Abstract
Background
There is a growing interest in developing scalable interventions, including internet-based cognitive behavioral therapy (iCBT), to meet the increasing demand for mental health services. Given the growth in diversity worldwide, it is essential that the clinical trials of iCBT for depression include diverse samples or, at least, report information on the race, ethnicity, or other background indicators of their samples. Unfortunately, the field lacks data on how well diversity is currently reported and represented in the iCBT literature.
Objective
Thus, the main objective of this systematic review was to examine the overall reporting of racial and ethnic identities in published clinical trials of iCBT for depression. We also aimed to review the representation of specific racial and ethnic minoritized groups and the inclusion of alternative background indicators such as migration status or country of residence.
Methods
Studies were included if they were randomized controlled trials in which iCBT was compared to a waiting list, care-as-usual, active control, or another iCBT. The included papers also had to have a focus on acute treatment (eg, 4 weeks to 6 months) of depression, be delivered via the internet on a website or a smartphone app and use guided or unguided self-help. Studies were initially identified from the METAPSY database (n=59) and then extended to include papers up to 2022, with papers retrieved from Embase, PubMed, PsycINFO, and Cochrane (n=3). Risk of bias assessment suggested that reported studies had at least some risk of bias due to use of self-report outcome measures.
Results
A total of 62 iCBT randomized controlled trials representing 17,210 participants are summarized in this study. Out of those 62 papers, only 17 (27%) of the trials reported race, and only 12 (19%) reported ethnicity. Reporting outside of the United States was very poor, with the United States accounting for 15 (88%) out of 17 of studies that reported race and 9 (75%) out of 12 for ethnicity. Out of 3,623 participants whose race was reported in the systematic review, the racial category reported the most was White (n=2716, 74.9%), followed by Asian (n=209, 5.8%) and Black (n=274, 7.6%). Furthermore, only 25 (54%) out of the 46 papers conducted outside of the United States reported other background demographics.
Conclusions
It is important to note that the underreporting observed in this study does not necessarily indicate an underrepresentation in the actual study population. However, these findings highlight the poor reporting of race and ethnicity in iCBT trials for depression found in the literature. This lack of diversity reporting may have significant implications for the scalability of these interventions.
Keywords: diversity; cognitive behavioral therapy; internet-based; depression; race; racial; ethnicity; culture; depressive; diverse; inclusive; inclusivity; DEI; diversity, equity, and inclusion; internet-based cognitive behavioral therapy; mental health; ethnic; cultures; culturally; review methods; review methodology; systematic; clinical trial; clinical trials; randomized controlled trial; randomized controlled trials; controlled trial; controlled trials; reporting; immigrant; migrant; migrants; immigrants; psychotherapy; underrepresented; underrepresentation; representation; mobile phone
Introduction
Background
In 2020, approximately 34% of the US population identified themselves as belonging to racial minoritized groups, and 19% identified as members of ethnic minoritized groups [1]. Following the terminology used by other scholars [2], we employ the term “minoritized” rather than “minorities” to emphasize that these individuals’ experiences are not intrinsic qualities of statistically small groups; instead, they are the result of dominant groups subordinating and, consequently, “minoritizing” them. The proportion of individuals belonging to a racial or ethnic minoritized group in the United States is expected to continue growing [3]. This increase in the proportion of minoritized groups is also expected in other countries. There are currently an estimated 272 million immigrants worldwide, with 82 million residing in Europe, 59 million in North America, and 49 million in Northern Africa and Western Asia [4]. Therefore, it is essential that mental health research responds to this increase in racial and ethnic diversity.
Mental health is one of the leading causes of disability in the United States and worldwide [5]. Among mental disorders, depression is the leading cause of significant disability [6] with an estimated economic burden of around US $210.5 billion per year in the United States alone [6]. Thus, given that mental health is strongly correlated with racial-ethnic identity and with other factors that are themselves linked to mental health (eg, socioeconomic status), there is a strong imperative for mental health research to represent the racial-ethnic diversity in our populations [7-9].
Current Reporting on Race and Ethnicity
Current research in mental health continues to use primarily non-Hispanic White populations, which fails to reflect the demographic makeup of countries worldwide. For example, in a study by Mak and colleagues [10], they reviewed 379 National Institute of Mental Health–funded clinical trials for various mental health disorders published between 1995 and 2004 to investigate how many trials reported sex, race, and ethnicity. They found that 91.6% of the National Institute of Mental Health–funded published trials reported sex. However, only 47.8% included race or ethnicity in their demographics, and 25.6% had incomplete race or ethnicity information.
Since then, the overall pattern of reporting demographic information has improved slightly. A more recent meta-analysis by Polo and colleagues [11] examines the trends in reporting and representation of racial-ethnic diversity in randomized controlled trials (RCT) of psychotherapy for depression for over 36 years. They found that reporting of racial-ethnic group membership increased from 16% to 55% during this time. This increase was attributed to the introduction of new guidelines aimed at increasing gender, race, and ethnicity reporting on RCTs. These guidelines included the National Institutes of Health Guidelines on the Inclusion of Women and Minorities as Subjects in Clinical Research in 1994 [12], the CONSORT (Consolidated Standards of Reporting Trials) [13] in 2001, and the American Psychological Association Publications and Communications Board Working Group on Journal Article Reporting Standards (JARS) in 2008. However, the reporting of treatment effects by ethnic groups remained at a low at 2.1% [11]. Additionally, only non-Hispanic Black and Latino individuals were represented significantly more than in previous years. Asian Americans, multiracial individuals, Native Americans or Native Alaskans, and Native Hawaiians or Pacific Islanders were still underrepresented in the literature, with no significant change across time [11] despite evidence that participants are willing to engage in web-based health-related research [14].
Depression and Health Disparities
Existing research on depression and race-ethnicity presents a somewhat complex picture. In the United States, apart from Native Americans, who have the highest rates of depression, minoritized groups tend to have lower rates of depression than non-Hispanic White individuals [15]. However, minoritized individuals may be at a higher risk for more severely debilitating depression when compared to non-Hispanic White individuals [16]. Additionally, the costs associated with treating depression may impact racial groups differently. For example, those who are middle class and Black tend to encounter more obstacles to upward mobility (ie, moving from one social class to another) and are more susceptible to downward mobility, which may impede their access to mental health care [17,18]. In 2020, 53% Black individuals experienced worse access to care than White individuals. Similarly, 29% of Asian individuals had worse access to care, while American Indian or Alaska Native individuals presented the largest disparity with 50% receiving worse access to care than White individuals. Native Hawaiian and Other Pacific Islander individuals, however, experienced the same level of access to care as White individuals [19].
Furthermore, substantial barriers in access to mental health care tend to affect minoritized racial-ethnic groups more than nonminoritized groups. For example, there is evidence that interpersonal factors (eg, stigma and personal shame), sociocultural factors (eg, fear of negative evaluation by family or peers, preference for traditional coping strategies such as withdrawal and “accepting fate”), and systemic factors (eg, lack of culturally centered clinical environments and culturally responsive services and language barriers) can make it difficult for members of racial-ethnic minoritized groups to access mental health care [20]. These barriers may be particularly pronounced in face-to-face mental health treatment settings, where patients need to engage fully with another person for it to be successful; however, innovative internet-based delivery methods (eg, internet-based cognitive behavioral therapy [iCBT] self-help) may reduce barriers to treatment by making it more accessible [21]. Moreover, there is evidence that shows that Latinx and non-Hispanic Black individuals may be willing to engage in smartphone-based interventions and bibliotherapy, respectively [22,23].
In addition to race and ethnicity, migration status is another crucial sociodemographic factor associated with depressive and anxious symptoms. For example, in a study involving 37,076 individuals from 20 European countries, first-generation migrants exhibited higher levels of depression, with rates significantly elevated for those born outside Europe [24]. Research on refugees resettled in high-income countries indicates that they experience increased rates of anxiety and depression compared to the general population [25]. These findings suggest that aspects such as migration status, country of origin, refugee status, and other related demographics play a significant role in predicting depression and anxiety symptoms, emphasizing the importance of providing mental health services to cater to these populations.
iCBT for Depression
One of the most studied and promising internet-based interventions for depression is iCBT. iCBT involves the provision of self-help materials (eg, websites, apps, and videos) that impart psychoeducation and teach skills that individuals can use to manage their symptoms. iCBT is usually delivered in 1 of 2 formats: guided or unguided. In guided self-help, individuals access self-help material and are assisted by a trained mental health professional or paraprofessional [26]. In unguided self-help, individuals access materials independently, without assistance or support. Both guided and unguided iCBT treatments have been shown to be more efficacious than waiting list controls [27].
