Abstract
Background:
Elder mistreatment (EM) is associated with adverse health outcomes and healthcare utilization patterns that differ from other older adults. However, the association of EM with healthcare costs has not been examined. Our goal was to compare healthcare costs between legally adjudicated EM victims and controls.
Methods:
We used Medicare insurance claims to examine healthcare costs of EM victims in the two years surrounding initial mistreatment identification in comparison to matched controls. We adjusted costs using the Centers for Medicare and Medicaid Services Hierarchical Condition Categories (CMS-HCC) risk score.
Results:
We examined healthcare costs in 114 individuals who experienced EM and 410 matched controls. Total Medicare Parts A and B healthcare costs were similar between cases and controls in the 12 months prior to initial EM detection ($11,673 vs. $11,402, p=0.92), but cases had significantly higher total healthcare costs during the 12 months after initial mistreatment identification. ($15,927 vs. $10,805, p=0.04). Adjusting for CMS-HCC scores, cases had, in the 12 months after initial EM identification, $5,084 of additional total healthcare costs (95% confidence interval [$92, $10,077], p=0.046) and $5,817 of additional acute/subacute/post-acute costs (95% confidence interval [$1,271, $10,362], p=0.012) compared with controls. The significantly higher total costs and acute/sub-acute/post-acute costs among EM victims in the post-year were concentrated in the 120 days after EM detection.
Conclusions:
Older adults experiencing EM had substantially higher total costs during the 12 months after mistreatment identification, driven by an increase in acute/sub-acute/post-acute costs and focused in the period immediately after initial EM detection.
Keywords: elder mistreatment, elder abuse, healthcare costs, legally adjudicated elder abuse cases
INTRODUCTION
Elder Mistreatment (EM) is defined as action or negligence against an older adult that causes harm or risk of harm committed by a person in a trust relationship and includes physical abuse, sexual abuse, neglect, psychological abuse, and financial exploitation.1 Elder mistreatment occurs commonly and may have serious health consequences. As many as 1 in 10 community-dwelling older adults experience mistreatment each year,2,3 and the prevalence among institutionalized older adults is even higher.4 The recent COVID-19 pandemic made older adults even more susceptible to mistreatment, with one study reporting an 84% increase.5 Elder mistreatment may lead to a wide range of adverse health outcomes, including traumatic injuries, depression, and exacerbations of chronic illness.6 Previous research has shown that older adults experiencing mistreatment have increased rates of emergency department (ED) use7,8 and hospitalization,9 particularly in the 12 months before and 12 months after initial mistreatment identification.10 Recent research has also suggested that elder mistreatment victims are more likely during the 24 months surrounding mistreatment identification to present to the ED for injuries as well as for nonurgent issues and ambulatory care sensitive conditions (ACSCs),11 which may be prevented by outpatient primary care interventions.10 Hypothesized causes of this pattern of increased utilization of acute, unscheduled care include medical issues directly resulting from mistreatment as well as that elder mistreatment may lead to isolation and poor connection to outpatient care.
That older adults experiencing mistreatment have greater utilization of EDs and hospitals also suggests that they may have higher healthcare costs surrounding initial mistreatment identification. Studies focused on child abuse and intimate partner violence have found significantly higher healthcare costs among victims, both in the short-term and long-term, compared to non-victims.12-15 These increased costs represent a crucial component of the overall economic burden of these types of family violence. We know of no analogous research in elder mistreatment.
Using Medicare data, we examined the healthcare costs of legally adjudicated elder mistreatment victims in the 24 months surrounding the initial identification date compared to matched controls. We also categorized healthcare costs into acute/sub-acute/post-acute and ambulatory/outpatient /non-acute to provide a complete picture of the association of elder mistreatment with costs.
