This systematic review and meta-analysis characterizes digital health interventions for reducing hypertension and assesses the association of these interventions with blood pressure changes in adults experiencing health disparities.
Key Points
Question
Are digital health interventions associated with reducing blood pressure (BP) levels in US populations experiencing health disparities, and what types of tailored modalities have been used to manage hypertension in demographically and socioeconomically diverse subgroups?
Findings
In this systematic review and meta-analysis of 28 studies, patients with health disparities receiving a digital health intervention compared with standard care had greater reductions in systolic BP at 6 and 12 months. Most studies involved multicomponent interventions, primarily remote BP monitoring.
Meaning
These findings suggest that digital health interventions are associated with improved BP levels in populations experiencing health disparities.
Abstract
Importance
Hypertension remains a leading factor associated with cardiovascular disease, and demographic and socioeconomic disparities in blood pressure (BP) control persist. While advances in digital health technologies have increased individuals’ access to care for hypertension, few studies have analyzed the use of digital health interventions in vulnerable populations.
Objective
To assess the association between digital health interventions and changes in BP and to characterize tailored strategies for populations experiencing health disparities.
Data Sources
In this systematic review and meta-analysis, a systematic search identified studies evaluating digital health interventions for BP management in the Cochrane Library, Ovid Embase, Google Scholar, Ovid MEDLINE, PubMed, Scopus, and Web of Science databases from inception until October 30, 2023.
Study Selection
Included studies were randomized clinical trials or cohort studies that investigated digital health interventions for managing hypertension in adults; presented change in systolic BP (SBP) or baseline and follow-up SBP levels; and emphasized social determinants of health and/or health disparities, including a focus on marginalized populations that have historically been underserved or digital health interventions that were culturally or linguistically tailored to a population with health disparities. The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline.
Data Extraction and Synthesis
Two reviewers extracted and verified data. Mean differences in BP between treatment and control groups were analyzed using a random-effects model.
Main Outcomes and Measures
Primary outcomes included mean differences (95% CIs) in SBP and diastolic BP (DBP) from baseline to 6 and 12 months of follow-up between digital health intervention and control groups. Shorter- and longer-term follow-up durations were also assessed, and sensitivity analyses accounted for baseline BP levels.
Results
A total of 28 studies (representing 8257 participants) were included (overall mean participant age, 57.4 years [range, 46-71 years]; 4962 [60.1%], female). Most studies examined multicomponent digital health interventions incorporating remote BP monitoring (18 [64.3%]), community health workers or skilled nurses (13 [46.4%]), and/or cultural tailoring (21 [75.0%]). Sociodemographic characteristics were similar between intervention and control groups. Between the intervention and control groups, there were statistically significant mean differences in SBP at 6 months (−4.24 mm Hg; 95% CI, −7.33 to −1.14 mm Hg; P = .01) and SBP changes at 12 months (−4.30 mm Hg; 95% CI, −8.38 to −0.23 mm Hg; P = .04). Few studies (4 [14.3%]) reported BP changes and hypertension control beyond 1 year.
Conclusions and Relevance
In this systematic review and meta-analysis of digital health interventions for hypertension management in populations experiencing health disparities, BP reductions were greater in the intervention groups compared with the standard care groups. The findings suggest that tailored initiatives that leverage digital health may have the potential to advance equity in hypertension outcomes.
Introduction
Hypertension is an important risk factor for cardiovascular disease (CVD), which accounts for approximately 1 in 5 deaths in the US.1 Nearly half (47%) of all US adults, or 116 million individuals, have hypertension (defined as systolic blood pressure [SBP]≥130 mm Hg or diastolic blood pressure [DBP]≥80 mm Hg). Only 24% of those with hypertension have their condition under control.2,3 Racial, ethnic, and socioeconomic disparities in hypertension prevalence, awareness, and treatment persist. Notably, population-based studies have shown that Black and Hispanic adults have lower BP awareness and control despite a higher overall burden of hypertension compared with non-Hispanic White individuals.4,5,6,7,8
Emerging research has shown digital health technology to be a promising avenue for managing uncontrolled hypertension, particularly in underserved populations impacted by barriers to accessing care. Current digital health approaches for hypertension management typically involve text message reminders for medication adherence,9,10,11 remote BP monitoring,12,13 and virtual behavioral coaching.14,15 There is also growing evidence for the value of tailored, multicomponent approaches for hypertension management.16,17 Home monitoring can identify “white-coat hypertension” (BP measurements are high in the clinic but normal at home) and masked hypertension (BP measurements are normal in the clinic but high at home) and empower patients to take more control over their health.12,18 When combined with a centralized medical team to respond to elevated home BP readings, home monitoring has potential to significantly improve BP control. Despite the intended benefits of home monitoring and other digital health interventions for hypertension control, there are varying effects on cardiovascular risk factor control, potentially because of the need for technology support and remote engagement.19,20,21,22 Studies that incorporate a social determinants of health framework in the development and implementation of digital health interventions could prevent further widening of the digital divide and existing health disparities.23
Accordingly, this systematic review and meta-analysis aimed to assess the association between digital health interventions and BP changes among populations experiencing health disparities. It also aimed to characterize the diversity of contemporary strategies used to meet the needs of populations experiencing health disparities.
Methods
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline.24 The study protocol and methods were registered with PROSPERO a priori (CRD42021257529).
Search Strategy and Study Selection
A systematic search of the literature was conducted by a medical librarian (A.A.G.) in the Cochrane Library, Ovid Embase, Google Scholar, Ovid MEDLINE, PubMed, Scopus, and Web of Science Core Collection databases to identify relevant articles published from the earliest record in the respective database to October 30, 2023. Databases were searched using a combination of controlled vocabulary and free-text terms for digital health, hypertension, social determinants of health, and demographic and/or socioeconomic disparities. The search was not limited by publication type, language, or year. The search was peer reviewed by a second medical librarian using Peer Review of Electronic Search Strategies. Details of the full search strategy are listed in eTable 1 in Supplement 1. CitationChaser was used to search the reference lists of included studies and to retrieve articles that had cited the included studies to find additional relevant studies not retrieved by the database search.
Included studies were randomized clinical trials (RCTs) or cohort studies that investigated digital health interventions for managing hypertension and were conducted in adult populations (age ≥18 years). Studies were not excluded based on the type of digital health intervention used. Included studies presented change in SBP and/or baseline and follow-up SBP levels as primary or secondary outcomes. Studies were excluded if they possessed the following characteristics: review articles, abstracts, editorials or letters, animal studies, or case reports. Conference abstracts were excluded given that detailed information was required on follow-up BP levels, participants’ sociodemographic characteristics, and an in-depth description of the digital health intervention being assessed.
Additionally, given the objective of this systematic review and meta-analysis to assess the outcomes of digital health interventions in populations experiencing health disparities, the studies that were included at the full-text review stage were required to possess any of the following characteristics: (1) a clear emphasis on social determinants of health and/or health disparities, (2) study eligibility criteria focusing on the exclusive or predominant recruitment and enrollment of marginalized populations that have historically been underserved and underrepresented in medical and public health research, (3) study design and conduct approaches involving intentional community partnership and stakeholder engagement, and (4) digital health intervention strategies that were culturally and/or linguistically tailored to the populations they were meant to serve. It was not feasible to include these criteria as part of the first stage of eligibility determination because this information is frequently not included in a study’s title or abstract, thereby necessitating full review of the methods and results.
Citations from all databases were imported into an EndNote 20 library (Clarivate Analytics). Duplicate citations were removed using the Yale Reference Deduplicator. The deduplicated results were imported into Covidence for screening and data extraction. Two independent screeners (M.E.K., R.M.) performed a title and abstract review, and a third screener (E.S.S.) resolved disagreements. The full texts of the resulting studies were then reviewed for inclusion by 2 independent screeners (M.E.K., R.M.), with a third screener (E.S.S.) resolving disagreements.
