Abstract
Purpose
Radial dysplasia, also termed radial club hand is an abnormality along the longitudinal axis of the hand characterized by hypoplasia or aplasia of radial structures. Surgery that centralize the wrist on the distal end of the ulna gives quite good results in terms of anatomical recovery but affecting range of motion of the wrist and fingers, limbs length. We conducted this study to evaluate the outcome of serial casting followed by centralization at our institution.
Materials and methods
We conducted a prospective study involving 20 pediatric patients with 25 limbs affected by Bayne Types III and IV radial dysplasia, with an average follow-up period of 4.2 years. Each limb underwent progressive soft tissue stretching via serial casting, followed by centralization. Clinical and radio-graphic data were collected at surgery and during follow-up assessments.
Results
The study achieved an average correction of 60° in radial deviation, with a decrease in wrist range of motion from 79° to 28° over the follow-up period. Finger mobility showed increased stiffness. Ulnar length recovery reached 57% of the normal contra-lateral side. Final results, based on the Bayne and Klug criteria, revealed that 24 out of 25 hands (96%) exhibited good or satisfactory outcomes.
Conclusion
Early intervention employing gradual corrective casting followed by centralization is an effective treatment for radial dysplasia in children, consistently resulting in good or satisfactory outcomes. However, this approach entails a trade-off with reduced wrist and finger range of motion and potential implications for limb growth.
Keywords: Early treatment, Radial dysplasia, Range of motion, Centralization, Serial casting
1. Introduction
Radial dysplasia, also known as club hand, represents a congenital abnormality primarily affecting the longitudinal axis of the hand. It is characterized by the underdevelopment or absence of radial structures, including the radius, carpal bones, and the thumb. This condition is often accompanied by ulnar curvature, further accentuating the malformation and creating the illusion of a shortened forearm.
Numerous surgical approaches have been proposed by various authors to address radial dysplasia. Centralization of the hand and wrist to the distal ulna remains one of the widely practiced methods for its management.1 This technique enhances the anatomical alignment of the forearm. Nevertheless, it may result in limitations in wrist and finger mobility post-surgery, a concern highlighted in studies by Bayne,2 Saini,3 and Murphy.4
The potential for deformity recurrence following centralization surgery, as well as concerns about its impact on limb growth, has been raised by researchers such as Damore5 and Sestero.6 Notably, Bayne2 observed that children operated on before the age of 3 tend to have more favorable treatment outcomes compared to their older counterparts in his investigation.
Given the considerations mentioned above, we conducted an evaluation focused on children under the age of 3 with radial dysplasia who had undergone a combination of serial cast application and wrist centralization surgery at our institution.
2. Materials and methods
2.1. Setting and participants
This prospective study was carried out at our institution over the duration spanning from September 2016 to September 2023.
Throughout this investigation, comprehensive data were compiled from a cohort of 20 patients, encompassing a total of 25 affected limbs, all of which underwent a therapeutic regimen involving serial casting followed by centralization. Inclusion criteria for this study involved patients below 36 months of age who presented with Bayne type III and IV radial dysplasia. Notably, individuals exhibiting extension elbow contractures were excluded from the study, primarily due to the potential impairment they might face in bringing their hand to their mouth post-centralization.
2.2. Measurement
The clinical and radio-graphic aspects of congenital radial dysplasia cases in our study were meticulously documented both at the time of surgery and during subsequent follow-up examinations.
The clinical features encompassed pertinent patient demographics such as age, gender, the affected limbs, presence of thumb abnormalities, wrist range of motion, and the range of motion of individual fingers from the index to the little finger within the hand exhibiting radial dysplasia. The evaluation of finger movements (Passive Range of Motion) involved the individual assessment of each finger, considering the cumulative digital motion. This encompassed the combined movement at the metacarpophalangeal joint (MCP joint), proximal interphalangeal joint (PIP joint), and distal interphalangeal joint (DIP joint).
Radio-graphic assessments included anteroposterior and lateral forearm radiographs, where the hand and forearm were optimally positioned to maintain wrist alignment while avoiding excessive tension. Several radiographic parameters were employed for evaluation:
Ulnar Bowing (UB): This was quantified as the angle formed between a line perpendicular to the distal end of the ulna and a line perpendicular to the proximal end of the ulna on anteroposterior forearm imaging.
