Abstract
Tinnitus is highly prevalent among military Veterans. Severe tinnitus can be associated with negative impacts on daily life. Veterans with severe tinnitus may also have greater difficulties in functional roles, including work. However, few studies have explicitly explored this relationship. Traumatic brain injury (TBI), also prevalent among Veterans, is associated with tinnitus and can additionally impair work functioning. This quantitative investigation used a population-based survey to assess the relationship between tinnitus severity, measured using the Tinnitus Functional Index (TFI), and the impact of tinnitus on work, measured using a composite score from the Tinnitus History Questionnaire, among a stratified random sample of VA healthcare-using Veterans diagnosed with tinnitus, with and without comorbid TBI. Analyses were weighted to account for sampling design and Veteran non-response; multiple imputation was used to account for missing data. Results indicated that for every 1-point increase in TFI score, there was an average 8% increase in the odds of reporting a high level of impact on work functioning (OR: 1.08; 95% CI: 1.06, 1.11). Veterans with a comorbid TBI diagnosis, compared with those without, were more likely to have high tinnitus-related impact on work functioning (OR: 2.69, 95% CI: 1.85, 3.91), but the relationship between tinnitus severity and the impact of tinnitus on work functioning did not differ by TBI status. These data can help researchers and clinicians understand complex symptoms experienced by Veterans with tinnitus, with and without TBI, supporting the improved provision of clinical services to these patients.
Keywords: disability, tinnitus, traumatic brain injury, Veterans, work functioning
Tinnitus is characterized by a phantom auditory perception of sound, typically in the form of buzzing, ringing, or high-pitched whistling, in the absence of an objective external stimulus (Jastreboff 1990). The most common cause of tinnitus is noise exposure (Axelsson & Sandh 2009; National Research Council (US) Committee on Hearing 1982), although age and traumatic brain injury (TBI) are also commonly implicated (Hoffman & Reed 2004). Tinnitus is a major concern for the U.S. military and the Department of Veterans Affairs (VA). Among males aged ≥20 years in the United States, the prevalence of chronic tinnitus in former military service members is estimated to be 2.3 times greater than in those without a history of military service (11.7 vs. 5.4%, respectively; Folmer et al. 2011). Additionally, according to the Veterans Benefits Administration's Annual Benefits Report, tinnitus is the most prevalent military service-related disability condition among Veterans—over 2.3 million received tinnitus-related disability payments in fiscal year 2020 alone (US Department of Veterans Affairs 2020).
The degree of severity and impact of symptoms vary greatly among individuals with tinnitus. For many, tinnitus goes away on its own or does not cause excess stress (Hoffman & Reed 2004). However, others can experience persistent, bothersome tinnitus, and have symptoms that can substantially affect their sleep, concentration, emotional stability, and quality of life (Clarke et al. 2020; Holmes & Padgham 2009). Past research has also identified associations between tinnitus and several domains of cognitive functioning, including working memory, executive functioning, processing speed, and verbal abilities (Eggermont & Roberts 2004; Langguth et al. 2011; Mohamad et al. 2016; Sherlock & Brungart 2021).
Given the potential for emotional, mental, and psychosocial impacts, it is likely that some individuals with tinnitus also have difficulties working and/or functioning in workplace environments. Past research supports this notion. For example, in a qualitative study of individuals with tinnitus, Colagrosso et al. (2019) reported that tinnitus caused interferences with participants' work functioning. Additionally, in nationally representative data from the 2007 National Health Interview Survey, Bhatt et al. (2017) found that individuals with tinnitus reported significantly more missed workdays than those without tinnitus. And, in a sample of current and recent military service members, Henry et al. (2019) reported that 10 to 27% of service members and 15 to 28% of Veterans reported varying types of work limitations due to their tinnitus. Despite these findings, the interplay between tinnitus, tinnitus severity, and work limitations has not been adequately explored, particularly among military Veterans, for whom it is critically important to understand the multiple complicating factors contributing to post-military adjustment to civilian work (Keeling et al. 2018).
The study of the potential interaction between tinnitus and TBI history among service members and Veterans may also warrant more attention than it receives at present. TBI, prevalent among military service members and Veterans, is often co-diagnosed with tinnitus; TBI symptoms and sequelae may exacerbate the negative influence of tinnitus on work functioning (Carlson et al. 2019; Henry et al. 2012; Lew et al. 2007; Silverberg et al. 2018). Mutual reinforcement of symptoms linked to TBI and tinnitus may produce substantial challenges to patients' work functioning.
Understanding the impact that tinnitus, both with and without comorbid TBI, has on work functioning could inform the diagnostic, management, and rehabilitation services provided to Veterans, whether in the VA or in other healthcare systems that care for individuals with these conditions. Therefore, in this study, we examined associations between tinnitus severity and self-reported work functioning in a generalizable, national sample of Veterans who use VA healthcare and were diagnosed with tinnitus, both with and without comorbid TBI.
Methods
Overview
This quantitative study utilized data from a population-based survey of Veterans who used VA healthcare and were diagnosed with tinnitus between October 1, 2011, and September 30, 2016. Randomly sampled Veterans were sent a survey asking them to report the severity of their tinnitus and its impact on their daily functioning. Those who completed the survey received $20 compensation. This study's design and implementation was approved by the VA Portland Health Care System Institutional Review Board (IRB) and Research and Development Committees.
Study Sample
Data from the VA Corporate Data Warehouse, which holds healthcare records of all Veterans receiving VA services, were used to identify the ∼8 million Veterans who used VA health services nationally, at least once, during the study period. An initial random sample of 10% of VA users was generated from this population. Veterans were excluded from the sample if they were deceased, were enrolled in palliative care, or had not received VA outpatient care during the study period. Among 715,400 remaining Veterans, we retained 20,873 who were diagnosed with tinnitus, operationalized as having received one or more tinnitus diagnoses during an inpatient stay, or two or more diagnoses during separate outpatient visits, during the 5-year study period. This definition, used to reduce the likelihood of false-positive classifications, has been used in previous research in which International Classification of Diseases (ICD) diagnosis codes from administrative data were used to identify diagnoses of interest (e.g., Carlson et al. 2018, 2019; Trivedi et al. 2015). We used ICD—9th Revision—Clinical Modification (ICD-9-CM) codes to identify diagnoses assigned through September 30, 2015, and ICD-10-CM codes to identify those assigned after October 1, 2015; equivalent diagnoses between the two systems were identified using a mapping table published by the Centers for Medicare & Medicaid Services.
Among Veterans diagnosed with tinnitus, we then identified those who (1) used VA healthcare services within the prior year (to ensure the most up-to-date mailing addresses); (2) were noninstitutionalized; (3) were not missing a recorded age and were <90 years of age; and (4) had a complete mailing address. The age cut-point was used to maximize the likelihood of reaching independently living Veterans who were most likely to receive outpatient tinnitus rehabilitation services, as this was the target population for the research study. From the remaining 19,867 Veterans, we selected 1,800 individuals using stratified random sampling (see Fig. 1 for flow diagram). A total of 300 Veterans were sampled from each of six strata, which were created using age categories (<30; 30–40; >40 years of age) and TBI diagnosis status (yes/no), based on the same criteria used to identify tinnitus diagnoses in Veterans' healthcare records. The ICD codes used to identify tinnitus, TBI, and other diagnoses of interest are available upon request.
Figure 1.
