Abstract
Purpose of Review
This review aims to summarize the current burden of heart failure (HF) in the United States, specifically in patients with low socioeconomic position (SEP), and synthesize recommendations to prevent HF-related hospital readmissions in this vulnerable population.
Recent Findings
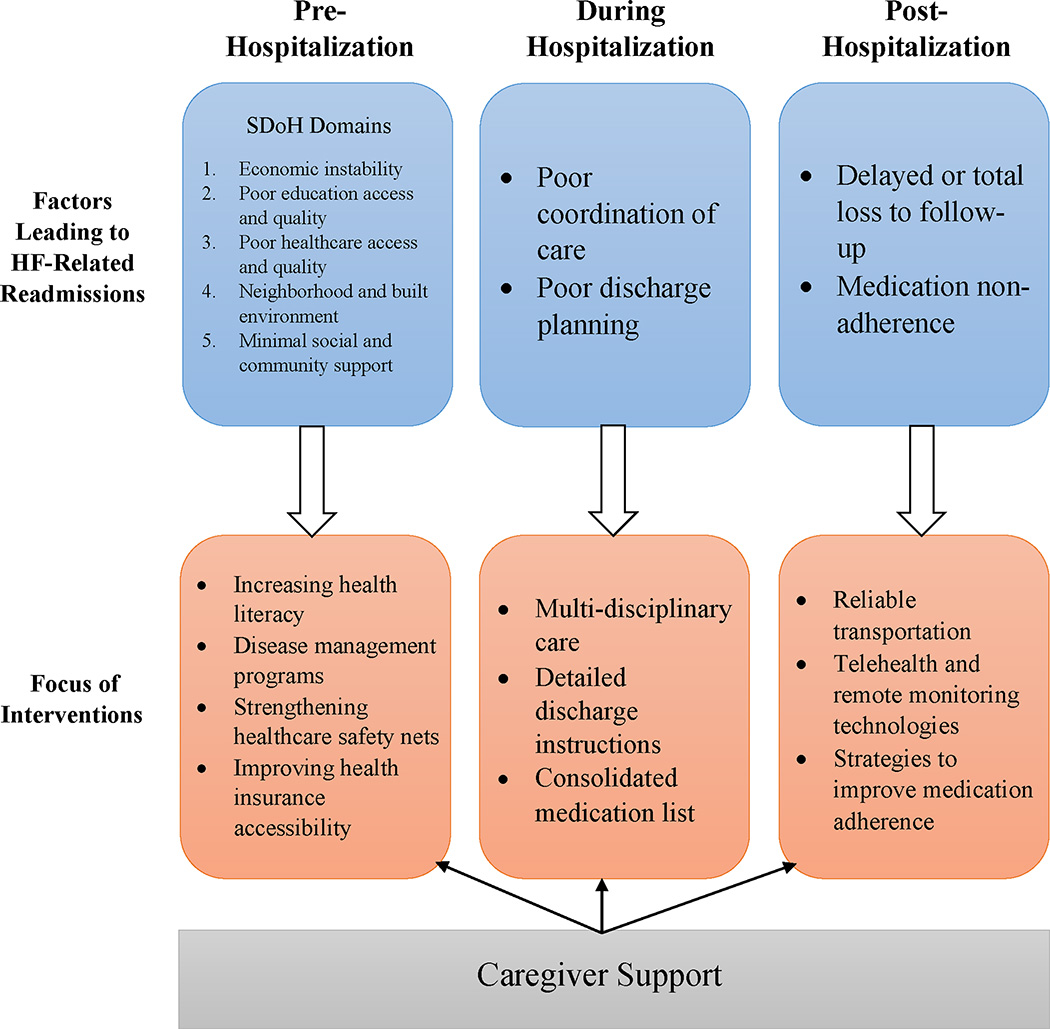
As treatments have improved, HF-related mortality has declined over time, resulting in more patients living with HF. This has led to an increase in hospitalizations, however, putting excess strain on our healthcare system. HF patients with low SEP are a particularly vulnerable group, as they experience higher rates of hospitalization and readmission compared to their high SEP counterparts. The Hospital Readmission Reduction Program (HRRP) was created to motivate interventions that reduce hospital readmissions across diseases, with HF being a primary target. Numerous readmission prevention efforts have been suggested to target the pre-hospitalization, hospitalization, and post-hospitalization phases, including addressing social determinants of health (SDoH), improving coordination of care, optimizing discharge plans, and improving adherence to follow-up care and medication regimens. Many of these proposed interventions show promise in reducing HF-related readmissions and issues surrounding adequate caregiver support may be particularly important to reduce readmissions among persons in low SEP.