Ulna Length (UL): The ulna length was determined by a line connecting the midpoint of the distal head to the midpoint of the proximal ulna on a straight film. The ulna length on the unaffected side was also measured for comparison.
Hand Forearm Angle (HFA): This angle was calculated by measuring the angle formed by a line perpendicular to the distal ulna and the axis of the third metacarpal on anteroposterior imaging.
Family satisfaction with the treatment outcomes was assessed employing a modified SF-12 questionnaire (Table 1), comprising 12 tailored questions designed for parents to evaluate their contentment following operative intervention for radial dysplasia. If parents provided affirmative responses to six or more questions, their satisfaction with the treatment results was considered.
Table 1.
SF-12 modified questionnaire for parents of children with radial dysplasia.
| Question | Answer |
|---|---|
| 1/In general, how is the baby's health? | a/Excellent (Positive). |
| b/Very good (Positive). | |
| c/Good (Positive). | |
| d/Average | |
| e/Poor | |
| 2/How does the baby hold objects, movement limitation? | a/Extreme limitation. |
| b/Little Limitation (Positive) | |
| c/No limitation (Positive) | |
| 3/How often is the use of the hand with radial dysplasia? | a/Frequent usage (Positive) |
| b/Few or no usage | |
| 4/Regarding physical health: do you feel that your child is accomplishing less than you expect? | a/Yes |
| b/No (Positive) | |
| 5/In terms of physical health: do parents feel that the child's use of the affected limb helps the healthy limb more? (If your child has both limbs, skip this sentence.) | a/Yes (Positive) |
| b/No | |
| 6/In terms of mental health: do you feel your child is accomplishing less than you expect? | a/Yes |
| b/No (Positive) | |
| 7/Regarding mental health: do parents feel that children cry and fuss more? | a/Yes |
| b/No (Positive) | |
| 8/Do parents feel that the appearance of the baby's limbs is better? | a/Yes (Positive) |
| b/No | |
| 9/Do parents find other family members rated their appearance better after surgery? | a/Yes (Positive) |
| b/No | |
| 10/Do parents feel more comfortable about the child social development in the future? | a/Yes (Positive) |
| b/No | |
| 11/After surgery, do parents find that the baby becomes more active? | a/Yes (Positive) |
| b/No | |
| 12/Both physically and mentally: after the surgery do you feel your baby's future will be better after the treatment? | a/Agree (Positive) |
| b/Not agree |
Treatment outcomes were categorized into three groups in accordance with the criteria established by Bayne and Klug,2 which were as follows: good results, satisfactory results, and poor results, predicated on parameters including wrist range of motion, hand forearm angle, and family satisfaction. Furthermore, we conducted assessments to identify complications, including pin infections, broken pins, vascular issues, and nerve injuries.
3. Serial casting and operative technique
3.1. Casting method
For children under 2 months of age, families are provided with specific guidance. They are instructed to gently manipulate and stretch the wrists during routine activities such as diaper changes and feeding. This involves stretching the wrist into a straighter position without applying excessive tension or causing the baby distress. Continuous splinting is maintained until the child reaches the age of 2 months.
Once the child reaches 2 months of age or older, a series of long arm casts is utilized to facilitate the stretching of soft tissues along the radial side of the forearm. The casting process unfolds in three distinct stages:
In the initial stage, casting is applied to the fingers, excluding the thumb. Subsequently, the hand and wrist alignment is corrected and stabilized through casting. Importantly, care is taken to avoid overstretching. In the final stage, the cast is extended proximally along the forearm and elbow, with the elbow flexed at a ninety-degree angle. The cast is replaced and reshaped on a weekly basis until further correction is unattainable.
Following this casting regimen, the limb is maintained in a splint until the child reaches at least 6 months of age. At this juncture, the wrist centralization procedure is performed.
