Abstract
Evidence supports that older adults with cognitive impairment can reliably communicate their values and choices, even as cognition may decline. Shared decision-making, including the patient, family members, and healthcare providers, is critical to patient-centered care. The aim of this scoping review was to synthesize what is known about shared decision-making in persons living with dementia. A scoping review was completed in PubMed, CINAHL, and Web of Science. Keywords included content areas of dementia and shared decision-making. Inclusion criteria were as follows: description of shared or cooperative decision making, cognitively impaired patient population, adult patient, and original research. Review articles were excluded, as well as those for which the formal healthcare provider was the only team member involved in the decision-making (e.g., physician), and/or the patient sample was not cognitively impaired. Systematically extracted data were organized in a table, compared, and synthesized. The search yielded 263 non-duplicate articles that were screened by title and abstract. Ninety-three articles remained, and the full text was reviewed; 32 articles were eligible for this review. Studies were from across Europe (n = 23), North America (n = 7), and Australia (n = 2). The majority of the articles used a qualitative study design, and 10 used a quantitative study design. Categories of similar shared decision-making topics emerged, including health promotion, end-of-life, advanced care planning, and housing decisions. The majority of articles focused on shared decision-making regarding health promotion for the patient (n = 16). Findings illustrate that shared decision-making requires deliberate effort and is preferred among family members, healthcare providers, and patients with dementia. Future research should include more robust efficacy testing of decision-making tools, incorporation of evidence-based shared decisionmaking approaches based on cognitive status/diagnosis, and consideration of geographical/cultural differences in healthcare delivery systems.
Keywords: dementia, Alzheimer’s disease and related dementias, shared-decision making, health promotion, end-of-life, advanced care planning, housing, review, instrumentation
Introduction
Dementia describes a group of symptoms that include cognitive impairment and an individual’s inability to perform activities of daily living (Hebert et al., 2013). Alzheimer’s disease and related dementias describe the group of conditions that cause symptoms referred to as dementia. Brain lesions found in Alzheimer’s disease cause difficulties with memory, language, problem-solving, and other cognitive skills (Fazio et al., 2018; Mantzavinos & Alexiou, 2017), which may contribute to difficulty communicating by and with people living with dementia. However, evidence supports that older adults with cognitive impairment can reliably communicate their values and choices, even as cognition may decline (Feinberg & Whitlatch, 2001). Unfortunately, adults living with dementia’s decision-making capacity is often overlooked or revoked by family members or healthcare professionals due to the communication barriers that present with the disease. Caregivers and healthcare providers are frequently tasked with making decisions for these individuals. As a result, people living with dementia may experience a loss of individuality and dignity due to this communication barrier.
Shared decision-making in dementia refers to the practice of working with patients, caregivers, and/or providers to choose how to proceed in issues related to healthcare based on at least two persons’ preferences, values, and health trajectory (Van der Flier et al., 2017). The Alzheimer’s Association presents Dementia Care Practice Recommendations with patient-centered care as a focus, and these guidelines include the use of communication systems to facilitate the delivery of care (Fazio et al., 2018). However, the guidelines do not outline what these communication systems are or define shared decision-making as one of them. Similarly, in the past decade, legislation has been passed to recognize patients with dementia should participate in the decision-making process, but there is limited evidence on how to incorporate and respect patient preferences of persons with varying cognitive impairment (Daly et al., 2018).
There is inadequate evidence regarding best practices for maintaining the dignity and independence in patients with AD regarding decision making. One challenge to best practice may be that family care partners and long-term care staff underestimate Alzheimer’s patients’ desire and ability to participate in decision-making (Daly et al., 2018). Previous reviews of decision-making in dementia focused solely on a long-term care population (Daly et al., 2018), which limits generalizability of findings to the majority of decision-making that occurs outside of institutionalized, long-term care settings. Changes are being made slowly to give patients with dementia more dignity in day-to-day decision-making, but the current evidence around shared decision-making for older adults with dementia has not been sufficiently explored. Using the enhanced scoping review methodology presented by Daudt et al (2013) and original approach by Arksey and O’Malley’ (2005), the aim of this scoping review was to synthesize what is known about shared-decision making (SDM) in older adults living with dementia. The research question was purposely broad to capture the extent, range and nature of research activity (Daudt et al, 2013).
Methods
The literature search was developed under the guidance of a professional medical librarian (DW). Once the project team agreed on the keywords and controlled vocabulary, the librarian performed the search in PubMed, CINAHL, and Web of Science in July 2021. English language was the only search limit used across the databases. The PubMed search consisted of the MeSH terms and keywords listed below. Searches in the CINAHL and Web of Sciences databases were performed using keywords and phrases from the PubMed search: (“cooperative decision making” OR “decision making, shared”[mesh] OR “shared decision making”) AND (Alzheimer OR “Alzheimer disease”[mesh] OR “mild cognitive impairment” OR “cognitive dysfunction”[mesh] OR dementia OR “dementia”[mesh] OR “Parkinson’s disease dementia” OR “Lewy body disease” OR “Lewy body disease”[mesh] OR “Corticobasal syndrome” OR “posterior cortical atrophy” OR “frontotemporal degeneration” OR “frontotemporal dementia”[mesh] OR “vascular dementia” OR “dementia, vascular”[mesh] AND (English[Filter]). After the initial search across the three databases, all results were exported into the citation manager, Sciwheel, where duplicates were removed. The remaining unique citations were then exported into Covidence to facilitate the screening process.
Title/Abstract Screening
A small, interdisciplinary team was assembled to develop the research question and to ensure comprehensive review, rigor, and reproducibility (Daudt et al, 2013). All the articles were screened using the following inclusion criteria: studies that focused on (1) shared decision making or cooperative decision making, (2) some kind of cognitive impairment, and (3) adult patients. All the articles were jointly assessed by two authors, and disagreements were resolved by the consensus of three authors (MM, JG, & IW) based on the recommended approach of Levac et al (2010).
Full-Text Screening
The full text of the articles was then attached to the articles that made it through the initial screening process. All the articles were jointly assessed by two authors, and a final decision was made by consensus of the three authors who reviewed the articles (MM, JG, & IW).
Data Extraction and Analysis
After completing the final article list, the team created a table summarizing the findings for each article using the following headings: Covidence study number; author, date, title; country; aims or purpose; study design; setting; sample description; decision-making groups represented; the decision of interest; decision-making measures; primary outcome or study variable of interest; SDM findings; and limitations. The research team organized the data based on Arksey and O’Malley’s (2005) approach to sorting by theme and issues that emerged during the review process. Specifically, articles with shared categories of interest (e.g., qualitative study design) were described and presented in individual tables based on the decision of interest. To enhance our approach, we used Excel for visualization and organization based on Daudt et al’s (2013) framework. 13 headings were used for data extraction were included in the Excel document, then summarized and sorted into categories by the study team. No hierarchy emerged when categories were created, although the categories that did emerge were chosen to promote adherence to answering the original research question. Two headings were excluded in the published table: (1) the Covidence study number and (2) decision-making measures. Decision-making measures were not included in the published table due to insufficient data extracted from the final article list. The descriptive analysis plan was determined a priori based on Arksey and O’Malley’s framework that uses a “descriptive numerical summary related to the general information collected and a thematic construction” (Daudt et al, 2013, S1) and went one step further to consider Levac et al (2010) recommendations to discuss implications for future research, practice and policy.
