Summary
Background
Ensuring that access to health care is affordable for everyone—financial protection—is central to universal health coverage (UHC). Financial protection is commonly measured using indicators of financial barriers to access (unmet need for health care) and financial hardship caused by out-of-pocket payments for health care (impoverishing and catastrophic health spending). We aim to assess financial hardship and unmet need in Europe and identify the coverage policy choices that undermine financial protection.
Methods
We carry out a cross-sectional study of financial hardship in 40 countries in Europe in 2019 (the latest available year of data before COVID-19) using microdata from national household budget surveys. We define impoverishing health spending as out-of-pocket payments that push households below or further below a relative poverty line and catastrophic health spending as out-of-pocket payments that exceed 40% of a household's capacity to pay for health care. We link these results to survey data on unmet need for health care, dental care, and prescribed medicines and information on two aspects of coverage policy at country level: the main basis for entitlement to publicly financed health care and user charges for covered services.
Findings
Out-of-pocket payments for health care lead to financial hardship and unmet need in every country in the study, particularly for people with low incomes. Impoverishing health spending ranges from under 1% of households (in six countries) to 12%, with a median of 3%. Catastrophic health spending ranges from under 1% of households (in two countries) to 20%, with a median of 6%. Catastrophic health spending is consistently concentrated in the poorest fifth of the population and is largely driven by out-of-pocket payments for outpatient medicines, medical products, and dental care—all forms of treatment that should be an essential part of primary care. The median incidence of catastrophic health spending is three times lower in countries that cover over 99% of the population than in countries that cover less than 99%. In 16 out of the 17 countries that cover less than 99% of the population, the basis for entitlement is payment of contributions to a social health insurance (SHI) scheme. Countries that give greater protection from user charges to people with low incomes have lower levels of catastrophic health spending.
Interpretation
It is challenging to identify with certainty the coverage policy choices that undermine financial protection due to the complexity of the policies involved and the difficulty of disentangling the effects of different choices. The conclusions we draw are therefore tentative, though plausible. Countries are more likely to move towards UHC if they reduce out-of-pocket payments in a progressive way, decreasing them for people with low incomes first. Coverage policy choices that seem likely to achieve this include de-linking entitlement from payment of SHI contributions; expanding the coverage of outpatient medicines, medical products, and dental care; limiting user charges; and strengthening protection against user charges, particularly for people with low incomes.
Funding
The European Union (DG SANTE and DG NEAR) and the Government of the Autonomous Community of Catalonia, Spain.
Keywords: Affordable access to health care, Europe, Financial hardship, Financial protection, Out-of-pocket payments, Universal health coverage, Unmet need
Research in context.
Evidence before this study
A systematic review of financial hardship in Europe identified 54 country, regional or global studies published between January 2000 and July 2017 and drawing on data up to 2011. It found that the literature had limited value for policy purposes because most studies focused on the level of financial hardship and did not consider distribution or drivers or involve policy analysis. The studies mainly covered middle-income countries. Variation in the methods and data sources used limited the potential for international comparison.
Global monitoring carried out by the World Bank and the World Health Organization (WHO) in the context of the Sustainable Development Goals (SDGs) draws on data up to 2017. Although all global studies use the same method to monitor catastrophic health spending (the ‘budget share’ approach adopted to measure SDG 3.8.2), and similar data sources (mainly household budget surveys), they focus on the level of financial hardship, do not consider key distributional issues such as wealth, and are limited in terms of country-level analysis. In the absence of global data on unmet need for health care, global studies use the service coverage index (SDG 3.8.1) instead, but this lacks relevance for policy because it does not show who is most likely to be at risk of weaker service coverage within countries.
Regional monitoring carried out by WHO/Europe in response to regional commitments includes a series of over 20 country-based studies and a comparative analysis published in 2019. The comparative analysis covers 24 high- and middle-income countries, draws on data up to 2016 and uses the same method (the ‘capacity to pay’ approach used in this study) and data sources (household budget surveys). It not only assesses the level, distribution and drivers of financial hardship but also looks at unmet need and includes some analysis of coverage policy.
A comparison of the budget share approach used to measure catastrophic health spending at global level (SDG 3.8.2) and the capacity to pay approach used in Europe finds that the global method is less sensitive to equity than the regional method. SDG 3.8.2 overestimates financial hardship among high-income households and underestimates financial hardship among households with low incomes.
Added value of this study
This study provides new evidence on financial protection in Europe. It covers 40 countries including, for the first time, the whole of the European Union, and draws on data from 2019 to form a pre-COVID-19 assessment of regional progress towards UHC. Using equity-sensitive methods, the study shows that households with low incomes are most likely to experience financial hardship and unmet need and that financial hardship is mainly driven by out-of-pocket payments for outpatient medicines, medical products and dental care, reflecting important gaps in the coverage of primary care, even in Europe's richest countries. By pairing analysis of survey data with policy analysis, the study takes steps to identify some of the coverage policy choices that undermine financial protection.
Implications of all the available evidence
Research shows that financial protection is generally weaker when public spending on health is low relative to gross domestic product and out-of-pocket payments account for a relatively high share of current spending on health. Simply increasing public spending on health may not be enough to improve financial protection, however. Policy choices matter. Countries are more likely to move towards UHC if they reduce out-of-pocket payments in a progressive way, decreasing them for people with low incomes first. Coverage policy choices that seem likely to achieve this include de-linking entitlement to publicly financed health care from payment of contributions in countries with contributory SHI schemes; broadening the basis for entitlement from legal residence to residence, which allows refugees, asylum seekers and undocumented migrants to be fully covered; expanding the coverage of outpatient medicines, medical products and dental care, so that primary care covers treatment as well as consultations and diagnosis; limiting the use of user charges; and strengthening protection against user charges, particularly for people with low incomes or chronic conditions. How financial protection is monitored also has a bearing on progress towards UHC. Monitoring that combines statistical and policy analysis at country level, and draws on insights from comparative analysis, can foster action by identifying the policy changes needed in specific contexts.
Introduction
Ensuring that access to health care is affordable for everyone—financial protection—is central to universal health coverage (UHC). Financial protection is undermined by out-of-pocket payments for health care. Out-of-pocket payments can cause financial hardship for people using health services, leading to impoverishing and catastrophic health spending. They can also be a barrier to access, resulting in unmet need for health care. Without financial protection people may be forced to choose between health care and other basic needs, which can deepen poverty, erode health and well-being, and increase inequalities.1, 2, 3 For this reason financial protection is widely regarded as a core dimension of health system performance assessment.4
Countries in Europe first committed to strengthening financial protection through the Tallinn Charter on Health Systems for Health and Wealth, signed in 2008.5 This was followed by the Sustainable Development Goals (SDG 3.8) in 2015, the European Pillar of Social Rights (article 16) in 2017, and WHO's European Programme of Work (core priority 1) in 2021, all of which include a commitment to UHC.6, 7, 8
Monitoring financial protection can help countries to make progress towards UHC, especially if monitoring generates actionable evidence for policy—evidence that identifies the people who lack financial protection, the health services that drive unmet need and financial hardship due to out-of-pocket payments and, crucially, the policies responsible for these negative outcomes. In practical terms, this has two main implications. First, it means that monitoring should be based on metrics that are sensitive to equity, to reduce the risk of underestimating adverse outcomes among people with low incomes. Second, it means looking closely at the health system policies that influence financial protection. Coverage policy—the way in which health coverage is designed and implemented—is an important starting point for policy analysis because it is the primary mechanism through which people are exposed to out-of-pocket payments and a key determinant of the distribution of out-of-pocket payments across the population.3
Although the framework for monitoring UHC established through the SDGs serves global advocacy objectives, it is limited in its ability to generate actionable evidence for policy due to its choice of metrics and a heavy emphasis on quantitative analysis (see the research in context panel for details).2,3,9,10 In Europe, however, equity-sensitive metrics for financial hardship and unmet need have been combined with information on coverage policy to produce a growing body of country-level and comparative analysis.3,11
Building on this work, we present a comparative analysis of financial protection in 40 countries in Europe including, for the first time, the whole of the European Union. Our study has two aims. First, to measure the level, distribution, and drivers of financial hardship and unmet need using established indicators to assess the situation in Europe before the COVID-19 pandemic. Second, to identify the coverage policy choices that undermine financial protection.
