Medical authorities have long recommended that food manufacturers reduce the amount of salt added to processed foods because of concerns about adverse cardiovascular effects of high salt intakes (>5–6 g/day).1 Putting aside debate on the potential risks and benefits of population-wide reductions in salt intake, what is the evidence that reducing the salt content of processed foods will succeed in reducing mean salt intake to 5 or 6 g/day or lower? Recently, substantial reductions of salt concentrations in processed foods in England failed to significantly decrease mean salt intake in women, despite being coupled with a public health awareness campaign that mainly targeted women.2 The results of the food reformulation program in England, and the failure of salt intake to decrease over the past 10 years in England and the US,2,3 suggest that new approaches to preventing salt-induced hypertension are needed that do not depend on reducing mean salt intake in the population.
IMPACT OF FOOD SALT REDUCTION
In March 2006, the UK Food Standards Agency (FSA) began publishing salt reduction targets for foods that account for most salt in the diet. According to He and colleagues,1 “since the targets were set in 2006, nearly all manufacturers and retailers have made significant reductions in the amount of salt added to food.” They further note that “since 2007, more than 11 million kilograms of salt have been removed from food covered by the FSA’s salt reduction targets.” 1
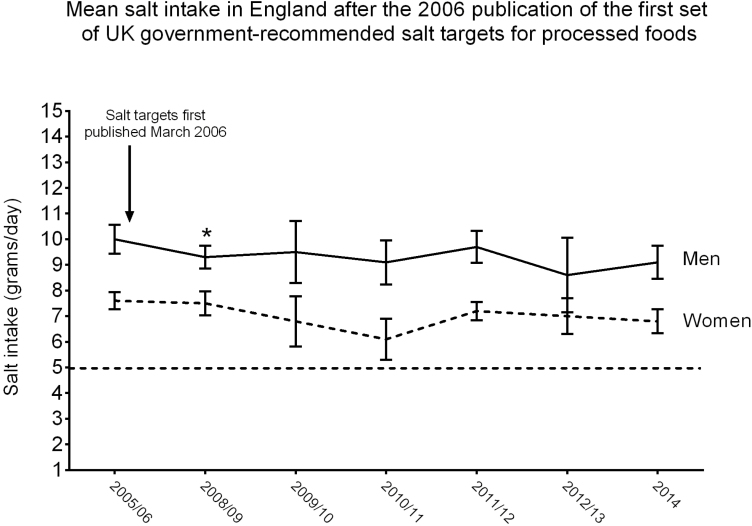
However, according to counterintuitive findings by Public Health England, the reduction of salt in processed foods was not associated with a significant decrease in mean salt intake in adult women in England.2 Specifically, mean salt intake failed to significantly decrease in women at any time from 2005/06 to 2014 (Figure 1).2 In men, mean salt intake decreased 7% between 2005/06 and 2008/09 (Figure 1).2 However, between 2008/09 and 2014 (date of the most recently completed survey on salt intake in England), there was no significant downward trend or further significant step change in salt intake in men or women (Figure 1).2 The failure of salt intake to decrease in women is particularly surprising given that the public health awareness campaign on salt and health that was run from October 2004 to October 2009 was mainly targeted at adult women.
Figure 1.
Arithmetic means and 95% confidence intervals for salt intake in men and women in England2 before and after the 2006 publication of the first set of UK-government recommended salt targets for processed foods. The straight dashed line represents the level of salt intake recommended by the World Health Organization. *Statistically significant decrease in salt intake only in men, and only between 2005/06 and 2008/09 as reported by Public Health England.2 In women, there was no statistically significant downward step-change between 2006/06 and 2008/09 or between later years. The trend analysis reported by Public Health England was performed with log-transformed data and geometric means due to the skewed nature of the raw data.2
Why did mean salt intake fail to significantly decrease in women between 2005/06 and 2014, and in men between 2008/09 and 2014, despite the reduction of salt in processed foods? MacGregor and colleagues4 might attribute the failure of salt intake to significantly decrease in both women and men to political meddling in the salt reduction program by the UK coalition government formed in 2010. However, political meddling cannot explain why salt intake failed to significantly decrease in women between 2005/06 and 2008/09 when salt intake in men appeared to significantly decrease.2 Perhaps women consume a lower proportion of the foods that happened to meet salt reduction targets than do men. If so, one might suppose that with more aggressive efforts to meet salt reduction targets for all food categories of interest, it will be feasible to significantly reduce mean salt intake in both women and men to 6 g/day. However, an analysis by scientists interested in the physiologic mechanisms influencing the amount of salt we consume suggests an alternative possibility.5
DO PHYSIOLOGIC MECHANISMS LIMIT THE CAPACITY OF FOOD REFORMULATION PROGRAMS TO REDUCE SALT INTAKE?
