Abstract
Background:
Motor learning involves both explicit and implicit learning processes that are fundamental to post-stroke rehabilitation as they are often utilized in concert. However, stroke may damage the neural substrates underlying explicit or implicit learning, leading to deficits in overall motor performance.
Objective:
Determine if individuals with chronic stroke have impaired explicit and/or implicit learning, when assessed during a locomotor task that elicits dissociable contributions from both.
Methods:
We compared explicit and implicit locomotor learning in individuals with chronic stroke to age- and sex-matched neurologically intact controls. We assessed implicit learning using split-belt adaptation (where two treadmill belts move at different speeds). We assessed explicit learning by providing visual feedback during split-belt walking to help individuals explicitly correct for step length errors created by the split-belts. The removal of visual feedback after the first 40 strides of split-belt walking, combined with task instructions, minimized contributions from explicit learning for the remainder of the task. This manipulation, combined with computational modeling, allowed us to determine the individual contributions of explicit and implicit motor learning to overall performance.
Results:
The behavioral and computational analyses revealed that, compared to controls, individuals with chronic stroke demonstrated deficits in both explicit and implicit contributions to locomotor learning.
Conclusions:
Post-stroke locomotor rehabilitation involves interventions that rely on explicit and implicit motor learning. Our results demonstrate that both forms of learning are impaired when examined in a single task. Future work should determine how locomotor rehabilitation interventions can be structured to optimize overall motor learning.
Introduction
Motor learning, the ability to acquire and maintain motor skills with practice,1 involves both explicit and implicit processes. Explicit learning is critical for skill acquisition because it provides the means for fast, flexible changes in movements.2–4 Implicit processes keep movements finely calibrated in the face of changes to the body or environment.3–6 Normally, both processes work together within a motor task to help humans acquire and maintain motor skills.7 However, stroke may damage the neural substrates underlying explicit or implicit learning, leading to deficits in overall motor performance. Since motor learning is foundational to rehabilitation of individuals post-stroke, it is important to determine if they have impairments in one or both processes.
Explicit learning (sometimes called voluntary correction7 or cognitive strategies8) refers to consciously directing specific changes in movement patterns. For example, a patient may consciously increase their step length in response to a clinician’s verbal instructions. Explicit learning plays a critical role in skill acquisition and motor memory for neurologically intact individuals, and is mediated primarily in prefrontal cortex.5,9–11 We assume this process is driven by target error, the difference between a movement outcome and the task goal.6,12,13 Explicit learning can be used during gait in both neurologically intact individuals and those post-stroke by providing visual feedback and specific task instructions.14–16 A key feature of this process is that it can be volitionally “switched” on or off in response to context or instructions.3,13,17,18
Sensorimotor adaptation is an implicit motor learning process that is essential for maintaining well-calibrated movements in response to ever-changing environments and body states. Sensorimotor adaptation, which we refer to here as “implicit adaptation”, is driven by sensory prediction error, the difference between the actual and expected sensory consequences of a motor command, and mediated in large part by the cerebellum.19–23 During gait, implicit adaptation can be elicited using a split-belt treadmill where the belts under each limb move at different speeds.24 This perturbation initially produces asymmetric gait patterns (e.g., step length asymmetries) which are slowly recalibrated back to baseline asymmetry levels.25,26 The hallmark of implicit adaptation is the storage of the adapted stepping pattern when the belts return to the same speed, termed an “implicit aftereffect”.26 When tested in isolation during locomotion, individuals with non-cerebellar stroke adapt to a similar magnitude as neurologically intact participants by the end of learning, but they do so at a slower rate.27–30
While explicit learning and implicit adaptation are typically used simultaneously to learn new skills in everyday life, including rehabilitation practice, they are mostly studied individually during gait.13,14,17,18,26 This may be because when they are studied within the same task, it can be difficult to dissociate the individual contributions of each process to overall behavior.7,31–33 However, a study in young neurotypical adults accomplished this using visual feedback to induce explicit learning that helped correct the step length errors produced by the split-belt treadmill7. They found explicit learning improved performance during split-belt walking compared to a group that did not receive feedback. However, the implicit aftereffects (measured without visual feedback) were similar between groups, indicating explicit learning did not impact the recalibration of motor commands (i.e., implicit adaptation). Thus, the authors concluded that, within the same locomotor learning task, while explicit learning improves overall performance, implicit adaptation proceeds despite involvement from explicit learning in individuals with intact neurologic systems. Critically, it is unclear to what degree explicit learning versus implicit adaptation is impaired in individuals post-stroke when assessed in a task requiring dissociable contributions from both.
Only two studies, both in reaching movements, have attempted to tackle this question, but with mixed results.11,34 To date, no studies have assessed these two processes in the same locomotor task in individuals post-stroke. This is critical because gait rehabilitation post-stroke involves a combination of explicit learning and implicit adaptation (e.g., a patient may explicitly try to increase step length based on their therapist’s instructions while simultaneously implicitly adapting to small movement-related errors). Understanding how each is impaired, when occurring together in the same task, has important implications for how rehabilitation of locomotor tasks should be optimally structured.
