Abstract
Introduction
The prevalence of adults with partially dental arches is expected to be more than imagined and patients requiring replacement of missing teeth are slowly increasing in number too. Removable partial dentures are known to provide for substantial replacement for the missing teeth with also added advantages when compared to fixed or implant prosthesis, mainly in elderly patients. Denture base material performance and durability are greatly influenced by wettability and water contact angle. In the case of dentures; adequate moisture distribution is necessary to ensure excellent wettability which has an influence on comfort and oral health. The purpose of conducting this study was to find out whether the advancements made using PEEK (Polyether ether ketone) would prove to be more beneficial than the current upgrades in the current material spectrum.
Materials and methods
This study was performed under in vitro conditions. All the fabrication and processing was done only by one operator. The materials used were divided into three groups each comprising 20 samples. Group A was modified polymethylmethacrylate (Bredent Polyan), Group B was polyoxymethylene acetal resin (Biodentaplast) and Group C was PEEK. An Ossila Goniometer was used to measure the contact angle. The three types of liquids used for the testing included distilled water, natural saliva and mouth wetting solution (Wet Mouth Liquid, ICPA India). Human saliva was collected from an individual with no medical conditions and normal salivary secretion.
Results
The data was analyzed using One-way ANOVA test and a pairwise comparison using the Post Hoc Tukey’s Honest Significant Difference. Table 1 consists of the mean water contact angles of the denture base materials and mean contact angles of various denture base materials. In saliva, mouth wetting solution and distilled water, the highest mean and least mean contact angle was seen in Polyan and Biodentaplast respectively. A signicant difference was seen between PEEK and Polyan and Biodentaplast and Polyan on further comparison.
Conclusion
From the resources and the materials at our disposal, it could be concluded that Polyan, Biodentaplast and PEEK and could be used as viable options in cast partial denture framework.
Keywords: Partial denture [MeSH terms], PEEK, Biodentaplast, Polyan, Contact angle, Wettability [MeSH terms]
Introduction
The prevalence of adults with partially dental arches is expected to be more than imagined and patients requiring replacement of missing teeth are slowly increasing in number too [1, 2]. Among the options available, removable partial dentures are known to provide for substantial replacement for the missing teeth with also added advantages when compared to fixed or implant prosthesis, mainly in elderly patients [3]. A variety of materials are available for the manufacturing of a cast partial denture. Traditionally these dentures are made from casting of a wax framework [4] but with the advent of computer aided design and computer aided manufacturing(CADCAM), these prosthesis can now be designed and delivered using digital techniques too [5]. The metal framework could be produced using either cobalt chromium alloys or even titanium on which conventional acrylic material could be used. Acrylic could also be replaced by newer materials as thermoplastic acrylic, polyoxymethylene, PEEK and even flexible resins. Denture base material performance and durability are greatly influenced by wettability and water contact angle. The ability of a material to spread and cling to saliva or water is referred to as wettability [6, 7]. In the case of dentures, adequate moisture distribution is necessary to ensure excellent wettability, which in turn influences comfort and oral health. Better wettability, or the ability of a material to absorb moisture more easily, is indicated by a lower water contact angle. This is crucial since tissue irritation and oral health problems can be brought on by dryness.
With the increase in allergies seen in patients to the classic polymethylmethacrylate materials [8, 9] many dentists now opt for presumably hypoallergenic denture base resins that include polyurethane, polyethylenterephthalate, polybutylenterephthalate and modified methacrylate based denture bases [10]. Polyan is considered to be a thermoplastic modified methacrylate product which displayed less residual monomer content [11–23].
Since 1986, polyoxymethylene (POM), commonly known as acetal resin, has been used as an alternate denture foundation and denture clasp material, largely to improve aesthetics [24]. An example of this material would be Biodentaplast. Acetal resins have been employed as a denture base and clasp material as an alternative [25]. They are made from formaldehyde polymerization and have been proposed as an alternate material for removable denture framework production in individuals who have allergies to cobalt–chromium alloys [24]. It has enough resilience and modulus of elasticity, as well as high impact strength and resistance to organic solvents, oils, and hot and cold water [26], to be used in the fabrication of frameworks, retentive clasps, connectors, and support elements for removable partial dentures [26]. Another well-known high-performance thermoplastic aromatic polymer is poly ether-ether-ketone (PEEK). It’s a two-phase, semicrystalline polymer with a crystallinity of 30 to 35%, depending on the manufacturing method [27]. It has good mechanical qualities as well as excellent biocompatibility. It is thought to be a good material for removable denture frameworks and their components, including esthetic clasps [28–30].
