Abstract
Increased use of fossil fuels has led to global warming with concomitant increases in the severity and frequency of extreme weather events such as wildfires and sand and dust storms. These changes have led to increases in air pollutants such as particulate matter and greenhouse gases. Global warming is also associated with increases in pollen season length and pollen concentration. Particulate matter, greenhouse gases, and pollen synergistically increase incidence and severity of allergic diseases. Other indirect factors such as droughts, flooding, thunderstorms, heat waves, water pollution, human migration, deforestation, loss of green space, and decreasing biodiversity (including microbial diversity) also affect incidence and severity of allergic disease.
Global warming and extreme weather events are expected to increase in the coming decades, and further increases in allergic diseases are expected, exacerbating the already high health care burden associated with these diseases. There is an urgent need to mitigate and adapt to the effects of climate change to improve human health. Human health and planetary health are connected and the concept of One Health, which is an integrated, unifying approach to balance and optimize the health of people, animals and the environment needs to be emphasized. Clinicians are trusted members of the community and they need to take a strong leadership role in educating patients on climate change and its adverse effects on human health. They also need to advocate for policy changes that decrease use of fossil fuels and increase biodiversity and green space to enable a healthier and more sustainable future.
Keywords: Allergy, asthma, mitigation, adaptation, climate change, pollen, particulate matter, thunderstorms, sandstorms, ozone, wildfires
Introduction
Allergic diseases have continued to increase in prevalence during the last 50 years with sensitization rates to one or more common allergens for school aged children approaching 40–50%.1, 2 A study by the CDC found that between 1997 and 2011, food allergy (FA) among children (0 – 17 years old) increased from 3.4% to 5.1% and skin allergies increased from 7.4% to 12.5%.3 More recently, it has been estimated that 8% of children and 11% of adults have FA.4 Additionally, allergic rhinitis (AR) and atopic dermatitis (AD) are estimated to affect approximately 29.4% and 26.1% of adults globally.5 According to the CDC the prevalence of asthma is 5.8% in children and 8.4% in adults.6 Allergic diseases affect millions of people worldwide and pose a huge global health and socio-economic burden.7
Air pollution caused by global warming and climate change events are implicated in the increasing prevalence and severity of allergic disease.8 Anthropogenic use of fossil fuels have increased global temperatures and air pollution through emission of heat trapping greenhouse gases (GHGs) such as carbon dioxide (CO2), methane (CH4), nitrous oxide (N2O), ozone (O3), and fluorinated gases.9 The Intergovernmental Panel on Climate Change (IPCC) has reported that global warming is now approximately 1°C higher than pre-industrial times and is continuing to increase.10 Global warming has increased the frequency and intensity of wildfires and sand and dust storms leading to further increases in air pollutants, primarily in the form of particulate matter (PM). Pollen is also an air pollutant of concern for allergic diseases. There is now evidence that pollen season length and pollen concentration are increased with global warming and increased levels of GHGs.11 Other indirect factors that adversely affect allergic diseases include droughts, flooding, thunderstorms, heat waves, water pollution, human migration, deforestation, and decreasing biodiversity.
The increasing prevalence of allergic diseases is a cause for concern. They pose a significant health burden, both in direct and indirect health care costs. They are often chronic needing long-term treatment. Further, epidemiological studies have shown that individuals who develop one atopic condition are more likely to develop other atopic diseases over time. Individuals often develop AD in early infancy or childhood and later develop food allergies, AR, and asthma.12 This phenomenon has been termed the Allergic or Atopic March.13 In the United States, the direct costs of treating asthma was estimated to be 57.9 billion dollars7; between 252 – 314 million dollars for atopic dermatitis7, > 4.6 billion for allergic rhinitis,14 and 24.8 billion for childhood FA.15 Indirect costs include absenteeism and presentism and a lower quality of life.7
Here, we review the climate change events, environmental and other factors that directly and indirectly impact allergic diseases. We also explore One Health, which is an integrated, unifying approach to balance and optimize the health of people, animals and the environment.16, 17 As trusted members of the community, clinicians should take a lead role in educating their patients and advocating for policies to better adapt and mitigate the effects of climate change in order to reduce the incidence and prevalence of allergic disease and enable a healthier and more sustainable future.18
Climate Change Events and Associated Factors Affecting Prevalence of Allergic Diseases
Although genetics has been shown to play a role in the etiology of allergic diseases, the rate of increase in allergic diseases is too rapid to be explained by genetics alone. Epidemiological studies suggest that environmental and lifestyle factors aid in the development and exacerbation of these diseases. The main factors that have been implicated in the global increases in allergic diseases include (1) changes in lifestyle (increased hygiene and decreased exposure to biodiverse plants, animals, and microbes) leading to decreases in the development of immune tolerance and increases in microbial dysbiosis and (2) increased exposure to environmental pollutants leading to epithelial barrier disruption and immune dysregulation. These include both natural and synthetic pollutants. Natural air pollutants include GHGs, PM, pollen, and mold, which have increased with climate change events such as wildfires, sand and dust storms, thunderstorms, and flooding (Figure 1). A recent study of chemical inventories from around the world found that around 350,000 chemicals and mixtures of chemicals are registered for production and use.19 In addition, secondary effects such as water pollution and migration due to climate change also affect allergic diseases.
Figure 1.
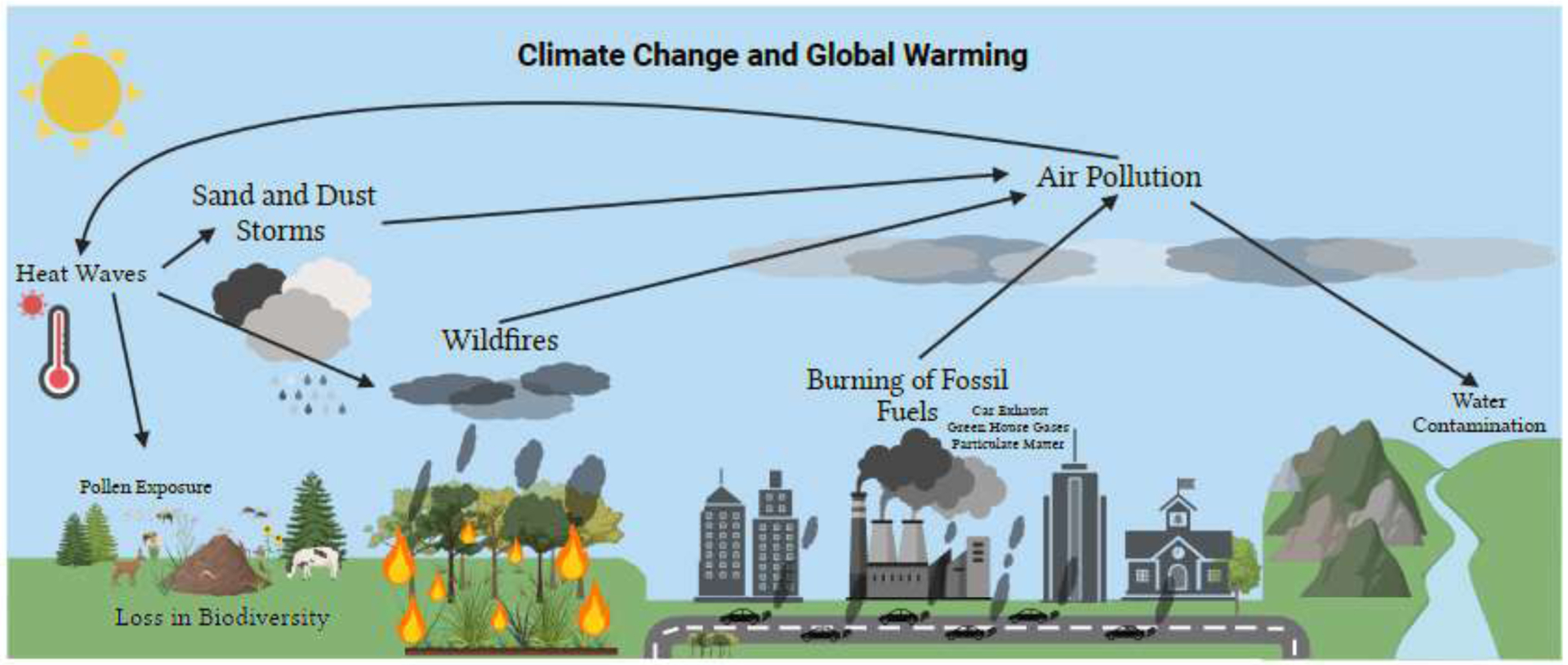
Factors contributing to an increase in air pollution and its effect on the environment. One-way arrows indicate a causal relationship. Created with BioRender.com.
