Abstract
Chronic low-grade adipose tissue inflammation is associated with metabolic disorders. Inflammation results from the intertwined cross-talks of pro-inflammatory and anti-inflammatory pathways in the immune response of adipose tissue. In addition, adipose FABP4 levels and lipid droplet proteins are involved in systemic and tissue inflammation. Dysregulated adipocytes help infiltrate immune cells derived from bone marrow responsible for producing cytokines and chemokines. When adipose tissue expands in excess, adipocyte exhibits increased secretion of adipokines and is implicated in metabolic disturbances due to the release of free fatty acids. This review presents an emerging concept in adipose tissue fat metabolism, fatty acid handling and binding proteins, and lipid droplet proteins and their involvement in inflammatory disorders.
Keywords: Metabolic syndrome, Dietary fats, n-3 PUFA, LCPUFA, Obesity, Inflammation
Introduction
Adipose tissue contains multiple cell types, such as adipocytes, monocytes/macrophages, pericytes, endothelial cells, and stem cells. Adipose tissue is a loose connective dynamic tissue with many functions [1]. Adipose tissue stores triacylglycerol (TAGs) and regulates the secretion of free fatty acids (FFAs) to the plasma for their transport and metabolism in different tissues. Promoting lipolysis and releasing FFAs into the bloodstream also affects adipose tissue metabolism [2]. Adipose tissue fatty acid uptake involves several steps, including intestinal absorption, incorporation into chylomicron TAGs, and the subsequent release of FFAs by hydrolysis of TAGs by lipoprotein lipase (LPL) for adipocyte uptake. After being released from adipose tissue, FFAs are transported into circulation for delivery to various tissues.
Adipose tissue is increasingly considered an essential connector of cardiovascular disease (CVD), diabetes mellitus and insulin resistance, inflammation, and other obesity-related disorders. Adipose tissue regulates whole-body metabolism by altering the function of the liver, brain, heart, skeletal muscle, and vascular endothelium via the secretion of adipokines, resistin, leptin, fatty acid binding protein (FABP), and other factors. Adipose tissue has two types: brown adipose tissue (BAT) and white adipose tissue (WAT) [3]. WAT is distributed in several depots in the body, including subcutaneous, visceral, and other organs. Subcutaneous and visceral adipocytes are physiologically different from each other. WATs are less insulin sensitive, critical for energy storage, metabolically active, and have greater lipolytic activity [4].
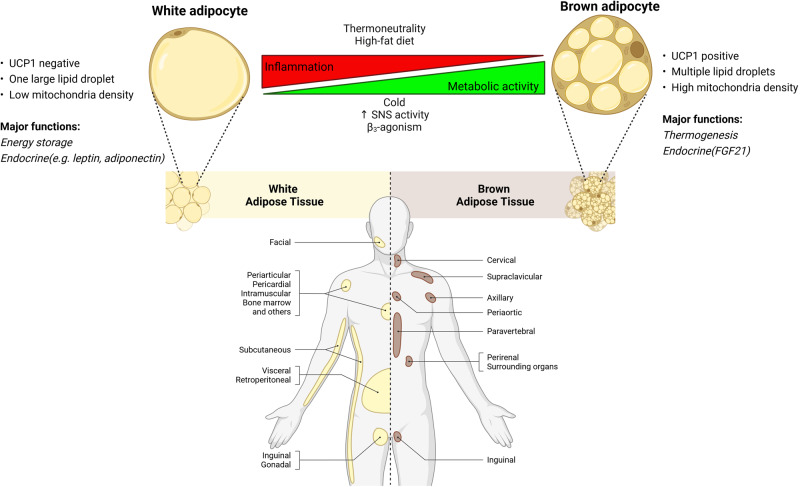
On the other hand, BAT produces thermogenesis from TAGs in humans and is present mainly in newborns. BAT was initially thought to maintain body temperature in human babies, but imaging studies confirmed metabolically active BAT in thoracic parts of adult humans [5]. BAT is involved in fat oxidation, thus maintaining the physiological function of adipose tissue in humans. Despite recent studies on the significance of BAT, its deposits do not appear to have a substantial impact on adult human metabolism [6]. Another adipose subtype, “beige,” is recently reported. Figure 1 describes the adipose tissue types, location, and browning process. Beige adipose contains brown and white adipocytes that develop within subcutaneous WAT. Activated beige adipose tissue can enhance body weight loss and inhibits obesity [7]. Thus, adipose is vital for metabolic homeostasis, whereas its dysfunction contributes to obesity and associated metabolic disease.
Fig. 1.
Adipose tissue types, location, and browning process. White adipocytes are large unilocular droplets enriched with a small number of small mitochondria, with a little UCP1 expression. In contrast, brown adipocytes are small multilocular with dense mitochondria with a high UCP1 expression. White adipose tissue is predominant in amount, supporting energy storage, and metabolically less active. On the other hand, brown adipose tissue is metabolically active, produces heat energy, promotes thermogenesis and browning (beige adipocytes) and reduces inflammation. White adipocytes can convert into brown adipocytes via cold stimulus, sympathetic nervous system (SNS) overdrive, and β3-agonism. UCP1, uncoupling protein 1
Obesity, metabolic syndrome, CVD, diabetes mellitus, and insulin resistance are public health challenges worldwide [8]. A crucial pathophysiological basis of obesity involves excess adiposity, associated with hypertrophy and hyperplasia due to the storage of excess fats [9]. Visceral adiposity is associated with a higher risk of obesity-related disorders such as insulin resistance, type 2 diabetes, CVD, and dyslipidemia [10] than peripheral adiposity, as per epidemiological observation. A relationship between inflammation and peripheral lipids is observed in the metabolic syndrome [11–13]. Dietary fats and their metabolism can affect inflammation by synthesizing various lipid mediators, immune response, and homeostasis [14, 15]. Adipose tissue can regulate inflammation by producing fatty acid-binding proteins, adipokines, resistin, leptin, and lipid droplet proteins [16, 17]. This review describes the roles of fatty acids and their binding proteins in adipose tissue and lipid droplets in modulating obesity-linked inflammatory diseases.
Fatty Acid Uptake and Metabolism in Adipose Tissue
The effect of fatty acids on adipose tissue metabolisms and consequently on vascular functionality, inflammatory response, blood pressure, and hemostasis are reviewed [18]. Adipose tissue is critically involved in the uptake, storage, and metabolism of fatty acids. Blood fatty acids can be taken up into adipose tissue, either stored as TAGs or oxidized to provide energy [19]. Insulin supports the uptake of fatty acids as well as glucose into the adipose tissue [20]. Besides insulin, growth hormones, glucocorticoids, and catecholamines can control the uptake and metabolism of fatty acids in this tissue [21]. After being stored in adipose, fatty acids are processed in one of two ways: lipogenesis or lipolysis. As opposed to lipolysis, which breaks down stored triglycerides into fatty acids to produce energy, lipogenesis is the process by which fatty acids are synthesized and stored in TAGs [22]. A complicated interaction of hormones and metabolic cues controls the ratio of lipogenesis to lipolysis [22]. Lipid droplets in adipose tissue comprise lipid esters produced by the adipocytes or from circulating lipids [23]. Adipocytes release FFAs into the bloodstream via lipolysis of lipids from lipid droplets involving several lipases such as adipose triglyceride lipase (ATGL), hormone-sensitive lipase (HSL), and monoglyceride lipase (MGL) [24]. Several natriuretic peptides, insulin, and catecholamines regulate the activity of HSL and ATGL. Basal lipolysis and insulin resistance correlate with high TAG levels [25].
Adipocytes regulate plasma lipid profile via the uptake of fatty acids from TAGs of circulating lipoprotein particles, such as chylomicrons and VLDLs [26]. Since adipocytes are a great source of LPL, dysfunction in the TAG/LPL axis can adversely affect plasma lipids-associated disorders [27]. After hydrolysis, FFAs are taken up by the adipocytes, and they are re-esterified in the TAGs [28]. Fatty acids can be differentially incorporated into chylomicrons or hydrolyzed from chylomicrons. For example, eicosapentaenoic acid,20:5n-3 (EPA) esters in chylomicrons, are relatively resistant to hydrolysis by LPL compared to other polyunsaturated fatty acids (8). Consequently, EPA may accumulate at the surface of chylomicron remnants as TAG or DAG and are not immediately available for tissue uptake.
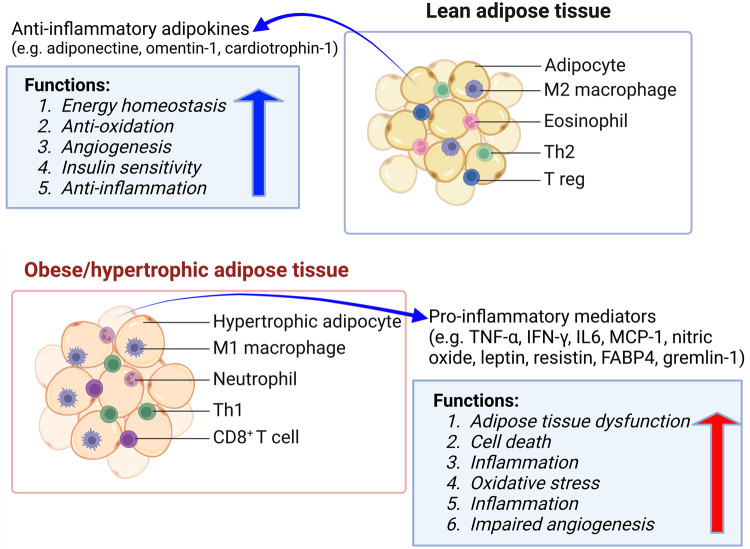
Adipose tissue can modulate other tissues’ insulin sensitivity and energy metabolism by secreting hormones and cytokines [29]. For example, adipose tissue can affect the hypothalamus to control hunger and energy by producing leptin [30]. Adiponectin, which improves insulin sensitivity and has anti-inflammatory properties, is also produced by adipose tissue [31]. Normally, adipose tissue stores lipids during the postprandial state, whereas it releases fatty acids to provide energy in an energy-demanding state. Metabolic disorders observed in obesity, insulin resistance, and type 2 diabetes can be attributed to dysregulated adipose tissue metabolism and hormone/adipokines secretion [18, 32]. Figure 2 describes the involvement of adipose tissue types in modulating inflammation.
Fig. 2.
Modulation of inflammation by adipose tissue types. White adipose tissue predominantly secretes adipokines from adipocytes in lean subjects, while pro-inflammatory cytokines are secreted from macrophages, neutrophils, and activated T-cells in adipose tissue in obese persons. Adipose tissue in lean supports angiogenesis, insulin sensitivity, and anti-inflammation, while adipose tissue dysfunction is reported in obese subjects. IFN interferon, IL interleukin, TNF tumor necrotic factor, FABP4 fatty acid binding protein4, Th1 type 1 T helper cells, MCP-1 monocyte chemoattractant protein-1
The adipocyte hypertrophy and increased basal lipolysis could result in adipose dysfunction in obesity-linked diseases [33]. Thus, understanding the factors that regulate adipose lipid droplets may reveal the mechanisms of obesity-associated risks in metabolic disorders.
The Transport of Fatty Acids: Roles of Adipose Tissue Proteins
Circulatory fatty acids are transported to adipose tissue as FFAs. Apart from simple diffusion, fatty acid transport into adipocytes is a protein-mediated process. Membrane transport and intracellular transport of FFAs are mediated via several membrane fatty acid binding/transport (FAT/CD36, FATPs, and FABPpm) and intracellular FABPs [34, 35]. These proteins are involved with both the cellular uptake and the intracellular transport of long-chain fatty acids (LCFAs) (c > 14) [36]. Intracellular transport of LCFAs requires the involvement of low molecular weight proteins (15 kDa) known as cytoplasmic fatty acid-binding proteins (FABPs) [37]. Fatty acid membrane transport and fatty acid-binding proteins greatly influence the uptake and metabolism of fatty acids in adipose tissue.
The presence of FABP in rat jejunum was first reported by Ockner et al. in 1972 [38]. Subsequently, several FABPs were detected in different tissues, such as the liver, myocardium, adipose tissue, placenta, brain, kidney, and prostate [34]. FABPs are named after the first tissue from which they are detected [39]. In mammals, nine different FABPs with a tissue‐specific distribution were identified. [40]. However, the contribution of different FABPs and their dysregulation to the progression of disorders associated with various diseases still needs to be fully understood [41, 42]. FABPs are thought to be involved in high-fat diet-mediated obesity, diabetes, dyslipidemia, atherosclerosis, and modulation of immune responses [43]. Therefore, targeting FABPs associated with metabolism, cell growth, and proliferation may offer therapeutic opportunities for various pathologies in metabolic diseases. FABPs are highlighted as potential therapeutic targets for various related disorders, including obesity, diabetes, and atherosclerosis.
