Abstract
Background
Acute Hepatopancreatic Necrosis Disease (AHPND) causes significant mortality in shrimp aquaculture. The infection is primarily instigated by Vibrio parahaemolyticus (Vp) strains carrying a plasmid encoding the binary toxin PirAB. Yet, comprehension of supplementary virulence factors associated with this relatively recent disease remains limited. Furthermore, the same holds for gastroenteritis in humans caused by other Vp genotypes. Additionally, given the prevalent use of antibiotics to combat bacterial infections, it becomes imperative to illuminate the presence of antimicrobial resistance genes within these bacteria.
Results
A subsampled number of 1,036 Vp genomes was screened for the presence of antimicrobial resistance genes, revealing an average prevalence of 5 ± 2 (SD) genes. Additional phenotypic antimicrobial susceptibility testing of three Vp strains (M0904, TW01, and PV1) sequenced in this study demonstrated resistance to ampicillin by all tested strains. Additionally, Vp M0904 showed multidrug resistance (against ampicillin, tetracycline, and trimethoprim-sulfamethoxazole). With a focus on AHPND, a screening of all Vibrio spp. for the presence of pirA and/or pirB indicates an estimated prevalence of 0.6%, including four V. campbellii, four V. owensii, and a Vibrio sp. next to Vp. Their pirAB-encoding plasmids exhibited a highly conserved backbone, with variations primarily in the region of the Tn3 family transposase. Furthermore, an assessment of the subsampled Vp genomes for the presence of known virulence factors showed a correlation between the presence of the Type 3 Secretion System 2 and tdh, while the presence of the Type 6 Secretion System 1 was clade dependent. Furthermore, a genome-wide association study (GWAS) unveiled (new) genes associated with pirA, pirB, tdh, and trh genotypes. Notable associations with the pirAB genotype included outer membrane proteins, immunoglobulin-like domain containing proteins, and toxin-antitoxin systems. For the tdh + /trh + genotypes (containing tdh, trh, or both genes), associations were found with T3SS2 genes, urease-related genes and nickel-transport system genes, and genes involved in a ‘minimal’ type I-F CRISPR mechanism.
Conclusions
This study highlights the prevalence of antimicrobial resistance and virulence genes in Vp, identifying novel genetic markers associated with AHPND and tdh + /trh + genotypes. These findings contribute valuable insights into the genomic basis of these genotypes, with implications for shrimp aquaculture and food safety.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12864-024-10093-9.
Keywords: Vibrio parahaemolyticus, Acute Hepatopancreatic Necrosis Disease, Whole genome sequencing, Antimicrobial resistance, Genome-wide association, Aquaculture, Shrimp, PirAB toxins
Background
Acute Hepatopancreatic Necrosis Disease (AHPND), previously referred to as Early Mortality Syndrome (EMS), is an emerging bacterial disease in shrimp. It has inflicted substantial economic losses on the shrimp industry, particularly in Asian countries like Thailand, Vietnam, and Malaysia, as well as in South America and the United States [1–4]. AHPND is caused by specific strains of the Gram-negative bacterium Vibrio parahaemolyticus carrying a conjugative plasmid (pVA1) of approximately 69 kbp in size, housing the pirABvp genes [5]. The binary pore-forming toxin PirAB is homologous to toxins secreted by Photorhabdus spp. (Pir) and is responsible for the characteristic lesions observed in the shrimp’s hepatopancreas [4, 5]. More recently, other Vibrio (V.) species have been reported to carry plasmids homologous to pVA1, that carry the pirAB genes, such as V. harveyi [6], V. campbellii [7–9], V. owensii [10] and V. punensis [11]. The plasmid-borne nature of these toxins facilitates their mobility and spread to different Vibrio species, which makes it more difficult to control the disease [12, 13]. Increased horizontal gene transfer of this mobile genetic element (MGE) is facilitated by the number of genes associated with conjugative transfer and plasmid mobilization, rendering the plasmid self-transmissible [1, 5]. This principle has been demonstrated in vitro by the successful horizontal transfer of a pVA1-type plasmid from V. parahaemolyticus to a non-pathogenic V. campbellii [14]. Furthermore, the plasmid encompasses a post-segregational killing system, ensuring its consistent inheritance [1, 5, 12, 15]. The plasmid contains a set of transfer-related genes, including the Tn903 (3.5 kbp) transposon where the pirABvp genes are located, and four transposases (ORF15, 48, 55, and 68) able to trigger the transfer of the DNA transposon [12, 16]. This has resulted in plasmid variants such as deletions of the pirA gene, total loss of pirA, and partial loss of pirB coding sequences [15, 17, 18].
Recent research has shown a geographical distinction between plasmids originating from Asian strains and Latin American strains. Specifically, Asian strains lack the Tn3 transposon that is present in all Latin American strains [19, 20]. However, a broader phylogenomic analysis by Yang et al. (2019) has suggested that V. parahaemolyticus is divided into four diverse populations, VppUS1, VppUS2, VppX, and VppAsia [21]. The VppUS1 and VppUS2 populations are largely restricted to the US and Northern Europe, while VppX and VppAsia are found worldwide, with VppAsia making up the great majority of seawater isolates around Asia [21].
Next to the aforementioned plasmid-encoded toxins, V. parahaemolyticus can contain chromosome-encoded virulence factors, such as hemolysins (thermostable direct hemolysin (TDH) and TDH-related hemolysin (TRH)), two Type III secretion systems (T3SS1 and T3SS2) and two T6SSs (T6SS1 and T6SS2). Genotypes carrying tdh and/or trh genes are highly pathogenic in humans, causing gastroenteritis after consumption of contaminated seafood. Throughout this manuscript, these genotypes are referred to as ‘tdh + /trh + genotypes’. Additionally, T3SS2 was shown to be present in these genotypes. TDH, TRH, and T3SS2 are exclusively found in these human clinical isolates responsible for human acute gastroenteritis and are not related to pathogenesis in shrimp [22, 23]. In contrast, T3SS1 and T6SS2 are highly conserved and are suggested to play a role in virulence in both human infections and AHPND infections in shrimp. However, their working mechanisms are not fully understood yet [24, 25].
Over the last few years, aquaculture has expanded significantly, resulting in an increase in disease prevalence. This, in turn, has led to increased antibiotic usage among farms worldwide [26]. However, the improper, empirical, and extensive application of antibiotics has resulted in the emergence of antimicrobial resistance in a substantial amount of V. parahaemolyticus strains in the environment [27–29]. Every year, there is a reported increase in the multidrug resistance of pathogenic V. parahaemolyticus to clinically important antimicrobial drugs. This not only reduces the effectiveness of antibiotics used in aquaculture practices but also poses a threat to human health due to the transmission of V. parahaemolyticus strains carrying (mobilizable) antimicrobial resistance genes (ARGs) to humans upon consumption [27, 30, 31].
In the scope of this study, three distinct AHPND-associated V. parahaemolyticus strains were sequenced, originating from three different geographical sources: Mexico, Thailand, and China. The identification of antimicrobial resistance genes (ARGs) was linked to phenotypic antimicrobial susceptibility testing against a panel of 13 different antibiotics. In addition, using publicly available whole genome sequencing (WGS) data, extensive genomic mining, phylogenetics, and genome-wide association studies (GWAS) were performed to elucidate and characterize putative genetic mediators in pathogenic V. parahaemolyticus strains with a focus on AHPND and tdh + /trh + genotypes.
Results
Long-read whole genome sequencing statistics and quality check
As summarized in Additional file 1: Table S1, our newly sequenced isolates Vp M0904 (CP133891-CP133899), Vp PV1 (JAVKPG000000000), and Vp TW01 (CP133900-CP133905) showed 100% genome completeness, an average GC content of 45.3%, genome sizes of 5.6 Mbp (± 0.2 Mbp), longest contigs of 3.5 Mbp (± 0.04 Mbp), and an average of 5,718 (± 169) predicted genes. These values are all in line with the RIMD 2210633 V. parahaemolyticus (NC_004603.1) NCBI reference strain.
Phenotypic antibiotic susceptibility testing and genomic ARG screening
The results from the antibiotic susceptibility testing can be found in Table 1. All three strains were resistant to ampicillin, with Vp M0904 showing additional resistance to piperacillin, tetracycline, and trimethoprim-sulfamethoxazole. Furthermore, both Vp TW01 and Vp PV1 were intermediately resistant to piperacillin. Interestingly, these phenotypes were supported by chromosome-encoded ARGs. While strains M0904 and PV1 encoded a blaCARB-23 beta-lactamase, strain Vp TW01 had a blaCARB-21 gene, explaining the observed phenotypes against ampicillin and piperacillin. Comparable, the Vp M0904 strain was the only strain carrying a tet(B) and dfrA6 gene, supporting the resistance phenotypes against tetracycline and trimethoprim-sulfamethoxazole, respectively. Also, a QnrVC5 gene was found in its genome, though no phenotypic resistance against any of the tested fluoroquinolones was observed. As shown in Additional file 2 and Additional file 1: Table S4, the CRP, msbA, tet(35), and ugd genes were found in all three genomes.
Table 1.