The purpose of conducting this study was to find out whether the advancements made using PEEK would prove to be more beneficial than the current upgrades in the current material spectrum. According to the authors knowledge no such study or research has been conducted before comparing the efficacy of these three materials specifically.
The null hypothesis is that modified methacrylate, polyoxymethylene and polyetheretherketone(PEEK) all have the same physical properties when used in the fabrication of removable partial dentures.
Materials and methods
This study was performed under in vitro conditions. All the fabrication and processing was done only by one operator. The materials used were divided into three groups. Group A was modified polymethylmethacrylate (Bredent Polyan), Group B was polyoxymethylene acetal resin (Biodentaplast) and Group C was Polyethertetherketone (PEEK).
The three types of liquids used for the testing included distilled water, natural saliva and mouthwetting solution(Wet Mouth Liquid, ICPA India). The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the Institute, Saveetha Dental College And Hospitals [Protocol number: SRB/SDC/PROSTHO-2102/22/105; Date: 09/08/2022]. The study protocol was developed, and all subjects gave their written informed consent for inclusion before they participated in the study.
Sample fabrication
Polyan
20 wax patterns of the dimensions 22 mm x 17 mm x 3 mm were fabricated. An STL file (Fig. 1) was created of the correct dimensions and the wax was milled into 3 specimens (Roland DGShape, DWX 52D). This was done to avoid any error in the thickness of the slice obtained. Once fabricated, they were then invested in a flask specifically for this material after which dewaxing was carried out. A film sprue is attached to the wax model to benefit from the mechanical properties of the thermoplastics. Sprue application is done using a 1.5 mm thick wax plate. A 10 mm thick injection moulding sprue directly to the model with the help of a 1.5 mm wax plate. Polyan material was then loaded into an aluminum cartridge. The processing is carried out in Thermopress 400 (Fig. 2) injection moulding device with the processing parameters already present in the device as per the manufacturers recommendations. The surface which acts as the tissue surface is not polished. A tungsten carbide bur was used to remove extra resin from the specimens before finishing them with wet silicon carbide sheets (600-grit, 800-grit, 1000-grit, and 1200-grit). Only one surface was wet in order to simulate laboratory techniques and it was polished with a cloth wheel and pumice. A final size of 20 mm x 15 mm x 2 mm was obtained. Each Polyan slice was then used for one media only.
Fig. 1.
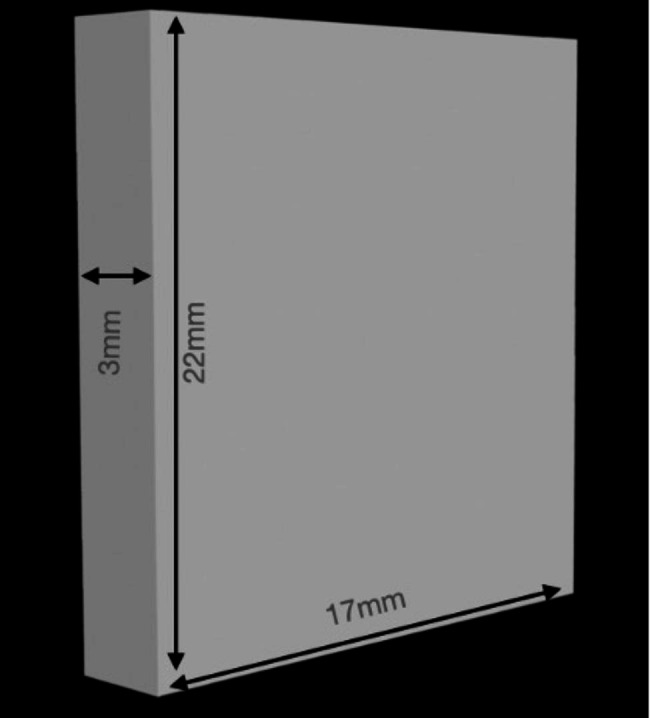
The dimensions of the designed STL file to be milled
Fig. 2.
Thermopress 400
Biodentaplast
20 wax patterns of the dimensions 22 mm x 17 mm x 3 mm were fabricated. The same design was used for the creation of the wax pattern. Once obtained, special flasks were used to carry out the investing followed by the dewaxing. A sprue was attached to achieve the benefits of the thermoplastic materials. The ‘Thermopress 400’ machine was used for the processing as per the manufacturers recommendations. Polishing was done on only one surface that would act as the denture base area. Each Biodentaplast slice was then used for one media only.
