Abstract
During the pandemic, many individuals with chronic or infectious diseases other than COVID-19 were unable to receive the care they needed due to the high demand for respiratory care. Our study aims to assess the impact of the COVID-19 pandemic on services provided to people with chronic diseases in Peru from 2016 to 2022. We performed a secondary database analysis of data registered by the comprehensive health insurance (SIS), the intangible solidarity health fund (FISSAL), and private healthcare institutions (EPS), using interrupted time series analysis. Our study identified 21,281,128 individual users who received care. The pooled analysis revealed an average decrease of 1,782,446 in the number of users receiving care in the first month of the pandemic compared with the expected values for that month based on pre-pandemic measurements. In addition, during the pandemic months, there was an average increase of 57,911 in the number of new additional single users who received care per month compared with the previous month. According to the time-series analysis of users receiving care per month based on each chronic disease group, the most significant decreases included people with diabetes without complications and chronic lung disease.
Keywords: Interrupted time series analysis, Chronic diseases, COVID-19, Peru
Subject terms: Health care, Public health
Introduction
The COVID-19 pandemic occurred against a backdrop of the high prevalence of chronic diseases globally1. During the pandemic, people with chronic or infectious diseases other than COVID-19 often had difficulty accessing the care they needed. This was due to the prioritization of treatment for respiratory diseases, mainly COVID-19, which led to overburdened health systems2. As a result, the people with chronic diseases were not addressed or included in prevalence reports. For example, according to the cases reported by the Finnish healthcare system, new cancer cases decreased by 5%, and type-2 diabetes cases decreased by more than 16%3. This decrease in chronic disease care may be attributed to complications in timely diagnosis and treatment during the pandemic2. In addition, the pandemic changed people’s lifestyle4 and access to medication5. As a result, individuals with pre-existing diseases experienced a 2.6-fold increase in disease severity 6, so the need for health insurance for the entire Peruvian population became more evident.
Global public health insurance is crucial to achieving universal health insurance7. Public health insurance can reduce access inequalities and ensure quality care among low-income individuals8,9. Public health insurance is designed to cover a specific set of chronic diseases, high-cost conditions, and health issues that are a state priority10. In Peru, the population's need for public health insurance is more evident due to the inequities inherent to the existing socioeconomic context, which is accompanied by a deficient health system, even though 97.8% of citizens have some form of health insurance11; and there are different types of insurance, such as private insurance and insurance derived from public entities such as the National Police and the Army (2%)11.
The Seguro Integral de Salud (SIS) is the most widely used public insurance system and covers more than 71% of the Peruvian population. It provides coverage to people who do not have any other type of insurance as well as to the general population and guarantees access to health services12,13. In addition, the SIS, through the Intangible Solidarity Health Fund (FISSAL), finances high-cost benefits. On the other hand, the main Peruvian private insurances are the Private Healthcare Entities (EPS), which are responsible for more than 3% of the total health services provided in the country11.
The pandemic affected public health systems worldwide and reduced their capacity to provide healthcare14. However, this impact was higher in low- and middle-income countries such as Peru15. At the beginning of the pandemic, a significant decrease in the Peruvian health system’s capacity to provide healthcare was observed16. Since it is a fragmented system, we cannot measure its capacity accurately or determine whether its healthcare capacity has been recovered, especially for individuals with chronic diseases. For this reason, our study aims to assess the impact of the COVID-19 pandemic on the services provided to individuals with chronic diseases in Peru from 2016 to 2022. Our approach focuses on analyzing the progression of the healthcare services provided by the Peruvian SIS over those years. Healthcare services are represented by the number of single users who receive care every month, which will provide a comprehensive perspective on the progression of the health system and its capacity to provide healthcare to the insured population.
Method
Design
We conducted a secondary database analysis according to the data registered by the SIS and FISSAL (insurer that finances the high-cost benefits of the SIS), both belonging to the Peruvian Ministry of Health (MINSA), as well as private Healthcare Entities (EPS) during the 2016–2022 period using an interrupted time series analysis (ITSA).
Participants
The sample unit consisted of the number of monthly users that received care. Users’ healthcare services were funded by SIS, private EPS, and the FISSAL. All users attending a medical consultation from January 2016 to December 2022 were included. Records with no ID data (national identity document) and with diagnostic inconsistencies (inconsistent diagnosis with sex or age group) were excluded, and only patients 0–99 years old were included.
Variables
Number of users who received care per month
It was defined as the number of users who received care during a given month, such care being funded by SIS, EPS, or FISSAL.
Sociodemographic variables
Subjects included were classified by sex (male or female) and age, which included early childhood (0–11 years), adolescence (12–17 years), adulthood (18–64 years), and old age (65 years or over). Additionally, users were grouped by the geographical code of their residence (department, province, and district) and by the district wealth quintile in Peru, based on the data provided by the National Institute of Statistics and Computing of Peru. Moreover, subjects included were grouped based on their healthcare system (SIS, EPS, or FISSAL).
Diagnosis of chronic diseases
Diagnoses were classified according to International Classification of Diseases-10 and grouped into 17 diseases based on Mary Charlson’s classification (Myocardial infarction, Congestive heart failure, Peripheral vascular disease, Cerebrovascular disease, Dementia, Chronic pulmonary disease, Connective tissue disease, Ulcer disease, Liver disease, Diabetes or diabetes with organic lesion, Hemiplegia, Kidney disease, Neoplasms, Leukemia, Malignant lymphoma, Solid metastasis, and AIDS)17. We defined a case of chronic disease if the participant received a definitive diagnosis of one of Mary Charlson's classifications of chronic disease during the analysis period (2016–2022). We believe this is a valid measure, as these are chronic conditions that, by their nature, do not go away over time.
