Abstract
By comparing smooth wild-type Brucella spp. to their rough mutants, we show that the LPS O chain restricted the activation of the ERK1/2 and p38 mitogen-activated protein kinase (MAPK) pathways, thus preventing the synthesis of immune mediators that regulate host defense. We conclude that the MAPKs are a target for immune intervention by virulent smooth Brucella.
Brucella spp. are major veterinary pathogens that can cause serious human disease. The strains which are pathogenic for humans (Brucella abortus, Brucella suis, and Brucella melitensis) carry a smooth lipopolysaccharide (LPS) involved in the virulence of the bacteria. The mutants which derive from these strains and express a rough phenotype are attenuated in animals or isolated macrophages compared to the parental Brucella (1, 9, 11, 16, 31, 38, 39, 48), suggesting that they can be used as live vaccine strains. The properties of the LPS O chain, a linear homopolymer of α1,2-linked perosamine (5), explain this attenuation. The LPS O chain protects the bacteria from cellular cationic peptides (13, 30), oxygen metabolites (45), and complement-mediated lysis (10, 27), is a key molecule for Brucella invasion and development (36), and impairs the apoptotic or necrotic signals directed against the infected cells (11, 35). Recently, we showed that immune molecules that elicit macrophage defense are produced at higher levels in rough Brucella-infected macrophages than in smooth Brucella-infected macrophages (26, 40). Production of immune molecules depends on intracellular signaling pathways that connect receptor-mediated events to transcriptional response within the nucleus. One important group of signaling pathways, the mitogen-activating protein kinase (MAPK) signaling cascade, is implicated in bacterial pathogenesis as demonstrated by the induction or inhibition of ERK1/2 and p38 MAPKs during infection with Salmonella enterica serovar Typhimurium (21), Yersinia spp. (34, 42), Listeria monocytogenes (46, 47), and Mycobacterium spp. (43). Therefore, the discrepancies in the virulence of smooth and rough Brucella could be linked to the MAPK pathways triggered by these bacteria. We thus analyzed these pathways and their possible relationship with the divergent responses of macrophages infected with smooth or rough Brucella. The results obtained with intact live Brucella greatly suggest that because of their relationship with the LPS O chain, the MAPKs are a target for immune intercession by virulent smooth Brucella.
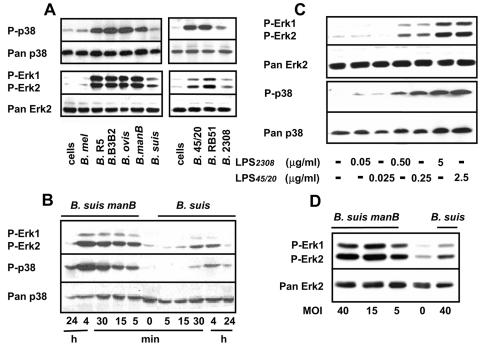
Table 1 shows the Brucella strains used in the study. As mentioned in previous reports (1, 14, 26, 36), all of the rough Brucella assessed displayed a great attenuation in mouse or isolated macrophages compared to smooth Brucella. To analyze the activation of p38 and ERK1/2 kinases during infection, J774.A1 cells (106/well) were incubated with the different Brucella strains (multiplicity of infection [MOI] = 40) at 37°C. They were then rinsed twice with phosphate-buffered saline (PBS) and lysed in 150 μl of buffer containing 50 mM HEPES (pH 7.4), 150 mM NaCl, 10 mM NaF, 10 mM iodoacetamide, 1% NP-40, 1 mM Na2VO3, and 1 μg/ml of each protease inhibitor (leupeptin, apoprotein, and chymostatin) and centrifuged. The cytosolic fraction denatured by the addition of reducing buffer and boiling was analyzed by Western blotting with anti-phospho-p38 MAPK and anti-phospho-ERK 1/2 (Cell Signaling Technology, Beverly, MA), which recognize the phosphorylated (i.e., activated) form of the MAPKs (28, 29). Pan p38 (anti-p38MAPK) (Cell Signaling) and pan ERK2 (anti-ERK2) (Santa Cruz Biotechnology, Inc., CA), which detect both active and inactive forms of kinases, were applied on stripped blots to verify that equivalent amounts of proteins were loaded per lane (28, 29). Figure 1A shows that at 30 min postinfection (p.i.), the activation process triggered by the rough Brucella resulted in a potent phosphorylation of the p38 and ERK1/2 MAP kinases. Infections with smooth Brucella induced a markedly weaker (or no visible) stimulation of these kinases, with B. suis and B. abortus 2308 demonstrating a slightly higher capacity of activation than B. melitensis, a difference which could be due to the genetic background of the different bacteria. Figure 1B shows that B. suis manB-induced phosphorylation of ERK1/2 and p38 MAPKs occurred within 5 min of infection and increased until at least 4 h p.i. This was true for the other rough Brucella, demonstrating that the activation resulted from a long active process which involved the attachment, ingestion, and early death of the bacteria, as shown with macrophages infected with virulent mycobacteria (41). The weak phosphorylation triggered by B. suis, which was visible at 30 min p.i., increased modestly but always remained at a much lower level than the phosphorylation induced by B. suis manB. Therefore, the slight activation observed at 30 min p.i. was not