Abstract
Introduction
Chronic cervical radiculopathy is a common condition characterised by neck and arm pain, numbness and weakness. Both neck muscle activation and strengthening exercises are widely recognised treatments for cervical radiculopathy, but there is a research gap on the efficacy of neck muscle activation versus strengthening. This protocol will determine the efficacy of neck muscle activation alongside conventional care versus strengthening exercise and conventional care for cervical radiculopathy.
Methods and analysis
We planned a 5-week parallel, two-arm randomised clinical trial on 80 participants with chronic cervical radiculopathy (lasting over 3 months) between July and December 2023. Participants will be recruited from Dhaka’s Agrani Specialised Physiotherapy Centre in Bangladesh and randomly assigned to two groups in a 1:1 ratio. Both groups will receive 14 sessions, each lasting 30–45 min. Post-treatment evaluations will be employed on Brief Pain Inventory (BPI), range of motion, craniovertebral angle (CVA), strength, endurance and Neck Disability Index (NDI) after 5 weeks and follow-up after 12 weeks of post-test analysis. Primary outcomes (strength, endurance and CVA) will be measured using a handheld dynamometer, digital inclinometer and goniometer. Secondary outcomes (pain, range of motion and disability) will be assessed through the BPI scale, digital inclinometer and NDI.
Ethics and dissemination
The Institute of Physiotherapy Rehabilitation and Research of Bangladesh Physiotherapy Association has approved the study. All participants will provide informed consent, and data will be anonymised and accessible only to authorised personnel. The study’s findings will be disseminated in peer-reviewed journals and conferences.
Clinical trial registry India
CTRI/2023/09/057587 (13/09/2023)
Keywords: Cervical spine, Muscle damage/injuries, Disability, Physical Therapy, Strength isometric isokinetic
WHAT IS ALREADY KNOWN ON THIS TOPIC
Before this study, the existing scientific knowledge on chronic cervical radiculopathy highlighted the efficacy of neck muscle activation and strengthening exercises as individual treatments. However, a notable research gap persisted regarding directly comparing these two approaches.
WHAT THIS STUDY ADDS
This study addresses the need for comparative evidence, aiming to discern the superior efficacy between activation and strengthening exercises and find out valuable outcomes on Brief Pain Inventory, range of motion, craniovertebral angle, strength, endurance and Neck Disability Index to guide clinicians and researchers in optimising therapeutic interventions for individuals with chronic cervical radiculopathy.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
By establishing the relative efficacy of neck muscle activation and strengthening exercises, our study will highlight evidence-based practices and guide physiotherapists and healthcare professionals in tailoring interventions for better patient outcomes. Additionally, these insights could influence future research directions, paving the way for more targeted investigations related to the rehabilitation of individuals suffering from chronic cervical radiculopathy.
Introduction
Cervical radiculopathy, a condition characterised by nerve root compression in the neck, is a rising global concern.1 It leads to persistent pain, weakness and sensory changes, lasting beyond the typical healing period of 3–6 months.2 Neck pain, affecting over 30% of individuals annually, ranks as the fourth-leading cause of disability.3 Remarkably, 20%– 70% of people will experience neck pain disrupting their daily lives at some point.4 Recent data from the European Journal of Pain reveal that cervical radiculopathy results in disability for approximately 352.0 cases per 100 000 individuals worldwide over the past 3 decades.4 Notably, the incidence of cervical radiculopathy stands at 83.2 cases per 100 000 people, with the highest occurrence between ages 40 and 50.5 6 This translates to a yearly incidence of 107.3 cases per 100 000 men and 63.5 cases per 100 000 women.5
Herniated cervical discs, mainly affecting the C6 or C7 nerve roots in 80% of cases, lead to cervical radiculopathy.6 Symptoms encompass neck discomfort, radiating arm or shoulder pain, numbness, tingling, upper-limb weakness and altered reflexes.6 Diagnosis relies on clinical assessment, MRI and a manual spurling’s test.7 8 When substantial nerve root compression causes radiculopathy, it is expected to result in muscular weakness in the specific muscle innervated by that affected nerve root.9 Studies have confirmed increased muscle fatigue and reduced neck muscle function in patients with cervical radiculopathy.10 These statistics underscore the growing prevalence and impact of cervical radiculopathy, emphasising the need for effective management and prevention strategies. Therapeutic exercises, including muscle strengthening, stretching and stabilisation, are vital for mitigating these effects and promoting recovery in chronic neck and nerve pain.11 12
Strengthening the neck muscles is pivotal in enhancing cervical spine stability and alleviating the burden on adjacent muscles and joints.13–15 Some randomised controlled trials targeting chronic neck pain have demonstrated the efficacy of exercises, particularly deep neck flexor activation and strengthening, in significantly reducing pain levels compared with non-exercisers.16 17 However, the specific impact of neck muscle activation training versus strengthening remains inadequately studied, particularly in chronic cervical radiculopathy. This research gap necessitates a closer examination of the outcomes associated with activation training versus strengthening for patients with cervical radiculopathy. Neck muscles are crucial in upholding proper posture and cervical spine stability. Weakness or imbalance in these muscles can lead to poor posture, reduced cervical stability and increased stress on other neck structures like intervertebral discs and facet joints. Individuals with chronic cervical radiculopathy may enhance their posture, elevate functional capabilities and mitigate stress on other neck structures by activating or strengthening these muscles. Hence, there is a compelling need for targeted exercises to discern their comparative efficacy on cervical muscle function.