Peek
20 rectangular slices of dimensions 22 mm x 17 mm x 3 mm were first milled in wax. The slices were then placed in a flask and dewaxing was carried out after which they were placed in the Thermopress 400 and processed based on the preset settings. After processing and polishing, each obtained PEEK slice was used for one media.
Wettability and contact angle
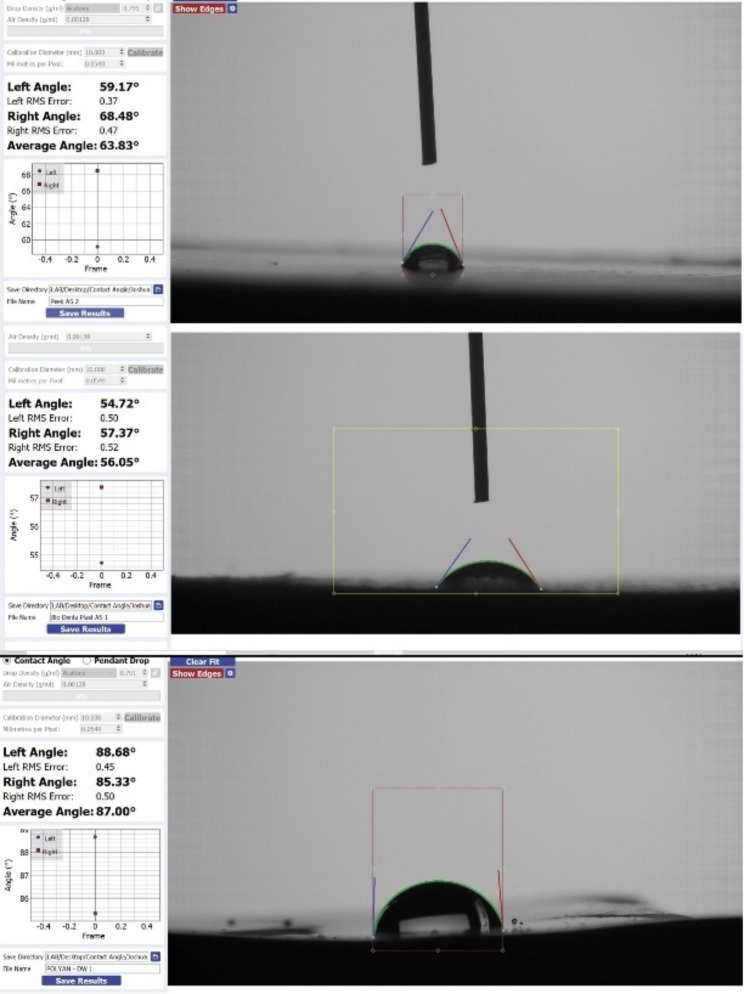
A micropipette was used and a drop of media in a volume of 1.0 L, the sessile drop method was used to calculate the static contact angle. Within 2 s of placing the media on the surface of the specimen, a set of 3 photos was taken, and the contact angle was then determined using the Ossila contact angle goniometer (Fig. 3) and axisymmetric drop shape analysis. Getting a picture of a droplet on a flat surface is the first stage in the measurement. The baseline of the droplet is manually designated at the intersection of the real image and its reflection after the droplet on the flattened specimen has been captured in an image.
Fig. 3.

Ossila Goniometer
The contact angle goniometer software programmatically marks the tracing of the droplet edge and the gradient of the tangent of the droplet edge to the point where it meets the baseline, and then calculates the contact angle between them on the left and right sides of the sample. All of the samples’ contact angles were measured and the baseline of the droplet inside the field of interest was marked by a single operator. The same observer again measured the sessile drop contact angle for all the remaining samples. Care was taken to completely rinse the dispensing syringe with water before adding the fluid that would be analyzed to the specimen.
The groups were divided in the following manner:
Group A
Saliva and Polyan.
Mouth wetting solution and Polyan.
Distilled water and Polyan.
Group B
Saliva and Biodentaplast.
Mouth wetting solution and Biodentaplast.
Distilled water and Biodentaplast.
Group C
Saliva and PEEK.
Mouth wetting solution and PEEK.
Distilled water and PEEK.
To avoid any error, each media was applied thrice on the specimen. In total 9 groups were formed.
Statistical analysis was done using IBM SPSS Software (version 23).
Results
The data was analyzed using One-way ANOVA test and a pairwise comparison using the Post Hoc Tukey’s Honest Significant Difference.
