Abstract
Background:
Cervical cancer is a leading cause of cancer-associated mortality among women in India, with 96,922 new cases and 60,078 deaths each year, almost one-fifth of the global burden. In 2018, Sikkim state in India introduced human papillomavirus (HPV) vaccine for 9–13-year-old girls, primarily through school-based vaccination, targeting approximately 25,000 girls. We documented the program’s decision-making and implementation processes.
Methods:
We conducted a post-introduction evaluation in 2019, concurrent with the second dose campaign, by interviewing key stakeholders (state, district, and local level), reviewing planning documents, and observing cold chain sites in two purposefully-sampled community areas in each of the four districts of Sikkim. Using standard questionnaires, we interviewed health and education officials, school personnel, health workers, community leaders, and age-eligible girls on program decision-making, planning, training, vaccine delivery, logistics, and communication.
Results:
We conducted 279 interviews and 29 observations in eight community areas across four districts of Sikkim. Based on reported administrative data, Sikkim achieved >95% HPV vaccination coverage among targeted girls for both doses via two campaigns; no severe adverse events were reported. HPV vaccination was well accepted by all stakeholders; minimal refusal was reported. Factors identified for successful vaccine introduction included strong political commitment, statewide mandatory school enrollment, collaboration between health and education departments at all levels, and robust social mobilization strategies.
Conclusions:
Sikkim successfully introduced the HPV vaccine to multiple-age cohorts of girls via school-based vaccination, demonstrating a model that could be replicated in other regions in India or similar low- and middle-income country settings.
Keywords: HPV vaccine, Cervical cancer, Vaccine introduction, School-based vaccination, Sikkim
1. Background
Cervical cancer is the second most common type of cancer among women in India, with an estimated 96,922 new cases and 60,078 deaths each year, accounting for almost one-fifth of the global burden of cervical cancer and approximately 6–29% of all cancers among women in India [1–3]. The World Health Organization (WHO) recommends a comprehensive approach to prevent and control cervical cancer, including vaccination, screening for precancerous lesions, treatment, and palliative care, as indicated. For primary prevention, two doses of human papillomavirus (HPV) vaccination of girls aged 9–14 years, separated by a minimum of six months, is recommended [4–6].
Sikkim state is a northeastern state in India, bordering Nepal, Bhutan, and China, with a total population of less than one million people. Cervical cancer cases represent 10% of the total number of cancer cases among women in Sikkim [7]. To address cervical cancer burden, the Government of Sikkim took a landmark decision to be the first state in India to introduce HPV vaccine to all girls aged 9–13 years, via a statewide multiple-age cohort, school-based vaccination delivery strategy. To determine the most appropriate strategies for vaccine delivery and social mobilization, Sikkim utilized the compilation of lessons learned from prior pilot HPV vaccine introductions in Punjab and Delhi in India, as well as the nationwide introduction in neighboring Bhutan, and applied these to the state-specific context [8–10].
In July 2018 and April 2019, Sikkim conducted vaccination campaigns to deliver the first and second doses of the HPV vaccine, respectively, to girls aged 9–13 years [9]. The total target population for vaccination included almost 25,000 girls across five age cohorts in all four districts; Sikkim planned vaccination in >1000 primary and secondary schools (government and private sector). Age-eligible girls not attending school were encouraged to be vaccinated at schools or health facilities, using community linkages for social mobilization.
WHO recommends conducting a post-introduction evaluation 6–12 months following a new vaccine introduction to highlight best practices, identify challenges, and implement timely program improvements [11,12]. Because the target age group for HPV vaccine does not routinely access health services in many low- and middle-income countries, conducting a post-introduction evaluation of an HPV vaccine introduction allows for exploring the feasibility of vaccine delivery in a non-healthcare setting (i.e., schools), understanding community perceptions regarding this new vaccine, as well as understanding the impact of this vaccine introduction on the local health system [13,14].
Following the HPV vaccine introduction in Sikkim state, the state government requested WHO-India Country Office, in collaboration with the Ministry of Health and Family Welfare and international partners, to conduct a post-introduction evaluation in May 2019, with the primary objective of documenting the HPV vaccine introduction activities (i.e., decision-making, planning and implementation) in selected locations to inform future programmatic decision-making in Sikkim, as well as other parts of India planning to introduce the HPV vaccine. In this report, we describe HPV vaccine introduction and implementation in Sikkim state and share collective findings from the post-introduction evaluation.
2. Methods
We collected and collated information regarding decision-making, planning, and implementation of HPV vaccine introduction through the post-introduction evaluation. In consultation with state health officials, we adapted the WHO New Vaccine Post-Introduction Evaluation standardized methodology and data collection tools to meet the Sikkim state context, and we used these materials to systematically collect data in the field [12].
2.1. Sampling
The evaluation included all four districts of Sikkim state (Fig. 1). We purposefully-sampled two health facilities and two schools in each district to include one high- and one low-performing health center (as determined by routine infant immunization coverage) in each district and different types of schools (i.e. government/public and private schools) to gather a broad perspective on HPV vaccine implementation (Fig. 2)[15]. We interviewed personnel from the state and district health and education offices, as well as health workers and community stakeholders at each health facility catchment area. Health workers responsible for conducting vaccination clinics at the health facility were interviewed and community stakeholders (including school heads and teachers, religious leaders, community health workers, and age-eligible girls) were identified by convenience sampling. Additionally, we observed cold chain facilities at state-, district-, and health facility-level, as well as the waste management at health facilities.