The purpose of this study was to determine if individuals with chronic, hemiparetic stroke demonstrate impaired explicit learning and/or implicit adaptation during a locomotor task involving dissociable contributions from both processes. We accomplished this through a combination of behavioral testing and computational modeling. Since explicit learning involves cognitive processes9,11 that are often impaired in stroke,35 we hypothesized that individuals with stroke would demonstrate impaired explicit learning compared to controls. Additionally, because the rate of implicit adaptation on the split-belt treadmill is slow but the magnitude is intact in persons post-stroke27–29 we hypothesized that individuals with stroke would demonstrate similar levels of implicit adaptation as controls.
Materials and methods
Participants
We recruited 21 (10 Female) individuals with one prior unilateral, stroke to participate in this study and 18 (9 Female) healthy age- and sex-matched control participants. Individuals with stroke were included if they were between 18 and 85 years old, had a single unilateral hemiparetic stroke (confirmed by an MRI or CT scan) more than 6 months prior, and were able to walk without assistance from another person. Individuals with stroke were excluded if they had evidence of cerebellar stroke, other neurologic diagnoses aside from stroke, inability to walk outside of the home prior to stroke, pain limiting walking, neglect, or significant aphasia. Control participants were excluded if they had any conditions that might limit their walking or motor learning, any neurologic conditions, or uncorrected vision or hearing loss. All individuals provided written informed consent prior to participating and the study was approved by the University of Delaware Institutional Review Board (IRB #1139080).
Experimental design
To determine if individuals with stroke have impaired explicit learning or implicit adaptation during a locomotor learning task that requires contributions from both processes, we combined the split-belt adaptation paradigm with real-time visual feedback, similar to a previous study (Figure 1A).7 Participants performed 4 phases of treadmill walking: Baseline, Practice, Adaptation, and De-adaptation (Figure 1B). During the Baseline and Practice, both the treadmill belts moved at the same speed. During the Baseline phase, no visual feedback was provided on the screen and individuals were told to “walk comfortably”. The Practice phase served to introduce participants to the visual feedback (details below). Step length targets first appeared at each participant’s baseline step length for 90 seconds, at which point, they were verbally oriented to the feedback and instructed to practice changing their step lengths by stepping both above and below the targets. For the next 30 seconds, the step length targets shifted 10 cm longer for the limb taking the longer baseline step and 10 cm shorter for the limb taking the shorter baseline step. This allowed participants to practice hitting targets that were not their baseline step lengths. The targets shifted back to the baseline step lengths for the final 60 seconds of the Practice phase and individuals were asked to “walk comfortably”.
Figure 1. Experimental Design.
(A) Individuals walked on a split-belt treadmill with a vertically mounted television screen in front of them. The visual feedback was a grid of 12 different step lengths, each 10 cm in height. The step length feedback was represented on the screen as blue (left) and red (right) feet that appeared on the screen as soon as heel strike was detected and disappeared once toe off was detected. (B) All participants completed 4 walking phases: 1) A Baseline (Bsl) phase of normal walking where no feedback was on the screen; 2) A Practice phase where individuals were introduced to the visual feedback while walking (purple shading); 3) An Adaptation phase where the slow belt (dotted black line) moved at half the speed of the fast belt (solid black line), with feedback activated during only the first 40 strides (purple shading); 4) A De-adaptation phase where the belts returned to the same speed. The length of each phase (in minutes) is displayed in the grey shading at the bottom of the figure.
During the Adaptation phase (8 minutes), the fast belt speed was set at the fastest overground gait speed (constrained between 0.6 and 1.0 m/s), and the slow belt moved at half the speed of the fast belt, producing a 2:1 speed ratio.29,37 For all participants, the limb that took the longer step during the Baseline phase was placed on the fast belt. This perturbation produces a large asymmetry of the left and right step lengths (defined as the distance between two feet at heel strike), and is corrected on a stride-by-stride basis through implicit adaptation.26,27,37 Lastly, participants performed a De-adaptation phase (8 minutes) where they were instructed to “walk comfortably”, and both belts moved at the same speed as the Baseline phase (i.e., the slow belt speed) so that we could measure the size of the implicit aftereffect, our measure of the total magnitude of implicit adaptation.
To assess explicit learning, we provided visual feedback of the left and right step lengths during the first 40 strides of the Adaptation phase. The real-time visual feedback was displayed on a vertically orientated LCD television screen placed 100 cm in front of the treadmill (Figure 1A; Size: 123.3 × 71.1 cm; Sony Tokyo, Japan). The Motion Monitor software (Innovative Sports Training Inc., Chicago, IL, USA) was used to display the visual feedback during the experiment. The feedback consisted of a target grid of 12 possible step lengths, each 10 cm in height. This grid had a 1:1 correspondence with the actual step length. The left and right step length feedback was displayed as a red and blue foot, respectively. Each foot was presented in the center of the row corresponding to that step length window, and appeared as soon as heel strike was detected, then disappeared once the subsequent swing phase began. The target right and left step lengths during the Adaptation phase were set at each participant’s left and right baseline step lengths, denoted by highlighting the corresponding row of the grid. Participants were instructed to “hit the targets” when the feedback was visible. Therefore, because the targets were set at baseline step length, the feedback guided participants to voluntarily correct the step length asymmetry induced by the split-belt treadmill via explicit learning.