Membrane protein transporters that facilitate adipose fatty acid uptake are fatty acid translocase (FAT/CD36), plasma membrane fatty acid-binding protein (FABPpm), and fatty acid transport protein (FATP4) [35, 37, 44, 45].
Adipose FABP or FABP4 is abundantly expressed in adipose tissue, and several elements, including FFAs, insulin and glucocorticoids, and others, control its expression [46]. Abnormal expression or dysfunction of these proteins is involved in several diseases, especially those concerning lipid metabolism. FAT/CD36 was identified as a critical LCFA transporter in the adipose tissue [47]. Expression of FABPpm is increased during the preadipocyte differentiation [34]. FATP4 affects adipose droplet size and pool size of other complex lipids. Once inside, FFAs are bound by FABP, thus stimulating fatty acid absorption and cytoplasmic transportation [37]. FABP4 is the most abundantly expressed in adipocytes though the relative content of FABP4 in different fat tissue depots in humans. FABP4 involves in the intracellular traffic of FFAs and their subsequent metabolism.
The FABP4 mRNA level is co-related with the insulin levels in obese individuals [48]. Expression of FABP4 in adipose tissue and macrophages is associated with inflammation [49]. However, no data is available on the expression of FABPs/FATPs/CD36/ FABPpm involved in the accretion of lipids in the visceral and subcutaneous adipose of morbidly obese. Although cellular trafficking of FABP in modulating various metabolic diseases have been proposed [50], limited data are available on the direct roles of FABP4 in adipose tissue inflammation in human. The FABP4’s presence in macrophages has been linked with the promotion of inflammation in adipocytes [51], and coronary atherosclerosis [52] in modulating CVD risks.
The adipose depot acts as a buffer for the high consumption of dietary fats. Therefore, fatty acid protein transporters’ expression and/or content would be enhanced to compensate for the increased availability of lipids. Aberrant circulatory FABP4 level is associated with insulin resistance [52], diabetes mellitus [53], gestational diabetes, and metabolic syndrome [54]. FABP4 is related to atherosclerosis and CVD prevalence [52, 55]. The amount of FABP4 mRNA is higher in the epicardial than in the subcutaneous adipose. FABP4 mRNA is associated with atherosclerosis status in patients who underwent coronary bypass surgery [55]. The FABP4 levels also correlate to the extent of left atrial adipose tissue volume in patients with atrial fibrillation. FABP4 is a marker of atrial fibrillation after ablation [56]. Expression of FABP4 and inflammation genes was inhibited by the sodium-glucose cotransporter 2 inhibitor [57], suggesting its possible relationship with hypertension and inflammation. FABP4 can synergistically increase fatty acid oxidation with leptin’s help during adipose inflammation. However, their effects on mitochondrial fatty acid oxidation remain unclear.
Metabolic syndrome with combined features of central obesity with insulin resistance, dyslipidemia, and hypertension increases the ĆVD risk [58]. The dietary fat types can affect insulin sensitivity via several lipid mediators mechanisms, changing cell membranes’ fatty acid composition and others [59]. Dietary fat rich in unsaturated fatty acids, such as the Mediterranean diet, may prevent the development of metabolic syndrome, diabetes, and CVD risk [60–63]. However, the detrimental effect of consuming saturated fat or the benefit of polyunsaturated fat in humans is controversial [64–68].
On the other hand, a saturated fat-containing diet promotes obesity, insulin resistance, and metabolic syndrome [64, 69, 70]. Furthermore, the roles of fatty acids and their metabolites in developing chronic, low-grade inflammatory states in metabolic syndrome are elucidated [71]. However, a recent meta-analysis showed that a pro-inflammatory diet was not associated with an increased risk of metabolic syndrome. Still, it was significantly associated with a 35% higher risk of CVD [72]. Furthermore, a high-fat diet containing saturated fat increases the incidence of CVD by raising total plasma cholesterol and LDL cholesterol. However, a meta-analysis did not find evidence to associate high-fat intakes with an increased risk of CVD [73].
FAT/CD36 is involved in LCFA transport across the plasma membrane in many tissues, including the adipose tissue [47, 74–78]. The mRNA and protein expression of membrane fatty acid uptake/binding proteins (FAT/CD36, FABPpm, FATP4) in the visceral and subcutaneous adipose and the LPL, PPARγ, FABP4, and FABP5 of obese patients were investigated. An increase was observed in the expression of FAT/CD36 in obese patients. The increased expression of the FAT/CD36 gene is at least partly due to the excessive lipid in adipose. Increased expression of FAT/CD36 at mRNA and plasma membranes protein levels) in visceral adipose in patients with morbid obesity. Bower et al. [79] demonstrated that the mRNA expression of FAT/CD36 in the visceral adipose of obese Afro-American and Caucasian women is higher than in Caucasian women. In addition to the observation in morbidly obese Caucasian subjects, an elevated plasma membrane FAT/CD36 and mRNA expression were also measured in the visceral adipose of lean individuals. However, the visceral adipose of obese subjects might have more potential for the uptake of LCFA, similar to other reports [79].
An increased expression of both PPARγ and LPL was observed in adipose tissue in obese individuals. PPARγ, the promoter of adipogenesis, acts as a transcription factor for the expression of FAT/CD36 [80]. Thus, increased LPL expression and FAT/CD36 in adipose increased the storage of TAGs in adipose. FABPpm mRNA expression was substantially lower in the subcutaneous and visceral adipose obese individuals compared to the non-obese subjects. Lappas et al. [81] also demonstrated a significant decrease in FABPpm mRNA expression in the subcutaneous adipose of obese people. However, the decrease in mRNA levels did not correlate with FABPpm protein levels. No change in FATP4 mRNA and protein expression in the subcutaneous and visceral adipose of the subjects with obesity compared to the lean control. Thus, FATP4 may not directly affect fatty acid uptake by adipocytes. This was also demonstrated in a mouse model with inactivated adipocyte fatp4 gene [82]. This study showed that the lack of FATP4 expression did not affect fatty acid uptake in these cells. Several studies demonstrated that FAT/CD36 is a major LCFA transporter for adipose fatty acid uptake, especially in the visceral adipose tissue [47].
Fatty Acid Storage in Adipose: Roles of Lipid Droplet Proteins
Lipid droplets are the organelles that store lipids in adipose tissue. The size and composition of lipid droplets depend on cellular metabolic status and environmental factors. Lipid droplets are predominantly composed of TAGs [83]. Fatty acids released from lipid droplets act as signaling molecules or precursors for bioactive lipids, including eicosanoids, retinoic acid, endocannabinoids, and ceramides [84]. Adipose tissue takes up fatty acids and stores them in lipid droplets via different fatty acid membranes and cellular transporters, and binding proteins. Emerging studies have revealed that lipid droplets protect cellular integrity and function via other mechanisms. For example, lipid droplet-mediated signaling affects mitochondrial function, the lipid metabolism [85], and the inflammation [84, 86]. Lipid droplets can consume excess lipids, protecting cells from lipotoxicity. Excessive lipid accumulation in lipid droplets can lead to obesity, diabetes, atherosclerosis, and fatty liver [87–89]. Similarly, a lack of lipids or lipid droplets in adipose tissues can lead to diseases such as lipodystrophy.
The dysregulation of lipid droplets can lead to disease states. Lipid droplets protect cell membranes and maintain cell homeostasis, modulate autophagy, provide signaling mediators, sequester toxic lipids and proteins, store energy, and preserve the redox balance [90, 91]. Lipid droplets carry out these functions in cooperation with other cellular organelles. However, the complex interplay between lipid droplets and other organelles is still unknown.
Several proteins are required for regulating lipid storage in lipids droplets. Lipid droplet structural proteins maintain lipid droplets’ function, structure, and morphology. Perilipin 1 (PLIN1) is the most abundant lipid droplet that protects lipid droplets from lipolysis. PLIN1, ADRP/ADFP/PLIN2, Tip47/PLIN3, S3-12/PLIN4, and OXPAT/PLIN5, the so-called “PAT” family proteins, are the main structural proteins are renamed as PLIN1-5 [92]. PLIN1 and PLIN2 are predominant subtypes localized in the lipid droplets [93]. PLIN1 regulates the accessibility of lipases to lipid droplets [94]. PLIN1 regulates lipid storage and lipolysis in response to the metabolic requirement of the adipose tissue. PLIN1 is phosphorylated by cAMP-dependent protein kinase A (PKA). The phosphorylated form of PLIN1 increases lipid storage or lipolysis depending on the metabolic status of the cell [94]. PLIN2 is predominantly present in the liver and muscle and involved in hepatic lipid accumulation [95], and improves insulin sensitivity in the skeletal muscle [96]. Like PLIN2, PLIN5 increases TAG storage and suppresses insulin resistance [96]. Additionally, COX-2 is found in inflamed lipid droplets, and the product of this enzyme carries essential inflammatory signals [97, 98]. Lipid droplets containing MAPKs, PKC, PI3K, and other critical enzymes are implicated in the intracellular signaling of diverse cellular responses [99, 100].
Adipose Tissue-derived Proteins and their Roles in Inflammation
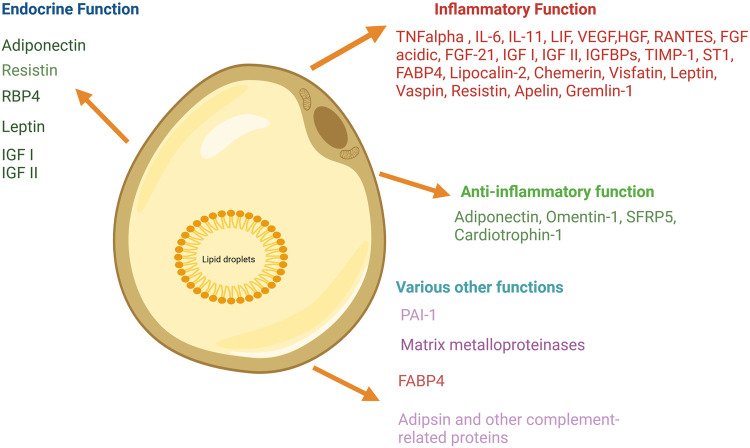
The adipose depot secretes various proteins such as cytokines, chemokines, and hormonal factors that regulate inflammation, immunity, adiposity, and lipid metabolism. Adipokines are released and synthesized by adipose tissue and are crucial for controlling inflammation and immune system function. More than 600 adipokines have been identified [101]. These adipokines and fatty acids maintain metabolic homeostasis through the adipose tissue cross-talk with other tissues [102]. The adipose tissue performs as an endocrine organ and secreted several proteins those potentially modulate inflammatory function in target tissues. The dysregulation of these proteins leads to several metabolic and inflammatory diseases. Figure 3 describes adipose tissue-secreted proteins and their inflammation modulatory functions.
Fig. 3.
Adipose tissue secreted proteins and their functions. Adipocyte primarily stores energy through triacylglycerols and secretes many proteins involved in endocrine and inflammation modulatory functions. RBP4: retinal binding protein 4, IGF: insulin growth factors, IL: interleukin, TNF tumor necrotic factor, LIF leukemia inhibitory factor, VEGF vascular endothelial growth factor, HGF hepatocyte growth factor, RANTES regulated on activation, normal T cell expressed and secreted, FGF fibroblast growth factor, IGFBP insulin growth factor binding protein, TIMP1 tissue inhibitor of metalloproteinases, FABP4 fatty acid binding protein 4
FFAs produced by adipose lipolysis can act as inflammatory mediators in immune cells. ATGL-mediated lipolysis regulates the synthesis of pro-inflammatory eicosanoids in mastocytes [103]. ATGL-mediated lipolysis increased lipid droplets but reduced the levels of eicosanoids in human-activated mastocytes. This suggests that lipolysis of TAGs produces arachidonic acid,20:4n-6, a precursor for eicosanoids [103]. Similarly, inhibition of ATGL caused a significant decrease of PGD2, LTE4, LTB2, and thromboxane B2 in murine neutrophils. Exudates from ATGL-deficient mice significantly inhibited eicosanoid synthesis, indicating that this is involved in inflammatory signaling processes [84]. Inhibition of HSL reduced lipolysis by the non-selective β-adrenergic agonist-mediated release of eicosanoids. Lean WAT has regulatory and immunosuppressive immune cells such as M2-like adipose macrophages, regulatory T cells, Th2 cells, iNKT cells, and eosinophils. The M2 adipose macrophages are uniformly distributed within the tissue and perform various physiological functions, inhibiting the proliferation of adipocyte progenitors and secreting anti-inflammatory cytokines such as IL-10, IL-4, IL-13, and IL-1Rα [104, 105].