Although unguided forms of self-help are more scalable and easier to access, guided self-help has been shown to be more effective than unguided self-help and as effective as face-to-face treatment [27]. Individuals may also adhere to it more closely [28]. Considering the wide support for the efficacy of iCBT, this format has the potential to reduce the public health burden of untreated depression, especially among individuals from a racial-ethnic minoritized group [21,29]. Given the potential for iCBT to reach minoritized communities, it is important to understand the reporting and representation of race-ethnicity in iCBT studies. If individuals from racial-ethnic minoritized groups are being underreported, it would be difficult to determine how well our current interventions meet the needs of these individuals.
For these reasons, we explored the reporting and representation of racial-ethnic diversity in clinical trials of iCBT for depression. Our first aim was to examine the overall reporting of individuals from racial-ethnic minoritized groups in published RCTs of iCBT for depression. Our second aim was to explore the representation of specific racial-ethnic minoritized groups in RCTs of iCBT for depression. To achieve these aims, we conducted a systematic review of RCTs of iCBT for depression and examined the reporting of race-ethnicity along with the representation (ie, the sample composition) [30-90]. We also explored the reporting of other background factors (eg, migration status).
Methods
Search Strategies
To identify RCTs, we employed a 2-pronged search strategy. First, we searched METAPSY, a database of randomized clinical trials for depression created by Cuijpers [91] and colleagues [92]. The public version of the database covers a search of trials between January 1, 1966, and January 2018, including Risk of Bias (ROB) assessments. We obtained an updated database version from one of the METAPSY lead researchers (P Cuijpers), which included studies up to January 1, 2021. The database of 763 studies was created from a search on PubMed, PsycINFO, Embase, and the Cochrane Library. The search was performed using terms involving psychotherapy (eg, “psychotherapy” and “cognitive-behavioral therapy”) and depression (eg, “depressive symptoms” and “major depression”). An example of the search string for PubMed can be found in Multimedia Appendix 1. Studies were included if they were an RCT in which a psychotherapy condition was compared to another. Control conditions included waiting list, treatment as usual, pill placebo, pharmacotherapy, alternate therapy delivery modalities (eg, single vs group therapy), or any other active control condition. Exclusion criteria included (1) no statement of randomization; (2) depression not being an inclusion criterion; (3) not being focused on acute treatment (eg, maintenance or relapse prevention); (4) studies with children or adolescents; (5) dissertation studies; (6) studies in which the depression was not the target of treatment; (7) if effect sizes could not be calculated; and (8) studies in languages other than English, Spanish, German, or Dutch. METAPSY contains a risk-of-bias assessment using the risk-of-bias assessment tool from the Cochrane Collaboration for papers published before 2018 [92]. Two raters (ARH-D and RDJ-R) examined the titles and abstracts of the 763 studies identified in METAPSY to decide whether they were relevant for review.
To obtain more recent papers, we used the same search string used for METAPSY [92] with the addition of a search term for internet-based studies to search Cochrane, PubMed, PsycINFO, and Embase for papers published between January 1, 2021, and July 18, 2022. An example search string for PubMed is available in Multimedia Appendix 2. This second search yielded an additional 2159 studies, of which 590 were duplicates. We also identified an additional paper by cross-referencing a study protocol. Further, 4 raters used a randomized, counterbalanced design to review the titles and abstracts of the remaining 1570 studies (ARH-D, JFB, LL-L, and RDJ-R). Disagreements between the raters were resolved by consensus.
We included randomized controlled trials in which iCBT was compared to a waiting list, care-as-usual, active control, or another iCBT treatment (eg, 2 different iCBTs or unguided vs guided iCBT). The included papers must have also focused on acute treatment (eg, 4 weeks to 6 months) of depression, delivered via the internet on a website or a smartphone app as guided or unguided self-help iCBT. In addition to the exclusion criteria used for METAPSY [91,92], we also excluded studies if the (1) interventions were not delivered via the internet, and (2) interventions focused on specific medical or psychiatric subpopulations (eg, individuals with cannabis use disorder). We excluded studies that used specific subpopulation samples because we aimed to study the general reporting and representation of race-ethnicity in trials of iCBT for depression [93,94]. Additionally, we concentrated on studies that examined depression to prevent overlapping treatment outcomes (eg, chronic pain, sleep, and biases due to the specificity of the pool of participants) [95]. Of the 2333 studies, 282 were identified as relevant to self-help iCBT for depression. We then examined the full text of these studies and excluded those that did not meet our inclusion criteria. See Figure 1 for the PRISMA (Preferred Reporting Items for Systematic Reviews) flowchart. We assessed the ROB for 20 papers that did not already have an ROB assessment in the public version of the METAPSY database, 17 that were provided in the METAPSY update and 3 we found in our systematic search (Multimedia Appendix 3).
Figure 1.
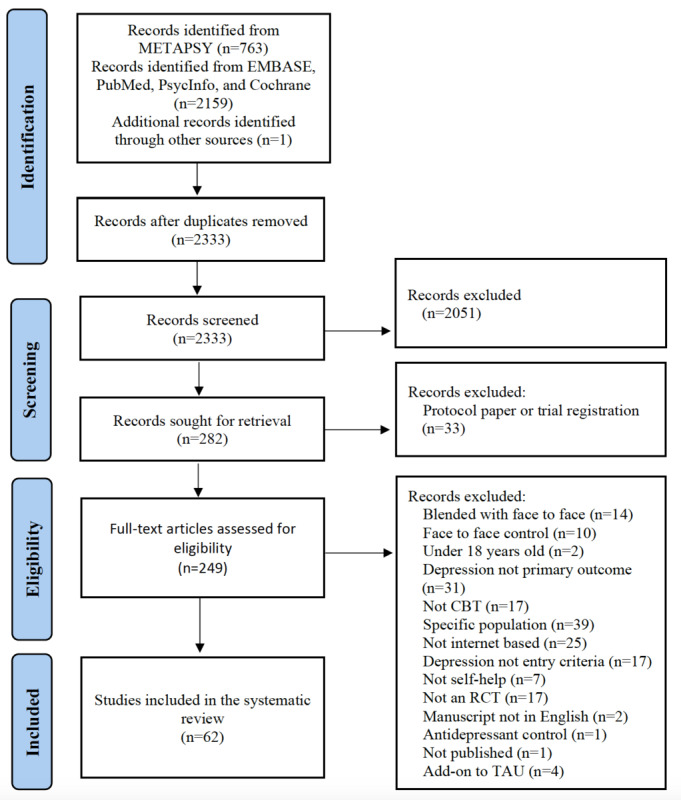
Flow diagram of papers at each stage of the screening process. CBT: cognitive behavioral therapy; RCT: randomized controlled trial; TAU: treatment as usual.
Coding
Coders rated study characteristics, trial design aspects, intervention type, and control group. They also coded various study-level features, including year of publication, whether the studies used guided or unguided iCBT and the country from which the study was sampled. For our primary question of interest, we first coded whether studies included race or ethnicity as “1” if they did or “0” if they did not. Additionally, when studies reported race or ethnicity, we recorded the number of participants in the sample that belonged to the different racial and ethnic groups. We then calculated the proportion of minoritized group members in the sample for the studies that reported overall race or ethnicity. Finally, given that we included studies conducted outside the United States, where there may be different conceptualizations of race and ethnicity, we also recorded other alternative variables indicative of participant background, including migration status, country of birth, country of residence, nationality, or native language. Agreement between raters was based on consensus, with disagreements being resolved by the principal investigator (LL-L).
Results
Study Selection and Characteristics
In total, 62 papers met the criteria of an RCT of iCBT for depression in adults. Some studies used samples from multiple countries or reported multiple arms, therefore, there are more interventions and control conditions than the number of studies (ie, 62). These studies included a total of 64 interventions of which 41 (64%) included guided self-help, and 23 (36%) included unguided self-help. Regarding control groups, 34 (52%) out of the 65 control groups included were compared to waiting lists, 12 (18%) to treatment as usual, 12 (18%) to active controls, and 7 (11%) used an internet-based active treatment comparator (ie, guided or unguided iCBT). The studies drew on samples from 13 countries: United States (n=17), Germany (n=12), Australia (n=10), Sweden (n=10), the Netherlands (n=6), China (n=2), Finland (n=2), United Kingdom (n=2), Canada (n=1), Colombia (n=1), Ireland (n=1), New Zealand (n=1), and Switzerland (n=1). The 62 papers included in this study had a total sample of 17,210 participants. ROB information is available in Multimedia Appendix 3 and suggests that reported studies had at least some ROB. However, most of this bias was due to self-reporting as an outcome measure. In the other ROB domains, 14 (70%) out of 20 of studies had low risk concerning missing outcome data, while 18 (90%) out of 20 of studies showed low risk for deviation from intended interventions.
