Abstract
Superficial acral fibromyxoma, also known as digital fibromyxoma, is a slow-growing, benign, solitary soft tissue tumor. First described in 2001 by Fetsch et al., it is a condition that often occurs in middle-aged individuals. However, it has also been reported across a wide range of ages, ranging from 4 to 86 years, with males more commonly reported. The condition often presents as solitary soft tissue swelling over the periungual or subungual.
We present the management experience of the rare presentation of this rare tumor and a detailed review of the past literature on this condition. Detailed management of the condition has been described, along with the outcome after 2 years of follow-up and treatment experience.
Our detailed analysis shows that 2 years is the shortest duration of follow-up to rule out recurrence. Hence, most of the cases reported earlier had given the false sense of the recurrence rate of the tumor, which could lead to undertreatment of the condition.
The purpose of this article is to allow the readers to understand better the tumor’s characteristics with bone involvement and the tumor's diagnostic strategies and treatment options.
Keywords: superficial acral fibromyxoma, digital fibromyxoma, periungual tumor, benign tumor, isolated finger clubbing, bone scalloping
Introduction
Superficial acral fibromyxoma, also known as digital fibromyxoma, is a slow-growing, benign, solitary soft tissue tumor (1). It was first described in 2001 by Fetsch et al. (2). Currently, 326 cases have been reported worldwide since its description. After its initial description, this particular tumor was not classified until 12 years later. It is categorized as a ‘Tumor of uncertain differentiation’, per the WHO classification of soft tissue tumors in the 2013 (fourth) edition (3). Although it is more commonly found in middle-aged individuals, it has been observed across a wide range of ages, from 4 to 86 years old. Notably, males are more frequently affected, according to Gupta et al. (4). The condition often presents as solitary soft tissue swelling over the periungual or subungual region (2). Here, we describe a case of a rare presentation of acral fibromyxoma with bone involvement, diagnostic strategies, treatment of the condition, and the literature review. Our case is also the first reported case in Malaysia.
Case review
A 34-year-old Malay gentleman presented with isolated right ring finger clubbing for 6 years and initially started with swelling over the right ring fingertip with disturbance of normal finger contour, progressively worsening and painless, ignored by the patient as not disturbing daily routine. However, due to the worsening of the finger deformity, the patient seeks medical attention. The patient is otherwise well and can perform his daily routine without difficulties – no other associated constitutional symptoms.
Clinical examination shows an isolated bulbous enlargement with shiny change in the right ring fingernail. Both longitudinal and transverse curvatures of the right ring fingernail plate are disturbed, obliteration of the Lovibond’s angle (>180°), positive in Curth’s modified profile sign, and obliteration of the Schamroth’s diamond window. The findings are consistent with grade 5 clubbing (Figs 1, 2 and 3). Otherwise, the sensation and the perfusion of the right ring finger pulp remained intact.
Figure 1.

Dorsal profile of the right hand, with isolated clubbing of the right ring finger.
Figure 2.

Medial profile of the right ring finger.
Figure 3.

Lateral profile of the right ring finger.