Summary
Reducing HF-related hospital readmissions is possible, even in vulnerable populations like those with low SEP, but this will require coordinated efforts across the healthcare system and throughout the life course of these patients. Caregiver support is a necessary part of optimized care for low SEP HF patients and future efforts should consider interventions that support these caregivers.
Keywords: Heart Failure, Low Socioeconomic Position, Hospital Readmissions, Preventing Heart Failure Exacerbation
Introduction
Heart failure (HF) is a chronic and progressive condition affecting millions of people worldwide that poses substantial challenges to patients, caregivers, and healthcare systems. Despite significant advancements in medical treatments, HF remains associated with high morbidity, mortality, and frequent re-hospitalizations. For patients with low socioeconomic position (SEP), HF presents a particularly daunting burden, as these patients often encounter numerous barriers to adequate healthcare access, face challenges to adherence to treatment regimens, experience gaps in disease management, are facing other social determinants of health, and often have limited caregiver support. This review summarizes the recent literature on heart failure in patients with low SEP and highlights interventions proposed to prevent heart failure readmission in this population.
Heart Failure in the United States
The lifetime risk of HF in the US remains high, ranging from 20–45% among those aged 45+, and 10% of Americans living with HF have advanced HF [1–2]. Although it has been reported that >40% of HF patients die within 5-years of their initial diagnosis, improvements in HF treatments have led to overall greater survival after HF diagnosis over the past few decades [3–4]. This decrease in HF mortality is a success for the healthcare community, yet the number of persons living with HF continues to increase and the prevalence of HF is projected to rise by 46% by 2030 [5].
In addition to its high mortality rate, HF is one of the leading causes of hospitalization in the US, resulting in >1 million annual hospitalizations nationwide [6]. As the population ages and the prevalence of HF increases, the number of HF hospitalizations have also increased, contributing significantly to the overall burden on our healthcare systems [2, 7]. Despite advancements in therapy, heart failure patients face a high risk of readmission after discharge due to disease exacerbation or complications. Recent readmission risk for heart failure patients range from 20% to 30% within 30 days of initial discharge and temporal trends have demonstrated that both 30- and 90-day adjusted HF-related readmissions have increased over time following an index HF hospitalization [8–9]. These frequent readmissions place a strain on hospital resources and increase healthcare costs. Several factors contribute to these high HF readmissions, including inadequate discharge planning, medication non-adherence, lack of follow-up care, comorbidities such as diabetes and hypertension, and other social factors like income, education, and access to reliable transportation, among others [2].
Impact of Low SEP on Heart Failure Outcomes
SEP is traditionally measured by income, education, or occupational status and is one of the most influential factors contributing to variations in health outcomes [10]. Patients in low SEP have little income or wealth to buffer against the negative impacts of adverse health events [11]. In comparison to their White and Asian counterparts, Black and Hispanic individuals in the US are less likely to graduate from college and have lower median household income [10]. Studies have demonstrated a strong association between low SEP and an increased risk of cardiovascular disease, including HF, hospitalization, and death [12–15]. Factors such as poverty, limited education, unstable housing, inadequate access to healthcare services and numerous other social factors are recognized as critical contributors to the prevalence of HF among this population [16–17]. Moreover, low SEP has been linked to a higher incidence of risk factors for HF, including hypertension, diabetes, smoking and obesity further exacerbating the disease burden [18].
Limited access to quality healthcare services, including primary care, specialty care, and medications is a key obstacle faced by HF patients with low SEP. Financial constraints, lack of health insurance, and geographic barriers have been shown to impede timely access to essential medical interventions and adequate follow-up care [19]. Additionally, medication non-adherence is common in this population due to cost-related issues, leading to suboptimal disease management and increased readmission rates [20].
Individuals from low socioeconomic backgrounds often experience significant psychosocial stressors, such as chronic financial strain, social isolation, and discrimination, which have been linked to increased HF readmission rates [21]. The chronic stress associated with these factors can exacerbate HF symptoms, compromise self-care behaviors, and lead to poor treatment adherence [22].
