of the European Academy of Dermatology and Venereology, British Journal of Dermatology, and Journal of the American Academy of Dermatology may be the core journals of research on psoriasis and MetS. Among the top 10 journals, only two journals (Journal of the American Academy of Dermatology, IF 2022=15.487; British Journal of Dermatology, IF 2022=11.113) had an IF higher than 10.0. Two of the journals, including Journal of the European Academy of Dermatology and Venereology (IF 2022=9.228), and International Journal of Molecular Sciences (IF 2022=6.208) had an IF between 5.0 and 10.0. These results indicate that it is a challenge to publish articles about psoriasis and MetS in high-IF journals.
From the perspective of references, “references with citation bursts” was a helpful method to follow emerging trends of corresponding research. The term denotes the frequent citations of relevant research during a specific timeframe. This indicates significant interest in scientific publications, revealing the dynamic changes and current trends within the field. Sixty-four percent of the references had citation bursts from 2009 to 2019. The latest sources displaying citation surges were identified in 2018 and 2019, and these surges persist. This is due to two publications in Journal of the American Academy of Dermatology by Takeshita et al2 and in Clinics in Dermatology by Gisondi et al,1 which deserve further attention.
The Hotspots and Frontiers
Close Association of Psoriasis and MetS
Psoriasis is closely related to the clinical characteristics of MetS, such as insulin resistance, obesity, type 2 diabetes, hypertension, atherosclerotic dyslipidemia, and non-alcoholic fatty liver disease. Increasing observational studies have repeatedly confirmed the strong associations of psoriasis with MetS and its components. Between 20% and 50% of psoriatic patients have MetS, and those who have psoriasis are at least twice as likely to develop MetS as non-psoriatic controls.1 MetS has the potential to significantly impede the quality of life for psoriatic patients.
There are various hypotheses proposing reasons for the higher risk of psoriasis in MetS patients, including genetic predisposition, multiple metabolic risk factors, and pathogenic mechanisms.1 One widely accepted hypothesis suggests that increased inflammation marker levels in MetS lead to an increased risk of psoriasis. Both psoriasis and MetS share the same inflammatory pathways, including T helper (Th)-17-mediated or Th-1-mediated inflammatory pathways.29 The pathological mechanisms of both psoriasis and impaired lipid regulation involve many other similar cytokines.42,43 Moreover, patients with central obesity possess an excess of adipose tissue that secretes adipokines, initiating the chronic inflammation processes of psoriasis.44 An additional hypothesis proposes that psoriasis and MetS share genetic loci. There could be shared susceptibility genes for psoriasis vulgaris and MetS among the Chinese Han population.5 Nevertheless, several studies have shown no genetic links between the two diseases.45–48
It is yet to be established which components of MetS are potential risk factors for psoriasis. Previous studies have reported positive associations of all MetS components with psoriasis risk.49–51 However, several robust recent studies pointed to abdominal obesity and dyslipidemia as the primary MetS components that strongly correlate with psoriasis risk. In contrast, there was no significant association between blood pressure and fasting glucose levels with the risk of psoriasis.1,22,52–56 Most recently, Lee et al57 discovered that waist circumference had the strongest association with psoriasis, followed by high-density lipoprotein (HDL) and triglyceride levels. They found no significant association between fasting glucose and psoriasis risk. Notably, blood pressure was linked to lower risk in the MetS group.57
The relationship between MetS and the severity of psoriasis has been disputed. Numerous clinical studies reveal that patients with psoriasis and MetS are more severe compared to those without MetS. A team of Japanese researchers found markedly elevated psoriasis area severity index (PASI) in the psoriatic group with MetS in comparison to those in the non-MetS group, implying a close association between MetS and the severity of psoriasis.58 Furthermore, the study suggests that MetS may exacerbate or worsen the pathological process of psoriasis.58 A systematic review of 3791 psoriasis patients demonstrated an increased incidence of MetS with the worsening of psoriasis.59 Patients experiencing severe plaque psoriasis were more prone to MetS than those with mild psoriasis. Huang et al60 investigated 399 individuals with chronic plaque psoriasis from Taiwan and found that the increase in body mass index (BMI) was linearly correlated with the severity of psoriasis, and obesity had a more pronounced effect on the severity of psoriasis in male patients. In addition, C-reaction protein (CRP) can be adopted as a marker to evaluate the severity of psoriasis, and its level of patients with MetS is higher than that of those without MetS, providing further evidence for the link between MetS and the severity of psoriasis.29
Nevertheless, some studies have shown no correlation between MetS and the severity of psoriasis. The prevalence of MetS and the severity of psoriasis did not correlate, according to a cross-sectional research of 244 psoriasis patients.49 A retrospective study conducted on 86 Chinese patients with erythrodermic psoriasis revealed a greater incidence of metabolic syndrome components, such as abdominal obesity, hypertension, and dyslipidemia, among those suffering from the condition.61 However, there was no difference in the incidence of hyperglycemia.61 Interestingly, the study found no correlation between the severity of erythrodermic psoriasis and the prevalence of MetS.61 A case–control study conducted in Thailand reported that there was no significant variation in the severity of psoriasis between the MetS group and the non-MetS group in Southeast Asia.62
An increasing number of studies have substantiated that psoriasis is not merely an inflammation of the skin, but also affects the whole-body system.63 CRP is a classic biomarker for identifying systemic inflammation.64–66 Studies have found that CRP levels in individuals with psoriasis are higher than in the healthy population, and its levels are directly proportionate to the severity of skin lesions.67 Furthermore, patients with arthropathic psoriasis exhibited higher levels of CRP than those with skin psoriasis alone.68 This indicates an increased systemic inflammation level when psoriasis affects other tissues or organs.