Analysis
We used ITSA, a quasi-experimental approach, to estimate the impact of the COVID-19 pandemic on the services provided by the Peruvian health system. The choice of an ITSA was due to its ability to assess the impact of an event (in this case, the COVID-19 pandemic) over time. Therefore, time series analysis was more appropriate for our data because we used discrete measures that collapsed the number of cases into one month. In addition, ITSA allow us to decompose temporal effects into level and trend changes, providing a richer understanding of how the pandemic changed the use of health services. Furthermore, the use of ITSA has been useful in assessing the impact of the pandemic in different health contexts in Peru16,18.
For our study, we established a discrete number of measurements per month. A descriptive analysis was conducted, which included the number of users receiving care per month and their sociodemographic variables. In addition, an ITSA was conducted, considering a censoring period when the Peruvian government declared a state of emergency due to COVID-19 (March 16, 2020), because during this month a strict lockdown was decreed, which reduced the access of public health. A segmented regression analysis with Newey–West standard errors was used for data modeling19, and monthly time units were considered. We considered before the pandemic (01 January 2016–28 February 2020) and during the lockdown (01 April 2020–31 December 2022). The estimated impact of the COVID-19 pandemic on outcomes was assessed in terms of the change in the level (intercept) and the change in the slope of the number of users in treatment per month over the time series before and after the interruption of the intervention. The change in the intercept is only the immediate change in the level of prevalence of the outcome, whereas the change in the slope of the number of users receiving care per month reflects the change in the trend of the number of users over time in each quarter. Subgroup analyses were performed for age group, sex, wealth quintile and health subsystem. Values with a 95% hypothesis test (p < 0.05) were considered significant. Users with missing data were excluded. Cumby–Huizinga tests were used with the “actest” command to check autocorrelation20. Analyses were conducted with Stata® software, version 17.
Procedure
Firstly, information from the databases of SIS, FISSAL, and EPS was downloaded through the accessible data platform SUSALUD (http://datos.susalud.gob.pe/). Secondly, the databases were pooled. Thirdly, a data consistency analysis was conducted, which implied confirming that subjects includer’s diagnoses were consistent with their sex or that their age was between 0 and 99 years. Fourthly, the data analyses were conducted, and the research report was written.
Ethical aspects
Our study uses information from the open data provided by SUSALUD, which is of public access and can be accessed through this link: 10.6084/m9.figshare.25207196. Available data is coded to remain anonymous, and no ethical risks can be identified for the subjects included.
Results
Sociodemographic characteristics
We initially analyzed 21,283,302 records, excluding 1922 records because the diagnosis did not match the biological sex of the subjects included (e.g. men with uterine cancer) and 252 records because the diagnosis did not match the age of the subjects included (e.g. children under three years of age diagnosed with pre-eclampsia). No duplicate records were identified. After this review of inconsistencies, less than 0.01% of records were excluded from the analyses.
Our study identified 21,281,128 single users who received care from January 2016 to December 2022 (84 months). Out of 95.5% of the users who received care per month were affiliated with the SIS (n = 20,313,146).
Regarding sociodemographic characteristics, most single users were women (n = 11,517,384; 54.1%), belonged to the lowest wealth quintile (n = 77,021,243; 32.7%) and were of working age, i.e. from 18 to 65 years (n = 5,539,129; 26.0%). As of Charlson’s diseases prevalence, 2.3% of users were diagnosed with diabetes without complications (n = 5,336,813), 1.3% were diagnosed with cancer (n = 3,089,318), 1.3% were diagnosed with chronic pulmonary disease (n = 3,147,185), and a lower percentage was diagnosed with other diseases that are shown in Table 1. Additionally, Table 1 shows the sociodemographic characteristics of users who received care per month before and during the pandemic for each type of Health Insurance Funds Administrative Institutions (IAFAS): SIS, EPS, and FISSAL.
Table 1.
Sociodemographic characteristics of single users per month, pooled before and during the pandemic (2016–2022).