Reporting of Race and Ethnicity
Of the 62 papers, only 17 (27%) reported race, and 12 (19%) reported ethnicity. Despite this overall low reporting rate, we observed that reporting differed markedly by the country sampled in the study (Fisher exact test P<.001). Of the studies conducted in the United States (n=17), almost all included race (n=15, 88%). Outside of the United States, only 2 studies conducted in the United Kingdom (n=1) and Australia (n=1) reported race. RCTs using samples from Germany, the Netherlands, Sweden, Ireland, Switzerland, China, Finland, Canada, Colombia, and New Zealand did not report race. Similarly, ethnicity was only reported in 12 studies, 4 of which grouped ethnicity with race. A fifth trial described reporting ethnicity, but it combined racial and ethnic categories; therefore, it was labeled as reporting both race and ethnicity. Additionally, 2 of them were conducted specifically on a minoritized group. The results are summarized in Table 1. Translating the reporting numbers to individuals, of the 17,210 participants in all these RCTs, 13,587 (78.9%) had no reported race, and 14,810 (86.1%) had no reported ethnicity.
Table 1.
Number of published randomized controlled trials of internet-based cognitive behavioral therapy that reported race or ethnicity, by reported source country (N=62).
| Country | Papers | Reported race, n (%) | Report ethnicity, n (%) |
| United States | 17 | 15 (88) | 9 (53) |
| Germany | 12 | 0 (0) | 0 (0) |
| Australia | 10 | 1(10) | 1 (10) |
| Sweden | 10 | 0 (0) | 0 (0) |
| Netherlands | 6 | 0 (0) | 1 (17) |
| China | 2 | 0 (0) | 0 (0) |
| Finland | 2 | 0 (0) | 0 (0) |
| United Kingdom | 2 | 1 (50) | 1 (50) |
| Canada | 1 | 0 (0) | 0 (0) |
| Colombia | 1 | 0 (0) | 0 (0) |
| Ireland | 1 | 0 (0) | 0 (0) |
| New Zealand | 1 | 0 (0) | 0 (0) |
| Switzerland | 1 | 0 (0) | 0 (0) |
Representation of Individuals From Racial and Ethnic Minoritized Groups
Of the 17 papers that reported race, 4 (24%) categorized groups into “minority” versus “non-minority” or “White” versus “other.” The other papers included the following groups on their breakdown: American Indian or Alaskan Native (n=3); Asian (n=8); Black or African American (n=12); Middle Eastern or North African (n=1); multiracial (n=8); Native American (n=1); other (n=8) which included “not specified,” “declined to answer,” and not reported as White; Pacific Islander (n=3); unknown (n=18); and White (n=16) (see Table 2).
Table 2.
Total number of participants by race for trials of internet-based cognitive behavioral therapy for depression that reported race (N=3623).
| Race | Participants, n (%) |
| AIANa | 14 (0.4) |
| Asian | 209 (5.8) |
| Black | 274 (7.6) |
| MENAb | 1 (0) |
| Multiple | 143 (3.9) |
| Native American | 3 (0.1) |
| Not specified | 75 (2.1) |
| Other | 76 (2.1) |
| Pacific Islander | 6 (0.2) |
| Unknown | 106 (2.9) |
| White | 2716 (74.9) |
aAIAN: American Indian or Alaskan Native.
bMENA: Middle Eastern or North African.
The papers that reported ethnicity (Table 3) reported the following ethnic groups: American (n=1), Chinese (n=1), European (n=1), Hispanic or Latino (n=9), other (n=1), Turkish (n=1), and White British (n=1). Many papers specified ethnicity for minoritized member groups (eg, Hispanic) but not for majority members (eg, non-Hispanic).
Table 3.
Total number of participants by ethnicity for trials of internet-based cognitive behavioral therapy for depression that reported ethnicity (N=2496).
| Ethnicity | Participants, n (%) |
| American | 2 (0) |
| Chinese | 148 (5.9) |
| European | 11(0) |
| Hispanic | 281 (11.3) |
| Not specified (eg, reported ethnicity for some but not other individuals) | 1886 (75.6) |
| Other | 9 (0) |
| Turkish | 96 (3.8) |
| White British | 63 (2) |
Representation of Race in iCBT Trials in the United States
Given that reporting of race was highest in the United States, we explored the representation of individuals from racial-ethnic minoritized groups in the 15 RCTs from that country that reported race (n=3354). A total of 2568 out of 3354 (76.6%, 95% CI 75.1-78.0) of individuals in these samples were identified as White. By way of comparison, 61.6% of adults in the United States were reported as being White in the US census [1]. These rates are significantly different (χ21=316.9, P<.001). Extrapolating the number of individuals that would be expected to be White based on the 12-month prevalence of depression reported in the latest epidemiological study (National Epidemiologic Survey on Alcohol and Related Conditions-III: 10.4%) [96] and racial-ethnic differences reported in National Epidemiologic Survey on Alcohol and Related Conditions-III, one would expect 67.3% of individuals in a 12-month depression sample to be non-Hispanic White. The rate of White individuals represented in our study was statistically significantly different from 67.3% (χ21=130.4, P<.001). When using lifetime prevalence rates, one would expect 72.5% of individuals with lifetime depression to be White. The rate of White individuals we found was significantly higher (χ21=27.6, P<.001), though it was a relatively small difference (4.1%).
Reporting of Other Group Demographics Outside of the United States
Out of the 46 articles conducted outside of the United States, only 25 (54%) reported on other demographic factors, such as language proficiency (n=13), country of residence (n=11), country of origin (n=5), migration status (n=2), and nationality (n=2). Most (n=11) of the studies that reported language only did so indirectly, as an inclusion criterion (eg, “participants must speak Dutch fluently”). Similarly, most (n=9) of the studies that reported the country of residence did so indirectly, (eg, “participants must reside in Sweden”). Some studies reported on multiple of the aforementioned demographics, therefore, there are more reported demographic variables (ie, 33) than the number of studies reporting these (ie, 25).
Discussion
Principal Findings
Our first aim was to examine the overall reporting of racial and ethnic diversity in RCTs of iCBT for depression. The second aim was to explore the representation of specific minoritized groups within the studies reporting race-ethnicity. Our search revealed substantial gaps in the literature. Out of the 62, only 17 (27%) of the papers included in this paper had data on race, and 12 (19%) included ethnicity. Focusing on the United States, even when race was reported, White individuals were overrepresented in samples relative to US census population estimates (61.6%) [97] and the expected estimate of non-Hispanic White individuals in depression samples (67.3%) [98].
Limitations
Before interpreting our findings, several caveats are worth noting. First, we recognize that failure to report racial-ethnic identity information does not guarantee that racial-ethnic diversity is not well-represented in a trial's sample. However, we believe that it is unlikely that researchers are collecting very racially diverse samples and choosing not to report on that aspect of the sample composition. In some countries reporting race or ethnicity might be more limited by regulations like ethical review board approval. Nonetheless, only 25 (54%) out of 46 of studies conducted outside of the United States reported other characteristics such as nationality, country of origin, or migration status. Additionally, it is worth noting that it is not always clear what the implications of underreporting are. For example, in a large individual-patient data meta-analysis, Karyotaki et al [99] reported that individuals from racial-ethnic minoritized groups experienced poorer outcomes in guided iCBT than “native-born” participants. These findings are worth replicating as they imply that racial-ethnic groups may respond differently to iCBTs and are concerning regarding the underrepresentation of minoritized groups in iCBT research. Nonetheless, even if race-ethnicity was not a predictor of outcomes in treatment, the differential enrollment of participants from different racial-ethnic groups is itself a racial-ethnic disparity. We excluded gray literature such as posters and other unpublished works. While these exclusions represent a limitation of this study (ie, fewer RCTs included), it is not clear that including these would have changed our conclusions that the reporting of representation is poor in RCTs of self-help iCBT. Finally, we chose to focus on iCBT, given its popularity and potential to reduce the public health burden of depression [100,101]. However, self-help iCBTs are not the only low-intensity treatment available. For example, bibliotherapy (ie, printed self-help media) is also a low-intensity treatment that may be preferred by many individuals, with some evidence suggesting that some racial-ethnic minoritized groups may prefer bibliotherapy over digital interventions [23].