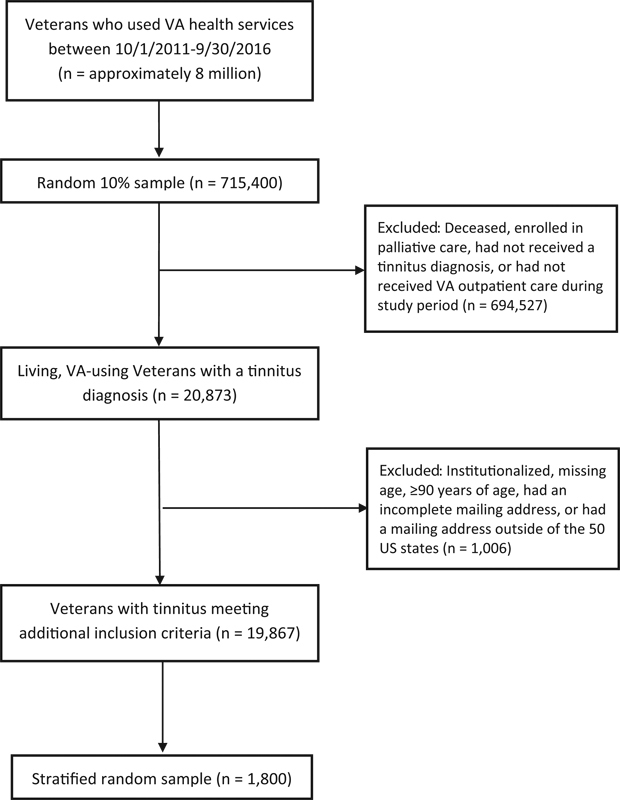
Flow diagram of study participants based on inclusion and exclusion criteria.
Survey Procedures
The final sample of 1,800 Veterans were mailed information by U.S. Mail about participating in the study. To help maximize the response rate, survey mailings were conducted following Dillman's Tailored Design Method (Millar & Dillman 2011), modified slightly to meet VA and IRB stipulations. Veterans were mailed an initial introductory letter, followed by a full survey packet, and then a separate reminder notice. This first mailing was followed by a second full survey packet and a subsequent reminder notice, and then by a final survey packet, sent by express courier service, followed by a final reminder notice by mail. Survey packets included a letter describing the study's purpose, an information sheet that met requirements for informed consent, a paper survey booklet, instructional materials, and a pre-paid return envelope. Instructions for completing the survey online, as an alternative to the paper booklet, were also included. The online version of the survey was created using REDCap (Research Electronic Data Capture), a secure, internet-based research platform hosted at Oregon Health and Science University (Harris et al. 2009, 2019).
Measures
Dependent variable. The level of impact of tinnitus on an individual's work or other activities (hereafter referred to as “work functioning”) was assessed using items from the Tinnitus History Questionnaire (THQ), a frequently used clinical questionnaire that includes items for scaling the emotional impact of tinnitus, hearing problems associated with tinnitus, and general health (Meikle et al. 2012; Theodoroff 2021). For this analysis, we included the following seven work functioning-related questions with binary (yes/no) response options: Over the past six months, because of your tinnitus, have you: (1) had to take frequent rests when doing work or other activities; (2) cut down on the amount of time you spend on work or other activities; (3) accomplished less than you would like; (4) did not do work or other activities as carefully as usual; (5) were limited in the kind of work you do or other activities; (6) had difficulty performing work or other activities; and (7) needed special assistance (from others or special devices). A composite score representing overall limitations in work functioning was created based on the proportion of affirmative responses over the total number of responses (a minimum of six completed responses were required to retain the measure for analysis). Thus, for a respondent who completed all seven items, a score of 1.0 represents affirmative responses to all seven questions, while a score of 0 indicates no affirmative responses. Using the range of resulting composite scores, we created a binary variable representing those whose tinnitus had a high impact on their work (0.8–1.0), versus all other participants whose tinnitus had none or a low impact on their work (0 to < 0.8). The cut-point for these categories was based on the top tertile of composite scores.
Independent variable. Tinnitus severity was measured using the Tinnitus Functional Index (TFI), a self-report questionnaire that is validated for quantifying tinnitus severity and treatment-related change (Chandra et al. 2018; Henry et al. 2016; Meikle et al. 2012). The TFI consists of 25 items with Likert-type response options corresponding to values from 0 to 10. The overall TFI score is obtained by multiplying the mean of all responses by 10, with overall scores ranging from 0 to 100; lower scores equate to less intrusive tinnitus symptoms and higher scores represent more burdensome or even debilitating problems with tinnitus. The 25 TFI items can also be grouped into eight subdomains: Auditory, Cognitive, Control, Emotional, Intrusive, Quality of Life, Relaxation, and Sleep. The method for calculating TFI subdomain scores follows the method for calculating total TFI scores, with scores similarly ranging from 0 to 100. In the current analyses, TFI total scores and subdomain scores were analyzed as continuous variables. The literature recommends the following TFI severity categories, which were also used to help interpret data: 0–17 = tinnitus is not a problem; 18–31 = tinnitus is a small problem; 32–53 = tinnitus is a moderate problem; 54–72 = tinnitus is a big problem; and 73–100 = tinnitus is a very big problem (Henry et al. 2016).
Covariates. Demographic and military service information was measured using VA administrative data and Veterans' responses to survey items. Categories within each variable were defined based on prior research, meaningfulness in regard to the independent and dependent variables of interest, and ensuring sufficient observations at each level to conduct robust multivariable modeling. These variables included age at the time of survey distribution (categorized as <30, 30–40, and >40 years), sex (male vs. female), race (Black or African American; White; and non-White, non-Black, or unknown), marital status (married/in a relationship vs. separated/divorced/single), education level (high school diploma; some college or vocational degree; and college graduate or more), annual household income (<$25,000; $25,000–$74,999; and ≥$75,000), military branch (Air Force; Army; Coast Guard/Navy; and Marines), duration of military service (≤4; 5–10; and >10 years), VA service-connected disability status (no service-connected disability; service-connected disability at 0 to < 50%; and service-connected disability at ≥50%), subjective hearing function (categorized as excellent or good; a little or moderate trouble hearing; and a lot of trouble hearing, or deaf), and overall health (excellent, very good, or good vs. fair or poor). Self-reported depression and anxiety were measured in the survey using the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith 1983), as previously reported (Prewitt et al. 2021). Depression and anxiety were defined based on scores of 8 or higher on the seven depression and seven anxiety screening questions, respectively. Finally, using the same approach used to identify Veterans' tinnitus and TBI diagnosis status, we also extracted Veterans' diagnoses for any mental health disorder, posttraumatic stress disorder (PTSD), and pain during the 5-year study period.
Data Analysis
Inverse probability weighting was used to account for the stratified sampling design as well as survey non-response (Little 1986). We also used multiple imputation by chained equations to impute missing data for all variables, including covariates (missingness for individual variables in the dataset ranged from 0.3 to 5.2%). Results of analyses using imputed data were compared with those based on non-imputed data and no meaningful differences were observed; imputed results are presented.