METHODS
Study Design and Subjects
We used Medicare data to examine healthcare costs among legally adjudicated older adults experiencing mistreatment in the 12 months before and 12 months after initial mistreatment identification in comparison to matched controls who had no documented exposure. Details of our approach have been published elsewhere.16 Briefly, we examined cohorts of older adults experiencing mistreatment who were from Brooklyn, New York17 and Seattle, Washington.18 These cohorts included a total of 503 cases initially identified in 2003-2012. The cases, which have been used in research previously,10,17,18 are unique: as the perpetrators have pled guilty or been convicted in criminal court, the occurrence of elder mistreatment has been verified. Also, for each case, the date when the mistreatment initially was identified by the authorities is known. Most commonly, initial identification occurred when the older adult experiencing mistreatment or another person called 911. Notably, when mistreatment was initially identified by the authorities, it may already have been ongoing for months or years. As we often did not have reliable information about when mistreatment began, we did not analyze it. Additionally, the actual legal adjudication may not have occurred until long after initial mistreatment identification by the authorities. We did not examine any dates related to adjudication. The Brooklyn cohort includes only cases of physical abuse, while the Seattle cohort includes physical abuse and other types of mistreatment.
Linking Cases to Medicare Data
We linked these cases to fee-for-service/traditional Medicare data to examine healthcare utilization. Fee-for-service Medicare is the largest repository of healthcare data for US older adults,19 offering comprehensive information about utilization of Medicare covered healthcare services. To link, we used social security number and/or a combination of sex, last name, date of birth, and residential zip code. Among those successfully linked, we included for analysis those continuously enrolled in traditional Medicare Parts A and B for the 12 months before and 12 months after initial mistreatment detection. The resulting sample contained 114 cases (23%). Among the 114 cases, the distribution of mistreatment types was: 54 physical abuse (47.4%), 51 financial exploitation (44.7%), 37 verbal/emotional/psychological abuse (32.5%), 2 neglect (1.8%), with 2 experiencing an unspecified type of mistreatment and 28 (24.6%) experiencing multiple types of mistreatment. Details of linking have been published elsewhere.10
Control Subjects
We selected from fee-for-service Medicare data a maximum of 4 controls per case, matched on age (+/−2 years), sex, race (white, non-white, unknown), and residential zip code (during the month of initial identification). We matched on these demographic criteria because of their known strong correlation with variations in healthcare utilization. Each control subject for a case was required to have had 12 months of continuous enrollment in Medicare before and 12 months including and after the month of the case’s mistreatment identification. The continuous enrollment requirement allowed us to compare healthcare costs incurred during the same time period between EM cases and their matched controls and removed insurance status as a potential explanation of any difference in healthcare costs. Controls were not required to have any healthcare utilization during the time period under study.
Measures of Healthcare Costs
The primary outcome we examined was total Medicare Parts A and B costs. This is the sum of all payment (made by Medicare, the patient, and third-party payers if any) for inpatient, outpatient, physician, home health, durable medical equipment (DME), and hospice care.20 We did not include prescription drug costs in our analysis (and thus did not require enrollment in Medicare Part D), as Part D went into effect in 2006, three years after the start of our study period.
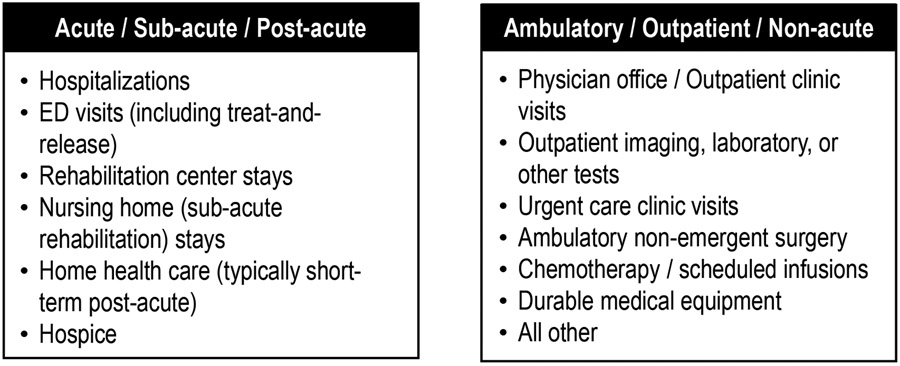
We broke total costs down into two meaningful sub-categories for analysis: acute/sub-acute/post-acute and ambulatory/outpatient/non-acute. We did this to differentiate costs from acute, unscheduled care (which typically has high cost) vs. outpatient, scheduled care (which typically has lower cost and may prevent or reduce use of unscheduled, acute care). This is because previous evidence that elder mistreatment may increase use of acute, unscheduled care.7-10 Figure 1 describes in detail the types of healthcare costs we included in each sub-category. Specifically, we based the categorization on the types of Medicare data files as well as information from the claim line records including: Revenue Center Codes, Healthcare Common Procedure Coding System (HCPCS) codes, and Place of Service codes. Details of our categorization strategy are shown in Online Supplementary Table 1. Notably, we included skilled nursing facility and home health care in acute/sub-acute/post-acute rather than ambulatory/outpatient/non-acute because these services, when covered by Medicare, are typically short-term and related to a specific medical need that is expected to improve. Longer-term custodial care that assists older adults with activities of daily living at home or in an institution is not covered by Medicare.21
Figure 1:
Types of Healthcare Encounters included in Acute/Sub-acute/Post-acute and Ambulatory/Outpatient/Non-acute Cost Sub-categories for Analysis
Time Period Examined Relative to Mistreatment Identification
For all measures of healthcare costs, we examined three time periods: 12 months before initial mistreatment identification, 12 months after identification (including the month of identification), and the 24 months surrounding identification (which includes both 12 months before and after initial mistreatment identification).