Air Pollution
Air pollution, both indoor and outdoor, increase risk and severity of allergic diseases. The World Health Organization (WHO) estimates that 99% of the global population live in areas with air that exceeds the WHO guideline limits for air pollutants, especially in low- and middle-income communities.20 Many studies, including meta-analyses, have found associations between air pollutants and atopic diseases21 such as asthma22–28, AD29–31, FA32, and AR33–35.
Indoor air pollution sources include open fires or stoves for cooking fueled by biomass or coal, tobacco smoke, and consumer products such as cleaning supplies. Pollutants found in indoor air pollution include PM, various chemicals (including volatile organic compounds from cleaning supplies and building materials), and allergens (from pet and insect dander and from molds).36 Outdoor pollution sources include industrial and vehicular emissions (GHGs, PM, and other toxins) as well as from wildfires and sand and dust storms. Another natural source of air pollutants that affect allergic diseases is pollen, which is affected by increasing heat, CO2 levels, and climate events such as thunderstorms. Air pollutants are thought to increase risk for and exacerbate respiratory disease by four main mechanisms: oxidative stress and epithelial damage, airway remodeling, inflammatory pathways and immunological responses, and enhancement of respiratory sensitization.37 In AD, air pollutants have been shown to cause epidermal injury38 leading to water loss and changes in microflora.39
Particulate Matter
PM is a major air pollutant that adversely affects allergic disease. PM concentrations tend to be higher in winter months, due to increased car traffic and domestic heating.40 A meta-analysis of 35 studies across 12 countries (453,470 participants) showed a positive association between air pollution and the prevalence of AR.41 PM consists of a mixture of solid particles and liquid droplets with varying chemical composition, depending on the source. Those that are smaller than 10 microns (PM10) can enter the lungs, which on deposition on the lung surface can induce tissue damage and lung inflammation. Those that are smaller than 2.5 microns (PM2.5) are considered the most harmful due to their ability to travel deep into the bronchioles and alveoli of the lungs and enter the bloodstream.42, 43. A systematic review and meta-analysis found that the odds ratio associated with a 10 μg/m3 increase in exposure PM10 and PM2.5 and risk of AR was 1.13 and 1.12, respectively.44 In another meta-analysis and systematic review, increased longitudinal childhood exposure to PM2.5 was associated with increasing risk of subsequent asthma in childhood with an odds ratio of 1.14.45 In response to the health risks associated with PM exposure, the WHO changed its guidelines for PM2.5 from 10 ug/m3 to 5ug/m3.46
Pollen
Climate change and global warming are increasing pollen concentrations. Pollen season varies depending on the source. For example tree pollen is more common in the spring while weed pollen is more common in the fall.47 Climate change in North America has been estimated to contribute to about 50% of the lengthening pollen season.48 Studies have shown that pollen concentrations are on the rise and estimated to increase by 200% by the end of the century.49 Higher temperatures and elevated CO2 levels stimulate photosynthesis, plant growth, and pollen production.49, 50 Further, pollen season is starting earlier and lasting longer, exacerbating the problem.49, 51 The increases in pollen concentration has significant consequences for public health outcomes, especially for atopic diseases such as allergy and asthma. A systemic review and meta-analysis found a statistically significant increase in the number of asthma emergency department visits with increases of 10 grass pollen grains per cubic meter of exposure.52 Pollen exposure is associated with increased rates of asthma and allergies, specifically AR.49 It is estimated that 30% of people globally have been affected by AR, with the prevalence projected to increase in the coming years.53
Ozone
O3 is a major constituent of smog and is formed when volatile organic compounds and oxides of nitrogen react in sunlight. Ozone is more readily formed in warmer climates, and thus tends to be higher during the summer months.54 Ground level O3 is a GHG and a potent oxidant. It is one of the six criteria air pollutants established by the EPA. In the United States, the current National Ambient Air Quality Standards (NAAQS) for O3 is 70ppb (8-h maximum within a day).55 In the US, in 2016, 90% of non-compliance to NAAQS was due to O3.56
The Global Burden of Disease estimated that in 2019, 365,000 people died from exposure to ambient O3 pollution.57 Ambient O3 has been linked to respiratory tract irritation, inflammation, oxidative stress, decreased function and increased epithelial barrier permeability. Using crowd-sourced allergy symptom data in addition to pollen, weather, and air quality data, a study found that O3 affects symptom severity of pollen allergy.58 It is thought to cause an inflammatory cascade in the airways through an increase in proinflammatory mediators, chemokines, and neutrophils.59 A study used national and regional emergency room visit rates among people with asthma using published survey data and estimated that in 2015, 9–23 million (8–20% of total) asthma-related emergency room visits globally were attributable to O3.60 A systematic review found that increases in long-term exposure to O3 exposure in children was associated with a decrease in forced expiratory volume in one second (FEV1).61
Water Pollution
Since the start of the industrial revolution, many potentially harmful metals, such as cadmium, chromium, copper, nickel, zinc, lead, and mercury have been introduced into our waterways.62, 63 A study, which analyzed how climate change affects the transport of heavy metals, found enhanced cadmium and zinc contamination in lowland catchments (groundwater) in the Netherlands due to enhanced runoff and accelerated leaching.62 In some areas, heavy metals such as arsenic and cadmium are found in drinking water,64–66 which can cause adverse effects on the epithelial barrier and immune function. A study found that maternal arsenic and cadmium exposure was associated with alterations in the T-cell population in cord blood of infants, suggesting these exposures might contribute to altered immune function of infants.67 Another study has shown that exposure to arsenic is associated with high levels of Th2 mediators, IL-4, IL-6 and IL-13, which in turn results in increased susceptibility to allergic asthma.68
Detergents, allergens, and other pollutants have also been shown to have adverse effects on the immune system by disruption of the epithelium barrier and promoting inflammation. This has been termed the epithelial barrier hypothesis.38, 69 Multiple studies have been published linking detergents to disrupted epithelium barriers.70–72 A study demonstrated that laundry detergents, even at a very high dilution (1:25,000) show significant cell toxicity by disrupting barrier integrity of human bronchial epithelial cells.70 Detergents have been shown to disrupt epithelial barrier integrity through their effects on tight junction or adhesion molecules and promote inflammation through epithelial alarmin release.73 Epithelial barrier dysfunction and increased permeability can trigger an immune response and contribute to the development of allergies and other immune-related disorders.74
Climate Change Events
As the number, frequency, and severity of climatic events have increased with climate change, they adversely impact human health, including allergies and asthma. Some of the major climate change events that impact allergies are wildfires, sand and dust storms, thunderstorms, heat waves, and flooding. These are discussed below.