Cardiovascular Disease and Psoriasis
Recently, the association of psoriasis with CVD has aroused considerable attention. The association between psoriasis and CVD has been verified through numerous clinical trials.69 Furthermore, the elevated risk of CVD positively correlates with the severity of psoriasis. The mechanism may be due to the systemic inflammatory response that occurs in psoriasis which induces insulin resistance, damages endothelial cells, and ultimately leads to CVD, a process that Boehncke refers to as the “psoriatic march”.28 Psoriasis and CVD share similar pathogeneses, involving common genetic factors, insulin resistance, oxidative stress, lipid metabolism, vascular endothelial cell dysfunction, and inflammatory pathways such as tumour necrosis factor (TNF) -α and interleukin (IL)-23/Th-17 pathways.69,70 Concerning the genetic background, polymorphisms of the IL-23 gene are associated with the development or progression of CVD, whereas the polymorphisms of IL-12 and IL-17 gene are not.71
The visceral adipose tissue can release several adipokines (resistin, leptin, and visfatin), cytokines (TNF-α, IL-6, and IL-8), and chemokines (monocyte chemoattractant protein 1, MCP-1), which encourage atherosclerosis.72 Enhanced resistin and leptin levels activate inflammatory cytokines, thereby initiating and organizing vascular inflammation.73 Further research has shown that IL-17 has been linked to collagen deposition, fibrosis, and atherosclerosis.74 As a result, it is hypothesized that by targeting inflammatory pathways or cytokines, biologics could potentially benefit psoriatic patients with CVD. These findings are supported by studies which report that Secukinumab, a biological treatment, has the potential to improve flow-mediated dilation and endothelial function, ultimately resulting in a protective effect for psoriatic individuals with CVD.75
Recent research indicates that erythrodermic psoriasis is frequently associated with cardiovascular disease.61 Metabolic syndrome, abdominal adiposity, and hypertension independently predict erythrodermic psoriasis, and their presence can lead to the development of cardiovascular disease.61 Therefore, active intervention to manage these cardiovascular risk factors is recommended for the management of erythrodermic psoriasis.61 There is limited research on whether psoriatic individuals with MetS have a higher risk of CVD compared to those without MetS. A study conducted in Spain found that psoriatic patients with MetS had an elevated risk of CVD.76 Therefore, clinicians should monitor the CVD risk in psoriatic patients with MetS while treating psoriasis. Additionally, systemic inflammation of both psoriasis and MetS should be inhibited to prevent the development of CVD.
Psoriatic Arthritis and Metabolic Syndrome
Compared to the general population and other autoimmune diseases, patients with PsA have a higher risk and prevalence of MetS and its related components.77–80 PsA patients are prone to metabolic syndrome and insulin resistance.81 Approximately 40.6%–44% of patients with PsA have MetS.81–83 Furthermore, patients with PsA have a high prevalence of obesity, hypertension, diabetes, hyperlipidemia, and CVD, which was about 30%–37%, 33.6%–38.7%, 11.5%–13.6%, 17.5%–20.7%, and 3.2%–7.5%, respectively.83 A recent study has shown that high prevalence of MetS in PsA correlates with the severity of PsA.84
The common pathogenesis of PsA and MetS has not been fully elucidated. A chronic pro- inflammatory state and white adipose tissue (WAT) are supposed to explain the potential interconnections between them. WAT releases a large amount of adipokines that have synergistic effect on PsA inflammation and metabolic state.85,86 Pro-inflammatory cytokines including TNF-α, IL-6 and IL-17 are elevated in skin, peripheral blood, fluid and synovial membrane of PsA patients.87 These mediators induce insulin resistance.
Leptin is a representative adipokine involved in MetS as well in PsA pathogenesis.86 The plasma concentrations of leptin show positive correlations with body fat mass.86 Previous studies have found that leptin levels are higher in PsA patients than in non-PsA individuals.88–91 Resistin can induce insulin resistance.92 Elevated levels of resistin and visfatin have been found in PsA patients.93,94 Although serum levels of resistin, adiponectin, and visfatin are found higher in PsA patients, its pathophysiological implications have to be explored with more extensive studies. Therefore, it is necessary for dermatologists to screen, comprehensively evaluate, and closely monitor MetS and its components of psoriatic patients. Researchers could delve deeper into the link of psoriatic arthritis with pathogenetic aspects of MetS.
Liver Fibrosis in Psoriasis and MetS
A recent study has shown that nearly 10% of patients with psoriasis are highly susceptible to advanced liver fibrosis, whereas 78% fall under the low-risk category.95 Moreover, metabolic syndrome (MetS) and its components, such as hypertension, dyslipidemia, and diabetes mellitus, are significant risk factors for liver fibrosis. It is worth noting that disease-related factors such as severe psoriasis and PsA did not exhibit a statistically significant correlation with liver fibrosis, which was surprising. Previous research has indicated an association between non-alcoholic fatty liver disease (NAFLD) and the development of liver fibrosis in individuals with psoriasis.95,96 Ortolan et al97 discovered that insulin resistance was the principal determinant of liver fibrosis, with PsA not proving to be a significant predictor. Methotrexate (MTX)-induced liver fibrosis is reported to be rare. Thus, MetS and its risk factors, including insulin resistance, could be a greater risk factor for liver fibrosis than the use of MTX.98
The close relationship between MetS or its components and NAFLD among psoriasis patients suggests that local and systemic pro-inflammatory/anti-inflammatory cytokine imbalance are pathogenic mechanisms shared by them.99 These cytokines include IL-1, IL-6, IL-17 and TNF-α and they can act locally on the epidermis and dermis by disrupting the proliferation and differentiation of keratinocytes, thus forming psoriatic plaques.100,101 However, they may also play a systemic role and cause insulin resistance and other inflammatory mediators involved in NAFLD with metabolic dysfunction. To be specific, IL-17 can promote the activation of hepatic stellate cells to produce collagen, which is central to the development of liver fibrosis.102 IL-17 blockade has been shown in mouse models to restore insulin sensitivity and prevents NAFLD inflammation.103 Besides, genetic ablation of the IL-17A receptor also alleviates NAFLD.103 Due to the impact of NAFLD on psoriasis, recommendations for managing psoriasis comorbidities, including MetS and NAFLD, were published recently.104,105
The Holistic Approach to Psoriasis Patients with MetS
This study explores the potential for advancements in the research of psoriasis and MetS, highlighting the complex connection between the two conditions. Therefore, it is crucial to take a holistic approach when treating patients who have both psoriasis and MetS. This approach prioritizes the patient’s needs and treats them as a whole person rather than a collection of separate conditions.106 Additionally, Camela et al107 found that co-morbidities associated with psoriasis can restrict the selection of suitable treatments, but effective drugs targeting disorders with co-morbid pathological pathways can overcome this challenge. Patients with psoriasis and metabolic syndrome can be treated with co-medications for both conditions, reducing the need for multiple medications and potential drug interactions.