Descriptive analyses were conducted for demographic characteristics, military history variables, clinical and self-reported health characteristics, and tinnitus severity (overall TFI score and the eight subdomains, separately). Population proportions and means were estimated for each variable with 95% confidence intervals (CIs). We then cross-tabulated the data by the two-category work functioning variable (high impact vs. none/low impact) to examine associations between variables. Bivariable logistic regression models were used to calculate odds ratios (ORs) and 95% CIs to estimate the strength of the associations between Veteran characteristics, tinnitus severity, and high tinnitus-related impact on work functioning. Multivariable logistic regression models were then used to estimate associations between tinnitus severity and tinnitus-related work functioning while controlling for possible confounding. Covariates included in the models were selected based on a directed acyclic graph (Sauer & VanderWeele 2013), a copy of which is available upon request. We additionally estimated the average marginal effects, or predicted probability, of high tinnitus impact on work function by TFI score for straightforward interpretation of the association.
We conducted a stratified analysis to examine whether any observed associations between tinnitus severity and work functioning differed by Veterans' TBI diagnosis status. Population means and 95% CIs were calculated for overall TFI scores and each of the eight TFI subdomains among Veterans with and without a TBI diagnosis. For each stratum, we then ran multivariable logistic regression models to estimate associations between tinnitus severity and work functioning while controlling for potential confounders. Resulting ORs and 95% CIs were compared for notable differences between Veterans with and without TBI diagnosis. Multiple imputation procedures, survey weighting calculation, and data analyses were conducted in Stata software version 17.0 (StataCorp 2021).
Results
Among 1,800 Veterans who were mailed surveys, 110 (6.1%) were returned as undeliverable, 10 (0.5%) were returned with a message that the Veteran was deceased, and 789 did not respond (43.8%). A total of 891 completed surveys were returned (adjusted response rate = 53% of those not undeliverable). Among the completed surveys, 692 (77.7%) were returned by U.S. Mail and 199 (22.3%) were submitted online using REDCap.
Characteristics of Veteran VA Users Diagnosed with Tinnitus
Table 1 presents population characteristics based on weighted data (i.e., representing the entire sampling frame). Most of the population was male (95.6%; 95% CI: 93.6, 97.7), white (74.8%; 95% CI: 70.2, 79.5), and married or in a relationship (72.9%; 95% CI: 68.0, 77.8). About half of the population had at least some college education or vocational training (51.4%; 95% CI: 45.8, 57.1) and 60.4% (95% CI: 54.6, 66.2) had an annual household income of $25,000 to $75,000. Over half of the population served in the Army (58.0%; 95% CI: 52.6, 63.4) and 59.6% (95% CI: 54.2, 64.6) had a service duration of ≤4 years. During the study period, 5.6% (95% CI: 4.8, 6.4) received a TBI diagnosis from their VA healthcare providers; 29.5% (95% CI: 24.8, 34.1) received a PTSD diagnosis, 56.7% (95% CI: 51.3, 62.0) received any mental health disorder diagnosis, and 75.4% (95% CI: 70.6, 80.2) received a pain diagnosis.
Table 1. Population characteristics of Veteran VA users diagnosed with tinnitus, by tinnitus-related impact on work functioning.
| Level of tinnitus-related impact on work functioning | |||||
|---|---|---|---|---|---|
| High n = 239 (17.0%; 95% CI: 13.0, 21.0) |
None/Low n = 630 (83.0%; 95% CI: 79.0, 87.0) |
||||
| Veteran characteristics | n | Proportion (95% CI) | n | Proportion (95% CI) | Bivariable OR (95% CI) |
| Demographics | |||||
| Age (y) | |||||
| < 30 | 12 | 11.2 (4.4, 18.1) | 62 | 88.8 (81.9, 95.6) | Reference |
| 30–40 | 64 | 26.9 (20.0, 33.8) | 156 | 73.1 (66.2, 80.0) | 2.9 (1.3, 6.3) |
| > 40 | 163 | 16.4 (12.1, 20.8) | 412 | 83.6 (79.2, 87.9) | 1.6 (0.7, 3.3) |
| Sex | |||||
| Male | 221 | 17.1 (13.0, 21.3) | 593 | 82.9 (78.8, 87.0) | Reference |
| Female | 18 | 14.0 (6.8, 26.0) | 37 | 86.0 (76.6, 95.4) | 0.8 (0.3, 1.8) |
| Race | |||||
| Black/African American | 37 | 32.3 (17.1, 47.6) | 61 | 67.7 (52.4, 83.0) | Reference |
| Non-White/non-Black/unknown | 31 | 16.4 (5.7, 27.1) | 72 | 83.6 (72.9, 94.3) | 0.4 (0.1, 1.2) |
| White | 171 | 14.7 (10.5, 19.0) | 499 | 85.3 (81.0, 89.5) | 0.4 (0.2, 0.8) |
| Marital status | |||||
| Married/in relationship | 165 | 17.9 (13.1, 22.7) | 427 | 82.1 (77.3, 86.9) | Reference |
| Separated/divorced/single | 71 | 14.6 (7.5, 21.7) | 193 | 85.4 (78.3, 92.5) | 0.8 (0.4, 1.5) |
| Education level | |||||
| High-school diploma | 41 | 12.8 (4.4, 21.2) | 102 | 87.2 (78.8, 95.6) | Reference |
| Some college/vocational degree | 126 | 21.6 (15.3, 27.8) | 330 | 78.4 (72.2, 84.7) | 1.9 (0.8, 4.4) |
| College graduate or more | 67 | 11.6 (5.7, 17.5) | 188 | 88.4 (82.5, 94.3) | 0.9 (0.3, 2.4) |
| Annual household income | |||||
| < $25,000 | 68 | 28.5 (17.0, 40.0) | 100 | 71.5 (60.0, 83.0) | Reference |
| $25,000–$74,999 | 122 | 14.2 (9.5, 18.9) | 367 | 85.8 (81.1, 90.5) | 0.4 (0.2, 0.8) |
| ≥$75,000 | 35 | 13.6 (5.0, 22.2) | 129 | 86.4 (77.8, 95.0) | 0.4 (0.2, 1.0) |
| Level of service connection | |||||
| Not service connected | 28 | 17.3 (8.8, 25.9) | 105 | 82.7 (74.1, 91.2) | Reference |
| < 50% service connected | 40 | 12.1 (5.2, 19.0) | 147 | 87.9 (81.1, 94.8) | 0.7 (0.3, 1.6) |
| ≥50% service connected | 171 | 19.7 (13.9, 25.6) | 378 | 80.3 (74.4, 86.1) | 1.2 (0.6, 2.4) |
| Military service characteristics | |||||
| Military service branch | |||||