Fig. 1.
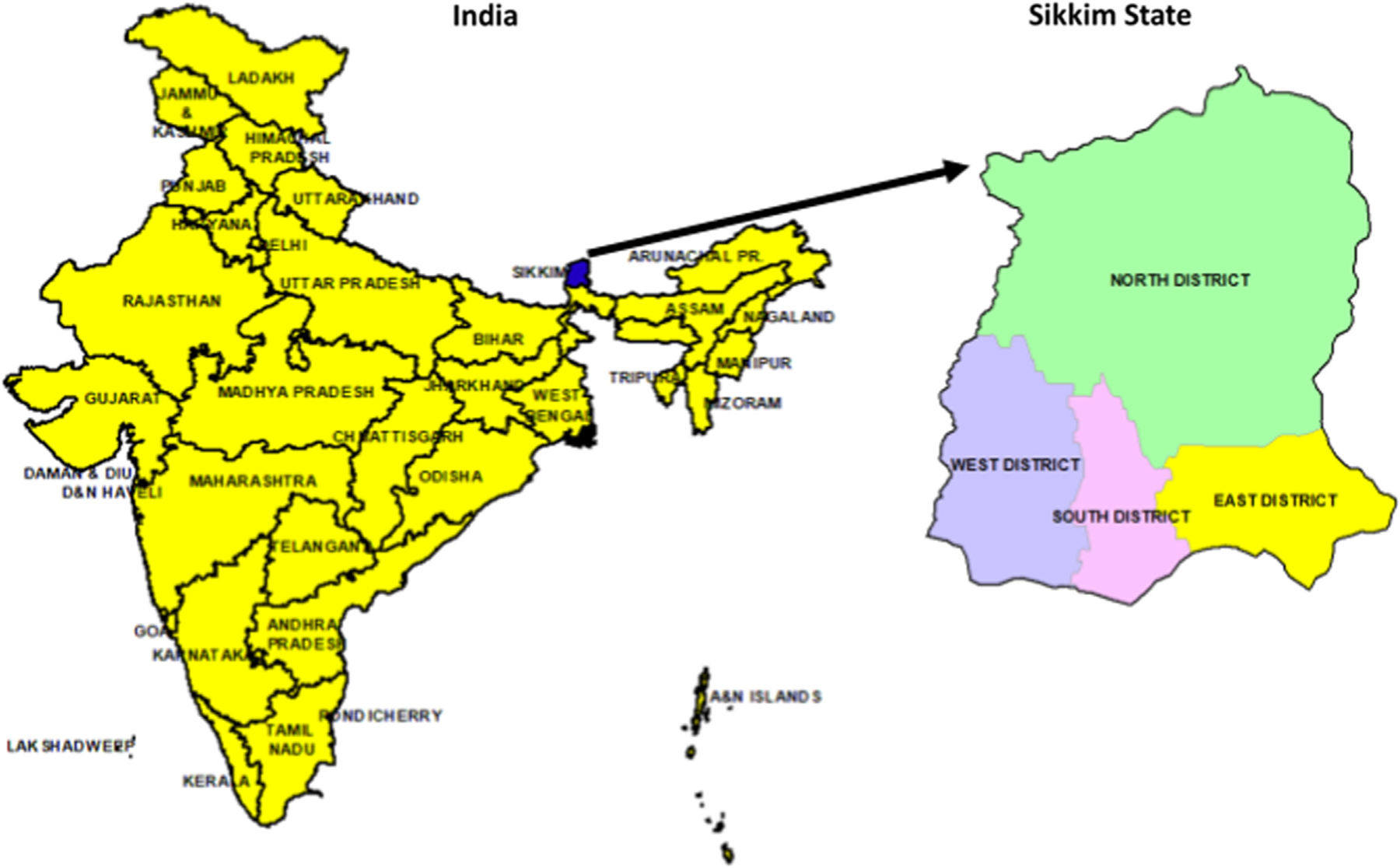
Map of Sikkim State in India–2019.
Fig. 2.

Sampling approach for the HPV vaccine post-introduction evaluation including sectors and areas visited at the state and district levels in Sikkim State, India–2019.
2.2. Data collection
Data collection consisted of three primary components: (1) interviews with key stakeholders, (2) desk review of planning documents, and (3) observation of cold chain and waste management facilities. We interviewed the health and education officials at the state and district levels, health care workers, teachers and school heads, community leaders, and age-eligible girls in the target population. We used standard interview guides, adapted to the Sikkim state context, which included questions across the following main thematic areas: decision-making, introduction planning and coordination, training, vaccine delivery and coverage, recording and reporting, cold chain and vaccine logistics, monitoring, waste management, injection safety, advocacy, communication, and attitudes and perception among age-eligible girls. Interview questions were written in English; interviews were conducted in English or the local language by a trained data collector. We conducted desk reviews of HPV vaccine introduction planning and monitoring documents at the state and district public health office, including policy documents, operational guidelines, training materials, data recording and reporting sheets, and communication materials. Administrative coverage data was obtained from the reporting sheets at district-level. We observed the vaccine cold chain equipment, dry storage areas, and waste management facilities, using a structured checklist.