To provide additional insights regarding cost and its relationship to mistreatment identification date, we divided the 24-month period for each case into 6 equal-length sub-periods of 4 months, as in previous research.10 We labeled these periods, consistent with previous research, as: chronic pre-identification (360-241 days prior to mistreatment identification date), sub-acute pre-identification (240-121 days prior), acute pre-identification (120-1 day prior), identification/acute post-identification (mistreatment identification date-120 days post), sub-acute post-identification (121-240 days post), and chronic post-identification (241-360 days post).
Adjusting for HCC Score
To ensure comparability between cases and controls on underlying health conditions as well as other reasons to incur healthcare costs, we adjusted comparison between the cases and controls using Centers for Medicare and Medicaid Services Hierarchical Condition Categories (CMS-HCC) risk scores.22-25 CMS-HCC risk scores were designed to predict future healthcare costs for Medicare beneficiaries and use combinations of International Classification of Diseases (ICD) diagnostic codes in Medicare claims and demographic variables, including age, sex, Medicaid eligibility, and disability.25 Different risk score algorithms were developed (and updated annually) for Medicare enrollees who are dwelling in the community, institutionalized, new enrollees, or enrolled in Special Needs Plans. We used the algorithm developed for community-dwelling enrollees.
We decided to adjust for rather than match cases and controls on HCC scores because we were concerned about potential overmatching. Also, we recognized that, with a relatively small sample, increasing the number of factors on which we match would impair our ability to analyze cases because of inability to find a control. Notably, regression incorporating covariates can yield accurate estimates under mild imbalances between cases and controls but may encounter difficulties in scenarios of substantial imbalances. In this analysis, we did not find substantial imbalances in HCC scores, reducing concern about this.
For this study, we used the community risk score. For each case and controls matched on demographic characteristics, we calculated the CMS-HCC risk score using data from the 12 months before mistreatment identification. For cases with a mistreatment identification date between July 1 and December 31 of a year, we used the CMS algorithm pertaining to the calendar year of the mistreatment identification date. For cases with a mistreatment identification date between January 1 and June 30, we used the algorithm pertaining to the calendar year prior to mistreatment identification.
Statistical Analysis
We estimated generalized linear models (GLMs) of healthcare costs, with a Log link function and using the Modified Park Test to determine the distribution of the error term for each outcome we examined.26 For each outcome, we estimated an unadjusted and an adjusted (for CMS-HCC score) model. We derived robust standard errors by taking into account clustering of cases and controls in the same matched group. Given that initial identification of elder mistreatment may have coincided with admission to an ED or hospitalization, we conducted a sensitivity analysis by excluding all costs that were incurred on the same day of the initial identification. This sensitivity analysis was conducted to ensure that any increase in costs was not completely explained by the costs related to care for the event that precipitated identification.
Analysis was conducted within the CMS’s Virtual Research Data Center using Stata 17.0 within the Analytic Containers. The Weill Cornell Institutional Review Board approved this research. This work is reported based on STROBE guidelines (Online Supplementary Table 3 is checklist).27
RESULTS
We examined in detail healthcare costs for Medicare Parts A and B covered services for 114 legally adjudicated elder mistreatment cases and 410 matched controls over the 24 months surrounding mistreatment identification. Cases and controls were 64.9% female, with a median age of 72 and were 77.9% non-Hispanic white, 21.8% other race/ethnicity (11.3% black, 4.8% Asian, 1.2% North American native, 1.3% Hispanic, 3.2% Other race), and 0.4% of unknown race. Among cases at the time of their case identification, 104 (92.1%) were community-dwelling, 5 lived in senior living / retirement centers / assisted living settings, 1 lived in an adult family home, and 4 had unknown living setting.
