Abstract
Objectives
Enhanced recovery pathways (ERPs) are evidence-based approaches to improving perioperative surgical care. However, the role of electronic health records (EHRs) in their implementation is unclear. We examine how EHRs facilitate or hinder ERP implementation.
Materials and Methods
We conducted interviews with informaticians and clinicians from US hospitals participating in an ERP implementation collaborative. We used inductive thematic analysis to analyze transcripts and categorized hospitals into 3 groups based on process measure adherence. High performers exhibited a minimum 80% adherence to 6 of 9 metrics, high improvers demonstrated significantly better adherence over 12 months, and strivers included all others. We mapped interrelationships between themes using causal loop diagrams.
Results
We interviewed 168 participants from 8 hospitals and found 3 thematic clusters: (1) “EHR difficulties” with the technology itself and contextual factors related to (2) “EHR enablers,” and (3) “EHR barriers” in ERP implementation. Although all hospitals experienced issues, high performers and improvers successfully integrated ERPs into EHRs through a dedicated multidisciplinary team with informatics expertise. Strivers, while enacting some fixes, were unable to overcome individual resistance to EHR-supported ERPs.
Discussion and Conclusion
We add to the literature describing the limitations of EHRs’ technological capabilities to facilitate clinical workflows. We illustrate how organizational strategies around engaging motivated clinical teams with informatics training and resources, especially with dedicated technical support, moderate the extent of EHRs’ support to ERP implementation, causing downstream effects for hospitals to transform technological challenges into care-improving opportunities. Early and consistent involvement of informatics expertise with frontline EHR clinician users benefited the efficiency and effectiveness of ERP implementation and sustainability.
Keywords: electronic health records, clinical pathway, health plan implementation, perioperative care, patient safety
Background and significance
Electronic health records (EHRs) are ubiquitous in modern healthcare delivery and have demonstrated a substantial positive impact on healthcare quality and cost.1,2 Concurrent with healthcare’s adoption of EHRs, the surgical community has shifted to using enhanced recovery pathways (ERPs) to improve the safety and quality of perioperative care. ERPs bundle several evidence-based interventions to create a pathway that guides patient care before, during, and after surgical procedures.3 ERPs focus on patient and family engagement, early mobility, and less reliance on opioid pain medications, which has been effective at reducing morbidity,4 mortality,5 and cost,6 while increasing care quality and patient experience.5–11 ERPs have become the standard of care for elective colorectal surgery—with strong adoption in other specialties—and have been implemented widely in the United States.7–9 However, wide variations in how successfully ERPs are implemented and eventually sustained speak to the manifold challenges that often undermine efforts to integrate these pathways into routine practice.10–12
While EHRs and ERPs both have the capacity to standardize and improve care, little is known about the use of EHRs as a strategy to support ERP implementation. There is some evidence that EHRs would assist ERP implementation through ERP-standardized clinician order sets,13 which could act as a form of decision support,14 promoting ERP adherence and clinical quality.15 However, EHRs can also present challenges such as clinician resistance,16 workflow complications resulting from technical malfunctions,17 and limitations with clinical functionality.18
To the authors’ knowledge, this study is one of the first to investigate the benefits and drawbacks of using EHRs to support ERP implementation. Unlike most other work assessing EHR-supported pathway implementation,19–22 which were predominantly conducted in large, academic institutions, we draw upon a characteristically diverse sample of US hospitals (eg, by geography, capacity, and teaching status) and objectively distinguish between hospitals using quantitatively defined process measures. In this study, we examine the contextual factors of how EHRs can facilitate or hinder the adoption of ERPs and the organizational strategies used to integrate EHRs into the ERP workflow.
Methods
Overview of ERP collaborative
From 2017 to 2022, the Agency for Healthcare Research and Quality’s (AHRQ’s) Safety Program for Improving Surgical Care and Recovery (ISCR) was a partnership between Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality, American College of Surgeons, and Westat, Inc. that was dedicated to national ERP implementation.23 ISCR is an evidence-based initiative extending the principles and practices from AHRQ’s Comprehensive Unit-based Safety Program for reducing patient harm.7 Participating hospitals established a dedicated ISCR team and received best-practice resources,24 including an 18-month-long intervention period for planning, implementing, and sustaining ERPs with professional support and peer learning. The program included pathways for colorectal, orthopedic (ie, total joint replacement and hip fracture), gynecologic, and emergency general surgery.
Data collection
A sequential explanatory design was conducted with hospitals enrolled in ISCR’s colorectal pathway. We used mixed methods to quantitatively capture objective measurements of implementation outcomes, which are limited in previous evaluations of EHR-supported clinical pathways,25 while qualitatively uncovering the underlying effects and mechanisms. Purposive sampling was done to recruit hospitals with diversity in ownership, teaching status, size, and geographic location.
From June 2018 to October 2019, a multidisciplinary team of 3-6 researchers from Johns Hopkins and the University of California, San Francisco conducted semistructured interviews with administrators, clinicians, and staff members from each hospital (n = 168 participants) who were most engaged in and affected by ERP implementation (Supplementary Material). Each interview lasted approximately 30-60 min. Research team members had expertise in surgery, nursing, health services research, human factors, and implementation science. After obtaining informed consent, the interviews were audio-recorded and then professionally transcribed. Procedures were approved by the Johns Hopkins School of Medicine Institutional Review Board [Approval #: IRB00130799].
Quantitative data on hospital implementation performance was collected from a surgical registry containing process measures for compliance and outcomes hosted on the National Surgical Quality Improvement Program platform. Nine mandatory metrics of interest were collected from participating hospitals: preoperative bowel preparation, preoperative oral antibiotics, regional analgesia, early mobilization, early liquid intake, early solid intake, early Foley catheter removal, multimodal pain control, and venous thromboembolism prophylaxis.26,27 Data were collected from patients 18 years or older who underwent elective colorectal surgery.