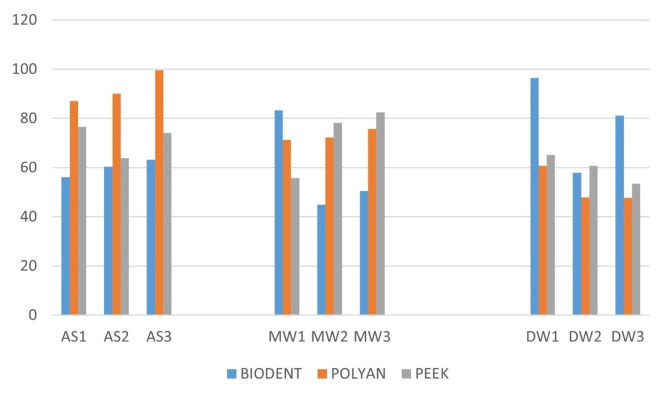
Table 1 depicts the mean contact angles of various denture base materials. In saliva, mouth wetting solution and distilled water, the highest mean and least mean contact angle was seen in Polyan and Biodentaplast respectively.
Table 1.
Mean contact angle of the DBMs in different solutions
| SOLUTION | DBM | Mean | Std. Deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| SALIVA | PEEK | 71.4667 | 6.73914 | 63.83 | 76.58 |
| POLYAN | 92.2133 | 6.61158 | 87.00 | 99.65 | |
| BIODENTAPLAST | 59.8767 | 3.58984 | 56.05 | 63.17 | |
| Total | 74.5189 | 15.06006 | 56.05 | 99.65 | |
| MW | PEEK | 72.1333 | 14.34481 | 55.76 | 82.49 |
| POLYAN | 83.0300 | 2.31715 | 71.25 | 75.65 | |
| BIODENTAPLAST | 59.4967 | 20.74487 | 44.82 | 83.23 | |
| Total | 68.2200 | 14.25932 | 44.82 | 83.23 | |
| DW | PEEK | 59.7433 | 5.87746 | 53.45 | 65.09 |
| POLYAN | 78.510 | 7.47115 | 47.74 | 60.74 | |
| BIODENTAPLAST | 52.113 | 19.41509 | 57.91 | 96.47 | |
| Total | 63.4556 | 15.97578 | 47.74 | 96.47 |
In saliva, a significant difference in the contact angle was seen between the three different materials (p = 0.001). However with respect to distilled water and mouth wetting solution, no significant difference was observed between the three materials (p > 0.05). [Table 2]
Table 2.
Comparison of mean contact angle between the three different DBMs using One way ANOVA test
| SOLUTION | DBM | F | Sig |
|---|---|---|---|
| Saliva |
PEEK POLYAN BIODENTAPLAST |
23.679 | 0.001 |
| MW |
PEEK POLYAN BIODENTAPLAST |
0.804 | 0.491 |
| DW |
PEEK POLYAN BIODENTAPLAST |
3.554 | 0.096 |
Table 3 depicts the pairwise comparisons between the DBMs in saliva. A significant difference was observed between the mean contact angle of PEEK and Polyan, as well as between Polyan and Biodentaplast. However, no significant difference was seen between PEEK and Biodentaplast. Polyan exhibited the highest contact angle followed by PEEK and Biodentaplast (Figs. 4 and 5).
Table 3.
Pairwise comparison of mean contact angle between the DBMs in saliva using Post hoc Tukey’s HSD test
| Medium | (I) DBM | (J) DBM | Mean Difference (I-J) | Std. Error | Sig. |
|---|---|---|---|---|---|
| ARTIFICIAL SALIVA | PEEK | POLYAN | -20.74667* | 4.76133 | 0.011 |
| BIODENTAPLAST | 11.59000 | 4.76133 | 0.111 | ||
| POLYAN | PEEK | 20.74667* | 4.76133 | 0.011 | |
| BIODENTAPLAST | 32.33667* | 4.76133 | 0.001 | ||
| BIODENTAPLAST | PEEK | -11.59000 | 4.76133 | 0.111 | |
| POLYAN | -32.33667* | 4.76133 | 0.001 |
Fig. 4.
Contact angle measured for Polyan, Biodentapalst and PEEK
Fig. 5.
