Abstract
Study Design
A prospective study.
Objective
to evaluate the impact of vertebral body comminution and Posterior Ligamentous Complex (PLC) integrity on the treatment recommendations of thoracolumbar fractures among an expert panel of 22 spine surgeons.
Methods
A review of 183 prospectively collected thoracolumbar burst fracture computed tomography (CT) scans by an expert panel of 22 trauma spine surgeons to assess vertebral body comminution and PLC integrity. This study is a sub-study of a prospective observational study of thoracolumbar burst fractures (Spine TL A3/A4). Each expert was asked to grade the degree of comminution and certainty about the PLC disruption from 0 to 100, with 0 representing the intact vertebral body or intact PLC and 100 representing complete comminution or complete PLC disruption, respectively.
Results
≥45% comminution had a 74% chance of having surgery recommended, while <25% comminution had an 86.3% chance of non-surgical treatment. A comminution from 25 to 45% had a 57% chance of non-surgical management. ≥55% PLC injury certainity had a 97% chance of having surgery, and ≥45-55% PLC injury certainty had a 65%. <20% PLC injury had a 64% chance of having non-operative treatment. A 20 to 45% PLC injury certainity had a 56% chance of non-surgical management. There was fair inter-rater agreement on the degree of comminution (ICC .57 [95% CI 0.52-.63]) and the PLC integrity (ICC .42 [95% CI 0.37-.48]).
Conclusion
The study concludes that vetebral comminution and PLC integrity are major dterminant in decision making of thoracolumbar fractures without neurological deficit. However, more objective, reliable, and accurate methods of assessment of these variables are warranted.
Keywords: posterior ligamentous complex, vertebral comminution, thoracolumbar fractures, equipoise study, burst fractures, A3, A4, computed tomography, magnetic resonance imaging, AO spine thoracolumbar injury classification
Introduction
Despite multiple classification schemes and algorithms, deciding when to operate on thoracolumbar (TL) burst fractures in neurologically intact patients remains debatable. 1 White and Panjabi et al identified post-traumatic instability in TL fractures as developing a neurological deficit, bony instability, or ligamentous instability. 2 Therefore, for TL burst fractures with intact neurology, it is generally agreed that the degree of bony instability and the integrity of the posterior ligamentous complex (PLC) are the two critical determinants in decision-making. 3 Nevertheless, the lack of agreed-on criteria for bony instability or PLC injury may explain why decision-making in TL burst fractures has been controversial.4,5
The criteria used to indicate bony instability have changed across various classification systems over the years.6-9 Denis et al. defined bony instability as middle column or three-column injury. 6 The newest AO Spine classification for TL fractures differentiates the degree of bony instability based on the presence of superior and inferior endplate fractures (A4) vs a single endplate fracture (A3), each with associated posterior body involvement, which differentiates them from A1 and A2. 7 Although vertebral body comminution is though to predict poor fracture healing and progressive kyphosis, it was not formally included in the AO Spine classification.7,10 A possible explanation is the lack of an agreed-upon definition of vertebral body comminution that mirrors its definition in long bone fractures as at least three fragments. 10 The McCormack Load-Sharing Classification (LSC) is the only recognized classification incorporating fracture comminution, besides fragment diastasis and kyphosis degree, to quantify the severity of vertebral body injury 11 A high score on the load-sharing classification suggested that short-segment posterior instrumentation might fail. However, the load-sharing classification has not gained much popularity because of its complexity and low reliability. 12
The posterior ligamentous complex (PLC) represents the posterior tension bands that protect the spine from excessive movements and progressive forward bending.4,13 PLC disruption might result in delayed instability manifested as kyphosis, progressive back pain, or even new neurological deficits; hence, surgical stabilization has been recommended in these cases. 14 The AO Spine Thoracolumbar Injury classification distinguishes between fractures with and without PLC disruption: Type B and Type A, respectively. 7 The current AO Spine classification is CT-based, recognizing the challenges in obtaining MRIs for many centers. 7 However, CT does not allow for the direct assessment of PLC; instead, PLC injury could be inferred from secondary signs such as facet diastasis and horizontal laminar or spinous process fracture, among other findings. 15 Because of the limited accuracy and reliability of PLC assessment in CT, there is often uncertainty about the PLC status. This uncertainty is reflected in the indeterminate category (M1 modifier) in the AO Spine Classification system. 7 Therefore, the perceived probability of PLC injury remains an essential driver for the decision-making of TL burst fractures and contributes to the continued controversy surrounding the treatment of these injuries. 2
This article investigates how comminution and PLC integrity, as assessed by an expert panel, influenced treatment recommendations in 183 thoracolumbar burst fractures without a neurologic deficit.
