Abstract
Background
The prevalence and burden of substance and opium use have increased worldwide over the past decades. In light of rapid population changes in Tehran, we aimed to evaluate the prevalence of opium and other substance use among adult residents in Tehran, Iran.
Method
From March 2016 to March 2019, we utilized data from 8 296 participants in the Tehran Cohort Study recruitment phase (TeCS). We calculated the age-sex-weighted prevalence of substance use and the geographic distribution of substance use in Tehran. We also used logistic regression analysis to determine possible determinants of opium use.
Result
We analyzed data from 8 259 eligible participants with complete substance use data and the average age of participants was 53.7 ± 12.75 years. The prevalence of substance use was 5.6% (95% confidence interval [CI]: 4.6- 7.1%). Substance use was more common in males than females (Prevalence: 10.5% [95% CI: 8.6- 12.6%] vs. 0.5% [95% CI: 0.2- 1.2%], respectively). The age-sex weighted prevalence of substance use was 5.4% (95% CI: 4.6-7.1%). Moreover, opium was the most frequently used substance by 95.8% of substance users. Additionally, we found that male gender (Odds ratio [OR]: 12.1, P < 0.001), alcohol intake (OR: 1.3, P = 0.016), and smoking (OR: 8.5, P < 0.001) were independently associated with opium use.
Conclusions
We found that the prevalence of substance use in Tehran was 5.6%, and opium was the most frequently used substance. In addition, male gender, lower levels of education, alcohol, and tobacco consumption are the main risk factors for substance use in Tehran. Healthcare providers and policymakers can utilize our results to implement preventive strategies to minimize substance use in Tehran.
Keywords: Substance use, Opium, Prevalence, Addiction, Iran, Tehran
Introduction
Substance use is a significant cause of disability and premature mortality globally [1–3]. It puts a huge burden on societies and governments significantly, including high economic costs, healthcare expenditures, lost productivity, increased violence, and poor treatment compliance [4]. The World Health Organization (WHO) estimates that in 2021, approximately 296 million people aged 15–64 engaged in substance use, reflecting a 26% increase over the preceding decade [5]. Cannabis constituted the predominant choice, with 219 million users, followed by opioids (60 million users) and methamphetamine (32 million users) worldwide [5]. However, the prevalence of substance use and the associated disease burden differed significantly across countries and varied among geographical regions [6]. According to the Global Burden of Disease report, the most substantial contributors to disability-adjusted life-years (DALYs) attributable to substance use were identified in the domains of substance use disorders (20.4 million DALYs), cancer (1.6 million DALYs), liver cirrhosis (4.8 million DALYs), and human immunodeficiency virus (HIV) (3.2 million DALYs) [6]. Moreover, substance use is responsible for almost 452,000 deaths annually.
Opioid dependence is one of the most common substance use disorders, with rates of 1.2% of the adult population worldwide, half of which is situated in South Asia or South-West Asia [5]. Moreover, opioids persist as the most lethal category of substances, responsible for approximately two-thirds of direct substance-related deaths, primarily through overdoses [5]. Consistently with global trends, substance use, particularly opium in Iran, has increased recently [7]. This is due to several factors, including the fact that Iran shares its border with Afghanistan, the world’s largest producer of opium, and Iran is a significant route for opium transport to Europe [8]. Another significant factor is Iran’s primary host of Afghan refugees (over three million). Given the historical prevalence of opium use among the Afghan population, prior evidence depicted the continuation of opium use among Afghan refugees in Iran [9]. These factors contribute to the escalated prevalence of opium use in Iran, facilitated by easy accessibility and low cost. In line with this, the WHO report illustrated Iran has the highest rate of opium users worldwide, and opium use disorder among Iranians is three times higher than global usage [10]. Moreover, previous literature demonstrated that around two million people in Iran are estimated to consume illicit substances, which equals 2.7% of the total population [11].
In accordance with robust evidence, substance use was strongly associated with mental, physical, and social health problems [12–14]. In spite of the high spectrum of problems associated with industrial substances, opium use as a traditional substance is related to several physical disabilities, including cancers and cardiovascular diseases [7].. Nevertheless, with the introduction of various health policies, substance use has still significantly increased in recent years [15–18]. In addressing this issue, health policymakers should be aware of the determinants influencing substance use to develop and implement proper prevention programs, potentially leading to a reduction in the incidence of substance use in society [19].
As of yet, a number of epidemiological and regional surveys have assessed substance use prevalence among Iranians, but their results were curtailed by small sample sizes and demographic differences among study populations [20, 21]. Furthermore, the prevalence of substance and opium use remains uncertain in Tehran, the capital of Iran, and available data are sparse and only encompass limited areas of the city. Additionally, previous investigations suggest that the male gender, younger age, socioeconomic status, as well as alcohol and tobacco use [22, 23]. Nevertheless, comprehensive data on predictors or determinants of substance and opium use in Tehran is still lacking.
Considering the ongoing population changes in Tehran, conducting a comprehensive study on substance use prevalence would be necessary to provide suitable insight into the current situation of substance use in Tehran for developing healthcare-related programs and governmental implementations [24, 25]. Therefore, as the first comprehensive investigation, we aimed to evaluate the prevalence and epidemiology of substance use, notably opium, in Tehran utilizing the recruitment phase data from the Tehran Cohort study (TeCS) data with a focus on identifying independent determinants associated with opium use.
Methods
Study design and participants
We examined data from TeCS, a population-based prospective study that involved adult residents of Tehran, the densely populated capital of Iran. Our study protocol has previously been published, providing a comprehensive description of the sampling methods and the recruitment phase of the TeCS study [26].. From March 2016 to March 2019, systematic random sampling was applied to recruit adults aged ≥ 35 years from all regions of Tehran. A total of 4 215 households, including 8 296 adults aged ≥ 35 years, enrolled in this study. Various demographic and medical data were collected, including past medical history, medications, familial history, anthropometric and physiological measurements, biochemistry, and laboratory tests. For this analysis, we included participants who had complete data on substance use. The TeCS protocol was reviewed and approved by the Deputy of Research and the Committee of Ethics at Tehran University of Medical Sciences (IR. TUMS.MEDICINE. REC.1399.074). All participants provided written informed consent upon enrollment in the study.