Hospital Readmission Reduction Program (HRRP)
In 2012, the Affordable Care Act (ACA) established the Hospital Readmission Reduction Program (HRRP) to mitigate heart failure readmissions and their associated costs [23–24]. Under this program, hospitals are financially penalized if they have higher than expected risk-standardized 30-day readmission rates for acute myocardial infarction, pneumonia, chronic obstructive pulmonary disease (COPD), elective hip and knee replacement, coronary artery bypass graft (CABG) or HF. As a result, many hospitals have invested in a variety of general transitional care interventions including optimizing discharge planning, implementing post-discharge follow-up programs, providing patient education, and enhancing medication adherence [23]. Additionally, for low SEP persons and other marginalized groups with HF, recent literature has highlighted the benefits of addressing social determinants of health through community-based interventions.
Early analyses demonstrate a reduction in readmissions after the implementation of HRRP [23]. This reduction could be a result of the relationships HRRP has created or enhanced between hospitals, other medical institutions, and in surrounding communities. To avoid penalties, these organizations have invested in improving the overall patient experience, both during and after hospitalization. Although HRRP implementation has led to numerous improvements, the program is not without limitations. Initial risk-adjustment models did not account for SEP, a variable that is associated with increased risk of readmission after hospitalization [24]. Unsurprisingly, subsequent analyses have shown that hospitals caring for patients with a lower SEP are at higher risk of incurring penalties [23]. This suggests that the HRRP may be unintentionally penalizing hospitals that care for disadvantaged populations, potentially adding to the barriers to accessing reliable healthcare for low SEP persons with HF.
Interventions to Reduce Heart Failure Readmissions in Patients with Low SEP
Pre-Hospitalization: Social Determinants of Health
Social determinants of health (SDoH) describe the conditions and spaces in which people are born, live, and age. There are 5 primary domains of SDoH: economic stability, education access and quality, healthcare access and quality, neighborhood and built environment, and social and community context [25]. In addition to low income and education, many individuals in low SEP are often uninsured or do not have access to timely preventative health care, live in neighborhoods with high levels of pollution or limited access to green spaces like parks, and are more likely to experience the negative effects of structural racism, discrimination, and implicit bias [10, 26–27].
For decades, studies have found associations between these upstream SDoHs and the development of a variety of downstream diseases, including HF, and the World Health Organization reports that these SDoH contribute to ~30–55% of poor health outcomes [28–29]. Lack of reliable transportation, lack of insurance, and living far away from clinics and hospitals are all barriers to routine health care. This coupled with low health literacy can lead to delayed identification and treatment of important cardiovascular risk factors or make it difficult for low SEP individuals to afford necessary medications, both of which have been linked to the development of HF [30]. Interventions that target these pre-hospitalization SDoH in low SEP patients have the potential to prevent HF hospitalizations, slow the progression of HF, and, hopefully, avoid the development of HF all-together.
Current interventions targeting SDoH include improving housing stability, providing employment opportunities, increasing health literacy, addressing food insecurity, and building more community recreation spaces [31]. Disease management programs tailored to the specific needs of low SEP populations have shown promise in improving HF outcomes. These programs often include structured education, lifestyle coaching, and social support, addressing both medical and psychosocial aspects of HF management [32–33]. Policy interventions aimed at strengthening healthcare safety nets, expanding Medicare and Medicaid coverage, and improving health insurance accessibility can play a crucial role in mitigating the disparities in HF readmission rates among low SES populations.
Collaboration between healthcare systems and social service agencies can facilitate comprehensive care that addresses both medical and social determinants of health [34]. This integration can enhance patient outcomes and reduce HF readmissions in vulnerable populations. To achieve sustainable and lasting improvements, it is imperative to address the structural inequities that perpetuate disparities in HF outcomes. This involves challenging systemic barriers and promoting health equity through policy and community-based initiatives.
During Hospitalization: Multidisciplinary Care and Optimized Discharge Planning
Once a patient is hospitalized for an HF exacerbation, the priority shifts from prevention to stabilizing the patient and developing a plan to manage the patient’s symptoms long-term. Evidence suggests that comprehensive care coordination, involving physicians, nurses, pharmacists, social workers, and community health workers, can significantly reduce HF readmissions in patients with low SEP [35]. In 2019, Chava et al. demonstrated that implementing a multidisciplinary HF rounding team decreased 30-day hospitalizations from 27.6% to 17.2% and also decreased the average length of stay [36]. Additionally, collaborative efforts to enhance patient education, medication management, and self-care skills have demonstrated positive outcomes in managing HF and preventing readmissions [8, 37].