Strengths and Limitations
This study offers a systematic and comprehensive analysis of worldwide research on psoriasis and MetS through bibliometric methods. The analysis explores the current status, progress, hotspots, and frontiers in the field. Using visualized mapping, this study presents the holistic landscape of this field intuitively, facilitating managing knowledge structure effectively, especially for new academic researchers. To ensure comprehensive assessment, we adopt two visualization tools for analysis from various aspects. All the data came from SCIE of WoSCC database, one of the most comprehensive databases of scientific outputs, ensuring the consistency of the analytical data and the quality of the analysis. And almost all the articles of high quality were included. Moreover, our analysis revealed the scientific research capability of various authors, affiliations and countries, and even collaborative partnerships among them, thereby serving as a guidance for further study and potential collaboration.
However, our study inevitably has several limitations. Firstly, the data retrieval on psoriasis and MetS publications was completed within a single day, and the data were restricted to the period 2004 to 2022. Because we take into account that the database updates continuously and some literatures may be retracted afterwards. Besides, CiteSpace software has a limited analysis of time span. Thus, most recent findings were not included in this research. Secondly, our data was only obtained from SCIE of WoSCC database, considering the limited capabilities of the analysis software. As a result, publications in other databases may have been omitted. This may lead to potentially incomplete analytical data. Thirdly, publications only written in English were included in this study. Hence, it is possible that significant accomplishments published in other languages have not been considered. All mentioned above could incur deviations of bibliometric analysis from actual publications to varying degrees. Nevertheless, we believe that the vast majority of scientific outputs relating to psoriasis and MetS have been incorporated in this research, and the deviations are slight and considered acceptable, making the conclusions not be changed.
Conclusions
This bibliometric study reveals the knowledge domain of research on psoriasis and MetS, showcasing current hotspots and emerging trends. Research on psoriasis and MetS has received extensive interest. Based on the current global trends, scientific outputs in this field will be on the rise and may flourish in the future. The United States has made tremendous progress, and actually, dominated in this research area. Further attention will be paid to vascular inflammation, cardiovascular disease, psoriatic arthritis and liver fibrosis. Especially, the pathogenic mechanism shared by psoriasis and MetS, including gene expression and adipose tissue, may be the emerging popular topics in the research of psoriasis and MetS.
Funding Statement
This study was funded by the National Natural Science Foundation of China (No. 82273530) and Beijing Natural Science Foundation (No. 7224344).
Abbreviations
MetS, metabolic syndrome; SCIE, science citation index expanded; WoSCC, web of science core collection; IF, impact factor; JCR, journal citation reports; CVD, cardiovascular disease; PsA, psoriatic arthritis; Th, T helper; HDL, high-density lipoprotein; PASI, psoriasis area severity index; BMI, body mass index; CRP, C-reaction protein; TNF, tumour necrosis factor; IL, interleukin; MCP-1, monocyte chemoattractant protein 1; WAT, white adipose tissue; NAFLD, non-alcoholic fatty liver disease; MTX, methotrexate.
Data Sharing Statement
The data used to support the findings in this study can be made available by the corresponding authors Rui Wang and Cheng-xin Li, without undue reservation.
Ethics Approval and Consent to Participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Gisondi P, Fostini AC, Fossà I, Girolomoni G, Targher G. Psoriasis and the metabolic syndrome. Clin Dermatol. 2018;36(1):21–28. doi: 10.1016/j.clindermatol.2017.09.005 [DOI] [PubMed] [Google Scholar]
- 2.Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases: epidemiology. J Am Acad Dermatol. 2017;76(3):377–390. doi: 10.1016/j.jaad.2016.07.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN. Psoriasis. Lancet. 2021;397(10281):1301–1315. doi: 10.1016/S0140-6736(20)32549-6 [DOI] [PubMed] [Google Scholar]
