Abstract
Background
The Directly Observed Treatment-Short Course (DOTS) Programme was implemented by WHO and includes a combination of four anti-tuberculosis (TB) drugs (isoniazid, pyrazinamide, ethambutol and rifampicin) for a period of six months to eradicate the TB infection completely. Diabetes mellitus (DM) is recognized as one of a strong contributor of TB according to World Health Organization (WHO). The presence of diabetes mellitus type 2 (DM type 2) makes TB treatment complicated. Thus, the objective of the current meta-analysis was to identify and quantify the impact of type 2 DM on treatment outcomes of TB patients treated under the DOTS Programme.
Methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Through a systematic review of relevant literature, we focused on studies investigating treatment outcomes including extended treatment duration and recurrence for individuals with both TB and DM undergoing DOTS therapy. The extracted information included study designs, sample sizes, patient characteristics and reported treatment results.
Results
In 44 studies from different parts of the world, the pooled HR for the impact of DM on extended treatment duration and reoccurrence were HR 0.72, 95% CI 0.56–0.83, p < .01 and HR 0.93, 95% CI 0.70–1.04, p = .08, respectively. The pooled HR for impact of DM on composite TB treatment outcomes was calculated as 0.76 (95% CI 0.60–0.87), p < .01 with an effect size of 41.18. The heterogeneity observed among the included studies was moderate (I2 = 55.79%).
Conclusions
A negative impact of DM was found on recurrence and extended treatment duration in TB patients treated with DOTS therapy. DM type 2 is responsible for the TB treatment prolongation and TB recurrence rates. By implementing effective management strategies and advancing research, the challenges can be mitigated, arising due to the complex interaction between DM and TB.
Keywords: Diabetes mellitus, tuberculosis, comorbidity, extended treatment duration, recurrence, disease progression
Introduction
Tuberculosis (TB) infection is a serious global health problem. According to World Health Organization (WHO), approximately 5.8 million people were diagnosed with TB and almost 1.5 million people experienced death due to TB [1]. Diabetes mellitus (DM) is recognized as one of a strong contributor of TB according to WHO [2]. Diabetes mellitus and TB co-existence has become a major health concern worldwide [3]. The presence of DM may be responsible for increasing the severity of TB disease [4]. Patients with DM are three times more susceptible to TB as compared to the normal population [3]. Diabetes mellitus is becoming more prevalent in various regions of the world [4]. The estimated global prevalence of TB-DM comorbid patients was 13.73% [5]. The WHO highlights that DM worsens treatment outcomes for TB and thus causes TB disease progression [6]. DM is responsible for extended treatment duration, lower treatment success rates [7], high risks of recurrence or relapse, drug resistance [8] and even death in TB patients [7, 9]. DM accounts for approximately 11% of deaths in TB patients worldwide [10]. Controlling TB-DM comorbid conditions can enhance TB treatment success rates by reducing the risk of TB treatment prolongation, death, TB recurrence and drug resistance. It can also reduce the risk of complications caused by DM comorbidity in TB patients, thus improving patient quality of life [11]. Due to the presence of DM in TB patients, TB treatment has become a challenge [12].
The WHO and the International Union Against TB and Lung Disease (IUATLD) framework aims to reduce the dual burden of TB and DM in affected populations through mutual efforts and developing effective treatment approaches [13]. Thus, the Directly Observed Treatment-Short Course (DOTS) Programme was introduced by WHO in 1993 and implemented in 187 countries in 2005 [14]. Approximately, 4.9 million TB patients were treated under the DOTS Programme during the implementation year [14]. It makes sure that patients adhere to their medications and aims to enhance TB treatment success rates [15]. The DOTS strategy includes a combination of four anti-TB drugs (isoniazid, pyrazinamide, ethambutol and rifampicin) for a period of six months to completely eradicate the TB infection [16]. The presence of DM makes TB treatment complicated and is responsible for the extended treatment duration [17]. It is suggested that the duration of TB treatment may extend from six months to nine months due to the presence of DM [17]. Thus, it is necessary that DM be confirmed earlier to prevent TB progression in TB patients [18].
Previous systematic review and meta-analysis reported the impact of DM on TB treatment results. There were following limitations present in these earlier systematic review and meta-analysis: unadjusted covariates [19], small sample size, not specifically focused on type 2 DM [20], and no specified therapy guidelines [21]. No previous review specifically assessed the impact of type 2 DM on TB patients treatment outcomes including extended treatment duration and recurrence following the DOTS Programme for TB treatment. Thus, keeping in mind the limitations of the previous systematic reviews and meta-analysis, the objective of the current meta-analysis was to identify and quantify the impact of type 2 DM on treatment outcomes of TB patients treated under the DOTS Programme.
Methodology
Search strategy and study selection
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [22]. The databases PubMed, Google Scholar, EMBASE, Web of Science and Cochrane library were searched (till June 2023) for studies reporting the DM impact on TB treatment outcomes in which the treatment regimen given to TB patients was DOTS therapy recommended by WHO guidelines and the outcomes were defined by WHO criteria. According to PICOs, the following Mesh terms were used to extract relevant articles: ‘Diabetes Mellitus’ [Mesh] OR ‘Diabetes Mellitus, Type 2’ [Mesh] AND ‘Tuberculosis’ [Mesh] OR ‘Tuberculosis, Pulmonary’ [Mesh] AND ‘TB treatment’ OR ‘TB patients without Type 2 Diabetes Mellitus’ OR ‘Treatment Outcome’ [Mesh] AND ‘Risk Factors’ [Mesh] OR ‘extended treatment duration’ OR ‘recurrence’. The references provided at the end of each included study were also searched for inclusion of relevant studies in this meta-analysis. Only English-language articles were considered.
Inclusion criteria
The studies were included in this meta-analysis based on the following PICOs criteria: (1) adult patients with diagnosis of TB, involving both TB-diabetes mellitus type 2 (DM type 2) comorbid patients and alone TB patients. (2) Research articles in which the treatment regimen given to TB patients was DOTS therapy recommended by WHO. (3) Research articles comparing DM impact on TB treatment outcomes including extended treatment duration and recurrence in TB-DM comorbid patients vs. TB patients only. (4) Research articles in which patients had their data reported on any of the following TB treatment outcomes, unsuccessful: extended treatment duration and recurrence. (5) Research articles having a prospective and retrospective cohort, cross-sectional or case-control study design. (6) Original research articles are published in English only.
Exclusion criteria
The studies were excluded from this meta-analysis: (1) if they were non-human studies, studies involving children, pregnant women and studies involving patients with any critical illness. (2) Studies involving patients using different anti-TB therapies, patients receiving any type of integrated care. (3) Studies analysing type 1 DM patients. (4) Studies analysing sputum culture conversion only. (5) Non-research articles, case reports, case series, models and editorials. (6) Studies for which no full text was available and studies other than English language.
The articles were reviewed on the basis of inclusion and exclusion criteria by two reviewers independently. The third reviewer reviewed the extracted data. Conflicts, if any, were then resolved through discussion with a fourth reviewer, if needed.
Data extraction and quality assessment
The data that were extracted from the included studies by two reviewers independently in a data extraction form are as follows: author name, country, publication year of the study, study design, study duration, sample size (TB patients, TB-DM patients), covariates and TB treatment outcome assessed. The data extraction form was then reviewed and verified by a third reviewer, and conflicts were discussed with a fourth reviewer and sorted out for consensus until a final decision was taken. The summaries of the included studies are provided in Table 1. The quality of the studies included in this meta-analysis was checked individually by using the Newcastle-Ottawa Scale (NOS) [63]. The NOS examines potential bias in three different domains: selection of study groups (four points), group comparability (two points) and outcome assessment (three points), assigning greater points for a lower likelihood of bias in each of these domains, up to a maximum of nine points. A score of six or greater indicated less bias and high study quality.
Table 1.
