Abstract
Studies have shown that a series of molecular events caused by oxidative stress is associated with ferroptosis and oxidation after ischemic stroke (IS). Differential analysis was performed to identify differentially expressed mRNA (DEmRNAs) between IS and control groups. Critical module genes were identified using weighted gene co-expression network analysis (WGCNA). DEmRNAs, critical module genes, oxidative stress-related genes (ORGs), and ferroptosis-related genes (FRGs) were crossed to screen for intersection mRNAs. Candidate mRNAs were screened based on the protein–protein interaction (PPI) network and the MCODE plug-in. Biomarkers were identified based on two types of machine learning algorithms, and the intersection was obtained. Functional items and related pathways of the biomarkers were identified using gene set enrichment analysis (GSEA). Finally, single-sample GSEA (ssGSEA) and Wilcoxon tests were used to identify differential immune cells. An miRNA-mRNA-TF network was created. Quantitative real-time polymerase chain reaction (qRT-PCR) was performed to verify the expression levels of biomarkers in the IS and control groups. There were 8287 DE mRNAs between the IS and control groups. The genes in the turquoise module were selected as critical module genes for IS. Thirty intersecting mRNAs were screened for overlaps. Seventeen candidate mRNAs were also identified. Four biomarkers (CDKN1A, GPX4, PRDX1, and PRDX6) were identified using two types of machine-learning algorithms. GSEA results indicated that the biomarkers were associated with steroid biosynthesis. Nine types of immune cells (activated B cells and neutrophils) were markedly different between the IS and control groups. We identified 3747 miRNA-mRNA-TF regulatory pairs in the miRNA-mRNA-TF regulatory network, including hsa-miR-4469-CDKN1A-BACH2 and hsa-miR-188-3p-GPX4-ATF2. CDKN1A, PRDX1, and PRDX6 were upregulated in IS samples compared with control samples. This study suggests that four biomarkers (CDKN1A, GPX4, PRDX1, and PRDX6) are significantly associated with IS. This study provides a new reference for the diagnosis and treatment of IS.
Keywords: Oxidative stress, Ischemic stroke, Ferroptosis, Biomarkers, Bioinformatics analysis
Subject terms: Cell biology, Genetics, Immunology, Molecular biology, Neuroscience, Biomarkers, Diseases, Molecular medicine, Neurology
Introduction
Ischemic stroke (IS) is a disease caused by the interaction of multiple environmental and genetic risk factors and is the most common cause of disability1. In contrast, IS is caused by reduced blood supply in certain areas of the brain owing to vascular obstruction2. IS can cause a series of complex neuropathological and physiological events (including excitotoxicity, oxidative stress, neuroinflammation, and apoptosis, etc.) leading to brain injury3. Therefore, if the disease cannot be effectively prevented or slowed, it will become a serious public health problem. Currently, the routine treatment for IS is a tissue plasminogen activator (tPA) for intravenous thrombolysis. However, owing to the narrow therapeutic window and possibility of severe bleeding, the benefit range for patients is small4. Biomarker-based IS assessments may help predict diagnosis and determine the treatment direction for each patient.
Oxidative stress (OS) is an important factor in neuroinflammation and neuronal necrosis in IS and is mainly caused by an imbalance between the production and consumption of reactive oxygen species (ROS). Excess ROS can induce lipid peroxidation and the oxidation of proteins, DNA, and RNA, leading to neuronal dysfunction and death5. Ferroptosis is an iron-dependent oxidative stress-induced cell death pathway that plays an important role in IS6. In animal cells, it has been confirmed that mitochondrial oxidative stress regulates ferroptosis through the NRF2-ARE pathway7. In addition, a series of molecular events due to oxidative stress have been shown to be associated with ferroptosis and oxidation processes after the onset of IS, and to have common molecular targets such as lipid peroxidation and GSH depletion8,9. Therefore, exploring the role of oxidative stress- and ferroptosis-related genes in the pathogenesis of IS is helpful for further understanding its pathophysiology. More importantly, the discovery of biomarkers associated with oxidative stress and ferroptosis in IS may provide new clues for diagnosis and treatment.
Based on data from the Gene Expression Omnibus (GEO) public database, this study aimed to explore biomarkers related to oxidative stress-ferroptosis in IS, using a series of bioinformatics methods to lay a theoretical foundation for the diagnosis and treatment of IS.
Methods
Data sources
The IS-related datasets of blood samples in this study were acquired from the GEO database (http://www.ncbi.nlm.nih.gov/geo/). Based on previous research10, there were 15 samples (five control and 10 IS samples) in the GSE122709 dataset using the Empirical Bayes method, which was utilized as a training set. The validation set GSE140275 contained three control samples and three IS samples. In addition, 1399 oxidative stress-related genes (ORGs) and 259 ferroptosis-related genes (FRGs) were identified based on published literatures11,12.
Differential expression analysis and weighted gene co-expression network analysis (WGCNA)
In our study, differentially expressed mRNA (DEmRNAs) between the IS and control groups in the GSE122709 dataset were acquired using the limma-trend method after processing the data using the edgeR (v 3.36.0)13 package (adj.p.value < 0.05, |log2FC|> 0.5). Heat and volcano maps of DE mRNA between the IS and control groups were plotted using the p heat map (v 0.7.7) (14 and ggplot2 (v 3.3.2)15 packages, respectively. WGCNA was performed on all the samples in the GSE122709 dataset to screen for critical modules. First, outlier samples were eliminated to ensure precision of the analysis using sample clustering. An appropriate soft threshold (β) was selected, such that the engagement between genes conformed to a scale-free distribution to the maximum extent. Then, according to the standard hybrid dynamic tree cutting algorithm, the minimum number of genes per gene module was set to 30, and MEDissThres was set to 0.2 to merge similar modules (the similarity correlation value was 0.8). Subsequently, correlation analysis was used to evaluate the relationships between modules and traits (IS and control groups). Finally, the genes in the module most relevant to IS were defined as critical module genes (hub mRNAs).
The acquisition of candidate mRNAs
The above DEmRNAs, Hub mRNAs in the critical module, 1399 ORGs, and 259 FRGs were crossed to screen the intersection mRNAs. Furthermore, to investigate the related biological functions and pathways of the intersection mRNAs, Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG)16–18 enrichment analyses were performed using the clusterProfiler (v 3.14.3) package19 (adj.p < 0.05). In addition, to explore whether there was an interaction among these intersecting mRNAs, we used the STRING online database (https://string-db.org/) to create a protein–protein interaction (PPI) network (confidence = 0.4). The MCODE plug-in was used to identify the key submodules of the PPI network, and mRNAs in the submodules were treated as candidate mRNAs.
Identification and verification of biomarkers
Based on the above candidate mRNAs, least absolute shrinkage and selection operator (LASSO) and Support Vector Machine-Recursive Feature Elimination (SVM-RFE) algorithms were implemented to acquire feature mRNAs. The LASSO algorithm was performed using the glmnet (v 4.0–2) package20(family = ‘binomial,’ type.measure = ‘class,’ and nfold = 10). The SVM-RFE algorithm21 was performed using the E1071 (v 1.7-9) package22 (five-fold cross validation). Furthermore, the feature mRNAs acquired using the LASSO algorithm and those identified using the SVM-RFE algorithm were crossed to screen for biomarkers. In addition, to evaluate the diagnostic ability of biomarkers for IS, receiver operating characteristic (ROC) curves of these biomarkers were plotted in the GSE122709 (training set) and GSE140275 (validation set) datasets. Finally, the expression levels of the biomarkers were extracted from the training set GSE122709 and validation set GSE140275, and the expression levels of the above biomarkers between the IS and control groups were compared using the ggplot2 (v. 3.3.2) package14.
Enrichment analysis and immune infiltration analysis
To further understand the related biological functions and involved signaling pathways of the biomarkers, gene set enrichment analysis (GSEA) was implemented based on the KEGG pathway gene set using GSEA Software (v 4.0.3)23, with a significance threshold of |NES|> 1 and NOM p.val < 0.05. Subsequently, to evaluate the degree of immune cell infiltration, the ssGSEA algorithm was used to analyze the infiltration abundance of 28 immune cells in all samples in the training set. Differential immune cells between IS and control samples were identified using the Wilcoxon test. The relationships between the biomarkers and differential immune cells were computed using Spearman’s method.
The construction of regulatory network and drug prediction
Subsequently, miRNAs of these biomarkers were predicted based on the miRNet database (https://www.mirnet.ca/miRNet/home.xhtml) and miRDB online database (https://mirdb.org/). The human transcription factor target (hTFtarget) online database (http://bioinfo.life.hust.edu.cn/hTFtarget#!/) was used to predict the transcription factors (TFs) of the biomarkers. Finally, the miRNAs and TFs regulated by the same mRNA were screened and an miRNA-mRNA-TF network was created. In addition, the IC50 of chemical drugs as biomarkers for IS patients was predicted according to the gene expression profile and cell line expression profile in the Genomics of Drug Sensitivity in Cancer (GDSC) online database (https://www.cancerrxgene.org/). The Wilcoxon test was used to compute the differences in drug sensitivity between the IS and control groups.