Data collection and measurements
We interviewed every participant to collect data on demographic characteristics, such as age, marital status, ethnicity, educational level, employment status, medical history, pre-existing comorbidities, metabolic and behavioral risk factors, physical activity, level of education, alcohol and tobacco consumption, and substance use status. Several anthropometric indices were measured in all participants, including weight and height. Body mass index (BMI) was calculated by dividing weight by the height square (kg/m2). In addition, blood pressure (BP) was measured in a sitting position after at least five minutes of rest using a digital brachial cuff, and this assessment was conducted at least twice within a time frame of four hours based on recent guidelines [27].
Definitions
We recorded the presence of diabetes, hypertension, dyslipidemia, chronic kidney disease, and cerebral vascular accident (CVA) in the participants based on history taking, medical documents, or medications. All information in the case of definitions of these conditions was completely explained in our previous reports from TeCS [28–30]. In brief, diabetes mellitus is characterized by a confirmed medical diagnosis of type 2 diabetes from healthcare professionals, fasting blood glucose (FBG) levels exceeding 126 mg/dl after an overnight fast lasting 8–12 h, or the utilization of glucose-lowering medications like oral hypoglycemic agents or insulin. Moreover, hypertension is defined as either a self-reported prior diagnosis of hypertension, systolic BP measurements equal to or exceeding 140 mmHg, diastolic BP measurements equal to or exceeding 90 mmHg, or the use of antihypertensive medications. Dyslipidemia is defined as suboptimal levels of high-density lipoprotein (HDL) cholesterol and/or elevated levels of triglycerides or low-density lipoprotein (LDL) cholesterol, accompanied by the use of lipid-lowering medications.
In the in-person interview questionnaire, we employed a subjective Likert scale to categorize average daily physical activity into low, intermediate, and high levels. We also asked them about their tobacco smoking status, whether current or past. We classified those who smoked cigarettes, pipes, or hookah occasionally or daily as current tobacco users. We defined former tobacco users as those who had quit smoking at least one month before the interview. We also asked about alcohol consumption in the last year, including any type of alcoholic drink.
We interviewed the participants using a comprehensive questionnaire that asked about their substance use patterns. We employed skilled interviewers who underwent comprehensive training in accordance with the Tehran Heart Center protocol to minimize data gaps and ensure clarity in our specialized inquiries, such as drug usage information. Our questionnaire included the type, frequency, and route of administration of substances. In the details, substances included opioids (such as heroin, morphine, opium, and opioid derivatives), cannabis, cocaine, and amphetamines. We considered an acceptable range of street names and custom labels associated with prevalent substances in Iran to make sure we identified all the substances in the participants. We defined current substance use as frequent use (on a daily basis) of any substance at least three months before the interview. We also asked them if they had quit using any substances based on their self-reports. Participants who did not report current substance consumption during the interview but provided a history of past substance use or indicated they had ceased using substances were classified as former substance users. Also, recreational users are individuals who have employed substances irregularly, notably opium, in traditional patterns, on specific occasions, or as a form of medication to alleviate pain and certain medical conditions. Participants who reported any level of opium consumption were categorized as opium users in the previous year.
Statistical analysis
We reported categorical variables as frequencies and percentages for both men and women and compared them using the Chi-square test or Fisher exact test. We expressed continuous variables as means and standard deviations and compared them using the independent t-test for two groups or one-way ANOVA for more than two groups. We also calculated the total and sex-specific prevalence of substance use in our study population and the prevalence of opium and non-opium users. We weighted the prevalence of opium and substance use by age and sex based on the 2016 national census [31]. We evaluated the effect of baseline covariates on the odds of opium use utilizing a logistic regression model for ordinal dependent variables adjusting for age, sex, marital status, ethnicity, employment, level of education, BMI, diabetes mellitus, hypertension, dyslipidemia, CVA, chronic kidney disease, physical activity level based on Likert scale, tobacco use, and alcohol consumption. The adjusted association of the variables with opium use was reported through odds ratio (OR) with a 95% confidence interval (CI). We mapped the geographic distribution of substance use in Tehran based on the first three digits of the participants’ zip code using shp2dta and spmap modules in Stata software, release 14.2 (College Station, TX: Stata Corp LP.). We performed statistical analyses using IBM SPSS Statistics for Windows, version 23.0 (Armonk, NY: IBM Corp).
Results
General characteristics of the study population
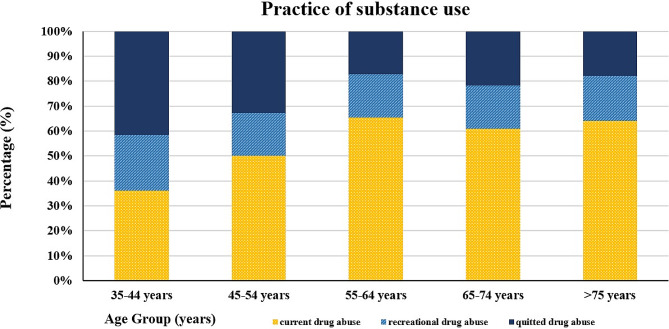
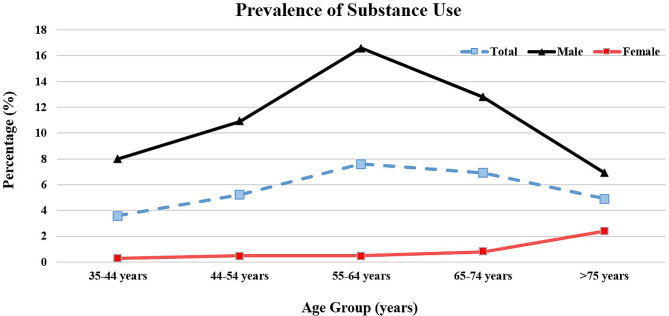
In this study, out of 8 296 adults aged ≥ 35 years, we assessed data from 8 259 eligible participants who had complete data on substance use (mean age: 53.7 ± 12.75, 54% women) and found a 5.6% prevalence of substance use among our study population in Tehran. The prevalence of substance use varied by age group, with the highest rate (7.6%) among participants aged 55 to 64. Males were much more likely to use substances than females, with a weighted prevalence of 10.9% (95% CI: 9.0–13.2) versus 0.6% (95% CI: 0.2–1.3). Opium use was the most prevalent substance in participants with a history of substance use, and the weighted prevalence was 5.3% (95% CI: 4.6–7.1), with a significant gender difference (weighted prevalence in males: 10.5% [95% CI: 8.6–12.6], weighted prevalence in females: 0.5% [95% CI: 0.2–1.2]). Moreover, among all subjects with a history of substance use, recreational and former patterns of use accounted for 1.0% and 1.5% of the study population, respectively (Figure 1). Table 1 summarizes all demographic, anthropometric, and medical characteristics comparisons between non-substance and substance users among our study population considering gender subgroups.