Previous analysis has shown that the incidence of catastrophic health spending is closely linked to a health system's reliance on out-of-pocket payments, and that countries can reduce out-of-pocket payments by increasing public spending on health.3,12 Our study adds to this by shedding light on what countries can do to mitigate the damage caused by out-of-pocket payments.
Methods
This study pairs cross-sectional analysis of nationally representative survey data from 40 countries in Europe with policy analysis. Its contribution comes from quantitative analysis of financial hardship due to out-of-pocket payments (referred to from here on as financial hardship), using microdata from national household budget surveys, and qualitative analysis of key dimensions of coverage policy. We bring these two elements together for 40 countries for the first time. The study also draws on publicly available survey data on unmet need for health care, dental care, and prescribed medicines.
We present data for 2019 or the latest available year before the COVID-19 pandemic to establish a pre-pandemic baseline for Europe. We do not use survey data gathered during the pandemic (2020–2022) because some surveys were disrupted and patterns of household spending and health-seeking behaviour were likely to have been skewed by lockdowns and other factors, making them difficult to interpret from a comparative perspective. Post-pandemic survey data (2023) are not yet available.
In the year of analysis, 29 of the 40 countries were classified as high income, 9 as upper-middle income (Albania, Armenia, Bosnia and Herzegovina, Bulgaria, Georgia, Montenegro, North Macedonia, Serbia and Türkiye) and 2 as lower-middle income (Republic of Moldova and Ukraine).
We define out-of-pocket payments as formal and informal payments made by people at the time of using any health care good or service delivered by any type of provider.13 Unless otherwise stated, we use the term ‘health care’ when discussing all health services, including medicines, medical products, and dental care, and the term ‘dental care’ when referring to dental services only. The category ‘medical products’ includes items like hearing aids, glasses and contact lenses, nebulisers, and wheelchairs. The category ‘diagnostic tests’ includes diagnostic tests and other paramedical services such as physiotherapy.
Assessing financial protection
Health accounts data on the out-of-pocket payment share of current spending on health and on out-of-pocket payments by type of health care can be used as a proxy measure of gaps in health coverage. Across the study countries, and in the year of the analysis, out-of-pocket payments range from just under 10% of current spending on health in France to 84% in Armenia, with a median of around 21%; they account for more than a third of current spending on health in 12 countries (see the Supplementary File). In the same year, the types of health care that are most likely to be financed through out-of-pocket payments are medical products (61% of current spending on medical products), dental care (59%), and outpatient medicines (40%); out-of-pocket payments account for a much smaller share of spending on outpatient care (27%), diagnostic tests (13%), and inpatient care (6%) (see the Supplementary File).
These data do not tell us about the distribution of out-of-pocket payments across the population, however, or whether gaps in coverage lead to financial hardship and unmet need. For this we need data from household surveys. The following paragraphs describe in more detail our approach to assessing financial protection and our data sources.
Financial hardship due to out-of-pocket payments is measured using two indicators: impoverishing and catastrophic health spending. Both indicators can be calculated in different ways, with varying implications for equity.2 We use metrics developed by WHO/Europe because of their greater sensitivity to equity.2,3,9
The WHO/Europe approach to measuring financial hardship uses the normative cost of meeting basic needs for food, housing (rent), and utilities (water, electricity, and heating) to determine a relative poverty line, referred to as the ‘basic needs line’. The basic needs line is derived from the average amount spent on food, rent, and utilities per equivalent adult (using Organisation for Economic Co-operation and Development (OECD) equivalence scales) among households ranked between the 25th and 35th percentiles of total consumption per equivalent adult in each country and year. These households are selected on the assumption that they are likely to be able to meet their basic needs for food, rent, and utilities and are unlikely to exceed them. The derived amount is then adjusted to household level accounting for household size and composition.
To assess the level of financial hardship, households are defined in the following way:
-
•
Impoverishing health spending counts households who are impoverished or further impoverished. A household is impoverished if its total spending (consumption) is below the basic needs line after out-of-pocket payments (it can no longer meet its basic needs—food, housing, and utilities) and further impoverished if its total spending is below the basic needs line (it is already unable to meet its basic needs) and it incurs out-of-pocket payments.
-
•
Catastrophic health spending counts households whose out-of-pocket spending is greater than 40% of their capacity to pay for health care—that is, more than 40% of their budget (their total annual consumption) net of the normative cost of food, rent, and utilities adjusted for household size and composition.
To assess the distribution of financial hardship, we disaggregate households with catastrophic health spending by consumption quintile. Consumption quintiles are based on total consumption per adult equivalent using OECD equivalence scales.
To assess the drivers of financial hardship, we show the breakdown of out-of-pocket payments in households with catastrophic health spending by type of health care using six categories: medicines, medical products, dental care, diagnostic tests, outpatient care, and inpatient care.
Impoverishing and catastrophic health spending are calculated using microdata from nationally representative household budget surveys, which are typically available with a time lag of two years. Many countries only collect data every five years and some only make microdata available to national researchers. As a result, microdata were obtained and analysed on a country-by-country basis by WHO/Europe or country experts or both, which means we do not have a single, harmonised dataset. Also, to enhance international comparability, we focus on one year only, giving us a total of 40 observations. We do not use statistical methods to explore relationships between financial hardship and other factors because we do not think it is plausible to draw causal inference in this way with only 40 observations.
The financial hardship results we report for the Netherlands cannot be compared to other countries, are likely to be an underestimate, and should be interpreted with caution. In contrast to every other country in the study, the Dutch household budget survey does not include data on household spending through the deductible (a form of user charge that is applied to many publicly financed health services in the Netherlands) because the Dutch authorities view the deductible as mandatory spending (i.e. like a tax) rather than out-of-pocket spending. This is inconsistent with internationally recognized standards for classifying health spending (the System of Health Accounts)13 and biases the incidence of catastrophic health spending in the Netherlands downwards.
For a more detailed description of the WHO/Europe approach to measuring financial hardship, see Cylus et al. (2018),9 WHO Regional Office for Europe (2019),3 and the supplementary file.
We complement our analysis of financial hardship using survey data on the level and distribution of unmet need for health care, dental care, and prescribed medicines. These data are publicly available from the Eurostat database and come from nationally representative household surveys that ask people if there was a time in the last year when they needed health care but were not able to access it due to health system factors such as cost, distance or waiting time.14
Self-reported data on unmet need for health care (‘medical examination or treatment’) and unmet need for dental care (‘dental examination or treatment’) due to cost, distance and waiting time are available for 34 of the study countries and come from European Union Statistics on Income and Living Conditions (EU-SILC), an annual survey carried out in EU countries and Albania, Montenegro, North Macedonia, Serbia, Switzerland, and Türkiye. The denominator for unmet need is people aged 16 years and over.
Data on unmet need for prescribed medicines due to cost are available for 29 of the study countries from the European Health Interview Survey (EHIS) carried out in EU countries and Serbia and Türkiye. The denominator for unmet need is different from EU-SILC—it is people aged 15 years and over reporting a need for prescribed medicines—so the two sets of results are not comparable.
To illustrate how out-of-pocket payments can affect people differently we aggregate data on unmet need for dental care by income quintile and the role of dental care in driving catastrophic health spending by consumption quintile in 33 countries.
Identifying the coverage policy choices that undermine financial protection
People are exposed to out-of-pocket payments when the way in which health coverage is designed and implemented leads to the following gaps, which may in turn lead to unmet need and financial hardship.3
-
•
People are not covered (or not fully covered) because entitlement to most publicly financed health care is based on criteria that they do not meet—for example, legal residence, payment of contributions to a social health insurance (SHI) scheme, income, employment or age.
-
•
The range of health services that is publicly financed—the benefits package—is not broad enough to meet population health needs.
-
•
There are user charges (co-payments) in place for covered health care, without effective protection mechanisms.
-
•
Administrative barriers prevent people from accessing entitlements.
