Abstract
The inhalation of Francisella tularensis biovar A causes pneumonic tularemia associated with high morbidity and mortality rates in humans. Exposure to F. tularensis usually occurs by accident, but there is increasing awareness that F. tularensis may be deliberately released in an act of bioterrorism or war. The development of a vaccine against pneumonic tularemia has been limited by a lack of information regarding the mechanisms required to protect against this disease. Vaccine models for F. tularensis in inbred mice would facilitate investigations of the protective mechanisms and significantly enhance vaccine development. Intranasal vaccination with the attenuated live vaccine strain (LVS) of F. tularensis reproducibly protected BALB/c mice, but not C57BL/6 mice, against intranasal and subcutaneous challenges with a virulent clinical isolate of F. tularensis biovar A (NMFTA1). The resistance of LVS-vaccinated BALB/c mice to intranasal NMFTA1 challenge was increased 100-fold by boosting with live NMFTA1 but not with LVS. The protective response was specific for F. tularensis and required both CD4 and CD8 T cells. The vaccinated mice appeared outwardly healthy for more than 2 months after NMFTA1 challenge, even though NMFTA1 was recovered from more than half of the vaccinated mice. These results show that intranasal vaccination induces immunity that protects BALB/c mice from intranasal infection by F. tularensis biovar A.
Tularemia is caused by infection with the small gram-negative coccobacillus Francisella tularensis. Pneumonic tularemia is the most serious form of tularemia and is caused by inhalation of either of the two pathogenic F. tularensis subspecies, F. tularensis subsp. tularensis (biovar A) or F. tularensis subsp. holarctica (biovar B) (8). The incidence of naturally occurring pneumonic tularemia is relatively low and is generally associated with activities such as farming and gardening that cause F. tularensis to be aerosolized and dispersed. However, the potential that F. tularensis may be prepared as a bioweapon and intentionally released as an aerosol to cause high mortality rates in the general public has led the Centers for Disease Control and Prevention of the U.S. government to list it as a category A bioterrorism agent. F. tularensis subsp. tularensis is the more virulent of the two pathogenic F. tularensis subspecies and has been estimated to cause >90% of the detected tularemia cases in North America. It is thought that the inhalation of fewer than 25 CFU of biovar A bacteria causes fulminant disease in humans (31, 34). The disease appears abruptly 3 to 5 days after exposure and can rapidly progress to severe pneumonia, respiratory failure, and death (32). Antibiotic treatments are highly effective but must be initiated early in disease development. However, diagnosis and therapeutic intervention are often delayed because of the variable clinical features of pneumonic tularemia.
Preventative vaccination appears to be the best approach against pneumonic tularemia. However, there is no vaccine currently available that has been shown to completely protect humans from this disease. There is also very little information from vaccine studies of animal models to guide future vaccine development. The few vaccine studies to date have examined only the protective effects of subcutaneous (s.c.) vaccination with the highly attenuated live vaccine strain (LVS). A small study with 18 human volunteers showed that vaccination by scarification with LVS does not provide complete protection against aerosol challenge with the biovar A strain SCHU S4, and two of the vaccinated volunteers developed symptoms as severe as those in volunteers without vaccination (31). This result suggests that vaccination by scarification will likely have an unacceptably high rate of failure to protect against respiratory infections by virulent F. tularensis. The success rate may be improved by delivering the vaccine directly into the respiratory tract, like vaccines against other respiratory pathogens such as influenza virus (28) and Mycobacterium tuberculosis (2, 22). In fact, aerogenic LVS vaccination protected guinea pigs and monkeys better than s.c. LVS vaccination against respiratory infection by the biovar A strain SCHU S5 (11). However, these studies were limited in size and detail because of the animal models used, and therefore, additional studies will be required to establish the effectiveness of vaccination by the respiratory route.
Mouse models are ideal for evaluating the protective effects generated by respiratory vaccination and for quickly dissecting the pulmonary immune response mediating protection. Inbred mouse strains such as BALB/c and C57BL/6 mice frequently respond differently to respiratory infections (18, 20, 24, 26, 35) and can be used to determine the mechanisms and genetic bases of resistance and susceptibility. Mouse models are also more useful for detailed analyses of the pulmonary immune responses to respiratory infections than other animal models because of the availability of transgenic and knockout mouse strains as well as analytical tools. However, mice are highly susceptible to intranasal (i.n.) (14) and aerogenic (16) LVS infections, with estimated 50% lethal dose (LD50) values of 1 × 102 and 1.5 × 103 CFU, respectively, and no murine model has been developed thus far to evaluate the protective effects of vaccination through these routes. Most studies have instead vaccinated mice intradermally (i.d.) or s.c. Two of these studies specifically examined protection against an aerosol challenge with biovar A strains and obtained conflicting results: Hodge et al. found that s.c. vaccination protected mice against SCHU S5 for at least 30 days (16), whereas Chen et al. reported that i.d. vaccination failed to protect mice against biovar A strain 33 (5). These inconsistencies highlight the need to further investigate not only the protective effects generated by s.c. or i.d. vaccination but also those generated by respiratory vaccination. A more extensive understanding of pulmonary immunity against F. tularensis biovar A will greatly improve new vaccine development.
The purpose of the present study was to determine whether i.n. LVS vaccination induces effective protection in mice against an i.n. challenge with F. tularensis biovar A strains. We report that i.n. vaccination generated T-cell-dependent immunity in BALB/c mice but not in C57BL/6 mice which provided substantial resistance to i.n. and s.c. challenges with an F. tularensis biovar A strain.
MATERIALS AND METHODS
Mice and bacteria.
Female BALB/c, C3H/HeN, and DBA/2 mice were purchased from Harlan Sprague Dawley (Indianapolis, Ind.), and C57BL/6 mice were purchased from The Jackson Laboratory (Bar Harbor, Maine). The mice were housed in ventilated cages in a specific-pathogen-free facility at The University of New Mexico. The F. tularensis strain LVS was obtained from the U.S. Army Medical Research Institute of Infectious Diseases (Frederick, Md.). The F. tularensis biovar A strain NMFTA1, originally isolated during an autopsy of a dead cat in New Mexico, was obtained from the New Mexico Department of Health, Scientific Laboratory Division (Albuquerque, N.Mex.). Stocks were made from bacteria cultured in Mueller-Hinton II broth (Becton Dickinson Microbiology Systems, Sparks, Md.) supplemented with 1.2 mM CaCl2, 1 mM MgCl2, 335 nM Fe4(P2O7)3, 0.1% glucose, and 2% Isovitalex and were stored in aliquots at −70°C. The viability of the stocks after storage at −70°C was >50%. The concentration of viable bacteria in the stocks after freezing was 2.35 × 109 CFU/ml for LVS and 4.5 × 109 CFU/ml for NMFTA1. Yersinia pestis was obtained from the New Mexico Department of Health, Scientific Laboratory Division, and stocks were made from bacteria cultured on 5% sheep blood agar plates (Remel, Lenexa, Kans.) at 26°C. All protocols have been approved by the Institutional Animal Care and Use Committee and the Biosafety Committee at the University of New Mexico.