Fig. 1.
Practice of substance use in the different age groups
Table 1.
Baseline characteristics of the eligible participants (divided by gender) in the Tehran Cohort Study according to substance use status
| Demographic Characteristics* | Total (n = 8259) | Women (n = 4461) | Men (n = 3798) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-substance users (n = 7800) | Substance users (n = 459) | P value# | Non-substance users (n = 4435) | Substance users (n = 26) | P value | Non-substance users (n = 3365) | Substance users (n = 433) | P value | |
| Age, mean(SD), y | 53.6 (12.78) | 56.4 (11.67) | < 0.001 | 52.9 (12.33) | 60.5 (15.22) | 0.017 | 54.6 (13.3) | 56.2 (11.4) | 0.008 |
| Age subgroups, n (%) | |||||||||
| 35–44 | 2233 (28.6) | 84 (18.3) | 1312 (29.6) | 4 (15.4) | 921 (27.4) | 80 (18.5) | |||
| 45–54 | 2086 (26.7) | 115 (25.1) | 1119 (26.9) | 6 (23.1) | 895 (26.6) | 109 (25.2) | |||
| 55–64 | 1811 (23.2) | 148 (32.2) | < 0.001 | 1095 (24.7) | 5 (19.2) | 0.011 | 716 (21.3) | 143 (33.0) | < 0.001 |
| 65–74 | 1131 (14.5) | 84 (18.3) | 593 (13.4) | 5 (19.2) | 538 (16.0) | 79 (18.2) | |||
| > 75 | 539 (6.9) | 28 (6.1) | 244 (5.5) | 6 (23.1) | 295 (8.8) | 22 (5.1) | |||
| Ethnicity, n (%) | |||||||||
| Fars | 3798 (48.7) | 226 (49.3) | 2164 (48.8) | 13 (50) | 1634 (48.6) | 213 (49.3) | |||
| Azari | 2318 (29.7) | 130 (28.4) | 1300 (29.3) | 4 (15.4) | 1018 (30.3) | 126 (29.2) | |||
| Gilak | 314 (4.0) | 18 (3.9) | 192 (4.3) | 1 (3.8) | 122 (3.6) | 17 (3.9) | |||
| Lor | 297 (3.8) | 20 (4.4) | 157 (3.5) | 1 (3.8) | 140 (4.2) | 19 (4.4) | |||
| Kurd | 181 (2.3) | 12 (2.6) | 0.882 | 98 (2.2) | 2 (7.7) | 0.139 | 83 (2.5) | 10 (2.3) | 0.609 |
| Mixed | 640 (8.2) | 42 (9.2) | 397 (9.0) | 3 (11.5) | 243 (7.2) | 39 (9.0) | |||
| Other | 198 (2.5) | 9 (2.0) | 96 (2.2) | 2 (7.7) | 102 (3.0) | 7 (1.6) | |||
| Immigrants/Refugees | 48 (0.6) | 1 (0.2) | 30 (0.7) | 0 (0.0) | 18 (0.5) | 1 (0.2) | |||
| Marital status, n (%) | |||||||||
| Single | 63 (0.8) | 3 (0.7) | 41 (0.9) | 0 (0.0) | 22 (0.7) | 3 (0.7) | |||
| Married | 7547 (96.8) | 445 (96.9) | 0.937 | 4251 (95.9) | 24 (92.3) | 0.378 | 3296 (98) | 421 (97.2) | 0.436 |
| Other | 187 (2.4) | 11 (2.4) | 143 (3.2) | 2 (7.7) | 44 (1.3) | 9 (2.1) | |||
| Education years, n (%) | |||||||||
| Illiterate | 542 (7.0) | 43 (9.4) | 419 (9.4) | 8 (30.8) | 123 (3.7) | 35 (8.1) | |||
| 1–5 years | 782 (10.0) | 58 (12.6) | < 0.001 | 507 (11.4) | 5 (19.2) | 0.002 | 275 (8.2) | 53 (12.2) | < 0.001 |
| 6–12 years | 4008 (51.4) | 284 (61.9) | 2348 (53) | 10 (38.5) | 1660 (49.4) | 274 (63.3) | |||
| >12 years | 2462 (31.6) | 74 (16.1) | 1160 (26.2) | 3 (11.5) | 1302 (38.8) | 71 (16.4) | |||
| Employment | |||||||||
| Unemployed | 4669 (59.9) | 179 (39.0) | < 0.001 | 3610 (81.4) | 22 (84.6) | 0.805 | 1059 (31.5) | 157 (36.3) | 0.046 |
| Employed | 3128 (40.1) | 280 (61.0) | 825 (18.6) | 4 (15.4) | 2303 (68.5) | 276 (63.7) | |||
| Body mass index, mean(SD), kg/m2 | 28.1 (4.83) | 26.6 (4.51) | < 0.001 | 28.7 (5.17) | 28.9 (4.16) | 0.846 | 27.3 (4.21) | 26.4 (4.5) | < 0.001 |
| Body mass index subgroups, n (%) | |||||||||
| <20 | 195 (2.5) | 30 (6.6) | 98 (2.2) | 0 (0.0) | 97 (2.9) | 30 (7.0) | |||
| 20-24.99 | 1930 (24.9) | 142 (31.3) | 1035 (23.6) | 3 (13.0) | 895 (26.8) | 139 (32.3) | |||
| 25-29.99 | 3237 (41.8) | 182 (40.1) | < 0.001 | 1649 (37.5) | 12 (52.2) | 0.629 | 1588 (47.5) | 170 (39.4) | < 0.001 |
| 30-34.99 | 1712 (22.1) | 81 (17.8) | 1092 (24.9) | 5 (21.7) | 620 (18.5) | 76 (17.6) | |||
| > 35 | 663 (8.6) | 19 (4.2) | 520 (11.8) | 3 (13.0) | 143 (4.3) | 16 (3.7) | |||
| Physical activity, n (%) | |||||||||
| Low | 1338 (17.3) | 110 (24.4) | 851 (19.3) | 11 (42.3) | 487 (14.6) | 99 (23.3) | |||
| Intermediate | 4520 (58.3) | 239 (53.0) | 0.001 | 2677 (60.6) | 10 (38.5) | 0.01 | 1843 (55.3) | 229 (53.9) | < 0.001 |
| High | 1890 (24.4) | 102 (22.6) | 888 (20.1) | 5 (19.2) | 1002 (30.1) | 97 (22.8) | |||
| Alcohol use, n (%) | |||||||||
| No | 7157 (92.0) | 341 (74.9) | < 0.001 | 4294 (97.0) | 23 (88.5) | 0.045 | 2863 (85.5) | 318 (74.1) | < 0.001 |
| Yes | 622 (8.0) | 114 (25.1) | 135 (3.0) | 3 (11.5) | 487 (14.5) | 111 (25.9) | |||
| Tobacco use, n (%) | |||||||||
| Never | 6244 (80.1) | 94 (20.5) | 4057 (91.5) | 16 (61.5) | 2187 (65.0) | 78 (18.0) | |||