Summaries of the included studies.
| Reference | Country | Research design | Study duration | TB patients | TB-DM comorbid patients | Inclusion criteria | Covariates | Unsuccessful treatment outcomes assessed |
|---|---|---|---|---|---|---|---|---|
| Adane et al. [2] | Ethiopia | Prospective | 2020–2021 | 267 | 24 | Patients on first-line anti-TB treatment | Age, BMI, gender, smoking, alcohol | Extended treatment duration |
| Chang et al. [23] | Taiwan | Prospective | 2004–2005 | 192 | 60 | Patients followed treatment recommendations | NR | Extended treatment duration |
| Eksombatchai et al. [1] | South Korea | Retrospective | 2017–2020 | 199,571 | 47,952 | TB patients who completed TB treatment successfully | Age, region, household income, nationality, TB lesions, previous TB history, AFB smear, disability, CCI scores | Recurrence |
| Viswanathan et al. [24] | India | Retrospective | NR | 245 | 96 | TB-DM comorbid patients for analysis | NR | Extended treatment duration |
| Satung et al. [25] | Thailand | Retrospective | 2010–2012 | 7805 | 555 | Patients who were smear positive before treatment | Age, sex, occupation, comorbidity, sputum smear, DM | Extended treatment duration |
| Alisjahbana et al. [26] | Indonesia | Prospective | 2000–2005 | 634 | 94 | TB-DM comorbid patients | NR | Extended treatment duration |
| Ghanta et al. [27] | India | Prospective | NR | 100 | 50 | TB-DM comorbid patients | NR | Extended treatment duration |
| Jiménez-Corona et al. [28] | Mexico | Prospective | 1995–2010 | 1262 | 374 | TB-DM comorbid patients | Gender, smoking, HIV infection, BMI | Extended treatment duration, recurrence |
| Yoon et al. [29] | South Korea | Prospective | 2012–2014 | 661 | 157 | TB-DM comorbid patients with age ≥ 18 years | Age, BMI, smoking, DM status, presence of comorbidity, sputum positive smear | Extended treatment duration |
| Prakash [30] | India | Retrospective | NR | 160 | 80 | TB-DM comorbid patients with age ≥ 18 years | NR | Extended treatment duration |
| Kang et al. [31] | South Korea | Retrospective | 2000–2002 | 1407 | 239 | MDR-TB patients | NR | Extended treatment duration |
| Siddiqui et al. [32] | India | Prospective | 2014 | 316 | 50 | TB patients with age more than 15 years and receiving DOTS therapy | Age, gender, BMI, TB history, clinical presentation | Extended treatment duration |
| Barss et al. [33] | Canada | Retrospective | 2007–2012 | 690 | 136 | Patients with age ≥18 years, appropriate clinical charts | Age, ethnicity, immunocompromised state | Extended treatment duration, recurrence |
| Delgado-Sánchez et al. [34] | Mexico | Retrospective | 2000–2012 | 181,378 | 34,988 | TB patients with age ≥20 years | Age, gender, previous TB treatment, malnutrition | Extended treatment duration |
| Ayeni et al. [35] | Nigeria | Retrospective | 2011–2012 | 424 | 36 | Patients with age >18 years | NR | Extended treatment duration |
| Kornfeld et al. [36] | India | Prospective | 2014–2018 | 389 | 256 | Pulmonary TB patients with age 25–60 years | Age, gender, height, smoking, income, alcohol intake | Extended treatment duration |
| Gil-Santana et al. [37] | Brazil | Retrospective | 2004–2010 | 244 | 128 | TB-DM comorbid patients and TB-non-DM patients with age ≥ 18 years | Age, gender | Extended treatment duration |
| Magee et al. [38] | Georgia | Retrospective | 2009–2011 | 1349 | 72 | Patients with age ≥18 years, patients with confirmed MDR-TB | Age, gender, BMI, smoking, alcohol, HIV, previous TB treatment, cavitary disease, disseminated TB | Extended treatment duration |
| Mukhtar and Butt [39] | Pakistan | Prospective | NR | 614 | 113 | Patients with age ≥15 years, no prior intake of ATT | Age, smoking, BMI, area of residence | Extended treatment duration |
| Chiang et al. [40] | Taiwan | Retrospective | 2005–2010 | 1473 | 705 | Culture positivity in TB patients, patients with DM history | Age, gender, sputum smear, drug resistance, smoking | Extended treatment duration |
| Magee et al. [41] | Georgia | Prospective | 2011–2014 | 318 | 37 | Patients with age 7–35 years, new TB cases, HbA1c tested, eligible for standard treatment | Age, gender, HIV infection, smoking | Extended treatment duration |
| Muñoz-Torrico et al. [42] | Mexico | Retrospective | 2010–2015 | 90 | 49 | MDR-TB and XDR-TB patients | NR | Extended treatment duration |
| Perez-Navarro et al. [43] | Mexico | Prospective | 2006–2014 | 507 | 183 | Patients with MDR-TB, prior DM diagnosis | Age, gender, overcrowding, smoking | Extended treatment duration, recurrence |
| Sembiah et al. [44] | India | Prospective | 2014–2017 | 662 | 82 | Adult patients with age ≥18 years | NR | Extended treatment duration |
| Arriaga et al. [45] | Brazil | Prospective | 2015–2019 | 643 | 107 | Patients with pulmonary TB, age ≥18 years, treatment completion | Age, gender, alcohol, HIV infection, smoking | Extended treatment duration |
| Sulaiman et al. [46] | Malaysia | Retrospective | 2006–2007 | 1267 | 338 | Registered TB patients | NR | Extended treatment duration, Recurrence |
| Rout et al. [47] | India | Case control | 2019–2020 | 120 | 60 | Patients with age 18–64, received treatment | NR | Extended treatment duration |
| Leung et al. [17] | China | Prospective | 2006–2010 | 21,414 | 3331 | Patients treated at clinics | Age, gender, ethnicity, residence, employment, alcohol, smoking, HIV, previous TB treatment | Recurrence |
| Sahakyan et al. [48] | Armenia | Retrospective | 2013–2014 | 621 | 36 | adult TB patients | Weight, sputum smear | Extended treatment duration |
| Lee et al. [49] | South Korea | Retrospective | 2010–2012 | 1044 | 252 | Patients with age >30 years, diagnosed pulmonary TB | NR | Extended treatment duration, recurrence |
| Haile Workneh et al. [50] | Ethiopia | Prospective | 2013–2015 | 1314 | 109 | TB patients with age ≥15 years, completed TB treatment | Age, gender, BMI, HIV infection area of residence, adherence to TB treatment | Extended treatment duration |
| You et al. [51] | China | Retrospective | 2017 | 89,788 | 335 | TB-DM patients, age ≥18 years | NR | Extended treatment duration |
| Hongguang et al. [52] | China | Prospective | 2010–2011 | 1126 | 182 | Patients with confirmed PTB diagnosis | NR | Extended treatment duration, recurrence |
| Wang et al. [7] | Taiwan | Retrospective | 2003–2006 | 217 | 74 | Patients with diagnosed and confirmed pulmonary TB | Age, gender | Extended treatment duration |
| Mahato et al. [53] | Nepal | Prospective | NR | 408 | 102 | Patients with diagnosed TB, undergoing TB treatment | Age, employment, history of TB | Extended treatment duration |
| Lin et al. [54] | China | Prospective | 2015–201 | 306 | 128 | Patients with age ≥18 years, diagnosed TB | Age | Extended treatment duration |
| Wu et al. [55] | China | Retrospective | 2007–2008 | 201 | 40 | Pulmonary TB patients, residents | Age, gender, smoking history, pulmonary cavities, sputum smear status and TB treatment duration. | Extended treatment duration, recurrence |
| Mi et al. [56] | China | Retrospective | 2011–2012 | 1589 | 189 | Patients with diagnosed TB | Age, previous TB treatment | Extended treatment duration |
| Nandakumar et al. [57] | India | Retrospective | 2010–2011 | 3116 | 667 | Adult TB patients received DOTS therapy thrice-weekly | Age, gender, site and type of TB, smear status, HIV infection | Extended treatment duration |
| Mave et al. [58] | India | Prospective | 2013–2019 | 574 | 225 | Patients with age ≥18 years, confirmed pulmonary TB and DM | Age, gender, employment status, smoking, alcohol, BMI, smear status | Extended treatment duration, recurrence |
| Choi et al. [59] | Nigeria | Retrospective | 2014–2016 | 1000 | 200 | Diagnosed TB patients | Age, gender, HIV status, smoking | Extended treatment duration |
| Xhardo et al. [60] | Albania | Cross-sectional | 2018–2019 | 140 | 13 | Patients with diagnosed TB | Age, gender, BMI, smoking, alcohol, HIV status | Extended treatment duration |
| Baltas et al. [61] | UK | Retrospective | NR | 838 | 126 | Diagnosed TB patients | Age, gender, ethnicity, BMI, smoking, alcohol, comorbidities, previous TB treatment | Extended treatment duration |
| Tok et al. [62] | Malaysia | Retrospective | 2014–2017 | 97,505 | 2464 | Registered TB patients | Age, gender, education, residence, HIV, comorbidities | Extended treatment duration |
ATT: anti-tuberculosis treatment; BMI; body mass index; CCI: Charlson Comorbidity Index; DOTS: Directly Observed Treatment-Short Course; HIV: human immunodeficiency virus; ICD: international classification of diseases; MDR-TB: multi-drug resistant tuberculosis; NR: not reported; PTB: pulmonary tuberculosis; WHO: World Health Organization; XDR-TB: extensively drug-resistant tuberculosis.