Quantitative real-time PCR (qRT-PCR) verification
Blood samples were obtained from patients with IS and control subjects, with written informed consent for participation in the study. This study was approved by the Ethics Committee of the First Affiliated Hospital of Kunming Medical University. Twenty pairs of blood samples were divided into two groups: 10 IS and 10 control. Total RNA was isolated from the samples and purified using TRIzol reagent (Ambion, Austin, Texas, U.S.) following the manufacturer’s instructions. The concentration of extracted RNA was measured using a nanophotometer (N50). Next, reverse transcription via SureScript-First-strand-cDNA-synthesis-kit (Servicebio, Wuhan, China) by an ordinary PCR instrument. The reverse transcription product cDNA was diluted 5–20 times with ddH2O (RNase/DNase-free). Polymerase chain reaction (PCR) amplification was performed on a CFX96 real-time quantitative PCR instrument. The samples were denatured at 95 °C for (pre-denaturation), followed by denaturation at 95 °C for 20 s (denaturation), annealing at 55 °C for 20 s (annealing), and elongation at 72 °C for 30 s (elongation). The reactions were subjected to 40 cycles. The primer sequences used are listed in Table 1.
Table 1.
The primer sequences of biomarkers.
| Primer | Sequence |
|---|---|
| CDKN1A F | GCACGGAAGGACTTTGTAAGG |
| CDKN1A R | CGGCGTTTGGAGTGGTAGAA |
| GPX4 F | CCTTTGCCGCCTACTGAAG |
| GPX4 R | GGTCGACGAGCTGAGTGTAG |
| PRDX1 F | TTCTTGCCTGTTGCCTCTTCC |
| PRDX1 R | GGTTCAACCAGGTTCCCGCA |
| PRDX6 F | GCTTCTTCGCCAGAACCAAC |
| PRDX6 R | GACGGTGGTATTGGCCTCAA |
| Internal reference-GAPDH F | CGAAGGTGGAGTCAACGGATTT |
| Internal reference-GAPDH R | ATGGGTGGAATCATATTGGAAC |
Ethics approval and consent to participate
This study conformed to the ethical guidelines of the Science Foundation of the National Natural Science Foundation of China. Written informed consent was obtained from the individual(s) and minor(s) legal guardian/next of kin for publication of any potentially identifiable images or data included in this study.
Consent for publication
Written informed consent for the publication of clinical details and/or images was obtained from the patient/parent/guardian/relative of the patient.
Results
Acquisition of DEmRNAs and key modules
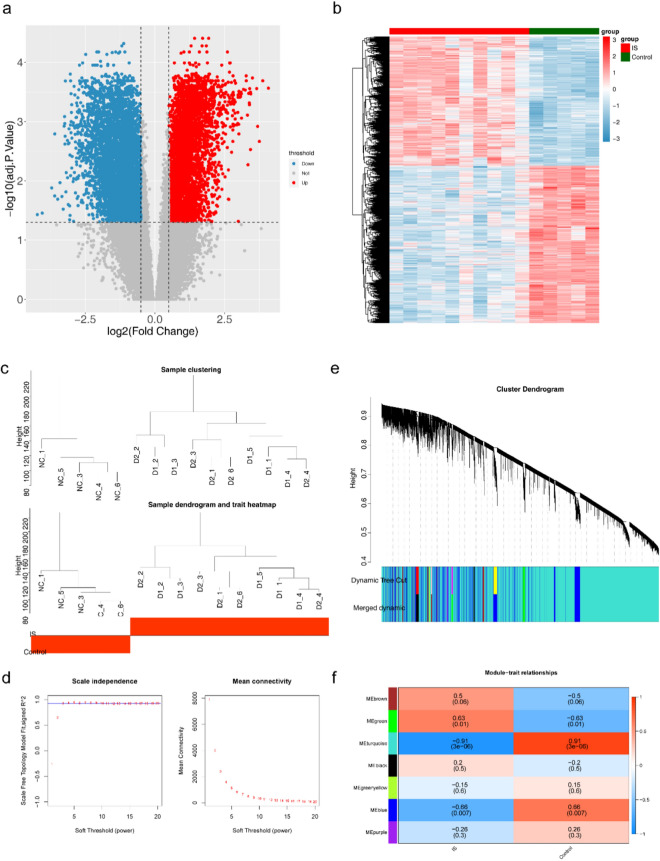
In the GSE122709 dataset, there were 8287 DEmRNAs between the IS and control groups (Fig. 1a). The expression heat map of IS-associated DE mRNAs in the GSE122709 dataset is shown in Fig. 1b. Subsequently, WGCNA was used to select the critical module genes for clinical traits (IS and control). To ensure the accuracy of the analysis, we clustered samples to eliminate outliers. The results indicate that there were no outlier samples in the GSE122709 dataset. Thus, all the samples were used for subsequent analyses (Fig. 1c). In addition, when the soft threshold was three, the network was closest to the distribution without the network scale (Fig. 1d). Seven modules were obtained after the merging (Fig. 1e). The turquoise module (|Cor|= 0.91 and p < 0.05) was highly relevant to IS and control, and was therefore selected as the critical module. Therefore, the turquoise module contained 17799 Hub mRNAs was used for subsequent analyses (Fig. 1f).
Figure 1.
Acquisition of DEmRNAs and key modules. (a) Volcano map of mRNAs expression between groups. (b) Heat map of mRNA expression between groups. (c) Cluster analysis of dataset samples and Data Sample Clustering and Phenotypic Information. (d) Scale free soft threshold distribution. (e) Module Clustering Tree. (f) Heat map of correlation between modules and clinical traits.
17 candidate mRNAs were identified
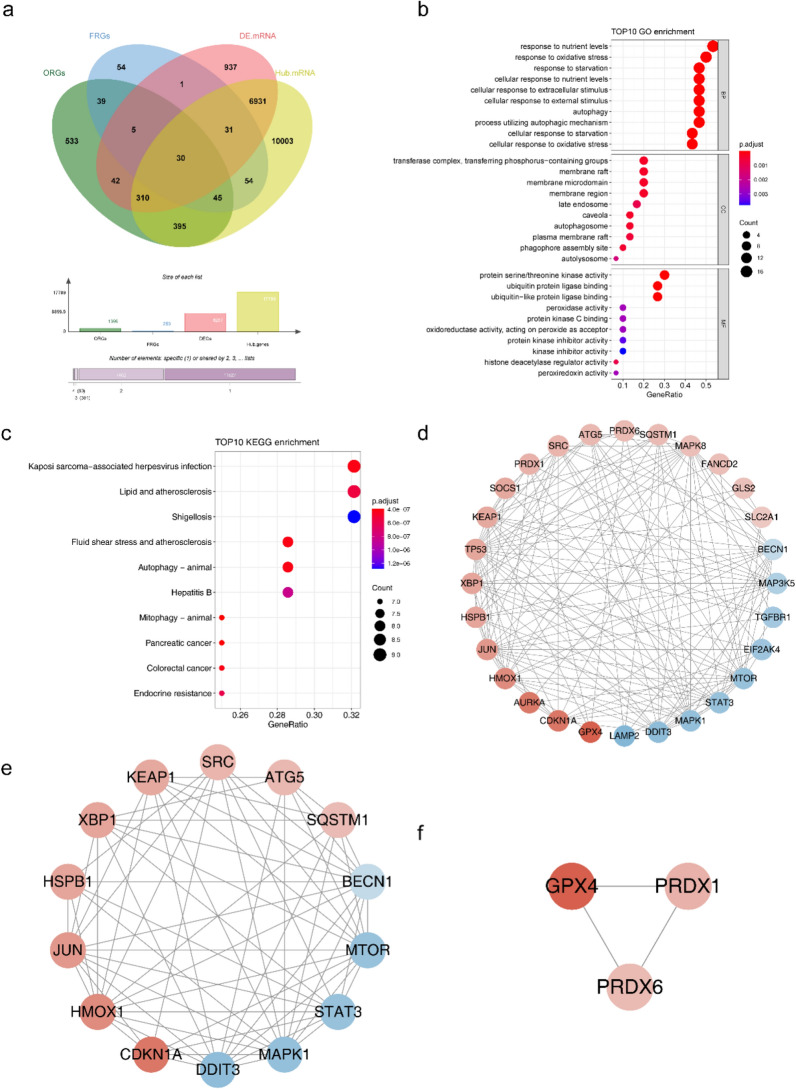
There were 30 intersection mRNAs overlapping 8287 DE mRNAs, 17799 hub mRNAs in the critical module, 1399 ORGs, and 259 FRGs (Fig. 2a). According to the GO functional enrichment analysis, intersecting mRNAs mainly participated in cellular responses to oxidative stress, cellular responses to extracellular stimuli, and responses to oxidative stress (Fig. 2b, Supplementary Table 1). KEGG functional enrichment analysis revealed that the intersecting mRNAs were associated with lipid and atherosclerosis, fluid shear stress, and atherosclerosis (Fig. 2c, Supplementary Table 2). Additionally, 154 protein interaction pairs were obtained from the PPI network, including 28 nodes. Moreover, MAPK8 showed higher connectivity in the PPI network (Fig. 2d). Seventeen candidate mRNAs were identified using the two key submodules. Cluster 1 had 14 candidate mRNAs, including BECN1, MTOR, STAT3, MAPK1, DDIT3, CDKN1A, HMOX1, JUN, HSPB1, XBP1, KEAP1, SRC, ATG5, and SQSTM1, and cluster 2 contained three candidate mRNAs (GPX4, PRDX1, and PRDX6) (Fig. 2e–f).