Wildfires
Wildfires have become more frequent and severe with global warming releasing large amounts of PM, O3, and carbon monoxide.75, 76 Although summer months have historically been considered wildfire season, global warming is causing wildfires to be a year round problem. In California, after the onset of a wildfire in 2020, PM2.5, O3, and carbon monoxide concentrations increased by approximately 220%, 20% and 151%, respectively.77 By increasing GHGs, wildfires accelerate climate change leading to a positive feedback loop.78 Wildfire smoke has been associated with increased rates of asthma79 and increased levels of proinflammatory markers such as C-reactive protein (CRP) and IL-1B, which can worsen asthma and allergy symptoms.80 A study by Aguilera et al. found that PM2.5 emissions from wildfire smoke was about 10 times more harmful on children’s respiratory health than from PM2.5 emissions from vehicles, particularly for children aged 0 to 5 years.81 After the 2016 Fort McMurray fire in Alberta, Canada, there was an increase in asthma consultations among firefighters involved in fighting the fire. FEV1 and FVC were positively associated with increasing exposure. A fifth of the firefighters also had a positive methacholine challenge test and bronchial wall thickening.82 These findings highlight the need for measures to prevent wildfires and protect individuals from their harmful effects.
Sand and Dust Storms
Sand and dust storms (SDS) have become more frequent and severe in recent years due to increased temperatures, droughts, and deforestation.83 According to a report by the United Nations, approximately 2 billion tons of dust are emitted into the atmosphere each year, with the Asia-Pacific region contributing 27% of those emissions.84 Studies have shown that SDS can exacerbate air pollution levels, including higher levels of PM, CO2, and O3.85 In addition, SDS is known to include pathogens and microorganisms such as bacteria, fungi and spores.86 Research has shown how particles in dust storms can travel long distances leading to respiratory infections, asthma and allergies.87 For example, in California, an increase in Coccidiomycosis infection, caused by the fungi Coccidioides immitis, was associated with dust exposure and dust storms.88 A study found that over a five-year period, on days with dust storms, same day asthma and respiratory admission at hospitals increased significantly.89
Thunderstorms and flooding
Thunderstorm asthma (TA) refers to an observed increases in asthma incidence following the occurrence of thunderstorms when pollen counts are high, generally in late spring and early summer.90 TA can result in significant morbidity and mortality.91 For example, on November 21, 2016, Melbourne, Australia experienced a catastrophic epidemic of TA. Grass pollen concentrations were extremely high (>100 grains/m3) and within 30 hours, there was a 672% increase in respiratory issues at the emergency department and a 992% increase in asthma related admissions, compared to the past three years. This incident resulted in the death of 10 individuals.92 During thunderstorms, the high humidity causes pollen grains to rupture into sub pollen allergenic particles by osmotic shock resulting in each grain releasing hundreds of small (<5μm) allergenic granules, which are capable of reaching the lower airways.93
Flooding is also associated with increased asthma and other respiratory systems. After major floods, there is proliferation of mold spores due to increased dampness exposing residents to indoor aeroallergen exposure93, 94. In the aftermath of Hurricane Harvey, flood-exposed individuals were at increased risk of upper respiratory tract allergic symptoms with exposures to dirty water and mold associated with increased risk of multiple allergic symptoms.95
Extreme temperatures
Heat waves are becoming more frequent and severe due to climate change, with many regions experiencing record-breaking temperatures. Extreme temperatures and heat waves are defined as persistent periods of ambient temperature higher than the average.96, 97The National Weather Service published a heat index chart categorizing heat ranges as “Caution”, “Extreme Caution”, “Danger” and “Extreme Danger”.98For example, any temperature above 105°F (41°C) is considered “Dangerous” to human health. According to the United States Environmental Protection Agency, heat waves have increased in frequency, duration, and intensity.99 Studies suggests that exposure to extreme temperatures may be a risk for asthma. A meta-analysis of 111 studies found that the pooled relative risks for asthma attacks in extreme heat was 1.07.100
Analysis of data from asthma hospital visits at all medical facilities in Shenzhen, China between 2016–2020 found that during extreme temperature events the cumulative relative risk of asthma during heat waves compared to other days was 1.06.101 Further, a study by Jin et al, found strong evidence that temperature-related hospitalization risk increased with PM level, with the effects of PM2.5 being stronger than that of PM10.102
Biodiversity and Green Space
The biodiversity hypothesis suggests that contact with natural and a biodiverse environment enriches the human microbiome, promotes immune balance and protects from allergic disease.103 Human activities such as deforestation and urbanization has led to habitat and biodiversity loss with significant impacts on the functioning of the ecosystem and human health. Since 1970, it is estimated that within wildlife populations there has been a 69% decrease in biodiversity.104 One study found that climate change has led to a reduction in microbial diversity in grassland soil. The researchers analyzed soil samples and found that experimental warming decreased richness of bacteria by 9.6%, fungi by 14.5% and protists by 7.5%.105 Increased hygiene, more time spent indoors and decreased exposure to green space and to farm animals and pets has been shown to have adverse effects on immune health and increase risk of atopic diseases including allergy and inflammatory disorders.103
Studies have linked a decrease in the gut microbiome to allergic, inflammatory, and autoimmune diseases. Particularly for infants, research highlights how the gut microbiome plays an important role in the development of FA.106 For example, a study found that higher microbial diversity at 3 months of age was associated with a resolution of milk allergy by age 8.107 Another study found that lower microbial richness and imbalances in specific gut bacteria were significantly associated with atopic sensitization.108 Additionally, research has shown that individuals with allergies have significantly lower fecal microbial richness.109 A recent case study found that fecal microbiota transplantation was a successful treatment for a patient with FA and chronic urticaria.110 The lung microbiome also acts as an important layer of biodiversity and affects health outcomes of patients. For example, one study found that children living on farms and experiencing greater microbial diversity, were significantly less likely to develop asthma compared to children not on farms.111
In addition to microbial diversity, some studies have found an inverse relationship between the amount of forest cover close to children’s home and the development of allergic disease.112, 113 Living close to a green environment at birth was protective and decreased the risk of developing allergic diseases and asthma by age 7.114 More research is emerging, highlighting how living in an environment with more biodiversity or green space can enhance immunological resilience and prevent allergic diseases and asthma.115 However, a recent systematic review and meta-analysis found that greenspace exposure on asthma and AR was not significant. Further research is needed.116
Migration
Currently 55% of the world lives in urban cities, but it is estimated to grow to nearly 70% by 2050.117 The World Bank estimates that by 2050, 143 million people in Sub-Saharan Africa, South Asia, and Latin America will become displaced due to climate change.118 Increased urbanization results in increased exposure to air pollution and a higher risk of developing respiratory diseases such as asthma. A study conducted in Canada found that asthma rates were higher in urban environments compared to rural areas.119 Another study in the UK found that individuals living in urban areas recorded greater hay fever symptoms than in rural environments.120 They also found that the severity of the symptoms correlated with pollutant and pollen levels.120 Increases in the prevalence of allergy has been observed between migrants and native-born and between second and first generation migrants.121. These varying patterns offer clues regarding the mechanisms underlying allergic disorders and emphasize the role of the environment in allergic disease.
Next Steps
To improve human health, there is an urgent need to adapt to and mitigate the effects of climate change. As climate change effects the health of all human beings, a concerted effort is needed from each and every one of us from an individual, community, national, and global level. Physicians as trusted members of the community working with vulnerable and at-risk populations on the front lines can play a critical and important role in leading the efforts in mitigating the effects of climate change (Figure 2). Healthcare providers can assist in these efforts in numerous ways. They can educate patients about climate change related risks and advocate for policy change.122, 123
Figure 2.