TB treatment outcomes
The TB treatment outcomes analysed in this study were categorized by WHO criteria. The outcomes analysed in this study were unsuccessful outcomes (extended treatment duration and recurrence). Since studies used different meanings for recurrence and relapse, we considered them as one-recurrence [64]. TB treatment outcomes were defined as extended treatment duration (TB patients with positive sputum culture results even after the fifth month of treatment or later or TB treatment failure patients with progression and worsening of infection in TB patients despite following the prescribed treatment protocol) and recurrence (TB symptoms reappear in TB patients after treatment, even if the patient was cured before) [64].
Statistical analysis
Multivariable logistic regression results for TB unsuccessful treatment outcomes (extended treatment duration and recurrence) were preferably extracted. For pooling the estimates of DM impact on TB treatment outcomes, a fixed-effects model was used to calculate pooled hazards ratio (HR 95% CI). Heterogeneity was assessed between studies using I2 statistics. The studies reported higher heterogeneity if I2 values were greater than 50%. For TB treatment outcomes, the forest plots were also constructed. All analysis were conducted through licensed Statistical software package Stata V.16 (Stata Corp, College Station, TX).
Results
Search results
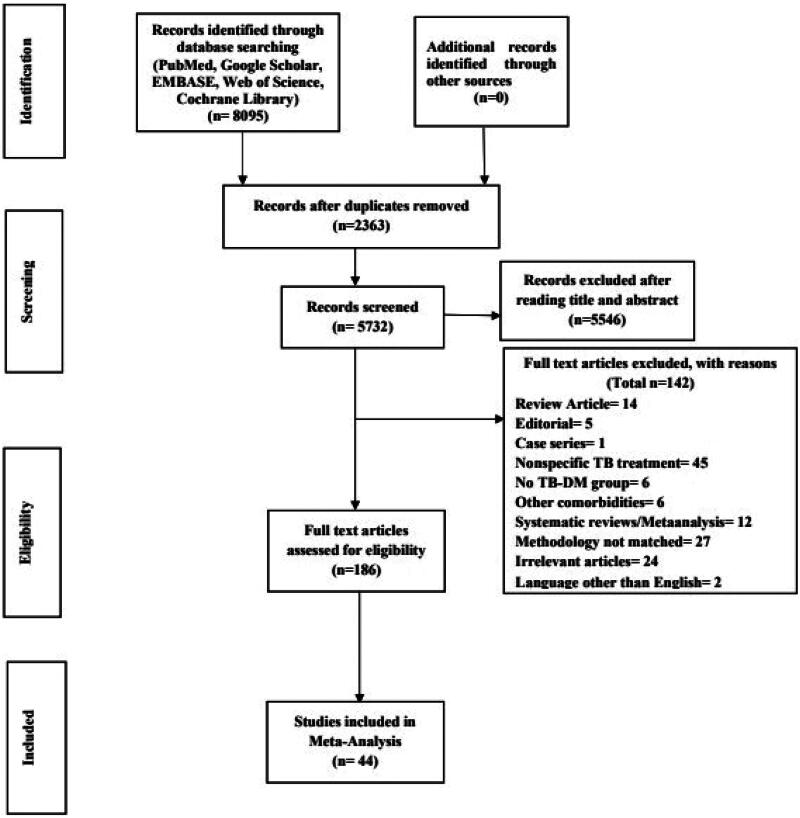
The databases searched a total of 8095 studies. After the removal of 2363 duplicates, 5732 articles were eligible for screening. After thoroughly screening the titles and abstracts, 186 studies were selected for full-text reading. The full text was not available for three studies, even after contacting the authors. A total of 44 studies were selected for inclusion in this meta-analysis. The search strategy is given in Figure 1.
Figure 1.
Study selection process in line with the PRISMA guidelines.
Study characteristics
Out of 49 studies included in this meta-analysis, nine studies were from India [24, 27, 30, 32, 36, 44, 47, 57,58], four from South Korea [1, 29, 31, 49], three from Taiwan [7, 23, 40], two from Ethiopia [2, 50], four from Mexico [28, 34, 42,43], six from China [17, 51,52, 54–56], one from Thailand [25], two from Malaysia [46, 62], two from Nigeria [35, 59], two from Brazil [37, 45], two from Georgia [38, 41] and one each from Indonesia [26], Canada [33], Pakistan [39], London [61], Armenia [48], Nepal [53] and Albania [60]. Among these, the study design of 23 studies was retrospective cohort, 19 studies were prospective, one study was a cross-sectional study and one study was a case-control study. The sample size for TB patients ranged from 90 to 199,571, and for TB-DM patients, the sample size varied from 13 to 47,952. The pooled sample size for TB patients in this meta-analysis was 623,989, and for TB-DM patients, it was 95,494.
