Abstract
Introduction
Cone beam computed tomography (CBCT) plays a significant role in studying the anatomical structures of the mandible.
Aim
This retrospective study aimed to assess the role of CBCT at the pre-assessment stage of mandibular surgery.
Materials and methods
A total of 250 CBCT images were collected. The inferior alveolar canal (IAC) and mental foramen (MF) were measured bilaterally to the mandibular teeth apexes, including molars, premolars, and canines, to the buccal, lingual cortical bone, and to the inferior border of the mandible.
Results
There were no differences in the average number of extracted teeth between the right and left sides (P-value > 0.05, median = three teeth). It was noticed that the average measures of each point of the IAC and MF on the right side were closely matched to the similar point on the left side (P-value > 0.05). T-tests showed that there were differences between males and females on the M2 and M3 on the right side (P-value < 0.05) and on the M1, M2, and M3 on the left side (P-value < 0.05). Using one-way ANOVA tests, results showed that there were some differences in measures at P0 (F = 3.376, P-value = 0.003), P4 (F = 3.782, P-value = 0.001) on the right side, and at P3 (F = 5.620, P-value = 0.019) on the left side of the mandible.
Conclusions
There were no significant differences in IAC and MF positions between the right and left sides. However, between males and females, MF measurements showed significant differences on some points on the right and left sides. Although the history of extracted teeth showed no statistically significant difference in the location of IAC and MF, the number of extracted teeth showed an effect in the IAC position on the right and left sides, but not with the MF.
Keywords: CBCT, Inferior alveolar canal, Mental foramen, Dental extraction, Dental implants, Oral surgery
1. Introduction
For many years, radiological assessment of surgical procedures in the maxilla or mandible has been routinely carried out by using plain film such as a panoramic radiograph (Mallya and Lam, 2018). However, it is worth mentioning that panoramic radiograph only gives a two-dimensional (2D) view of the teeth and their related vital structures, such as maxillary sinuses, mandibular canal, and alveolar bone (Mallya and Lam, 2018).
Additionally, a panoramic radiograph does not give accurate details of the root structures from all views; for example, internal or external resorption on the palatal aspect of the root; hence another technique is crucially needed (Marinescu et al., 2019).
Furthermore, a thorough assessment of the condition of the roots of adjacent teeth may not be achieved through intraoral radiographs, which have a limited field of view and only show the proximal outline of the roots, and may fail to show conditions such as root resorption taking place from the palatal aspect (Follin and Lindvall, 2005). Hence, it has been recommended to consider using an advanced radiographic technique such as cone beam computed tomography (CBCT).
There are various benefits of using CBCT when compared to a panoramic radiograph. For example, CBCT provides multiplane images of jaws (coronal, axial, and sagittal sections), and enables 3D construction, image manipulation using computer software, linear and angular measurement, and accurate tracing and highlighting of various mandibular anatomical structures. These advantages make CBCT the choice of radiographic technique for most dental specialists employing CBCT when they develop a treatment plan for patients who require surgical procedures in the oral and maxillofacial region (Mah and Hatcher, 2004).
Nerve injury resulting from dental extraction, placement of the dental implant, bilateral sagittal split osteotomy surgery, or genioplasty surgery are not uncommon (Morse, 1997). Unfortunately, the treatment of nerve injury in the jaw area is not always a straightforward task and is related to several factors, including age and gender, cause of injury, healing status, and medical history of the patient (Neal and Zuniga, 2022). Treatment of nerve injury is costly due to the time needed for long-term follow-up, the cost of medication, and the possibility of the need for further corrective surgery (Van der Cruyssen et al., 2022). Therefore, it is always crucial to consider all measures that help to prevent nerve injury prior to surgery involving the mandible and/or maxilla.
Utilising CBCT has been shown to reduce nerve injury significantly when compared to a panoramic radiograph (Renton, 2010). Furthermore, CBCT provides 3D views of the object when compared to other plain radiographs such as panoramic radiographs; hence it improves the quality of treatment. It has been reported that poor pre-dental surgery assessments increase the risk of inferior alveolar canal (IAC) and/or mental foramen (MF) injuries, which necessitates considering an advanced radiographic technique such as CBCT (Renton, 2010). Accordingly, this retrospective study aimed to assess the role of CBCT at the pre-assessment stage of mandibular surgery.
2. Materials and methods
2.1. Study design and setting
This was a five-year retrospective study (March 2016 to April 2020) of 2000 CBCTs for dental patients who received dental treatment at the Department of Oral and Maxillofacial Surgery at Riyadh Elm University (Riyadh, Saudi Arabia). CBCT assessed by a consultant oral and maxillofacial radiologist (RJ) and by a postgraduate resident of oral and maxillofacial surgery (JK) at Riyadh Elm University (Riyadh, Saudi Arabia).
2.2. Inclusion and exclusion criteria
CBCTs for all adult patients (male and female) aged eighteen years and older were included. Additionally, any CBCTs for patients with a previous neurosensory deficit due to trauma or pathology to the ramus area, or with a history of trigeminal neuralgia, were excluded. In addition, CBCTs for patients who had a history of major mandibular surgeries such as open reduction and fixation of the mandible were excluded. Moreover, CBCTs with technical errors or defects were excluded. For example, CBCTs that did not include the full body of the mandible or had scattered images due to prosthetic treatment (i.e. crown or prothesis) were excluded.