| Air Force | 20 | 14.1 (4.3, 23.9) | 76 | 85.9 (76.1, 95.7) | Reference |
| Army | 147 | 18.3 (12.9, 23.7) | 368 | 81.7 (76.3, 87.1) | 1.4 (0.6, 3.3) |
| Coast Guard/Navy | 34 | 11.6 (3.4, 19.9) | 96 | 88.4 (80.1, 96.6) | 0.8 (0.3, 2.5) |
| Marines | 36 | 21.3 (8.4, 34.2) | 88 | 78.7 (65.8, 91.6) | 1.6 (0.5, 5.0) |
| Duration of military service (years) | |||||
| < 1 to 4 | 101 | 17.1 (11.7, 22.5) | 261 | 83.0 (77.5, 88.3) | Reference |
| 5–10 | 68 | 24.7 (14.6, 34.8) | 175 | 75.3 (65.2, 85.4) | 1.6 (0.8, 3.1) |
| > 10 | 66 | 9.8 (3.7, 15.8) | 186 | 90.2 (84.2, 96.3) | 0.5 (0.2, 1.2) |
| Past clinical diagnoses | |||||
| Traumatic brain injury | |||||
| No | 83 | 16.0 (11.8, 20.2) | 351 | 84.0 (79.8, 88.2) | Reference |
| Yes | 156 | 33.9 (29.3, 38.5) | 279 | 66.1 (61.5, 70.7) | 2.7 (1.9, 3.9) |
| PTSD | |||||
| No | 82 | 12.8 (8.3, 17.2) | 332 | 87.2 (82.8, 91.7) | Reference |
| Yes | 157 | 27.2 (19.2, 35.2) | 308 | 72.8 (64.8, 80.8) | 2.6 (1.4, 4.5) |
| Any mental health disorder | |||||
| No | 23 | 7.5 (3.1, 12.1) | 172 | 92.4 (88.0, 96.9) | Reference |
| Yes | 216 | 24.2 (18.3, 30.1) | 458 | 75.8 (69.9, 81.7) | 3.9 (1.9, 8.0) |
| Pain disorder | |||||
| No | 13 | 9.3 (3.0, 15.6) | 107 | 90.7 (84.4, 97.0) | Reference |
| Yes | 226 | 19.5 (14.7, 24.3) | 523 | 80.5 (75.7, 85.3) | 2.4 (1.1, 5.3) |
| Patient-reported clinical characteristics | |||||
| Anxiety | |||||
| None/Low | 51 | 8.5 (4.6, 12.5) | 328 | 91.5 (87.5, 95.4) | Reference |
| High | 181 | 34.9 (26.4, 43.4) | 290 | 65.1 (56.7, 73.6) | 5.7 (3.0, 10.9) |
| Depression | |||||
| None/Low | 86 | 8.7 (5.1, 12.3) | 417 | 91.3 (87.7, 94.9) | Reference |
| High | 146 | 39.2 (29.2, 49.3) | 201 | 60.8 (50.7, 70.8) | 6.8 (3.6, 12.8) |
| Hearing function | |||||
| Excellent/good | 14 | 7.1 (0.0, 14.0) | 113 | 93.0 (86.0, 100.0) | Reference |
| A little/moderate trouble | 131 | 14.4 (9.6, 19.3) | 388 | 85.6 (80.7, 90.4) | 2.2 (0.7, 6.9) |
| A lot of trouble/deaf | 92 | 25.5 (16.9, 34.2) | 123 | 74.5 (65.8, 83.1) | 4.5 (1.4, 14.3) |
| Overall health | |||||
| Excellent/very good/good | 93 | 9.9 (5.9, 13.9) | 397 | 90.1 (86.1, 94.1) | Reference |
| Fair/poor | 141 | 28.9 (20.8, 36.9) | 222 | 71.1 (63.1, 79.2) | 3.7 (2.0, 6.7) |
Abbreviations: CI, confidence interval; OR, odds ratio; PTSD, posttraumatic stress disorder.
Notes: Sample n s based on raw data; population proportions calculated after survey weighting and multiple imputation. Bold font indicates statistical significance at p < 0.05.
Work Functioning
Of the 891 Veteran participants, 239 (weighted proportion: 17.0%; 95% CI: 13.0, 21.0) reported a high tinnitus-related impact on their work functioning, and 650 (weighted proportion: 83.0%; 95% CI: 79.0, 87.0) reported none/low impact on work functioning. Level of work functioning varied by Veterans' demographic and military history characteristics and VA diagnoses. Compared with Veterans younger than 30 years, a higher proportion of Veterans aged 30 to 40 years (26.9%; 95% CI: 20.0, 33.8) reported that their tinnitus had a high impact on work functioning (OR: 2.9; 95% CI: 1.3, 6.3). White Veterans were less than half as likely to report that tinnitus had a high impact on work functioning compared with Black/African American Veterans (OR: 0.4; 95% CI: 0.2, 0.8). Higher proportions of Veterans with, versus without, TBI (33.9%; 95% CI: 29.3, 38.5 vs. 16.0%; 95% CI: 11.8, 20.2), any mental health disorder (24.2%; 95% CI: 18.3, 30.1 vs. 7.5%; 95% CI: 3.1, 12.1), pain disorder (19.5%; 95% CI: 14.7, 24.3 vs. 9.3%; 95% CI: 3.0, 15.6), and PTSD diagnoses (27.2; 95% CI: 19.2, 35.2 vs. 12.8%; 95% CI: 8.3, 17.2) reported that tinnitus had a high impact on work functioning. Similarly, self-reported anxiety, depression, subjective hearing function, and fair/poor overall health were associated with a high impact on work functioning.
Tinnitus Severity and Impact on Work Functioning
Table 2 presents the tabulated means and ORs for the total TFI score and the eight TFI subdomains by tinnitus-related work functioning (high impact vs. none/low impact). Bivariable analysis of the relationship accounting for population weighting showed that for every 1-point increase in TFI score, there was an average 8% increase in the odds of reporting a high level of impact on work functioning (OR: 1.08; 95% CI: 1.06, 1.10). Results were similar when adjusting for potentially confounding variables (OR: 1.08; 95% CI: 1.06, 1.11).
Table 2. Associations between tinnitus severity and high tinnitus-related impact on work functioning among Veteran VA users diagnosed with tinnitus.
| Level of tinnitus-related impact on work functioning | ||||
|---|---|---|---|---|
| High n = 239 (17.0%; 95% CI: 13.0, 21.0) |
None/Low n = 630 (83.0%; 95% CI: 79.0, 87.0) |
|||
| Mean (95% CI) | Mean (95% CI) | Bivariable OR (95% CI) |
Multivariable OR (95% CI) |
|
| Total TFI score | 75.4 (71.3, 79.5) | 45.0 (42.3, 47.7) | 1.08 (1.06, 1.10) | 1.08 (1.06, 1.11) |
| TFI subdomains | ||||
| Auditory | 79.5 (74.4, 84.6) | 57.9 (54.7, 61.2) | 1.04 (1.02, 1.05) | 1.04 (1.02, 1.06) |
| Cognitive | 73.9 (69.1, 78.8) | 39.4 (36.4, 42.4) | 1.07 (1.05, 1.09) | 1.07 (1.05, 1.09) |
| Control | 76.3 (70.3, 82.4) | 53.3 (50.0, 56.5) | 1.04 (1.02, 1.06) | 1.03 (1.01, 1.05) |
| Emotional | 76.3 (71.0, 81.5) | 34.6 (31.2, 37.9) | 1.06 (1.05, 1.08) | 1.06 (1.04, 1.08) |
| Intrusive | 75.5 (70.7, 80.2) | 56.7 (53.5, 59.9) | 1.03 (1.02, 1.05) | 1.03 (1.02, 1.05) |
| QOL | 72.7 (68.2, 77.2) | 37.2 (34.0, 40.5) | 1.06 (1.05, 1.08) | 1.06 (1.04, 1.08) |
| Relaxation | 77.0 (72.1, 81.9) | 45.2 (41.6, 48.7) | 1.05 (1.03, 1.06) | 1.04 (1.03, 1.06) |
| Sleep | 72.9 (67.6, 78.1) | 38.4 (34.7, 42.1) | 1.04 (1.03, 1.05) | 1.04 (1.02, 1.05) |
Abbreviations: CI, confidence interval; OR, odds ratio; TFI, Tinnitus Functional Index; QOL, quality of life.