Subspecies genotyping by direct PCR.
Whole-cell DNAs were prepared by use of a DNeasy tissue kit (QIAGEN, Valencia, Calif.) according to the manufacturer's protocol for the isolation of genomic DNA from gram-negative bacteria. PCRs were performed in 20-μl reaction mixes containing 1 μl of template DNA, 1 μl (10 μM) each of the forward primer TuF1705 (GAT AGA TAC ACG CCT TGC TCA CA) and the reverse primer TuR3740 (GAG CCA TCG ATC GGT CTT CA), and 1 U of Taq DNA polymerase (Promega, Madison, Wis.). The template DNA was amplified by 35 cycles at 94°C for 5 s, 55°C for 1 min, and 72°C for 2 min. The products were analyzed by agarose gel electrophoresis, and DNAs were visualized by ethidium bromide staining. F. tularensis positive controls were SCHU S4 (biovar A) and LVS (biovar B). The SCHU S4 DNA was kindly provided by May C. Chu (Centers for Disease Control and Prevention, Fort Collins, Colo.) and is from the same origin as the SCHU S4 sequence being published by the sequencing consortium. The PCRs detected the presence of an insertional element (ISFtu2) in biovar B strains that is absent from biovar A strains and F. tularensis subsp. novicida. The expected amplicon size for biovar A strains and F. tularensis subsp. novicida was 2,036 bp and that for biovar B strains was 2,896 bp (data not shown). The GenBank accession number for the ISFtu2 sequence comparison is AY062040.
Immunization and infection.
Frozen stocks of F. tularensis were thawed anew for each experiment and diluted in phosphate-buffered saline (PBS). For i.n. vaccination, mice were lightly anesthetized with isoflurane (Abbott Laboratories, Chicago, Ill.) and instilled i.n. with 50 μl of the inoculum. For s.c. vaccination, the mice were shaved and injected s.c. in the right flank with 100 μl of the inoculum. For determinations of the deposition of bacteria in the lung, mice were killed an hour after i.n. infection by overexposure to CO2, and their entire lungs were removed aseptically and homogenized in 1 ml of PBS by use of a BeadBeater (Biospec Products, Bartlesville, Okla.). Fifty microliters of each homogenate was plated onto a cysteine heart agar plate with 5% sheep blood (Remel) by use of an Autoplate 4000 plater (Spiral Biotech, Bethesda, Md.). The bacteria were enumerated by Qcount colony counter (Spiral Biotech). A similar procedure was followed to process whole lungs, spleens, and livers to determine the bacterial burden in the three organs at the indicated time points after infection.
Determination of LD50 and mean time to death.
Mice were infected i.n. with increasing numbers of F. tularensis and monitored for survival for a period of 30 days. The LD50 was determined by the method developed by Reed and Muench (29). The mean time to death was calculated by dividing the sum of the survival times of all mice by the total number of mice examined.
Tissue processing and histopathological assessment.
Lungs were inflated with 10% neutral buffered formalin via a tracheal cannula and removed en bloc from the thorax. Lungs and other tissues were fixed for 24 to 72 h and then trimmed for paraffin embedding. Lungs were trimmed along the edges of the left main-stem bronchus and the right cranial, middle, and caudal lobar bronchi. The tissues were sectioned into 5-μm-thick sections and stained with hematoxylin and eosin. Histopathological assessments of lesions were performed by a board-certified veterinary pathologist. Four sections of each tissue were examined for each mouse. The lungs were examined in sections parallel to and including the main conducting airways (left lung, right caudal, right middle, and right cranial). Lesions were scored on a scale of 1 to 4 (minimal = 1, mild = 2, moderate = 3, and marked = 4) based upon the severity and distribution of the lesions. The scores for the animals were then averaged for the exposure group.
T-cell depletion in vivo.
Ascites fluids were produced at Taconic Farm (Germantown, N.Y.) by use of the hybridoma clones GK1.5 (anti-CD4; immunoglobulin G2b [IgG2b]), 2.43 (anti-CD8α), and SFR8-B6 (anti-HLA-Bw6; IgG2b), and the IgG concentrations were determined by high-performance liquid chromatography. Vaccinated mice were injected i.p. with 0.5 mg of the indicated depleting antibody every 7 days starting 3 days before infection. On the day of infection, the efficiency of depletion was determined. Lymphocytes were enriched from the peripheral blood of treated mice by the use of Lympholyte-M density separation medium (Cedarlane, Ontario, Canada), stained with peridinin chlorophyll protein-conjugated anti-CD8 (clone 53-6.7) and allophycocyanin-conjugated anti-CD4 (clone RM4-5) antibodies (BD Pharmingen, San Diego, Calif.), and analyzed by flow cytometry on a FACScalibur flow cytometer (BD Immunocytometry Systems, San Jose, Calif.). The antibody treatment reduced CD8 T cells from 10% to <0.1% and CD4 T cells from 33% to 0.8%.
Statistics.
Kaplan-Meier analyses of survival data and log-rank analyses were performed with Prism 4 software (GraphPad Software, San Diego, Calif.). Differences were considered significant when P values were <0.05.
RESULTS
Characterization of a clinically isolated F. tularensis biovar A strain.
We decided to develop a murine model of pneumonic tularemia using a strain of F. tularensis biovar A that is more clinically relevant than the more commonly studied strain SCHU S4. NMFTA1 was classified as a biovar A strain by use of a PCR-based genotyping assay that distinguished biovar A strains from biovar B strains (data not shown). NMFTA1 is a fast-growing strain that produces shiny, grayish colonies on cysteine heart agar plates in 3 days. Intranasal infection with an estimated dose of <10 NMFTA1 organisms killed all BALB/c, C57BL/6, DBA/2, and C3H/HeN mice in 5 to 7 days (Table 1). This dose is similar to the reported LD50 of aerosolized SCHU S5 of 80 CFU for LAF1 mice (16) and of strain 33 of 10 to 20 CFU for BALB/c and C57BL/6 mice (6).