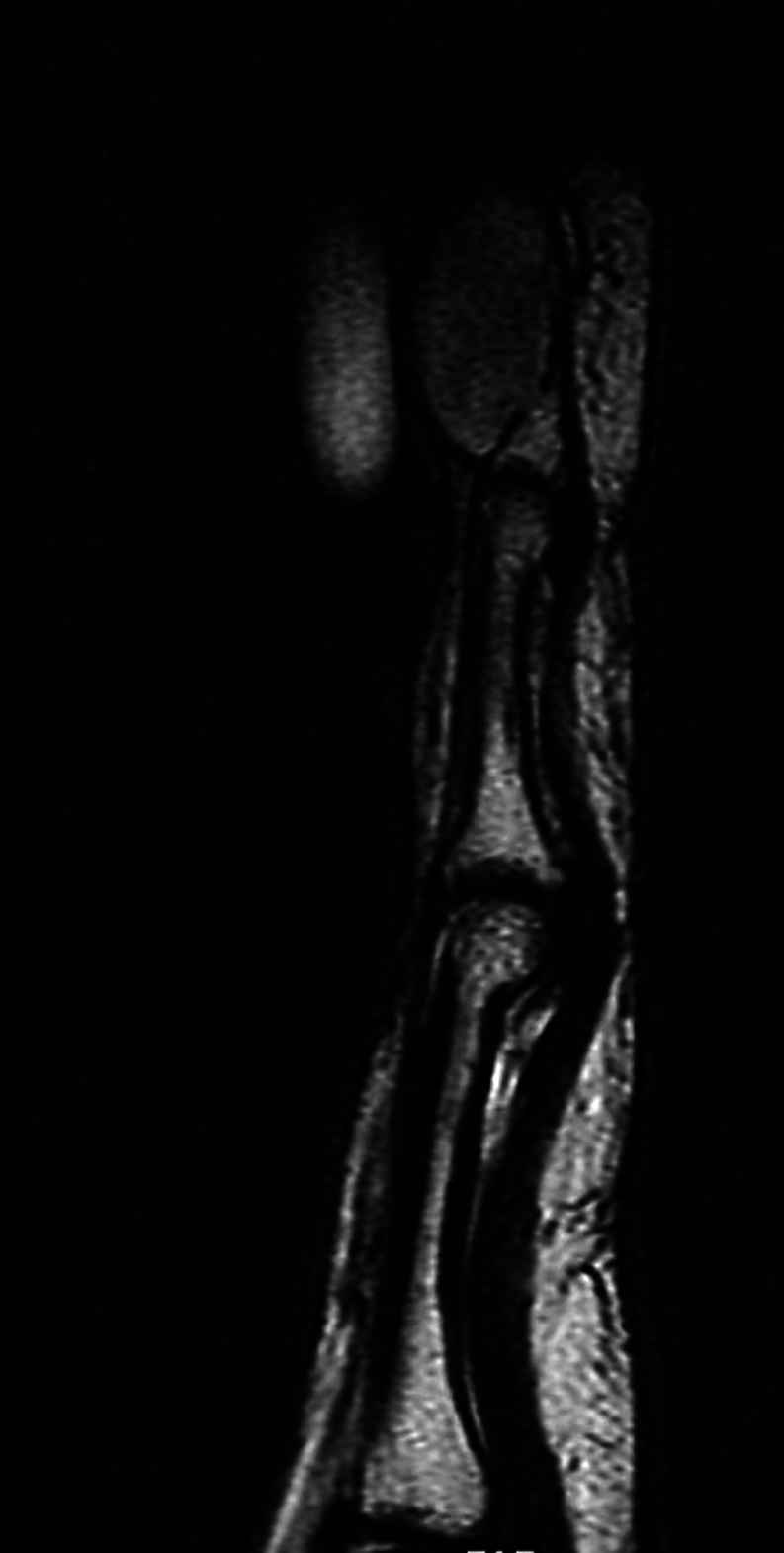
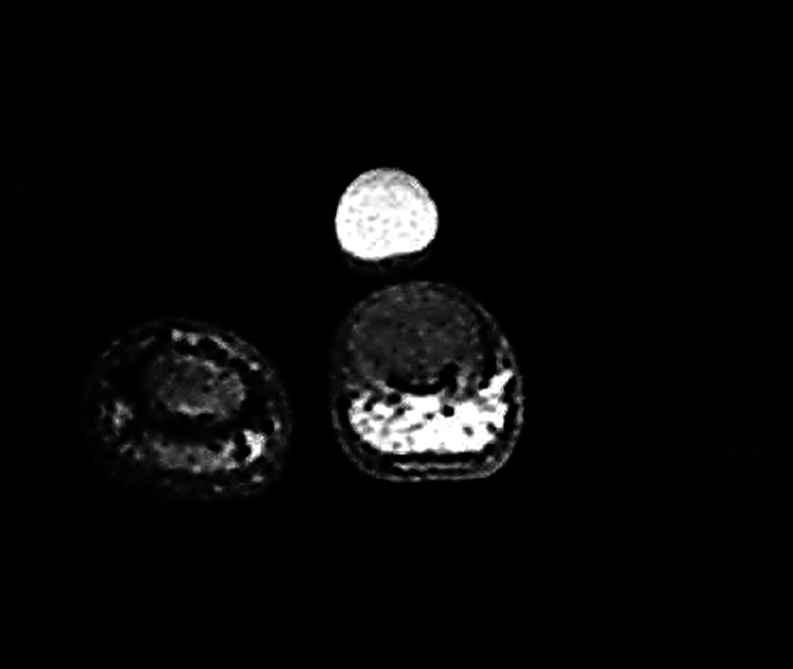
Radiographs of the right ring finger show an increased dorsal tissue shadow with scalloping of the mid and distal part of the distal phalanx without calcification or adjacent periosteal reaction (Figs 4 and 5). MRI shows a localized, solitary homogeneous soft tissue swelling (low T1 and high T2 signals) over the dorsum of the distal phalanx within the subcutaneous tissue level with scalloping of the distal phalanx (Figs 6, 7 and 8).
Figure 4.
Posteroanterior radiograph (X-ray, PA view) of lateral three digits of the right hand, showing signs of scalloping of the distal phalanx of the right ring finger.
Figure 5.
Lateral view of the right ring finger radiograph (X-ray), showing increased soft tissue shadow over the dorsum with scalloping of the distal phalanx of the right ring finger.
Figure 6.
Sagittal plane MRI image of the right ring finger, with the tumor exhibiting low signal intensity in T1.
Figure 7.
Axial plane MRI image of the right ring finger, with the tumor exhibiting low signal intensity in T1.
Figure 8.
Axial plane MRI image of the right ring finger, with the tumor exhibiting high homogeneous signal intensity in T2.