Impact of type 2 DM on TB treatment outcomes
Extended TB treatment duration
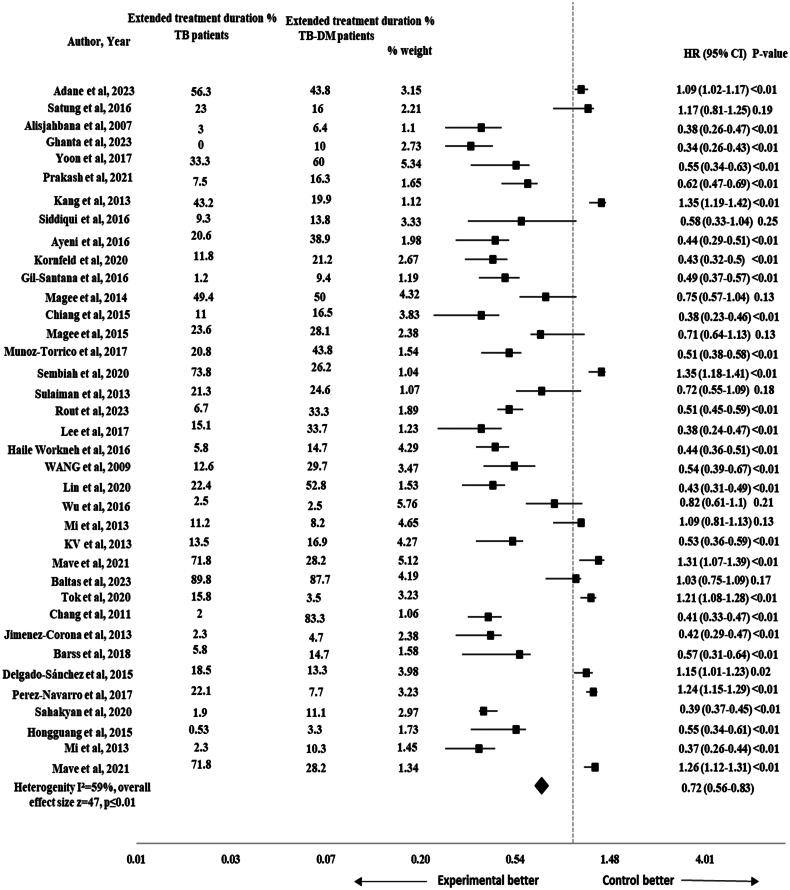
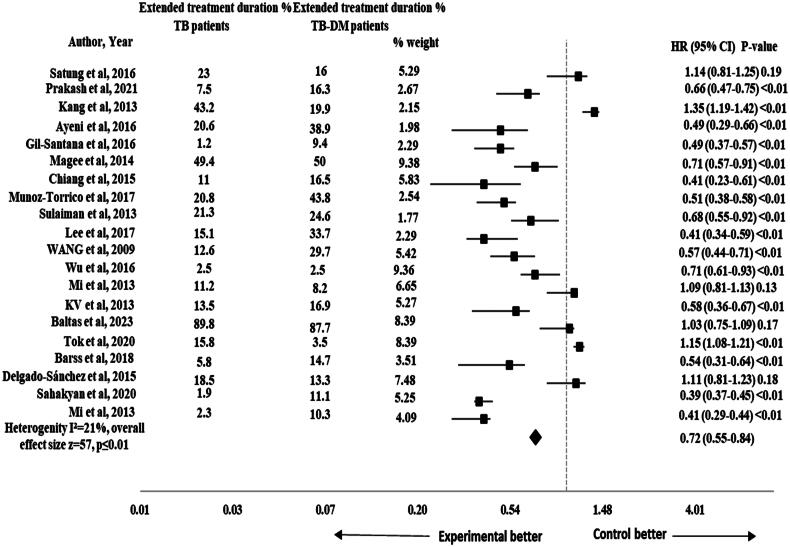
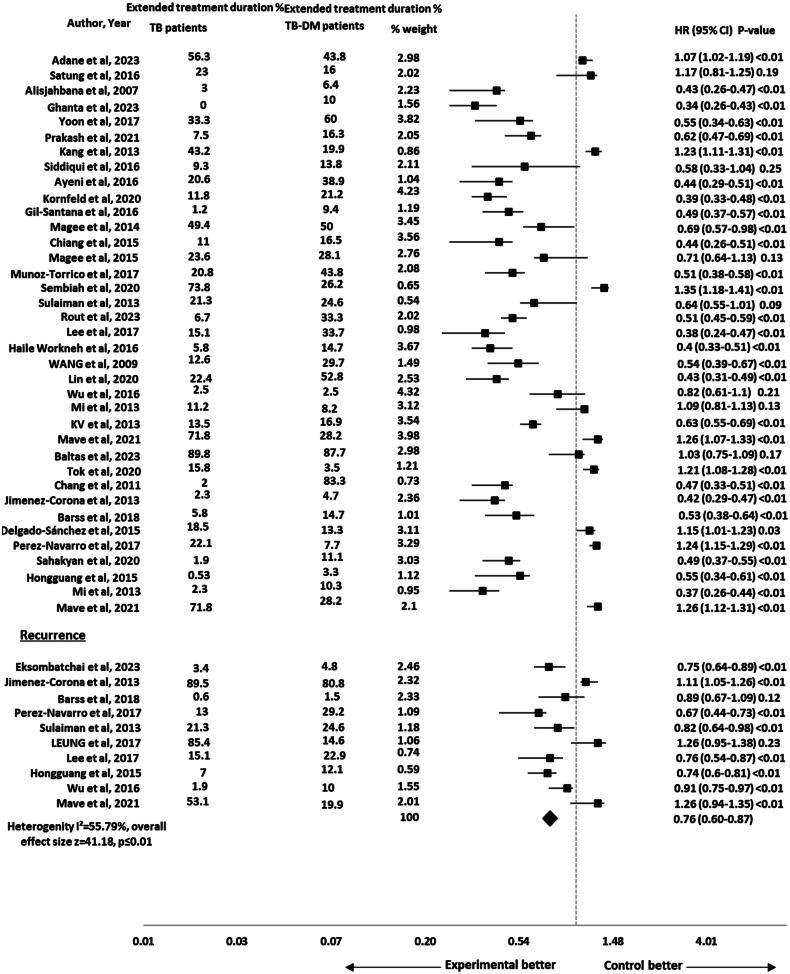
The risk of extended treatment duration was reported in 37 studies [2, 7, 23, 25–38, 40–50, 52, 54–58, 60–62]. The pooled HR for the impact of DM on extended treatment duration was significant (HR 0.72, 95% CI 0.56-0.83), p ≤ .01 with 47 effect size and moderate heterogeneity (I2 = 59%) as shown in Figure 2. The subgroup analysis was performed by study design to assess the impact of different study designs on the pooled results. The results remained significant after performing sub-group analysis for extended treatment duration by study design (HR 0.72, 95% CI 0.55–0.84), p ≤ .01 and the heterogeneity was reduced to 21% (I2 = 21%) as shown in Figure 3.
Figure 2.
Forest plot for impact of DM on extended treatment duration in TB-DM comorbid patients.
Figure 3.
Forest plot of sub-group analysis for extended treatment duration in TB-DM comorbid patients.
Recurrence
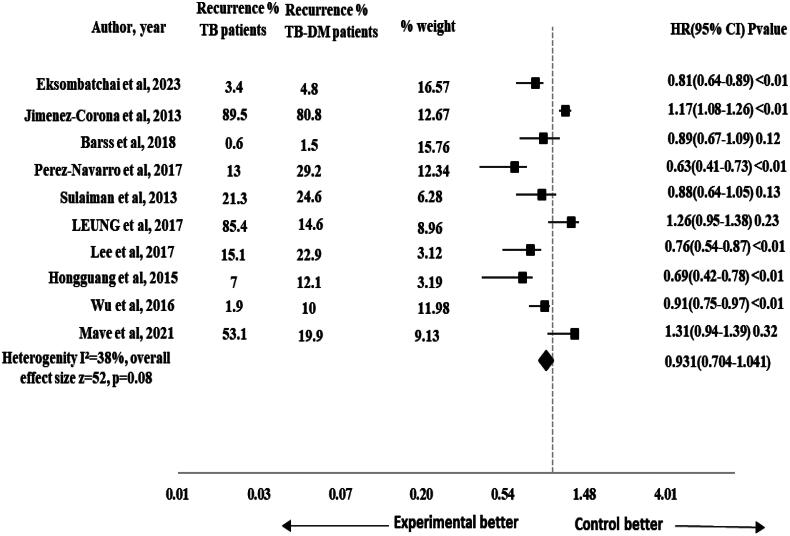
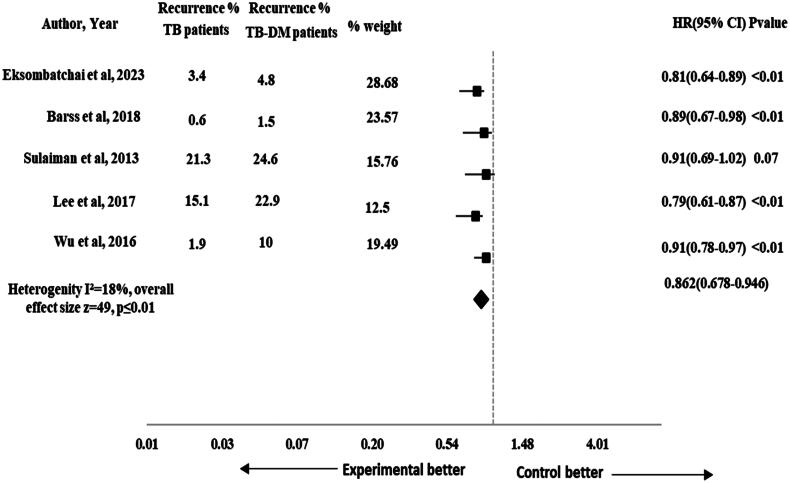
The risk of TB recurrence was reported in 10 studies [1, 17, 28, 33, 43, 46, 49, 52, 55, 58]. The pooled HR for the impact of DM on recurrence was non-significant (HR 0.931, 95% CI 0.704–1.041), p = .08 with 52 effect size. The heterogeneity observed across the studies was moderate (I2 = 38%) as shown in Figure 4. The subgroup analysis was performed by study design to assess the impact of different study designs on the pooled results. The results were significant for recurrence after performing sub-group analysis by study design (HR 0.862, 95% CI 0.678–0.946), p ≤ .01 and the heterogeneity was reduced to 18% (I2 = 18%) that showed consistent results across studies as shown in Figure 5.