Data analysis
Hospitals were categorized into 3 groups based on adherence to process measures over the study period. Linear regression with process measure adherence against time for each hospital was performed to identify slopes that were then ranked in quartiles.7 High performers consisted of hospitals in which at least 80% of patients were adherent to 6 of 9 measures. High improvers included hospitals with significantly improved adherence over at least 12 months, measured by being in the top quartile. All other hospitals were grouped as strivers (ie, hospitals working towards high performer or high improver status).
Given the novelty of studying the use of EHRs to support ERP implementation, we used a grounded theory approach with inductive thematic analysis without preconceived analytic categories.28 A multidisciplinary coding team first reviewed and coded interview transcripts line-by-line. To validate assignments, identically grouped quotes were iteratively compared, with particular emphasis on how categories linked together until no new concepts emerged at theoretical saturation.29 Finally, qualitative data were divided by their hospital implementation category (ie, high improver, high performer, or striver).
We created causal loop diagrams (CLDs) to visually depict how themes interrelate,30 specifically focusing on how different hospitals employed EHRs during ERP implementation. Arrows were drawn to emphasize intervention strategies for how hospitals successfully, or unsuccessfully, incorporated EHRs for more efficient and effective clinician workflow following ERP guidelines. CLDs were iteratively refined. First, guided by criteria from systems dynamics literature (eg, clarity, causality existence, predicted effect existence, alternate possible causes, case-effect direction, and tautology),31 the primary data coders [J.W., C.Y.] created the original CLDs. Other coding team members and an ERP nurse then reviewed CLDs for accuracy and consistency with the qualitative data. Finally, CLDs were discussed until consensus among the entire study team.
Results
Participants from 8 hospitals participated in the study (Table 1). At least one clinician and ERP implementation member were present across all hospitals. Further, hospital characteristics varied by ownership type, number of beds, teaching status, and location.
Table 1.
Hospital and interview participant characteristics.
| Performance category | High improver |
High performer |
Striver |
|||||
|---|---|---|---|---|---|---|---|---|
| Hospital 1 | Hospital 2 | Hospital 3 | Hospital 4 | Hospital 5 | Hospital 6 | Hospital 7 | Hospital 8 | |
| Hospital characteristics | ||||||||
| Ownership type | Voluntary nonprofit | Govt., district | Voluntary nonprofit | Govt., city-county | Govt., state | Voluntary nonprofit | Govt., district | Voluntary nonprofit |
| Teaching status | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Size (#beds) | >700 | 300–700 | <300 | >700 | 300–700 | <300 | >700 | 300–700 |
| Geographic location | Northeast | West | Northeast | South | West | Northeast | Midwest | West |
| Participant characteristicsa | ||||||||
| Surgeon | 3 | 7 | 2 | 5 | 1 | 5 | 3 | 3 |
| Anesthesiologist | 1 | 2 | 1 | 2 | 0 | 3 | 1 | 2 |
| Nurse | 8 | 4 | 6 | 3 | 7 | 7 | 11 | 3 |
| Informatician | 4 | 3 | 0 | 0 | 3 | 3 | 1 | 1 |
| Quality | 8 | 4 | 8 | 5 | 4 | 9 | 6 | 3 |
| Otherb | 2 | 2 | 5 | 2 | 1 | 1 | 3 | 0 |
| Total | 26 | 22 | 22 | 17 | 16 | 28 | 25 | 12 |
Characteristics include the individual’s primary professional role (many individuals also held leadership positions in the organization).
Other professional roles include pharmacist, physician assistant, epidemiologist, dietician, and physical therapist.
Three thematic clusters emerged. “EHR difficulties” (n = 61 quotes) captured themes concerning issues with the EHR itself, which could be divided between technology and user-related subcategories (Table 2). “EHR enablers” (n = 58; Table 3) and “EHR barriers” (n = 49; Table 4) in ERP implementation respectively included themes of facilitating and hindering factors that stemmed from using the EHR but beyond its intrinsic issues.
Table 2.
Themes in “EHR difficulties” and their illustrative quotes.
| Theme | Illustrative quote |
|---|---|
| Technology-related EHR difficulties | |
| Limited clinically useful features | “If [the EHR] had reminders at a specific time … that would help.” (Quality) |
| Limited interoperability | “It’s a big barrier because again, our group works in [EHR 1]. It doesn’t cross talk with [EHR 2].” (Surgeon) |
| Software bugs | “People are familiar with [the EHR] and the pathway crashed… one part was missing. We put a patient on [the ERP] and a whole chunk was missing.” (Nurse) |
| User-related EHR difficulties | |
| Long IT service times | “I think our hospital process is challenging, too. I'm not really sure if the program itself is that hard but I know you got to go through this committee and that committee and you got to talk to this guy and that guy.” (Surgeon) |
| Inadequate training | “So, [the EHR] really… there’s a lot of things you can do, but we don’t know what we can do.” (Nurse) |
| Physician resistance | “One of [the physicians] kind of refuses to use [the order set]. I’ve talked to the CNS from my department and she says, ‘I cannot make him. I cannot make him use it. He won’t listen to me.’” (Quality) |
Table 3.
Themes in “EHR enablers” in ERP implementation and their illustrative quotes.
| Theme | Illustrative quote |
|---|---|
| Greater ERP compliance | “We would audit the process of the universal protocol to make sure everybody was completing all of the elements, but those same elements were also defined within [the EHR], and so, we were able to create a report that basically pulled out all of those documented elements and showed us what our compliance was.” (Nurse) |
| Collaborative EHR improvement | “We had a lot of feedback from our team about what [order sets] should look like and a lot of reviews. I would say we spent probably our first year really making sure they were first rate and then you learn more about your practice and then you want to make changes to it, so they have to be a living document, not just a one and done thing. So, I think that’s where the kind of buy in commitment really has to happen.” (Nurse) |
| Dedicated EHR team | “Without the buy in of the, I’ll call them the [EHR] team … we could never have done it.” (Quality) |
Table 4.
