Key Clinical Message
Scapulothoracic dissociation is a rare upper extremity injury caused by high‐velocity trauma over anterolateral shoulder leading to disruption of scapulothoracic articulation. It is considered as a limb threatening injury. Very few cases of scapulothoracic dissociation have been reported in medical literature. In this article, we report a unique case of open injury involving laterally displaced and comminuted scapula accompanied by redundant acromioclavicular joint, total brachial plexus injury, and complete transection of brachial artery. The patient underwent a forequarter amputation after a failed vascular repair.
Keywords: amputation, case report, fracture, Scapulothoracic dissociation
Communited fragments of the scapula removed in piecemeal fashion during forequarter amputation for open SD.

1. INTRODUCTION
Scapulothoracic dissociation (SD) is a rare injury caused by high‐velocity trauma over the anterolateral shoulder leading to complete disruption of scapular relationship with thorax. It was first reported by Oreck et al. in 1984. 1 Only a few hundred case reports have been reported in the medical literature since then. However, in recent years, cases have been more frequently reported. Fewer number of reported cases in the past may be attributed to a substantial proportion of individuals affected by SD succumbing to mortality prior to undergoing comprehensive evaluation and diagnosis. 2 SD usually presents as a massive swelling over the shoulder, palpable hematoma, and gross scapular subluxation from thorax in form of lateralization along with signs and symptoms of neurovascular compromise. The typical radiological features of SD include lateral displacement of the scapula along with possible acromioclavicular separation, a displaced clavicular fracture, or sternoclavicular disruption. 3 , 4 , 5
There have been very few cases of SD reported in the medical literature. Here, we report a rare case of open SD with surgical technique fore‐forequarter amputation and share our insights gained from managing this case.
2. CASE PRESENTATION
2.1. History and examination
A 32‐year‐old man sustained an injury over the left shoulder following a motorcycle accident. Primary management of the case was performed in a rural center and the patient was referred to our center for further management. The patient arrived at our center 8 h after the incident. On initial evaluation, his blood pressure was 130/80 mm of Hg with pulse 130/min, respiratory rate 22 breaths/min, and Glasgow Coma Scale of 15.
There was an extensive circumferential laceration measuring 20 × 10 × 5 cm present over the left shoulder along with abrasion over the face and mild swelling of the left eye (Figure 1). Examination of the left upper extremity revealed absent sensation and movement from the left shoulder to hands. The affected limb was cold below the elbow joint. Radial, ulnar, and brachial pulse were not palpable, and there was no reading in the pulse oximeter.
FIGURE 1.

Patient with lacerated wound over the shoulder and axilla.
2.2. Investigation
Chest X‐ray revealed a laterally displaced scapula, comminuted scapular fracture (Ideberg Grade VI), and a floating shoulder. A computed tomography angiography with 3D reconstruction was performed which demonstrated absence of opacification of the brachial artery below the axilla, comminuted scapula fracture, widened acromioclavicular (AC) joint, and a separate fragment of scapula consisting of the acromion making the AC joint redundant (Figure 2). The case was diagnosed as Zelle Grade IV Open SD.
FIGURE 2.
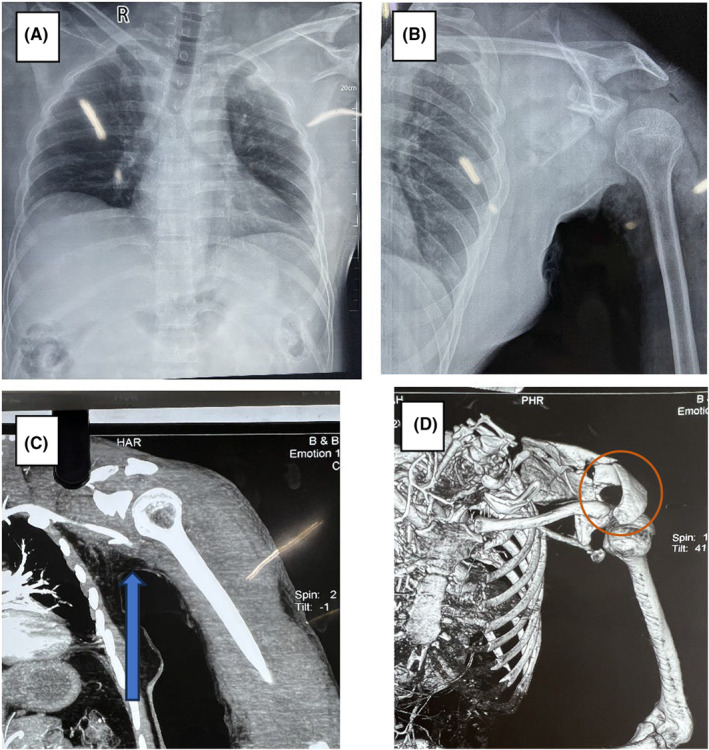
Radiographs and imaging. (A) Chest X‐ray AP showing laterally displaced comminuted scapula fracture. (B) Multiple laterally displaced scapula fracture with separate glenoid fragment (floating shoulder). (C) CT Angio—showing non opacification of the brachial artery (Blue arrow). (D) CT with 3D reconstruction showing comminuted scapula fracture with separate fragment consisting the part forming the acromioclavicular (AC) joint (Circle). AC joint is widened.