Notes: Sample n s based on raw data; population proportions calculated after survey weighting and multiple imputation. Bold font indicates statistical significance at p < 0.05. Multivariable models include the following covariates: age, sex, race, marital status, education, income, military branch, duration of service, level of service connection, traumatic brain injury diagnosis, mental health disorder diagnosis, pain disorder diagnosis, posttraumatic stress disorder diagnosis, self-reported anxiety, self-reported depression, subjective hearing function, and overall health.
As seen in Table 2 , Veterans with no or low tinnitus-related impact on work had an average TFI score of 45.0 (95% CI: 42.3, 47.7), and Veterans with a high level of tinnitus-related impact on work had an average TFI score of 75.4 (95% CI: 71.3, 79.5). Results from our multivariable model (not shown) indicated that individuals with a TFI score of 45.0 had a 5.2% (95% CI: 2.0, 8.4) predicted probability of high impact on work, whereas those with a TFI score of 75.4 had a 36.7% (95% CI: 28.6, 44.9) predicted probability. Fig. 2 shows predicted probabilities of high impact on work by TFI scores ranging from 0 to 100 in 10-point increments.
Figure 2.
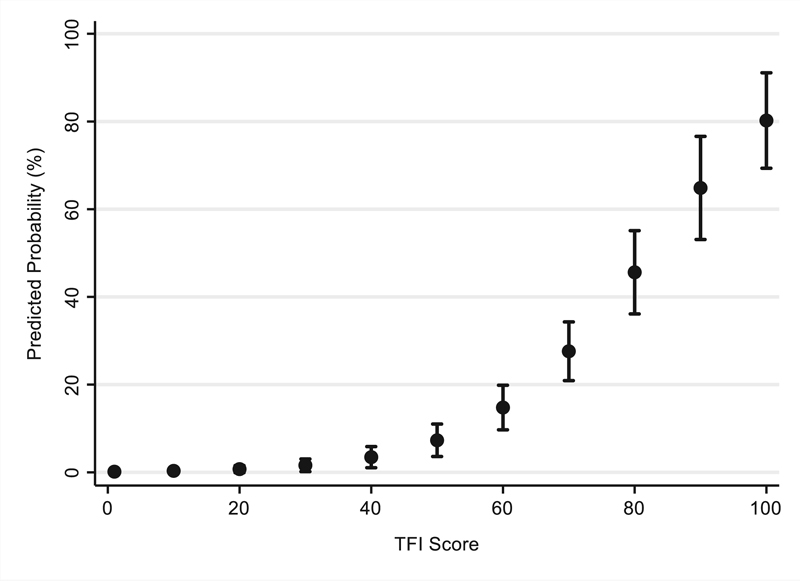
Predicted probabilities of high tinnitus-related impact on work functioning by Tinnitus Functional Index (TFI) score.
Regarding the subdomain analyses, all eight TFI subdomains were significantly associated with high tinnitus-related impact on work in both bivariable and multivariable models. The Auditory subdomain had the highest mean TFI scores (indicating more severe symptoms) for both the Veterans that reported high impact on work functioning (79.5; 95% CI: 74.4, 84.6) and those that reported none/low impact on work functioning (57.9; 95% CI: 54.7, 61.2). For those with high impact on work functioning, the subdomain with the next highest mean TFI score was Relaxation (77.0; 95% CI: 72.1, 81.9). The lowest mean scores among Veterans in both work functioning groups were in the Quality of Life subdomain (high = 72.7; 95% CI: 68.2, 77.2; none/low = 37.2; 95% CI: 34.0, 40.5).
Tinnitus Severity and Impact on Work Functioning, by TBI Status
Table 3 presents the associations between TFI scores and tinnitus-related work functioning stratified by TBI diagnosis. Mean total TFI scores among Veterans who reported a high impact on work functioning did not differ between Veterans with and without TBI diagnosis (77.5; 95% CI: 75.0, 80.1 vs. 75.1; 95% CI: 70.5, 79.8, respectively). Similarly, mean total TFI scores among Veterans who reported none/low impact on work functioning differed only slightly between Veterans with and without TBI (50.2; 95% CI: 47.7, 52.7 vs. 44.8; 95% CI: 41.9, 47.6, respectively). In other words, regardless of TBI history, Veterans with more severe tinnitus, represented via greater TFI scores, averaged more severe impact on work functioning. The eight TFI subdomains followed similar patterns between Veterans with and without comorbid TBI diagnosis. However, bivariable logistic regression models revealed that the strength of the associations between tinnitus severity, according to overall TFI scores and the TFI subdomains, and tinnitus-related work functioning did not differ between Veterans with and without TBI.
Table 3. Associations between tinnitus severity and high tinnitus-related impact on work functioning among Veteran VA users diagnosed with tinnitus, stratified by traumatic brain injury diagnosis.
| TBI diagnosis | No TBI diagnosis | |||||
|---|---|---|---|---|---|---|
| Level of tinnitus-related impact on work functioning | Level of tinnitus-related impact on work functioning | |||||
| High n = 156 (33.9%; 95% CI: 29.3, 38.5) |
None/Low n = 279 (66.1%; 95% CI: 61.5, 70.7) |
High n = 83 (16.0%; 95% CI: 11.8, 20.2) |
None/Low n = 351 (84.0%; 95% CI: 79.8, 88.2) |
|||
| Mean (95% CI) |
Mean (95% CI) |
Bivariable OR (95% CI) | Mean (95% CI) |
Mean (95% CI) |
Bivariable OR (95% CI) | |
| Total TFI score | 77.5 (75.0, 80.1) | 50.2 (47.7, 52.7) | 1.07 (1.06, 1.09) | 75.1 (70.5, 79.8) | 44.8 (41.9, 47.6) | 1.08 (1.06, 1.11) |
| TFI subdomains | ||||||
| Auditory | 79.2 (76.4, 82.1) | 58.6 (55.4, 61.9) | 1.04 (1.03, 1.05) | 79.6 (73.8, 85.4) | 57.9 (54.4, 61.4) | 1.04 (1.02, 1.06) |
| Cognitive | 77.8 (74.9, 80.6) | 49.8 (47.0, 52.7) | 1.06 (1.05, 1.07) | 73.4 (67.9, 79.0) | 38.9 (35.7, 42.1) | 1.07 (1.05, 1.09) |
| Control | 79.3 (76.5, 82.0) | 60.4 (57.7, 63.1) | 1.05 (1.04, 1.06) | 75.9 (69.1, 82.7) | 53.0 (49.5, 56.4) | 1.04 (1.02, 1.06) |
| Emotional | 75.7 (72.5, 79.0) | 38.9 (35.8, 42.0) | 1.06 (1.04, 1.07) | 76.3 (70.3, 82.2) | 34.3 (30.8, 37.9) | 1.06 (1.04, 1.08) |
| Intrusive | 78.3 (75.1, 81.5) | 58.7 (55.8, 61.6) | 1.04 (1.03, 1.05) | 75.1 (69.7, 80.5) | 56.6 (53.2, 60.0) | 1.03 (1.02, 1.05) |
| QOL | 74.5 (71.3, 77.8) | 41.9 (38.7, 45.0) | 1.06 (1.04, 1.07) | 72.5 (67.4, 77.6) | 37.0 (33.6, 40.4) | 1.06 (1.05, 1.08) |
| Relaxation | 76.5 (73.3, 79.7) | 42.7 (39.3, 46.0) | 1.04 (1.03, 1.05) | 79.6 (71.1, 82.2) | 44.8 (41.0, 48.6) | 1.05 (1.03, 1.06) |
| Sleep | 76.5 (73.3, 79.7) | 42.7 (39.3, 46.0) | 1.05 (1.04, 1.06) | 72.7 (66.9, 78.5) | 38.8 (34.7, 42.8) | 1.04 (1.03, 1.05) |
Abbreviations: CI, confidence interval; OR, odds ratio; QOL, quality of life; TBI, traumatic brain injury; TFI, Tinnitus Functional Index.