- 4.Bavoso NC, Pinto JM, Soares MMS, Diniz MDS, Teixeira Júnior AL. Psoriasis in obesity: comparison of serum levels of leptin and adiponectin in obese subjects - cases and controls. An Bras Dermatol. 2019;94(2):192–197. doi: 10.1590/abd1806-4841.20197716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Y, Li X, Huang YP, et al. Association of polymorphisms of metabolism-related genes with psoriasis vulgaris in Han Chinese. Biomed Res Int. 2021;2021:9920631. doi: 10.1155/2021/9920631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Eck NJ, Waltman L. Software survey: vOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. doi: 10.1007/s11192-009-0146-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen C, Song M. Visualizing a field of research: a methodology of systematic scientometric reviews. PLoS One. 2019;14(10):e0223994. doi: 10.1371/journal.pone.0223994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma D, Yang B, Guan B, et al. A bibliometric analysis of pyroptosis from 2001 to 2021. Front Immunol. 2021;12:731933. doi: 10.3389/fimmu.2021.731933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu T, Yang L, Mao H, Ma F, Wang Y, Zhan Y. Knowledge domain and emerging trends in podocyte injury research from 1994 to 2021: a bibliometric and visualized analysis. Front Pharmacol. 2021;12:772386. doi: 10.3389/fphar.2021.772386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu X, Hu J, Deng S, et al. Bibliometric and visual analysis of research on the links between the gut microbiota and depression from 1999 to 2019. Front Psychiatry. 2021;11:587670. doi: 10.3389/fpsyt.2020.587670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qin A, Sun J, Gao C, Li C. Bibliometrics analysis on the research status and trends of adult-onset Still’s disease: 1921–2021. Front Immunol. 2022;13:950641. doi: 10.3389/fimmu.2022.950641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang J, Chen P, Miao L. A bibliometric and scientific knowledge-map study of the chimeric antigen receptor (CAR) natural killer (NK) cell-related research from 2010 to 2022. Front Immunol. 2022;13:969196. doi: 10.3389/fimmu.2022.969196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang S, Zhao S, Ye Y, Jia L, Lou Y. Global research trends on the links between gut microbiota and cancer immunotherapy: a bibliometric analysis (2012–2021). Front Immunol. 2022;13:952546. doi: 10.3389/fimmu.2022.952546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen C, Dubin R, Kim MC. Emerging trends and new developments in regenerative medicine: a scientometric update (2000 – 2014). Expert Opin Biol Ther. 2014;14(9):1295–1317. doi: 10.1517/14712598.2014.920813 [DOI] [PubMed] [Google Scholar]
- 15.Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB, Gelfand JM. Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol. 2006;55(5):829–835. doi: 10.1016/j.jaad.2006.08.040 [DOI] [PubMed] [Google Scholar]
- 16.Sommer DM, Jenisch S, Suchan M, Christophers E, Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res. 2006;298(7):321–328. doi: 10.1007/s00403-006-0703-z [DOI] [PubMed] [Google Scholar]
- 17.Gisondi P, Tessari G, Conti A, et al. Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study. Br J Dermatol. 2007;157(1):68–73. doi: 10.1111/j.1365-2133.2007.07986.x [DOI] [PubMed] [Google Scholar]
- 18.Langan SM, Seminara NM, Shin DB, et al. Prevalence of metabolic syndrome in patients with psoriasis: a population-based study in the United Kingdom. J Invest Dermatol. 2012;132(3 Pt 1):556–562. doi: 10.1038/jid.2011.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai TF, Wang TS, Hung ST, et al. Epidemiology and comorbidities of psoriasis patients in a national database in Taiwan. J Dermatol Sci. 2011;63(1):40–46. doi: 10.1016/j.jdermsci.2011.03.002 [DOI] [PubMed] [Google Scholar]
- 20.Augustin M, Reich K, Glaeske G, Schaefer I, Radtke M. Co-morbidity and age-related prevalence of psoriasis: analysis of health insurance data in Germany. Acta Derm Venereol. 2010;90(2):147–151. doi: 10.2340/00015555-0770 [DOI] [PubMed] [Google Scholar]
- 21.Gisondi P, Del Giglio M, Di Francesco V, Zamboni M, Girolomoni G. Weight loss improves the response of obese patients with moderate-to-severe chronic plaque psoriasis to low-dose cyclosporine therapy: a randomized, controlled, investigator-blinded clinical trial. Am J Clin Nutr. 2008;88(5):1242–1247. doi: 10.3945/ajcn.2008.26427 [DOI] [PubMed] [Google Scholar]
- 22.Love TJ, Qureshi AA, Karlson EW, Gelfand JM, Choi HK. Prevalence of the metabolic syndrome in psoriasis: results from the national health and nutrition examination survey, 2003–2006. Arch Dermatol. 2011;147(4):419–424. doi: 10.1001/archdermatol.2010.370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Love TJ, Zhu Y, Zhang Y, et al. Obesity and the risk of psoriatic arthritis: a population-based study. Ann Rheum Dis. 2012;71(8):1273–1277. doi: 10.1136/annrheumdis-2012-201299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qureshi AA, Choi HK, Setty AR, Curhan GC. Psoriasis and the risk of diabetes and hypertension: a prospective study of US female nurses. Arch Dermatol. 2009;145(4):379–382. doi: 10.1001/archdermatol.2009.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gelfand JM, Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB. Risk of myocardial infarction in patients with psoriasis. JAMA. 2006;296(14):1735–1741. doi: 10.1001/jama.296.14.1735 [DOI] [PubMed] [Google Scholar]
- 26.Armstrong AW, Harskamp CT, Armstrong EJ. Psoriasis and metabolic syndrome: a systematic review and meta-analysis of observational studies. J Am Acad Dermatol. 2013;68(4):654–662. doi: 10.1016/j.jaad.2012.08.015 [DOI] [PubMed] [Google Scholar]
- 27.Naldi L, Chatenoud L, Linder D, et al. Cigarette smoking, body mass index, and stressful life events as risk factors for psoriasis: results from an Italian case-control study. J Invest Dermatol. 2005;125(1):61–67. doi: 10.1111/j.0022-202X.2005.23681.x [DOI] [PubMed] [Google Scholar]