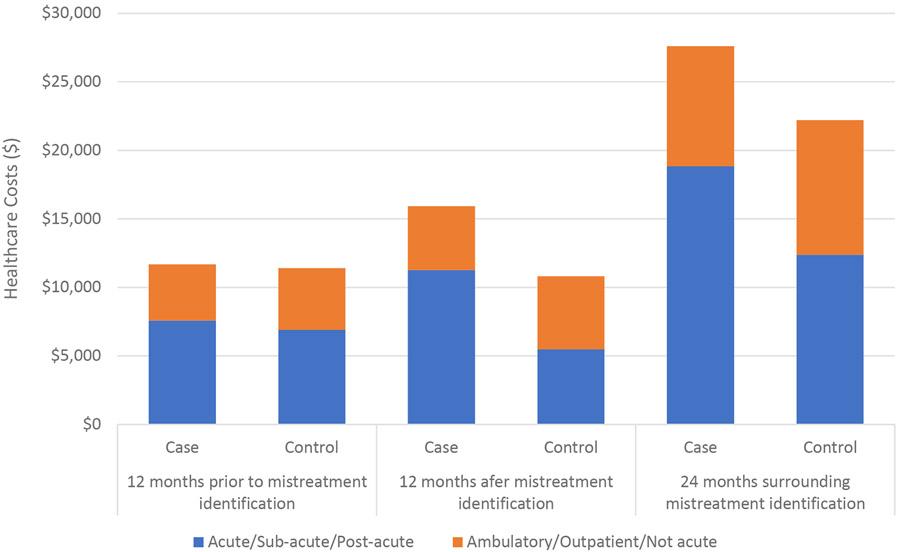
In unadjusted analyses (Figure 2), legally adjudicated elder mistreatment victims had higher Medicare Parts A and B costs over the 24 months surrounding initial mistreatment identification ($27,600 vs. 22,207, p=0.20) compared to their matched controls, though the difference was not statistically significant. While costs were similar between cases and controls in the 12 months prior to initial mistreatment identification ($11,673 vs. $11,402, p=0.92), cases had significantly higher total healthcare costs during the 12 months after initial mistreatment identification. ($15,927 vs. $10,805, p=0.04). Acute/sub-acute/post-acute costs were also higher in the 24 months surrounding initial mistreatment ($18,823 vs. $12,369, p=0.07), though this difference did not reach statistical significance. This difference in acute/sub-acute/post-acute costs was significant for the 12 months after initial mistreatment identification ($11,255 vs. $5,472, p=0.005), with a smaller difference in the 12 months before initial identification ($7,568 vs. $6,897, p=0.79) that did not achieve statistical significance. Notably, cases had lower nonacute/ambulatory/outpatient costs than controls in both the 12 months before ($4,106 vs. $4,505, p=0.50) and after ($4,672 vs. $5,334, p=0.42) mistreatment identification, but the differences did not achieve statistical significance. Acute/sub-acute/post-acute costs accounted for 70.7% of total Medicare Parts A and B costs among elder mistreatment victims during the 12 months after mistreatment identification compared to 50.6% among controls.