Methods
Study Design
The study is part of a prospective observational study of TL Fractures, the Spine TL A3/A4 study. For a complete description of the selection process, inclusion and exclusion criteria, please refer to the manuscript Dandurand et al. “Understanding Decision Making as it Influences Treatment in Thoracolumbar Burst Fractures Without Neurological Deficit: Conceptual Framework and Methodology” from the same Journal Focus issue.
Assessment of Degree of Comminution and Posterior Ligamentous Complex Injury Certainty
The 22 Spine Trauma experts with extensive experience managing spinal trauma were recruited from the AO Spine Knowledge Forum Trauma (KF Trauma). Each expert panel member reviewed the DICOM images of the 183 TL fracture cases and was asked to classify each injury based on the AO TL Injury Classification system. Each expert was asked to grade the degree of comminution from 0 to 100, with 0 representing the intact vertebral body and 100 representing complete comminution. For PLC evaluation, each expert was asked to quantify how certain they were about the PLC being disrupted from 0 to 100, with 0 reflecting a completely intact PLC and 100 representing complete disruption. Finally, they were asked to recommend treatment – either surgical or non-operative. These experts were agnostic to the patient’s actual treatment within the Spine TL A3/A4 study and were also agnostic to any results of the Spine TL A3/A4 study.
Statistical Analysis
The association of the degree of comminution with fracture type and the surgical decision was done using the independent sample test. The distribution of PLC across categories of A3 and A4 was analyzed using the independent samples Mann-Whitney U test. The interobserver reliability for PLC injury certainty and degree of comminution was analyzed using Inter Class Correlation (ICC). The association between PLC injury certainty or degree of comminution and surgery recommendation was analyzed using Classification and Regression Trees (CART). The results of CART were cross-validated using the k-fold cross-validation, where the dataset is split into k equal-sized folds. The model is trained on k-1 of these folds and tested on the remaining fold. This process is repeated k times, with each fold used as the test set once. The results of the k-tests are then averaged to produce an overall estimate of the model’s performance. 16 Rstudio and SPSS were used for data analysis, and P-values of .05 were considered statistically significant. 16 We applied the type of decision tree model, which is helpful for non-normal distributions of data and specifically for a binary outcome (the outcome of this study is recommending surgery or not).
Results
Correlation of the Degree of Comminution (0-100%) With Fracture Type
The degree of comminution was significantly higher for A4 fractures than A3 (58.0% vs 34.6%, P < .001) and for non-A3/A4 than A3/A4 fractures (45.9% vs 54.0%, P < .001, Table 1).
Table 1.
Correlation of the Degree of Comminution With Fracture Type and Surgical Recommendation by the Expert Panel.
| N | Mean | Std. Deviation | Std. Error Mean | |||
|---|---|---|---|---|---|---|
| Comminution | Primary injury type | A3 | 1831 | 34.55 | 15.147 | .354 |
| A4 | 1713 | 58.07 | 19.488 | .471 | ||
| Surgery recommendation | Yes | 2118 | 56.29 | 19.487 | .423 | |
| No | 1895 | 36.34 | 19.395 | .446 | ||
Correlation of the Degree of Comminution With Choosing Surgical Treatment
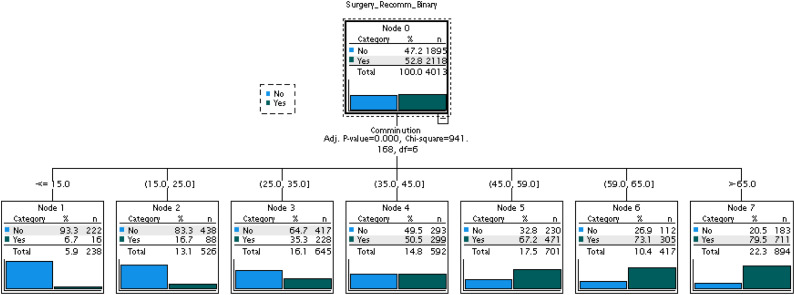
Fractures recommended for surgical treatment showed a significantly higher degree of comminution than those recommended for non-surgical treatment (56.3% vs 36.3%, P < .001, Table 1). Fractures with ≥45% comminution had a 74% chance of having a recommendation for surgery, while fractures with <25% comminution had an 86.3% chance of having a recommendation for non-surgical treatment. Fractures with comminution from 25 to 45% had a slightly higher chance of having a recommendation for non-surgical than surgical treatment (57% vs 43%, Figure 1).