| All (n = 21,281,128) | SIS (n = 20,313,146) | EPS (n = 1,041,537) | FISSAL (n = 326,098) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Sex | Female | 11,517,384 | 54.1% | 11,039,051 | 54.3% | 512,648 | 49.2% | 201,132 | 61.7% |
| Male | 9,763,744 | 45.9% | 9,274,095 | 45.7% | 528,889 | 50.8% | 124,966 | 38.3% | |
| Age group | 0–11 | 6,613,849 | 31.1% | 6,414,147 | 31.6% | 217,274 | 20.9% | 24,757 | 7.6% |
| 12–17 | 2,122,957 | 10.0% | 2,058,859 | 10.1% | 69,552 | 6.7% | 8727 | 2.7% | |
| 18–64 | 10,965,666 | 51.5% | 10,296,584 | 50.7% | 719,160 | 69.0% | 186,311 | 57.1% | |
| 65 or more | 1,578,656 | 7.4% | 1,543,556 | 7.6% | 35,551 | 3.4% | 106,303 | 32.6% | |
| Wealth quartile | Q1 | 5,539,129 | 26.0% | 5,531,139 | 27.2% | 10,452 | 1.0% | 35,936 | 11.0% |
| Q2 | 4,548,038 | 21.4% | 4,502,281 | 22.2% | 53,460 | 5.1% | 54,683 | 16.8% | |
| Q3 | 3,804,676 | 17.9% | 3,659,220 | 18.0% | 162,816 | 15.6% | 78,266 | 24.0% | |
| Q4 | 3,688,104 | 17.3% | 3,495,267 | 17.2% | 210,867 | 20.2% | 82,616 | 25.3% | |
| Q5 | 3,701,181 | 17.4% | 3,125,239 | 15.4% | 603,942 | 58.0% | 74,597 | 22.9% | |
| Pandemic* | Before | 16,869,327 | 79.3% | 16,011,798 | 78.8% | 923,116 | 88.6% | 278,757 | 85.5% |
| During | 15,750,626 | 74.0% | 15,002,322 | 73.9% | 817,714 | 78.5% | 265,627 | 81.5% | |
| Health system* | SIS | 20,313,146 | 95.5% | 20,313,146 | 100.0% | 75,836 | 7.3% | 323,812 | 99.3% |
| EPS | 1,041,537 | 4.9% | 75,836 | 0.4% | 1,041,537 | 100.0% | 999 | 0.3% | |
| FISSAL | 326,098 | 1.5% | 323,812 | 1.6% | 999 | 0.1% | 326,098 | 100.0% | |
| Charlson’s classification* | Others | 21,247,086 | 99.8% | 20,282,496 | 99.8% | 1,040,421 | 99.9% | 321,940 | 98.7% |
| Cancer | 624,948 | 2.9% | 610,016 | 3.0% | 14,539 | 1.4% | 158,425 | 48.6% | |
| Metastatic carcinoma | 56,104 | 0.3% | 54,912 | 0.3% | 1365 | 0.1% | 27,624 | 8.5% | |
| Dementia | 37,717 | 0.2% | 35,804 | 0.2% | 2029 | 0.2% | 4956 | 1.5% | |
| Diabetes with complications | 211,689 | 1.0% | 200,105 | 1.0% | 12,449 | 1.2% | 56,719 | 17.4% | |
| Diabetes without complications | 1,402,344 | 6.6% | 1,333,632 | 6.6% | 74,735 | 7.2% | 134,405 | 41.2% | |
| Cerebrovascular disease | 187,407 | 0.9% | 167,681 | 0.8% | 20,761 | 2.0% | 24,326 | 7.5% | |
| Mild liver disease | 327,339 | 1.5% | 297,491 | 1.5% | 31,589 | 3.0% | 38,527 | 11.8% | |
| Moderate or severe liver disease | 39,612 | 0.2% | 38,605 | 0.2% | 1118 | 0.1% | 6172 | 1.9% | |
| Chronic pulmonary disease | 1,373,631 | 6.5% | 1,195,715 | 5.9% | 190,080 | 18.2% | 60,875 | 18.7% | |
| Kidney disease | 188,812 | 0.9% | 181,427 | 0.9% | 7854 | 0.8% | 80,438 | 24.7% | |
| Rheumatic and connective tissue diseases | 330,849 | 1.6% | 311,557 | 1.5% | 20,590 | 2.0% | 28,386 | 8.7% | |
| Peptic ulcer disease | 120,284 | 0.6% | 108,878 | 0.5% | 12,131 | 1.2% | 11,001 | 3.4% | |
| Peripheral vascular disease | 25,383 | 0.1% | 22,315 | 0.1% | 3183 | 0.3% | 5291 | 1.6% | |
| Myocardial infarction | 37,417 | 0.2% | 35,246 | 0.2% | 2391 | 0.2% | 6098 | 1.9% | |
| Congestive heart failure | 173,053 | 0.8% | 162,330 | 0.8% | 11,307 | 1.1% | 33,459 | 10.3% | |
| Paraplegia and hemiplegia | 40,388 | 0.2% | 38,635 | 0.2% | 1916 | 0.2% | 6348 | 1.9% | |
| HIV AIDS | 157,771 | 0.7% | 156,896 | 0.8% | 1560 | 0.1% | 7705 | 2.4% | |
SIS comprehensive health insurance (in Spanish), EPS private healthcare entities (in Spanish), FISSAL intangible solidarity health fund (in Spanish).
*Values do not add up to 100%.
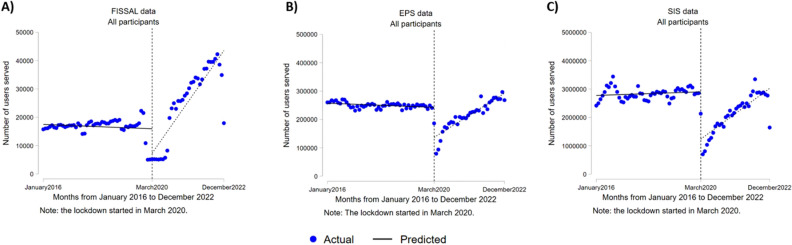
Users who received care per month
The pooled analysis of the three types of IAFAS (SIS, EPS, and FISSAL) identified an average decrease of 1,782,446 (95% CI − 2,165,401–− 1,399,490) in the number of users who received care during the first month at the beginning of the pandemic (March 2020) as opposed to the expected values for that month based on the measurements taken before the pandemic (p < 0.001). In addition, during the pandemic months, an average increase of 57,911 (95% CI 35,383–80,439) in the number of new additional single users who received care per month was observed as opposed to the prior month (p < 0.001). Figure 1 shows the change in the number of users for the pooled analyses. In addition, similar results were observed for the age, sex, and wealth quintile groups in the pooled analyses for SIS, EPS, and FISSAL (see Table 2).
Figure 1.

Interrupted time series analysis of the number of users who received care per month from January 2016 to December 2022. SIS comprehensive health insurance (in Spanish), EPS private healthcare entities (in Spanish), FISSAL intangible solidarity health fund (in Spanish).
Table 2.