Statistical Analysis
Data Extraction and Analysis
Data were extracted and verified by 2 authors (M.E.K., R.M.). These data consisted of study characteristics including the following: study design (RCTs or cohort studies), study type (eg, pilot study status), study duration and location, type of digital health intervention(s), population characteristics and eligibility criteria, primary and secondary outcome measures, and type or level of cultural tailoring and community engagement. Additionally, we reported means and SDs or frequencies and proportions for the following sociodemographic characteristics for each study: age, sex, race and ethnicity (categories included non-Hispanic Black, non-Hispanic White, Hispanic, and other race [Asian and multiracial]), income, level of completed education, and insurance status and type. The outcomes of interest included baseline and follow-up SBP and DBP levels (in mm Hg) at 3, 6, 12, 18, or 24 months and SBP and DBP changes from baseline. In studies that either did not report the SD value for the BP outcomes or reported IQR or SE values instead, we used several algebraic conversions to produce the proper SD measure of variation to integrate into our meta-analysis.25
The methods of the meta-analysis were established prior to data extraction. Mean differences in BP between treatment and control groups were analyzed with random-effects meta-analysis using the restricted maximum likelihood method. Analysis was stratified by follow-up duration in months. Study heterogeneity was evaluated using Higgins I2 statistics with thresholds of 25%, 50%, and 75%, corresponding with low, moderate, and high levels of heterogeneity, respectively.25 If the I2 value was 50% or greater, we explored heterogeneity using leave-one-out sensitivity analysis, subgroup analysis, and metaregression for outcomes with at least 10 studies. Subgroups included studies that tested remote BP monitoring in the intervention arm, focused on Black or Hispanic individuals, were pilot studies, identified BP as the primary outcome, and were limited to patients with controlled BP at baseline. Metaregression included the same subgroup variables and the proportion of study participants who were female, were Black or Hispanic, and/or had a lower level of completed education. Statistical analysis was performed using Stata/BE, version 17.0 (StataCorp LLC). Two-sided P < .05 was considered significant.
Assessment of Study Quality and Publication Bias
The quality of observational studies was assessed independently by 2 investigators (M.E.K., R.M.) and scored on the Newcastle-Ottawa Scale, and interobserver agreement was calculated using the Cohen k coefficient.26 Discrepancies were resolved by the senior reviewer (E.S.S.). Publication bias was assessed visually by inspection of a funnel plot and through the Egger test of intercept.27
Results
Study Characteristics
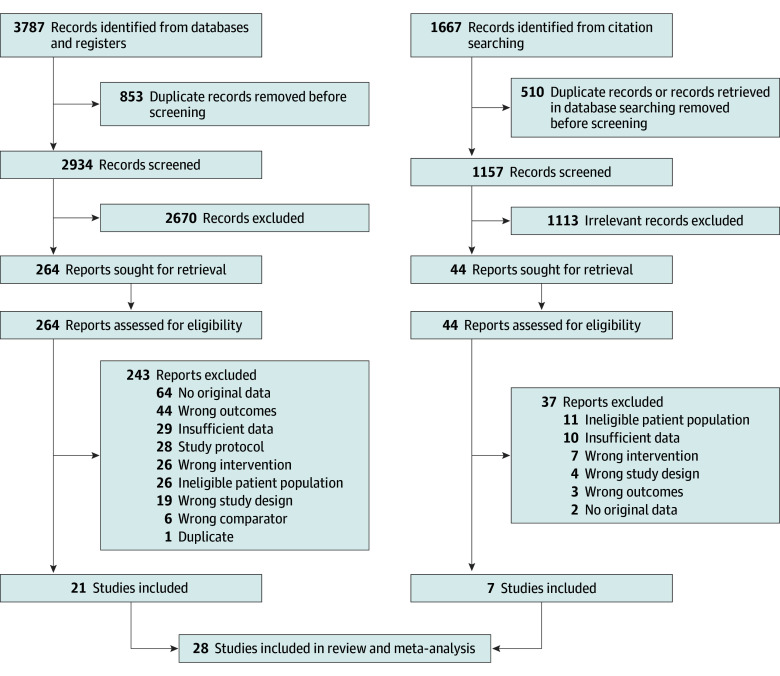
Our initial literature search yielded 4091 studies after removing duplicate publications (Figure 1). Of these, 308 full-text articles were evaluated, and 28 studies28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55 (27 RCTs [96.4%]29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55 and 1 cohort study [3.6%]28) were ultimately included in this systematic review and meta-analysis (Table 1 and Table 2). Among the included studies, the eligibility criteria for participant recruitment varied widely, although most used a diagnosis of hypertension and/or a history of taking antihypertensive medications (eTable 2 in Supplement 1).28,30,31,32,33,36,37,41,42,43,44,46,47,48,49,50,51,52,53,54 Eighteen studies (64.3%) included remote BP monitoring,28,30,31,32,33,34,37,41,43,44,46,48,49,51,52,53,54,55 and all studies incorporated multiple digital health components, including electronic health reminders, education, and behavioral support programs. Other interventions included the integration of community health workers (CHWs) or skilled nurses (13 studies [46.4%]28,29,32,34,35,36,38,40,41,43,45,46,53), wearable or ingestible sensors (4 studies [14.3%]40,43,50,54), and tailored messaging or reminders based on cultural, linguistic, behavioral, and/or psychosocial considerations (21 studies [75.0%]29,31,32,33,34,35,36,38,39,40,41,42,43,45,46,47,48,52,53,54,55) (eTable 3 in Supplement 1). Additionally, 5 studies (17.9%) directly involved active medication management for hypertension control as part of the digital health intervention.28,35,41,43,48 Studies excluded from this systematic review and meta-analysis and the corresponding rationales are presented in eTables 4 and 5 in Supplement 1. Few studies (4 [14.3%]) reported the BP outcomes of interest beyond 1 year of follow-up.
Figure 1. Flowchart Depicting Study Methods in Accordance With the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Guideline.
Table 1. Study Characteristics and Participant Information for the 28 Included Studies Meeting Eligibility Criteria.