2.3. Data analysis
We entered interview responses and observational data into an Excel spreadsheet and completed a descriptive analysis. The district-level evaluation teams collated their impressions from interviews, desk reviews, and observations to generate synthesized findings, by thematic area, at the district level. The state-level study team collated all impressions and data from the four district-level teams to generate state-level impressions. Discrepancies in impressions collected within the district and state level teams were resolved through discussion and consensus.
3. Results
We conducted a total of 279 interviews and 29 observations at the state level, across four districts, in eight purposefully-sampled community areas (Table 1).
Table 1.
Total stakeholder interviews and observations conducted for the HPV post-introduction evaluation in Sikkim State, India–2019.
| Stakeholder Category | Number interviewed | Number observed |
|---|---|---|
| State Health Office | 1 | |
| State Education Office | 1 | |
| District Health Office | 4 | |
| District Education Office | 4 | |
| Health Workers | 24 | |
| Teachers | 25 | |
| Community Leaders | 21 | |
| Age-eligible girls | 199 | |
| Cold Chain Points | 17 | |
| Health Facilities: Waste Management | 12 | |
| Total | 279 | 29 |
Synthesized findings on HPV vaccine program decision-making, planning, and implementation across each main area are described below.
3.1. Decision-making, introduction planning, and coordination
Decision-making on HPV vaccine introduction in Sikkim state was largely driven by the evidence of high cervical cancer burden in India and Sikkim, coupled with WHO recommendations for primary cervical cancer prevention through HPV vaccination [1–3]. The Sikkim State Technical Advisory Group for Immunization (STAG), an independent group of experts advising the state on immunization policy, recommended HPV vaccine introduction in Sikkim to 9–13-year-old girls, based on 2014 WHO recommendations [16]. State political leaders prioritized HPV vaccine introduction, allocating state government budget to procure vaccine from the manufacturer directly. The Government of Sikkim identified financial resources for procurement of HPV vaccine and completed desired approval processes; vaccine procurement was done for both doses with provisions to sustain the program longer-term. Procurement was completed through UNICEF Supply Division in Copenhagen; the UNICEF-India Country Office facilitated required coordination.
The STAG selected a primarily school-based vaccine delivery strategy because of Sikkim’s mandatory school enrollment policy for children less than 14 years of age and resulting high rates of primary and secondary school enrollment, as well as prior experience vaccinating children in schools through the state’s existing school health program [17].
The state health department led the HPV vaccine introduction planning, in partnership with WHO-India, and developed an operational plan, which included clear policies on the target age eligibility, vaccine implementation plan, training strategy for health workers and school personnel, and community social mobilization plans. Recently developed micro-planning tools and social mobilization materials, along with operational funds, were distributed to districts and local levels before the vaccination launch.
The state health department coordinated planning and implementation with the state and district education offices to ensure ownership from the education sector and school preparedness. The education departments at state and district-levels supported schools to identify nodal (focal) teachers to lead preparations for HPV vaccine delivery at their school. Districts coordinated all preparatory activities with the school health coordinators and nodal teachers at each school, using WhatsApp with staff from health facility catchment areas and districts and HPV vaccine coordination group conference calls. Health officials used routine task force meetings at district and community block levels as mechanisms to coordinate with the education department.
Microplanning was conducted at the health facility and school levels, primarily by teachers and health facility staff, to identify and enumerate all in-school and out-of-school girls within the catchment area. Health facilities communicated vaccine supply needs to the district health departments, who subsequently communicated supply needs to the state health department. Standardized forms were developed to enumerate the age-eligible target population, record the number of the HPV vaccine doses administered, and report these data up to district and state level.
3.2. Training
Comprehensive training materials (e.g., Operational Guidelines, Frequently Asked Questions-FAQs for healthcare workers, teachers’ handbooks, and leaflets for community health workers) were developed through a partnership between the state immunization program and WHO-India (Fig. 3).
Fig. 3.

Examples of training and advocacy materials developed for the HPV vaccine introduction in Sikkim State, India–2018.
All four districts in Sikkim State conducted training workshops at district and community levels that targeted various stakeholders (e.g., public health, education, political leaders, non-governmental organizations, and religious leaders). Cascaded trainings were conducted for health workers, nodal teachers, and community health workers at district and community levels. In total, over 100 trainings on HPV vaccine introduction were conducted across Sikkim State reaching >3000 participants. Trainings included the following key components: burden of cervical cancer, benefits of the HPV vaccine, correct vaccine administration/technique, proper storage practices, adverse events following immunization (AEFI), recording, reporting, and monitoring of uptake of the HPV vaccine. Trainings consisted of slide presentations, print materials, and discussions. Subsequently, health workers and teachers received slide decks and print materials to conduct cascaded trainings in their respective health facilities and schools.