Themes in “EHR barriers” in ERP implementation and their illustrative quotes.
| Theme | Illustrative quote |
|---|---|
| EHR-Induced ERP breakdown | “There’s a push and pull of what is helpful and what is almost impeding your workflow because you have to like, go through the computer and click.” (Nurse) |
| Selecting parts of ERP | “[Physicians] really wanted to mold a lot of stuff… they kind of picked and chose and that kind of bothered me a little bit.” (Pharmacist) |
| Clinician difficulties learning EHR | “I really wanted [the use of EHR pathway] to work. I’ve seen demos on it, but we haven’t gotten there yet. It won’t work because it’s complicated.” (Quality) |
High performers
Facing EHR difficulties, high performers demonstrated consistently effective integration of EHRs to support ERP implementation (Figure 1). Initially, EHR-induced breakdowns in supporting ERP practices arose from the EHRs’ lack of interoperability and easy-to-use features that would have facilitated clinical workflow. Without interoperability, many participants voiced their dissatisfaction with the difficulties of transferring information from non-EHR systems to EHRs. One participant reflected on the challenges of having to navigate to an external website for ERP data as preoperative clinical offices were not on the EHR: “We use outside sources and website that are not EHR transparent to follow [ERPs] … It’s very annoying, to be honest, that pre-op is on that one website” (Nurse). With EHR functionalities, participants commonly wished for clearer patient identification in the EHR that would create a standard for where the information was recorded as most clinicians “put the identification in the comment section, but it’s not consistent” (Informatician).
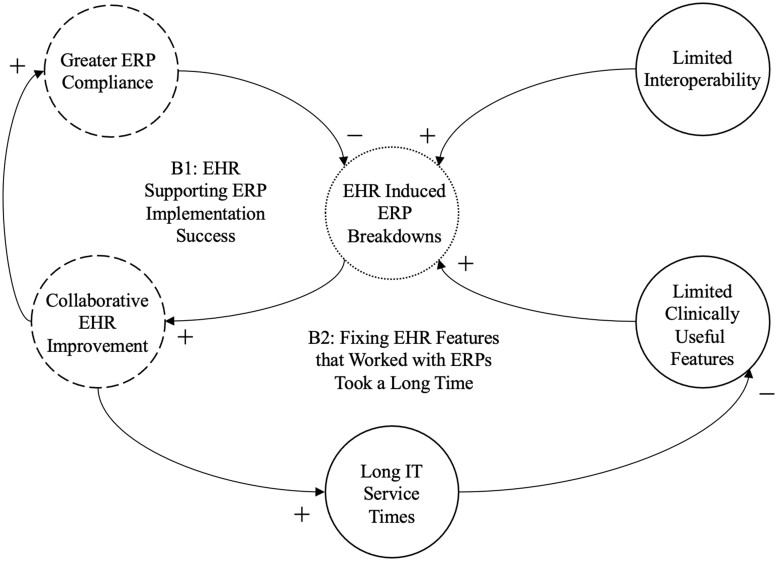
Figure 1.
High performers’ causal loop diagram. Key feedback loops for High performers portraying how qualitative themes under EHR Difficulties (solid-lined circles), EHR Enablers (dashed-lined circles), and EHR Barriers (dotted-lined circles) affected ERP implementation success. “B” describes balancing loops that include both + and − arrows. Arrows with a + sign indicate variables that increase or decrease together. Arrows with a − sign indicate variable relationships where increase (decrease) in one means decrease (increase) in the other.
To overcome these hurdles, high performers developed a collaborative and iterative EHR improvement process. Change began from open communication with frontline EHR users, inviting “a lot of feedback about what order sets should look like” (Nurse) and making them “more logical” (Informatician). In turn, high performers utilized these responses in an extensive planning period during the “first year to make sure [order sets] were first rate” (Nurse). Even after primary evaluations, high performers iteratively sought feedback. As one participant summarized, “The order set has to be a living document, not just a one and done thing” (Nurse).
Consequently, high performers adapted EHRs to assume a core part of the ERP workflow, utilizing the EHR system to embed ERP practices and promote documentation of ERP compliance. Several participants mentioned how EHR order sets were used to standardize ERP practices across the organization and serve as decision-support tools at the point of care that were “certainly helpful in guiding the way that we’re to care for patients” (Nurse). Moreover, a participatory approach to developing EHR order sets with clinician end-users positively affected ERP adoption by creating a sense of shared ownership and understanding. By building order sets with physicians, ERP champions mitigated resistance by using the development process to familiarize hesitant physicians with the reason behind each selection in the order set and the ERP’s significance overall. As one nurse stated, “I showed [the resistant physicians] the order sets and I tried to use everything to my advantage to really get buy-in from them.”
However, high performers’ open, collaborative approach unintentionally caused delays as information technology (IT) service staff became overwhelmed by newly arising issues. Seemingly minor fixes were bottlenecked: “Making changes in the EHR, even if there’s something very minute like an unchecked box versus a checked box, can take months. That’s just been frustrating for lots of people” (Physician Assistant). The extensive wait times arose from inefficiencies in communicating the problem. One surgeon “was surprised at the number of emails it took” to begin the problem-solving process. On the informatics side, IT staff were inundated by outstanding inquiries with “a million small things everywhere and nobody knowing what’s first” (Quality). Participants suggested a better equipped team may have overcome the workload: “I’ll be 100% honest with you, [the informaticists] are mismanaged, overwhelmed, and under-resourced” (Quality).