2.3. Treatment
The vascular team performed an interposition graft using a great saphenous vein from the distal axillary artery to the mid‐brachial artery along with fasciotomy of the forearm and arm. Two days after the vascular repair the limb did not show any signs of revascularization and limb ischemia was evident with bluish discoloration of the skin, edema, and multiple blisters distal to the mid arm (Figure 3A,B). The limb was insensate below the deltoid region. A forequarter amputation was performed on the third day of the injury.
FIGURE 3.

Ischemia after vascular repair. (A) Ischemia over the forearm with sutured index would. (B) Bullous changes over skin of the over forearm, bulging soft tissue and muscle over fasciotomy incision.
2.4. Surgical technique of forequarter amputation
The surgery was performed under general anesthesia. The patient was kept in a right lateral position with arm support at axilla. A sterile bandage was applied up to the axilla. An anterior incision was given starting in the deltopectoral groove and extended toward the axilla. The axillary artery was identified and ligated. The medial and posterior cords of the brachial plexus were found to have been avulsed while the lateral cord was stretched. The lateral cord was ligated and cut. The pectoralis major muscle fibers were split and separated from the humerus. The coracoid process was freed from the pectoralis minor and the clavicle was cut using a zigly saw on the lateral third.
The dissection was then taken posteriorly starting from the acromion process and extending toward the axilla, connecting to the anterior incision.
The supraspinatus, infraspinatus, teres major and minor, rhomboids, latissimus dorsi, and serratus anterior were released from the comminuted fragments of the scapula. The arm with humeral was then removed en bloc. Comminuted fragments of scapula were removed in a piecemeal fashion. A large portion of the contused, non‐viable rotator cuff muscles and periscapular muscles were removed leaving only the subscapularis muscle in the floor of the thorax. We had initially planned to raise a large posterior flap to excise the comminuted scapula as in tumor surgeries, but as the scapula was lateralized it was not necessary, enabling easy opposition and primary closure of the wound.
The latissimus dorsi muscle was sutured with pectoralis major and minor muscle using Polyester 5 to cover the defect. Two 16 Gauge vacuum drains were placed in the wound. The skin was closed with mattress Nylon sutures. Povidone Iodine dressing was applied and held with compression bandaging. The surgical steps are depicted in Figure 4A–I.
FIGURE 4.
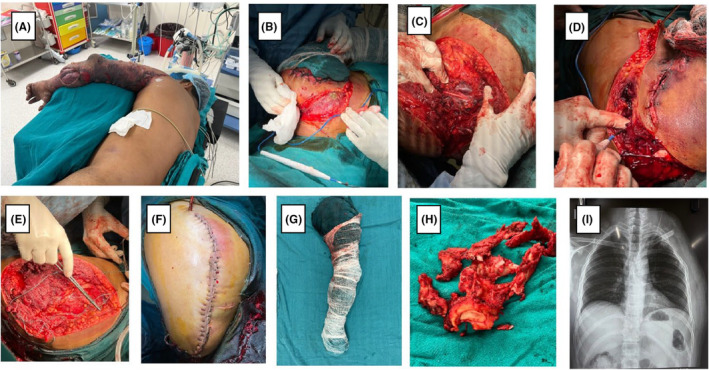
Surgical steps. (A) Lateral position. (B) Anteior incision over deltopectoral groove. (C) Identification of neurovascular structure and ligation (D) Posterior incision joining with anterior. (E) Defect after removal of the arm and scapula. (F) Closure with drains insitu. (G) Amputated limb. (H) Communited scapula. (I) Postoperative X‐ray.