3.2. Operative technique
Palmar Incision: A longitudinal volar radial forearm skin incision is made to expose the robust volar fascia. The excision of this fascia is conducted with meticulous care to ensure the protection and exposure of critical structures, including the median nerve (a superficial palmar and radial structure that may be mistaken for tendons) and, when present, the radial artery (as illustrated in Fig. 1). The tendon of the flexor carpi radialis muscle is subsequently divided.
Fig. 1.
Intraoperative photographs. (A–B) Preoperative. (C–D) Exploration and protection of important structures such as the median nerve and extensor tendon compartments. (E–F) Follow-up photographs.
Dorsal Incision: An L-shaped skin incision is performed along the ulnar margin and the transverse skin fold at the wrist. This facilitates access to the extensor tendon compartments, with careful measures taken to safeguard these tendons. An incision in the ulno-carpal capsule along the distal ulna exposes the distal ulna. The carpal bones become visible on the palmar side of the distal ulna. A gradual release of tight soft tissue is executed until alignment of the carpal row with the distal ulna is achieved. On occasion, it becomes necessary to eliminate the proximal row of wrist bones (Fig. 2) or delicately remove a thin layer from the articular cartilage of the distal ulna. Subsequently, under C-arm guidance, the hand is secured above the distal ulna, carpal row, and 3rd metacarpal using a K-wire inserted through the 3rd metacarpal, traversing the carpus, and into the distal ulna. The K-wire then buried inside the 3rd metacarpal small incision.
Fig. 2.
Final X-ray follow-up.
In cases where the ulna exhibits a curvature exceeding 30°, an ulnar osteotomy is performed, which is stabilized using either the original K-wire or a secondary one. The extensor carpi radialis tendon is then transferred to the attachment point of the Extensor Carpi Ulnaris, and the Extensor Carpi Ulnaris tendon is shortened to enhance wrist stability. Subsequent steps involve suturing the joint capsule with nylon, suturing subcutaneous tissues, and closing the skin. The limb is immobilized in a splint with the elbow flexed at a 90-degree angle.
3.3. Post operative follow up
All patients were immobilized in a splint for a duration of 2 weeks. The removal of the K-wire was scheduled to take place 6 months post-surgery. Furthermore, the children were instructed to utilize a night brace until reaching skeletal maturity.
4. Results
Over an 84-month duration, spanning from September 2016 to September 2023, we conducted a study at our institution involving 20 children with a total of 25 limbs affected by radial dysplasia. All participants in this study were male. The median age at the time of the surgical intervention was 17.88 months, with an age range from 6 to 35 months. The mean follow-up period for these cases was 50.4 months, with a range between 26 and 84 months.
Among the affected limbs, there were 12 left (48%) and 13 right (52%) limbs with radial dysplasia. Additionally, five children exhibited bilateral radial dysplasia. Bayne Type IV radial dysplasia was more prevalent in this study, with 20 limbs affected, as opposed to Bayne Type III radial dysplasia, which affected 5 limbs. Notably, all children with radial hypoplasia exhibited concurrent thumb hypoplasia. A complete absence of the thumb (Blauth Type V) was observed in 56% of the cases (Table 2).
Table 2.
Characteristics of patients who underwent centralization at our institution in 2016–2023.
| Variables | Total, n(%) |
|---|---|
| Age, months | |
| <12 months | 8 (40) |
| 12–24 months | 5 (25) |
| 25–36 months | 7 (35) |
| Sex | |
| Male | 20 (100) |
| Female | 0 (0) |
| Side affected | |
| Left | 12 (48) |
| Right | 13 (52) |
| Bayne Classification | |
| Bayne IV | 20 (80) |
| Bayne III | 5 (20) |
| Thumb Hypoplasia | |
| Blauth I | 0 (0) |
| Blauth II | 0 (0) |
| Blauth IIIa | 1 (4) |
| Blauth IIIb | 6 (24) |
| Blauth IV | 4 (16) |
| Blauth V | 14 (56) |
It was observed that the radial digits exhibited greater stiffness compared to the ulnar digits. The range of motion in the fingers tended to decrease progressively from the index finger to the little finger after undergoing serial casting and surgical centralization. Furthermore, wrist range of motion decreased from 79° pre-surgery to 28° during post-operative follow-up (Table 3).
Table 3.