Results
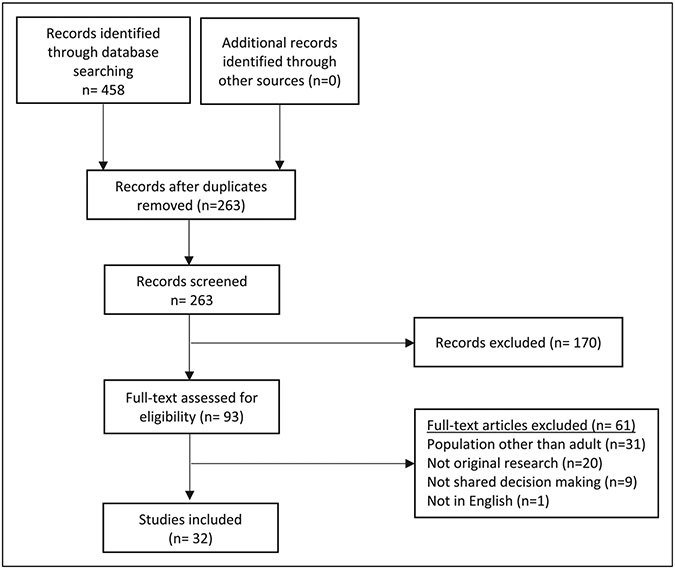
The initial search retrieved 458 articles from the three databases (PubMed [170], CINAHL [130], and Web of Science [158]). All results were exported into the citation manager, Sciwheel, where 195 duplicates were removed. The 263 unique citations were then exported into Covidence to facilitate the screening process. Following the title/abstract screen, 170 articles were deemed not relevant. 60 articles were excluded using the following reasons: wrong patient population (n = 31), not original research (n = 20), not shared decision making as an outcome (n = 9), not in English (n = 1). The authors were satisfied with the results of the full-text screen, so no additional articles were included either through citation chaining or other sources. The total number of articles included was 32 (see Figure 1 for modified PRISMA Flow Diagram and Table 1 for Included Study Characteristics).
Figure 1.
PRISMA flow diagram.
Table 1.
Subject Characteristics, Methods, and Outcomes of Included Studies.
| Author (Date) |
Country | Study purpose | Study design | Specific study design |
Setting | Sample description |
Type of cognitive impairment |
Decisions of interest | Primary outcome or study variables of interest |
Findings/Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Aaltonen et al. (2021) | Finland | To detect different ways people with memory disorder and their spouse CG strive and influence formal care; to recognize situations where their influence is described as restricted or nonexistent. | Qualitative | Descriptive | Participant’s homes or the Alzheimer Society office | N = 34 persons with memory disorders, or their spousal CG | Memory disorder (diverse cognitive health status) | Influence of people receiving care and their spouses’ will on care (content, quality, delivery) | Identified limitations and diversity in how people can influence care from formal providers; demonstrated importance of family CG | 4 themes: acquiescence; negotiating care; lack of influence; taking control |
| Adekpedjou et al. (2019) | Canada | To assess the effect of training home-care teams in interprofessional SDM on the proportion of CGs who report being active in housing decisions involving cognitively impaired older adults. | Quantitative | Pragmatic cluster randomized trial | Health centers | N = 296 CGs from 16 health centers | Dementia | Housing | The proportion of CGs who reported playing an active role in decision making; the matches between preferred option and decision made; impacts on the outlying cluster; CGs’ preferred health-related housing option, the decision made, decisional conflict, decision regret, or burden of care | Intervention increased the proportion of CGs who reported an active role in decision making by at least 12%; increased the proportion of matches between the decision-making role a caregiver preferred and the role they assumed; SDM training had less of an impact on the outlying cluster and no effect on CGs’ outcomes. |
| Ampe et al. (2016) | Belgium | To pilot ’we DECide’ and assess its influence on ACP policy and practice in nursing home dementia care units and barriers for its implementation. | Mixed Methods | Quasi-experimental pre-test-post-test | Dementia care units in nursing homes | N = 90 nursing home staff from 18 dementia care units | Dementia | ACP for end-of-life care | ACP-audit score; barrier; frequency of ACP or involvement of families and residents | Following “we DECide” training, nursing home policy regarding ACP improved significantly, though the actual practice did not; intervention had no significant impact on frequency of ACP or involvement of families and residents. |
| Bilodeau et al. (2019) | Canada | To identify patient decision aids’ (Decision boxes) features for older adults with dementia and their family CGs. | Mixed Methods | Multiple case study within an iterative user centered design approach | Community based healthcare | N = 23 PWDs (≥ 75 years), their 27 CGs (1, friend) | Dementia | Dementia care (case 1. choosing a non-pharmacological treatment to manage agitation, aggression, or psychotic symptoms; case 2. deciding whether to stop driving following diagnosis; case 3. deciding whether to prepare a power of attorney) | The revised template designed for patient decision aids to meet the needs of adults living with dementia and their CGs better | Participants recommended adding pictures and diminishing complexity; appreciated check-boxes; mixed feedback on providing information regarding quality of evidence but overall positive regarding the decision aid for assistance in decision-making. |
| Bolt et al. (2019) | Netherlands | To investigate relatives’ experiences with end-of-life care for PWDs, comparing the nursing home and home setting. | Qualitative | In-depth interviews, thematic analysis | Nursing home vs. home setting | N = 32 bereaved of PWDs | Dementia | End-of-life care | Relatives’ experiences with care for PWDs in the final months of life | In both settings, open discussion with professionals aided decision-making about end-of-life care; regardless of discussion of end-of-life wishes with the PWD, relatives faced challenges and questioned about ’moral rightness’ of their decisions. |
| Boucher et al. (2019) | Canada | To explore burden of care for informal CGs who had made housing decisions on behalf of a cognitively impaired older person. | Quantitative | Cross-sectional study (secondary analysis of a cluster randomized trial) | Community health and social services centers in rural and urban setting within the Province of Quebec | N = 296 CGs (from 16 centers) of a cognitively impaired older person receiving service from home care team | Dementia | Housing | Factors associated with higher burden of care | Greater perception of joint decision-making process was linked to a higher burden of care |
| Davies et al. (2021) | UK | To explore the decision-making process and factors that influence decision-making in dementia end of life care and to produce a model of decision-making in the context. | Qualitative | Semi-structured inteviews, thematic analysis | Community | N = 11 PWDs, 21 CGs (including 6 dyads) | Dementia | End-of-life care | Process of making decisions and factors influencing decisions | Contextual influencing factors: personal preferences; advanced care planning and Lasting Power of Attorney; capacity, health and wellbeing of the PWD; support from others and clarity of roles. Process of making decisions: identifying the decision maker or team; sharing and exchanging information; clarifying values and preferences; managing and considering emotions; considering the feasibility of options; balancing the preferred choice and the actual choice; implementation and reflecting on outcomes. |
| Dooley et al. (2018) | UK | To explore how doctors involve patients with dementia in decisions to start medication. | Quantitative | Observational | Memory clinics within UK National Health Service trusts in either London (urban) or Devon (rural) | N = 71 PWDs, 67 companions, 21 medical doctors | Dementia | Medication | Patient participation in the decision on medication | No association between patient acceptance or resistance and whether medication was prescribed; patients significantly less satisfied with communication when not given a choice in taking the medication. |
| Elidor et al. (2020) | Canada | To identify factors associated with decision regret among informal CGs engaging in housing decisions for cognitively impaired older adults. | Quantitative | Cross-sectional study (secondary analysis of a cluster randomized trial) | Home care settings | N = 296 CGs | Dementia | Housing | Factors associated with less decision regret; factors associated with more decision regret | The perception that a joint decision-making process occurred was linked to less decision regret |
| Garvelink et al. (2019) | Netherlands | To assess the extent to which housing decisions for PWDs with their formal and informal CGs correspond to an interprofessional (IP) SDM approach and their experience with decision making. | Qualitative | Secondary data analysis on material collected in a qualitative study with a longitudinal multiperspective design, semi-structured individual interviews | Community | N = 23 care networks (23 PWDs, 2 CGs, and 2 HCP for each) | Early or moderate dementia | Housing for PWDs | The extent the decision-making process about housing for PWDs with their formal and informal CGs corresponds to an IP-SDM approach | IP-SDM model is overall a useful model in dementia care networks. Limitations: decreased involvement of PWDs over time; no deliberation among all network members to reach a common understanding; lack of collaboration; poor match between preferences and the actual decision made |
| Givens et al. (2018) | US | To describe aspects of ACP among PWDs and examine the association between ACP and health care proxy acceptance of patients’ illness. | Quantitative | Cross-sectional, observational | Community (outpatient geriatric and memory disorder clinics) | N = 62 health care proxy of PWDs | Dementia (mild, moderate/severe) | Advance care planning | Proxy acceptance of dementia | 31% of patients had communicated with their physician regarding preferences for care; 77% communicated with the HCP. 44% of proxies wanted more discussion with the patient regarding care preferences. The proxies having discussed care preferences with the patient was associated with greater acceptance of the patient’s illness. |