Results of antibiotic susceptibility tests of the V. parahaemolyticus (Vp) strains. Strains were resistant (R) or susceptible (S) to the antibiotics or showed an intermediate (I) profile. Identified ARGs, supporting the observed resistance phenotypes are included. A visual overview of all identified ARGS is given in Additional file 2
| Antibiotic class | Antibiotic | Vp M0904 | Vp TW01 | Vp PV1 |
|---|---|---|---|---|
| Β-lactam | ||||
| - Penams | ampicillin (10 µg) | R blaCARB-23 | R blaCARB-21 | R blaCARB-23 |
| amoxicillin-clavulanate (20/10 µg) | S | S | S | |
| ampicillin-sulbactam (10/10 µg) | S | S | S | |
| piperacillin (100 µg) | R blaCARB-23 | I blaCARB-21 | I blaCARB-23 | |
| - Cephalosporins | cefotaxime (30 µg) | S | S | S |
| ceftazidime (30 µg) | S | S | S | |
| Aminoglycosides | amikacin (30 µg) | S | S | S |
| gentamicin (10 µg) | S | S | S | |
| Tetracyclines | tetracycline (30 µg) | R tet(B) | S | S |
| Fluoroquinolones | ciprofloxacin (5 µg) | S | S | S |
| levofloxacin (5 µg) | S | S | S | |
| ofloxacin (5 µg) | S | S | S | |
| Folate pathway inhibitors | trimethoprim-sulfamethoxazole (5 µg) | R dfrA6 | S | S |
Whenever expanding our ARG screening to our subsampled dataset, we observed an average presence of 5 ± 2 (SD) ARGs per V. parahaemolyticus genome (Additional file 2 and Additional file 1: Table S4). This also confirmed the overall high prevalence of the CRP (99.7%), msbA (99.0%), tet(35) (99.3%), and ugd (84.4%) genes within the V. parahaemolyticus species. Notably, these genes showed relatively low nucleotide identity scores to the references as compared to other ARGs; 80.0% ± 0.1%, 66.5% ± 0.2%, 82.6% ± 0.2%, and 69.7% ± 0.9% nucleotide identity, for CRP, msbA, tet(35), and ugd, respectively. A substantial amount of V. parahaemolyticus strains harbored either the blaCARB-23 (44.3%) or blaCARB-21 (55.1%) gene, suggesting a high resistance prevalence against β-lactams such as ampicillin and piperacillin. Other β-lactamases that were identified included the blaCARB-22 (0.2%), blaCTX-M-14 (3.1%), blaCTX-M-15 (0.1%), blaNDM-1 ( 0.2%), blaTEM-1 (0.1%), blaTEM-116 (0.1%), blaVEB-1 (2.2%). Aversely, resistance towards tetracycline and trimethoprim-sulfamethoxazole is suggested to be rather low as the tet(B) and dfrA6 genes were only found in 3.1% and 4.1% of subsampled strains. Additionally, other tetracycline (tet(59) (1.9%), tet(A) (0.6%), tet(C) (0.1%), tetI (0.2%), and tetM (0.8%)) and trimethoprim-sulfamethoxazole-associated ARGs (dfrA1 (0.1%), dfrA16 (0.1%), dfrA23 (0.1%), dffrA27 (0.2%), dfrA32 (0.1%), sul1 (1.1%), and sul2 (3.8%)) were identified. Of note, while a variety of other ARGs were identified at low prevalence (Additional file 1: Table S4), ARGs associated with aminoglycoside resistance ranged from 0.1% up to 3.1% prevalence, including the AAC(3)-IV, AAC(6’)-Iia, AAC(6’)-Ib9, ANT(2’’)-Ia, APH(3’’)-Ib, APH(3’)-Ia, APH(6)-Id. These genes seemed to be limited to strains showing a substantially higher (≥ 10 per strain) number of encoded ARGs. Furthermore, as shown in Additional file 2, this data is suggestive of the acquisition of a putative multidrug resistance MGE (e.g., plasmid or integron) that defines a subclade within the VppAsia clade.
Prevalence of AHPND-positive Vibrio species and associated plasmids
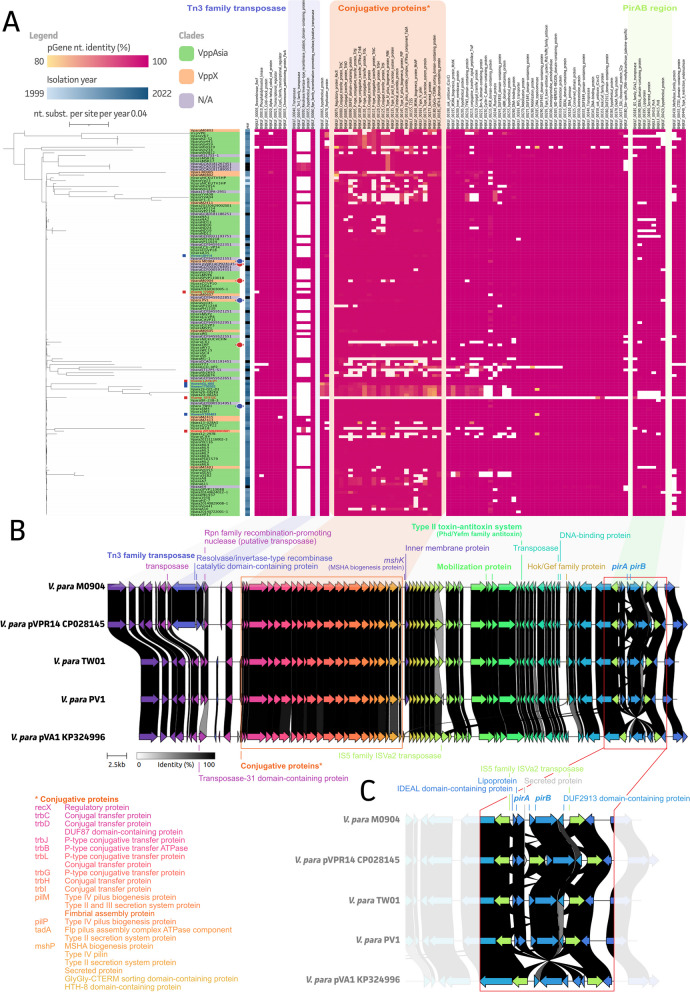
With a focus on AHPND, all available Vibrio spp. genomes from NCBI (24,758 accessed on 05/24/2023) were screened for the presence of pirA and pirB genes. A total of 142 (0.6%) of all available genome assemblies were pirA and/or pirB positive, including 133 V. parahaemolyticus, four V. campbellii, four V. owensii, and one Vibrio sp. A phylogenetic inference of these plasmids, encoding AHPND-associated genes, showed a highly conserved plasmid backbone (Fig. 1A and Additional file 1: Table S6). The region encoding for a Tn3 family transposase was the most variable one, showing its presence in 30 (21.1%) of the pirAB-associated plasmids. While ten (out of a total of 13 VppX strains; 76.9%) of these belonged to the VppX cluster (orange), five (out of a total of 108 VppAsia strains; 4.6%) belonged to the VppAsia cluster (green). For the remaining 15 (out of 21; 71.4%) no data on strain location was available. The plasmids originating from other Vibrio species clustered along the Maximum-Likelihood (ML) tree and did not show diverging plasmid compositions, except for strain 15112C from V. campbellii, which only had a few matching plasmid genes. Our two Asian strains (TW01 and PV1) and the M0904 Mexican strain showed high sequence concordance and plasmid build-up as compared to the used reference (pVPR14; CP028145) (Fig. 1B). As highlighted in Fig. 1C, our M0904 strain showed the presence of a Tn3 family transposon comparable to the pVPR14 (CP028145) reference plasmid. This transposon was missing in both Asian strains as complying with the pVA1 (KP324996) reference plasmid. While the conjugative protein operons, mobilization proteins, and the type II toxin-antitoxin system were highly conserved between all plasmids, the PirA/B region showed some heterogeneity (Fig. 1C). An extra IS5 family ISVa2 transposon was found in the pVPR14 (CP028145) plasmid immediately upstream of the pirA coding sequence, which was absent in our M0904 strain. This PirA/B region was conserved in our TW01 and PV1 strain, whereas the pVA1 (KP324996) plasmid showed an inverted PirA/B region between the two IS5 family ISVa2 transposons.
Fig. 1.