Figure 2.
Identification of IS-related DEmRNAs and functional enrichment. (a) Venn diagram of intersection mRNA. (b) Bubble plot of intersection mRNA GO TOP10 enrichment results. (c) Bubble plot of intersection mRNA KEGG TOP10 enrichment results. (d) Protein Interaction Network Diagram. (e, f) Key sub modules in PPI network.
Four biomarkers were screened out
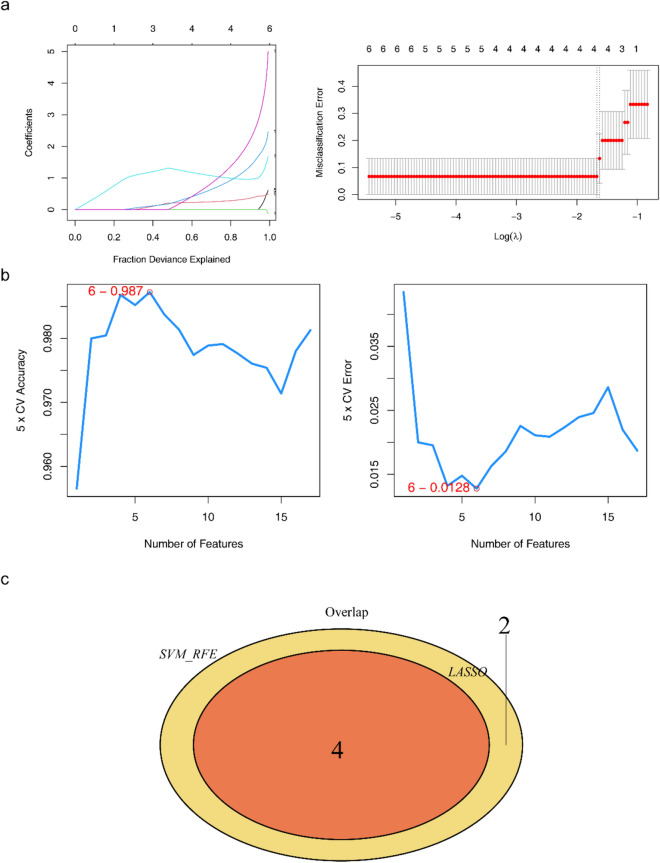
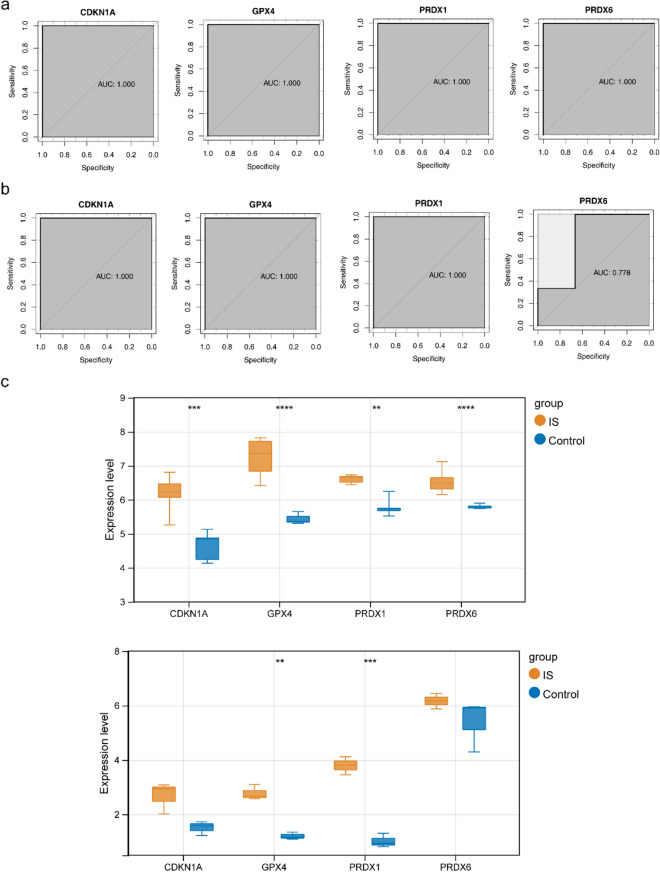
In total, four mRNAs, CDKN1A, GPX4, PRDX1, and PRDX6, were identified using the LASSO algorithm (Fig. 3a). Six mRNAs (PRDX6, GPX4, PRDX1, CDKN1A, XBP1, and HMOX1) were identified using the SVM-RFE algorithm (Fig. 3b). Therefore, four biomarkers were screened by overlapping CDKN1A, GPX4, PRDX1, and PRDX6 (Fig. 3c). Furthermore, in the training set GSE122709, the area under the curve (AUC) values of the four biomarkers were all above 0.9, indicating that the biomarkers had the diagnostic ability to distinguish between the IS and control samples (Fig. 4a). In the validation set GSE140275, the AUC value of each biomarker was above 0.75, further verifying the diagnostic value of the biomarkers (Fig. 4b). Additionally, the expression levels of GPX4 and PRDX1 in the IS and control groups were significantly different between the training and validation sets. Although CDKN1A and PRDX6 levels did not differ in the validation set, the expression trend was consistent with that in the training set, and the four biomarkers showed an upward trend in the IS samples (Fig. 4c).
Figure 3.
Machine learning for screening biomarkers. (a) Changes in mRNA coefficients in the LASSO model and LASSO Logic Coefficient Penalty Graph. (b) Support Vector Machine Model Accuracy (Left) and Error Rate (Right). (c) Venn diagram of biomarkers.
Figure 4.
Analysis of biomarker expression and diagnostic value. (a) ROC curve of biomarkers (CDKN1A, GPX4, PRDX1, and PRDX6) in the training set. (b) ROC curves of Validation for concentrated biomarkers (CDKN1A, GPX4, PRDX1, and PRDX6). (c) Expression box diagram of biomarkers (CDKN1A, GPX4, PRDX1, and PRDX6) in the training set and expression box diagram for verifying the expression of concentrated biomarkers (CDKN1A, GPX4, PRDX1, and PRDX6).
GSEA of the biomarkers and the ssGSEA
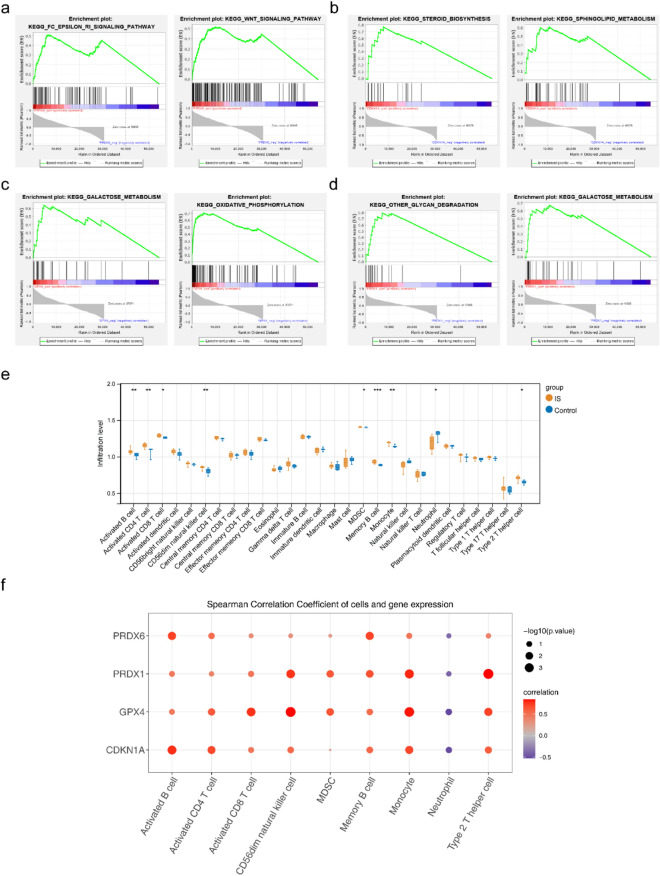
According to KEGG functional enrichment analysis, PRDX6 was mainly enriched in the FC epsilon RI and WNT signaling pathways. CDKN1A is associated with steroid biosynthesis and sphingolipid metabolism. GPX4 is involved in galactose metabolism and oxidative phosphorylation. Besides, it was found to PRDX1 participated in glycan degradation and galactose metabolism (Fig. 5a–d, Supplementary Table 3). Furthermore, we performed immune infiltration analysis using the GSE122709dataset. The results showed that there were nine immune cells with significant differences (p < 0.05) between IS and control samples, including activated CD8 T cells, activated CD4 T cells, activated B cells, MDSC, CD56dim natural killer cells, neutrophils, type 2T helper cells, memory B cells, and monocytes (Fig. 5e). A strong positive correlation was observed between PRDX1 and type 2T helper cells, and GPX4 showed the strongest negative association with neutrophils (Fig. 5f, Supplementary Table 4).