So, this study aims to evaluate the efficacy of neck muscle activation versus strengthening for adults with chronic cervical radiculopathy. The specific objectives are to (1) determine the sociodemographic status related to chronic cervical radiculopathy; (2) evaluate the baseline comparability between two groups at the pretest; (3) find out the effect on pain, range of motion, strength and endurance after neck muscle activation and strengthening at post-test, and follow-up; and (4) estimate the status of disability at post-test and follow-up. The study has two-tailed hypotheses. The activation or strengthening group will exhibit noticeably greater improvements in muscle strength, endurance, pain relief, posture, range of motion and reduction of disability for chronic cervical radiculopathy at 5 weeks after being recruited into the study.
Methods
Study design
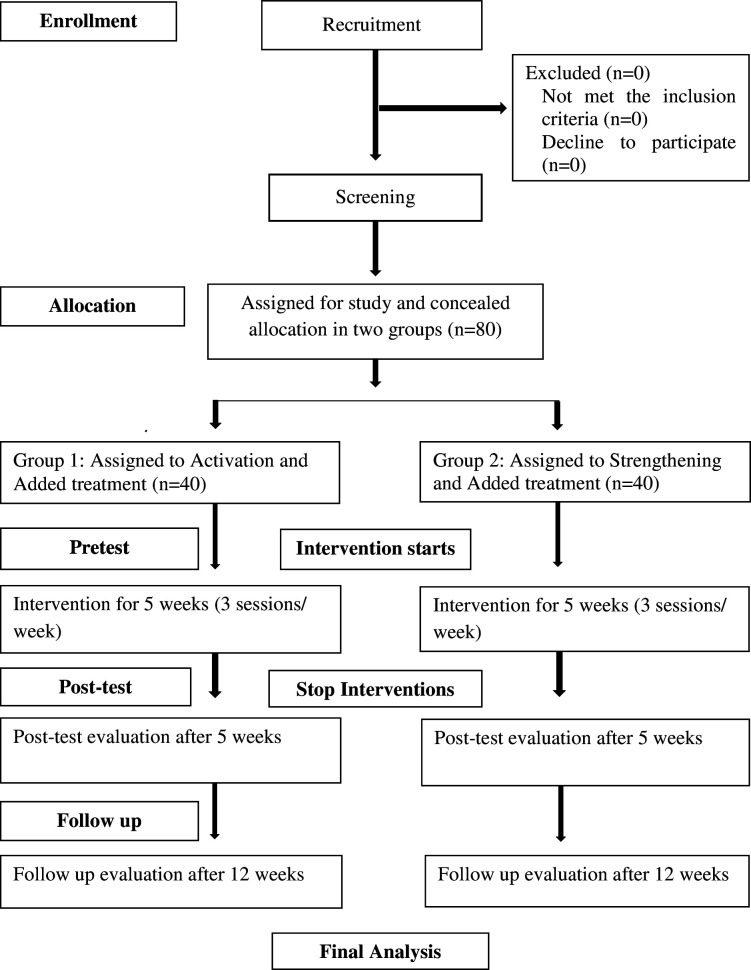
This investigation will be a single-centred, parallel, assessor and patient-blinded randomised clinical trial carried out for 5 weeks with an additional follow-up period of 12 weeks from September 2023 to November 2023 at Agrani Specialized Physiotherapy Center in Dhaka, Bangladesh. The protocol has been developed in line with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) statement, which aims to improve the clarity and comprehensiveness of research content (table 1). The trial findings will be reported following the rules of the Consolidated Standards of Reporting Trials statement, which ensures transparent and comprehensive reporting of findings (figure 1).
Table 1.
