In this issue of the Journal, Matthay and colleagues (pp. 37–47) propose a new global definition of acute respiratory distress syndrome (ARDS) (1). This definition extends the Berlin definition of ARDS on three important points: 1) inclusion of high-flow nasal cannula (HFNC); 2) use of oxygen saturation as measured by pulse oximetry (SpO2)/FiO2 in patients in whom PaO2 measurements are not available; and 3) allowance of lung ultrasound (LUS) as an alternative imaging modality to chest X-ray (CXR) and computed tomography. The panel of 32 experts is to be congratulated for their courage to have challenged such a controversial topic. The purpose of this editorial is to contextualize the proposed changes by asking seven questions that arise after examining the paper.
Why Do We Need a New Definition?
In the past decade, intensive care management of patients with acute respiratory failure has changed considerably. HFNC is frequently preferred over noninvasive ventilation or invasive ventilation, more patients are managed without arterial blood gases now that SpO2 is often used for oxygenation targets, and the new generation of physicians is more comfortable with LUS as a diagnostic modality. In resource-limited settings, invasive ventilation, arterial blood gas measurements, and CXRs are sometimes not available at all, precluding the diagnosis of ARDS based on the Berlin definition. These observations may not be of much consequence for clinical management, as there is no specific treatment for ARDS, but they may have important consequences for epidemiological and intervention studies.
Why Extend the Definition to Nonintubated Patients?
With a desire inspired by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic to intervene earlier in the course of ARDS and to include patients on a global scale, trial groups have already started to allow inclusion of patients fulfilling most of the Berlin ARDS criteria but allowing inclusion without a positive end-expiratory pressure (PEEP) of at least 5 cm H2O, now coined “nonintubated ARDS.” This group partly includes patients who received noninvasive ventilation or would be intubated before the widespread use of HFNC and therefore maintains the epidemiological characteristics of ARDS. Indeed, patients who were consequently intubated frequently fulfilled the Berlin ARDS criteria (2). Yet, HFNC is also applied in other patients with milder lung injury, who would not have progressed to require invasive ventilation. Inclusion of patients on HFNC will therefore result in increased ARDS prevalence. In settings with limited resources, the new global definition for ARDS eliminates the need for both PEEP and a minimum flow rate of oxygen, thereby contributing to an even more diluted characterization of ARDS in such environments. Interestingly, inclusion of this population is in line with the original description by Ashbaugh and colleagues of the syndrome, in which 5 out of 12 patients did not receive invasive mechanical ventilation (3), and the American-European consensus definition.
Is SpO2 a Sufficiently Validated Alternative to PaO2?
SpO2 can replace PaO2 under the proposed global definition as a marker of severity of hypoxia. Crucially, PaO2/FiO2 already has important limitations, including its dependence on the amount of PEEP and FiO2 (4). For SpO2, these challenges are expanded, as it is only meaningful when the value is below 97% and as it provides a biased assessment in patients with darker skin color and/or shock (5, 6). These issues will likely have an important impact on the prevalence of ARDS, especially when used on a global scale, and are insufficiently understood today.
What Are the Challenges with the Imaging Criteria?
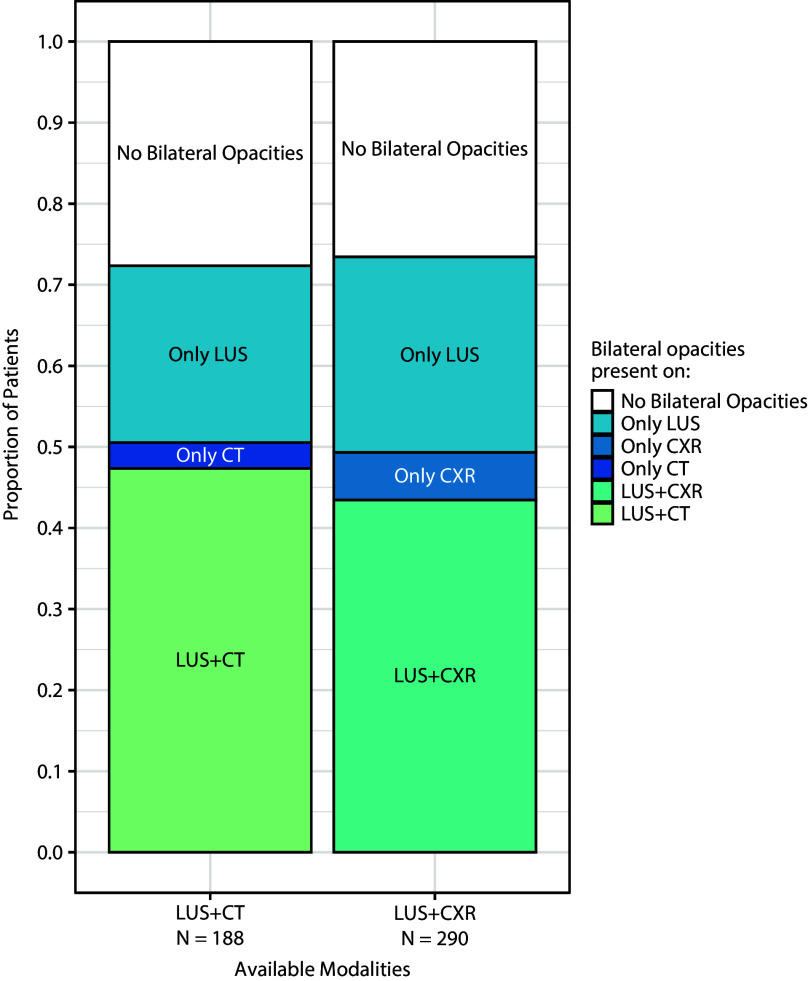