Yet, high performers maintained consistent compliance because some clinician users independently found manual workarounds. For example, one participant adjusted to the lack of interoperable information sharing by “copying and pasting data to the EHR” (Nurse). Another individual built automatically insertable texts called “Dot Phrases” to identify ERP patients: “I just wrote a Word document, copied it to be a ‘Dot Phrase,’ and then I trained the nurses to go into the encounter put the ‘dot ERAS’ or whatever the name of it is” (Quality). Through systematic and ad hoc solutions, High performers gradually lessened the burden of EHR challenges and successfully adopted EHRs to support ERP work.
High improvers
Like high performers, high improvers’ most prevalent EHR challenge was with limited clinically useful features (Figure 2). High performer participants also conveyed troubles with the EHRs’ complexity, often finding the system to prompt for the same information multiple times and leading to redundant inputs: “There is an element of doing what you need to do and then documenting what you need to do and then re-documenting that you documented” (Nurse). As a result, information retrieval was an issue as there was no “defined place where people would consistently document information” since the EHRs’ design gave users “the ability to document in different areas and still get the same end result” (Nurse).
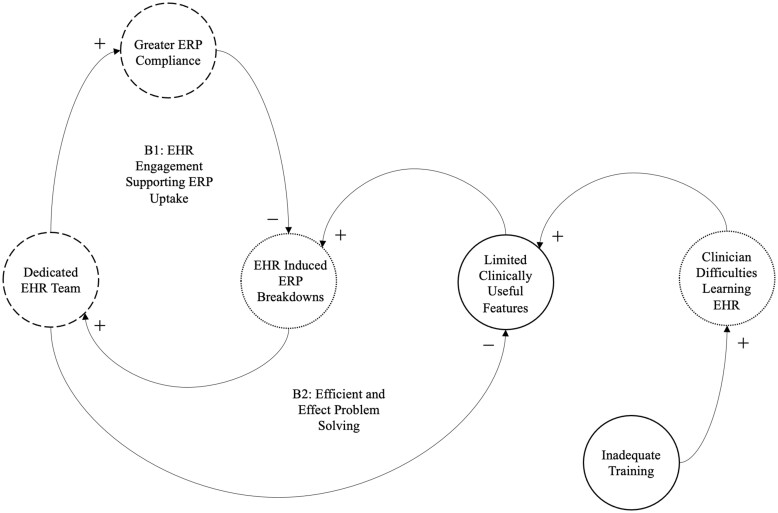
Figure 2.
High improvers’ causal loop diagram. Key feedback loops for high improvers portraying how qualitative themes under EHR Difficulties (solid-lined circles), EHR Enablers (dashed-lined circles), and EHR Barriers (dotted-lined circles) affected ERP implementation success. “B” describes balancing loops that include both + and − arrows. Arrows with a + sign indicate variables that increase or decrease together. Arrows with a − sign indicate variable relationships where increase (decrease) in one means decrease (increase) in another.
However, high improvers had distinct causes to EHR difficulties and strategies to overcome those shortcomings that gradually maximized the technology’s added benefits. For example, many high improvers attributed the limited usefulness of the EHR to clinicians’ inadequate training of both the EHR itself and its integration into the ERP workflow. Several interviewees commented on their rudimentary grasp of the EHRs’ capabilities: “So, [the EHR] is really big. There’s a lot of things you can do, but we don’t know what we can do” (Nurse). With the EHR learning curve, difficulties commonly appeared under 2 reasons: (1) There was ambiguity around who would be included in formal didactic training [eg, “Something we struggled with was … are we training all the nurses in the entire site or just on a specific unit?” (Informatician)]; And (2) on-the-job training was limited by the scarce number of patient cases [eg, “It’s hard, too, because of volume, right? Like, this one nurse that I worked with yesterday might not get another colorectal patient for a couple weeks” (Informatician)].
High improvers also developed unique solutions, particularly with forming a multidisciplinary EHR team dedicated to facilitating EHR use and troubleshooting problems. This group developed 4 main methods for improved EHR-ERP alignment: (1) Engaging the IT team as early as possible [eg, “We had our IT partners engaged early” (Quality)]; (2) involving physician champions in building order sets [eg, “The colorectal surgeon is very cognizant of the [ERP] protocols and he was present in every step of the way in the order set developing … that’s what really informed pathway development” (Nurse)]; (3) devoting personnel exclusively for facilitating intra- and inter-departmental communication during order set builds [eg, “My main role …. I kind of helped a lot more with the system integration, specifically with order sets in order management through the various ERAS orders” (Informatician)]; And (4) investing in end-user testing to receive real-world feedback from the intended frontline audience [eg, “We got engaged to work on what’s called ‘operational readiness’ to make sure the end users are comfortable and capable to use the tool once they get the patients” (Informatician)].
In time, high improvers saw increased compliance with ERP measures as several interviewees, as with those from HIGH PERFORMERS, mentioned that order sets provided “substance” to the ERP (Surgeon). The digital workflow further simplified how hospitals kept track of their ERP performance:
It was originally a completely manual process where we would go around with our forms and our clipboards, and we would audit the process of the protocol to make sure everybody was completing all the elements. But those same elements were also defined within [the EHR], and so, we were able to create a report that basically pulled out all of those documented elements and showed us what our compliance was (Nurse).
Moreover, a well-resourced EHR team efficiently and effectively solved issues, avoiding lengthy holdups as with high performers. While high improver participants likewise expressed how the EHRs’ unintuitive nature stemmed from a disconnect in communicating clinicians’ wants to informaticians [eg, “The hardest thing was translating what was agreed upon on those paper pathways into [the EHR] build” (Informatician)], high improvers enrolled a “special reporting person” who acted as an intermediary between clinicians and technicians, exchanging information across departments from “figuring out what elements [the physicians] needed … to going back to the build team to figure out where that stuff sat in the background” (Nurse).
