Abstract
Objective:
To describe cardiac rehabilitation (CR) utilization in a cohort of Medicare beneficiaries eligible for CR events in 2017.
Patients and Methods:
We identified Medicare fee-for-service beneficiaries who experienced a CR-eligible event in January 2017 and assessed their CR participation (one or more CR sessions in 365 days), engagement, and completion (36 or more sessions in 36 weeks) rates through September 7, 2019. Measures were assessed overall, by beneficiary characteristics and state of residence, and by primary (myocardial infarction; coronary artery bypass surgery; heart valve repair/replacement; percutaneous coronary intervention; or heart/heart-lung transplant) and secondary (angina; heart failure) qualifying event type.
Results:
In 2017, 412,080 Medicare beneficiaries had a primary CR-eligible event and 28.6% completed at least one session of CR within 365 days after discharge from a qualifying event. Among beneficiaries who completed at least one CR session, the mean total number of visits was 25±12 and 27.6% completed 36 or more sessions. Nebraska had the highest enrollment rate (56.1%), with 4 other states also achieving an enrollment rate above 50% and 23 states falling below the over-all rate for the United States
Conclusion:
Enrollment into CR after hospitalization among Medicare beneficiaries in the United States was likely modestly improved in 2017, compared with 2016. However, the absolute enrollment, engagement, and program completion rates remain low, indicating that many patients did not benefit or fully benefit from a class I guideline-recommended therapy. Additional research and continued widespread dissemination and adoption of existing successful initiatives are needed, especially among identified populations.
Keywords: Medicare, cardiac rehabilitation, utilization, 2017
Exercise-based cardiac rehabilitation (CR) is an underutilized service with well documented clinical and functional benefits for patients with cardiovascular disease1–4. To address this long-standing utilization gap, over the past decade several professional, governmental and private organizations have adopted performance measures and developed strategies that target increasing enrollment, engagement and completion of CR.5–8 One such approach is Million Hearts, a national initiative co-led by the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare & Medicaid Services (CMS), with the goal of preventing one million acute cardiovascular events in five years. In 2015, Million Hearts convened a CR Collaborative (Collaborative), a forum of multi-disciplinary professionals which included in its roadmap a goal to increase CR participation to 70% by 2022.9,10
We previously reported CR enrollment and engagement metrics in a cohort of Medicare fee-for-service (FFS) beneficiaries hospitalized in 2016 with a qualifying event,11 representing an older adult patient group with multiple morbidities that are known to benefit from CR.12,13 Using administrative claims, over-all enrollment (i.e., at least 1 CR visit in 1 year) was 24.4%, which is generally consistent with other disease- and state-specific data.14,15 Additionally, participation in CR varied based on age, race, gender, type of qualifying event, and geographic region.11,14–22 To assist with ongoing efforts to improve CR-related performance metrics and help monitor progress toward the Collaborative’s goal, providing contemporary surveillance data remains important.
This study updates CR utilization data in a cohort of Medicare beneficiaries hospitalized for CR-eligible events in 2017, including stratification by select patient demographics and state of residence. It also provides an updated methodology for using claims data to assess CR utilization in other patient populations.
METHODS
The sample for this study included all United States Medicare FFS beneficiaries aged ≥ 65 years who had a CR qualifying event between January 1, 2017 and December 31, 2017. Data were derived from the CMS Virtual Research Data Center for Medicare Part A and Part B claims during 2017, 2018 and through September 7, 2019. In alignment with Medicare’s benefit guidance,23,24 beneficiaries were considered eligible for outpatient CR if they experienced one or more of the following during 2017 (referred to collectively as primary qualifying events): hospitalization for acute myocardial infarction (MI); coronary artery bypass graft (CABG) surgery; heart valve repair or replacement; percutaneous coronary intervention (PCI); or heart or heart-lung transplant. Events were identified based on beneficiaries’ receipt of specified International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis (first- or second-listed code) or procedural codes (any location) on inpatient claims or current procedural terminology (CPT) codes (any location) on outpatient or provider claims (Table in the Supplement). Unlike our prior paper that only included patients who underwent a PCI as part of hospitalization,11 the current analysis also includes patients who underwent an elective PCI and were not hospitalized over-night, a so-called “same-day discharge”.
Beneficiaries without a primary qualifying event were also considered CR-eligible if they currently had documented stable angina pectoris or chronic heart failure during 2017 (referred to collectively as secondary qualifying events). Angina was defined as having a specified ICD-10-CM code (in any location) on two or more outpatient claims (Table in the Data Supplement). Heart failure was defined in two ways to match Medicare’s clinical eligibility criteria for CR (CMS 2014). Diagnosis-based heart failure was defined as having a specified ICD-10-CM code (any location) for chronic systolic (or systolic/diastolic) heart failure on two or more outpatient claims or on an inpatient claim with no subsequent cardiovascular disease-related hospitalization occurring within 6 weeks (see Supplement). Procedure-based heart failure was defined as having a specified ICD-10-CM procedure code or current procedural terminology (CPT) code in an inpatient or outpatient encounter for either insertion of an implantable ventricular assist device or biventricular pacemaker (see Supplement).
Data are described using standard statistical summary measures such as means and standard deviations for continuous variables and percentages for count data. To be included in the analyses, beneficiaries had to be alive for >21 days after their qualifying event; have continuous Medicare Part A and Part B enrollment for 12 or more months after their qualifying event unless they died; not be a nursing home resident (defined as 90 or more consecutive days of skilled nursing facility care); not receive hospice care either before the qualifying event or for 21 or less days after discharge for the initial qualifying event; and not be entitled to Medicare benefits due to end-stage renal disease. Among beneficiaries with more than 1 primary qualifying event, the first event was considered the index event. Beneficiaries with multiple primary qualifying events occurring within 21 days were recoded as combinations (e.g., MI with CABG). Additional steps were taken to identify the index date among beneficiaries meeting the angina and heart failure criteria (Methods in the Supplement).
An outpatient CR session was defined as having a Healthcare Common Procedure Coding System code for physician services for outpatient CR with (93798) or without (93797) continuous electrocardiographic monitoring or intensive CR with or without continuous electrocardiographic monitoring and with (G0422) or without (G0423) exercise, in combination with a place of service code of 11 (office), 19 (off-campus outpatient hospital), or 22 (on-campus outpatient hospital).