Implications of Underrepresentation and Methodological Considerations
Our results suggest that the rate of reporting of ethnicity in iCBT studies in the United States has improved relative to the prior report by Polo and colleagues [11] for RCTs of face-to-face psychotherapy for depression. However, reporting of background characteristics in iCBT RCTs is relatively poor in Europe and elsewhere. Indeed, only 2 RCTs of iCBT for depression conducted outside of the United States reported race or ethnicity, one of which was a cultural adaptation. This finding is surprising given that an estimated 23 million non-European citizens (5% of the population) live in Europe [102]. This underreporting makes it challenging to determine how well our current interventions fit with the experiences of minoritized groups. While it is a possibility that logistic barriers such as internet access may be responsible for the lower representation of individuals from racial-ethnic minoritized groups in iCBT studies, it is unclear if these differences are large enough to account for the disparities in trial representation [103]. Ramos et al [29] noted that diversity, equity, and inclusion were not guiding principles in iCBT research. Similarly, our findings suggest a need to understand how individuals from racial-ethnic minoritized groups engage in iCBT research and how to increase that engagement.
Another explanation for the lack of reporting and representation could be group differences in the acceptability of iCBT (ie, internet-based self-help not being a preferred format). However, there is evidence that compared to non-Hispanic White adults, Asian, Hispanic, non-Hispanic Black, and other racial-ethnic groups report either equal or greater willingness to use and choose to learn about iCBTs. Thus, overall willingness to use iCBTs is unlikely to explain differences in initiating iCBT trials.
Furthermore, the relevance of race and ethnicity as terms in countries outside the United States warrants additional examination. It is essential to investigate alternative methods of describing samples that are appropriate for different countries while allowing for cross-country comparisons. The low number of iCBT studies focusing on minoritized individuals' mental health makes it challenging to advocate for the using of iCBT to reduce health disparities in these populations, especially outside the United States. Hence, it is essential to conduct research that encompasses diverse populations and reports on their characteristics.
Future Directions
This lack of knowledge regarding race and ethnicity has implications for implementing iCBT programs globally. Providers, for example, worry about the lack of diversity represented in the literature since this could lead to engagement challenges [104]. Acknowledging that a primarily White sample does not represent the general population may be an essential step to improving engagement. Numerous efforts to culturally adapt interventions to increase cultural competence of clinicians have been made [105]. However, we still lack information on how these adaptations translate to a self-help format to reduce barriers to access for minoritized groups. Currently, hundreds of online mental health resources are available to the public, but it is sometimes unclear what they offer users [106]. Clinicians and clients have no easy way of knowing which resources are evidence-based and suitable for individuals from racial-ethnic minoritized groups. The label “CBT” (cognitive behavioral therapy) could be a way to identify evidence-based mental health services. However, it is hard to determine whether digital interventions apply CBT principles correctly and whether this delivery format is ideal for members of racial-ethnic minoritized groups.
The extent to which racial-ethnic minoritized groups, other than US non-Hispanic Black adults, use self-help iCBT has received little attention [11,29]. It has been more than a decade since the National Institutes of Health, CONSORT, and JARS guidelines [12,13,107] introduced criteria regarding race and ethnicity, and the outlook has not improved significantly. Although reporting of race has improved, it is not being reported to the extent that it could be helpful. Further, a potential future direction includes developing new guidelines similar to the CONSORT and JARS [13,107] for journals oriented toward internet-based mental health. These guidelines could involve (1) including racial-ethnic groups with a breakdown; (2) describing the type and intensity of support being provided for guided self-help; (3) ensuring that samples are representative of gender, racial-ethnic groups, and other underreported identities; and (4) detailing which elements of CBT are included in the protocol. This standardization could facilitate the implementation of similar protocols in hospitals, mental health foundations, and businesses interested in providing mental health services to a broader population. The lack of reporting could also be improved by increasing outreach efforts and ensuring racial-ethnic diversity is included in RCTs for self-help iCBT.
Conclusions
There is a lack of reporting of racial and ethnic diversity in clinical trials of iCBT, and the representation of individuals from racial-ethnic minoritized groups is quite poor. This gap has significant implications for the generalizability of the findings currently in the literature, as these might not apply to individuals from racial-ethnic minoritized groups. Therefore, improving the representation of racial-ethnic diversity in trials of iCBT should be a key direction for the field going forward.
Acknowledgments
This research was partially funded by the Global Mental Health Fellowship (principal investigator: LL-L), the National Institute of Mental Health (grant T32 MH103213-06) and (grants KL2TR002530 and UL1TR002529) (A Shekhar, principal investigator) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award (principal investigator: LL-L).
Abbreviations
- CBT
cognitive behavioral therapy
- CONSORT
Consolidated Standards of Reporting Trials
- iCBT
internet-based cognitive behavioral therapy
- JARS
Journal Article Reporting Standards
- PRISMA
Preferred Reporting Items for Systematic Reviews
- RCT
randomized controlled trial
- ROB
Risk of Bias
Search string from MetaPsy.
Search string for articles published from 2021 to 2022.
Risk of bias assessment for articles not included in MetaPsy (n=20).
Footnotes
Conflicts of Interest: LL-L has received consulting fees from Syra Health, Inc who were not involved with the current work.
References
- 1.U.S. Census Buerau 2020 census illuminates racial and ethnic composition of the country. Census.gov. 2020. [2022-06-06]. https://www.census.gov/library/stories/2021/08/improved-race-ethnicity-measures-reveal-united-states-population-much-more-multiracial.html .
- 2.Wingrove-Haugland E, McLeod J. Not "minority" but "minoritized". Teach Ethics. 2021;21(1):1–11. doi: 10.5840/tej20221799. [DOI] [Google Scholar]
- 3.Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. United States Census Bureau. 2015. [2023-12-05]. https://www.census.gov/library/publications/2015/demo/p25-1143.html .
- 4.United Nations International Migration 2019. Department of Economic Affaris. 2019. [2023-12-05]. https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2019_internationalmigration_highlights.pdf .
- 5.Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, Bruffaerts R, de Girolamo G, de Graaf Ron, Gureje O, Haro JM, Karam EG, Kessler RC, Kovess V, Lane MC, Lee S, Levinson D, Ono Y, Petukhova M, Posada-Villa J, Seedat S, Wells JE. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–850. doi: 10.1016/S0140-6736(07)61414-7. https://europepmc.org/abstract/MED/17826169 .S0140-6736(07)61414-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010) J Clin Psychiatry. 2015;76(2):155–162. doi: 10.4088/JCP.14m09298. https://www.psychiatrist.com/jcp/economic-burden-adults-major-depressive-disorder-united/ [DOI] [PubMed] [Google Scholar]
- 7.Pascoe EA, Richman LS. Perceived discrimination and health: a meta-analytic review. Psychological Bulletin. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carter RT, Lau MY, Johnson V, Kirkinis K. Racial discrimination and health outcomes among racial/ethnic minorities: a meta-analytic review. J Multicult Couns Devel. 2017;45(4):232–259. doi: 10.1002/jmcd.12076. [DOI] [Google Scholar]
- 9.Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26(4):392–407. doi: 10.3109/09540261.2014.928270. [DOI] [PubMed] [Google Scholar]
- 10.Mak WWS, Law RW, Alvidrez J, Pérez-Stable EJ. Gender and ethnic diversity in NIMH-funded clinical trials: review of a decade of published research. Adm Policy Ment Health. 2007;34(6):497–503. doi: 10.1007/s10488-007-0133-z. [DOI] [PubMed] [Google Scholar]
- 11.Polo AJ, Makol BA, Castro AS, Colón-Quintana N, Wagstaff AE, Guo S. Diversity in randomized clinical trials of depression: a 36-year review. Clin Psychol Rev. 2019;67:22–35. doi: 10.1016/j.cpr.2018.09.004. https://www.sciencedirect.com/science/article/abs/pii/S0272735818303684?via%3Dihub .S0272-7358(18)30368-4 [DOI] [PubMed] [Google Scholar]
- 12.NIH policy and guidelines on the inclusion of women and minorities as subjects in clinical research. National Institutes of Health. 2001. [2022-06-06]. http://grants1.nih.gov/grants/funding/women_min/guidelines_amended_10_2001.htm .