Excision biopsy was performed with a surgical tourniquet and adequate magnification with the insertion of autologous bone graft. The sterile matrix was preserved for functional and cosmetic purposes. The tumor was gently dissected from the sterile matrix. The tumor could be traced to the insertion site of the terminal tendon sheath and was removed in an en bloc manner. Subsequently, the underlying bone was curetted. As for the bony defect, a corticocancellous bone graft was taken from the distal radius and temporarily fixed to the donor region with a k-wire. As the fingernail was severely deformed, a temporary sterile artificial fingernail was reinserted to splint the eponychium fold. Macroscopically, the nodule (2 cm × 1 cm × 0.8 cm) appeared well circumscribed but unencapsulated, soft to firm (Fig. 9), and gelatinous white-grayish cut surface without necrosis or hemorrhage. Microscopically, the tumor comprises spindled and stellate-shaped fibroblasts in loose fascicular and broad storiform growth patterns embedded in a collagenous to a myxoid matrix (Fig. 10). There are mildly accentuated vasculature and many mast cells in the stroma. Mitotic figures are sparse (<1 mitosis per 10 high-power fields) – no multinucleate cells seen. Immunohistochemical studies showed the tumor has moderate-to-strong positivity to CD34 and is negative for S100 (Figs 9, 10 and 11).
Figure 9.

Macroscopic features of the nodule after excision. Measuring 2 cm × 1 cm × 0.8 cm. The nodule appeared well circumscribed, unencapsulated, and soft to firm in consistency.
Figure 10.