As we noted in the introduction, coverage policy is complex and multi-dimensional. An absence of indicators makes it difficult to assess the comprehensiveness of coverage at country level—a challenge that is magnified when comparing across countries. It is also difficult to disentangle the effects of different dimensions. The following paragraphs summarise these challenges and describe the approach we use in this study.
The share of the population entitled to publicly financed health care (referred to as population coverage) is amenable to international comparison, but it is not always monitored at country level; it typically focuses on coverage of legal residents and is therefore likely to be overestimated because undocumented migrants lack coverage in many countries that report covering the whole population3,15; and it fails to capture in-country variation in the range of health care to which covered people are entitled. Bearing in mind these limitations, we identify the level of population coverage, which we define as the share of the population covered by the main publicly financed benefits package, and the principal basis for entitlement in 39 of the 40 countries.
There are very few benchmarks for the adequacy of the publicly financed benefits package; most countries do not define the whole of the benefits package in detail,16 so it is difficult to determine the extent of coverage at country level; complexity—in this case, the wide range of health services that should be covered, from prevention to palliative care—makes international comparison particularly challenging; and if covered health services are subject to user charges it can be hard to distinguish the effects of these two dimensions. We do not attempt a systematic assessment of benefits packages.
A large body of evidence shows that even relatively small user charges can prevent people from using needed health care, reduce adherence to treatment, lead to financial hardship, and adversely affect health.17, 18, 19, 20, 21, 22, 23 If applied, user charges should therefore be carefully designed to protect people through mechanisms such as exemptions, caps, and the replacement of percentage co-payments with low, fixed co-payments.3,24 Significant variation in the application and design of user charges across countries is a challenge for measurement and international comparison. In the absence of a single indicator, we identify the presence of user charges for the six categories of health care listed above and map key elements of the design of user charges policy for outpatient prescribed medicines (the main driver of financial hardship in Europe) in 40 countries, highlighting the type of user charge and exemptions and caps.
The information on coverage policy we present comes mainly from a WHO/Europe series of country-based reports on financial protection and a new online platform, UHC watch,11 complemented in some cases by information from key informants (the European Financial Protection Network), the MISSOC database25 and Health System in Transition reports.26 We gathered information on user charges using a questionnaire (see the Supplementary File). The coverage policy information obtained from these sources was reviewed by at least two of the authors, including the first author.
Role of the funding source
The funders had no role in study design, data collection, data analysis, data interpretation or preparation of the manuscript.
Results
Assessing financial protection
Fig. 1, Fig. 2, Fig. 3 show the level, distribution, and drivers of financial hardship due to out-of-pocket payments in 40 countries in 2019 or the latest available year before COVID-19. These results are based on our analysis of microdata from national household budget surveys.
Fig. 1.
Share of households with impoverishing health spending, 2019 or the latest available year before COVID-19. Notes: AL: Albania, AM: Armenia, AT: Austria, BA: Bosnia and Herzegovina, BE: Belgium, BG: Bulgaria, CH: Switzerland, CY: Cyprus, CZ: Czechia, DE: Germany, DK: Denmark, EE: Estonia, EL: Greece, ES: Spain, FI: Finland, FR: France, GE: Georgia, HR: Croatia, HU: Hungary, IE: Ireland, IL: Israel, IT: Italy, LT: Lithuania, LU: Luxembourg, LV: Latvia, MD: Republic of Moldova, ME: Montenegro, MK: North Macedonia, MT: Malta, NL: Netherlands, PL: Poland, PT: Portugal, RO: Romania, RS: Serbia, SE: Sweden, SI: Slovenia, SK: Slovakia, TR: Türkiye, UA: Ukraine, UK: United Kingdom. The Netherlands cannot be compared to other countries for the reasons set out in the methods section.
Source: WHO Regional Office for Europe.
Fig. 2.
Share of households with catastrophic health spending by consumption quintile, 2019 or the latest available year before COVID-19. Notes: see the list of abbreviations and the note on the Netherlands in Fig. 1. Consumption quintiles are based on per person consumption adjusted for household size and composition using OECD equivalence scales.
Source: WHO Regional Office for Europe.
Fig. 3.
Breakdown of out-of-pocket payments by type of health care in households with catastrophic health spending on average (a) and in the poorest consumption quintile (b), 2019 or the latest available year before COVID-19. Notes: see the list of abbreviations and the note on the Netherlands in Fig. 1. Countries are sorted by the incidence of catastrophic health spending (lowest in Slovenia, highest in Armenia). Different types of health care are sorted by the average across countries. In Spain dentures are classified as medical products in the household budget survey; in most other countries they are classified as dental care. In Ukraine the medicines category includes inpatient medicines; in most other countries the medicines category refers to outpatient medicines only. Data are not available for Switzerland.
Source: WHO Regional Office for Europe.
Out-of-pocket payments lead to financial hardship in all 40 countries. The incidence of impoverishing health spending ranges from under 1% of households in Belgium, Ireland, Slovenia, Spain, and the United Kingdom to over 4% in Bosnia and Herzegovina, Georgia, Hungary, Italy, Latvia, Lithuania, Montenegro, the Republic of Moldova and Romania, and over 7% in Albania, Armenia, Bulgaria, Serbia, and Ukraine, with a median value of 3% (Fig. 1). The incidence of catastrophic health spending ranges from under 2% of households in Ireland, Spain, Slovenia, Sweden and the United Kingdom to over 14% in Armenia, Bulgaria, Georgia, Latvia, Lithuania, and Ukraine, with a median value of 6% (Fig. 2).
Households in the poorest consumption quintile are most likely to experience financial hardship due to out-of-pocket payments. They account for at least 40% of households with catastrophic health spending in every country in the study and for over 70% in Croatia, Czechia, Hungary, Ireland, France, Luxembourg, Slovakia, and Sweden (Fig. 2). Within countries, the incidence of catastrophic health spending in the poorest quintile is two to four times higher than the national level. In 33 out of 40 countries, at least 20% of households with catastrophic health spending are also further impoverished after out-of-pocket payments—that is, they do not have enough to meet their basic needs but still incur out-of-pocket payments (data not shown). This share rises to 40% in 15 out of 40 countries.
Outpatient medicines are the main driver of financial hardship, accounting on average for 38% of out-of-pocket payments in households with catastrophic health spending, followed by dental care (18%), medical products (15%), inpatient care (13%), and outpatient care (10%) (Fig. 3). In the poorest consumption quintile, the outpatient medicines share of catastrophic health spending rises to 60% and the share spent on the other types of care falls to 12% (medical products), 10% (dental care), 8% (outpatient care), and 5% (inpatient care).
Across countries, drivers differ depending on the extent of catastrophic health spending. In countries with a lower incidence of catastrophic health spending (below the median value of 6% of households), the main drivers are dental care (26%), followed by medical products (22%) and outpatient medicines (19%); the other shares remain similar. In countries with a higher incidence (above the median value), the main driver is overwhelmingly outpatient medicines (55%), followed by inpatient care (13%), dental care (10%), and medical products (8%).
Within countries, drivers differ by household socioeconomic status. Outpatient medicines consistently account for a larger share of catastrophic health spending in the poorest quintile than in the other quintiles (Fig. 3). Conversely, inpatient care and dental care usually account for a larger share of catastrophic health spending in richer than poorer quintiles.
Figs. 4 and 5 show publicly available data on self-reported unmet need for health care, dental care, and prescribed medicines on average and by income quintile.
Fig. 4.
Unmet need for health care (a) and dental care (b) due to cost, distance, and waiting time by income quintile, 2019 or the latest available year before COVID-19. Notes: see the list of abbreviations and the note on the Netherlands in Fig. 1. Countries are sorted by the incidence of catastrophic health spending (lowest in Slovenia, highest in Bulgaria). Data on unmet need for health and dental care are for the same year as data on catastrophic health spending, except for Albania (2017). Data are not available for all countries.
Source: WHO Regional Office for Europe, using EU-SILC data from Eurostat.14
Fig. 5.
Unmet need for prescribed medicines due to cost by income quintile, 2019. Notes: see the list of abbreviations and the note on the Netherlands in Fig. 1. Countries are sorted by the incidence of catastrophic health spending (lowest in Slovenia, highest in Bulgaria). Data are not available for all countries.