2.5. Outcome
During the postoperative period, the patient received three pints of blood transfusion. Although the patient remained afebrile after the surgery, a repeat debridement was performed on the 7th postoperative day due to persistent large‐volume serous discharge from the wound. The non‐viable subscapularis muscle fibers were removed during the debridement. The patient was discharged on the 14th postoperative day. The wound was found to be healthy and fully healed after one and a half months (Figure 5).
FIGURE 5.

Completely healed would with good contour of pectoralis major muscle 6 weeks after the injury.
3. DISCUSSION AND CONCLUSION
Scapulothoracic dissociation is a devastating injury caused by either a traction force to the upper extremity or massive direct blunt force trauma to the shoulder. It involves musculoskeletal and neurovascular injuries resulting from traumatic disruption of the relationship of the scapula and upper extremity with the thorax. 3 The identification of this condition is often delayed due to the presence of usually multiple other severe distracting injuries. 4
Oreck et al. first described the lateral displacement of the scapula with intact skin as a different variant of traumatic forequarter amputation. 1 Majorities of the case reports have described it in terms of intact overlying skin with symptoms like massive swelling, palpable hematoma, gross shoulder subluxation, weakness, and tenderness. Only a handful open SD cases have been reported. 3 , 5 Here, we present a unique case of open SD with floating shoulder with anterior dissociation resulting from a redundant AC joint, brachial artery injury and complete brachial plexus injury.
Chest X‐ray is an important diagnostic method in identifying SD. Lateral displacement of the involved scapula greater than 1 cm is pathognomonic sign of SD. It is difficult to identify the lateral deviation of the scapula on initial chest X‐rays as they are often not properly aligned in a true anteroposterior position in acute trauma setting. 6 The chest X‐ray of our patient was not aligned properly. However, the deviation of scapula was evident (Figure 2A,B). CT‐3D construction can be done to confirm the diagnosis. MRI may be indicated to explore injuries of the brachial plexus.
SD presents with acromioclavicular joint separation, displaced clavicle fractures or sternoclavicular joint separation. 1 , 3 An immediate X‐ray of the chest in our case revealed lateral scapular deviation along with acromioclavicular joint widening. The clavicle and sternoclavicular joint were intact (Figure 2A,B). The part of the scapula forming the AC joint had broken off from the body of the scapula making the AC joint redundant (Figure 2D). This mechanism of SD has not been reported previously.
SD with vascular injuries commonly present with injuries to the axillary artery. However, in our case the vascular injury was identified at the level of the brachial artery (Figure 2C). Very few studies have tried to assess epidemiology, complications, and mortality. Althausen et al. 4 found vascular lesions to be reported in 70% of cases, neurological injury in 94%, early amputation in 21%, and death in 10%. SD has been classified according to degree of musculoskeletal, vascular, and neurological injury by Zelle et al from grade I to IV. Zelle Grade IV has associated complete brachial plexus injury and results in the worst functional outcome. 7
Specific management and outcome of this devastating injury are still unknown due to inadequate studies. Ebrahein et al. 8 suggested the treatment principle in 3 phases. Phase‐I (first 24 h) diagnosis and resuscitation along with urgent angiography to localize the vascular insult, phase‐II (day 1 to 2 weeks) amputation and glenohumeral arthrodesis and phase‐III (after 2 weeks) prosthesis fitting and tendon transfer. However, some authors prefer early amputation rather than attempting to repair the injuries especially when brachial plexus avulsion is identified. 5 Zeljko et al. 9 recommended initial plate fixation along with thorough surgical debridement and primary wound closure to provide rigid fixation and to protect brachial plexus for the management of open SD with intact brachial plexus.