| Quitted | 273 (3.5) | 60 (13.1) | < 0.001 | 46 (1.0) | 0 (0.0) | < 0.001 | 227 (6.7) | 60 (13.9) | < 0.001 |
| Yes | 1282 (16.4) | 305 (66.4) | 332 (7.5) | 10 (38.5) | 950 (28.2) | 295 (68.1) | |||
| Diabetes mellitus, n (%) | |||||||||
| No | 6249 (81.5) | 364 (81.4) | 0.969 | 3582 (81.8) | 17 (68.0) | 0.113 | 2667 (81.1) | 347 (82.2) | 0.573 |
| Yes | 1418 (18.5) | 83 (18.6) | 796 (18.2) | 8 (32.0) | 622 (18.9) | 75 (17.8) | |||
| Hypertension, n (%) | |||||||||
| No | 5614 (72.0) | 325 (71.0) | 0.636 | 3125 (70.5) | 17 (65.4) | 0.57 | 2489 (74.0) | 308 (71.3) | 0.235 |
| Yes | 2185 (28.0) | 133 (29.0) | 1309 (29.5) | 9 (34.6) | 876 (26.0) | 124 (28.7) | |||
| Dyslipidemia, n (%) | |||||||||
| No | 5243 (67.2) | 318 (69.4) | 0.328 | 2893 (65.2) | 18 (69.2) | 0.67 | 2350 (69.8) | 300 (69.4) | 0.867 |
| Yes | 2556 (32.8) | 140 (30.6) | 1541 (34.8) | 8 (30.8) | 1015 (30.2) | 132 (30.6) | |||
| Cerebral vascular accident, n (%) | |||||||||
| No | 7692 (98.6) | 445 (96.9) | 0.003 | 4380 (98.8) | 25 (96.2) | 0.276 | 3312 (98.5) | 420 (97) | 0.028 |
| Yes | 106 (1.4) | 14 (3.1) | 54 (1.2) | 1 (3.8) | 52 (1.5) | 13 (3) | |||
| Chronic kidney disease, n (%) | |||||||||
| No | 7734 (99.2) | 454 (98.9) | 0.597 | 4401 (99.2) | 26 (100.0) | > 0.0999 | 3333 (99.0) | 428 (98.8) | 0.605 |
| Yes | 66 (0.8) | 5 (1.1) | 34 (0.8) | 0 (0.0) | 32 (1.0) | 5 (1.2) | |||
| Systolic blood pressure, mean (SD), mmHg | 121.6 (18.77) | 124.3 (19.99) | 0.005 | 119.2 (19.39) | 120.1 (20.93) | 0.813 | 124.8 (17.42) | 124.6 (19.93) | 0.852 |
| Diastolic blood pressure, mean (SD), mmHg | 80.8 (10.75) | 79.6 (12.01) | 0.033 | 80.8 (10.72) | 81.1 (12.83) | 0.892 | 80.9 (10.78) | 79.5 (11.96) | 0.026 |
Abbreviations: SD: Standard deviation
* Continuous variables with normal distribution are shown as mean ± standard deviation.
# P < 0.05 was considered statistically significant.
Demographic assessment of participants with substance use
Based on our results, a total of 459 participants self-reported the use of substances during their lifetime. In detail, 95.8% (n = 440) of these participants consumed opium only, while 8.9% used other substances with or without opium (n = 42). Additionally, substance users were older than their peers in both genders (women: P = 0.017, men: P = 0.008). Regarding gender subgroups, substance use was also more prevalent among males in the 55–64 age subgroup (P < 0.001). Besides, older female subgroups were more likely to use substances (P = 0.011). Furthermore, substance use rates decreased with higher education levels (P < 0.001); however, most substance users had 6–12 years of education. In addition, employed participants had a higher rate of substance use (P < 0.001). Mainly, employed men were more likely to use substances than unemployed peers (P = 0.046). Besides, substance users had lower physical activity levels in both groups (P = 0.01, P < 0.001 for women and men, respectively), while non-substance users had higher BMIs, particularly among the men subgroup (P < 0.001). Participants who used substances also reported higher rates of alcohol (women: P = 0.045, men: P < 0.001) and tobacco use (P < 0.001 for both subgroups). Further, males with a history of substance were more likely to have experienced CVA (P = 0.028) among female participants; however, there were no significant differences. Compared to their peers, substance users had significantly higher systolic BP (P = 0.005); however, there were no statistical differences between gender subgroups. Additionally, Among men, substance users had significantly lower diastolic BP than non-users (P = 0.026). Marital status, diabetes, hypertension, dyslipidemia, and chronic kidney disease were similar in both groups. Figure 2 exhibited the frequency of substance use by gender and age group.
Fig. 2.
Comparison of substance use prevalence among both genders and different age groups
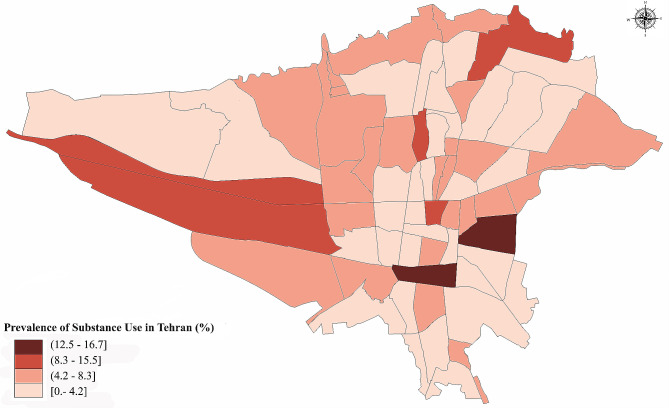
Method and geographical pattern of use
Most participants (77.2%) used inhalation as their preferred mode of consumption, followed by ingestion (28.9%), and 7.33% reported using more than one mode. Substance use was higher in areas known for substance trafficking. Figure 3 displayed substance use prevalence in different regions of Tehran based on the first three digits of the zip codes.