Optimized discharge planning aims to seamlessly transition patients from a hospital setting to their next level of care, which is often back home for low SEP patients. Discharge planning involves having follow-up and home care pre-arranged, patient and caregiver education of what to expect once the patient is back home, detailed care instructions, an organized list of medications and dosing instructions, and signs that the patient should contact their physician or return to the hospital [38]. Optimized planning ensures continuity of care to improve the patient’s quality of life and has been shown to reduce early readmission rates by up to 25% [38]. HF patients, along with patients who have had an MI or major surgery, often require more robust discharge planning than other hospitalized patients and low SEP patients may require additional instructions and resources [39].
Post-Hospitalization: Follow-Up Programs, Telehealth, and Medication Adherence
The priority of care for low SEP patients after hospitalization for HF exacerbation is adherence to follow-up care. Follow-up care is a vitally important piece of efforts to reduce HF-related hospital readmissions. A 2020 study by Nair et al. demonstrated that the 30-day readmission rate of CHF patients was reduced in half, from 28% in 2017 to 14% in 2018, after the implementation of their 2-week follow-up appointment program [8]. Other studies have shown that in-person clinic follow-up within 7 days after discharge from a HF-related hospitalization is also associated with lower 30-day readmission [40–41]. This demonstrates that follow-up programs work to reduce HF-related readmissions, but the barriers low SEP patients face in completing their follow-up appointments need to be addressed.
Although follow-up programs have proven to reduce the risk of hospital readmission, many low SEP individuals do not have reliable transportation or a social support network to help them be physically present at a follow-up appointment. Telehealth and remote monitoring technologies have emerged as potential solutions to bridge the gap in healthcare access for patients with low SEP [41]. These technologies enable healthcare providers to monitor HF patients’ vital signs, symptoms, and medication adherence remotely, leading to early intervention and timely adjustments to treatment plans. The THRIVE Study found that early, structured telephone follow-up after hospitalization reduced 30-day HF readmissions to similar levels as the in-person clinic follow-up intervention [40]. The potential benefit from telehealth technologies is vast, yet far from streamlined, as several studies have shown that telehealth may be further perpetuating health inequities due to differing levels of digital access, digital fluency, and capacity for health advocacy between advantaged and disadvantaged groups [42]. Nonetheless, technology is becoming more and more accessible, and future efforts should focus on maximizing its potential for connecting marginalized groups with providers.
Follow-up with a physician either in-person or over the phone after a HF-related hospitalization is essential, but reliable access and adherence to medications is another critical determinant of HF management and readmission prevention. Inadequate adherence to necessary medications can lead to HF exacerbations, a major cause of hospital readmissions and increased mortality [43]. The primary reasons for low medication adherence are cost, polypharmacy, lack of symptoms, misunderstanding medication instructions, and forgetfulness due to advanced age or disease [44]. A 2017 study demonstrated that HF patients with low or intermediate medication adherence had a 30-day readmission risk of 20.0%, which was twice the readmission rate for patients with high medication adherence (9.3%) [45]. This increase in 30-day readmission risk highlights the importance of interventions that help HF patients adhere to their medication regimens. This is particularly important for patients with low SEP as they are at excess risk of poor medication adherence [20].
A few studies have tested interventions to improve medication adherence. Studies promoting linking medication management with existing habits and text message programs to remind patients to take their medications have both shown promise in increasing medication adherence [46]. Other studies have found, however, that face-to-face interventions appear to be most helpful for patients with a history of medication non-adherence [47]. This suggests that having adequate caretaker support to serve as a reminder or to administer medications should be highly recommended, especially for elderly or forgetful patients. Although remembering to take ones medications is one aspect of medication adherence, being able to afford ones medications is often a significant factor. Without insurance, the cost of certain medications can be prohibitive to medication adherence in low SEP patients, and some patients spend less on basic needs in order to afford their medications [48]. Medication assistance programs that provide financial support and discounted prescriptions have been shown to substantially improve medication adherence in patients with low SEP [49].