Overview of standard procedure and data collection according to Standard Protocol Items: Recommendations for Interventional Trials 2013 criteria
| Time point | Enrolment | Allocation | Postallocation | ||
| -T1 | T0 | T1 | T2 | T3 | |
| Enrolment | |||||
| Eligibility screen | X | ||||
| Informed consent | X | ||||
| Demographic assessment | X | ||||
| Group allocation | X | ||||
| Intervention | |||||
| Neck muscles activation | X | X | |||
| Neck muscles strengthening | X | X | |||
| Conventional care | X | X | |||
| Assessment | |||||
| BPI | X | X | X | ||
| ROM | X | X | X | ||
| Muscle strength | X | X | X | ||
| Endurance | X | X | X | ||
| CVA | X | X | X | ||
| NDI | X | X | X | ||
BPI, Brief Pain Inventory; CVA, craniovertebral angle; NDI, Neck Disability Scale; ROM, range of motion; T0, group allocation; -T1, prestudy enrolment; T1, baseline before the intervention; T2, measurement taken in 5 weeks after T1; T3, measurement taken after 12 weeks of T1.
Figure 1.
Reporting guideline (Consolidated Standards for Reporting Trials)
Study setting
Patients seeking treatment for chronic cervical radiculopathy will be recruited via hospital-based simple randomisation at the Agrani Specialized Physiotherapy Center in Dhaka. Eligible participants, providing voluntary written consent, will be allocated to either the neck muscle activation with conventional care group or the neck muscle strengthening with conventional care group via computer-generated concealed allocation in a 1:1 ratio. Blinding will be maintained for patients and assessors to prevent data cross-contamination, while physiotherapists delivering interventions will be fully informed about the treatments.
Sample size calculation
The study necessitates a sample size of 74 participants, calculated based on the anticipated minimal clinically important differences (MCID) in neck strength using a handheld dynamometer (14.20±6.52).18 Using a 30% minimal clinical improvement at baseline, the absolute difference between the two means was 4.26, as the mean of group one was 14.2 and group two was 9.94. In this study, with an enrolment ratio of 1:1, the probability of type II error with 80% statistical power was .84, and the probability of type I error was 0.05 (alpha value), which concluded that 37 individuals with chronic cervical radiculopathy would be assigned to each group, totalling 74 participants. Allowing a 20% dropout rate, we intended to include 40 patients in each group, resulting in 80 participants. Power analysis, conducted using ClinCalc software, focused on the key outcome of the neck-strength assessment.
Recruitment and screening procedures
From September to November 2023, patients with chronic cervical radiculopathy at the Agrani Specialized Physiotherapy Center in Dhaka, Bangladesh will be assessed for eligibility and randomly selected. Eligible participants will undergo baseline assessment, and randomisation will occur just before the first treatment session. Here is a more detailed explanation of the patient recruitment and screening process:
A research assistant will assess patient eligibility.
Eligible patients will provide written informed consent.
Randomisation using concealed allocation will assign patients to either the neck muscle activation with the conventional care group or neck muscle strengthening with the conventional care group.
Patients will remain blinded to their group assignment.
Baseline assessments will be conducted for all participants.
Treatment sessions commence immediately following the completion of baseline assessments.
This recruitment and screening process is designed to ensure that the study is conducted fairly and unbiasedly.
Eligibility criteria
A screening procedure will be used to evaluate if participants meet the study’s inclusion and exclusion requirements.
Inclusion criteria
To qualify for participation, participants must meet at least two or three of the following chronic cervical radiculopathy criteria8: (1a) presence of radicular pain on one or both sides of the body and may or may not be accompanied by neck pain, (1b) symptoms like paresthesia, numbness, weakness or altered reflexes in C2-C8 dermatome or myotome and (1c) MRI confirmation of nerve root compression related to clinical findings. Additional inclusion criteria are as follows: (2) age 18–50 with informed consent,19 20 (3) any gender,19 21 (4) chronic cervical radiculopathy duration over 3 months, (5) Neck Disability Index (NDI) score <15/50,14 16 (6) Brief Pain Inventory (BPI) severity score 1–6 on an 11-point scale20 and (7) poor performance on craniocervical flexion test. Patients cannot elevate the target pressure from 20 mm Hg to 22 mm Hg and hold for 3 s before returning to the initial relaxing position.14 21
Exclusion criteria
Conversely, participants will be excluded if they have (1) prior cervical spine surgery14 16 19; (2) a history of congenital/acquired postural deformity, tumour, instability, inflammatory disease, spinal cord compression, fracture or infection19 21; and (3) inability to increase blood pressure by at least 4 mm Hg beyond the initial 20 mm Hg during the second-stage pressure.16
Randomisation procedures
Potential participants who are found to be eligible and participants who consent to participate in the study will be concealed allocation randomly assigned to one of the physiotherapy intervention groups. A computer-generated sequence will randomly assign participants to receive neck muscle activation or strengthening exercises. The ‘rand’ function in Microsoft Excel 2010 will perform concealed allocation to groups once the sample is collected. Both patients and outcome assessors who fill out the questionnaire will remain blinded to group allocation, but physiotherapists will be well informed about the interventions.