TABLE 1.
Susceptibility of mouse strains to i.n. infection with NMFTA1
| Mouse strain | Bacterial inoculum (CFU) | Survival ratioa | Mean time to death (days) |
|---|---|---|---|
| BALB/c | 8 × 100 | 1/10 | 6.0 |
| 4 × 101 | 0/10 | 5.7 | |
| 2 × 102 | 0/10 | 5.1 | |
| 1 × 103 | 0/10 | 4.9 | |
| C57BL/6 | 8 × 100 | 1/10 | 5.6 |
| 4 × 101 | 0/10 | 5.2 | |
| 2 × 102 | 0/10 | 4.5 | |
| 1 × 103 | 0/10 | 4.2 | |
| DBA/2 | 8 × 100 | 5/10 | 6.5 |
| 4 × 101 | 1/10 | 6.1 | |
| 2 × 102 | 0/10 | 5.2 | |
| 1 × 103 | 0/10 | 5.0 | |
| C3H/HeN | 8 × 100 | 2/10 | 6.2 |
| 4 × 101 | 0/10 | 5.3 | |
| 2 × 102 | 0/10 | 5.1 | |
| 1 × 103 | 0/10 | 4.4 |
Survival ratio, number of mice alive/total number of mice inoculated 6 days after challenge. All mice died 7 days after challenge.
To further characterize the phenotype of NMFTA1 in vivo, we inoculated naïve BALB/c mice i.n. with approximately 200 CFU of NMFTA1. The number of bacteria in the lungs increased 100-fold within the first day and >10-fold every day thereafter (Table 2). When the bacterial burden in the lung approached 105 CFU 1 to 2 days after infection, systemic dissemination to the spleen and liver became evident. NMFTA1 continued to expand exponentially in the spleen and liver, reaching 108 to 109 CFU when the infected mice died 5 to 6 days after infection.
TABLE 2.
Kinetics of NMFTA1 growth and dissemination to reticuloendothelial organsa
| Day after infection | Log10F. tularensis cells/organ (CFU)c
|
||
|---|---|---|---|
| Lung | Spleen | Liver | |
| 0 | 2.30 ± 0.10 | <2.30b | <2.30 |
| 1 | 4.98 ± 0.04 | <2.30 | <2.30 |
| 2 | 6.52 ± 0.05 | 3.40 ± 0.18 | 3.57 ± 0.15 |
| 3 | 7.47 ± 0.12 | 6.18 ± 0.56 | 6.33 ± 0.44 |
| 4 | 8.53 ± 0.10 | 9.08 ± 0.25 | 7.66 ± 0.17 |
BALB/c mice were inoculated i.n. with approximately 200 CFU of NMFTA1. Three mice were killed on the day of infection (day 0) and four mice were killed every day thereafter to determine the bacterial burdens in the indicated organs.
The limit of detection was 200 CFU.
Data are means ± standard deviations.
Intranasal LVS vaccination provides better protection than subcutaneous vaccination from intranasal F. tularensis challenge.
Efforts to vaccinate mice against pulmonary infection of virulent F. tularensis strains by i.d. or s.c. inoculation of LVS have not produced consistent results (5, 16). We hypothesized that i.n. vaccination would protect mice better against an i.n. NMFTA1 challenge than s.c. vaccination. We first determined the growth kinetics of LVS in naïve BALB/c mice because it would be ideal to measure the resistance of vaccinated mice after LVS had been cleared. Preliminary experiments had indicated that i.n. inoculation with 5 × 103 CFU of LVS would kill all naïve BALB/c mice in 7 to 9 days (data not shown), and therefore, the kinetics of LVS growth and clearance were determined for naïve BALB/c mice inoculated with a sublethal dose of approximately 2 × 102 CFU of LVS. Five days after inoculation, the LVS burden reached over 106 CFU in the lung and 105 in the liver and spleen (Fig. 1). The number of LVS started to decline 10 days after infection and continued until the bacterial burden in the three organs fell below the detection limit of 2 × 102 CFU. Similar kinetics have been reported for the growth and clearance of LVS following i.d. vaccination (12, 14).
FIG. 1.
Kinetics of growth and clearance of LVS in naïve BALB/c mice. BALB/c mice were inoculated i.n. with approximately 200 CFU of LVS. Four mice were killed every 5 days to determine the bacterial burdens in the indicated organs. The horizontal dashed line represents the level of detection for the assay, and when the number of bacteria fell below this level, a value of 200 CFU was used to calculate the mean. The error bars show standard deviations.
Intranasal LVS vaccination completely protected BALB/c mice from an i.n. challenge with 2 × 102 CFU of NMFTA1 (P < 0.01) (Fig. 2A) and prolonged their survival after an i.n. challenge with 2 × 103 CFU of NMFTA1 approximately 9 days longer than that of unvaccinated mice (Fig. 2B; P < 0.01). Intranasal vaccination did not protect BALB/c mice from an i.n. challenge with 2 × 104 CFU of NMFTA1 (data not shown) or 104 CFU (LD100) of Y. pestis (Table 3) (P = 0.32). Subcutaneous LVS vaccination prolonged the survival of BALB/c mice challenged i.n. with 2 × 102 CFU of NMFTA1 (P < 0.01), but in contrast to the i.n. vaccinated mice, 40 to 80% of the s.c. vaccinated mice died <20 days after challenge (Fig. 2A) and none of them survived an i.n. challenge with 2 × 103 CFU of NMFTA1 (Fig. 2B). These results show that i.n. vaccination induced a stronger specific immunity to i.n. NMFTA1 challenge than did s.c. vaccination.
FIG. 2.
Intranasal vaccination provides more protection against respiratory NMFTA1 challenge than s.c. vaccination. BALB/c mice (four to five per group) were vaccinated i.n. with 2 × 102 CFU or s.c. with 2 × 105 CFU of LVS. Twenty-one days after vaccination, i.n. and s.c. vaccinated mice and unvaccinated mice were challenged i.n. with 2 × 102 (A) or 2 × 103 (B) CFU of NMFTA1. All vaccinated mice that survived infection beyond 30 days survived at least two more months.
TABLE 3.