The contact angles for the three materials when tested with Saliva, Mouth wetting solution and distilled water
Discussion
Denture base materials with superior wettability help maintain a moist oral environment, preventing dryness, discomfort, and irritation for the wearer. This is particularly important as dryness can lead to tissue inflammation and oral health issues. On the other hand, poor wettability can result in water droplets forming on the surface, making dentures uncomfortable and potentially affecting speech and mastication [31]. Denture base materials’ performance and patient satisfaction are significantly influenced by the contact angle. The capacity of a material to moisten or spread across a surface is determined by the contact angle. It can also contribute to bacterial colonization, leading to hygiene concerns. Additionally, it may restrict normal speech and mastication, making it difficult for the wearer to properly talk and eat. Materials with favorable wettability characteristics contribute to better patient satisfaction and oral well-being.
The forces required to completely remove the denture from its basal seat are related to denture retention [32]. Wetting of the denture and palate via the respective adhesive forces at the two interfaces is required prior to retention [33]. The retention force, according to Stanitz, is a function of saliva surface tension, liquid film thickness, surface of contact, and liquid-denture contact angle [34].
With the exception of some specific cases, such as perfectly wettable solids, theoretical considerations and experimental results have demonstrated that the contact angle of the advancing liquid front on a dry solid surface (advancing contact angle A) differs from the receding contact angle (R) formed when the liquid recedes on a previously wet surface [35, 36]. In this study, the technique of the goniometer involves the use of the sessile drop. The measurement of the right and left contact angle which then gives an average contact angle measurement [37]. The contact angle which is > 90° leads to the formation of droplets of the liquid over the surface of the denture base material hence rendering it to be hydrophobic. The contact angle when measured to be < 90° causes uniform distribution of the liquid over the surface of the denture base material and that is what leads to increased wettability. This angle is formed is formed at an intersection interface of solid, liquid and gas. With the increase in the wettability; there is an increase in the retention of the denture base to the oral tissues. High contact angles can make the denture base materials reject saliva while allowing water droplets to condense on the surface [37]. This could lead to hygienic problems and intraoral infections by the formation of retention sites for bacteria and debris. Low contact angle materials, on the other hand, encourage uniform moisture dispersion, which can support improved oral hygiene. According to Monsenego et al., in his in vitro study, the most convenient denture base material would be one with the highest contact angle hysteresis, such as a high advancing contact angle and a low receding contact angle [32, 38]. Waters et al. came to the conclusion that higher contact angle hysteresis values of soft-lining denture materials compared to polymethylmethacrylate denture base material indicated that all soft lining materials would improve denture stability under dislodgement forces [39].
In the study conducted, significant difference was only noted in the among the groups when saliva was the liquid in contact. PEEK and Biodentplast showed no significant difference between them whereas there was a difference that was noted among the PEEK and Polyan group and the Biodentaplast and Polyan group. Polyan displayed the highest mean contact angle (92.2133) which signifies an increased contact angle and thus reduced wettability. The specimens of Biodentaplast and PEEK on the other hand displayed a lower mean contact angle when tested with the saliva sample. Biodentaplast was developed as a material to overcome the challenges that were noted by the conventional acrylic resins. A low modulus of elasticity, lack of reactivity to different solutions, good polishability, a proven tensile and mechanical strength, good colour properties and non allergic makes Biodentaplast a suitable option for the cst partial denture framework [40]. Due to its lack of free energy on the surface, it also attracts less bacteria in the oral cavity. It is retentive when used as a framework material and harbours less microorganisms when used as a clasp material. PEEK is a high performance polymer which has been developed to be used as a multipurpose material in dentistry. Its use in esthetic clasp partial dentures has now become popular due to good surface properties, strength and the sufficient esthetic advantage [41–43].
Various surface properties also play a key role in the wettability and contact angle of denture base materials. Factors such as the heterogeneity, polishing properties, roughness, deformation and adherence to other substances are noted to alter the wettability(Bin et al., 2017). The presence of an increased surface energy can result in the quicker formation of a biofilm and a lack of retention. The materials that were selected had similar properties when they were placed in both the solutions. This observation can be correlated from a study conducted by Ramanna [44]. The mouth wetting solutions that are commercially available are of two types: mucin based and carboxymethylcellulose(CMC) based. Studies have gone to show that both these substitutes are effective in cases of dry mouth in denture wearers and reduce discomfort that could be associated(Bin et al., 2017). The contact angle of that of saliva and these substitutes are nearly similar with most materials.
Choosing a denture base material with good wettability can lead to an increase in the comfort to the tissues and oral health, good aesthetics, better masticatory performance, and longevity. The increased wettability makes it less susceptible to contamination and degradation over the long run.