Three CR utilization-related factors were assessed. First, enrollment rate, defined as the percentage of eligible beneficiaries who participated in CR, represents a CR-eligible beneficiary participating in one or more CR sessions within 21, 90, and 365 days after discharge from a qualifying event. The discharge date was defined as the latter of procedure date or the hospital discharge date that occurred during the 21-day period after the qualifying event. Timely initiation was defined as CR enrollment in 21 days or less because it aligns with the definition of a quality measure endorsed by major societies.5 Time to enrollment was expressed as the mean number of days from the latter of procedure date or hospital discharge date to date of CR enrollment. Second, among patients that attend at least one CR session in 365 days, engagement describes the total number of CR sessions attended by the beneficiary within 36 weeks of their first CR session and was expressed as both mean total sessions completed and percentage of patients completing ≥2, ≥12, and ≥24 sessions, with the latter representing an important threshold for conveying health benefits.25 Third, completion rate refers to the percentage of beneficiaries completing 36 or more CR sessions. Data pertinent to both engagement and completion of CR are expressed within 36 weeks of their first CR session, because that is the period when Medicare will pay for standard CR once a patient has started (CMS 2006 and 2014). Also, we report utilization rates corresponding to the recent CR-specific Healthcare Effectiveness Data and Information Set (HEDIS) measures that address initiation in 30 days, level of engagement in 90 and 180 days, and achievement in 180 days.7
The above three CR utilization-related factors were also stratified by age, sex, race/ethnicity, dual Medicare and Medicaid coverage status, and the beneficiary’s primary state of residence. This research was considered exempt from Institutional Review Board review under 45 Code of Federal Regulations 46.101[b] [5] which covers Department of Health and Human Services research and demonstration projects which are designed to study, evaluate, or examine public benefit or service programs.
RESULTS
In 2017, 412,080 Medicare beneficiaries (77±8 years old, 59.7% men, 86.3 non-Hispanic White) had a primary CR-eligible event (Table 1), among whom 117,794 (28.6%) completed at least 1 session of CR within 365 days. Enrollment rates tended to be higher in men (31.9%), those aged 65–74 years (34.3%), Non-Hispanic Whites (30.0%), and those undergoing CABG surgery (56.6%). Over-all, the mean elapsed time between hospital discharge and first CR session was 45 ±52 days, and this period tended to be longer in women, Non-Hispanic Blacks, beneficiaries age ≥85 years, and those having experienced an acute MI with no revascularization procedure. Among beneficiaries with at least one CR visit within 365 days, 10.1% started withing 21 days.
Table 1.
Cardiac Rehabilitation Enrollment, Engagement and Completion Among Medicare Beneficiaries Aged ≥65 years Who Had a Primary Qualifying Event in 2017
| Eligible N | Enrollment/Initiation | Engagement/Participation** | Completion/ Achievement** | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ≥1 Session in ≤ 21 d (%)* | ≥1 Session in ≤ 90 d (%)* | ≥1 Session in ≤ 365 d (%)* | Number of Days from Discharge to First Billed CR Session (Mean ± SD)** | Number of Sessions in 36 wk (Mean ± SD) | ≥ 2 Sessions in 36 wk (%) | ≥ 12 Sessions in 36 wk (%) | ≥ 24 Sessions in 36 wk (%) | ≥ 36 Sessions in 36 wk (%) | ||
| Total | 412080 | 10.1 | 25.4 | 28.6 | 45±52 | 25±12 | 96.1 | 80.4 | 60.1 | 27.6 |
| Age (yr) | ||||||||||
| 65–74 | 198228 | 12.3 | 30.7 | 34.3 | 44±51 | 25±12 | 96.2 | 80.7 | 60.1 | 27.8 |
| 75–84 | 150026 | 9.7 | 24.5 | 27.8 | 46±53 | 25±12 | 96.1 | 80.7 | 61.0 | 28.0 |
| ≥ 85 | 63826 | 4.2 | 10.9 | 12.6 | 49±54 | 23±13 | 94.8 | 76.1 | 55.1 | 24.5 |
| Sex | ||||||||||
| Men | 246073 | 11.6 | 28.5 | 31.9 | 44±51 | 26±12 | 96.3 | 82.0 | 62.0 | 29.0 |
| Women | 166007 | 7.8 | 20.7 | 23.7 | 48±53 | 24±13 | 95.7 | 77.2 | 56.2 | 24.9 |
| Race/Ethnicity *** | ||||||||||
| Non-Hispanic White | 355480 | 10.7 | 26.07 | 30.0 | 45±52 | 25±12 | 96.1 | 80.6 | 60.0 | 27.7 |
| Non-Hispanic Black | 22305 | 4.5 | 14.5 | 17.3 | 55±60 | 25±13 | 95.6 | 78.6 | 61.7 | 29.2 |
| Hispanic | 17014 | 4.9 | 13.8 | 16.0 | 51±57 | 24±13 | 94.3 | 75.8 | 57.8 | 25.1 |
| Asian | 7660 | 5.0 | 16.3 | 18.9 | 52±55 | 24±12 | 96.0 | 79.7 | 59.3 | 25.6 |
| Dual Medicare/Medicaid Coverage **** | ||||||||||
| No | 374619 | 10.8 | 27.1 | 30.5 | 45±52 | 25±12 | 96.3 | 81.0 | 60.6 | 27.9 |
| Yes | 37461 | 2.8 | 7.6 | 9.2 | 55±64 | 19±14 | 90.0 | 62.4 | 42.5 | 17.8 |
| Primary Qualifying Event ***** | ||||||||||
| AMI | 196259 | 7.3 | 17.7 | 20.2 | 47±55 | 25±12 | 96.8 | 80.6 | 60.5 | 27.7 |
| With procedure | 88019 | 14.1 | 33.6 | 37.1 | 42±47 | 25±12 | 97.1 | 81.3 | 61.3 | 28.4 |
| No procedure | 108240 | 1.8 | 4.9 | 6.5 | 67±76 | 24±13 | 95.4 | 76.9 | 56.7 | 24.7 |
| CABG | 55378 | 20.3 | 52.1 | 56.6 | 40±41 | 27±12 | 98.1 | 85.3 | 65.3 | 30.5 |
| With AMI | 16205 | 20.0 | 46.6 | 51.0 | 40±43 | 26±12 | 97.8 | 84.2 | 64.4 | 30.3 |
| No AMI | 39173 | 20.4 | 54.3 | 59.0 | 41±41 | 27±11 | 98.2 | 85.7 | 65.7 | 30.6 |
| PCI | 206860 | 11.5 | 27.5 | 31.0 | 45±54 | 24±13 | 94.9 | 78.3 | 57.9 | 27.0 |
| With AMI | 72712 | 13.0 | 31.2 | 34.5 | 43±48 | 25±13 | 96.9 | 80.6 | 60.4 | 27.8 |
| No MI | 134148 | 10.6 | 25.5 | 29.1 | 47±57 | 24±13 | 93.6 | 76.8 | 56.3 | 26.4 |
| Heart Valve | 56870 | 13.0 | 36.8 | 41.0 | 45±46 | 25±12 | 97.4 | 82.6 | 61.2 | 27.5 |
| With AMI | 2536 | 13.6 | 32.5 | 37.3 | 45±49 | 26±12 | 96.7 | 82.5 | 63.3 | 29.5 |
| No AMI | 54334 | 13.0 | 37.0 | 41.2 | 45±45 | 25±12 | 97.4 | 82.6 | 61.5 | 27.4 |
| TAVR only | 21738 | 8.6 | 26.4 | 29.7 | 48±47 | 24±12 | 96.3 | 77.1 | 55.4 | 23.8 |
| Heart Transplant | 439 | 10.0 | 28.3 | 37.4 | 62±57 | 27±11 | 97.6 | 84.2 | 70.1 | 27.4 |
| With AMI | 4 | 0.0 | 50.0 | 50.0 | 41±26 | 37±1 | 100.0 | 100.0 | 100.0 | 100.0 |
| No AMI | 435 | 10.1 | 28.1 | 37.2 | 63±57 | 27±11 | 97.5 | 84.0 | 69.8 | 26.5 |
| CABG & heart valve | 10219 | 19.4 | 50.8 | 55.8 | 42±44 | 27±11 | 97.8 | 86.2 | 65.3 | 31.4 |
CR=cardiac rehabilitation, AMI=acute myocardial infarction, CABG=coronary artery bypass surgery, PCI=percutaneous coronary intervention, TAVR=transcatheter aortic valve replacement/repair,
Among all eligible beneficiaries,
Among all beneficiaries with at least one CR session,
Unknown and “other” race and ethnicity groups not shown,
Dual eligible here only includes those age 65+, per overall inclusion criteria,
Eligible conditions/procedures that occurred in combination had to occur within 21 days of each other
Several levels of engagement in CR, as measured over 36 weeks after initiation, are also described in Table 1. The mean and the median (data not shown in table) total number of visits for all patients who completed at least 1 session was 25±12 sessions and 29 (interquartile range: 15 – 36), respectively. Completion of at least 12 and 24 sessions tended to be more frequent in men, those undergoing CABG surgery, and people < 85 years of age. Among beneficiaries who completed at least one CR session, 27.6% completed 36 or more CR sessions, and this measure of program completion also tended to be higher in men, those undergoing CABG surgery, and those < 85 years of age.