- 28.Boehncke WH, Boehncke S, Tobin AM, Kirby B. The ‘psoriatic march’: a concept of how severe psoriasis may drive cardiovascular comorbidity. Exp Dermatol. 2011;20(4):303–307. doi: 10.1111/j.1600-0625.2011.01261.x [DOI] [PubMed] [Google Scholar]
- 29.Davidovici BB, Sattar N, Prinz J, et al. Psoriasis and systemic inflammatory diseases: potential mechanistic links between skin disease and co-morbid conditions. J Invest Dermatol. 2010;130(7):1785–1796. doi: 10.1038/jid.2010.103 [DOI] [PubMed] [Google Scholar]
- 30.Mallbris L, Granath F, Hamsten A, Ståhle M. Psoriasis is associated with lipid abnormalities at the onset of skin disease. J Am Acad Dermatol. 2006;54(4):614–621. doi: 10.1016/j.jaad.2005.11.1079 [DOI] [PubMed] [Google Scholar]
- 31.Herron MD, Hinckley M, Hoffman MS, et al. Impact of obesity and smoking on psoriasis presentation and management. Arch Dermatol. 2005;141(12):1527–1534. doi: 10.1001/archderm.141.12.1527 [DOI] [PubMed] [Google Scholar]
- 32.Shapiro J, Cohen AD, David M, et al. The association between psoriasis, diabetes mellitus, and atherosclerosis in Israel: a case-control study. J Am Acad Dermatol. 2007;56(4):629–634. doi: 10.1016/j.jaad.2006.09.017 [DOI] [PubMed] [Google Scholar]
- 33.Setty AR, Curhan G, Choi HK. Obesity, waist circumference, weight change, and the risk of psoriasis in women: nurses’ Health Study II. Arch Intern Med. 2007;167(15):1670–1675. doi: 10.1001/archinte.167.15.1670 [DOI] [PubMed] [Google Scholar]
- 34.Kaye JA, Li L, Jick SS. Incidence of risk factors for myocardial infarction and other vascular diseases in patients with psoriasis. Br J Dermatol. 2008;159(4):895–902. doi: 10.1111/j.1365-2133.2008.08707.x [DOI] [PubMed] [Google Scholar]
- 35.Prodanovich S, Kirsner RS, Kravetz JD, Ma F, Martinez L, Federman DG. Association of psoriasis with coronary artery, cerebrovascular, and peripheral vascular diseases and mortality. Arch Dermatol. 2009;145(6):700–703. doi: 10.1001/archdermatol.2009.94 [DOI] [PubMed] [Google Scholar]
- 36.Cohen AD, Sherf M, Vidavsky L, Vardy DA, Shapiro J, Meyerovitch J. Association between psoriasis and the metabolic syndrome. A cross-sectional study. Dermatology. 2008;216(2):152–155. doi: 10.1159/000111512 [DOI] [PubMed] [Google Scholar]
- 37.Chen YJ, Wu CY, Shen JL, et al. Psoriasis independently associated with hyperleptinemia contributing to metabolic syndrome. Arch Dermatol. 2008;144(12):1571–1575. doi: 10.1001/archderm.144.12.1571 [DOI] [PubMed] [Google Scholar]
- 38.Mehta NN, Azfar RS, Shin DB, Neimann AL, Troxel AB, Gelfand JM. Patients with severe psoriasis are at increased risk of cardiovascular mortality: cohort study using the General Practice Research Database. Eur Heart J. 2010;31(8):1000–1006. doi: 10.1093/eurheartj/ehp567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Armstrong AW, Harskamp CT, Armstrong EJ. The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr Diabetes. 2012;2(12):e54. doi: 10.1038/nutd.2012.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller IM, Ellervik C, Yazdanyar S, Jemec GB. Meta-analysis of psoriasis, cardiovascular disease, and associated risk factors. J Am Acad Dermatol. 2013;69(6):1014–1024. doi: 10.1016/j.jaad.2013.06.053 [DOI] [PubMed] [Google Scholar]
- 41.Parisi R, Symmons DP, Griffiths CE, Ashcroft DM. Identification and management of psoriasis and associated comorbidiTy (IMPACT) project team. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133(2):377–385. doi: 10.1038/jid.2012.339 [DOI] [PubMed] [Google Scholar]
- 42.Ferretti G, Bacchetti T, Campanati A, Simonetti O, Liberati G, Offidani A. Correlation between lipoprotein(a) and lipid peroxidation in psoriasis: role of the enzyme paraoxonase-1. Br J Dermatol. 2012;166(1):204–207. doi: 10.1111/j.1365-2133.2011.10539.x [DOI] [PubMed] [Google Scholar]
- 43.Armstrong EJ, Krueger JG. Lipoprotein metabolism and inflammation in patients with psoriasis. Am J Cardiol. 2016;118(4):603–609. doi: 10.1016/j.amjcard.2016.05.060 [DOI] [PubMed] [Google Scholar]
- 44.Hjuler KF, Gormsen LC, Vendelbo MH, Egeberg A, Nielsen J, Iversen L. Increased global arterial and subcutaneous adipose tissue inflammation in patients with moderate-to-severe psoriasis. Br J Dermatol. 2017;176(3):732–740. doi: 10.1111/bjd.15149 [DOI] [PubMed] [Google Scholar]
- 45.Gupta Y, Möller S, Zillikens D, Boehncke WH, Ibrahim SM, Ludwig RJ. Genetic control of psoriasis is relatively distinct from that of metabolic syndrome and coronary artery disease. Exp Dermatol. 2013;22(8):552–553. doi: 10.1111/exd.12192 [DOI] [PubMed] [Google Scholar]
- 46.Lu Y, Chen H, Nikamo P, et al. Association of cardiovascular and metabolic disease genes with psoriasis. J Invest Dermatol. 2013;133(3):836–839. doi: 10.1038/jid.2012.366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gerdes S, Osadtschy S, Buhles N, Baurecht H, Mrowietz U. Cardiovascular biomarkers in patients with psoriasis. Exp Dermatol. 2014;23(5):322–325. doi: 10.1111/exd.12381 [DOI] [PubMed] [Google Scholar]