The CXR has been found to be an unreliable tool for the assessment of bilateral edema to diagnose ARDS, with high interrater variability resulting in wildly variable diagnostic accuracies between readers that only improve marginally with training (7). LUS has been adopted as a bedside, radiation-free tool by many clinicians worldwide and is used in the diagnostic approach of respiratory failure because of high sensitivity and specificity for pneumothorax, pulmonary edema, and pneumonia (8, 9). Operators can be trained rapidly and reliably. However, the exact diagnostic criteria for ARDS are underdeveloped. The proposed criteria rely primarily on bilateral B-lines or consolidations, which are known to be very sensitive but quite nonspecific (10). In fact, in a dataset recently published in this journal (11), such criteria would result in a 20% increase in the prevalence of ARDS, irrespective of the reference method (Figure 1). Additional work is needed to clarify how pleural line abnormalities can be incorporated into the diagnosis of ARDS, for example via data-driven methods, as was recently done in the development and validation of the LUS-ARDS score (11).
Figure 1.
Lung ultrasound (LUS) would overdiagnose acute respiratory distress syndrome based on the proposed criteria in an intubated patient with PaO2/FiO2 < 300 mm Hg. CT = computed tomography; CXR = chest X-ray.
How Will the Newly Proposed Definition Influence Epidemiological Research?
The proposed global definition for ARDS will allow epidemiological studies to have a global reach and thus teach us more about the underlying risk factors, disease course, and outcomes of patients fulfilling the criteria. One of the potential pitfalls of the broadening of the definition according to the new global definition may be that many more patients with acute respiratory failure will fulfill the definition of ARDS, especially in resource-limited settings. For example, some patients breathing spontaneously with hypoxemia from atelectasis may be labeled as having ARDS, whereas hypoxemia would be reversed with positive pressure ventilation. The many important uncertainties surrounding the epidemiological consequences of the proposed broadening of the criteria for ARDS should be the focus of future research, which may lead to further refinement.
How Will the Global Definition Shape Intervention Trials?
The recognition of the category of nonintubated patients with ARDS will facilitate earlier inclusion of patients into intervention trials. Based on preclinical data and the experience with coronavirus disease (COVID-19), this may allow for more beneficial effects of pharmacological interventions. Simultaneously, the included population may become even more heterogeneous. Thus, such a broadened definition should be accompanied by a form of phenotyping within trials to reduce clinical, physiological, or biological heterogeneity. Indeed, inclusion of patients with respiratory failure because of a single pathogen was part of the recipe for success in COVID-19 trials. For nonpharmacological interventions such as ventilation strategies and extracorporeal support, the global definition will likely have fewer consequences, as these interventions are typically linked to the type of respiratory support.
Is This the End of the Berlin Definition for ARDS?
Rather than a new definition, the global definition is an extension of Berlin. The intubated category retains the PaO2/FiO2 severity cutoffs described before but allows the use of SpO2/FiO2 when no arterial blood gas measurement is available. It adds two new categories, nonintubated ARDS and ARDS in resource-limited settings, that would otherwise not be classified as ARDS. Because the global definition is not formally endorsed by any of the scientific societies, it should not replace Berlin. Yet, it would also be detrimental to work with multiple ARDS definitions. Therefore, to ensure comparability, we strongly encourage that authors keep reporting effect estimates for patients fulfilling Berlin criteria, even when a broader population is included. A formal redefinition is very much needed and will benefit from the proposed global definition and the research that will follow.