| Author, yeara | Pilot study | Study population | Focus on disparities | Follow-up, mo | Remote monitoring | Study location |
|---|---|---|---|---|---|---|
| Naqvi et al,41 2022 | Yes | Individuals with an acute ischemic or hemorrhagic stroke discharged after hospitalization with HTN | Involved a clinical site primarily serving a Hispanic, low-income community | 3 | Yes | Northern Manhattan, New York |
| Brewer et al,40 2022 | Yes | Black or African American individuals able to engage in moderate physical activity | Focused on Black or African American individuals | 6 | No | Rochester and Minneapolis–St Paul, Minnesota |
| Clark et al,28 2021 | No | Individuals with uncontrolled HTN | Focused on a predominately rural and low-income population | 6 | Yes | Mississippi |
| Schoenthaler et al,42 2020 | Yes | Black or African American patients with uncontrolled HTN and/or diabetes | Focused on Black or African American individuals | 3 | No | New York, New York |
| Vaughan et al,35 2021 | No | Hispanic, Spanish-speaking individuals with diabetes without insurance earning ≤250% of the federal poverty level | Focused on Hispanic individuals with a low income and no health insurance | 6 | No | Houston, Texas |
| Zha et al,43 2020 | Yes | Individuals with uncontrolled HTN taking anti-HTN medications and living in public housing units | Focused on individuals living in public housing units | 6 | Yes | Newark, New Jersey |
| Schroeder et al,31 2020 | No | Individuals with HTN | Focused on multiple racial and ethnic groups receiving care at an Urban Indian Health Organization | 12 | Yes | Albuquerque, New Mexico |
| Still et al,32 2020 | Yes | African American individuals with HTN prescribed anti-HTN medications | Focused on Black or African American individuals | 3 | Yes | Cleveland, Ohio |
| Persell et al,44 2020 | No | Individuals with HTN | Included a large proportion of Black or African American individuals | 6 | Yes | Chicago, Illinois |
| Tuot et al,45 2019 | Yes | Individuals with CKD with recent clinical visit(s) | Focused on individuals with low income receiving care at safety-net clinics; intervention was language concordant and culturally tailored | 12 | No | San Francisco, California |
| Chandler et al,46 2019 | No | Hispanic individuals with HTN and prescribed anti-HTN medications | Focused on Hispanic individuals | 9 | Yes | Charleston County, South Carolina |
| Bennett et al,47 2018 | No | Individuals with HTN, obesity, diabetes, and hyperlipidemia | Focused on socioeconomically disadvantaged primary care patients | 12 | No | Central North Carolina |
| Bosworth et al,48 2018 | No | Veterans enrolled at 1 of 3 primary care clinics with HTN or hypercholesterolemia | Focused on US veterans | 12 | Yes | North Carolina and Virginia |
| Skolarus et al,33 2018 | Yes | Individuals with HTN | Used a community-based participatory research framework and focused on Black or African American individuals | 6 | Yes | Flint, Michigan |
| Morawski et al,49 2018 | No | Individuals with HTN on anti-HTN medications | Included a large proportion of Black or African American individuals | 3 | Yes | Not indicated or unclear |
| Fortmann et al,29 2017 | No | Uninsured or underinsured Hispanic individuals with diabetes | Focused on Hispanic individuals with minimal or no health insurance | 6 | No | San Diego and Riverside, California |
| Frias et al,50 2017 | Yes | Individuals with uncontrolled HTN and diabetes with previously failed HTN treatment | Included a large proportion of Hispanic individuals and those with low income | 3 | No | California and Colorado |
| Bove et al,37 2013 | No | Individuals with HTN | Conducted in an underserved, urban community and included a large proportion of Black or African American individuals | 6 | Yes | Philadelphia, Pennsylvania, and Wilmington, Delaware |
| Crowley et al,34 2013 | No | Black individuals with diabetes with recent clinical visit(s) | Focused on Black or African American individuals | 12 | Yes | Durham, North Carolina |
| Rifkin et al,51 2013 | No | Individuals with stage 3 CKD and established HTN attending a VA clinic | Conducted among older veterans | 6 | Yes | San Diego, California |
| Margolis et al,30 2013 | No | Individuals with uncontrolled HTN | Included a large proportion of individuals with low income | 12 | Yes | Minneapolis–St Paul, Minnesota |
| Bennett et al,36 2012 | No | Individuals with a BMI of 30-50, weighing <180 kg, taking anti-HTN medications, and with recent clinical visit(s) | Focused on socioeconomically disadvantaged individuals with a large proportion of Black or African American individuals | 24 | No | Boston, Massachusetts |
| McKee et al,52 2011 | Yes | Individuals with HTN receiving care for diabetes | Tailored intervention to a multiethnic, low-income, primary care population | 6 | Yes | Bronx, New York |
| Frosch et al,38 2011 | No | Individuals with diabetes with recent clinical visit(s) | Focused on low-income, uninsured, and ethnically diverse patients | 6 | No | Los Angeles, California |
| Anderson et al,39 2010 | No | Individuals with diabetes with recent clinical visit(s) | Tailored intervention to meet the cultural and linguistic needs of an underserved, predominantly Hispanic population | 12 | No | Connecticut |
| Brennan et al,53 2010 | No | Black individuals with HTN and a PCP | Focused on Black or African American individuals | 12 | Yes | Not indicated or unclear |
| Bosworth et al,54 2009 | No | Individuals with HTN taking anti-HTN medications and residing in specific zip codes with an upcoming PCP appointment | Tailored intervention to patients’ literacy and social support among a large proportion of Black or African American individuals | 24 | Yes | North Carolina |
| Shea et al,55 2009 | No | Medicare beneficiaries with diabetes | Focused on Medicare beneficiaries living in a medically underserved area | 12 | Yes | New York |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CKD, chronic kidney disease; HTN, hypertension; PCP, primary care physician; VA, US Department of Veterans Affairs.
All included studies were randomized clinical trials except for Clark et al,28 which was a prospective cohort study.
Table 2. Specific Information on the Digital Health Intervention Components Used for the 28 Included Studies Meeting the Eligibility Criteria.
| Study | Digital health intervention component |
|---|---|
| Naqvi et al,41 2022 |
|
| Brewer et al,40 2022 |
|
| Clark et al,28 2021 |
|
| Schoenthaler et al,42 2020 |
|
| Vaughan et al,35 2020 |
|
| Zha et al,43 2020 |
|
| Schroeder et al,31 2020 |
|
| Still et al,32 2020 |
|
| Persell et al,44 2020 |
|
| Tuot et al,45 2019 |
|
| Chandler et al,46 2019 |
|
| Bennett et al,47 2018 |
|
| Bosworth et al,48 2018 |
|
| Skolarus et al,33 2018 |
|
| Morawski et al,49 2018 |
|
| Fortmann et al,29 2017 |
|
| Frias et al,50 2017 |
|
| Bove et al,37 2013 |
|
| Crowley et al,34 2013 |
|
| Rifkin et al,51 2013 |
|
| Margolis et al,30 2013 |
|
| Bennett et al,36 2012 |
|
| McKee et al,52 2011 |
|
| Frosch et al,38 2011 |
|
| Anderson et al,39 2010 |
|
| Brennan et al,53 2010 |
|
| Bosworth et al,54 2009 |
|
| Shea et al,55 2009 |
|
Abbreviations: BP, blood pressure; CHW, community health worker; CKD, chronic kidney disease; FAITH!, Fostering African American Improvement in Total Health; FNCH, First Nations Community Healthsource; SMS, short message service.
Baseline Sociodemographic Characteristics
Overall, 8257 individuals from the 28 studies were included in this systematic review and meta-analysis, of whom 3828 (46.4%) were assigned to an intervention group and 4429 (53.6%) were assigned to a control group. The mean pooled age of participants was 57.4 years (range, 46-71 years); 3295 (39.9%) were men, and 4962 (60.1%) were women (eTable 3 in Supplement 1). Overall, 1631 individuals (19.8%) were Hispanic; 3531 (42.8%), non-Hispanic Black; 2607 (31.6%), non-Hispanic White; and 488 (5.9%), other race. Regarding socioeconomic characteristics, 1471 individuals (17.8%) had a low level of completed education (often defined as less than high school), and 1884 (22.8%) were classified as having low income. Additionally, 1177 individuals (14.3%) had Medicaid, 2146 (26.0%) had Medicare, and 548 (6.6%) had no insurance coverage. In total, 17 studies (60.7%) focused on Black or Hispanic individuals or included a large proportion of individuals self-identifying as Black or Hispanic.29,32,33,34,35,36,37,39,40,41,42,44,46,49,50,53,54 Regarding socioeconomic characteristics, 15 studies (53.6%) were specifically conducted in socioeconomically disadvantaged communities or among individuals with a low income or who were uninsured or underinsured.28,29,30,35,36,37,38,39,41,43,45,47,50,52,55 Several studies were also conducted among veterans (2 [7.1%]48,51) and rural populations (3 [10.7%]28,47,54).
SBP Changes
Across all studies included in the meta-analysis regardless of follow-up duration, the mean (SD) SBP at baseline for the digital health intervention and control groups was 138.6 (16.3) mm Hg and 139.2 (16.2) mm Hg, respectively. The mean (SD) follow-up SBP at the final follow-up time point was 131.8 (15.9) mm Hg in the intervention groups and 135.3 (16.5) mm Hg in the control groups.
Among the 10 studies that reported change in SBP at 6 months,28,30,31,33,36,37,40,44,47,51 we found a mean difference of −2.74 mm Hg (95% CI, −6.43 to 0.95 mm Hg; P = .15; I2 = 80.32%) between the digital health intervention and control groups (Figure 2). At 12 months’ follow-up, there was a statistically significant mean difference of −4.30 mm Hg (95% CI, −8.38 to −0.23 mm Hg; P = .04; I2 = 71.43%) in the 4 studies reporting SBP change.30,31,36,47 For the SBP change outcome, 3 or fewer studies had complete information at the 3-month,41,49,50 18-month,30,36 and 24-month36 follow-up. Among the 12 studies that presented follow-up SBP, we found a statistically significant mean difference of −4.24 mm Hg (95% CI, −7.33 to −1.14 mm Hg; P = .01; I2 = 77.36%) at 6 months (Figure 3).28,29,30,31,33,35,38,40,43,44,51,52 The greatest mean difference in 6-month SBP between intervention and control groups was −13.70 mm Hg (95% CI, −16.62 to −10.78 mm Hg),28 while the smallest (most positive) mean difference was 1.90 mm Hg (95% CI, −4.66 to 8.46 mm Hg).29
Figure 2. Differences in Systolic Blood Pressure (SBP) Changes From Baseline to Follow-Up Time Points Between Digital Health Intervention and Control Groups.