due to a delayed kinetic of activation but reflected the poor capacity of activation of the bacteria. In Salmonella, the LPS O chain is crucial for the signaling triggered by the direct interaction between the bacterial LPS and macrophages (32). Furthermore, the LPS lipid As of smooth and rough B. abortus are structurally different (4). There was no significant difference in ERK1/2 and p38 MAPK activation elicited by the LPS from virulent smooth B. abortus 2308 or rough vaccine strain B. abortus 45/20 (Fig. 1C). Moreover, when added at 100 ng in the assays, the LPS from B. abortus 2308 did not modify the ERK1/2 and p38 MAPK activation induced by B. abortus 45/20 or B. suis manB (MOI = 40) (data not shown). Therefore, neither a direct effect of the O chain on macrophages, nor the sole structural change of the lipid A explain the potent ability of intact rough Brucella to activate MAPKs compared to smooth Brucella. Owing to the absence of the O chain, the MAPK activation could be due to increased numbers of lipid A molecules exposed at the surface of the bacteria. However, the amount of LPS carried by 4 × 107 rough Brucella, which corresponds to a MOI of 40 and is theoretically lower than 50 ng LPS (33), promoted no perceptible activation of MAPKs (Fig. 1C) and therefore eliminated such a possibility. Finally, in accordance with its poor endotoxic potential (17, 23), the LPS appears to be a minor actor of MAPK activation by intact rough Brucella. This result appears to coincide with recent reports claiming that TLR2 but not TLR4 are involved in macrophage stimulation by heat-killed Brucella (15, 22). Phagocytes express a variety of receptors that participate in Brucella recognition and internalization (3). Because of the exposition of ligands normally hidden by the O chain in smooth Brucella at the surface of the bacteria, the rough mutants bind to macrophages and penetrate into these cells to a much higher extent than the parental smooth Brucella (9, 31, 36, 40). The rough Brucella-elicited activation could result from a saturation of the macrophage receptors engaged by these different ligands. However, the MAPK activation triggered by B. ovis REO198 eliminated this possibility. B. ovis REO198 binds to and penetrate macrophages or J774A.1 cells to a similar extent as smooth Brucella (reference 14 and data not shown), but it activated the MAPKs at a level similar to those of other rough Brucella spp. (Fig. 1). It is thus likely that only few favored receptors elicited MAPK activation during infection with rough Brucella. This possibility agrees with the data in Fig. 1D, which compare the activation of ERK1/2 triggered by B. suis and B. suis manB when the rough mutant MOI decreased from 40 to 5. Under these conditions, which tended to equalize the uptake of B. suis (18,500 ± 5,210 CFU/106 cells for a MOI of 40) and B. suis manB (25,430 ± 7,840 CFU/106 cells for a MOI of 5), the discrepancy in ERK1/2 activation was still observed.
TABLE 1.
Brucella strains used in the studya
| Strain | Genotypic and/or phenotypic description | CFU/spleen at 3 wk p.i.b | DI for J774A.1 cellsc |
|---|---|---|---|
| B. melitensis 16M | Spontaneous smooth nalidixic acid-resistant mutant of B. melitensis 16M (49) | >104 | 50-200 |
| B. melitensis R5 | Natural rough mutant of B. melitensis 16M (CITA collection, Zaragoza, Spain) | <10 | <0.002 |
| B. melitensis B3B2 | Rough mini-Tn5 insertion mutant of B. melitensis 16M invalidated on the perosamine synthase gene, kanamycin resistant (16) | <10 | <0.01 |
| B. suis 1330 | Smooth wild-type B. suis (ATCC 23444) | >5 × 105 | 100-500 |
| B. suis manB | Rough mini-Tn5 insertion mutant of B. suis 1330 invalidated on phosphomannose gene, kanamycin resistant (12) | <10 | <0.02 |
| B. ovis REO198 | Natural rough strain, CO2-independent B. ovis. Laboratory collection, CITA, Zaragoza, Spain | <10 | <0.02 |
| B. abortus 2308 | Smooth wild-type B. abortus. Laboratory collection, CITA, Zaragoza, Spain | >106 | 50-200 |
| B. abortus RB51 | Vaccine strain. Rough mutant of B. abortus 2308, rifampin resistant. G. G. Schurig, Virginia (44) | <10 | <0.1 |
| B. abortus 45/20 | Vaccine strain. Rough mutant of B. abortus 2308. Laboratory collection, CITA, Zaragoza, Spain | ND | <0.1 |
The smooth and rough phenotype of the different Brucella strains was assessed by crystal violet staining and verified by immunoblotting techniques involving monoclonal antibodies which recognize the smooth LPS or rough LPS of Brucella (8). ND, not done.
BALB/c mice were injected intraperitoneally with 5 × 104 CFU of one of the following bacteria: B. suis 1330, B. suis manB, B. melitensis 16M, B. melitensis B3B2, B. melitensis R5, B. ovis Reo 198, B. abortus 2308, and B. abortus RB51. Six mice per group were killed by CO2 asphyxiation 3 weeks postinoculation. Spleens were aseptically removed and homogenized with 10 ml of PBS for determining Brucella counts (CFU/spleen) as indicated in references 24 and 25.