Intranasal LVS vaccination induced specific protection against i.n. challenge of F. tularensis but not Y. pestis
| Expt no. | Vaccination status | Challenge organism | Survival (no. of survivors/no. tested) | Mean time to death (days) |
|---|---|---|---|---|
| 1a | None | LVS | 0/4 | 6.5 |
| LVS | LVS | 4/4 | ||
| None | NMFTA1 | 0/4 | 5.5 | |
| LVS | NMFTA1 | 4/4 | ||
| 2b | None | NMFTA1 | 0/4 | 5.0 |
| LVS | NMFTA1 | 3/3 | ||
| None | Y. pestis | 0/4 | 4.0 | |
| LVS | Y. pestis | 0/4 | 4.0 | |
| 3c | None | Y. pestis | 0/10 | 3.2 |
| LVS | Y. pestis | 0/10 | 3.6 |
Vaccinated BALB/c mice were challenged i.n. with 5 × 104 CFU of LVS or 2 × 102 CFU of NMFTA1. The results show survival ratios on day 16 postinfection.
Vaccinated BALB/c mice were challenged i.n. with 2 × 102 CFU of NMFTA1 or 104 CFU of Y. pestis. The results show survival ratios on day 26 postinfection.
Vaccinated BALB/c mice were challenged i.n. with 104 CFU of Y. pestis and were monitored until death.
Previous LVS vaccination studies using rats showed that virulent SCHU S4 can be recovered from the lungs and the cervical and mediastinal lymph nodes 14 days after an i.n. or aerogenic challenge (21). To determine whether NMFTA1 infection follows a similar course in vaccinated mice, we determined the bacterial burden at various time points up to 15 days after the i.n. NMFTA1 challenge. In naïve BALB/c mice, NMFTA1 proliferated exponentially in the lungs and spleen, reaching upwards of 108 to 109 CFU when the infected mice died 4 to 5 days after challenge (Fig. 3). In vaccinated BALB/c mice, NMFTA1 proliferation in the lungs was controlled 2 days after infection and was limited to a maximum of 3 × 105 CFU (Fig. 3A). The bacterial load decreased 20-fold in the next 2 days and then was maintained at a relatively stable level of slightly over 104 CFU. NMFTA1 was found in the spleen and liver 1 day after infection, and after a brief initial expansion, the numbers of bacteria were maintained at relatively stable levels of 104 CFU in the spleen (Fig. 3B) and 103 CFU in the liver (data not shown). NMFTA1 was recovered from 12 of 19 mice that survived infection for over 2 months and appeared clinically healthy (data not shown).
FIG. 3.
Intranasally vaccinated mice control NMFTA1 proliferation in vivo. BALB/c mice were vaccinated i.n. with 2 × 102 CFU of LVS and 21 days later were challenged i.n. with 2 × 102 CFU of NMFTA1. NMFTA1 burdens in the lungs (A) and spleens (B) of five naïve mice and three to six vaccinated mice were determined up to 15 days after challenge. The error bars show standard devations. The results from two independent experiments were pooled.
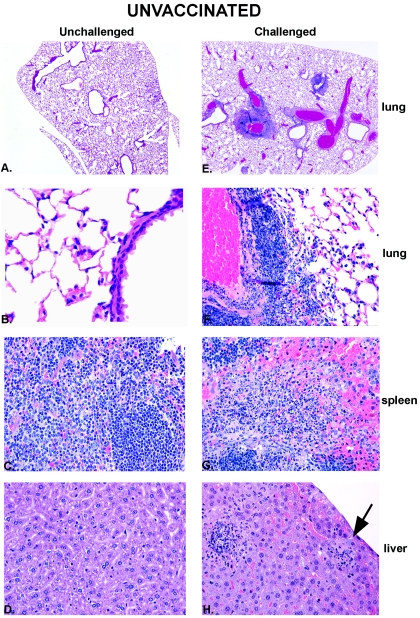
Histological appearance of tissues from unvaccinated and vaccinated BALB/c mice after NMFTA1 infection.
Tissues from unvaccinated and i.n. vaccinated BALB/c mice were examined immediately prior to challenge and 4 days after an i.n. challenge with 2 × 102 CFU of NMFTA1. Representative histologic images of lungs, spleens, and livers from unvaccinated mice that were left unchallenged as controls (unvaccinated/unchallenged) or challenged with NMFTA1 (unvaccinated/challenged) are shown in Fig. 4. Four days after the challenge, the lungs from unvaccinated/challenged mice had moderate, multifocal to coalescing, pyogranulomatous and lymphocytic to necrotizing peribronchovascular inflammation, often with neutrophilic to necrotizing vasculitis, and moderate, multifocal pyogranulomatous to necrotizing bronchopneumonia (Fig. 4E and F). The spleens from the unvaccinated/challenged mice demonstrated multifocal to coalescing areas of neutrophilic to pyogranulomatous splenitis with necrosis involving the splenic red pulp and also showed apoptosis of splenic lymphocytes (Fig. 4G). The livers from the unvaccinated/challenged mice showed multifocal neutrophilic and lymphohistiocytic hepatitis with prominent hepatocellular necrosis and many small colonies of extracellular bacteria (Fig. 4H).
FIG. 4.
Histologic appearance of unvaccinated BALB/c mice preceding and 4 days after intranasal NMFTA1 infection. Hematoxylin- and eosin-stained tissues from unvaccinated, unchallenged (control) mice are shown on the left (A to D), and those from unvaccinated, challenged mice are shown on the right (E to H). Necrotizing inflammation is evident in all tissues from challenged mice. The arrow points to a small colony of extracellular bacteria. Approximate magnifications: ×10 (A and E) and ×200 (B to D and F to H).
The same set of tissues were examined immediately before (vaccinated/unchallenged) and 4 days after (vaccinated/challenged) the vaccinated mice were challenged i.n. with 2 × 102 CFU of NMFTA1. The lungs from the vaccinated/unchallenged mice showed mild, multifocal, lymphohistiocytic and plasmacytic peribronchovascular inflammation with infrequent neutrophils and minimal foci of histiocytic and neutrophilic alveolitis (Fig. 5A and B). No lesions were observed in the spleens of vaccinated/unchallenged mice, and the livers showed only minimal foci of random lymphohistiocytic inflammation in the hepatic parenchyma and in the periportal triad regions (Fig. 5C and D). Sections of livers and lungs from the vaccinated/unchallenged mice were Gram stained to facilitate the detection of LVS in these tissues, but no bacteria were detected. The lungs of vaccinated/challenged mice showed mild to moderate, multifocal, lymphohistiocytic and plasmacytic peribronchovascular inflammation with occasional neutrophils and minimal, multifocal, neutrophilic and histiocytic alveolitis (Fig. 5E and F). The inflammatory foci were slightly expanded compared to those in vaccinated/unchallenged mice shown in Fig. 5A and B. The spleens from the vaccinated/challenged mice did not have lesions (Fig. 5G), and the livers exhibited mild, multifocal, random neutrophilic and lymphohistiocytic hepatitis with only minimal hepatocellular necrosis (Fig. 5H).
