Abstract
Background
Periprosthetic femoral fractures are a serious complication that put a high burden on patients. However, comprehensive analyses of their incidence, mortality, and complication rates based on large-registry data are scarce.
Questions/purposes
In this large-database study, we asked: (1) What is the incidence of periprosthetic femoral fractures in patients 65 years and older in the United States? (2) What are the rates of mortality, infection, and nonunion, and what factors are associated with these outcomes?
Methods
In this retrospective, comparative, large-database study, periprosthetic femoral fractures occurring between January 1, 2010, and December 31, 2019, were identified from Medicare physician service records encompassing services rendered in medical offices, clinics, hospitals, emergency departments, skilled nursing facilities, and other healthcare institutions from approximately 2.5 million enrollees. These were grouped into proximal, distal, and shaft fractures after TKA and THA. We calculated the incidence of periprosthetic femur fractures by year. Incidence rate ratios (IRR) were calculated by dividing the incidence in 2019 by the incidence in 2010. The Kaplan-Meier method with Fine and Gray subdistribution adaptation was used to calculate the cumulative incidence rates of mortality, infection, and nonunion. Semiparametric Cox regression was applied with 23 measures as covariates to determine factors associated with these outcomes.
Results
From 2010 to 2019, the incidence of periprosthetic femoral fractures increased steeply (TKA for distal fractures: IRR 3.3 [95% CI 1 to 9]; p = 0.02; THA for proximal fractures: IRR 2.3 [95% CI 1 to 4]; p = 0.01). One-year mortality rates were 23% (95% CI 18% to 28%) for distal fractures treated with THA, 21% (95% CI 19% to 24%) for proximal fractures treated with THA, 22% (95% CI 19% to 26%) for shaft fractures treated with THA, 21% (95% CI 18% to 25%) for distal fractures treated with TKA, 22% (95% CI 17% to 28%) for proximal fractures treated with TKA, and 24% (95% CI 19% to 29%) for shaft fractures treated with TKA. The 5-year mortality rate was 63% (95% CI 54% to 70%) for distal fractures treated with THA, 57% (95% CI 54% to 62%) for proximal fractures treated with THA, 58% (95% CI 52% to 63%) for shaft fractures treated with THA, 57% (95% CI 52% to 62%) for distal fractures treated with TKA, 57% (95% CI 49% to 65%) for proximal fractures treated with TKA, and 57% (95% CI 49% to 64%) for shaft fractures treated with TKA. Age older than 75 years, male sex, chronic obstructive pulmonary disease (HR 1.48 [95% CI 1.32 to 1.67] after THA and HR 1.45 [95% CI 1.20 to 1.74] after TKA), cerebrovascular disease after THA, chronic kidney disease (HR 1.28 [95% CI 1.12 to 1.46] after THA and HR 1.50 [95% CI 1.24 to 1.82] after TKA), diabetes mellitus, morbid obesity, osteoporosis, and rheumatoid arthritis were clinical risk factors for an increased risk of mortality. Within the first 2 years, fracture-related infections occurred in 5% (95% CI 4% to 7%) of patients who had distal fractures treated with THA, 5% [95% CI 5% to 6%]) of patients who had proximal fractures treated with THA, 6% (95% CI 5% to 7%) of patients who had shaft fractures treated with THA, 6% (95% CI 5% to 7%) of patients who had distal fractures treated with TKA, 7% (95% CI 5% to 9%) of patients who had proximal fractures treated with TKA, and 6% (95% CI 4% to 8%) of patients who had shaft fractures treated with TKA. Nonunion or malunion occurred in 3% (95% CI 2% to 4%) of patients with distal fractures treated with THA, 1% (95% CI 1% to 2%) of patients who had proximal fractures treated with THA, 2% (95% CI 1% to 3%) of patients who had shaft fractures treated with THA, 4% (95% CI 3% to 5%) of those who had distal fractures treated with TKA,, 2% (95% CI 1% to 4%) of those who had proximal fractures treated with TKA, and 3% (95% CI 2% to 4%) of those who had shaft fractures treated with TKA.
Conclusion
An increasing number of periprosthetic fractures were observed during the investigated period. At 1 and 5 years after periprosthetic femur fracture, there was a substantial death rate in patients with Medicare. Conditions including cerebrovascular illness, chronic kidney disease, diabetes mellitus, morbid obesity, osteoporosis, and rheumatoid arthritis are among the risk factors for increased mortality. After the surgical care of periprosthetic femur fractures, the rates of fracture-related infection and nonunion were high, resulting in a serious risk to affected patients. Patient well-being can be enhanced by an interdisciplinary team in geriatric traumatology and should be improved to lower the risk of postoperative death. Additionally, it is important to ensure that surgical measures to prevent fracture-related infections are followed diligently. Furthermore, there is a need to continue improving implants and surgical techniques to avoid often-fatal complications such as fracture-associated infections and nonunion, which should be addressed in further studies.
Level of Evidence
Level III, therapeutic study.
Introduction
With the success of joint arthroplasty and the progressive increase in the number of hip and knee arthroplasties that are performed, periprosthetic fractures are an increasing challenge [24]. Periprosthetic femoral fractures impose a major burden on patients, affecting their quality of life and overall well-being. These fractures not only lead to physical limitations but also result in psychologic and emotional distress. Patients often experience pain, reduced mobility, and loss of independence [9, 15]. Early studies indicated an increase in the incidence of periprosthetic femoral fractures [3, 13]. Since then, the number of THAs has increased, with projections estimating a 174% growth to 572,000 annual procedures by 2030 in the United States [11]. Cumulative risk rates of postoperative periprosthetic femur fractures were reported to be 3.5% to 6.6% [1, 20].