Figure 4.
Forest plot for impact of DM on recurrence in TB-DM comorbid patients.
Figure 5.
Forest plot of sub-group analysis for recurrence in TB-DM comorbid patients.
Composite TB treatment outcomes
The pooled HR (95% CI) for impact of DM on composite TB treatment outcomes (extended treatment duration and reoccurrence) was calculated as 0.76 (95% CI 0.60–0.87), p ≤ .01 with an effect size of 41.18. The heterogeneity observed among the included studies was moderate (I2 = 55.79%) as shown in Figure 6.
Figure 6.
Forest plot for composite TB treatment outcomes in TB-DM comorbid patients.
Assessment of risk of bias
This meta-analysis used the NOS to evaluate the risk of bias in each individual study [63]. For studies analysing the impact of DM on TB treatment outcomes, the mean score of NOS was seven (out of a maximum of nine points), indicating the high quality of the studies included in this meta-analysis. The risk of bias in the included studies is provided in Table 2.
Table 2.
Newcastle-Ottawa Scale.
| Study | Study design | Selection | Comparability | Outcome/exposure | NOS score |
|---|---|---|---|---|---|
| Adane et al. [2], Ethiopia | Prospective | *** | ** | *** | 8 |
| Chang et al. [23], Taiwan | Prospective | *** | ** | 5 | |
| Eksombatchai et al. [1], South Korea | Retrospective | ** | * | *** | 6 |
| Viswanathan et al. [24], India | Retrospective | *** | * | ** | 6 |
| Satung et al. [25], Thailand | Retrospective | **** | ** | ** | 8 |
| Alisjahbana et al. [26], Indonesia | Prospective | *** | * | ** | 6 |
| Ghanta et al. [27], India | Prospective | *** | * | ** | 6 |
| Jiménez-Corona et al. [28], Mexico | Prospective | **** | ** | ** | 8 |
| Yoon et al. [29], South Korea | Prospective | **** | ** | * | 7 |
| Prakash [30], India | Retrospective | **** | * | * | 6 |
| Kang et al. [31], South Korea | Retrospective | **** | * | ** | 7 |
| Siddiqui et al. [32], India | Prospective | *** | ** | * | 6 |
| Barss et al. [33], Canada | Retrospective | **** | ** | * | 7 |
| Delgado-Sánchez et al. [34], Mexico | Retrospective | **** | ** | * | 7 |
| Ayeni et al. [35], Nigeria | Retrospective | **** | * | * | 6 |
| Kornfeld et al. [36], India | Prospective | *** | ** | ** | 7 |
| Gil-Santana et al. [37], Brazil | Retrospective | **** | ** | * | 7 |
| Magee et al. [38], Georgia | Retrospective | **** | ** | * | 7 |
| Mukhtar and Butt [39], Pakistan | Prospective | **** | ** | ** | 8 |
| Chiang et al. [40], Taiwan | Retrospective | **** | ** | *** | 9 |
| Magee et al. [41], Georgia | Prospective | **** | ** | *** | 9 |
| Muñoz-Torrico et al. [42], Mexico | Retrospective | **** | * | *** | 8 |
| Perez-Navarro et al. [43], Mexico | Prospective | **** | ** | *** | 9 |
| Sembiah et al. [44], India | Prospective | **** | * | *** | 8 |
| Arriaga et al. [45], Brazil | Prospective | **** | ** | *** | 9 |
| Sulaiman et al. [46], Malaysia | Retrospective | **** | * | * | 6 |
| Rout et al. [47], India | Case control | *** | * | * | 5 |
| Leung et al. [17], China | Prospective | **** | ** | *** | 9 |
| Sahakyan et al. [48], Armenia | Retrospective | **** | ** | * | 7 |
| Lee et al. [49], South Korea | Retrospective | **** | * | * | 6 |
| Haile Workneh et al. [50], Ethiopia | Prospective | **** | ** | ** | 8 |
| You et al. [51], China | Retrospective | **** | * | * | 6 |
| Hongguang et al. [52], China | Prospective | **** | * | * | 6 |
| Wang et al. [7], Taiwan | Retrospective | **** | ** | * | 7 |
| Mahato et al. [53], Nepal | Prospective | **** | ** | ** | 8 |
| Lin et al. [54], China | Prospective | *** | ** | * | 6 |
| Wu et al. [55], China | Retrospective | **** | ** | * | 7 |
| Mi et al. [56], China | Retrospective | **** | ** | ** | 8 |
| Nandakumar et al. [57], India | Retrospective | **** | ** | *** | 9 |
| Mave et al. [58], India | Prospective | **** | ** | ** | 8 |
| Choi et al. [59], Nigeria | Retrospective | **** | ** | *** | 9 |
| Xhardo et al. [60], Albania | Cross-sectional | **** | ** | * | 7 |
| Baltas et al. [61], London | Retrospective | **** | ** | *** | 9 |
| Tok et al. [62], Malaysia | Retrospective | **** | ** | *** | 9 |
Each asterisk (*) represents a point that contributes to the overall quality score of the study. One * means one point.
Discussion
This study conducted a meta-analysis to examine the impact of type 2 DM on TB treatment outcomes in pulmonary TB-DM comorbid patients. The analysis extensively reviewed articles specifically focusing on patients with TB treatment outcomes including extended treatment duration and recurrence who were given treatment following the DOTS therapy recommended by the WHO. Our findings explored that DM negatively influenced TB treatment outcomes. TB-non-DM patients had a lower risk of extended treatment duration and TB recurrence when compared with TB-DM comorbid patients.
This meta-analysis showed a significantly lower risk for extended treatment duration in TB-non-DM comorbid patients as compared to TB-DM patients (HR 0.72, 95% CI 0.56–0.83), p = .01 with moderate heterogeneity (I2 = 59%) across the studies. After performing sub-group analysis by study design, the risk for extended treatment duration remained lower in TB-non-DM comorbid patients as compared to TB-DM patients (HR 0.72, 95% CI 0.55–0.84), p = .01. The results were also found to be significant in previous study and systematic review [19, 21, 65]. But the results were inconsistent with previous studies that reported non-significant results [66–68]. The study’s small sample size could result in insufficient statistical power to detect minor differences. Statistical variability may also introduce uncertainty, contributing to non-significant results. Patient characteristics (age, gender, disease state) and healthcare system disparities could mask DM effects on treatment outcomes. Uncontrolled factors like socioeconomic status, healthcare access and adherence might complicate interpretation. These considerations highlight the diverse complexity of the results and suggest that the combined influence of these factors contributed to the non-significant relationship between DM and extended treatment duration in TB-DM comorbid patients [19].
Limitations in their study design or methodology might have affected their ability to detect a significant impact of DM on treatment prolongation. The study’s sample size and the characteristics of the patient population might not have been adjusted for detecting such an association. Similarly, another study might have had challenges related to patient enrolment, data collection or the duration of follow-up, potentially affecting their ability to identify a significant effect [38]. Additionally, the extended 5-year follow-up period in another study [61] reported confounding variables such as changes in treatment protocols, access to healthcare, or the presence of other comorbidities, which could make it challenging to clearly understand the association between DM and treatment prolongation. These factors highlight the need for accurate research design and interpretation when studying complex health outcomes, in order to obtain significant results.