The key manipulation that allowed us to assess the magnitude of explicit learning was to turn off the feedback after the first 40 strides of Adaptation and instruct participants to “walk comfortably”. This should “turn off” any explicit learning they were using while the visual feedback was on, leaving only implicit adaptation. Thus, the difference between the step length behavior when the feedback was on and when it was first turned off represents the magnitude of explicit learning.7
Data collection and analysis
Kinetic and kinematic data were collected using the split-belt treadmill force plates and motion capture cameras, respectively (see supplemental material for full details). Step lengths, calculated in real-time using the Motion Monitor, was defined as the anterior-posterior distance between the two ankle markers at heel strike. We calculated step length asymmetry, and normalized to each participant’s perturbation size to measure Adaptation Index on each stride (s)7,37,38:
| (1a) |
| (1b) |
| (1c) |
The min and max step length asymmetries used to determine the perturbation in equation 1c were calculated only within the first 10 strides of each respective phase.37 Thus, during the Adaptation phase, an Adaptation Index of 0 represents the minimum step length asymmetry (i.e., the max perturbation), and 1 indicates the perturbation has been fully corrected. The reverse is true during the De-adaptation phase.
To test our hypotheses, we averaged Adaptation Index during 4 key timepoints of interest: 1) Feedback On: the final five strides of the feedback being on during Adaptation, 2) Feedback Off: the five strides immediately after the feedback was turned off during Adaptation, 3) End Adaptation: the last five strides of Adaptation, and 4) Implicit Aftereffect: the first five strides of De-adaptation. Our hypothesis for explicit learning was tested by comparing Feedback On (implicit adaptation plus explicit learning), to Feedback Off (implicit adaptation only). Thus, larger differences between Feedback On and Feedback Off indicate greater explicit learning. We assessed the interaction between group (stroke vs control) and time (Feedback On vs Feedback Off) as our primary behavioral measure testing for impaired explicit learning in the stroke group. A secondary behavioral measure of explicit learning was between group differences during Feedback On, as this reflected the ability of individuals to use the visual feedback during implicit adaptation. Our primary behavioral measure to test for implicit adaptation impairments was comparing the Implicit Aftereffect between groups.22,26 A secondary behavioral measure of implicit adaptation was a between groups comparison at End Adaptation.
Computational modeling
We also used a computational model to characterize explicit learning and implicit adaptation. With this approach, we can map the underlying learning processes onto the data. Specifically, we fit the model to individual data to obtain a unique set of parameter values for each participant. Since these parameters represent specific aspects of explicit and implicit learning, we can make inferences regarding the function of these underlying learning components.7,37,38 Then, we compared the individual learning processes (i.e., model parameters) between the stroke and control groups.
This “voluntary correction” model was previously used to capture explicit and implicit learning in this paradigm,7 and the implicit adaptation component of the model can successfully capture split-belt adaptation behavior in individuals with stroke.37 The computational modeling used here followed that of Roemmich et al.,7 which defines the Adaptation Index (x) on each stride (s) as the sum of both explicit learning (xeplicit) and implicit adaptation (ximplicit):
| (2) |
Both processes correct for the same error , where the perturbation = 1 during Adaptation and 0 during De-adaptation. Explicit learning is only active when the feedback is on:
| (3) |
The free parameter, Bexplicit, represents the learning rate for explicit learning as it is the proportion of error that is explicitly corrected from one stride to the next (i.e., higher values indicate faster learning). The implicit adaptation process has dual components, fast and slow, and is active throughout the Adaptation and De-adaptation phases7,39:
| (4a) |
| (4b) |
| (4c) |
Implicit learning has four free parameters. The learning rates, Bfast and Bslow, represent the proportion of the error that is implicitly corrected from one stride to the next, and the retention rates, Afast and Aslow, represent the proportion of the current adapted state that is retained. The fast process quickly learns from errors, but also quickly forgets, while the slow process takes longer to learn from errors but retains longer.39
We fit the model to each participant’s Adaptation Index data during the Adaptation and De-adaptation phases using MATLAB’s fmincon function, setting the objective function as the sum of squared errors between the model output (x) and the data. We calculated model fits (r2) by resampling the data with replacement 1000 times for each group and fitting the model to these bootstrapped samples.37 We report the mean and 95% confidence intervals of the bootstrapped r2 values. Additionally, to ensure that the five-parameter, voluntary correction model did not overfit the data, we also fit two additional models, both of which do not included an explicit component39,40 (see supplemental methods for details), and performed model selection using Akaike Information Criterion (AIC).
Statistical analysis
We utilized the bayes-toolbox Python package41 for performing Bayesian inference for all hypotheses. This allowed us to report the full range of credible differences between the groups along with the probability of a difference, given our data. We provide details in supplemental material, but briefly, we estimated between (across group) and within (across time) subject effects of the Adaptation Index data. We compared these effects as the posterior distributions of between group differences which are presented as histograms representing the full distribution of possible differences based on the data we collected. For each posterior distribution, we report the mean and 95% high density interval (HDI), defined as the narrowest span of credible values that contain 95% of the distribution.42 The HDI can be interpreted as the true value falling between this range with 95% certainty. We also report the probability of a difference as a percentage of posterior distribution samples on one side of zero (e.g., pdifference = 94.7%).
Data availability
The data that support the findings of this study and code are available at Open Science Framework (https://osf.io/pws2k/).