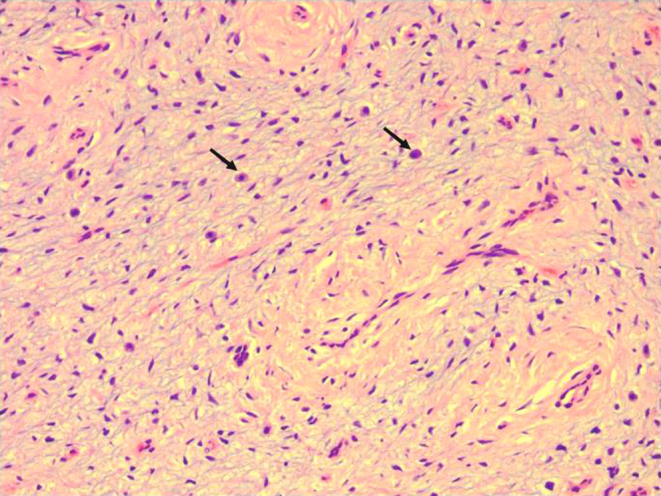
Photomicrograph of tumor showing spindle and stellate cells in a loose fibromyxoid background, traversed by fine blood vessels. Scattered mast cells are present (arrow). Hematoxyllin and eosin 20×.
Figure 11.
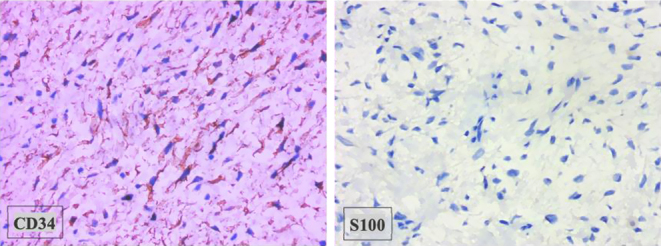
Photomicrograph showing CD34 cytopositivity (brown signals) and S100 negativity of the tumor cells. Immunohistochemistry 40×.
Postoperatively, the patient recovered well and returned to work without any disability or recurrence on follow-up by 1 year. However, there was a recurrence at the same site during the 2-year follow-up. The patient was counseled for amputation, considering the bony structure of the distal phalanx was minimal and to eliminate the risk of recurrence, which the patient refused due to the debilitating effect and cultural factors.
Literature review chart
The summary of the literature is listed in Supplementary Table 1 (see the section on supplementary materials given at the end of this article).
Discussion
Finger clubbing is a clinical condition whereby there is uniform bulbous swelling of the soft tissue of the terminal phalanx of a digit/toe – also known as drumstick fingers or Hippocratic fingers. A well-known clinical description could be traced back to 400b c by Hippocrates in an empyema patient. Many causes and etiology of such had been described, primarily systemic causes (ranging from pulmonary, infective, heart, hepatobiliary, gastrointestinal, and endocrine to even congenital) and some rare local causes (intraosseous epidermoid cyst, enchondroma, glomus tumor). The local single-clubbed finger is a rare condition due to the local proliferation of tissues/bone leading to clubbed features (1, 5).
Superficial acral fibromyxoma or digital fibromyxoma is still a relatively uncommon entity: it was first described in 2001 by Fetsch et al. (2), enlisted by WHO under ‘Tumors of uncertain differentiation’ in 2013 (3). Our literature search shows 326 cases reported worldwide since 1970 (41 retrospective cases reported by the UK from 1970 to 2006). The etiology of superficial acral fibromyxoma or an established predisposing factor is not well established. Though 20% of the reported cases were preceded by trauma, there is no clear association between the two. It is the possibility that the trauma drew the patient’s attention to the swelling (6). Clinically, the condition presents as a solitary nodular mass with firm consistency with a higher frequency of occurrence at the finger (125 cases) and toe region (150 cases), mainly occurring in the periungual/subungual locations. However, a small number of cases were reported in the other areas of the extremities, such as the hand (11 cases), foot (10 cases), heel (5 cases), leg (2 cases), and even thigh (1 case). There is a higher predisposition in middle-aged male patients with an estimated ratio of 2:1 (male:female), which is consistent with our analysis that revealed between the ages of 40 and 49 years had the highest incidence rate and slightly higher male predilection with a ratio of 1.5:1 (male:female). The unique characteristic of superficial acral fibromyxoma is the slow-growing tumor, which appears harmless. Still, it has been previously reported to cause scalloping of the underlying bone and block the small joint’s range of motion due to the pressure effect (7).