Wrist and finger range of motion before and after surgery.
| Range of motion (degrees) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Wrist | Before surgery | After surgery | ||||||
| 79 | 28 | |||||||
| Fingers | Index | Middle | Ring | Little | ||||
| Before | After | Before | After | Before | After | Before | After | |
| 117 | 109 | 138 | 127 | 162 | 149 | 186 | 177 | |
In our X-ray follow-up studies, we recorded ulnar length in the 15 unilateral cases during the final follow-up examination. Ulnar length on the affected side was found to be 57% of that observed in the normal, uninvolved, contralateral forearm. The hand forearm angle was reduced from 71° pre-surgery to 11° at the final follow-up, resulting in a total correction of 60°.
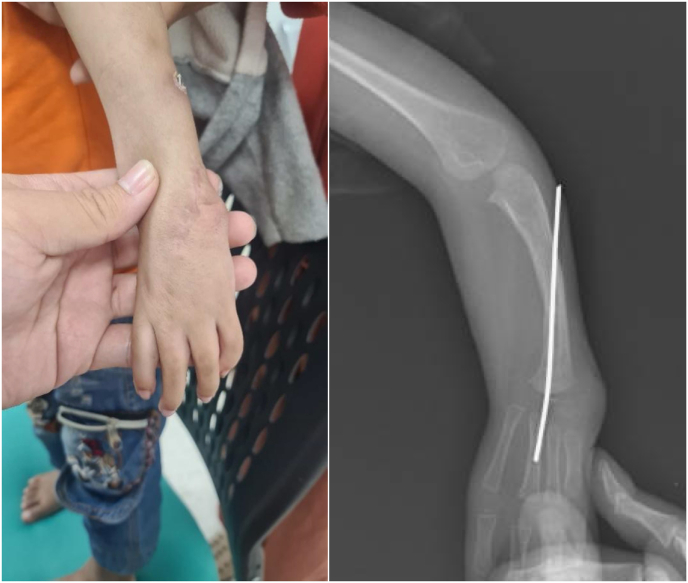
Among the 25 limbs, one case (4%) developed pressure ulcers due to the serial cast application. Notably, there were no cases of postoperative wound infections. Irritant dermatitis was observed in two limbs (8%). Additionally, three limbs (12%) experienced pin protrusion, which led to skin irritation (as shown in Fig. 3). No vascular complications were reported during the course of this study. Only one limb (4%) exhibited recurrent deformity after intervention and follow-up.
Fig. 3.
Nail protrusion complication.
Overall, the parents of the patients expressed their satisfaction with the treatment outcomes, as indicated by the modified SF-12 questionnaire. Ninety-six percent of the limbs were classified as either "good" or "satisfactory" based on the Bayne and Klug criteria, with 5 limbs falling into the "good" category and 19 limbs into the "satisfactory" category. Only one case was categorized as "poor" due to recurrent deformity (as depicted in Fig. 4).
Fig. 4.
Recurrence of the deformity in one patient.
5. Discussion
Pfister et al.7 studied 28 pediatric patients with radial dysplasia over 7 years (range 2–20 years). Their approach, which included soft tissue stretching with external fixation and wrist centralization using a permanent pin, showed improved HFA but necessitated 18 re-operations due to complications, ultimately leading to wrist joint fusion. Ekblom8 explored the impact of radial dysplasia on children's participation in daily life activities, emphasizing the importance of wrist and finger range of motion over radial deviation correction. She recommended avoiding wrist joint fusion and advocated for pin removal after some period to restore wrist mobility. In our study, removing pins after 6 months resulted in an average wrist range of motion of 28°, with five limbs exceeding 30°.
In our finger range of motion analysis, we observed a gradual increase from the index finger to the little finger, in line with Lamb9 and Saini's3 findings. Pre-surgery, the index finger had 117°, the middle finger 138°, the ring finger 162°, and the little finger 186°. After surgery, there was a slight reduction, with the index finger at 109°, the middle finger at 127°, the ring finger at 149°, and the little finger at 177°. While Bayne's study2 covering 64 pediatric patients undergoing wrist centralization surgery over 8.6 years reported no significant reduction in finger function, a more extended follow-up is essential to comprehensively assess post-operative outcomes.