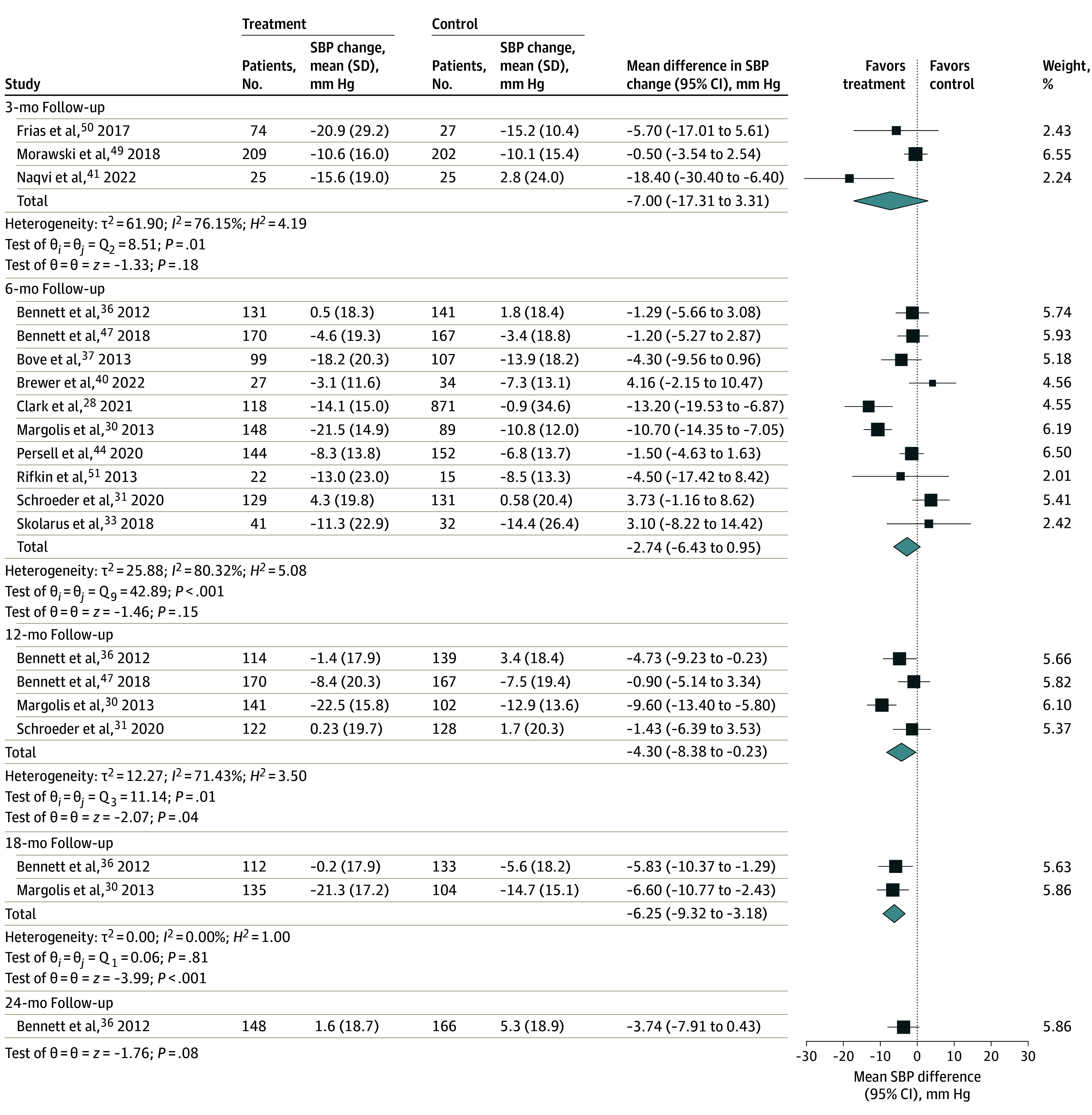
Random-effects restricted maximum likelihood model. Squares indicate mean SBPs, with horizontal lines indicating 95% CIs and the size of the squares representing weight; diamonds indicate pooled estimates, with outer points of the diamonds indicating 95% CIs.
Figure 3. Differences in Follow-Up Systolic Blood Pressure (SBP) Between Digital Health Intervention and Control Groups at Different Time Points.
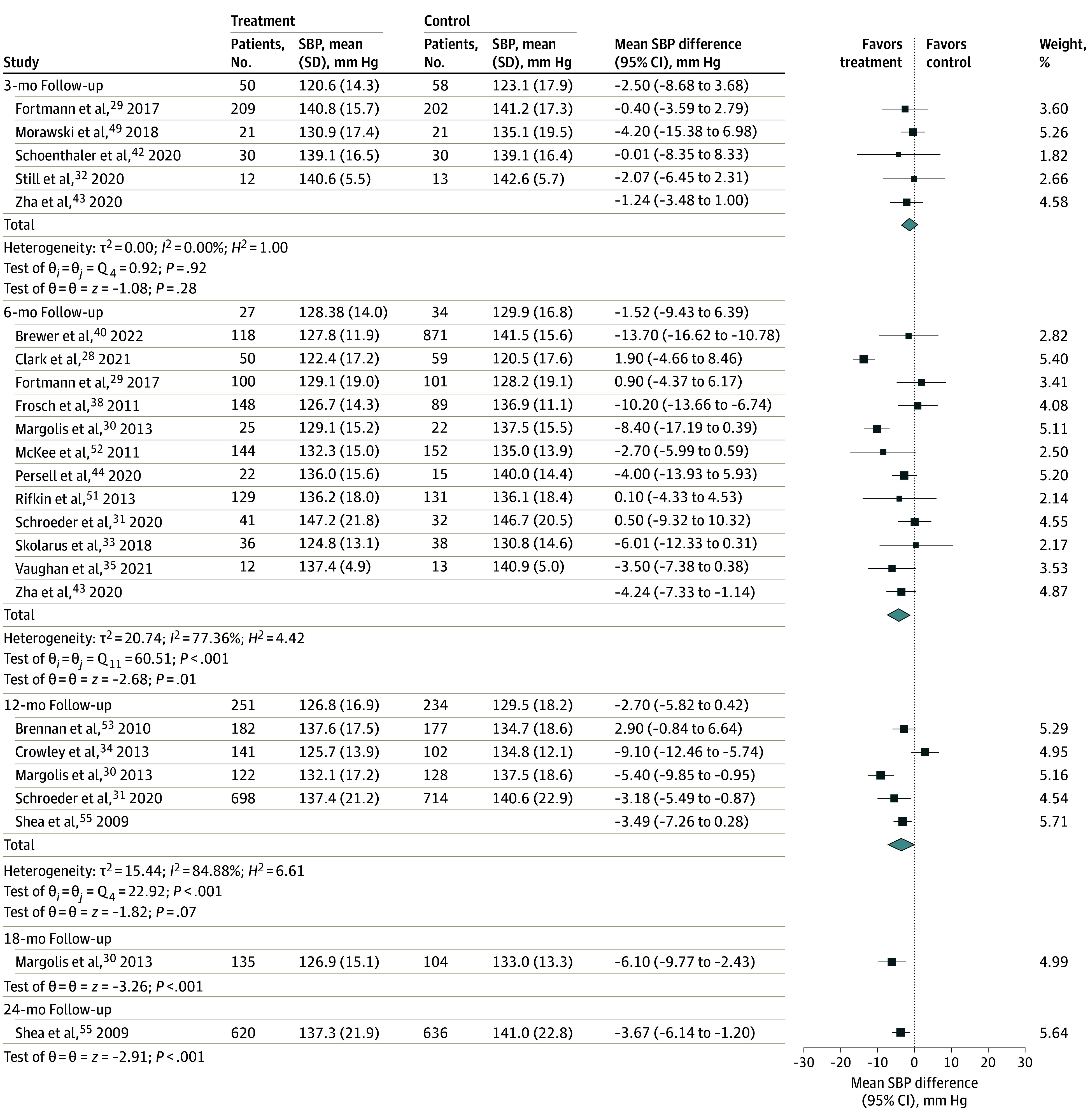
Random-effects restricted maximum likelihood model. Squares indicate mean SBPs, with horizontal lines indicating 95% CIs and the size of the squares representing weight; diamonds indicate pooled estimates, with outer points of the diamonds indicating 95% CIs.