FIG. 5.
Histologic appearance of vaccinated BALB/c mice preceding and 4 days after intranasal NMFTA1 infection. Hematoxylin- and eosin-stained tissues from vaccinated, unchallenged mice are shown on the left (A to D), and those from vaccinated, challenged mice are shown on the right (E to H). The challenge with NMFTA1 increased the pulmonary and hepatic inflammation compared to that in vaccinated, unchallenged mice. Approximate magnifications: ×10 (A and E) and ×200 (B to D and F to H).
A comparison of the lesions in unvaccinated/challenged mice (Fig. 4E to H) and vaccinated/challenged mice (Fig. 5E to H) revealed the protective effects of i.n. LVS vaccination. The vaccinated/challenged mice exhibited less inflammation than the unvaccinated/challenged mice after the i.n. NMFTA1 challenge and, perhaps more importantly, the inflammation was less necrotizing. This correlated with the absence of detectable bacterial colonies in the hematoxylin- and eosin-stained sections from the vaccinated/challenged mice. These histological results, together with the results of the bacteriological studies, show that i.n. LVS vaccination induced a very effective immune response that controlled NMFTA1 proliferation and associated tissue destruction.
Boosting intranasal LVS-vaccinated mice with a sublethal dose of NMFTA1 increases their resistance to i.n. NMFTA1 challenge.
We next determined whether the protection elicited by i.n. LVS vaccination could be enhanced by boosting with either LVS or NMFTA1 prior to challenges with increasing numbers of NMFTA1. Both LVS and NMFTA1 were used because differences in the antigens expressed by these two strains may affect the result of the boost. BALB/c mice were vaccinated i.n. with 2 × 102 CFU of LVS and then boosted i.n. 21 days later with 5 × 104 CFU of LVS or 2 × 102 CFU of NMFTA1. This prime-boost protocol was well tolerated, and all of the mice appeared healthy 3 weeks after the boost, when they were challenged i.n. with NMFTA1. LVS-vaccinated mice that were boosted with NMFTA1 were significantly more protected from an i.n. challenge with 2 × 103 CFU of NMFTA1 than vaccinated mice without a boost (Fig. 6A; P < 0.01). Interestingly, the vaccinated mice that had been treated with PBS instead of the NMFTA1 boost were no longer protected from an i.n. challenge with 2 × 103 CFU of NMFTA1 (Fig. 6A). The inability of vaccinated mice to resist an NMFTA1 challenge could reflect a more general loss of immunity against F. tularensis, including LVS. However, the vaccinated mice treated with PBS remained resistant to i.n. challenge with a lethal dose of 5 × 104 CFU of LVS (Fig. 6B; P < 0.01).
FIG. 6.
Boosting LVS-vaccinated mice with NMFTA1 but not LVS increases their resistance to i.n. NMFTA1 challenge. (A and B) LVS-vaccinated BALB/c mice (four to six per group) were boosted i.n. with 2 × 102 CFU of NMFTA1 and 21 days later were challenged i.n. with 2 × 103 CFU of NMFTA1 (A) or 5 × 104 CFU of LVS (B). (C and D) Vaccinated BALB/c mice (five per group) were boosted i.n. with 2 × 102 CFU of NMFTA1 (C) or 5 × 104 CFU of LVS (D) and challenged i.n. 21 days later with the indicated doses of NMFTA1.
To determine whether the strain of F. tularensis used for the boost affected the level of resistance to i.n. NMFTA1 challenge, we challenged vaccinated BALB/c mice boosted with 2 × 102 CFU of NMFTA1 or 5 × 104 CFU of LVS i.n. with 2 × 103, 2 × 104, or 2 × 105 CFU of NMFTA1. Boosting with NMFTA1 enabled the vaccinated mice to survive i.n. challenges up to 2 × 104 but not 2 × 105 CFU of NMFTA1 (Fig. 6C) and increased the i.n. LD50 of NMFTA1 from 900 CFU to 1.1 × 104 CFU. In contrast, boosting with LVS failed to increase the resistance of vaccinated mice against an i.n. challenge with 2 × 103 CFU of NMFTA1 (Fig. 6D; P = 0.17).
LVS-vaccinated C57BL/6 mice survive longer but succumb to intranasal NMFTA1 infection.
LVS vaccination did not protect C57BL/6 mice as well as BALB/c mice against an i.d. challenge with F. tularensis biovar A (5). We wanted to determine whether this difference also existed when the two strains of mice were vaccinated i.n. with LVS and then challenged i.n. with NMFTA1. Intranasal vaccination significantly prolonged the survival of C57BL/6 mice challenged i.n. with 2 × 102 CFU of NMFTA1 (Fig. 7A; P < 0.01), but unlike the vaccinated BALB/c mice that survived the length of observation, all vaccinated C57BL/6 mice died within 12 days of challenge (Fig. 7B; P < 0.01). Boosting the vaccinated C57BL/6 mice with 5 × 104 CFU of LVS did not prolong their survival compared to that of vaccinated C57BL/6 mice that did not receive a boost (Fig. 7C; P = 0.15).
FIG. 7.
LVS vaccination does not protect C57BL/6 mice as well as BALB/c mice against i.n. NMFTA1 challenge. (A) Vaccinated and unvaccinated C57BL/6 mice (n = 4) were challenged i.n. with 2 × 102 CFU of NMFTA1 22 days after vaccination. (B) Survival rates of vaccinated C57BL/6 mice (n = 4) and vaccinated BALB/c mice (n = 5) after i.n. challenge with 2 × 102 CFU of NMFTA1. (C) Naïve, freshly vaccinated C57BL/6 mice and vaccinated C57BL/6 mice boosted with 5 × 104 CFU of LVS (five to six per group) were challenged i.n. with 2 × 102 CFU of NMFTA1.
Intranasal vaccination protects mice against subcutaneous F. tularensis infection.
An ideal vaccine protects not only against respiratory infection but also against infections through other portals of entry. Accordingly, we determined whether i.n. LVS vaccination also protected mice against an s.c. NMFTA1 challenge. BALB/c mice were vaccinated i.n. with 2 × 102 CFU of LVS and then challenged s.c. 3 weeks later with 2 × 102 or 2 × 103 CFU of NMFTA1 on the right flank. Subcutaneous NMFTA1 infection did not cause detectable skin lesions in any of the mouse groups. The unvaccinated mice died within a week of s.c. challenge, whereas eight of nine vaccinated mice challenged with 2 × 102 CFU (P < 0.01) and seven of nine mice challenged with 2 × 103 CFU of NMFTA1 (P < 0.02) survived at least 30 days after challenge (Table 4).