Leptin is the product of the obese (ob) gene in mice and the lep gene in humans [106]. Leptin is produced by the subcutaneous WAT [107]. In addition to controlling energy balance, leptin is associated with the immune system and inflammation. The leptin receptors, such as long (ObRb) and short form (ObRa), are expressed by immune cells. The binding of leptin to ObRb stimulates the proliferation of clonal immune cells [108]. Leptin also affects both the innate and adaptive immune systems.
Monocytes and adipose macrophages express ObRa and ObRb, whereas dendritic cells express ObRb. Leptin stimulates the proliferation of monocytes and the expression of inflammatory cytokines such as TNFα and IL-6 [109]. It also expresses pro-inflammatory cytokines such as IL-1β, IL-6, and MCP-1 in the eosinophils [110]. Leptin also promotes neutrophil chemotaxis. The migration of neutrophils to the peritoneum in mice is also induced by leptin. These effects are mediated by inducing the production of TNFα and chemokines by monocytes and macrophages [111]. The surface expression of the adhesion molecules ICAM-1 and CD18 increases, while ICAM-3 and L-selectin are down-loaded in eosinophils by leptin.
Adiponectin, another well-reported adipokine, has anti-inflammatory and insulin-sensitizing properties. Adipocytes produce and secrete a protein called adiponectin, which has reportedly inhibited the synthesis of pro-inflammatory cytokines like TNFα and IL-6 [112]. Additionally, improving insulin sensitivity, adiponectin is thought to control lipid and glucose metabolism [113].
Resistin, visfatin, and omentin are other adipokines affecting individuals’ inflammation and modulation of immunity. Insulin resistance and metabolic diseases have been linked to resistin’s pro-inflammatory actions [114]. Conversely, visfatin reduces inflammation and improves insulin sensitivity [115]. Another adipokine with anti-inflammatory properties, omentin, regulates glucose metabolism [116].
Thus, several adipose tissue-derived proteins are directly or indirectly involved in modulating insulin sensitivity and inflammation in the target tissue by controlling lipid and glucose metabolism.
Fatty Acid-binding Protein 4 of Adipose Tissue and its Role in Inflammation
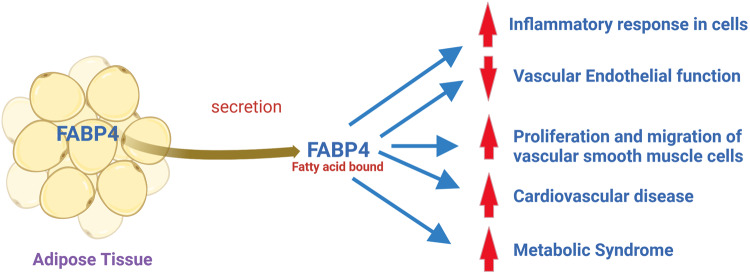
FABP4 activation has been linked to atherosclerosis, coronary artery disease, and heart failure due to its involvement in angiogenesis [117, 118]. It has been established that FABPs are dysregulated in the CVD [119, 120]. FABP4 plays a role in developing metabolic syndrome through various pathways involving adipocytes and macrophages [121]. The adipocytes [52] and macrophages [122] regulate the levels of FABP4 in circulation. Fatty acids, PPARγ agonists, insulin, lipopolysaccharide, and oxLDL regulate the levels of FABP4 in adipocytes and macrophages [123]. Reduced lipolysis was reported in FABP4-knockout mice [124], indicating that FABP4 regulates lipolysis.
Apolipoprotein-E-deficient mice with FABP4 deficiency did not develop atherosclerosis from a high-cholesterol diet [120]. However, the lack of FABP4 can modulate insulin resistance and lipid metabolism, but the mechanism is unknown. At the same time, the physiological role of FABP4 in circulation is unknown but can be used as a biomarker for metabolic syndrome and CVD [54]. FABP4 modulates inflammation by changing cholesterol concentration in macrophages. The cholesterol-lowering statin suppresses FABP4 expression in macrophages [125]. Increased cholesterol efflux was described in macrophages with elevated PPARγ isolated from FABP4-deficient mice. This indicates macrophage FABP4 plays a role in foam-cell formation via PPARγ–liver X receptor-α (LXRα)–ATP-binding cassette A1 (ABCA1) pathway. Reduced cytokine production and pro-inflammatory mediators, such as TNFα and COX2, were observed in macrophages isolated from FABP4-deficient mice [126]. Upregulation of FABP4 was not observed in adipocytes of FABP5-deficient mice due to a higher level of FABP4 [127].
In macrophages, the FABP4/FABP5 ratio is identical; no compensatory expression of FABP5 was observed in FABP4-knockout mice [128]. Various in vivo phenotypes on FABP5 expression are relevant to the metabolic syndrome. Overexpression of FABP5 in adipose tissue increased the lipolysis [129] and decreased insulin sensitivity [127]. On the other hand, increased insulin sensitivity in adipocytes from FABP5-deficient mice was reported [127]. The macrophage-loaded adipose tissues are responsible for inflammatory response, insulin resistance, and CVD in obesity [130]. FABP4 and FABP5 in adipocytes and macrophages contribute to inflammatory and metabolic disorders [51].
Adipocytes and macrophages were generally insulin-sensitive in FABP-deficient mice. Obese mice deficient in both FABP4 and FABP5 had reduced storage of fatty acids in adipose tissue and no insulin resistance [131]. ApoE-/- mice had less atherosclerosis and increased survival compared to wild-type and individual FABP-knockout counterparts [132]. The mice deficient in FABP4 and/or FABP5 also exhibited increased plasma FFA levels [133]. This indicates that the bioavailability of intracellular FFAs is more relevant to developing metabolic syndrome. Increased plasma level of FABP4 in diabetic patients with peripheral arterial disease was described [119]. The enhanced plasma level of FABP4 was independent of age, sex, or prior history of CVD. Therefore it raises the possibility of using FABP4 plasma levels as a biomarker for diagnosing coronary artery disease risk in diabetic patients. FABPs are increasingly reported in modulating the pathophysiology of CVD, especially in inflammation and metabolic imbalance. However, more studies are required to understand how FABPs contribute to CVD pathogenesis and discover possible therapeutic targets for preventing and treating CVD. Figure 4 describes the putative mechanism of the development of CVD by secreted FABP4 from adipose tissue.
Fig. 4.
Putative mechanism of the development of CVD by secreted FABP4 from adipose tissue. The secretion of FABP4 from adipocytes can activate endothelial cells, increase the proliferation/migration of vascular smooth muscle cells (VSMC), and induce pro-inflammatory responses in macrophages, vascular endothelial cells, and VSMC, leading to the development of atherosclerotic phenotype
Adipose Tissue Metabolism and Its Roles in Cardiovascular Disease
Adipose tissue is an important site of energy storage in the body and can be mobilized during energy demand through lipolysis. Lipolysis is regulated by a variety of angiogenic growth factors, including insulin, vascular endothelial growth factor (VEGF), and angiopoietin-like protein 4 (ANGPTL4)/ fasting-induced adipose factor (FIAF).
In adipose, insulin plays a crucial role in controlling lipolysis. Stimulating LPL, which converts TAGs into FFAs for storage, prevents lipolysis [134]. HSL, which converts TAGs into FFAs for use as fuel, is likewise inhibited by insulin [134]. Increased lipolysis and the release of excess FFAs can be caused by insulin resistance, a characteristic feature of obesity-associated type 2 diabetes. Insulin resistance can also promote inflammation and insulin resistance in sensitive target tissues, advancing the development of CVD [135]. Adipocytes produce VEGF, a growth factor that stimulates the development of angiogenesis. Obesity has been linked to higher VEGF levels and a higher risk of CVD [136].
Adipocytes produce the protein ANGPTL4, which is involved in controlling lipolysis. It blocks LPL, which decreases FFA absorption into adipose tissue and increases FFA release into the bloodstream [137]. Exercise and fasting raise ANGPTL4 levels, which have been linked to a lower risk of CVD [138]. ANGPTL4 regulates the catabolism of TAG-rich lipoproteins, thus controlling plasma levels of lipoproteins and the accretion of lipids in tissues. Though ANGPTL4 is relevant in whole-body lipid metabolism, the specific contribution of ANGPTL4 in regulating lipid metabolism in different tissues has yet to be discovered. In adipose tissue, the role of ANGPTL4 in ectopic lipid deposition [139], metabolism of lipids [140, 141], glucose homeostasis[137, 142], and vascular disease [143] are emerging.
Overall, the coordinated interplay of adipose lipolysis, insulin, VEGF, and ANGPTL4-mediated actions control the pathogenesis of developing CVD. Therefore, for optimal metabolic health and to lower the risk of CVD, adipose tissue must maintain a good balance between energy mobilization and storage.
Dietary Fats and Their Cross-talks with Adipose Tissue: Effects on Inflammation and Metabolic Disease
Overall, the type and amount of dietary fats consumed can significantly affect adipose tissue inflammation, immune function, and the expression of adipose-derived proteins. Consuming a diet rich in unsaturated fats and low in saturated and trans fats may help to reduce inflammation and improve metabolic health. In obesity, inflammation in adipose tissue is one of the factors responsible for insulin resistance. Immune cells of both innate and adaptive immune systems in adipose tissue regulate inflammation and insulin resistance. M2 macrophages, eosinophils, and Tregs maintain insulin sensitivity in lean adipose tissue by secreting Th2-type cytokines. In contrast, M1 macrophages, Th1 cells, CD8 T cells, and mast cells that secrete Th1-type cytokines dominate adipose tissue via pro-inflammatory responses and insulin resistance in obese individuals. Adipocytes are critical regulatory cells that control inflammation through cytokine secretion and antigen presentation activity.
Dietary lipids contain saturated fatty acids (SFA), monounsaturated acids (MUFA), polyunsaturated fatty acids (PUFAs), and trans fatty acids. Therefore, the diet’s quality and amounts of fatty acids play a crucial role in several features of the CVD [144, 145]. Dietary lipids affect adipose tissue homeostasis by controlling the expression of adipose-derived proteins involved in immune response and inflammation. Furthermore, dietary lipids modulate the fatty acid composition of plasma membrane phospholipids [146, 147]. Adipose tissue inflammation caused by saturated and trans fats is linked to the release of inflammatory cytokines in immune cells [148]. The emergence of metabolic disorders, including type 2 diabetes mellitus and obesity, is assumed to be due to this persistent low-grade inflammation [149].
In contrast, diets high in n-3 and low n-6 PUFAs, have anti-inflammatory effects in adipose tissue [150]. These fats have been demonstrated to alter the adiponectin receptor in adipose tissue, which is linked to improved insulin sensitivity and anti-inflammatory properties [150]. Substituting dietary SFAs with MUFAs positively affects CVD risk factors. This exchange of fatty acids lowers LDL-cholesterol levels [151], improves the postprandial plasma lipid profile [152], and lowers blood pressure [14]. N-3 and n-6 PUFAs and their metabolites have differential metabolic effects on fat utilization in the body. The pro-inflammatory roles of excess n-6 PUFAs in promoting adipose tissue inflammation have recently been reviewed extensively [153]. Therefore, increased dietary intake of sea foods rich in n-3 LCPUFAs could be beneficial in improving several features of CVD risk factors. Docosahexaenoic acid, 22:6 n-3 (DHA), and EPA decrease levels of TAGs, increase plasma HDL-cholesterol, and have less pro-inflammatory effects, thus can inhibit CVD and metabolic syndrome.
Fatty acids are associated with the pathogenesis and treatment of the metabolic syndrome. Fatty acids are involved in membrane structure and function, energy, signaling, and immunoregulation. In addition, depending on the double bonds and chain length, fatty acids regulate the pathogenetic mechanisms of glucose transport disturbance, insulin resistance, chronic inflammation, oxidative stress formation, and mitochondrial dysfunction in MetS. For example, replacing SFAs with MUFAs produces beneficial effects on MetS.
N-3 PUFAs decreased body fat in mice compared with a low-fat diet, and SFAs or n-6 PUFA (equivalent energy) in rats fed for seven weeks on a high-fat diet [154]. The anti-obesity effects of n-3 PUFAs are mediated by WAT re-esterification, resulting in energy expenditure [155] and changing the fetal thermogenic development of adipose in mice [156]. The n-3 PUFA level in plasma was inversely correlated with insulin resistance and glucose intolerance in 447 Norton Sound Inuits [157]. Fish oil consumption decreased 40% with reduced oxidation of carbohydrates, increased lipids, and non-oxidative glucose disposal in healthy humans [158]. Fish oil consumption for two months to insulin-resistant rats increased the plasma level of adiponectin and reduced insulin resistance and dyslipidemia [159]. Feeding mice with partially replaced vegetable fats with EPA and DHA increased plasma adiponectin levels [160]. EPA enhanced the release of adiponectin in obese and high-fat diet-induced obese mice and obese people [158]. n-3 PUFAs may benefit metabolic syndrome via decreasing plasma TAG levels and adiposity and increasing plasma adiponectin levels. The n-3 PUFA-derived resolvins, protectins, and maresins are known as specialized pro-resolving lipid mediators (SPMs), autacoids proposed to mediate immuno-resolving activity due to their anti-inflammatory roles in reducing adipose inflammation, and enhances insulin sensitivity in rodent [161]. The inflammatory resolution is involved by reducing neutrophil infiltration and proinflammatory mediators, activating macrophage-mediated clearance, and tissue remodeling [162]. However, clinical findings about SPM’s roles in adipose inflammation are scanty.