Source: WHO Regional Office for Europe, using EHIS data from Eurostat.14
EU-SILC data on unmet need for health care and dental care due to cost, distance, and waiting time indicate that dental care (Fig. 4b) is a greater driver of unmet need than health care (Fig. 4a). EHIS data on unmet need for health care, dental care, and prescribed medicines due to cost also find dental care to be the largest driver of unmet need, followed by health care and prescribed medicines (data not shown but available from Eurostat).14
Cost is usually the main reason people give for unmet need for health care, but in some countries waiting time is either the main reason (Czechia, Denmark, Estonia, Finland, Lithuania, Poland, Spain, Slovakia, Slovenia, Sweden, and the United Kingdom) or on a par with cost (Germany) (data not shown but available from Eurostat).14 Cost is the main reason given for unmet need for dental care in all except Finland and Slovenia, where the main reason is waiting time.
For all three types of health care, levels of unmet need are consistently higher among people in the poorest income quintile (Figs. 4 and 5).
Looking at unmet need and financial hardship together shows that in countries with a higher incidence of catastrophic health spending, levels of unmet need for health care, dental care and prescribed medicines are generally also higher (Figs. 4 and 5). There is a similar pattern for health care in countries with a below median incidence of catastrophic health spending: in many of these countries, unmet need for health care and income inequality in unmet need for health care are also lower (with some exceptions—Belgium, Croatia, Finland, Ireland, Slovenia, Türkiye, and the United Kingdom) (Fig. 4a). In contrast, unmet need for dental care and prescribed medicines—and income inequality in unmet need—are often quite high in countries with a below median incidence of catastrophic health spending (Figs. 4b and 5).
Looking at unmet need and financial hardship together also shows that gaps in the coverage of different types of health care can affect richer and poorer people differently. Fig. 6 shows that across countries dental care is often a larger driver of financial hardship in richer households (the columns), reflecting higher levels of unmet need for dental care in poorer households (the dots). In contrast, outpatient medicines lead to high levels of financial hardship and unmet need for poorer households (see Figs. 3b and 5).
Fig. 6.
Dental care as a share of out-of-pocket payments in households with catastrophic health spending and the share of people reporting unmet need for dental care due to cost, distance, and waiting time by quintile, 2019 or the latest available year before COVID-19. Notes: data are for 33 out of the 34 countries in the study for which data on unmet need are available and are for the same year as the incidence of catastrophic health spending except for the United Kingdom (unmet need data are for 2018). People refers to those aged 16 years and over. Quintiles are based on consumption for catastrophic health spending and income for unmet need.
Source: WHO Regional Office for Europe, using EU-SILC data on unmet need from Eurostat.14
Identifying the coverage policy choices that undermine financial protection
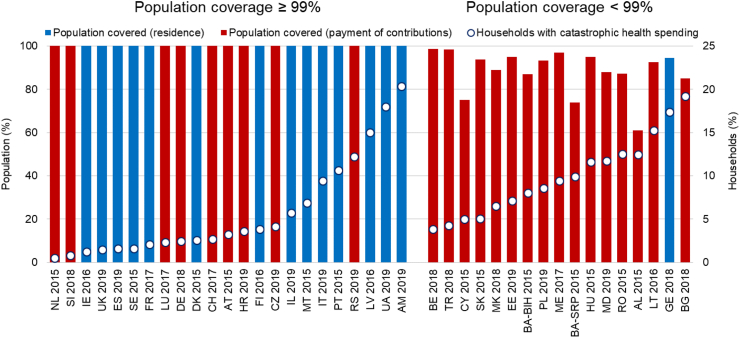
Fig. 7 combines the incidence of catastrophic health spending with information on population coverage and the principal basis for entitlement to publicly financed health care in 39 countries. It shows that 23 out of the 39 countries report universal (100%) or near universal (over 99%) population coverage (those on the left of Fig. 7). In the remaining 16 countries (those on the right of Fig. 7), the share of the population lacking coverage ranges from around 1.5% in Belgium and Türkiye to 15% in Bulgaria, 25% in Cyprus, and 39% in Albania.
Fig. 7.
Population coverage, the main basis for entitlement to publicly financed health care, and catastrophic health spending, 2019 or the latest available year before COVID-19. Notes: see the list of abbreviations and the note on the Netherlands in Fig. 1. The share of the population covered is for the same year as catastrophic health spending and does not necessarily reflect the current situation. Blue columns: the main basis for entitlement is legal residence. Red columns: the main basis for entitlement is payment of contributions. Authorities in Bosnia and Herzegovina report different levels of population coverage for the Federation of Bosnia and Herzegovina and the Republic of Srpska. The figure excludes Greece because we could not find published data on the share of the population covered by the SHI scheme, which offers the main publicly financed benefits package.
Source: WHO Regional Office for Europe, using OECD27 for population coverage in OECD countries and WHO/Europe reports on financial protection or UHC watch for population coverage in non-OECD countries.
In countries that report universal or near universal coverage, the principal basis for entitlement is evenly divided between legal residence (the blue columns) and payment of contributions to a social health insurance (SHI) scheme (the red columns). In contrast, in countries with lower levels of population coverage (those on the right of Fig. 7, entitlement to publicly financed health care is overwhelmingly linked to payment of SHI contributions (the red columns). The sole exception is Georgia, where people with high incomes do not have access to the full range of publicly financed health care.28
The median incidence of catastrophic health spending is three times lower in countries that report universal or near universal coverage (3%) than in the countries with larger gaps in population coverage (9%).
Even in countries that report covering the whole population, however, the incidence of catastrophic health spending ranges from under 1% of households to over 20%. This suggests that being covered is not enough to guarantee financial protection12—other aspects of coverage policy are likely to play a role too.
Tables 1 and 2 combine the incidence of catastrophic health spending with information on user charges for different types of health care (Table 1) and the design of user charges for outpatient prescribed medicines (Table 2) in 40 countries.
Table 1.
User charges for publicly financed health are by type of care and catastrophic health spending, 2019 or the latest available year before COVID-19.