According to McCarron and colleagues,5 the lower normal physiologic limit for mean salt intake in societies where salt is widely available is approximately 120 mmol/day (7 g/day) and that attempts to drive mean salt intake much below this level may be futile. Given that women consume approximately 25% less salt than men,5 the analysis of McCarron and colleagues suggests that the lower normal physiologic limit for mean salt intake may be approximately 6–7 g/day in women and around 8–9 g/day in men. As reductions in food salt content cause mean salt intake to fall closer to these levels, biologic systems determining salt-seeking behavior may attenuate the capacity of reductions in food salt content to cause further reductions in mean salt intake. At some point in response to progressive reductions in the salt content of all processed foods, individuals may begin to add more salt to their diet, or begin to consume greater amounts of salt-containing processed foods, or both.
When salt reduction targets were first published in 2006, mean salt intake of women in England was already close to 7 g/day,2 a level near the lower normal physiologic limit of mean salt intake posited by McCarron and colleagues.5 Accordingly, the view of McCarron et al. raises the possibility that in 2006, the capacity to further reduce salt intake in women by decreasing salt concentrations of processed foods may have been offset by physiologic activation of factors that influence the amount of salt consumed. In contrast, mean salt intake in men was around 10 g/day in 2006,2 a level considerably greater than the lower normal physiologic limit of mean salt intake proposed by McCarron and colleagues.5 Thus, in 2006, reducing salt concentrations in processed foods may have succeeded in moderately decreasing salt consumption in men because their salt intake was well above the normal lower physiologic limit for mean salt intake at that time.
In rural parts of China in which consumption of manufactured foods is relatively low, mean salt intake is over 6 g/day because people voluntarily add large amounts of salt to their food at home. When consumers (not food manufacturers) mainly determine the amount of salt added to food, they may choose to add salt in amounts greater than those recommended by health authorities.
NEW STRATEGIES FOR PREVENTING SALT-INDUCED HYPERTENSION
The limited success of food salt reduction programs and educational campaigns in reducing salt intake over the past 10 years2,3 suggests the need for new approaches to preventing salt-induced hypertension. We propose that improved understanding of the biologic factors determining salt intake will facilitate discovery of novel strategies beyond educational and regulatory approaches. We further propose that greater efforts be made to correct the nutritional deficiencies and biologic abnormalities that make subsets of the population susceptible to the hypertensive effects of a high salt diet in the first place.6,7 By harnessing the mechanisms usually involved in protecting against salt-induced increases in blood pressure in normal individuals (salt-resistant normotensive subjects), it should be possible to prevent or correct common abnormalities mediating salt sensitivity.6
Meanwhile, policy makers worldwide are promoting food salt reduction programs under the assumption that decreasing the salt content of processed foods by 40% or more will help decrease population salt intake by 40% or more (to a mean of 6 g/day or lower). Perhaps government regulators will someday propose that beverage manufacturers reduce alcohol levels in beer, wine, and spirits by 40% in an effort to reduce alcohol intake and decrease the risk for liver disease and dementia. If so, we can expect scientists interested in the complex factors determining alcohol intake to also question the assumptions behind that strategy.
DISCLOSURES
TWK is a co-founder and stockholder of Mission Salt, Inc, that has filed patents for salty food compositions including nitrate-rich vegetable ingredients. The company goal is to develop methods to prevent salt-induced hypertension. TWK does not receive any financial support from Mission Salt and no funds from Mission Salt were used for the submitted work. The other authors declared no conflict of interest.
DISCLAIMER
The Opinions of the authors are their own and do not necessarily represent the opinions of the Editors or of the American Journal of Hypertension.
REFERENCES
- 1. He FJ, Brinsden HC, MacGregor GA. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens 2014; 28:345–352. [DOI] [PubMed] [Google Scholar]
- 2. Public Health England. National Diet and Nutrition Survey: Assessment of Dietary Sodium in Adults in England, 2014. 2016. https://www.gov.uk/government/statistics/national-diet-and-nutrition-survey-assessment-of-dietary-sodium-in-adults-in-england-2014. Accessed 22 March 2016.
- 3. Brouillard AM, Kraja AT, Rich MW. Trends in dietary sodium intake in the United States and the impact of USDA guidelines: NHANES 1999–2016. Am J Med 2019; 132:1199–1206. [DOI] [PubMed] [Google Scholar]
- 4. MacGregor GA, He FJ, Pombo-Rodrigues S. Food and the responsibility deal: how the salt reduction strategy was derailed. BMJ 2015; 350:h1936. [DOI] [PubMed] [Google Scholar]
- 5. McCarron DA, Geerling JC, Kazaks AG, Stern JS. Can dietary sodium intake be modified by public policy? Clin J Am Soc Nephrol 2009; 4:1878–1882. [DOI] [PubMed] [Google Scholar]
- 6. Morris RC Jr, Pravenec M, Šilhavý J, DiCarlo SE, Kurtz TW. Small amounts of inorganic nitrate or beetroot provide substantial protection from salt-induced increases in blood pressure. Hypertension 2019; 73:1042–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McCarron DA. A consensus approach to electrolytes and blood pressure. Could we all be right? Hypertension 1991; 17:I170–I172. [DOI] [PubMed] [Google Scholar]