To conclude, the proposed global definition of ARDS extends the criteria formulated in the Berlin definition and will broaden the population on a global scale. There are important uncertainties surrounding the epidemiological consequences of these changes, which require close inspection and further research. Formal reformulation of the ARDS definition through scientific societies will need to follow.
Footnotes
Supported by Amsterdam University Medical Centers AUMC fellowship (L.D.J.B.) and Lung Foundation Netherlands grant Health Holland PPP.
Originally Published in Press as DOI: 10.1164/rccm.202308-1369ED on September 7, 2023
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Matthay MA, Arabi Y, Arroliga AC, Bernard G, Bersten AD, Brochard LJ, et al. A new global definition of acute respiratory distress syndrome. Am J Respir Crit Care Med . 2024;209:37–47. doi: 10.1164/rccm.202303-0558WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ranieri VM, Tonetti T, Navalesi P, Nava S, Antonelli M, Pesenti A, et al. High-flow nasal oxygen for severe hypoxemia: oxygenation response and outcome in patients with COVID-19. Am J Respir Crit Care Med . 2022;205:431–439. doi: 10.1164/rccm.202109-2163OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults Lancet 1967. 2 319 323 4143721 [Google Scholar]
- 4. Villar J, Blanco J, del Campo R, Andaluz-Ojeda D, Díaz-Domínguez FJ, Muriel A, et al. Spanish Initiative for Epidemiology, Stratification & Therapies for ARDS (SIESTA) Network Assessment of PaO2/FiO2 for stratification of patients with moderate and severe acute respiratory distress syndrome. BMJ Open . 2015;5:e006812. doi: 10.1136/bmjopen-2014-006812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sjoding MW, Dickson RP, Iwashyna TJ, Gay SE, Valley TS. Racial bias in pulse oximetry measurement. N Engl J Med . 2020;383:2477–2478. doi: 10.1056/NEJMc2029240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wong AI, Charpignon M, Kim H, Josef C, de Hond AAH, Fojas JJ, et al. Analysis of discrepancies between pulse oximetry and arterial oxygen saturation measurements by race and ethnicity and association with organ dysfunction and mortality. JAMA Netw Open . 2021;4:e2131674. doi: 10.1001/jamanetworkopen.2021.31674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peng J-M, Qian C-Y, Yu X-Y, Zhao M-Y, Li S-S, Ma X-C, et al. China Critical Care Clinical Trial Group (CCCCTG) Does training improve diagnostic accuracy and inter-rater agreement in applying the Berlin radiographic definition of acute respiratory distress syndrome? A multicenter prospective study. Crit Care . 2017;21:12. doi: 10.1186/s13054-017-1606-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Winkler MH, Touw HR, van de Ven PM, Twisk J, Tuinman PR. Diagnostic accuracy of chest radiograph, and when concomitantly studied lung ultrasound, in critically ill patients with respiratory symptoms: a systematic review and meta-analysis. Crit Care Med . 2018;46:e707–e714. doi: 10.1097/CCM.0000000000003129. [DOI] [PubMed] [Google Scholar]
- 9. Yuan X, Liu L, Chang W, Wu Z, Huang L, Chao Y, et al. Diagnosis accuracy of lung ultrasound for ARF in critically ill patients: a systematic review and meta-analysis. Front Med (Lausanne) . 2021;8:705960. doi: 10.3389/fmed.2021.705960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vercesi V, Pisani L, van Tongeren PSI, Lagrand WK, Leopold SJ, Huson MMA, et al. Lung Ultrasound Consortium External confirmation and exploration of the Kigali modification for diagnosing moderate or severe ARDS. Intensive Care Med . 2018;44:523–524. doi: 10.1007/s00134-018-5048-5. [DOI] [PubMed] [Google Scholar]
- 11. Smit MR, Hagens LA, Heijnen NFL, Pisani L, Cherpanath TGV, Dongelmans DA, et al. DARTS Consortium members Lung ultrasound prediction model for acute respiratory distress syndrome: a multicenter prospective observational study. Am J Respir Crit Care Med . 2023;207:1591–1601. doi: 10.1164/rccm.202210-1882OC. [DOI] [PMC free article] [PubMed] [Google Scholar]