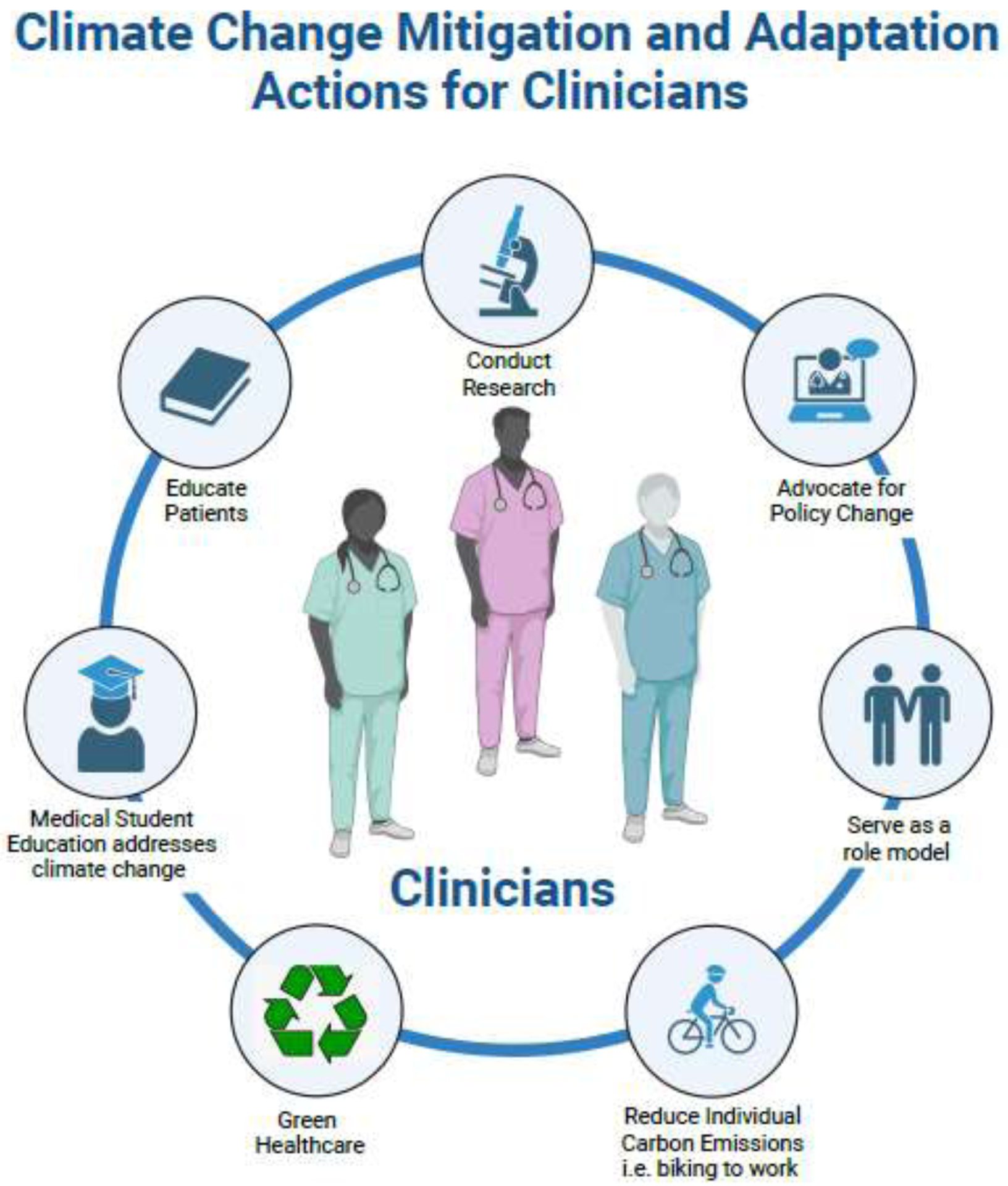
Mitigation and adaptation actions for clinicians to help address the effects of climate change and global warming. Created with BioRender.com.
A study conducted in a hospital in Wisconsin found that 44% of patients in a waiting room thought climate change affected their health, with 6% expecting their physician to be the main source of information on this topic. Meanwhile, the same study found that although 64% of physicians believed climate change was affecting their patients’ health, only 17% were comfortable counseling their patients.124 This study shows that although the majority of physicians, and a substantial number of patients believe climate change affects their health, many feel inadequately prepared to discuss it with their patients.124 There is now a push for medical school and residency training programs to incorporate curricula on climate change and its effects on health.125, 126 This can empower physicians to advocate for climate reform policies, treat patients experiencing the effects of climate change, educate patients to reduce their carbon footprint and their exposure to air and other pollutants.
In the United States, it is estimated that the healthcare sector is responsible for 8.5% of carbon emissions127 making it imperative to develop a more environmental approach to practicing and delivering healthcare by developing green healthcare systems that reduce carbon emissions and waste production and create more sustainable practices.127 On an individual level, physicians can reduce their own carbon footprint, for example, by biking, walking, or using public transport to commute to work when possible, rather than using a car.122, 123, 128
Further mechanistic research is warranted, especially in understanding the effect of climate change on immune responses to allergens and pollutants. This will assist with the development of novel therapeutics for treating the increasing number of patients with allergic disease.129 An environmental justice focus is also necessary to ensure that vulnerable populations, including those with pre-existing respiratory conditions, low-income communities, the elderly, and children are not disproportionately impacted by the impacts of climate change. Finally, a One Health approach should be considered, which recognizes the interconnectedness of human, animal, and environmental health. This approach emphasizes collaboration across sectors to address the complex challenges presented by climate change and emphasizes the importance of protecting biodiversity and the health of the planet.
Conclusion
Global warming and climate change have significant implications for the environment and human health including allergic and atopic disease. To address these challenges, a multifaceted, environmental justice and One Health, approach is necessary. Mitigation strategies, such as reducing GHG emissions and transitioning to renewable energy sources, can help to slow the rate of climate change and reduce the severity of its impacts. Adaptation strategies, including heat mitigation and disaster preparedness, can help to reduce the vulnerability of communities to the impacts of climate change. Ultimately, research to better understand the effects of climate change on human health and particularly on allergy, asthma, and atopic disease, is necessary to provide the best care for patients. Physicians as trusted members of the community should educate their patients on climate change and be role models for decreasing their and the health care sector’s carbon footprint. They should also educate their patients and the community on how to mitigate and adapt to climate change. Lastly, they should advocate for policies that reduce the effects of climate change.
Funding Source
NIAID grants (R21AI1492771, R21EB030643, U01AI147462, U01AI140498, R01AI140134, P01AI153559, U19AI057229), NHLBI grant P01HL152953, and NIEHS grants (R21ES03304901 and R01ES032253)
Conflict of Interest
Dr. Nadeau reports grants from National Institute of Allergy and Infectious Diseases (NIAID), National Heart, Lung, and Blood Institute (NHLBI), National Institute of Environmental Health Sciences (NIEHS), and Food Allergy Research & Education (FARE); Stock options from IgGenix, Seed Health, ClostraBio, Cour, Alladapt;Advisor at Cour Pharma; Consultant for Excellergy, Red tree ventures, Before Brands, Alladapt, Cour, Latitude, Regeneron, and IgGenix; Co-founder of Before Brands, Alladapt, Latitude, and IgGenix; National Scientific Committee member at Immune Tolerance Network (ITN), and National Institutes of Health (NIH) clinical research centers; patents include, “Mixed allergen com-position and methods for using the same,” “Granulocyte-based methods for detecting and monitoring immune system disorders,” and “Methods and Assays for Detecting and Quantifying Pure Subpopulations of White Blood Cells in Immune System Disorders”. Hana Seastedt reports no COI.