Burden on Caregivers
As the population ages and the prevalence of chronic disease increases, more and more family members, friends, or neighbors are taking on the role of caregiver for their loved ones. Unpaid, non-medical caregivers play an important role in the care of HF patients, especially among those with low SEP who likely cannot afford a professional caregiver [50]. These caregivers provide support in numerous ways, but some of their biggest roles include providing transportation to follow-up visits, ensuring patients are adherent with their medications, taking care of daily tasks like cooking meals and cleaning, and acting as a support system for the physical, psychosocial, and financial needs of the patients [50]. In 2017, it was estimated that the economic value of caregivers in the US was nearly half a billion dollars, clearly demonstrating the value of this role [51].
Being a caregiver for a loved one can be extremely rewarding, but long-term care for a chronic patient may eventually take a toll on the caregiver [52]. For patients with advanced HF, the burden placed on their caregivers can be especially high due to their decreased functionality. Additionally, caregivers often have jobs and responsibilities outside of taking care of their loved ones and, financially, it is not an option for many low SEP caregivers to take time off from work to provide care. This situation can lead to physical, mental, emotional, and financial strain as well as isolation of these caregivers from the other people in their life [52]. Caregiver issues can often be overlooked when discussing ways to prevent HF-related readmissions, but supporting them may be the key to further reducing readmission rates.
Caregivers play an important role in the pre-hospitalization, hospitalization, and post-hospitalizations stages discussed earlier. In addition to the other interventions discussed for each stage, finding more consistent ways to support caregivers seems necessary to keep low SES HF patients out of the hospital. A 2015 paper by Sullivan and Miller outlines 10 tips to avoid caregiver burnout: (1) become educated about the disease, (2) take care of yourself, (3) practice healthy living, (4) stay social, (5) accept help, (6) acknowledge your emotions, (7) allow for healthy expression of your feelings with one another, (8) allow for caregiving holidays, (9) encourage healthy independence of your loved one, and (10) see help through your local organizations [53]. Becoming a new caregiver can be overwhelming, yet extremely beneficial to the overall care of a loved one with HF, so future interventions should take the role of caregivers into consideration and provide them with the support they need.
Future Directions
Low SEP individuals are more likely to develop HF, be hospitalized and subsequently readmitted for HF exacerbations, and die compared to their high SEP counterparts. Although this review discusses multiple interventions to reduce readmissions at different points in a patient’s HF journey (summarized in Figure 1), the burden HF places on the community and our healthcare system remains high. Future efforts should focus on the SDoH that prevent low SEP persons from being able to access reliable preventative care, coordination of care and optimized discharge planning while in the hospital, follow-up programs and interventions to improve medication adherence, and additional support and resources for non-medical caregivers taking care of these HF patients.
Figure 1.
Interventions to Prevent Heart Failure-Related Readmissions in Low SEP Patients by Hospitalization Stage
Conclusion
HF readmissions continue to present a considerable healthcare and economic burden. Preventing HF readmission in patients with low SEP requires a multifaceted approach that addresses not only medical factors but also the complex interplay of psychosocial factors. The evidence presented in this review highlights the importance of addressing SDoH, optimizing coordination of care and discharge planning, and targeted interventions to improve HF follow-up care and medication adherence to reduce readmission rates in this vulnerable population. Through policy changes, increased healthcare access, and holistic support, the healthcare community can work towards achieving health equity and better outcomes for all HF patients, regardless of SEP.
Funding statement:
Sydney Browder is funded by an NIH pre-doctoral Cardiovascular (CVD) Epidemiology Training Grant (NRSA: T32-HL007055-46).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent: This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association [published correction appears in Circulation. 2022 Sep 6;146(10):e141]. Circulation. 2022;145(8):e153–e639. doi: 10.1161/CIR.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 2.Roger VL. Epidemiology of Heart Failure: A Contemporary Perspective. Circ Res. 2021;128(10):1421–1434. doi: 10.1161/CIRCRESAHA.121.318172 [DOI] [PubMed] [Google Scholar]
- 3.Loehr LR, Rosamond WD, Chang PP, Folsom AR, and Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study). Am J Cardiol. 2008;101:1016–1022. doi: 10.1016/j.amjcard.2007.11.061 [DOI] [PubMed] [Google Scholar]
- 4.Ni H, Xu J. Recent Trends in Heart Failure-related Mortality: United States, 2000–2014. NCHS Data Brief. 2015;(231):1–8. [PubMed] [Google Scholar]
- 5.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–619. doi: 10.1161/HHF.0b013e318291329a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lahoz R, Fagan A, McSharry M, Proudfoot C, Corda S, Studer R. Recurrent heart failure hospitalizations are associated with increased cardiovascular mortality in patients with heart failure in Clinical Practice Research Datalink. ESC Heart Fail. 2020;7(4):1688–1699. doi: 10.1002/ehf2.12727 * Recurrent heart failure hospitalizations are strongly associated with cardiovascular mortality and the risk of death increases with each additional hospitalization.