- 48.Koch M, Baurecht H, Ried JS, et al. Psoriasis and cardiometabolic traits: modest association but distinct genetic architectures. J Invest Dermatol. 2015;135(5):1283–1293. doi: 10.1038/jid.2015.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Milčić D, Janković S, Vesić S, et al. Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based cross-sectional study. An Bras Dermatol. 2017;92(1):46–51. doi: 10.1590/abd1806-4841.20175178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim HN, Han K, Park YG, Lee JH. Metabolic syndrome is associated with an increased risk of psoriasis: a nationwide population-based study. Metabolism. 2019;99:19–24. doi: 10.1016/j.metabol.2019.07.001 [DOI] [PubMed] [Google Scholar]
- 51.Miller IM, Ellervik C, Zarchi K, et al. The association of metabolic syndrome and psoriasis: a population- and hospital-based cross-sectional study. J Eur Acad Dermatol Venereol. 2015;29(3):490–497. doi: 10.1111/jdv.12595 [DOI] [PubMed] [Google Scholar]
- 52.Snekvik I, Nilsen TIL, Romundstad PR, Saunes M. Metabolic syndrome and risk of incident psoriasis: prospective data from the HUNT Study, Norway. Br J Dermatol. 2019;180(1):94–99. doi: 10.1111/bjd.16885 [DOI] [PubMed] [Google Scholar]
- 53.Meziane M, Kelati A, Najdi A, Berraho A, Nejjari C, Mernissi FZ. Metabolic syndrome in Moroccan patients with psoriasis. Int J Dermatol. 2016;55(4):396–400. doi: 10.1111/ijd.12623 [DOI] [PubMed] [Google Scholar]
- 54.Mebazaa A, El Asmi M, Zidi W, et al. Metabolic syndrome in Tunisian psoriatic patients: prevalence and determinants. J Eur Acad Dermatol Venereol. 2011;25(6):705–709. doi: 10.1111/j.1468-3083.2010.03856.x [DOI] [PubMed] [Google Scholar]
- 55.Danielsen K, Wilsgaard T, Olsen AO, et al. Elevated odds of metabolic syndrome in psoriasis: a population-based study of age and sex differences. Br J Dermatol. 2015;172(2):419–427. doi: 10.1111/bjd.13288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Albareda M, Ravella A, Castelló M, Saborit S, Peramiquel L, Vila L. Metabolic syndrome and its components in patients with psoriasis. Springerplus. 2014;3:612. doi: 10.1186/2193-1801-3-612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee HJ, Han KD, Park HE, et al. Changes in metabolic syndrome and risk of psoriasis: a nationwide population-based study. Sci Rep. 2021;11(1):24043. doi: 10.1038/s41598-021-03174-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Takahashi H, Iinuma S, Honma M, Iizuka H. Increased serum C-reactive protein level in Japanese patients of psoriasis with cardio- and cerebrovascular disease. J Dermatol. 2014;41(11):981–985. doi: 10.1111/1346-8138.12632 [DOI] [PubMed] [Google Scholar]
- 59.Singh S, Young P, Armstrong AW. Relationship between psoriasis and metabolic syndrome: a systematic review. G Ital Dermatol Venereol. 2016;151(6):663–677. [PubMed] [Google Scholar]
- 60.Huang YH, Yang LC, Hui RY, et al. Relationships between obesity and the clinical severity of psoriasis in Taiwan. J Eur Acad Dermatol Venereol. 2010;24(9):1035–1039. doi: 10.1111/j.1468-3083.2010.03573.x [DOI] [PubMed] [Google Scholar]
- 61.Ma AR, Liu F, Wang R, et al. Prevalence of metabolic syndrome in Chinese patients with erythrodermic psoriasis: a case-control study. Front Endocrinol. 2021;12:677912. doi: 10.3389/fendo.2021.677912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chularojanamontri L, Wongpraparut C, Silpa-Archa N, Chaweekulrat P. Metabolic syndrome and psoriasis severity in South-East Asian patients: an investigation of potential association using current and chronological assessments. J Dermatol. 2016;43(12):1424–1428. doi: 10.1111/1346-8138.13540 [DOI] [PubMed] [Google Scholar]
- 63.Grozdev I, Korman N, Tsankov N. Psoriasis as a systemic disease. Clin Dermatol. 2014;32(3):343–350. doi: 10.1016/j.clindermatol.2013.11.001 [DOI] [PubMed] [Google Scholar]
- 64.Navarro SL, Kantor ED, Song X, et al. Factors associated with multiple biomarkers of systemic inflammation. Cancer Epidemiol Biomarkers Prev. 2016;25(3):521–531. doi: 10.1158/1055-9965.EPI-15-0956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pay JB, Shaw AM. Towards salivary C-reactive protein as a viable biomarker of systemic inflammation. Clin Biochem. 2019;68:1–8. doi: 10.1016/j.clinbiochem.2019.04.006 [DOI] [PubMed] [Google Scholar]
- 66.Michels KB, Keller K, Pereira A, et al. Association between indicators of systemic inflammation biomarkers during puberty with breast density and onset of menarche. Breast Cancer Res. 2020;22(1):104. doi: 10.1186/s13058-020-01338-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Uysal S, Yılmaz FM, Karatoprak K, Artüz F, Cumbul NU. The levels of serum pentraxin3, CRP, fetuin-A, and insulin in patients with psoriasis. Eur Rev Med Pharmacol Sci. 2014;18(22):3453–3458. [PubMed] [Google Scholar]
- 68.Lin YC, Dalal D, Churton S, et al. Relationship between metabolic syndrome and carotid intima-media thickness: cross-sectional comparison between psoriasis and psoriatic arthritis. Arthritis Care Res. 2014;66(1):97–103. doi: 10.1002/acr.22144 [DOI] [PubMed] [Google Scholar]