Although a few studies have provided insights into the epidemiology and complication rate after periprosthetic femoral fractures, most of them were retrospective and monocentric, and included a small sample. Only two other registry-based studies were identified, one using the Swedish National Hip Arthroplasty Register and one using a Finnish registry [14, 17]. However, the first study did not differentiate between fracture types, and the second reported on proximal and distal periprosthetic femoral fractures only. Thus, despite being a valuable resource for stakeholders in the healthcare system, a comprehensive analysis of incidence, mortality, and complication rates in terms of fracture-related infection and nonunion, differentiating between periprosthetic femoral fracture types after THA and TKA based on large datasets, has not been performed for the United States.
Therefore, we asked: (1) What is the incidence of periprosthetic femoral fractures in patients 65 years and older in the United States? (2) What are the rates of mortality, infection, and nonunion, and what factors are associated with these outcomes?
Patients and Methods
Study Design and Setting
This was a retrospective, comparative, large-database study. Periprosthetic femur fractures that occurred between January 1, 2010, and December 31, 2019, were identified for this study from Medicare physician service records. These records encompassed services rendered in medical offices, clinics, hospitals, emergency departments, skilled nursing facilities, and other healthcare institutions. They were compiled by the Centers for Medicare and Medicaid Services, and after deidentification, were made available for research use, known as the Limited Data Set (LDS). These LDS data are based on a 5% sample of Medicare beneficiaries, equivalent to the medical records from approximately 2.5 million enrollees. The 5% data are sampled in such a way that the same beneficiary (or new beneficiary who meets the sampling definition) is sampled in the LDS from year to year, which allowed patients to be followed longitudinally for survivorship and outcome analyses. Each year, the 5% LDS data captured 18,000 patients with femur fractures and approximately 140,000 femur fracture–related physician records. The population of interest included patients with Medicare (65 years and older) who had a prior THA or TKA and experienced a traumatic periprosthetic femur fracture during the study period. Because these LDS datasets were generated from Medicare fee-for-service enrollees, those enrolled in a Medicare health maintenance organization, those younger than 65 years but who qualified for Medicare benefits, or those residing outside of the 50 states were excluded.
Patients
We used International Classification of Diseases (ICD)-9 and ICD-10 to identify femur fractures from these physician records. Diagnosis in claims submitted before October 1, 2015, were recorded in ICD-9-Clinical Modification and in a later part of the same document, in ICD-10-CM. For this analysis, we grouped traumatic femur fractures into proximal, shaft, distal, and fracture of an unspecified part of the femur using the ICD codes to identify each type of fracture (Supplemental Table 1; http://links.lww.com/CORR/B228). Identification of periprosthetic fractures required additional diagnosis codes, because in the ICD-9 and ICD-10 coding systems, precise coding of periprosthetic femur fractures cannot always be taken for granted. To achieve a survey that is as complete as possible, we pursued the following approach. Under ICD-10, periprosthetic fracture is identified by M97.0 (with prosthetic hip) or M97.1 (with prosthetic knee). There are several additional codes in the M97 series that identify involvement of other or unspecified prosthetic joints. Under ICD-9, however, all periprosthetic fractures are identified by one code: 996.44. To ascertain the prosthetic joint associated with the femur fracture, we checked for the ICD-9 codes V93.64 (hip) or V93.65 (knee), which indicated the presence of a hip or knee prosthesis. Fortunately, if a prosthetic joint was recognized as periprosthetic, its presence was almost always noted. The equivalent codes in ICD-10 are Z96.64 (hip) or Z96.65 (knee), which we also used to help resolve patients with an unspecified prosthetic joint in the M97 code. In addition, we also checked for the appearance of Common Procedural Terminology codes associated with THA (such as 27130) or TKA (such as 27447) before the femur fracture to provide supplemental information about the nature of the periprosthetic fracture. Approximately 5% of periprosthetic femur fractures could not be linked to a prosthetic hip or knee.
We implemented several steps to ensure the identified fracture was true. We retained only records with femur fracture listed as the primary diagnosis, unless preceded by another fracture in those with multiple fractures. Concurrent fracture of different parts of the femur (such as a shaft and a head or neck fracture) was not uncommon, and each was counted under the respective femur fracture type. Some patients experienced the same femur fracture type more than once during the 10-year study period. However, from one fracture to the next, a minimal interval of 1 year was required to ensure the next fracture was not associated with continued care for the previous fracture. This screening was especially useful for fractures coded under ICD-9, where the code was less precise. For fractures coded using ICD-10, we used a seventh digit, with “A,” “B,” or “C” to denote a new encounter with that condition. Other seventh-digit values indicated a subsequent encounter, malunion or nonunion, or sequalae. Such records were not retained because these conditions were consistent only with preexisting fractures. Finally, we took steps to check the records in the days after the fracture to ensure that the pattern of service was consistent. For example, we eliminated records that mentioned femur fracture but had no record of any radiologic imaging of the lower limbs, no mention of hospital stay, and no mention of any lower limb–related repair procedure. Such a “fracture” was likely not a true fracture and was eliminated. Two authors (ECL and NW) screened the patients for corresponding CPT codes.
Primary and Secondary Study Outcomes
Our primary goal was to determine the incidence of periprosthetic femoral fractures in patients 65 years and older in the United States. For this, we calculated the incidence of periprosthetic femur fracture by year and the rate of fracture by dividing the fracture frequency with the corresponding Medicare enrollments. The proximal, shaft, and distal femur fracture rates, the overall femur fracture rate, and age-specific and sex-specific incidence rates were calculated. The overall periprosthetic femur fracture rate included fractures in an unspecified part of the femur or those with unspecified joint involvement. In addition, overall femur fracture rates also discounted instances in which multiple parts of the femur were fractured in the same incidence. Incidence rate ratios (IRR) were calculated by dividing the incidence in 2019 by the incidence in 2010. Incidence rates were compared using the two-sample z-test.