Results
Of the 21 individuals recruited to participate in the stroke group, we removed 4 from the analysis due to an inability to properly complete the task (n=3) or follow instructions (n=1). Average participant characteristics for each group are displayed in Table 1. In Figure 2, we display the mean, baseline-corrected step length asymmetry data during the Adaptation and De-adaptation phases for both groups. For ease of group comparisons, we present our primary analyses using the Adaptation Index. We note that similar results were obtained when using step length asymmetry index, with no impact on any of our inferences.
Table 1. Group characteristics.
Demographic and clinical characteristics of participants. All continuous variables are represented as mean ± 1 SD. (F = female, M = male, R = right, L = left)
| Stroke Group (n=17) | Control Group (n=18) | |
|---|---|---|
| Age (years) | 64.5 ± 10.2 | 64.8 ± 9.6 |
| Sex | 9M / 8F | 9M / 9F |
| Time since stroke (months) | 71.0 ± 49.1 | |
| Side of brain lesion | 7R/10L | |
| Self-selected (overground) walking speed (m/s) | 0.92 ± 0.27 | 1.33 ± 0.28 |
| Fastest (overground) walking speed | 1.29 ± 0.38 | 1.81 ± 0.22 |
| Fast treadmill belt speed | 0.94 ± 0.12 | 1.00 ± 0 |
| Lower Extremity Fugl Meyer | 25.41 ± 6.27 |
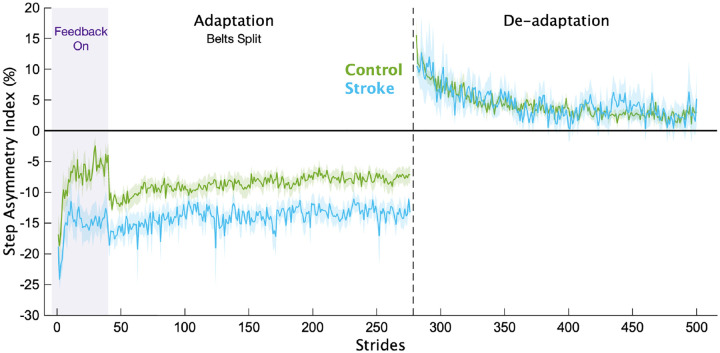
Figure 2. Step length asymmetry.
Mean baseline-corrected step length asymmetry for each group for the Adaptation and De-adaptation phases. Purple shading is the time when the feedback was on. The vertical dashed line separates the Adaptation and De-adaptation phases. Each phase was truncated to the participant with the shortest phase for visualization purposes. Shading represents ±1 SEM.
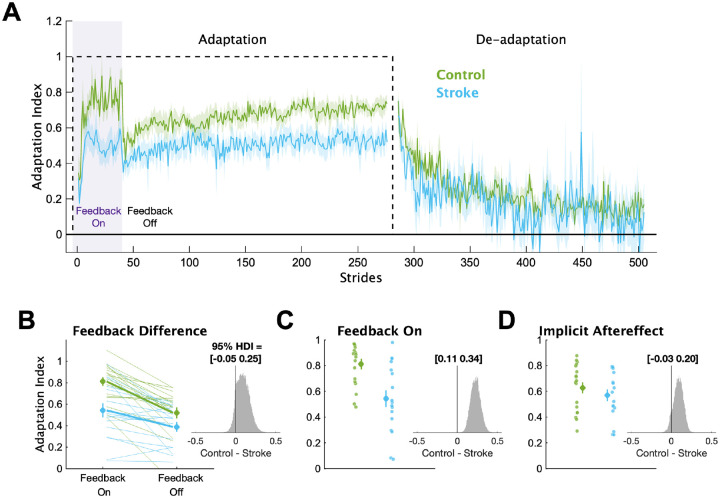
In Figure 3, we display the mean Adaptation Index data and key timepoints of interest for each group. First, we determined if individuals with stroke had impairments in explicit learning (Figure 3B). Based on our instructions and previous work,7 we assumed participants used explicit learning only while the feedback was on during the Adaptation phase. Therefore, explicit learning magnitude was characterized as the difference in Adaptation Index between Feedback On and Feedback Off. This difference was larger for the control group (mean interaction effect [95% HDI] = 0.09 [−0.05 0.25], pdifference = 88.7%), providing evidence that the individuals with stroke had diminished explicit learning compared to controls. Additionally, individuals in the stroke group were less able to use the visual feedback during Adaptation compared to controls (Figure 3C), with much lower Adaptation Index values during Feedback On (mean group difference = 0.23 [0.11 0.34], pdifference = 100.0%). Combined, these results point to impairments in explicit learning in individuals with stroke compared to controls.
Figure 3. Adaptation Index.
(A) Group averaged Adaptation Index data for the Adaptation and De-adaptation phases. The dashed line represents the walking period when the belts were split (i.e., the perturbation). Purple shading represents the time when the feedback was turned on. For visualization purposes, data for each phase were truncated to the individual with least number of strides. Solid lines represent group means, shading represents ±1 SEM. (B) Group and individual data for the Feedback On and Feedback Off timepoints. Thick lines represent the group average slopes. (C) Group and individual data for the Feedback On timepoint. (D) Group and individual data for the Implicit Aftereffect timepoint. For panels B-D, large circles and error bars represent the group means ±1 SEM and smaller dots represent individuals. The insets display a histogram of the posterior distribution for the between group differences. The black vertical line in the histogram is there to aid visualization of the credibility of a between group difference (i.e., how much of the posterior probability distribution is on one side of zero). We report the 95% HDI regarding the range of credible effect sizes above the insets of the posterior distributions.