- 69.Cai J, Cui L, Wang Y, Li Y, Zhang X, Shi Y. Cardiometabolic comorbidities in patients with psoriasis: focusing on risk, biological therapy, and pathogenesis. Front Pharmacol. 2021;12:774808. doi: 10.3389/fphar.2021.774808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chandrashekar L, Kumarit GR, Rajappa M, Revathy G, Munisamy M, Thappa DM. 25-hydroxy vitamin D and ischaemia-modified albumin levels in psoriasis and their association with disease severity. Br J Biomed Sci. 2015;72(2):56–60. doi: 10.1080/09674845.2015.11666797 [DOI] [PubMed] [Google Scholar]
- 71.Piaserico S, Orlando G, Messina F. Psoriasis and cardiometabolic diseases: shared genetic and molecular pathways. Int J Mol Sci. 2022;23(16):9063. doi: 10.3390/ijms23169063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nosalski R, Guzik TJ. Perivascular adipose tissue inflammation in vascular disease. Br J Pharmacol. 2017;174(20):3496–3513. doi: 10.1111/bph.13705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cerman AA, Bozkurt S, Sav A, Tulunay A, Elbaşi MO, Ergun T. Serum leptin levels, skin leptin and leptin receptor expression in psoriasis. Br J Dermatol. 2008;159(4):820–826. doi: 10.1111/j.1365-2133.2008.08742.x [DOI] [PubMed] [Google Scholar]
- 74.Huang LH, Zinselmeyer BH, Chang CH, et al. Interleukin-17 drives interstitial entrapment of tissue lipoproteins in experimental psoriasis. Cell Metab. 2019;29(2):475–487.e7. doi: 10.1016/j.cmet.2018.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.von Stebut E, Reich K, Thaçi D, et al. Impact of secukinumab on endothelial dysfunction and other cardiovascular disease parameters in psoriasis patients over 52 weeks. J Invest Dermatol. 2019;139(5):1054–1062. doi: 10.1016/j.jid.2018.10.042 [DOI] [PubMed] [Google Scholar]
- 76.Belinchón I, Vanaclocha F, de la Cueva-Dobao P, et al. Metabolic syndrome in Spanish patients with psoriasis needing systemic therapy: prevalence and association with cardiovascular disease in PSO-RISK, a cross-sectional study. J DermatolTreat. 2015;26(4):318–325. doi: 10.3109/09546634.2014.983039 [DOI] [PubMed] [Google Scholar]
- 77.Caso F, Del Puente A, Oliviero F, et al. Metabolic syndrome in psoriatic arthritis: the interplay with cutaneous involvement. Evidences from literature and a recent cross-sectional study. Clin Rheumatol. 2018;37(3):579–586. doi: 10.1007/s10067-017-3975-0 [DOI] [PubMed] [Google Scholar]
- 78.Edson-Heredia E, Zhu B, Lefevre C, et al. Prevalence and incidence rates of cardiovascular, autoimmune, and other diseases in patients with psoriatic or psoriatic arthritis: a retrospective study using clinical practice research datalink. J Eur Acad Dermatol Venereol. 2015;29(5):955–963. doi: 10.1111/jdv.12742 [DOI] [PubMed] [Google Scholar]
- 79.Adeodato Ramos LM, Gomes KWP, de Saboia Mont’Alverne AR, Braga MV, Costa Vasconcelos AH, Rodrigues CEM. High prevalence of metabolic syndrome in patients with psoriatic arthritis from northeastern Brazil: association with traditional cardiovascular risk factors and biologic disease-modifying antirheumatic drugs. J Clin Rheumatol. 2021;27(6S):S186–S192. doi: 10.1097/RHU.0000000000001631 [DOI] [PubMed] [Google Scholar]
- 80.Mok CC, Ko GT, Ho LY, Yu KL, Chan PT, To CH. Prevalence of atherosclerotic risk factors and the metabolic syndrome in patients with chronic inflammatory arthritis. Arthritis Care Res. 2011;63(2):195–202. doi: 10.1002/acr.20363 [DOI] [PubMed] [Google Scholar]
- 81.Haroon M, Gallagher P, Heffernan E, FitzGerald O. High prevalence of metabolic syndrome and of insulin resistance in psoriatic arthritis is associated with the severity of underlying disease. J Rheumatol. 2014;41(7):1357–1365. doi: 10.3899/jrheum.140021 [DOI] [PubMed] [Google Scholar]
- 82.Özkan SG, Yazısız H, Behlül A, Gökbelen YA, Borlu F, Yazısız V. Prevalence of metabolic syndrome and degree of cardiovascular disease risk in patients with Psoriatic Arthritis. Eur J Rheumatol. 2017;4(1):40–45. doi: 10.5152/eurjrheum.2017.16052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Carneiro S, Palominos PE, Anti SMA, et al. Brazilian society of rheumatology 2020 guidelines for psoriatic arthritis. Adv Rheumatol. 2021;61(1):69. doi: 10.1186/s42358-021-00219-y [DOI] [PubMed] [Google Scholar]
- 84.Song Z, Deng X, Xie W, Li B, Zhang Z. Clinical characteristics of psoriatic arthritis in Chinese patients: a cross-sectional study. Rheumatol Ther. 2021;8(4):1845–1857. doi: 10.1007/s40744-021-00384-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Caso F, Postiglione L, Covelli B, et al. Pro-inflammatory adipokine profile in psoriatic arthritis: results from a cross-sectional study comparing PsA subset with evident cutaneous involvement and subset ”sine psoriasis”. Clin Rheumatol. 2019;38(9):2547–2552. doi: 10.1007/s10067-019-04619-w [DOI] [PubMed] [Google Scholar]
- 86.Chiricozzi A, Raimondo A, Lembo S, et al. Crosstalk between skin inflammation and adipose tissue-derived products: pathogenic evidence linking psoriasis to increased adiposity. Expert Rev Clin Immunol. 2016;12(12):1299–1308. doi: 10.1080/1744666X.2016.1201423 [DOI] [PubMed] [Google Scholar]
- 87.Caso F, Chimenti MS, Navarini L, et al. Metabolic Syndrome and psoriatic arthritis: considerations for the clinician. Expert Rev Clin Immunol. 2020;16(4):409–420. doi: 10.1080/1744666X.2020.1740593 [DOI] [PubMed] [Google Scholar]