Fig. 3.
Geographic distribution of substance use in 22 districts of Tehran based on the first three digits of the residential zip codes. Suburban areas, particularly southern districts, are recognized for being prominent routes for drug trade and experiencing elevated levels of drug trafficking. More information about the details of the Tehran population and the distribution of participants from each district were indicated in our protocol [26]
Determinants associated with opium use
With regards to Table 2, opium use was strongly associated with male gender (P < 0.001), alcohol use (P = 0.016), and tobacco use (P < 0.001). Among ethnicities, the Azeri population had the lowest opium use prevalence (OR: 0.75, P = 0.028). Higher education levels were protective against opium use. Compared to those without formal education, participants with 1–5 years of education had a 40% lower opium use risk (OR:0.60, P = 0.051), and those with more than 12 years of education had an OR of 0.15 (P < 0.001). Nonetheless, physical activity was inversely related to opium use (high physical activity: OR: 0.52, P < 0.001).
Table 2.
Independent determinants of opium use in Tehran Cohort Study
| Characteristics | Odds ratio | (95% CI) | P value* |
|---|---|---|---|
| Age | 1.002 | 0.991–1.013 | 0.75 |
| Gender | |||
| Female | Reference | ||
| Male | 12.101 | 7.562–19.367 | < 0.001 |
| Ethnicity | |||
| Fars | Reference | ||
| Azari | 0.750 | 0.580–0.970 | 0.028 |
| Other | 0.946 | 0.715–1.251 | 0.695 |
| Marital status | |||
| Single | Reference | ||
| Married | 1.178 | 0.263–5.287 | 0.831 |
| Other | 1.620 | 0.309–8.497 | 0.568 |
| Education years | |||
| Illiterate | Reference | ||
| 1–5 years | 0.604 | 0.364–1.002 | 0.051 |
| 6–12 years | 0.4555 | 0.294–0.707 | < 0.001 |
| >12 years | 0.153 | 0.092–0.254 | < 0.001 |
| Employment | |||
| Unemployed | Reference | ||
| Employed | 0.964 | 0.728–1.277 | 0.798 |
| Body mass index | 0.964 | 0.940–0.989 | 0.005 |
| Physical activity | |||
| Low | Reference | ||
| Intermediate | 0.642 | 0.484–0.851 | 0.002 |
| High | 0.526 | 0.376–0.736 | < 0.001 |
| Alcohol use | |||
| No | Reference | ||
| Yes | 1.394 | 1.064–1.825 | 0.016 |
| Tobacco use | |||
| Never | Reference | ||
| Quitted | 6.131 | 4.184–8.984 | < 0.001 |
| Yes | 8.536 | 6.493–11.220 | < 0.001 |
| Diabetes mellitus | |||
| No | Reference | ||
| Yes | 0.869 | 0.640–1.178 | 0.366 |
| Hypertension | |||
| No | Reference | ||
| Yes | 1.232 | 0.920–1.649 | 0.161 |
| Dyslipidemia | |||
| No | Reference | ||
| Yes | 0.963 | 0.736–1.259 | 0.782 |
| Cerebral vascular accident | |||
| No | Reference | ||
| Yes | 1.632 | 0.800–3.331 | 0.178 |
| Chronic kidney disease | |||
| No | Reference | ||
| Yes | 0.742 | 0.256–2.150 | 0.583 |
Abbreviations: CI: Confidence interval
* P < 0.05 was considered statistically significant.
Discussion
The current study aimed to determine the prevalence, patterns, and risk factors associated with substance use among adults 35 years old and greater in the Tehran population. As the first comprehensive investigation, our findings revealed a prevalence of 5.6% for substance use among the study population, with opioids being the most commonly used substance among our population. In addition, our results illustrated that opium use was independently associated with male gender, lower education levels, and alcohol and tobacco consumption.
Across the globe, substance use significantly contributes to major health-related problems, such as an escalation in infectious diseases such as hepatitis C and HIV, as well as an increase in physical and psychological disabilities [32–34]. Communities and governments are also confronted with significant challenges due to substance addiction, including the burden of substantial costs, high healthcare costs, functional impairment, violence, and criminal activities. According to the World Drug Report, a concerning rise in substance use has occurred over the past decade [35]. The report states that from 2006 to 2015, the percentage of substance users worldwide increased from 4.9 to 5.6%. This upward trend has considerably impacted the lives of millions worldwide, affecting approximately 275 million individuals.
There exists a long-term historical practice of employing opium as a traditional therapy in regions where opium is traditionally produced [36]. In Afghanistan, women engaged in the carpet weaving industry resort to opium for pain relief and to relax their children. Moreover, in Morocco, the opium poppy has been traditionally utilized to relieve pain, diarrhea, cough, and insomnia. Additionally, opium has conventionally been utilized as a pain-relieving substance, particularly among the elderly population in Iran [36]. A survey conducted in 2010 demonstrated that substance use in Iran is linked to tripled mortality rates among females and almost doubled mortality rates among males from 1990 to 2010 [33, 37].. In addition, based on a 2005 rapid assessment of substance use among the Iranian population, 1 200 000–1 800 000 people (2.4 − 2.65%) had a history of substance use [38]. Moreover, the National Survey on Substance Users and the National Survey on Mental Health estimated that substance use was 2.65% and 2.8%, respectively [39, 40]. Besides, the Iranian household mental health survey conducted in 2011 demonstrated that the prevalence of substance use is 2.09% and 2.44% based on DSM-IV and DSM-5, respectively [17]. Concerning related studies [11, 18, 41], our finding highlights the increasing trend of substance use in the Tehran population.
In accordance with global trends, males were more likely to use substances than females [18, 39, 42]. Moreover, the incidence of substance use exhibited a consistent upward trend in individuals aged 35 and above, reaching its apex within the 55–64 age group. This finding is alarming since the elderly population is more vulnerable to the adverse effects of substance use due to age-related physiological changes. Additionally, the association between lower educational level [18, 39], alcohol and tobacco consumption [42, 43], lower physical activity [43], and lesser BMI [43, 44] and substance use has been revealed in several studies. Prior investigations have also explained that the prevalence of substance use in Iran peaks at older ages compared to international reports [45, 46]. Albeit, there is a controversy over the results. Some studies support our findings by depicting a higher prevalence of substance use in the 5th and 6th decades of life [18, 39]; on the other hand, other studies considered the 3rd and 4th decades of life the highest prevalence of substance use [17]. Also, the prevalence of substance use has been reported in prior studies to be higher in previously married (divorced, separated, or widowed) individuals [18, 39]; However, our findings demonstrated no association between marital status and substance use [18].