Notes: Population means calculated after survey weighting and multiple imputation. Bold font indicates statistical significance at p < 0.05.
Discussion
This study represents the first known investigation of the association between tinnitus severity and tinnitus-related impairment in work functioning among Veterans. Additionally, this is the first known study to assess tinnitus severity and work functioning by TBI diagnosis status. A population-based survey was used to estimate associations between tinnitus severity and the impact of tinnitus on work, and data from electronic health records were used as clinical covariates. Both tinnitus and TBI are significant concerns for the VA, and this work contributes to our understanding of how tinnitus affects Veterans' functioning and quality of life. The long-term application of this research helps inform tinnitus-related therapies for Veterans, including the provision of vocational rehabilitation services. The data presented also emphasize the importance of managing comorbid mental health conditions, chronic pain, and TBI when assessing Veterans' work functioning. Future investigations into potential impacts on work among active-duty service members with tinnitus, and non-military populations (civilians), are also warranted.
As hypothesized, the results of this study illustrated that more severe tinnitus was associated with increased difficulties with work functioning. Specifically, each 1-point increase in total TFI score equated to, on average, an 8% increase in the odds of reporting a high impact of tinnitus on work. Research on tinnitus-related work difficulties is limited. Among the studies available, researchers have documented that people who have tinnitus miss significantly more workdays compared with people without tinnitus (Bhatt et al. 2016). Missed workdays and poorer work productivity lead to lost wages. Researchers estimate that tinnitus-related work difficulties may account for almost 20 billion dollars per year in the United States (Bhatt et al. 2016). The estimated cost burden for Veterans with tinnitus is still unknown and is an interesting future step for this research.
Our understanding of tinnitus-related work difficulties is largely informed by qualitative studies (Andersson & Edvinsson 2009; Colagrosso et al. 2019; Watts et al. 2018). For example, Watts et al. (2018) analyzed clinical data from patients at a tinnitus treatment center in the United Kingdom. Among the problems reported, patients said that tinnitus interfered with their ability to do their job, and in some cases, tinnitus caused them to not be able to work. While qualitative research is illuminating, the current study illustrates a practical assessment method for specifically quantifying work-related distress that may be leveraged for both clinical service delivery and for future research. The Tinnitus History Questionnaire items used in this analysis may be used to complement formal tinnitus severity questionnaires, such as the TFI, to quantitatively measure tinnitus difficulties that are associated with work.
Identifying the ways in which tinnitus affects daily life is an important step in understanding the complex interactions between severe tinnitus and other disorders, such as depression and cognitive issues (Langguth et al. 2011). Based on the World Health Organization's International Classification of Functioning, Disability and Health, researchers have suggested that tinnitus-related activity limitations such as work difficulties are a downstream effect of impacts on emotional well-being (e.g., depression and anxiety), sleep, concentration, and hearing (Tyler et al. 2014). For example, if an individual has difficulty with sleep attributed to their tinnitus, then they may also experience difficulties being productive at work. Similarly, if an individual reports difficulty hearing that they attribute to tinnitus, they may also have difficulty communicating with supervisors or colleagues at work. Additional research is warranted to identify the potential mediating factors between tinnitus and work difficulties.
The results of this study support the need to consider tinnitus impacts on work in tinnitus management. Indeed, many of the functional requirements for work overlap with domains affected by tinnitus, such as concentration, focus, communication, and level of fatigue. Identifying individual patient characteristics (such as impact on work functioning) can help lead to more individualized therapies and more effective interventions (Theodoroff 2021). Given the current study's findings, it may be appropriate to optimize current rehabilitation approaches to specifically target tinnitus-related work difficulties.
Progressive Tinnitus Management (PTM) is an evidence-based approach to managing tinnitus that has been shown to be effective for Veterans (Henry et al. 2017). PTM involves an interdisciplinary approach to tinnitus rehabilitation including sound therapy and cognitive-behavioral approaches (Beck et al. 2019). PTM has been shown to reduce distress attributed to tinnitus symptoms resulting in an improvement in TFI scores (Henry et al. 2017), including among Veterans with a history of TBI (Henry et al. 2019). PTM involves five stepped levels of care, with patients receiving only the levels they need. For example, patients who progress to level 3 receive skills education for self-management of tinnitus, and attend sessions led by a mental health provider who provides coping skills as utilized in cognitive-behavioral therapy. To target tinnitus-related work difficulties, PTM groups may be formed with individuals for whom tinnitus severely affects their work functioning. Where appropriate, patients may benefit from learning coping and self-management skills to manage tinnitus-related work difficulties.
Although the current study did not illuminate many distinctions in work functioning by the subdomains of the TFI, we did find that Veterans with, for example, intrusive tinnitus, or auditory or emotional effects of tinnitus, may be experiencing considerable impact on work functioning. Used clinically, a TFI subdomain analysis may help further characterize the impact of tinnitus on daily life, individualize interventions, and lead to more precise measures of response to treatment. This work contributes to the growing body of research documenting associations between TBI and tinnitus (Clifford et al. 2019; Fausti et al. 2009; Henry et al. 2012; Jury & Flynn 2001; Moring et al. 2017; Sindhusake et al. 2004). However, research on tinnitus symptom presentation among people with a history of TBI, including how tinnitus affects daily life, is a relatively unexplored area. Past research has shown that patients with trauma-associated tinnitus, including noise trauma, whiplash, and head trauma, experience greater functional impairments when compared with patients with tinnitus from unknown or other factors (Kreuzer et al. 2012).
We found that the odds of having tinnitus-related work difficulty were 2.7 times greater for Veterans with a TBI diagnosis compared with Veterans without a TBI diagnosis. However, the effect of tinnitus severity on work functioning was not modified by TBI status. In other words, Veterans with severe tinnitus were more likely to experience high tinnitus-related impacts on work functioning compared with Veterans with less severe tinnitus, regardless of TBI status. Given that both tinnitus and TBI are prevalent in the Veteran population, these data represent a step toward understanding complex symptoms for this population and may eventually help inform more individualized rehabilitation approaches.
This is the first known study to explore work functioning among a nationally representative population of Veterans with tinnitus with and without TBI. Past studies have investigated the impacts of TBI, tinnitus, and other relevant clinical conditions, individually, on employment. For example, Carlson et al. (2018) found that, among recent Veterans with TBI, nearly half reported unemployment (Carlson et al. 2018). Additionally, studies in civilian TBI populations have found that TBI is associated with a reduced likelihood of obtaining and retaining employment, and an increased likelihood of earning lower wages (Gamboa et al. 2006; Lefebvre et al. 2008; Radford et al. 2013; Vandana et al. 2022). Among the few studies examining the association between tinnitus and employment, Bartels and colleagues found that patients in the Netherlands who had chronic tinnitus were more likely to be unemployed compared with ear-nose-throat (ENT) patients without tinnitus (Bartels et al. 2010). In addition, studies have examined work dysfunction among other patient populations, such as individuals with mental health disorders, PTSD, or chronic pain. For example, Dueñas et al. (2016) conducted a systematic review of the impacts of chronic pain in patients' daily lives, and found that, due to pain, patients experienced missed days of work, reduced efficiency, and lower productivity (Dueñas et al. 2016). Given past findings and the results of the current study, investigations are warranted to further explore the economic and functional impacts on employment among individuals with both tinnitus and TBI.