- 13.Schulz KF, Altman DG, Moher D, CONSORT Group CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2011;9(8):672–677. doi: 10.1016/j.ijsu.2011.09.004. https://www.sciencedirect.com/science/article/pii/S1743919111005620?via%3Dihub .S1743-9191(11)00562-0 [DOI] [PubMed] [Google Scholar]
- 14.King DB, O'Rourke N, DeLongis A. Social media recruitment and online data collection: a beginner's guide and best practices for accessing low-prevalence and hard-to-reach populations. Can Psychol. 2014;55(4):240–249. doi: 10.1037/a0038087. [DOI] [Google Scholar]
- 15.Budhwani H, Hearld KR, Chavez-Yenter D. Depression in racial and ethnic minorities: the impact of nativity and discrimination. J Racial Ethn Health Disparities. 2015;2(1):34–42. doi: 10.1007/s40615-014-0045-z. https://link.springer.com/article/10.1007/s40615-014-0045-z .10.1007/s40615-014-0045-z [DOI] [PubMed] [Google Scholar]
- 16.Woodward AT, Taylor RJ, Abelson JM, Matusko N. Major depressive disorder among older African Americans, Caribbean Blacks, and non-Hispanic Whites: secondary analysis of the National Survey of American Life. Depress Anxiety. 2013;30(6):589–597. doi: 10.1002/da.22041. http://hdl.handle.net/2027.42/98298 . [DOI] [PubMed] [Google Scholar]
- 17.McBrier DB, Wilson G. Going down? Race and downward occupational mobility for white-collar workers in the 1990s. Work Occup. 2004;31(3):283–322. doi: 10.1177/0730888404266383. [DOI] [Google Scholar]
- 18.Hardaway CR, McLoyd VC. Escaping poverty and securing middle class status: how race and socioeconomic status shape mobility prospects for African Americans during the transition to adulthood. J Youth Adolesc. 2009;38(2):242–256. doi: 10.1007/s10964-008-9354-z. https://europepmc.org/abstract/MED/19636721 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality. Rockville, MD: 2021. [2023-12-05]. 2021 National Healthcare Quality and Disparities Report. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr21/index.html . [PubMed] [Google Scholar]
- 20.Holden KB, McGregor BS, Blanks SH, Mahaffey C. Psychosocial, socio-cultural, and environmental influences on mental health help-seeking among African-American men. J Mens Health. 2012;9(2):63–69. doi: 10.1016/j.jomh.2012.03.002. https://europepmc.org/abstract/MED/22905076 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramos G, Chavira DA. Use of technology to provide mental health care for racial and ethnic minorities: evidence, promise, and challenges. Cogn Behav Pract. 2022;29(1):15–40. doi: 10.1016/j.cbpra.2019.10.004. [DOI] [Google Scholar]
- 22.Schueller SM, Hunter JF, Figueroa C, Aguilera A. Use of digital mental health for marginalized and underserved populations. Curr Treat Options Psych. 2019;6(3):243–255. doi: 10.1007/s40501-019-00181-z. [DOI] [Google Scholar]
- 23.De Jesús-Romero R, Wasil A, Lorenzo-Luaces L. Willingness to use internet-based versus bibliotherapy interventions in a representative US sample: cross-sectional survey study. JMIR Form Res. 2022;6(8):e39508. doi: 10.2196/39508. https://formative.jmir.org/2022/8/e39508 .v6i8e39508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levecque K, Van Rossem R. Depression in Europe: does migrant integration have mental health payoffs? A cross-national comparison of 20 European countries. Ethn Health. 2015;20(1):49–65. doi: 10.1080/13557858.2014.883369. [DOI] [PubMed] [Google Scholar]
- 25.Henkelmann JR, de Best S, Deckers C, Jensen K, Shahab M, Elzinga B, Molendijk M. Anxiety, depression and post-traumatic stress disorder in refugees resettling in high-income countries: systematic review and meta-analysis. BJPsych Open. 2020;6(4):e68. doi: 10.1192/bjo.2020.54. https://www.cambridge.org/core/journals/bjpsych-open/article/anxiety-depression-and-posttraumatic-stress-disorder-in-refugees-resettling-in-highincome-countries-systematic-review-and-metaanalysis/8AC75A92D4164C16A8755B333E8D4DB8 .S205647242000054X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mohr DC, Cuijpers P, Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Internet Res. 2011;13(1):e30. doi: 10.2196/jmir.1602. https://www.jmir.org/2011/1/e30/ v13i1e30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cuijpers P, Noma H, Karyotaki E, Cipriani A, Furukawa TA. Effectiveness and acceptability of cognitive behavior therapy delivery formats in adults with depression: a network meta-analysis. JAMA Psychiatry. 2019;76(7):700–707. doi: 10.1001/jamapsychiatry.2019.0268. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2730724 .2730724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohr DC, Duffecy J, Ho J, Kwasny M, Cai X, Burns MN, Begale M. A randomized controlled trial evaluating a manualized TeleCoaching protocol for improving adherence to a web-based intervention for the treatment of depression. PLoS One. 2013;8(8):e70086. doi: 10.1371/journal.pone.0070086. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0070086 .PONE-D-13-05935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramos G, Ponting C, Labao JP, Sobowale K. Considerations of diversity, equity, and inclusion in mental health apps: a scoping review of evaluation frameworks. Behav Res Ther. 2021;147:103990. doi: 10.1016/j.brat.2021.103990. https://www.sciencedirect.com/science/article/pii/S0005796721001893?via%3Dihub .S0005-7967(21)00189-3 [DOI] [PubMed] [Google Scholar]
- 30.Andersson G, Bergström J, Holländare F, Carlbring P, Kaldo V, Ekselius L. Internet-based self-help for depression: randomised controlled trial. Br J Psychiatry. 2005;187:456–61. doi: 10.1192/bjp.187.5.456.S0007125000168400 [DOI] [PubMed] [Google Scholar]
- 31.Ly KH, Trüschel A, Jarl L, Magnusson Susanna, Windahl Tove, Johansson Robert, Carlbring Per, Andersson Gerhard. Behavioural activation versus mindfulness-based guided self-help treatment administered through a smartphone application: a randomised controlled trial. BMJ Open. 2014;4(1):e003440. doi: 10.1136/bmjopen-2013-003440. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=24413342 .bmjopen-2013-003440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lindner P, Olsson E, Johnsson A, Dahlin M, Andersson G, Carlbring P. The impact of telephone versus e-mail therapist guidance on treatment outcomes, therapeutic alliance and treatment engagement in internet-delivered CBT for depression: a randomised pilot trial. Internet Interventions. 2014;1(4):182–187. doi: 10.1016/j.invent.2014.09.001. [DOI] [Google Scholar]
- 33.Lappalainen P, Langrial S, Oinas-Kukkonen H, Tolvanen Asko, Lappalainen Raimo. Web-based acceptance and commitment therapy for depressive symptoms with minimal support: a randomized controlled trial. Behav Modif. 2015;39(6):805–34. doi: 10.1177/0145445515598142.0145445515598142 [DOI] [PubMed] [Google Scholar]
- 34.Berger T, Hämmerli K, Gubser N, Andersson G, Caspar F. Internet-based treatment of depression: a randomized controlled trial comparing guided with unguided self-help. Cogn Behav Ther. 2011;40(4):251–66. doi: 10.1080/16506073.2011.616531. [DOI] [PubMed] [Google Scholar]
- 35.Löbner M, Pabst A, Stein J, Dorow Marie, Matschinger Herbert, Luppa Melanie, Maroß Astrid, Kersting Anette, König Hans-Helmut, Riedel-Heller Steffi G. Computerized cognitive behavior therapy for patients with mild to moderately severe depression in primary care: A pragmatic cluster randomized controlled trial (@ktiv) J Affect Disord. 2018;238:317–326. doi: 10.1016/j.jad.2018.06.008.S0165-0327(18)30515-9 [DOI] [PubMed] [Google Scholar]
- 36.Meyer B, Bierbrodt J, Schröder J, Berger T, Beevers Cg, Weiss M, Jacob G, Späth C, Andersson G, Lutz W, Hautzinger M, Löwe B, Rose M, Hohagen F, Caspar F, Greiner W, Moritz S, Klein Jp. Effects of an Internet intervention (Deprexis) on severe depression symptoms: randomized controlled trial. Internet Interventions. 2015;2(1):48–59. doi: 10.1016/j.invent.2014.12.003. [DOI] [Google Scholar]
- 37.Moritz S, Schilling L, Hauschildt M, Schröder Johanna, Treszl András. A randomized controlled trial of internet-based therapy in depression. Behav Res Ther. 2012;50(7-8):513–21. doi: 10.1016/j.brat.2012.04.006.S0005-7967(12)00075-7 [DOI] [PubMed] [Google Scholar]