Maximum-Likelihood (ML) tree of pirAB-associated V. parahaemolyticus plasmid sequences and identified plasmid genes (pgenes). A All identified genes are classified per region in the plasmid based on the pVPR14 (CP028145). Our three new strains and the reference strains were indicated with blue and red circles, respectively and clades were colored using the color code presented by Yang et al., 2019 [21]. Plasmids originating from V. campbellii and V. owensii isolates were indicated with a red and blue box, respectively; B The genetic landscape of our three new isolates in relation to some reference strains; C Zoom-in on the versatile pirAB region within the plasmid highlighting
Prevalence and genome-wide associations of common virulence-associated genes in V. parahaemolyticus
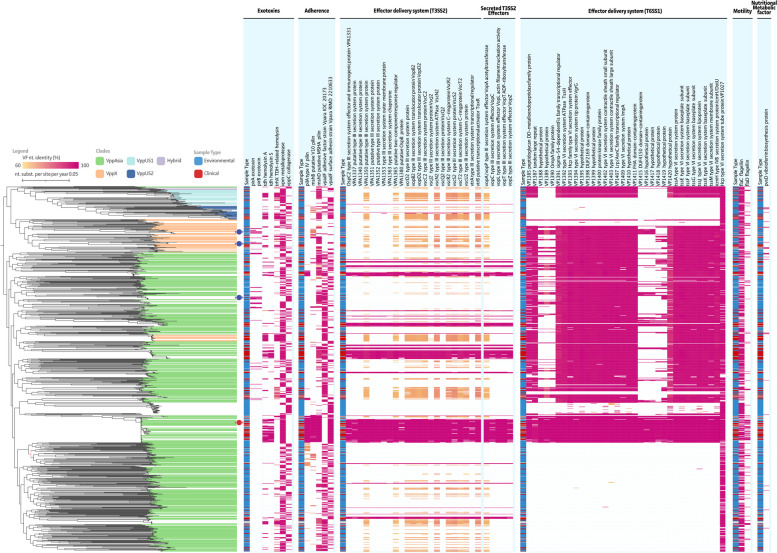
From a total of 301 putative virulence factors, 224 were shown to be present in 90% of our isolates (Additional file 1: Table S5). Hence, these were excluded from further analyses. The remaining 77 genes were visualized in Fig. 2. A relatively low prevalence of pirA (4.8%) and pirB (4.3%) was observed, with 10% of the pirA + genotypes showing the presence of pirA only (i.e., complete pirB deletion or partial below Abricate cut-offs; –minid 80 –mincov 80). While our three newly sequenced strains were all pirA/pirB positive, they lacked the chromosome-encoded tdh and trh genes. The overall prevalence of the TDH hemolysin and TRH hemolysin were estimated at 18.9% and 19.3%, respectively. The presence of the TDH hemolysin showed an apparent correlation with the presence of genes linked to the Type III Secretion System on its second chromosome (T3SS2 on NC_004605 as reference). These genes were found to be present in the V. parahaemolyticus population ranging between 13.7% and 15.7%. Of note, for some T3SS2 genes, other V. parahaemolyticus strains showed the presence of T3SS2 genes at a lower nucleotide identity, raising its prevalence to 34.1%-36.8% (orange-yellow in Fig. 2). Interestingly, when looking at the Type VI Secretion System on the first chromosome (T6SS1 on NC_004603 as reference), a clear clade-dependent trend can be observed. This results in a clear split within the VppAsia cluster (green), which is also true for the VppX (beige) and VppUS1 (light blue) clusters. The VppUS2 (dark blue) strains do not seem to possess the T6SS. Overall the presence of T6SS-associated genes was estimated to range between 56.5% and 58.6%. Comparable to the exclusiveness of pirA/pirB or tdh/trh genes within a single V. parahaemolyticus genome, exotoxin genes vpm (a metalloprotease with an estimated prevalence of 64.5%) and vppC (a collagenase with an estimated prevalence of 33.7%) were shown to never occur together in any of the studied strains. Furthermore, only 1.8% of V. parahaemolyticus are suggested to be negative for both exotoxins, the genotype to which our new V. parahaemolyticus PV1 strain also belongs. To completion, virulence factors involved in adherence, motility, and nutritional metabolism were included (Fig. 2 and Additional file 1: Table S5).
Fig. 2.
Maximum-Likelihood (ML) tree of subsampled V. parahaemolyticus WGS assemblies and identified virulence factor (VF) genes. All identified VFs are classified per subcategory and clades were colored using the color code presented by Yang et al., 2019 [21]. A repeated metadata band is represented highlighting the clinical (red) or environmental (blue) type of the samples. Our three new strains and the reference strain (V. parahaemolyticus RIMD 2210633; NC_004603 and NC_004605) were indicated with blue and red circles, respectively
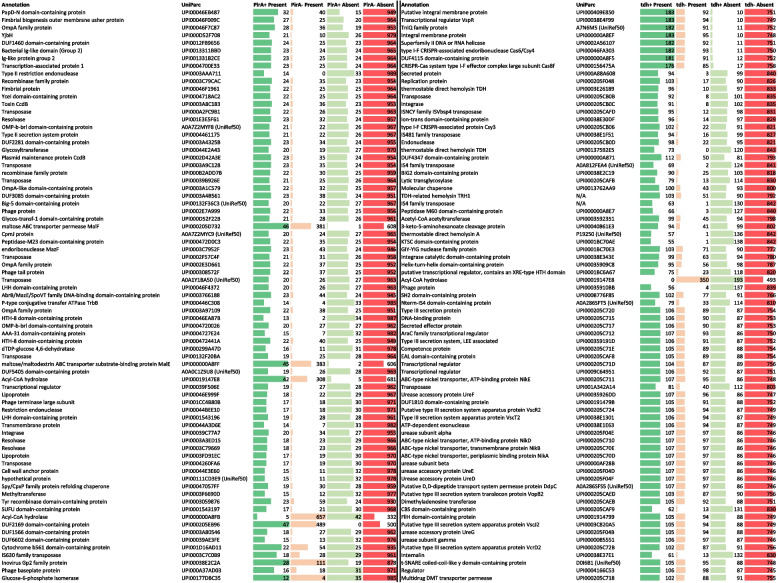
To understand the involvement of other genetic mediators in both AHPND and human acute gastroenteritis phenotypes, a gene-based genome-wide association study (GWAS) was performed for the pirAB and tdh/trh genes. The top 75 associated genes for pirA and tdh are highlighted in Table 2, whereas the results for pirB and trh are enclosed as Additional file 1: Table S8 and S10. Of note, for pirAB GWAS outputs, the pirAB-plasmid associated genes were filtered out, as it is evident that a plasmid-encoded gene will be highly associated with other plasmid-located genes. A complete overview can be found in Additional file 1: Table S7-S10. From our 75 top genes associated with pirA presence, 23 were proteins with predicted domains, a domain of unknown function (DUF), or hypothetical proteins. The remaining 52 non-pirA plasmid associated genes comprised proteins belonging to the family of transposable elements (n = 8), outer membrane proteins and fimbriae (n = 9, including ompA-like and OMP-b-brl proteins), metabolic enzymes (n = 6, including Glycosyltransferase, maltose ABC transporter permease MalF, maltose/maltodextrin ABC transporter substrate-binding protein MalE, Acyl-CoA hydrolase, and Glucose-6-phosphate isomerase) phage-associated proteins (n = 4), recombinases (n = 3), restriction endonucleases (n = 2), transcriptional regulators (n = 2), Immunoglobulin-like proteins (n = 2), the YjbH adaptor protein, the toxin ccdB, the endoribonuclease mazF, a lipoprotein, a Spy/CpxP family protein refolding chaperone, and methyltransferase. A GWAS analysis for pirB resulted in the same set of associated genes (Additional file 1: Table S8), with the addition of some extra associated genes (maltose/maltodextrin ABC transporter substrate-binding protein MalE, a holin (UPI0001BC6B02), Lipoprotein GfcB, amongst other proteins with predicted/DUF domains). Of note, these genes were also found in the pirA non-plasmid associated top 100 list (indicated in red in Additional file 1: Table S7 and S8).
Table 2.
Top 75 associated genes with pirA and tdh presence. Gene annotations are shown along with their UniParc accession where available. For some genes, only a UniRef accession was available. Bars indicated number of isolates present/absent in positive (pirA + or tdh +) or negative (pirA- or tdh-) strains. For pirA, the top 75 non-pirA plasmid-associated genes are highlighted
For the tdh gene, 18 of the top 75 associated genes were proteins with putative functions, a predicted domain, or DUF. Interestingly, the GWAS confirms the association of Type III secretion genes (n = 7, including vcrD2, vopB2, vscJ2, vscR2, and vscT2) with the presence of the tdh gene. Next to this also urease-associated genes (n = 7, including urease subunit alpha, beta, and gamma, along with accessory genes ureDEFG), transcriptional regulators (n = 6, including vspR), transposable elements (n = 6), metabolic enzymes (n = 4, including acetyl-CoA acetyltransferase, 3-keto-5-aminohexanoate cleavage protein, acyl-CoA hydrolase, dimethyl adenosine transferase), an ABC-type nickel transporter operon (n = 4, nikABDE), a type I-F CRISPR-associated endoribonuclease Cas6/Csy4 and CRISPR-Cas system type I-F effector complex large subunit Cas8f, an uncharacterized secreted (effector) protein (UPI000A88A608 and UPI000205C717), a lytic trans glycosylase, a competence protein, an internalin, and a multidrug DMT transporter permease were found to be associated with tdh positive strains. Again, comparable results were obtained for the GWAS using trh positivity. Still some extra genes popped up, including seven extra Type III secretion genes, an OmpA-like domain-containing protein (UPI0001914797), two transcriptional regulators, a virulence-associated protein (UPI0005B6DDF1), cytotoxin (UPI000205CAF6; cytotoxic necrotizing factor Rho-activating domain-containing protein), and hemolysin B subunit protein (UPI000359204B), the Type VII secretion protein EssB, and the RTX toxin-activating lysine-acyltransferase, amongst other proteins with putative functions, a predicted domain, or DUF. Comparable to the pirAB GWAS outputs, most of these trh-associated genes were also found in the top 100 list of tdh-associated genes. A complete overview of the GWAS results and associated statistics is given in Additional file 1: Table S9 and S10, with extra trh-associated genes indicated in red.
Discussion
The three strains sequenced in this study were confirmed to be of the species Vibrio parahaemolyticus, carrying a pVA1-like plasmid containing the AHPND-related pirAB genes. The genomes of these strains, along with a representative subsample of 1,036 (of a total of 8,897) V. parahaemolyticus genomes available on NCBI, were analyzed to strengthen our understanding of AHPND and tdh + /trh + genotypes. Furthermore, we showed that long-read ONT sequencing can deliver complete circular V. parahaemolyticus genome and plasmid assemblies.