Figure 2:
Unadjusted Healthcare Costs in the 24 Months Surrounding Initial Mistreatment Identification for Legally Adjudicated Older Adults Experiencing Elder Mistreatment (n=114) and Matched Controls (n=410)
Adjusting for CMS-HCC scores yielded similar findings, shown in Table 1. Compared with controls, legally adjudicated elder mistreatment victims had a predicted incremental cost of $5,084 (95% confidence interval [$92, $10,077], p=0.046) in Medicare Parts A and B costs, and $5,817 (95% confidence interval [$1,271, $10,362], p=0.012) in acute/sub-acute/post-acute costs in the 12 months after initial mistreatment identification in comparison with controls. Again, we found lower predicted nonacute costs in both years among cases, but the differences were not statistically significant. (Table 1)
Table 1:
Predicted Healthcare Costs for Legally Adjudicated Older Adults Experiencing Elder Mistreatment (n=114) and Matched Controls (n=410) in the 24 Months Surrounding Initial Mistreatment Identification Adjusted for Centers for Medicare and Medicaid Services Hierarchical Condition Categories Risk Score and based on Generalized Linear Model
| Estimated Cost | Incremental costs associated with elder mistreatment (95% Confidence Interval) |
P value | ||
|---|---|---|---|---|
| Case | Control | |||
| Total Cost | ||||
| 24 months surrounding mistreatment identification | $28,320 | $22,051 | $6,269 (−$835, $13,373) | 0.08 |
| 12 months prior to mistreatment identification | $12,556 | $11,184 | $1,372 (−$2,599, $5,344) | 0.50 |
| 12 months after mistreatment identification | $15,896 | $10,811 | $5,084 ($92, $10,077) | 0.05 |
| Acute/Sub-acute/Post-acute | ||||
| 24 months surrounding mistreatment identification | $20,039 | $12,164 | $7,875 ($973, $14,776) | 0.03 |
| 12 months prior to mistreatment identification | $8,870 | $6,628 | $2,243 (−$2,013, $6,498) | 0.30 |
| 12 months after mistreatment identification | $11,285 | $5,468 | $5,817 ($1,271, $10,362) | 0.01 |
| Ambulatory/Outpatient/Not acute | ||||
| 24 months surrounding mistreatment identification | $10,281 | $11,114 | −$833 (−$3,175, $1,510) | 0.49 |
| 12 months prior to mistreatment identification | $4,946 | $5,154 | −$208 (−$1,486, $1,070) | 0.75 |
| 12 months after mistreatment identification | $5,354 | $5,966 | −$612 (−$2,049, $825) | 0.40 |
Examining costs in the six subperiods revealed that the significantly higher total costs and acute/sub-acute/post-acute costs among legally adjudicated elder mistreatment victims in the post-identification year were concentrated in the first 120 days after mistreatment detection. (Figure 3). Toal costs were significantly higher in this first 120 days for cases vs. controls ($8,705 vs. $3,312, p=0.003), as were acute/sub-acute/post-acute costs ($7,154 vs. $1,463, p=0.002).
Figure 3:
Predicted Healthcare Costs for Legally Adjudicated Older Adults Experiencing Elder Mistreatment (n=114) in the Time Periods Surrounding Initial Mistreatment Identification in Comparison to Matched Controls (n= 410)
We found similar results from the sensitivity analysis excluding all claims on the initial mistreatment identification date. (Online Supplementary Figures 1,2 and Table 2)
DISCUSSION
This is, to our knowledge, the first study to examine the association of elder mistreatment with healthcare costs. We found that, compared with controls, legally adjudicated older adults experiencing elder mistreatment had similar total healthcare costs during the 12 months prior to mistreatment identification but substantially higher total costs during the 12 months after mistreatment identification. This finding persists after adjustment for CMS-HCC risk score. This higher total cost was driven by an increase in acute/sub-acute/post-acute costs, which represented a much larger percentage of total costs for cases than controls.
By demonstrating higher healthcare costs for legally adjudicated elder mistreatment victims, our findings provide evidence of the financial impact of the phenomenon. These findings highlight the potential value of identification, intervention, and prevention, providing support to the business case for devoting resources to address this issue. To date, few have attempted to quantify the healthcare costs associated directly and indirectly with elder mistreatment or to project the potential financial impact of programs to address it. Fullin and colleagues in 1994 estimated that elder mistreatment added $5.3 billion to annual US healthcare expenditures,28 but the details of this analysis were not published, and more recent analyses have not been reported. Expanding on the findings we report here and performing additional analyses is critical to offer tools to policymakers to assess make decisions about funding elder mistreatment programs.
Our finding that the cost increase was driven primarily by an increase in acute/sub-acute/post-acute costs is consistent with findings of our previous research in that older adults experiencing elder mistreatment used the ED and hospital more frequently than other older adults, including in non-optimal ways (e.g. ED visits and hospitalizations for ACSCs, low-urgency ED visits). 10 Connecting older adults experiencing elder mistreatment more effectively to outpatient and preventative care, which is typically less expensive, may be impactful in reducing healthcare costs for these older adults. Additionally, it may avert exacerbations of health conditions and mistreatment-related health issues that then require acute, unscheduled care.16 Nevertheless, the novel analytic approach we used here to sub-categorize health care costs from insurance claims into acute/sub-acute/post-acute vs. nonacute/ambulatory/outpatient may also be useful in exploring the costs associated with other health conditions and trends over time.