Limitations
This study focused on Veterans diagnosed with tinnitus who receive care in VA healthcare settings, and therefore it is not clear the extent to which similar results would be seen among non-Veteran populations, or among Veterans receiving care outside of the VA. Additionally, the THQ questions asked about difficulties at work or other activities, but did not necessarily invoke work specifically, or work performed for one's occupation. It is possible that Veterans reported on their tinnitus-related difficulties in work, or other activities, that were not actually related to gainful employment (e.g., volunteer work or hobbies). Additionally, a validation study on the THQ has yet to be undertaken; therefore, the accuracy of this measure for identifying levels of work dysfunction is unclear. ICD codes and self-reported screening measures were used as proxies for Veterans' diagnoses and clinical attributes, and thus we may have inadvertently misclassified some individuals. We attempted to minimize false-positive diagnoses by requiring a patient to have received a respective ICD code during at least one inpatient stay or at least two outpatient visits during the study period to be considered to have a respective condition. Finally, these data did not identify the severity of Veterans' TBI. Future studies that have access to this information will be equipped to expand on this work to investigate relationships between TBI severity, tinnitus severity, and their combined impact on work functioning.
Conclusions
In this nationally representative sample of Veteran VA users diagnosed with tinnitus, severe tinnitus was strongly associated with tinnitus-related work difficulties. The impact of tinnitus severity on work functioning was not moderated by TBI status, although Veterans with comorbid TBI were more likely to experience impacts on work functioning than those without. Further investigation is warranted to describe tinnitus-related impacts on life functioning and effective diagnostic, management, and rehabilitation strategies for Veterans with and without a history of TBI.
Funding Statement
Funding/Acknowledgments We are grateful to the Veterans who participated in this survey for their contributions to health sciences and their service to the U.S. military. This research was supported by grants from the Veterans Health Administration, Office of Research and Development, Rehabilitation Research and Development Service (SPiRE I21 RX002216-01 to K.F.C.; C9427S to J.A.H.) and from the Oregon Clinical and Translational Research Institute at Oregon Health and Science University (1 UL1 RR024140 01).
Footnotes
Conflict of Interest None declared.
References
- Andersson G, Edvinsson E.(2009). Mixed feelings about living with tinnitus: a qualitative study 6 (1), 48–54. Accessed June 2, 2023 at: https://doi.org/10.1080/16513860801899355
- Axelsson A, Sandh A.(2009). Tinnitus in noise-induced hearing loss 19 (4), 271–276. Accessed June 2, 2023 at: https://doi.org/10.3109/03005368509078983 [DOI] [PubMed]
- Bartels H, Middel B, Pedersen S S, Staal M J, Albers F WJ. The distressed (Type D) personality is independently associated with tinnitus: a case-control study. Psychosomatics. 2010;51(01):29–38. doi: 10.1176/appi.psy.51.1.29. [DOI] [PubMed] [Google Scholar]
- Beck J E, Zaugg T L, Egge J L, Lima E N, Thielman E J.Progressive Tinnitus Management at two Veterans Affairs medical centers: clinical implementation with modified protocols Am J Audiol 201928(1S):162–173. [DOI] [PubMed] [Google Scholar]
- Bhatt J M, Bhattacharyya N, Lin H W. Relationships between tinnitus and the prevalence of anxiety and depression. Laryngoscope. 2017;127(02):466–469. doi: 10.1002/lary.26107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatt J M, Lin H W, Bhattacharyya N. Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol Head Neck Surg. 2016;142(10):959–965. doi: 10.1001/jamaoto.2016.1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson K F, Gilbert T A, O'Neil M Eet al. Health care utilization and mental health diagnoses among Veterans with tinnitus Am J Audiol 201928(1S):181–190. [DOI] [PubMed] [Google Scholar]
- Carlson K F, Pogoda T K, Gilbert T Aet al. Supported employment for Veterans with traumatic brain injury: patient perspectives Arch Phys Med Rehabil 201899(2S):S4–S13., 13.e1 [DOI] [PubMed] [Google Scholar]
- Chandra N, Chang K, Lee A, Shekhawat G S, Searchfield G D. Psychometric validity, reliability, and responsiveness of the Tinnitus Functional Index. J Am Acad Audiol. 2018;29(07):609–625. doi: 10.3766/jaaa.16171. [DOI] [PubMed] [Google Scholar]
- Clarke N A, Henshaw H, Akeroyd M A, Adams B, Hoare D J.(2020). Associations Between Subjective Tinnitus and Cognitive Performance: Systematic Review and Meta-Analyses 24 . Accessed June 2, 2023 at: https://doi.org/10.1177/2331216520918416 [DOI] [PMC free article] [PubMed]
- Clifford R E, Baker D, Risbrough V B, Huang M, Yurgil K A.Impact of TBI, PTSD, and hearing loss on tinnitus progression in a US Marine cohort Mil Med 2019184(11-12):839–846. [DOI] [PubMed] [Google Scholar]
- Colagrosso E MG, Fournier P, Fitzpatrick E M, Hébert S. A qualitative study on factors modulating tinnitus experience. Ear Hear. 2019;40(03):636–644. doi: 10.1097/AUD.0000000000000642. [DOI] [PubMed] [Google Scholar]
- Dueñas M, Ojeda B, Salazar A, Mico J A, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457–467. doi: 10.2147/JPR.S105892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggermont J J, Roberts L E. The neuroscience of tinnitus. Trends Neurosci. 2004;27(11):676–682. doi: 10.1016/j.tins.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Fausti S A, Wilmington D J, Gallun F J, Myers P J, Henry J A. Auditory and vestibular dysfunction associated with blast-related traumatic brain injury. J Rehabil Res Dev. 2009;46(06):797–810. doi: 10.1682/jrrd.2008.09.0118. [DOI] [PubMed] [Google Scholar]
- Folmer R L, McMillan G P, Austin D F, Henry J A. Audiometric thresholds and prevalence of tinnitus among male veterans in the United States: data from the National Health and Nutrition Examination Survey, 1999-2006. J Rehabil Res Dev. 2011;48(05):503–516. doi: 10.1682/jrrd.2010.07.0138. [DOI] [PubMed] [Google Scholar]
- Gamboa A M, Jr, Holland G H, Tierney J P, Gibson D S. American Community Survey: earnings and employment for persons with traumatic brain injury. NeuroRehabilitation. 2006;21(04):327–333. [PubMed] [Google Scholar]