2.3. Variables and procedures
This retrospective study had five variables, and these were 1) age of the patients in years, 2) gender (male or female), 3) variation of the mandibular canal due to ageing, 4) history of mandibular teeth extraction, and lastly 5) the number of extracted teeth.
Patients’ demographic data (i.e. age, medical history, and gender) were retrieved from the patient’s medical records at Riyadh Elm University Dental Hospital (Riyadh, Saudi Arabia), while radiographic images were recruited from the Radiology Center at the Oral and Maxillofacial Department at Riyadh Elm University (Riyadh, Saudi Arabia). A written and verbal consent form was obtained from each patient before taking CBCT or starting dental treatment at the teaching hospital for research purposes.
2.4. Measures
All images were taken by the same CBCT machine and were obtained using recommended exposure and patient positioning protocols (85kVp, 5–7 mA, and 14 s) with a CBCT unit by Sirona Galileos, Germany. Images were viewed using digital image analysis software (Galaxis 3D imaging software version 1.9.4497.23802, 2006–2011 Sirona dental system), which allowed the measurement of the landmarks on 287 μm cuts. IAC and MF tracing were measured along the path tool, which uses multiple points in the Galaxis 3D imaging software. Multiple points in many directions on the tracing line of IAC from mandibular foramen to MF were measured by the measure tool in the Galaxis 3D imaging software in millimetres. All images were assessed by two assessors. For the sake of intra-observer reliability, all the measurements were done twice by the same assessor at different points in time and an average of these values was considered as the final measurement. The maximum duration for performing the repetition of measurements was one week for any given specific measurement.
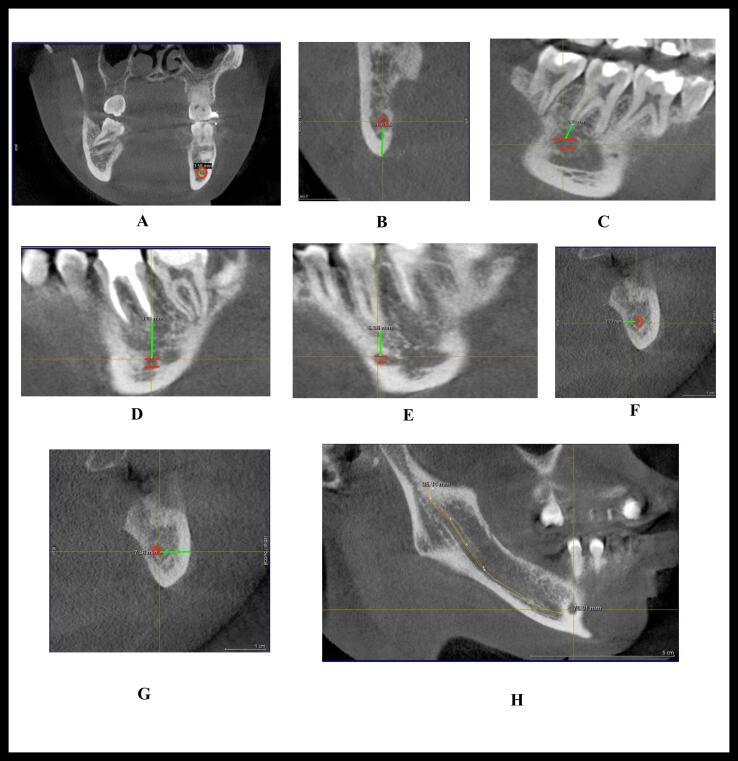
The points were measured as explained in Fig. 1, Fig. 2:
-
•
P0: Horizontal diameter of IAC on the halfway point of the tracing line of the IAC course “point on the half of total length of IAC” in cross-section view.
-
•
P1: Distance measured between the inferior border of IAC to the inferior border of the mandible on to the halfway point of the tracing line of the IAC “point on the half of total length of IAC” in cross-section view.
-
•
P2: Distance measured between the apex of the distal root of the second molar to the nearest point in the superior border of the IAC in cross-section view.
-
•
P3: Distance measured between the apex of the distal root of the first molar to the nearest point in the superior border of the IAC in sagittal view.
-
•
P4: Distance measured between the apex of the second premolar to the nearest point in the superior border of the IAC in sagittal view.
-
•
P5: Distance measured between the lingual cortical plate to the nearest point to the halfway point of the tracing line of the IAC course “point on the half of total length of IAC” in cross-section view.
-
•
P6: Distance measured between the buccal cortical plate to the nearest point to the halfway point of the tracing line of the IAC course “point on the half of total length of IAC” in cross-section view.
-
•
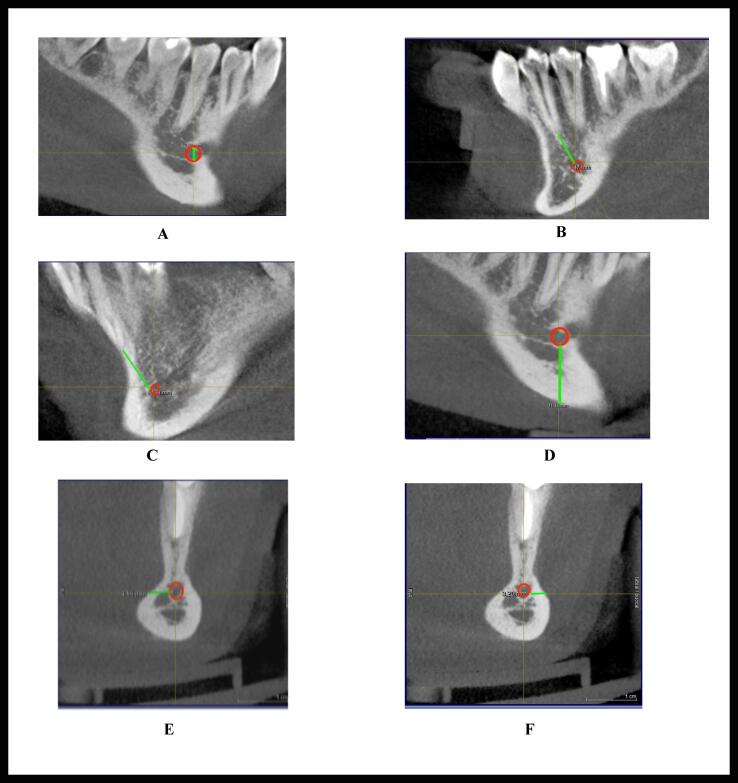
M0: Maximum vertical height of MF in sagittal view.