Increases in cost existed in the year after mistreatment identification and were concentrated in the 120 days immediately after mistreatment identification. This finding is likely at least partially explained by the costs associated with treating the injuries sequelae of the mistreatment that precipitated identification. Additionally, though, it is possible that identifying elder mistreatment may lead to detection of other previously unmanaged health issues in older adults not well-connected to the healthcare system. That the costs after 120 days return to a level similar to other older adults suggests potentially that it is possible to address and stabilize these issues, and that elevated healthcare costs don’t continue indefinitely among older adults experiencing elder mistreatment after identification. Future research is needed to examine impact on healthcare costs of elder mistreatment over a longer time window.
Also, though costs were similar in the year prior to mistreatment identification, they were higher (though the difference did not reach statistical significance) in the 120 days prior to mistreatment identification. Though not statistically significant, this may suggest an elevated level of healthcare utilization during this period potentially with missed opportunities for early detection.
Limitations
This study has several limitations. Due to the requirement to link cases to Medicare data and for 24 months of continuous enrollment in fee-for-service Medicare surrounding mistreatment identification, we were unable to include most of the elder mistreatment cases from our study cohorts. Additionally, the small number of cases we examined had elder mistreatment that was identified and successfully adjudicated by the legal system. Such individuals represent a small percentage of all EM cases, and older adults analyzed here may have experienced more acute or severe mistreatment than other victims, allowing identification. Less intensive cases of mistreatment that are more challenging to detect and prosecute may not have been included. Cases examined in this article also may reflect older adults with a better support system (compared to those with similar experience of EM but not identified and adjudicated), increased ability to report mistreatment, and better healthcare and legal literacy. As a result, they may be a biased rather than representative subset of elder mistreatment victims.
The cost of healthcare services provided to an older adult depends on factors beyond the services themselves. The same services may be billed very differently by different providers or institutions. Therefore, the variations in healthcare costs between cases and controls described here may be partially due to the billing practices of those providing the care. Given that in many cases, the elder mistreatment triggering identification also led directly to an ED visit and potential hospitalization, some of the higher costs that we found could be explained by this. We conducted a sensitivity analysis by excluding costs of ED visits and hospitalizations on the day of mistreatment identification, though, and our findings persisted. Further, this research relies on evaluation of administrative data, which was designed for billing rather than research and may have incomplete or inconsistent information. Notably, this may have impacted our effort to accurately sub-categorize costs into meaningful categories. Our small sample size prevented us from further sub-dividing costs into additional categories. Future research with a larger sample would be helpful to provide insights.
Conclusion
We found that older adults experiencing elder mistreatment that was legally adjudicated had higher healthcare costs in the year after initial mistreatment identification, primarily driven by an increase in acute/subacute/post-acute costs. That all of the small number of cases examined were legally adjudicated reduces the generalizability of our findings. Additional research is needed to further characterize the higher costs we found and explore this issue using a larger and more representative group of EM victims.
Supplementary Material
Online Supplementary Table 1: Strategy for Categorization of Medicare Fee-for-Service Insurance Claims as Acute/Sub-acute/Post-acute vs. Ambulatory/Outpatient/Non-acute
Online Supplementary Figure 1: Healthcare Costs in the Two Years Surrounding Abuse Detection, Excluding Healthcare Services on the Detection Date
Online Supplementary Table 2: Predicted Healthcare Costs Based on Generalized Linear Model, Excluding Healthcare Services on the Detection Date
Online Supplementary Figure 2: Predicted Healthcare Costs in the 6 Subperiods, excluding Healthcare Services on the Detection Date
Online Supplementary Table 3: STROBE Guidelines Checklist
KEY POINTS.
Older adults experiencing elder mistreatment had similar total healthcare costs during the 12 months prior to mistreatment identification compared to other older adults but substantially higher total costs during the 12 months after mistreatment identification.
This higher total cost in the 12 months after identification was driven by an increase in acute/sub-acute/post-acute costs, which represented a much larger percentage of total costs for elder mistreatment victims than non-victim controls.