TABLE 4.
Intranasal LVS vaccination protected mice against s.c. NMFTA1 challengea
| Vaccination status | Challenge dose (CFU) | Survival (no. of survivors/no. tested) |
|---|---|---|
| None | 2 × 102 | 0/9 |
| None | 2 × 103 | 0/4 |
| LVS | 2 × 102 | 8/9 |
| LVS | 2 × 103 | 7/9 |
BALB/c mice were vaccinated i.n. with 200 CFU of LVS and 3 weeks later were challenged s.c. with 2 × 102 or 2 × 103 CFU of NMFTA1. The results show survival ratios on day 30 postchallenge, and all deaths occurred 5 to 6 days after challenge.
αβ T cells are required for generating protective immunity and for controlling chronic infection.
To determine the role of αβ T cells in the resistance against i.n. NMFTA1 challenge, we depleted unvaccinated and LVS-vaccinated BALB/c mice of CD4, CD8, or both CD4 and CD8 T cells before challenging them i.n. with 2 × 102 CFU of NMFTA1. T-cell depletion did not further increase the susceptibility of unvaccinated BALB/c mice to the i.n. NMFTA1 challenge (Fig. 8A). Most of the vaccinated BALB/c mice depleted of either CD8 or CD4 T cells lived 4 days longer than unvaccinated mice (P < 0.01 and P = 0.01, respectively) but still died 10 to 13 days after infection (Fig. 8B). The depletion of both CD4 and CD8 T cells eliminated the protective effects of vaccination (P < 0.01), and the mice died at approximately the same time as unvaccinated mice after the i.n. NMFTA1 challenge.
FIG. 8.
αβ T cells are required for protection against respiratory NMFTA1 infection. Naïve (A) and vaccinated (B) BALB/c mice (n = 5) were depleted of CD4, CD8, or both CD4 and CD8 T cells by intraperitoneal injection of ascites fluid. Three days after antibody treatment, the T-cell-depleted mice were challenged i.n. with 2 × 102 CFU of NMFTA1.
DISCUSSION
Intranasal LVS vaccination provided BALB/c mice with strong protection against a lethal i.n. challenge with the virulent F. tularensis biovar A strain NMFTA1. Boosting the LVS-vaccinated mice i.n. with a sublethal dose of NMFTA1 further increased the level of protection, enabling the vaccinated mice to resist a 100-fold larger dose of NMFTA1. The protection was mediated by a T-cell-dependent mechanism that was specific for F. tularensis. Intranasal vaccination did not inhibit the early proliferation of NMFTA1 in the lung or systemic dissemination to the spleen and liver but prevented NMFTA1 from proliferating to lethal levels. This limited the damage inflicted on the various organs by the infection and associated inflammatory responses. Intranasal vaccination also protected BALB/c mice against s.c. NMFTA1 challenge, showing that i.n. vaccination provided generalized protection against tularemia.
Our results support a growing body of literature showing that i.n. or aerogenic vaccination induces the best protection against respiratory infections by microbial pathogens such as F. tularensis biovar A (11, 36), influenza virus (28), and M. tuberculosis (2, 22). Respiratory vaccination is unique in its ability to induce long-lived memory T cells in the lung that can rapidly respond to respiratory infections (15). The importance of these cells is suggested by the correlation between the decline of resident memory T cells in the lung and the loss of cellular immunity to respiratory virus infections (4, 17, 23). The complex process by which these cells are induced and maintained in the lung is only beginning to be understood. Respiratory vaccination can deliver bacterial antigens directly to the lung-associated lymph nodes to induce antigen-specific memory T cells that home to the lung (15, 27). Bacteriological studies with Macaca irus monkeys (10, 25, 37) and a survival study with Macaca mulatta monkeys (11) showed that LVS could be cultured from the tracheobronchial and cervical lymph nodes very consistently across time points after aerogenic vaccination, which protected eight of eight monkeys from a respiratory challenge with the biovar A strain SCHU S5, but very sporadically after intracutaneous vaccination, which protected only four of seven monkeys against SCHU S5. Such a mechanism may also determine the level of protection in mice, since LVS was recovered from the mediastinal lymph node after aerogenic vaccination (16), but whether this result is unique to respiratory vaccination and cannot be achieved through other vaccination routes remains to be resolved. We propose that the localization of memory T cells to the lungs and associated lymph nodes is essential for mice to resist respiratory infection by F. tularensis biovar A.
Boosting LVS-vaccinated mice with NMFTA1 but not LVS significantly increased their resistance to a secondary i.n. NMFTA1 infection. This could have resulted from the expansion of T cells that recognize antigens that are expressed exclusively on NMFTA1 in addition to those T cells that recognize antigens shared by both LVS and NMFTA1. This hypothesis is consistent with a previous report from Eigelsbach et al. showing that the adoptive transfer of splenocytes from LVS-immunized mice boosted with SCHU S4 but not with LVS protected naïve mice from an intraperitoneal infection with the virulent biovar A strain SCHU S5 (9). Broekhuijsen et al. recently showed that there are eight regions of differences encompassing 21 open reading frames that are present in biovar A strains but not in biovar B strains (3). These open reading frames may encode proteins that contain the immunodominant epitopes expressed exclusively by biovar A strains and thereby direct the T-cell response specifically against biovar A strains. A second possibility is that the NMFTA1 boost induced superior protection because NMFTA1 survived much longer in vaccinated mice than LVS and sustained an enhanced T-cell immunity that contained the infection. This is supported by the observation that 12 of 19 vaccinated BALB/c mice carried NMFTA1 infection for more than 2 months after the boost, whereas LVS was cleared below detectable levels more rapidly after the boost (data not shown). The protracted NMFTA1 infection in vaccinated BALB/c mice is similar to murine models of tuberculosis (13) and leishmaniasis (1) that are actively controlled by a T-cell-dependent immune response and can be reactivated by immune suppression. It remains to be determined whether the extended latent infection is a unique feature of the murine vaccine model or is found in humans as well. We are not aware of any evidence that individuals who recovered from primary tularemia carry latent F. tularensis infections or develop recurrent tularemia associated with an immune deficiency or suppression. This is to be expected because humans are usually treated at the first sign of primary tularemia with highly effective antibiotics that completely eliminate the infection (8). There is also very little, if any, information on the long-term bacterial burden following secondary infections in individuals who have previously recovered from pneumonic tularemia or were vaccinated against F. tularensis, as modeled in this study.