J774A.1 cells were infected with the different strains of Brucella (MOI = 40) as indicated in the table. The number of intracellular bacteria was then measured at 90 min p.i. and 48 h p.i. The development index [DI = (CFU48 h/well)/(CFU90 h/well)] was then calculated for each bacterium at 48 h p.i. (6). Each infection was performed at least three times.
FIG. 1.
Activation of ERK1/2 and p38 MAPKs in J774A.1 cells treated with different Brucella strains or with Brucella LPSs. ERK1/2 and p38 MAPKs were determined by Western immunoblotting of J774A.1 cells treated (A) for 30 min with different strains of smooth or rough Brucella (MOI = 40), (B) for different periods of time with B. suis manB or B. suis (MOI = 40), or (C) for 30 min with different concentrations of purified LPSs from smooth B. abortus 2308 (0.050 μg/ml to 5 μg/ml) or rough B. abortus 45/20 (0.025 μg/ml to 2.5 μg/ml). The LPSs were obtained from I. Moriyón (University of Navarra, Pamplona, Spain). They were carefully solubilized by sonication. Their purification and properties have been reported elsewhere (2, 14). The effect of the smooth LPS was assessed at concentrations double those for the rough LPS to compare the lipid A of both LPSs (I. Moriyón, personal communication) (D) or for 30 min with B. suis manB (MOI = 40, 15, and 5) or B. suis (MOI = 40); 2 × 106 J774A.1 cells were cultured at 37°C for the indicated periods of time in 150 μl of RPMI 1640 alone (cells) or supplemented with B. suis, B. melitensis 16 M (B. mel), B. abortus 2308 (B. 2308), B. ovis REO198 (B. ovis), B. suis manB (B. manB), B. melitensis R5 (B. R5), B. melitensis B3B2 (B. B3B2), B. abortus RB51 (B. RB51) or B. abortus 45/20 (B. 45/20), or with different concentrations of the purified LPS from B. abortus 2308 or B. abortus 45/20. They were then rinsed, lysed, and after sodium dodecyl sulfate-10% acrylamide gel electrophoresis and transfer to nitrocellulose membrane, analyzed with phosphospecific antibodies against ERK1/2 or p38 active kinases. The blots were stripped and reprobed with pan antibodies (A and C). In panel B, the same blot was sequentially analyzed for phospho-ERK1/2, phospho-p38, and pan p38 MAPKs. Results are representative of three separate experiments which gave identical results.
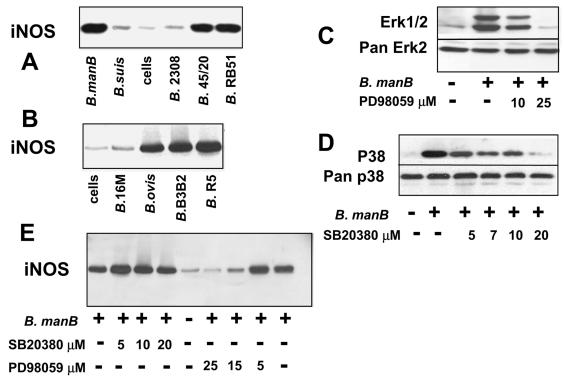
J774A.1 cells infected with rough Brucella synthesize nitric oxide (NO) (26), a deleterious radical that controls the intracellular development of Brucella at the onset of infection (19, 50, 51). NO is not produced in smooth Brucella-invaded cells, and the purified LPS of B. abortus 2308 (100 ng) did not impair the production of NO elicited by rough Brucella (data not shown). The expression of the inducible nitric oxide synthase (iNOS) explains these data, with iNOS being induced only in rough Brucella-infected cells (Fig. 2A). In phagocytes, the transcription of the nos2 gene can be triggered by p38 and/or ERK1/2 MAPK pathways (7). Therefore, iNOS could constitute a link between the MAPK responses induced by rough and smooth Brucella and the relative capacity of invasiveness of these bacteria. To determine whether ERK1/2 and p38 MAPKs were involved in iNOS induction, iNOS in cells infected with B. suis manB in the presence or absence of specific pharmacological inhibitors of these kinases was measured. SB203580 (which inhibits p38MAPK activation) and PD98059 (which represses activation of MEK-1, the kinase upstream of ERK-1/2) (28, 29), respectively, impaired the B. suis manB-triggered phosphorylation of p38 and ERK1/2 MAPKs in a dose-dependent manner (Fig. 2B and C), with a complete inhibition at 25 μM for PD98059 and 20 μM for SB203580. In parallel, PD98059 impaired the induction of iNOS, while SB20380 consistently had no effect on the expression of this enzyme (Fig. 2E), a result confirmed by the effect of the inhibitors on NO release (data not shown). It demonstrated that only the ERK1/2 MAPK pathway was meaningful for iNOS induction and that the weak activation of the ERK1/2 MAPK induced by smooth Brucella was not sufficient to induce iNOS expression (Fig. 2A). This explains why in macrophages invaded by these bacteria the expression of iNOS requires an additional signal elicited, for instance, by exogenous gamma interferon (19, 50). The rough Brucella were capable of bypassing this signal, perhaps because they potently activated the ERK1/2 MAPK pathway, these kinases being one possible branch of gamma interferon signaling (37). However, other unidentified pathways, not related to p38 MAPK, could also participate in iNOS induction.