Our secondary goal was to determine the rate of three types of outcomes as well as factors associated with these outcomes: postfracture mortality risk, postfracture infection risk, and the likelihood of malunion or nonunion after periprosthetic fracture. ICD-9 and ICD-10 diagnosis codes were used to identify these subsequent conditions (Supplemental Table 1; http://links.lww.com/CORR/B228). For malunion or nonunion, we imposed a 9-month postfracture blackout period to ensure the record indicating malunion or nonunion was justified and reliable. For infection, we focused on infection associated with the orthopaedic implant, including fixation devices. Except for mortality, we restricted the outcomes analyzed to those that occurred within 2 years after the femur fracture. Adverse events such as periprosthetic infections and implant loosening occurred after 2 years, but in much smaller numbers. Because the diagnosis codes for most of these adverse events were not implant-specific or body region–specific, the risk of mistaken attribution between the adverse event and femur fracture increased with increasing time. For mortality, the date of death for each beneficiary is part of the Medicare enrollment data. As such, survival was evaluated for the full 10 years of the study period. We analyzed survival in two ways. We compared patients who had sustained a periprosthetic femur fracture with other Medicare enrollees who had never experienced a femur fracture. For each patient with a fracture, three enrollees from the same state and county and of the same age and sex were sampled to form a case-control group. Mortality was calculated, and the overall difference in survival was estimated. We also compared patients who had sustained a fracture among themselves according to the part of the femur that suffered the fracture. The unique patient ID allowed us to track subsequent events after the femur fracture. Individuals were tracked from the date of the periprosthetic fracture until the outcome occurred, until death, until the end of enrollment, or until the end of the study on December 31, 2019, whichever came first.
We used survival analysis techniques to analyze these outcomes. We used the Kaplan-Meier method with the Fine and Gray subdistribution adaptation to calculate the cumulative incidence rate of malunion or nonunion and infection. Because these patients with fractures were 65 years and older, many of them died during the study period. The Fine and Gray technique was used to account for death as a competing event. For mortality or survivorship, the conventional Kaplan-Meier method was appropriate. We also used the semiparametric Cox regression to investigate these outcomes and compare the risk between different types of femur fracture, after adjusting for a number of potential confounding factors. Patients with a replaced hip or knee were analyzed separately. It is believed that the femur fracture interacts with the hip or the knee differently, and the resulting outcomes—and factors associated with these outcomes—are potentially different. The Cox models incorporated demographic, clinical, and several community-level socioeconomic measures as covariates. The demographic factors included age, gender, race, resident region, and Medicare buy-in (as a surrogate for patient economic status). Clinical factors included osteoporosis, obesity, diabetes, rheumatoid arthritis, chronic kidney disease, cigarette smoking, regular use of anticoagulants, hypertensive disease, ischemic heart disease, cerebrovascular disease, chronic obstructive pulmonary disease, and congestive heart failure identified by ICD-9 and ICD-10 codes (Supplemental Table 1; http://links.lww.com/CORR/B228). These conditions were identified from physician records in a 1-year period before the fracture. These conditions could appear as either the primary or secondary diagnosis. The socioeconomic measures for the patients’ resident counties were population, median household income, percentage of population with at least a college education, percentage of population living on less than USD 36 per day, percentage of individuals who were not employed, and a measure of the urban-rural character of the county. These measures were obtained from the United States Census, the Census Bureau’s American Community Survey program, and the Economic Research Service of the United States Department of Agriculture (accessible at: https://www.census.gov/programs-surveys/acs/data.html and https://www.ers.usda.gov/data-products/county-level-data-sets/). These measures help characterize the resident county of the patient and highlight the association between socioeconomic effects and health outcomes among patients with periprosthetic femoral fractures. We characterized fractures as open or closed, and whether there was another bone fracture involved in a concomitant fracture. We also checked to see whether the fracture was related to a fall or a vehicle collision, because those events could affect the outcomes.
Typical surgical treatment after femur fracture was also investigated. In physician records, CPT codes were used to identify procedures and operations. Surgical procedures involving the hip, pelvis, and femur range from 27000 to 27599. We searched for such procedures in the 30 days after the fracture. If we found multiple procedures, we selected procedures closest in time to the fracture date. Additionally, if we identified multiple procedures as “closest” to the fracture date (for example, two procedures on the day after the fracture), then the procedure that received the highest amount of Medicare payment was assigned as the treatment. We also required that the patients had at least 30 days of postfracture observations for this part of the analysis. This criterion was included to eliminate fractures that occurred only days from the end of the study period or patients who died very shortly after the fracture and did not undergo repair or reconstruction procedures.
Ethical Approval
This study is based on data from the Medicare Physician Service Records Data Base. These records encompassed diagnoses and treatments rendered in medical offices, outpatient clinics, hospitals, emergency departments, skilled nursing homes, and other healthcare facilities. They were compiled by the Centers for Medicare and Medicaid Services, and after deidentification were made available to researchers, known as the LDS. Because the Centers for Medicare and Medicaid Services data are deidentified, the study was exempt from review by our institutional review board.
Statistical Analysis
All data processing and statistical analyses were performed using SAS statistical software (Version 9.4, SAS Institute), and significance was determined at α < 0.05.