The different susceptibilities of BALB/c and C57BL/6 mice to respiratory pathogens usually manifest following primary infection (18, 20, 26). However, we did not detect a difference in the susceptibilities of these two inbred strains until the secondary NMFTA1 infection in vaccinated mice, perhaps due to the extremely high growth rate of NMFTA1 in naïve mice. C57BL/6 mice appear to be more susceptible than BALB/c mice to respiratory infections by a variety of pathogens, such as Bacillus anthracis (24), Pseudomonas aeruginosa (26), Chlamydia pneumoniae, Chlamydia psittaci (18), Cryptococus neoformans (20), and Sindbis virus (35). Our results now show that vaccinated C57BL/6 mice are also more susceptible to i.n. NMFTA1 infection than vaccinated BALB/c mice, surviving only a few days longer than naive C57BL/6 mice. These results are consistent with the earlier observation that i.d. vaccinated C57BL/6 mice were more susceptible than vaccinated BALB/c mice to an i.d. challenge with the virulent biovar A strain 33 and to aerogenic infection with the virulent biovar B strain 108 (5). There are undoubtedly many factors that determine the susceptibility of vaccinated C57BL/6 mice and the resistance of vaccinated BALB/c mice to secondary NMFTA1 infections, as recently suggested by studies of Leishmania major infections (30). For example, pulmonary infections appear to cause more severe tissue damage in C57BL/6 mice than in BALB/c mice (19, 33) and possibly kill the infected mice by preventing normal organ functions. C57BL/6 mice can also produce higher levels of factors such as nitric oxide that suppress effective antibacterial immunity (18). A third possibility is that the predisposition of C57BL/6 mice to develop a Th2 phenotype in the lung (7) precludes them from developing a protective Th1 response. Finally, it is possible that LVS vaccination failed to induce and maintain sufficient numbers of antigen-specific memory T cells in the lungs of C57BL/6 mice to respond effectively to the i.n. NMFTA1 challenge.
The finding that i.n. vaccination reproducibly protected BALB/c mice from respiratory tularemia is a major advancement in vaccine development. It shows that for mice, as for other animal models, including nonhuman primates, respiratory vaccination generated the most protection against pneumonic tularemia. This murine model will enable investigators to study the pulmonary immune responses that protect against respiratory infection with virulent F. tularensis and to develop strategies to induce those protective responses in humans.
Acknowledgments
This work was funded by Infectious Disease and Inflammation Training Program grant 2 T32 AI007538-06 and Defense Advanced Research Projects Agency grant N00178-01-C-3069.
We thank May C. Chu for providing the SCHU S4 DNA, primer sequences, and the protocol for genotyping NMFTA1 as a biovar A strain. We are also grateful to Mary F. Lipscomb, Julie A. Lovchik, and Erin L. Ashbeck for thoughtful discussions and advice.
Editor: J. D. Clements
REFERENCES
- 1.Aebischer, T., S. F. Moody, and E. Handman. 1993. Persistence of virulent Leishmania major in murine cutaneous leishmaniasis: a possible hazard for the host. Infect. Immun. 61:220-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barclay, W. R., W. M. Busey, D. W. Dalgard, R. C. Good, B. W. Janicki, J. E. Kasik, E. Ribi, C. E. Ulrich, and E. Wolinsky. 1973. Protection of monkeys against airborne tuberculosis by aerosol vaccination with bacillus Calmette-Guerin. Am. Rev. Respir. Dis. 107:351-358. [DOI] [PubMed] [Google Scholar]
- 3.Broekhuijsen, M., P. Larsson, A. Johansson, M. Bystrom, U. Eriksson, E. Larsson, R. G. Prior, A. Sjostedt, R. W. Titball, and M. Forsman. 2003. Genome-wide DNA microarray analysis of Francisella tularensis strains demonstrates extensive genetic conservation within the species but identifies regions that are unique to the highly virulent F. tularensis subsp. tularensis. J. Clin. Microbiol. 41:2924-2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cauley, L. S., T. Cookenham, T. B. Miller, P. S. Adams, K. M. Vignali, D. A. Vignali, and D. L. Woodland. 2002. Cutting edge: virus-specific CD4+ memory T cells in nonlymphoid tissues express a highly activated phenotype. J. Immunol. 169:6655-6658. [DOI] [PubMed] [Google Scholar]
- 5.Chen, W., H. Shen, A. Webb, R. KuoLee, and J. W. Conlan. 2003. Tularemia in BALB/c and C57BL/6 mice vaccinated with Francisella tularensis LVS and challenged intradermally, or by aerosol with virulent isolates of the pathogen: protection varies depending on pathogen virulence, route of exposure, and host genetic background. Vaccine 21:3690-3700. [DOI] [PubMed] [Google Scholar]
- 6.Conlan, J. W., W. Chen, H. Shen, A. Webb, and R. KuoLee. 2003. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microb. Pathog. 34:239-248. [DOI] [PubMed] [Google Scholar]
- 7.Constant, S. L., K. S. Lee, and K. Bottomly. 2000. Site of antigen delivery can influence T cell priming: pulmonary environment promotes preferential Th2-type differentiation. Eur. J. Immunol. 30:840-847. [DOI] [PubMed] [Google Scholar]
- 8.Dennis, D. T., T. V. Inglesby, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, A. M. Friedlander, J. Hauer, M. Layton, S. R. Lillibridge, J. E. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763-2773. [DOI] [PubMed] [Google Scholar]
- 9.Eigelsbach, H. T., D. H. Hunter, W. A. Janssen, H. G. Dangerfield, and S. G. Rabinowitz. 1975. Murine model for study of cell-mediated immunity: protection against death from fully virulent Francisella tularensis infection. Infect. Immun. 12:999-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eigelsbach, H. T., J. J. Tulis, M. H. McGavran, and J. D. White. 1962. Live tularemia vaccine. I. Host-parasite relationship in monkeys vaccinated intracutaneously or aerogenically. J. Bacteriol. 84:1020-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eigelsbach, H. T., J. J. Tulis, E. L. Overholt, and W. R. Griffith. 1961. Aerogenic immunization of the monkey and guinea pig with live tularemia vaccine. Proc. Soc. Exp. Biol. Med. 108:732-734. [DOI] [PubMed] [Google Scholar]