Our study showed non-significant results for recurrence (HR 0.93, 95% CI 0.70–1.04), p = .08. The results were comparable with a previous study that reported no statistically significant impact of DM on recurrence in TB-DM comorbid patients [69]. On sub-group analysis by study design, the results were significant for recurrence (HR 0.86, 95% CI 0.67–0.94), p < .01. It showed that TB-non-DM patients were at lower risk of recurrence when compared with TB-DM comorbid patients. The previous systematic review and meta-analysis also reported a significant DM impact on recurrence in TB-DM comorbid patients [21, 70,71]. DM weakens the immune system of TB patients, making them more susceptible to TB infection. The pooled HR (95% CI) for impact of DM on composite TB treatment outcomes was 0.76 (95% CI 0.60–0.87), p = .01 in our study. Such disparities highlight the need for cautious interpretation. Due to the presence of type 2 DM, the cell-mediated immune functions are compromised in TB patients [72]. The type 2 DM if left uncontrolled can also impair the cytokine functions and disrupts type 1 cytokines responses [73]. The factors can contribute to unfavourable TB treatment outcomes including death, TB treatment prolongation and TB recurrence emphasizing the importance of future research for a more comprehensive understanding of the TB-DM comorbidity’s effect on TB treatment outcome including recurrence and TB treatment prolongation.
When comparing the results of this meta-analysis with previous research, it is noted that different studies have shown both significant and insignificant effects of DM on TB treatment results. These differences were discussed considering the limitations of the studies, like sample size, patient characteristics, methodological differences and uncontrolled factors. Still, despite these differences, the main findings of this study have given us a valuable understanding of how DM affects TB treatment outcomes, confirming the harmful impact of DM on different aspects of TB treatment. The strengths of this meta-analysis lie in its comprehensive analysis of a significant number of studies, focusing on a specific patient population treated under DOTS therapy. We focused on specific subtypes of DM and TB, providing a more refined understanding of their interaction. However, our study also had several limitations. We included relevant studies from different geographical regions by searching and reviewing the existing literature. There may be the possibility of publication bias, despite our efforts to include a comprehensive set of studies. The biasness may arise from underreporting of negative results or exclusion of studies with negative results leading to potential emphasis on significant findings only and such bias could affect the overall findings of our study. The method of diagnosis for type 2 DM was different in different studies. There was misclassification in the diagnosis of type 2 DM that can affect the results in examining the association between type 2 DM and TB. The glucose levels are increased temporarily during TB but some studies did not emphasize that either DM was diagnosed before TB or during TB or patients can be diagnosed as type 2 DM on the basis of short-term elevation of blood glucose levels. This factor can also impact our findings. The use of statistical methods for controlling diversity in the study designs can make the results unclear.
For future concern, this study highlights the importance of conducting more thorough research with large groups of people, using consistent methods, type 2 DM diagnosis and considering other variables that might affect the results. This would help gain a better understanding of how type 2 DM affects TB treatment outcomes.
Conclusions
A negative impact of DM was found on recurrence and extended treatment duration in TB patients treated with DOTS therapy. Diabetes mellitus type 2 is responsible for the TB treatment prolongation and TB recurrence rates. By implementing effective management strategies and advancing research, the challenges can be mitigated arising due to the complex interaction between DM and TB.
Funding Statement
No funding was received.
Author contributions
M.K., A.R. and T.M.; methodology, M.K., A.R. and M.S.A., software, R.H. and Z.S.; validation, M.F.R., S.A.A. and M.S.A.; formal analysis, A.R., M.K. and A.H.; resources, A.R. and A.H.; data curation, M.K., S.Z.F. and M.F.N.; writing-original draft preparation, M.K., A.R., A.H. and M.S.A.; writing-review and editing, O.M.A., A.A.B., S.A.A. and H.M.A., Z.S.; supervision, A.R. All authors have read and agreed to the published version of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available on request from the corresponding author.
References
- 1.Eksombatchai D, Jeong D, Mok J, et al. Sex differences in the impact of diabetes mellitus on tuberculosis recurrence: a retrospective national cohort study. Int J Infect Dis. 2023;127:1–15. doi: 10.1016/j.ijid.2022.11.037. [DOI] [PubMed] [Google Scholar]
- 2.Adane HT, Howe RC, Wassie L, et al. Diabetes mellitus is associated with an increased risk of unsuccessful treatment outcomes among drug-susceptible tuberculosis patients in Ethiopia: a prospective health facility-based study. J Clin Tuberc Other Mycobact Dis. 2023;31:100368. doi: 10.1016/j.jctube.2023.100368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Amri S, Singh J, Al Balushi L, et al. Prevalence and associated factors of diabetes mellitus type 2 among tuberculosis patients in Muscat, Oman, 2017–2020. Oman Med J. 2023;38(4):e526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shrestha N, Mishra SR, Ghimire S, et al. Burden of diabetes and prediabetes in Nepal: a systematic review and meta-analysis. Diabetes Ther. 2020;11(9):1935–1946. doi: 10.1007/s13300-020-00884-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li M, Chen T, Hua Z, et al. Global, regional, and national prevalence of diabetes mellitus in patients with pulmonary tuberculosis: a systematic review and meta-analysis. Diabetol Metab Syndr. 2021;13(1):127. doi: 10.1186/s13098-021-00743-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Global Tuberculosis Report . Geneva: World Health Organization; 2020. Licence: CC by-NC-SA 3.0 IGO. Geneva, Switzerland: WHO; 2021. [Google Scholar]
- 7.Wang CS, Yang CJ, Chen HC, et al. Impact of type 2 diabetes on manifestations and treatment outcome of pulmonary tuberculosis. Epidemiol Infect. 2009;137(2):203–210. doi: 10.1017/S0950268808000782. [DOI] [PubMed] [Google Scholar]
- 8.Yuan B, Du J, Lan X, et al. Effect of type 2 diabetes mellitus on sputum negative conversion and treatment effects of multi-drug-resistant tuberculosis. Biomed Res. 2017;28(9):3917–3922. [Google Scholar]
- 9.Shewade HD, Jeyashree K, Mahajan P, et al. Effect of glycemic control and type of diabetes treatment on unsuccessful TB treatment outcomes among people with TB-diabetes: a systematic review. PLOS One. 2017;12(10):e0186697. doi: 10.1371/journal.pone.0186697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kyu HH, Maddison ER, Henry NJ, et al. The global burden of tuberculosis: results from the Global Burden of Disease Study 2015. Lancet Infect Dis. 2018;18(3):261–284. doi: 10.1016/S1473-3099(17)30703-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anyanwu MO, Ajumobi OO, Afolabi NB, et al. Diabetes mellitus and its associated factors among patients with tuberculosis attending directly observed treatment centres in Oyo State, Nigeria: a cross-sectional evaluation. BMJ Open. 2022;12(4):e059260. doi: 10.1136/bmjopen-2021-059260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization . Collaborative framework for care and control of tuberculosis and diabetes. Geneva (Switzerland): World Health Organization; 2011. [PubMed] [Google Scholar]