Next, we determined if individuals with stroke had impaired implicit adaptation by comparing the size of the implicit aftereffect (Figure 3D). The control group demonstrated larger implicit aftereffects compared to the stroke group (group difference = 0.09 [−0.03 0.20], pdifference = 91.4%), providing evidence that individuals with stroke have impaired implicit adaptation compared to controls. Additionally, we found large and reliable differences between the groups at End Adaptation (group difference = 0.17 [0.06 0.28], pdifference = 99.9%). Overall, the behavioral results indicate that impairments may exist in both explicit learning and implicit adaptation.
To shed light on these behavioral results, we applied a series of computational models to the data. The voluntary correction model, specifically, allowed us to map each individual’s behavior to explicit learning and implicit adaptation processes (Figure 4). This model fit the bootstrapped data well, with mean r2 values of 0.71 and 0.90 for the stroke and control groups, respectively. Critically, we also confirmed that the voluntary correction model had better (lower) AICs than both the single rate model (AIC difference mean [95% HDI] = 196 [154 237], pdifference = 100.0%) and the dual rate model (AIC difference = 64 [24 107]; pdifference = 99.8%), indicating that the voluntary correction model accurately characterizes learning on this task without overfitting. As the single- and dual-rate state-space models do not include a voluntary correction process, these results also support our assumption that explicit learning contributed to behavioral change specifically when visual feedback was on.
Figure 4. Computational model results.
Mean model fits to bootstrapped samples plotted against the empirical data for the (A) stroke group and (B) control group. See supplemental Figures 1 and 2 for the model fits for each individual participant. Purple shading represents the time when the feedback was turned on. For visualization purposes, data for each phase were truncated to the individual with least number of strides. Shading represents ±1 SEM (C-G) Model parameter values for each group. Large circles and error bars represent the group means ±1 SEM and smaller dots represent individuals. The insets are histograms of the posterior of the between groups difference (contrast) in parameter values. We report the 95% HDI regarding the range of credible effect sizes above the insets of the posterior distributions. Note the scale of the x-axis varies for these inset plots.
Comparing the individual parameters from the voluntary correction model allowed us to determine the specific components of learning that were impaired. The learning rate parameter for the explicit learning, Bexplicit, served as a measure of each individual’s explicit learning ability, with higher values indicating faster explicit learning (Figure 4C). The stroke group had much smaller Bexplicit values compared to the control group (group difference = 0.24 [0.06 0.41], pdifference = 99.5%), providing strong support for the hypothesis that explicit learning is impaired in individuals with stroke compared to controls. Next, we examined the four implicit adaptation process parameters (Figure 4F–G). While there was evidence of differences between groups for most parameters, the magnitude of differences for three of the four were near zero (group differences: Aslow = 0.00 [−0.00 0.01], pdifference = 90.0%; Bslow = 0.00 [−0.00 0.00], pdifference = 52.8%, Bfast = 0.01 [−0.01 0.03], pdifference = 76.6%). In contrast, there was a marked difference in the retention rate for the fast state (Afast group difference = 0.15 [−0.02 0.36], pdifference = 96.9%). Thus, it appears that individuals with stroke, as a group, have a specific impairment in their ability to retain what was learned by the fast implicit adaptation process. In sum, the results of our computational modeling provided strong support for the hypothesis that explicit learning is impaired post-stroke and revealed that the retention rate for the fast state could underlie slower implicit adaptation in stroke.
Discussion
In the current study, we examined explicit learning and implicit adaptation within the same locomotor learning task in individuals with chronic, hemiparetic stroke. We combined a behavioral manipulation and computational modeling to determine the presence, and potential degree, of impairment in both learning processes. The majority of work in motor learning and stroke has primarily studied implicit adaptation,27–29,37,43–46 with less attention paid to explicit learning.11,15,16,34 While some studies have examined both processes in the same task,33,47–50 few attempts have been made to discern their individual contributions to overall motor learning.11,34 To our knowledge, the current study is the first to assess explicit and implicit motor learning within the same task in individuals with chronic stroke using both behavioral manipulations and computational modeling. Our results provide strong evidence that stroke impairs explicit learning and the rate of implicit adaptation during a locomotor task that elicits dissociable contributions from both processes. This has important implications for the design of locomotor learning tasks in post-stroke rehabilitation because many interventions involve both implicit and explicit motor learning.
Explicit learning is impaired in chronic stroke
We found that individuals with chronic, hemiparetic stroke have impairments in explicit learning in a locomotor learning task involving both explicit learning and implicit adaptation. Individuals with stroke had a smaller change in behavior compared to controls after the visual feedback, intended to drive and support explicit learning, was removed. Additionally, the computational modeling revealed significantly slower explicit learning in individuals with stroke.
This finding aligns with a previous study showing that individuals with lateral prefrontal cortex (LPFC) lesions demonstrate impairments in explicit learning.11 In this reaching study, the authors dissociated explicit learning and implicit adaptation using specific task instructions and found the group with LPFC lesions had worse explicit learning compared to controls. This and other work raises the possibility that cognitive processes such as working memory or general cognition in reaching studies,34,51–53 and fluid cognition in gait studies16 contribute to explicit motor learning, but more work is required to determine the specific contribution of cognition to explicit learning in stroke.