Abbreviations/Acronyms
- AD
Atopic Dermatitis
- AR
Allergic Rhinitis
- CH4
Methane
- CO2
Carbon Dioxide
- FA
Food Allergy
- GHG
Green House Gases
- N2O
Nitrous Oxide
- O3
Ozone
- PM
Particulate Matter
- SDS
Sand and Dust Storm
- TA
Thunderstorm Asthma
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pawankar R, Canonica GW, Holgate ST, Lockey RF, Blaiss MS. WAO white book on allergy. Milwaukee, WI: World Allergy Organization. 2011;3:156–157. [Google Scholar]
- 2.AAAAI.Allergy Statistics.https://www.aaaai.org/about/news/for-media/allergy-statistics. Accessed on May 30. 2023.
- 3.Jackson KD, Howie LD, Akinbami LJ. Trends in allergic conditions among children: United States, 1997–2011. NCHS Data Brief. 2013:1–8. [PubMed] [Google Scholar]
- 4.Gupta RS, Warren CM, Smith BM, Blumenstock JA, Jiang J, Davis MM, Nadeau KC. The Public Health Impact of Parent-Reported Childhood Food Allergies in the United States. Pediatrics. 2018;142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Savouré M, Bousquet J, Jaakkola JJK, Jaakkola MS, Jacquemin B, Nadif R. Worldwide prevalence of rhinitis in adults: A review of definitions and temporal evolution. Clin Transl Allergy. 2022;12:e12130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC.Most Recent National Asthma Data.https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm. Accessed on May 30. 2023.
- 7.Dierick BJH, van der Molen T, Flokstra-de Blok BMJ, Muraro A, Postma MJ, Kocks JWH, van Boven JFM. Burden and socioeconomics of asthma, allergic rhinitis, atopic dermatitis and food allergy. Expert Rev Pharmacoecon Outcomes Res. 2020;20:437–453. [DOI] [PubMed] [Google Scholar]
- 8.Singh AB, Kumar P. Climate change and allergic diseases: An overview. Front Allergy. 2022;3:964987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.EPA.Overview of Greenhouse Gases.https://www.epa.gov/ghgemissions/overview-greenhouse-gases. Accessed on May 30. 2023.
- 10.Intergovernmental Panel on Climate Change.Climate Change 2022: Impacts, Adaptation and Vulnerability.https://www.ipcc.ch/report/sixth-assessment-report-working-group-ii/. Accessed on May 30.
- 11.D’Amato G, D’Amato M. Climate change, air pollution, pollen allergy and extreme atmospheric events. Curr Opin Pediatr. 2023;35:356–361. [DOI] [PubMed] [Google Scholar]
- 12.Yang L, Fu J, Zhou Y. Research Progress in Atopic March. Front Immunol. 2020;11:1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hill DA, Spergel JM. The atopic march: Critical evidence and clinical relevance. Ann Allergy Asthma Immunol. 2018;120:131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roland LT, Wise SK, Wang H, Zhang P, Mehta C, Levy JM. The cost of rhinitis in the United States: a national insurance claims analysis. Int Forum Allergy Rhinol. 2021;11:946–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta R, Holdford D, Bilaver L, Dyer A, Holl JL, Meltzer D. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 2013;167:1026–1031. [DOI] [PubMed] [Google Scholar]
- 16.Jutel M, Mosnaim GS, Bernstein JA, Del Giacco S, Khan DA, Nadeau KC, et al. The One Health approach for allergic diseases and asthma. Allergy. 2023. [DOI] [PubMed] [Google Scholar]
- 17.CDC.One health.https://www.cdc.gov/onehealth/index.html. Accessed on May 30. 2023.
- 18.Rothenberg ME. The climate change hypothesis for the allergy epidemic. J Allergy Clin Immunol. 2022;149:1522–1524. [DOI] [PubMed] [Google Scholar]
- 19.Wang Z, Walker GW, Muir DCG, Nagatani-Yoshida K. Toward a Global Understanding of Chemical Pollution: A First Comprehensive Analysis of National and Regional Chemical Inventories. Environmental Science & Technology. 2020;54:2575–2584. [DOI] [PubMed] [Google Scholar]
- 20.WHO.Ambient (outdoor) air pollution.https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health. Accessed on May 30. 2023.
- 21.Wang H, Li XB, Chu XJ, Cao NW, Wu H, Huang RG, et al. Ambient air pollutants increase the risk of immunoglobulin E-mediated allergic diseases: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2022;29:49534–49552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altman MC, Kattan M, O’Connor GT, Murphy RC, Whalen E, LeBeau P, et al. Associations between outdoor air pollutants and non-viral asthma exacerbations and airway inflammatory responses in children and adolescents living in urban areas in the USA: a retrospective secondary analysis. Lancet Planet Health. 2023;7:e33–e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang J, Yang X, Fan F, Hu Y, Wang X, Zhu S, et al. Outdoor air pollution and the risk of asthma exacerbations in single lag0 and lag1 exposure patterns: a systematic review and meta-analysis. J Asthma. 2022;59:2322–2339. [DOI] [PubMed] [Google Scholar]
- 24.Zheng XY, Orellano P, Lin HL, Jiang M, Guan WJ. Short-term exposure to ozone, nitrogen dioxide, and sulphur dioxide and emergency department visits and hospital admissions due to asthma: A systematic review and meta-analysis. Environ Int. 2021;150:106435. [DOI] [PubMed] [Google Scholar]
- 25.Bettiol A, Gelain E, Milanesio E, Asta F, Rusconi F. The first 1000 days of life: traffic-related air pollution and development of wheezing and asthma in childhood. A systematic review of birth cohort studies. Environ Health. 2021;20:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang I, McCreery A, Azimi P, Gramigna A, Baca G, Hayes W, et al. Impacts of residential indoor air quality and environmental risk factors on adult asthma-related health outcomes in Chicago, IL. Journal of Exposure Science & Environmental Epidemiology. 2022. [DOI] [PubMed] [Google Scholar]
- 27.Khreis H, Cirach M, Mueller N, de Hoogh K, Hoek G, Nieuwenhuijsen MJ, Rojas-Rueda D. Outdoor air pollution and the burden of childhood asthma across Europe. Eur Respir J. 2019;54. [DOI] [PubMed] [Google Scholar]
- 28.Perera F, Ashrafi A, Kinney P, Mills D. Towards a fuller assessment of benefits to children’s health of reducing air pollution and mitigating climate change due to fossil fuel combustion. Environ Res. 2019;172:55–72. [DOI] [PubMed] [Google Scholar]