Strivers
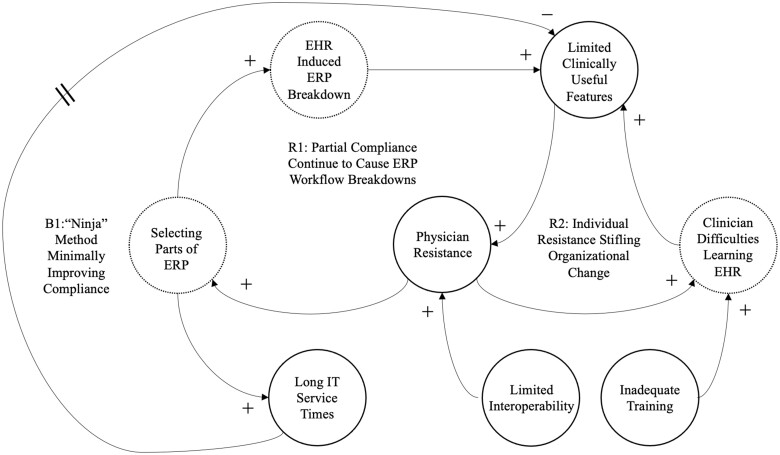
Strivers exhibited EHR difficulties common to both high performers and high improvers (Figure 3). Interoperability limitations particularly became “a big barrier” at one hospital because the colorectal surgery service line used a different EHR vendor that did not “cross talk” with others (Nurse). At multihospital sites, several participants commented on interoperability challenges due to different coding schemes. One quality manager explained how their idea of creating an evaluative dashboard to monitor and demonstrate good practice encountered difficulties because the original patients were documented using International Classification of Disease, Tenth Revision codes while others were in Current Procedural Terminology codes. Further, participants recalled many instances of workflow breakdowns due to inadequate training, with clinicians not yet adjusted to using order sets. For example, an order “that should’ve been clear” was placed for a restrictive diet of no food or drink, but the “catering associate didn’t check and they sent [the patient] a tray of food after surgery anyways” (Quality). Such breakdowns became especially problematic during patient hand-offs across departments, exemplified by a nurse who described how the dietary staff left documentation for nurses to complete: “[Dieticians] don’t always fill it out when they pull the tray and leave it for the nursing staff”.
Figure 3.
Strivers’ causal loop diagram. Key feedback loops for Strivers portraying how qualitative themes under EHR Difficulties (solid-lined circles), EHR Enablers (dashed-lined circles), and EHR Barriers (dotted-lined circles) affected ERP implementation success. “B” describes balancing loops that include both + and − arrows. “R” describes reinforcing loops that only include + arrows. Arrows with a + sign indicate variables that increase or decrease together. Arrows with a − sign indicate variable relationships where increase (decrease) in one means decrease (increase) in another. A hashed line on an arrow indicates a delay in effect.
Unlike with high performers and high improvers, EHR difficulties contributed to individual physician resistance to EHRs and ERPs in general. For example, one interviewee described how physicians were perplexed by lack of interoperability: “[Surgeons] would say, ‘What do you mean it doesn’t talk to each other? How is that not possible?’” (Informatician). Physicians also rejected ERPs outright without explanation: “Once again, we do have a hold-out doctor that has not updated his order set. He’s not down for it … I don’t know how you change one person’s practice” (Quality). Two explanations for this phenomenon emerged: (1) Physicians did not have time to learn the EHR system, preferring familiar order sets instead [eg, “Our physicians don’t make a lot of time to learn the information systems, so once they got their favorites order sets built, they don’t want to take the time to create new ones” (Nurse)]; And (2) physicians believed they did not have the responsibility to maintain order sets [eg, “The surgeon would say it’s the office’s fault for not carrying over the orders” (Anesthesiologist)]. Further, these uncooperative individuals were, in turn, difficult to train, creating a problematic feedback loop that stifled organizational change. Several participants also observed that some physicians did not reject the order set outright, but only complied with certain components of the ERPs they actively selected as part of a customized order set:
[The surgeon] says that elements of the ERP are in his orders, but he doesn’t use the ERP orders (Nurse).
Some of the surgeons won’t utilize the entire [order set]. They pick components of it (Nurse).
To overcome this barrier, strivers uniquely enacted “the ninja approach” where pre-established order sets discretely replaced a physician’s old builds (Surgeon). Described by one pro-ERP surgeon:
We had several meetings where we came up with a standardized order set and once things are kind of pre-checked … you’re kind of sneaking them in. A lot of these guys won’t go in and change it unless there was some kind of contraindication … So, you sneak up on ‘em. The ninja approach.
Concerns were expressed for this method as “a little too radical,” but one surgeon defended the reason for the approach was to deal with “residents [who] are really good at getting around the order sets” and sidestep a “time consuming, cumbersome process” of establishing consensus. However, the plan was eventually scrapped for a more moderate, opt-out approach where physicians were alerted pre-change:
We emailed all the surgeons and said, ‘We want to know what changes you would like to see.’ And we didn’t hit threatening, we just said, “For your information, this is going to be instituted in thirty days. If you don’t respond, then this is what we have” (Nurse).
These iterative adjustments “took the longest to get going” in the administrative process, with technical changes further compounding the delay (Nurse). Ultimately, ERP compliance minimally improved as some physicians only went through the motions of following the order sets. As one participant described: “It’s been kind of hard at this point because the ‘yeses’ are using the order sets, but I’ve still got a list of patients that did not get [ERP treatment]” (Quality).