Results
Incidence of Periprosthetic Femoral Fractures in the United States Population 65 Years and Older
From 2010 to 2019, the incidence of periprosthetic femoral fractures of all types increased steeply (Fig. 1). The incidence in 2019 was 8 per 100,000 population for distal fractures (IRR 3.1 [95% CI 1 to 13]; p = 0.12), 30 per 100,000 population for proximal fractures (IRR 2.3 [95% CI 1 to 4]; p = 0.01), and 16 per 100,000 population for shaft fractures (IRR 2.2 [95% CI 1 to 5]; p = 0.08) after THA. After TKA, the incidence was 17 per 100,000 population for distal fractures (IRR 3.3 [95% CI 1 to 9]; p = 0.02), 5 per 100,000 population for proximal fractures (IRR 1.6 [95% CI 1 to 7]; p = 0.54), and 9 per 100,000 population for shaft fractures (IRR 2.8 [95% CI 1 to 11]; p = 0.12) (Table 1). Periprosthetic femoral fractures affected more women than men, with an increasing incidence rate with age (Fig. 2). Distal fractures were mainly treated with fixation, proximal fractures were mostly treated with arthroplasty, and the highest percentage of shaft fractures was treated with a plate or screw (Supplemental Fig. 1; http://links.lww.com/CORR/B229). Open fractures constituted 1.4% (147 of 10,284) of fractures. In total, 0.3% (31 of 10,284) of fractures were vehicle collision–related and 17% (1758 of 10,284) were fall-related.
Fig. 1.
This graph shows the incidence of periprosthetic femoral fractures grouped into distal, proximal, and shaft fractures after hip and knee arthroplasty. A color image accompanies the online version of this article.
Table 1.
Historic development of periprosthetic femur fracture diagnoses between 2010 and 2019
| Fracture type | Year | Medicare enrollees | Incidence/100,000 after THA | Incidence/100,000 after TKA |
| Distal | 2010 | 1,458,043 | 2.6 | 5.0 |
| 2011 | 1,477,801 | 3.2 | 7.5 | |
| 2012 | 1,509,564 | 3.2 | 7.1 | |
| 2013 | 1,531,684 | 3.1 | 8.9 | |
| 2014 | 1,546,499 | 4.5 | 10.5 | |
| 2015 | 1,565,215 | 4.6 | 11.6 | |
| 2016 | 1,602,680 | 6.2 | 10.6 | |
| 2017 | 1,609,249 | 6.5 | 11.9 | |
| 2018 | 1,619,824 | 10.0 | 12.4 | |
| 2019 | 1,631,331 | 8.0 | 16.5 | |
| 2010 to 2019 | 15,551,890 | 5.4 | 10.8 | |
| Proximal | 2010 | 1,458,043 | 13.3 | 3.0 |
| 2011 | 1,477,801 | 13.4 | 3.9 | |
| 2012 | 1,509,564 | 12.9 | 2.9 | |
| 2013 | 1,531,684 | 16.5 | 4.6 | |
| 2014 | 1,546,499 | 17.0 | 4.2 | |
| 2015 | 1,565,215 | 21.3 | 5.6 | |
| 2016 | 1,602,680 | 27.2 | 3.5 | |
| 2017 | 1,609,249 | 26.8 | 2.9 | |
| 2018 | 1,619,824 | 32.3 | 2.7 | |
| 2019 | 1,631,331 | 30.3 | 4.7 | |
| 2010 to 2019 | 15,551,890 | 22.2 | 4.0 | |
| Shaft | 2010 | 1,458,043 | 7.4 | 3.0 |
| 2011 | 1,477,801 | 8.3 | 2.9 | |
| 2012 | 1,509,564 | 7.6 | 3.2 | |
| 2013 | 1,531,684 | 7.9 | 4.2 | |
| 2014 | 1,546,499 | 9.6 | 5.9 | |
| 2015 | 1,565,215 | 8.8 | 5.2 | |
| 2016 | 1,602,680 | 13.5 | 4.9 | |
| 2017 | 1,609,249 | 12.2 | 5.3 | |
| 2018 | 1,619,824 | 17.9 | 5.5 | |
| 2019 | 1,631,331 | 16.0 | 8.5 | |
| 2010 to 2019 | 15,551,890 | 11.5 | 5.1 |
Fig. 2.
The historic age-specific and sex-specific incidence rates of periprosthetic femoral fractures are shown here. Male patients are shown in green; female patients are shown in blue. A color image accompanies the online version of this article.
Rate of Mortality, Nonunion, and Infection, and Associated Factors
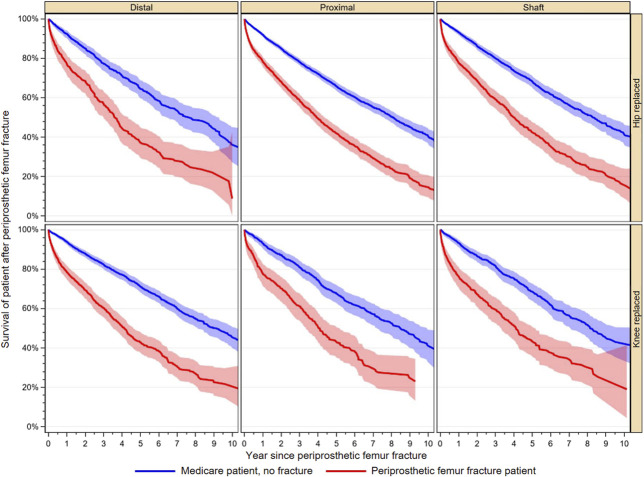
For periprosthetic distal femoral fractures after THA, the survival rates were 77% (95% CI 72% to 82%) after 1 year, 37% (95% CI 30% to 46%) after 5 years, and 9% (95% CI 0.1% to 43%) after 10 years. For periprosthetic proximal femoral fractures after THA, the survival rates were 79% (95% CI 76% to 81%) after 1 year, 42% (95% CI 38% to 46%) after 5 years, and 15% (95% CI 9% to 21%) after 10 years, whereas 78% (95% CI 74% to 81%) of the patients with periprosthetic femoral shaft fractures after THA survived after 1 year, 43% (95% CI 37% to 48%) survived after 5 years, and 15% (95% CI 8% to 24%) survived after 10 years (Fig. 3). For distal fractures after TKA, survival rates were 79% (95% CI 75% to 82%) after 1 year, 43% (95% CI 38% to 48%) after 5 years, and 22% (95% CI 15% to 30%) after 10 years. For proximal fracture after TKA, survival rates were 78% (95% CI 72% to 83%) after 1 year, 43% (95% CI 35% to 51%) after 5 years, and 25% (95% CI 16% to 35%) after 10 years. Of the patients with a periprosthetic shaft fracture after TKA, 76% (95% CI 71% to 81%) were still alive after 1 year, 43% (95% CI 36% to 51%) were still alive after 5 years, and 19% (95% CI 4% to 42%) were alive after 10 years (Supplemental Table 2; http://links.lww.com/CORR/B230). Factors associated with death included age, male sex, chronic obstructive pulmonary disease (HR 1.48 [95% CI 1.32 to 1.67] after THA and HR 1.45 [95% CI 1.20 to 1.74] after TKA), cerebrovascular disease after THA, chronic kidney disease (HR 1.28 [95% CI 1.12 to 1.46] after THA and HR 1.50 [95% CI 1.24 to 1.82] after TKA), diabetes mellitus, morbid obesity, osteoporosis, and rheumatoid arthritis (Table 2).