Demographically, most cases were reported from the Western Hemisphere and Western Europe (UK, USA, Spain, and France). In contrast, only a few isolated cases were reported from Eastern countries (China, Japan, Korea, and India), as shown in Fig. 12. The lower reported incidence from the Eastern countries could be due to the lower incidence in the region or the possibility of underreporting cases. Further future studies are required to establish the underlying rationale.
Figure 12.
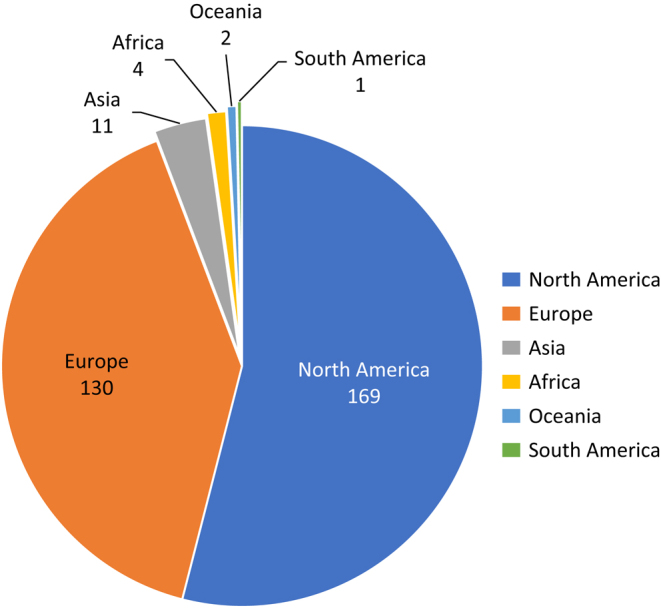
Pie chart summarizing the incidence of superficial acral fibromyxoma based on continents.
Histologically, superficial acral fibromyxoma presented as an unencapsulated tumor with star- or spindle-shaped fibroblasts in broad storiform growth patterns embedded in a myxoid or collagenous matrix. Mast cells and vasculatures are common in variable degrees. Nuclear atypia and mitotic figures are rare and atypical. Immunohistochemically, in the majority of reported cases, the tumor cells showed strong and most consistent immunoreactivity to CD34 and negative for S100, actin, calponin, caldesmon, desmin, cytokeratin, and HMB-45, corresponding to our presenting case. Another less-mentioned protein, vimentin, proved to be of assistive value, as it was positive in all the previous literature when tested. The other proteins (EMA, CD99) were inconsistent (8, 9, 10, 11). Malignant transformation has never been reported in this tumor. There are other differential tumors with myxoid histological appearance or tumors with distal extremity predilection (Tables 1 and 2).
Table 1.
Summarized list of tumors with myxoid histological appearances and their features (Source: WHO Classifications of Tumors 2020 (3)).
| Tumor | Features |
|---|---|
| Neurofibromas | |
| S100 positive | |
| CD34 negative | |
| Superficial angiomyxoma | |
| Predilection for trunk and head and neck region | |
| Inflammatory component usually seen | |
| Positive for CD34 | |
| Negative for S100, SMA, and muscle specific actin | |
| Myxoid dermatofibrosarcoma protuberans (myxoid variant) | |
| Uncommon | |
| With storiform pattern | |
| Positive for CD34 | |
| Negative for EMA | |
| Diagnostic: 17 and 22 translocations with COL1A1–PDGFB fusion gene | |
| Low-grade fibromyxoid sarcoma | |
| Deep-seated tumors | |
| Alternating collagenous and myxoidal areas with rosette formation | |
| CD34 +/− | |
| Digital mucous cyst/mucinous cyst | |
| Ganglion-related lesion | |
| Commonly involving the synovium | |
| Loose, cystic area | |
| Low cellularity | |
| Superficial angiomyxoma | |
| Head and neck region | |
| Distinctive lobulated pattern | |
| Inflammatory cells are seen | |
| Low-grade myxofibrosarcoma | |
| Seen in extremities | |
| Curvilinear capillary pattern with myeloid matrix | |
| Perivascular condensation of tumor cells | |
| Marked nuclear atypia | |
| Variable for CD34 immunoreactivity | |
| EMA – negative |
Table 2.