DBP Changes
Across all included studies regardless of follow-up duration, the mean (SD) DBP at baseline for the digital health intervention and control groups was 81.4 (11.8) mm Hg and 81.7 (11.7) mm Hg, respectively. The mean follow-up DBP at the end of the included studies (time of last follow-up) was 77.8 (10.5) mm Hg in the intervention groups and 79.6 (11.2) mm Hg in the control groups.
Among 10 studies that reported 6-month DBP changes, we found a mean difference of −1.11 mm Hg (95% CI, −3.09 to 0.87 mm Hg; P = .27; I2 = 70.45%) (eFigure 1 in Supplement 1).28,30,31,33,36,37,40,44,47,51 The most prominent mean difference in DBP changes between the intervention and control groups was −6.10 mm Hg (95% CI, −11.02 to −1.18 mm Hg).28 Across the 12 studies with 6-month data on follow-up DBP (42.9%), we found a mean difference of −1.86 mm Hg (95% CI, −3.82 to 0.10 mm Hg; P = .06; I2 = 67.57%) (eFigure 2 in Supplement 1).28,29,30,31,33,35,38,40,43,44,51,52 The largest mean difference was −6.70 mm Hg (95% CI, −9.98 to −3.42 mm Hg),30 while the smallest (most positive) mean difference between the intervention and control groups was 1.50 mm Hg (95% CI, −1.53 to 4.53 mm Hg).31
Subgroup Analysis, Metaregression, and Sensitivity Analysis
Among the studies with 6-month follow-up data for the BP outcomes of interest,28,29,30,31,33,35,38,40,43,44,51,52 each of the 6-month outcomes had moderate-high heterogeneity (I2 = 67.57%-80.32%). On sensitivity analysis, removing individual studies had minimal effect on the pooled result (eFigures 3-6 in Supplement 1). Subgroup analyses based on whether studies included remote BP monitoring, were limited to specific racial or ethnic groups, were pilot studies, enrolled patients with controlled BP at baseline, or had BP as the primary outcome also found little effect on statistical heterogeneity (eTables 5-9 in Supplement 1). Metaregression using the proportion of study participants who were female, Black, or Hispanic and/or had a lower level of education had little effect on heterogeneity. Similarly, metaregression including the subgroup variables had little effect on heterogeneity except whether the mean baseline BP was controlled (SBP ≤140 mm Hg). For the outcome of change in SBP, 4 studies had a mean baseline SBP of 140 mm Hg or lower.31,36,40,47 On metaregression, 50.3% of the heterogeneity was explained by this variable (β = 7.1; P = .02). For the other 3 BP outcomes at 6 months, the studies with a mean baseline SBP of 140 mm Hg or lower29,31,35,36,38,40,47,52 found less benefit of digital health interventions, but the differences were not statistically significant.
Publication Bias
Among included studies presenting complete outcome information such as change in BP or follow-up BP,28,29,30,31,32,33,34,35,36,37,38,40,41,42,43,44,47,49,50,51,52,53,55 inclusion of fewer than 10 studies limited formal assessment of publication bias (eFigures 3-6 in Supplement 1). Given that only the 6-month time point had 10 or more studies reporting BP changes or BP at follow-up, this was the only duration that we were able to assess for publication bias. The Egger regression intercept showed no significant publication bias among studies that reported change in SBP,28,30,31,33,36,37,40,44,47,51 follow-up SBP,28,29,30,31,33,35,38,40,43,44,51,52 change in DBP,28,30,31,33,36,37,40,44,47,51 and follow-up DBP.28,29,30,31,33,35,38,40,43,44,51,52
Study Quality
Overall, there were few concerns regarding the quality of included studies in our systematic review and meta-analysis. The domain-specific judgements on study quality ranged from low risk of bias to some concerns of potential bias. In total, 8 of the 28 studies (28.6%) had some concerns, most often attributed to bias due to missing outcome data (eFigure 7 in Supplement 1).28,33,34,40,41,45,50,52 Only 1 study (3.6%) had an overall judgement score of “some concerns.”34
Discussion
To our knowledge, this was the first large-scale, contemporary analysis of more than 8257 participants from 28 studies to characterize existing evidence on the outcomes of digital health interventions for hypertension management in populations experiencing health disparities. Our systematic review and meta-analysis included a diverse sample of participants and a breadth of culturally tailored strategies seeking to integrate racial, ethnic, and socioeconomic determinants into the study design and intervention delivery. We found statistically significant and clinically relevant mean differences in SBP at 6 months (−4.24 mm Hg) and SBP changes at 12 months (−4.30 mm Hg). Only 3 studies30,36,55 assessed BP changes beyond 1 year of follow-up.
This study found evidence of BP improvements in populations experiencing health disparities, strengthening the case for digital health as an efficient and effective tool for hypertension management in these groups. At 6 months of follow-up, individuals who received a digital health intervention had a 4.24 mm Hg greater reduction in SBP compared with those in a control group. Importantly, these results are consistent with findings from meta-analyses that focused on digital health interventions to lower BP levels in the general population.17,56,57,58 One systematic review conducted among 4271 participants from 11 RCTs demonstrated net changes of −3.85 mm Hg in SBP and −2.19 mm Hg in DBP in the combined digital health intervention group,56 which are similar to the mean differences observed in the current study.
The findings of our study can be evaluated in the context of the growing body of evidence linking health disparities with hypertension management and CVD. While this systematic review and meta-analysis focused on populations experiencing health disparities and assessed digital health interventions for culturally tailored components, we found that 17 studies were specifically focused on enrolling a large proportion of Black and Hispanic individuals.29,32,33,34,35,36,37,39,40,41,42,44,46,49,50,53,54 However, subgroup analysis based on whether studies were limited to specific racial or ethnic groups had little effect on statistical heterogeneity. Black and Hispanic adults and individuals with low income and lower level of completed education experience a disproportionately higher burden of hypertension and have higher rates of morbidity and mortality associated with CVD.2,59,60 Moreover, individuals without insurance have been shown to have worse CVD outcomes.60,61 These inequities may be driven by individual-, relational-, and system-level inequities. For example, lifestyle behaviors (ie, physical activity, diet, and sleep quality), interpersonal and structural racism and implicit bias, and differences in access to high-quality care can impact BP control rates.62 Black and Hispanic individuals face an increased level of discrimination, which has been associated with hypertension.63 In recent years, Hispanic and non-Hispanic Black individuals in the US have shown a stagnation and even a decline in hypertension awareness, treatment, and control, with widening gaps in BP control.5,6,64
Several of the included studies addressed these challenges. For example, we observed a diverse range of recruitment strategies and culturally tailored interventions, ranging from faith-based community partnerships to motivational coaching based on personal belief frameworks. While nearly all of the studies included a combination of home BP monitoring with synchronized digital cuffs, medication adherence messaging, or motivational reminders, 21 studies made these reminders linguistically and/or culturally tailored to their patient population.29,31,32,33,34,35,36,38,39,40,41,42,43,45,46,47,48,52,53,54,55 In the Cholesterol, Hypertension, and Glucose Education (CHANGE) study focusing on non-Hispanic Black patients with diabetes, nurses underwent cultural sensitivity training that provided information on the unique challenges that non-Hispanic Black individuals face in their community.34 Additionally, there was a diverse set of community-engaged aspects of the study design and conduct, including the integration of community health centers, involvement of local church leadership for faith-based recruitment and intervention delivery, and participation of community health educators and patient advisory councils.29,31,32,33,35,36,37,38,39 Community-based interventions have been shown to ease the psychosocial stressors often associated with clinical settings, such as white coat syndrome, along with building trust between research staff and study participants.17
Given our aim to characterize approaches to tailoring digital health intervention delivery for populations experiencing health disparities, we have provided several examples to help inform future work seeking to expand access to these strategies. The Reach Out Churches study by Skolarus et al33 was conducted across community centers and places of worship. The community-based participatory research intervention was designed by community and academic leaders to address needs such as food insecurity, cost-related medication nonadherence, poverty, and health literacy in a majority Black neighborhood. Although BP reduction was not statistically significant in that pilot trial, high participation and engagement provided evidence for the feasibility of community-based programs to focus on high-risk groups that are otherwise difficult to reach via traditional medical avenues. Additionally, in the Fostering African American Improvement in Total Health (FAITH!) trial, Brewer and colleagues40 developed and analyzed a community-informed mobile health intervention (FAITH! app) for promoting ideal cardiovascular health among African American individuals in faith communities. In addition to organizing an advisory board composed of diverse community stakeholders to provide study oversight and ensure community centeredness, the research team convened joint congregation community recruitment kickoff events and developed educational materials incorporating practical strategies to overcome barriers from social determinants of health.