FIG. 2.
(A and B) Analysis of iNOS expression in J774A.1 cells infected with different Brucella strains. J774A.1 cells (106) in 100 μl of RPMI 1640 were infected for 30 min at 37°C with the different Brucella strains analyzed in Fig. 1 (MOI = 40) or not infected (cells). They were then extensively washed and cultured in gentamicin-supplemented RPMI 1640-10% FCS. At 24 h p.i., they were lysed and analyzed by Western immunoblotting, with a mouse anti-iNOS serum (Alexis Corp., San Diego, Calif.) as previously described (19). (C and D) Inhibition of ERK1/2 and p38 MAPK activation elicited by B. suis manB. J774A.1 cells were pretreated for 30 min with the indicated concentrations of PD98059 or SB20380 in RPMI 1640 at 37°C. They were then infected (or not) for 30 min with B. suis manB (MOI = 40) in the presence of the MAPK inhibitor applied during the pretreatment. They were lysed and analyzed by Western immunoblotting as mentioned in Fig. 1, with phosphospecific antibodies against ERK1/2 or p38 active kinase. The stripped blots were then reprobed with pan antibodies. (E) Effect of PD98059 and SB20380 on iNOS expression in J774A.1 cells infected with B. suis manB. J774A.1 cells were pretreated (or not) for 30 min with the indicated concentrations of PD98059 or SB20380 in RPMI 1640 at 37°C. They were then infected for 30 min with B. suis manB in the presence of the MAPK inhibitor applied during the pretreatment, cultured for a further 4 h in RPMI 1640-10% FCS supplemented with 30 μg/ml gentamicin in the presence of PD98059 or SB20380. The MAPK inhibitors were then removed by washing, and the infected cells were cultured again in the gentamicin-supplemented medium. At 24 h p.i., the expression of iNOS was analyzed by Western immunoblotting as in panels A and B. Each experiment was performed at least three times. The MAPK inhibitors were dissolved in dimethyl sulfoxide (DMSO) so that the DMSO dilution was always lower than 0.1% in assays. At this dilution, the DMSO affected neither MAPKs nor iNOS induction. B. manB, B. suis manB; B. 2308, B. abortus 2308; B. 45/20, B. abortus 45/20; B. RB51, B. abortus RB51; B. 16M, B. melitensis 16 M; B. ovis, B. ovis REO198; B. B3B2, B. melitensis B3B2; B. R5, B. melitensis R5.
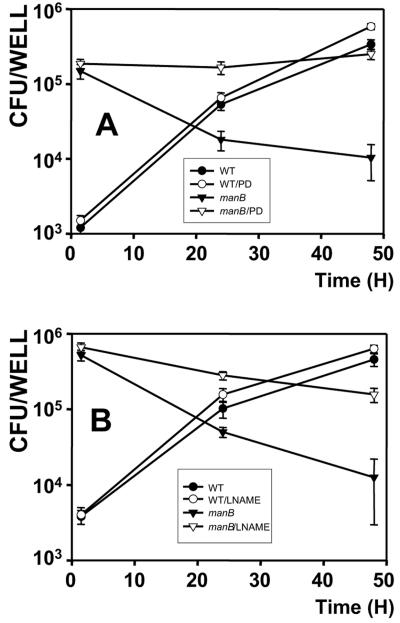
To verify whether the ERK1/2 MAPK activation pathway influences the intracellular outcome of Brucella, we tested the influence of PD98059 on macrophage infection. Assays were performed with 24-well plates (Falcon; Becton Dickinson, Meylan, France). J774A.1 cells in RPMI 1640-10% fetal calf serum (FCS) (106 cells ml−1 per well) were pretreated with PD98059 at 25 μM for 30 min prior to infection; they were then incubated for 30 min at 37°C with a suspension of B suis manB or B. suis (MOI = 40) in the presence of the drug. After washing three times with PBS to remove extracellular bacteria, the infected macrophages were reincubated with PD98059 for an additional 4 h in RPMI-10% FCS supplemented with 30 μg/ml gentamicin before the drug was washed and the cells were cultured in the same medium. In these conditions, PD98059 did not induce any toxicity as determined by microscopic observations and trypan blue exclusion (41 and data not shown). At several times p.i., the cells were washed twice and the number of viable intracellular bacteria was determined after cell lysis in 0.1% Triton X-100 (18). As with HeLa cells infected with Brucella (20), PD98059 had no effect on the phagocytosis of B. suis manB (P > 0.3) (or B. suis, P > 0.4). However, in macrophages, it significantly reversed the elimination of intracellular B. suis manB which occurred in the absence of drug (Fig. 3A) (26, 36) (P < 0.005 at 48 h). This indicated that the ERK1/2 MAPK pathway triggered by B. suis manB, which had no influence on the entrance of the bacteria, was determinant for its future. Blocking the ERK1/2 signaling pathway was beneficial to the bacteria, which meant that its activation favored the elimination of the B. suis manB once they were phagocytosed. These results paralleled those observed with infection performed in the presence or absence of L-NAME (N-ω-nitro-l-arginine methyl ester), a specific inhibitor of iNOS (Fig. 3B). Altogether, the data showed that the B. suis manB-induced ERK1/2 MAPK pathway regulated the killing of bacteria and that it could be through the induction of iNOS. This possibility was in accordance with the results observed during the infection of J774A1 cells with B. suis: when iNOS was not induced, PD98059 (or L-NAME) did not significantly modify the bacterial invasiveness (Fig. 3) (19) (P > 0.5 or P > 0.2 at 48 h compared to B. suis alone). Therefore, the B. suis