Blinding
To prevent bias, participants will be unaware of the study hypothesis and interventions in the other group. Treating clinicians cannot be blinded, but outcome assessors and patients will be. In the informed consent, participants will be aware of the interventions and blinded to group allocation. They will not know about their assigned group. We will use a consent envelope, and the patient will be treated in two separate rooms on two different floors after the allocation. Different assessors for each group will be assigned, and an uninvolved individual will handle randomisation. A trial manager and an independent monitoring team will oversee the study for coordination and oversight. This blinding procedure is important to ensure that the study results are not biased by participants’ knowledge of their group allocation.
Details of the intervention
Two physiotherapists with over 8 years of extensive practical experience in manual therapy and the Structural Diagnosis and Management (SDM) approach, including isolated contractions, activations and strengthening of the cervical muscles, will treat the patients. First, the patient will be assessed through cervical spine assessment of SDM by the experienced physiotherapist and selected for the interventions. To maintain consistency in the delivery of the interventions, the therapists will regularly assess each other’s treatment sessions. Additionally, a researcher not directly involved in delivering the interventions will conduct audits to ensure that the treatments follow the study protocol.
The two groups of participants will undergo two distinct treatments lasting for 5 weeks. One group will receive muscle activation, while the other will receive strengthening exercises supplemented with additional treatment.
Neck muscle activation + added treatment (experimental)
The experimental group will receive neck muscle activation and added treatment consisting of a SDM approach for the neck.
On the first five sessions, the patient will receive the following: a graded myofascial release for 3–5 min, exceeding not more than 7–10 with 1 min interval ×2 sets on the upper trapezius, scalene, supraspinatus, sternocleidomastoid, levator scapulae and pectoralis major; stretching for 5–7 repeats (reps) with 15–30 s hold ×3 sets on the upper trapezius, scalene, supraspinatus, sternocleidomastoid, levator scapulae and pectoralis major; and neural stretching for 3 reps with 30 s hold with 1 min rest ×3 sets on the radial, median, ulnar nerve and cold compression for 10 min. After that, within the sixth–10th sessions, the patient will receive previous treatment along with activation exercise for 5–15 slow reps 3 times/day at an intensity of 20%–75% of maximal voluntary contraction of the pectoralis major, triceps and scapular stabilisers, and during the 10th–14th sessions, neck flexors, extensor and rotator activation will be added with previous treatment.
Neck muscle strengthening + added treatment (control)
The control group will receive neck muscle strengthening exercises and added treatment consisting of a SDM approach for the neck.
On the first five sessions, the patient will receive the following: a graded myofascial release for 3–5 min, exceeding not more than 7–10 with 1 min interval ×2 sets on the upper trapezius, scalene, supraspinatus, sternocleidomastoid, levator scapulae and pectoralis major, stretching exercise for 5–7 reps with 15–30 s hold ×3 sets on the upper trapezius, scalene, supraspinatus, sternocleidomastoid, levator scapulae and pectoralis major; and neural stretching for 3 reps with 30 s hold with 1 min rest ×3 sets on the radial, median, ulnar nerve and cold compression for 10 min. After that, within the sixth–10th sessions, the patient will receive previous treatment along with isometric strengthening for four sets ×2 min of isometric contraction with 1–3 min rest between sets, 3 days per week, at an intensity of 30%–40% of maximal voluntary contraction of the pectoralis major, triceps and scapular stabilisers, and during the 10th–14th sessions, neck flexors, extensor and rotator strengthening will be added with previous treatment.
Progression of interventions
For both groups, the initial physiotherapy sessions will be 1 hour long, and subsequent sessions will be provided daily, each lasting 30–45 min. Patients will get care three times each week throughout the 5 weeks of the intervention period. The frequency and duration of treatment will vary with each patient pragmatically. The duration and number of treatments will be monitored.
Outcome measures and assessment points
The main outcome measures will focus on neck muscle strength, endurance and craniovertebral angle (CVA). Secondary outcomes will assess pain levels, range of motion and disability. Generalised predictors and moderators will encompass sociodemographic information such as age, gender, duration of symptoms, MRI results and family history, among other factors associated with chronic cervical radiculopathy.
Sociodemographic information
The researcher will prepare a structured questionnaire to collect participants’ sociodemographic information, including personal details, demographics and other disease-related information.