The sampled genomes were screened for the presence of ARGs and other virulence genes. In general, an average of 5 ± 2 (SD) ARGs per V. parahaemolyticus genome could be identified. For the three newly sequenced strains, five ARGs were identified in the genomes of Vp TW01 and Vp PV1, but eight ARGs for Vp M0904. This was also reflected in the phenotypical antimicrobial susceptibility testing (AST), where Vp M0904 showed resistance to four antibiotics (out of the panel of 13), whereas Vp TW01 and Vp PV1 were only resistant against a single antibiotic drug (and one intermediately sensitive) antibiotic. As strain Vp M0904 is resistant to antimicrobials of three different categories (β-lactams, tetracyclines, and trimethoprim-sulfamethoxazole), it is regarded as a multidrug-resistant (MDR) organism. Our phenotypic observations against ampicillin and piperacillin could be linked with the presence of specific ARGs, namely the β-lactamases blaCARB-21 and blaCARB-23. Resistance towards tetracycline and trimethoprim-sulfamethoxazole is suggested to be due to the chromosomal presence of a tet(B) and dfrA6 gene. Unfortunately, substantial phenotypic metadata is lacking for the available genomes on NCBI. However, screening the subsampled genomes revealed a high estimated prevalence of these β-lactamases in the V. parahaemolyticus population (54.9% and 44.4% for blaCARB-21 and blaCARB-23, respectively). Available literature also suggests a high resistance prevalence towards β-lactams, which we phenotypically confirmed in this study by the resistance of all three strains towards ampicillin and piperacillin. Larger-scale (n > 36) phenotypical studies are confirming this too, with high reported resistance prevalence towards both penams [e.g., 45–100% to ampicillin [6, 28, 30–33] and 68–100% to penicillin [30–32]] and cephalosporins [e.g., 49.6–84% to cefazolin [31, 34], 52–73% to cefotaxime [33, 35] and 24–82% to cephalothin [30, 34]].
An estimated 3.1% of strains showed the presence of the tet(B) gene, with a lower prevalence of other tetracycline resistance-associated genes such as tet(59), tet(A), tet(C), tet(E), tetM. Comparable results were obtained for dfrA6 prevalence (4.0%), with the rare identification of dfrA1, dfrA16, dfrA23, dfrA27, and dfrA32 potentially conferring strains resistant to trimethoprim-sulfamethoxazole. In addition, even though no phenotypic resistance was observed in our strains, ARG prevalence suggests low prevalence of resistance towards aminoglycosides (aminoglycoside acetyltransferase, nucleotidyltransferase, and phosphotransferase genes) and fluoroquinolones (quinolone resistance genes). This is again reflected in phenotypical studies on V. parahaemolyticus clinical and environmental strains, where low prevalence of resistance towards tetracyclines [e.g,. 0.3% to doxycycline [30, 31, 36], 0–15% to tetracycline [27, 28, 30–33, 35, 36]], trimethoprim-sulfamethoxazole [0–7% [27, 30, 31, 33]], and fluoroquinolones (e.g,. 0% to ciprofloxacin [27, 30] and 0–1% to levofloxacin [27, 33]] were reported. However, reported resistance prevalence against aminoglycosides is very variable [e.g,. 0–64% to amikacin [27, 28, 30, 33] and 15–50% to kanamycin [30, 33, 34]]. It should be noted that resistance to aminoglycosides is often the result of mutations of the ribosome [37], a factor that was not included in our analysis. As a result, there is a possibility of underestimating the extent of this resistance. Furthermore, most of the phenotypical AST screening studies focused on samples from one geographical region, and there might be large differences between V. parahaemolyticus populations of different locations. Furthermore, differences in applied AST screening methods (i.e., disc diffusion testing versus broth microdilution method), as well as sample types (e.g., clinical, environmental, seafood or surface water samples, among others), differ between studies, possibly resulting in large differences and potential underestimations of actual resistance prevalence towards certain antibiotics. Hence, using WGS-based ARG genotyping in V. parahaemolyticus seems to be a good predictive tool to identify, study, understand, and follow up on the dissemination of drug-resistance genotypes in the population. Many studies reported the presence of at least one multidrug-resistant isolate like Vp M0904 [27, 28, 38]. These isolates represent an even bigger threat to aquaculture and human health, as they are more difficult to control with antibiotics, and are an important reservoir of ARGs. This is also highlighted in the identification of a V. parahaemolyticus cluster showing the presence of a putative plasmid carrying multiple ARGs. Most of the genomes presented within this genetic clade originate from China and were part of an unpublished study on the occurrence and genetic environments of blaCTX-M-14 among foodborne Vibrio spp. (PRJNA622672). Still, researchers should be encouraged to link phenotypic and genotypic observations and be aware of potential ARGs not contributing to resistance phenotypes and/or being the result of contaminating contigs in the assembly. To completion, point mutations (e.g., in rRNA, gyrA, parC genes) should also be considered as a potential source of resistance, which requires accurate metadata and genomics to establish proper associations [39, 40]). This was highlighted in the very high prevalence of ARGs CRP (99.7%), msbA (99.0%), tet(35) (99.3%), and ugd (84.4%). CRP is suggested to be involved in macrolide, penam, and fluoroquinolone resistance [41], msbA in nitroimidazole resistance [42], tet(35) in tetracycline resistance and ugd in resistance against peptide antibiotics [43], but do not seem to induce resistance in V. parahaemolyticus. It is plausible that these are so-called ‘silent’ genes, that might only be activated in specific conditions or expressed at low levels [28, 44]. The high prevalences of especially CRP, msbA, and tet(35) (≥ 99%) suggests that these might be intrinsic resistance genes [45]; however, their relatively low nucleotide identity (CRP 80.0% ± 0.1%, msbA 66.5% ± 0.2%, tet(35) 82.6% ± 0.2%, and ugd 69.7% ± 0.9%) compared to other ARGs suggests that these genes might be degenerated and have lost functionality over time. In contrast, all other identified ARGs are suggested to be acquired, as these are strain-specific [45].
Next, screening of all available Vibrio spp. genomes showed an overall low (0.57%) prevalence of pirA and/or pirB genes, and a prevalence of 4.8% and 4.3% in V. parahaemolyticus, respectively. In accordance with previous research [19], the two Asian strains Vp TW01 and PV1 did not possess the Tn3 transposon on their plasmid, while the Latin-American (Mexican) strain Vp M0904 did. The pirAB region is usually flanked by two identical IS5 family ISVa2 transposases in opposite directions that form a composite transposon called Tn903 or Tn6264 [19]. This region was conserved in the three newly sequenced strains. As observed before [46], an extra IS5 family transposon was found in pVPR14 immediately upstream of the pirA coding sequence. Interestingly, this insertion seems to have no effect on the transcription of the genes, but instead inhibits translation of the PirAB proteins [46]. Furthermore, compared to the other analyzed plasmids, the pirAB region between the two IS5 family transposons of the pVA1 plasmid is inverted compared to the other plasmids. Here our plasmid screening and characterization showed a highly conserved backbone of the pirAB-encoding plasmid, highlighting the biggest genetic diversity at the Tn3 transposon region. Still, it is important to note that our plasmid analysis is limited to the available data in NCBI as insufficient sequencing depth might result in the lack of data on plasmids. Also, the choice of sequencing platform affects the actual recovery of plasmid information, hence care should be taken when performing this type of analyses on genome assemblies available in the public domain. The choice of sequencing technology might also impact the potential duplication and orientation of transposons due to their repetitive regions [47–50].
The three newly sequenced Vp strains, as well as the subsampled genomes, were screened for the presence of virulence-associated genes. As expected, Vp M0904, TW01, and PV1 possessed the pirA and pirB genes, and lacked the tdh and trh hemolysin genes. Furthermore, the presence of tdh was strongly associated with the presence of genes linked to the T3SS2. These observations confirm the suggestions made before, that: (i) AHPND genotypes are not pathogenic to humans since they lack the tdh and trh genes, along with the absence of the T3SS2 and (ii) there is a correlation between the presence of tdh and trh genes and the T3SS2 [22, 23]. Genes related to the T6SS on the first chromosome (T6SS1) were absent in the VppUS2 clade, and present in only a subpart of the other three clades VppAsia, VppX, and VppUS1. Although previously it has been suggested that T6SS1 is present in all AHPND and human clinical isolated, and not in non-pathogenic environmental strains [22], this is not supported by our results.
Many Vp AHPND strains have been identified and different rates of mortality in infected shrimps were reported [51], indicating that the PirAB toxin is not the only factor contributing to virulence in shrimp. The same holds for gastroenteritis in humans, where illness is linked with the presence of tdh/trh and T3SS2, but other factors might contribute to virulence. To gain more insight into contributing factors, a GWAS was performed for the pirAB and tdh/trh genes. For pirAB it is important to note that most associations were with the plasmid genes themselves, as it is evident that a plasmid-encoded gene will be highly associated with other plasmid-located genes. These genes have been filtered out in our analyses so we could focus better on chromosome-encoded associations. Many transposon- (n = 8), phage-related (n = 4) proteins were identified. Both are often associated with the insertion of new genes primarily by horizontal gene transfer and expressing novel pathogenic properties [51], and CRISPRs are suggested to be able to prevent the invasion of prophages into bacteria, being a barrier of defense to fight against foreign DNA [51]. A previous study indicated the lack of these CRISPR elements in Vp AHPND strains, allowing the prophage insertion of virulence genes, possibly contributing to the virulence of Vp AHPND strains [51]. These observations seem to be confirmed in the present GWAS. Multiple outer membrane proteins (OMPs) were also among the associated genes, of which several were related to OmpA. For many Gram-negative bacteria, this is a key virulence factor involved in bacterial biofilm formation, eukaryotic cell infection, antibiotic resistance, and immunomodulation [52]. In V. parahaemolyticus, several OMPs have been shown to be involved in ampicillin resistance [53] and osmoregulation [54]. Furthermore, a Spy/CpxP family protein refolding chaperone was present in the GWAS of pirAB, and is demonstrated to protect OMPs against protein-unfolding stress in E. coli [55]. Possibly, it is important in the protection against unfolding of the previously mentioned OmpA and other OMPs. The association with two immunoglobulin-like domain-containing proteins is seen, which are often surface proteins involved in cell-to-cell recognition, adhesion, biofilm formation, and conjugative transfer [56, 57]. These domains are widely present in numerous proteins, and several have been identified in V. parahaemolyticus, such as adhesive factor VpadF [56, 57]. Association with toxin gene ccdB indicated the importance of the toxin-antitoxin (TA) system ccdA-ccdB, consisting of the stable toxin ccdB and less stable antitoxin ccdA to neutralize the toxin. It is defined as a plasmid maintenance system, acting through post-segregational killing of plasmid-free cells [58, 59]. The endoribonuclease mazF is also part of the chromosomal type II TA system mazEF. It has been identified in multiple bacteria where it regulates virulence factors, such as biofilm production in E. coli and in Staphylococcus (S.) aureus, but it may be involved in other functions such as antibiotic resistance and programmed cell death under stressful conditions [59, 60]. However, its role in Vibrionaceae has not been studied to the author’s knowledge.