-
•
M1: Distance measured between the apex of the first premolar to the nearest point in the superior border of the MF in sagittal view.
-
•
M2: Distance measured between the apex of the canine to the nearest point in the superior border of the mental canal (MeC) in sagittal view.
-
•
M3: Distance measured between the inferior border of MF to the inferior border of the mandible in sagittal view.
-
•
M4: Distance measured between the lingual cortical plate to the nearest point in tracing line of MeC in cross-section view.
-
•
M5: Distance measured between the buccal cortical plate to the nearest point in the tracing line of MeC in cross-section view.
Fig. 1.
Measurements of inferior alveolar canal (IAC); A) P0, B) P1, C) P2, D) P3, E) P4, F) P5, G) P6, and H) Halfway of the tracing line of IAC.
Fig. 2.
Measurements of mental canal and foramen; A) M0, B) M1, C) M2, D) M3, E) M4, and F) M5.
2.5. Sample size calculation
The effect size of this study was calculated using the data from similar research by Aksoy et al. (2018). The G*Power sample size software version 3.1.9.4 was used to compute the sample size. The acceptable level of significance was set at 0.05, and the power of the study was set at 80%. With an effect size of 0.364, a minimum sample size per gender group (i.e. 94 females and 94 males) participants was estimated for this study. Therefore, the minimum overall sample size was 188 participants. However, our study sample size is 250 which is greater than the minimum sample size required (N = 188).
2.6. Statistical analysis
Simple descriptive statistics using percentages and frequencies were used. Means and standard deviations were used to describe averages of the continuous data (i.e. age, variation of the mandibular canal, and MF). Chi-squared tests and t-tests or one-way ANOVA tests were used to assess significant differences between subgroups for the categorical (i.e. gender, medical history, and history of teeth extraction (yes versus no)) and non-categorical (number of extracted teeth) variables, respectively. The statistical significance was assumed at a 5% level, and all the analyses were carried out using IBM SPSS® version 25.0.
3. Results
Table 1 presents the characteristics of the study’s sample. The average age of patients of these 250 CBCTs was 44.3 years old (SD = 14.11). The majority of these CBCTs belonged to female patients (58.8%) versus 41.2% male patients. Most of the CBCTs belonged to fit and healthy patients (86.8%), followed by diabetic patients (4.8%), hypertensive patients (2.4%), patients with a high cholesterol level (2.4%), both diabetic and hypertensive patients (2%), patients with chronic heart diseases (0.8%) or bronchial asthma (0.8%). Statistical analyses showed that there were no mandibular variations.
Table 1.
Sample characteristics.
| Variable |
Total |
|||
|---|---|---|---|---|
| N | % | |||
| Age (mean; years) | 44.3; SD = 14.11 | |||
| Gender | Male | 103 | 41.2 | |
| Female | 147 | 58.8 | ||
| Medical history | Medically free | 217 | 86.8 | |
| Diabetes mellitus | 12 | 4.8 | ||
| Hypertension | 6 | 2.4 | ||
| High cholesterol level | 6 | 2.4 | ||
| Diabetes and hypertension | 5 | 2.0 | ||
| Chronic heart disease | 2 | 0.8 | ||
| Bronchial asthma | 2 | 0.8 | ||
| Right | Variation of the mandibular canal | No | 250 | 100 |
| Variation of the mental foramen | No | 250 | 100 | |