| Goossens et al. (2020) | Belgium | To explore how health professionals and residents with dementia perceive the level of SDM during ACP conversations ; to investigate professionals’ perceptions of the importance of SDM, their perceived competence and self-reported frequency of utilizing SDM. | Quantitative | Cross-sectional | Nursing homes | N = 311 care and non-care professionals, 42 residents, 4 external raters | Dementia | Advance care planning (individual goals and preference) | Level of SDM rated by health professionals, residents or families, and external raters, and health professionals’ perception of the importance of SDM | Average achieved level of SDM: 71.53/100 by professionals, 81.11/100 by residents, 26.97/100 by external raters. 23.8% of residents referred to ACP as the topic of the conversation. Although professionals considered SDM to be important, the scores of the frequency and competence with which these skills were practiced were lower. |
| Griffin et al. (2020) | US | To understand what potential best practices are for including CGs of people with Alzheimer’s disease and related dementias (ADRD) into clinical appointments from the perspective of CGs and people with ADRD. | Qualitative | Cross-sectional | Online focus groups | N = 42 spousal CGs, 36 non-spousal CGs, 15 PWDs | ADRD | Involvement of CGs in clinical practice | Best practices for engaging CGs | Best practice for decision making train providers in SDM and how to resolve conflicts with CGs and PWDs; help navigate SDM processes; involve multiple people (CGs); consider CG capacity and values; set a pattern of SDM early in the disease process; value the significance of non-spousal CG’s role. |
| Groen-van de Ven et al. (2017) | Netherlands | To explore how PWDs, their informal CGs and their professionals participate in decision making about daycare; to develop a typology of participation trajectories. | Qualitative | Prospective, multiperspective | Community living, nursing homes | N = 19 PWDs, 36 CGs, 38 HCPs | Early and moderate stages of dementia | Daycare | The way care networks proceed through the process of decision making about daycare | Decision making process: initial expectations about daycare; negotiating about trying daycare; trying daycare. Types of participating trajectories: working together positively toward daycare (type 1), bringing conflicting perspectives together toward trying daycare (type 2), not reaching a commitment to try daycare (type 3) |
| Groen-van de Ven et al. (2017) | Netherlands | To describe the process elements of decision-making in dementia care networks; to enrich the model of collaborative deliberation to facilitate SDM in dementia care networks. | Qualitative | Secondary analysis of interviews | Community living, nursing homes | N = 23 PWDs, 44 CGs, 46 HCPs | Dementia | Dementia care (not explicitly indicated) | The model of collaborative deliberation in dementia care networks | The enriched model: preparatory work (constructive network engagement, recognizing the need for a decision, defining what to decide on), rational discussion (developing alternatives, constructing preferences through deliberation, and trying out alternatives), coalitions (multiple preferences integration, evaluating decision-making) |
| Groen-van de Ven et al. (2017) | Netherlands | To examine the decisions made and the related key events in the trajectories of care networks. | Qualitative | Prospective, multiperspective | Community living, nursing homes | N = 23 PWDs, 44 CGs, 46 HCPs | Beginning to advanced stages of dementia | Decisions with consequences for daily life over the course of time | Decisions made, when decisions occur, characteristic patterns in the sequence of decisions in the care networks | Decisions made: managing daily life with the dementia, arranging care and support, living in society, and representing the PWD. Key events in the decision trajectories: (beginning stage) concerns before the diagnosis, the diagnosis, the inactivity of the PWD, and safety incidents; (middle stage) safety incidents, inactivity of the PWD, 24-hr monitoring, hospitalization, and nursing home admission; (advanced stage) nursing home admission, adjustment issues, and switching between wards. These patterns differ between people living alone and those with an in-live informal CG. |
| Groen-van de Ven et al. (2018) Abstract only | Netherlands | To describe the challenges of SDM in dementia care networks. | Qualitative | Multi-perspective qualitative study using face-to-face interviews; content analysis | Community | N = 113 (23 care networks = 23 PWDs, 44 CGs, and 46 HCPs) | Dementia | Dementia care | Challenges of shared decision-making | Challenges: adapting to a situation of diminishing independence, including shifting roles in the decision making; tensions in network interactions, resulting from different perspectives and interests and requiring agreement about what constitutes a problem in the situation; timing decision well |
| Hamann et al. (2011) | Germany | To analyze the preferences of patients with amnestic mild cognitive impairment (aMCI) and mild AD regarding different aspects of decisions; to correlate these findings with different measures of patient decision-making capacity; to explore the views of the patients’ relatives and of the referring physicians. | Quantitative | Cross-sectional | Memory clinic | N = 100 PWDs, 99 relatives, and 93 of their referring physicians | aMCI and mild AD | Healthcare-related decision | Patient participation preferences | Patients prefer to have the greatest say in social decision making and want their relatives to have little influence on social or medical decisions. Higher patient confidence in their decisional capacity and their MMSE score were predictors of higher patient participation preferences. There was only weak correlation between patient’s relative’s, and physician’s estimate, MacArthur Competence Assessment Toll for Treatment of the patients’ decisional capacity. |
| Hill et al. (2017) | UK | To identify the aspects of end-of-life care for PWDs that are most important to them and their CGs. | Mixed methods | Q-methodology | Community | N = 57 (14 PWDs, 21 CGs, and 22 bereaved CGs) | Early-stage dementia | End-of-life care | The views shared by PWDs, current family CGs and bereaved CGs about the elements of care considered important towards and at end-of-life | Shared viewpoints: family involvement, living in the present, and pragmatic expectations. Areas of consensus: compassionate care, decisions being made by healthcare professions, and information availability when making decisions. |
| Kwak et al. (2019) | US | To understand ADP and decision making among PWDs and CGs. | Quantitative | Cross-sectional | Rural health care facilities (outpatient family practice clinics) | N = 47 CGs of PWDs | AD and related dementias | End-of-life care | PWD’s advance directive completion and the role of the family in proxy decision making | 60% of PWDs had completed an advance directive; 57% preferred equally SDM between family (including the PWD) and physicians. Under a hypothetical scenario for PWDs, 40% of the CGs chose comfort; 55% palliative care treatment. Hispanic PWDs were less likely to complete an advance directive and to choose only pain and symptom management than non-Hispanic White counterparts. |
| Mariani et al. (2018) | Italy, Netherlands | To analyze the effects of training nursing home staff in the implementation of SDM on agreement of residents’ ’life-and-care plans’ with the recommendations and on family CGs’ quality of life and sense of competence, and staff’s job satisfaction. | Mixed methods | Intervention | Nursing home | N = 49 residents and CGs, 34 HCPs | Dementia | Dementia care | Agreement of residents’ ‘life-and-care plans’ with the recommendations (primary outcome), family CGs’ quality of life and sense of competence, and staff’s job satisfaction (secondary outcomes) | Most care plans showed a high level of agreement with the care planning recommendations and improvement in the number of clear problem statements. In Italy, significant improvements were also found regarding specific care objectives, documentation of objectives met and of residents and families’ involvement. No impact was found on secondary outcomes. |
| McCabe et al. (2019) | UK | To measure SDM when starting cholinesterase inhibitors; to investigate associations with contextual factors and explore satisfaction and experience of the diagnostic meeting. | Quantitative | Observational | Memory clinics | N = 74 PWDs, 69 companions (5 patients were not accompanied), and 21 doctors | Dementia | Starting cholinesterase inhibitors | Decision-making subscale of the Autonomy Preference Index; satisfaction with Decision scale | Low SDM scores with 50% of patients and 1/3 of companions reporting negative experiences of receiving a diagnosis of dementia. Patients with mixed dementia were more involved in decision-making compared with AD alone. |
| Meyer et al. (2019) | Australia | To outline the development of a discussion tool that can support service providers to provide choice for PWDs and their CGs in addressing high falls risk factors. | Quantitative | Longitudinal study (baseline, 6-, 12-month assessments) | Community care agencies | N = 25 dyads (PWD and CG) | AD, dementia with Lewy bodies, mixed dementia, vascular dementia, and frontotemporal dementia | Falls prevention strategies | The discussion tool, a person-centered approach to addressing high risk falls risk factors | Capacity and desire to participate meaningfully in their HCPs impetus for providing genuine choice through SDM in service provision, for which this tool is useful. |