manB-triggered ERK1/2 MAPK activation armed the host cells with a NO-generating system. The capacity of defense of the cells against the bacteria was thus reinforced by a microbicidal weapon which was missing during infections with smooth wild-type B. suis. Regarding the data of Fig. 1 and 2, the ERK1/2 MAPK activation and its consequence on iNOS induction appeared to be a general property of the rough Brucella spp. which participate in the clearance of the bacteria during an active infection. In addition, when it is produced in large amounts, NO is deleterious to cells. Therefore, in certain conditions of infections, the rough Brucella-elicited activation could favor the death of the host cells and thus negatively affect the apparent development of the bacteria. This could be the case in infections performed at elevated MOIs (35) or in the absence of serum (11). In any case, by indirectly preventing the ERK1/2 MAPK activation, the LPS O chain impaired NO formation and thus favored the intramacrophagic development of smooth Brucella.
FIG. 3.
Intracellular behavior of B. suis manB or B. suis within J774A.1 cells treated with PD98059 (A) or L-NAME (B). (A) J774A.1 cells pretreated for 30 min with 25 μM PD98059 (▿, ○) or not treated (▾, •) were infected with B. suis manB (▾, ▿) or B. suis (•, ○) as described in the text. They were then washed and cultured for a further 4 h in gentamicin-supplemented RPMI 1640-10% FCS in the presence 25 μM PD98059 (▿, ○) or not (▾, •). The MAPK inhibitor was then removed by washing, the infected cells being cultured in the gentamicin-supplemented medium. At different times p.i., the intracellular number of bacteria was measured as described in reference 26. (B) J774A.1 cells were infected with B. suis manB (▾, ▿) or B. suis (•, ○) (MOI = 40). Thirty minutes after the onset of the infection, they were cultured in gentamicin-supplemented RPMI 1640-10% FCS in the presence (▿, ○) or absence of 3 mM L-NAME (▾, •). At different times, the intracellular number of bacteria was measured as described in reference 26. Infections were performed in triplicate. Results were expressed as CFU/well ± standard deviation. DMSO used to dissolve PD98059 did not affect the infection of J774A.1 cells with Brucella, a dilution of 0.1% having been applied in the assays. Both experiments were repeated at least four times, giving similar results. Where indicated in the text, CFU values relative to different assays at one time p.i. were compared by using the Student t test.
We evaluated the effect of MAPK activation on the intracellular development of Brucella by analyzing the infected macrophages for the induction of iNOS. This particular protein was chosen because it is known that NO was involved in the elimination of Brucella in the first 48 h p.i. (19, 50). However, it is evident that other pathways are involved in the elimination of intracellular rough Brucella (see introduction). Inflammatory cytokines and chemokines (interleukin-1, tumor necrosis factor alpha, MIP-1α and others), for instance, participate in the clearance of Brucella (26, 40). In numerous situations, the production of these mediators depends on the activation of the p38 and ERK1/2 MAPKs alone or in coordination (7). Therefore, our results, which indicated that the p38 and ERK1/2 MAP kinases were strongly activated upon infection of mouse macrophages with rough Brucella, but not upon infection with smooth Brucella, defined the MAPKs as critical signaling molecules in the reactions of macrophages to Brucella. Although the LPS O chain has no direct action on the MAPK pathway, it interferes with this pathway by regulating the interaction between bacteria and host cells during uptake of Brucella. The resulting interference appears instrumental in determining the eventual fate of the bacteria. The slight MAPK activation associated with virulent smooth Brucella infections suggests a novel point of immune intervention by Brucella.
Acknowledgments
This work was supported by grants from INSERM, from the European Community (QLK2-1999-0014), and from INIA, Spain (SC98-047). We are grateful to the Region Languedoc-Roussillon and Aragón (CTP FDG/CS68 for INSERM and CTPMO1/2002 for Aragón) and to Ministerio de Educación Cultura y Deporte (Programa de Estancias de Investigadores en el Extranjero, PR2001-0053) and INSERM (Poste Vert) for exchange grants to María P. Jiménez de Bagüés.
We thank A. Cloeckaert from INRA, France, for providing the LPS monoclonal antibodies and I. Moriyón from Universidad de Navarra and E. Moreno from Universidad National Costa Rica for providing the LPS. We thank Morjaria Sejal for correcting and improving our English.