In addition, it should be mentioned due to ongoing population changes and different ethnicities and populations within Iran, substance use, particularly opioid use, is prevalent at varying rates among regions. Regarding prior studies, the northern and southern parts of Iran have been found to have a higher prevalence of substance use [43, 47]. Evidence has also illustrated a higher prevalence of opioid use in Iran’s rural population than in its urban residents [48, 49]. As a novel finding of our study Tehran district substance users’ concertation in suburban areas, especially southern parts was significantly higher than in other areas. Additionally, we used separate analyses for each gender because the disparity in the prevalence of substance use between the sexes is evident in Middle Eastern populations. Since opium use and smoking are considered taboo in women, Middle Eastern women demonstrate considerably lower rates of substance use in comparison to their counterparts in Western regions [50]. Further, it is imperative to mention that the available data on substance use among women in Iran, particularly in Tehran, was limited, which also underscored the significance of our findings.
Conversely, to recent literature [51], our study also indicates that drug use is more prevalent among employed participants, mainly men. Concerning this observation, we can gain insight into the relationship between substance use and employment status. Various factors could contribute to this phenomenon, including stress and pressure associated with work demands [52]. In addition, substance use patterns may be influenced by the work environment itself. Further, the availability and social dynamics within the workplace can contribute to the greater prevalence of substance use among employed individuals, particularly men.
These results highlight that substance use, particularly opium, is a major public health challenge in the region that requires tailored interventions to mitigate its harms and disabilities. Moreover, regular surveillance of substance use trends and risk factors is essential for developing evidence-based policies and programs. Ultimately, a collaborative effort from policymakers, healthcare providers, and the community is needed to address the issue of substance use and its consequences in Iran and other affected countries.
Strengths and limitations
The primary strength of this study lies in our provision of the first investigation and comprehensive data on substance and opium use in Tehran. The findings have the potential to serve as a foundational cornerstone for future studies and the development of public health plans and interventions in order to curb substance use, particularly opium, irregularly in Tehran. Similar to all cross-sectional studies, the current study also has some limitations, such as the presence of non-responders poses a challenge to accurately reporting the prevalence of substance and opium use in Tehran. Moreover, the observational design may be confounded by unknown variables. Furthermore, the limited number of females with substances in some analyses might impede the identification of significant differences. The broad objectives of TeCS necessitated the inclusion of only general inquiries about substance use status due to time constraints during data collection. Participants were interviewed for multiple questionnaires, and anthropometric measurements were conducted in a limited half-day session. Subsequently, detailed data on substance behaviors, such as the age of initiation and the exact amount of consumption, was lacking. Additionally, it is important to note that TeCS excluded adults aged ≥ 35 years,, potentially impacting our estimations, particularly for emerging substances like cannabis, which are believed to be more prevalent among the younger population.
Conclusion
This study reported the prevalence, patterns, and associated determinants of substance and opium use in Tehran, Iran. We found that substance use prevalence was 5.6%, and opium was the most frequently consumed substance. Inhalation was the preferred mode of substance consumption, as well as substance use, was higher in areas known for substance trafficking. Independent determinants of opium use included male gender, alcohol and tobacco use, and lower education levels. In order to minimize Tehran’s substance use problem, healthcare sectors and policymakers should address our findings to develop preventive strategies and approaches, especially among vulnerable populations.
Acknowledgements
The Tehran Cohort Study team thanks all the study participants for their time and cooperation. The drafting of this manuscript was supported by the Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran.
Abbreviations
- BMI
Body mass index
- 95% CI
95% confidence intervals
- CVA
Cerebrovascular accident
- DALY
Disability-adjusted life-years
- HIV
Human immunodeficiency virus
- OR
Odds ratio
- TeCS
Tehran cohort study
- WHO
World Health Organization
Author contributions
FM and AS: Study concept, Data collecting, and drafting the initial manuscript and final approval; AH: Drafting the initial manuscript, revision critically, and final approval; NsH, KT: Drafting the initial manuscript and final approval; AJ: Study design, supervision, data cleaning, interpretation, analysis, and final approval; SN: revised the study critically and final approval, FA, SoSa, AV: study management, revised the study critically and final approval; SaSa, MB, AK: Supervision, study management, revision, and final approval; VAA: revision the study critically and final approval. All the authors read and approved the final version of the manuscript.
Funding
This study was financially supported by the Iranian Ministry of Health and the Tehran Heart Center.
Data availability
The data underlying this article will be shared at a reasonable request to the corresponding author.
Declarations
Ethics approval and consent to participate
This project was approved by the Tehran Heart Center’s review board and the ethical committee of the Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1399.074). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all study participants before enrollment.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Farzad Masoudkabir and Akbar Shafiee contributed equally to this manuscript and should be considered the first author.
References
- 1.Network GBDC. Global burden of disease study 2017 (GBD 2017) results. Seattle, United States: Institute for health metrics and evaluation (IHME). 2018.
- 2.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heidari N, Hajikarim-Hamedani A, Heidari A, Ghane Y, Sadat-Shirazi M-S, Ashabi G, Zarrindast M-R. Alcohol: Epigenome Alteration and Transgenerational Effect. In: Preprintsorg Preprints.org; 2023. [DOI] [PubMed]
- 4.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–33. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 5.World Drug Report. 2023 [https://www.unodc.org/unodc/en/data-and-analysis/world-drug-report-2023.html].