- 38.Nyström MBT, Stenling A, Sjöström E, Neely Gregory, Lindner Philip, Hassmén Peter, Andersson Gerhard, Martell Christopher, Carlbring Per. Behavioral activation versus physical activity via the internet: a randomized controlled trial. J Affect Disord. 2017;215:85–93. doi: 10.1016/j.jad.2017.03.018. https://linkinghub.elsevier.com/retrieve/pii/S0165-0327(16)32224-8 .S0165-0327(16)32224-8 [DOI] [PubMed] [Google Scholar]
- 39.Oehler C, Görges F, Rogalla M, Rummel-Kluge Christine, Hegerl Ulrich. Efficacy of a guided web-based self-management intervention for depression or dysthymia: randomized controlled trial with a 12-month follow-up using an active control condition. J Med Internet Res. 2020;22(7):e15361. doi: 10.2196/15361. https://www.jmir.org/2020/7/e15361/ v22i7e15361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stiles-Shields C, Montague E, Kwasny MJ, Mohr David C. Behavioral and cognitive intervention strategies delivered via coached apps for depression: pilot trial. Psychol Serv. 2019;16(2):233–238. doi: 10.1037/ser0000261. https://europepmc.org/abstract/MED/30407055 .2018-56150-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.O'moore KA, Newby JM, Andrews G, Hunter David J, Bennell Kim, Smith Jessica, Williams Alishia D. Internet cognitive-behavioral therapy for depression in older adults with knee osteoarthritis: a randomized controlled trial. Arthritis Care Res (Hoboken) 2018;70(1):61–70. doi: 10.1002/acr.23257. [DOI] [PubMed] [Google Scholar]
- 42.Salamanca-Sanabria A, Richards D, Timulak L, Connell Sarah, Mojica Perilla Monica, Parra-Villa Yamilena, Castro-Camacho Leonidas. A culturally adapted cognitive behavioral internet-delivered intervention for depressive symptoms: randomized controlled trial. JMIR Ment Health. 2020;7(1):e13392. doi: 10.2196/13392. https://mental.jmir.org/2020/1/e13392/ v7i1e13392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Titov N, Dear BF, Staples LG, Terides M D, Karin E, Sheehan J, Johnston L, Gandy M, Fogliati V J, Wootton B M, McEvoy P M. Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: a randomized controlled trial. J Anxiety Disord. 2015;35:88–102. doi: 10.1016/j.janxdis.2015.08.002. https://linkinghub.elsevier.com/retrieve/pii/S0887-6185(15)30008-6 .S0887-6185(15)30008-6 [DOI] [PubMed] [Google Scholar]
- 44.Ruwaard J, Schrieken B, Schrijver M, Broeksteeg Janneke, Dekker Jack, Vermeulen Hans, Lange Alfred. Standardized web-based cognitive behavioural therapy of mild to moderate depression: a randomized controlled trial with a long-term follow-up. Cogn Behav Ther. 2009;38(4):206–21. doi: 10.1080/16506070802408086.908748225 [DOI] [PubMed] [Google Scholar]
- 45.Smith J, Newby JM, Burston N, Murphy Michael J, Michael Sarah, Mackenzie Anna, Kiln Felicity, Loughnan Siobhan A, O'Moore Kathleen A, Allard Benjamin J, Williams Alishia D, Andrews Gavin. Help from home for depression: a randomised controlled trial comparing internet-delivered cognitive behaviour therapy with bibliotherapy for depression. Internet Interv. 2017;9:25–37. doi: 10.1016/j.invent.2017.05.001. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(17)30022-2 .S2214-7829(17)30022-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schröder J, Brückner K, Fischer A, Lindenau Matthias, Köther Ulf, Vettorazzi Eik, Moritz Steffen. Efficacy of a psychological online intervention for depression in people with epilepsy: a randomized controlled trial. Epilepsia. 2014;55(12):2069–76. doi: 10.1111/epi.12833. https://onlinelibrary.wiley.com/doi/10.1111/epi.12833 . [DOI] [PubMed] [Google Scholar]
- 47.Richards D, Timulak L, O'Brien E, Hayes C, Vigano N, Sharry J, Doherty G. A randomized controlled trial of an internet-delivered treatment: its potential as a low-intensity community intervention for adults with symptoms of depression. Behav Res Ther. 2015;75:20–31. doi: 10.1016/j.brat.2015.10.005.S0005-7967(15)30045-0 [DOI] [PubMed] [Google Scholar]
- 48.Vernmark K, Lenndin J, Bjärehed J, Carlsson Mattias, Karlsson Johan, Oberg Jörgen, Carlbring Per, Eriksson Thomas, Andersson Gerhard. Internet administered guided self-help versus individualized e-mail therapy: a randomized trial of two versions of CBT for major depression. Behav Res Ther. 2010;48(5):368–76. doi: 10.1016/j.brat.2010.01.005.S0005-7967(10)00006-9 [DOI] [PubMed] [Google Scholar]
- 49.Schure MB, Lindow JC, Greist JH, Nakonezny Paul A, Bailey Sandra J, Bryan William L, Byerly Matthew J. Use of a fully automated internet-based cognitive behavior therapy intervention in a community population of adults with depression symptoms: randomized controlled trial. J Med Internet Res. 2019;21(11):e14754. doi: 10.2196/14754. https://www.jmir.org/2019/11/e14754/ v21i11e14754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Titov N, Andrews G, Davies M, McIntyre Karen, Robinson Emma, Solley Karen. Internet treatment for depression: a randomized controlled trial comparing clinician vs. technician assistance. PLoS One. 2010;5(6):e10939. doi: 10.1371/journal.pone.0010939. https://dx.plos.org/10.1371/journal.pone.0010939 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ünlü Ince B, Cuijpers P, van 't Hof E, van Ballegooijen Wouter, Christensen Helen, Riper Heleen. Internet-based, culturally sensitive, problem-solving therapy for Turkish migrants with depression: randomized controlled trial. J Med Internet Res. 2013;15(10):e227. doi: 10.2196/jmir.2853. https://www.jmir.org/2013/10/e227/ v15i10e227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Williams AD, Blackwell SE, Mackenzie A, Holmes Emily A, Andrews Gavin. Combining imagination and reason in the treatment of depression: a randomized controlled trial of internet-based cognitive-bias modification and internet-CBT for depression. J Consult Clin Psychol. 2013;81(5):793–9. doi: 10.1037/a0033247. https://europepmc.org/abstract/MED/23750459 .2013-20188-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Warmerdam L, van Straten A, Twisk J, Riper Heleen, Cuijpers Pim. Internet-based treatment for adults with depressive symptoms: randomized controlled trial. J Med Internet Res. 2008;10(4):e44. doi: 10.2196/jmir.1094. https://www.jmir.org/2008/4/e44/ v10i4e44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhao C, Wampold BE, Ren Z, Zhang Lin, Jiang Guangrong. The efficacy and optimal matching of an internet-based acceptance and commitment therapy intervention for depressive symptoms among university students: a randomized controlled trial in China. J Clin Psychol. 2022;78(7):1354–1375. doi: 10.1002/jclp.23329. [DOI] [PubMed] [Google Scholar]
- 55.Pots WTM, Fledderus M, Meulenbeek PAM, ten Klooster Peter M, Schreurs Karlein M G, Bohlmeijer Ernst T. Acceptance and commitment therapy as a web-based intervention for depressive symptoms: randomised controlled trial. Br J Psychiatry. 2016;208(1):69–77. doi: 10.1192/bjp.bp.114.146068.S0007125000240385 [DOI] [PubMed] [Google Scholar]
- 56.Pihlaja S, Lahti J, Lipsanen JO, Ritola Ville, Gummerus Eero-Matti, Stenberg Jan-Henry, Joffe Grigori. Scheduled telephone support for internet cognitive behavioral therapy for depression in patients at risk for dropout: pragmatic randomized controlled trial. J Med Internet Res. 2020;22(7):e15732. doi: 10.2196/15732. https://www.jmir.org/2020/7/e15732/ v22i7e15732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zagorscak P, Heinrich M, Sommer D, Wagner Birgit, Knaevelsrud Christine. Benefits of individualized feedback in internet-based interventions for depression: a randomized controlled trial. Psychother Psychosom. 2018;87(1):32–45. doi: 10.1159/000481515.000481515 [DOI] [PubMed] [Google Scholar]
- 58.Reins JA, Boß L, Lehr D, Berking Matthias, Ebert David Daniel. The more I got, the less I need? efficacy of internet-based guided self-help compared to online psychoeducation for major depressive disorder. J Affect Disord. 2019;246:695–705. doi: 10.1016/j.jad.2018.12.065.S0165-0327(18)31112-1 [DOI] [PubMed] [Google Scholar]
- 59.Bücker L, Schnakenberg P, Karyotaki E, Moritz Steffen, Westermann Stefan. Diminishing effects after recurrent use of self-guided internet-based interventions in depression: randomized controlled trial. J Med Internet Res. 2019;21(10):e14240. doi: 10.2196/14240. https://www.jmir.org/2019/10/e14240/ v21i10e14240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Roepke AM, Jaffee SR, Riffle OM, McGonigal Jane, Broome Rose, Maxwell Bez. Randomized controlled trial of SuperBetter, a smartphone-based/internet-based self-help tool to reduce depressive symptoms. Games Health J. 2015;4(3):235–46. doi: 10.1089/g4h.2014.0046. [DOI] [PubMed] [Google Scholar]