Of the 24 health workers interviewed, 96% were trained on the HPV vaccine; 92% reported being satisfied with the training they received. Almost all health workers (96%) reported receiving print materials on the HPV vaccine to help respond to inquiries from parents and community members. All health workers interviewed demonstrated a good knowledge of the HPV vaccine schedule and correct vaccine administration techniques, including vaccination site isolation and post-vaccination observation time. All 25 nodal teachers interviewed across four districts stated that they received training on the HPV vaccine; 96% received written materials about the HPV vaccine implementation.
The evaluation team noted some important gaps in training. Trainings were conducted consistently before the delivery of the first dose of HPV vaccine (July 2018) in all four districts of Sikkim State; however, refresher trainings before the delivery of the second dose of HPV vaccine (April 2019) were inconsistent at district and sub-district levels. District officials from one district identified a need for refresher training of health workers, particularly on identifying adverse events following immunization (AEFI). In one health facility, nurses demonstrated knowledge gaps in forecasting vaccine supply requirements and calculating vaccine wastage rates for all routine vaccines. At schools, nodal teachers did not train all teachers equally at each school; therefore, a knowledge transfer gap was noted if a teacher moved out or was absent on vaccination days. The team observed that only nodal teachers were able to correctly answer the HPV vaccine knowledge questions or respond to inquiries about vaccine implementation. Teachers and community leaders expressed a need for additional training to address questions and concerns from caregivers and other community members about HPV vaccine safety.
3.3. Advocacy, communication, and social mobilization
The evaluation team found high acceptance and demand for the HPV vaccine among stakeholders across health and education sectors at all levels. Comprehensive communication materials (teacher guidebooks, FAQs, leaflets, banners, and posters) were developed by the state government with support from development partners (Fig. 3); all materials were field-tested. We noted that materials were visibly displayed in all areas visited during the post-introduction evaluation. Following health worker and nodal teacher trainings, all schools conducted parent-teacher meetings and community sensitization meetings together with health workers to raise awareness about the HPV vaccination campaign and address any questions.
Intense advocacy efforts were undertaken to sensitize technical stakeholders, such as the government, state and district officials, private pediatricians, local political leaders, and community leaders, using one-on-one meetings, sensitization workshops, and cascade trainings. This ensured uniformity of messages disseminated among key stakeholders, who further acted as advocates for the HPV vaccine in their communities. State public health officials held sensitization workshops with the representatives of major radio and print media outlets. Launching ceremonies were conducted at state and district levels—in several communities, with the presence of prominent political and community influencers. The State Chief Minister led these ceremonies during the state launch; high media coverage of these launching ceremonies was ensured for maximum dissemination of campaign messages to the community. At the local level, school rallies, drawing competitions, and mikings (community announcements by megaphone or microphone) were conducted in the local language to permeate campaign messages to the community. A promotional documentary video about the HPV vaccine introduction in Sikkim was developed by the state government, following the first HPV vaccination round. This video aimed to build confidence among community members and showcase this landmark initiative.
Among 24 health workers interviewed, 22 (92%) reported that they did not encounter vaccine hesitancy or refusal from caregivers or girls. Of the 199 girls interviewed, 157 (79%) correctly identified the benefits of the HPV vaccine. To avoid the potential spreading of misinformation and reduced demand for the HPV vaccine, the Sikkim state health department established mechanisms to identify rumors, misinformation, and clusters of lack of vaccine acceptance through frequent communication with the district and sub-district levels. A State Government plan for proactive response to misinformation, rumors, or community concerns about the HPV vaccine that arose before and during the campaign was developed before starting the HPV vaccine campaign. A state-level crisis communication spokesperson was designated to respond to any media inquiry during the HPV vaccination campaigns. Stakeholders interviewed reported that high levels of community literacy could also have contributed to widespread acceptance of the HPV vaccine.
The evaluation team noted a few gaps in communication planning as follows. Districts and health centers did not have a structured crisis communication plan, and no tailored messaging was provided to the health workers or school staff to counter misinformation, rumors, or lack of vaccine acceptance. Caregiver leaflets (Fig. 3) were only available in English. While many residents of Sikkim speak English and literacy is high, community members suggested that the back of the leaflet be translated to Nepali for future HPV vaccination campaigns.
3.4. Vaccine delivery and coverage
School-based vaccination sessions were conducted in the first week of the vaccination campaign each year, followed by health facility vaccination conducted during the second and third weeks throughout the state. Health facility staff mobilized to schools to deliver the vaccines during the school campaigns. Eligible girls who missed the vaccination day in schools were mobilized to receive the vaccine at the nearby health facilities. A total of 2081 vaccination sessions were conducted in schools across the two vaccination campaigns (1123 and 958 schools, respectively). Additional vaccination sessions were conducted in 29 health facilities during both campaigns.
Most schools followed the state policy of implied consent for routine vaccination; 38 (3%) schools in the first campaign and 34 (4%) schools in the second campaign sought written consent from parents, the majority of which were private schools.
To record administered vaccines and identify the girls vaccinated, vaccination teams provided new vaccination cards (home-based records) and marked girls’ fingers. Daily reporting of administrative coverage on standard forms occurred from the health facility level up to the district and state levels during both campaign rounds. Paper-based records of vaccine coverage were maintained at health facility, district and state health department levels. Health workers prepared paper-based coverage reports at the end of each vaccination session, which were compiled at sub-district planning units, and finally at district level. Districts prepared reports in electronic (Excel) format and shared with the state, where reports from all districts were consolidated. Electronic reporting from subdistrict levels could not be implemented, due to limitations of internet connectivity. As HPV vaccination in Sikkim was a state initiative, reporting was not included in the national electronic reporting system. WHO teams provided technical assistance to the state government to analyze reports.