List of soft tissue tumors with distal extremity predilection and their features (Source: WHO Classifications of Tumors (3)).
| Tumor | Features |
|---|---|
| Sclerosing perineurioma | |
| Cell arranged in onion-skin pattern | |
| CD34 +/−, usually negative | |
| EMA positive | |
| Acquired digital fibrokeratomas | |
| Exophytic, paucicellular, with interwoven thick vertical-oriented collagen bundles | |
| CD34 +/− (not consistent) | |
| EMA – negative | |
| S100 – negative | |
| Periungual fibroma | |
| Multiple in nature | |
| Associated with tuberous sclerosis | |
| Abundant fibrous connective tissue | |
| Vertical-oriented collagen bundles | |
| Acral myxoinflammatory fibroblastic sarcoma | |
| Virocyte or Reed–Sternberg-like cells with hyaline areas | |
| Abundant inflammatory cells | |
| EMA – negative |
Currently, there are no proper diagnostic criteria for this tumor. We proposed a diagnostic feature based on the review and analysis of all 326 cases reported. From the analysis of all previously reported cases, CD34 is not diagnostic or unique to superficial acral fibromyxoma; it requires a combination of clinical, histological, and immunohistochemical features to diagnose. It is crucial to make an accurate diagnosis to plan for the management and prevent overtreatment (amputation) or undertreatment (risk of recurrence).
Diagnostic features
Presentation:
Mass/nodule of acral, palm, or foot in the location.
Radiological investigation:
2. Scalloping of the underlying bone.
3. Low T1 and moderate-to-high T2 signal under MRI.
Histology features
4. Star-/spindle-shaped fibroblasts in a storiform pattern embedded in a myxoid or collagenous matrix.
Immunohistochemical features
Positive – any one
Immunoreactive to vimentin.
Immunoreactive to CD34.
Immunoreactive to CD99.
Negative
4. Immunohistochemically negative for cytokeratin, smooth muscle, skeletal muscle, and melanocyte markers.
In our case, the excision was performed by experienced hand surgeons under optimal conditions, with adequate magnification and bloodless field, as well as gentle handling and excision of the tumor, yet the tumor recurred. Intraoperatively, it was noted that there were multiple sinuses over the bone surface where the tumor was situated (Fig. 13), which was believed to be the reason for the recurrence in our case. Despite extended curettage being performed using bone burr, recurrence occurred. Hence, based on our experience, a wider resection margin must be considered in the presence of bone scalloping. However, in these acral-prone tumors, the availability of bone stock can be a limiting factor; amputation would be the treatment of choice to achieve a clear margin. In the previous literature, out of eight amputations, none discussed the differences in management. For instance, two cases were reported by Varikatt et al. (6) with bone scalloping of the distal phalanx, one subjected to excision and the other to amputation, while the differences in management and the follow-up were not mentioned in the study. Similarly, Luzar et al. (12) reported 1 case of amputation and 13 cases of local excision. Lastly, Fetsche et al. (2) reported that 4 out of 37 patients underwent amputation without further description of management specifics. Overall, the management of superficial acral fibromyxoma still needs to be standardized, though local excision was done for most of the cases in the literature (235 out of 250 patients). Based on the literature review and our experience, marginal excision could be done in these acral-prone benign tumors. However, in the event of bone involvement/bone scalloping, depending on the extent of the tumor, extended excision with a clear bone margin or amputation is advocated for disease clearance.