- 6.Alcohol GBD, Drug Use C. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012. doi: 10.1016/S2215-0366(18)30337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohebbi E, Kamangar F, Rahimi-Movaghar A, Haghdoost AA, Etemadi A, Amirzadeh S, Najafi F, Shafeie F, Fakhari A, Ghaleban K, et al. An Exploratory Study of Units of Reporting Opium Usein Iran: implications for epidemiologic studies. Arch Iran Med. 2019;22(10):541–5. [PubMed] [Google Scholar]
- 8.Malloch-Brown M. Opium production in Afghanistan. BMJ. 2008;336(7651):972. doi: 10.1136/bmj.39554.402199.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jack H, Masterson AR, Khoshnood K. Violent conflict and opiate use in low and middle-income countries: a systematic review. Int J Drug Policy. 2014;25(2):196–203. doi: 10.1016/j.drugpo.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Soroosh D, Neamatshahi M, Zarmehri B, Nakhaee S, Mehrpour O. Drug-induced prolonged corrected QT interval in patients with methadone and opium overdose. Subst Abuse Treat Prev Policy. 2019;14(1):8. doi: 10.1186/s13011-019-0196-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eskandarieh S, Jafari F, Yazdani S, Hazrati N, Saberi-Zafarghandi MB. Compulsory maintenance treatment program amongst Iranian injection drug users and its side effects. Int J High Risk Behav Addict. 2014;3(4):e21765. doi: 10.5812/ijhrba.21765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sommers I, Baskin D, Baskin-Sommers A. Methamphetamine use among young adults: health and social consequences. Addict Behav. 2006;31(8):1469–76. doi: 10.1016/j.addbeh.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Shariatirad S, Maarefvand M, Ekhtiari H. Methamphetamine use and methadone maintenance treatment: an emerging problem in the drug addiction treatment network in Iran. Int J Drug Policy. 2013;24(6):e115–6. doi: 10.1016/j.drugpo.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Fronczak CM, Kim ED, Barqawi AB. The insults of illicit drug use on male fertility. J Androl. 2012;33(4):515–28. doi: 10.2164/jandrol.110.011874. [DOI] [PubMed] [Google Scholar]
- 15.Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the global burden of Disease Study 2010. PLoS ONE. 2015;10(2):e0116820. doi: 10.1371/journal.pone.0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Momtazi S, Noroozi A, Rawson R. An overview of Iran drug treatment and harm reduction programs. Textbook Addict Treatment: Int Perspect Milano: Springer 2015:543–54.
- 17.Amin-Esmaeili M, Rahimi-Movaghar A, Sharifi V, Hajebi A, Radgoodarzi R, Mojtabai R, Hefazi M, Motevalian A. Epidemiology of illicit drug use disorders in Iran: prevalence, correlates, comorbidity and service utilization results from the Iranian Mental Health Survey. Addiction. 2016;111(10):1836–47. doi: 10.1111/add.13453. [DOI] [PubMed] [Google Scholar]
- 18.Mohebbi E, Haghdoost AA, Noroozi A, Molavi Vardanjani H, Hajebi A, Nikbakht R, Mehrabi M, Jabbarinejad Kermani A, Salemianpour M, Baneshi MR. Awareness and attitude towards opioid and stimulant use and lifetime prevalence of the drugs: a study in 5 Large Cities of Iran. Int J Health Policy Manag. 2019;8(4):222–32. doi: 10.15171/ijhpm.2018.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kok G, Gottlieb NH, Peters GJ, Mullen PD, Parcel GS, Ruiter RA, Fernández ME, Markham C, Bartholomew LK. A taxonomy of behaviour change methods: an intervention mapping approach. Health Psychol Rev. 2016;10(3):297–312. doi: 10.1080/17437199.2015.1077155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khademi H, Malekzadeh R, Pourshams A, Jafari E, Salahi R, Semnani S, Abaie B, Islami F, Nasseri-Moghaddam S, Etemadi A. Opium use and mortality in Golestan Cohort Study: prospective cohort study of 50 000 adults in Iran. BMJ 2012, 344. [DOI] [PMC free article] [PubMed]
- 21.Fallahzadeh MA, Salehi A, Naghshvarian M, Fallahzadeh MH, Poustchi H, Sepanlou SG, Gandomkar A, Malekzadeh R. Epidemiologic study of Opium Use in Pars Cohort Study: a study of 9000 adults in a rural Southern Area of Iran. Archives Iran Med (AIM) 2017, 20(4). [PubMed]
- 22.Fleury MJ, Grenier G, Bamvita JM, Perreault M, Caron J. Predictors of alcohol and drug dependence. Can J Psychiatry. 2014;59(4):203–12. doi: 10.1177/070674371405900405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moradinazar M, Najafi F, Jalilian F, Pasdar Y, Hamzeh B, Shakiba E, Hajizadeh M, Haghdoost AA, Malekzadeh R, Poustchi H, et al. Prevalence of drug use, alcohol consumption, cigarette smoking and measure of socioeconomic-related inequalities of drug use among Iranian people: findings from a national survey. Subst Abuse Treat Prev Policy. 2020;15(1):39. doi: 10.1186/s13011-020-00279-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heydari Z, Baneshi MR, Sharifi H, Zamanian M, Haji-Maghsoudi S, Zolala F. Evaluation of the treatment failure ratio in individuals receiving methadone maintenance therapy via the network scale up method. Int J Drug Policy. 2019;73:36–41. doi: 10.1016/j.drugpo.2019.07.022. [DOI] [PubMed] [Google Scholar]
- 25.Shokoohi M, Baneshi MR, Haghdoost A-A. Size estimation of groups at high risk of HIV/AIDS using network scale up in Kerman, Iran. Int J Prev Med. 2012;3(7):471. [PMC free article] [PubMed] [Google Scholar]
- 26.Shafiee A, Saadat S, Shahmansouri N, Jalali A, Alaeddini F, Haddadi M, Tajdini M, Ashraf H, Omidi N, Masoudkabir F. Tehran cohort study (TeCS) on cardiovascular diseases, injury, and mental health: design, methods, and recruitment data. Global Epidemiol. 2021;3:100051. doi: 10.1016/j.gloepi.2021.100051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, Myers MG, Ogedegbe G, Schwartz JE, Townsend RR, et al. Measurement of blood pressure in humans: A Scientific Statement from the American Heart Association. Hypertension. 2019;73(5):e35–e66. doi: 10.1161/HYP.0000000000000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oraii A, Shafiee A, Jalali A, Alaeddini F, Saadat S, Masoudkabir F, Vasheghani-Farahani A, Heidari A, Sadeghian S, Boroumand M, et al. Prevalence, awareness, treatment, and control of type 2 diabetes mellitus among the adult residents of tehran: Tehran Cohort Study. BMC Endocr Disord. 2022;22(1):248. doi: 10.1186/s12902-022-01161-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oraii A, Shafiee A, Jalali A, Alaeddini F, Saadat S, Sadeghian S, Poorhosseini H, Boroumand M, Karimi A, Franco OH. Prevalence, awareness, treatment, and Control of Hypertension among adult residents of Tehran: the Tehran Cohort Study. Glob Heart. 2022;17(1):31. doi: 10.5334/gh.1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shafiee A, Oraii A, Jalali A, Alaeddini F, Saadat S, Masoudkabir F, Tajdini M, Ashraf H, Omidi N, Heidari A, et al. Epidemiology and prevalence of tobacco use in Tehran; a report from the recruitment phase of Tehran cohort study. BMC Public Health. 2023;23(1):740. doi: 10.1186/s12889-023-15629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carapetis J, Dadi AF. Erratum: Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 (The Lancet (2017) 390 (10100)(1211–1259)(S0140673617321542)(10.1016/S0140-6736 (17) 32154-2)). The Lancet 2017, 390(10106):e38. [DOI] [PMC free article] [PubMed]
- 32.Seth P, Scholl L, Rudd RA, Bacon S. Overdose deaths involving opioids, Cocaine, and psychostimulants - United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–58. doi: 10.15585/mmwr.mm6712a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moazen B, Shokoohi M, Noori A, Rahimzadeh S, Saeedi Moghaddam S, Rezaei F, Lotfizadeh M, Kazemi MR, Jamshidi HR, Pazhuheian F, et al. Burden of Drug and Alcohol Use disorders in Iran: findings from the global burden of Disease Study 2010. Arch Iran Med. 2015;18(8):480–5. [PubMed] [Google Scholar]
- 34.Schalkoff CA, Lancaster KE, Gaynes BN, Wang V, Pence BW, Miller WC, Go VF. The opioid and related drug epidemics in Rural Appalachia: a systematic review of populations affected, risk factors, and Infectious diseases. Substance Abuse. 2020;41(1):35–69. doi: 10.1080/08897077.2019.1635555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Azizi H, Buhler A, Bussink C, Campello G, Carpentier C, Eichinger N, Hariga F, Kamminga J, Korenblik A, Koutsenok I. The World Drug Report 2015. 2015.