- 7.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al. ; on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2019 update: a report from the American Heart Association [published correction appears in Circulation. 2020;141:e33]. Circulation. 2019; 139:e56–e528. doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 8.Nair R, Lak H, Hasan S, Gunasekaran D, Babar A, Gopalakrishna KV. Reducing All-cause 30-day Hospital Readmissions for Patients Presenting with Acute Heart Failure Exacerbations: A Quality Improvement Initiative. Cureus. 2020;12(3):e7420. Published 2020 Mar 25. doi: 10.7759/cureus.7420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khan MS, Sreenivasan J, Lateef N, et al. Trends in 30- and 90-Day Readmission Rates for Heart Failure. Circ Heart Fail. 2021;14(4):e008335. doi: 10.1161/CIRCHEARTFAILURE.121.008335 * Following an index HF hospitalization, 30- and 90- day adjusted HF-related and all-cause readmissions increased significantly between 2010 and 2017 in the U.S.
- 10.Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychol. 2016;35(4):407–411. doi: 10.1037/hea0000242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leonard T, Hughes AE, Pruitt SL. Understanding how low-socioeconomic status households cope with health shocks: An analysis of multi-sector linked data. Ann Am Acad Pol Soc Sci. 2017;669(1):125–145. doi: 10.1177/0002716216680989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hawkins NM, Jhund PS, McMurray JJ, Capewell S. Heart failure and socioeconomic status: accumulating evidence of inequality. Eur J Heart Fail. 2012;14(2):138–146. doi: 10.1093/eurjhf/hfr168 [DOI] [PubMed] [Google Scholar]
- 13. Hung CL, Chao TF, Su CH, et al. Income level and outcomes in patients with heart failure with universal health coverage. Heart. 2021;107(3):208–216. doi: 10.1136/heartjnl-2020-316793 ** Low-income individuals have a significantly higher risk of HF readmission compared to higher-income individuals. Implementation of nationwide universal health coverage appears to mitigate the differences in HF outcomes across income groups over time.
- 14.Schrage B, Lund LH, Benson L, et al. Lower socioeconomic status predicts higher mortality and morbidity in patients with heart failure. Heart. 2021;107(3):229–236. doi: 10.1136/heartjnl-2020-317216 [DOI] [PubMed] [Google Scholar]
- 15.Teng TK, Tay WT, Richards AM, et al. Socioeconomic Status and Outcomes in Heart Failure With Reduced Ejection Fraction From Asia. Circ Cardiovasc Qual Outcomes. 2021;14(4):e006962. doi: 10.1161/CIRCOUTCOMES.120.006962 [DOI] [PubMed] [Google Scholar]
- 16.Kreatsoulas C, Anand SS. The impact of social determinants on cardiovascular disease. Can J Cardiol. 2010;26 Suppl C(Suppl C):8C–13C. doi: 10.1016/s0828-282x(10)71075-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Powell-Wiley TM, Baumer Y, Baah FO, et al. Social Determinants of Cardiovascular Disease. Circ Res. 2022;130(5):782–799. doi: 10.1161/CIRCRESAHA.121.319811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fogacci F, Borghi C, Tocci G, Cicero AFG. Socioeconomic status as determinant of individual cardiovascular risk. Atherosclerosis. 2022;346:82–83. doi: 10.1016/j.atherosclerosis.2022.02.020 [DOI] [PubMed] [Google Scholar]
- 19.Lazar M, Davenport L. Barriers to Health Care Access for Low Income Families: A Review of Literature. J Community Health Nurs. 2018;35(1):28–37. doi: 10.1080/07370016.2018.1404832 [DOI] [PubMed] [Google Scholar]