Among health workers surveyed, 91% reported no challenges in recording vaccination sessions and calculating health facility level vaccination coverage.
Based on reported administrative coverage data, Sikkim State achieved a high two-dose vaccination coverage for the HPV vaccine, primarily using a school-based delivery platform; >95% coverage was achieved for the first dose, and >90% coverage was achieved for the second dose in each district (Fig. 4).
Fig. 4.

District-level HPV vaccination coverage for the first (HPV1) and second (HPV2) HPV vaccine doses in Sikkim state, India—(2018–2019).
All interviewed stakeholders attributed the high HPV vaccination coverage to the strong partnership between health and education sectors and mandatory school enrollment policy for children less than 14 years of age, which led to most age-eligible girls being enrolled in school.
Health workers and public health officials in all districts made extensive efforts to ensure that girls who received the first HPV vaccine dose received the second dose and to minimize drop-out. Individual vaccination record cards were kept at the schools after the first dose to facilitate tracking and monitoring of the target population for the second dose. To track girls that moved after the first dose, health workers and public health officials communicated through social media channels and made repeated phone calls to caregivers. Health workers maintained lists of girls who missed first or second dose HPV vaccination at the school and mobilized them to the nearest health facility.
However, the evaluation team identified some missed opportunities for vaccination. Girls vaccinated during the first dose campaign became the target population for the second dose campaign; thus, girls who missed vaccination during the first round were not permitted to receive the HPV vaccine during the second round. As per operational guidelines, birthdate cut-offs for both doses were followed strictly; therefore, girls even a day older than the eligible age were refused vaccination. Girls were required to show proof of age (e.g., birth certificate) before vaccination; although extensive efforts were made to obtain records, some girls were refused vaccination if no birthdate documentation was found. In some cases, if it was understood that girls would not be in the state for the second dose, they were denied the first dose of the HPV vaccine. School staff interviewed stated that tracking girls for both doses across two academic years proved challenging because some girls moved out of state or left school after the academic year. Keeping individual vaccination record cards at schools helped to track the target population for the second dose of the HPV vaccine. However, some families moved to other areas in Sikkim State after the first dose of the HPV vaccine and found it difficult to obtain the second dose of the HPV vaccine in the new location without proof that they received the first dose of the vaccine. Finally, enumeration and verification of tracking out-of-school girls at sub-district levels were lacking.
3.5. Vaccine management, cold-chain, transport, injection safety, and waste management
In total, the evaluation team observed 17 cold chain points and dry storage areas. All cold chain storage units were noted to be clean and functioning, including internal thermometers, and good cold chain practices were observed at all sites visited. Syringes were stored optimally in a clean, dry, and organized manner at all cold chain points. The evaluation team did not observe any expired or unusable vaccine, and none was reported. Vaccine fridge temperatures were recorded twice daily in temperature log-books, including weekends and holidays. Job aids for vaccine management and storage were visibly displayed at all cold chain points. There were no reported stock-outs of the HPV vaccine or syringes during the delivery of the first or second dose of the vaccine.
To accommodate cold storage of a large amount of the HPV vaccine, the state proactively purchased a new walk-in cooler for the state. The Government of India supplied new cold chain equipment for the district and sub-district levels (i.e., ice-lined refrigerators, deep freezers, portable cold boxes). This new cold chain equipment accommodated the state’s HPV vaccine supply and helped strengthen the state’s overall cold chain system. These efforts to expand Sikkim’s cold chain capacity better prepared the state for the subsequent measles-rubella vaccination campaign and rotavirus vaccine introduction.
Vaccines from the state cold storage were transported to the districts before the campaign in a temperature-controlled vaccine truck; vaccine distribution from the district to the last cold chain points was completed within two days of vaccine receipt to maintain vaccine quality. At the end of each day that vaccine was offered, all used and unused HPV vaccine vials were returned to the sub-district cold chain point, stored, or disposed of as per standard protocols. Following the first HPV vaccination campaign, unused vaccines were returned to the district and from the district to the state; these vaccines were reissued for the second campaign, using a “first-in, first-out” standard procedure at all cold chain points. The evaluation team identified a few challenges with vaccine management, including the lack of cold chain handlers at all cold chain points, power outages in some remote areas without back-up generators present, and the lack of transport to hard-to-reach areas.
Negligible vaccine wastage occurred with this single-dose vial vaccine during the first and second campaigns (13(<0.05%)/24,459 vials and 6 (<0.05%)/27,498 vials, respectively). Overall strong injection safety practices and correct vaccine administration techniques were observed in all health facilities; a few errors in techniques (e.g., injection angle, recapping needles) were observed during campaign monitoring by supervisors, and those errors were immediately corrected.
Correct waste management protocols were in place. However, in some communities, the evaluation team observed some gaps, such as waste disposal pits not being compliant with regulations (i.e. open with no lid and in poor condition), lacking waste disposal pits in some health facilities, and some health facilities dumping biohazard waste in the open.