| Murphy and Oliver (2012) | UK | To explore whether Talking Mats (TM) could help PWDs and family CGs feel more involved in decisions about managing their daily living than using their usual communication methods. | Mixed methods | Questionnaires, focus groups | Home setting | N = 18 dyads of PWD and CG | Dementia | How participants manage their daily living including personal care, getting around, housework, activities | Participants’ feeling of involvement in discussions when using the TM framework, compared with their usual methods, and their satisfaction with the outcome of the discussions | The TM significantly increased feelings of involvement and overall satisfaction with the discussion for PWDs and family CGs. Both PWDs and family CGs reported that the TM helped them in the SDM process. |
| Reitz and Dalemans (2016) | Netherlands | To observe the effect of Talking Mats (TM) on shared decisions in communication with PWDs; to assess if TM affects the use of language by PWDs in conversation; to get insight in the usability of the Dutch version of TM for PWDs and their relatives. | Mixed methods | Quasi-experimental with semi-structured interviews | Nursing homes and a dementia self-help group | N = 6; all in stage 2 of AD, all between 84-90 years old; 5 women, all with their daughters | AD | Three conversations with regard to planning daily activities and care | Usability of Talking Mats in SDM process; difference in the use of language of the participants with AD | The Dutch version of Talking Mats led to an increase in SDM practices about daily activities and care. It is not clear whether Talking Mats has an effect on the use of language of PWDs. Participants stated the TM was easy to use and made it possible to understand the thoughts of one another more. |
| Smebye et al. (2012) | Norway | To gain a better understanding of how PWDs participated in making decisions about health care and how their family CGs and professional CGs influenced decision making. | Qualitative | Multi case design, semi-structured interviews (family CGs, HCPs), observation (PWDs, HCPs) | Home settings, sheltered housing or a nursing home | N = 10 triads (PWD, family CG, HCP) | Moderate dementia | Decisions concerning daily activities, medical care and moving to sheltered housing or a nursing home | How PWDs participated in making decisions about health care and how their family CGs and HCPs influenced decision making | SDM seemed to be the most typical pattern in decision making, demonstrating that PWDs were dependent on others. Helpers compensated for lost abilities or facilitated the use of retained functions. There was typically an exchange of information and a questioning and answering pattern in the dialogue. |
| Span et al. (2015) | Netherlands | To examine what PWDs, CGs, and case managers think of the user-friendliness of the DecideGuide, whether users were satisfied with it and how easily they accepted it, and what value they put on it for decision-making. | Mixed methods | 5-month field study; structured interviews (PWDs, CGs, case manages), observations of home visits, information that the participants logged in the DecideGuide | Community | N = 19 (4 PWD, 12 CGs, 3 case managers) | Mild to moderate dementia | Shared decisions about healthcare | User-friendliness of the chat for PWDs, CGs, and case managers | Participants felt more involved and shared more information about daily issues than they had done before using the DecideGuide. They deemed the new tool valuable in SDM . The chat function specifically appeared powerful in helping members engage with one another. |
| Stevenson et al. (2016) | Northern Ireland | To understand the risks that present most concern to family CGs, attitudes and approaches of this group towards risk; to examine how information about risks is shared between family CGs, care recipients and professionals working in dementia care. | Qualitative | Focus groups | Health and Social Care Trust areas which deliver publicly funded health and social care services | N = 22 dyads | AD, vascular dementia, dementia with Lewy Bodies, frontotemporal dementia | Risk communication regarding activities of daily life | The risks that present most concern to family CGs; attitudes and approaches towards risk | Discussions about risk were related to medical treatment, supports in the home, and health and safety issues. The process of risk communication appeared as significant as the outcome for family members. Discussions with PWD tended to revolve around raising awareness of risks. Risk communication with professionals and the PWD could effectively support CGs in managing risks in the community, identifying solutions to risks, and modifying concerns. |
| Stirling et al. (2012) | Australia | To explore the meanings given by stakeholders to a decision aid to support dementia CGs to select community-based respite services. | Qualitative | Secondary analysis of interviews (CGs, expert advisors) and focus groups (HCPs) | Community | N = 18 (12 CGs, 3 expert advisors, 3 HCPs) | Early to moderate dementia | Selecting community-based respite services | Meanings given by stakeholders to a decision aid to support dementia CGs to select community-based respite services; HCPs’ perspectives on decision support needs and their clients’ perspective | There were differences amongst HCPs regarding the type of information they believed was appropriate to share with CGs. Many participants felt that CGs would benefit from the decision aid, and some felt that the use of aid would be useful for HCPs to work through with CGs. |
| Tilburgs et al. (2020) | Netherlands | To explore the implementation of the ACP educational intervention for general practitioners (GPs); to explore the impact of the intervention’s mechanisms on daily practice and the experiences of GPs, PWD and their CGs. | Mixed methods | Clustered randomized control trial; descriptive statistics; focus group interview of intervention providers | Two workshops for GPs in primary care practice | N = 36 GP, 140 dyads of PWD and CGs | Unspecified dementia | Medical and non-medical care preferences, not restricted to end of life care (ACP planning) | Intervention’s reach and acceptability, adoption and appropriateness of ACP in daily practice; experiences of GPs, PWD and their CGs. | Most CGs indicated that starting ACP that suited the PWD’s needs influenced their current situation and quality of life and that ACP provided tranquility, clarity, increased their knowledge about dementia, improved their contact with their GP and increased their trust in healthcare professionals. Some felt that ACP had mostly focused on the PWD’s illness and medical preferences. |
| Visser et al. (2018) | Netherlands | To describe naturalistic clinician-patient communication during routine diagnostic clinical consultations in a wide range of memory clinics. | Mixed methods | Multicenter, observational study; audio-recorded diagnostic consultations; surveys for clinicians and patients/CGs | Memory clinics | N = 41 clinicians interviewing a total of 136 patients/CGs | Unspecified dementia; had to score 18 or above on the Mini-Mental State Examination | Diagnostic testing (neuropsychological assessment/testing, structural imaging by means of MRI/CT, amyloid testing or other relevant tests) | Naturalistic clinician-patient communication during routine diagnostic clinical consultations | In almost all pretesting consultations in which diagnostic testing was addressed, one or more decisions were made on testing. Clinicians often presented decisions as a recommendation rather than an option. Observed clinician behavior to involve the patient in the decision-making process was limited. PWDs/CGs rarely expressed if and how they would like to be involved in decision-making. |
| Casey et al. (2015) | To identify professional competencies in facilitating SDM in care networks of PWDs. | Qualitative | Interviews and focus groups | Nursing home | N = 15 networks (15 PWDs, 2 CGs, and 2 professionals) | Professional competencies in facilitating SDM | Identified competencies and attitudes: facilitating patient autonomy of the PWD and CGs; planning decisions over time; facilitating reciprocal information-exchange within the care network; using a step-wise approach of reaching shared decisions; and sharing responsibility for decision-making within the care network |
Of the 32 articles eligible for this review, studies were from across Europe (n = 23), North America (n = 7), and Australia (n = 2). In studies originating in Europe, 11 were from the Netherlands, one from the Netherlands and Italy, five from the UK, two from Belgium, one from Northern Ireland, one from Norway, one from Finland, and one from Germany. Articles from North America were comprised of four from Canada and three from the US.
The majority of the articles used a qualitative study design (n = 21; qualitative only, n = 13; mixed-methods, n = 9), and 10 used a quantitative study design (experimental, n = 1; quasi-experimental, n = 1; descriptive, n = 8). Of the 21 qualitative studies, 13 used qualitative methods only, and 9 used a mixed-methods approach. Of the 10 that used a quantitative study design, one was experimental, one was quasi-experimental, and eight were descriptive studies.
Study populations included patients with dementia (n = 24); caregiver, proxy, or relative (n = 30); and healthcare team members (n = 19). There were a range of cognitive evaluations and inclusion/exclusion criteria for each study for the patient population living with dementia. Participant cognitive status varied across and within individual studies, ranging from mild cognitive impairment to severe/advanced dementia.
Articles were summarized in tables and recategorized based on similarities in SDM topics that emerged through a review of the article and synthesis by three investigators (MM, JG, & IW). The categories included: health promotion (n = 11); advanced care planning (n = 6) and end-of-life (n = 3); development of a decision-making aid (n = 7); and housing (n = 4) and daycare (n = 1).