- 13.Ayeni FA, Oyetunde OO, Aina BA.. The effect of collaborative care on treatment outcomes of newly diagnosed tuberculosis patients with type-2 diabetes mellitus and adverse drug reaction presentations: a prospective study. Int J Mycobacteriol. 2021;10(3):285–292. doi: 10.4103/ijmy.ijmy_124_21. [DOI] [PubMed] [Google Scholar]
- 14.Moosazade M, Jamshidi M, Amiresmaili M, et al. A comparison of directly observed therapy and self-administered therapy strategies in treatment of pulmonary tuberculosis: a cohort study in North of Iran. Middle East J Sci Res. 2012;11(7):873–880. [Google Scholar]
- 15.Broekmans JF, Migliori GB, Rieder HL, et al. European framework for tuberculosis control and elimination in countries with a low incidence. Recommendations of the World Health Organization (WHO), International Union against Tuberculosis and Lung Disease (IUATLD) and Royal Netherlands Tuberculosis Association (KNCV) Working Group. Eur Respir J. 2002;19(4):765–775. doi: 10.1183/09031936.02.00261402. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization and S.T. Initiative . Treatment of tuberculosis: guidelines. Geneva (Switzerland): World Health Organization; 2010. [Google Scholar]
- 17.Leung CC, Yew WW, Mok TYW, et al. Effects of diabetes mellitus on the clinical presentation and treatment response in tuberculosis. Respirology. 2017;22(6):1225–1232. doi: 10.1111/resp.13017. [DOI] [PubMed] [Google Scholar]
- 18.Jeon CY, Harries AD, Baker MA, et al. Bi‐directional screening for tuberculosis and diabetes: a systematic review. Trop Med Int Health. 2010;15(11):1300–1314. doi: 10.1111/j.1365-3156.2010.02632.x. [DOI] [PubMed] [Google Scholar]
- 19.Baker MA, Harries AD, Jeon CY, et al. The impact of diabetes on tuberculosis treatment outcomes: a systematic review. BMC Med. 2011;9(1):81. doi: 10.1186/1741-7015-9-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huangfu P, Ugarte-Gil C, Golub J, et al. The effects of diabetes on tuberculosis treatment outcomes: an updated systematic review and meta-analysis. Int J Tuberc Lung Dis. 2019;23(7):783–796. doi: 10.5588/ijtld.18.0433. [DOI] [PubMed] [Google Scholar]
- 21.Han X, Wang Q, Wang Y, et al. The impact of diabetes on tuberculosis treatment outcomes: evidence based on a cumulative meta-analysis. Int J Diabetes Dev Ctries. 2016;36(4):490–507. doi: 10.1007/s13410-016-0514-5. [DOI] [Google Scholar]
- 22.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang J-T, Dou H-Y, Yen C-L, et al. Effect of type 2 diabetes mellitus on the clinical severity and treatment outcome in patients with pulmonary tuberculosis: a potential role in the emergence of multidrug-resistance. J Formos Med Assoc. 2011;110(6):372–381. doi: 10.1016/S0929-6646(11)60055-7. [DOI] [PubMed] [Google Scholar]
- 24.Viswanathan V, Vigneswari A, Selvan K, et al. Effect of diabetes on treatment outcome of smear-positive pulmonary tuberculosis—a report from South India. J Diabetes Complicat. 2014;28(2):162–165. doi: 10.1016/j.jdiacomp.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Satung J, Kaewkungwal J, Silachamroon U, et al. Treatment outcomes among diabetic patients with tuberculosis in Thailand. Southeast Asian J Trop Med Public Health. 2016;47(6):1209–1220. [PubMed] [Google Scholar]
- 26.Alisjahbana B, Sahiratmadja E, Nelwan EJ, et al. The effect of type 2 diabetes mellitus on the presentation and treatment response of pulmonary tuberculosis. Clin Infect Dis. 2007;45(4):428–435. doi: 10.1086/519841. [DOI] [PubMed] [Google Scholar]
- 27.Ghanta J, Panja B, Goswami D, et al. The effect of diabetes mellitus on the treatment outcome of tuberculosis. Indian J Public Health Res Dev. 2023;14(2):107–114. [Google Scholar]
- 28.Jiménez-Corona ME, Cruz-Hervert LP, García-García L, et al. Association of diabetes and tuberculosis: impact on treatment and post-treatment outcomes. Thorax. 2013;68(3):214–220. doi: 10.1136/thoraxjnl-2012-201756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoon YS, Jung J-W, Jeon EJ, et al. The effect of diabetes control status on treatment response in pulmonary tuberculosis: a prospective study. Thorax. 2017;72(3):263–270. doi: 10.1136/thoraxjnl-2015-207686. [DOI] [PubMed] [Google Scholar]
- 30.Prakash V. Impact of type 2 diabetes on manifestations of pulmonary tuberculosis and its treatment outcome. Roman J Diabetes Nutr Metab Dis. 2021;28(4):430–436. [Google Scholar]
- 31.Kang YA, Kim SY, Jo K-W, et al. Impact of diabetes on treatment outcomes and long-term survival in multidrug-resistant tuberculosis. Respiration. 2013;86(6):472–478. doi: 10.1159/000348374. [DOI] [PubMed] [Google Scholar]
- 32.Siddiqui AN, Khayyam KU, Sharma M.. Effect of diabetes mellitus on tuberculosis treatment outcome and adverse reactions in patients receiving directly observed treatment strategy in India: a prospective study. Biomed Res Int. 2016;2016:7273935. doi: 10.1155/2016/7273935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barss L, Sabur N, Orlikow E, et al. Diabetes mellitus in adult patients with active tuberculosis in Canada: presentation and treatment outcomes. Can J Respir Crit Care Sleep Med. 2019;3(2):84–90. doi: 10.1080/24745332.2018.1507615. [DOI] [Google Scholar]
- 34.Delgado-Sánchez G, García-García L, Castellanos-Joya M, et al. Association of pulmonary tuberculosis and diabetes in Mexico: analysis of the National Tuberculosis Registry 2000–2012. PLOS One. 2015;10(6):e0129312. doi: 10.1371/journal.pone.0129312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ayeni F, Aina B, Oyetunde O, et al. Associated factors and treatment outcomes of tuberculosis patients with diabetes mellitus in a secondary health facility in Lagos Nigeria. West Afr J Pharm. 2016;27(1):1–9. [Google Scholar]
- 36.Kornfeld H, Sahukar SB, Procter-Gray E, et al. Impact of diabetes and low body mass index on tuberculosis treatment outcomes. Clin Infect Dis. 2020;71(9):e392–e398. doi: 10.1093/cid/ciaa054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gil-Santana L, Almeida-Junior JL, Oliveira CAM, et al. Diabetes is associated with worse clinical presentation in tuberculosis patients from Brazil: a retrospective cohort study. PLOS One. 2016;11(1):e0146876. doi: 10.1371/journal.pone.0146876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Magee MJ, Kempker RR, Kipiani M, et al. Diabetes mellitus, smoking status, and rate of sputum culture conversion in patients with multidrug-resistant tuberculosis: a cohort study from the country of Georgia. PLOS One. 2014;9(4):e94890. doi: 10.1371/journal.pone.0094890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mukhtar F, Butt ZA.. Risk of adverse treatment outcomes among new pulmonary TB patients co-infected with diabetes in Pakistan: a prospective cohort study. PLOS One. 2018;13(11):e0207148. doi: 10.1371/journal.pone.0207148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chiang CY, Bai KJ, Lin HH, et al. The influence of diabetes, glycemic control, and diabetes-related comorbidities on pulmonary tuberculosis. PLOS One. 2015;10(3):e0121698. doi: 10.1371/journal.pone.0121698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Magee MJ, Kempker RR, Kipiani M, et al. Diabetes mellitus is associated with cavities, smear grade, and multidrug-resistant tuberculosis in Georgia. Int J Tuberc Lung Dis. 2015;19(6):685–692. doi: 10.5588/ijtld.14.0811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muñoz-Torrico M, Caminero-Luna J, Migliori GB, et al. Diabetes is associated with severe adverse events in multidrug-resistant tuberculosis. Arch Bronconeumol. 2017;53(5):245–250. doi: 10.1016/j.arbr.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 43.Perez-Navarro LM, Restrepo BI, Fuentes-Dominguez FJ, et al. The effect size of type 2 diabetes mellitus on tuberculosis drug resistance and adverse treatment outcomes. Tuberculosis. 2017;103:83–91. doi: 10.1016/j.tube.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 44.Sembiah S, Nagar V, Gour D, et al. Diabetes in tuberculosis patients: an emerging public health concern and the determinants and impact on treatment outcome. J Family Community Med. 2020;27(2):91–96. doi: 10.4103/jfcm.JFCM_296_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arriaga MB, Araújo-Pereira M, Barreto-Duarte B, et al. The effect of diabetes and prediabetes on antituberculosis treatment outcomes: a multicenter prospective cohort study. J Infect Dis. 2022;225(4):617–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sulaiman SAS, Khan AH, Ahmad N, et al. Impact of diabetes mellitus on treatment outcomes of tuberculosis patients in tertiary care setup. Am J Med Sci. 2013;345(4):321–325. doi: 10.1097/MAJ.0b013e318288f8f3. [DOI] [PubMed] [Google Scholar]