Table 2 provides the same information about enrollment, engagement and completion of CR for beneficiaries with a secondary qualifying event of angina or heart failure. Enrollment in CR, defined as ≥ 1 session in 365 days, was low for both conditions (angina: 3.9%; heart failure: 2.6%). Among beneficiaries with heart failure, enrollment, engagement, and completion of CR was observed to be highest among those receiving a ventricular assist device at 44.3%, 27 sessions, and 31.4%, respectively.
Table 2.
Cardiac Rehabilitation Enrollment, Engagement and Completion Among Medicare Beneficiaries Aged ≥65 years Who Had a Secondary Qualifying Event in 2017
| Eligible N8453 | Enrollment/Initiation | Engagement/Participation** | Completion/ Achievement** | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ≥1 Session in ≤ 21 d (%)* | ≥1 Session in ≤ 90 d (%)* | ≥1 Session in ≤ 365 d (%)* | Number of Days from Discharge to First Billed CR Session (Mean ± SD)** | Number of Sessions in 36 wk (Mean + SD) | ≥ 2 Sessions in 36 wk (%) | ≥ 12 Sessions in 36 wk (%) | ≥ 24 Sessions in 36 wk (%) | ≥ 36 Sessions in 36 wk (%) | ||
| Stable Angina | 158453 | 2.6 | 3.2 | 3.9 | NA | 24±12 | 96.6 | 78.9 | 54.1 | 22.5 |
| Heart Failure | 397314 | 1.3 | 1.7 | 2.6 | NA | 22±13 | 94.4 | 72.8 | 51 | 20.1 |
| Diagnosis based | 380868 | 1.2 | 1.6 | 2.5 | NA | 22±13 | 94.3 | 72.5 | 50.3 | 19.7 |
| Procedure based | 16446 | 2.5 | 3.6 | 5.1 | 67±98 | 24±13 | 95.1 | 75.7 | 58.2 | 24.0 |
| VAD | 158 | 26.6 | 35.4 | 44.3 | 42±67 | 27±12 | 95.7 | 82.9 | 68.6 | 31.4 |
| BiV pacemaker | 16288 | 2.3 | 3.3 | 4.7 | 70±100 | 24±13 | 95.0 | 75.0 | 57.2 | 23.3 |
VAD=ventricular assist device, BiV=biventricular; CR=cardiac rehabilitation; NA = not applicable
Among all eligible beneficiaries,
Among all beneficiaries with at least one CR session
Table 3 stratifies enrollment, engagement and completion data for CR by each state. Figure 1 presents the CR enrollment rate for each state, compared to the over-all rate for the United States of 28.6%. Nebraska had an enrollment at 56.1%, with 4 other states (Iowa, Minnesota, South Dakota, Wisconsin) achieving an enrollment rate above 50% and 23 states falling below the over-all rate for the United States.
Table 3.
Cardiac Rehabilitation Enrollment, Engagement and Completion Among Medicare Beneficiaries Sorted by State for People Aged ≥65 years Who Had a Primary Qualifying Event in 2017
| Eligible N | Enrollment/Initiation | Engagement/Participation** | Completion/Achievement** | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ≥1 Session in ≤ 21 d (%)* | ≥1 Session in ≤ 90 d (%)* | ≥1 Session in ≤ 365 d (%)* | Number of Days from Discharge to First Billed CR Session (Mean ± SD)** | Number of Sessions in 36 wk (Mean + SD) | ≥ 2 Sessions in 36 wk (%) | ≥ 12 Sessions in 36 wk (%) | ≥ 24 Sessions in 36 wk (%) | ≥ 36 Sessions in 36 wk (%) | ||
| Alabama | 7932 | 4.6 | 13.8 | 16.2 | 53±60 | 25±13 | 97.4 | 78.7 | 59.3 | 31.2 |
| Alaska | 906 | 6.6 | 18.7 | 23.2 | 59±63 | 25±13 | 93.8 | 79.5 | 60.0 | 33.8 |
| Arizona | 8201 | 6.6 | 24.8 | 28.1 | 50±51 | 24±12 | 96.8 | 79.8 | 58.7 | 19.0 |
| Arkansas | 7759 | 7.6 | 16.7 | 19.3 | 48±64 | 25±13 | 95.9 | 80.0 | 59.2 | 32.5 |
| California | 29205 | 4.1 | 16.1 | 19.3 | 58±57 | 25±13 | 95.8 | 79.8 | 63.8 | 26.7 |
| Colorado | 3802 | 22.4 | 43.6 | 46.8 | 36±45 | 25±12 | 97.4 | 80.2 | 58.6 | 27.5 |
| Connecticut | 3979 | 8.1 | 28.4 | 32.3 | 48±45 | 28±12 | 96.7 | 83.9 | 70.6 | 41.1 |
| Delaware | 1723 | 12.4 | 33.4 | 39.4 | 51±52 | 25±12 | 97.5 | 82.2 | 58.1 | 23.5 |
| Florida | 31288 | 6.8 | 19.4 | 22.6 | 51±60 | 24±12 | 92.8 | 75.6 | 55.8 | 25.6 |