Health Promotion
There were 11 studies that focused on health promotion related to SDM. Topics included SDM in general patient care (Aaltonen et al., 2021; Groen-van De Ven et al., 2017, 2018; Hamann et al., 2011), activities of daily living (Groen-van De Ven et al., 2017; Stevenson & Taylor, 2016), clinical appointments (Griffin et al., 2020; Groen-van De Ven et al., 2017), diagnostic testing (Visser et al., 2018), and medication use (Dooley et al., 2018; Mccabe et al., 2019). Of the 11 studies, five were qualitative (Aaltonen et al., 2021; Griffin et al., 2020; Groen-van De Ven et al., 2017, 2018; Stevenson & Taylor, 2016), two used mixed methods (Murphy & Oliver, 2012; Span et al., 2015; Visser et al., 2018), and three quantitative approaches (Dooley et al., 2018; Hamann et al., 2011; Mccabe et al., 2019).
The most common form of health promotion discussed as part of SDM among the articles was general patient care. In Aaltonen et al (2021), researchers described the limitations and range of influence of caregivers when discussing care of persons with dementia with formal healthcare providers. Groen-van de Ven et al (2017) asked about specific topics such as managing daily life with dementia, arranging care and support, living in society, and representing the persons with dementia. They explored how these decisions were made, when decisions occurred, and characteristic patterns in the sequence of decisions in the care networks, and ultimately found the patterns differed between people living alone and those with an informal caregiver living in the same home (Groen-van De Ven et al., 2017). In a secondary analysis of the same sample, researchers identified challenges to SDM, including adapting to diminishing independence, including shifting roles in SDM; tensions in network interactions; and timing decisions well (Groen-Van De Ven et al., 2018). In the only study focused on mild cognitive impairment and early-stage dementia, Hamann et al (2011) found that patients preferred to have the greatest say in social decision making and “want their relatives to have little influence on social or medical decisions.” This quantitative study measured patient confidence, and better decisional capacity and Mini Mental Status Examination scores were found to be predictors of stronger patient participation preferences (Hamann et al., 2011).
There were two studies that described the role of SDM when determining a patient’s activities of daily living. One qualitative study described how risk information was shared among family caregiver-care recipient-and healthcare professionals to better understand the SDM process (Stevenson & Taylor, 2016). Groen-van de Ven et al (2017) discussed managing daily life for persons with dementia and the importance of activities of daily living when arranging care and support (Groen-van De Ven et al., 2017).
There were two studies that discussed clinical appointments as an important topic to consider for SDM for persons with dementia (Griffin et al., 2020; Groen-van De Ven et al., 2017; Visser et al., 2018) Groen-van de Ven et al (2017) presented findings on SDM related to clinical appointments, and Griffin et al (2020) conducted online focus groups with persons with dementia and their caregivers to provide evidence on best practice for decision making. They found that participants thoughts healthcare providers should be trained in SDM, the importance and significance of family caregivers in the decision-making process, and how to resolve conflicts between or among multiple decision-makers (Griffin et al., 2020). Finally, a mixed-methods study on the ABIDE project presented findings on patient-clinician communication during the process of undergoing diagnostic testing (Visser et al., 2018).
Two studies addressed SDM regarding medication use in older adults with dementia (Dooley et al., 2018; Mccabe et al., 2019). In a study with persons with dementia and healthcare providers (Dooley et al., 2018), there was found to be no association between patient acceptance or resistance and whether a medication was prescribed. However, patients stated they were significantly less satisfied with patient-provider communication when they were not given a choice in taking the medication. McCabe et al (2019) examined the process of SDM when deciding to start anticholinesterase inhibitors across different types of dementia. The quantitative study used the decision-making subscale of the Autonomy Preference Index and Satisfaction with Decision Scale to measure SDM of patients and caregivers/companions. Lower SDM scores were found for patients compared to companions, and patients with mixed dementia were more involved in decision-making compared with AD alone.
Housing & Daycare
Four articles focused explicitly on housing decisions for persons with dementia (Adekpedjou et al., 2019; Boucher et al., 2019; Elidor et al., 2020; Garvelink et al., 2019). Three of the four articles focused primarily on caregiver outcomes, using quantitative/discrete measurements of caregiver preferences and perceptions. The fourth article used qualitative methods, including separate interviews with persons with dementia and their caregivers.
A SDM training intervention for home care teams increased the proportion of caregivers reporting an active role in decision-making and their preferred decision-making role regarding housing (Adekpedjou et al., 2019). For caregivers involved in housing decisions, a greater perception of a joint decision-making process was linked to a higher burden of care and less decision regret (Boucher et al., 2019; Elidor et al., 2020). Housing decision-making involving patients and caregivers tended to correspond with elements of the Interprofessional (IP)- SDM model (Légaré et al, 2011; Garvelink et al., 2019). Although patients and caregivers preferred for persons with dementia to remain at home as long as possible, cognitive decline typically made moving inevitable eventually (Garvelink et al., 2019). Finally, though not explicitly focused on housing decisions, an additional qualitative study found that persons with dementia had less autonomy in decisions related to moving/housing, as compared to less consequential decisions (e.g., daily activities; Smebye et al., 2012).
One article focused on decisions regarding daycare for persons with dementia, including data from qualitative interviews with persons with dementia and informal and professional caregivers (Groen-Van De Ven et al., 2018). The authors identified three critical points in the decision-making process that resulted in various decision trajectories (i.e., the decision to attend or not attend daycare). Critical issues included initial expectations, followed by negotiation and trying daycare.
End-of-Life & Advanced Care Planning
Studies focused on EOL primarily made decisions around the process of and experiences with care at the EOL (Bolt et al., 2019; Davies et al., 2021; Hill et al., 2017). For all three studies, the individuals who were part of the decision-making process included the family caregivers, persons with dementia, and bereaved caregivers. Of the three studies, two were qualitative (Bolt et al., 2019; Davies et al., 2021), and one study used mixed methods. Findings can be summarized around consensus building amongst decision-makers (Davies et al., 2021; Hill et al., 2017); challenges around “moral rightness” of their decisions or considering emotions (Bolt et al., 2019; Davies et al., 2021), and sharing and exchanging information (Davies et al., 2021; Hill et al., 2017). The small sample sizes in both qualitative and mixed-method studies limited generalizability, and these SDM studies did not include a healthcare provider.
Six articles focused on advanced care planning with a focus on the degree of involvement of families and the older adult in the process (Ampe et al., 2017; Goossens et al., 2020; Tilburgs et al., 2020), as well as the level of SDM by examining patient preferences in conjunction with those of their physicians (Goossens et al., 2020; Kwak et al., 2019; Mariani et al., 2018), the importance of shared-decision making (Goossens et al., 2020; Tilburgs et al., 2020), and preparedness of proxy to engage in shared-decision making (Kwak et al., 2019; Mariani et al., 2018). Of the six studies, three studies (Givens et al., 2018; Goossens et al., 2020; Kwak et al., 2019) used quantitative methods to examine SDM, while three studies used mixed methods (Ampe et al., 2017; Mariani et al., 2018; Tilburgs et al., 2020). Of the SDM instruments used across all studies, only one instrument was used in more than one study, the OPTION scale (Ampe et al., 2017; Goossens et al., 2020). There were two other studies (Kwak et al., 2019; Tilburgs et al., 2020) that also included whether or not the SDM process resulted in a completed advanced care planning or documented advanced care planning conversations. One study (Mariani et al., 2018) that focused on life care planning was not specific to advanced care planning. Still, it showed similar results of improvement of residents and family members in the SDM process. Overall, the results illustrated that SDM was important and preferred SDM among family members, physicians, and patients. Results also indicated that having SDM increased their acceptance of the patient’s illness (Ampe et al., 2017; Givens et al., 2018; Goossens et al., 2020; Kwak et al., 2019; Tilburgs et al., 2020). Areas for future research builds on the limitations, which included small sample sizes (Kwak et al., 2019; Mariani et al., 2018), using proxy accounts of the patient’s preferences (Givens et al., 2018; Kwak et al., 2019), not including a measure of cognitive decline of the older adult (Goossens et al., 2020), and differences between documentation of a completed advanced care planning versus just having a conversation (Tilburgs et al., 2020).