3.6. Adverse events following immunization (AEFI)
A state-level AEFI policy for all vaccines was in place. There were AEFI committees at the state and district levels, as per state guidelines; however, district-level AEFI committees were not active and member lists were not updated. All districts and community areas reported that medical officers and health workers were oriented on AEFIs during the HPV vaccine trainings. Health facilities reported that anaphylaxis kits were present at each vaccination session site, and AEFI kits were observed at all health centers visited by the evaluation team. AEFI registers were properly maintained; the study team observed good records and AEFI monitoring practices in almost all (81%) sites visited. School vehicles and/or ambulances were kept on standby in most communities during the campaign for transporting any serious or severe AEFI cases. The WHO-recommended three-room vaccination delivery strategy was strictly followed in all districts. Girls were engaged in recreational activities (e.g., singing, watching movies) at schools during the 30-minute post-vaccination observation time. In one health facility, the evaluation team observed that health workers lacked awareness of AEFI crisis communication policies and procedures.
During the first vaccination campaign, 119 minor, one serious, and no severe AEFI cases were reported; during the second campaign, 83 minor, three serious, and no severe AEFI cases were reported. All reported serious AEFI cases were appropriately managed and patients recovered; among these, two were syncope, one was suspected anaphylaxis, and one was an anxiety-related reaction. A few health facilities reported very low or zero minor AEFIs.
4. Discussion
Sikkim state, in northeastern India, made a landmark decision to be the first state in India to introduce HPV vaccine statewide in 2018–2019, targeting multiple-age cohorts of girls to prevent cervical cancer [9]. Sikkim State successfully delivered two doses of the HPV vaccine to 9–13-year-old girls, primarily through school-based vaccination campaigns, achieving a high (>95%) two-dose coverage across the state in 2018–2019. Through a post-introduction evaluation involving interviewing key stakeholders at state, district, and local levels, we found that the successful first year of HPV vaccination in Sikkim State was largely attributed to strong political leadership and commitment, mandatory school enrollment policy for children <14 years of age, the exceptional collaboration between health and education sectors at all levels, ownership of the program by the education department, and robust advocacy and social mobilization strategies.
The HPV vaccination campaign in Sikkim witnessed strong leadership by the state political and public health leaders towards self-financing a lifesaving vaccine and strengthening its commitment towards the prevention of cervical cancer. The state’s chief minister has previously demonstrated commitment to public health initiatives well in advance of other states in India, largely following WHO recommendations and public health initiatives of high- and upper-middle-income countries. Joined by other state political leaders with support from the national government and based on recommendations from the independent advisory group of immunization experts in the state (STAG), the state’s chief minister prioritized HPV vaccine introduction for the state as part of its broader agenda for cervical cancer elimination, and the government allocated state budget for vaccine procurement and delivery.
Following government policy and vaccine procurement efforts, a strong partnership between the health and education sectors at all levels was critical for the successful planning and advocacy efforts. Intense mobilization efforts by health workers, teachers, and community leaders—driven by state government policy and commitment— ensured reaching a high two-dose HPV vaccine coverage. Sikkim’s mandatory school enrollment, the existing school health program, and prior precedence of vaccination in schools facilitated seamless implementation utilizing school-based vaccination campaigns.
Sikkim State employed widespread and comprehensive efforts for advocacy, communication, and social mobilization to build community awareness, ensure high visibility of the campaign, and build public confidence in the HPV vaccine. Sikkim prioritized early investments in building community demand for HPV vaccination, a critical driver for high vaccine uptake. The PIE did not directly measure literacy rates, although existing data indicate high levels of literacy in Sikkim State, including women [17].
Sikkim State plans to continue offering the HPV vaccine to nine-year-old girls by designating two months per year when the vaccine will be delivered in schools. The state government has allocated state budget funds to procure and deliver HPV vaccine for at least the next three years. Timely vaccine procurement, a continued partnership between health and education, refresher trainings for health workers and school personnel, and seamless community social mobilization will be critical for program sustainability and continued high HPV vaccine coverage. Operational guidelines for HPV vaccination should be modified to indicate the new routine single-age target group while eliminating missed opportunities for vaccination of girls <14 years old. Minor gaps observed in vaccine logistics, waste management, and AEFI knowledge should continue to be addressed via routine immunization trainings and supply management.
For secondary prevention of cervical cancer, Sikkim state intends to continue to strengthen the screening of women for cervical cancer, using an innovative total health checkup program—Comprehensive Annual and Total Checkup for Healthy Sikkim (CATCH) [18]. CATCH aims to provide comprehensive annual health checkups for all citizens while determining appropriate individual interventions, including the screening of all women >30 years old for cervical cancer using Visual Inspection with Acetic Acid (VIA). Any positive VIA case is referred for further management to appropriate tertiary health care hospitals, and cases of precancerous lesions are managed in the state referral hospitals, while invasive cervical cancer cases are referred to hospitals outside the state.