- 29.Fadadu RP, Abuabara K, Balmes JR, Hanifin JM, Wei ML. Air Pollution and Atopic Dermatitis, from Molecular Mechanisms to Population-Level Evidence: A Review. Int J Environ Res Public Health. 2023;20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park SK, Kim JS, Seo HM. Exposure to air pollution and incidence of atopic dermatitis in the general population: A national population-based retrospective cohort study. J Am Acad Dermatol. 2022;87:1321–1327. [DOI] [PubMed] [Google Scholar]
- 31.Hsiao YY, Chen YH, Hung WT, Tang KT. The relationship between outdoor air pollutants and atopic dermatitis of adults: A systematic review and meta-analysis. Asian Pac J Allergy Immunol. 2022;40:295–307. [DOI] [PubMed] [Google Scholar]
- 32.Zhang X, Lu C, Li Y, Norbäck D, Murthy P, Sram RJ, Deng Q. Early-life exposure to air pollution associated with food allergy in children: Implications for ‘one allergy’ concept. Environ Res. 2023;216:114713. [DOI] [PubMed] [Google Scholar]
- 33.Kim JY, Park Y, Kim SH, Kim SP, Park SW, Yoon HJ. Effect of Ambient Air Pollutants on the Medical Costs of Allergic Rhinitis in Seoul, Korea. Laryngoscope. 2022. [DOI] [PubMed] [Google Scholar]
- 34.Savouré M, Lequy É, Bousquet J, Chen J, de Hoogh K, Goldberg M, et al. Long-term exposures to PM(2.5), black carbon and NO(2) and prevalence of current rhinitis in French adults: The Constances Cohort. Environ Int. 2021;157:106839. [DOI] [PubMed] [Google Scholar]
- 35.Zhang S, Fu Q, Wang S, Jin X, Tan J, Ding K, et al. Association between air pollution and the prevalence of allergic rhinitis in Chinese children: A systematic review and meta-analysis. Allergy Asthma Proc. 2022;43:e47–e57. [DOI] [PubMed] [Google Scholar]
- 36.Tran VV, Park D, Lee YC. Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality. Int J Environ Res Public Health. 2020;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383:1581–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Celebi Sozener Z, Ozdel Ozturk B, Cerci P, Turk M, Gorgulu Akin B, Akdis M, et al. Epithelial barrier hypothesis: Effect of the external exposome on the microbiome and epithelial barriers in allergic disease. Allergy. 2022;77:1418–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pan Z, Dai Y, Akar-Ghibril N, Simpson J, Ren H, Zhang L, et al. Impact of Air Pollution on Atopic Dermatitis: A Comprehensive Review. Clin Rev Allergy Immunol. 2023. [DOI] [PubMed] [Google Scholar]
- 40.Przybysz A, Nersisyan G, Gawroński SW. Removal of particulate matter and trace elements from ambient air by urban greenery in the winter season. Environ Sci Pollut Res Int. 2019;26:473–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li S, Wu W, Wang G, Zhang X, Guo Q, Wang B, et al. Association between exposure to air pollution and risk of allergic rhinitis: A systematic review and meta-analysis. Environmental Research. 2022;205:112472. [DOI] [PubMed] [Google Scholar]
- 42.Yang L, Li C, Tang X. The Impact of PM(2.5) on the Host Defense of Respiratory System. Front Cell Dev Biol. 2020;8:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu L, Urch B, Poon R, Szyszkowicz M, Speck M, Gold DR, et al. Effects of ambient coarse, fine, and ultrafine particles and their biological constituents on systemic biomarkers: a controlled human exposure study. Environ Health Perspect. 2015;123:534–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li S, Wu W, Wang G, Zhang X, Guo Q, Wang B, et al. Association between exposure to air pollution and risk of allergic rhinitis: A systematic review and meta-analysis. Environ Res. 2022;205:112472. [DOI] [PubMed] [Google Scholar]
- 45.Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, et al. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a meta-analysis of birth cohort studies. Allergy. 2015;70:245–256. [DOI] [PubMed] [Google Scholar]
- 46.Hoffmann B, Boogaard H, de Nazelle A, Andersen ZJ, Abramson M, Brauer M, et al. WHO Air Quality Guidelines 2021-Aiming for Healthier Air for all: A Joint Statement by Medical, Public Health, Scientific Societies and Patient Representative Organisations. Int J Public Health. 2021;66:1604465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Asthma and Allergy Foundation of America.2022 Allergy Capitals: The most challenging places to live with allergies.https://www.aafa.org/wp-content/uploads/2022/08/aafa-2022-allergy-capitals-report.pdf. Accessed on July 22. 2023.
- 48.Anderegg WRL, Abatzoglou JT, Anderegg LDL, Bielory L, Kinney PL, Ziska L. Anthropogenic climate change is worsening North American pollen seasons. Proc Natl Acad Sci U S A. 2021;118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Y, Steiner AL. Projected climate-driven changes in pollen emission season length and magnitude over the continental United States. Nat Commun. 2022;13:1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ziska LH, Beggs PJ. Anthropogenic climate change and allergen exposure: The role of plant biology. J Allergy Clin Immunol. 2012;129:27–32. [DOI] [PubMed] [Google Scholar]
- 51.Paudel B, Chu T, Chen M, Sampath V, Prunicki M, Nadeau KC. Increased duration of pollen and mold exposure are linked to climate change. Sci Rep. 2021;11:12816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Erbas B, Jazayeri M, Lambert KA, Katelaris CH, Prendergast LA, Tham R, et al. Outdoor pollen is a trigger of child and adolescent asthma emergency department presentations: A systematic review and meta-analysis. Allergy. 2018;73:1632–1641. [DOI] [PubMed] [Google Scholar]
- 53.Schmidt CW. Pollen Overload: Seasonal Allergies in a Changing Climate. Environ Health Perspect. 2016;124:A70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.United States Environmental Protection Agency.Trends in Ozone Adjusted for Weather Conditions.https://www.epa.gov/air-trends/trends-ozone-adjusted-weather-conditions. Accessed on July 21. 2023.
- 55.EPA.NAAQS Table.https://www.epa.gov/criteria-air-pollutants/naaqs-table. Accessed on May 30. 2023.
- 56.Zhang JJ, Wei Y, Fang Z. Ozone Pollution: A Major Health Hazard Worldwide. Front Immunol. 2019;10:2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chemical Sciences Laboratory.A systematic analysis for the Global Burden of Disease Study 2019.https://csl.noaa.gov/news/2020/293_1015.html. Accessed on May 30. 2023.