Development of Decision-Making Aid
Eight articles presented approaches or findings related to the development of a decision-making aid. Tools were developed for patients to use in discussions (Bilodeau et al., 2019; Groen-van De Ven et al., 2017; Murphy & Oliver, 2012; Reitz & Dalemans, 2016; Span et al., 2015; Stirling et al., 2012), providers to use with patients (Casey et al., 2015; Meyer et al., 2019; Stirling et al., 2012), and relatives to use with persons with dementia (Murphy & Oliver, 2012; Reitz & Dalemans, 2016). SDM tools were meant to be used for general SDM targeting persons with dementia (Bilodeau et al., 2019; Casey et al., 2015; Groen-van De Ven et al., 2017; Murphy & Oliver, 2012; Reitz & Dalemans, 2016; Span et al., 2015), fall prevention (Meyer et al., 2019), and caregiver respite services (Stirling et al., 2012). Three studies used a qualitative research design (Casey et al., 2015; Groen-van De Ven et al., 2017; Stirling et al., 2012), four used mixed methods (Bilodeau et al., 2019; Murphy & Oliver, 2012; Reitz & Dalemans, 2016; Span et al., 2015), and one quantitative intervention study (Meyer et al., 2019).
Three studies describing SDM tool development used a qualitative research design (Casey et al., 2015; Groen-van De Ven et al., 2017; Stirling et al., 2012). Casey et al (2015) examined social interactions among nursing home residents and identified competencies and attitudes that facilitate patient autonomy, making decisions over time, reciprocal information exchange, use of a step-wise approach to SDM, and shared responsibility for decision-making within the care network (Casey et al., 2015). In another qualitative study, a secondary analysis was performed to create a model of collaborative deliberation in dementia care networks to support SDM. They propose an enriched model that includes preparatory work, rational discussion, and coalitions (Groen-van De Ven et al., 2017). Another study described how SDM can aid in selecting community-based respite services (Stirling et al., 2012). In one of the few studies that did not include persons with dementia, researchers found that there were differences amongst healthcare providers regarding the “type of information they believed was appropriate to share” with caregivers (Stirling et al., 2012). Many participants felt that caregivers would benefit from the use of the decision aid, and some felt that the use of aid would be useful for healthcare providers to work with caregivers (Stirling et al., 2012).
Three studies used a mixed-method design to aid in decision-aid development. Span et al (2015) evaluated a SDM tool to make decisions focusing on patient preference and ease of use called DecideGuide. When using DecideGuide, participants felt more involved and shared more information about daily issues than they had done without a formal SDM tool. In Murphy and Oliver (2012)’s mixed-method study, they describe how couples (persons with dementia and family caregivers) discuss personal care, getting around, housework, and activities of daily living using a SDM aid called Talking Mats (Murphy & Oliver, 2012). The tool significantly increased feelings of involvement and overall satisfaction with the SDM process for participants. Bilodeau et al (2019) present persons with dementia and their caregiver’s feedback on a revised SDM tool trialed across three case studies. A Dutch version of Talking Mats was used in SDM discussions about daily activities and care (Reitz & Dalemans, 2016). Findings demonstrate the feasibility of use in a different language from the original design, and participants stated the tool made it possible to understand each other better (Reitz & Dalemans, 2016). The only quantitative study described the development of a “discussion tool” to help persons with dementia and their caregivers talk about fall prevention strategies (Meyer et al., 2019). The tool facilitated discussion and collaboration among persons with dementia, caregivers, and health professionals.
Discussion
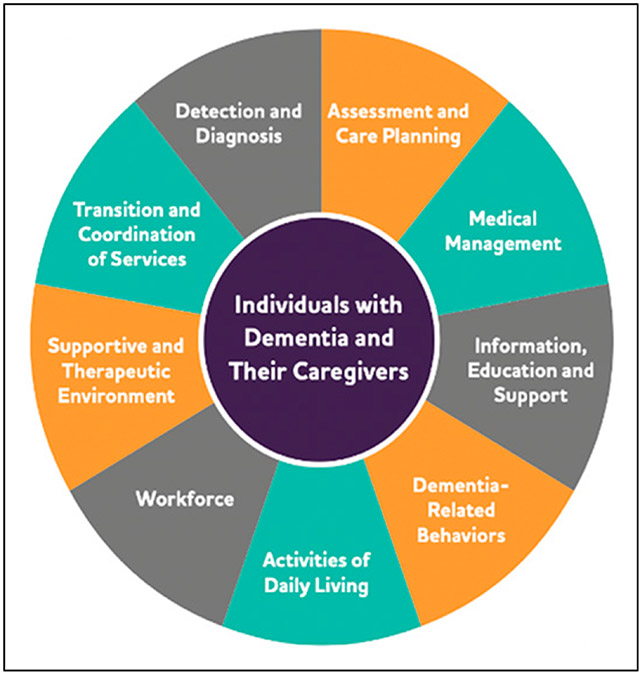
This scoping review illustrates that SDM requires deliberate effort from caregivers and healthcare providers to discuss and understand patient preferences. Findings from this scoping review included identification of decision topics between or among persons with dementia, caregivers, and healthcare providers that focused on health promotion, advanced care planning, and housing. Shared decision-making was preferred among family members, healthcare providers, and persons with dementia (Dooley et al, 2018; Hamann et al, 2011; Hill et al, 2017; Kwak et al, 2019), and models that incorporate SDM were found to promote patient and family satisfaction (Garvelink et al, 2019; Murphy et al, 2012; Reitz & Dalemans, 2016; Span et al, 2015; Stirling et al., 2012; Tilburgs et al., 2020). Articles also discussed the role of healthcare providers in the decision-making process and how their roles should be trained in shared-decision making (Casey et al., 2015; Griffin et al., 2020; Groen-van De Ven et al., 2017), including communication and how to incorporate and respect patient and caregiver/family preferences. Study findings highlight a patient-centered approach to decision making, as supported by Alzheimer’s Association’s (AA) Dementia Care Practice Recommendations (see Figure 2). AA Recommendations focus on the person-centered delivery of care model, depicting individuals with dementia and their caregivers in the center model (see Figure 2). This scoping review presents evidence that shared decision-making can be used to address various topics across the dementia continuum, ranging from current preferences in medication use to long-term care planning. Situating study findings within the Model, promoting decision-making capacity within the individual with dementia-caregiver dyad has the potential to impact all areas of care and care coordination.
Figure 2.
Alzheimer’s Association person-centered delivery model.
The majority of the articles identified in this scoping review used a qualitative study design. Qualitative articles across topics aimed to describe or understand patient, caregiver, and/or healthcare professional decision-making approaches and preferences to facilitate successful decision making. Researchers approached decision-making as a process requiring re-evaluation over time. This approach to decision-making was supported by the quantitative literature that identified patients’ decision-making capacity as a significant challenge to the decision-making process. Challenges to the determination of decision-making capacity were identified in studies with persons living with later-stage dementias and supported by a recent study by Sun et al (2020) that found decision-making ability “under risk” is only impaired in later-stage AD, not in MCI or normal cognition groups (Sun et al., 2020). In earlier stages of cognitive impairment, such as MCI, patients preferred to have greater input in social decision-making and wanted their relatives to have little influence on decisions. This was supported by Hamann et al. (2011), who found that better decisional capacity and cognitive status were found to be predictors of stronger patient decision-making participation preferences. This is an important consideration as there was significant study variation in inclusion and exclusion criteria for persons with dementia in this review, which may influence the generalizability of study findings to different dementia etiologies and staging. It is also possible that interventions or tools to improve decision-making may demonstrate varied efficacy.
In the AA Dementia Care Practice Recommendations, there is a considerable focus on the person-centered delivery of care model, depicting individuals with dementia and their caregivers in the center model (see Figure 2). This scoping review provides evidence that persons with dementia are recognized as important, if not vital, members of the care team, regardless of cognitive status. Most studies included in the review described persons with dementia across different stages of dementia with varying neuropsychological assessments or clinical diagnoses. As presented in the literature, guidelines for person-centered care should include communication systems to facilitate the delivery of care (Fazio et al., 2018). However, the AA guidelines do not provide characteristics of successful communication systems or approaches, nor does the AA define shared decision-making as an essential component of the Person-Centered Delivery Model. As presented in a recent review of SDM in long-term care facilities, there is limited evidence on incorporating and respecting patient preferences of persons with varying cognitive impairments (Daly et al., 2018).