Figure 5.
GSEA enrichment analysis of PRDX6 and immunocyte infiltration analysis. (a) enplot_KEGG_FC_EPSILON_RI and WNT_signaling pathway. (b) enplot_KEGG_steroid biosynthesis and sphingolipid metabolism. (c) enplot_KEGG_galactose metabolism and oxidative phosphorylation. (d) enplot_KEGG_other glycan degradation and galactose metabolism. (e) Box plot of 28 immune cell expressions between groups. (f) Bubble chart of correlation between biomarkers and differential immune cells.
The construction of miRNA-mRNA-TF network and chemical drug prediction
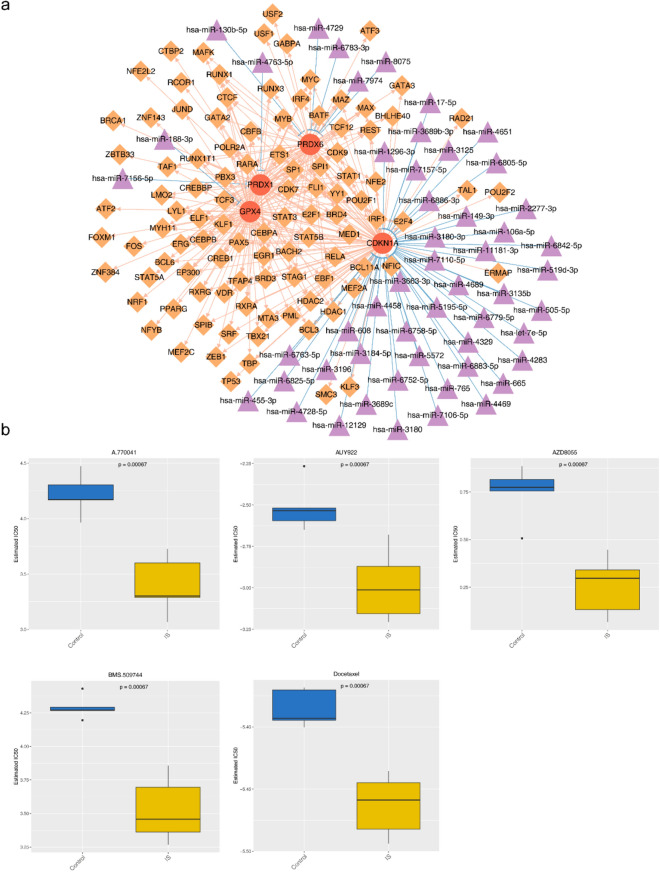
A total of 52 mRNA-miRNA pairs were screened, including 52 miRNAs and four mRNAs. Moreover, 260 mRNA-TF pairs were obtained, including 102 TFs and 4 mRNAs. There were 3747 miRNA-mRNA-TF regulatory pairs in the miRNA-mRNA-TF regulatory network, including hsa-miR-4469-CDKN1A-BACH2 and hsa-miR-188-3p-GPX4-ATF2 (Fig. 6a, Supplementary Table 5). In addition, there were significant differences in the therapeutic sensitivity of the 50 drugs in the IS samples, including A.770041, AUY922, AZD8055, BMS.509744, and docetaxel (Fig. 6b, Supplementary Table 6).
Figure 6.
Construction of biomarker regulatory network and chemical drug prediction analysis. (a) Network diagram of miRNA-mRNA-TF regulatory mechanism. (b) IC50 Box Chart of A.770041, AUY922, AZD8055, BMS.509744, and Docetaxel Therapeutically Sensitive Drugs.
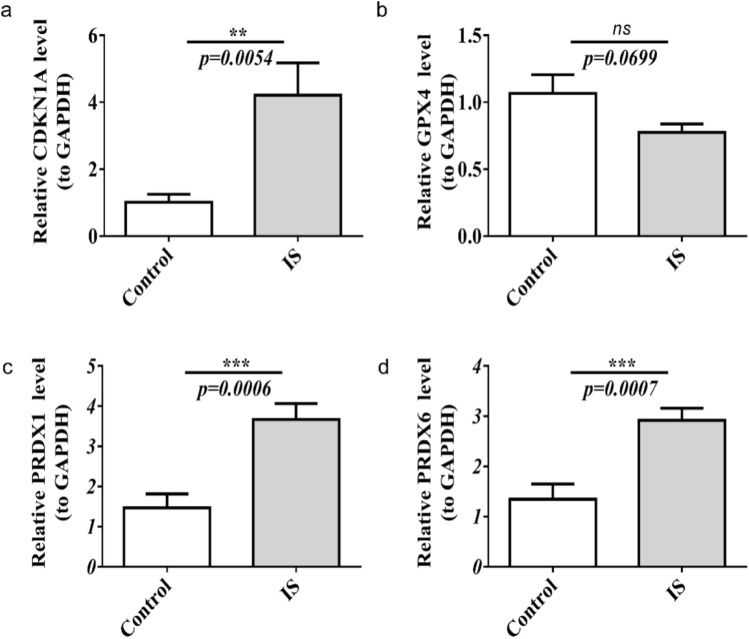
The verification of qRT-PCR
Based on the qRT-PCR results, CDKN1A, PRDX1, and PRDX6 were upregulated in IS samples, and the validation results were consistent with the above analysis (Fig. 7a–d).
Figure 7.
The relative mRNA expression level in patients with IS. (a–d) The relative CDKN1A, GPX4, PRDX1, and PRDX6 mRNA expression level in patients with IS. ns, not significant, ** p < 0.01, *** p < 0.001.
Discussion
Studies have found that stroke triggers neuronal ferrozoticism and that the use of siderotic inhibitors can reduce the degree of neuronal damage24. In IS, oxidative stress can lead to increased iron levels within the nerve cells and increased brain damage. Inhibits the activity of ACSL4 and lipoxygenase isotype 5 (LOX-5), thereby protecting cells from ferrozoticism25. The ROS scavengers ferrostatin-1 and liproxstatin-1 can specifically reduce ROS and inhibit ferroptosis26. Therefore, oxidative stress- and ferroptzosis-related genes play important roles in the occurrence and development of IS, and studying the relationship between oxidative stress and ferroptzosis-related genes can help determine the prognosis, efficacy, and therapeutic targets of IS patients.
In this study, four biomarkers, CDKN1A, GPX4, PRDX1, and PRDX6, were used to diagnose stroke and assess the treatment effects. Previous research has found that the antioxidant enzyme PRDX1 controls stroke-associated microglia in acute ischemic stroke27. CDKN1A/JUN is a robust and promising diagnostic biomarker for identifying patients with IS and may regulate ferroptosis during IS progression via the C9orf106/C9orf139-miR-22-3p-CDKN1A and GAS5-miR-139-5p/miR-429-JUN axes28. GPX4 can reduce peroxidized lipids; thus, inhibition of GPX4 or cystine import can induce ferroptosis29. Coenzyme Q10 (CoQ10) can reverse lipid peroxidation independently of GPX4; ferroptosis suppressor protein 1 (FSP1) can act as an oxidoreductase of CoQ10, shuttling reductants to the lipid bilayer plasma membrane to protect against peroxidation damage29. Phospholipase A2 of PRDX6 can improve cerebral ischemia/reperfusion inflammatory injury by reducing the expression of the inflammatory cytokines IL-1β, IL-17, and IL-23 and oxidative stress30,31. According to KEGG functional enrichment analysis, PRDX6 is mainly enriched in the FC epsilon ri and WNT signaling pathways, and the WNT signaling pathway plays an important role in the regulation of oxidative stress32. GPX4 is involved in galactose metabolism and oxidative phosphorylation33. Studies have found that glutathione peroxidase 4 (GPX4) uses glutathione as a substrate for redox reactions, reducing cellular lipid peroxides to their corresponding alcohols. Glutathione produces oxidized glutathione, thereby preventing cell death caused by the accumulation of lipid peroxides34. Recent studies have shown that GPX4 is also involved in ischemia–reperfusion-induced brain injury35. CDKN1A was also known as P21, when DNA damage occurs at cell telomeres, CDKN1A is able to cause cell cycle arrest and DNA repair by inhibiting the activity of cell cycle protein-dependent kinases, allowing cells to return to homeostasis36. CDKN1A, a regulator of ischemia–reperfusion injury, is associated with atherosclerosis and risk of myocardial infarction progression37,38. The myocardial infarction-related exosomes miR-208b and miR-208b regulate the growth of HUVECs by regulating CDKN1A expression39. Fan et al. suggested that CDKN1A could be a robust and promising diagnostic biomarker for IS by regulating ferroptosis during IS progression28. PRDX1 (peroxyregen 1) is a typical 2-cysteine (Cys) peroxyrein that catalyzes the reduction reaction and converts hydrogen peroxide (H2O2) to water as a multifunctional antioxidant40. The upregulation of PRDX1 in cells and tissues under oxidative stress is thought to be a cellular response to oxidative injury40–42. PRDX6 not only catalyzes the catalytic reduction of hydrogen peroxide and short-chain organic fatty acid peroxide activities of PRDX1, but also reduces phospholipid hydroperoxides, calcium-independent phospholipase A2 activity43, and lysophosphatidyltransferase activity44. PRDX6 repairs regenerated oxidized cell membranes45,46. Previous studies have shown that PRDX6 secreted by Schwann-like cells protects neurons against IS in rats via the PTEN/PI3K/AKT pathway47. Therefore, CDKN1A, GPX4, PRDX1, and PRDX6 are associated with ischemia–reperfusion-induced oxidative stress and ferroptosis. To observe the changes in the four biomarkers CDKN1A, GPX4, PRDX1, and PRDX6 in patients with ischemic stroke, we measured their expression of these four biomarkers in peripheral blood using RT-PCR. The results showed that CDKN1A, PRDX1, and PRDX6 expression levels were significantly increased, which was consistent with our study, suggesting that CDKN1A, PRDX1, and PRDX6 may be involved in the occurrence and development of ischemic stroke. Furthermore, in the training set GSE122709, the AUC values of all four biomarkers were above 0.9, indicating that the genes could perfectly distinguish between the IS and control samples. This superior performance might be attributable to the limited sample size, which could artificially enhance the discriminative precision of the biomarkers. To corroborate these findings, we assessed the efficacy of the model by using an independent validation set. Consistently, the biomarkers maintained high AUC values in this validation cohort, further substantiating the robustness of the model and its potential to be generalized across previously unseen data. These observations were consistent with those of previous studies48–50.