The GWAS of the tdh/trh genes, related to human gastroenteritis, confirmed the association with the T3SS2, as seven genes were present in the top 75. Additionally, multiple urease-associated genes are linked to tdh, which are virulence factors in various pathogenic bacteria [61]. The ability of ureases to raise the pH in the immediate environment inside the host contributes to the survival of the bacteria in the host digestive tract [38]. Although there seems to be an association between tdh and urease genes, phenotypically this association seems to be more correct for trh since multiple reports have mentioned that all trh genotypes were urease positive, which was not the case for tdh [62, 63]. The association with trh was also confirmed in our GWAS, and the urease-related genes were ranked higher in the top 75 than for tdh (7 genes ranked between place 27 and 41 for trh compared to 7 genes ranked between place 51 and 70 for tdh). Furthermore, it was demonstrated that the genes for an ATP-binding cassette-type nickel transport system, which may play a role in nickel transport through the bacterial cytoplasmic membrane, are located adjacent to the urease gene cluster on the genome of V. parahaemolyticus, and that this region is in close proximity to the trh gene [63, 64]. Interestingly, this nickel transport system is indeed associated with tdh and trh according to the current GWAS. Possibly, this system aids in providing nickel for incorporation into the metallocentre within the active sites of the ureases [63]. Another interesting finding from the tdh-based GWAS was the association of a type I-F CRISPR-associated endoribonuclease Cas6/Csy4. This is related to a variant of the subtype I-F CRISPR-Cas system called the ‘minimal’ type, which showed a strong association with tdh in previous reports as well [65, 66]. Furthermore, genes for TniQ and a Cas8f-like protein also returned in our GWAS, which are all possibly linked with the minimal type I-F system. Interestingly, it was shown that this system was present within a Tn7-like transposon in V. parahaemolyticus and that the pathogenicity island containing the T3SS2 was correlated [67]. Association with trh on the other hand with genes of this minimal type I-F CRISPR-Cas system was a lot lower. Furthermore, the presence of many transposable elements (n = 6) as well as a competence protein is underlining the importance of genetic diversity that is associated with these genes.
Conclusion
This study has provided a comprehensive characterization of three AHPND-inducing V. parahaemolyticus strains and their associated PirAB-encoding plasmids. Additionally, to the author’s knowledge, this is the first in-depth and comprehensive genome mining study on V. parahaemolyticus ARGs and virulence genes. The presence of ARGs and important virulence genes were examined and correlated with phylogenomic analysis of an extensive dataset of V. parahaemolyticus genomes. We recommend this approach to fellow researchers for rapid antibiotic resistance screening and to contain dissemination of the ARGs and resistance plasmids, particularly in light of the emergence of multidrug-resistant strains, as observed not only in this study but also in related studies. Furthermore, through GWAS, we have successfully identified known and novel genetic markers associated with the AHPND and tdh + /trh + genotypes of V. parahaemolyticus. This discovery holds promise for the development of rapid and precise discriminatory tests targeting these genotypic variations. Collectively, these findings significantly enhance our comprehension of pathogenic V. parahaemolyticus, underscoring the importance of close monitoring of antimicrobial resistance of the bacteria.
Methods
Bacterial strains and growth conditions
Three new V. parahaemolyticus strains were used in this study: M0904, isolated in northwestern Mexico (originally received from A.C. Mazatlàn unit of Aquaculture), TW01, isolated in Southern Thailand, and PV1, isolated in China (both received from Robins McIntosh). All three strains were isolated from AHPND-affected shrimp and were previously confirmed to produce PirAB by Western Blot [68]. One colony of each strain was inoculated in Marine Broth (MB) (Carl Roth – CP73.1) and grown overnight (6 ± 2 h) at 28°C with shaking at 140 rpm.
Antibiotic susceptibility testing
The three V. parahaemolyticus strains and the reference strain Escherichia (E.) coli ATCC 25922 (strain LMG8223 from the Belgian Coordinated Collection of Microorganisms BCCM) were tested for antibiotic resistance using the disc diffusion method, in compliance with the Clinical and Laboratory Standards Institute (CLSI) M45 guidelines for Vibrio spp. A total of 13 different antibiotics (all purchased from Oxoid Limited, UK) were tested: ampicillin (10 µg), amoxicillin-clavulanate (20/10 µg), ampicillin-sulbactam (10/10), piperacillin (100 µg), cefotaxime (30 µg), ceftazidime (30 µg), amikacin (30 µg), gentamicin (10 µg), tetracycline (30 µg), ciprofloxacin (5 µg), levofloxacin (5 µg), ofloxacin (5 µg) and trimethoprim-sulfamethoxazole (1.25/23.75 µg). Briefly, the bacteria were grown on Mueller–Hinton Agar (MHA, Carl Roth, Germany) plates after which a direct colony suspension was prepared in a 0.85% NaCl solution, and turbidity was adjusted to 0.5 McFarland standard. The MHA plates were inoculated with 100 µL of this suspension which was spread with a sterile triangle rod. Plates were allowed to dry for 5 to 10 min prior to applying the antibiotic disks onto the agar with sterile tweezers. The plates were incubated inverted at 35°C for 16 ± 2 h. The reference strain E. coli ATCC 25922 was used as a control to monitor the accuracy of the disk diffusion tests.
Genomic DNA extraction and whole genome long-read sequencing
A freshly grown overnight culture of each of the three strains was subjected to the isolation of High Molecular Weight (HMW) DNA using the DNA MiniPrep Kit (Zymo Research, USA) as described before [40]. Manufacturer’s instructions were followed with the addition of a 30-min proteinase K (500 ng μL−1; Promega, USA) treatment at 56°C after two cycles of bead bashing in a TissueLyzer (30 oscillations per minute for 5 min; Qiagen, Germany). The quality of the resulting DNA was confirmed on a NanoDrop device. Whenever A260/A280 and/or A260/A230 measures did not reach 1.7 or 1.5 cut-offs, an extra DNA clean-up was performed using CleanNGS (CleanNA, The Netherlands) magnetic beads at a 1:1 ratio. For subsequent long-read Nanopore sequencing, 400 ng DNA was used in rapid library preparation (RBK-004), barcoding each sample for 48h sequencing on an R9.4.1 MinION flow cell. Data were acquired on a GridION device (Oxford Nanopore Technologies Ltd., UK), supporting real-time, super accurate base calling, and demultiplexing with guppy (v6.1.5; ONT).
Genome assembly and annotation
The obtained reads were used in an in-house established bacterial genome assembly pipeline, which includes read quality checking (NanoComp v.1.10.0; [69]), read filtering (filtlong v0.2.1; –min_length 1,000 –keep_percent 95; https://github.com/rrwick/Filtlong), Trycycler subsampling (v0.5.3; –min_read_depth 50 –count 10 –genome_size 5 M; [47]) for independent genome assemblies using Flye (v2.9; –nano-hq -g 3m; [70]), raven (v1.8.1; [71]), wtdbg2 (v1.12; [72]), and miniasm_miniplish.sh (v0.3; -x ont -g 3m; https://github.com/rrwick/Minipolish) with default settings if not depicted. Subsequent trycycler commands were run as instructed using default settings, followed by read polishing using minimap2 (v.2.20; -a -x map-ont; [73]) and medaka (v.1.5.0; consensus –model r941_min_sup_g507 –batch_size 50; stitch –no-fillgaps; ONT). The quality of the resulting genomes was checked using CheckM (v.1.1.0; [74]), including 1,084 markers from 70 Vibrio spp. genomes. Species classification was done using rMLST via the pubMLST web interface [75]. Average Nucleotide Identity (ANI) of the three new strains against the V. parahaemolyticus reference strain RIMD 2210633 (NC_004605.1) was calculated using the ANI tool on the EZBioCloud web interface [76]. An overview of raw read statistics, quality checks, and NCBI accession numbers can be found in Additional file 1: Table S1.