Fig. 3.
This graph shows patient survival after periprosthetic femoral fracture compared with that of patients who never experienced a femur fracture. A color image accompanies the online version of this article.
Table 2.
Factors associated with death after periprosthetic femoral fractures
| After THA | After TKA | |||
| Factor | HR (95% CI) | p value | HR (95% CI) | p value |
| Age 70 to 74 years (compared with 65 to 69 years) | 1.36 (1.03 to 1.80) | 0.03 | 1.09 (0.76 to 1.56) | 0.65 |
| Age 75 to 79 years (compared with 65 to 69 years) | 1.75 (1.35 to 2.27) | < 0.001 | 1.55 (1.10 to 2.18) | 0.01 |
| Age 80 + years (compared with 65 to 69 years) | 3.57 (2.82 to 4.51) | < 0.001 | 3.30 (2.42 to 4.49) | < 0.001 |
| Distal versus proximal fracture | 1.08 (0.97 to 1.19) | 0.15 | 1.06 (0.95 to 1.18) | 0.27 |
| Shaft versus proximal fracture | 1.00 (0.94 to 1.07) | 0.95 | 1.03 (0.91 to 1.16) | 0.64 |
| Female sex | 0.84 (0.75 to 0.94) | 0.002 | 1.04 (0.87 to 1.26) | 0.65 |
| Anticoagulant use | 1.04 (0.89 to 1.21) | 0.66 | 1.11 (0.87 to 1.42) | 0.42 |
| Chronic obstructive pulmonary disease | 1.48 (1.32 to 1.67) | < 0.001 | 1.45 (1.20 to 1.74) | < 0.001 |
| Cerebrovascular disease | 1.18 (1.04 to 1.34) | 0.01 | 1.01 (0.82 to 1.25) | 0.90 |
| Chronic kidney disease | 1.28 (1.12 to 1.46) | < 0.001 | 1.50 (1.24 to 1.82) | < 0.001 |
| Concomitant fracture | 1.17 (0.99 to 1.37 | 0.06 | 0.90 (0.72 to 1.12) | 0.34 |
| Congestive heart failure | 1.48 (1.30 to 1.69) | < 0.001 | 1.47 (1.24 to 1.76) | < 0.001 |
| Diabetes mellitus | 1.20 (1.07 to 1.35) | 0.002 | 1.09 (0.92 to 1.29) | 0.32 |
| Fall to related fracture (compared with all other fracture types) | 1.01 (0.91 to 1.11) | 0.87 | 1.00 (0.87 to 1.14) | 0.94 |
| Hypertension | 1.02 (0.90 to 1.14) | 0.80 | 1.00 (0.84 to 1.20) | 0.96 |
| Ischemic heart disease | 1.11 (0.99 to 1.24) | 0.07 | 1.12 (0.94 to 1.33) | 0.20 |
| Morbid obesitya | 0.56 (0.36 to 0.87) | 0.01 | 1.12 (0.79 to 1.59) | 0.52 |
| Osteoporosis | 1.50 (1.18 to 1.92) | 0.001 | 0.93 (0.72 to 1.19) | 0.56 |
| Rheumatoid arthritis | 1.25 (1.02 to 1.54) | 0.03 | 1.10 (0.80 to 1.51) | 0.57 |
| Cigarette smoking | 1.12 (0.81 to 1.54) | 0.49 | 0.71 (0.36 to 1.37) | 0.30 |
| Percentage of population with a college degree (compared with + 1%)b | 0.99 (0.98 to 1.00) | 0.07 | 1.00 (0.99 to 1.02) | 0.81 |
| Percentage of population living on less than USD 36 per day (compared with + 1%)c | 1.01 (0.99 to 1.03) | 0.37 | 1.02 (0.99 to 1.05) | 0.19 |
| Percentage of population who are unemployed (compared with + 1%)d | 0.98 (0.94 to 1.02) | 0.39 | 0.99 (0.94 to 1.04) | 0.69 |
| County population (compared with + 100,000) | 1.00 (1.00 to 1.00) | 0.59 | 1.00 (0.99 to 1.00) | 0.45 |
| Median household income (compared to + USD 5000) | 1.00 (0.97 to 1.03) | 0.95 | 1.02 (0.97 to 1.07) | 0.40 |
BMI ≥ 40 kg/m2.
This factor was compared with a hypothetical reference population with a 1% increase in the number of people with a college degree.
This factor was compared with a hypothetical reference population with a 1% increase in the number of people living on less than USD 36 per day.
This factor was compared with a hypothetical reference population with a 1% increase in the number of people who are unemployed.