The limitations of the study include the use of only a certain materials and not all the materials that could be incorporated as cast partial denture framework materials. The use of only a CMC solution and not a mucin based one could also lead to certain changes. More clinical trials are required for the same.
Conclusion
From the resources and the materials at our disposal, it could be concluded that Polyan, Biodentaplast and PEEK and could be used as viable options in cast partial denture framework. PEEK and biodnetpalast showed almost similar readings compared to Polyan which showed lesser properties compared to the other two materials and a significant difference was noted in saliva and mouth wetting solutions. Hence the null hypothesis was rejected. Although more research and clinical trials are needed to prove the same.
Acknowledgements
The authors thank the Director of Academics at Saveetha Dental College for encouraging them to pursue research, as well as the university’s Chancellor and Dean of the Dental College for their invaluable assistance.
List of abbreviations
- DW
Distilled water
- MW
Mouth wetting solution
- PEEK
Polyether ether ketone
Authors’ contributions
Conceptualization JN; NA; methodology, JN; NA; GRJ; software, JN; and NA; formal analysis, JN and NA.; investigation, JN; and NA; data curation, JN; and NA; writing—original draft preparation, YS, MMM; M.C.; G.M. and VR; writing—review and editing, MM; MC.; G.M.; supervision, GM; funding acquisition, YS; administration: YS. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability
The data will be available on reasonable request from the corresponding author.
Declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the Institute, Saveetha Dental College And Hospitals [Protocol number: SRB/SDC/PROSTHO-2102/22/105; Date: 09/08/2022]. The study protocol was developed, and all subjects gave their written informed consent for inclusion before they participated in the study.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nabeel Ahmed, Email: nabeel.5610@gmail.com.
Yuliia Siurkel, Email: yuliasiurkel@ieu.edu.ua.
Giuseppe Minervini, Email: giuseppe.minervini@unicampania.it.
References
- 1.Cooper LF. The current and future treatment of Edentulism. J Prosthodont. 2009;18:116–22. doi: 10.1111/j.1532-849X.2009.00441.x. [DOI] [PubMed] [Google Scholar]
- 2.Steele JG, Treasure ET, O’Sullivan I, Morris J, Murray JJ. Adult Dental Health Survey 2009: transformations in British oral health 1968–2009. Br Dent J. 2012;213:523–7. doi: 10.1038/sj.bdj.2012.1067. [DOI] [PubMed] [Google Scholar]
- 3.Abt E, Carr AB, Worthington HV. Interventions for replacing missing teeth: partially absent dentition. Cochrane Database of Systematic Reviews. 2019 doi: 10.1002/14651858.CD003814.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Venkatesh KV, Nandini VV. Direct metal laser sintering: a Digitised Metal Casting Technology. J Indian Prosthodontic Soc. 2013;13:389–92. doi: 10.1007/s13191-013-0256-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arafa KAO. Assessment of the fit of removable partial denture fabricated by computer-aided designing/computer aided manufacturing technology. Saudi Med J. 2018;39:17–22. doi: 10.15537/smj.2018.1.20796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar P, Vadavadagi SV, Lahari M, Shetty N, Deb S, Dandekeri S. Evaluation of Wettability of three saliva substitutes on heat-polymerized Acrylic Resin-An in vitro study. J Contemp Dent Pract. 2019;20:557–60. doi: 10.5005/jp-journals-10024-2557. [DOI] [PubMed] [Google Scholar]
- 7.Lo Russo L, Guida L, Mariani P, Ronsivalle V, Gallo C, Cicciù M, et al. Effect of Fabrication Technology on the Accuracy of Surgical guides for Dental-Implant Surgery. Bioengineering. 2023;10:875. doi: 10.3390/bioengineering10070875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Douglas WH, Bates JF. The determination of residual monomer in polymethylmethacrylate denture-base resins. J Mater Sci. 1978;13:2600–4. doi: 10.1007/BF02402746. [DOI] [Google Scholar]
- 9.Vilaplana J, Romaguera C, Cornellana F. Contact dermatitis and adverse oral mucous membrane reactions related to the use of dental prostheses. Contact Dermat. 1994;30:80–4. doi: 10.1111/j.1600-0536.1994.tb00568.x. [DOI] [PubMed] [Google Scholar]
- 10.Price CA. A history of dental polymers. Aust Prosthodont J. 1994;8:47–54. [PubMed] [Google Scholar]
- 11.Pfeiffer P, Rosenbauer E-U. Residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J Prosthet Dent. 2004;92:72–8. doi: 10.1016/j.prosdent.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Soegiantho P, Suryawinata PG, Tran W, Kujan O, Koyi B, Khzam N, et al. Survival of single immediate implants and reasons for loss: a systematic review. Prosthesis. 2023;5(2):378–424.