Editor: D. L. Burns
REFERENCES
- 1.Allen, C. A., L. G. Adams, and T. A. Ficht. 1998. Transposon-derived Brucella abortus rough mutants are attenuated and exhibit reduced intracellular survival. Infect. Immun. 66:1008-1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aragon, V., R. Diaz, E. Moreno, and I. Moriyón. 1996. Characterization of Brucella abortus and Brucella melitensis native haptens as outer membrane O-type polysaccharides independent from the smooth lipopolysaccharide. J. Bacteriol. 178:1070-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campbell, G. A., L. G. Adams, and B. A. Sowa. 1994. Mechanisms of binding of Brucella abortus to mononuclear phagocytes from cows naturally resistant or susceptible to brucellosis. Vet. Immunol. Immunopathol. 41:295-306. [DOI] [PubMed] [Google Scholar]
- 4.Campos, M. A., G. M. Rosinha, I. C. Almeida, X. S. Salgueiro, B. W. Jarvis, G. A. Splitter, N. Qureshi, O. Bruna-Romero, R. T. Gazzinelli, and S. C. Oliveira. 2004. Role of Toll-like receptor 4 in induction of cell-mediated immunity and resistance to Brucella abortus infection in mice. Infect. Immun. 72:176-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caroff, M., D. R. Bundle, and M. B. Perry. 1984. Structure of the O-chain of the phenol-phase soluble cellular lipopolysaccharide of Yersinia enterocolitica serotype O:9. Eur. J. Biochem. 139:195-200. [DOI] [PubMed] [Google Scholar]
- 6.Caron, E., T. Peyrard, S. Köhler, S. Cabane, J. P. Liautard, and J. Dornand. 1994. Live Brucella spp. fail to induce TNF-α excretion in U-937-derived phagocytes. Infect. Immun. 62:5267-5274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang, L., and M. Karin. 2001. Mammalian MAP kinase signalling cascades. Nature 410:37-40. [DOI] [PubMed] [Google Scholar]
- 8.Cloeckaert, A., P. de Wergifosse, G. Dubray, and J. N. Limet. 1990. Identification of seven surface-exposed Brucella outer membrane proteins by use of monoclonal antibodies: immunogold labeling for electron microscopy and enzyme-linked immunosorbent assay. Infect. Immun. 58:3980-3987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Detilleux, P. G., B. L. Deyoe, and N. F. Cheville. 1990. Penetration and intracellular growth of Brucella abortus in nonphagocytic cells in vitro. Infect. Immun. 58:2320-2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernandez-Prada, C. M., M. Nikolich, R. Vemulapalli, N. Sriranganathan, S. M. Boyle, G. G. Schurig, T. L. Hadfield, and D. L. Hoover. 2001. Deletion of wboA enhances activation of the lectin pathway of complement in Brucella abortus and Brucella melitensis. Infect. Immun. 69:4407-4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez-Prada, C. M., E. B. Zelazowska, M. Nikolich, T. L. Hadfield, R. M. Roop II, G. L. Robertson, and D. L. Hoover. 2003. Interactions between Brucella melitensis and human phagocytes: bacterial surface O-polysaccharide inhibits phagocytosis, bacterial killing, and subsequent host cell apoptosis. Infect. Immun. 71:2110-2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foulongne, V., G. Bourg, C. Cazevieille, S. Michaux-Charachon, and D. O'Callaghan. 2000. Identification of Brucella suis genes affecting intracellular survival in an in vitro human macrophage infection model by signature-tagged transposon mutagenesis. Infect. Immun. 68:1297-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freer, E., E. Moreno, I. Moriyón, J. Pizarro-Cerdá, A. Weintraub, and J. P. Gorvel. 1996. Brucella-Salmonella lipopolysaccharide chimeras are less permeable to hydrophobic probes and more sensitive to cationic peptides and EDTA than are their native Brucella sp. counterparts. J. Bacteriol. 178:5867-5876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freer, E., J. Pizarro-Cerdá, A. Weintraub, J.-A. Bengoechea, I. Moriyón, K. Hultenby, J.-P. Gorvel, and E. Moreno. 1999. The outer membrane of Brucella ovis shows increased permeability to hydrophobic probes and is more susceptible to cationic peptides than are the outer membranes of mutant rough Brucella abortus strains. Infect. Immun. 67:6181-6186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giambartolomei, G. H., A. Zwerdling, J. Cassataro, L. Bruno, C. A. Fossati, and M. T. Philipp. 2004. Lipoproteins, not lipopolysaccharide, are the key mediators of the proinflammatory response elicited by heat-killed Brucella abortus. J. Immunol. 173:4635-4642. [DOI] [PubMed] [Google Scholar]