- 61.Carlbring P, Hägglund M, Luthström A, Dahlin Mats, Kadowaki Åsa, Vernmark Kristofer, Andersson Gerhard. Internet-based behavioral activation and acceptance-based treatment for depression: a randomized controlled trial. J Affect Disord. 2013;148(2-3):331–7. doi: 10.1016/j.jad.2012.12.020.S0165-0327(12)00853-1 [DOI] [PubMed] [Google Scholar]
- 62.Bur OT, Krieger T, Moritz S, Klein Jan Philipp, Berger Thomas. Optimizing the context of support of web-based self-help in individuals with mild to moderate depressive symptoms: a randomized full factorial trial. Behav Res Ther. 2022;152:104070. doi: 10.1016/j.brat.2022.104070. https://boris.unibe.ch/id/eprint/167861 .S0005-7967(22)00041-9 [DOI] [PubMed] [Google Scholar]
- 63.Choi I, Zou J, Titov N, Dear Blake F, Li Stephen, Johnston Luke, Andrews Gavin, Hunt Caroline. Culturally attuned internet treatment for depression amongst Chinese Australians: a randomised controlled trial. J Affect Disord. 2012;136(3):459–68. doi: 10.1016/j.jad.2011.11.003.S0165-0327(11)00716-6 [DOI] [PubMed] [Google Scholar]
- 64.Perini S, Titov N, Andrews G. Clinician-assisted internet-based treatment is effective for depression: randomized controlled trial. Aust N Z J Psychiatry. 2009;43(6):571–8. doi: 10.1080/00048670902873722.911151658 [DOI] [PubMed] [Google Scholar]
- 65.Jelinek L, Arlt S, Moritz S, Schröder Johanna, Westermann Stefan, Cludius Barbara. Brief web-based intervention for depression: randomized controlled trial on behavioral activation. J Med Internet Res. 2020;22(3):e15312. doi: 10.2196/15312. https://www.jmir.org/2020/3/e15312/ v22i3e15312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Johansson O, Bjärehed J, Andersson G, Carlbring Per, Lundh Lars-Gunnar. Effectiveness of guided internet-delivered cognitive behavior therapy for depression in routine psychiatry: a randomized controlled trial. Internet Interv. 2019;17:100247. doi: 10.1016/j.invent.2019.100247. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(19)30010-7 .S2214-7829(19)30010-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Flygare A-L, Engström I, Hasselgren M, Jansson-Fröjmark Markus, Frejgrim Rikard, Andersson Gerhard, Holländare Fredrik. Internet-based CBT for patients with depressive disorders in primary and psychiatric care: is it effective and does comorbidity affect outcome? Internet Interv. 2020;19:100303. doi: 10.1016/j.invent.2019.100303. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(19)30093-4 .S2214-7829(19)30093-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kenter RMF, Cuijpers P, Beekman A, van Straten Annemieke. Effectiveness of a web-based guided self-help intervention for outpatients with a depressive disorder: short-term results from a randomized controlled trial. J Med Internet Res. 2016;18(3):e80. doi: 10.2196/jmir.4861. https://www.jmir.org/2016/3/e80/ v18i3e80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Krämer R, Köhler S. Evaluation of the online-based self-help programme "Selfapy" in patients with unipolar depression: study protocol for a randomized, blinded parallel group dismantling study. Trials. 2021;22(1):264. doi: 10.1186/s13063-021-05218-4. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05218-4 .10.1186/s13063-021-05218-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kivi M, Eriksson MCM, Hange D, Petersson Eva-Lisa, Vernmark Kristofer, Johansson Boo, Björkelund Cecilia. Internet-based therapy for mild to moderate depression in Swedish primary care: short term results from the PRIM-NET randomized controlled trial. Cogn Behav Ther. 2014;43(4):289–98. doi: 10.1080/16506073.2014.921834. https://europepmc.org/abstract/MED/24911260 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fischer A, Schröder J, Vettorazzi E, Wolf Oliver T, Pöttgen Jana, Lau Stephanie, Heesen Christoph, Moritz Steffen, Gold Stefan M. An online programme to reduce depression in patients with multiple sclerosis: a randomised controlled trial. Lancet Psychiatry. 2015;2(3):217–23. doi: 10.1016/S2215-0366(14)00049-2.S2215-0366(14)00049-2 [DOI] [PubMed] [Google Scholar]
- 72.Tomasino KN, Lattie EG, Ho J, Palac Hannah L, Kaiser Susan M, Mohr David C. Harnessing peer support in an online intervention for older adults with depression. Am J Geriatr Psychiatry. 2017;25(10):1109–1119. doi: 10.1016/j.jagp.2017.04.015. https://europepmc.org/abstract/MED/28571785 .S1064-7481(17)30308-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rosso IM, Killgore WDS, Olson EA, Webb Christian A, Fukunaga Rena, Auerbach Randy P, Gogel Hannah, Buchholz Jennifer L, Rauch Scott L. Internet-based cognitive behavior therapy for major depressive disorder: a randomized controlled trial. Depress Anxiety. 2017;34(3):236–245. doi: 10.1002/da.22590. https://europepmc.org/abstract/MED/28009467 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Guo Y, Hong YA, Cai W, Li Linghua, Hao Yuantao, Qiao Jiaying, Xu Zhimeng, Zhang Hanxi, Zeng Chengbo, Liu Cong, Li Yiran, Zhu Mengting, Zeng Yu, Penedo Frank J. Effect of a WeChat-based intervention (Run4Love) on depressive symptoms among people living with HIV in China: a randomized controlled trial. J Med Internet Res. 2020;22(2):e16715. doi: 10.2196/16715. https://www.jmir.org/2020/2/e16715/ v22i2e16715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hallgren M, Kraepelien M, Öjehagen A, Lindefors Nils, Zeebari Zangin, Kaldo Viktor, Forsell Yvonne. Physical exercise and internet-based cognitive-behavioural therapy in the treatment of depression: randomised controlled trial. Br J Psychiatry. 2015;207(3):227–34. doi: 10.1192/bjp.bp.114.160101.S0007125000239111 [DOI] [PubMed] [Google Scholar]
- 76.Christensen H, Griffiths KM, Mackinnon AJ, Brittliffe Kylie. Online randomized controlled trial of brief and full cognitive behaviour therapy for depression. Psychol Med. 2006;36(12):1737–46. doi: 10.1017/S0033291706008695.S0033291706008695 [DOI] [PubMed] [Google Scholar]
- 77.Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. BMJ. 2004;328(7434):265. doi: 10.1136/bmj.37945.566632.EE. https://europepmc.org/abstract/MED/14742346 .bmj.37945.566632.EE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Donker T, Bennett K, Bennett A, Mackinnon Andrew, van Straten Annemieke, Cuijpers Pim, Christensen Helen, Griffiths Kathleen M. Internet-delivered interpersonal psychotherapy versus internet-delivered cognitive behavioral therapy for adults with depressive symptoms: randomized controlled noninferiority trial. J Med Internet Res. 2013;15(5):e82. doi: 10.2196/jmir.2307. https://www.jmir.org/2013/5/e82/ v15i5e82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kingston J, Becker L, Woeginger J, Ellett L. A randomised trial comparing a brief online delivery of mindfulness-plus-values versus values only for symptoms of depression: does baseline severity matter? J Affect Disord. 2020;276:936–944. doi: 10.1016/j.jad.2020.07.087.S0165-0327(20)32532-5 [DOI] [PubMed] [Google Scholar]
- 80.Forand NR, Barnett JG, Strunk DR, Hindiyeh Mohammed U, Feinberg Jason E, Keefe John R. Efficacy of guided iCBT for depression and mediation of change by cognitive skill acquisition. Behav Ther. 2018;49(2):295–307. doi: 10.1016/j.beth.2017.04.004. https://europepmc.org/abstract/MED/29530267 .S0005-7894(17)30055-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hobfoll SE, Blais RK, Stevens NR, Walt Lisa, Gengler Richard. Vets prevail online intervention reduces PTSD and depression in veterans with mild-to-moderate symptoms. J Consult Clin Psychol. 2016;84(1):31–42. doi: 10.1037/ccp0000041.2015-39661-001 [DOI] [PubMed] [Google Scholar]