| Georgia | 10939 | 6.6 | 22.5 | 26.0 | 52±53 | 25±13 | 95.5 | 77.5 | 62.0 | 33.3 |
| Hawaii | 955 | 2.0 | 7.6 | 9.4 | 62±73 | 17±10 | 95.6 | 66.7 | 20.0 | 3.3 |
| Idaho | 1951 | 15.3 | 28.8 | 31.6 | 39±51 | 26±13 | 97.1 | 79.9 | 62.7 | 41.3 |
| Illinois | 18084 | 14.3 | 35.8 | 39.8 | 43±48 | 26±12 | 94.6 | 82.5 | 67.6 | 30.4 |
| Indiana | 10283 | 18.2 | 36.2 | 39.0 | 35±45 | 23±12 | 94.0 | 80.4 | 53.4 | 23.7 |
| Iowa | 5883 | 35.3 | 52.9 | 55.3 | 26±38 | 21±12 | 96.3 | 78.9 | 41.8 | 15.4 |
| Kansas | 6003 | 19.4 | 34.4 | 37.1 | 34±45 | 26±12 | 98.1 | 83.3 | 62.6 | 35.1 |
| Kentucky | 7482 | 7.2 | 22.0 | 24.4 | 45±47 | 25±13 | 97.6 | 79.7 | 60.7 | 30.2 |
| Louisiana | 6661 | 7.5 | 16.2 | 18.5 | 47±60 | 26±13 | 96.3 | 80.9 | 64.6 | 35.8 |
| Maine | 2355 | 11.9 | 26.5 | 30.2 | 44±52 | 23±12 | 96.9 | 79.7 | 54.9 | 17.2 |
| Maryland | 7896 | 5.1 | 23.7 | 27.6 | 54±51 | 27±12 | 96.9 | 83.7 | 67.4 | 35.9 |
| Massachusetts | 9684 | 7.2 | 21.0 | 26.0 | 58±60 | 23±12 | 95.4 | 80.6 | 53.6 | 19.5 |
| Michigan | 15534 | 10.0 | 26.8 | 30.2 | 47±52 | 23±12 | 97.4 | 78.4 | 53.4 | 22.3 |
| Minnesota | 3541 | 36.4 | 49.6 | 51.7 | 25±40 | 22±12 | 95.1 | 74.9 | 46.3 | 15.5 |
| Mississippi | 5725 | 6.5 | 18.8 | 20.7 | 43±52 | 23±12 | 97.9 | 79.5 | 52.2 | 21.3 |
| Missouri | 9345 | 15.9 | 35.7 | 39.0 | 40±48.6 | 27±13 | 96.3 | 81.4 | 65.8 | 36.6 |
| Montana | 1941 | 19.9 | 41.4 | 45.4 | 39±49 | 24±13 | 96.4 | 77.6 | 55.8 | 22.9 |
| Nebraska | 3251 | 36.9 | 53.9 | 56.1 | 25±34 | 24±11 | 98.6 | 84.4 | 53.0 | 20.8 |
| Nevada | 2909 | 5.0 | 15.5 | 17.7 | 50±56 | 24±13 | 94.4 | 78.7 | 59.3 | 34.3 |
| New Hampshire | 2522 | 13.7 | 33.5 | 37.2 | 42±46 | 21±11 | 95.6 | 78.3 | 40.4 | 11.4 |
| New Jersey | 14929 | 4.3 | 19.9 | 24.1 | 60±57 | 27±11 | 97.4 | 84.9 | 69.4 | 26.4 |
| New Mexico | 2453 | 6.4 | 16.6 | 18.6 | 46±57 | 26±13 | 95.0 | 80.4 | 66.2 | 28.8 |
| New York | 21859 | 2.1 | 11.6 | 15.4 | 69±60 | 26±12 | 97.4 | 82.0 | 65.4 | 31.1 |
| North Carolina | 12952 | 6.8 | 25.9 | 29.7 | 53±51 | 27±12 | 97.7 | 85.1 | 66.8 | 35.3 |
| North Dakota | 1352 | 29.4 | 44.9 | 47.6 | 28±39 | 21±13 | 92.4 | 73.6 | 45.4 | 22.7 |
| Ohio | 16025 | 9.6 | 28.2 | 31.5 | 46±49 | 26±12 | 97.7 | 83.4 | 65.8 | 27.7 |
| Oklahoma | 8187 | 10.7 | 23.0 | 25.7 | 42±54 | 26±13 | 96.3 | 81.1 | 65.9 | 32.6 |
| Oregon | 4081 | 11.8 | 32.8 | 37.2 | 47±52 | 21±13 | 93.5 | 70.9 | 47.5 | 15.7 |
| Pennsylvania | 17217 | 8.9 | 24.7 | 27.9 | 46±51 | 25±11 | 98.2 | 83.5 | 59.1 | 22.2 |
| Rhode Island | 1376 | 5.7 | 20.4 | 23.8 | 54±53 | 26±12 | 95.4 | 82.6 | 64.6 | 25.0 |
| South Carolina | 7850 | 9.8 | 33.4 | 37.1 | 46±46 | 27±12 | 97.7 | 85.3 | 68.0 | 34.7 |
| South Dakota | 1601 | 40.7 | 52.9 | 55.1 | 24±42 | 23±13 | 95.5 | 77.4 | 52.0 | 21.5 |
| Tennessee | 10125 | 8.1 | 24.7 | 27.2 | 45±49 | 27±12 | 97.5 | 82.9 | 67.3 | 41.1 |
| Texas | 27045 | 10.4 | 23.6 | 26.1 | 42±52 | 25±13 | 93.6 | 78.2 | 61.9 | 30.0 |
| Utah | 2202 | 31.2 | 38.9 | 40.4 | 21±39 | 18±14 | 90.0 | 61.0 | 37.9 | 16.6 |
| Vermont | 1493 | 10.6 | 32.9 | 36.4 | 45±46 | 25±12 | 97.8 | 83.6 | 61.3 | 26.7 |
| Virginia | 11680 | 8.0 | 27.3 | 31.0 | 50±54 | 26±12 | 97.3 | 83.3 | 60.8 | 28.2 |
| Washington | 8378 | 6.7 | 25.3 | 29.0 | 52±53 | 25±13 | 95.4 | 79.7 | 61.6 | 26.9 |
| West Virginia | 4407 | 5.2 | 15.5 | 17.9 | 51±55 | 26±12 | 98.0 | 80.5 | 65.3 | 31.3 |
| Wisconsin | 6948 | 34.8 | 41.5 | 53.6 | 26±37 | 24±13 | 96.7 | 78.5 | 56.0 | 25.6 |
| Wyoming | 1071 | 22.1 | 38.1 | 40.7 | 32±40 | 22±13 | 95.9 | 76.2 | 46.1 | 24.3 |
CR=cardiac rehabilitation;
Among all eligible beneficiaries,
Among all beneficiaries with at least one CR session
Figure 1.