We opted for vascular repair to salvage the limb. The ensuing ischemia in background of severe soft tissue and osseous injury of shoulder joint and scapula led us to the decision of forequarter amputation. Forequarter amputation for treatment of closed SD was first described by Oreck et al. 1 Takashi Kuroiwa et al 10 reported a case which was similar to ours—open SD with comminuted scapular fracture and recommended complete removal of comminuted scapular fragments to avoid re‐debridement. However, despite removing all comminuted fragments we had to debride the wound on the 7th day to remove dead necrotic tissue. A thorough debridement during the amputation may have prevented this but at the cost of increased operative time and blood loss.
SD is a rare condition with varying presentations requiring different interventions in each case, thus our method of treatment may not be generalizable to all cases.
SD is a severe and possibly disabling condition that involves various musculoskeletal and neurovascular injuries which can be overlooked, because of other severe associated injuries. One should remain vigilant for signs of scapulothoracic dissociation in all patients with severe polytrauma. Prompt identification and management of such complex open injury pattern can prevent sepsis and other devastating complications. Forequarter amputation should be considered in patient with ensuing ischemia, complete brachial plexus injury, and severe soft tissue injury over the shoulder.
AUTHOR CONTRIBUTIONS
Arun Upreti: Conceptualization; writing – original draft; writing – review and editing. Dibya Purush Dhakal: Conceptualization; supervision; writing – original draft; writing – review and editing. Subarna Paudel: Conceptualization; writing – original draft; writing – review and editing. Sagar Bishowkarma: Conceptualization; writing – original draft; writing – review and editing. Umesh Ray: Conceptualization; writing – original draft; writing – review and editing.
FUNDING INFORMATION
No funding was required for the work.
CONFLICT OF INTEREST STATEMENT
None to declare.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
None.
Upreti A, Dhakal DP, Paudel S, Bishowkarma S, Ray U. Forequarter amputation for open scapulothoracic dissociation: A case report and surgical technique. Clin Case Rep. 2024;12:e8535. doi: 10.1002/ccr3.8535
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
REFERENCES
- 1. Oreck SL, Burgess A, Levine AM. Traumatic lateral displacement of the scapula: a radiographic sign of neurovascular disruption. J Bone Joint Surg Am. 1984;66(5):758‐763. [PubMed] [Google Scholar]
- 2. Choo AM, Schottel PC, Burgess AR. Scapulothoracic dissociation: evaluation and management. J Am Acad Orthop Surg. 2017;25(5):339‐347. [DOI] [PubMed] [Google Scholar]
- 3. Bali K, Rangdal S, Kumar V, Jain M, Rawall S. Open scapulothoracic dissociation: a case report and review of literature. Eur Orthop Traumatol. 2011;2(1–2):67‐70. [Google Scholar]
- 4. Althausen PL, Lee MA, Finkemeier CG. Scapulothoracic dissociation: diagnosis and treatment. Clin Orthop Relat Res. 2003;416(416):237‐244. [DOI] [PubMed] [Google Scholar]
- 5. Anbarasan A, Mohamad NH, Mariapan S. Open traumatic scapulothoracic dissociation: case report of a rare injury. Trauma Case Rep. 2018;18:42‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vergano LB, Monesi M. Scapulothoracic dissociation: a devastating “floating shoulder” injury. Acta Biomed. 2019;90(7):150‐153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zelle BA, Pape HC, Greich TG, et al. Functional outcome following Scapulothoracic dissociation. J Bone Joint Surg Am. 2004;86‐A:2‐8. [DOI] [PubMed] [Google Scholar]
- 8. Ebrahein NA, Pearlstein SR, Savolaine ER, et al. Scapulothoracic dissociation (closed avulsion of the scapula, subclavian artery and brachial plexus): a newly recognized variant, a new classification and a review of literature and treatment options. J Orthop Trauma. 1987;1(1):18‐23. [DOI] [PubMed] [Google Scholar]
- 9. Stepanovic ZL, Milisavljevic SS, Prodanovic NS, Stahel PF. Open scapulothoracic dissociation. J Trauma Acute Care Surg. 2015;79(4):698‐700. [DOI] [PubMed] [Google Scholar]
- 10. Kuroiwa T, Kawano Y, Maeda A, et al. A case of open scapulothoracic dissociation with forequarter amputation. JSES Int. 2021;5(5):846‐849. doi: 10.1016/j.jseint.2021.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.