MAPK8 showed high connectivity in the PPI networks. Studies have shown that MAPK8 is also involved in the regulation of oxidative stress in tissues and cells51,52. In the PPI network, Cluster 1 contained 14 candidate mRNAs, including BECN1, MTOR, STAT3, MAPK1, DDIT3, CDKN1A, HMOX1, JUN, HSPB1, XBP1, KEAP1, SRC, ATG5, and SQSTM1. Recent studies have shown that the ATM-CHK2-Beclin 1 axis promotes autophagy to maintain ROS homeostasis under oxidative stress in a rat model of cerebral stroke53. Inhibition of PI3K/Akt/mTOR signaling by NDRG2 contributes to neuronal apoptosis and autophagy in IS54. Neuronal STAT3/HIF-1α/PTRF axis-mediated bioenergetics can exacerbate cerebral ischemia–reperfusion injury via PLA2G4A55. The β-Arrestin-2-ERK1/2 cPLA2α axis mediates TLR4 signaling and influences the induction of eicosanoids in the ischemic brain56. Activation of ATF4-DDIT3-mediated ER stress promotes proliferation and protects cortical neural stem cells in vitro57. The expression of miR-20a is upregulated by stroke serum, which promotes MSC proliferation by regulating the cell cycle inhibitor p21 CDKN1A58. heme oxygenase 1 (HMOX1)-mediated neurogenesis after permanent IS in mice59. The absentia homolog 1/Jun N-terminal kinase pathway can reduce oxidative stress and mitochondrial damage in rats with cerebral ischemia–reperfusion injury60. HspBs, HspB1, and HspB5 may be most important in the neuronal stress response to ischemia/reperfusion injury in the brain and may be involved in neuroprotection61. Downregulation of XBP-1 can rescue pyroptosis induced by cerebral ischemia/reperfusion injury through the NLRP3/Caspase-1/GSDMD axis62. The Keap1-Nrf2/ARE signaling pathway is activated by butylphthalide during IS treatment63. Inhibition of the Src-PP2B-mTOR pathway activity could improve neuronal ischemic injury64. ATG5 knockdown attenuates ischemia‒reperfusion injury by reducing excessive autophagy-induced ferroptosis65. SQSTM1 attenuates oxygen–glucose deprivation/re-oxygenation-induced neuronal injury in vitro66. Therefore, these intersecting mRNAs may play important roles in the occurrence and development of IS.
Stroke-prone immunosuppression (SIID) occurs in both experimental models and clinical cases. SIID is characterized by lymphopenia, upregulation of anti-inflammatory cytokines, and splenomegaly atrophy67. Other factors that influence SIID include glucocorticoids, acetylcholine, epinephrine, and norepinephrine68. However, the mechanisms by which stroke causes cellular immune dysfunction remain unclear. In 1979, Czlonkowska et al.69 found a decrease in the total number of peripheral blood lymphocytes and a concomitant decrease in T lymphocytes in stroke patients, suggesting that it is related to stress. Berczi70 suggested that cerebral infarction causes increased functional activity of the hypothalamic–pituitary–adrenal axis, producing large amounts of adrenocorticotropic hormones, which decreases the number of CD3+ and CD4+ T lymphocytes, thus suppressing the immunity of the body. Fiorina71 observed that cerebral infarction was associated with a decrease in plasma melatonin (MT) levels, but not adrenocortical hormone levels. Campanella et al.72 used flow cytometry to detect a significant increase in lymphocytes after cell isolation in cerebellar tissue from cerebral infarction, further suggesting that the decrease in peripheral blood T-lymphocytes may be due to a large number entering the center. In this study, immune infiltration analysis showed that nine immune cell types were significantly different between the IS and control groups: activated CD8 T cells, activated CD4 T cells, activated B cells, MDSC, CD56dim natural killer cells, neutrophils, type 2T helper cells, memory B cells, and monocytes. However, the mechanism of inhibition in previous studies remains unclear and requires further investigation. Further studies found that PRDX1 had the strongest positive correlation with type 2T helper cells, consistent with previous studies73,74, and GPX4 had the strongest negative correlation with neutrophils, consistent with previous studies75,76.
miRNAs play an important role in IS development77. In this study, 3747 miRNA-mRNA-TF regulatory pairs were identified in the miRNA-mRNA-TF regulatory network, including hsa-miR-4469-CDKN1A-BACH2 and hsa-miR-188-3p-GPX4-ATF2. The current study found that the miR-188-3p/GPX4 Signaling axis is involved in the improvement of germacrone-mediated diabetic nephropathy by regulating ferroptosis78, and miR-4469-CDKN1A is only involved in the development of multiple cancers79,80. In addition, there were significant differences in the therapeutic sensitivities of the 50 drugs in the IS samples, including A.770041, AUY922, AZD8055, BMS.509744, and docetaxel. A previous study found that A-770041 could reverse paclitaxel and doxorubicin resistance in osteosarcoma cells and prevent organ allograft rejection81,82. Inhibition of Hsp90 by AUY922 is an effective strategy for the treatment of myxoid liposarcoma83. Moreover, AZD8055 induces autophagy and AMPK activation-related cell death in hepatocellular carcinoma84. BMS-509744 is a selective inhibitor of interleukin-2-inducible T-cell kinase, and topical application can ameliorate imiquimod-induced skin inflammation in mice85. Docetaxel can remodel the immune microenvironment of prostate cancer and enhance immunotherapy based on checkpoint inhibitors86. However, none of these drugs has been used in the treatment and research of IS, which needs to be confirmed in further studies. These results provide a theoretical basis for the treatment, evaluation, and research on the efficacy of IS.
This study identified a diagnostic association between oxidative stress-ferrozosis and IS genes, and drug prediction analysis was performed to provide a new reference for the diagnosis and treatment of patients with IS. However, this study had some limitations.
Initially, the identification of biomarkers was constrained by the limited scope of clinical samples available in public databases, which necessitates the critical expansion of the sample size for robust analysis. Furthermore, while the diagnostic utility of these biomarkers has been appraised using ROC curves, it is imperative to recognize that this approach represents only a single assessment dimension. A more comprehensive and substantiated basis for clinical decision making involves integrating clinical data with multiple evaluative metrics. Consequently, the purported clinical diagnostic merit of the four identified biomarkers warrants further validation through extensive validation using large-scale clinical samples. Furthermore, it is necessary to compare these four biomarkers with standard IS biomarkers to evaluate their value in the prognosis and treatment effectiveness of patients with IS. Correspondingly, the efficacy and cost-effectiveness of the resultant targeted therapies derived from analytical methods must be evaluated thoroughly. Finally, future research endeavors should prioritize elucidating the molecular mechanisms underlying these biomarkers by utilizing well-constructed animal or cellular models.
Conclusions
Oxidative stress can increase the intracellular iron concentration, and iron-catalyzed Fenton and Haber–Weiss reactions can produce a large amount of free radicals, further exacerbating the oxidative stress response. During ferroptosis, iron reacts with unsaturated fatty acids in the cell membrane to form hydroxyl radicals, which can cause membrane lipid peroxidation and induce ferroptosis. Therefore, the relationship between oxidative stress and iron death is very close, and the two mutually promote and affect each other, respectively. In this study, we identified biomarkers associated with oxidative stress and ferroptosis using bioinformatics and achieved good classification results, which can provide new directions and methods for the early diagnosis and treatment of IS. We also analyzed the biological functions of biomarkers and revealed the important roles of oxidative stress and iron death in IS pathogenesis, providing new clues and theoretical support for a deeper understanding of IS pathogenesis. We believe that our research direction and results make our research novel and unique with academic value.