Figure 13.

Intraoperative picture showing the tumor (curved arrow) and revealing the dorsum of distal phalanx with multiple sinuses (straight arrows).
The recurrence rate in the literature could be underreported due to the inconsistency and inadequacy in the follow-up duration. Based on our literature review, almost a third of the case reports/case series did not comment on follow-up/recurrence (19 out of 51 case reports/case series), 16 reported up to 1-year postoperative period, 9 reported until 2 years, and 4 reported beyond 2 years. For instance, Cogrel et al. (13) reported three cases with different follow-up periods for each subject (9, 12, and 22 months), and the case series of two patients by Kazakov et al. (14) reported on the follow-up specifics in one case but not in the other. Hence, the actual recurrence rate could not be determined. Superficial acral fibromyxoma is a benign, slow-growing tumor that would take longer for the recurrence to occur. Therefore, a more extended follow-up period will be required to exclude early recurrences. In one of the few large case series reported by Fetsch et al. (2), two recurrences were revealed in their study, which occurred at 2 years 10 months and the second case at 10 years of follow-up. Similarly, Hollman et al. (15) reported recurrence occurred at a mean interval of 27 months in 10 patients, where the recurrence period is consistent with our study (at 2 years of follow-up). Hence, it is inevitable that in more than half of the case reports/case series where follow-up for less than 2 years, the recurrence status is considered unknown (38 out of 51 case reports/case series). Based on our literature analysis, all the recurrences reported were after 2 years of follow-up, with a mean of 26.5 months. The earliest recurrence was reported at 20 months post excision by Goo et al. (16), the only case where the recurrence was reported before 2 years of follow-up. Our literature review has covered the most significant number of reported cases. In contrast, the recurrence of the tumor was previously reported to be 10–20%; our analysis revealed an exact recurrence rate of 13% (22/164 of all reported cases) or 16% (22/135) where the analysis was taken from the reported cases follow-up beyond 2 years, including our case. However, the exact recurrence rate of the condition with bone involvement could not be analyzed separately.
Limitation
Analyzing the recurrence rate of superficial acral fibromyxoma with bone involvement remains challenging as it is a rare and uncommon tumor. A future study on the long-term follow-up of the condition with bone involvement is recommended.
Conclusion
In conclusion, we presented and summarized a poorly recognized entity with unique combinations of clinical and histopathological features. Superficial acral fibromyxoma is still uncommon to us. Due to the benign nature of the tumor, it would be commonly missed and ignored by the patient as it rarely disturbs the daily function. However, delayed cases could lead to morbidity and loss of function of the affected joint/bone. In the presence of bone scalloping, a wider margin of resection or amputation will be warranted to avoid recurrence. Hence, this paper aims to introduce and assist in the management of future cases. Moreover, a more extended follow-up review is recommended.
Supplementary Materials
ICMJE Conflict of Interest Statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the case study reported.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Patient perspective
The patient had consented to publish the article without the patient’s identification for academic purposes and to assist in the future management of the uncommon condition. The patient is currently well with full hand function despite the recurrence. The patient is not keen on further surgery as the patient still has the full function of the hand and will consider further surgery later.
Acknowledgements
We are grateful to the NOCERAL at the University of Malaya for providing us with the resources and support we needed to complete this project. We would also like to thank our colleagues at the University of Malaya for their feedback and support throughout the research process.