Primary outcomes
Neck muscle strength
A standard and certified automated portable dynamometer (activforce 2) will assess isometric neck strength. Fixed-framed dynamometers have been proven reliable, where the concurrent validity was moderate to good for all measurements. Intraclass correlation values were 0.74 for flexion, 0.82 for extension, 0.74 for right lateral flexion and 0.68 for left lateral flexion, for measuring cervical muscle force in both individuals with and without neck disorders, with measurements recorded in kilogram-force (kgf).22
Neck muscle endurance
Cervical muscle endurance will be assessed by timing participants’ ability to maintain specific positions via stopwatch, which has proven reliable. Participants will lift their head 2.5 cm off the ground for cervical flexors with a tucked chin. For cervical extensors, they will lay face down with their head extended and chin retracted. The minimal detectable change for flexor endurance is 17.8 s, and the minimal clinically relevant difference for extensor endurance is 73 s. Reliability was excellent for the neck flexor test (intraclass correlation coefficient (ICC)=0.93) and good for the neck extensor test (ICC=0.88).23
Craniovertebral angle
Measuring the CVA involves assessing the alignment between the head and cervical spine. This process includes taking two side-view photographs of a seated individual without back support. Specific markings are made from the seventh cervical vertebra (C7) to the ear tragus, forming a right angle at C7.24 Goniometry, a widely accepted method for measuring joint range of motion determines the angle between the horizontal line and the line connecting C7 to the ear tragus. This technique is suitable for measuring the CVA, for which Cronbach’s alpha value of 0.893 showed good internal consistency.25
Secondary outcome
Pain
The pain level will be evaluated using BPI, a widely endorsed tool for evaluating musculoskeletal pain outcomes. It consists of three subscales: pain severity, affective interference and physical interference. In BPI, a 0–10 scale gauges pain intensity, with the mean of four items computed. There was good overall internal consistency (Cronbach’s alpha: 0.87) in the BPI scale. Test-retest reliability was excellent for pain intensity and interference scores of Short-Form BPI (ICC: 0.90 and 0.96, respectively), as well as inter-rater reliability for both dimensions (ICC: 0.77).26
Range of motion
The digital inclinometer (activforce 2) will assess the cervical spine’s range of motion, offering precise measurements of joint movement. This inclinometer method is the standard for evaluating cervical spine rotations, including sagittal, frontal, transversal and rotational movements. Intraclass correlation values for flexion, extension, lateral flexion and rotation range from 0.89 to 0.94, demonstrating excellent measurement reliability.27
Disability
NDI will assess disability from cervical radiculopathy. It is a validated tool, widely used in research and clinical contexts, and reliably measures self-reported disability in patients with cervical radiculopathy. Test-retest reliability was moderate for the NDI (ICC=0.68; 95% CI, 0.30 to 0.90).28
Study procedure and data collection methods
Eligible participants will receive a study explanation and written informed consent after initial screening from data collectors. Baseline assessments will gather sociodemographic data and clinical information, conduct BPI, measure range of motion, assess muscle strength and endurance, determine CVA and evaluate neck disability using NDI. Two assessors from three different centres will complete these assessments using a questionnaire. Once baseline assessments are completed, files will be collected, and participants will be randomly assigned to their respective groups using a concealed process. After 5 weeks, blinded assessors will conduct post-treatment and follow-up assessments after 12 weeks, including pain, range of motion, CVA, strength, endurance and disability.
The quality of the interventional study, study procedure and data collection methods will be ensured by adhering to this experiment’s SPIRIT 2023 criteria (table 1).
Data management
Regular checks will scrutinise files for omissions or errors to ensure data integrity. Data will be double-checked by the assessors every day after the assessment, and the trial manager, principal investigator and data auditors will have access to the final trial data set. After completing the trials, all the authors will have equal access to the anonymous data. All the hard copies and soft copies of data collection will be kept to the principal investigator, and there will not be any disclosure or access to the identification of trial patients. There will be post-trial care only if any adverse effects are noted during the trial. Manual data entry will be held twice for error reduction. Electronic data will be securely stored on password-protected servers at the postgraduate programme in physiotherapy and rehabilitation. Each participant will have an identification number, and all data will be encoded using this number. A separate list of identification numbers will be securely maintained apart from deidentified data. Statistical analysis will use deidentified data, and results will be presented in aggregated form to protect confidentiality.
Statistical analysis
Data analysis will be conducted by a statistician using SPSS V.22 for Windows, with encoded data. Normal distribution will be assessed through the Kolmogorov-Smirnov test, Shapiro-Wilk test, bell curve, kurtosis and skewness. Descriptive statistics, such as mean, SD, frequency and percentage, will summarise categorical and continuous data. Multivariate analysis of variance and Analysis of variance test will be conducted to determine between groups among observation change. Based on data distribution, baseline comparability among two-group and between-group analysis will be assessed using the Mann-Whitney or Independent t-test. Within-group analysis will be determined with paired sample t-tests or the Wilcoxon test. Intention-to-treat analysis will address missing data issues.