Supplementary Information
Acknowledgements
We would like to express our gratitude to AJE, an English editing company, for revising and providing comments that have significantly improved our manuscript.
Abbreviations
- IS
Ischemic stroke
- SIID
Stroke-prone immunosuppression
- WGCNA
Weighted gene co-expression network analysis
- GEO
Gene expression omnibus
- GSEA
Gene Set Enrichment Analysis
- DEGs
Differentially expressed genes
- PRDX1
Peroxyregen 1
- H2O2
Hydrogen peroxide
- MT
Melatonin
- HMOX1
Heme oxygenase 1
- PTMs
Protein post-translational modifications
- qRT-PCR
Quantitative real-time polymerase chain reaction
- GPX4
Glutathione peroxidase 4
- LOX-5
Lipoxygenase isotype 5
- OS
Oxidative stress
- ORGs
Oxidative stress-related genes
- FRGs
Ferroptosis-related genes
- DEmRNA
Differentially expressed mRNA
- ORGs
Oxidative stress-related genes
- PPI
Protein–protein interaction
- OS
Oxidative stress
- ROS
Reactive oxygen species
Author contributions
M.L., X.L., and L.Z. conceptualized and planned the study; G.X., X.X., Q.Z.,and B.Z. performed the experiments; Xin-ling Liang, Guei-fei Xiong, and xuan-lin Xin analyzed the data. Ming-wei Liu wrote the manuscript. X.X. prepared figures 1-7 All authors have read and approved the final version of the manuscript.
Funding
This work was supported by The Major Science and Technology Special Project of Yunnan Province under Grant [No. 202102AA100061], Nature Science Foundation of China under Grant [No. 82060252] and [No. 81960350], Yunnan Applied Basic Research Project-Union Foundation of China under Grant [No. 202201AY070001-091],Yunnan Basic Research Projects under Grant [No.2018FB115], and Applied Basic Research of Yunnan Neurological Disease Diagnosis and Treatment Center under Grant [NO.ZX2019-03-05].
Data availability
All other raw data were accessed by contacting the corresponding author, if any qualified researcher required them.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Lin-Ming Zhang and Xing-ling Liang.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-54555-2.
References
- 1.Chehaibi K, Trabelsi I, Mahdouani K, Slimane MN. Correlation of oxidative stress parameters and inflammatory markers in ischemic stroke patients. J. Stroke Cerebrovasc. Dis. 2016;25(11):2585–2593. doi: 10.1016/j.jstrokecerebrovasdis.2016.06.042. [DOI] [PubMed] [Google Scholar]
- 2.Paul S, Candelario-Jalil E. Emerging neuroprotective strategies for the treatment of ischemic stroke: An overview of clinical and preclinical studies. Exp. Neurol. 2021;335:113518. doi: 10.1016/j.expneurol.2020.113518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pluta R, Januszewski S, Czuczwar SJ. The role of gut microbiota in an ischemic stroke. Int. J. Mol. Sci. 2021;22:2. doi: 10.3390/ijms22020915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu R, Song P, Gu X, Liang W, Sun W, Hua Q, et al. Comprehensive landscape of immune infiltration and aberrant pathway activation in ischemic stroke. Front. Immunol. 2021;12:766724. doi: 10.3389/fimmu.2021.766724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ren JX, Li C, Yan XL, Qu Y, Yang Y, Guo ZN. Crosstalk between oxidative stress and ferroptosis/oxytosis in ischemic stroke: Possible targets and molecular mechanisms. Oxid. Med. Cell Longev. 2021;2021:6643382. doi: 10.1155/2021/6643382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Q, Han X, Lan X, Gao Y, Wan J, Durham F, et al. Inhibition of neuronal ferroptosis protects hemorrhagic brain. JCI Insight. 2017;2(7):e90777. doi: 10.1172/jci.insight.90777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen GH, Song CC, Pantopoulos K, Wei XL, Zheng H, Luo Z. Mitochondrial oxidative stress mediated Fe-induced ferroptosis via the NRF2-ARE pathway. Free Radic. Biol. Med. 2022;180:95–107. doi: 10.1016/j.freeradbiomed.2022.01.012. [DOI] [PubMed] [Google Scholar]
- 8.Seiler A, Schneider M, Förster H, Roth S, Wirth EK, Culmsee C, et al. Glutathione peroxidase 4 senses and translates oxidative stress into 12/15-lipoxygenase dependent- and AIF-mediated cell death. Cell Metab. 2008;8(3):237–248. doi: 10.1016/j.cmet.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Yang WS, SriRamaratnam R, Welsch ME, Shimada K, Skouta R, Viswanathan VS, et al. Regulation of ferroptotic cancer cell death by GPX4. Cell. 2014;156(1–2):317–331. doi: 10.1016/j.cell.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wen Z, Wu L, Wang L, Ou Q, Ma H, Wu Q, Zhang S, Song Y. Comprehensive genetic analysis of tuberculosis and identification of candidate biomarkers. Front. Genet. 2022;13:832739. doi: 10.3389/fgene.2022.832739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fan J, Cao S, Chen M, Yao Q, Zhang X, Du S, et al. Investigating the AC079305/DUSP1 axis as oxidative stress-related signatures and immune infiltration characteristics in ischemic stroke. Oxid. Med. Cell Longev. 2022;2022:8432352. doi: 10.1155/2022/8432352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y, Chen G, Shao W. Identification of ferroptosis-related genes in alzheimer's disease based on bioinformatic analysis. Front. Neurosci. 2022;16:823741. doi: 10.3389/fnins.2022.823741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robinson MD, McCarthy DJ, Smyth GK. edgeR: A Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 2010;26(1):139–140. doi: 10.1093/bioinformatics/btp616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolde, R. pheatmap: Pretty Heatmaps. R package version 061 (2018).
- 15.Ito K, Murphy D. Application of ggplot2 to pharmacometric graphics. CPT Pharmacometr. Syst. Pharmacol. 2013;2(10):e79. doi: 10.1038/psp.2013.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanehisa M, Goto S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28(1):27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanehisa M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. 2019;28(11):1947–1951. doi: 10.1002/pro.3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanehisa M, Furumichi M, Sato Y, Kawashima M, Ishiguro-Watanabe M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 2023;51(1):D587–D592. doi: 10.1093/nar/gkac963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu T, Hu E, Xu S, Chen M, Guo P, Dai Z, et al. clusterProfiler 4.0: A universal enrichment tool for interpreting omics data. Innovat. (Camb). 2021;2(3):100141. doi: 10.1016/j.xinn.2021.100141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J. Stat. Softw. 2010;33(1):1–22. doi: 10.18637/jss.v033.i01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luo L, Zhang S, Guo N, Li H, He S. ACSF2-mediated ferroptosis is involved in ulcerative colitis. Life Sci. 2023;313:121272. doi: 10.1016/j.lfs.2022.121272. [DOI] [PubMed] [Google Scholar]
- 22.Huang ML, Hung YH, Lee WM, Li RK, Jiang BR. SVM-RFE based feature selection and Taguchi parameters optimization for multiclass SVM classifier. Sci. World J. 2014;2014:795624. doi: 10.1155/2014/795624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. U. S. A. 2005;102(43):15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cui Y, Zhang Y, Zhao X, Shao L, Liu G, Sun C, et al. ACSL4 exacerbates ischemic stroke by promoting ferroptosis-induced brain injury and neuroinflammation. Brain Behav. Immun. 2021;93:312–321. doi: 10.1016/j.bbi.2021.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Li C, Sun G, Chen B, Xu L, Ye Y, He J, et al. Nuclear receptor coactivator 4-mediated ferritinophagy contributes to cerebral ischemia-induced ferroptosis in ischemic stroke. Pharmacol. Res. 2021;174:105933. doi: 10.1016/j.phrs.2021.105933. [DOI] [PubMed] [Google Scholar]
- 26.Li S, Zhou C, Zhu Y, Chao Z, Sheng Z, Zhang Y, et al. Ferrostatin-1 alleviates angiotensin II (Ang II)- induced inflammation and ferroptosis in astrocytes. Int. Immunopharmacol. 2021;90:107179. doi: 10.1016/j.intimp.2020.107179. [DOI] [PubMed] [Google Scholar]