In recent years, research has shown that hypertension management and control are low across all Hispanic and Latino groups, with rates lower than those among non-Hispanic White individuals and lowest among Hispanic adults without health insurance.65,66 The integration of CHWs has been a well-studied and validated approach to increasing health care access in these groups. Previous evidence has shown that CHWs who provide technical support, engage in participant recruitment, and are knowledgeable about community resources collectively aid in improving the adoption and acceptability of a digital health intervention.67 In this systematic review and meta-analysis, a subset of studies specified whether an intervention was available in the participants’ native or preferred language and whether culturally sensitive messaging was present, both of which would further enhance access to digital health interventions. In particular, Still et al32 partnered with nurses from the Cleveland Council of Black Nurses, who, similar to CHWs, served as a bridge between underserved communities and their health care needs. While the intervention and control groups did not have significant differences in BP control at 3 months, clinically relevant BP reduction was observed in the intervention group. Additionally, in the TIME Study, Vaughan and colleagues35 incorporated CHW-participant mobile health communication, CHW-led diabetes group visits, and CHW-physician diabetes training and support via telehealth in a population of Hispanic and Spanish-speaking individuals. Compared with control participants, those enrolled in TIME had significant BP improvement (SBP: −6.89 mm Hg vs 0.03 mm Hg; DBP: −3.36 mm Hg vs 0.2 mm Hg).
Limitations
The findings from our systematic review and meta-analysis should be interpreted in the context of several limitations. First, this study was limited in its ability to examine comprehensive, patient-level data on BP changes beyond 1 year. With few studies reporting longer-term follow-up data and the proportion of individuals with controlled hypertension at the end of the study period, the outcomes that were sufficiently powered both overall and for subgroup analyses were limited. However, despite this limitation, statistically significant and clinically meaningful data for SBP changes at 6 and 12 months were identified. Second, since there was inconsistently reported information on sociodemographic characteristics and studies used different definitions for specific subpopulations experiencing health disparities, our literature search may not have captured all studies of digital health interventions conducted in these populations. For example, studies conducted in rural areas may not have been identified if not cataloged as such. To improve our capture of studies, we used a snowball approach, identifying studies referenced by articles that did meet our search criteria.
Third, several studies involved significant investment in community partnerships, patient engagement, and digital health interventions. While questions related to cost, sustainability, and scalability were beyond the scope of this study, they remain important challenges that should be considered in future interventions to address disparities in hypertension control. Last, given that many of the digital health interventions possessed multiple components, we were unable to isolate the effects of each component. Future scoping reviews may be particularly helpful in assessing the breadth of and heterogeneity in digital health intervention components. Relatedly, the control or standard care groups varied widely across included studies and may have impacted the observed effects accordingly.
Conclusions
In this systematic review and meta-analysis of digital health interventions for hypertension management in populations experiencing health disparities, significant and clinically relevant differences in BP lowering between the intervention and control groups were detected. We also identified a breadth of interventions and community engagement strategies, such as participant recruitment and educational programming through faith-based organizations and community centers; however, few studies were conducted beyond 1 year. With the increased use of digital health technologies in medicine, it is important that researchers, clinicians, and public health professionals continue to adapt digital health interventions to meet the needs of demographically and socioeconomically diverse populations with different challenges to improving BP control. More personalized approaches to remote BP monitoring may help to eliminate inequities in hypertension management and outcomes.
eTable 1. Search Strategies and Additional Methods
eTable 2. Additional Study Characteristics for the 28 Included Studies Meeting Eligibility Criteria
eTable 3. Baseline Demographic and Socioeconomic Characteristics of Participants in the 28 Included Studies
eTable 4. Excluded Studies From the Original Search With Reasons for Exclusion
eTable 5. Excluded Studies That Were Eliminated From the Citation Chasing With Corresponding Rationale
eTable 6. Subgroup Analysis Showing Change in SBP at 6 Months
eTable 7. Subgroup Analysis Showing Change in DBP at 6 Months
eTable 8. Subgroup Analysis Showing SBP Values at 6 Months
eTable 9. Subgroup Analysis Showing DBP Values at 6 Months
eFigure 1. Differences in Diastolic Blood Pressure Changes From Baseline to Follow-Up Time Points Between Digital Health Intervention and Control Groups
eFigure 2. Differences in Follow-Up Diastolic Blood Pressures Between Digital Health Intervention and Control Groups at Different Time Points
eFigure 3. Sensitivity Analysis for Presence of Publication Bias Using Change in SBP Outcome at 6-Month Follow-Up and Leave-One-Out Meta-Analysis Results for Same Outcome
eFigure 4. Sensitivity Analysis for Presence of Publication Bias Using Follow-Up SBP Value Outcome at 6-Month Follow-Up and Leave-One-Out Meta-Analysis Results for Same Outcome
eFigure 5. Sensitivity Analysis for Presence of Publication Bias Using Change in DBP Outcome at 6-Month Follow-Up and Leave-One-Out Meta-Analysis Results for Same Outcome
eFigure 6. Sensitivity Analysis for Presence of Publication Bias Using Follow-Up DBP Value Outcome at 6-Month Follow-Up and Leave-One-Out Meta-Analysis Results for Same Outcome
eFigure 7. Risk of Bias Assessment for Included Studies
Data Sharing Statement
References
- 1.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153-e639. doi: 10.1161/CIR.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 2.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233-1241. doi: 10.1161/01.CIR.0000158136.76824.04 [DOI] [PubMed] [Google Scholar]
- 3.Leigh JA, Alvarez M, Rodriguez CJ. Ethnic minorities and coronary heart disease: an update and future directions. Curr Atheroscler Rep. 2016;18(2):9. doi: 10.1007/s11883-016-0559-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ritchey MD, Gillespie C, Wozniak G, et al. Potential need for expanded pharmacologic treatment and lifestyle modification services under the 2017 ACC/AHA hypertension guideline. J Clin Hypertens (Greenwich). 2018;20(10):1377-1391. doi: 10.1111/jch.13364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pool LR, Ning H, Lloyd-Jones DM, Allen NB. Trends in racial/ethnic disparities in cardiovascular health among US adults from 1999-2012. J Am Heart Assoc. 2017;6(9):e006027. doi: 10.1161/JAHA.117.006027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pilkerton CS, Singh SS, Bias TK, Frisbee SJ. Changes in cardiovascular health in the United States, 2003-2011. J Am Heart Assoc. 2015;4(9):e001650. doi: 10.1161/JAHA.114.001650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aggarwal R, Chiu N, Wadhera RK, et al. Racial/ethnic disparities in hypertension prevalence, awareness, treatment, and control in the United States, 2013 to 2018. Hypertension. 2021;78(6):1719-1726. doi: 10.1161/HYPERTENSIONAHA.121.17570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324(12):1190-1200. doi: 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buis L, Hirzel L, Dawood RM, et al. Text messaging to improve hypertension medication adherence in African Americans from primary care and emergency department settings: results from two randomized feasibility studies. JMIR Mhealth Uhealth. 2017;5(2):e9. doi: 10.2196/mhealth.6630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thakkar J, Kurup R, Laba TL, et al. Mobile telephone text messaging for medication adherence in chronic disease: a meta-analysis. JAMA Intern Med. 2016;176(3):340-349. doi: 10.1001/jamainternmed.2015.7667 [DOI] [PubMed] [Google Scholar]