Although SDM is not explicitly mentioned within the Model, the categories or topics that emerged from this review incorporating SDM are consistent with critical components of the Model. For example, the scoping review category of health promotion included topics including medical management (medication use), activities of daily living, and detection and diagnosis (diagnostic testing). There was overlap among Model categories of transition and coordination of services, assessment and care planning, and supportive and therapeutic environment with the review categories of advanced care planning and end-of-life care. The purpose of this review was not intended to create similar categories to those of the Model; however, it is interesting that the categories or topics that emerged from this review are consistent with the AA Person-Centered Delivery Model for persons living with dementia. This review provides evidence that there have been evidence-based attempts to use SDM for various topics of interest in the care of persons living with dementia. SDM can be a critical component in communication for person-centered care, as supported by SDM practices or approaches by patients, caregivers, and healthcare providers.
There is a general lack of experimental research on SDM for persons with dementia. Most of the articles retrieved were qualitative studies with small sample sizes, and mixed-method studies were likely to be pilot studies focused on instrument creation or program evaluation. Overall, limited evidence was available across any topic to provide generalizable findings outside of the individual study samples. SDM tools were created and used in eight articles, but none provided critical evidence of validity and reliability. Tools for SDM could provide the framework and guidance necessary for healthcare providers to provide options for persons with dementia and their families as well as increase family and provider confidence in decision making. There should be targeted efforts to develop and test evidence-based SDM tools or frameworks to ensure patient and family preferences are incorporated into the current care and future decisions.
Limitations
There are limitations to conducting a scoping review. Although we systematically searched the literature to answer the research question, the purpose of the review is limited to describing the current state of the science. Categories of similar decisions in this population and SDM approaches are presented, but as a scoping review, the intent was to have broader scope and “more expansive inclusion criteria” to describe what is currently known about SDM in dementia (Peters et al., 2020). Our diverse findings coupled with the overall purpose of the scoping review support the need for targeted future efforts to develop tools and use SDM for persons with dementia, families, and healthcare providers.
Conclusion
Our findings demonstrate a lack of validity and reliability in SDM tools and approaches to engage persons with dementia and caregivers in SDM. Although our review found that SDM in this population has spanned three continents, the variability in methodological approaches and outcome measures indicates the need for tools to promote patient communication of values and choices, even as cognition may decline. Our decision to place the person living with dementia at the center of all decision-making and finding similar categories emerged from the scoping review was consistent with the AA Person-Centered Delivery Model for persons living with dementia. Refining new tools and conducting psychometric studies addressing the same AA Model topics identified as the categories of the review are vital to person-centered care delivery in persons with dementia are critical to moving this field forward. Future research should include more robust efficacy testing of decision-making tools, incorporation of evidence-based SDM approaches based on cognitive status/diagnosis, and consideration of geographical/cultural differences in healthcare delivery systems. Clinicians should include persons with dementia, families, and healthcare providers in shared decision-making to promote patient and family satisfaction.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number K76AG074942. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Biographies
Meghan K Mattos designed the study, performed title/abstract screening and full-text screening, analyzed and organized findings, drafted the manuscript, and approved the manuscript.
Jessie S Gibson designed the study, performed title/abstract screening and full-text screening, analyzed and organized findings, drafted the manuscript, and approved the manuscript.
Dan Wilson designed the study, performed the literature search, exported search results, provided guidance in analysis, drafted the manuscript, and approved the manuscript.
Laura Jepson performed full-text screening, extracted data, drafted the manuscript, and approved the manuscript.
Soojung Ahn performed full-text screening, extracted data, drafted the manuscript, and approved the manuscript.
Ishan C Williams designed the study, performed title/abstract screening and full-text screening, analyzed and organized findings, drafted the manuscript, and approved the manuscript.
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributor Information
Meghan K Mattos, School of Nursing, University of Virginia, USA.
Jessie S Gibson, School of Nursing, University of Virginia, USA.
Dan Wilson, Health Sciences Library, University of Virginia, USA.
Laura Jepson, School of Nursing, University of Virginia, USA.
Soojung Ahn, School of Nursing, Vanderbilt University, USA.
Ishan C Williams, School of Nursing, University of Virginia, USA.
References
- Aaltonen MS, Martin-Matthews A, Pulkki JM, Eskola P, & Jolanki OH (2021). Experiences of people with memory disorders and their spouse carers on influencing formal care: “They ask my wife questions that they should ask me”. Dementia, 20(7), 2307–2322. 10.1177/1471301221994300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adekpedjou R, Stacey D, Brière N, Freitas A, Garvelink MM, Dogba MJ, Durand PJ, Desroches S, Croteau J, Rivest LP, Légaré F, & Meeks S (2020). Engaging caregivers in health-related housing decisions for older adults with cognitive impairment: A cluster randomized trial. The Gerontologist, 60(5), 947–957. 10.1093/geront/gnz045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ampe S, Sevenants A, Smets T, Declercq A, & van Audenhove C (2017). Advance care planning for nursing home residents with dementia: Influence of ‘we DECide’ on policy and practice. Patient Education and Counseling, 100(1), 139–146. 10.1016/j.pec.2016.08.010. [DOI] [PubMed] [Google Scholar]
- Arksey H, & O’Malley L (2005). Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Bilodeau G, Witteman H, Légaré F, Lafontaine-Bruneau J, Voyer P, Kröger E, Tremblay MC, & Giguere AMC (2019). Reducing complexity of patient decision aids for community-based older adults with dementia and their caregivers: Multiple case study of decision boxes. BMJ Open, 9(5), Article e027727. 10.1136/bmjopen-2018-027727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolt S, van der Steen J, Schols J, Zwakhalen S, & Meijers J (2019). What do relatives value most in end-of-life care for people with dementia? International Journal of Palliative Nursing, 25(9), 432–442. DOI: 10.12968/ijpn.2019.25.9.432. [DOI] [PubMed] [Google Scholar]
- Boucher A, Haesebaert J, Freitas A, Adekpedjou R, Landry M, Bourassa H, Stacey D, Croteau J, Geneviève PG, & Légaré F (2019). Time to move? Factors associated with burden of care among informal caregivers of cognitively impaired older people facing housing decisions: Secondary analysis of a cluster randomized trial. BMC Geriatrics, 19(1), 249–311. 10.1186/s12877-019-1249-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey A-N, Low L-F, & Jeon Y (2015). I had friends when we were young”: Social interactions of residents with moderate to severe dementia in a nursing home. International Psychogeriatrics, 27(S1), S45–S69. 10.1017/s104161021500215x. [DOI] [PubMed] [Google Scholar]
- Daly RL, Bunn F, & Goodman C (2018). Shared decision-making for people living with dementia in extended care settings: A systematic review. BMJ open, 8(6), Article e018977. 10.1136/bmjopen-2017-018977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daudt HML, van Mossel C, & Scott SJ (2013). Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Medical Research Methodology, 13(1). 10.1186/1471-2288-13-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies N, de Souza T, Rait G, Meehan J, & Sampson EL (2021). Developing an applied model for making decisions towards the end of life about care for someone with dementia. PLoS ONE, 16(5), Article e0252464. 10.1371/journal.pone.0252464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooley J, Bass N, Livingston G, & McCabe R (2019). Involving patients with dementia in decisions to initiate treatment: Effect on patient acceptance, satisfaction and medication prescription. The British journal of psychiatry: the journal of mental science, 214(4), 213–217. 10.1192/bjp.2018.201. [DOI] [PubMed] [Google Scholar]