Conjugated linoleic acids (CLAs) improve obesity and cardiovascular functions in several animal studies [163]. The effects of CLA on lipid metabolism depend on its isomers [164]. The anti-diabetic effects of CLA are due to the 10t,12c-isomer [165, 166]. A CLA mixture and the 10t,12c-CLA isomer prevented obesity-induced hypertension [167–169]. Many animal studies have demonstrated the anti-obesity, anti-atherogenic, anti-diabetic, and hypotensive effects of CLAs [170]. However, the mechanism of CLAs and isomer-specific impact on CVD risk factors in the clinical set-up is yet to be proved. CLAs increase the β-oxidation of fatty acids in adipose tissues and suppress fatty acid synthesis in hepatocytes. In addition to these effects, CLAs regulate the synthesis of adipokines, such as adiponectin, leptin, and angiotensinogen [167–169]. Consuming a CLA mixture (1.8 g/day) for three months decreased a 4% in body fat compared with olive oil in healthy men and women [171]. Supplementing conjugated DHA reduced the fat deposition in the liver and epididymal adipose tissue and improved lipid and carbohydrate metabolism in rats [172]. The anti-obesity and lipid-lowering effects of conjugated EPA were also demonstrated [173].
Lipid Metabolism and Fatty Acid Binding Proteins are Involved in Inflammation-induced Endothelial Dysfunction
Adipose secretion of inflammatory IL-6, TNFα, and leptin contributes to endothelial dysfunction, platelet activation, hypercoagulability, and impaired fibrinolysis [174–177]. Plasma lipids interact with endothelial cells through specific cell membrane receptors or direct interchange with endothelial plasma membranes. LOX-1 (the receptor of oxLDL) is highly expressed when endothelial cells are incubated with oxLDL [90. Endothelial cells can recognize acetylated and oxLDL via surface receptors such as CD36/FAT and SR-B1 [178]. Lysophosphatidylcholine, an oxidative constituent of LDL, can reduce NO release from endothelial cells [179]. Other oxidative constituents of LDL, such as 13-hydroperoxyoctadecadienoate (13HPODE) and 7-ketocholesterol, and 7-β-hydroxycholesterol can affect the L-arginine-NO pathway in bovine aortic endothelial cells [179]. Endothelin-3 stimulated-NO release is suppressed by TAG-rich lipoproteins [180].
The endothelium is the source of some components essential for both thrombosis and fibrinolysis; definitive conclusions on the influences of lipids still need to be confirmed. Endothelial cells modulate coagulation and fibrinolysis processes. The effects of lipids on endothelium-dependent vasodilatation can be reversed by decreasing plasma lipids and providing L-arginine, the nitric oxide synthetase substrate, LDL and TAG-rich lipoproteins can stimulate the adhesion of leukocytes to the endothelial surface. Adipose tissue can control these processes via adipokines and lipid metabolism. Several cytokines, such as TNFα and IL-1, can induce adherence and penetration of the endothelium by leukocytes. The initial rolling represents an interaction between leukocytes and selectins, with subsequent adherence occurring through ICAM and VCAM. The expression of increased adhesion molecules for leukocyte adhesion was demonstrated in different conditions [181].
In contrast to elevated LDL’s pro-adhesive effects, HDL and apoA1 decrease the expression of adhesion molecules. P Selectin, stored in the Weibel-Palade bodies of endothelial cells, is expressed in the membranes of the atheromatous segments of human arteries. Hyperlipidemic and CVD patients show increased extracellular domains of adhesion molecules. Circulating ICAM and P selectin are increased in patients with CVD, and soluble ICAM, VCAM, and selectin in patients with hypertriglyceridemia [182].
Conclusions
Dysfunctional adipose tissue is characterized by adipocyte hypertrophy, dyslipidemia, metabolic syndrome, and inflammation. Adipose tissue releases several bioactive factors, adipokines, and FABP4, which are involved in glucose and lipid metabolism. In obesity, some adipokines are upregulated and affect homeostasis via their pro-inflammatory, pro-atherosclerotic, or pro-diabetic properties. At the same time, beneficial adipokines are down-regulated and thus fail to protect normal adipose biology. A complex interaction of fatty acid-handling proteins, hormones, and adipokines controls the aspects of lipogenesis and lipolysis in adipose tissues. In addition to lipid droplet proteins, FABP4, FABPpm, and FAT/CD36 regulate adipose physiology and pathology. FABP4 is a critical lipid mediator of inflammation. Plsama levels of FABP4 are associated with metabolic syndrome and CVD. Due to its implication in various diseases, FABP4 has become a promising target for developing small molecule inhibitors and neutralizing antibodies for disease treatment. The genetic variation of these proteins may also play a role in obesity, metabolic syndrome, and the response to dietary and pharmacological therapies.
Author contributions
A.K.D.R. conceived, performed the literature search, and wrote the manuscript. SB, RM, RD, AB, SP1, and SP2 contributed to writing the manuscript and critically revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital).
Compliance with ethical standards
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ye RZ, Richard G, Gevry N, Tchernof A, Carpentier AC. Fat cell size: measurement methods, pathophysiological origins, and relationships with metabolic dysregulations. Endocrine Reviews. 2022;43:35–60. doi: 10.1210/endrev/bnab018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park J, Kim M, Sun K, An YA, Gu X, Scherer PE. VEGF-A-expressing adipose tissue shows rapid beiging and enhanced survival after transplantation and confers IL-4-independent metabolic improvements. Diabetes. 2017;66:1479–1490. doi: 10.2337/db16-1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenwald M, Wolfrum C. The origin and definition of brite versus white and classical brown adipocytes. Adipocyte. 2014;3:4–9. doi: 10.4161/adip.26232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arner P. Differences in lipolysis between human subcutaneous and omental adipose tissues. Annals of Medicine. 1995;27:435–438. doi: 10.3109/07853899709002451. [DOI] [PubMed] [Google Scholar]
- 5.Zingaretti MC, Crosta F, Vitali A, Guerrieri M, Frontini A, Cannon B, Nedergaard J, Cinti S. The presence of UCP1 demonstrates that metabolically active adipose tissue in the neck of adult humans truly represents brown adipose tissue. The FASEB Journal. 2009;23:3113–3120. doi: 10.1096/fj.09-133546. [DOI] [PubMed] [Google Scholar]
- 6.Townsend K, Tseng YH. Brown adipose tissue: Recent insights into development, metabolic function and therapeutic potential. Adipocyte. 2012;1:13–24. doi: 10.4161/adip.18951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ikeda K, Maretich P, Kajimura S. The common and distinct features of brown and beige adipocytes. Trends in Endocrinology & Metabolism. 2018;29:191–200. doi: 10.1016/j.tem.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lebeck J. Metabolic impact of the glycerol channels AQP7 and AQP9 in adipose tissue and liver. Journal of Molecular Endocrinology. 2014;52:R165–R178. doi: 10.1530/JME-13-0268. [DOI] [PubMed] [Google Scholar]
- 9.Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–867. doi: 10.1038/nature05485. [DOI] [PubMed] [Google Scholar]
- 10.Cancello R, Tordjman J, Poitou C, Guilhem G, Bouillot JL, Hugol D, Coussieu C, Basdevant A, Bar Hen A, Bedossa P, et al. Increased infiltration of macrophages in omental adipose tissue is associated with marked hepatic lesions in morbid human obesity. Diabetes. 2006;55:1554–1561. doi: 10.2337/db06-0133. [DOI] [PubMed] [Google Scholar]
- 11.Reddy P, Lent-Schochet D, Ramakrishnan N, McLaughlin M, Jialal I. Metabolic syndrome is an inflammatory disorder: A conspiracy between adipose tissue and phagocytes. Clinica Chimica Acta. 2019;496:35–44. doi: 10.1016/j.cca.2019.06.019. [DOI] [PubMed] [Google Scholar]
- 12.Lambert, C., Cubedo, J., Padro, T. Sanchez-Hernandez, J. Antonijoan, R. M. Perez, A. Badimon, L. (2017). Phytosterols and Omega 3 Supplementation Exert Novel Regulatory Effects on Metabolic and Inflammatory Pathways: A Proteomic Study. Nutrients, 9 10.3390/nu9060599. [DOI] [PMC free article] [PubMed]
- 13.Gilroy DW, Bishop-Bailey D. Lipid mediators in immune regulation and resolution. British Journal of Pharmacology. 2019;176:1009–1023. doi: 10.1111/bph.14587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Serhan CN, Chiang N, Dalli J. New pro-resolving n-3 mediators bridge resolution of infectious inflammation to tissue regeneration. Molecular Aspects of Medicine. 2018;64:1–17. doi: 10.1016/j.mam.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aursnes M, Tungen JE, Vik A, Colas R, Cheng CY, Dalli J, Serhan CN, Hansen TV. Total synthesis of the lipid mediator PD1n-3 DPA: configurational assignments and anti-inflammatory and pro-resolving actions. Journal of Natural Products. 2014;77:910–916. doi: 10.1021/np4009865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu LE, Samocha-Bonet D, Whitworth PT, Fazakerley DJ, Turner N, Biden TJ, James DE, Cantley J. Identification of fatty acid binding protein 4 as an adipokine that regulates insulin secretion during obesity. Molecular Metabolism. 2014;3:465–473. doi: 10.1016/j.molmet.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konigorski S, Janke J, Drogan D, Bergmann MM, Hierholzer J, Kaaks R, Boeing H, Pischon T. Prediction of circulating adipokine levels based on body fat compartments and adipose tissue gene expression. Obesity Facts. 2019;12:590–605. doi: 10.1159/000502117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jung UJ, Choi MS. Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. International Journal of Molecular Sciences. 2014;15:6184–6223. doi: 10.3390/ijms15046184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmadian M, Duncan RE, Jaworski K, Sarkadi-Nagy E, Sul HS. Triacylglycerol metabolism in adipose tissue. Future Lipidology. 2007;2:229–237. doi: 10.2217/17460875.2.2.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cignarelli, A., Genchi, V. A., Perrini, S., Natalicchio, A., Laviola, L., Giorgino, F. (2019). Insulin and insulin receptors in adipose tissue development. International Journal of Molecular Sciences, 20 10.3390/ijms20030759. [DOI] [PMC free article] [PubMed]
- 21.Zhang, D.; Wei, Y., Huang, Q., Chen, Y., Zeng, K., Yang, W., Chen, J., Chen, J. (2022). Important hormones regulating lipid metabolism. Molecules, 27 10.3390/molecules27207052. [DOI] [PMC free article] [PubMed]
- 22.Saponaro C, Gaggini M, Carli F, Gastaldelli A. The subtle balance between lipolysis and lipogenesis: a critical point in metabolic homeostasis. Nutrients. 2015;7:9453–9474. doi: 10.3390/nu7115475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fujimoto, T., Parton, R. G. (2011). Not just fat: the structure and function of the lipid droplet. Cold Spring Harbor Perspectives in Biology, 3 10.1101/cshperspect.a004838. [DOI] [PMC free article] [PubMed]