| History of mandibular teeth extraction | Yes | 217 | 86.8 | |
| No | 33 | 13.2 | ||
| Number of extracted teeth (Median; number) | 3 | |||
| Left | Variation of the mandibular canal | No | 250 | 100 |
| Variation of the mental foramen | No | 250 | 100 | |
| History of mandibular teeth extraction | Yes | 221 | 88.4 | |
| No | 29 | 11.6 | ||
| Number of extracted teeth (Median; number) |
3 | |||
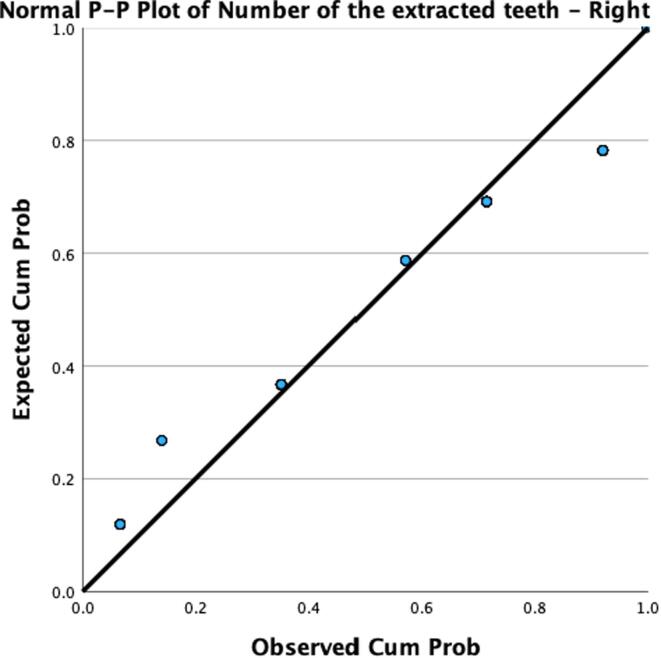
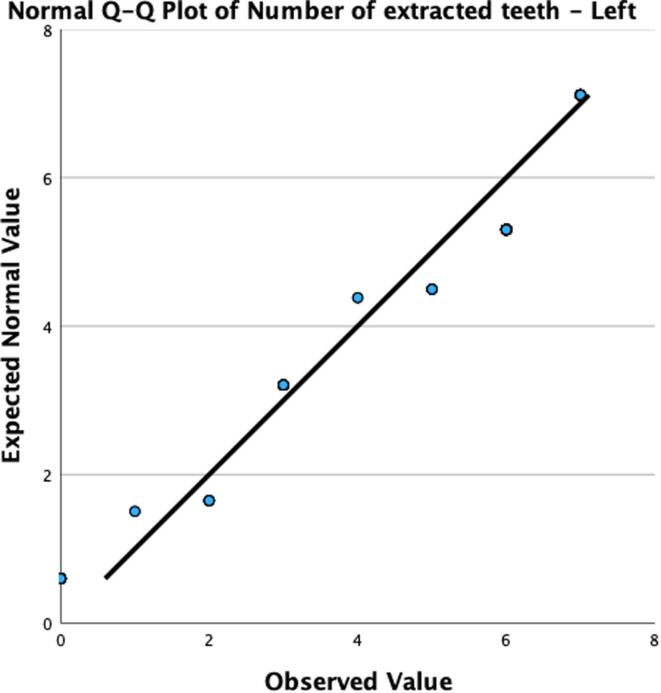
Besides, there was a history of dental extraction on the left side (88.4%) more than on the right side (86.8%). Statistical analyses showed there were no differences in the average number of extracted teeth between the right and left sides (P-value > 0.05, median = three teeth) – see Fig. 3a and 3b.
Fig. 3.
A: P-P plot of the number of the extracted teeth – right side. Fig. 3b: P-P plot of the number of the extracted teeth – left side.
Table 2 presents variations of the mandibular canal and MF on the right and left sides. It was noticed that the average measures of each point of the mandibular canal on the right side were closely matched to the similar point on the left side. For example, the average measure of P0 on the right side was 8.82 (SD = 4.2) compared to 8.78 (SD = 3.7) on the left side; P1 measure on the right side was 6.81 (SD = 2.1) compared to 7 (SD = 2.3) on the left side; P2 measure was 3.70 (SD = 3.0) compared to 3.82 (SD = 3.0); P3 measure on the right side was 4.81 (SD = 3.2) compared to 4.75 (SD = 3.2) on the left side; P4 measure on the right side was 4.20 (SD = 2.8) compared to 3.95 (SD = 2.9); P5 measure on the right side was 3.72 (SD = 1.1) compared to 3.82 (SD = 1.2) on the left side, and lastly P6 measure on the right side was 5.11 (SD = 1.5) compared to 4.8 (SD = 1.4). Similarly, it was noticed that the average measures of each point of the MF on the right side were equivalent to the similar point on the left side. For example, the M0 measure on the right side was 3.02 (SD = 0.8) compared to 3.09 (SD = 0.9) on the left side; M1 measure on the right side was 6.63 (SD = 2.7) compared to 6.55 (SD = 3.0) on the left side; M2 measure on the right side was 9.31 (SD = 3.2) compared to 9.06 (SD = 3.2) on the left side; M3 measure on the right side was 11.6 (SD = 3.9) compared to 11.84 (SD = 3.8) on the left side; M4 measure on the right side was 4.88 (SD = 1.7) compared to 4.96 (SD = 1.7) on the left side and lastly M5 measure on the right side was 2.92 (SD = 1.0) compared to 2.98 (SD = 0.9) on the left side. Statistical analyses using t-tests showed that there were no significant differences found between right and left-side measures (P-value > 0.05).
Table 2.
Variations of the mandibular canal and mental foramen on the right and left sides.
|
Variation of mandibular canal and mental foramen | ||
|---|---|---|
| Right | Left | |
| Mean; SD* | Mean; SD* | |
| P0 | 8.82; 4.2 | 8.78; 3.7 |
| P1 | 6.81; 2.1 | 7.00; 2.3 |
| P2 | 3.70; 3.0 | 3.82; 3.0 |
| P3 | 4.81; 3.2 | 4.75; 3.2 |
| P4 | 4.20; 2.8 | 3.95; 2.9 |
| P5 | 3.72; 1.1 | 3.82; 1.2 |
| P6 | 5.11; 1.5 | 4.80; 1.4 |
| M0 | 3.02; 0.8 | 3.09; 0.9 |
| M1 | 6.63; 2.7 | 6.55; 3.0 |
| M2 | 9.31; 3.2 | 9.06; 3.2 |
| M3 | 11.6; 3.9 | 11.84; 3.8 |
| M4 | 4.88; 1.7 | 4.96; 1.7 |
| M5 | 2.92; 1.0 | 2.98; 0.9 |
*No significant differences were found between right and left side measures (P-value > 0.05).