- 36.Kamali M, Tajadini H, Mehrabani M, Moghadari M. Consequences of opioid abuse and their treatments in Persian Medicine: a review study. Addict Health. 2020;12(1):46–57. doi: 10.22122/ahj.v12i1.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Naghavi M, Shahraz S, Sepanlou SG, Dicker D, Naghavi P, Pourmalek F, Mokdad A, Lozano R, Vos T, Asadi-Lari M, et al. Health transition in Iran toward chronic diseases based on results of global burden of Disease 2010. Arch Iran Med. 2014;17(5):321–35. [PubMed] [Google Scholar]
- 38.Narenjiha HRH, Baghestani AR, et al. et al. In: Rapid Assessment of Substance Abuse in Iran- second study. Center for Research and Education on abuse and substance abuse. Tehran, et al.et al., editors. Iran: University of Social Welfare and Rehabilitation Sciences, office of UN Proliferation Control Program; 2005. [Google Scholar]
- 39.Noorbala AA, Saljoughian A, Bagheri Yazdi SA, Faghihzadeh E, Farahzadi MH, Kamali K, Faghihzadeh S, Hajebi A, Akhondzadeh S, Mousavi MT. Evaluation of drug and alcohol abuse in people aged 15 years and older in Iran. Iran J Public Health. 2020;49(10):1940–6. doi: 10.18502/ijph.v49i10.4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Damari B, Sarami H, Alikhani S, Mirzaei H. A National survey on substance use among Iranian industrial workers. Med J Islam Repub Iran. 2020;34:20. doi: 10.34171/mjiri.34.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Noori R, Daneshmand R, Farhoudian A, Ghaderi S, Aryanfard S, Moradi A. Amphetamine-type stimulants in a group of adults in Tehran, Iran: a rapid situation assessment in twenty-two districts. Iran J Psychiatry Behav Sci 2016, 10(4).
- 42.Sarani EM, Ahmadi J, Oji B, Mahi-Birjand M, Bagheri N, Bazrafshan A, Manshadi MD, Yaghoubi S, Dezhkam A, Khatami M, et al. Investigating the sequential patterns of methamphetamine use initiation in Iran. Subst Abuse Treat Prev Policy. 2020;15(1):52. doi: 10.1186/s13011-020-00297-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fallahzadeh MA, Salehi A, Naghshvarian M, Fallahzadeh MH, Poustchi H, Sepanlou SG, Gandomkar A, Malekzadeh R. Epidemiologic study of Opium Use in Pars Cohort Study: a study of 9000 adults in a rural Southern Area of Iran. Arch Iran Med. 2017;20(4):205–10. [PubMed] [Google Scholar]
- 44.Yousefzadeh G, Sheikhvatan M. Age and gender differences in the clustering of metabolic syndrome combinations: a prospective cohort research from the Kerman Coronary Artery Disease Risk Study (KERCADRS) Diabetes Metab Syndr. 2015;9(4):337–42. doi: 10.1016/j.dsx.2013.02.023. [DOI] [PubMed] [Google Scholar]
- 45.Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70. doi: 10.1016/S0140-6736(11)61138-0. [DOI] [PubMed] [Google Scholar]
- 46.Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, Freedman G, Burstein R, Johns N, Engell RE, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the global burden of Disease Study 2010. Lancet. 2013;382(9904):1564–74. doi: 10.1016/S0140-6736(13)61530-5. [DOI] [PubMed] [Google Scholar]
- 47.Khademi H, Malekzadeh R, Pourshams A, Jafari E, Salahi R, Semnani S, Abaie B, Islami F, Nasseri-Moghaddam S, Etemadi A, et al. Opium use and mortality in Golestan Cohort Study: prospective cohort study of 50,000 adults in Iran. BMJ. 2012;344:e2502. doi: 10.1136/bmj.e2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ziaaddini H, Ziaaddini T, Nakhaee N. Pattern and trend of substance abuse in eastern rural Iran: a household survey in a rural community. J Addict. 2013;2013:297378. doi: 10.1155/2013/297378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ziaaddini H, Sharifi A, Nakhaee N, Ziaaddini A. The prevalence of at least one-time substance abuse among Kerman Pre-university Male Students. Addict Health. 2010;2(3–4):103–10. [PMC free article] [PubMed] [Google Scholar]
- 50.Kheirkhah MT, Mokarrami M, Kazemitabar M, Garcia D. Inequalities in care for Iranian women suffering from the comorbidity of substance use and mental illness: the need for integrated treatment. Health Promot Perspect. 2023;13(3):198–201. doi: 10.34172/hpp.2023.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nolte-Troha C, Roser P, Henkel D, Scherbaum N, Koller G, Franke AG. Unemployment and substance use: an updated review of studies from North America and Europe. Healthc (Basel) 2023, 11(8). [DOI] [PMC free article] [PubMed]
- 52.Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–30. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared at a reasonable request to the corresponding author.