Interrupted time series regression analysis for the number of users who received care.
| Coefficient | p | 95% CI | |||||
|---|---|---|---|---|---|---|---|
| SIS, EPS, and FISSAL | All users | Change in the number of users | − 1,782,446 | 0.000 | − 2,165,401 | − 1,399,490 | |
| (See Fig. 1) | Change in trend | 57,911 | 0.000 | 35,383 | 80,439 | ||
| Sex | Female | Change in the number of users | − 1,070,674 | 0.000 | − 1,304,861 | − 836,486 | |
| Change in trend | 34,694 | 0.000 | 20,983 | 48,404 | |||
| Male | Change in the number of users | − 711,772 | 0.000 | − 861,671 | − 561,872 | ||
| Change in trend | 23,218 | 0.000 | 14,341 | 32,095 | |||
| Age group | 0 − 11 | Change in the number of users | − 775,180 | 0.000 | − 924,827 | − 625,532 | |
| Change in trend | 22,246 | 0.000 | 14,019 | 30,473 | |||
| 12 − 17 | Change in the number of users | − 194,264 | 0.000 | − 240,556 | − 147,971 | ||
| Change in trend | 6441 | 0.000 | 3969 | 8913 | |||
| 18 − 64 | Change in the number of users | − 655,394 | 0.000 | − 831,290 | − 479,498 | ||
| Change in trend | 26,088 | 0.000 | 15,265 | 36,911 | |||
| 65 or over | Change in the number of users | − 157,608 | 0.000 | − 190,360 | − 124,855 | ||
| Change in trend | 3136 | 0.002 | 1161 | 5111 | |||
| Wealth quintile | Q1 | Change in the number of users | − 511,590 | 0.000 | − 632,458 | − 390,722 | |
| Change in trend | 13,694 | 0.000 | 6805 | 20,582 | |||
| Q2 | Change in the number of users | − 377,054 | 0.000 | − 462,041 | − 292,066 | ||
| Change in trend | 12,202 | 0.000 | 7237 | 17,167 | |||
| Q3 | Change in the number of users | − 306,688 | 0.000 | − 370,878 | − 242,498 | ||
| Change in trend | 10,642 | 0.000 | 6841 | 14,442 | |||
| Q4 | Change in the number of users | − 298,300 | 0.000 | − 355,946 | − 240,654 | ||
| Change in trend | 10,116 | 0.000 | 6639 | 13,594 | |||
| Q5 | Change in the number of users | − 288,814 | 0.000 | − 348,169 | − 229,458 | ||
| Change in trend | 11,257 | 0.000 | 7663 | 14,851 | |||
| SIS | All users | Change in the number of users | − 1,667,830 | 0.000 | − 2,028,320 | − 1,307,340 | |
| (See Fig. 2C) | Change in trend | 51,779 | 0.000 | 30,204 | 73,355 | ||
| Sex | Female | Change in the number of users | − 1,018,928 | 0.000 | − 1,242,834 | − 795,022 | |
| Change in trend | 31,765 | 0.000 | 18,513 | 45,017 | |||
| Male | Change in the number of users | − 648,902 | 0.000 | − 787,035 | − 510,768 | ||
| Change in trend | 20,014 | 0.000 | 11,614 | 28,415 | |||
| Age group | 0 − 11 | Change in the number of users | − 740,199 | 0.000 | − 885,050 | − 595,348 | |
| Change in trend | 20,693 | 0.000 | 12,665 | 28,721 | |||
| 12 − 17 | Change in the number of users | − 186,031 | 0.000 | − 231,256 | − 140,806 | ||
| Change in trend | 6069 | 0.000 | 3652 | 8486 | |||
| 18 − 64 | Change in the number of users | − 590,469 | 0.000 | − 750,171 | − 430,767 | ||
| Change in trend | 22,378 | 0.000 | 12,198 | 32,557 | |||
| 65 or over | Change in the number of users | − 151,131 | 0.000 | − 182,242 | − 120,020 | ||
| Change in trend | 2640 | 0.006 | 766 | 4514 | |||
| Wealth quintile | Q1 | Change in the number of users | − 509,975 | 0.000 | − 630,391 | − 389,560 | |
| Change in trend | 13,543 | 0.000 | 6681 | 20,406 | |||
| Q2 | Change in the number of users | − 371,488 | 0.000 | − 455,166 | − 287,810 | ||
| Change in trend | 11,797 | 0.000 | 6898 | 16,695 | |||
| Q3 | Change in the number of users | − 291,621 | 0.000 | − 352,660 | − 230,581 | ||
| Change in trend | 9627 | 0.000 | 5970 | 13,284 | |||
| Q4 | Change in the number of users | − 277,509 | 0.000 | − 331,114 | − 223,903 | ||
| Change in trend | 8837 | 0.000 | 5537 | 12,136 | |||
| Q5 | Change in the number of users | − 217,237 | 0.000 | − 263,814 | − 170,660 | ||
| Change in trend | 7976 | 0.000 | 4901 | 11,050 | |||
| FISSAL | All users | Change in the number of users | − 8634 | 0.013 | − 15,389 | − 1878 | |
| (see Fig. 2A) | Change in trend | 1128 | 0.000 | 748 | 1509 | ||
| Sex | Female | Change in the number of users | − 5163 | 0.023 | − 9593 | − 733 | |
| Change in trend | 780 | 0.000 | 529 | 1031 | |||
| Male | Change in the number of users | − 3470 | 0.004 | − 5823 | − 1118 | ||
| Change in trend | 349 | 0.000 | 219 | 479 | |||
| Age group | 0 − 11 | Change in the number of users | − 956 | 0.002 | − 1538 | − 373 | |
| Change in trend | 77 | 0.000 | 48 | 106 | |||
| 12 − 17 | Change in the number of users | − 241 | 0.033 | − 462 | − 20 | ||
| Change in trend | 37 | 0.000 | 25 | 49 | |||
| 18 − 64 | Change in the number of users | − 3971 | 0.057 | − 8060 | 118 | ||
| Change in trend | 692 | 0.000 | 461 | 923 | |||
| 65 or over | Change in the number of users | − 3466 | 0.001 | − 5442 | − 1490 | ||
| Change in trend | 323 | 0.000 | 212 | 433 | |||
| Wealth quintile | Q1 | Change in the number of users | − 930 | 0.002 | − 1502 | − 358 | |
| Change in trend | 106 | 0.000 | 74 | 139 | |||
| Q2 | Change in the number of users | − 1517 | 0.007 | − 2612 | − 423 | ||
| Change in trend | 177 | 0.000 | 114 | 239 | |||
| Q3 | Change in the number of users | − 2010 | 0.026 | − 3775 | − 244 | ||