Monitoring
Two individuals not involved directly in the trial will form the monitoring team. Their responsibilities will include monitoring the intervention protocol, adverse effects and group enrolment of participants. Additionally, they will review the data and conduct an interim analysis. The principal investigator will inform the Ethical Review Board of any study methods or treatment changes.
Safety measures and adverse effect management
While the treatment is expected not to yield significant adverse events, the monitoring team will vigilantly watch for unforeseen incidents during and after the intervention, promptly notifying relevant professionals. Any occurrences will be documented in the treating therapist’s SOAP note and reported to the primary investigator. Patients will be preinformed about potential pain, skin irritation or discomfort and advised to contact their physiotherapist promptly if these issues arise. A comprehensive report will be included in the trial’s final publication if any serious adverse effects emerge. The lead investigator will inform the Institutional Review Board of any intervention or technique modifications through the monitoring team.
Ethical issues and informed consent
The trial received ethical approval from the Institute of Physiotherapy Rehabilitation and Research, Bangladesh Physiotherapy Association, on 1 July 2023 (Approval Number: BPA-IPRR/IRB/992/07/2023/652). It was also prospectively registered with the Clinical Trial Registry India (CTRI) on 13 September 2023, with registration number CTRI/2023/09/057587. Ethical guidelines, following the Helsinki Declaration, will be strictly adhered to. Participants will provide written informed consent before enrolment, and their participation is entirely voluntary, with the option to withdraw without impacting their treatment. Completed data will be anonymised and accessible only to authorised personnel. Confidentiality agreements bind investigators involved in data collection. Post-trial treatment will be provided in case of unfavourable consequences.
Study status
Participant recruitment for the study has started recruiting patients.
Dissemination
On completion of the trial, the research findings will be disseminated as follows: First, a seminar will be organised to present the results to physiotherapists, researchers and healthcare professionals. Second, an original research paper will be submitted to a peer-reviewed journal indexed in a database, expanding the reach of the findings. Third, training sessions for physiotherapists will be conducted, sharing the most effective treatment approach. Lastly, the study’s results will be published as an open-access journal article, ensuring accessibility to all, irrespective of financial constraints. These efforts aim to maximise the impact on patients with chronic cervical radiculopathy.
Discussion
This current study aimed to compare the efficacy of neck muscle activation versus strengthening interventions in patients with chronic cervical radiculopathy, addressing a global issue of increasing neck pain-related functional limitations.1 Estimates suggest that 20%–70% of the population will experience neck pain at some point, leading to muscle weakness and altered function, often contributing to chronic cervical radiculopathy.4 7 12 13 Numerous studies have explored neck muscle activation and strengthening exercises for neck pain and patients with chronic cervical radiculopathy.16 17 19 29 30 However, no study has directly compared the efficacy of these two approaches. Given the limited supporting evidence, a well-designed randomised clinical trial is crucial to guide physiotherapists’ clinical decisions. This study is meticulously designed to ensure a sample size capable of detecting significant treatment effects while minimising biases. It closely replicates interventions administered by experienced physiotherapists specialising in musculoskeletal conditions, particularly cervical spine issues. This emphasis on mirroring real-world clinical practice enhances the study’s relevance and applicability. Ultimately, the findings will contribute to the understanding of optimal treatments for chronic cervical radiculopathy, addressing a condition that significantly impacts neck pain and function globally. By comparing activation and strengthening interventions, this research fills a critical gap in the current knowledge and provides valuable guidance to clinicians facing treatment decisions for patients with chronic cervical radiculopathy.
In summary, this study will compare the efficacy of two treatment approaches for chronic cervical radiculopathy: neck muscle activation and neck muscle strengthening, both with conventional care. The findings of this study will help clinicians guide their clinical decision-making by providing evidence on the most effective treatment approach for chronic cervical radiculopathy.
The study will also provide important information for patients with cervical radiculopathy, who can use the findings to make informed decisions about their treatment.
Here are some of the specific benefits of this study:
It will provide the first direct comparison of neck muscle activation and neck muscle strengthening for cervical radiculopathy.
It will be conducted in a rigorous, randomised clinical trial design.
It will include a large sample size of patients with cervical radiculopathy.
It will measure various outcomes, including pain, range of motion, strength, endurance, CVA and disability.
The findings of this study will be valuable to clinicians, patients and researchers. They will help to improve the understanding of cervical radiculopathy and the development of more effective treatment options.
bmjsem-2023-001819supp001.pdf (403.9KB, pdf)
bmjsem-2023-001819supp002.pdf (46.6KB, pdf)
Acknowledgments
The authors acknowledge Dr M Shahadat Hossain and Dr Sapia Akter from the Agrani Specialized Physiotherapy Center for their guidelines in preparing the intervention for the protocol and giving permission to use the data collection tools from their department.