The Hand Forearm Angle (HFA) is a crucial parameter in radial dysplasia treatment. In Kotwal's study,10 untreated cases saw an HFA increase from 66 to 85° over a 10-year period. In contrast, treated patients displayed substantial HFA reductions, as evident in short-term studies like Saini's.3 However, several long-term investigations, including Damore,5 Manske,11 and Vuillermin12, showed limited HFA improvement. This limited improvement could signify deformity recurrence, defined as HFA exceeding 30°, a common complication following wrist centralization.2 Our study identified only one case (4%) of recurrence, attributed to non-compliance with brace usage. In compliant cases, favorable outcomes were achieved. Recurrence may result from various factors, including surgical issues such as inadequate wrist axis correction, insufficient soft tissue release, early pin removal, and tendon force imbalances.2 Damore5 advocated pin removal after 8 weeks, similar to other authors.13,14 On the contrary, some studies, like Kotwal10 and Pfister,7 supported prolonged pin fixation to prevent deformity recurrence. Consistency in post-surgery brace use significantly helps prevent radial deviation deformity recurrence9 (Table 4).
Table 4.
Hand forearm angle in studies by various authors.
| Author | Time Follow up (year) | HFA (Initial) | HFA (Final) | The Difference |
|---|---|---|---|---|
| Damore5 | 6.5 | 83 | 63 | 20 |
| Saini3 | 2 | 61 | 7 | 54 |
| Manske11* | 6 | 53 | 36 | 17 |
| Manske11** | 10 | 53 | 27 | 26 |
| Vuillermin12 | 9.2 | 88 | 64 | 24 |
| Pfister7 | 7 | 76 | 12 | 64 |
| Kotwal10* | 10.1 | 66 | 85 | −19 |
| Kotwal10** | 11.1 | 63 | 12 | 49 |
| Our study | 4.2 | 71 | 11 | 60 |
Manske*: The group had soft tissue stretching before centralization.
Manske**: The team only centralizes, not stretches the soft tissue.
Kotwal*: Group without surgical intervention.
Kotwal**: Group with surgical intervention.
Limb length is vital in radial dysplasia assessment. In affected limbs, the ulnar length typically reaches 60–65% of the standard ulnar length.15 However, centralization surgery can further reduce limb length, as the ulna grows to only about 48–58% of its standard length due to physis damage during surgery. Vilkki16 employed vascularized 2nd toe metatarsal and proximal phalanx as a pillar to support the radial carpus bone to minimize the possibility of recurrence and maximize the growth of the limb without crossing the physis. The results of long-term follow-up for 11 years showed that ulna length was 67% of the unaffected contralateral limb. Yang17 described 4 cases treated by vascularized fibula transfer and these limbs demonstrated 67.9% of the contralateral limb length. Sestero6 found that in the group without surgical intervention, ulnar length could potentially reach 64% of the standard ulnar length, while the centralization group only achieved 58% of the normal ulnar length. This indicates that wrist centralization surgery can restore limb axis alignment but raises concerns about the ulna's longitudinal growth. In our 15 cases, the ulnar length at the last follow-up measured 57% of the unaffected limb, aligning with Sestero's findings. The surgical intervention for wrist centralization and joint stabilization with a pin crossing the physis likely impacted ulnar longitudinal growth.
In Bayne's extensive case series,2 outcomes were distributed with 21 cases showing good results, 22 cases with satisfactory results, and 10 cases with poor results. An important finding in Bayne's study was the relationship between the timing of surgery and outcomes. Notably, 53% of patients who underwent surgery before the age of 3 achieved good results, while only 24% achieved good results when surgery was performed on children older than 3 years. Saini3 reported treating 18 limbs (17 patients) with radial dysplasia, with patients having an average age of 11 months (ranging from 20 days to 24 months). They were followed for an average of 2 years. The treatment approach involved a combination of casting and external immobilization frames to facilitate soft tissue stretching before surgical wrist centralization. Impressively, 89% of the patients achieved good or satisfactory results in this study, assessed according to Bayne and Klug criteria. In our study, the majority of children, around 76%, were classified as achieving satisfactory results, primarily due to residual wrist stiffness. This may be attributed to the relatively short follow-up period. Interestingly, our combined proportion of good and satisfactory results exceeded those reported by Bayne and Saini. However, this difference could be associated with the critical factor that all children in our study received intervention and surgery before the age of 3. Importantly, our case series did include one case of unfavorable treatment outcome, attributed to deformity recurrence after 37 months of follow-up, mainly due to the patient's non-compliance with our prescribed night brace protocol following longitudinal stabilizing pin removal.