Contrary to the current findings, prior work in reaching34 and gait15,16 observed no differences in explicit learning in individuals with stroke compared to controls. However, the studies in gait did not use a split-belt perturbation in addition to visual feedback, likely making the task easier, which could reduce the ability to detect explicit learning deficits in stroke. The reaching study dissociated explicit learning and implicit adaptation using visual cues (the color and shape of a cursor). It is possible that either this manner of distinguishing between explicit and implicit processes or the broader inclusion criteria for their stroke group can account for the differences between their findings and those of the current study. Similar to Taylor and Ivry,11 we provided clear instructions and removed all visual feedback to ensure explicit learning was “switched off”, and provided a narrower range of inclusion criteria, potentially explaining why our results were more consistent with theirs. Still, it is critical to determine if the manner of eliciting explicit learning (a specific type of cue or instruction) impacts the ability to use this process in stroke given its ubiquity in rehabilitation settings.
Slower implicit adaptation in stroke is due to worse retention of the fast process
Contrary to our hypothesis, we found evidence that implicit adaptation is impaired after stroke. The stroke group demonstrated smaller implicit aftereffects and a lower plateau at the end of the Adaptation phase indicating a smaller overall magnitude of implicit adaptation. Prior studies in locomotor adaptation after stroke indicate that the overall magnitude of implicit adaptation is similar to controls, but the rate is slower.27–30 While these studies may seem to conflict with the current findings, it is possible that the relatively short Adaptation phase in the current study (8 minutes compared to 10–15 minutes in the prior studies) prevented us from observing asymptotic adaptation.
Another possibility is that the visual feedback interfered with implicit adaptation for the stroke group. However, prior work in young individuals with intact neurologic systems demonstrate that visual feedback used to either help or hinder performance during split-belt walking does not change the total magnitude of implicit adaptation.7,31,32 Additionally, individuals with stroke can successfully adapt to the split-belt treadmill while also explicitly learning to change a separate gait parameter (knee flexion angle) using visual feedback.33 Therefore, it is unlikely that explicit learning itself hindered implicit adaptation in the current study since implicit adaptation proceeds in spite of explicit learning across reaching and walking paradigms,6,7 including in stroke.11,33,34 However, it may be possible that any cognitive task could interfere with implicit adaptation in stroke (i.e., a dual task effect). Even neurologically intact individuals demonstrate slower adaptation of certain gait parameters when engaged in a separate cognitive task,32 but more work is needed to determine if this is the case in stroke.
The computational modeling utilized in this study provides insight into why the learning rate of implicit adaptation was impaired in stroke in this task. The voluntary correction model incorporates a dual-rate model of adaptation which frames implicit adaptation as the combination of a fast state and a slow state.39 These states represent updates to an internal model, a prediction of the sensory consequences of movement, that could occur either in the cerebellum or motor cortex.39 One theory suggests that the motor cortex is responsible for retention of the adapted state while the cerebellum is responsible for learning.54,55 Thus, damage to motor cortices could explain poor retention of the fast process in individuals with stroke. Alternatively, the fast process has been closely linked to explicit learning during visuomotor rotation tasks.5,11 However, to date there is no evidence of contributions from explicit learning to standard split-belt adaptation (i.e., without additional visual feedback).7,37,38 Another possibility is that the fast state represents a reactive balance element that is sensitive to environmental changes.56 Future studies are required to dissociate between these potential explanations.
Conclusion
Motor learning involves multiple processes, both explicit and implicit, that work together to improve overall task performance. We found that individuals with chronic stroke have impairments in explicit learning and implicit adaptation during a locomotor task that elicits dissociable contributions from both. These findings are important because of the potential application to post-stroke rehabilitation, which often combines different forms of learning in a single task. To improve outcomes, future work should determine how locomotor rehabilitation interventions can be structured to target these deficits and optimize overall motor learning.
Supplementary Material
Acknowledgements
We would like to thank Saunders Penn for helping to create Figure 1A.
Funding Acknowledgements
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health [NIH 2R01HD078330-05A1] (DSR).
Funding Statement
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health [NIH 2R01HD078330-05A1] (DSR).
Footnotes
Declaration of Conflicting Interests
The Authors declare that there is no conflict of interest.
Supplementary material
Supplementary material is available online.