Footnotes
Contributors: FSS: conceptualisation, methodology, writing original draft, writing review and editing. MAI: writing review and editing. KMAH: supervision and formal analysis. FK: writing review and editing, and validation. MZH: resources and validation. SJ: investigation. ER: data curation.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. Electronic data will be securely stored on password-protected servers at the postgraduate programme in physiotherapy and rehabilitation. Each participant will have an identification number, and all data will be encoded using this number. A separate list of identification numbers will be securely maintained apart from deidentified data. Completed data will be anonymised and accessible only to authorised personnel.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the Ethics Committee(s) or Institutional Board(s): Bangladesh Physiotherapy Association, Institute of Physiotherapy, Rehabilitation and Research Review Board (reference number or ID: BPA-IPRR/IRB/992/07/2023/652). Participants gave informed consent to participate in the study before taking part.
References
- 1.Rodine RJ, Vernon H. Cervical radiculopathy: a systematic review on treatment by spinal manipulation and measurement with the neck disability index. J Can Chiropr Assoc 2012;56:18–28.:22457538. [PMC free article] [PubMed] [Google Scholar]
- 2.Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International classification of diseases (ICD-11). Pain 2019;160:19–27. 10.1097/j.pain.0000000000001384 [DOI] [PubMed] [Google Scholar]
- 3.Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc 2015;90:284–99. 10.1016/j.mayocp.2014.09.008 [DOI] [PubMed] [Google Scholar]
- 4.Childs JD, Cleland JA, Elliott JM, et al. Neck pain: clinical practice guidelines linked to the International classification of functioning, disability, and health from the Orthopaedic section of the American physical therapy Association. The Journal of Women’s & Pelvic Health Physical Therapy 2011;35:57–90. 10.1097/JWH.0b013e3182267762 [DOI] [PubMed] [Google Scholar]
- 5.Safiri S, Kolahi A-A, Hoy D, et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: systematic analysis of the global burden of disease study 2017. BMJ 2020;368:m791. 10.1136/bmj.m791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radhakrishnan K, Litchy WJ, O’Fallon WM, et al. Epidemiology of cervical radiculopathy: a population-based study from rochester, Minnesota, 1976. Brain 1994;117:325–35. 10.1093/brain/117.2.325 [DOI] [PubMed] [Google Scholar]
- 7.Mansfield M, Smith T, Spahr N, et al. Cervical spine radiculopathy epidemiology: a systematic review. Musculoskeletal Care 2020;18:555–67. 10.1002/msc.1498 [DOI] [PubMed] [Google Scholar]
- 8.Lam KN, Heneghan NR, Mistry J, et al. Classification criteria for cervical radiculopathy: an international E-Delphi study. Musculoskelet Sci Pract 2022;61:102596. 10.1016/j.msksp.2022.102596 [DOI] [PubMed] [Google Scholar]
- 9.Bellew JW. Special tests for orthopedic examination, Ed 3. Phys Ther 2006;86:1311. 10.2522/ptj.2006.86.9.1311.1 [DOI] [Google Scholar]
- 10.Persson LC, Moritz U, Brandt L, et al. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar a prospective, controlled study. Eur Spine J 1997;6:256–66. 10.1007/BF01322448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halvorsen M, Abbott A, Peolsson A, et al. Endurance and fatigue characteristics in the neck muscles during sub-maximal Isometric test in patients with cervical radiculopathy. Eur Spine J 2014;23:590–8. 10.1007/s00586-013-3060-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peolsson A, Söderlund A, Engquist M, et al. Physical function outcome in Cervical Radiculopathy patients after Physiotherapy alone compared with anterior surgery followed by Physiotherapy. Spine (Phila Pa 1976) 2013;38:300–7. 10.1097/BRS.0b013e31826d2cbb [DOI] [PubMed] [Google Scholar]
- 13.Borisut S, Vongsirinavarat M, Vachalathiti R, et al. Effects of strength and endurance training of superficial and deep neck muscles on muscle activities and pain levels of females with chronic neck pain. J Phys Ther Sci 2013;25:1157–62. 10.1589/jpts.25.1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jull GA, Falla D, Vicenzino B, et al. The effect of therapeutic exercise on activation of the deep Cervical Flexor muscles in people with chronic neck pain. Man Ther 2009;14:696–701. 10.1016/j.math.2009.05.004 [DOI] [PubMed] [Google Scholar]