- 88.Eder L, Jayakar J, Pollock R, et al. Serum adipokines in patients with psoriatic arthritis and psoriasis alone and their correlation with disease activity. Ann Rheum Dis. 2013;72(12):1956–1961. doi: 10.1136/annrheumdis-2012-202325 [DOI] [PubMed] [Google Scholar]
- 89.Feld J, Nissan S, Eder L, et al. Increased prevalence of metabolic syndrome and adipocytokine levels in a psoriatic arthritis cohort. J Clin Rheumatol. 2018;24(6):302–307. doi: 10.1097/RHU.0000000000000721 [DOI] [PubMed] [Google Scholar]
- 90.Vachatova S, Andrys C, Krejsek J, et al. Metabolic syndrome and selective inflammatory markers in psoriatic patients. J Immunol Res. 2016;2016:5380792. doi: 10.1155/2016/5380792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kyriakou A, Patsatsi A, Sotiriadis D, Goulis DG. Serum leptin, resistin, and adiponectin concentrations in psoriasis: a meta-analysis of observational studies. Dermatology. 2017;233(5):378–389. doi: 10.1159/000481882 [DOI] [PubMed] [Google Scholar]
- 92.Wolk K, Sabat R. Adipokines in psoriasis: an important link between skin inflammation and metabolic alterations. Rev Endocr Metab Disord. 2016;17(3):305–317. doi: 10.1007/s11154-016-9381-0 [DOI] [PubMed] [Google Scholar]
- 93.Kyriakou A, Patsatsi A, Sotiriadis D, Goulis DG. Effects of treatment for psoriasis on circulating levels of leptin, adiponectin and resistin: a systematic review and meta-analysis. Br J Dermatol. 2018;179(2):273–281. doi: 10.1111/bjd.16437 [DOI] [PubMed] [Google Scholar]
- 94.Dikbas O, Tosun M, Bes C, Tonuk SB, Aksehirli OY, Soy M. Serum levels of visfatin, resistin and adiponectin in patients with psoriatic arthritis and associations with disease severity. Int J Rheum Dis. 2016;19(7):672–677. doi: 10.1111/1756-185X.12444 [DOI] [PubMed] [Google Scholar]
- 95.Bellinato F, Gisondi P, Mantovani A, Girolomoni G, Targher G. Risk of non-alcoholic fatty liver disease in patients with chronic plaque psoriasis: an updated systematic review and meta-analysis of observational studies. J Endocrinol Invest. 2022;45(7):1277–1288. doi: 10.1007/s40618-022-01755-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Candia R, Ruiz A, Torres-Robles R, Chávez-Tapia N, Méndez-Sánchez N, Arrese M. Risk of non-alcoholic fatty liver disease in patients with psoriasis: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2015;29(4):656–662. doi: 10.1111/jdv.12847 [DOI] [PubMed] [Google Scholar]
- 97.Ortolan A, Lorenzin M, Tadiotto G, et al. Metabolic syndrome, non-alcoholic fatty liver disease and liver stiffness in psoriatic arthritis and psoriasis patients. Clin Rheumatol. 2019;38(10):2843–2850. doi: 10.1007/s10067-019-04646-7 [DOI] [PubMed] [Google Scholar]
- 98.Maybury CM, Jabbar-Lopez ZK, Wong T, Dhillon AP, Barker JN, Smith CH. Methotrexate and liver fibrosis in people with psoriasis: a systematic review of observational studies. Br J Dermatol. 2014;171(1):17–29. doi: 10.1111/bjd.12941 [DOI] [PubMed] [Google Scholar]
- 99.Perez-Carreras M, Casis-Herce B, Rivera R, Fernandez I, Martinez-Montiel P, Villena V. Non-alcoholic fatty liver disease in patients with intestinal, pulmonary or skin diseases: inflammatory cross-talk that needs a multidisciplinary approach. World J Gastroenterol. 2021;27(41):7113–7124. doi: 10.3748/wjg.v27.i41.7113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mantovani A, Gisondi P, Lonardo A, Targher G. Relationship between non-alcoholic fatty liver disease and psoriasis: a novel hepato-dermal axis? Int J Mol Sci. 2016;17(2):217. doi: 10.3390/ijms17020217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Prussick RB, Miele L. Nonalcoholic fatty liver disease in patients with psoriasis: a consequence of systemic inflammatory burden? Br J Dermatol. 2018;179(1):16–29. doi: 10.1111/bjd.16239 [DOI] [PubMed] [Google Scholar]
- 102.de Morales JMG R, Puig L, Daudén E, et al. Critical role of interleukin (IL)-17 in inflammatory and immune disorders: an updated review of the evidence focusing in controversies. Autoimmun Rev. 2020;19(1):102429. doi: 10.1016/j.autrev.2019.102429 [DOI] [PubMed] [Google Scholar]
- 103.Gomes AL, Teijeiro A, Burén S, et al. Metabolic inflammation-associated IL-17A causes non-alcoholic steatohepatitis and hepatocellular carcinoma. Cancer Cell. 2016;30(1):161–175. doi: 10.1016/j.ccell.2016.05.020 [DOI] [PubMed] [Google Scholar]
- 104.Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80(4):1073–1113. doi: 10.1016/j.jaad.2018.11.058 [DOI] [PubMed] [Google Scholar]
- 105.Dauden E, Blasco AJ, Bonanad C, et al. Position statement for the management of comorbidities in psoriasis. J Eur Acad Dermatol Venereol. 2018;32(12):2058–2073. doi: 10.1111/jdv.15177 [DOI] [PubMed] [Google Scholar]
- 106.Camela E, Potestio L, Fabbrocini G, Ruggiero A, Megna M. New frontiers in personalized medicine in psoriasis. Expert Opin Biol Ther. 2022;22(12):1431–1433. doi: 10.1080/14712598.2022.2113872 [DOI] [PubMed] [Google Scholar]
- 107.Camela E, Potestio L, Fabbrocini G, Pallotta S, Megna M. The holistic approach to psoriasis patients with comorbidities: the role of investigational drugs. Expert Opin Investig Drugs. 2023;32(6):537–552. doi: 10.1080/13543784.2023.2219387 [DOI] [PubMed] [Google Scholar]