References
- 1.Schmidt RA, Lee TD. Motor control and learning: A behavioral emphasis, 4th ed. Champaign, IL, US: Human Kinetics; 2005:vi, 535. [Google Scholar]
- 2.Huberdeau DM, Krakauer JW, Haith AM. Practice induces a qualitative change in the memory representation for visuomotor learning. J. Neurophysiol. 2019;122:1050–1059. [DOI] [PubMed] [Google Scholar]
- 3.Bond KM, Taylor JA. Flexible explicit but rigid implicit learning in a visuomotor adaptation task. J. Neurophysiol. 2015;113:3836–3849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roemmich RT, Bastian AJ. Closing the Loop: From Motor Neuroscience to Neurorehabilitation. Annu. Rev. Neurosci. 2018;41:415–429. [DOI] [PubMed] [Google Scholar]
- 5.Krakauer JW, Hadjiosif AM, Xu J, Wong AL, Haith AM. Motor Learning. In: Comprehensive Physiology. American Cancer Society; 2019:613–663. [DOI] [PubMed] [Google Scholar]
- 6.Mazzoni P, Krakauer JW. An implicit plan overrides an explicit strategy during visuomotor adaptation. J. Neurosci. 2006;26:3642–3645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roemmich RT, Long AW, Bastian AJ. Seeing the Errors You Feel Enhances Locomotor Performance but Not Learning. Curr. Biol. 2016;26:2707–2716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor JA, Ivry RB. Flexible cognitive strategies during motor learning. Diedrichsen J, ed. PLoS Comput. Biol. 2011;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDougle SD, Ivry RB, Taylor JA. Taking Aim at the Cognitive Side of Learning in Sensorimotor Adaptation Tasks. Trends Cogn. Sci. 2016;20:535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haith AM, Huberdeau DM, Krakauer JW. The Influence of Movement Preparation Time on the Expression of Visuomotor Learning and Savings. J. Neurosci. 2015;35:5109–5117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor JA, Ivry RB. Cerebellar and prefrontal cortex contributions to adaptation, strategies, and reinforcement learning. Prog. Brain Res. 2014;210:217–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor JA, Ivry RB. The role of strategies in motor learning. Ann. N. Y. Acad. Sci. 2012;1251:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.French MA, Morton SM, Charalambous CC, Reisman DS. A locomotor learning paradigm using distorted visual feedback elicits strategic learning. J. Neurophysiol. 2018;120:1923–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hussain SJ, Hanson AS, Tseng S-C, Morton SM. A locomotor adaptation including explicit knowledge and removal of postadaptation errors induces complete 24-hour retention. J. Neurophysiol. 2013;110:916–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.French MA, Morton SM, Reisman DS. Use of explicit processes during a visually guided locomotor learning task predicts 24-h retention after stroke. J. Neurophysiol. 2021;125:211–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.French MA, Cohen ML, Pohlig RT, Reisman DS. Fluid Cognitive Abilities Are Important for Learning and Retention of a New, Explicitly Learned Walking Pattern in Individuals After Stroke. Neurorehabil. Neural Repair. 2021;35:419–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wood JM, Kim HE, French MA, Reisman DS, Morton SM. Use-dependent plasticity explains aftereffects in visually guided locomotor learning of a novel step length asymmetry. J. Neurophysiol. 2020;124:32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wood JM, Morton SM, Kim HE. The Consistency of Prior Movements Shapes Locomotor Use-Dependent Learning. eNeuro. 2021;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krakauer JW, Pine ZM, Ghilardi M-F, Ghez C. Learning of visuomotor transformations for vectorial planning of reaching trajectories. J. Neurosci. 2000;20:8916–8924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morton SM, Bastian AJ. Cerebellar contributions to locomotor adaptations during splitbelt treadmill walking. J. Neurosci. 2006;26:9107–9116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shadmehr R, Smith MA, Krakauer JW. Error Correction, Sensory Prediction, and Adaptation in Motor Control. Annu. Rev. Neurosci. 2010;33:89–108. [DOI] [PubMed] [Google Scholar]
- 22.Shadmehr R, Mussa-Ivaldi FA. Adaptive representation of dynamics during learning of a motor task. J. Neurosci. 1994;14:3208–3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tseng Y, Diedrichsen J, Krakauer JW, Shadmehr R, Bastian AJ. Sensory prediction errors drive cerebellum-dependent adaptation of reaching. J. Neurophysiol. 2007;98:54–62. [DOI] [PubMed] [Google Scholar]
- 24.Dietz V, Zijlstra W, Duysens J. Human neuronal interlimb coordination during split-belt locomotion. Exp. Brain Res. 1994;101. [DOI] [PubMed] [Google Scholar]
- 25.Malone LA, Bastian AJ, Torres-Oviedo G. How does the motor system correct for errors in time and space during locomotor adaptation? J. Neurophysiol. 2012;108:672–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reisman DS, Block HJ, Bastian AJ. Interlimb coordination during locomotion: what can be adapted and stored? J. Neurophysiol. 2005;94:2403–2415. [DOI] [PubMed] [Google Scholar]