- 82.Dahne J, Collado A, Lejuez CW, Risco Cristina M, Diaz Vanessa A, Coles Lisa, Kustanowitz Jacob, Zvolensky Michael J, Carpenter Matthew J. Pilot randomized controlled trial of a Spanish-language behavioral activation mobile app (¡Aptívate!) for the treatment of depressive symptoms among United States Latinx adults with limited English proficiency. J Affect Disord. 2019;250:210–217. doi: 10.1016/j.jad.2019.03.009. https://europepmc.org/abstract/MED/30870770 .S0165-0327(18)33073-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Clarke G, Reid E, Eubanks D, O'Connor Elizabeth, DeBar Lynn L, Kelleher Chris, Lynch Frances, Nunley Sonia. Overcoming Depression on the Internet (ODIN): a randomized controlled trial of an internet depression skills intervention program. J Med Internet Res. 2002;4(3):E14. doi: 10.2196/jmir.4.3.e14. https://www.jmir.org/2002/3/e14/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Arean PA, Hallgren KA, Jordan JT, Gazzaley Adam, Atkins David C, Heagerty Patrick J, Anguera Joaquin A. The use and effectiveness of mobile apps for depression: results from a fully remote clinical trial. J Med Internet Res. 2016;18(12):e330. doi: 10.2196/jmir.6482. https://www.jmir.org/2016/12/e330/ v18i12e330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Birney AJ, Gunn R, Russell JK, Ary Dennis V. MoodHacker mobile web app with email for adults to self-manage mild-to-moderate depression: randomized controlled trial. JMIR mHealth uHealth. 2016;4(1):e8. doi: 10.2196/mhealth.4231. https://mhealth.jmir.org/2016/1/e8/ v4i1e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Clarke G, Eubanks D, Reid E, Kelleher Chris, O'Connor Elizabeth, DeBar Lynn L, Lynch Frances, Nunley Sonia, Gullion Christina. Overcoming Depression on the Internet (ODIN) (2): a randomized trial of a self-help depression skills program with reminders. J Med Internet Res. 2005;7(2):e16. doi: 10.2196/jmir.7.2.e16. https://www.jmir.org/2005/2/e16/ v7i2e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Beevers CG, Pearson R, Hoffman JS, Foulser A Alban, Shumake Jason, Meyer Björn. Effectiveness of an internet intervention (Deprexis) for depression in a United States adult sample: a parallel-group pragmatic randomized controlled trial. J Consult Clin Psychol. 2017;85(4):367–380. doi: 10.1037/ccp0000171.2017-08289-001 [DOI] [PubMed] [Google Scholar]
- 88.Dahne J, Lejuez CW, Diaz VA, Player Marty S, Kustanowitz Jacob, Felton Julia W, Carpenter Matthew J. Pilot randomized trial of a self-help behavioral activation mobile app for utilization in primary care. Behav Ther. 2019;50(4):817–827. doi: 10.1016/j.beth.2018.12.003. https://europepmc.org/abstract/MED/31208690 .S0005-7894(18)30157-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Clarke G, Kelleher C, Hornbrook M, Debar Lynn, Dickerson John, Gullion Christina. Randomized effectiveness trial of an internet, pure self-help, cognitive behavioral intervention for depressive symptoms in young adults. Cogn Behav Ther. 2009;38(4):222–34. doi: 10.1080/16506070802675353. https://europepmc.org/abstract/MED/19440896 .911169469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.de Graaf LE, Gerhards SAH, Arntz A, Riper H, Metsemakers J F M, Evers S M A A, Severens J L, Widdershoven G, Huibers M J H. Clinical effectiveness of online computerised cognitive-behavioural therapy without support for depression in primary care: randomised trial. Br J Psychiatry. 2009;195(1):73–80. doi: 10.1192/bjp.bp.108.054429. https://core.ac.uk/reader/15457383?utm_source=linkout .S0007125000007406 [DOI] [PubMed] [Google Scholar]
- 91.Cuijpers P. Four decades of outcome research on psychotherapies for adult depression: an overview of a series of meta-analyses. Can Psychol. 2017;58(1):7–19. doi: 10.1037/cap0000096. [DOI] [Google Scholar]
- 92.Cuijpers P, Karyotaki E, Ebert D, Harrer M. METAPSY Database. 2021. [2022-06-06]. https://www.metapsy.org/database/depression-psychotherapy .
- 93.Lorenzo-Luaces L, Zimmerman M, Cuijpers P. Are studies of psychotherapies for depression more or less generalizable than studies of antidepressants? J Affect Disord. 2018;234:8–13. doi: 10.1016/j.jad.2018.02.066. https://www.sciencedirect.com/science/article/abs/pii/S016503271732356X?via%3Dihub .S0165-0327(17)32356-X [DOI] [PubMed] [Google Scholar]
- 94.Lorenzo-Luaces L, Johns E, Keefe JR. The generalizability of randomized controlled trials of self-guided internet-based cognitive behavioral therapy for depressive symptoms: systematic review and meta-regression analysis. J Med Internet Res. 2018;20(11):e10113. doi: 10.2196/10113. https://www.jmir.org/2018/11/e10113/ v20i11e10113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lopez-Quintero C, de los Cobos JP, Hasin DS, Okuda M, Wang S, Grant BF, Blanco C. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug Alcohol Depend. 2011;115(1-2):120–130. doi: 10.1016/j.drugalcdep.2010.11.004. https://www.sciencedirect.com/science/article/abs/pii/S0376871610003753?via%3Dihub .S0376-8716(10)00375-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Smith SM, Goldstein RB, Grant BF. The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) J Psychiatr Res. 2016;82:16–22. doi: 10.1016/j.jpsychires.2016.06.022. https://europepmc.org/abstract/MED/27455424 .S0022-3956(16)30131-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Race and ethnicity in the United States: 2010 census and 2020 census. US Census Bureau. 2021. [2023-12-05]. https://www.census.gov/library/visualizations/interactive/race-and-ethnicity-in-the-united-state-2010-and-2020-census.html .
- 98.Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, Grant BF. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. doi: 10.1001/jamapsychiatry.2017.4602. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2671413 .2671413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Karyotaki E, Ebert DD, Donkin L, Riper H, Twisk J, Burger S, Rozental A, Lange A, Williams AD, Zarski AC, Geraedts A, van Straten A, Kleiboer A, Meyer B, Ince BBÜ, Buntrock C, Lehr D, Snoek FJ, Andrews G, Andersson G, Choi I, Ruwaard J, Klein JP, Newby JM, Schröder J, Laferton JAC, Van Bastelaar K, Imamura K, Vernmark K, Boß Leif, Sheeber LB, Kivi M, Berking M, Titov N, Carlbring P, Johansson R, Kenter R, Perini S, Moritz S, Nobis S, Berger T, Kaldo V, Forsell Y, Lindefors N, Kraepelien M, Björkelund C, Kawakami N, Cuijpers P. Do guided internet-based interventions result in clinically relevant changes for patients with depression? An individual participant data meta-analysis. Clin Psychol Rev. 2018;63:80–92. doi: 10.1016/j.cpr.2018.06.007. https://www.sciencedirect.com/science/article/abs/pii/S0272735818300199?via%3Dihub .S0272-7358(18)30019-9 [DOI] [PubMed] [Google Scholar]
- 100.Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clin Psychol Sci. 2013;1(2):170–191. doi: 10.1177/2167702612463566. [DOI] [Google Scholar]
- 101.Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect Psychol Sci. 2011;6(1):21–37. doi: 10.1177/1745691610393527.6/1/21 [DOI] [PubMed] [Google Scholar]
- 102.Migration and migrant population statistics. Eurostat. 2022. [2023-12-05]. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Migration_and_migrant_population_statistics .
- 103.Internet/broadband fact sheet. Pew Research Center. 2021. [2023-12-05]. https://www.pewresearch.org/internet/fact-sheet/internet-broadband/
- 104.Southam-Gerow MA, Rodríguez A, Chorpita BF, Daleiden EL. Dissemination and implementation of evidence based treatments for youth: challenges and recommendations. Prof Psychol Res Pr. 2012;43(5):527–534. doi: 10.1037/a0029101. [DOI] [Google Scholar]
- 105.Huey SJ, Tilley JL, Jones EO, Smith CA. The contribution of cultural competence to evidence-based care for ethnically diverse populations. Annu Rev Clin Psychol. 2014;10:305–338. doi: 10.1146/annurev-clinpsy-032813-153729. https://www.annualreviews.org/doi/10.1146/annurev-clinpsy-032813-153729 . [DOI] [PubMed] [Google Scholar]
- 106.Jennings K. Venture funding for mental health startups hits record high as anxiety, depression skyrocket. Forbes Magazine. 2021. [2022-06-06]. https://www.forbes.com/sites/katiejennings/2021/06/07/venture-funding-for-mental-health-startups-hits-record-high-as-anxiety-depression-skyrocket/?sh=76021c8c1116 .
- 107.APA Publications and Communications Board Working Group on Journal Article Reporting Standards Reporting standards for research in psychology: why do we need them? what might they be? Am Psychol. 2008;63(9):839–851. doi: 10.1037/0003-066X.63.9.839. https://europepmc.org/abstract/MED/19086746 .2008-17400-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search string from MetaPsy.
Search string for articles published from 2021 to 2022.
Risk of bias assessment for articles not included in MetaPsy (n=20).