The significantly higher total costs and acute/sub-acute/post-acute costs among elder mistreatment victims in the post-year were concentrated in the 120 days after mistreatment identification.
WHY DOES IT MATTER?
These quantitative findings suggest the potential impact of elder mistreatment on healthcare costs. This may inform policymakers and highlights the potential value of identification, intervention, and prevention.
ACKNOWLEDGEMENTS
Conflicts of Interest:
Financial Conflicts: Our work has been supported by a grant from the National Institute on Aging (R01 AG060086). E-Shien Chang’s participation was supported by K01 AG081540 from the National Institute on Aging. The funders have not been involved in the design or conduct of the research.
Personal Conflicts: The authors have nothing to disclose.
Full or adequate disclosure: Other than the funding listed above, the authors have nothing to disclose.
Disclosures:
Grants: Our work has been supported by a grant from the National Institute on Aging (R01 AG060086). E-Shien Chang’s participation was supported by K01 AG081540 from the National Institute on Aging. The funders have not been involved in the design or conduct of the research.
Conflicts of Interest: None other than the grant listed above
Footnotes
Sponsor’s Role: The funders were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
REFERENCES
- 1.Hall JE, Karch DL, Crosby AE. Elder Abuse Surveillance: Uniform Definitions and Recommended Core Data Elements For Use In Elder Abuse Surveillance. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. 2016; [Google Scholar]
- 2.Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. Feb 2010;100(2):292–7. doi: 10.2105/AJPH.2009.163089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosay ABP, Mulford CFP. Prevalence estimates and correlates of elder abuse in the United States: The National Intimate Partner and Sexual Violence Survey. J Elder Abuse Negl. Jan-Feb 2017;29(1):1–14. doi: 10.1080/08946566.2016.1249817 [DOI] [PubMed] [Google Scholar]
- 4.Yon Y, Ramiro-Gonzalez M, Mikton CR, Huber M, Sethi D. The prevalence of elder abuse in institutional settings: a systematic review and meta-analysis. Eur J Public Health. Feb 1 2019;29(1):58–67. doi: 10.1093/eurpub/cky093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang ES, Levy BR. High Prevalence of Elder Abuse During the COVID-19 Pandemic: Risk and Resilience Factors. Am J Geriatr Psychiatry. Nov 2021;29(11):1152–1159. doi: 10.1016/j.jagp.2021.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lachs MS, Pillemer KA. Elder Abuse. N Engl J Med. Nov 12 2015;373(20):1947–56. doi: 10.1056/NEJMra1404688 [DOI] [PubMed] [Google Scholar]
- 7.Lachs MS, Williams CS, O'Brien S, et al. ED use by older victims of family violence. Ann Emerg Med. Oct 1997;30(4):448–54. doi: 10.1016/s0196-0644(97)70003-9 [DOI] [PubMed] [Google Scholar]
- 8.Dong X, Simon MA. Association between elder abuse and use of ED: findings from the Chicago Health and Aging Project. Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't. Am J Emerg Med. Apr 2013;31(4):693–8. doi: 10.1016/j.ajem.2012.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dong X, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. May 27 2013;173(10):911–7. doi: 10.1001/jamainternmed.2013.238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosen T, Zhang H, Wen K, et al. Emergency Department and Hospital Utilization Among Older Adults Before and After Identification of Elder Mistreatment. JAMA Network Open. 2023;6(2):e2255853–e2255853. doi: 10.1001/jamanetworkopen.2022.55853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Purdy S, Griffin T, Salisbury C, Sharp D. Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health. Feb 2009;123(2):169–73. doi: 10.1016/j.puhe.2008.11.001 [DOI] [PubMed] [Google Scholar]
- 12.Brown DS, Fang X, Florence CS. Medical costs attributable to child maltreatment a systematic review of short- and long-term effects. Am J Prev Med. Dec 2011;41(6):627–35. doi: 10.1016/j.amepre.2011.08.013 [DOI] [PubMed] [Google Scholar]
- 13.Florence C, Brown DS, Fang X, Thompson HF. Health care costs associated with child maltreatment: impact on medicaid. Pediatrics. Aug 2013;132(2):312–8. doi: 10.1542/peds.2012-2212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones AS, Dienemann J, Schollenberger J, et al. Long-term costs of intimate partner violence in a sample of female HMO enrollees. Womens Health Issues. Sep-Oct 2006;16(5):252–61. doi: 10.1016/j.whi.2006.06.007 [DOI] [PubMed] [Google Scholar]