| Country | Year | Catastrophic health spending (% households) | Emergency visits | Primary care visits | Diagnostic tests | Specialist visits | Inpatient care | Medical products | Dental care | Outpatient prescribed medicines |
|---|---|---|---|---|---|---|---|---|---|---|
| NL | 2015 | 0.5 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| SI | 2018 | 0.8 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| IE | 2016 | 1.2 | Yes | Varies | No | No | Yes | Varies | Varies | Yes |
| UK | 2019 | 1.5 | No | No | No | No | No | Yes | Yes | Yes |
| ES | 2019 | 1.6 | No | No | No | No | No | Yes | Varies | Yes |
| SE | 2015 | 1.6 | No | Yes | No | Yes | Yes | Yes | Yes | Yes |
| FR | 2017 | 2.1 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| LU | 2017 | 2.3 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| DE | 2018 | 2.4 | No | No | No | No | Yes | Yes | Yes | Yes |
| DK | 2015 | 2.6 | No | No | No | No | No | Yes | Yes | Yes |
| CH | 2017 | 2.9 | Yes | Yes | Yes | Yes | Yes | Yes | Varies | Yes |
| AT | 2015 | 3.2 | No | Yes | No | Yes | Yes | Yes | Yes | Yes |
| HR | 2019 | 3.6 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| FI | 2016 | 3.8 | Yes | Yes | No | Yes | Yes | Varies | Yes | Yes |
| BE | 2018 | 3.8 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| CZ | 2019 | 4.2 | Yes | No | No | No | No | Yes | Yes | Yes |
| TR | 2018 | 4.3 | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| CY | 2015 | 5.0 | Yes | Yes | Yes | Yes | Varies | No | Yes | Yes |
| SK | 2015 | 5.1 | Yes | No | No | No | No | Yes | Yes | Yes |
| IL | 2019 | 5.7 | No | No | Yes | Yes | No | No | Yes | Yes |
| MK | 2018 | 6.5 | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| MT | 2015 | 6.9 | No | No | No | No | No | Varies | Varies | Varies |
| EE | 2019 | 7.2 | Yes | No | No | Yes | Yes | Yes | Yes | Yes |
| PL | 2019 | 8.6 | No | No | No | No | No | Yes | No | Yes |
| BA | 2015 | 8.8 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| EL | 2019 | 8.9 | No | No | Yes | No | Yes | Yes | Yes | Yes |
| ME | 2017 | 9.4 | No | Yes | Yes | Yes | Yes | Yes | Varies | Yes |
| IT | 2019 | 9.4 | Yes | No | Yes | Yes | No | No | Yes | Yes |
| PT | 2015 | 10.6 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| HU | 2015 | 11.6 | No | No | No | No | No | Yes | Yes | Yes |
| MD | 2019 | 11.7 | No | No | No | No | No | No | Varies | Yes |
| RS | 2019 | 12.2 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| AL | 2015 | 12.5 | No | No | Yes | No | No | No | Varies | Yes |
| RO | 2015 | 12.5 | No | No | No | No | Yes | Yes | Yes | Yes |
| LV | 2016 | 15.0 | No | Yes | Yes | Yes | Yes | Yes | Varies | Yes |
| LT | 2016 | 15.2 | No | No | No | No | No | No | Varies | Yes |
| GE | 2018 | 17.4 | Yes | Varies | Yes | Yes | Yes | No | Not covered | Yes |
| UA | 2019 | 18.0 | No | No | No | No | No | No | No | Yes |
| BG | 2018 | 19.2 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| AM | 2019 | 20.3 | No | No | Yes | No | Yes | Not covered | Yes | Yes |
Notes: see the list of abbreviations and the note on the Netherlands in Fig. 1. Countries are sorted by the incidence of catastrophic health spending (lowest in Slovenia, highest in Armenia). Types of health care are sorted based on the application of user charges. Information on user charges is for the same year as data on catastrophic health spending and may not reflect the current situation. Yes: user charges are applied. No: user charges are not applied. Varies: there are no user charges for some covered people but other people must pay the full price out of pocket. Not covered: the type of care is not covered. Balance billing is treated as a type of user charge. The table does not capture extra billing. In Greece, user charges apply to inpatient care and diagnostic tests in contracted private facilities. In the United Kingdom, user charges for medical products and outpatient medicines are only applied in England. The range of covered diagnostic tests, medical products, dental care and outpatient prescribed medicines varies substantially across countries.
Table 2.
User charges for publicly financed outpatient prescribed medicines and catastrophic health spending, 2019 or the latest available year before COVID-19.
| Country | Year | Catastrophic health spending (% households) | Type of user charge | Exemption from user charges | Cap on user charges |
|---|---|---|---|---|---|
| NL | 2015 | 0.5 | D, RP | Yes, but not based on income | No, but the deductible limits co-payments |
| SI | 2018 | 0.8 | PC, RP | Yes, based on income | No, but VHI covers co-payments for >90% of the population |
| IE | 2016 | 1.2 | FC | Yes, but not based on income | Yes, based on income |
| UK | 2019 | 1.5 | FC | Yes, based on income | Yes, but not based on income; only for people who request it in advance |
| ES | 2019 | 1.6 | PC | Yes, based on income | Yes, based on income, but only for pensioners |
| SE | 2015 | 1.6 | D, PC | Yes, based on income | Yes, but not based on income |
| FR | 2017 | 2.1 | FC, PC | Yes, based on income for FC, but not based on income for PC | No, but VHI covers co-payments for >90% of the population and is provided for free to people with low incomes |
| LU | 2017 | 2.3 | PC, RP | Yes, but not based on income | Yes, based on income |
| DE | 2018 | 2.4 | PC, RP | Yes, but not based on income | Yes, based on income |
| DK | 2015 | 2.6 | D, FC, PC, RP | Yes, based on income | Yes, but not based on income |
| CH | 2017 | 2.9 | D, PC | Yes, but not based on income | Yes, but not based on income |
| AT | 2015 | 3.2 | FC | Yes, based on income | Yes, based on income |
| HR | 2019 | 3.6 | FC, RP | Yes, but not based on income | No, but VHI covers co-payments for most people who have to make co-payments and is provided for free to people with low incomes |
| FI | 2016 | 3.8 | D, PC | Yes, based on income | No, but there is a threshold for reduced co-payments |
| BE | 2018 | 3.8 | FC, PC, RP | Yes, but not based on income | Yes, based on income |
| CZ | 2019 | 4.2 | RP | No | Yes, but not based on income |
| TR | 2018 | 4.3 | FC, PC | Yes, but not based on income | No |
| CY | 2015 | 5.0 | FC | No | No |
| SK | 2015 | 5.1 | PC | Yes, but not based on income | Yes, but not based on income and only for disabled people, pensioners, and people above 60 |
| IL | 2019 | 5.7 | PC | Yes, but not based on income | Yes, but not based on income and only for people with chronic conditions |
| MK | 2018 | 6.5 | PC, RP | Yes, but not based on income | No |
| MT | 2015 | 6.9 | None for some covered people | NA | NA |
| EE | 2019 | 7.2 | FC, PC, RP | Yes, but not based on income | No, but there is a threshold for reduced co-payments |
| PL | 2019 | 8.6 | FC, PC, RP | Yes, but not based on income | No |
| BA | 2015 | 8.8 | FC, PC, RP | Yes, based on income (some cantons) | No |
| EL | 2019 | 8.9 | FC, PC, RP | Yes, based on income | No |
| ME | 2017 | 9.4 | FC | Yes, based on income | No |
| IT | 2019 | 9.4 | FC, RP | Yes, based on income (some regions) | No |
| PT | 2015 | 10.6 | PC | Yes, but not based on income | No |
| HU | 2015 | 11.6 | PC | Yes, but not based on income | No |
| MD | 2019 | 11.7 | FC, PC, RP | Yes, based on income | No |
| RS | 2019 | 12.2 | FC, PC | Yes, but not based on income | No |
| AL | 2015 | 12.5 | PC, RP | Yes, but not based on income | No |
| RO | 2015 | 12.5 | PC | Yes, but not based on income | No |
| LV | 2016 | 15.0 | FC, PC, RP | Yes, based on income | No |
| LT | 2016 | 15.2 | PC, RP | Yes, but not based on income | No |
| GE | 2018 | 17.4 | PC | Yes, based on income | No |
| UA | 2019 | 18.0 | RP | Yes, but not based on income | No |
| BG | 2018 | 19.2 | PC, RP | Yes, but not based on income | No |
| AM | 2019 | 20.3 | PC | Yes, based on income | No |
Notes: see the list of abbreviations and the note on the Netherlands in Fig. 1. Countries are sorted by the incidence of catastrophic health spending (lowest in Slovenia, highest in Armenia). Information on user charges is for the same year as data on catastrophic health spending and may not reflect the current situation. D: deductible. FC: fixed co-payment. PC: percentage co-payment. RP: reference pricing. Malta has no user charges for covered outpatient prescribed medicines; people pay the full price out of pocket if they are not entitled to a ‘yellow’ or ‘pink’ card. The range of covered outpatient prescribed medicines varies across countries.
Table 1 shows that user charges are present in all of the study countries: 14 countries apply user charges to emergency visits; 18 to primary care visits; 22 to diagnostic tests; 23 to specialist visits; 25 to inpatient care; 31 to medical products (and not covered at all in 1 country); 37 to dental care (not covered in 1); and 40 to outpatient prescribed medicines. Only four countries apply user charges to all types of health care (Belgium, France, Luxembourg, and Switzerland).
There appears to be substantial variation in the application of user charges and the incidence of catastrophic health spending across countries, which may reflect differences in the design of user charges policy across countries—the type of user charges in place, the presence of mechanisms to protect people from user charges (for example, exemptions and caps), and the extent to which these mechanisms explicitly aim to protect people with low incomes. It could also reflect differences in the range of services covered, particularly for dental care, medical products and medicines.