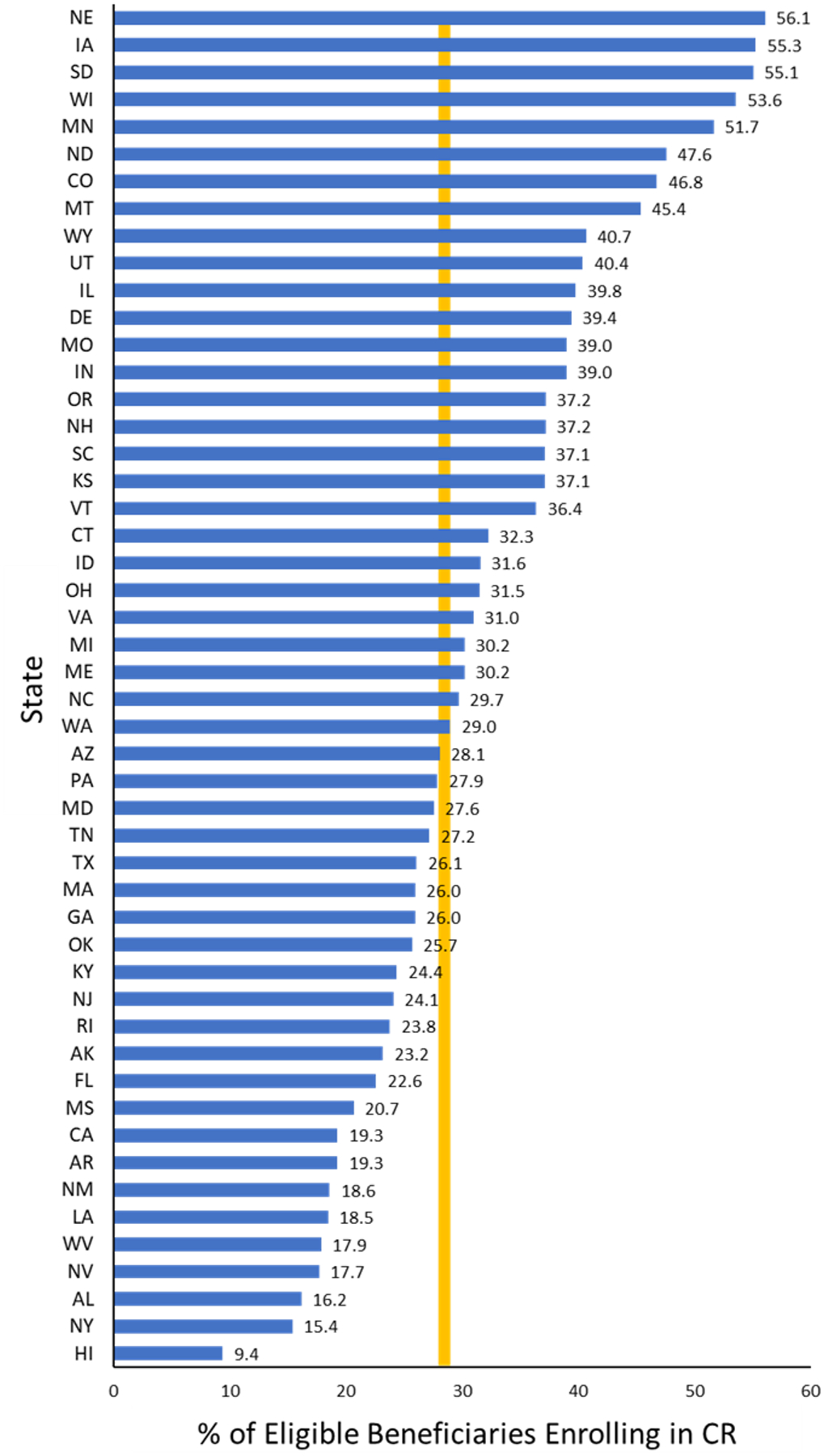
The percentage of cardiac rehabilitation eligible Medicare beneficiaries hospitalized in 2017 in each state that completed at least one cardiac rehabilitation (CR) session within 365 days after experiencing a primary qualifying event. The solid vertical line indicates the over-all enrollment rate of 28.6% for all Medicare beneficiaries in the United States in 2017.
The 2020 CR-specific HEDIS measures applied to beneficiaries who had a primary qualifying event are shown in Table 4. Initiation, defined as 2 or more sessions in 30 days, was 11.8%; engagement in 12 or more sessions in 90 days was 58.0%; engagement in 24 or more sessions in 180 days was 53.5%; and achievement of 36 or more sessions in 180 days was 21.5%.
Table 4.
Among all Eligible Beneficiaries Who had a Primary Qualifying Event in 2017, a Summary of Cardiac Rehabilitation Utilization Rates According to the Measures Specified in the 2020 Healthcare Effectiveness Data and Information Set (HEDIS)
| Eligible N |
Initiation | Engagement | Achievement | ||
|---|---|---|---|---|---|
| ≥2 Sessions in 30 d (%) | ≥ 12 Sessions in 90 d (%) | ≥ 24 Sessions in 180 d (%) | ≥ 36 Sessions in 180 d (%) | ||
| Total | 412080 | 11.8 | 58.0 | 53.5 | 21.5 |
| Sex | |||||
| Men | 246073 | 13.7 | 60.8 | 55.7 | 23.0 |
| Women | 166007 | 9.1 | 52.4 | 49.1 | 18.4 |
| Race/Ethnicity | |||||
| Non-Hispanic White | 355480 | 12.6 | 58.6 | 53.6 | 21.6 |
| Non-Hispanic Black | 22305 | 5.6 | 48.8 | 52.3 | 21.6 |
| Hispanic | 17014 | 5.6 | 50.6 | 50.1 | 17.7 |
| Asian | 7660 | 6.0 | 51.3 | 51.6 | 18.7 |
DISCUSSION
In a large national cohort of demographically and clinically diverse Medicare FFS beneficiaries eligible for CR following a primary qualifying event we found that over-all CR utilization within one year remains alarmingly low (28.6%) in the United States. Enrollment in CR was highest among those undergoing CABG surgery (56.6%) and lowest among patients with an MI and no revascularization procedure (6.5%). Additionally, among patients who enroll in CR, both the average number of sessions completed in 36 weeks (25 sessions) and the percentage of patients completing 36 or more sessions of CR (27.6%) were less than optimal.5,9 Low enrollment rates were observed for both chronic angina and heart failure at 3.9% and 2.6%, respectively, and there is considerable state-level variation for several of the key metrics that pertain to CR enrollment, engagement and completion. Finally, to our knowledge, this study is the first to report national-level data for CR utilization among older adults undergoing transcatheter aortic valve replacement, with enrollment at 29.7% (Table 1).