- 16.Godefroid, F., B. Taminiau, I. Danese, P. Denoel, A. Tibor, V. Weynants, A. Cloeckaert, J. Godefroid, and J. J. Letesson. 1998. Identification of the perosamine synthetase gene of Brucella melitensis 16M and involvement of lipopolysaccharide O side chain in Brucella survival in mice and in macrophages. Infect. Immun. 66:5485-5493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldstein, J., T. Foffman, C. Frasch, E. F. Lizzio, P. Beining, D. Hochstein, Y. L. Lee, R. D. Angus, and B. Golding. 1992. Lipopolysaccharide (LPS) from Brucella abortus is less toxic than that from Escherichia coli, suggesting the possible use of B. abortus or LPS from B. abortus as a carrier in vaccines. Infect. Immun. 60:1385-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gross, A., S. Bertholet, J. Mauel, and J. Dornand. 2004. Impairment of Brucella growth in human macrophagic cells that produce nitric oxide. Microb. Pathog. 36:75-82. [DOI] [PubMed] [Google Scholar]
- 19.Gross, A., S. Speisser, A. Terraza, B. Rouot, E. Caron, and J. Dornand. 1998. Expression and bactericidal activity of nitric oxide synthase in Brucella suis-infected murine macrophages. Infect. Immun. 66:1309-1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guzman-Verri, C., E. Chaves-Olarte, C. von Eichel-Streiber, I. Lopez-Goni, M. Thelestam, S. Arvidson, J. P. Gorvel, and E. Moreno. 2001. GTPases of the Rho subfamily are required for Brucella abortus internalization in nonprofessional phagocytes: direct activation of Cdc42. J. Biol. Chem. 276:44435-44443. [DOI] [PubMed] [Google Scholar]
- 21.Hobbie, S., L. M. Chen, R. J. Davis, and J. E. Galan. 1997. Involvement of mitogen-activated protein kinase pathways in the nuclear responses and cytokine production induced by Salmonella typhimurium in cultured intestinal epithelial cells. J. Immunol. 159:5550-5559. [PubMed] [Google Scholar]
- 22.Huang, L. Y., J. Aliberti, C. A. Leifer, D. M. Segal, A. Sher, D. T. Golenbock, and B. Golding. 2003. Heat-killed Brucella abortus induces TNF and IL-12p40 by distinct MyD88-dependent pathways: TNF, unlike IL-12p40 secretion, is Toll-like receptor 2 dependent. J. Immunol. 171:1441-1446. [DOI] [PubMed] [Google Scholar]
- 23.Jarvis, B. W., T. H. Harris, N. Qureshi, and G. A. Splitter. 2002. Rough lipopolysaccharide from Brucella abortus and Escherichia coli differentially activates the same mitogen-activated protein kinase signaling pathways for tumor necrosis factor alpha in RAW 264.7 macrophage-like cells. Infect. Immun. 70:7165-7168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiménez de Bagüés, M. P., M. Barberan, C. M. Marin, and J. M. Blasco. 1995. The Brucella abortus RB51 vaccine does not confer protection against Brucella ovis in rams. Vaccine 13:301-304. [DOI] [PubMed] [Google Scholar]
- 25.Jiménez de Bagüés, M. P., P. H. Elzer, J. M. Blasco, C. M. Marin, C. Gamazo, and A. J. Winter. 1994. Protective immunity to Brucella ovis in BALB/c mice following recovery from primary infection or immunization with subcellular vaccines. Infect. Immun. 62:632-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiménez de Bagüés, M. P., A. Terraza, A. Gross, and J. Dornand. 2004. Different responses of macrophages to smooth and rough Brucella spp.: relationship to virulence. Infect. Immun. 72:2429-2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joiner, K. A. 1985. Studies on the mechanism of bacterial resistance to complement-mediated killing and on the mechanism of action of bactericidal antibody. Curr. Top. Microbiol. Immunol. 121:99-133. [DOI] [PubMed] [Google Scholar]
- 28.Lafont, V., J. Liautard, M. Sable-Teychene, Y. Sainte-Marie, and J. Favero. 2001. Isopentenyl pyrophosphate, a mycobacterial non-peptidic antigen, triggers delayed and highly sustained signaling in human γδ T lymphocytes without inducing down-modulation of T cell antigen receptor. J. Biol. Chem. 276:15961-15967. [DOI] [PubMed] [Google Scholar]
- 29.Lafont, V., F. Ottones, J. Liautard, and J. Favero. 1999. Evidence for a p21ras/Raf-1/MEK-1/ERK-2-independent pathway in stimulation of IL-2 gene transcription in human primary T lymphocytes. J. Biol. Chem. 274:25743-25748. [DOI] [PubMed] [Google Scholar]
- 30.Martínez de Tejada, G., J. Pizarro-Cerdá, E. Moreno, and I. Moriyón. 1995. The outer membranes of Brucella spp. are resistant to bactericidal cationic peptides. Infect. Immun. 63:3054-3061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McQuiston, J. R., R. Vemulapalli, T. J. Inzana, G. G. Schurig, N. Srianganathan, D. Fritzinger, T. L. Hadfield, R. A. Warren, N. Snellings, D. Hoover, S. M. Halling, and S. M. Boyle. 1999. Genetic characterization of a Tn5-disrupted glycosyltransferase gene homolog in Brucella abortus and its effect on lipopolysaccharide composition and virulence. Infect. Immun. 67:3830-3835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muroi, M., and K. Tanamoto. 2002. The polysaccharide portion plays an indispensable role in Salmonella lipopolysaccharide-induced activation of NF-κB through human toll-like receptor 4. Infect. Immun. 70:6043-6047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neidhardt, F. C., J. L. Ingraham, and M. Schaechter. 1990. Physiology of the bacterial cell, p. 4. Sinauer Associates, Inc., Sunderland, Mass.