- 47.Rout P, Jagaty S, Behera D, et al. Impact of diabetes mellitus on treatment outcome of newly diagnosed smear-positive pulmonary tuberculosis patients: a case–control study. Med J Dr D Y Patil Vidyapeeth. 2023;16(7):S47–S50. [Google Scholar]
- 48.Sahakyan S, Petrosyan V, Abrahamyan L.. Diabetes mellitus and treatment outcomes of pulmonary tuberculosis: a cohort study. Int J Public Health. 2020;65(1):37–43. doi: 10.1007/s00038-019-01277-2. [DOI] [PubMed] [Google Scholar]
- 49.Lee EH, Lee JM, Kang YA, et al. Prevalence and impact of diabetes mellitus among patients with active pulmonary tuberculosis in South Korea. Lung. 2017;195(2):209–215. doi: 10.1007/s00408-017-9978-4. [DOI] [PubMed] [Google Scholar]
- 50.Haile Workneh M, Aksel Bjune G, Abebe Yimer S.. Diabetes mellitus is associated with increased mortality during tuberculosis treatment: a prospective cohort study among tuberculosis patients in South-Eastern Amahra Region, Ethiopia. Infect Dis Poverty. 2016;5(2):22. doi: 10.1186/s40249-016-0115-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.You N, Pan H, Zeng Y, et al. A risk score for prediction of poor treatment outcomes among tuberculosis patients with diagnosed diabetes mellitus from Eastern China. Sci Rep. 2021;11(1):11219. doi: 10.1038/s41598-021-90664-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hongguang C, Min L, Shiwen J, et al. Impact of diabetes on clinical presentation and treatment outcome of pulmonary tuberculosis in Beijing. Epidemiol Infect. 2015;143(1):150–156. doi: 10.1017/S095026881400079X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mahato RK, Laohasiriwong W, Koju R. The role of diabetes mellitus comorbidity on tuberculosis treatment outcomes in Nepal: a prospective cohort study. South East Eur J Public Health. 2023. doi: 10.56801/seejph.vi.260. [DOI] [Google Scholar]
- 54.Lin Y, Bai Y, Zhang T, et al. Unfavourable treatment outcomes in tuberculosis patients with different vitamin D status and blood glucose levels in a programme setting in China. Trop Med Int Health. 2020;25(3):373–379. doi: 10.1111/tmi.13355. [DOI] [PubMed] [Google Scholar]
- 55.Wu Z, Guo J, Huang Y, et al. Diabetes mellitus in patients with pulmonary tuberculosis in an aging population in Shanghai, China: prevalence, clinical characteristics and outcomes. J Diabetes Complicat. 2016;30(2):237–241. doi: 10.1016/j.jdiacomp.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 56.Mi F, Tan S, Liang L, et al. Diabetes mellitus and tuberculosis: pattern of tuberculosis, two‐month smear conversion and treatment outcomes in Guangzhou, China. Trop Med Int Health. 2013;18(11):1379–1385. doi: 10.1111/tmi.12198. [DOI] [PubMed] [Google Scholar]
- 57.Nandakumar KV, Duraisamy K, Balakrishnan S, et al. Outcome of tuberculosis treatment in patients with diabetes mellitus treated in the revised national tuberculosis control programme in Malappuram District, Kerala, India. PLOS One. 2013;8(10):e76275. doi: 10.1371/journal.pone.0076275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mave V, Gaikwad S, Barthwal M, et al. Diabetes mellitus and tuberculosis treatment outcomes in Pune, India. Open Forum Infect Dis. 2021;8(4):ofab097. doi: 10.1093/ofid/ofab097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Choi S-I, Lee SC, Kong SJ, et al. The effect of diabetes mellitus on treatment outcomes in pulmonary tuberculosis. Korean J Med. 2003;65:558–567. [Google Scholar]
- 60.Xhardo HE, Hysenbelli B, Ylli D, et al. Prevalence and impact of diabetes mellitus in adult tuberculosis patients: a cross-sectional study. Endocr Abstr. 2023. doi: 10.1530/endoabs.90.P341. [DOI] [Google Scholar]
- 61.Baltas I, Sturdy A, Kavallieros K, et al. Diabetes mellitus is not a predictor of poor TB treatment outcomes. Int J Tuberc Lung Dis. 2023;27(2):140–145. doi: 10.5588/ijtld.22.0470. [DOI] [PubMed] [Google Scholar]
- 62.Tok PSK, Liew SM, Wong LP, et al. Determinants of unsuccessful treatment outcomes and mortality among tuberculosis patients in Malaysia: a registry-based cohort study. PLOS One. 2020;15(4):e0231986. doi: 10.1371/journal.pone.0231986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alebel A, Wondemagegn AT, Tesema C, et al. Prevalence of diabetes mellitus among tuberculosis patients in sub-Saharan Africa: a systematic review and meta-analysis of observational studies. BMC Infect Dis. 2019;19(1):254. doi: 10.1186/s12879-019-3892-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.World Health Organization . Definitions and reporting framework for tuberculosis – 2013 revision: updated December 2014 and January 2020. Geneva (Switzerland): World Health Organization; 2013. [Google Scholar]
- 65.Ruslami R, Aarnoutse RE, Alisjahbana B, et al. Implications of the global increase of diabetes for tuberculosis control and patient care. Trop Med Int Health. 2010;15(11):1289–1299. doi: 10.1111/j.1365-3156.2010.02625.x. [DOI] [PubMed] [Google Scholar]
- 66.Singla R, Khan N, Al-Sharif N, et al. Influence of diabetes on manifestations and treatment outcome of pulmonary TB patients. Int J Tuberc Lung Dis. 2006;10(1):74–79. [PubMed] [Google Scholar]
- 67.Khanna A, Lohya S, Sharath BN, et al. Characteristics and treatment response in patients with tuberculosis and diabetes mellitus in New Delhi, India. Public Health Action. 2013;3(Suppl. 1):S48–S50. doi: 10.5588/pha.13.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chiang CY, Lee J-J, Yu M-C, et al. Tuberculosis outcomes in Taipei: factors associated with treatment interruption for 2 months and death. Int J Tuberc Lung Dis. 2009;13(1):105–111. [PubMed] [Google Scholar]
- 69.Vasankari T, Holmström P, Ollgren J, et al. Risk factors for poor tuberculosis treatment outcome in Finland: a cohort study. BMC Public Health. 2007;7(1):291. doi: 10.1186/1471-2458-7-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gautam S, Shrestha N, Mahato S, et al. Diabetes among tuberculosis patients and its impact on tuberculosis treatment in South Asia: a systematic review and meta-analysis. Sci Rep. 2021;11(1):2113. doi: 10.1038/s41598-021-81057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jeon CY, Murray MB.. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med. 2008;5(7):e152. doi: 10.1371/journal.pmed.0050152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Al-Attiyah R, Mustafa A.. Mycobacterial antigen-induced T helper type 1 (Th1) and Th2 reactivity of peripheral blood mononuclear cells from diabetic and non-diabetic tuberculosis patients and Mycobacterium bovis bacilli Calmette–Guérin (BCG)-vaccinated healthy subjects. Clin Exp Immunol. 2009;158(1):64–73. doi: 10.1111/j.1365-2249.2009.04000.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Restrepo BI, Fisher-Hoch SP, Pino PA, et al. Tuberculosis in poorly controlled type 2 diabetes: altered cytokine expression in peripheral white blood cells. Clin Infect Dis. 2008;47(5):634–641. doi: 10.1086/590565. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on request from the corresponding author.