In December 2017, the Indian National Technical Advisory Group on Immunization (NTAGI)—an independent advisory group of experts on immunization advising India’s national immunization program—recommended the nationwide introduction of the HPV vaccine to address the high cervical cancer burden in India. Following NTAGI’s recommendations, the national government is considering this vaccine for their routine immunization program. Sikkim’s strong HPV vaccine introduction experience and ongoing program sustainability will be highly informative for the national program, as well as similar settings outside of India. Political commitment to allocate government funds is critical to self-finance this high-cost vaccine, as well as securing the necessary funds for vaccine delivery [19–21]. While Sikkim has secured state government funds to continue this program through 2021, discussions on future sustainability should remain active. As has been demonstrated in other low- and middle-income country settings, school-based vaccination for adolescent girls is effective in quickly achieving high HPV vaccine coverage in locations with high school enrollment and attendance [13,22–24]. Other states in India or similar countries could consider introducing the HPV vaccine through routine outreach; however, vaccinating girls in schools has been demonstrated repeatedly as an effective approach for reaching high vaccine coverage. Although costly and resource-intensive, the rigorous efforts for social mobilization and crisis communication planning in Sikkim were a critical investment for demand generation and enhancing the sustainability of HPV vaccination in Sikkim [25,26].
In settings with high cervical cancer burden and poor access to screening and treatment, HPV vaccine introduction offers the best, and sometimes the only opportunity to prevent disease. Sikkim has successfully introduced HPV vaccine statewide, demonstrating a model that could be replicated in other regions in India or similar low- and middle-income country settings.
5. Keypoints
This manuscript describes the decision-making process, implementation details and lessons learned from the first statewide multiple-age cohort HPV vaccine introduction in India in 2018–2019.
6. Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position, policies, or views of the U.S. Centers for Disease Control and Prevention or the World Health Organization.
Acknowledgments
Ministry of Health and Family Welfare, Government of India.
Government of Sikkim, Education Department.
Government of Sikkim, Immunization Program.
Dr Deviprasad, Dr Jayesh Mehta, Dr MujIb Sayyed, Dr S M Tripathi (WHO-India).
Mr Amandeep, Singh Global Health Strategies.
Dr Arindam Ray, Bill and Melinda Gates Foundation (BMGF).
Dr Kavitha Dhanasekaran, Dr Roopa Hariprasad, Indian Council of Medical Research (ICMR).
Dr Sumit Juneja, National Cold Chain and Vaccine Management Resource Centre (NCCVMRC).
National Institute of Health and Family Welfare (NIHFW).
Dr Maulik Shah, UNICEF.
Dr Ashish Srivastava, Ms Harki Tarnang (JHPIEGO).
Mr Jitendra Awale, CORE Group Polio Project.
This article was published as part of a supplement supported by Centers for Disease Control and Prevention Global Immunization Division. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or World Health Organization. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors.
Footnotes
CRediT authorship contribution statement
Danish Ahmed: Conceptualization, Methodology, Investigation, Project administration, Formal analysis, Writing - original draft, Writing - review & editing, Supervision, Data curation, Visualization. Kristin VanderEnde: Conceptualization, Methodology, Investigation, Project administration, Formal analysis, Writing - original draft, Writing - review & editing, Supervision, Data curation, Visualization. Pauline Harvey: Conceptualization, Writing - review & editing, Supervision. Pankaj Bhatnagar: Conceptualization, Writing - review & editing, Supervision. Nitasha Kaur: Conceptualization, Methodology, Investigation, Project administration, Formal analysis, Writing - original draft, Writing - review & editing, Supervision, Data curation, Visualization. Subhendu Roy: Conceptualization, Methodology, Investigation, Project administration, Formal analysis, Writing - original draft, Writing - review & editing, Supervision, Data curation, Visualization. Neelam Singh: Conceptualization, Methodology, Investigation, Project administration, Formal analysis, Writing - original draft, Writing - review & editing, Supervision, Data curation, Visualization. Phumzay Denzongpa: Conceptualization, Methodology, Investigation, Project administration, Formal analysis, Writing - original draft, Writing - review & editing, Supervision, Data curation, Visualization. Pradeep Haldar: Conceptualization, Writing - review & editing, Supervision. Anagha Loharikar: Conceptualization, Methodology, Investigation, Project administration, Formal analysis, Writing - original draft, Writing - review & editing, Supervision, Data curation, Visualization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Disclaimer
The authors alone are responsible for the views expressed in this article, which do not necessarily represent the views, decisions or policies of the institutions with which the authors are affiliated.
Data statement
I am not linking or uploading my research data, as this is public health observation data. Data can be made available upon request.