Table 3 presents the impact of gender on the variations of the mandibular canal and MF. T-tests showed that there were differences between males and females on the M2 (M2 measures were 9.26 (SD = 3.5) versus 9.35 (SD = 2.9), P-value = 0.047, respectively) and M3 (M3 measures were 11.56 (SD = 4.5) versus 11.70 (SD = 3.5), P-value = 0.001, respectively) on the right side. Similarly, using t-tests, results showed that there were differences between males and females on the M1 (M1 measures were 6.88 (SD = 3.4) versus 6.31 (SD = 2.7), P-value = 0.003, respectively), M2 (M2 measures were 9.25 (SD = 3.5) versus 8.92 (SD = 3.0), P-value = 0.017, respectively), and M3 (M3 measures were 12.05 (SD = 4.2) versus 11.70 (SD = 3.4), P-value = 0.048, respectively) on the left side.
Table 3.
Impact of gender on the variations of the mandibular canal and the mental foramen.
|
Right |
Left |
||||||
|---|---|---|---|---|---|---|---|
| Male mm | Female mm | P-value* | Male mm | Female mm | P-value | ||
| Variation of the mandibular canal and mental foramen | P0 | 9.85; 4.2 | 8.09; 4.1 | 0.100 | 9.09; 3.8 | 8.57; 3.6 | 0.469 |
| P1 | 6.66; 2.2 | 6.92; 2.0 | 0.136 | 7.07; 2.5 | 6.95; 2.2 | 0.495 | |
| P2 | 4.41; 3.1 | 3.20; 2.7 | 0.098 | 4.55; 3.0 | 3.31; 2.8 | 0.495 | |
| P3 | 5.39; 3.3 | 4.40; 3.2 | 0.522 | 5.36; 3.1 | 4.32; 3.2 | 0.993 | |
| P4 | 4.67; 3.0 | 3.87; 2.6 | 0.309 | 4.35; 2.9 | 3.67; 2.7 | 0.945 | |
| P5 | 3.43; 0.9 | 3.93; 1.2 | 0.104 | 3.69; 1.1 | 3.91; 1.2 | 0.274 | |
| P6 | 4.84; 1.5 | 5.30; 1.4 | 0.413 | 4.72; 1.5 | 4.85; 1.3 | 0.476 | |
| M0 | 3.18; 0.8 | 2.92; 0.8 | 0.600 | 3.31; 0.9 | 2.94; 0.8 | 0.293 | |
| M1 | 7.16; 2.9 | 6.26; 2.5 | 0.072 | 6.88; 3.4 | 6.31; 2.7 | 0.003* | |
| M2 | 9.26; 3.5 | 9.35; 2.9 | 0.047 | 9.25; 3.5 | 8.92; 3.0 | 0.017* | |
| M3 | 11.56; 4.5 | 11.70; 3.5 | 0.001 | 12.05; 4.2 | 11.70; 3.4 | 0.048* | |
| M4 | 4.85; 1.6 | 4.90; 1.7 | 0.734 | 4.88; 1.7 | 5.02; 1.7 | 0.936 | |
| M5 | 3.06; 1.1 | 2.81; 0.9 | 0.460 | 3.11; 0.9 | 2.89; 1.0 | 0.283 | |
*T-test (P-value < 0.05).
Table 4 presents the impact of the history of dental extraction on the variations of the mandibular canal and mental foramen. Using t-tests, results showed that there were no significant differences between the right and left sides of the mandible after the history of dental extractions (P-value > 0.05). All measures almost had similar margins.
Table 4.
Impact of a history of dental extraction on the variations of the mandibular canal and the mental foramen.
|
Right |
Left |
||||||
|---|---|---|---|---|---|---|---|
| Dental extraction | No dental extraction | P-value* | Dentalextraction | No dental extraction | P-value* | ||
| Variation of mandibular canal and mental foramen | P0 | 8.82; 4.3 | 8.79; 3.9 | 0.324 | 8.73; 3.7 | 9.15; 3.7 | 0.989 |
| P1 | 6.85; 2.1 | 6.53; 2.4 | 0.304 | 7.04; 2.4 | 6.70; 2.1 | 0.291 | |
| P2 | 3.66; 3.0 | 3.97; 2.8 | 0.761 | 3.76; 3.0 | 4.27; 2.6 | 0.517 | |
| P3 | 4.70; 3.2 | 5.56; 3.2 | 0.742 | 4.58; 3.2 | 6.07; 3.3 | 0.746 | |
| P4 | 4.08; 2.8 | 4.98; 2.8 | 0.357 | 3.85; 2.9 | 4.71; 2.2 | 0.372 | |
| P5 | 3.81; 1.1 | 3.16; 1.1 | 0.546 | 3.83; 1.2 | 3.72; 0.8 | 0.079 | |
| P6 | 5.12; 1.5 | 5.06; 1.4 | 0.964 | 4.76; 1.4 | 5.06; 1.6 | 0.126 | |
| M0 | 3.02; 0.8 | 3.07; 0.9 | 0.128 | 3.09; 0.9 | 3.16; 0.8 | 0.511 | |
| M1 | 6.61; 2.5 | 6.78; 3.4 | 0.260 | 6.48; 2.9 | 7.02; 3.5 | 0.470 | |
| M2 | 9.25; 3.2 | 9.77; 3.3 | 0.677 | 9.02; 3.2 | 9.37; 3.6 | 0.313 | |
| M3 | 11.70; 3.9 | 11.29; 4.3 | 0.581 | 11.82; 3.7 | 12.03; 4.1 | 0.844 | |
| M4 | 4.85; 1.7 | 5.10; 1.7 | 0.915 | 4.91; 1.7 | 5.36; 1.7 | 0.822 | |
| M5 | 2.91; 0.9 | 2.95; 1.5 | 0.094 | 2.97; 1.0 | 3.08; 0.9 | 0.765 | |
*T-test (P-value < 0.05).