- 24.Duncan RE, Ahmadian M, Jaworski K, Sarkadi-Nagy E, Sul HS. Regulation of lipolysis in adipocytes. Annual Review of Nutrition. 2007;27:79–101. doi: 10.1146/annurev.nutr.27.061406.093734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ryden M, Arner P. Subcutaneous adipocyte lipolysis contributes to circulating lipid levels. Arteriosclerosis, Thrombosis, and Vascular Biology. 2017;37:1782–1787. doi: 10.1161/ATVBAHA.117.309759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bickerton AS, Roberts R, Fielding BA, Hodson L, Blaak EE, Wagenmakers AJ, Gilbert M, Karpe F, Frayn KN. Preferential uptake of dietary Fatty acids in adipose tissue and muscle in the postprandial period. Diabetes. 2007;56:168–176. doi: 10.2337/db06-0822. [DOI] [PubMed] [Google Scholar]
- 27.Nielsen TS, Jessen N, Jorgensen JO, Moller N, Lund S. Dissecting adipose tissue lipolysis: molecular regulation and implications for metabolic disease. Journal of Molecular Endocrinology. 2014;52:R199–R222. doi: 10.1530/JME-13-0277. [DOI] [PubMed] [Google Scholar]
- 28.Young SG, Zechner R. Biochemistry and pathophysiology of intravascular and intracellular lipolysis. Genes & Development. 2013;27:459–484. doi: 10.1101/gad.209296.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith U, Kahn BB. Adipose tissue regulates insulin sensitivity: role of adipogenesis, de novo lipogenesis and novel lipids. Journal of Internal Medicine. 2016;280:465–475. doi: 10.1111/joim.12540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pico C, Palou M, Pomar CA, Rodriguez AM, Palou A. Leptin as a key regulator of the adipose organ. Reviews in Endocrine & Metabolic Disorders. 2022;23:13–30. doi: 10.1007/s11154-021-09687-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khoramipour, K., Chamari, K., Hekmatikar, A. A., Ziyaiyan, A., Taherkhani, S., Elguindy, N. M., Bragazzi, N. L. (2021). Adiponectin: structure, physiological functions, role in diseases, and effects of nutrition. Nutrients, 13 10.3390/nu13041180. [DOI] [PMC free article] [PubMed]
- 32.Hunter KA, Crosbie LC, Horgan GW, Miller GJ, Dutta-Roy AK. Effect of diets rich in oleic acid, stearic acid and linoleic acid on postprandial haemostatic factors in young healthy men. British Journal of Nutrition. 2001;86:207–215. [PubMed] [Google Scholar]
- 33.Choe SS, Huh JY, Hwang IJ, Kim JI, Kim JB. Adipose tissue remodeling: its role in energy metabolism and metabolic disorders. Frontiers in Endocrinology. 2016;7:30. doi: 10.3389/fendo.2016.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dutta-Roy AK. Cellular uptake of long-chain fatty acids: role of membrane-associated fatty-acid-binding/transport proteins. Cellular and Molecular Life Sciences. 2000;57:1360–1372. doi: 10.1007/pl00000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duttaroy AK. Fatty acid-activated nuclear transcription factors and their roles in human placenta. European Journal of Lipid Science and Technology. 2006;108:70–83. doi: 10.1002/ejlt.200500272. [DOI] [Google Scholar]
- 36.Duttaroy AK, Basak S. Maternal fatty acid metabolism in pregnancy and its consequences in the feto-placental development. Frontiers in Physiology. 2021;12:787848. doi: 10.3389/fphys.2021.787848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duttaroy AK. Transport of fatty acids across the human placenta: a review. Progress in Lipid Research. 2009;48:52–61. doi: 10.1016/j.plipres.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 38.Ockner RK, Manning JA, Poppenhausen RB, Ho WK. A binding protein for fatty acids in cytosol of intestinal mucosa, liver, myocardium, and other tissues. Science. 1972;177:56–58. doi: 10.1126/science.177.4043.56. [DOI] [PubMed] [Google Scholar]
- 39.Esteves A, Ehrlich R. Invertebrate intracellular fatty acid binding proteins. Comp Biochem Physiol C Toxicol Pharmacol. 2006;142:262–274. doi: 10.1016/j.cbpc.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 40.Chmurzynska A. The multigene family of fatty acid-binding proteins (FABPs): function, structure and polymorphism. Journal of Applied Genetics. 2006;47:39–48. doi: 10.1007/BF03194597. [DOI] [PubMed] [Google Scholar]
- 41.Leckie RL, Manuck SB, Bhattacharjee N, Muldoon MF, Flory JM, Erickson KI. Omega-3 fatty acids moderate effects of physical activity on cognitive function. Neuropsychologia. 2014;59:103–111. doi: 10.1016/j.neuropsychologia.2014.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hardman WE. (n-3) fatty acids and cancer therapy. Journal of Nutrition. 2004;134:3427S–3430S. doi: 10.1093/jn/134.12.3427S. [DOI] [PubMed] [Google Scholar]
- 43.Mallick, R., Basak, S., Duttaroy, A. K. (2021). Fatty acids and evolving roles of their proteins in neurological, cardiovascular disorders and cancers. Progress in Lipid Research 10.1016/j.plipres.2021.101116. [DOI] [PubMed]
- 44.Zhou D, Samovski D, Okunade AL, Stahl PD, Abumrad NA, Su X. CD36 level and trafficking are determinants of lipolysis in adipocytes. The FASEB Journal. 2012;26:4733–4742. doi: 10.1096/fj.12-206862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DuttaRoy AK. Fatty acid transport and metabolism in the feto-placental unit and the role of fatty acid-binding proteins. Journal of Nutritional Biochemistry. 1997;8:548–557. doi: 10.1016/s0955-2863(97)00087-9. [DOI] [Google Scholar]
- 46.Newell-Fugate AE. The role of sex steroids in white adipose tissue adipocyte function. Reproduction. 2017;153:R133–R149. doi: 10.1530/REP-16-0417. [DOI] [PubMed] [Google Scholar]
- 47.Coburn CT, Knapp FF, Febbraio M, Beets AL, Silverstein RL, Abumrad NA. Defective uptake and utilization of long chain fatty acids in muscle and adipose tissues of CD36 knockout mice. Journal of Biological Chemistry. 2000;275:32523–32529. doi: 10.1074/jbc.M003826200. [DOI] [PubMed] [Google Scholar]
- 48.Fisher RM, Thorne A, Hamsten A, Arner P. Fatty acid binding protein expression in different human adipose tissue depots in relation to rates of lipolysis and insulin concentration in obese individuals. Molecular and Cellular Biochemistry. 2002;239:95–100. doi: 10.1023/A:1020532823751. [DOI] [PubMed] [Google Scholar]
- 49.Rodríguez-Calvo R, Girona J, Alegret JM, Bosquet A, Ibarretxe D, Masana L. Role of the fatty acid-binding protein 4 in heart failure and cardiovascular disease. Journal of Endocrinology. 2017;233:R173–r184. doi: 10.1530/joe-17-0031. [DOI] [PubMed] [Google Scholar]
- 50.Basak, S., Mallick, R., Banerjee, A., Pathak, S., Duttaroy, A. K. (2022). Cytoplasmic fatty acid-binding proteins in metabolic diseases and cancers. In Advances in Protein Chemistry and Structural Biology, Academic Press: 132, 143−174. [DOI] [PubMed]
- 51.Furuhashi M, Fucho R, Gorgun CZ, Tuncman G, Cao H, Hotamisligil GS. Adipocyte/macrophage fatty acid-binding proteins contribute to metabolic deterioration through actions in both macrophages and adipocytes in mice. Journal of Clinical Investigation. 2008;118:2640–2650. doi: 10.1172/JCI34750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Furuhashi M, Saitoh S, Shimamoto K, Miura T. Fatty Acid-Binding Protein 4 (FABP4): Pathophysiological Insights and Potent Clinical Biomarker of Metabolic and Cardiovascular Diseases. Clinical Medicine Insights. Cardiology. 2014;8:23–33. doi: 10.4137/CMC.S17067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tso AW, Xu A, Sham PC, Wat NM, Wang Y, Fong CH, Cheung BM, Janus ED, Lam KS. Serum adipocyte fatty acid binding protein as a new biomarker predicting the development of type 2 diabetes: a 10-year prospective study in a Chinese cohort. Diabetes Care. 2007;30:2667–2672. doi: 10.2337/dc07-0413. [DOI] [PubMed] [Google Scholar]
- 54.Xu A, Wang Y, Xu JY, Stejskal D, Tam S, Zhang J, Wat NM, Wong WK, Lam KS. Adipocyte fatty acid-binding protein is a plasma biomarker closely associated with obesity and metabolic syndrome. Clinical Chemistry. 2006;52:405–413. doi: 10.1373/clinchem.2005.062463. [DOI] [PubMed] [Google Scholar]
- 55.Gormez S, Erdim R, Akan G, Caynak B, Duran C, Gunay D, Sozer V, Atalar F. Relationships between visceral/subcutaneous adipose tissue FABP4 expression and coronary atherosclerosis in patients with metabolic syndrome. Cardiovascular Pathology. 2020;46:107192. doi: 10.1016/j.carpath.2019.107192. [DOI] [PubMed] [Google Scholar]
- 56.Lopez-Canoa JN, Baluja A, Couselo-Seijas M, Naveira AB, Gonzalez-Melchor L, Rozados A, Martinez-Sande L, Garcia-Seara J, Fernandez-Lopez XA, Fernandez AL, et al. Plasma FABP4 levels are associated with left atrial fat volume in persistent atrial fibrillation and predict recurrence after catheter ablation. International Journal of Cardiology. 2019;292:131–135. doi: 10.1016/j.ijcard.2019.04.031. [DOI] [PubMed] [Google Scholar]
- 57.Mori K, Tsuchiya K, Nakamura S, Miyachi Y, Shiba K, Ogawa Y, Kitamura K. Ipragliflozin-induced adipose expansion inhibits cuff-induced vascular remodeling in mice. Cardiovasc Diabetol. 2019;18:83. doi: 10.1186/s12933-019-0886-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–2716. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 59.Storlien LH, Baur LA, Kriketos AD, Pan DA, Cooney GJ, Jenkins AB, Calvert GD, Campbell LV. Dietary fats and insulin action. Diabetologia. 1996;39:621–631. doi: 10.1007/BF00418533. [DOI] [PubMed] [Google Scholar]
- 60.Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. The New England Journal of Medicine. 2018;378:e34. doi: 10.1056/NEJMoa1800389. [DOI] [PubMed] [Google Scholar]
- 61.Godos J, Zappala G, Bernardini S, Giambini I, Bes-Rastrollo M, Martinez-Gonzalez M. Adherence to the Mediterranean diet is inversely associated with metabolic syndrome occurrence: a meta-analysis of observational studies. International Journal of Food Sciences and Nutrition. 2017;68:138–148. doi: 10.1080/09637486.2016.1221900. [DOI] [PubMed] [Google Scholar]
- 62.Salas-Salvado, Diaz-Lopez J, Ruiz-Canela A, M, Basora, Fito J, M, Corella D, Serra-Majem L, Warnberg J, Romaguera D, Estruch R, et al. Effect of a Lifestyle Intervention Program With Energy-Restricted Mediterranean Diet and Exercise on Weight Loss and Cardiovascular Risk Factors: One-Year Results of the PREDIMED-Plus Trial. Diabetes Care. 2019;42:777–788. doi: 10.2337/dc18-0836. [DOI] [PubMed] [Google Scholar]
- 63.Salas-Salvado J, Bullo M, Babio N, Martinez-Gonzalez MA, Ibarrola-Jurado N, Basora J, Estruch R, Covas MI, Corella D, Aros F, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care. 2011;34:14–19. doi: 10.2337/dc10-1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Feskens EJ, Virtanen SM, Rasanen L, Tuomilehto J, Stengard J, Pekkanen J, Nissinen A, Kromhout D. Dietary factors determining diabetes and impaired glucose tolerance. A 20-year follow-up of the Finnish and Dutch cohorts of the Seven Countries Study. Diabetes Care. 1995;18:1104–1112. doi: 10.2337/diacare.18.8.1104. [DOI] [PubMed] [Google Scholar]
- 65.Marshall JA, Bessesen DH, Hamman RF. High saturated fat and low starch and fibre are associated with hyperinsulinaemia in a non-diabetic population: the San Luis Valley Diabetes Study. Diabetologia. 1997;40:430–438. doi: 10.1007/s001250050697. [DOI] [PubMed] [Google Scholar]
- 66.Trevisan M, Krogh V, Freudenheim J, Blake A, Muti P, Panico S, Farinaro E, Mancini M, Menotti A, Ricci G. Consumption of olive oil, butter, and vegetable oils and coronary heart disease risk factors. The Research Group ATS-RF2 of the Italian National Research Council. JAMA. 1990;263:688–692. doi: 10.1001/jama.1990.03440050082038. [DOI] [PubMed] [Google Scholar]