Figure 1.
Association of the degree of comminution with operative vs non-operative recommendation using classification and regression trees.
Correlation of the Posterior Ligamentous Complex Injury Certainty (0-100%) With Fracture Type and M1 Modifier
A4 fractures were associated with a significantly higher degree of PLC injury certainty than A3 (30.6% vs 21.16%, P < .001, Table 2). B and C-type fractures were associated with a significantly higher degree of PLC certainty than A3/A4 and A1/2 (86.5% vs 25.28% and 6.6%. respectively, P < .001, ANOVA). The use of the M1 modifier was associated with a significantly higher degree of PLC injury certainty than others (54.6% vs 14.9%, P < .001, Table 2).
Table 2.
Correlation of the PLC Injury Certainty With Fracture Type and Surgical Recommendation by the Expert Panel.
| N | Mean | Std. Deviation | Std. Error Mean | |||
|---|---|---|---|---|---|---|
| PLC injury certainty | Primary injury type | A3 | 1831 | 21.09 | 23.35 | .549 |
| A4 | 1713 | 30.84 | 27.29 | .659 | ||
| Surgery recommendation | Yes | 2118 | 56.29 | 19.487 | .423 | |
| No | 1895 | 36.34 | 19.395 | .446 | ||
| M1 modifier | Yes | 2346 | 14.95 | 20.47 | .421 | |
| No | 1684 | 54.57 | 28.14 | .693 | ||
Correlation of PLC Injury Certainty (0-100%) With Choosing Surgical Treatment
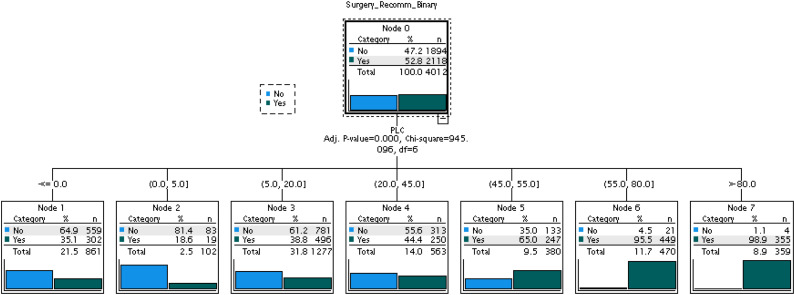
Fractures in which surgery was recommended had a significantly higher degree of PLC injury than those in which non-operative treatment was recommended (56.3% vs 36.3%, P < .001, independent sample test). Fractures with ≥55% PLC injury had a 97% chance of having surgery recommended, and fractures with ≥45-55% PLC disruption had a 65% chance of having surgery recommended. Fractures with <20% PLC injury had a 64% chance of having a recommendation for non-surgical treatment. Patients with PLC injuries from 20 to 45% had a slightly higher chance of non-surgical than a surgical recommendation (56% vs 44%, Figure 2).
Figure 2.
Association of the posterior ligamentous complex injury certainty with operative vs non-operative recommendation using classification and regression trees.
The correct classification result after cross-validation for the communication model was 71.3%, and for the PLC model was 69.5%.
Inter-Rater Reliability Agreement of the Degree of Comminution and Posterior Ligamentous Complex
There was a fair inter-rater agreement among the 22 expert reviewers on the degree of comminution (ICC .57 [95% CI 0.52-.63]) and the PLC integrity (ICC .42 [95% CI 0.37-.48]).