- 58.Berger M, Bastl K, Bastl M, Dirr L, Hutter HP, Moshammer H, Gstottner W. Impact of air pollution on symptom severity during the birch, grass and ragweed pollen period in Vienna, Austria: Importance of O3 in 2010–2018. Environ Pollut. 2020;263:114526. [DOI] [PubMed] [Google Scholar]
- 59.Bromberg PA. Mechanisms of the acute effects of inhaled ozone in humans. Biochim Biophys Acta. 2016;1860:2771–2781. [DOI] [PubMed] [Google Scholar]
- 60.Anenberg SC, Henze DK, Tinney V, Kinney PL, Raich W, Fann N, et al. Estimates of the Global Burden of Ambient [Formula: see text], Ozone, and [Formula: see text] on Asthma Incidence and Emergency Room Visits. Environ Health Perspect. 2018;126:107004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Holm SM, Balmes JR. Systematic Review of Ozone Effects on Human Lung Function, 2013 Through 2020. Chest. 2022;161:190–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wijngaard RR, van der Perk M, van der Grift B, de Nijs TCM, Bierkens MFP. The Impact of Climate Change on Metal Transport in a Lowland Catchment. Water Air Soil Pollut. 2017;228:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oyewo OA, Adeniyi A, Bopape MF, Onyango MS. Heavy metal mobility in surface water and soil, climate change, and soil interactions. Climate Change and Soil Interactions: Elsevier; 2020:51–88. [Google Scholar]
- 64.Sanders AP, Desrosiers TA, Warren JL, Herring AH, Enright D, Olshan AF, et al. Association between arsenic, cadmium, manganese, and lead levels in private wells and birth defects prevalence in North Carolina: a semi-ecologic study. BMC Public Health. 2014;14:955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ngoc NTM, Chuyen NV, Thao NTT, Duc NQ, Trang NTT, Binh NTT, et al. Chromium, Cadmium, Lead, and Arsenic Concentrations in Water, Vegetables, and Seafood Consumed in a Coastal Area in Northern Vietnam. Environ Health Insights. 2020;14:1178630220921410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zwolak I The Role of Selenium in Arsenic and Cadmium Toxicity: an Updated Review of Scientific Literature. Biol Trace Elem Res. 2020;193:44–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nygaard UC, Li Z, Palys T, Jackson B, Subbiah M, Malipatlolla M, et al. Cord blood T cell subpopulations and associations with maternal cadmium and arsenic exposures. PLoS One. 2017;12:e0179606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rahman A, Islam MS, Tony SR, Siddique AE, Mondal V, Hosen Z, et al. T helper 2-driven immune dysfunction in chronic arsenic-exposed individuals and its link to the features of allergic asthma. Toxicol Appl Pharmacol. 2021;420:115532. [DOI] [PubMed] [Google Scholar]
- 69.Akdis CA. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat Rev Immunol. 2021;21:739–751. [DOI] [PubMed] [Google Scholar]
- 70.Wang M, Tan G, Eljaszewicz A, Meng Y, Wawrzyniak P, Acharya S, et al. Laundry detergents and detergent residue after rinsing directly disrupt tight junction barrier integrity in human bronchial epithelial cells. J Allergy Clin Immunol. 2019;143:1892–1903. [DOI] [PubMed] [Google Scholar]
- 71.Xian M, Wawrzyniak P, Rückert B, Duan S, Meng Y, Sokolowska M, et al. Anionic surfactants and commercial detergents decrease tight junction barrier integrity in human keratinocytes. J Allergy Clin Immunol. 2016;138:890–893.e899. [DOI] [PubMed] [Google Scholar]
- 72.Ogulur I, Pat Y, Aydin T, Yazici D, Rückert B, Peng Y, et al. Gut epithelial barrier damage caused by dishwasher detergents and rinse aids. J Allergy Clin Immunol. 2023;151:469–484. [DOI] [PubMed] [Google Scholar]
- 73.Wright BL, Masuda MY, Ortiz DR, Dao A, Civello B, Pyon GC, et al. Allergies Come Clean: The Role of Detergents in Epithelial Barrier Dysfunction. Curr Allergy Asthma Rep. 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van den Bogaard EH, Elias PM, Goleva E, Berdyshev E, Smits JPH, Danby SG, et al. Targeting Skin Barrier Function in Atopic Dermatitis. J Allergy Clin Immunol Pract. 2023;11:1335–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Westerling AL. Increasing western US forest wildfire activity: sensitivity to changes in the timing of spring. Philos Trans R Soc Lond B Biol Sci. 2016;371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mansoor S, Farooq I, Kachroo MM, Mahmoud AED, Fawzy M, Popescu SM, et al. Elevation in wildfire frequencies with respect to the climate change. J Environ Manage. 2022;301:113769. [DOI] [PubMed] [Google Scholar]
- 77.Meo SA, Abukhalaf AA, Alomar AA, Alessa OM, Sami W, Klonoff DC. Effect of environmental pollutants PM-2.5, carbon monoxide, and ozone on the incidence and mortality of SARS-COV-2 infection in ten wildfire affected counties in California. Sci Total Environ. 2021;757:143948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Van der Werf GR, Morton DC, DeFries RS, Olivier JG, Kasibhatla PS, Jackson RB, et al. CO2 emissions from forest loss. Nature geoscience. 2009;2:737–738. [Google Scholar]
- 79.Stowell JD, Yang C-E, Fu JS, Scovronick NC, Strickland MJ, Liu Y. Asthma exacerbation due to climate change-induced wildfire smoke in the Western US. Environmental Research Letters. 2021;17:014023. [Google Scholar]
- 80.Prunicki MM, Dant CC, Cao S, Maecker H, Haddad F, Kim JB, et al. Immunologic effects of forest fire exposure show increases in IL-1β and CRP. Allergy. 2020;75:2356–2358. [DOI] [PubMed] [Google Scholar]
- 81.Aguilera R, Corringham T, Gershunov A, Benmarhnia T. Wildfire smoke impacts respiratory health more than fine particles from other sources: observational evidence from Southern California. Nat Commun. 2021;12:1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cherry N, Barrie JR, Beach J, Galarneau JM, Mhonde T, Wong E. Respiratory Outcomes of Firefighter Exposures in the Fort McMurray Fire: A Cohort Study From Alberta Canada. J Occup Environ Med. 2021;63:779–786. [DOI] [PubMed] [Google Scholar]
- 83.Pielke RA Sr. Climate vulnerability: understanding and addressing threats to essential resources: Elsevier; 2013. [Google Scholar]
- 84.United Nations Publication.Sand and Dust Storms in Asia and the Pacific: Opportunities for Regional Cooperation and Action.https://www.unescap.org/sites/default/files/UNESCAP%20SDS%20Report_1.pdf. Accessed on May 30. 2023.
- 85.Meo SA, Almutairi FJ, Abukhalaf AA, Alessa OM, Al-Khlaiwi T, Meo AS. Sandstorm and its effect on particulate matter PM 2.5, carbon monoxide, nitrogen dioxide, ozone pollutants and SARS-CoV-2 cases and deaths. Sci Total Environ. 2021;795:148764. [DOI] [PubMed] [Google Scholar]
- 86.Schweitzer MD, Calzadilla AS, Salamo O, Sharifi A, Kumar N, Holt G, et al. Lung health in era of climate change and dust storms. Environ Res. 2018;163:36–42. [DOI] [PubMed] [Google Scholar]
- 87.Pourmand A, Prospero JM, Sharifi A. Geochemical fingerprinting of trans-Atlantic African dust based on radiogenic Sr-Nd-Hf isotopes and rare earth element anomalies. Geology. 2014;42:675–678. [Google Scholar]
- 88.Pearson D, Ebisu K, Wu X, Basu R. A Review of Coccidioidomycosis in California: Exploring the Intersection of Land Use, Population Movement, and Climate Change. Epidemiol Rev. 2019;41:145–157. [DOI] [PubMed] [Google Scholar]
- 89.Thalib L, Al-Taiar A. Dust storms and the risk of asthma admissions to hospitals in Kuwait. Sci Total Environ. 2012;433:347–351. [DOI] [PubMed] [Google Scholar]
- 90.D’Amato G, Annesi-Maesano I, Urrutia-Pereira M, Del Giacco S, Rosario Filho NA, Chong-Neto HJ, et al. Thunderstorm allergy and asthma: state of the art. Multidiscip Respir Med. 2021;16:806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Idrose NS, Dharmage SC, Lowe AJ, Lambert KA, Lodge CJ, Abramson MJ, et al. A systematic review of the role of grass pollen and fungi in thunderstorm asthma. Environ Res. 2020;181:108911. [DOI] [PubMed] [Google Scholar]
- 92.Thien F, Beggs PJ, Csutoros D, Darvall J, Hew M, Davies JM, et al. The Melbourne epidemic thunderstorm asthma event 2016: an investigation of environmental triggers, effect on health services, and patient risk factors. Lancet Planet Health. 2018;2:e255–e263. [DOI] [PubMed] [Google Scholar]
- 93.Rorie A, Poole JA. The Role of Extreme Weather and Climate-Related Events on Asthma Outcomes. Immunol Allergy Clin North Am. 2021;41:73–84. [DOI] [PubMed] [Google Scholar]
- 94.D’Amato G, Chong-Neto HJ, Monge Ortega OP, Vitale C, Ansotegui I, Rosario N, et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy. 2020;75:2219–2228. [DOI] [PubMed] [Google Scholar]
- 95.Oluyomi AO, Panthagani K, Sotelo J, Gu X, Armstrong G, Luo DN, et al. Houston hurricane Harvey health (Houston-3H) study: assessment of allergic symptoms and stress after hurricane Harvey flooding. Environ Health. 2021;20:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.CDC.About Extreme Heat.https://www.cdc.gov/disasters/extremeheat/heat_guide.html. Accessed on Aug 16. 2023.