Table 5 shows the impact of the number of extracted teeth on the variations of the mandibular canal and MF. Using one-way ANOVA tests, results showed that there were some differences in measures between the right and left sides of the mandible on the number of extracted teeth. For example, results showed that there were differences on the right side of the mandible at P0 (F = 3.376, P-value = 0.003), and P4 (F = 3.782, P-value = 0.001). While on the left side of the mandible, results showed that there was a difference on the left side of the mandible in only one measure. Using a one-way ANOVA test, results showed that there was a difference on the left side at the P3 measure (F = 5.620, P-value = 0.019).
Table 5.
Impact of the number of extracted teeth on the variations of the mandibular canal and the mental foramen.
|
Right |
Left |
||||
|---|---|---|---|---|---|
|
F mm |
P-value* |
F mm |
P-value* | ||
| Variation of mandibular canal and mental foramen | P0 | 3.376 | 0.003 | 0.314 | 0.576 |
| P1 | 0.723 | 0.631 | 0.534 | 0.466 | |
| P2 | 1.561 | 0.159 | 0.682 | 0.410 | |
| P3 | 2.121 | 0.052 | 5.620 | 0.019 | |
| P4 | 3.782 | 0.001 | 2.300 | 0.131 | |
| P5 | 1.708 | 0.120 | 0.235 | 0.628 | |
| P6 | 0.295 | 0.939 | 1.143 | 0.286 | |
| M0 | 1.503 | 0.178 | 0.155 | 0.694 | |
| M1 | 0.893 | 0.501 | 0.806 | 0.370 | |
| M2 | 1.457 | 0.194 | 0.293 | 0.588 | |
| M3 | 1.306 | 0.255 | 0.083 | 0.774 | |
| M4 | 1.499 | 0.179 | 1.761 | 0.186 | |
| M5 | 0.473 | 0.828 | 0.304 | 0.582 | |
*One-way ANOVA test (P-value < 0.05).
4. Discussion
This retrospective study aimed to track and assess IAC and MF positions in CBCTs in multiple locations. This would provide valuable information for any dental specialists who employ CBCT in their surgical procedures. The study has shown a significant difference in some locations of IAC and MF between males and females bilaterally. In addition, bony changes due to teeth extraction have an impact on IAC width.
4.1. IAC measures
In our study, the diameter of IAC on the halfway point of the tracing line of the canal (P0) was 8.82 mm and 8.78 mm on the right and left sides, respectively. This outcome was different from Gerlach et al.’s study, which showed the mean of the maximum diameter of MC at 3.19 mm (Gerlach et al., 2014). In addition, Komal et al.’s study showed a different diameter of MC than the present study. The MC diameter in Komal et al. was 2.326 mm and 2.28 mm on the right and left side, respectively (Komal et al., 2020). The differences in measurement were due to huge variations in sample size and the difference in population among studies.
A different measurement was the vertical diameter of IAC to the inferior border of the mandible (P1). Our study showed a 6.81 mm and 7.00 mm mean distance on the right and left sides, respectively. Ahmed et al. (2021) reported that the mean of the vertical diameter from the inferior border of the mandible to IAC was 6.71 mm. On the other hand, Saeed et al. (2022) showed the mean vertical distance of IAC to the inferior border of the mandible was 8.32 mm, which was different from our outcome. The differences were because of the difference in sample size and population.
Furthermore, our study showed the vertical distances of the superior border of IAC to the apex of the distal root of the second molar (P2) on the right and left sides were 3.70 mm and 3.83 mm, respectively. This outcome was comparable to Bürklein et al.'s (2015) study which showed that the vertical distances to the second molars on the right and left sides were 2.7 mm and 2.9 mm, respectively. In addition, there was a comparable outcome with Aksoy et al. (2018), who showed that the mean distance was 4.2 mm on both sides.
On the other hand, the distance of IAC to the apex of the distal root of the first molar (P3) in this study was 4.81 mm and 4.75 mm on the right and left sides, respectively. Our findings were similar to Aksoy et al., whose study showed the same distance (5.6 ± 2.81 mm) bilaterally (Aksoy et al., 2018), and was also similar to Aljarbou et al. (2019), who found the distance was 4.28 ± 2.12 mm.
In our study, P4, the distance of IAC to the apex of the second premolar on the right and left sides was 4.20 mm and 3.95 mm, respectively. This result was similar to Bürklein et al. (2015), who showed the vertical distances were 4.2 ± 2.4 mm and 4.3 ± 2.3 mm on the right and left sides, respectively. Also, this was in agreement with Aksoy et al. (2018), who showed that the distances were 5.19 ± 2.9 mm and 5.26 ± 2.85 mm on the right and left sides, respectively.