References
- 1.Altman RD & Tenenbaum J. Hypertrophic osteoarthropathy. In Textbook of Rheumatology, 5th ed., pp. 1514–1520. Eds Kelly WN Harris ED & Ruddy S. Philadelphia: WB Saunders Company, 1997. [Google Scholar]
- 2.Fetsch JF Laskin WB & Miettinen M. Superficial acral fibromyxoma: a clinicopathologic and immunohistochemical analysis of 37 cases of a distinctive soft tissue tumor with a predilection for the fingers and toes. Human Pathology 200132704–714. ( 10.1053/hupa.2001.25903) [DOI] [PubMed] [Google Scholar]
- 3.WHO Classification of Tumours Editorial Board. Soft tissue and bone tumours . WHO classification of tumours series, 5th ed., vol. 3. Lyon,France: International Agency for Research on Cancer; 2020. Available at: https://publications.Iarc.fr/588 [Google Scholar]
- 4.Gupta R Malhotra A Arora S & Bansal V. Superficial acral fibromyxoma: a rare and distinct clinicopathological entity: a case report and review of literature. Human Pathology 20181216–18. ( 10.1016/j.ehpc.2017.12.006) [DOI] [Google Scholar]
- 5.Sarkar M Mahesh DM & Madabhavi I. Digital clubbing. Lung India 201229354–362. ( 10.4103/0970-2113.102824) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Varikatt W Soper J Simmons G Dave C Munk J & Bonar F. Superficial acral fibromyxoma: a report of two cases with radiological findings. Skeletal Radiology 200837499–503. ( 10.1007/s00256-008-0454-3) [DOI] [PubMed] [Google Scholar]
- 7.Quaba O Evans A Al-Nafussi AA & Nassan A. Superficial acral fibromyxoma. British Journal of Plastic Surgery 200558561–564. ( 10.1016/j.bjps.2004.03.006) [DOI] [PubMed] [Google Scholar]
- 8.Raghupathi DS Krishnamurthy J & Kakoti LM. Cytological diagnosis of superficial acral fibromyxoma: a case report. Journal of Cytology 20153239–41. ( 10.4103/0970-9371.155234) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Messeguer F Nagore E Agustí-Mejias A & Traves V. Fibromixoma acral superficial, un tumor periungueal CD34 positivo. Actas Dermo-Sifiliograficas 201210367–69. ( 10.1016/j.ad.2011.03.028) [DOI] [PubMed] [Google Scholar]
- 10.Tardío JC Butrón M & Martín-Fragueiro LM. Superficial acral fibromyxoma: report of 4 cases with CD10 expression and lipomatous component, two previously underrecognized features. American Journal of Dermatopathology 200830431–435. ( 10.1097/DAD.0b013e31817eec0f) [DOI] [PubMed] [Google Scholar]
- 11.André J Theunis A Richert B & de Saint-Aubain N. Superficial acral fibromyxoma: clinical and pathological features. American Journal of Dermatopathology 200426472–474. ( 10.1097/00000372-200412000-00005) [DOI] [PubMed] [Google Scholar]
- 12.Luzar B & Calonje E. Superficial acral fibromyxoma: clinicopathological study of 14 cases with emphasis on a cellular variant. Histopathology 200954375–377. ( 10.1111/j.1365-2559.2008.03209.x) [DOI] [PubMed] [Google Scholar]
- 13.Cogrel O Stanislas S Coindre JM Guillot P Beylot-Barry M Doutre MS & Vergier B. Superficial acral fibromyxoma: three cases. Annales de Dermatologie et de Venereologie 2010137789–793. ( 10.1016/j.annder.2010.08.003) [DOI] [PubMed] [Google Scholar]
- 14.Kazakov DV Mentzel T Burg G & Kempf W. Superficial acral fibromyxoma: report of two cases. Dermatology 2002205285–288. ( 10.1159/000065853) [DOI] [PubMed] [Google Scholar]
- 15.Hollmann TJ Bovée JV & Fletcher CD. Digital fibromyxoma (superficial acral fibromyxoma): a detailed characterization of 124 cases. American Journal of Surgical Pathology 201236789–798. ( 10.1097/PAS.0b013e31824a0b83) [DOI] [PubMed] [Google Scholar]
- 16.Goo J Jung YJ Kim JH Lee SY & Ahn SK. A case of recurrent superficial acral fibromyxoma. Annals of Dermatology 201022110–113. ( 10.5021/ad.2010.22.1.110) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



 This work is licensed under a
This work is licensed under a