Although the methodology we used in this study differed slightly from our prior paper involving Medicare beneficiaries hospitalized in 2016,11 in that we now include beneficiaries who underwent a same-day discharge after an outpatient PCI procedure, the analyses performed are generally comparable. The 4.2 percentage point increase reported here-in [28.6% for primary qualifying events in 2017 versus 24.4% for primary qualifying events in 201611] likely represents a modest one-year improvement in CR enrollment among Medicare beneficiaries. Such an increase may be due, in part, to the many effective strategies that are being implemented at state, federal and organizational levels to improve CR enrollment in the United States.6,8,26,27
The observed 4.4 percentage point increase in CR use is favorable; however, it is important to point out that the absolute enrollment rate in the United States of 28.6% remains sub-optimal. Hundreds of thousands of CR-eligible Medicare beneficiaries in 2017 did not initiate CR, a class I guideline-recommended secondary prevention therapy,28–33 and tens of thousands more may have received a sub-optimal dose (i.e., mean number of sessions completed was 25 and only 27.6% completed 36 sessions).25,34,35 Additional research is needed to (a) improve attendance in CR36 and (b) describe the dose-response relationship across various age groups and subpopulations. Also, state-level enrollment rates for CR varied substantially (range: Nebraska = 56.1%, Hawaii = 9.4%) (Figure 1), likely influenced by the availability and capacity of CR programs in each state (so-called “CR deserts”).10 Additional research is needed to elucidate further the factors that enhance CR utilization at the state level. By identifying these factors in higher performing states, novel, effective strategies to improve CR utilization may then be disseminated and implemented in other states.
For example, in the state of Michigan, the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2),37 regularly brings together CR professionals, cardiologists, and hospital clinical quality personnel and administrators, to discuss common challenges and share best practices to improve CR utilization throughout the state.38 The BMC2 works closely with the Michigan Value Collaborative,39,40 a quality improvement program that uses administrative claims to support high-value health care, to provide individual hospitals and providers with site-specific CR utilization reports for their patients with CR qualifying events. This consortium not only allows hospitals and providers to identify opportunities for improvement, it also provides a forum to discuss and rapidly disseminate CR-specific information pertaining to best practices and pertinent policies (e.g., approval of virtual CR reimbursement by Medicare).41 Started in 2019, the effect of the BMC2 consortium on improving CR utilization is yet to be quantified; however, it represents a coalition model that other states could duplicate using state-level CR and cardiology societies.
To achieve meaningful improvements in CR enrollment and completion, both effective initiatives and changes in the reimbursement structure may be needed. One such initiative that is currently experiencing strong momentum world-wide, due partly to the pandemic and its effect on outpatient services at-large,42 is the use of hybrid CR.27,43–45 This model combines a patient-tailored number of facility-based CR sessions with audiovisual synchronous (real-time) virtual (i.e., telehealth) supervised exercise sessions and possibly remote, asynchronous patient contact via telephone or another technology platform.4,46–49 This approach strives to enroll and engage those patients who are limited in their ability to access facility-based CR due to dependent care duties, concerns associated with exercising in-person or with others, transportation issues, conflicts with program-specified hours of operation, and return to work obligations.10,50–52
Another practical strategy to improve CR utilization involves clinical teams working effectively across settings to decrease the time between hospital discharge and/or cardiac procedure and first CR visit. Our current data shows an average of 45 days between discharge after a primary qualifying event and first CR visit, which is more than twice the recommended quality measure of 21 days or less.5 Striving to achieve CR initiation within 21 days is important because there is approximately a 1% decrease in CR enrollment for each day that passes after hospital discharge.53,54 Process improvement strategies used to decrease discharge-to-start time might include incorporating an opt-out automatic referral to CR as part of a hospital’s discharge order set,26 having a CR liaison meet with eligible patients prior to hospital discharge to discuss CR and schedule their first outpatient CR appointment,6 and revising insurance verification/pre-authorization workflow to decrease turnaround time between inquiry and response. Also, for CR programs that incorporate an orientation session prior to starting CR, adopting a 2–4-person group (versus individual) approach may increase operational efficiency and create a sense of community.6
Based on our data, CR is particularly under-utilized in several populations. Specifically, low levels of enrollment were identified for non-Hispanic Blacks (17.3%), Hispanics (16.0%), persons older than 85 years of age (12.6%), women (23.7%), and those with angina (3.9%) or heart failure (2.6%). Feasible population-specific strategies and additional timely research are needed to improve CR utilization and completion among these groups.36,55–58 Older adults may have distinctive challenges due to frailty, multimorbidity, cognitive decline and other complexities associated with age.12 Finally, we concur with the recent call-to-action that “clinicians, health care leaders, and payers should prioritize incorporating CR as part of the standard of care for patients with HF”.28
In 2016, we estimated the total costs for CR at $227.6 million, which was based on an average outpatient payment of $103 per session and included the out-of-pocket costs paid by beneficiaries and supplemental insurance payments.11 For 2017, using an outpatient payment of $110 per session, we estimate total costs for CR to be $323 million, with the majority of the increase in 2017 due to our inclusion of patients who underwent a same-day discharge after an outpatient PCI procedure.
Strengths and Limitations.
The major strength of this study is that it assessed contemporary CR utilization data among Medicare FFS beneficiaries age 65 years and older and as a result, we provide evidence that can be used to help guide health policy, clinical practice pathways, and research directions for a defined and large cohort of patients in whom coronary heart disease and heart failure are highly prevalent; a cohort associated with increased risk for mortality and multiple morbidities (e.g., frequent hospitalizations, reduced exercise capacity and quality of life).12,59 However, these findings may not be generalizable to younger patients who likely have different CR use rates and/or are covered by other health insurance plans.
Regarding limitations, the administrative claims-based definitions used have not been validated through chart review for coding errors or definitions for qualifying events, the latter most likely having its effect on the definitions used for identifying eligible beneficiaries with heart failure status. Also, despite our exclusion criteria, we were likely unable to exclude all beneficiaries for whom CR is not appropriate and as a result, our enrollment rates may be underestimated.
CONCLUSION
Over-all enrollment into CR after hospitalization among Medicare FFS beneficiaries was moderately improved in 2017 compared with 2016. However, absolute enrollment rate (28.6%), engagement (mean = 25 sessions per enrollee), and program completion rate (27.6%) remain low, indicating that many patients eligible for CR in 2017 did not benefit or fully benefit from a class I guideline-recommended secondary prevention therapy. Continued and more widespread dissemination and adoption of existing successful initiatives, novel strategies, and additional research that targets improved enrollment and engagement, is needed, especially among identified populations.
Supplementary Material
Acknowledgements
The authors gratefully acknowledge the contributions of Thomas Schaffer, MHS and Jess McNeely, PhD from the Centers for Medicare and Medicaid Services for their assistance with the development of the original Million Hearts cardiac rehabilitation surveillance framework and analysis coding used in this project.