The infection rate was 5% (currently at risk: 344 [95% CI 4% to 7%]) for distal fractures, 5% (currently at risk: 1510 [95% CI 5% to 6%]) for proximal fractures, and 6% (currently at risk: 779 [95% CI 5% to 7%]) for shaft fractures after THA after 24 months. After TKA, infection rates were 6% (currently at risk: 747 [95% CI 5% to 7%]) for distal fractures, 7% (currently at risk: 313 [95% CI 5% to 9%]) for proximal fractures, and 6% (currently at risk: 338 [95% CI 4% to 8%]) for shaft fractures after 24 months (Fig. 4). The occurrence of fracture-related infection was less common in patients older than 75 years. Factors associated with a fracture-related infection included anticoagulant use (HR 1.30 [95% CI 0.83 to 2.02] after THA and HR 1.82 [95% CI 1.01 to 3.26] after TKA), congestive heart failure, hypertensive disease (HR 1.49 [95% CI 1.04 to 2.12] after THA and HR 1.62 [95% CI 0.92 to 2.82] after TKA), morbid obesity, and osteoporosis (Supplemental Table 3; http://links.lww.com/CORR/B231).
Fig. 4.
The rate of fracture-related infections after periprosthetic femoral fracture as a function of time is shown here.
After 24 months, nonunion or malunion occurred in 3% (currently at risk: 352 [95% CI 2% to 4%]) of patients with a distal fracture, 1% (currently at risk: 1583 [95% CI 1% to 2%]) of patients with a proximal fracture, and 2% (currently at risk: 808 [95% CI 1% to 3%]) of patients with a shaft fracture after THA. There were higher percentages for periprosthetic fractures after TKA: 4% (currently at risk: 759 [95% CI% 3 to 5%]) for distal fractures, 2% (currently at risk: 323 [95% CI 1% to 4%]) for proximal fracture, and 3% (currently at risk: 345 [95% CI 2% to 4%]) for shaft fractures after 24 months (Fig. 5). Fracture healing complications after THA were more likely to occur in patients older than 80 years, more likely to occur in distal fractures than in proximal fractures, and more likely to occur in patients with osteoporosis (Supplemental Table 3; http://links.lww.com/CORR/B231).
Fig. 5.
The rate of nonunion or malunion after periprosthetic femoral fracture depending on time is shown here.
Discussion
Periprosthetic femoral fractures are a serious complication that put a high burden on patients. Large-scale studies using nationwide registries provide valuable insights into the incidence, mortality, and complication rates, benefiting stakeholders in the healthcare system. However, to date, only two studies have examined these aspects using nationwide registries, without differentiating between distinct fracture types after THA and TKA [14, 17]. The presented data from the United States reveal a substantial increase in the incidence of periprosthetic femoral fractures, high mortality rates, and associated factors that can be addressed through appropriate therapeutic interventions.
Limitations
The data used in this study were derived from Medicare physician claims, which is fundamentally a type of administrative record, not a true clinical dataset. All the limitations associated with administrative records are present in the data used here [21, 22]. Our analysis especially relies on correct coding and data management in the claim submission. The switch from ICD-9 to ICD-10 coding in October 2015 may have affected the results and must be considered. Further, under both ICD-9 and ICD-10 coding systems, precise coding of periprosthetic femur fractures cannot always be taken for granted. Therefore, several steps were implemented to verify the accuracy in identifying periprosthetic femoral fractures based on ICD codes. These included, for instance, reviewing for the simultaneous appearance of a CPT code indicating previous THA or TKA or codes indicating the presence of a hip or knee prosthesis. In addition, we screened for typical records that are documented for in-hospital fracture care, such as a record of any radiologic imaging of the lower limbs, in-hospital stay, or codes for any fracture treatment. In the absence of such records, the presence of a periprosthetic fracture was not assumed. Considering this stepwise approach, the results should be interpreted cautiously, meaning that some fractures might not have been coded accurately. Thus, the presented incidences might be underestimated. In particular, the coding system of vis-à-vis specific surgical procedures is often inaccurate from a surgical perspective and can only describe the exact surgical procedure to a limited extent. Therefore, an analysis of treatment concepts and their influence on mortality and postoperative complications was not a focus of the present study. In contrast, it can be assumed that the extensive information on patient characteristics and complications is high quality because of this information’s relevance to billing and insertion of the data by appropriate specialists. In addition, whereas other research reported a higher occurrence of periprosthetic femoral fractures in patients with uncemented stem protheses than in those with cemented stems [1], the underlying data only allowed differentiation into subgroups according to the index joint, but not according to the implant type. Further, the analysis was based on a 5% sample. The 5% LDS records are sampled systematically across the entire Medicare population without varying the sampling proportion by region, age group, or any other factors. Thus, the 5% sample is a true and representative cross-section of the Medicare population. Additionally, because the sampling weight is constant, including weight would not affect any of the results. Finally, the sociodemographic variables are based on the patient’s county. To address this issue, several indirect measures reflecting the county population and general economic health of the community were considered in the analysis.