Discussion
By analyzing how EHRs supported ERP implementation at hospitals of varying pathway implementation success, this study captured improvement strategies, and their potential breakdowns, on how clinician and informatics teams can leverage EHRs to improve perioperative care quality through ERPs. Across all hospitals, we found limitations with the EHRs’ technical functionalities to facilitate the implementation of ERP practices. However, high performers and high improvers successfully mitigated these issues through solutions driven chiefly by extensive and iterative collaboration between technical development and clinician end-users. Strivers, while enacting some fixes to maximize buy-in, were unable to overcome physician resistance to novel ERP methods through EHR-ERP workflows.
Our findings further health IT implementation literature by identifying organizational behaviors that can both facilitate and undermine the use of EHRs to advance evidence-based protocols. Our results echo concerns with certified EHRs’ lack of important capabilities and interoperable systems.32–34 To overcome these technical hurdles, prior EHR implementation studies have demonstrated the advantages of strong clinician advocacy for increasing EHR adoption.35–37 In our case, when the EHR shifts from the targeted “technology” to be implemented to the “strategy” used to support implementation of another tool, clinician users’ vocalness likewise encouraged problem-solving in team members. Moreover, as EHRs become synonymous with the ERP workflow, clinician champions often became first lines of communication for anything pertaining to EHRs and ERPs, which usually necessitated above average expertise in both areas. With growing awareness of the informatician’s importance, interdisciplinary training could greatly enhance the practicality of informatics know-how.38 Users with above-average EHR training have been shown to foster greater EHR implementation success, which facilitated technical solution finding during ERP implementation.35 Indeed, Strivers who could not fully engage such personnel saw slower ERP implementation success.
Strivers exhibited strategies to improve EHR-ERP uptake, but their scope was limited to problem identification instead of problem-solving—a response galvanized by dedicated IT teams in high improvers and high performers. The disconnect between the development process and improved outcomes may be attributed to limitations in how effectively Strivers involved clinician end-users and educated them on the EHRs’ functionalities.39 Further, Strivers’ unique challenges with clinician resistance demonstrate how individual-level barriers may be more difficult to systematically overcome than technical ones, with EHR use potentially exacerbating tensions. Computerizing care pathways have been shown to elevate concerns within clinicians over their professional autonomy to make decisions, stemming from what is generally understood to be a benefit of ERPs and EHRs—standardization.40–42 While promoting safer, higher quality, and more cost-efficient care, standardization may infringe upon a physician’s ability to customize treatments for a patient’s unique needs.43,44 Further qualitative studies with hold-out users could elucidate whether flexibility is needed in ERP protocol, EHR features, or both.
Standardization benefited hospitals with successful ERP implementation who took advantage of the EHRs’ strengths. As high improver and high performer participants recognized, EHRs operationalized ERP practices into clickable orders, a benefit to standardization.1,45 For hesitant clinicians, high improvers purposefully involved them with the IT team developers as early as possible to both proactively identify potential issues and gradually gain their buy-in through a participatory approach. Indeed, prior research supports how closely involving end-users during the electronic clinical pathway development increases uptake.22,39 Despite their advantages, such iterative collaborations can be time consuming—a barrier plaguing high performers.22 This should not detract but rather reinforce the importance of investing in IT teams. A well-staffed and resourced IT team could attend to more straightforward, technical fixes, which the overwhelming number of inquiries burdened hospitals, and forgo the need to summon more time and budget consuming vendor-executed changes.46
Several limitations should be considered when interpreting our findings. First, given the complexity of actors, scale, and timeframe of implementation, a myriad of factors beyond EHR use contributed to measured performance differences across hospitals. While interactions with EHRs were necessary to engage with the ERP order sets, implementation success was captured by an array of compliance outcomes that extended beyond clinician and administrative EHR experience. However, one meta-analysis noted that past studies on computerized care pathways neither accounted for measured effects on clinical practice nor detailed examinations into associations between specific parts of the technology and outcomes—2 elements this study addresses by analyzing EHR-ERP interactions in light of ERP implementation success.40 Second, although we had a diverse sample of hospitals in terms of size, geographic location, ownership type, and teaching status, the generalizability of the findings may be limited. Because participation was voluntary, enrolled hospitals were not selected at random. Third, patient perspectives were not considered in the study, potentially ignoring important shortcomings of EHRs (eg, decreased patient–clinician interactions) in relation to patient engagement-promoting characteristics of the ERP. As ERPs are designed to foster meaningful patient interaction, future studies are needed to analyze how patient–clinician communication are hindered or facilitated by EHR use with programs designed to promote collaborative exchanges.
Conclusion
The degree to which EHRs can facilitate ERP implementation and, subsequently improvements in perioperative care, depends in large part on the collaborative efforts between clinicians and informaticians. We found that organizational management moderates how advantageous EHRs could be in standardizing practice and gaining compliance. Our results suggest a participatory design approach with early and consistent engagement of informatics expertise with frontline users in an interdisciplinary implementation team benefited the implementation and sustainability of a widely used evidence-based care protocol.
Supplementary Material
Acknowledgments
Statements in the manuscript do not necessarily represent the official views of, or imply endorsement by, the United States Agency for Healthcare Research and Quality or Department of Health and Human Services.
Contributor Information
JunBo Wu, Department of Anesthesiology and Critical Care Medicine, Armstrong Institute for Patient Safety and Quality, Johns Hopkins University School of Medicine, Baltimore, MD 21205, United States.
Christina T Yuan, Department of Anesthesiology and Critical Care Medicine, Armstrong Institute for Patient Safety and Quality, Johns Hopkins University School of Medicine, Baltimore, MD 21205, United States; Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD 21205, United States.