- 27.Kim S, Lee W, Jo H, Sonn SK, Jeong SJ, Seo S, et al. The antioxidant enzyme Peroxiredoxin-1 controls stroke-associated microglia against acute ischemic stroke. Redox Biol. 2022;54:102347. doi: 10.1016/j.redox.2022.102347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fan J, Chen M, Cao S, Yao Q, Zhang X, Du S, et al. Identification of a ferroptosis-related gene pair biomarker with immune infiltration landscapes in ischemic stroke: A bioinformatics-based comprehensive study. BMC Genom. 2022;23(1):59. doi: 10.1186/s12864-022-08295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pan Y, Wang X, Liu X, Shen L, Chen Q, Shu Q. Targeting ferroptosis as a promising therapeutic strategy for ischemia-reperfusion injury. Antioxid. (Basel) 2022;11(11):2196. doi: 10.3390/antiox11112196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shanshan Y, Beibei J, Li T, Minna G, Shipeng L, Li P, Yong Z. Phospholipase A2 of peroxiredoxin 6 plays a critical role in cerebral ischemia/reperfusion inflammatory injury. Front. Cell Neurosci. 2017;11:99. doi: 10.3389/fncel.2017.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liao J, Zhang Y, Chen X, Zhang J. The roles of peroxiredoxin 6 in brain diseases. Mol. Neurobiol. 2021;58(9):4348–4364. doi: 10.1007/s12035-021-02427-5. [DOI] [PubMed] [Google Scholar]
- 32.Zhou L, Chen X, Lu M, Wu Q, Yuan Q, Hu C, et al. Wnt/β-catenin links oxidative stress to podocyte injury and proteinuria. Kidney Int. 2019;95(4):830–845. doi: 10.1016/j.kint.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ursini F, Maiorino M. Lipid peroxidation and ferroptosis: The role of GSH and GPx4. Free Radic. Biol. Med. 2020;152:175–185. doi: 10.1016/j.freeradbiomed.2020.02.027. [DOI] [PubMed] [Google Scholar]
- 34.Miao Y, Chen Y, Xue F, Liu K, Zhu B, Gao J, et al. Contribution of ferroptosis and GPX4's dual functions to osteoarthritis progression. EBioMedicine. 2022;76:103847. doi: 10.1016/j.ebiom.2022.103847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yuan Y, Zhai Y, Chen J, Xu X, Wang H. Kaempferol ameliorates oxygen-glucose deprivation/reoxygenation-induced neuronal ferroptosis by activating Nrf2/SLC7A11/GPX4 axis. Biomolecules. 2021;11:7. doi: 10.3390/biom11070923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.López-Domínguez JA, Rodríguez-López S, Ahumada-Castro U, Desprez PY, Konovalenko M, Laberge RM, et al. Cdkn1a transcript variant 2 is a marker of aging and cellular senescence. Aging (Albany N. Y.) 2021;13(10):13380–13392. doi: 10.18632/aging.203110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Montaigne D, Marechal X, Modine T, Coisne A, Mouton S, Fayad G, et al. Daytime variation of perioperative myocardial injury in cardiac surgery and its prevention by Rev-Erbα antagonism: A single-centre propensity-matched cohort study and a randomised study. Lancet. 2018;391(10115):59–69. doi: 10.1016/S0140-6736(17)32132-3. [DOI] [PubMed] [Google Scholar]
- 38.Rodríguez I, Coto E, Reguero JR, González P, Andrés V, Lozano I, et al. Role of the CDKN1A/p21, CDKN1C/p57, and CDKN2A/p16 genes in the risk of atherosclerosis and myocardial infarction. Cell Cycle. 2007;6(5):620–625. doi: 10.4161/cc.6.5.3927. [DOI] [PubMed] [Google Scholar]
- 39.Jiang W, Song Q, Lu Z, Wang S, Liu T, Wang X, et al. Myocardial infarction-associated extracellular vesicle-delivered miR-208b affects the growth of human umbilical vein endothelial cells via regulating CDKN1A. Biomed. Res. Int. 2021;2021:9965639. doi: 10.1155/2021/9965639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neumann CA, Krause DS, Carman CV, Das S, Dubey DP, Abraham JL, et al. Essential role for the peroxiredoxin Prdx1 in erythrocyte antioxidant defence and tumour suppression. Nature. 2003;424(6948):561–565. doi: 10.1038/nature01819. [DOI] [PubMed] [Google Scholar]
- 41.Butterfield LH, Merino A, Golub SH, Shau H. From cytoprotection to tumor suppression: The multifactorial role of peroxiredoxins. Antioxid. Redox Signal. 1999;1(4):385–402. doi: 10.1089/ars.1999.1.4-385. [DOI] [PubMed] [Google Scholar]
- 42.Ledgerwood EC, Marshall JW, Weijman JF. The role of peroxiredoxin 1 in redox sensing and transducing. Arch. Biochem. Biophys. 2017;617:60–67. doi: 10.1016/j.abb.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 43.Li X, Chen J, Yuan S, Zhuang X, Qiao T. Activation of the P62-Keap1-NRF2 pathway protects against ferroptosis in radiation-induced lung injury. Oxid. Med. Cell Longev. 2022;2022:8973509. doi: 10.1155/2022/8973509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen D, Tavana O, Chu B, Erber L, Chen Y, Baer R, et al. NRF2 is a major target of ARF in p53-independent tumor suppression. Mol. Cell. 2017;68(1):224–232.e224. doi: 10.1016/j.molcel.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Q, Hu Y, Hu JE, Ding Y, Shen Y, Xu H, et al. Sp1-mediated upregulation of Prdx6 expression prevents podocyte injury in diabetic nephropathy via mitigation of oxidative stress and ferroptosis. Life Sci. 2021;278:119529. doi: 10.1016/j.lfs.2021.119529. [DOI] [PubMed] [Google Scholar]
- 46.Yu H, Yu Y, Zhao Z, Cui L, Hou J, Shi H. Prdx6 is required to protect human corneal epithelial cells against ultraviolet B injury. Eur. J. Ophthalmol. 2021;31(2):367–378. doi: 10.1177/1120672119896426. [DOI] [PubMed] [Google Scholar]
- 47.Tang B, Ni W, Zhou J, Ling Y, Niu D, Lu X, et al. Peroxiredoxin 6 secreted by Schwann-like cells protects neuron against ischemic stroke in rats via PTEN/PI3K/AKT pathway. Tissue Cell. 2021;73:101635. doi: 10.1016/j.tice.2021.101635. [DOI] [PubMed] [Google Scholar]
- 48.Xiao H, Wang K, Li D, Wang K, Yu M. Evaluation of FGFR1 as a diagnostic biomarker for ovarian cancer using TCGA and GEO datasets. PeerJ. 2021;9:e10817. doi: 10.7717/peerj.10817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saber MM. Diagnostic performance of PD-L1 versus PD-1 expression in circulating CD20 cells in diffuse large B-cell lymphoma. Antibodies (Basel) 2022;11(1):15. doi: 10.3390/antib11010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang Y, Zhang M, Hu X, Qin W, Wu H, Wei M. Colon cancer-specific diagnostic and prognostic biomarkers based on genome-wide abnormal DNA methylation. Aging (Albany N. Y.) 2020;12(22):22626–22655. doi: 10.18632/aging.103874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhai CL, Tang GM, Qian G, Han BJ, Hu HL, Wang SJ, et al. miR-190 protects cardiomyocytes from apoptosis induced by H2O2 through targeting MAPK8 and regulating MAPK8/ERK signal pathway. Int. J. Clin. Exp. Pathol. 2018;11(4):2183–2192. [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang SX, Yu CH. Silencing of UCA1 attenuates the ox-LDL-induced injury of human umbilical vein endothelial cells via miR-873-5p/MAPK8 axis. Kaohsiung J. Med. Sci. 2023;39(1):6–15. doi: 10.1002/kjm2.12612. [DOI] [PubMed] [Google Scholar]
- 53.Guo QQ, Wang SS, Zhang SS, Xu HD, Li XM, Guan Y, et al. ATM-CHK2-Beclin 1 axis promotes autophagy to maintain ROS homeostasis under oxidative stress. Embo J. 2020;39(10):e103111. doi: 10.15252/embj.2019103111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang Y, Wang B, Liu Y, Guo Y, Lu H, Liu X. Inhibition of PI3K/Akt/mTOR signaling by NDRG2 contributes to neuronal apoptosis and autophagy in ischemic stroke. J. Stroke Cerebrovasc. Dis. 2023;32(3):106984. doi: 10.1016/j.jstrokecerebrovasdis.2023.106984. [DOI] [PubMed] [Google Scholar]
- 55.Jin W, Zhao J, Yang E, Wang Y, Wang Q, Wu Y, et al. Neuronal STAT3/HIF-1α/PTRF axis-mediated bioenergetic disturbance exacerbates cerebral ischemia-reperfusion injury via PLA2G4A. Theranostics. 2022;12(7):3196–3216. doi: 10.7150/thno.71029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xiang Y, Wei X, Du P, Zhao H, Liu A, Chen Y. β-Arrestin-2-ERK1/2 cPLA(2)α axis mediates TLR4 signaling to influence eicosanoid induction in ischemic brain. Faseb J. 2019;33(5):6584–6595. doi: 10.1096/fj.201802020R. [DOI] [PubMed] [Google Scholar]