- 27.Reisman DS, Wityk R, Silver K, Bastian AJ. Locomotor adaptation on a split-belt treadmill can improve walking symmetry post-stroke. Brain. 2007;130:1861–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Savin DN, Tseng S-C, Whitall J, Morton SM. Poststroke Hemiparesis Impairs the Rate but not Magnitude of Adaptation of Spatial and Temporal Locomotor Features. Neurorehabil. Neural Repair. 2013;27:24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tyrell CM, Helm E, Reisman DS. Learning the spatial features of a locomotor task is slowed after stroke. J. Neurophysiol. 2014;112:480–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Malone LA, Bastian AJ. Spatial and Temporal Asymmetries in Gait Predict Split-Belt Adaptation Behavior in Stroke. Neurorehabil. Neural Repair. 2014;28:230–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Long AW, Roemmich RT, Bastian AJ. Blocking trial-by-trial error correction does not interfere with motor learning in human walking. J. Neurophysiol. 2016;115:2341–2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Malone LA, Bastian AJ. Thinking about walking: effects of conscious correction versus distraction on locomotor adaptation. J. Neurophysiol. 2010;103:1954–1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cherry-Allen KM, Statton MA, Celnik PA, Bastian AJ. A dual-learning paradigm simultaneously improves multiple features of gait post-stroke. Neurorehabil. Neural Repair. 2018;32:810–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Binyamin-Netser R, Goldhamer N, Avni I, Ressel Zviely A, Shmuelof L. Cognitive Impairments After Stroke Do Not Attenuate Explicit Visuomotor Adaptation in Reaching and Savings With the Unaffected Arm. Neurorehabil. Neural Repair. 2023;37:444–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barker-Collo S, Feigin V. The impact of neuropsychological deficits on functional stroke outcomes. Neuropsychol. Rev. 2006;16:53–64. [DOI] [PubMed] [Google Scholar]
- 36.Collen FM, Wade DT, Bradshaw CM. Mobility after stroke: reliability of measures of impairment and disability. Int. Disabil. Stud. 1990;12:6–9. [DOI] [PubMed] [Google Scholar]
- 37.Charalambous CC, Alcantara CC, French MA, et al. A single exercise bout and locomotor learning after stroke: physiological, behavioural, and computational outcomes: Effect of exercise on locomotor learning in chronic stroke survivors. J. Physiol. 2018;596:1999–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mawase F, Shmuelof L, Bar-Haim S, Karniel A. Savings in locomotor adaptation explained by changes in learning parameters following initial adaptation. J. Neurophysiol. 2014;111:1444–1454. [DOI] [PubMed] [Google Scholar]
- 39.Smith MA, Ghazizadeh A, Shadmehr R. Interacting adaptive processes with different timescales underlie short-term motor learning. Ashe J, ed. PLoS Biol. 2006;4:e179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thoroughman KA, Shadmehr R. Learning of action through adaptive combination of motor primitives. Nature. 2000;407:742–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim HE. bayes-toolbox: A Python package for Bayesian statistics. J. Open Source Softw. 2023;8:5526. [Google Scholar]
- 42.Kruschke J. Doing Bayesian Data Analysis: A Tutorial with R, JAGS, and Stan. Academic Press; 2014. [Google Scholar]
- 43.Betschart M, Lauzière S, Miéville C, McFadyen BJ, Nadeau S. Changes in lower limb muscle activity after walking on a split-belt treadmill in individuals post-stroke. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2017;32:93–100. [DOI] [PubMed] [Google Scholar]
- 44.Quattrocchi G, Greenwood R, Rothwell JC, Galea JM, Bestmann S. Reward and punishment enhance motor adaptation in stroke. J. Neurol. Neurosurg. Psychiatry. 2017;88:730–736. [DOI] [PubMed] [Google Scholar]
- 45.Scheidt RA, Stoeckmann T. Reach Adaptation and Final Position Control Amid Environmental Uncertainty After Stroke. J. Neurophysiol. 2007;97:2824–2836. [DOI] [PubMed] [Google Scholar]
- 46.Takahashi CD, Reinkensmeyer DJ. Hemiparetic stroke impairs anticipatory control of arm movement. Exp. Brain Res. 2003;149:131–140. [DOI] [PubMed] [Google Scholar]
- 47.Day KA, Cherry-Allen KM, Bastian AJ. Individualized feedback to change multiple gait deficits in chronic stroke. J. NeuroEngineering Rehabil. 2019;16:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moore RT, Piitz MA, Singh N, Dukelow SP, Cluff T. Assessing Impairments in Visuomotor Adaptation After Stroke. Neurorehabil. Neural Repair. 2022;36:415–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mutha PK, Sainburg RL, Haaland KY. Left Parietal Regions Are Critical for Adaptive Visuomotor Control. J. Neurosci. 2011;31:6972–6981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schaefer SY, Haaland KY, Sainburg RL. Dissociation of initial trajectory and final position errors during visuomotor adaptation following unilateral stroke. Brain Res. 2009;1298:78–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Anguera JA, Reuter-Lorenz PA, Willingham DT, Seidler RD. Failure to Engage Spatial Working Memory Contributes to Age-related Declines in Visuomotor Learning. J. Cogn. Neurosci. 2011;23:11–25. [DOI] [PubMed] [Google Scholar]
- 52.Seidler RD, Bo J, Anguera JA. Neurocognitive Contributions to Motor Skill Learning: The Role of Working Memory. J. Mot. Behav. 2012;44:445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vandevoorde K, Orban de Xivry J-J. Why is the explicit component of motor adaptation limited in elderly adults? J. Neurophysiol. 2020;124:152–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Galea JM, Vazquez A, Pasricha N, de Xivry J-JO, Celnik P. Dissociating the roles of the cerebellum and motor cortex during adaptive learning: the motor cortex retains what the cerebellum learns. Cereb. Cortex N. Y. N 1991. 2011;21:1761–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li CS, Padoa-Schioppa C, Bizzi E. Neuronal correlates of motor performance and motor learning in the primary motor cortex of monkeys adapting to an external force field. Neuron. 2001;30:593–607. [DOI] [PubMed] [Google Scholar]
- 56.Mariscal DM, Fjeld KL, Torres-Oviedo G. Characterization of the adaptation and generalization dynamics from high-dimensional neuromuscular data. In: Advances in Motor Learning and Motor Control (MLMC). Washington D.C.; 2023. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study and code are available at Open Science Framework (https://osf.io/pws2k/).