Rachel Moyal-Smith, Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD 21205, United States; Ariadne Labs: A Joint Center of the Harvard School of Public Health and Brigham and Women's Hospital, Harvard T.H. Chan School of Public Health, Boston, MA 02215, United States.
Elizabeth C Wick, Department of Surgery, University of California, San Francisco, San Francisco, CA 94143, United States.
Michael A Rosen, Department of Anesthesiology and Critical Care Medicine, Armstrong Institute for Patient Safety and Quality, Johns Hopkins University School of Medicine, Baltimore, MD 21205, United States.
Author contributions
J.W., C.Y., and M.R. made substantial contributions to the conception and design of the work. J.W., C.Y., R.M.S., and M.R. made substantial contributions to the acquisition, analysis, and interpretation of the data. JW and MR drafted the work. J.W., C.Y., R.M.S., E.W., and M.R. made critical revisions. All authors gave final approval of the version to be published.
Supplementary material
Supplementary material is available at Journal of the American Medical Informatics Association online.
Funding
This work was supported by the Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services grant number HHSP2332015000201/task order HHSP23337004T.
Conflict of interest
The authors have no competing interests to declare.
Data availability
The data underlying this article cannot be shared publicly due to the privacy of individuals who participated in the study. The data will be shared on reasonable request to the corresponding author.
References
- 1. Zlabek JA, Wickus JW, Mathiason MA.. Early cost and safety benefits of an inpatient electronic health record. J Am Med Inform Assoc. 2011;18(2):169-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Atasoy H, Greenwood BN, McCullough JS.. The digitization of patient care: a review of the effects of electronic health records on health care quality and utilization. Annu Rev Public Health. 2019;40(1):487-500. [DOI] [PubMed] [Google Scholar]
- 3. Wick E, Fischer C, McSwine S, et al. AHRQ safety program for ISCR expands scope to include emergency general surgery in 2020. 2020. Accessed February 27, 2023. https://bulletin.facs.org/2020/01/ahrq-safety-program-for-iscr-expands-scope-to-include-emergency-general-surgery-in-2020/
- 4. Grant M, Yang D, Wu C, et al. Impact of enhanced recovery after surgery and fast track surgery pathways on healthcare-associated infections: results from a systematic review and meta-analysis. Ann Surg. 2017;265(1):68-79. [DOI] [PubMed] [Google Scholar]
- 5. Thiele R, Rea K, Turrentine F, et al. Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg. 2015;220(4):430-443. [DOI] [PubMed] [Google Scholar]
- 6. Stone A, Grant M, Pio Roda C, et al. Implementation costs of an enhanced recovery after surgery program in the United States: a financial model and sensitivity analysis based on experiences at a quaternary academic medical center. J Am Coll Surg. 2016;222(3):219-225. [DOI] [PubMed] [Google Scholar]
- 7. Cardell CF, Knapp L, Cohen ME, et al. Successful implementation of enhanced recovery in elective colorectal surgery is variable and dependent on the local environment. Ann Surg. 2021;274(4):605-612. [DOI] [PubMed] [Google Scholar]
- 8. Spencer P, Scott M.. Implementing enhanced recovery after surgery across a United States health system. Anesthesiol Clin. 2022;40(1):1-21. [DOI] [PubMed] [Google Scholar]
- 9. Williams J, McConnell G, Allender J, et al. One-year results from the first US-based enhanced recovery after cardiac surgery (ERAS Cardiac) program. J Thorac Cardiovasc Surg. 2019;157(5):1881-1888. [DOI] [PubMed] [Google Scholar]
- 10. Pearsall E, Meghji Z, Pitzul K, et al. A qualitative study to understand the barriers and enablers in implementing an enhanced recovery after surgery program. Ann Surg. 2015;261(1):92-96. [DOI] [PubMed] [Google Scholar]
- 11. Stone A, Yuan C, Rosen M, et al. Barriers to and facilitators of implementing enhanced recovery pathways using an implementation framework: a systematic review. JAMA Surg. 2018;153(3):270-279. [DOI] [PubMed] [Google Scholar]
- 12. Regenbogen S, Cain-Nielsen A, Syrjamaki J, et al. Clinical and economic outcomes of enhanced recovery dissemination in Michigan hospitals. Ann Surg. 2021;274(2):199-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ancker J, Kern L, Edwards A, et al. ; HITEC Investigators. Associations between healthcare quality and use of electronic health record functions in ambulatory care. J Am Med Inform Assoc. 2015;22(4):864-871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bobb A, Payne T, Gross P.. Controversies surrounding use of order sets for clinical decision support in computerized provider order entry. J Am Med Inform Assoc. 2007;14(1):41-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thiel S, Asghar M, Micek S, et al. Hospital-wide impact of a standardized order set for the management of bacteremic severe sepsis. Crit Care Med. 2009;37(3):819-824. [DOI] [PubMed] [Google Scholar]
- 16. Jha A, DesRoches C, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628-1638. [DOI] [PubMed] [Google Scholar]
- 17. Wright A, Ai A, Ash J, et al. Clinical decision support alert malfunctions: analysis and empirically derived taxonomy. J Am Med Inform Assoc. 2018;25(5):496-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Office of the National Coordinator of Health Information Technology. Strategy on reducing regulatory and administrative burden relating to the use of health IT and EHRs final report. 2020. Accessed August 17, 2023. https://www.healthit.gov/topic/usability-and-provider-burden/strategy-reducing-burden-relating-use-health-it-and-ehrs