- 57.Roidl D, Hellbach N, Bovio PP, Villarreal A, Heidrich S, Nestel S, et al. DOT1L activity promotes proliferation and protects cortical neural stem cells from activation of ATF4-DDIT3-mediated ER stress in vitro. Stem Cells. 2016;34(1):233–245. doi: 10.1002/stem.2187. [DOI] [PubMed] [Google Scholar]
- 58.Kim EH, Kim DH, Kim HR, Kim SY, Kim HH, Bang OY. Stroke serum priming modulates characteristics of mesenchymal stromal cells by controlling the expression miRNA-20a. Cell Transplant. 2016;25(8):1489–1499. doi: 10.3727/096368916X690430. [DOI] [PubMed] [Google Scholar]
- 59.Nada SE, Tulsulkar J, Shah ZA. Heme oxygenase 1-mediated neurogenesis is enhanced by Ginkgo biloba (EGb 761®) after permanent ischemic stroke in mice. Mol. Neurobiol. 2014;49(2):945–956. doi: 10.1007/s12035-013-8572-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yang T, Wu J, Ge K, Wang F, Fan J. MicroRNA-193b-3p reduces oxidative stress and mitochondrial damage in rats with cerebral ischemia-reperfusion injury via the seven in absentia homolog 1/Jun N-terminal kinase pathway. Bioengineered. 2022;13(3):6942–6954. doi: 10.1080/21655979.2022.2036398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bartelt-Kirbach B, Slowik A, Beyer C, Golenhofen N. Upregulation and phosphorylation of HspB1/Hsp25 and HspB5/αB-crystallin after transient middle cerebral artery occlusion in rats. Cell Stress Chaperones. 2017;22(4):653–663. doi: 10.1007/s12192-017-0794-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang Y, Yao Z, Xiao Y, Zhang X, Liu J. Downregulated XBP-1 rescues cerebral ischemia/reperfusion injury-induced pyroptosis via the NLRP3/Caspase-1/GSDMD axis. Mediat. Inflamm. 2022;2022:8007078. doi: 10.1155/2022/8007078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang X, Wu Q, Wang Z, Li H, Dai J. Keap1-Nrf2/ARE signal pathway activated by butylphthalide in the treatment of ischemic stroke. Am. J. Transl. Res. 2022;14(4):2637–2646. [PMC free article] [PubMed] [Google Scholar]
- 64.Liu T, Han S, Dai Q, Zheng J, Liu C, Li S, et al. IL-17A-mediated excessive autophagy aggravated neuronal ischemic injuries via Src-PP2B-mTOR pathway. Front. Immunol. 2019;10:2952. doi: 10.3389/fimmu.2019.02952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhou B, Liu J, Kang R, Klionsky DJ, Kroemer G, Tang D. Ferroptosis is a type of autophagy-dependent cell death. Semin. Cancer Biol. 2020;66:89–100. doi: 10.1016/j.semcancer.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 66.Zeng T, Zhang S, He Y, Liu Z, Cheng Q. MiR-361-5p promotes oxygen-glucose deprivation/re-oxygenation induced neuronal injury by negatively regulating SQSTM1 in vitro. Metab. Brain Dis. 2021;36(8):2359–2368. doi: 10.1007/s11011-021-00845-x. [DOI] [PubMed] [Google Scholar]
- 67.Kamel H, Iadecola C. Brain-immune interactions and ischemic stroke: Clinical implications. Arch. Neurol. 2012;69(5):576–581. doi: 10.1001/archneurol.2011.3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang Y, Zhang JH, Sheng J, Shao A. Immunoreactive cells after cerebral ischemia. Front. Immunol. 2019;10:2781. doi: 10.3389/fimmu.2019.02781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Członkowska A, Cyrta B, Korlak J. Immunological observations on patients with acute cerebral vascular disease. J. Neurol. Sci. 1979;43(3):455–464. doi: 10.1016/0022-510X(79)90024-8. [DOI] [PubMed] [Google Scholar]
- 70.Berczi I. The stress concept and neuroimmunoregulation in modern biology. Ann. N. Y. Acad. Sci. 1998;851:3–12. doi: 10.1111/j.1749-6632.1998.tb08969.x. [DOI] [PubMed] [Google Scholar]
- 71.Fiorina P, Lattuada G, Silvestrini C, Ponari O, Dall'Aglio P. Disruption of nocturnal melatonin rhythm and immunological involvement in ischaemic stroke patients. Scand. J. Immunol. 1999;50(2):228–231. doi: 10.1046/j.1365-3083.1999.00579.x. [DOI] [PubMed] [Google Scholar]
- 72.Campanella M, Sciorati C, Tarozzo G, Beltramo M. Flow cytometric analysis of inflammatory cells in ischemic rat brain. Stroke. 2002;33(2):586–592. doi: 10.1161/hs0202.103399. [DOI] [PubMed] [Google Scholar]
- 73.Lv L, Bai J, Gao Y, Jin L, Wang X, Cao M, et al. Peroxiredoxin 1 interacts with TBK1/IKKε and negatively regulates pseudorabies virus propagation by promoting innate immunity. J. Virol. 2021;95(19):e0092321. doi: 10.1128/JVI.00923-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu GP, Xiang LX, Shao T, Lin AF, Shao JZ. Stimulatory function of peroxiredoxin 1 in activating adaptive humoral immunity in a zebrafish model. Dev. Comp. Immunol. 2018;84:353–360. doi: 10.1016/j.dci.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 75.Li P, Jiang M, Li K, Li H, Zhou Y, Xiao X, et al. Glutathione peroxidase 4-regulated neutrophil ferroptosis induces systemic autoimmunity. Nat. Immunol. 2021;22(9):1107–1117. doi: 10.1038/s41590-021-00993-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yee PP, Wei Y, Kim SY, Lu T, Chih SY, Lawson C, et al. Neutrophil-induced ferroptosis promotes tumor necrosis in glioblastoma progression. Nat. Commun. 2020;11(1):5424. doi: 10.1038/s41467-020-19193-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Can U, Marzioglu E, Akdu S. Some miRNA expressions and their targets in ischemic stroke. Nucleosides Nucleotid. Nucleic Acids. 2022;41(11):1224–1262. doi: 10.1080/15257770.2022.2098974. [DOI] [PubMed] [Google Scholar]
- 78.Jin J, Wang Y, Zheng D, Liang M, He Q. A novel identified circular RNA, mmu_mmu_circRNA_0000309, involves in germacrone-mediated improvement of diabetic nephropathy through regulating ferroptosis by targeting miR-188-3p/GPX4 signaling axis. Antioxid. Redox Signal. 2022;36(10–12):740–759. doi: 10.1089/ars.2021.0063. [DOI] [PubMed] [Google Scholar]
- 79.Cao T, Xiao T, Huang G, Xu Y, Zhu JJ, Wang K, et al. CDK3, target of miR-4469, suppresses breast cancer metastasis via inhibiting Wnt/β-catenin pathway. Oncotarget. 2017;8(49):84917–84927. doi: 10.18632/oncotarget.18171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Liu ZH, Yang SZ, Li WY, Dong SY, Zhou SY, Xu S. circRNA_141539 can serve as an oncogenic factor in esophageal squamous cell carcinoma by sponging miR-4469 and activating CDK3 gene. Aging (Albany N. Y.) 2021;13(8):12179–12193. doi: 10.18632/aging.103071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Duan Z, Zhang J, Ye S, Shen J, Choy E, Cote G, et al. A-770041 reverses paclitaxel and doxorubicin resistance in osteosarcoma cells. BMC Cancer. 2014;14:681. doi: 10.1186/1471-2407-14-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Burchat A, Borhani DW, Calderwood DJ, Hirst GC, Li B, Stachlewitz RF. Discovery of A-770041, a src-family selective orally active lck inhibitor that prevents organ allograft rejection. Bioorg. Med. Chem. Lett. 2006;16(1):118–122. doi: 10.1016/j.bmcl.2005.09.039. [DOI] [PubMed] [Google Scholar]
- 83.Steinmann S, Gali-Muhtasib H, Huebner K, Al-Halabi R, Abou Merhi R, Aman P, et al. Hsp90 inhibition by AUY922 as an effective treatment strategy against myxoid liposarcoma. Cancer Lett. 2015;367(2):147–156. doi: 10.1016/j.canlet.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 84.Hu M, Huang H, Zhao R, Li P, Li M, Miao H, et al. AZD8055 induces cell death associated with autophagy and activation of AMPK in hepatocellular carcinoma. Oncol. Rep. 2014;31(2):649–656. doi: 10.3892/or.2013.2890. [DOI] [PubMed] [Google Scholar]
- 85.Otake S, Otsubaki T, Uesato N, Ueda Y, Murayama T, Hayashi M. Topical application of BMS-509744, a selective inhibitor of interleukin-2-inducible T cell kinase, ameliorates imiquimod-induced skin inflammation in mice. Biol. Pharm. Bull. 2021;44(4):528–534. doi: 10.1248/bpb.b20-00850. [DOI] [PubMed] [Google Scholar]
- 86.Ma Z, Zhang W, Dong B, Xin Z, Ji Y, Su R, et al. Docetaxel remodels prostate cancer immune microenvironment and enhances checkpoint inhibitor-based immunotherapy. Theranostics. 2022;12(11):4965–4979. doi: 10.7150/thno.73152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All other raw data were accessed by contacting the corresponding author, if any qualified researcher required them.