| Change in trend | 278 | 0.000 | 182 | 375 | |||
| Q4 | Change in the number of users | − 2169 | 0.015 | − 3898 | − 441 | ||
| Change in trend | 298 | 0.000 | 201 | 394 | |||
| Q5 | Change in the number of users | − 2007 | 0.016 | − 3631 | − 383 | ||
| Change in trend | 269 | 0.000 | 176 | 363 | |||
| EPS | All users | Change in the number of users | − 105,982 | 0.000 | − 130,257 | − 81,707 | |
| (see Fig. 2B) | Change in trend | 5,004 | 0.000 | 3929 | 6078 | ||
| Sex | Female | Change in the number of users | − 46,583 | 0.000 | − 56,635 | − 36,531 | |
| Change in trend | 2149 | 0.000 | 1704 | 2,593 | |||
| Male | Change in the number of users | − 59,400 | 0.000 | − 73,715 | − 45,084 | ||
| Change in trend | 2855 | 0.000 | 2221 | 3489 | |||
| Age group | 0 − 11 | Change in the number of users | − 34,025 | 0.000 | − 39,484 | − 28,567 | |
| Change in trend | 1476 | 0.000 | 1232 | 1720 | |||
| 12 − 17 | Change in the number of users | − 7992 | 0.000 | − 9618 | − 6366 | ||
| Change in trend | 335 | 0.000 | 256 | 414 | |||
| 18 − 64 | Change in the number of users | − 60,954 | 0.000 | − 79,372 | − 42,536 | ||
| Change in trend | 3018 | 0.000 | 2201 | 3836 | |||
| 65 or over | Change in the number of users | − 3011 | 0.000 | − 4154 | − 1868 | ||
| Change in trend | 174,174 | 0.000 | 128 | 220 | |||
| Wealth quintile | Q1 | Change in the number of users | − 685 | 0.000 | − 825 | − 545 | |
| Change in trend | 44 | 0.000 | 37 | 51 | |||
| Q2 | Change in the number of users | − 4048 | 0.000 | − 4981 | − 3116 | ||
| Change in trend | 228 | 0.000 | 185 | 271 | |||
| Q3 | Change in the number of users | − 13,058 | 0.000 | − 16,115 | − 10,000 | ||
| Change in trend | 737 | 0.000 | 599 | 875 | |||
| Q4 | Change in the number of users | − 18,621 | 0.000 | − 23,120 | − 14,123 | ||
| Change in trend | 982 | 0.000 | 782 | 1182 | |||
| Q5 | Change in the number of users | − 69,570 | 0.000 | − 85,354 | − 53,786 | ||
| Change in trend | 3012 | 0.000 | 2317 | 3707 | |||
Change in the number of users at the beginning of the COVID-19 pandemic (change in the intercept). Change in the monthly trend regarding the number of users who received care during the pandemic (change in the slope [interaction]). SIS comprehensive health insurance (in Spanish). EPS private healthcare entities (in Spanish), FISSAL intangible solidarity health fund (in Spanish).
A counterfactual analysis was conducted to determine the impact of the pandemic on the number of single users who received care per month in the three IAFAS types (SIS, EPS, and FISSAL) and reported that the number of users who received care during the pandemic decreased by 26,332,506 (95% CI − 35,205,715–− 17,459,297; p < 0.001). This figure represents the number of users who did not receive medical care from March 2020 to December 2022 because of the pandemic, as opposed to a non-pandemic scenario.
The individual analyses conducted for each insurance institution indicated similar findings. Regarding users affiliated with the SIS, an average decrease of 2,028,320 in the number of users was observed (95% CI − 2,028,320–− 1,307,340) as opposed to the values expected for that month at the beginning of the COVID-19 pandemic in Peru (see Fig. 2C). Moreover, an average decrease of 8634 was identified for FISSAL (95% CI − 15,389–− 1878) and 105,982 for EPS (95% CI − 130,257–− 81,707) for the number of single users who received care during the first month of the pandemic (see Fig. 2A and B, respectively). This decrease was significant in all cases (p < 0.05).
Figure 2.
Interrupted time series analysis of the number of users who received care by type of health insurance funds administrative institution. (A) For the intangible solidarity health fund (FISSAL). (B) For healthcare entities (EPS). (C) For the comprehensive health system (SIS).
Regarding the SIS, an increasing trend of 5,004 was observed (95% CI 3929–6078) in the number of single users per month, meaning an average of more than five thousand new single users was observed in the SIS. As of FISSAL and EPS, a trend of 1128 (95% CI 748 to 1509) and 5004 (95% CI 3929 to 6078) was found for new single users per month. The increase was significant in all cases (p < 0.05). Other coefficients in the time series analyses can be seen in Supplementary Material 1.
Users by type of chronic disease
According to the time series analyses of the users who received care by the SIS, EPS, and FISSAL per month conducted for each group of chronic diseases based on Charlson’s classification17, there was a significant decrease in the number of users at the beginning of the pandemic for all diagnostic groups (see Table 3). A considerable decrease was observed in the first month of the pandemic compared to the previous months (p < 0.05). The most significant decreases include individuals with diabetes without complications and chronic pulmonary disease, with a decrease of 33,447 (p < 0.001; 95% CI − 43,781–− 23,114) and 31,365 (p < 0.001; 95% CI − 38,386–− 24,344) users per month, respectively.
Table 3.