Regarding complications, Bayne2 noted that roughly 6.9% of cases in their study developed skin infections. Fortunately, all these infections responded well to antibiotic treatment, eliminating the need for premature pin removal. In one case, an exceptionally short ulna was linked to distal physeal damage resulting from the use of a large pin. Another case involved compromised vascularity, requiring reoperation to slightly reposition the limb for successful revascularization. In Saini's study,3 approximately 37% of the 18 cases experienced postoperative swelling, and one case (5%) had a postoperative infection. Moreover, 26% of the limbs encountered issues with pin migration and skin irritation. One instance of pin infection was noted, but fortunately, vascular complications were absent in this series. Kanojia18 reported a series of wrist centralization cases involving 14 patients and 18 limbs, with no documented complications, including vascular injuries, recurrent deformity, or infections. However, Vikki16 documented three cases of microvascular failure in their series. Qazi,19 who utilized bilobed and Z-shaped flaps in his series (comprising 9 patients and 12 limbs), recorded a single case (8.3%) with Z-flap-related margin necrosis. The relatively minimal complications in our study can be attributed in part to the simplicity of our incisions. Importantly, the documented complications were effectively addressed without major implications. Our surgical method proves effective in reducing the potential complication of skin margin necrosis by avoiding the use of skin flaps. The volar incision strategy used in our study safeguards the median nerve while relieving tension in tight volar structures, especially the flexor carpi radialis.
Our study has several clinical implications. Firstly, our exclusive focus on children under 3 years old resulted in most achieving favorable outcomes, emphasizing the potential benefits of early interventions for radial dysplasia during childhood. Secondly, the problem of limited mobility of the fingers before and after surgery was demonstrated. The early wrist stiffness associated with a stable correction post-op may change with growth. It is possible that increased wrist mobility over time will be associated with some degree of recurrence of deformity. Lastly, our surgical approach offers advantages in protecting median nerves and preventing complications related to flap necrosis.
However, our study is limited by the small number of participants, given the rarity of types III and IV radial deficiencies in the Vietnamese population. These promising results should encourage further, extensive, and long-term investigations into this treatment and the condition itself.
6. Conclusion
Early treatment of radial dysplasia in children through the progressive application of serial casting followed by centralization is a viable treatment method. This approach consistently yields good or satisfactory results in terms of realigning hand anatomy, contingent upon patient compliance with postoperative brace wear. However, this method may potentially compromise wrist and finger range of motion and limb growth.
CRediT author statement
Phi Duong Nguyen, MD (Contribution: performed measurements, manuscript preparation).
Tuong Trong Mai, MD (Contribution: study design, take part in surgery).
Terry Richard Light, Prof (Conribution: Language editor, take part in surgery).