- 67.Mayer-Davis EJ, Monaco JH, Hoen HM, Carmichael S, Vitolins MZ, Rewers MJ, Haffner SM, Ayad MF, Bergman RN, Karter AJ. Dietary fat and insulin sensitivity in a triethnic population: the role of obesity. The Insulin Resistance Atherosclerosis Study (IRAS) The American Journal of Clinical Nutrition. 1997;65:79–87. doi: 10.1093/ajcn/65.1.79. [DOI] [PubMed] [Google Scholar]
- 68.McKeown NM, Meigs JB, Liu S, Saltzman E, Wilson PW, Jacques PF. Carbohydrate nutrition, insulin resistance, and the prevalence of the metabolic syndrome in the Framingham Offspring Cohort. Diabetes Care. 2004;27:538–546. doi: 10.2337/diacare.27.2.538. [DOI] [PubMed] [Google Scholar]
- 69.Vessby B. Dietary fat and insulin action in humans. British Journal of Nutrition. 2000;83:S91–S96. doi: 10.1017/s000711450000101x. [DOI] [PubMed] [Google Scholar]
- 70.Melanson EL, Astrup A, Donahoo WT. The relationship between dietary fat and fatty acid intake and body weight, diabetes, and the metabolic syndrome. Annals of Nutrition and Metabolism. 2009;55:229–243. doi: 10.1159/000229004. [DOI] [PubMed] [Google Scholar]
- 71.Denisenko YK, Kytikova OY, Novgorodtseva TP, Antonyuk MV, Gvozdenko TA, Kantur TA. Lipid-Induced Mechanisms of Metabolic Syndrome. Journal of Obesity. 2020;2020:5762395. doi: 10.1155/2020/5762395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Namazi N, Larijani B, Azadbakht L. Dietary Inflammatory Index and its Association with the Risk of Cardiovascular Diseases, Metabolic Syndrome, and Mortality: A Systematic Review and Meta-Analysis. Hormone and Metabolic Research. 2018;50:345–358. doi: 10.1055/a-0596-8204. [DOI] [PubMed] [Google Scholar]
- 73.Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. American Journal of Physiology-Endocrinology and Metabolism. 2010;91:535–546. doi: 10.3945/ajcn.2009.27725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bonen A, Parolin ML, Steinberg GR, Calles-Escandon J, Tandon NN, Glatz JF, Luiken JJ, Heigenhauser GJ, Dyck DJ. Triacylglycerol accumulation in human obesity and type 2 diabetes is associated with increased rates of skeletal muscle fatty acid transport and increased sarcolemmal FAT/CD36. The FASEB Journal. 2004;18:1144–1146. doi: 10.1096/fj.03-1065fje. [DOI] [PubMed] [Google Scholar]
- 75.Luiken JJ, Arumugam Y, Dyck DJ, Bell RC, Pelsers MM, Turcotte LP, Tandon NN, Glatz JF, Bonen A. Increased rates of fatty acid uptake and plasmalemmal fatty acid transporters in obese Zucker rats. Journal of Biological Chemistry. 2001;276:40567–40573. doi: 10.1074/jbc.M100052200. [DOI] [PubMed] [Google Scholar]
- 76.Luiken JJ, Arumugam Y, Bell RC, Calles-Escandon J, Tandon NN, Glatz JF, Bonen A. Changes in fatty acid transport and transporters are related to the severity of insulin deficiency. American Journal of Physiology-Endocrinology and Metabolism. 2002;283:E612–E621. doi: 10.1152/ajpendo.00011.2002. [DOI] [PubMed] [Google Scholar]
- 77.Steinberg GR, Dyck DJ, Calles-Escandon J, Tandon NN, Luiken JJ, Glatz JF, Bonen A. Chronic leptin administration decreases fatty acid uptake and fatty acid transporters in rat skeletal muscle. Journal of Biological Chemistry. 2002;277:8854–8860. doi: 10.1074/jbc.M107683200. [DOI] [PubMed] [Google Scholar]
- 78.Febbraio M, Abumrad NA, Hajjar DP, Sharma K, Cheng W, Pearce SF, Silverstein RL. A null mutation in murine CD36 reveals an important role in fatty acid and lipoprotein metabolism. Journal of Biological Chemistry. 1999;274:19055–19062. doi: 10.1074/jbc.274.27.19055. [DOI] [PubMed] [Google Scholar]
- 79.Bower JF, Davis JM, Hao E, Barakat HA. Differences in transport of fatty acids and expression of fatty acid transporting proteins in adipose tissue of obese black and white women. American Journal of Physiology-Endocrinology and Metabolism. 2006;290:E87–E91. doi: 10.1152/ajpendo.00194.2005. [DOI] [PubMed] [Google Scholar]
- 80.Tontonoz P, Spiegelman BM. Fat and beyond: the diverse biology of PPARgamma. Annual Review of Biochemistry. 2008;77:289–312. doi: 10.1146/annurev.biochem.77.061307.091829. [DOI] [PubMed] [Google Scholar]
- 81.Lappas M. Effect of pre-existing maternal obesity, gestational diabetes and adipokines on the expression of genes involved in lipid metabolism in adipose tissue. Metabolism. 2014;63:250–262. doi: 10.1016/j.metabol.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 82.Lenz LS, Marx J, Chamulitrat W, Kaiser I, Grone HJ, Liebisch G, Schmitz G, Elsing C, Straub BK, Fullekrug J, et al. Adipocyte-specific inactivation of Acyl-CoA synthetase fatty acid transport protein 4 (Fatp4) in mice causes adipose hypertrophy and alterations in metabolism of complex lipids under high fat diet. Journal of Biological Chemistry. 2011;286:35578–35587. doi: 10.1074/jbc.M111.226530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kraemer FB, Khor VK, Shen WJ, Azhar S. Cholesterol ester droplets and steroidogenesis. Molecular and Cellular Endocrinology. 2013;371:15–19. doi: 10.1016/j.mce.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schlager S, Goeritzer M, Jandl K, Frei R, Vujic N, Kolb D, Strohmaier H, Dorow J, Eichmann TO, Rosenberger A, et al. Adipose triglyceride lipase acts on neutrophil lipid droplets to regulate substrate availability for lipid mediator synthesis. Journal of Leukocyte Biology. 2015;98:837–850. doi: 10.1189/jlb.3A0515-206R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Haemmerle G, Moustafa T, Woelkart G, Buttner S, Schmidt A, van de Weijer T, Hesselink M, Jaeger D, Kienesberger PC, Zierler K, et al. ATGL-mediated fat catabolism regulates cardiac mitochondrial function via PPAR-alpha and PGC-1. Nature Medicine. 2011;17:1076–1085. doi: 10.1038/nm.2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Umamaheswaran S, Dasari SK, Yang P, Lutgendorf SK, Sood AK. Stress, inflammation, and eicosanoids: an emerging perspective. Cancer and Metastasis Reviews. 2018;37:203–211. doi: 10.1007/s10555-018-9741-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zimmermann R, Strauss JG, Haemmerle G, Schoiswohl G, Birner-Gruenberger R, Riederer M, Lass A, Neuberger G, Eisenhaber F, Hermetter A, et al. Fat mobilization in adipose tissue is promoted by adipose triglyceride lipase. Science. 2004;306:1383–1386. doi: 10.1126/science.1100747. [DOI] [PubMed] [Google Scholar]
- 88.Boren J, Taskinen MR, Olofsson SO, Levin M. Ectopic lipid storage and insulin resistance: a harmful relationship. Journal of Internal Medicine. 2013;274:25–40. doi: 10.1111/joim.12071. [DOI] [PubMed] [Google Scholar]
- 89.McManaman JL, Bales ES, Orlicky DJ, Jackman M, MacLean PS, Cain S, Crunk AE, Mansur A, Graham CE, Bowman TA, et al. Perilipin-2-null mice are protected against diet-induced obesity, adipose inflammation, and fatty liver disease. J Lipid Res. 2013;54:1346–1359. doi: 10.1194/jlr.M035063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Welte MA, Gould AP. Lipid droplet functions beyond energy storage. Biochim Biophys Acta Mol Cell Biol Lipids. 2017;1862:1260–1272. doi: 10.1016/j.bbalip.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Olzmann JA, Carvalho P. Dynamics and functions of lipid droplets. Nature Reviews Molecular Cell Biology. 2019;20:137–155. doi: 10.1038/s41580-018-0085-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Xu S, Zhang X, Liu P. Lipid droplet proteins and metabolic diseases. Biochimica et Biophysica Acta: Molecular Basis of Disease. 2018;1864:1968–1983. doi: 10.1016/j.bbadis.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 93.Londos C, Sztalryd C, Tansey JT, Kimmel AR. Role of PAT proteins in lipid metabolism. Biochimie. 2005;87:45–49. doi: 10.1016/j.biochi.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 94.Yamaguchi T, Omatsu N, Matsushita S, Osumi T. CGI-58 interacts with perilipin and is localized to lipid droplets. Possible involvement of CGI-58 mislocalization in Chanarin-Dorfman syndrome. Journal of Biological Chemistry. 2004;279:30490–30497. doi: 10.1074/jbc.M403920200. [DOI] [PubMed] [Google Scholar]
- 95.Crunk AE, Monks J, Murakami A, Jackman M, Maclean PS, Ladinsky M, Bales ES, Cain S, Orlicky DJ, McManaman JL. Dynamic regulation of hepatic lipid droplet properties by diet. PloS one. 2013;8:e67631. doi: 10.1371/journal.pone.0067631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bosma M, Hesselink MK, Sparks LM, Timmers S, Ferraz MJ, Mattijssen F, van Beurden D, Schaart G, de Baets MH, Verheyen FK, et al. Perilipin 2 improves insulin sensitivity in skeletal muscle despite elevated intramuscular lipid levels. Diabetes. 2012;61:2679–2690. doi: 10.2337/db11-1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Accioly MT, Pacheco P, Maya-Monteiro CM, Carrossini N, Robbs BK, Oliveira SS, Kaufmann C, Morgado-Diaz JA, Bozza PT, Viola JP. Lipid bodies are reservoirs of cyclooxygenase-2 and sites of prostaglandin-E2 synthesis in colon cancer cells. Cancer Research. 2008;68:1732–1740. doi: 10.1158/0008-5472.CAN-07-1999. [DOI] [PubMed] [Google Scholar]
- 98.Chen X, Xu S, Wei S, Deng Y, Li Y, Yang F, Liu P. Comparative Proteomic Study of Fatty Acid-treated Myoblasts Reveals Role of Cox-2 in Palmitate-induced Insulin Resistance. Scientific Reports. 2016;6:21454. doi: 10.1038/srep21454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yu W, Bozza PT, Tzizik DM, Gray JP, Cassara J, Dvorak AM, Weller PF. Co-compartmentalization of MAP kinases and cytosolic phospholipase A2 at cytoplasmic arachidonate-rich lipid bodies. The American Journal of Pathology. 1998;152:759–769. [PMC free article] [PubMed] [Google Scholar]
- 100.Yu W, Cassara J, Weller PF. Phosphatidylinositide 3-kinase localizes to cytoplasmic lipid bodies in human polymorphonuclear leukocytes and other myeloid-derived cells. Blood. 2000;95:1078–1085. doi: 10.1182/blood.V95.3.1078.003k16_1078_1085. [DOI] [PubMed] [Google Scholar]
- 101.Lehr S, Hartwig S, Sell H. Adipokines: a treasure trove for the discovery of biomarkers for metabolic disorders. Proteomics Clinical Applications. 2012;6:91–101. doi: 10.1002/prca.201100052. [DOI] [PubMed] [Google Scholar]
- 102.Stern JH, Rutkowski JM, Scherer PE. Adiponectin, Leptin, and Fatty Acids in the Maintenance of Metabolic Homeostasis through Adipose Tissue Crosstalk. Cell Metabolism. 2016;23:770–784. doi: 10.1016/j.cmet.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dichlberger A, Schlager S, Maaninka K, Schneider WJ, Kovanen PT. Adipose triglyceride lipase regulates eicosanoid production in activated human mast cells. Journal of Lipid Research. 2014;55:2471–2478. doi: 10.1194/jlr.M048553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nawaz A, Aminuddin A, Kado T, Takikawa A, Yamamoto S, Tsuneyama K, Igarashi Y, Ikutani M, Nishida Y, Nagai Y, et al. CD206(+) M2-like macrophages regulate systemic glucose metabolism by inhibiting proliferation of adipocyte progenitors. Nature Communications. 2017;8:286. doi: 10.1038/s41467-017-00231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. Journal of Clinical Investigation. 2007;117:175–184. doi: 10.1172/JCI29881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]
- 107.Wang J, Liu R, Hawkins M, Barzilai N, Rossetti L. A nutrient-sensing pathway regulates leptin gene expression in muscle and fat. Nature. 1998;393:684–688. doi: 10.1038/31474. [DOI] [PubMed] [Google Scholar]