- 11.Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52. doi: 10.2196/jmir.3951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shimbo D, Artinian NT, Basile JN, et al. ; American Heart Association and American Medical Association . Self-measured blood pressure monitoring at home: a joint policy statement from the American Heart Association and American Medical Association. Circulation. 2020;142(4):e42-e63. doi: 10.1161/CIR.0000000000000803 [DOI] [PubMed] [Google Scholar]
- 13.Khoong EC, Olazo K, Rivadeneira NA, et al. Mobile health strategies for blood pressure self-management in urban populations with digital barriers: systematic review and meta-analyses. NPJ Digit Med. 2021;4(1):114. doi: 10.1038/s41746-021-00486-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Margolius D, Bodenheimer T, Bennett H, et al. Health coaching to improve hypertension treatment in a low-income, minority population. Ann Fam Med. 2012;10(3):199-205. doi: 10.1370/afm.1369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guthrie NL, Berman MA, Edwards KL, et al. Achieving rapid blood pressure control with digital therapeutics: retrospective cohort and machine learning study. JMIR Cardio. 2019;3(1):e13030. doi: 10.2196/13030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McManus RJ, Little P, Stuart B, et al. ; HOME BP investigators . Home and online management and evaluation of blood pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial. BMJ. 2021;372:m4858. doi: 10.1136/bmj.m4858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cao W, Milks MW, Liu X, et al. mHealth interventions for self-management of hypertension: framework and systematic review on engagement, interactivity, and tailoring. JMIR Mhealth Uhealth. 2022;10(3):e29415. doi: 10.2196/29415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kario K, Thijs L, Staessen JA. Blood pressure measurement and treatment decisions. Circ Res. 2019;124(7):990-1008. doi: 10.1161/CIRCRESAHA.118.313219 [DOI] [PubMed] [Google Scholar]
- 19.Duan Y, Xie Z, Dong F, et al. Effectiveness of home blood pressure telemonitoring: a systematic review and meta-analysis of randomised controlled studies. J Hum Hypertens. 2017;31(7):427-437. doi: 10.1038/jhh.2016.99 [DOI] [PubMed] [Google Scholar]
- 20.Redfern J, Coorey G, Mulley J, et al. A digital health intervention for cardiovascular disease management in primary care (CONNECT) randomized controlled trial. NPJ Digit Med. 2020;3:117. doi: 10.1038/s41746-020-00325-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marvel FA, Spaulding EM, Lee MA, et al. Digital health intervention in acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2021;14(7):e007741. doi: 10.1161/CIRCOUTCOMES.121.007741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoppe KK, Smith M, Birstler J, et al. Effect of a telephone health coaching intervention on hypertension control in young adults: the MyHEART randomized clinical trial. JAMA Netw Open. 2023;6(2):e2255618. doi: 10.1001/jamanetworkopen.2022.55618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richardson S, Lawrence K, Schoenthaler AM, Mann D. A framework for digital health equity. NPJ Digit Med. 2022;5(1):119. doi: 10.1038/s41746-022-00663-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campbell M, McKenzie JE, Sowden A, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. doi: 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins JPT, Thomas J, Chandler J, et al. , eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.2. Cochrane; 2021. Updated February 2021. Accessed December 29, 2022. http://www.training.cochrane.org/handbook
- 26.Wells GA, O’Connell D, Peterson J, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Accessed November 11, 2022. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 27.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088-1101. doi: 10.2307/2533446 [DOI] [PubMed] [Google Scholar]
- 28.Clark D III, Woods J, Zhang Y, Chandra S, Summers RL, Jones DW. Home blood pressure telemonitoring with remote hypertension management in a rural and low-income population. Hypertension. 2021;78(6):1927-1929. doi: 10.1161/HYPERTENSIONAHA.121.18153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fortmann AL, Gallo LC, Garcia MI, et al. Dulce Digital: an mHealth SMS-based intervention improves glycemic control in Hispanics with type 2 diabetes. Diabetes Care. 2017;40(10):1349-1355. doi: 10.2337/dc17-0230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310(1):46-56. doi: 10.1001/jama.2013.6549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schroeder EB, Moore KR, Manson SM, et al. A randomized clinical trial of an interactive voice response and text message intervention for individuals with hypertension. J Clin Hypertens (Greenwich). 2020;22(7):1228-1238. doi: 10.1111/jch.13909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Still CH, Margevicius S, Harwell C, et al. A community and technology-based approach for hypertension self-management (COACHMAN) to improve blood pressure control in African Americans: results from a pilot study. Patient Prefer Adherence. 2020;14:2301-2313. doi: 10.2147/PPA.S283086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Skolarus LE, Cowdery J, Dome M, et al. Reach Out Churches: a community-based participatory research pilot trial to assess the feasibility of a mobile health technology intervention to reduce blood pressure among African Americans. Health Promot Pract. 2018;19(4):495-505. doi: 10.1177/1524839917710893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crowley MJ, Powers BJ, Olsen MK, et al. The Cholesterol, Hypertension, and Glucose Education (CHANGE) study: results from a randomized controlled trial in African Americans with diabetes. Am Heart J. 2013;166(1):179-186. doi: 10.1016/j.ahj.2013.04.004 [DOI] [PubMed] [Google Scholar]
- 35.Vaughan EM, Hyman DJ, Naik AD, Samson SL, Razjouyan J, Foreyt JPA. A telehealth-supported, integrated care with CHWs, and medication-access (TIME) program for diabetes improves HbA1c: a randomized clinical trial. J Gen Intern Med. 2021;36(2):455-463. doi: 10.1007/s11606-020-06017-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bennett GG, Warner ET, Glasgow RE, et al. ; Be Fit, Be Well Study Investigators . Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med. 2012;172(7):565-574. doi: 10.1001/archinternmed.2012.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bove AA, Homko CJ, Santamore WP, Kashem M, Kerper M, Elliott DJ. Managing hypertension in urban underserved subjects using telemedicine—a clinical trial. Am Heart J. 2013;165(4):615-621. doi: 10.1016/j.ahj.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 38.Frosch DL, Uy V, Ochoa S, Mangione CM. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med. 2011;171(22):2011-2017. doi: 10.1001/archinternmed.2011.497 [DOI] [PubMed] [Google Scholar]
- 39.Anderson DR, Christison-Lagay J, Villagra V, Liu H, Dziura J. Managing the space between visits: a randomized trial of disease management for diabetes in a community health center. J Gen Intern Med. 2010;25(10):1116-1122. doi: 10.1007/s11606-010-1419-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brewer LC, Jenkins S, Hayes SN, et al. Community-based, cluster-randomized pilot trial of a cardiovascular mobile health intervention: preliminary findings of the FAITH! trial. Circulation. 2022;146(3):175-190. doi: 10.1161/CIRCULATIONAHA.122.059046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Naqvi IA, Strobino K, Kuen Cheung Y, et al. Telehealth After Stroke Care pilot randomized trial of home blood pressure telemonitoring in an underserved setting. Stroke. 2022;53(12):3538-3547. doi: 10.1161/STROKEAHA.122.041020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schoenthaler A, Leon M, Butler M, Steinhaeuser K, Wardzinski W. Development and evaluation of a tailored mobile health intervention to improve medication adherence in Black patients with uncontrolled hypertension and type 2 diabetes: pilot randomized feasibility trial. JMIR Mhealth Uhealth. 2020;8(9):e17135. doi: 10.2196/17135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zha P, Qureshi R, Porter S, et al. Utilizing a mobile health intervention to manage hypertension in an underserved community. West J Nurs Res. 2020;42(3):201-209. doi: 10.1177/0193945919847937 [DOI] [PubMed] [Google Scholar]