List of Abbreviations
- BMC2
Blue Cross Blue Shield of Michigan Cardiovascular Consortium
- CABG
coronary artery bypass graft
- CDC
Centers for Disease Control and Prevention
- CMS
Centers for Medicare and Medicaid Services
- Collaborative
Million Hearts Cardiac Rehabilitation Collaborative
- CPT
current procedural terminology
- CR
cardiac rehabilitation
- FFS
fee-for-service
- HEDIS
Healthcare Effectiveness Data and Information Set
- ICD-10-CM
International Classification of Disease, Tenth Revision, Clinical Modification
- MI
myocardial infarction
- PCI
percutaneous coronary intervention
Footnotes
And all authors declare no conflicts of interest
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Heran BS, Chen JM, Ebrahim S, et al. Exercise-based Cardiac Rehabilitation for Coronary Heart Disease. Cochrane Database Syst Rev. 2011. Jul 6;(7):CD001800. doi: 10.1002/14651858.CD001800.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ades PA. Cardiac Rehabilitation and Secondary Prevention of Coronary Heart Disease. N Engl J Med. 2001;345:892–902. [DOI] [PubMed] [Google Scholar]
- 3.Lavie CJ, Milani RV. Cardiac Rehabilitation and Exercise Training in Secondary Coronary Heart Disease Prevention. Prog Cardiovasc Dis. 2011;53:397–403. [DOI] [PubMed] [Google Scholar]
- 4.Funahashi T, Borgo L, Joshi N. Saving Lives with Virtual Cardiac Rehabilitation. N Engl J Med. Catalyst https://catalyst.nejm.org/doi/full/10.1056/CAT.19.0624. Accessed March 1, 2021. [Google Scholar]
- 5.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2018;71:1814–1837. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Cardiac Rehabilitation Change Package. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2018. https://millionhearts.hhs.gov/files/Cardiac_Rehab_Change_Pkg.pdf. Accessed April 30, 2021. [Google Scholar]
- 7.National Committee for Quality Assurance. HEDIS Measures and Technical Resources - NCQA. https://www.ncqa.org/hedis/measures. Accessed May 19, 2021
- 8.Agency for Healthcare Research and Quality. TAKEheart. AHRQ’s Initiative to Increase Use of Cardiac Rehabilitation. https://takeheart.ahrq.gov. Accessed March 1, 2021.
- 9.Ades PA, Keteyian SJ, Wright JS, et al. Increasing Cardiac Rehabilitation Participation From 20% to 70%: A Road Map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92:234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wall HK, Stolp H, Wright JS, et al. The Million Hearts Initiative: CATALYZING UTILIZATION OF CARDIAC REHABILITATION AND ACCELERATING IMPLEMENTATION OF NEW CARE MODELS. J Cardiopulm Rehabil Prev. 2020;40:290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ritchey MD, Maresh S, McNeely J, et al. Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative. Circ Cardiovasc Qual Outcomes. 2020. Jan;13(1):e005902. doi: 10.1161/CIRCOUTCOMES.119.005902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Neill D, Forman DE. Never too old for cardiac rehabilitation. Clin Geriatr Med. 2019;35:407–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baldasseroni S, Pratesi A, Francini S, et al. Cardiac rehabilitation in very old adults: effects of baseline functional capacity on treatment effectiveness. J Am Geriatr Soc. 2016;64:1640–5. [DOI] [PubMed] [Google Scholar]
- 14.Fang J, Ayala C, Luncheon C, Ritchey M, Loustalot F. Use of Outpatient Cardiac Rehabilitation Among Heart Attack Survivors - 20 States and the District of Columbia, 2013 and Four States, 2015. Morb Mortal Wkly Rep. 2017;66:869–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thompson MP, Yaser JM, Hou H, et al. Determinants of Hospital Variation in Cardiac Rehabilitation Enrollment During Coronary Artery Disease Episodes of Care. Circ Cardiovasc Qual Outcomes. 2021. Feb;14(2):e007144. doi: 10.1161/CIRCOUTCOMES.120.007144. [DOI] [PubMed] [Google Scholar]
- 16.Sukul D, Seth M, Barnes GD, et al. Cardiac Rehabilitation Use After Percutaneous Coronary Intervention. J Am Coll Cardiol. 2019;73:3148–3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peters AE, Keeley EC. Trends and Predictors of Participation in Cardiac Rehabilitation Following Acute Myocardial Infarction: Data From the Behavioral Risk Factor Surveillance System. J Am Heart Assoc. 2017. Dec 29;7(1):e007664. doi: 10.1161/JAHA.117.007664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, Whooley MA. Geographic Variation in Cardiac Rehabilitation Participation in Medicare and Veterans Affairs Populations: Opportunity for Improvement. Circulation. 2018;137:1899–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park LG, Schopfer DW, Zhang N, Shen H, Whooley MA. Participation in Cardiac Rehabilitation Among Patients with Heart Failure. J Card Fail. 2017;23:427–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bachmann JM, Huang S, Gupta DK, et al. Association of Neighborhood Socioeconomic Context With Participation in Cardiac Rehabilitation. J Am Heart Assoc. 2017. Oct 11;6(10):e006260. doi: 10.1161/JAHA.117.006260.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun EY, Jadotte YT, Halperin W. Disparities in Cardiac Rehabilitation Participation in the United States: A SYSTEMATIC REVIEW AND META-ANALYSIS. J Cardiopulm Rehabil Prev. 2017;37:2–10. [DOI] [PubMed] [Google Scholar]
- 22.Castellanos LR, Viramontes O, Bains NK, Zepeda IA. Disparities in Cardiac Rehabilitation Among Individuals from Racial and Ethnic Groups and Rural Communities-A Systematic Review. J Racial Ethn Health Disparities. 2019;6:1–11. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Medicare and Medicaid Services. Decision Memo for Cardiac Rehabilitation Programs. CAG-00089R. https://www.cms.gov/medicarecoverage-database/details/nca-decision-memo.aspx?NCAId=164&NcaName=Cardiac+Rehabilitation+Programs&DocID=CAG-00089R. 2006. Accessed November 16, 2021.
- 24.Centers for Medicare and Medicaid Services. Decision Memo for Cardiac Rehabilitation Programs - Chronic Heart Failure. CAG-00437N. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=270. 2014. Accessed November 16, 2021.