- 108.Gainsford T, Willson TA, Metcalf D, Handman E, McFarlane C, Ng A, Nicola NA, Alexander WS, Hilton DJ. Leptin can induce proliferation, differentiation, and functional activation of hemopoietic cells. Proceedings of the National Academy of Sciences of the United States of America. 1996;93:14564–14568. doi: 10.1073/pnas.93.25.14564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Santos-Alvarez J, Goberna R, Sanchez-Margalet V. Human leptin stimulates proliferation and activation of human circulating monocytes. Cellular & Molecular Immunology. 1999;194:6–11. doi: 10.1006/cimm.1999.1490. [DOI] [PubMed] [Google Scholar]
- 110.Wong CK, Cheung PF, Lam CW. Leptin-mediated cytokine release and migration of eosinophils: implications for immunopathophysiology of allergic inflammation. European Journal of Immunology. 2007;37:2337–2348. doi: 10.1002/eji.200636866. [DOI] [PubMed] [Google Scholar]
- 111.Souza-Almeida G, D’Avila H, Almeida PE, Luna-Gomes T, Liechocki S, Walzog B, Hepper I, Castro-Faria-Neto HC, Bozza PT, Bandeira-Melo C, et al. Leptin Mediates In Vivo Neutrophil Migration: Involvement of Tumor Necrosis Factor-Alpha and CXCL1. Frontiers in Immunology. 2018;9:111. doi: 10.3389/fimmu.2018.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ouchi N, Walsh K. Adiponectin as an anti-inflammatory factor. Clinica Chimica Acta. 2007;380:24–30. doi: 10.1016/j.cca.2007.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yanai, H., Yoshida, H. (2019). Beneficial Effects of Adiponectin on Glucose and Lipid Metabolism and Atherosclerotic Progression: Mechanisms and Perspectives. International Journal of Molecular Sciences, 2010.3390/ijms20051190. [DOI] [PMC free article] [PubMed]
- 114.Jamaluddin MS, Weakley SM, Yao Q, Chen C. Resistin: functional roles and therapeutic considerations for cardiovascular disease. British Journal of Pharmacology. 2012;165:622–632. doi: 10.1111/j.1476-5381.2011.01369.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Heo YJ, Choi SE, Jeon JY, Han SJ, Kim DJ, Kang Y, Lee KW, Kim HJ. Visfatin Induces Inflammation and Insulin Resistance via the NF-kappaB and STAT3 Signaling Pathways in Hepatocytes. Journal of Diabetes Research. 2019;2019:4021623. doi: 10.1155/2019/4021623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Elsaid NH, Sadik NA, Ahmed NR, Fayez SE, Mohammed NAE. Serum omentin-1 levels in type 2 diabetic obese women in relation to glycemic control, insulin resistance and metabolic parameters. Journal of Clinical & Translational Endocrinology. 2018;13:14–19. doi: 10.1016/j.jcte.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Basak S, Sarkar A, Mathapati S, Duttaroy AK. Cellular growth and tube formation of HTR8/SVneo trophoblast: effects of exogenously added fatty acid-binding protein-4 and its inhibitor. Molecular and Cellular Biochemistry. 2018;437:55–64. doi: 10.1007/s11010-017-3095-9. [DOI] [PubMed] [Google Scholar]
- 118.Elmasri H, Ghelfi E, Yu C-W, Traphagen S, Cernadas M, Cao H, Shi G-P, Plutzky J, Sahin M, Hotamisligil G, et al. Endothelial cell-fatty acid binding protein 4 promotes angiogenesis: role of stem cell factor/c-kit pathway. Angiogenesis. 2012;15:457–468. doi: 10.1007/s10456-012-9274-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zamzam, A., Syed, M. H., Greco, E., Wheatcroft, M., Jain, S., Khan, H., Singh, K. K., Forbes, T. L., Rotstein, O., Abdin, R., et al. (2020). Fatty Acid Binding Protein 4-A Circulating Protein Associated with Peripheral Arterial Disease in Diabetic Patients. Journal of Clinical Medicine, 9 10.3390/jcm9092843. [DOI] [PMC free article] [PubMed]
- 120.Boord JB, Maeda K, Makowski L, Babaev VR, Fazio S, Linton MF, Hotamisligil GS. Adipocyte fatty acid-binding protein, aP2, alters late atherosclerotic lesion formation in severe hypercholesterolemia. Arteriosclerosis, Thrombosis, and Vascular Biology. 2002;22:1686–1691. doi: 10.1161/01.atv.0000033090.81345.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Nguyen, H. C., Qadura, M., Singh, K. K. (2020). Role of the Fatty Acid Binding Proteins in Cardiovascular Diseases: A Systematic Review. Journal of Clinical Medicine 9 10.3390/jcm9113390. [DOI] [PMC free article] [PubMed]
- 122.Shum BO, Mackay CR, Gorgun CZ, Frost MJ, Kumar RK, Hotamisligil GS, Rolph MS. The adipocyte fatty acid-binding protein aP2 is required in allergic airway inflammation. Journal of Clinical Investigation. 2006;116:2183–2192. doi: 10.1172/JCI24767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Makowski L, Hotamisligil GS. The role of fatty acid binding proteins in metabolic syndrome and atherosclerosis. Current Opinion in Lipidology. 2005;16:543–548. doi: 10.1097/01.mol.0000180166.08196.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Coe NR, Simpson MA, Bernlohr DA. Targeted disruption of the adipocyte lipid-binding protein (aP2 protein) gene impairs fat cell lipolysis and increases cellular fatty acid levels. Journal of Lipid Research. 1999;40:967–972. doi: 10.1016/S0022-2275(20)32133-7. [DOI] [PubMed] [Google Scholar]
- 125.Llaverias G, Noe V, Penuelas S, Vazquez-Carrera M, Sanchez RM, Laguna JC, Ciudad CJ, Alegret M. Atorvastatin reduces CD68, FABP4, and HBP expression in oxLDL-treated human macrophages. Biochemical and Biophysical Research Communications. 2004;318:265–274. doi: 10.1016/j.bbrc.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 126.Makowski L, Brittingham KC, Reynolds JM, Suttles J, Hotamisligil GS. The fatty acid-binding protein, aP2, coordinates macrophage cholesterol trafficking and inflammatory activity. Macrophage expression of aP2 impacts peroxisome proliferator-activated receptor gamma and IkappaB kinase activities. Journal of Biological Chemistry. 2005;280:12888–12895. doi: 10.1074/jbc.M413788200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Maeda K, Uysal KT, Makowski L, Gorgun CZ, Atsumi G, Parker RA, Bruning J, Hertzel AV, Bernlohr DA, Hotamisligil GS. Role of the fatty acid binding protein mal1 in obesity and insulin resistance. Diabetes. 2003;52:300–307. doi: 10.2337/diabetes.52.2.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Makowski L, Boord JB, Maeda K, Babaev VR, Uysal KT, Morgan MA, Parker RA, Suttles J, Fazio S, Hotamisligil GS, et al. Lack of macrophage fatty-acid-binding protein aP2 protects mice deficient in apolipoprotein E against atherosclerosis. Nature Medicine. 2001;7:699–705. doi: 10.1038/89076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hertzel AV, Bennaars-Eiden A, Bernlohr DA. Increased lipolysis in transgenic animals overexpressing the epithelial fatty acid binding protein in adipose cells. Journal of Lipid Research. 2002;43:2105–2111. doi: 10.1194/jlr.m200227-jlr200. [DOI] [PubMed] [Google Scholar]
- 130.Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. Journal of Clinical Investigation. 2003;112:1821–1830. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cao H, Maeda K, Gorgun CZ, Kim HJ, Park SY, Shulman GI, Kim JK, Hotamisligil GS. Regulation of metabolic responses by adipocyte/macrophage Fatty Acid-binding proteins in leptin-deficient mice. Diabetes. 2006;55:1915–1922. doi: 10.2337/db05-1496. [DOI] [PubMed] [Google Scholar]
- 132.Boord JB, Maeda K, Makowski L, Babaev VR, Fazio S, Linton MF, Hotamisligil GS. Combined adipocyte-macrophage fatty acid-binding protein deficiency improves metabolism, atherosclerosis, and survival in apolipoprotein E-deficient mice. Circulation. 2004;110:1492–1498. doi: 10.1161/01.CIR.0000141735.13202.B6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Maeda K, Cao H, Kono K, Gorgun CZ, Furuhashi M, Uysal KT, Cao Q, Atsumi G, Malone H, Krishnan B, et al. Adipocyte/macrophage fatty acid binding proteins control integrated metabolic responses in obesity and diabetes. Cell Metabolism. 2005;1:107–119. doi: 10.1016/j.cmet.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 134.Chakrabarti P, Kim JY, Singh M, Shin YK, Kim J, Kumbrink J, Wu Y, Lee MJ, Kirsch KH, Fried SK, et al. Insulin inhibits lipolysis in adipocytes via the evolutionarily conserved mTORC1-Egr1-ATGL-mediated pathway. Molecular and Cellular Biology. 2013;33:3659–3666. doi: 10.1128/MCB.01584-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wondmkun YT. Obesity, Insulin Resistance, and Type 2 Diabetes: Associations and Therapeutic Implications. Diabetes, Metabolic Syndrome and Obesity. 2020;13:3611–3616. doi: 10.2147/DMSO.S275898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Miyazawa-Hoshimoto S, Takahashi K, Bujo H, Hashimoto N, Saito Y. Elevated serum vascular endothelial growth factor is associated with visceral fat accumulation in human obese subjects. Diabetologia. 2003;46:1483–1488. doi: 10.1007/s00125-003-1221-6. [DOI] [PubMed] [Google Scholar]
- 137.Barchetta, I., Chiappetta, C., Ceccarelli, V., Cimini, F. A., Bertoccini, L., Gaggini, M., Cristofano, C. D., Silecchia, G., Lenzi, A., Leonetti, F., et al. (2020). Angiopoietin-Like Protein 4 Overexpression in Visceral Adipose Tissue from Obese Subjects with Impaired Glucose Metabolism and Relationship with Lipoprotein Lipase. International Journal of Molecular Sciences 21 10.3390/ijms21197197. [DOI] [PMC free article] [PubMed]
- 138.Ruppert PMM, Michielsen C, Hazebroek EJ, Pirayesh A, Olivecrona G, Afman LA, Kersten S. Fasting induces ANGPTL4 and reduces LPL activity in human adipose tissue. Molecular Metabolism. 2020;40:101033. doi: 10.1016/j.molmet.2020.101033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Aryal, B., Singh, A. K., Zhang, X., Varela, L., Rotllan, N., Goedeke, L., Chaube, B., Camporez, J. P., Vatner, D. F., Horvath, T. L., et al. (2018). Absence of ANGPTL4 in adipose tissue improves glucose tolerance and attenuates atherogenesis. JCI Insight, 3 10.1172/jci.insight.97918. [DOI] [PMC free article] [PubMed]
- 140.Koster A, Chao YB, Mosior M, Ford A, Gonzalez-DeWhitt PA, Hale JE, Li D, Qiu Y, Fraser CC, Yang DD, et al. Transgenic angiopoietin-like (angptl)4 overexpression and targeted disruption of angptl4 and angptl3: regulation of triglyceride metabolism. Endocrinology. 2005;146:4943–4950. doi: 10.1210/en.2005-0476. [DOI] [PubMed] [Google Scholar]
- 141.Kersten S. Role and mechanism of the action of angiopoietin-like protein ANGPTL4 in plasma lipid metabolism. Journal of Lipid Research. 2021;62:100150. doi: 10.1016/j.jlr.2021.100150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Singh AK, Aryal B, Chaube B, Rotllan N, Varela L, Horvath TL, Suarez Y, Fernandez-Hernando C. Brown adipose tissue derived ANGPTL4 controls glucose and lipid metabolism and regulates thermogenesis. Molecular Metabolism. 2018;11:59–69. doi: 10.1016/j.molmet.2018.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Katanasaka, Y., Saito, A., Sunagawa, Y., Sari, N., Funamoto, M., Shimizu, S., Shimizu, K., Akimoto, T., Ueki, C., Kitano, M., et al. (2022). ANGPTL4 Expression Is Increased in Epicardial Adipose Tissue of Patients with Coronary Artery Disease. Journal of Clinical Medicine, 11 10.3390/jcm11092449. [DOI] [PMC free article] [PubMed]
- 144.Riccardi G, Rivellese AA. Dietary treatment of the metabolic syndrome-the optimal diet. British Journal of Nutrition. 2000;83:S143–S148. doi: 10.1017/s0007114500001082. [DOI] [PubMed] [Google Scholar]