Interrupted time series regression analysis for the number of users who received care by SIS, EPS, and FISSAL by type of Charlson’s disease.
| Coefficient | p | 95% CI | |||
|---|---|---|---|---|---|
| Cancer | Change in the number of users | − 21,249 | 0.000 | − 29,070 | − 13,428 |
| Change in trend | 1175 | 0.000 | 703 | 1647 | |
| Solid metastatic tumor | Change in the number of users | − 716 | 0.000 | − 977 | − 455 |
| Change in trend | 67 | 0.000 | 44 | 89 | |
| Dementia | Change in the number of users | − 1067 | 0.000 | − 1255 | − 879 |
| Change in trend | 22 | 0.002 | 8 | 35 | |
| Diabetes with complications | Change in the number of users | − 6204 | 0.000 | − 7336 | − 5073 |
| Change in trend | 35 | 0.347 | − 39 | 109 | |
| Diabetes without complications | Change in the number of users | − 33,447 | 0.000 | − 43,781 | − 23,114 |
| Change in trend | 1153 | 0.003 | 412 | 1895 | |
| Cerebrovascular disease | Change in the number of users | − 3950 | 0.000 | − 4719 | − 3182 |
| Change in trend | 77 | 0.004 | 25 | 130 | |
| Mild liver disease | Change in the number of users | − 7347 | 0.000 | − 8551 | − 6143 |
| Change in trend | 141 | 0.000 | 65 | 218 | |
| Moderate liver disease | Change in the number of users | − 649 | 0.000 | − 754 | − 544 |
| Change in trend | 12 | 0.000 | 6 | 19 | |
| Chronic pulmonary disease | Change in the number of users | − 31,365 | 0.000 | − 38,386 | − 24,344 |
| Change in trend | 695 | 0.000 | 357 | 1033 | |
| Kidney disease | Change in the number of users | − 8741 | 0.000 | − 10,545 | − 6937 |
| Change in trend | 124 | 0.018 | 22 | 227 | |
| Rheumatic disease | Change in the number of users | − 7518 | 0.000 | − 9005 | − 6030 |
| Change in trend | 185 | 0.000 | 87 | 283 | |
| Peptic ulcer | Change in the number of users | − 1206 | 0.000 | − 1453 | − 960 |
| Change in trend | 41 | 0.000 | 26 | 57 | |
| Peripheral vascular disease | Change in the number of users | − 512 | 0.000 | − 597 | − 426 |
| Change in trend | 11 | 0.000 | 5 | 17 | |
| Myocardial infarction | Change in the number of users | − 364 | 0.000 | − 462 | − 267 |
| Change in trend | 8 | 0.019 | 1 | 14 | |
| Congestive heart failure | Change in the number of users | − 3734 | 0.000 | − 4340 | − 3129 |
| Change in trend | 46 | 0.025 | 6 | 86 | |
| Paraplegia and hemiplegia | Change in the number of users | − 1248 | 0.000 | − 1465 | − 1032 |
| Change in trend | 34 | 0.000 | 20 | 49 | |
| AIDS/HIV | Change in the number of users | − 5363 | 0.000 | − 6581 | − 4144 |
| Change in trend | 101 | 0.016 | 19 | 182 | |
Change in the number of users at the beginning of the COVID-19 pandemic (change in the intercept). Change in the monthly trend regarding the number of users who received care during the pandemic (change in the slope [interaction]). SIS comprehensive health insurance (in Spanish). EPS private healthcare entities (in Spanish). FISSAL intangible solidarity health fund (in Spanish).
However, during the pandemic, we observed an increasing number of users with these diseases in all Charlson’s diagnosis groups (p < 0.05), except for monthly users with diabetes with complications. A significant increase was found in the number of monthly users from the groups of cancer and diabetes without complications, with 1,175 (p < 0.001; 95% CI 703–1647) and 1153 (p = 0.003; 95% CI 412–1895) new users per month, respectively. Table 3 shows the rest of Charlson’s diseases, and Supplementary Material 2 shows other indicators of the time series analyses.
Discussion
Our study evaluated the impact of the COVID-19 pandemic on services provided to people with chronic diseases in Peru from 2016 to 2022 and showed a significant decrease in the number of users who received care during the first month of the pandemic as opposed to prior measurements. This decrease was observed in the pooled analysis of IAFAS (SIS, EPS, and FISSAL) and the individual analyses conducted for each type of insurer. In addition, we identified an average monthly increase in the number of users who received care during the pandemic as opposed to the previous month, which suggests a gradual recovery in the demand for healthcare services.
Our findings revealed a similar pattern regarding the number of users who received care per month and had chronic diseases based on Charlson’s classification17. There was a significant decrease in the number of users at the beginning of the pandemic, followed by an increasing trend during the pandemic, except for individuals with diabetes and complications. Nevertheless, we should highlight that the proportion of individuals with Charlson’s chronic diseases was lower in all cases during the pandemic than before. This finding suggests that many subjects with chronic diseases could not receive the care they needed during the pandemic since the health system prioritized responding to and caring for COVID-19 cases, failing to meet other demands21.
Our study identified that the Peruvian health system achieved a partial or complete recovery and could provide care for several patients similar to the one before the pandemic. However, there is still an open gap in the care provided during the pandemic. From March 2020 to December 2022, 26,332,506 individuals failed to receive care, which shows a significant interruption in healthcare and highlights the negative consequences of the pandemic regarding access to healthcare services. This occurred despite the implementation of strategies such as telemedicine to expand the services offered (teleinterconsultation, teleconsultation, teleorientation, telemonitoring, and diagnosis telesupport) as well as policies addressing the four axes of digital health (telemedicine, teletraining, telemanagement and teleinformation, and education and communication)22. We should highlight that users who did not receive care may have experienced considerable delay in the diagnosis, treatment, and follow-up of their conditions, which could potentially affect their long-term health and well-being. In addition, closing this gap would require significant public and private investments, which is discouraging given the finite healthcare capacity of the system. Even though the budget for health insurance significantly increased in Peru during the pandemic to address this health emergency23, its negative impact on healthcare access could not be avoided. Complete recovery of the healthcare capacity lost during the pandemic will require consistent efforts and effective strategies to address this cumulative delay and ensure equitable access to healthcare for all affected users.