Table 2, which focuses on the design of user charges for outpatient prescribed medicines, shows that percentage co-payments (user charges defined as a share of the medicine price) are the most common type of user charge in place (applied in 29 of the 40 countries). Only four countries only use fixed co-payments (user charges defined as a flat rate). All 40 countries attempt to protect people from co-payments for outpatient prescribed medicines, but the design of protection mechanisms—and the extent to which they aim to protect people with low incomes—varies significantly. Although all 40 countries have exemptions from co-payments, only 13 explicitly exempt people with low incomes. While 13 countries have a cap on co-payments for medicines, only 5 link the cap to a person's income, so that it is lower (more protective) for people with low incomes.
Countries that give greater protection from user charges for outpatient prescribed medicines to people with low incomes have lower levels of catastrophic health spending: 13 of the 20 countries with a lower incidence of catastrophic health spending (below the median of 6% of households) exempt people with low incomes from co-payments or have a cap that is linked to income or (in rare instances) provide free voluntary health insurance (VHI) covering co-payments to people with low incomes. In contrast, there is no cap in any of the 20 countries with a higher incidence of catastrophic health spending (above the median) and only 6 exempt people with low incomes from co-payments.
Discussion
We have assessed the level, distribution, and drivers of financial hardship and unmet need in 40 countries in 2019 or the latest available year before the COVID-19 pandemic to establish a pre-pandemic baseline for Europe. We paired this with analysis of two key dimensions of coverage policy (population coverage and user charges) to identify the coverage policy choices that undermine financial protection. Our findings can be summarised as follows.
Assessing financial protection: Out-of-pocket payments for health care lead to financial hardship and unmet need in every country in the study. These negative outcomes are consistently higher among people with lower incomes than people with higher incomes. Financial hardship is mainly driven by out-of-pocket payments for outpatient medicines, medical products, and dental services. Gaps in coverage affect people differently: out-of-pocket payments for dental care lead to financial hardship for richer households and unmet need for poorer households, while out-of-pocket payments for outpatient medicines result in both financial hardship and unmet need for poorer households.
Identifying the coverage policy choices that undermine financial protection: The median incidence of catastrophic health spending is three times lower in countries that report universal (100%) or near universal (>99%) population coverage than in countries with larger gaps in population coverage (<99%). Larger gaps in population coverage overwhelmingly occur in countries that base entitlement to publicly financed health care on payment of SHI contributions. Being covered is not enough to guarantee financial protection, however, because even in countries that report covering the whole population, the incidence of catastrophic health spending ranges from under 1% of households to over 20%. Countries that give greater protection from user charges to people with low incomes (through exemptions), and have caps on user charges, have lower levels of catastrophic health spending than countries without these protection mechanisms.
In the following paragraphs we explore our main findings in more detail, first discussing their implications for policy and then commenting on their implications for the monitoring of financial protection.
Coverage policy matters. Looking more closely at the people and services affected by policy choices that limit coverage helps to explain why financial hardship and unmet need are concentrated in people with low incomes and so heavily driven by household spending on outpatient medicines, medical products, and dental care.
Although being covered does not guarantee financial protection, it is likely to be a prerequisite for financial protection for two reasons. First, people who lack coverage rarely benefit from publicly financed access to non-urgent treatment of chronic conditions; their entitlements are usually limited to emergency care, treatment of some communicable diseases and, in a few countries, some outpatient visits.3,11,15 Gaps in population coverage are therefore likely to lead to substantial unmet need as well as financial hardship, and to increase inefficiency in the use of health care when people self-treat using over-the-counter medicines, are unable to adhere to treatment or benefit from coordinated care, delay seeking care or to turn to resource-intensive emergency services.17,18,21,23
Second, people who lack coverage tend to have low incomes. The largest gaps in population coverage are in countries that base entitlement on payment of contributions. With a few notable exceptions (France, for example), countries in Europe with contributory SHI schemes penalise people who do not pay contributions (when they are required to do so) by restricting their access to some or all publicly financed health care. This approach is most likely to cause gaps in coverage in countries with weak tax systems and a sizeable informal economy.29 As a result, non-covered people are typically those who face financial or administrative barriers to paying contributions because they lack work or their work is precarious—temporary, insecure, poorly paid and often informal.
By choosing to exclude or limit coverage for people who do not pay contributions, countries are using the health system to tackle a taxation problem, despite any evidence to suggest that health systems are effective in addressing weaknesses in tax collection or reducing labour market informality.30 It would be better for contributory schemes to let the tax agency deal with non-payment of mandatory contributions—something that countries with residence-based entitlement do as a matter of course.
Undocumented migrants, refugees and asylum seekers lack adequate coverage in many countries in Europe, even in those that report covering the whole population.3,11,15 Although this gap is small—undocumented migrants account for less than 1% of Europe's population31—it is likely to undermine financial protection because these groups of people are at very high risk of poverty and social exclusion.32
Our findings indicate that financial protection is largely undermined by gaps in the coverage of treatment in primary care. The main drivers of financial hardship are out-of-pocket payments for outpatient medicines, medical products, and dental care, all of which are included in international definitions of primary care spending.13,33,34 Professionals providing first contact care typically manage dental care and the treatment of vision and hearing problems; in this sense, they are (or should be) an essential part of primary care.
As with gaps in population coverage, gaps in the coverage of treatment in primary care settings are most likely to undermine financial protection for people with low incomes and chronic conditions. Richer households are more likely to be able to afford to pay for health care, even if it is needed on a regular basis, whereas households with low incomes may be forced to prioritise spending on outpatient medicines and experience unmet need for medicines and other services. This may explain why spending on outpatient medicines is a consistently larger driver of financial hardship among households with lower incomes, and why these households are more likely to experience unmet need.
Gaps in the coverage of primary care treatment reflect the limited scope of publicly financed benefits packages in some cases. For example, coverage of outpatient medicines is very limited in middle-income countries such as Georgia, the Republic of Moldova, and Ukraine,28,35,36 while coverage of outpatient dental care is limited not just in middle-income countries but in many high-income countries too.37 In many cases, however, these gaps reflect the application and design of user charges for covered services. User charges are most widely applied to outpatient medicines, dental care and medical products (see Table 1) and the design of user charges for outpatient prescribed medicines is much weaker in countries with a higher incidence of catastrophic health spending (see Table 2).
There are several implications for policy here.
First, covering higher cost specialist and inpatient treatment is not enough to secure financial protection. Our analysis suggests that the use of lower cost health care can be a major driver of unmet need and financial hardship.
Second, primary care involves more than just consultation and diagnosis and should not be seen as complete if it does not offer affordable access to treatment—especially medicines, but also treatment of dental, vision, and hearing problems.
Third, the design of user charges is an important determinant of financial protection, especially in countries that cover the whole population and in which the publicly financed benefits package is relatively comprehensive. In line with a large body of international evidence on the negative effects of even relatively small user charges,17, 18, 19, 20, 21, 22, 23 our analysis suggests that user charges should be applied sparingly; carefully designed to exempt people with low incomes or chronic conditions; and accompanied by an income-based cap that applies to all user charges. From country-level analysis we know that other factors are also important: keeping the design of user charges policy as simple and transparent as possible and using low, fixed co-payments rather than percentage co-payments to increase financial certainty for people using health care24; removing administrative barriers that stop people benefiting from protection mechanisms—digital tools can play a role in this38; and regular monitoring to make sure protection mechanisms are effective.3
How financial protection is monitored matters. WHO/Europe's equity-sensitive financial hardship metrics account for household capacity to pay for health care in a way that ensures that the effective threshold households must cross to be counted as incurring catastrophic health spending is consistently higher for richer than poorer households. Using a method that holds richer households to a higher standard offers two important advantages. First, it means our study is less likely to overestimate financial hardship among richer households and underestimate it among those with low incomes.2,9 Second, it means we are less likely to define so-called ‘discretionary’ or non-medically justified spending on health care as being catastrophic. Analysis of financial hardship encompasses all out-of-pocket payments, not only because the data involved do not allow us to isolate non-medically justified spending, but also because people may not know whether a good or service is medically justified or not, especially if it has been prescribed by a health care professional. If we assume, however, that spending on things like ‘cosmetic’ dentistry or expensive frames for glasses are more likely to be concentrated in richer households, out-of-pocket payments for these items will not be counted as catastrophic, unless they make up a very large share of a household's budget, due to the much higher effective threshold richer households face.