- 34.Palmer, L. E., S. Hobbie, J. E. Galan, and J. B. Bliska. 1998. YopJ of Yersinia pseudotuberculosis is required for the inhibition of macrophage TNF-α production and downregulation of the MAP kinases p38 and JNK. Mol. Microbiol. 27:953-965. [DOI] [PubMed] [Google Scholar]
- 35.Pei, J., and T. A. Ficht. 2004. Brucella abortus rough mutants are cytopathic for macrophages in culture. Infect. Immun. 72:440-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Porte, F., A. Naroeni, S. Ouahrani-Bettache, and J. P. Liautard. 2003. Role of the Brucella suis lipopolysaccharide O antigen in phagosomal genesis and in inhibition of phagosome-lysosome fusion in murine macrophages. Infect. Immun. 71:1481-1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ramana, C. V., M. P. Gil, R. D. Schreiber, and G. R. Stark. 2002. Stat1-dependent and -independent pathways in IFN-γ-dependent signaling. Trends Immunol. 23:96-101. [DOI] [PubMed] [Google Scholar]
- 38.Riley, L. K., and D. C. Robertson. 1984. Brucellacidal activity of human and bovine polymorphonuclear leukocyte granule extracts against smooth and rough strains of Brucella abortus. Infect. Immun. 46:231-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rittig, M. G., M.-T. Alvarez-Martinez, F. Porte, J.-P. Liautard, and B. Rouot. 2001. Intracellular survival of Brucella spp. in human monocytes involves conventional uptake but special phagosomes. Infect. Immun. 69:3995-4006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rittig, M. G., A. Kaufmann, A. Robins, B. Shaw, H. Sprenger, D. Gemsa, V. Foulongne, B. Rouot, and J. Dornand. 2003. Smooth and rough lipopolysaccharide phenotypes of Brucella induce different intracellular trafficking and cytokine/chemokine release in human monocytes. J. Leukoc. Biol. 74:1045-1055. [DOI] [PubMed] [Google Scholar]
- 41.Roach, S. K., and J. S. Schorey. 2002. Differential regulation of the mitogen-activated protein kinases by pathogenic and nonpathogenic mycobacteria. Infect. Immun. 70:3040-3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ruckdeschel, K., S. Harb, A. Roggenkamp, M. Hornef, R. Zumbihl, S. Kohler, J. Heesemann, and B. Rouot. 1998. Yersinia enterocolitica impairs activation of transcription factor NF-κB: involvement in the induction of programmed cell death and in the suppression of the macrophage tumor necrosis factor α production. J. Exp. Med. 187:1069-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schorey, J. S., and A. M. Cooper. 2003. Macrophage signalling upon mycobacterial infection: the MAP kinases lead the way. Cell. Microbiol. 5:133-142. [DOI] [PubMed] [Google Scholar]
- 44.Schurig, G. G., R. M. Roop, I. I., T. Bagchi, D. Boyle, D. Buhrman, and N. Sriranganathan. 1991. Biological properties of RB51; a stable rough strain of Brucella abortus. Vet. Microbiol. 28:171-188. [DOI] [PubMed] [Google Scholar]
- 45.Stinavage, P., L. E. Martin, and J. K. Spitznagel. 1989. O antigen and lipid A phosphoryl groups in resistance of Salmonella typhimurium LT-2 to nonoxidative killing in human polymorphonuclear neutrophils. Infect. Immun. 57:3894-3900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tang, P., I. Rosenshine, P. Cossart, and B. B. Finlay. 1996. Listeriolysin O activates mitogen-activated protein kinase in eucaryotic cells. Infect. Immun. 64:2359-2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tang, P., C. L. Sutherland, M. R. Gold, and B. B. Finlay. 1998. Listeria monocytogenes invasion of epithelial cells requires the MEK-1/ERK-2 mitogen-activated protein kinase pathway. Infect. Immun. 66:1106-1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ugalde, J. E., C. Czibener, M. F. Feldman, and R. A. Ugalde. 2000. Identification and characterization of the Brucella abortus phosphoglucomutase gene: role of lipopolysaccharide in virulence and intracellular multiplication. Infect. Immun. 68:5716-5723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Verger, J. M., M. Grayon, E. Chaslus-Dancla, M. Meurisse, and J. P. Lafont. 1993. Conjugative transfer and in vitro/in vivo stability of the broad-host-range IncP R751 plasmid in Brucella spp. Plasmid 29:142-146. [DOI] [PubMed] [Google Scholar]
- 50.Wang, M., N. Qureshi, N. Soeurt, and G. Splitter. 2001. High levels of nitric oxide production decrease early but increase late survival of Brucella abortus in macrophages. Microb. Pathog. 31:221-230. [DOI] [PubMed] [Google Scholar]
- 51.Zhan, Y., and C. Cheers. 1998. Control of IL-12 and IFN-γ production in response to live or dead bacteria by TNF and other factors. J. Immunol. 161:1447-1453. [PubMed] [Google Scholar]