Screening for ARGs and virulence factor, and phylogenomic analysis
A total of 8,897 V. parahaemolyticus genome assemblies were available on NCBI (accessed on 24/06/2023), which were subsampled to 1,036 genomes maintaining genomic diversity with minimal loss of resolution (Additional file 1: Table S2). Subsampling was done using a dendrogram, which was generated based on genomic blast (default settings), containing the sequences from V. parahaemolyticus based on its taxonomy ID 223926. While iteratively going through the nodes of this dendrogram, the average distance of each node to its leaves was calculated. Whenever this average distance dropped below 0.01, only one representative sequence from that node was retained. All genomes, including the newly obtained sequences were subjected to a virulence factor and ARG screening using Abricate (v.1.0.1; –minid 80 –mincov 80; https://github.com/tseemann/abricate) using the pre-built CARD [77] and a custom virulence factor database, which included a more extensive list of putative V. parahaemolyticus virulence-associated genes (n = 301) based on available literature. This list can be accessed in Additional file 1: Table S3. Complete Abricate outputs can be accessed in Additional file 1: Table S4 and S5. The subsampled dataset was also subjected to a single nucleotide polymorphism (SNP) based phylogenetic analysis as described by Kaas et al. [78]. In short, SNPs were identified by aligning all the sequences to the reference strain V. parahaemolyticus RIMD 2210633 (NC_004605.1), using the nucmer aligner from the MUMmer package (v3.1, -CIlrT; [79]). From this output, a concatenated alignment of the SNPs was produced, which was subjected to maximum-likelihood (ML) phylogenetic inference using IQtree (v.1.6.1; -m GTR + I + R -nt AUTO -bb 1000; [80]) applying the GTR + F + I model and 1,000 ultrafast bootstraps (–ufboot). Final tree visualizations were done in iTOL (v.5; [81]).
Plasmid characterization and genome-wide association study
All pirA and/or pirB positive strains, as obtained by virulence factor screening, were analyzed separately, to study their relatedness and genomic landscape. First, all pirA and/or pirB positive plasmid sequences were subjected to an SNP-based alignment as described before to obtain an ML phylogenetic inference. Next, our newly sequenced strains, along with some type strains (pVPR14: CP028145 and pVA1: KP324996) were used for plasmid annotation using Bakta (v1.8.2.; –db db-full –compliant –genus Vibrio –species parahaemolyticus –gram -; [82]). This allowed to generate a custom plasmid gene database for an Abricate-based search (–minid 80 –mincov 80) of all pirA and/or pirB-associated plasmid sequences. Database entries and Abricate output can be found in Additional file 1: Table S6. In addition, a visualization could be made of the pirA/pirB plasmid landscape in our new isolates. Gene maps were obtained using clinker (v.0.0.28; [83]). In addition, all subsampled genomes and new isolates were subjected to whole genome annotation using Bakta, with identical settings as depicted before, for use in a genome-wide association study (GWAS). The latter was done using Roary (v.3.13.0; -p 8 -e -n -v; [84]) and Scoary (v.3.6.16; -e 1000 -n tree.newick; [85]), allowing the association of coding sequences based on any pheno- or genotypic feature. Here, pirA/pirB/tdh/trh presence (addressed 1) and absence (addressed 0) were used in the GWAS metadata file as obtained from the Abricate output and highlighted in green in Additional file 1: Table S5. A complete overview of GWAS outputs can be found in Additional file 1: Table S7-S10.
Supplementary Information
Acknowledgements
Not applicable.
Authors’ contributions
M.V., P.B., D.V. and N.V. designed the study. M.V., S.C. and N.V. carried out the experimental work and analysis. The manuscript was written by M.V. and N.V.. All authors read and approved the final manuscript.
Funding
This work was financially supported by UGent (F2020/IOF-ConcepTT/045).
Availability of data and materials
The draft sequences of all three Vibrio parahaemolyticus strains can be found on NCBI (Vp M0904 CP133891-CP133899, Vp PV1 JAVKPG000000000, Vp TW01 CP133900-CP133905).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Peter Bossier, Nick Vereecke and Daisy Vanrompay share senior authorship.
References
- 1.Kumar R, Ng TH, Wang HC. Acute hepatopancreatic necrosis disease in penaeid shrimp. Rev Aquac. 2020;12(3):1867–1880. doi: 10.1111/raq.12414. [DOI] [Google Scholar]
- 2.Kumar V, Roy S, Behera BK, Bossier P, Das BK. Acute hepatopancreatic necrosis disease (Ahpnd): Virulence, pathogenesis and mitigation strategies in Shrimp aquaculture. Toxins. 2021;13(8):1–28. doi: 10.3390/toxins13080524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soto-Rodriguez SA, Lozano-Olvera R, Montfort GRC, Zenteno E, Sánchez-Salgado JL, Vibanco-Pérez N, Aguilar Rendón KG. New Insights into the Mechanism of Action of PirAB from Vibrio Parahaemolyticus. Toxins. 2022;14(4):243. doi: 10.3390/toxins14040243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han JE, Tang KFJ, Tran LH, Lightner DV. Photorhabdus insect-related (Pir) toxin-like genes in a plasmid of Vibrio parahaemolyticus, the causative agent of acute hepatopancreatic necrosis disease (AHPND) of shrimp. Dis Aquat Org. 2015;113(1):33–40. doi: 10.3354/dao02830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee CT, Chen IT, Yang YT, Ko TP, Huang YT, Huang JY, et al. The opportunistic marine pathogen Vibrio parahaemolyticus becomes virulent by acquiring a plasmid that expresses a deadly toxin. Proc Natl Acad Sci USA. 2015;112(34):10798–10803. doi: 10.1073/pnas.1503129112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muthukrishnan S, Defoirdt T, Ina-Salwany MY, Yusoff FM, Shariff M, Ismail SI, Natrah I. Vibrio parahaemolyticus and Vibrio harveyi causing Acute Hepatopancreatic Necrosis Disease (AHPND) in Penaeus vannamei (Boone, 1931) isolated from Malaysian shrimp ponds. Aquaculture. 2019;511:734227. doi: 10.1016/j.aquaculture.2019.734227. [DOI] [Google Scholar]
- 7.Dong X, Bi D, Wang H, Zou P, Xie G, Wan X, et al. pirABvp-Bearing Vibrio parahaemolyticus and Vibrio campbellii pathogens isolated from the Same AHPND-affected pond possess highly similar pathogenic plasmids. Front Microbiol. 2017;8:1859. doi: 10.3389/fmicb.2017.01859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ke HM, Prachumwat A, Yu CP, Yang YT, Promsri S, Liu KF, et al. Comparative genomics of Vibrio campbellii strains and core species of the Vibrio Harveyi clade. Sci Rep. 2017;7:41394. doi: 10.1038/srep41394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kondo H, Van PT, Dang LT, Hirono I. Draft genome sequence of non-Vibrio parahaemolyticus acute hepatopancreatic necrosis disease strain KC13.17.5, isolated from diseased shrimp in Vietnam. Genome Announc. 2015;3(5):e00978–15. doi: 10.1128/genomeA.00978-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu L, Xiao J, Zhang M, Zhu W, Xia X, Dai X, et al. A Vibrio owensii strain as the causative agent of AHPND in cultured shrimp, Litopenaeus vannamei. J Invertebr Pathol. 2018;153:156–164. doi: 10.1016/j.jip.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Restrepo L, Bayot B, Arciniegas S, Bajaña L, Betancourt I, Panchana F, Reyes Muñoz A. PirVP genes causing AHPND identified in a new Vibrio species (Vibrio punensis) within the commensal Orientalis clade. Sci Rep. 2018;8(1):13080. doi: 10.1038/s41598-018-30903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang H-C, Lin S-J, Mohapatra A, Kumar R, Wang H-C. A Review of the Functional Annotations of Important Genes in the AHPND-Causing pVA1 Plasmid. Microorganisms. 2020;8(7):996. doi: 10.3390/microorganisms8070996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Soto-Rodriguez SA, Gomez-Gil B, Lozano-Olvera R, Aguilar-Rendón KG, González-Gómez JP. Identification of new Vibrio campbellii strains harboring the pVA1 plasmid isolated from Penaeus vannamei postlarvae affected by outbreaks of acute hepatopancreatic necrosis disease (AHPND) in Mexico. Aquaculture. 2024;579:740221. doi: 10.1016/j.aquaculture.2023.740221. [DOI] [Google Scholar]
- 14.Dong X, Song J, Chen J, Bi D, Wang W, Ren Y, et al. Conjugative transfer of the PVA1-type plasmid carrying the PirABVP genes results in the formation of new AHPND-causing vibrio. Front Cell Infect Microbiol. 2019;9:195. doi: 10.3389/fcimb.2019.00195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aguilar-Rendón KG, Soto-Rodriguez SA, Gomez-Gil B, Lozano-Olvera R, Yáñez-Rivera B. Water microbiome dynamics of Pacific white shrimp Penaeus vannamei infected with Vibrio parahaemolyticus strains responsible for acute hepatopancreatic necrosis disease. Aquaculture. 2022;551:737871. doi: 10.1016/j.aquaculture.2021.737871. [DOI] [Google Scholar]
- 16.Xiao J, Liu L, Ke Y, Li X, Liu Y, Pan Y, Yan S. Shrimp AHPND-causing plasmids encoding the PirAB toxins as mediated by pirAB -Tn903 are prevalent in various Vibrio species. Nat Publ Group. 2016;2017:1–11. doi: 10.1038/srep42177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han JE, Tang KFJ, Aranguren LF, Piamsomboon P. Characterization and pathogenicity of acute hepatopancreatic necrosis disease natural mutants, pirABvp (‐) V. parahaemolyticus, and pirABvp (+) V. campbellii strains. Aquaculture. 2017;470:84–90. doi: 10.1016/j.aquaculture.2016.12.022. [DOI] [Google Scholar]