The distance of IAC to the lingual cortical plate (P5) was 3.72 mm, and 3.82 mm on the right and left sides, respectively. These results were comparable to Komal et al.'s (2020) study, which found the distance was 4.6 mm bilaterally. This was also like Sghaireen et al.'s (2020) study with distances of 3.83 ± 1.14 mm and 3.73 ± 1.14 mm, respectively. In addition, the distance of IAC to the buccal cortical plate in this study on the right and left sides were 5.11 mm and 4.80 mm, respectively. Komal et al. (2020) had a comparable outcome with 5.33 mm on the left side and 5.02 mm on the right side. Also, Sghaireen et al. (2020) found almost similar outcomes, where the distances were 5.17 ± 1.26 mm and 5.12 ± 1.32 mm on the right and left sides, respectively.
4.2. MF measures
The present study showed that the means of the MF vertical height (M0) diameter were 3.02 mm and 3.09 mm on the right and left sides, respectively. This outcome was in agreement with Sheikhi et al. (2015), who had a similar outcome in that the MF mean diameter was 3.59 mm bilaterally. Also, Nimigean et al. (2022) had a similar outcome, with their study concluding that the means of the diameters were 3.3 mm and 3.14 mm on the right and left sides, respectively.
The present study measured the distance from the first premolar apex to the MF (M1) bilaterally on the CBCT. The outcomes were 6.63 mm and 6.55 mm on the right and left sides, respectively. Aksoy et al. (2018) had a comparable distance on their retrospective study (5.76 ± 2.77 mm, 5.74 ± 2.88 mm) on the right and left sides, respectively. On the other hand, Komal et al. (2020) had different results from our study, with 2.4 mm and 2.8 mm on the right and left sides, respectively.
In the current study, one of the strongest points was the distance of the apex of the canine to the anterior loop of the MF (M2). To the author's knowledge, this measurement was not reported in the literature previously. Our study concludes that the distances on the right and left sides were 9.31 mm and 9.06 mm, respectively.
It is crucial to assess distance between the distance of the apex of the canine to the anterior loop of the MF as the nerve in this area is at risk of injury during genioplasty surgery. In a different measurement, the MF distances to the inferior border of the mandible (M3) in our study were 11.63 mm and 11.84 mm on the right and left sides, respectively. Mashyakhy et al. (2021) had slightly larger distances than ours. Their study concluded that the distances of MF to the mandible borders on the right and left sides were 14.09 ± 1.63 mm and 13,97 ± 1.53 mm, respectively. Nimigean et al. (2022) had a similar outcome to ours, with 10.36 mm on the right side, and 10.17 mm on the left side.
For the distance between the MeC and lingual cortical plate (M4), our study showed the mean distances were 4.88 mm and 4.96 mm on the right and left sides, respectively. This outcome was similar to Parnia et al. (2012) who concluded the distances to the lingual plate were 5.2 mm and 4.8 mm on the right and left sides.
To the author's knowledge, the distance between the MeC and buccal cortical plate (M5) was not reported in the literature. It is crucial to assess the distance between MeC and the buccal cortical plate, as the nerve in this area is at risk of injury during bilateral sagittal split osteotomy surgery.
4.3. Limitations of the study
Patients' ethnicity was not included in this study as a variable, and this is crucial to expand the findings. This study was conducted in a single centre; hence this is considered as a limitation to this study. In our study, many samples had multiple partially edentulous areas, and this would have probably influenced the results of our study since our study had included the measurements of IAC in the midpoint of the length of the canal. The findings of the study related to IAC are inapplicable to the third molar region.
5. Conclusions
There were no significant differences in IAC and MF positions between the right and left sides. Besides, between males and females, MF measurements showed significant differences on only certain points on the right side (M2, M3) and left (M1, M2, M3), but showed no differences on IAC measurement. Although the history of extracted teeth showed no statistically significant difference in the location of IAC and MF, the number of extracted teeth showed a significant effect in the IAC position on the right (P0, P4) and left (P3) sides. On the other hand, the number of extracted teeth showed no differences in the measurement of MF.
6. Future study
In view of the limitations of the present study, we suggest that future studies should collect the samples from multiple centres so that the results obtained can be more generalisable and consider an equal sample size between partially edentulous samples and fully dentate samples. Lastly, consider the inclusion of the “position of IAC” as one of the parameters, in the third molar region.
Ethical statement
Ethical approval was obtained from Riyadh Elm University Biomedical Ethics Committee (Approval Number: FPGRP/2021/620/541/60).
Funding
Ministry of Health (Approval Number: 1441-1780715).
CRediT authorship contribution statement
Jamal Kensara: Conceptualization, Methodology, Data curation, Writing – original draft, Visualization, Investigation, Validation, Writing – review & editing. Raviraj Jayam: Methodology, Visualization, Investigation, Validation, Writing – review & editing. Meshal Almanea: Data curation, Writing – review & editing. Muslat A Bin Rubaia'an: Data curation, Writing – review & editing. Njood Alshareef: Data curation, Writing – review & editing. Hassan Abed: Methodology, Visualization, Investigation, Validation, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Jamal Kensara, Email: jkensara@moh.gov.sa.
Hassan Abed, Email: hhabed@uqu.edu.sa.