- 15.Rovi S, Chen PH, Johnson MS. The economic burden of hospitalizations associated with child abuse and neglect. Am J Public Health. Apr 2004;94(4):586–90. doi: 10.2105/ajph.94.4.586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosen T, Bao Y, Zhang Y, et al. Identifying patterns of health care utilisation among physical elder abuse victims using Medicare data and legally adjudicated cases: protocol for case-control study using data linkage and machine learning. BMJ Open. Feb 5 2021;11(2):e044768. doi: 10.1136/bmjopen-2020-044768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosen T, LoFaso VM, Bloemen EM, et al. Identifying Injury Patterns Associated With Physical Elder Abuse: Analysis of Legally Adjudicated Cases. Ann Emerg Med. Sep 2020;76(3):266–276. doi: 10.1016/j.annemergmed.2020.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dion S, Gogia K, Elman A, et al. Developing a rigorous, systematic methodology to identify and categorize elder mistreatment in criminal justice data. J Elder Abuse Negl. Jan-Feb 2020;32(1):27–45. doi: 10.1080/08946566.2020.1733725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mues KE, Liede A, Liu J, et al. Use of the Medicare database in epidemiologic and health services research: a valuable source of real-world evidence on the older and disabled populations in the US. Clin Epidemiol. 2017;9:267–277. doi: 10.2147/CLEP.S105613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frank B. Definitions of ‘Cost’ in Medicare Utilization Files. ResDAC. Accessed November 14, 2022. https://resdac.org/sites/datadocumentation.resdac.org/files/Definitions%20of%20%27Cost%27%20in%20Medicare%20Utilization%20Files%20%28Slides%29.pdf [Google Scholar]
- 21.Grabowski DC. Medicare and Medicaid: conflicting incentives for long-term care. Milbank Q. Dec 2007;85(4):579–610. doi: 10.1111/j.1468-0009.2007.00502.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fortuna RJ, Clark JS, Johnson WE, et al. Association Between Physician Risk Assessment, Hierarchical Condition Categories, and Utilization of Medical Services. Popul Health Manag. Apr 2021;24(2):249–254. doi: 10.1089/pop.2019.0236 [DOI] [PubMed] [Google Scholar]
- 23.Li P, Kim MM, Doshi JA. Comparison of the performance of the CMS Hierarchical Condition Category (CMS-HCC) risk adjuster with the Charlson and Elixhauser comorbidity measures in predicting mortality. BMC Health Serv Res. Aug 20 2010;10:245. doi: 10.1186/1472-6963-10-245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehta HB, Dimou F, Adhikari D, et al. Comparison of Comorbidity Scores in Predicting Surgical Outcomes. Med Care. Feb 2016;54(2):180–7. doi: 10.1097/MLR.0000000000000465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watson MM. Documentation and Coding Practices for Risk Adjustment and Hierarchical Condition Categories. AHIMA; 2018. https://bok.ahima.org/doc?oid=302516#.ZEG3SnZKiZQ [Google Scholar]
- 26.Glick H. Identifying an appropriate link and family for generalized linear models. https://drhenryglick.com/wp-content/uploads/2021/05/ispor15.glmworkshop.glick_.052021pdf.pdf [Google Scholar]
- 27.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. Oct 16 2007;147(8):573–7. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 28.Mouton CP, Rodabough RJ, Rovi SL, et al. Prevalence and 3-year incidence of abuse among postmenopausal women. Am J Public Health. Apr 2004;94(4):605–12. doi: 10.2105/ajph.94.4.605 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplementary Table 1: Strategy for Categorization of Medicare Fee-for-Service Insurance Claims as Acute/Sub-acute/Post-acute vs. Ambulatory/Outpatient/Non-acute
Online Supplementary Figure 1: Healthcare Costs in the Two Years Surrounding Abuse Detection, Excluding Healthcare Services on the Detection Date
Online Supplementary Table 2: Predicted Healthcare Costs Based on Generalized Linear Model, Excluding Healthcare Services on the Detection Date
Online Supplementary Figure 2: Predicted Healthcare Costs in the 6 Subperiods, excluding Healthcare Services on the Detection Date
Online Supplementary Table 3: STROBE Guidelines Checklist