Country averages conceal major differences in impact. Looking at the distribution of financial hardship and unmet need across the population—and looking at these two indicators together—alerts us to the fact that out-of-pocket payments for different types of health care have different effects on richer and poorer households: some out-of-pocket payments do not drive financial hardship simply because they deter people from using health care. It also provides guidance on where countries should focus. Since financial hardship and unmet need are heavily concentrated in households with low incomes, progress towards UHC means reducing out-of-pocket payments for the most disadvantaged people in society first—an approach known as progressive universalism.39
Finally, although comparative analysis of coverage policy is challenging, it is essential to understanding why people lack financial protection and what countries can do to mitigate the damage caused by out-of-pocket payments. Our analysis has identified three common coverage policy choices that are likely to undermine financial protection and have a disproportionately negative impact on people with low incomes and chronic conditions: basing entitlement on payment of SHI contributions, limited coverage of treatment in primary care settings (outpatient medicines, medical products and dental care), and applying user charges to health care without effective protection mechanisms.
Limitations
We have used the most internationally comparable data available on unmet need and financial hardship, but the surveys they are derived from have several limitations.
First, classification tools such as the European Classification of Individual Consumption according to Purpose (ECOICOP) support the standardisation of household budget surveys across countries, but do not fully address variation in instruments and implementation.40 Because financial hardship indicators measure household spending ratios rather than absolute amounts, however, we do not think this variation is a major problem.
Second, the survey data we use do not adequately represent typically underserved groups of people, including refugees, asylum seekers, undocumented migrants, and homeless people, or people living in institutions14,41; nor do they allow us to identify households with these characteristics. We have partly addressed this limitation by providing information on the types of publicly financed health care to which ‘non-covered’ people are entitled.
Third, out-of-pocket payments for mental health care and long-term health care are likely to be an important driver of financial hardship and unmet need in Europe, but household budget surveys do not allow us to identify spending on these types of care.
Fourth, self-reported data on unmet need should be interpreted with caution, especially across countries. However, analyses have found a positive relationship between unmet need and a subsequent deterioration in health,42 and between unmet need and the out-of-pocket payment share of current spending on health,43 which suggests that unmet need can be a useful indicator of affordable access to health care.
Despite these limitations, the surveys we use enable valuable analysis. To improve data availability and quality, we encourage national statistics offices to carry out household budget surveys with greater regularity. We suggest that EU-SILC could be improved by adding questions on unmet need for prescribed medicines and unmet need for selected medical products, in addition to health care and dental care. Countries that are not currently part of EU-SILC should join it or add EU-SILC questions on unmet need to their own surveys, so that it is possible to compare unmet need across countries outside the European Union.
The focus of our policy analysis has been on coverage, but financial protection can be undermined by other factors such as staff shortages, service availability, quality of care, waiting times, and informal payments. Although we would expect the bulk of out-of-pocket payments arising from these factors to be concentrated in outpatient care and inpatient care, these types of health care do not drive financial hardship in most countries. One reason for this may be that richer households can afford to overcome problems such as long waiting times by paying for faster access out of pocket, or through voluntary health insurance, while households with lower incomes forego treatment and experience unmet need instead.
It has been challenging to identify with certainty the coverage policy choices that undermine financial protection because of the complexity involved; the lack of benchmarks and indicators; the difficulty of disentangling the effects of different dimensions within and across countries; and the small number of observations in our study, which ruled out statistical tests. The conclusions we have drawn are therefore tentative, though plausible.
Future efforts to monitor financial protection in Europe will be helped by UHC watch,11 WHO/Europe's new online platform, which not only makes data on financial hardship publicly available but also systematically collects and disseminates up to date country-level information on coverage policy.
Conclusions
This study is the first to assess the level, distribution, and drivers of financial protection in 40 countries in Europe, including the whole of the European Union. It provides a solid foundation for evidence-informed policy by using equity-sensitive metrics, looking at financial hardship and unmet need together, and taking steps to identify some of the coverage policy choices that undermine financial protection.
The study's findings and discussion suggest that countries are more likely to move towards UHC if they reduce out-of-pocket payments in a progressive way, decreasing them for people with low incomes first. Coverage policy choices that seem likely to achieve this include de-linking entitlement to publicly financed health care from payment of SHI contributions in countries with contributory SHI schemes; expanding the coverage of outpatient medicines, medical products, and dental care, so that primary care covers treatment as well as consultations and diagnosis; limiting the use of user charges; and strengthening protection against user charges, particularly for people with low incomes or chronic conditions.
Contributors
Sarah Thomson (ST), Jon Cylus (JC), Lynn Al Tayara (LT), Marcos Gallardo Martínez (MG), Jorge Alejandro García-Ramírez (JG), María Serrano Gregori (MS), José Cerezo-Cerezo (JCC), Marina Karanikolos (MK) and Tamás Evetovits (TE) contributed to obtaining and analysing microdata and information on coverage policy. JC and at least one other author verified the microdata analysis. ST and at least one other author verified the information on coverage policy. LT and MS prepared the tables. MG prepared the charts, the tables in the supplementary material, and the references. ST coordinated the study and led the writing of the manuscript. ST, JC and TE planned the manuscript. All authors contributed to the interpretation of results and critical revision of the draft. All authors approved the submission.
Data sharing statement
Data on health spending are publicly available from the WHO Global Expenditure Database and the OECD health database. Data on unmet need are publicly available from Eurostat. Microdata from household budgets surveys must be requested from national statistical offices in most countries or from Eurostat for some EU countries; they are not always available to non-researchers or to researchers outside a country, and access to national microdata sometimes incurs a fee. The financial hardship results and information on coverage policy included in the study are available from UHC watch (https://apps.who.int/dhis2/uhcwatch/).
Declaration of interests
All authors declare no competing interests.
Acknowledgements
The authors are grateful to the authors of WHO/Europe reports on financial protection and members of the European Financial Protection Network for their collaboration, and to the European Union (DG SANTE and DG NEAR) and the Government of the Autonomous Community of Catalonia, Spain for financial support. The authors alone are responsible for any mistakes.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanepe.2023.100826.