Discussion
Key Findings and Interpretations
This study evaluated the influence of vertebral comminution and PLC integrity on TL burst fracture decision-making amongst an expert panel of 22 spine surgeons. A high degree of comminution (>45%) or PLC injury (>55%) predicted a surgical recommendation among the expert panel. In contrast, a lower degree of comminution (<25%) or PLC injury (<20%) predicted a non-surgical recommendation. The intermediate degree of comminution or PLC injury (20-45%) could not differentiate the surgical vs non-surgical treatment recommendation amongst the panel. The results of this study confirm the importance of comminution and PLC integrity in the therapeutic decision-making for TL burst fractures with intact neurology. Meanwhile highlight the lack of an agreed-on CT criterion to define PLC integrity or comminution, to give clear guidance.
Correlation of the Degree of Comminution With Fracture Type and Surgical Decision
This study’s finding that the degree of vertebral comminution correlates well with decision-making by the expert group goes in line with the proposal that comminution predicts poor fracture healing and the potential for the development of delayed kyphosis. 10 However, the new AO Spine Classification of TL burst fractures does not account for vertebral comminution except indirectly by differentiating between the A3 and A4 fractures. 7 The current AO Spine TL Classification is simple and reliable for classifying burst fractures to mitigate the shortcomings of the old AO classification by Magerl. 7 However, previous studies failed to show a significant difference in the operative or non-operative outcome between A3 and A4 fractures. 1 The lack of outcome difference might be explained by the shortcomings of the validation studies or poor reliability in distinguishing A3 from A4.17,18 Another possibility is that a single criterion may be insufficient to encompass the broad injury spectrum of TL burst fractures. 19 In that case, additional markers, such as vertebral comminution, may be needed to adequately capture the spectrum of injury severity and, by extension, to correlate with clinical outcomes. 19 However, a more comprehensive classification may be associated with poor reliability and practicality. 20
How to Incorporate Comminution in Decision-Making
The question of incorporating comminution into classification schemes persists without a universally accepted definition of vertebral comminution or a reliable assessment method. 10 Defining comminution based on at least 3 fragments, similar to long bone fractures, may be too simplistic for the cancellous vertebral body. The load-sharing classification has defined comminution based on the percentage of comminution in the sagittal view, fragment diastasis in the axial view, and the amount of corrected traumatic kyphosis. 11 However, the original McCormack study’s results were questioned due to the small number of cases (n = 28) and the use of outdated instrumentation techniques. 21 The original McCormack study relied on the amount of corrected kyphosis, i.e., the difference between postoperative and preoperative kyphosis, which can not be implemented in preoperative decision-making. 11 In 2018 De Lure F et al proposed the ‘‘vertebral body spread”“ to objectively to evaluate the percentage of vertebral body comminution and spreading of the fractured fragments. 22 This method has proved helpful in guiding the decision of whether to do posterior or circumferential fixation. 22 The vertebral spread method and other artificial intelligence-based methods may hold promise for evaluating vertebral comminution in the future, but they are not being widely implemented in the mean time.
Correlation of the Certainty of Posterior Ligamentous Complex Injury With Fracture Type and Surgical Decision
This study found that the perceived probability of PLC injury correlated well with decision-making, with a higher probability of PLC injury predicting surgical recommendation and vice versa. The expert reviewers demonstrated moderate reliability in estimating the probability of PLC injury and wide variability in their perceived threshold for PLC certainty in choosing surgery or conservative treatment. These findings emphasize the importance of PLC injury in the therapeutic decision-making for TL burst fractures. Still, itthey highlight the need for more accurate and objective CT criteria for identifying PLC injury to improve the decision-making process. 23 2 recent studies proposed an algorithm to predict the probability of PLC injury based on the number of positive CT findings. More than 2 CT findings yielded a high enough PPV for PLC injury (91%), warranting its use as a surrogate marker of a likely PLC injury or type B injury.15,24 PLC status should be considered intact or type A if there are no positive CT findings (PPV 9%). A single CT finding is insufficiently accurate to rule in or rule out PLC injury and may indicate indeterminate PLC status or M1 modifier. 15 When using these CT criteria in a recent study, most TL burst fractures (88%) were correctly classified with CT, with MRI changing the classification to type B in only 12% of patients. 25 Furthermore, the M1 modifier, as defined by a single CT finding, could predict most of the upgrade from A3/A4 to type B (26% M1 modifier vs 5% no M1). The M1 modifier can help guide which TL burst fractures require additional MRI testing to rule in or rule out PLC injury. 22 However, CT-based PLC criteria (Including M1) require multicenter validation before being widely implemented. 26
The previous results imply that confusion about PLC status on CT images may have overestimated the impact of PLC injury in the decision-making process around TL burst fractures. The practicalities of MRI for TL burst fractures without neurological deficits may be simple; MRI can be conducted non-urgently within days of the injury, ensuring an accurate PLC evaluation 23 Alternatively, standing X-rays may demonstrate kyphosis consistent with a ligamentous injury, or these patients can be closely observed for their pain and early development of kyphosis.