During the first year of the pandemic, a systematic review encompassing 20 countries reported a 37% reduction in the general use of health services; this value is higher in subjects with chronic or severe health conditions14. In addition, a systematic review of 22 studies conducted in low- and middle-income African countries suggested that the decrease in the healthcare services provided during the pandemic may be due to the lack of adequate equipment, protocols to face health crises, and solid policies for remote care and limited resources24. Similar situations have been observed in Peru since its fragmented health system, lack of specialized health personnel before the pandemic and death of health personnel or leaves granted to them during the pandemic, as well as limited health budget, are the reasons why adequate care could not be provided25. This may account for the considerably reduced number of users who received care at the beginning of the pandemic. We should highlight that a limited number of health professionals available in the Peruvian health system is still being estimated. Medical training and residencies were delayed during the pandemic, so the chance to recover healthcare capacity may be obstructed by issues associated with the availability of human resources, as well as the fact that training opportunities are not equitably distributed throughout regions26.
Even though there still is an open gap in the number of healthcare services provided by the overall Peruvian health system during the pandemic up to 2022, this gap has been closed in some areas. An analysis of the mental care provided in Peru presented that, after 9 months, community mental health centers could provide care to the same number of users that had received care before the pandemic16. This achievement may be partially due to the increase in the prevalence of mental health issues during the pandemic in Peru18, resulting in a higher demand. Additionally, it is important to consider that this successful recovery may be due to the implementation of specific strategies during the COVID-19 pandemic and the increased resources destined for mental health27.
We consider two possible explanations for the fact that the number of people with diabetes with complications did not increase significantly during the pandemic. First, the nature of having diabetes with complications may have meant that patients with an additional complication, such as diabetic foot, were unable to access necessary care during the pandemic, resulting in deaths due to lack of access to timely care28. Second, having diabetes increased the likelihood of complications and mortality in the early years of the pandemic, as COVID-19 infection in these patients had a more severe prognosis compared to individuals without chronic disease29.
Some results were not equivalent between the pooled analysis and each of the Peruvian health subsystems, as in the case of FISSAL with specific individuals aged 18 to 64 years. This may be due to differences in the specific populations served by each system, for example, FISSAL covers care for high-cost diseases, which could generate different conditions than the other health subsystems in the context of the pandemic.
Strengths and limitations
The main strength of our study is that it contains the highest amount of information on the Peruvian health system collected up to date to assess the pandemic’s impact on healthcare services. As a result, we have acquired a wide and representative perspective of the situation and gained a better understanding of the implications of the pandemic on the access to and use of healthcare services in Peru. Given the considerable sample size of the study, our findings are more robust and can be generalized.
For the other hand, there are some limitations. Firstly, even though a significant percentage of all healthcare services of the Peruvian health system were included, other important subsystems were excluded, such as the Social Security Administration of Peru (EsSalud), which finances the services provided to around 29.9% of the Peruvian population. This may imply that our findings only partially represent some aspects of the medical care provided during the pandemic. Secondly, Peru does not have open-access clinical databases that comply with international health standards. Despite that, our study uses an administrative service database that includes the leading national health financing entities. Third, we use data from different subsystems of the Peruvian health system, which are subject to standardization processes for integration into a single database. Although there may be some inconsistent or erroneous cases in the records, we expect the proportion of these data to be minimal. In addition, these limitations are common in large health databases in low- and middle-income countries. Fourth, the variable of chronic disease diagnoses in our database may suffer from underreporting, recording errors, or other problems typical of low- and middle-income countries. However, we believe that these errors, if they exist, would be minimal and would not have a significant impact on the results of our study, so the findings should retain their validity.
Conclusions
Our study aimed to assess the impact of the COVID-19 pandemic on a wide set of users, with a total of 21,281,128 users receiving care per month in Peru from 2016 to 2022. Our findings reported a significant decrease in the number of users who received care during the first month of the pandemic, followed by an increasing trend (March 2020–December 2022). A positive aspect that should be highlighted is that the Peruvian health system recovered its capacity to provide healthcare since the number of users who received care per month by December 2022 was similar to that before the pandemic. We should mention that an estimated gap of 26,332,506 users who failed to receive care per month was observed during the pandemic.
Based on these findings, policies and strategies should be developed to strengthen both the public and private Peruvian health systems. Approaching this healthcare gap is essential to ensure that users who failed to receive care during the pandemic can access the necessary healthcare services. These policies should focus on improving the capacity to provide healthcare and the distribution of resources, as well as applying effective measures to close the healthcare gap and mitigate the long-term negative effects on the health and well-being of the Peruvian population. Additionally, databases that can be operated between subsystems and comply with international health standards should be developed to be used to make health-related decisions.
Supplementary Information
Author contributions
D.V.Z. and L.B.B. contributed to the conception of the idea. L.B.B. and D.V.Z. jointly designed the study. All authors participated in the interpretation of the data. D.V.Z. wrote the initial draft of the manuscript. D.V.Z., L.B.B., A.E., M.P.C. and P.V.M. critically reviewed and approved the final version of the article, accepting responsibility for the accuracy and completeness of the entire work.
Funding
The funding was supported by Dirección de Investigación de la Universidad Peruana de Ciencias Aplicadas (A-093-2024).
Data availability
This research used the freely accessible databases, available on the open data platform of SUSALUD (http://datos.susalud.gob.pe/dataset). It should be noted that the data are available in an anonymized form and do not allow identification of the users, therefore, the approval of an ethics committee will not be necessary, as we will not be working directly with the subjects included.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: David Villarreal-Zegarra and Luciana Bellido-Boza.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-54275-7.
References
- 1.Balasuriya L, et al. Impacts of the COVID-19 pandemic on nationwide chronic disease prevention and health promotion activities. Am. J. Prev. Med. 2023;64:452–458. doi: 10.1016/j.amepre.2022.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organitation. Universal health coverage (UHC). https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc) (2022).