- 13.Kazakova R, Tomov G, Vlahova A, Zlatev S, Dimitrova M, Kazakov S, et al. Assessment of Healing after Diode Laser Gingivectomy prior to prosthetic procedures. Appl Sci. 2023;13:5527. doi: 10.3390/app13095527. [DOI] [Google Scholar]
- 14.Yokoyama M, Shiga H, Ogura S, Sano M, Komino M, Takamori H, et al. Functional differences between chewing sides of implant-supported denture wearers. Prosthesis. 2023;5(2):346–57.
- 15.Vozzo LM, Azevedo L, Fernandes JCH, Fonseca P, Araújo F, Teixeira W, et al. The success and complications of complete-arch implant-supported fixed monolithic zirconia restorations: a systematic review. Prosthesis. 2023;5(2):425–36.
- 16.Chhikara K, Gupta S, Bose D, Kataria C, Chanda A. Development and trial of a multipurpose customized orthosis for activities of daily living in patients with spinal cord injury. Prosthesis. 2023;5(2):467–79.
- 17.Rosa A, Miranda M, Franco R, Guarino MG, Barlattani A, Bollero P. Experimental protocol of dental procedures in patients with hereditary angioedema: The role of anxiety and the use of nitrogen oxide. Oral Implantol (Rome). 2016;9:49–53. 10.11138/orl/2016.9.2.049. [DOI] [PMC free article] [PubMed]
- 18.Patil P, Madhav VNV, Alshadidi AAF, Saini RS, Aldosari LIN, Heboyan A, et al. Comparative evaluation of open tray impression technique: investigating the precision of four splinting materials in multiple implants. BMC Oral Health. 2023;23:844. doi: 10.1186/s12903-023-03583-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heboyan A, Bennardo F. New biomaterials for modern dentistry. BMC Oral Health. 2023;23:817. doi: 10.1186/s12903-023-03531-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hasanzade M, Zabandan D, Mosaddad SA, Habibzadeh S. Comparison of marginal and internal adaptation of provisional polymethyl methacrylate restorations fabricated by two three-dimensional printers: an in vitro study. Dent Res J (Isfahan) 2023;20:87. doi: 10.4103/1735-3327.384358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mosaddad SA, Talebi S, Hemmat M, Karimi M, Jahangirnia A, Alam M et al. Oral complications associated with the piercing of oral and perioral tissues and the corresponding degree of awareness among public and professionals: a systematic review. Diagnostics (Basel). 2023;13. [DOI] [PMC free article] [PubMed]
- 22.Mosaddad SA, Abduo J, Zakizade M, Tebyaniyan H, Hussain A. The Effect of various lasers on the bond strength between Orthodontic brackets and Dental ceramics: a systematic review and Meta-analysis. Photobiomodul Photomed Laser Surg. 2023 doi: 10.1089/photob.2023.0098. [DOI] [PubMed] [Google Scholar]
- 23.Taghva M, Mosaddad SA, Ansarifard E, Sadeghi M. Could various angulated implant depths affect the positional accuracy of digital impressions? An in vitro study. J Prosthodont. 2023 doi: 10.1111/jopr.13764. [DOI] [PubMed] [Google Scholar]
- 24.Turner JW, Radford DR, Sherriff M. Flexural properties and Surface Finishing of Acetal Resin Denture Clasps. J Prosthodont. 1999;8:188–95. doi: 10.1111/j.1532-849X.1999.tb00034.x. [DOI] [PubMed] [Google Scholar]
- 25.Fitton JS, Davies EH, Howlett JA, Pearson GJ. The physical properties of a polyacetal denture resin. Clin Mater. 1994;17:125–9. doi: 10.1016/0267-6605(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 26.Salamone JC. Polymeric materials encyclopedia. CRC Press; 2020.