Finding a Cut-Off Point of Posterior Ligamentous Complex Certainty and Comminution to Predict Surgical Decision
This study demonstrates a strong correlation between low or high comminution or PLC injury probability and non-surgical or surgical treatment recommendations. In contrast, intermediate degrees of comminution or PLC injury probability could not distinguish between surgical and non-surgical recommendations within the group. This study highlights the significance of comminution and PLC integrity in the TL burst fractures decision-making; however, determining a clear cut-off point to differentiate surgical from non-surgical treatment may prove more difficult.
Previous TL burst fracture classification schemes attempted a dichotomous separation between stable (complete) and unstable (incomplete) fractures, for example, A3 and A4. 19 This dichotomous classification disregards the broad injury severity spectrum and heterogeneity of TL burst fractures. We may also use graded criteria (unstable, stable, indeterminate) for every criterion used for classification. 19 For example, based on the findings of this study, we could include vertebral comminution >45% as an indicator of an unstable burst, 25% as stable, and between as indeterminate stability.
Strengths and Limitations
The use of CART analysis to examine the association of PLC or comminution probability with treatment recommendation has several advantages. CART can handle both categorical and can be used for classification and regression problems. Additionally, CART is computationally efficient and can handle large datasets. CART can handle it. 16 One limitation of the study is that it did not examine the relationship between comminution or PLC injury and clinical outcomes in patients treated operatively or non-operatively. In this study, we graded PLC certainty and comminution on a scale from 0 to 100, with 0 representing intact and 100 representing complete disruption, to assess the perceived grading by the reviewers. This grading, however, is subjective and cannot be implemented to guide the decison making in clinical practice. However, the subjective evaluation needs to be seen in the context of the study’s goal; to determine how much weight an expert panel puts on comminution or PLC assessment and how much they agreed or disagreed, given that there are no agreed-upon criteria. The study seeks to discover how expert panels evaluate these characteristics to lead future studies and maybe improve existing classification schemes. This study assessed comminution as the sole measure of bony instability without considering other indicators such as vertebral height loss, kyphotic angle, load-sharing classification, or canal compromise. 27 Initially, the study refrained from evaluating these radiographic parameters due to inherent measurement errors, variations in measurement methods, and poor reliability. However, on further discussion within the AO Spine Knowledge Forum Trauma, it was decided that studying the association of those parameters with decision-making could lead to a further depth of understanding. The relatively large number of reviewers from diverse regions and cases presents a crucial strength of this work.
Conclusions
This study evaluated the influence of vertebral comminution and PLC integrity on decision-making among an expert panel. A high degree of comminution (>45%) or PLC certainty (>55%) predicted a surgical decision among the expert panel. In contrast, a lower degree of comminution (<25%) or PLC certainty (<20%) predicted the non-operative decision. The intermediate degree of comminution or PLC certainty (20-45%) could not discriminate between surgical vs non-surgical decisions. The study concludes that while comminution and PLC integrity is essential in decision making, more objective, reliable, and accurate methods are warranted.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was organized and funded by AO Spine through the AO Spine Knowledge Forum Trauma, a focused group of international Trauma experts. AO Spine is a clinical division of the AO Foundation, which is an independent medically-guided not-for-profit organization. Study support was provided directly through AO Network Clinical Research.