- Elidor H, ben Charif A, Djade CD, Adekpedjou R, & Légaré F (2020). Decision regret among informal caregivers making housing decisions for older adults with cognitive impairment: A cross-sectional analysis. Medical Decision Making: An International Journal of the Society for Medical Decision Making, 40(4), 416–427. 10.1177/0272989X20925368. [DOI] [PubMed] [Google Scholar]
- Fazio S, Pace D, Maslow K, Zimmerman S, & Kallmyer B (2018). Alzheimer’s association ® dementia care practice recommendations. The Gerontologist, 58(suppl_1), S1–S9. 10.1093/geront/gnx182. https://academic.oup.com/gerontologist/article-abstract/58/suppl_1/NP/4847791 [DOI] [PubMed] [Google Scholar]
- Feinberg LF, & Whitlatch CJ (2001). Are persons with cognitive impairment able to state consistent choices? The Gerontologist, 41(3), 374–382. 10.1093/geront/41.3.374. https://academic.oup.com/gerontologist/article/41/3/374/632402 [DOI] [PubMed] [Google Scholar]
- Garvelink MM, Groen-Van De Ven L, Smits C, Franken R, Dassen-Vernooij M, & Légaré F (2019). Shared decision making about housing transitions for persons with dementia: A four-case care network perspective. The Gerontologist, 59(5), 822–834. 10.1093/geront/gny073. [DOI] [PubMed] [Google Scholar]
- Givens JL, Sudore RL, Marshall GA, Dufour AB, Kopits I, & Mitchell SL (2018). Advance care planning in community-dwelling patients with dementia. Journal of Pain and Symptom Management, 55(4), 1105–1112. 10.1016/j.jpainsymman.2017.12.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goossens B, Sevenants A, Declercq A, & van Audenhove C (2020). Shared decision-making in advance care planning for persons with dementia in nursing homes: A cross-sectional study. BMC Geriatrics, 20(1), 381. 10.1186/s12877-020-01797-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin JM, Riffin C, Havyer RD, Biggar VS, Comer M, Frangiosa TL, & Bangerter LR (2020). Integrating family caregivers of people with Alzheimer’s disease and dementias into clinical appointments: Identifying potential best practices. Journal of Applied Gerontology: The Official Journal of the Southern Gerontological Society, 39(11), 1184–1194. 10.1177/0733464819880449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groen-van de Ven L, Smits C, Oldewarris K, Span M, Jukema J, Eefsting J, & Vernooij-Dassen M (2017). Decision trajectories in dementia care networks: Decisions and related key events. Research on Aging, 39(9), 1039–1071. 10.1177/0164027516656741. [DOI] [PubMed] [Google Scholar]
- Groen-Van De Ven L, Smits C, Span M, Jukema J, Coppoolse K, de Lange J, Eefsting J, & Vernooij-Dassen M (2018). The challenges of shared decision making in dementia care networks. International Psychogeriatrics, 30(6), 843–857. 10.1017/S1041610216001381. [DOI] [PubMed] [Google Scholar]
- Hamann J, Bronner K, Margull J, Mendel R, Diehl-Schmid J, Bühner M, Klein R, Schneider A, Kurz A, & Perneczky R (2011). Patient participation in medical and social decisions in Alzheimer’s disease. Journal of the American Geriatrics Society, 59(11), 2045–2052. 10.1111/j.1532-5415.2011.03661.x. [DOI] [PubMed] [Google Scholar]
- Hebert LE, Weuve J, Scherr PA, & Evans DA (2013). Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology, 80(19). 10.1212/WNL.0b013e31828726f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill SR, Mason H, Poole M, Vale L, Robinson L, & SEED team (2017). What is important at the end of life for people with dementia? The views of people with dementia and their carers. International Journal of Geriatric Psychiatry, 32(9), 1037–1045. 10.1002/gps.4564. [DOI] [PubMed] [Google Scholar]
- Kwak J, Xie B, Champion JD, & Fleischmann KR (2019). Rural dementia caregivers in Southwest Texas: An exploratory study of advance directives and end-of-life proxy decision making. Journal of Gerontological Nursing, 45(9), 11–17. 10.3928/00989134-20190530-01. [DOI] [PubMed] [Google Scholar]
- Légaré F, Stacey D, Pouliot S, Gauvin F-P., Desroches S, Kryworuchko J, Dunn S, Elwyn G, Frosch D, Gagnon M-P, Harrison MB, Pluye P, & Graham ID (2011). Interprofessionalism and shared decision-making in primary care: a stepwise approach towards a new model. Journal of Interprofessional Care, 25(1), 18–25. 10.3109/13561820.2010.490502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D, Colquhoun H, & O’Brien KK (2010). Scoping studies: advancing the methodology. Implementation Science, 5(1), 69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantzavinos V, & Alexiou A (2017). Biomarkers for Alzheimer’s disease diagnosis. Current Alzheimer Research, 14(11), 1149–1154. 10.2174/1567205014666170203125942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani E, Chattat R, Ottoboni G, Koopmans R, Vernooij-Dassen M, & Engels Y (2018). The impact of a shared decision-making training program on dementia care planning in long-term care. Journal of Alzheimer’s disease: JAD, 64(4), 1123–1135. 10.3233/JAD-180279. [DOI] [PubMed] [Google Scholar]
- Mccabe R, Pavlickova H, Xanthopoulou P, Bass NJ, Livingston G, & Dooley J (2019). Patient and companion shared decision making and satisfaction with decisions about starting cholinesterase medication at dementia diagnosis. Age and Ageing, 48(5), 711–718. 10.1093/ageing/afz045. [DOI] [PubMed] [Google Scholar]
- Meyer C, Hill S, Hill KD, & Dow B (2019). Inclusive decision making for falls prevention: A discussion tool for use with people with dementia and their caregivers. Journal of Aging and Physical Activity, 27(5), 711–718. 10.1123/japa.2018-0167. [DOI] [PubMed] [Google Scholar]
- Murphy J, & Oliver T (2013). The use of Talking Mats to support people with dementia and their carers to make decisions together. Health & social care in the community, 21(2), 171–180. 10.1111/hsc.12005. [DOI] [PubMed] [Google Scholar]
- Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, Godfrey CM, & Khalil H (2020). Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis, 18(10), 2119–2126. 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- Reitz C, & Dalemans R (2016). The use of ‘Talking Mats’ by persons with Alzheimer in The Netherlands: Increasing shared decision-making by using a low- tech communication aid. Journal of Social Inclusion, 7(2), 35. 10.36251/josi.110. [DOI] [Google Scholar]
- Smebye KL, Kirkevold M, & Engedal K (2012). How do persons with dementia participate in decision making related to health and daily care? A multi-case study. BMC Health Services Research, 12(1), 241. 10.1186/1472-6963-12-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Span M, Smits C, Jukema J, Groen-van de Ven L, Janssen R, Vernooij-Dassen M, Eefsting J, & Hettinga M (2015). An interactive web tool for facilitating shared decision-making in dementia-care networks: A field study. Frontiers in Aging Neuroscience, 7(JUN), 128. 10.3389/fnagi.2015.00128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson M, & Taylor BJ (2016). Risk communication in dementia care: Family perspectives. Journal of Risk Research, 21(6), 692–709. 10.1080/13669877.2016.1235604. [DOI] [Google Scholar]
- Stirling C, Lloyd B, Scott J, Abbey J, Croft T, & Robinson A (2012). A qualitative study of professional and client perspectives on information flows and decision aid use. BMC Medical Informatics and Decision Making, 12(1), 26–28. 10.1186/1472-6947-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun T, Xie T, Wang J, Zhang L, Tian Y, Wang K, Yu X, & Wang H (2020). Decision-making under ambiguity or risk in individuals with Alzheimer’s disease and mild cognitive impairment. Frontiers in Psychiatry, 11, 218. 10.3389/fpsyt.2020.00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilburgs B, Koopmans R, Schers H, Smits C, Vernooij-Dassen M, Perry M, & Engels Y (2020). Advance care planning with people with dementia: A process evaluation of an educational intervention for general practitioners. BMC Family Practice, 21(1), 199. 10.1186/s12875-020-01265-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Flier WM, Kunneman M, Bouwman FH, Petersen RC, & Smets EMA (2017). Diagnostic dilemmas in Alzheimer’s disease: Room for shared decision making. Alzheimer’s and Dementia: Translational Research and Clinical Interventions, 3(3), 301–304). Elsevier Inc. 10.1016/j.trci.2017.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser LNC, Kunneman M, Murugesu L, van Maurik I, Zwan M, Bouwman FH, Schuur J, Wind HA, Blaauw MSJ, Kragt JJ, Roks G, Boelaarts L, Schipper AC, Schooneboom N, Scheltens P, van der Flier WM, & Smets EMA (2019). Clinician-patient communication during the diagnostic workup: The ABIDE project. IN: Alzheimer’s and Dementia: Translational Research and Clinical Interventions, 11(1), 520–528. 10.1016/j.dadm.2019.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]