- 27.Schwitalla AD, Spintig T, Kallage I, Müller W-D. Flexural behavior of PEEK materials for dental application. Dent Mater. 2015;31:1377–84. doi: 10.1016/j.dental.2015.08.151. [DOI] [PubMed] [Google Scholar]
- 28.Najeeb S, Zafar MS, Khurshid Z, Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J Prosthodont Res. 2016;60:12–9. doi: 10.1016/j.jpor.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 29.Minervini, G.; Franco, R.; Marrapodi, M.M.; Di Blasio, M.; Ronsivalle, V.; Cicciù, M. Children Oral health and parents education status: a cross sectional study. BMC Oral Health. 2023;23:787. 10.1186/s12903-023-03424-x. [DOI] [PMC free article] [PubMed]
- 30.Reddy LKV, Madithati P, Narapureddy BR, Ravula SR, Vaddamanu SK, Alhamoudi FH, et al. Perception about health applications (apps) in smartphones towards Telemedicine during COVID-19: a cross-sectional study. J Pers Med. 2022;12:1920. doi: 10.3390/jpm12111920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bin AH, Reddy V, Kumar P, Raj J, Babu SS. Evaluation of wetting ability of five new saliva substitutes on heat-polymerized acrylic resin for retention of complete dentures in dry mouth patients: a comparative study. Pan Afr Med J. 2017;27. [DOI] [PMC free article] [PubMed]
- 32.Monsénégo P, Proust J. Complete denture retention. Part I: physical analysis of the mechanism. Hysteresis of the solid-liquid contact angle. J Prosthet Dent. 1989;62:189–96. doi: 10.1016/0022-3913(89)90312-0. [DOI] [PubMed] [Google Scholar]
- 33.Murray MD. Physical aspects of complete denture retention. The University of Hong Kong; 1989.
- 34.Lindstrom RE, Pawelchak J, Heyd A, Tarbet WJ. Physical-chemical aspects of denture retention and stability: a review of the literature. J Prosthet Dent. 1979;42:371–5. doi: 10.1016/0022-3913(79)90134-3. [DOI] [PubMed] [Google Scholar]
- 35.Escobar JV, Castillo R. Force of Adhesion upon loss of Contact Angle Hysteresis: when a Liquid behaves like a solid. Phys Rev Lett. 2013;111:226102. doi: 10.1103/PhysRevLett.111.226102. [DOI] [PubMed] [Google Scholar]
- 36.Wang YJ, Guo S, Chen H-Y, Tong P. Understanding contact angle hysteresis on an ambient solid surface. Phys Rev E. 2016;93:052802. doi: 10.1103/PhysRevE.93.052802. [DOI] [PubMed] [Google Scholar]
- 37.Srinivas KGSJS. Estimation of wettability of topical fluoride gel on anterior and posterior teeth: an in vitro study. J Adv Pharm Technol Res. 2022;13:462–5. doi: 10.4103/japtr.japtr_262_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Franco R, Miranda M, Di Renzo L, De Lorenzo A, Barlattani A, Bollero P. Glanzmann’s thrombastenia: the role of tranexamic acid in oral surgery. Case Rep Dent. 2018;2018:1–4. 10.1155/2018/9370212. [DOI] [PMC free article] [PubMed]
- 39.Waters MGJ, Jagger RG, Jerolimov V, Williams KR. Wettability of denture soft-lining materials. J Prosthet Dent. 1995;74:644–6. doi: 10.1016/S0022-3913(05)80318-X. [DOI] [PubMed] [Google Scholar]
- 40.Thomas S, Nandini V. Acetal resin - a quantum leap in aesthetic restorative dentistry: a review. 2012;2.
- 41.Bathala L, Majeti V, Rachuri N, Singh N, Gedela S. The role of Polyether Ether Ketone (Peek) in Dentistry – A Review. J Med Life. 2019;12:5–9. doi: 10.25122/jml-2019-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minervini G, Franco R, Marrapodi MM, Fiorillo L, Cervino G, Cicciù M. The association between parent education level, oral health, and oral-related sleep disturbance. An observational crosssectional study. Eur J Paediatr Dent. 2023;24:218–23. 10.23804/ejpd.2023.1910. [DOI] [PubMed]
- 43.Uzunçıbuk H, Marrapodi MM, Meto A, Ronsivalle V, Cicciù M, Minervini G. Prevalence of temporomandibular disorders in clear aligner patients using orthodontic intermaxillary elastics assessed with diagnostic criteria for temporomandibular disorders (DC/TMD) Axis II evaluation: a cross-sectional study. J Oral Rehabil. 2024;51:500–09. 10.1111/joor.13614. [DOI] [PubMed]
- 44.Ramanna P. Wettability of three denture base materials to human saliva, saliva substitute, and distilled water: a comparative in vitro study. J Indian Prosthodontic Soc. 2018;18:248. doi: 10.4103/jips.jips_301_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data will be available on reasonable request from the corresponding author.