ORCID iDs
Mohamed M. Aly https://orcid.org/0000-0001-5221-8288
Charlotte Dandurand https://orcid.org/0000-0002-4520-6454
Emiliano Vialle https://orcid.org/0000-0003-1157-4889
Shanmuganathan Rajasekaran https://orcid.org/0000-0001-6043-006X
Mohammad El-Skarkawi https://orcid.org/0000-0001-6177-7145
Rishi M. Kanna https://orcid.org/0000-0001-5817-4909
Martin Holas https://orcid.org/0000-0002-3763-8767
Eugen Cezar Popescu https://orcid.org/0000-0001-5732-5402
Gaston Camino-Willhuber https://orcid.org/0000-0002-5684-7679
Andrei Fernandes Joaquim https://orcid.org/0000-0003-2645-0483
Sebastian Bigdon https://orcid.org/0000-0002-4649-0610
Jose A. Canseco https://orcid.org/0000-0002-2152-5725
References
- 1.Rometsch E, Spruit M, Härtl R, et al. Does operative or nonoperative treatment achieve better results in A3 and A4 spinal fractures without neurological deficit? Systematic literature review with meta-analysis. Global Spine J. 2017;7(4):350-372. doi: 10.1177/2192568217699202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenthal BD, Boody BS, Jenkins TJ, Hsu WK, Patel AA, Savage JW. Thoracolumbar burst fractures. Clin Spine Surg. 2018;31(4):143-151. doi: 10.1097/BSD.0000000000000634. [DOI] [PubMed] [Google Scholar]
- 3.Tanasansomboon T, Kittipibul T, Limthongkul W, Yingsakmongkol W, Kotheeranurak V, Singhatanadgige W. Thoracolumbar burst fracture without neurological deficit: review of controversies and current evidence of treatment. World Neurosurg. 2022;162(March):29-35. doi: 10.1016/j.wneu.2022.03.061. [DOI] [PubMed] [Google Scholar]
- 4.Van Middendorp JJ, Patel AA, Schuetz M, Joaquim AF. The precision, accuracy and validity of detecting posterior ligamentous complex injuries of the thoracic and lumbar spine: a critical appraisal of the literature. Eur Spine J. 2013;22(3):461-474. doi: 10.1007/s00586-012-2602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spiegl UJ, Josten C, Devitt BM, Heyde CE. Incomplete burst fractures of the thoracolumbar spine: a review of literature. Eur Spine J. 2017;26(12):3187-3198. doi: 10.1007/s00586-017-5126-3. [DOI] [PubMed] [Google Scholar]
- 6.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983;8(8):817-831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184-201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 8.Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013;38(23):2028-2037. doi: 10.1097/BRS.0b013e3182a8a381. [DOI] [PubMed] [Google Scholar]
- 9.Lee JY, Vaccaro AR, Lim MR, et al. Thoracolumbar injury classification and severity score: a new paradigm for the treatment of thoracolumbar spine trauma. J Orthop Sci. 2005;10(6):671-675. doi: 10.1007/s00776-005-0956-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mattei TA, Hanovnikian J, Dinh DH. Progressive kyphotic deformity in comminuted burst fractures treated non-operatively: the Achilles tendon of the Thoracolumbar Injury Classification and Severity Score (TLICS). Eur Spine J. 2014;23(11):2255-2262. doi: 10.1007/S00586-014-3312-0. [DOI] [PubMed] [Google Scholar]
- 11.McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine 1994;19(15):1741-1744. [DOI] [PubMed] [Google Scholar]
- 12.Schroeder GD, Harrop JS, Vaccaro AR. Thoracolumbar trauma classification. Neurosurg Clin. 2017;28(1):23-29. doi: 10.1016/j.nec.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Aly MM, Elemam R, El-Sharkawi M, Hurlbert JR. Injury of the thoracolumbar posterior ligamentous complex: a bibliometric literature review. World Neurosurg. Published online January 18, 2022;161:21-33. doi: 10.1016/J.WNEU.2022.01.041. [DOI] [PubMed] [Google Scholar]
- 14.Vaccaro AR, Lim MR, Hurlbert RJ, et al. Surgical decision making for unstable thoracolumbar spine injuries. J Spinal Disord Tech. 2006;19(1):1-10. doi: 10.1097/01.bsd.0000180080.59559.45. [DOI] [PubMed] [Google Scholar]