- 12.Elkins, K. L., D. A. Leiby, R. K. Winegar, C. A. Nacy, and A. H. Fortier. 1992. Rapid generation of specific protective immunity to Francisella tularensis. Infect. Immun. 60:4571-4577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flynn, J. L., and J. Chan. 2001. Immunology of tuberculosis. Annu. Rev. Immunol. 19:93-129. [DOI] [PubMed] [Google Scholar]
- 14.Fortier, A. H., M. V. Slayter, R. Ziemba, M. S. Meltzer, and C. A. Nacy. 1991. Live vaccine strain of Francisella tularensis: infection and immunity in mice. Infect. Immun. 59:2922-2928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gallichan, W. S., and K. L. Rosenthal. 1996. Long-lived cytotoxic T lymphocyte memory in mucosal tissues after mucosal but not systemic immunization. J. Exp. Med. 184:1879-1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hodge, F. A., W. R. Leif, and M. S. Silverman. 1968. Susceptibility to infection with Pasteurella tularensis and the immune response of mice exposed to continuous low dose rate gamma radiation. NRDL-TR-68-85. Res. Dev. Tech. Rep. 1968:1-28. [PubMed] [Google Scholar]
- 17.Hogan, R. J., E. J. Usherwood, W. Zhong, A. A. Roberts, R. W. Dutton, A. G. Harmsen, and D. L. Woodland. 2001. Activated antigen-specific CD8+ T cells persist in the lungs following recovery from respiratory virus infections. J. Immunol. 166:1813-1822. [DOI] [PubMed] [Google Scholar]
- 18.Huang, J., F. J. DeGraves, S. D. Lenz, D. Gao, P. Feng, D. Li, T. Schlapp, and B. Kaltenboeck. 2002. The quantity of nitric oxide released by macrophages regulates Chlamydia-induced disease. Proc. Natl. Acad. Sci. USA 99:3914-3919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huffnagle, G. B., M. B. Boyd, N. E. Street, and M. F. Lipscomb. 1998. IL-5 is required for eosinophil recruitment, crystal deposition, and mononuclear cell recruitment during a pulmonary Cryptococcus neoformans infection in genetically susceptible mice (C57BL/6). J. Immunol. 160:2393-2400. [PubMed] [Google Scholar]
- 20.Huffnagle, G. B., J. L. Yates, and M. F. Lipscomb. 1991. T cell-mediated immunity in the lung: a Cryptococcus neoformans pulmonary infection model using SCID and athymic nude mice. Infect. Immun. 59:1423-1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jemski, J. V. 1981. Respiratory tularemia: comparison of selected routes of vaccination in Fischer 344 rats. Infect. Immun. 34:766-772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lefford, M. J. 1977. Induction and expression of immunity after BCG immunization. Infect. Immun. 18:646-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liang, S., K. Mozdzanowska, G. Palladino, and W. Gerhard. 1994. Heterosubtypic immunity to influenza type A virus in mice. Effector mechanisms and their longevity. J. Immunol. 152:1653-1661. [PubMed] [Google Scholar]
- 24.Lyons, C. R., J. Lovchik, J. Hutt, M. F. Lipscomb, E. Wang, S. Heninger, L. Berliba, and K. Garrison. 2004. Murine model of pulmonary anthrax: kinetics of dissemination, histopathology, and mouse strain susceptibility. Infect. Immun. 72:4801-4809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGavran, M. H., J. D. White, H. T. Eigelsbach, and R. W. Kerpsack. 1962. Morphologic and immunohistochemical studies of the pathogenesis of infection and antibody formation subsequent to vaccination of Macaca irus with an attenuated strain of Pasteurella tularensis. I. Intracutaneous vaccination. Am. J. Pathol. 41:259-271. [PMC free article] [PubMed] [Google Scholar]
- 26.Morissette, C., E. Skamene, and F. Gervais. 1995. Endobronchial inflammation following Pseudomonas aeruginosa infection in resistant and susceptible strains of mice. Infect. Immun. 63:1718-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mullins, D. W., S. L. Sheasley, R. M. Ream, T. N. J. Bullock, Y. Fu, and V. H. Engelhard. 2003. Route of immunization with peptide-pulsed dendritic cells controls the distribution of memory and effector T cells in lymphoid tissues and determines the pattern of regional tumor control. J. Exp. Med. 198:1023-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Novak, M., Z. Moldoveanu, D. P. Schafer, J. Mestecky, and R. W. Compans. 1993. Murine model for evaluation of protective immunity to influenza virus. Vaccine 11:55-60. [DOI] [PubMed] [Google Scholar]
- 29.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 30.Sacks, D., and N. Noben-Trauth. 2002. The immunology of susceptibility and resistance to Leishmania major in mice. Nat. Rev. Immunol. 2:845-858. [DOI] [PubMed] [Google Scholar]
- 31.Saslaw, S., H. T. Eigelsbach, J. A. Prior, H. E. Wilson, and S. Carhart. 1961. Tularemia vaccine study. II. Respiratory challenge. Arch. Intern. Med. 107:702-714. [DOI] [PubMed] [Google Scholar]
- 32.Stuart, B. M., and R. L. Pullen. 1945. Tularemic pneumonia: review of American literature and report of 15 additional cases. Am. J. Med. Sci. 210:223-236. [Google Scholar]
- 33.Tam, M., G. J. Snipes, and M. M. Stevenson. 1999. Characterization of chronic bronchopulmonary Pseudomonas aeruginosa infection in resistant and susceptible inbred mouse strains. Am. J. Respir. Cell Mol. Biol. 20:710-719. [DOI] [PubMed] [Google Scholar]
- 34.Tarnvik, A. 1989. Nature of protective immunity to Francisella tularensis. Rev. Infect. Dis. 11:440-451. [PubMed] [Google Scholar]
- 35.Thach, D. C., T. Kimura, and D. E. Griffin. 2000. Differences between C57BL/6 and BALB/cBy mice in mortality and virus replication after intranasal infection with neuroadapted Sindbis virus. J. Virol. 74:6156-6161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tulis, J. J., H. T. Eigelsbach, and R. W. Kerpsack. 1970. Host-parasite relationship in monkeys administered live tularemia vaccine. Am. J. Pathol. 58:329-336. [PMC free article] [PubMed] [Google Scholar]
- 37.White, J. D., M. H. McGavran, P. A. Prickett, J. J. Tulis, and H. T. Eigelsbach. 1962. Morphologic and immunohistochemical studies of the pathogenesis of infection and antibody formation subsequent to vaccination of Macaca irus with an attenuated strain of Pasteurella tularensis. II. Aerogenic vaccination. Am. J. Pathol. 41:405-413. [PMC free article] [PubMed] [Google Scholar]