References
- Ahmed A.A., Ahmed R.M., Jamleh A., Spagnuolo G. Morphometric analysis of the mandibular canal, anterior loop, and mental foramen: a cone-beam computed tomography evaluation. Int. J. Environ. Res. Public Health. 2021;18:3365. doi: 10.3390/ijerph18073365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aksoy U., Aksoy S., Orhan K. A cone-beam computed tomography study of the anatomical relationships between mandibular teeth and the mandibular canal, with a review of the current literature. Microsc. Res. Tech. 2018;81:308–314. doi: 10.1002/jemt.22980. [DOI] [PubMed] [Google Scholar]
- Aljarbou F.A., Aldosimani M., Althumairy R.I., Alhezam A.A., Aldawsari A.I. An analysis of the first and second mandibular molar roots proximity to the inferior alveolar canal and cortical plates using cone beam computed tomography among the Saudi population. Saudi Med. J. 2019;40:189–194. doi: 10.15537/smj.2019.2.23602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bürklein S., Grund C., Schäfer E. Relationship between root apices and the mandibular canal: a cone-beam computed tomographic analysis in a German population. J. Endod. 2015;41:1696–1700. doi: 10.1016/j.joen.2015.06.016. [DOI] [PubMed] [Google Scholar]
- Follin M.E., Lindvall A.-M. Detection of lingual root resorptions in the intraoral radiographs. An experimental study. Swed. Dental J. 2005;29:35–42. [PubMed] [Google Scholar]
- Gerlach N.L., Ghaeminia H., Bronkhorst E.M., Bergé S.J., Meijer G.J., Maal T.J.J. Accuracy of assessing the mandibular canal on cone-beam computed tomography: a validation study. J. Oral Maxillofac. Surg. 2014;72:666–671. doi: 10.1016/j.joms.2013.09.030. [DOI] [PubMed] [Google Scholar]
- Komal A., Bedi R.S., Wadhwani P., Aurora J.K., Chauhan H. Study of normal anatomy of mandibular canal and its variations in Indian population using CBCT. J. Maxillofacial Oral Surg. 2020;19:98–105. doi: 10.1007/s12663-019-01224-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mah J., Hatcher D. Three-dimensional craniofacial imaging. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2004;126:308–309. doi: 10.1016/j.ajodo.2004.06.024. [DOI] [PubMed] [Google Scholar]
- Mallya S., Lam E. Elsevier Health Sciences; 2018. White and Pharoah's Oral Radiology: Principles and Interpretation. [Google Scholar]
- Marinescu I.R., Bănică A.C., Mercuţ V., Gheorghe A.G., Drăghici E.C., Cojocaru M.O., Scrieciu M., Popescu S.M. Root resorption diagnostic: role of digital panoramic radiography. Curr. Health Sci. J. 2019;45:156. doi: 10.12865/CHSJ.45.02.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mashyakhy M., Mostafa A., Abeery A., Sairafi Z., Hakami N., Alroomy R., Chohan H., Abu-Melha A. Structural Features of the mental foramen in a Saudi subpopulation: a retrospective CBCT study. Biomed Res. Int. 2021;2021:1138675. doi: 10.1155/2021/1138675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse D.R. Infection-related mental and inferior alveolar nerve paresthesia: literature review and presentation of two cases. J. Endod. 1997;23:457–460. doi: 10.1016/S0099-2399(97)80303-2. [DOI] [PubMed] [Google Scholar]
- Neal T.W., Zuniga J.R. Post-traumatic trigeminal neuropathic pain: factors affecting surgical treatment outcomes. Front. Oral Health. 2022;3 doi: 10.3389/froh.2022.904785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimigean V., Gherghiţă O.R., Păun D.L., Bordea E.N., Pellegrini A., Cismaş S.C., Nimigean V.R., Motaş N. Morphometric study for the localization of the mental foramen in relation to the vertical reference plane. Rom. J. Morphol. Embryol. 2022;63:161–168. doi: 10.47162/RJME.63.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parnia F., Moslehifard E., Hafezeqoran A., Mahboub F., Mojaver-Kahnamoui H. Characteristics of anatomical landmarks in the mandibular interforaminal region: a cone-beam computed tomography study. Med. Oral Patol. Oral Cir. Bucal. 2012;17:e420–e425. doi: 10.4317/medoral.17520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renton T. Prevention of iatrogenic inferior alveolar nerve injuries in relation to dental procedures. Dent. Update. 2010;37:350–363. doi: 10.12968/denu.2010.37.6.350. [DOI] [PubMed] [Google Scholar]
- Saeed T.-A., Alansy A.-S., Abdu Z.-A., Almaqtari O., Yu Z. Dentulous versus edentulous mandibles: CBCT-based morphometric assessment of mandibular canal and alveolar bone. J Clin Exp Dent. 2022;14:e986. doi: 10.4317/jced.59033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sghaireen M.G., Srivastava K.C., Shrivastava D., Ganji K.K., Patil S.R., Abuonq A., Mousa M.A., Dar-Odeh N., Sghaireen G.M., Kamal M.A. A CBCT based three-dimensional assessment of mandibular posterior region for evaluating the possibility of bypassing the inferior alveolar nerve while placing dental implants. Diagnostics. 2020;10:406. doi: 10.3390/diagnostics10060406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikhi M., Karbasi Kheir M., Hekmatian E. Cone-beam computed tomography evaluation of mental foramen variations: a preliminary study. Radiol. Res. Pract. 2015;2015 doi: 10.1155/2015/124635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Cruyssen F., Nys M., Renton T., Vandeleene G., Callens M., Vanhaecht K., Jacobs R., Politis C., Luyten J. Healthcare costs of post-traumatic trigeminal neuropathy in Belgium-A retrospective analysis. J. Cranio-Maxillofac. Surg. 2022;50:627–636. doi: 10.1016/j.jcms.2022.07.002. [DOI] [PubMed] [Google Scholar]