- 20.Lee H, Park JH, Floyd JS, Park S, Kim HC. Combined Effect of Income and Medication Adherence on Mortality in Newly Treated Hypertension: Nationwide Study of 16 Million Person-Years. J Am Heart Assoc. 2019;8(16):e013148. doi: 10.1161/JAHA.119.013148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kasireddy TR, Yukselen Z, Muthyala A, et al. Association of Psychosocial Risk Factors and Outcomes in Heart Failure: Does COVID-19 Affect Outcomes? [published online ahead of print, 2023 May 18]. Curr Probl Cardiol. 2023;48(10):101795. doi: 10.1016/j.cpcardiol.2023.101795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Endrighi R, Waters AJ, Gottlieb SS, et al. Psychological stress and short-term hospitalizations or death in patients with heart failure. Heart. 2016;102(22):1820–1825. doi: 10.1136/heartjnl-2015-309154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131(20):1796–1803. doi: 10.1161/CIRCULATIONAHA.114.010270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wadhera RK, Yeh RW, Joynt Maddox KE. The Hospital Readmissions Reduction Program - Time for a Reboot. N Engl J Med. 2019;380(24):2289–2291. doi: 10.1056/NEJMp1901225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jilani MH, Javed Z, Yahya T, et al. Social Determinants of Health and Cardiovascular Disease: Current State and Future Directions Towards Healthcare Equity. Curr Atheroscler Rep. 2021;23(9):55. Published 2021 Jul 26. doi: 10.1007/s11883-021-00949-w [DOI] [PubMed] [Google Scholar]
- 26.McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front Public Health. 2020;8:231. Published 2020 Jun 18. doi: 10.3389/fpubh.2020.00231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robinette JW, Charles ST, Gruenewald TL. Neighborhood Socioeconomic Status and Health: A Longitudinal Analysis. J Community Health. 2017;42(5):865–871. doi: 10.1007/s10900-017-0327-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization, Social determinants of health, accessed 17 August 2023, < https://www.who.int/health-topics/social-determinants-of-health>. [Google Scholar]
- 29.Enard KR, Coleman AM, Yakubu RA, Butcher BC, Tao D, Hauptman PJ. Influence of Social Determinants of Health on Heart Failure Outcomes: A Systematic Review. J Am Heart Assoc. 2023;12(3):e026590. doi: 10.1161/JAHA.122.026590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cajita MI, Cajita TR, Han HR. Health Literacy and Heart Failure: A Systematic Review. J Cardiovasc Nurs. 2016;31(2):121–130. doi: 10.1097/JCN.0000000000000229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Daniel H, Bornstein SS, Kane GC, et al. Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. Ann Intern Med. 2018;168(8):577–578. doi: 10.7326/M17-2441 [DOI] [PubMed] [Google Scholar]
- 32.AlHabeeb W Heart failure disease management program: A review. Medicine (Baltimore). 2022;101(31):e29805. doi: 10.1097/MD.0000000000029805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tan SS, Pisano MM, Boone AL, et al. Evaluation Design of EFFICHRONIC: The Chronic Disease Self-Management Programme (CDSMP) Intervention for Citizens with a Low Socioeconomic Position. Int J Environ Res Public Health. 2019;16(11):1883. Published 2019 May 28. doi: 10.3390/ijerph16111883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation’s Health. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington (DC): National Academies Press (US); 2019. Sep 25. 3, A Workforce to Integrate Social Care into Health Care Delivery. Available from: https://www.ncbi.nlm.nih.gov/books/NBK552605/ [PubMed] [Google Scholar]
- 35.Thaker R, Pink K, Garapati S, et al. Identify Early and Involve Everyone: Interdisciplinary Comprehensive Care Pathway Developed for Inpatient Management and Transitions of Care for Heart Failure Patients Reported Using SQUIRE 2.0 Guidelines. Cureus. 2022;14(1):e21123. Published 2022 Jan 11. doi: 10.7759/cureus.21123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chava R, Karki N, Ketlogetswe K, Ayala T. Multidisciplinary rounds in prevention of 30-day readmissions and decreasing length of stay in heart failure patients: A community hospital based retrospective study. Medicine (Baltimore). 2019;98(27):e16233. doi: 10.1097/MD.0000000000016233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rice H, Say R, Betihavas V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review. Patient Educ Couns. 2018;101(3):363–374. doi: 10.1016/j.pec.2017.10.002 [DOI] [PubMed] [Google Scholar]