References
- 1.Adrian F. CV Mosby Company; 1977. The Care if Congenital Hand Anomalies; pp. 286–327. [Google Scholar]
- 2.Bayne L.G., Klug M.S. Long-term review of the surgical treatment of radial deficiencies. J Hand Surg Am. 1987;12(2):169–179. doi: 10.1016/s0363-5023(87)80267-8. [DOI] [PubMed] [Google Scholar]
- 3.Saini N., Patni P., Gupta S., Chaudhary L., Sharma V. Management of radial clubhand with gradual distraction followed by centralization. Indian J Orthop. 2009;43(3):292–300. doi: 10.4103/0019-5413.53461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy G.R.F., Logan M.P.O., Smith G., Sivakumar B. Correction of "wrist" deformity in radial dysplasia: a systematic review and meta-analysis. J Bone Joint Surg Am. 2017;99(24):2120–2126. doi: 10.2106/JBJS.17.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Damore E., Kozin S.H., Thoder J.J., Porter S. The recurrence of deformity after surgical centralization for radial clubhand. J Hand Surg Am. 2000;25(4):745–751. doi: 10.1053/jhsu.2000.6460. [DOI] [PubMed] [Google Scholar]
- 6.Sestero A.M., Van Heest A., Agel J. Ulnar growth patterns in radial longitudinal deficiency. J Hand Surg Am. 2006;31(6):960–967. doi: 10.1016/j.jhsa.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 7.Pfister G., Le Hanneur M., Bachy M., Fitoussi F. Radial club hand treated with soft-tissue distraction and subsequent pin stabilization: mid- to long-term results. J Hand Surg Eur. 2020;45(7):729–736. doi: 10.1177/1753193420916694. [DOI] [PubMed] [Google Scholar]
- 8.Ekblom A.G., Dahlin L.B., Rosberg H.E., Wiig M., Werner M., Arner M. Hand function in children with radial longitudinal deficiency. BMC Muscoskel Disord. 2013;14:116. doi: 10.1186/1471-2474-14-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lamb D.W. Radial club hand. A continuing study of sixty-eight patients with one hundred and seventeen club hands. J Bone Joint Surg Am. 1977;59(1):1–13. [PubMed] [Google Scholar]
- 10.Kotwal P.P., Varshney M.K., Soral A. Comparison of surgical treatment and nonoperative management for radial longitudinal deficiency. J Hand Surg Eur. 2012;37(2):161–169. doi: 10.1177/1753193411413070. [DOI] [PubMed] [Google Scholar]
- 11.Manske M.C., Wall L.B., Steffen J.A., Goldfarb C.A. The effect of soft tissue distraction on deformity recurrence after centralization for radial longitudinal deficiency. J Hand Surg Am. 2014;39(5):895–901. doi: 10.1016/j.jhsa.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 12.Vuillermin C., Wall L., Mills J., et al. Soft tissue release and bilobed flap for severe radial longitudinal deficiency. J Hand Surg Am. 2015;40(5):894–899. doi: 10.1016/j.jhsa.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Bora F.W., Jr. Osterman AL, Kaneda RR, Esterhai J. Radial club-hand deformity. Long-term follow-up. J Bone Joint Surg Am. 1981;63(5):741–745. [PubMed] [Google Scholar]
- 14.Buck-Gramcko D. Radialization as a new treatment for radial club hand. J Hand Surg Am. 1985;10(6 Pt 2):964–968. doi: 10.1016/s0363-5023(85)80013-7. [DOI] [PubMed] [Google Scholar]
- 15.Mehta R., Ghanghurde B.A., Shah I.P., Thatte M. Long-term follow-up of ulnar growth in radial dysplasia treated by a combination of distraction and radialization. J Hand Surg Am. 2023;48(7) doi: 10.1016/j.jhsa.2022.01.025. 738 e1- e8. [DOI] [PubMed] [Google Scholar]
- 16.Vilkki S.K. Vascularized metatarsophalangeal joint transfer for radial hypoplasia. Semin Plast Surg. 2008;22(3):195–212. doi: 10.1055/s-2008-1081403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang J., Qin B., Li P., Fu G., Xiang J., Gu L. Vascularized proximal fibular epiphyseal transfer for Bayne and Klug type III radial longitudinal deficiency in children. Plast Reconstr Surg. 2015;135(1) doi: 10.1097/PRS.0000000000000836. 157e-66e. [DOI] [PubMed] [Google Scholar]
- 18.Kanojia R.K., Sharma N., Kapoor S.K. Preliminary soft tissue distraction using external fixator in radial club hand. J Hand Surg Eur. 2008;33(5):622–627. doi: 10.1177/1753193408093809. [DOI] [PubMed] [Google Scholar]
- 19.Qazi U.A., Rehman Orakzai I.U., Rashid M. The bilobed flap - a better option for soft tissue release in the management of Radial Club Hand. J Pakistan Med Assoc. 2017;67(5):698–700. [PubMed] [Google Scholar]