- 97.EPA U.Climate Change Indicators: Heat Waves.https://www.epa.gov/climate-indicators/climate-change-indicators-heat-waves. Accessed on Aug 16. 2023.
- 98.National Weather Service.Heat Index Chart.https://www.weather.gov/ffc/hichart. Accessed on Aug 16. 2023.
- 99.EPA.Climate Change Indicators: Heat Waves.https://www.epa.gov/climate-indicators/climate-change-indicators-heat-waves. Accessed on May 30. 2023.
- 100.Han A, Deng S, Yu J, Zhang Y, Jalaludin B, Huang C. Asthma triggered by extreme temperatures: From epidemiological evidence to biological plausibility. Environ Res. 2023;216:114489. [DOI] [PubMed] [Google Scholar]
- 101.Deng S, Han A, Jin S, Wang S, Zheng J, Jalaludin BB, et al. Effect of extreme temperatures on asthma hospital visits: Modification by event characteristics and healthy behaviors. Environ Res. 2023;226:115679. [DOI] [PubMed] [Google Scholar]
- 102.Jin X, Xu Z, Liang Y, Sun X, Yan S, Wu Y, et al. The modification of air particulate matter on the relationship between temperature and childhood asthma hospitalization: An exploration based on different interaction strategies. Environ Res. 2022;214:113848. [DOI] [PubMed] [Google Scholar]
- 103.Haahtela T A biodiversity hypothesis. Allergy. 2019;74:1445–1456. [DOI] [PubMed] [Google Scholar]
- 104.WWF.Living Planet report.https://livingplanet.panda.org/en-US/. Accessed on May 30. 2023. [Google Scholar]
- 105.Wu L, Zhang Y, Guo X, Ning D, Zhou X, Feng J, et al. Reduction of microbial diversity in grassland soil is driven by long-term climate warming. Nat Microbiol. 2022;7:1054–1062. [DOI] [PubMed] [Google Scholar]
- 106.Jungles KN, Jungles KM, Greenfield L, Mahdavinia M. The Infant Microbiome and Its Impact on Development of Food Allergy. Immunol Allergy Clin North Am. 2021;41:285–299. [DOI] [PubMed] [Google Scholar]
- 107.Bunyavanich S, Shen N, Grishin A, Wood R, Burks W, Dawson P, et al. Early-life gut microbiome composition and milk allergy resolution. J Allergy Clin Immunol. 2016;138:1122–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Azad MB, Konya T, Guttman DS, Field CJ, Sears MR, HayGlass KT, et al. Infant gut microbiota and food sensitization: associations in the first year of life. Clin Exp Allergy. 2015;45:632–643. [DOI] [PubMed] [Google Scholar]
- 109.Hua X, Goedert JJ, Pu A, Yu G, Shi J. Allergy associations with the adult fecal microbiota: Analysis of the American Gut Project. EBioMedicine. 2016;3:172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wu LQ, Yuan QF, Qin ZC, Xu YD, Li L, Xu JT, et al. Faecal microbiota transplantation for treatment of chronic urticaria with recurrent abdominal pain and food allergy. Singapore Med J. 2023. [DOI] [PubMed] [Google Scholar]
- 111.Ege MJ, Mayer M, Normand AC, Genuneit J, Cookson WO, Braun-Fahrländer C, et al. Exposure to environmental microorganisms and childhood asthma. N Engl J Med. 2011;364:701–709. [DOI] [PubMed] [Google Scholar]
- 112.Hanski I, von Hertzen L, Fyhrquist N, Koskinen K, Torppa K, Laatikainen T, et al. Environmental biodiversity, human microbiota, and allergy are interrelated. Proc Natl Acad Sci U S A. 2012;109:8334–8339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ruokolainen L, von Hertzen L, Fyhrquist N, Laatikainen T, Lehtomäki J, Auvinen P, et al. Green areas around homes reduce atopic sensitization in children. Allergy. 2015;70:195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cavaleiro Rufo J, Paciencia I, Hoffimann E, Moreira A, Barros H, Ribeiro AI. The neighbourhood natural environment is associated with asthma in children: A birth cohort study. Allergy. 2021;76:348–358. [DOI] [PubMed] [Google Scholar]
- 115.Haahtela T, Alenius H, Lehtimäki J, Sinkkonen A, Fyhrquist N, Hyöty H, et al. Immunological resilience and biodiversity for prevention of allergic diseases and asthma. Allergy. 2021;76:3613–3626. [DOI] [PubMed] [Google Scholar]
- 116.Wu B, Guo X, Liang M, Sun C, Gao J, Xie P, et al. Association of individual green space exposure with the incidence of asthma and allergic rhinitis: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2022;29:88461–88487. [DOI] [PubMed] [Google Scholar]
- 117.United Nations DoEaSA.World Urbanization Prospects: The 2018 revision.https://population.un.org/wup/publications/Files/WUP2018-Report.pdf. Accessed on May 30. 2023.
- 118.The world bank.Groundswell: Preparing for Internal Climate Migration.https://www.worldbank.org/en/news/infographic/2018/03/19/groundswell---preparing-for-internal-climate-migration. Accessed on May 30. 2023.
- 119.Lawson JA, Rennie DC, Cockcroft DW, Dyck R, Afanasieva A, Oluwole O, Afsana J. Childhood asthma, asthma severity indicators, and related conditions along an urban-rural gradient: a cross-sectional study. BMC Pulm Med. 2017;17:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gledson A, Lowe D, Reani M, Topping D, Hall I, Cruickshank S, et al. A comparison of experience sampled hay fever symptom severity across rural and urban areas of the UK. Sci Rep. 2023;13:3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tham EH, Loo EXL, Zhu Y, Shek LP. Effects of Migration on Allergic Diseases. Int Arch Allergy Immunol. 2019;178:128–140. [DOI] [PubMed] [Google Scholar]
- 122.Slater M, Bartlett S. Climate change: What healthcare professionals can do. J R Coll Physicians Edinb. 2023;53:7–8. [DOI] [PubMed] [Google Scholar]
- 123.Wellbery CE. Climate Change Health Impacts: A Role for the Family Physician. Am Fam Physician. 2019;100:602–603. [PubMed] [Google Scholar]
- 124.Boland TM, Temte JL. Family Medicine Patient and Physician Attitudes Toward Climate Change and Health in Wisconsin. Wilderness Environ Med. 2019;30:386–393. [DOI] [PubMed] [Google Scholar]
- 125.Goshua A, Gomez J, Erny B, Gisondi M, Patel L, Sampath V, et al. Child-focused climate change and health content in medical schools and pediatric residencies. Pediatr Res. 2023. [DOI] [PubMed] [Google Scholar]
- 126.Goshua A, Gomez J, Erny B, Burke M, Luby S, Sokolow S, et al. Addressing Climate Change and Its Effects on Human Health: A Call to Action for Medical Schools. Acad Med. 2021;96:324–328. [DOI] [PubMed] [Google Scholar]
- 127.Dzau VJ, Levine R, Barrett G, Witty A. Decarbonizing the U.S. Health Sector - A Call to Action. N Engl J Med. 2021;385:2117–2119. [DOI] [PubMed] [Google Scholar]
- 128.Storz MA. Mitigating climate change: using the physician’s tool of the trade. Br J Gen Pract. 2019;69:557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Breiteneder H, Diamant Z, Eiwegger T, Fokkens WJ, Traidl-Hoffmann C, Nadeau K, et al. Future research trends in understanding the mechanisms underlying allergic diseases for improved patient care. Allergy. 2019;74:2293–2311. [DOI] [PMC free article] [PubMed] [Google Scholar]