- 38.Desai AS, Stevenson LW. Rehospitalization for heart failure: predict or prevent?. Circulation. 2012;126(4):501–506. doi: 10.1161/CIRCULATIONAHA.112.125435 [DOI] [PubMed] [Google Scholar]
- 39.Kangovi S, Barg FK, Carter T, et al. Challenges faced by patients with low socioeconomic status during the post-hospital transition. J Gen Intern Med. 2014;29(2):283–289. doi: 10.1007/s11606-013-2571-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee KK, Thomas RC, Tan TC, Leong TK, Steimle A, Go AS. The Heart Failure Readmission Intervention by Variable Early Follow-up (THRIVE) Study: A Pragmatic Randomized Trial. Circ Cardiovasc Qual Outcomes. 2020;13(10):e006553. doi: 10.1161/CIRCOUTCOMES.120.006553 [DOI] [PubMed] [Google Scholar]
- 41.Morken IM, Storm M, Søreide JA, Urstad KH, Karlsen B, Husebø AML. Posthospitalization Follow-Up of Patients With Heart Failure Using eHealth Solutions: Restricted Systematic Review. J Med Internet Res. 2022;24(2):e32946. Published 2022 Feb 15. doi: 10.2196/32946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gergen Barnett K, Mishuris RG, Williams CT, et al. Telehealth’s Double-Edged Sword: Bridging or Perpetuating Health Inequities?. J Gen Intern Med. 2022;37(11):2845–2848. doi: 10.1007/s11606-022-07481-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gupta P, Voors AA, Patel P, et al. Non-adherence to heart failure medications predicts clinical outcomes: assessment in a single spot urine sample by liquid chromatography-tandem mass spectrometry (results of a prospective multicentre study). Eur J Heart Fail. 2021;23(7):1182–1190. doi: 10.1002/ejhf.2160 [DOI] [PubMed] [Google Scholar]
- 44.Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26(3):155–159. doi: 10.5001/omj.2011.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rosen OZ, Fridman R, Rosen BT, Shane R, Pevnick JM. Medication adherence as a predictor of 30-day hospital readmissions. Patient Prefer Adherence. 2017;11:801–810. Published 2017 Apr 20. doi: 10.2147/PPA.S125672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Badawy SM, Shah R, Beg U, Heneghan MB. Habit Strength, Medication Adherence, and Habit-Based Mobile Health Interventions Across Chronic Medical Conditions: Systematic Review. J Med Internet Res. 2020;22(4):e17883. Published 2020 Apr 28. doi: 10.2196/17883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Conn VS, Ruppar TM, Enriquez M, Cooper P. Medication adherence interventions that target subjects with adherence problems: Systematic review and meta-analysis. Res Social Adm Pharm. 2016;12(2):218–246. doi: 10.1016/j.sapharm.2015.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rohatgi KW, Humble S, McQueen A, et al. Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. J Am Board Fam Med. 2021;34(3):561–570. doi: 10.3122/jabfm.2021.03.200361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hung A, Blalock DV, Miller J, et al. Impact of financial medication assistance on medication adherence: a systematic review. J Manag Care Spec Pharm. 2021;27(7):924–935. doi: 10.18553/jmcp.2021.27.7.924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kitko L, McIlvennan CK, Bidwell JT, et al. Family Caregiving for Individuals With Heart Failure: A Scientific Statement From the American Heart Association. Circulation. 2020;141(22):e864–e878. doi: 10.1161/CIR.0000000000000768 [DOI] [PubMed] [Google Scholar]
- 51.Knowles KA, Xun H, Jang S, et al. Clinicians for CARE: A Systematic Review and Meta-Analysis of Interventions to Support Caregivers of Patients With Heart Disease. J Am Heart Assoc. 2021;10(24):e019706. doi: 10.1161/JAHA.120.019706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu Z, Heffernan C, Tan J. Caregiver burden: A concept analysis. Int J Nurs Sci. 2020;7(4):438–445. Published 2020 Jul 25. doi: 10.1016/j.ijnss.2020.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sullivan AB, Miller D. Who is Taking Care of the Caregiver?. J Patient Exp. 2015;2(1):7–12. doi: 10.1177/237437431500200103 [DOI] [PMC free article] [PubMed] [Google Scholar]