- 15.Jull GA, O’Leary SP, Falla DL. Clinical assessment of the deep Cervical Flexor muscles: the Craniocervical flexion test. J Manipulative Physiol Ther 2008;31:525–33. 10.1016/j.jmpt.2008.08.003 [DOI] [PubMed] [Google Scholar]
- 16.Kim JY, Kwag KI. Clinical effects of deep Cervical Flexor muscle activation in patients with chronic neck pain. J Phys Ther Sci 2016;28:269–73. 10.1589/jpts.28.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chiu TTW, Lam T-H, Hedley AJ. A randomized controlled trial on the efficacy of exercise for patients with chronic neck pain. Spine (Phila Pa 1976) 2005;30:E1–7. 10.1097/01.brs.0000149082.68262.b1 [DOI] [PubMed] [Google Scholar]
- 18.Versteegh T, Beaudet D, Greenbaum M, et al. Evaluating the reliability of a novel neck-strength assessment protocol for healthy adults using self-generated resistance with a hand-held Dynamometer. Physiother Can 2015;67:58–64. 10.3138/ptc.2013-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yadav H, Goyal M. Efficacy of muscle energy technique and deep neck flexors training in mechanical neck pain-a randomized clinical trial. IJTRR 2015;4:52. 10.5455/ijtrr.00000048 [DOI] [Google Scholar]
- 20.Siddique MAE, Rahman MM, Islam MdS, et al. Physiotherapy versus pain medication for managing chronic Cervical Radiculopathy: protocol for a multi-arm parallel-group randomized clinical trial. F1000Res 2023;12:465. 10.12688/f1000research.129158.1 [DOI] [Google Scholar]
- 21.Iqbal ZA, Rajan R, Khan SA, et al. Effect of deep Cervical Flexor muscles training using pressure Biofeedback on pain and disability of school teachers with neck pain. J Phys Ther Sci 2013;25:657–61. 10.1589/jpts.25.657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martins TS, Pinheiro-Araujo CF, Gorla C, et al. Neck strength evaluated with fixed and portable Dynamometers in asymptomatic individuals: correlation, concurrent validity, and agreement. J Manipulative Physiol Ther 2022;45:543–50. 10.1016/j.jmpt.2022.10.001 [DOI] [PubMed] [Google Scholar]
- 23.Edmondston SJ, Wallumrød ME, Macléid F, et al. Reliability of Isometric muscle endurance tests in subjects with postural neck pain. J Manipulative Physiol Ther 2008;31:348–54. 10.1016/j.jmpt.2008.04.010 [DOI] [PubMed] [Google Scholar]
- 24.Kuo YL, Lee TH, Tsai YJ. Evaluation of a cervical stabilization exercise program for pain, disability, and physical impairments in university violinists with nonspecific neck pain. Int J Environ Res Public Health 2020;17:5430. 10.3390/ijerph17155430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naik RV, Ingole PM. Modified universal goniometer for objective assessment of forward head posture in clinical settings. MGM Journal of Medical Sciences 2018;5:121–4. 10.5005/jp-journals-10036-1199 [DOI] [Google Scholar]
- 26.Erdemoglu AK, Koc R. Brief pain inventory score identifying and discriminating neuropathic and nociceptive pain. Acta Neurol Scand 2013;128:351–8. 10.1111/ane.12131 [DOI] [PubMed] [Google Scholar]
- 27.Bush KW, Collins N, Portman L, et al. Validity and Intertester reliability of cervical range of motion using Inclinometer measurements. Journal of Manual & Manipulative Therapy 2000;8:52–61. 10.1179/106698100790819546 [DOI] [Google Scholar]
- 28.Cleland JA, Fritz JM, Whitman JM, et al. The Reliability and construct validity of the neck disability index and patient specific functional scale in patients with Cervical Radiculopathy. Spine 2006;31:598–602. 10.1097/01.brs.0000201241.90914.22 Available: 10.1097/01.brs.0000201241.90914.22 [DOI] [PubMed] [Google Scholar]
- 29.Falla D, Jull G, Russell T, et al. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther 2007;87:408–17. 10.2522/ptj.20060009 [DOI] [PubMed] [Google Scholar]
- 30.Miller J, Gross A, D’Sylva J, et al. Manual therapy and exercise for neck pain: a systematic review. Man Ther 2010;15:334–54. 10.1016/j.math.2010.02.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2023-001819supp001.pdf (403.9KB, pdf)
bmjsem-2023-001819supp002.pdf (46.6KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. Electronic data will be securely stored on password-protected servers at the postgraduate programme in physiotherapy and rehabilitation. Each participant will have an identification number, and all data will be encoded using this number. A separate list of identification numbers will be securely maintained apart from deidentified data. Completed data will be anonymised and accessible only to authorised personnel.