- 3.Wikström K, Linna M, Laatikainen T. The impact of the COVID-19 pandemic on incident cases of chronic diseases in Finland. Eur. J. Public Health. 2022;32:982–984. doi: 10.1093/eurpub/ckac107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He W, et al. Changes in lifestyles and depressive symptom among patients with chronic diseases during COVID-19 lockdown. Sci. Rep. 2022;12:11407. doi: 10.1038/s41598-022-15333-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ismail H, Marshall VD, Patel M, Tariq M, Mohammad RA. The impact of the COVID-19 pandemic on medical conditions and medication adherence in people with chronic diseases. J. Am. Pharm. Assoc. JAPhA. 2022;62:834–839.e831. doi: 10.1016/j.japh.2021.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu H, Chen S, Liu M, Nie H, Lu H. Comorbid chronic diseases are strongly correlated with disease severity among COVID-19 patients: A systematic review and meta-analysis. Aging Dis. 2020;11:668–678. doi: 10.14336/ad.2020.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Darrudi A, KetabchiKhoonsari MH, Tajvar M. Challenges to achieving universal health coverage throughout the world: A systematic review. J. Prev. Med. Public Health Yebang Uihakhoe chi. 2022;55:125–133. doi: 10.3961/jpmph.21.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allen EM, Call KT, Beebe TJ, McAlpine DD, Johnson PJ. Barriers to care and health care utilization among the publicly insured. Med. Care. 2017;55:207–214. doi: 10.1097/mlr.0000000000000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barasa E, Kazungu J, Nguhiu P, Ravishankar N. Examining the level and inequality in health insurance coverage in 36 sub-Saharan African countries. BMJ Glob. Health. 2021 doi: 10.1136/bmjgh-2020-004712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Organización Panamericana de la Salud. Salud en las Américas (Organización Mundial de la Salud, 2017).
- 11.Superintendencia Nacional de Salud. Registro Nominal de Asegurados al 26 de Junio del 2023. (Superintendencia Nacional de Salud, 2023).
- 12.de Salud M. Seguro Integral de Salud. Ministerio de Salud; 2019. [Google Scholar]
- 13.Ministerio de Salud. Seguro Integral de Salud [Resolución Secretarial N.° 133–2022/SIS/SG]. (Ministerio de Salud, 2022).
- 14.Moynihan R, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open. 2021;11:e045343. doi: 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bong CL, et al. The COVID-19 pandemic: Effects on low- and middle-income countries. Anesth. Analg. 2020;131:86–92. doi: 10.1213/ane.0000000000004846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Villarreal-Zegarra D, et al. Provision of community mental health care before and during the COVID-19 pandemic: A time series analysis in Peru. Int. J. Soc. Psychiatry. 2023 doi: 10.1177/00207640231185026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Villarreal-Zegarra D, et al. Estimated impact of the COVID-19 pandemic on the prevalence and treatment of depressive symptoms in Peru: An interrupted time series analysis in 2014–2021. Soc. Psychiatry Psychiatr. Epidemiol. 2023 doi: 10.1007/s00127-023-02446-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Newey WK, West KD. A simple, positive semi-definite, heteroskedasticity and autocorrelation consistent covariance matrix. Econometrica. 1987;55:703–708. doi: 10.2307/1913610. [DOI] [Google Scholar]
- 20.Baum CF, Schaffer ME, Stillman S. Enhanced routines for instrumental variables/generalized method of moments estimation and testing. Stata J. 2007;7:465–506. doi: 10.1177/1536867X0800700402. [DOI] [Google Scholar]
- 21.World Health Organitation. La COVID-19 afectó el funcionamiento de los servicios de salud para enfermedades no transmisibles en las Américas. https://www.paho.org/es/noticias/17-6-2020-covid-19-afecto-funcionamiento-servicios-salud-para-enfermedades-no (2020).
- 22.de Salud M. Documento Técnico: Plan Nacional de Telesalud del Perú 2020–2023. Ministerio de Salud; 2020. [Google Scholar]
- 23.Presidenta del Consejo de Ministros. Decreto de urgencia que dicta medidas extraordinarias y urgentes en materia económica y financiera para fortalecer el aseguramiento universal en salud en el marco de la emergencia nacional por la COVID-19 (Presidenta del Consejo de Ministros, 2021).
- 24.Tessema GA, et al. The COVID-19 pandemic and healthcare systems in Africa: A scoping review of preparedness, impact and response. BMJ Glob. Health. 2021 doi: 10.1136/bmjgh-2021-007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carrillo-Larco RM, et al. Peru—Progress in health and sciences in 200 years of independence. Lancet Reg. Health Am. 2022;7:100148. doi: 10.1016/j.lana.2021.100148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.García-Serna J, et al. Characteristics of undergraduate, second speciality and sub-speciality mental health programmes in Peru: A scoping review. Researchsquare. 2022 doi: 10.21203/rs.3.rs-1303396/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Salud M. Plan de Salud Mental en el Contexto de COVID-19. Ministerio de Salud; 2020. [Google Scholar]
- 28.Salazar Salazar, A. A. & Varillas Valencia, M. Asociación entre la prevalencia de enfermedades no transmisibles y el exceso de muertes en personas mayores de 15 años durante la pandemia por COVID19 en el Perú. Professional degree of Bachelor in Nutrition and Dietetics, thesis, Universidad Peruana de Ciencias Aplicadas (2023).
- 29.More Bustos, H. A. C. & Bejarano Ramos, P. B. Muertes asociadas a la diabetes mellitus en el Perú entre los años 2017–2022. Professional degree of medical doctor thesis, Universidad Peruana Cayetano Heredia (2023).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This research used the freely accessible databases, available on the open data platform of SUSALUD (http://datos.susalud.gob.pe/dataset). It should be noted that the data are available in an anonymized form and do not allow identification of the users, therefore, the approval of an ethics committee will not be necessary, as we will not be working directly with the subjects included.