References
- [1].Globocan: Global Cancer Observatory India Fact Sheet. In: International Agency for Research on Cancer WHO, editor. Geneva, Switzerland: WHO; 2018. [Google Scholar]
- [2].Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- [3].Bobdey S, Sathwara J, Jain A, Balasubramaniam G. Burden of cervical cancer and role of screening in India. Ind J Med Paediatr Oncol : Off J Ind Soc Med Paediatr Oncol 2016;37(04):278–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].WHO position on HPV vaccines. Vaccine 2009;27:7236–7. [DOI] [PubMed] [Google Scholar]
- [5].Human papillomavirus vaccines. WHO position paper, May 2017-Recommendations. Vaccine 2017;35:5753–5. [DOI] [PubMed] [Google Scholar]
- [6].Guide to Introducing HPV Vaccine Into National Immunization Programmes. In: (WHO) WHO, editor. Geneva, Switzerland: WHO; 2016. [Google Scholar]
- [7].A Report on Cancer Burden in North Eastern States in India. In: Research NCfDIa, editor. Indian Council of Medical Research (ICMR), Bengaluru; 2017. [Google Scholar]
- [8].Chatterjee S, Chattopadhyay A, Samanta L, Panigrahi P. HPV and Cervical Cancer Epidemiology - Current Status of HPV Vaccination in India. Asian Pacific J Cancer Prevent : APJCP 2016;17:3663–73. [PubMed] [Google Scholar]
- [9].Sankaranarayanan R, Basu P, Kaur P, Bhaskar R, Singh GB, Denzongpa P, et al. Current status of human papillomavirus vaccination in India’s cervical cancer prevention efforts. Lancet Oncol 2019;20(11):e637–44. [DOI] [PubMed] [Google Scholar]
- [10].Dorji T, Tshomo U, Phuntsho S, Tamang TD, Tshokey T, Baussano I, et al. Introduction of a National HPV vaccination program into Bhutan. Vaccine 2015;33(31):3726–30. [DOI] [PubMed] [Google Scholar]
- [11].Principles and considerations for adding a vaccine to a national immunization programme: from decision to implementation and monitoring. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- [12].WHO. New Vaccine Post-Introduction Evaluation (PIE) Tool. Geneva, Switzerland: World Health Organization (WHO); 2010. [Google Scholar]
- [13].LaMontagne DS, Bloem PJN, Brotherton JML, Gallagher KE, Badiane O, Ndiaye C. Progress in HPV vaccination in low- and lower-middle-income countries. Int J Gynaecol Obstetr: Off Organ Int Federat Gynaecol Obstetr 2017;138(Suppl 1):7–14. [DOI] [PubMed] [Google Scholar]
- [14].Torres-Rueda S, Rulisa S, Burchett HED, Mivumbi NV, Mounier-Jack S. HPV vaccine introduction in Rwanda: Impacts on the broader health system. Sexual Reprod Healthcare : Off J Swedish Associat Midwives 2016;7:46–51. [DOI] [PubMed] [Google Scholar]
- [15].Research design: qualitative, quantitative and mixed methods approaches Research design: qualitative, quantitative and mixed methods approaches Creswell John W Sage 320 £29 0761924426 0761924426 [Formula: see text]. Nurse researcher. 2004;12:82–3. [DOI] [PubMed] [Google Scholar]
- [16].Human papillomavirus vaccines. WHO position paper, October 2014. Wkly Epidemiol Rec 2014;89:465–91. [PubMed] [Google Scholar]
- [17].Open Government Data Portal of Sikkim. In: Government S, editor.: Open Government Data Division of National Informatics Centre (NIC) Department of Electronics and Information Technology (DeitY), Government of India. [Google Scholar]
- [18].CATCH. In: Sikkim Go, editor.: Official Website of Government of Sikkim. [Google Scholar]
- [19].Levin A, Wang SA, Levin C, Tsu V, Hutubessy R. Costs of introducing and delivering HPV vaccines in low and lower middle income countries: inputs for GAVI policy on introduction grant support to countries. PloS one. 2014;9: e101114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hutubessy R, Levin A, Wang S, Morgan W, Ally M, John T, et al. A case study using the United Republic of Tanzania: costing nationwide HPV vaccine delivery using the WHO Cervical Cancer Prevention and Control Costing Tool. BMC Med 2012;10(1). 10.1186/1741-7015-10-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Levin CE, Van Minh H, Odaga J, Rout SS, Ngoc DNT, Menezes L, et al. Delivery cost of human papillomavirus vaccination of young adolescent girls in Peru, Uganda and Viet Nam. Bull World Health Organ 2013;91(8):585–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Gallagher KE, Howard N, Kabakama S, Mounier-Jack S, Griffiths UK, Feletto M, et al. Lessons learnt from human papillomavirus (HPV) vaccination in 45 low- and middle-income countries. PLoS One 2017;12(6):e0177773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Howard N, Gallagher KE, Mounier-Jack S, Burchett HED, Kabakama S, LaMontagne DS, et al. What works for human papillomavirus vaccine introduction in low and middle-income countries? Papillomavirus Res (Amsterdam, Netherlands: ). 2017;4:22–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].LaMontagne DS, Barge S, Le NT, Mugisha E, Penny M, Gandhi S, et al. Human papillomavirus vaccine delivery strategies that achieved high coverage in low- and middle-income countries. Bull World Health Organ 2011;89(11):821–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Foss HS, Oldervoll A, Fretheim A, Glenton C, Lewin S. Communication around HPV vaccination for adolescents in low- and middle-income countries: a systematic scoping overview of systematic reviews. Systemat Rev 2019;8:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Santhanes D, Wong CP, Yap YY, San SP, Chaiyakunapruk N, Khan TM. Factors involved in human papillomavirus (HPV) vaccine hesitancy among women in the South-East Asian Region (SEAR) and Western Pacific Region (WPR): A scoping review. Hum Vacc Immunother 2018;14(1):124–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
I am not linking or uploading my research data, as this is public health observation data. Data can be made available upon request.