- 18.Kanrar S, Dhar AK. Complete Genome Sequence of a Novel Mutant Strain of Vibrio parahaemolyticus from Pacific White Shrimp (Penaeus vannamei) Genome Announc. 2018;6(24):e00497–18. doi: 10.1128/genomeA.00497-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.González-Gómez JP, Soto-Rodriguez S, López-Cuevas O, Castro-del Campo N, Chaidez C, Gomez-Gil B. Phylogenomic Analysis Supports Two Possible Origins for Latin American Strains of Vibrio parahaemolyticus Associated with Acute Hepatopancreatic Necrosis Disease (AHPND) Curr Microbiol. 2020;77(12):3851–3860. doi: 10.1007/s00284-020-02214-w. [DOI] [PubMed] [Google Scholar]
- 20.Han JE, Tang KFJ, Lightner DV. Genotyping of virulence plasmid from Vibrio parahaemolyticus isolates causing acute hepatopancreatic necrosis disease in shrimp. Dis Aquat Org. 2015;115(3):245–251. doi: 10.3354/dao02906. [DOI] [PubMed] [Google Scholar]
- 21.Yang C, Pei X, Wu Y, Yan L, Yan Y, Song Y, et al. Recent mixing of Vibrio parahaemolyticus populations. ISME J. 2019;13(10):2578–2588. doi: 10.1038/s41396-019-0461-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li P, Kinch LN, Ray A, Dalia AB, Cong Q, Nunan LM, et al. Acute hepatopancreatic necrosis disease-causing Vibrio parahaemolyticus strains maintain an antibacterial type VI secretion system with versatile effector repertoires. Appl Environ Microbiol . 2017;83(13):e00737–17. doi: 10.1128/AEM.00737-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osorio CR. T3SS effectors in Vibrios: Homology in sequence, diversity in biological functions? Virulence. 2018;9:721–723. doi: 10.1080/21505594.2018.1435965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okada N, Iida T, Park KS, Goto N, Yasunaga T, Hiyoshi H, et al. Identification and characterization of a novel type III secretion system in trh-positive vibrio parahaemolyticus strain TH3996 reveal genetic lineage and diversity of pathogenic machinery beyond the species level. Infect Immun. 2009;77(2):904–913. doi: 10.1128/IAI.01184-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salomon D, Gonzalez H, Updegraff BL, Orth K. Vibrio parahaemolyticus Type VI Secretion System 1 Is Activated in Marine Conditions to Target Bacteria, and Is Differentially Regulated from System 2. PLoS ONE. 2013;8(4):e61086. doi: 10.1371/journal.pone.0061086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lulijwa R, Rupia EJ, Alfaro AC. Antibiotic use in aquaculture, policies and regulation, health and environmental risks: a review of the top 15 major producers. Rev Aquac. 2019;12(2):640–663. doi: 10.1111/raq.12344. [DOI] [Google Scholar]
- 27.Stratev D, Fasulkova R, Krumova-Valcheva G. Incidence, virulence genes and antimicrobial resistance of Vibrio parahaemolyticus isolated from seafood. Microb Pathog. 2023;177:106050. doi: 10.1016/j.micpath.2023.106050. [DOI] [PubMed] [Google Scholar]
- 28.Changsen C, Likhitrattanapisal S, Lunha K, Chumpol W, Jiemsup S, Prachumwat A, et al. Incidence, genetic diversity, and antimicrobial resistance profiles of Vibrio parahaemolyticus in seafood in Bangkok and eastern Thailand. PeerJ. 2023;11:e15283. doi: 10.7717/peerj.15283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zaafrane S, Maatouk K, Alibi S, Mansour HB. Occurrence and antibiotic resistance of Vibrio parahaemolyticus isolated from the Tunisian coastal seawater. J Water Health. 2022;20(2):369–384. doi: 10.2166/wh.2022.243. [DOI] [PubMed] [Google Scholar]
- 30.Elmahdi S, DaSilva LV, Parveen S. Antibiotic resistance of Vibrio parahaemolyticus and Vibrio vulnificus in various countries: A review. Food Microbiol. 2016;57:128–134. doi: 10.1016/j.fm.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 31.Tan CW, Rukayadi Y, Hasan H, Thung TY, Lee E, Rollon WD, et al. Prevalence and antibiotic resistance patterns of Vibrio parahaemolyticus isolated from different types of seafood in Selangor. Malaysia. Saudi J Biol Sci. 2020;27(6):1602–1608. doi: 10.1016/j.sjbs.2020.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amalina NZ, Santha S, Zulperi D, Amal MNA, Yusof MT, Zamri-Saad M, Ina-Salwany MY. Prevalence, antimicrobial susceptibility and plasmid profiling of Vibrio spp. isolated from cultured groupers in Peninsular Malaysia. BMC Microbiol . 2019;19(1):251. doi: 10.1186/s12866-019-1624-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee LH, Ab Mutalib NS, Law JW, Wong SH, Letchumanan V. Discovery on antibiotic resistance patterns of Vibrio parahaemolyticus in Selangor reveals carbapenemase producing Vibrio parahaemolyticus in marine and freshwater fish. Front Microbiol . 2018;9:2513. doi: 10.3389/fmicb.2018.02513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu X, Cheng J, Wu Q, Zhang J, Xie T. Prevalence, characterization, and antibiotic susceptibility of Vibrio parahaemolyticus isolated from retail aquatic products in North China. BMC Microbiol. 2016;16(1):1–9. doi: 10.1186/s12866-016-0650-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Letchumanan V, Pusparajah P, Tan LTH, Yin WF, Lee LH, Chan KG. Occurrence and antibiotic resistance of Vibrio parahaemolyticus from Shellfish in Selangor, Malaysia. Front Microbiol. 2015;6:1417. doi: 10.3389/fmicb.2015.01417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tan CW, Malcolm TTH, Kuan CH, Thung TY, Chang WS, Loo YY, et al. Prevalence and antimicrobial susceptibility of Vibrio parahaemolyticus isolated from short mackerels (Rastrelliger brachysoma) in Malaysia. Front Microbiol. 2017;8:1087. doi: 10.3389/fmicb.2017.01087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garneau-Tsodikova S, Labby KJ. Mechanisms of resistance to aminoglycoside antibiotics: Overview and perspectives. MedChemComm: Royal Society of Chemistry; 2016. pp. 11–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Igbinosa EO, Beshiru A, Igbinosa IH, Ogofure AG, Uwhuba KE. Prevalence and Characterization of Food-Borne Vibrio parahaemolyticus From African Salad in Southern Nigeria. Front Microbiol. 2021;12:632266. doi: 10.3389/fmicb.2021.632266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bokma J, Vereecke N, Nauwynck H, Haesebrouck F, Theuns S, Pardon B, Boyen F. Genome-Wide Association Study Reveals Genetic Markers for Antimicrobial Resistance in Mycoplasma bovis. Microbiol Spectr. 2021;9(2):e0026221. doi: 10.1128/Spectrum.00262-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vereecke N, Botteldoorn N, Brossé C, Bonckaert C, Nauwynck H, Haesebrouck F, et al. Predictive Power of Long-Read Whole-Genome Sequencing for Rapid Diagnostics of Multidrug-Resistant Brachyspira hyodysenteriae Strains. Microbiol Spectr. 2023;11(1):e0412322. doi: 10.1128/spectrum.04123-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nishino K, Senda Y, Yamaguchi A. CRP regulator modulates multidruf resistance of escherichia coli by repressing the mdtEF Multidrug Efflux Genes. J Antibiot. 2008;61(3):120–127. doi: 10.1038/ja.2008.120. [DOI] [PubMed] [Google Scholar]
- 42.Singh H, Velamakanni S, Deery MJ, Howard J, Wei SL, Van Veen HW. ATP-dependent substrate transport by the ABC transporter MsbA is proton-coupled. Nat Commun. 2016;7:12387. doi: 10.1038/ncomms12387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee H, Hsu FF, Turk J, Groisman EA. The PmrA-regulated pmrC gene mediates phosphoethanolamine modification of lipid A and polymyxin resistance in Salmonella enterica. J Bacteriol. 2004;186(13):4124–4133. doi: 10.1128/JB.186.13.4124-4133.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Deekshit VK, Srikumar S. ‘To be, or not to be’—The dilemma of ‘silent’ antimicrobial resistance genes in bacteria. J Appl Microbiol. 2022;133:2902–2914. doi: 10.1111/jam.15738. [DOI] [PubMed] [Google Scholar]
- 45.Munita JM, Arias CA. Mechanisms of Antibiotic Resistance. Microbiol Spectr. 2016;4(2):10.1128/microbiolspec.VMBF-0016-2015. 10.1128/microbiolspec.VMBF-0016-2015. [DOI] [PMC free article] [PubMed]
- 46.Caro LFA, Mai HN, Kanrar S, Cruz-Flores R, Dhar AK. A mutant of vibrio parahaemolyticus pirABvp (+) that carries binary toxin genes but does not cause acute hepatopancreatic necrosis disease. Microorganisms. 2020;8(10):1–13. doi: 10.3390/microorganisms8101549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wick RR, Judd LM, Wyres KL, Holt KE. Recovery of small plasmid sequences via oxford nanopore sequencing. Microb Genom. 2021;7(8):000631. doi: 10.1099/mgen.0.000631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arumugam K, Bessarab I, Haryono MAS, Liu X, Zuniga-Montanez RE, Roy S, et al. Recovery of complete genomes and non-chromosomal replicons from activated sludge enrichment microbial communities with long read metagenome sequencing. NPJ Biofilms Microbiomes. 2021;7(1):23. doi: 10.1038/s41522-021-00196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arredondo-Alonso S, Pöntinen AK, Cléon F, Gladstone RA, Schürch AC, Johnsen PJ, et al. A high-throughput multiplexing and selection strategy to complete bacterial genomes. Gigascience. 2021;10(12):giab079. doi: 10.1093/gigascience/giab079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Johnson J, Soehnlen M, Blankenship HM. Long read genome assemblers struggle with small plasmids. Microb Genom. 2023;9(5):mgen001024. doi: 10.1099/mgen.0.001024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yu LH, Teh CSJ, Yap KP, Ung EH, Thong KL. Comparative genomic provides insight into the virulence and genetic diversity of Vibrio parahaemolyticus associated with shrimp acute hepatopancreatic necrosis disease. Infect Genet Evol . 2020;83:104347. doi: 10.1016/j.meegid.2020.104347. [DOI] [PubMed] [Google Scholar]