Incidence of Periprosthetic Femoral Fractures in the United States Population 65 Years and Older
Incidence rates of periprosthetic femoral fractures increased for distal, proximal, and shaft fractures after THA and TKA from 2010 through 2019. This was the highest for distal periprosthetic fractures after TKA, for which the incidence tripled. The increased incidence could be attributable to the increase in primary arthroplasty procedures performed annually in the United States as well as to higher life expectancy, which yields more patients with more-advanced ages who have a joint prothesis in situ [1, 11, 24]. Some studies also provided insights into the epidemiology of periprosthetic femoral fractures related to timing. A study found a lower incidence rate than we did, with the rate of intraoperative periprosthetic femoral fractures ranging from 0.1% to 27.8% and from 0.07% to 18% for periprosthetic femoral fractures a minimum of 2 years after surgery [27]. The rising incidence of periprosthetic femoral fractures is an increasingly relevant topic for stakeholders in the healthcare system. Costs for the treatment of hip periprosthetic femoral fractures with internal fixation and revision THA have been calculated at USD 26,522 and USD 36,161, respectively [19]. Because periprosthetic femoral fractures are often complex injuries, with a high risk of mortality, complications, and 90-day readmission rates of 27.3% for periprosthetic femoral fractures after arthroplasty [23], resources must be used appropriately for their treatment. Strategies for reducing the incidence of periprosthetic femoral fractures could include the provision of thorough education to patients and their caregivers regarding fall prevention strategies, adherence to rehabilitation protocols, and the importance of maintaining overall bone health. For instance, such a program could focus on increasing muscle strength, joint stability, and balance to minimize the risk of falls and subsequent fractures. It could also include information on home modifications, assistive devices, and lifestyle modifications to reduce the risk of fractures. Collaboration among healthcare providers and patient engagement play crucial roles in achieving successful outcomes and reducing the incidence of periprosthetic fractures. Further, meticulous surgical techniques, including proper component alignment, accurate implant sizing, and adequate soft tissue balancing, should be used. Careful attention to surgical details can contribute to enhanced implant stability and reduce the risk of fractures. Thus, a thorough intraoperative assessment of bone quality is important. Special techniques such as intraoperative fluoroscopy [12] or other preoperative imaging modalities could be used to detect any structural weakness before finalizing implant fixation. Collaborating with a team of experienced orthopaedic surgeons and considering evidence-based guidelines can further inform the decision-making process.
The Rate of Mortality, Nonunion and Infection, and Associated Risk Factors
The 1-year mortality after periprosthetic fracture reported elsewhere has ranged from 10.5% to 26.5% [7, 17]. This is consistent with mortality at 1 year in our study. Khan et al. [10] demonstrated a mortality rate of up to 60% at 5 years after revision surgery. The highest proportion was among men older than 75 years with an American Society of Anesthesiologists classification greater than 3. Additionally, osteoporosis and rheumatoid arthritis were associated with mortality, which is consistent with our findings [6]. Compared with intracapsular femoral neck fracture, which is the most common femur fracture in patients older than 65 years [25], the mortality rate for periprosthetic femoral fractures showed an equal pattern. After 1 year, the mortality rate after a femoral neck fracture was between 18% and 31% [8, 26, 28], whereas in our investigation, 22.5% of patients died within the first year after fracture. In addition to the correlation between comorbidity status and mortality, another risk factor in patients with periprosthetic femoral fractures is the association between increased mortality and reduced walking mobility before the injury [18].
Akkawi et al. [2] showed a revision rate of 11% for all postoperative complications, including mechanical complications (9%), infection (1.8%), and nonunion (1.8%), which is in line with our analysis. Other research determined an overall complication rate of 18%, with septic complications in 2.7% of the patients [14], which is less than in our study. A recent registry-based study reported a fracture-related infection rate of 5% at 5 years after surgery [17]. Nonunion of periprosthetic femoral fractures is also a relevant issue and is associated with an increased rate of further complications such as infection and reduced functional outcome [5]. The present investigation demonstrates that 5.2% to 5.7% of all periprosthetic femoral fractures resulted in fracture-related infection within 24 months of follow-up, which is within the upper range of the already existing evidence (1.8% to 6.5%) [16, 19, 24]. To further reduce the risk of mortality, fracture-related infection, and nonunion, it would be valuable to develop a standardized preoperative risk assessment tool that incorporates patient-specific factors such as comorbidities, nutritional status, and bone quality and allows for tailored surgical plans. In addition, a structured postoperative follow-up plan to monitor implant stability, assess healing, and identify any potential complications early on may be beneficial. Regular clinical and radiologic evaluations may help identify and address any issues that could increase the risk of periprosthetic fractures. Further, the findings emphasize the importance of a multidisciplinary approach involving orthopaedic surgeons, infectious disease specialists, and rehabilitation experts in the management of periprosthetic femoral fractures.
Conclusion
An increasing number of periprosthetic fractures were observed during the investigated period. At 1 and 5 years after periprosthetic femur fracture, there was a substantial death rate in patients with Medicare. Conditions including cerebrovascular illness, chronic kidney disease, diabetes mellitus, morbid obesity, osteoporosis, and rheumatoid arthritis are among the risk factors for increased mortality. After the surgical care of periprosthetic femur fractures, the rates of fracture-related infection and nonunion were high, resulting in a serious risk to affected patients. Patient well-being can be enhanced by an interdisciplinary team in geriatric traumatology and should be improved to lower the risk of postoperative death. Additionally, it is important to ensure that surgical measures to prevent fracture-related infections are followed diligently. Furthermore, there is a need to continue improving implants and surgical techniques to avoid often-fatal complications such as fracture-associated infections and nonunion, which should be addressed in further studies.
Supplementary Material
Footnotes
One of the authors (ECL) certifies that they are an employee of Exponent Inc.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was waived by the ethics committee of the University Medical Center Regensburg, Germany.
The work was performed at the University Medical Center Regensburg, Regensburg, Germany.
Contributor Information
Nike Walter, Email: nike.walter@ukr.de.
Dominik Szymski, Email: dominik.szymski@ukr.de.
Steven M. Kurtz, Email: smk38@drexel.edu.
Volker Alt, Email: volker.alt@ukr.de.
David W. Lowenberg, Email: lowenbd@stanford.edu.
Edmund C. Lau, Email: edmundclau@gmail.com.
Markus Rupp, Email: markus.rupp@ukr.de.