- REDCap Consortium . Harris P A, Taylor R, Minor B L et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P A, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J G. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(02):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry J A, Galvez G, Turbin M B, Thielman E J, McMillan G P, Istvan J A. Pilot study to evaluate ecological momentary assessment of tinnitus. Ear Hear. 2012;33(02):179–290. doi: 10.1097/AUD.0b013e31822f6740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry J A, Griest S, Thielman E, McMillan G, Kaelin C, Carlson K F. Tinnitus Functional Index: development, validation, outcomes research, and clinical application. Hear Res. 2016;334:58–64. doi: 10.1016/j.heares.2015.06.004. [DOI] [PubMed] [Google Scholar]
- Henry J A, Thielman E J, Zaugg T L et al. Telephone-based progressive tinnitus management for persons with and without traumatic brain injury: a randomized controlled trial. Ear Hear. 2019;40(02):227–242. doi: 10.1097/AUD.0000000000000609. [DOI] [PubMed] [Google Scholar]
- Henry J A, Thielman E J, Zaugg T L et al. Randomized controlled trial in clinical settings to evaluate effectiveness of coping skills education used with progressive tinnitus management. J Speech Lang Hear Res. 2017;60(05):1378–1397. doi: 10.1044/2016_JSLHR-H-16-0126. [DOI] [PubMed] [Google Scholar]
- Hoffman H, Reed G. Hamilton, London: BC Decker Inc.; (2004). Epidemiology of tinnitus. [Google Scholar]
- Holmes S, Padgham N D. Review paper: more than ringing in the ears: a review of tinnitus and its psychosocial impact. J Clin Nurs. 2009;18(21):2927–2937. doi: 10.1111/j.1365-2702.2009.02909.x. [DOI] [PubMed] [Google Scholar]
- Jastreboff P J. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990;8(04):221–254. doi: 10.1016/0168-0102(90)90031-9. [DOI] [PubMed] [Google Scholar]
- Jury M A, Flynn M C.Auditory and vestibular sequelae to traumatic brain injury: a pilot study N Z Med J 2001114(1134):286–288. [PubMed] [Google Scholar]
- Keeling M E, Ozuna S M, Kintzle S, Castro C A.(2018). Veterans' Civilian Employment Experiences: Lessons Learnt From Focus Groups 46 (6), 692–705. Accessed June 2, 2023 at: https://doi.org/10.1177/0894845318776785
- TRI Database Study Group . Kreuzer P M, Landgrebe M, Schecklmann M, Staudinger S, Langguth B. Trauma-associated tinnitus: audiological, demographic and clinical characteristics. PLoS One. 2012;7(09):e45599. doi: 10.1371/journal.pone.0045599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langguth B, Landgrebe M, Kleinjung T, Sand G P, Hajak G. Tinnitus and depression. World J Biol Psychiatry. 2011;12(07):489–500. doi: 10.3109/15622975.2011.575178. [DOI] [PubMed] [Google Scholar]
- Lefebvre H, Cloutier G, Josée Levert M.Perspectives of survivors of traumatic brain injury and their caregivers on long-term social integration Brain Inj 200822(7-8):535–543. [DOI] [PubMed] [Google Scholar]
- Lew H L, Jerger J F, Guillory S B, Henry J A. Auditory dysfunction in traumatic brain injury. J Rehabil Res Dev. 2007;44(07):921–928. doi: 10.1682/jrrd.2007.09.0140. [DOI] [PubMed] [Google Scholar]
- Little R JA. Survey nonresponse adjustments for estimates of means. Int Stat Rev. 1986;54(02):139. [Google Scholar]
- Meikle M B, Henry J A, Griest S E et al. The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012;33(02):153–176. doi: 10.1097/AUD.0b013e31822f67c0. [DOI] [PubMed] [Google Scholar]
- Millar M M, Dillman D A. Improving response to web and mixed-mode surveys. Public Opin Q. 2011;75(02):249–269. [Google Scholar]
- Mohamad N, Hoare D J, Hall D A. The consequences of tinnitus and tinnitus severity on cognition: a review of the behavioural evidence. Hear Res. 2016;332:199–209. doi: 10.1016/j.heares.2015.10.001. [DOI] [PubMed] [Google Scholar]
- Moring J C, Peterson A L, Kanzler K E. Tinnitus, traumatic brain injury, and posttraumatic stress disorder in the military. Int J Behav Med. 2018;25(03):312–321. doi: 10.1007/s12529-017-9702-z. [DOI] [PubMed] [Google Scholar]
- National Research Council (US) Committee on Hearing, Bioacoustics, and Biomechanics . National Academies Press (US); (1982). Tinnitus: Facts, Theories, and Treatments. [PubMed] [Google Scholar]
- Prewitt A, Harker G, Gilbert T A et al. Mental health symptoms among Veteran VA users by tinnitus severity: a population-based survey. Mil Med. 2021;186 01:167–175. doi: 10.1093/milmed/usaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radford K, Phillips J, Drummond A et al. Return to work after traumatic brain injury: cohort comparison and economic evaluation. Brain Inj. 2013;27(05):507–520. doi: 10.3109/02699052.2013.766929. [DOI] [PubMed] [Google Scholar]
- Sauer B, VanderWeele T J.(2013). Use of directed acyclic graphsAHRQ Publication No. 12(13)-EHC099. Rockville, MD: Agency for Healthcare Research and Quality [Google Scholar]
- Sherlock L GP, Brungart D S.(2021). Functional impact of bothersome tinnitus on cognitive test performance 60 (12), 1000–1008. Accessed June 2, 2023 at: https://doi.org/10.1080/14992027.2021.1909760 [DOI] [PubMed]
- Silverberg N D, Panenka W J, Iverson G L. Work productivity loss after mild traumatic brain injury. Arch Phys Med Rehabil. 2018;99(02):250–256. doi: 10.1016/j.apmr.2017.07.006. [DOI] [PubMed] [Google Scholar]
- Sindhusake D, Golding M, Wigney D, Newall P, Jakobsen K, Mitchell P. Factors predicting severity of tinnitus: a population-based assessment. J Am Acad Audiol. 2004;15(04):269–280. doi: 10.3766/jaaa.15.4.2. [DOI] [PubMed] [Google Scholar]
- Theodoroff S M. Tinnitus questionnaires for research and clinical use. Curr Top Behav Neurosci. 2021;51:403–418. doi: 10.1007/7854_2020_175. [DOI] [PubMed] [Google Scholar]
- Trivedi R B, Post E P, Sun H et al. Prevalence, comorbidity, and prognosis of mental health among US Veterans. Am J Public Health. 2015;105(12):2564–2569. doi: 10.2105/AJPH.2015.302836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler R, Ji H, Perreau A, Witt S, Noble W, Coelho C. Development and validation of the tinnitus primary function questionnaire. Am J Audiol. 2014;23(03):260–272. doi: 10.1044/2014_AJA-13-0014. [DOI] [PubMed] [Google Scholar]
- US Department of Veterans Affairs (2020). Veterans Benefits Administration Annual Benefits ReportThe Fiscal 2020 Annual Benefits Report
- Vandana V, Darshini J K, Afsar M, Shukla D, Jamuna R. Getting back to work: cognitive-communicative predictors for work re-entry following traumatic brain injury. J Psychosoc Rehabil Ment Health. 2022 doi: 10.1007/s40737-022-00286-4. [DOI] [Google Scholar]
- Watts E J, Fackrell K, Smith S, Sheldrake J, Haider H, Hoare D J. Why is tinnitus a problem? A qualitative analysis of problems reported by tinnitus patients. Trends Hear. 2018;22:2.33121651881225E15. doi: 10.1177/2331216518812250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond A S, Snaith R P. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(06):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]