- 145.Vessby B, Uusitupa M, Hermansen K, Riccardi G, Rivellese AA, Tapsell LC, Nalsen C, Berglund L, Louheranta A, Rasmussen BM, et al. Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: The KANWU Study. Diabetologia. 2001;44:312–319. doi: 10.1007/s001250051620. [DOI] [PubMed] [Google Scholar]
- 146.Ma J, Folsom AR, Shahar E, Eckfeldt JH. Plasma fatty acid composition as an indicator of habitual dietary fat intake in middle-aged adults. The Atherosclerosis Risk in Communities (ARIC) Study Investigators. The American Journal of Clinical Nutrition. 1995;62:564–571. doi: 10.1093/ajcn/62.3.564. [DOI] [PubMed] [Google Scholar]
- 147.Ristic-Medic D, Suzic S, Vucic V, Takic M, Tepsic J, Glibetic M. Serum and erythrocyte membrane phospholipids fatty acid composition in hyperlipidemia: effects of dietary intervention and combined diet and fibrate therapy. General Physiology and Biophysics. 2009;28:190–199. [PubMed] [Google Scholar]
- 148.Duan Y, Zeng L, Zheng C, Song B, Li F, Kong X, Xu K. Inflammatory Links Between High Fat Diets and Diseases. Frontiers in Immunology. 2018;9:2649. doi: 10.3389/fimmu.2018.02649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Calder PC, Ahluwalia N, Brouns F, Buetler T, Clement K, Cunningham K, Esposito K, Jonsson LS, Kolb H, Lansink M, et al. Dietary factors and low-grade inflammation in relation to overweight and obesity. British Journal of Nutrition. 2011;106:S5–S78. doi: 10.1017/S0007114511005460. [DOI] [PubMed] [Google Scholar]
- 150.Djuricic, I., Calder, P. C. (2021). Beneficial Outcomes of Omega-6 and Omega-3 Polyunsaturated Fatty Acids on Human Health: An Update for 2021. Nutrients, 13 10.3390/nu13072421. [DOI] [PMC free article] [PubMed]
- 151.Rivellese AA, Maffettone A, Vessby B, Uusitupa M, Hermansen K, Berglund L, Louheranta A, Meyer BJ, Riccardi G. Effects of dietary saturated, monounsaturated and n-3 fatty acids on fasting lipoproteins, LDL size and post-prandial lipid metabolism in healthy subjects. Atherosclerosis. 2003;167:149–158. doi: 10.1016/s0021-9150(02)00424-0. [DOI] [PubMed] [Google Scholar]
- 152.Thomsen C, Rasmussen O, Lousen T, Holst JJ, Fenselau S, Schrezenmeir J, Hermansen K. Differential effects of saturated and monounsaturated fatty acids on postprandial lipemia and incretin responses in healthy subjects. The American Journal of Clinical Nutrition. 1999;69:1135–1143. doi: 10.1093/ajcn/69.6.1135. [DOI] [PubMed] [Google Scholar]
- 153.Poli, A., Agostoni, C.; Visioli, F. (2023). Dietary Fatty Acids and Inflammation: Focus on the n-6 Series. International Journal of Molecular Sciences, 24 10.3390/ijms24054567. [DOI] [PMC free article] [PubMed]
- 154.Wang H, Storlien LH, Huang XF. Effects of dietary fat types on body fatness, leptin, and ARC leptin receptor, NPY, and AgRP mRNA expression. American Journal of Physiology-Endocrinology and Metabolism. 2002;282:E1352–E1359. doi: 10.1152/ajpendo.00230.2001. [DOI] [PubMed] [Google Scholar]
- 155.Janovska P, Flachs P, Kazdova L, Kopecky J. Anti-obesity effect of n-3 polyunsaturated fatty acids in mice fed high-fat diet is independent of cold-induced thermogenesis. Physiological Research. 2013;62:153–161. doi: 10.33549/physiolres.932464. [DOI] [PubMed] [Google Scholar]
- 156.Srinivas V, Molangiri A, Varma S, Mallepogu A, Kona SR, Ibrahim A, Duttaroy AK, Basak S. Maternal omega-3 fatty acid deficiency affects fetal thermogenic development and postnatal musculoskeletal growth in mice. The Journal of Nutritional Biochemistry. 2023;112:109218. doi: 10.1016/j.jnutbio.2022.109218. [DOI] [PubMed] [Google Scholar]
- 157.Ebbesson SO, Risica PM, Ebbesson LO, Kennish JM, Tejero ME. Omega-3 fatty acids improve glucose tolerance and components of the metabolic syndrome in Alaskan Eskimos: the Alaska Siberia project. International Journal of Circumpolar Health. 2005;64:396–408. doi: 10.3402/ijch.v64i4.18016. [DOI] [PubMed] [Google Scholar]
- 158.Delarue J, Couet C, Cohen R, Brechot JF, Antoine JM, Lamisse F. Effects of fish oil on metabolic responses to oral fructose and glucose loads in healthy humans. American Journal of Physiology. 1996;270:E353–E362. doi: 10.1152/ajpendo.1996.270.2.E353. [DOI] [PubMed] [Google Scholar]
- 159.Rossi AS, Lombardo YB, Lacorte JM, Chicco AG, Rouault C, Slama G, Rizkalla SW. Dietary fish oil positively regulates plasma leptin and adiponectin levels in sucrose-fed, insulin-resistant rats. American Journal of Physiology-Endocrinology and Metabolism. 2005;289:R486–R494. doi: 10.1152/ajpregu.00846.2004. [DOI] [PubMed] [Google Scholar]
- 160.Flachs P, Mohamed-Ali V, Horakova O, Rossmeisl M, Hosseinzadeh-Attar MJ, Hensler M, Ruzickova J, Kopecky J. Polyunsaturated fatty acids of marine origin induce adiponectin in mice fed a high-fat diet. Diabetologia. 2006;49:394–397. doi: 10.1007/s00125-005-0053-y. [DOI] [PubMed] [Google Scholar]
- 161.Kwon Y. Immuno-Resolving Ability of Resolvins, Protectins, and Maresins Derived from Omega-3 Fatty Acids in Metabolic Syndrome. Molecular Nutrition Food Research. 2020;64:e1900824. doi: 10.1002/mnfr.201900824. [DOI] [PubMed] [Google Scholar]
- 162.Spite M, Clària J, Serhan CN. Resolvins, Specialized Proresolving Lipid Mediators, and Their Potential Roles in Metabolic Diseases. Cell Metabolism. 2014;19:21–36. doi: 10.1016/j.cmet.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Basak S, Duttaroy AK. Conjugated Linoleic Acid and Its Beneficial Effects in Obesity, Cardiovascular Disease, and Cancer. Nutrients. 2020;12:1913. doi: 10.3390/nu12071913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Basak S, Duttaroy AK. cis-9,trans-11 conjugated linoleic acid stimulates expression of angiopoietin like-4 in the placental extravillous trophoblast cells. Biochimica Et Biophysica Acta-Molecular and Cell Biology of Lipids. 2013;1831:834–843. doi: 10.1016/j.bbalip.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 165.Ryder JW, Portocarrero CP, Song XM, Cui L, Yu M, Combatsiaris T, Galuska D, Bauman DE, Barbano DM, Charron MJ, et al. Isomer-specific antidiabetic properties of conjugated linoleic acid. Improved glucose tolerance, skeletal muscle insulin action, and UCP-2 gene expression. Diabetes. 2001;50:1149–1157. doi: 10.2337/diabetes.50.5.1149. [DOI] [PubMed] [Google Scholar]
- 166.Henriksen EJ, Teachey MK, Taylor ZC, Jacob S, Ptock A, Kramer K, Hasselwander O. Isomer-specific actions of conjugated linoleic acid on muscle glucose transport in the obese Zucker rat. American Journal of Physiology-Endocrinology and Metabolism. 2003;285:E98–E105. doi: 10.1152/ajpendo.00013.2003. [DOI] [PubMed] [Google Scholar]
- 167.Nagao K, Inoue N, Wang YM, Hirata J, Shimada Y, Nagao T, Matsui T, Yanagita T. The 10trans,12cis isomer of conjugated linoleic acid suppresses the development of hypertension in Otsuka Long-Evans Tokushima fatty rats. Biochemical and Biophysical Research Communications. 2003;306:134–138. doi: 10.1016/s0006-291x(03)00929-x. [DOI] [PubMed] [Google Scholar]
- 168.Nagao K, Inoue N, Wang YM, Yanagita T. Conjugated linoleic acid enhances plasma adiponectin level and alleviates hyperinsulinemia and hypertension in Zucker diabetic fatty (fa/fa) rats. Biochemical and Biophysical Research Communications. 2003;310:562–566. doi: 10.1016/j.bbrc.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 169.Inoue N, Nagao K, Hirata J, Wang YM, Yanagita T. Conjugated linoleic acid prevents the development of essential hypertension in spontaneously hypertensive rats. Biochemical and Biophysical Research Communications. 2004;323:679–684. doi: 10.1016/j.bbrc.2004.08.139. [DOI] [PubMed] [Google Scholar]
- 170.Pariza MW, Park Y, Cook ME. The biologically active isomers of conjugated linoleic acid. Progress in Lipid Research. 2001;40:283–298. doi: 10.1016/s0163-7827(01)00008-x. [DOI] [PubMed] [Google Scholar]
- 171.Thom E, Wadstein J, Gudmundsen O. Conjugated linoleic acid reduces body fat in healthy exercising humans. Journal of Internal Medicine. 2001;29:392–396. doi: 10.1177/147323000102900503. [DOI] [PubMed] [Google Scholar]
- 172.Tsuzuki T, Kawakami Y, Nakagawa K, Miyazawa T. Conjugated docosahexaenoic acid inhibits lipid accumulation in rats. Journal of Nutritional Biochemistry. 2006;17:518–524. doi: 10.1016/j.jnutbio.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 173.Tsuzuki T, Kawakami Y, Suzuki Y, Abe R, Nakagawa K, Miyazawa T. Intake of conjugated eicosapentaenoic acid suppresses lipid accumulation in liver and epididymal adipose tissue in rats. Lipids. 2005;40:1117–1123. doi: 10.1007/s11745-005-1475-0. [DOI] [PubMed] [Google Scholar]
- 174.Morange PE, Alessi MC. Thrombosis in central obesity and metabolic syndrome: mechanisms and epidemiology. Journal of Thrombosis and Haemostasis. 2013;110:669–680. doi: 10.1160/TH13-01-0075. [DOI] [PubMed] [Google Scholar]
- 175.Napoleone E, A DIS, Amore C, Baccante G, di Febbo C, Porreca E, de Gaetano G, Donati MB, Lorenzet R. Leptin induces tissue factor expression in human peripheral blood mononuclear cells: a possible link between obesity and cardiovascular risk? Journal of Thrombosis and Haemostasis. 2007;5:1462–1468. doi: 10.1111/j.1538-7836.2007.02578.x. [DOI] [PubMed] [Google Scholar]
- 176.Popko K, Gorska E, Stelmaszczyk-Emmel A, Plywaczewski R, Stoklosa A, Gorecka D, Pyrzak B, Demkow U. Proinflammatory cytokines Il-6 and TNF-alpha and the development of inflammation in obese subjects. European Journal of Medical Research. 2010;15:120–122. doi: 10.1186/2047-783x-15-s2-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Campello E, Zabeo E, Radu CM, Spiezia L, Gavasso S, Fadin M, Woodhams B, Vettor R, Simioni P. Hypercoagulability in overweight and obese subjects who are asymptomatic for thrombotic events. Thromb Haemost. 2015;113:85–96. doi: 10.1160/TH14-02-0156. [DOI] [PubMed] [Google Scholar]
- 178.Knowles DM, Tolidjian B, Marboe C, D’Agati V, Grimes M, Chess L. Monoclonal anti-human monocyte antibodies OKM1 and OKM5 possess distinctive tissue distributions including differential reactivity with vascular endothelium. Journal of Immunology. 1984;132:2170–2173. doi: 10.4049/jimmunol.132.5.2170. [DOI] [PubMed] [Google Scholar]
- 179.Scalia R, Murohara T, Campbell B, Kaji A, Lefer AM. Lysophosphatidylcholine stimulates leukocyte rolling and adherence in rat mesenteric microvasculature. American Journal of Physiology. 1997;272:H2584–H2590. doi: 10.1152/ajpheart.1997.272.6.H2584. [DOI] [PubMed] [Google Scholar]
- 180.Minami M, Yokokawa K, Kohno M, Yasunari K, Yoshikawa J. Suppression of endothelin-3-induced nitric oxide synthesis by triglyceride in human endothelial cells. Journal of Cardiovascular Pharmacology. 1998;31:S467–S469. doi: 10.1097/00005344-199800001-00133. [DOI] [PubMed] [Google Scholar]
- 181.Weber C, Erl W, Weber PC. Enhancement of monocyte adhesion to endothelial cells by oxidatively modified low-density lipoprotein is mediated by activation of CD11b. Biochemical and Biophysical Research Communications. 1995;206:621–628. doi: 10.1006/bbrc.1995.1088. [DOI] [PubMed] [Google Scholar]
- 182.Jude EB, Douglas JT, Anderson SG, Young MJ, Boulton AJ. Circulating cellular adhesion molecules ICAM-1, VCAM-1, P- and E-selectin in the prediction of cardiovascular disease in diabetes mellitus. European Journal of Internal Medicine. 2002;13:185–189. doi: 10.1016/s0953-6205(02)00014-6. [DOI] [PubMed] [Google Scholar]