- 25.Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. [DOI] [PubMed] [Google Scholar]
- 26.Adusumalli S, Jolly E, Chokshi NP, et al. Referral Rates for Cardiac Rehabilitation Among Eligible Inpatients After Implementation of a Default Opt-Out Decision Pathway in the Electronic Medical Record. AMA Netw Open. 2021. Jan 4;4(1):e2033472. doi: 10.1001/jamanetworkopen.2020.33472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keteyian SJ, Ades PA, Beatty AL, et al. A Review of the Design and Implementation of a Hybrid Cardiac Rehabilitation Program: An Expanding Opportunity for Optimizing Cardiovascular Care. J Cardiopulm Rehabil Prev. 2021. (Accepted for publication, May 13, 2021). [DOI] [PubMed] [Google Scholar]
- 28.Bozkurt B, Fonarow GC, Goldberg LR, et al. Cardiac Rehabilitation for Patients with Heart Failure: JACC Expert Panel. J Am Coll Cardiol. 2021;77:1454–1469. [DOI] [PubMed] [Google Scholar]
- 29.Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes. Circulation. 2014;130:e344–426. [DOI] [PubMed] [Google Scholar]
- 30.O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. Circulation. 2013;127:e362–425. [DOI] [PubMed] [Google Scholar]
- 31.Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. Circulation. 2011;124:e652–735. [DOI] [PubMed] [Google Scholar]
- 32.Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease. Circulation. 2012;126:e354–471. [DOI] [PubMed] [Google Scholar]
- 33.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure. Circulation. 2013;128:e240–327. [DOI] [PubMed] [Google Scholar]
- 34.Brawner CA, Abdul-Nour K, Lewis B, et al. Relationship Between Exercise Workload During Cardiac Rehabilitation and Outcomes in Patients With Coronary Heart Disease. Am J Cardiol. 2016;117:1236–41. [DOI] [PubMed] [Google Scholar]
- 35.Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fleg JL, Keteyian SJ, Peterson PN, et al. Increasing Use of Cardiac and Pulmonary Rehabilitation in Traditional and Community Settings: OPPORTUNITIES TO REDUCE HEALTH CARE DISPARITIES. J Cardiopulm Rehabil Prev. 2020;40:350–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moscucci M, Share D, Kline-Rogers E, et al. The Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) collaborative quality improvement initiative in percutaneous coronary interventions. J Interv Cardiol. 2002;15:381–6. [DOI] [PubMed] [Google Scholar]
- 38.The Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2). Closing the Gap in Cardiac Rehabilitation use After Percutaneous Coronary Intervention. https://bmc2.org/about/what-we-do/cardiac-rehabilitation. Accessed April 22, 2021.
- 39.Ellimoottil C, Syrjamaki JD, Voit B, Guduguntla V, Miller DC, Dupree JM Validation of a claims-based algorithm to characterize episodes of care. Am J Manag Care. 2017;23:e382–e386. [PubMed] [Google Scholar]
- 40.Michigan Value Collaborative. https://michiganvalue.org. Accessed April 15, 2021
- 41.Centers for Medicare & Medicaid Services. Trump Administration Drives Telehealth Services in Medicaid and Medicare. https://www.cms.gov/newsroom/press-releases/trump-administration-drives-telehealth-services-medicaid-and-medicare. Accessed April 15, 2021.
- 42.Besnier F, Gayda M, Nigam A, Juneau M, Bherer L. Cardiac Rehabilitation During Quarantine in COVID-19 Pandemic: Challenges for Center-Based Programs. Arch Phys Med Rehabil. 2020;101:1835–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Keteyian SJ, Grimshaw C, Brawner CA, et al. A Comparison of Exercise Intensity in Hybrid Versus Standard Phase Two Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2021;41:19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hwang R, Bruning J, Morris NR, Mandrusiak A, Russell T. Home-based Telerehabilitation is not Inferior to a Centre-based Program in Patients with Chronic Heart Failure: a Randomised Trial. J Physiother. 2017;63:101–107. [DOI] [PubMed] [Google Scholar]
- 45.Piotrowicz E, Pencina MJ, Opolski G, et al. Effects of a 9-Week Hybrid Comprehensive Telerehabilitation Program on Long-term Outcomes in Patients with Heart Failure: The Telerehabilitation in Heart Failure Patients (TELEREH-HF) Randomized Clinical Trial. JAMA Cardiol. 2020;5:300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Drwal KR, Forman DE, Wakefield BJ, El Accaoui RN. Cardiac Rehabilitation During COVID-19 Pandemic: Highlighting the Value of Home-Based Programs. Telemed J E Health. 2020;26:1322–1324. Available at https://pubmed.ncbi.nlm.nih.gov/?term=Drwal+KR&sort=pubdate. Accessed May 25, 2021. [DOI] [PubMed] [Google Scholar]
- 47.Drwal KR, Wakefield BJ, Forman DE, Wu WC, Haraldsson B, El Accaoui RN. Home-Based Cardiac Rehabilitation: EXPERIENCE FROM THE VETERANS AFFAIRS. J Cardiopulm Rehabil Prev. 2021;41:93–99. [DOI] [PubMed] [Google Scholar]
- 48.Rohrbach G, Schopfer DW, Krishnamurthi N, et al. The Design and Implementation of a Home-Based Cardiac Rehabilitation Program. Fed Pract. 2017;34:34–39. [PMC free article] [PubMed] [Google Scholar]
- 49.Wakefield BJ, Drwal K, Paez M, et al. Creating and Disseminating a Home-based Cardiac Rehabilitation Program: Experience from the Veterans Health Administration. BMC Cardiovasc Disord. 2019;19:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khadanga S, Savage PD, Gaalema DE, Ades PA. Predictors of Cardiac Rehabilitation Participation: OPPORTUNITIES TO INCREASE ENROLLMENT. [published online ahead of print January 25,] J Cardiopulm Rehabil Prev. 2021. https://pubmed.ncbi.nlm.nih.gov/?term=Khadanga+s+2021&sort=pubdate10.1097/HCR.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shanmugasegaram S, Oh P, Reid RD, McCumber T, Grace SL. A comparison of barriers to use of home- versus site-based cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2013;33:297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schopfer DW, Nicosia FM, Ottoboni L, Whooley MA. Patient Perspectives on Declining to Participate in Home-Based Cardiac Rehabilitation: A MIXED-METHODS STUDY. J Cardiopulm Rehabil Prev. 2020;40:335–340. [DOI] [PubMed] [Google Scholar]
- 53.Pack QR, Mansour M, Barboza JS, et al. An early appointment to outpatient cardiac rehabilitation at hospital discharge improves attendance at orientation: a randomized, single-blind, controlled trial. Circulation. 2013;127:349–55. [DOI] [PubMed] [Google Scholar]
- 54.Russell KL, Holloway TM, Brum M, Caruso V, Chessex C, Grace SL. Cardiac rehabilitation wait times: effect on enrollment. J Cardiopulm Rehabil Prev. 2011;31:373–377. [DOI] [PubMed] [Google Scholar]
- 55.Weingarten MN, Salz KA, Thomas RJ, Squires RW. Rates of Enrollment for Men and Women Referred to Outpatient Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2011;31:217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Turk-Adawi K, Supervia M, Lopez-Jimenez F, Adawi A, Sadeghi M, Grace SL. Women-Only Cardiac Rehabilitation Delivery Around the World. Heat Lung Circ 2021;30:135–143. [DOI] [PubMed] [Google Scholar]
- 57.Gravely S, Anand SS, Stewart DE, Grace SL on behalf of the CRCARE Investigators. Effect of referral strategies on access to cardiac rehabilitation among women. Eur J Prev Cardiol. 2014;21:1018–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Beckie TM, Beckstead JW. The effects of a cardiac rehabilitation program tailored for women on their perceptions of health: a randomized clinical trial. J Cardiopulm Rehabil Prev. 2011;31:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kleipool EEF, Hoogendijk EO, Trappenburg MC, et al. Frailty in older adults with cardiovascular disease: cause, effect or both? Aging Dis. 2018;9:489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