Appendix A. Supplementary data
References
- 1.World Health Organization . World Health Organization; Geneva: 2010. The world health report: health systems financing: the path to universal coverage.https://iris.who.int/handle/10665/44371 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization, World Bank . World Health Organization; 2017. Tracking universal health coverage: 2017 global monitoring report.https://iris.who.int/handle/10665/259817 Available from: [Google Scholar]
- 3.Thomson S., Cylus J., Evetovits T. WHO Regional Office for Europe; 2019. Can people afford to pay for health care? New evidence on financial protection in Europe.https://iris.who.int/handle/10665/311654 Available from: [Google Scholar]
- 4.Papanicolas I., Smith P.C. WHO Regional Office for Europe; Copenhagen: 2013. Health system performance comparison: an agenda for policy, information and research. (European Observatory on Health Systems and Policies series) [Google Scholar]
- 5.World Health Organization Regional Office for Europe . 2008. The Tallinn Charter: health systems for health and wealth.https://iris.who.int/handle/10665/349648 Available from: [Google Scholar]
- 6.United Nations . Department of Economic and Social Affairs; 2015. Transforming our world: the 2030 agenda for sustainable development.https://sdgs.un.org/2030agenda Available from: [Google Scholar]
- 7.World Health Organization Regional Office for Europe . 2021. European programme of work 2020-2025: united action for better health.https://iris.who.int/handle/10665/339209 Available from: [Google Scholar]
- 8.European Commission . 2023. European pillar of social rights - building a fairer and more inclusive European Union.https://ec.europa.eu/social/main.jsp? Available from: [Google Scholar]
- 9.Cylus J., Thomson S., Evetovits T. Catastrophic health spending in Europe: equity and policy implications of different calculation methods. Bull World Health Organ. 2018;96(9):599–609. doi: 10.2471/BLT.18.209031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yerramilli P., Fernández Ó., Thomson S. Financial protection in Europe: a systematic review of the literature and mapping of data availability. Health Policy. 2018;122(5):493–508. doi: 10.1016/j.healthpol.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization Regional Office for Europe UHC watch. 2023. https://apps.who.int/dhis2/uhcwatch/#/ Available from:
- 12.Wagstaff A., Flores G., Hsu J., et al. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Glob Health. 2018;6(2):e169–e179. doi: 10.1016/S2214-109X(17)30429-1. [DOI] [PubMed] [Google Scholar]
- 13.Organisation for Economic Co-operation and Development, Eurostat, World Health Organization A system of health accounts 2011. 2017. https://www.oecd-ilibrary.org/content/publication/9789264270985-en Available from:
- 14.European Statistical Office Eurostat. 2023. https://ec.europa.eu/eurostat/web/main/data/database [cited 2023 Nov 15]. Available from:
- 15.Spencer S., Hughes V. COMPAS - Migration research at the University of Oxford; 2015. Outside and in: legal entitlements to health care and education for migrants with irregular status in Europe - COMPAS.https://www.compas.ox.ac.uk/2015/outside-and-in/ [cited 2023 Nov 15]. Available from: [Google Scholar]
- 16.Schreyögg J., Stargardt T., Velasco-Garrido M., Busse R. Defining the “health benefit basket” in nine European countries. Eur J Health Econ. 2005;6(Suppl 1):2–10. doi: 10.1007/s10198-005-0312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tamblyn R., Laprise R., Hanley J.A., et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285(4):421–429. doi: 10.1001/jama.285.4.421. [DOI] [PubMed] [Google Scholar]
- 18.Goldman D.P., Joyce G.F., Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61–69. doi: 10.1001/jama.298.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swartz K. Cost-sharing: effects on spending and outcomes. Synth Proj Res Synth Rep. 2010;20 [PubMed] [Google Scholar]
- 20.Madden J.M., Bayapureddy S., Briesacher B.A., et al. Affordability of medical care among medicare enrollees. JAMA Health Forum. 2021;2(12) doi: 10.1001/jamahealthforum.2021.4104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guindon G.E., Fatima T., Garasia S., Khoee K. A systematic umbrella review of the association of prescription drug insurance and cost-sharing with drug use, health services use, and health. BMC Health Serv Res. 2022;22(1):297. doi: 10.1186/s12913-022-07554-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gross T., Layton T.J., Prinz D. The liquidity sensitivity of healthcare consumption: evidence from social security payments. Am Econ Rev Insights. 2022;4(2):175–190. doi: 10.1257/aeri.20200830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fusco N., Sils B., Graff J.S., Kistler K., Ruiz K. Cost-sharing and adherence, clinical outcomes, health care utilization, and costs: a systematic literature review. J Manag Care Spec Pharm. 2023;29(1):4–16. doi: 10.18553/jmcp.2022.21270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salampessy B.H., Alblas M.M., Portrait F.R.M., Koolman X., van der Hijden E.J.E. The effect of cost-sharing design characteristics on use of health care recommended by the treating physician; a discrete choice experiment. BMC Health Serv Res. 2018;18(1):797. doi: 10.1186/s12913-018-3598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mutual Information System on Social Protection . 2023. MISSOC database.https://www.missoc.org/missoc-database/ [cited 2023 Nov 15]. Available from: [Google Scholar]
- 26.European Observatory on Health Systems and Policies . 2023. Health Systems in Transition series (HiTs)https://eurohealthobservatory.who.int/publications/health-systems-reviews [cited 2023 Nov 15]. Available from: [Google Scholar]
- 27.Organisation for Economic Co-operation and Development . 2023. OECD statistics.https://stats.oecd.org/Index.aspx?ThemeTreeId=9 [cited 2023 Nov 15]. Available from: [Google Scholar]
- 28.Goginashvili K., Nadareishvili M., Habicht T. WHO Regional Office for Europe; 2021. Can people afford to pay for health care? New evidence on financial protection in Georgia.https://iris.who.int/handle/10665/342815 [cited 2023 Nov 15]. Available from: [Google Scholar]
- 29.Yazbeck A.S., Soucat A.L., Tandon A., et al. Addiction to a bad idea, especially in low- and middle-income countries: contributory health insurance. Soc Sci Med. 2023;320 doi: 10.1016/j.socscimed.2022.115168. [DOI] [PubMed] [Google Scholar]
- 30.Pagés C., Rigolini J., Robalino D.A. Institute for the Study of Labor; 2013. Social Insurance, Informality and Labor Markets: How to Protect Workers While Creating Good Jobs. IZA Discussion Paper No. 7879. [Google Scholar]
- 31.Connor P., Passel J.S. Pew Research Center’s Global Attitudes Project; 2019. Europe’s unauthorized immigrant population peaks in 2016, then levels off.https://www.pewresearch.org/global/2019/11/13/europes-unauthorized-immigrant-population-peaks-in-2016-then-levels-off/ [cited 2023 Nov 15]. Available from: [Google Scholar]
- 32.European Statistical Office . 2023. Migrant integration statistics - at risk of poverty and social exclusion.https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Migrant_integration_statistics_-_at_risk_of_poverty_and_social_exclusion [cited 2023 Nov 15]. Available from: [Google Scholar]
- 33.World Health Organization . World Health Organization; 2022. Measuring primary health care expenditure under SHA 2011: technical note, December 2021.https://iris.who.int/handle/10665/352307 [cited 2023 Nov 22]. Available from: [Google Scholar]
- 34.World Health Organization Regional Office for Europe . WHO Regional Office for Europe; 2022. Tracking primary health-care spending in selected countries. System of health accounts 2011 methodology.https://iris.who.int/handle/10665/364680 [cited 2023 Nov 22]. Available from: [Google Scholar]
- 35.Garam I.,, Zadnipru M., Doronin V., Matei A., Mosca I. WHO Regional Office for Europe; 2020. Can people afford to pay for health care? New evidence on financial protection in the Republic of Moldova.https://iris.who.int/handle/10665/331667 [cited 2023 Nov 15]. Available from: [Google Scholar]
- 36.World Health Organization Regional Office for Europe . WHO Regional Office for Europe; 2023. Can people afford to pay for health care? New evidence on financial protection in Ukraine 2023.https://iris.who.int/handle/10665/369097 [cited 2023 Nov 15]. Available from: [Google Scholar]
- 37.Winkelmann J., Gómez Rossi J., van Ginneken E. Oral health care in Europe: financing, access and provision. Health Syst Transit. 2022;24(2):1–176. [PubMed] [Google Scholar]
- 38.World Health Organization Regional Office for Europe . 2023. Automating and increasing protection from user charges for outpatient medicines: the estonian experience.https://www.who.int/europe/publications/m/item/automating-and-increasing-protection-from-user-charges-for-outpatient-medicines-the-estonian-experience [cited 2023 Nov 15]. Available from: [Google Scholar]
- 39.Gwatkin D.R., Ergo A. Universal health coverage: friend or foe of health equity? Lancet. 2011;377(9784):2160–2161. doi: 10.1016/S0140-6736(10)62058-2. [DOI] [PubMed] [Google Scholar]
- 40.Publications Office of the European Union . ShowVoc; 2023. ECOICOP.https://showvoc.op.europa.eu/#/datasets/ESTAT_European_Classification_of_Individual_Consumption_according_to_Purpose_%28ECOICOP%29/data?resId=http:%2F%2Fdata.europa.eu%2Fed1%2Fecoicop%2F061 [cited 2023 Nov 15]. Available from: [Google Scholar]
- 41.Nicaise I., Schockaert I., Bircan T. 2019. The uncounted poor in EU-SILC: a statistical profile of the income and living conditions of homeless people, undocumented immigrants and travellers in Belgium; pp. 73–96. [Google Scholar]
- 42.Gibson G., Grignon M., Hurley J., Wang L. Here comes the SUN: self-assessed unmet need, worsening health outcomes, and health care inequity. Health Econ. 2019;28(6):727–735. doi: 10.1002/hec.3877. [DOI] [PubMed] [Google Scholar]
- 43.Chaupain-Guillot S., Guillot O. Health system characteristics and unmet care needs in Europe: an analysis based on EU-SILC data. Eur J Health Econ. 2015;16(7):781–796. doi: 10.1007/s10198-014-0629-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.