- 15.Aly MM, Al-Shoaibi AM, Alzahrani AJ, Al Fattani A. Analysis of the combined computed tomography findings improves the accuracy of computed tomography for detecting posterior ligamentous complex injury of the thoracolumbar spine as defined by magnetic resonance imaging. World Neurosurg. 2021;151:e760-e770. doi: 10.1016/j.wneu.2021.04.106. [DOI] [PubMed] [Google Scholar]
- 16.Hastie T, Tibshirani R, Friedman J. No title. In: The Elements of Statistical Learning: Data Mining, Inference, and Prediction. 2nd ed. Springer; 2009. [Google Scholar]
- 17.Schroeder GD, Kepler CK, Koerner JD, et al. A worldwide analysis of the reliability and perceived importance of an injury to the posterior ligamentous complex in AO type A fractures. Global Spine J. 2015;5(5):378-382. doi: 10.1055/s-0035-1549034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kepler CK, Vaccaro AR, Koerner JD, et al. Reliability analysis of the AOSpine thoracolumbar spine injury classification system by a worldwide group of naïve spinal surgeons. Eur Spine J. 2016;25(4):1082-1086. doi: 10.1007/s00586-015-3765-9. [DOI] [PubMed] [Google Scholar]
- 19.Aly MM, Al-Shoaibi AM, Al-Aithan A, et al. Can vertical laminar fracture further discriminate fracture severity between thoracolumbar AO type A3 and A4 fractures? World Neurosurg. Published online August 14, 2021;155:e177-e187. doi: 10.1016/J.WNEU.2021.08.035. [DOI] [PubMed] [Google Scholar]
- 20.Chhabra HS, Kaul R, Kanagaraju V. Do we have an ideal classification system for thoracolumbar and subaxial cervical spine injuries: what is the expert’s perspective? Spinal Cord. 2015;53(1):42-48. doi: 10.1038/SC.2014.194. [DOI] [PubMed] [Google Scholar]
- 21.Filgueira ÉG, Imoto AM, da Silva HEC, Meves R. Thoracolumbar burst fracture: McCormack load-sharing classification: systematic review and single-arm meta-analysis. Spine (Phila Pa 1976). 2021;46(9):E542-E550. doi: 10.1097/BRS.0000000000003826. [DOI] [PubMed] [Google Scholar]
- 22.De Iure F, Lofrese G, De Bonis P, Cultrera F, Cappuccio M, Battisti S. Vertebral body spread in thoracolumbar burst fractures can predict posterior construct failure. Spine J. 2018;18(6):1005-1013. doi: 10.1016/j.spinee.2017.10.064. [DOI] [PubMed] [Google Scholar]
- 23.Aly MM, Al-Shoaibi AM, Aljuzair AH, Ziad Issa T, Vaccaro AR. GSJ-systematic review A proposal for a standardized imaging algorithm to improve the accuracy and reliability for the diagnosis of thoracolumbar posterior ligamentous complex injury in computed tomography and magnetic resonance imaging. Global Spine J. 2023;13(3):1-24. doi: 10.1177/21925682221129220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khurana B, Prevedello LM, Bono CM, et al. CT for thoracic and lumbar spine fractures: can CT findings accurately predict posterior ligament complex injury? Eur Spine J. 2018;27(12):3007-3015. doi: 10.1007/s00586-018-5712-z. [DOI] [PubMed] [Google Scholar]
- 25.Aly MM, Al-Shoaibi AM, Abduraba Ali S, Al Fattani A, Eldawoody H. How often would MRI change the thoracolumbar fracture classification or decision-making compared to CT alone? Orig Res Glob Spine J. 2022;2022:1-14. doi: 10.1177/21925682221089579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aly MM. Letter: congress of neurological surgeons systematic review and evidence-based guidelines on the evaluation and treatment of patients with thoracolumbar spine trauma: radiological evaluation. Neurosurgery. 2022;91(5):e143-e144. doi: 10.1227/neu.0000000000002152. [DOI] [PubMed] [Google Scholar]
- 27.Maheswaran A, Aiyer SN, Farouk O, et al. Assessment of interobserver variability for CT scan–based evaluation of posterior ligament complex injury in thoracolumbar fractures: an international multicenter pilot study. Global Spine J. 2020;10(2):118-129. doi: 10.1177/2192568219839414. [DOI] [PMC free article] [PubMed] [Google Scholar]