- 52.Nie D, Hu Y, Chen Z, Li M, Hou Z, Luo X, et al. Outer membrane protein A (OmpA) as a potential therapeutic target for Acinetobacter baumannii infection. J Biomed Sci. 2020;27:1–8. doi: 10.1186/s12929-020-0617-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Meng X, Huang D, Zhou Q, Ji F, Tan X, Wang J, Wang X. The Influence of Outer Membrane Protein on Ampicillin Resistance of Vibrio parahaemolyticus. Can J Infect Dis Med Microbiol. 2023;2023:8079091. doi: 10.1155/2023/8079091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu C, Ren H, Wang S, Peng X. Proteomic analysis of salt-sensitive outer membrane proteins of Vibrio parahaemolyticus. Res Microbiol. 2004;155(10):835–842. doi: 10.1016/j.resmic.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 55.He W, Yu G, Li T, Bai L, Yang Y, Xue Z, et al. Chaperone Spy Protects Outer Membrane Proteins from Folding Stress via Dynamic Complex Formation. mBio. 2021;12(5):e0213021. doi: 10.1128/mBio.02130-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu M, Chen S. A novel adhesive factor contributing to the virulence of Vibrio parahaemolyticus. Sci Rep. 2015;5:1–10. doi: 10.1038/srep14449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang D, Wang H. In Silico Approach Gives Insights into Ig-like Fold Containing Proteins in Vibrio parahaemolyticus: A Focus on the Fibrillar Adhesins. Toxins. 2022;14(2):133. doi: 10.3390/toxins14020133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Song X, Lin Z, Yuan W. Toxin–antitoxin systems in pathogenic Vibrio species: a mini review from a structure perspective. 3 Biotech. 2022;12(6):125. doi: 10.1007/s13205-022-03178-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kamruzzaman M, Wu AY, Iredell JR. Biological functions of type ii toxin-antitoxin systems in bacteria. Microorganisms. 2021;9(6):1276. doi: 10.3390/microorganisms9061276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Amitai S, Yassin Y, Engelberg-Kulka H. MazF-mediated cell death in Escherichia coli: A point of no return. J Bacteriol. 2004;186(24):8295–8300. doi: 10.1128/JB.186.24.8295-8300.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Konieczna I, Arnowiec P, Kwinkowski M, Kolesiska B, Frczyk J, Kamiski Z, Kaca W. Bacterial Urease and its Role in Long-Lasting Human Diseases. Curr Protein Pept Sci. 2012;13(8):789–806. doi: 10.2174/138920312804871094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sujeewa AKW, Norrakiah AS, Laina M. Prevalence of toxic genes of Vibrio parahaemolyticus in shrimps (Penaeus monodon) and culture environment. Int Food Res J. 2009;16:89–95. [Google Scholar]
- 63.Park K-S, Iida T, Yamaichi Y, Oyagi T, Yamamoto K, Honda T. Genetic Characterization of DNA Region Containing the trh and ure Genes of Vibrio parahaemolyticus. Infect Immun. 2000;68(10):5742–8. doi: 10.1128/IAI.68.10.5742-5748.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ellingsen AB, Olsen JS, Granum PE, Rørvik LM, González-Escalona N. Genetic characterization of trh positive Vibrio spp. isolated from Norway. Front Cell Infect Microbiol . 2013;3:107. doi: 10.3389/fcimb.2013.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Baliga P, Shekar M, Venugopal MN. Investigation of direct repeats, spacers and proteins associated with clustered regularly interspaced short palindromic repeat (CRISPR) system of Vibrio parahaemolyticus. Mol Genet Genomics. 2019;294(1):253–262. doi: 10.1007/s00438-018-1504-8. [DOI] [PubMed] [Google Scholar]
- 66.Sun H, Li Y, Shi X, Lin Y, Qiu Y, Zhang J, et al. Association of CRISPR/cas evolution with vibrio parahaemolyticus virulence factors and genotypes. Foodborne Pathog Dis. 2015;12(1):68–73. doi: 10.1089/fpd.2014.1792. [DOI] [PubMed] [Google Scholar]
- 67.McDonald ND, Regmi A, Morreale DP, Borowski JD, Fidelma Boyd E. CRISPR-Cas systems are present predominantly on mobile genetic elements in Vibrio species. BMC Genomics. 2019;20(1):105. doi: 10.1186/s12864-019-5439-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vandeputte M, Verhaeghe M, Willocx L, Bossier P, Vanrompay D. Bovine Lactoferrin and Hen Ovotransferrin Affect Virulence Factors of Acute Hepatopancreatic Necrosis Disease (AHPND)-Inducing Vibrio parahaemolyticus Strains. Microorganisms . 2023;11(12):2912. doi: 10.3390/microorganisms11122912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.De Coster W, Rademakers R. NanoPack2: population-scale evaluation of long-read sequencing data. Bioinformatics. 2023;39(5):btad311. doi: 10.1093/bioinformatics/btad311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kolmogorov M, Yuan J, Lin Y, Pevzner PA. Assembly of long, error-prone reads using repeat graphs. Nat Biotechnol. 2019;37(5):540–546. doi: 10.1038/s41587-019-0072-8. [DOI] [PubMed] [Google Scholar]
- 71.Vaser R, Šikić M. Time- and memory-efficient genome assembly with Raven. Nature Computational Science. 2021;1(5):332–336. doi: 10.1038/s43588-021-00073-4. [DOI] [PubMed] [Google Scholar]
- 72.Ruan J, Li H. Fast and accurate long-read assembly with wtdbg2. Nat Methods. 2020;17(2):155–158. doi: 10.1038/s41592-019-0669-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Li H. Minimap2: pairwise alignment for nucleotide sequences. Bioinformatics. 2018;34(18):3094–3100. doi: 10.1093/bioinformatics/bty191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Parks DH, Imelfort M, Skennerton CT, Hugenholtz P, Tyson GW. CheckM: Assessing the quality of microbial genomes recovered from isolates, single cells, and metagenomes. Genome Res. 2015;25(7):1043–1055. doi: 10.1101/gr.186072.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jolley KA, Bliss CM, Bennett JS, Bratcher HB, Brehony C, Colles FM, et al. Ribosomal multilocus sequence typing: universal characterization of bacteria from domain to strain. Microbiology. 2012;158(4):1005–1015. doi: 10.1099/mic.0.055459-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yoon SH, Ha SM, Lim J, Kwon S, Chun J. A large-scale evaluation of algorithms to calculate average nucleotide identity. Antonie Van Leeuwenhoek. 2017;110(10):1281–6. doi: 10.1007/s10482-017-0844-4. [DOI] [PubMed] [Google Scholar]
- 77.Alcock BP, Huynh W, Chalil R, Smith KW, Raphenya AR, Wlodarski MA, et al. CARD 2023: expanded curation, support for machine learning, and resistome prediction at the Comprehensive Antibiotic Resistance Database. Nucleic Acids Res. 2023;51(1 D):D690–D9. doi: 10.1093/nar/gkac920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kaas RS, Leekitcharoenphon P, Aarestrup FM, Lund O. Solving the problem of comparing whole bacterial genomes across different sequencing platforms. PLoS ONE. 2014;9(8):e104984. doi: 10.1371/journal.pone.0104984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Delcher AL, Salzberg SL, Phillippy AM. Using MUMmer to Identify Similar Regions in Large Sequence Sets. Curr Protoc Bioinformatics. 2003;00:10.3.1–10.3.18. 10.1002/0471250953.bi1003s00. [DOI] [PubMed]
- 80.Vereecke N, Van Hoorde S, Sperling D, Theuns S, Devriendt B, Cox E. Virotyping and genetic antimicrobial susceptibility testing of porcine ETEC/STEC strains and associated plasmid types. Front Microbiol. 2023;14:1139312. doi: 10.3389/fmicb.2023.1139312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Letunic I, Bork P. Interactive tree of life (iTOL) v5: An online tool for phylogenetic tree display and annotation. Nucleic Acids Res. 2021;49(W1):W293–W296. doi: 10.1093/nar/gkab301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schwengers O, Jelonek L, Dieckmann MA, Beyvers S, Blom J, Goesmann A. Bakta: Rapid and standardized annotation of bacterial genomes via alignment-free sequence identification. Microb Genom. 2021;7(11):000685. doi: 10.1099/mgen.0.000685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gilchrist CLM, Chooi YH. Clinker & clustermap.js: Automatic generation of gene cluster comparison figures. Bioinformatics. 2021;37(16):2473–5. doi: 10.1093/bioinformatics/btab007. [DOI] [PubMed] [Google Scholar]
- 84.Page AJ, Cummins CA, Hunt M, Wong VK, Reuter S, Holden MTG, et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics. 2015;31(22):3691–3693. doi: 10.1093/bioinformatics/btv421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Brynildsrud O, Bohlin J, Scheffer L, Eldholm V. Rapid scoring of genes in microbial pan-genome-wide association studies with Scoary. Genome Biol. 2016;17(1):238. doi: 10.1186/s13059-016-1108-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The draft sequences of all three Vibrio parahaemolyticus strains can be found on NCBI (Vp M0904 CP133891-CP133899, Vp PV1 JAVKPG000000000, Vp TW01 CP133900-CP133905).