- 19. Bartlett A, Makhni S, Ruokis S, et al. Use of clinical pathways integrated into the electronic health record to address the coronavirus disease 2019 (COVID-19) pandemic. Infect Control Hosp Epidemiol. 2023;44(2):260-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goldberg MJ. POSNA precourse quality, safety, value: from theory to practice management session 4 deliverables supracondylar clinical pathway. J Pediatr Orthop. 2015;35(5 Suppl 1):S39-40. [DOI] [PubMed] [Google Scholar]
- 21. Katzan L, Fan Y, Speck M, et al. Electronic stroke carepath: integrated approach to stroke care. Circ Cardiovasc Qual Outcomes. 2015;8(6 Suppl 3):S179-S189. [DOI] [PubMed] [Google Scholar]
- 22. Lenz R, Blaser R, Beyer M, et al. IT support for clinical pathways—lessons learned. Int J Med Inform. 2007;76(Suppl 3):S397-S402. [DOI] [PubMed] [Google Scholar]
- 23. Wick E, Rosen M, Ko C. AHRQ safety program for improving surgical care and recovery. AHRQ [final report] June 2023. Accessed August 17, 2023. https://www.ahrq.gov/sites/default/files/wysiwyg/hai/tools/surgery/final-report.pdf
- 24. Agency for Healthcare Research and Quality, Rockville, MD. Toolkit for improving surgical care and recovery. 2023. Accessed August 11, 2023. https://www.ahrq.gov/hai/tools/enhanced-recovery/index.html
- 25. Neame T, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ban K, Gibbons M, Ko C, et al. Evidence review conducted for the agency for healthcare research and quality safety program for improving surgical care and recovery: focus on anesthesiology for colorectal surgery. Anesth Analg. 2019;128(5):879-889. [DOI] [PubMed] [Google Scholar]
- 27. Ban K, Gibbons M, Ko C, et al. Surgical technical evidence review for colorectal surgery conducted for the AHRQ safety program for improving surgical care and recovery. J Am Coll Surg. 2017;225(4):548-557.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bernard H. Social Research Methods: Qualitative and Quantitative Approaches. SAGE Publications, Inc; 2012. [Google Scholar]
- 29. Patton M. Qualitative Research & Evaluation Methods: Integrating Theory and Practice. SAGE Publications, Inc; 2014. [Google Scholar]
- 30. Barbrook-Johnson P, Penn A.. Causal loop diagrams. In: Penn A, Barbrook-Johnson P., eds. Systems Mapping: How to Build and Use Causal Models of Systems. Palgrave Macmillan; 2022;47-59. [Google Scholar]
- 31. Burns J, Musa P. Structural validation of causal loop diagrams. In: Atlanta System Dynamics Conference, Atlanta. 2001;1-13.
- 32. Topaz M, Ronquillo C, Peltonen L, et al. Nurse informaticians report low satisfaction and multi-level concerns with electronic health records: results from an international survey. AMIA Annu Symp Proc. 2017;2016(1):2016-2025. [PMC free article] [PubMed] [Google Scholar]
- 33. Nguyen L, Bellucci E, Nguyen L.. Electronic health records implementation: an evaluation of information system impact and contingency factors. Int J Med Inform. 2014;83(11):779-796. [DOI] [PubMed] [Google Scholar]
- 34. Sockolow P, Liao C, Chittams J, et al. Evaluating the impact of electronic health records on nurse clinical process at two community health sites. In:NI 2012: 11th International Congress on Nursing Informatics, June 23-27, 2012, Montreal, Canada; 2012:381. [PMC free article] [PubMed] [Google Scholar]
- 35. Yuan C, Bradley E, Nembhard I.. A mixed methods study of how clinician ‘super users’ influence others during the implementation of electronic health records. BMC Med Inform Decis Mak. 2015;15(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rajamani S, Hultman G, Bakker C, et al. The role of organizational culture in health information technology implementations: a scoping review. Learn Health Sys. 2022;6(3):e10299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gui X, Chen Y, Zhou X, et al. Physician champions’ perspectives and practices on electronic health records implementation: challenges and strategies. JAMIA Open. 2020;3(1):53-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hersh W. Who are the informaticians? What we know and should know. J Am Med Inform Assoc. 2006;13(2):166-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Schuld J, Schäfer T, Nickel S, et al. Impact of IT-supported clinical pathways on medical staff satisfaction: a prospective longitudinal cohort study. Int J Med Inform. 2010;80(3):151-156. [DOI] [PubMed] [Google Scholar]
- 40. Gooch P, Roudsari A.. Computerization of workflows, guidelines, and care pathways: a review of implementation challenges for process-oriented health information systems. J Am Med Inform Assoc. 2011;18(6):738-748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Phansalkar S, Weir C, Morris A, et al. Clinicians’ perceptions about use of computerized protocols: a multicenter study. Int J Med Inform. 2007;77(3):184-193. [DOI] [PubMed] [Google Scholar]
- 42. Goud R, van Engen-Verheul M, de Keizer N, et al. The effect of computerized decision support on barriers to guideline implementation: A qualitative study in outpatient cardiac rehabilitation. Int J Med Inform. 2010;79(6):430-437. [DOI] [PubMed] [Google Scholar]
- 43. Sinsky C, Bavafa H, Roberts R, et al. Standardization vs customization: finding the right balance. Ann Fam Med. 2021;19(2):171-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sangal R, Liu R, Cole K, et al. Implementation of an electronic health record integrated clinical pathway improves adherence to COVID-19 hospital care guidelines. Am J Med Qual. 2022;37(4):335-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Rothman B, Leonard J, Vigoda M.. Future of electronic health records: implications for decision support. Mt Sinai J Med. 2012;79(6):757-768. [DOI] [PubMed] [Google Scholar]
- 46. Edwards P, Moloney K, Jacko JA, et al. Evaluating usability of a commercial electronic health record: A case study. Int J Hu Comput. 2008;66(10):718-728. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared publicly due to the privacy of individuals who participated in the study. The data will be shared on reasonable request to the corresponding author.