References
- 1.Abdel MP, Watts CD, Houdek MT, Lewallen DG, Berry DJ. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Joint J. 2016;98:461-467. [DOI] [PubMed] [Google Scholar]
- 2.Akkawi I, Fabbri D, Romantini M, Laus M, Calogero A. Outcome of surgical treatment of 54 periprosthetic femoral fractures after total hip arthroplasty at mid term follow-up. Acta Biomed. 2021;92:e2021312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999;30:183-190. [DOI] [PubMed] [Google Scholar]
- 4.Corten K, Macdonald SJ, McCalden RW, Bourne RB, Naudie DDR. Results of cemented femoral revisions for periprosthetic femoral fractures in the elderly. J Arthroplasty. 2012;27:220-225. [DOI] [PubMed] [Google Scholar]
- 5.Crockarell JR, Berry DJ, Lewallen DG. Nonunion after periprosthetic femoral fracture associated with total hip arthroplasty. J Bone Joint Surg Am. 1999;81:1073-1079. [DOI] [PubMed] [Google Scholar]
- 6.Della Rocca GJ, Leung KS, Pape H-C. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011;25:S66-S70. [DOI] [PubMed] [Google Scholar]
- 7.El Khassawna T, Knapp G, Scheibler N, et al. Mortality, risk factors and risk assessment after periprosthetic femoral fractures-a retrospective cohort study. J Clin Med. 2021;10:4324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandez MA, Achten J, Parsons N, et al. Cemented or uncemented hemiarthroplasty for intracapsular hip fracture. N Engl J Med. 2022;386:521-530. [DOI] [PubMed] [Google Scholar]
- 9.Islam R, Lanting B, Somerville L, Hunter SW. Evaluating the functional and psychological outcomes following periprosthetic femoral fracture after total hip arthroplasty. Arthroplast Today. 2022;18:57-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan T, Middleton R, Alvand A, Manktelow ARJ, Scammell BE, Ollivere BJ. High mortality following revision hip arthroplasty for periprosthetic femoral fracture. Bone Joint J. 2020;102:1670-1674. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [DOI] [PubMed] [Google Scholar]
- 12.Lecoultre Y, Danek J, Rompen IF, et al. Intraoperative imaging in hip arthroplasty: a meta-analysis and systematic review of randomized controlled trials and observational studies. Arthroplasty. 2023;5:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lewallen DG, Berry DJ. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instr Course Lect. 1998;47:243-249. [PubMed] [Google Scholar]
- 14.Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20:857-865. [DOI] [PubMed] [Google Scholar]
- 15.Lotzien S, Hoberg C, Hoffmann MF, Schildhauer TA. Clinical outcome and quality of life of patients with periprosthetic distal femur fractures and retained total knee arthroplasty treated with polyaxial locking plates: a single-center experience. Eur J Orthop Surg Traumatol. 2019;29:189-196. [DOI] [PubMed] [Google Scholar]
- 16.Märdian S, Schaser K-D, Gruner J, Scheel F, Perka C, Schwabe P. Adequate surgical treatment of periprosthetic femoral fractures following hip arthroplasty does not correlate with functional outcome and quality of life. Int Orthop. 2015;39:1701-1708. [DOI] [PubMed] [Google Scholar]
- 17.Miettinen S, Sund R, Törmä S, Kröger H. How often do complications and mortality occur after operatively treated periprosthetic proximal and distal femoral fractures? A register-based study. Clin Orthop Relat Res. 2023;481:1940-1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moreta J, Uriarte I, Bidea I, Foruria X, Legarreta MJ, Etxebarría-Foronda I. High mortality rate following periprosthetic femoral fractures after total hip arthroplasty. A multicenter retrospective study. Injury. 2021;52:3022-3027. [DOI] [PubMed] [Google Scholar]
- 19.Pavlou G, Panteliadis P, MacDonald D, et al. A review of 202 periprosthetic fractures--stem revision and allograft improves outcome for type B fractures. Hip Int. 2011;21:21-29. [DOI] [PubMed] [Google Scholar]
- 20.Pivec R, Issa K, Kapadia BH, et al. Incidence and future projections of periprosthetic femoral fracture following primary total hip arthroplasty: an analysis of international registry data. J Long Term Eff Med Implants. 2015;25:269-275. [DOI] [PubMed] [Google Scholar]
- 21.Pugely AJ, Martin CT, Harwood J, Ong KL, Bozic KJ, Callaghan JJ. Database and registry research in orthopaedic surgery: part I: claims-based data. J Bone Joint Surg Am. 2015;97:1278-1287. [DOI] [PubMed] [Google Scholar]
- 22.Pugely AJ, Martin CT, Harwood J, Ong KL, Bozic KJ, Callaghan JJ. Database and registry research in orthopaedic surgery: part 2: clinical registry data. J Bone Joint Surg Am. 2015;97:1799-1808. [DOI] [PubMed] [Google Scholar]
- 23.Reeves RA, Schairer WW, Jevsevar DS. The national burden of periprosthetic hip fractures in the US: costs and risk factors for hospital readmission. Hip Int. 2019;29:550-557. [DOI] [PubMed] [Google Scholar]
- 24.Rupp M, Lau E, Kurtz SM, Alt V. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin Orthop Relat Res. 2020;478:1622-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rupp M, Walter N, Pfeifer C, et al. The incidence of fractures among the adult population of Germany–an analysis from 2009 through 2019. Dtsch Arztebl Int. 2021;118:665-669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shields E, Behrend C, Bair J, Cram P, Kates S. Mortality and financial burden of periprosthetic fractures of the femur. Geriatr Orthop Surg Rehabil. 2014;5:147-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sidler-Maier CC, Waddell JP. Incidence and predisposing factors of periprosthetic proximal femoral fractures: a literature review. Int Orthop. 2015;39:1673-1682. [DOI] [PubMed] [Google Scholar]
- 28.Veldman HD, Heyligers IC, Grimm B, Boymans TAEJ. Cemented versus cementless hemiarthroplasty for a displaced fracture of the femoral neck: a systematic review and meta-analysis of current generation hip stems. Bone Joint J. 2017;99:421-431. [DOI] [PubMed] [Google Scholar]