- 44.Persell SD, Peprah YA, Lipiszko D, et al. Effect of home blood pressure monitoring via a smartphone hypertension coaching application or tracking application on adults with uncontrolled hypertension: a randomized clinical trial. JAMA Netw Open. 2020;3(3):e200255. doi: 10.1001/jamanetworkopen.2020.0255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tuot DS, Rubinsky AD, Velasquez A, et al. Interventions to improve blood pressure control among socioeconomically disadvantaged patients with CKD: Kidney Awareness Registry and Education pilot randomized controlled trial. Kidney Med. 2019;1(5):242-252. doi: 10.1016/j.xkme.2019.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chandler J, Sox L, Kellam K, Feder L, Nemeth L, Treiber F. Impact of a culturally tailored mHealth medication regimen self-management program upon blood pressure among hypertensive Hispanic adults. Int J Environ Res Public Health. 2019;16(7):1226. doi: 10.3390/ijerph16071226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bennett GG, Steinberg D, Askew S, et al. Effectiveness of an app and provider counseling for obesity treatment in primary care. Am J Prev Med. 2018;55(6):777-786. doi: 10.1016/j.amepre.2018.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bosworth HB, Olsen MK, McCant F, et al. Telemedicine cardiovascular risk reduction in veterans: the CITIES trial. Am Heart J. 2018;199:122-129. doi: 10.1016/j.ahj.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 49.Morawski K, Ghazinouri R, Krumme A, et al. Association of a smartphone application with medication adherence and blood pressure control: the MedISAFE-BP randomized clinical trial. JAMA Intern Med. 2018;178(6):802-809. doi: 10.1001/jamainternmed.2018.0447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Frias J, Virdi N, Raja P, Kim Y, Savage G, Osterberg L. Effectiveness of digital medicines to improve clinical outcomes in patients with uncontrolled hypertension and type 2 diabetes: prospective, open-label, cluster-randomized pilot clinical trial. J Med Internet Res. 2017;19(7):e246. doi: 10.2196/jmir.7833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rifkin DE, Abdelmalek JA, Miracle CM, et al. Linking clinic and home: a randomized, controlled clinical effectiveness trial of real-time, wireless blood pressure monitoring for older patients with kidney disease and hypertension. Blood Press Monit. 2013;18(1):8-15. doi: 10.1097/MBP.0b013e32835d126c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McKee MD, Fletcher J, Sigal I, Giftos J, Schechter C, Walker EA. A collaborative approach to control hypertension in diabetes: outcomes of a pilot intervention. J Prim Care Community Health. 2011;2(3):148-152. doi: 10.1177/2150131911401028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brennan T, Spettell C, Villagra V, et al. Disease management to promote blood pressure control among African Americans. Popul Health Manag. 2010;13(2):65-72. doi: 10.1089/pop.2009.0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bosworth HB, Olsen MK, Grubber JM, et al. Two self-management interventions to improve hypertension control: a randomized trial. Ann Intern Med. 2009;151(10):687-695. doi: 10.7326/0000605-200911170-00148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shea S, Weinstock RS, Teresi JA, et al. ; IDEATel Consortium . A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16(4):446-456. doi: 10.1197/jamia.M3157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lu X, Yang H, Xia X, et al. Interactive mobile health intervention and blood pressure management in adults. Hypertension. 2019;74(3):697-704. doi: 10.1161/HYPERTENSIONAHA.119.13273 [DOI] [PubMed] [Google Scholar]
- 57.Li R, Liang N, Bu F, Hesketh T. The effectiveness of self-management of hypertension in adults using mobile health: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2020;8(3):e17776. doi: 10.2196/17776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mao Y, Lin W, Wen J, Chen G. Impact and efficacy of mobile health intervention in the management of diabetes and hypertension: a systematic review and meta-analysis. BMJ Open Diabetes Res Care. 2020;8(1):e001225. doi: 10.1136/bmjdrc-2020-001225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stringhini S, Carmeli C, Jokela M, et al. ; LIFEPATH consortium . Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet. 2017;389(10075):1229-1237. doi: 10.1016/S0140-6736(16)32380-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brooks EL, Preis SR, Hwang SJ, et al. Health insurance and cardiovascular disease risk factors. Am J Med. 2010;123(8):741-747. doi: 10.1016/j.amjmed.2010.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McClurkin MA, Yingling LR, Ayers C, et al. Health insurance status as a barrier to ideal cardiovascular health for US adults: data from the National Health and Nutrition Examination Survey (NHANES). PLoS One. 2015;10(11):e0141534. doi: 10.1371/journal.pone.0141534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Breathett K, Spatz ES, Kramer DB, et al. The groundwater of racial and ethnic disparities research: a statement from Circulation: Cardiovascular Quality and Outcomes. Circ Cardiovasc Qual Outcomes. 2021;14(2):e007868. doi: 10.1161/CIRCOUTCOMES.121.007868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dolezsar CM, McGrath JJ, Herzig AJM, Miller SB. Perceived racial discrimination and hypertension: a comprehensive systematic review. Health Psychol. 2014;33(1):20-34. doi: 10.1037/a0033718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Foti K, Wang D, Appel LJ, Selvin E. Hypertension awareness, treatment, and control in US adults: trends in the hypertension control cascade by population subgroup (National Health and Nutrition Examination Survey, 1999-2016). Am J Epidemiol. 2019;188(12):2165-2174. doi: 10.1093/aje/kwz177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Elfassy T, Zeki Al Hazzouri A, Cai J, et al. Incidence of hypertension among US Hispanics/Latinos: the Hispanic Community Health Study/Study of Latinos, 2008 to 2017. J Am Heart Assoc. 2020;9(12):e015031. doi: 10.1161/JAHA.119.015031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sorlie PD, Allison MA, Avilés-Santa ML, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27(6):793-800. doi: 10.1093/ajh/hpu003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu P, Astudillo K, Velez D, Kelley L, Cobbs-Lomax D, Spatz ES. Use of mobile health applications in low-income populations: a prospective study of facilitators and barriers. Circ Cardiovasc Qual Outcomes. 2020;13(9):e007031. doi: 10.1161/CIRCOUTCOMES.120.007031 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Search Strategies and Additional Methods
eTable 2. Additional Study Characteristics for the 28 Included Studies Meeting Eligibility Criteria
eTable 3. Baseline Demographic and Socioeconomic Characteristics of Participants in the 28 Included Studies
eTable 4. Excluded Studies From the Original Search With Reasons for Exclusion
eTable 5. Excluded Studies That Were Eliminated From the Citation Chasing With Corresponding Rationale
eTable 6. Subgroup Analysis Showing Change in SBP at 6 Months
eTable 7. Subgroup Analysis Showing Change in DBP at 6 Months
eTable 8. Subgroup Analysis Showing SBP Values at 6 Months
eTable 9. Subgroup Analysis Showing DBP Values at 6 Months
eFigure 1. Differences in Diastolic Blood Pressure Changes From Baseline to Follow-Up Time Points Between Digital Health Intervention and Control Groups
eFigure 2. Differences in Follow-Up Diastolic Blood Pressures Between Digital Health Intervention and Control Groups at Different Time Points
eFigure 3. Sensitivity Analysis for Presence of Publication Bias Using Change in SBP Outcome at 6-Month Follow-Up and Leave-One-Out Meta-Analysis Results for Same Outcome
eFigure 4. Sensitivity Analysis for Presence of Publication Bias Using Follow-Up SBP Value Outcome at 6-Month Follow-Up and Leave-One-Out Meta-Analysis Results for Same Outcome
eFigure 5. Sensitivity Analysis for Presence of Publication Bias Using Change in DBP Outcome at 6-Month Follow-Up and Leave-One-Out Meta-Analysis Results for Same Outcome
eFigure 6. Sensitivity Analysis for Presence of Publication Bias Using Follow-Up DBP Value Outcome at 6-Month Follow-Up and Leave-One-Out Meta-Analysis Results for Same Outcome
eFigure 7. Risk of Bias Assessment for Included Studies
Data Sharing Statement